AGENCY:
Centers for Medicare & Medicaid Services (CMS), HHS.
ACTION:
Final rule.
SUMMARY:
We are revising the Medicare hospital inpatient prospective payment systems (IPPS) for operating and capital-related costs of acute care hospitals to implement changes arising from our continuing experience with these systems for FY 2020 and to implement certain recent legislation. We also are making changes relating to Medicare graduate medical education (GME) for teaching hospitals and payments to critical access hospital (CAHs). In addition, we are providing the market basket update that will apply to the rate-of-increase limits for certain hospitals excluded from the IPPS that are paid on a reasonable cost basis, subject to these limits for FY 2020. We are updating the payment policies and the annual payment rates for the Medicare prospective payment system (PPS) for inpatient hospital services provided by long-term care hospitals (LTCHs) for FY 2020. In this FY 2020 IPPS/LTCH PPS final rule, we are addressing wage index disparities impacting low wage index hospitals; providing for an alternative IPPS new technology add-on payment pathway for certain transformative new devices and qualified infectious disease products; and revising the calculation of the IPPS new technology add-on payment. In addition, we are revising and clarifying our policies related to the substantial clinical improvement criterion used for evaluating applications for the new technology add-on payment under the IPPS.
We are establishing new requirements or revising existing requirements for quality reporting by specific Medicare providers (acute care hospitals, PPS-exempt cancer hospitals, and LTCHs). We also are establishing new requirements and revising existing requirements for eligible hospitals and critical access hospitals (CAHs) participating in the Medicare and Medicaid Promoting Interoperability Programs. We are updating policies for the Hospital Value-Based Purchasing (VBP) Program, the Hospital Readmissions Reduction Program, and the Hospital-Acquired Condition (HAC) Reduction Program.
DATES:
This final rule is effective October 1, 2019.
FOR FURTHER INFORMATION CONTACT:
Donald Thompson, (410) 786-4487, and Michele Hudson, (410) 786-4487, Operating Prospective Payment, MS-DRGs, Wage Index, New Medical Service and Technology Add-On Payments, Hospital Geographic Reclassifications, Graduate Medical Education, Capital Prospective Payment, Excluded Hospitals, Medicare Disproportionate Share Hospital (DSH) Payment Adjustment, Medicare-Dependent Small Rural Hospital (MDH) Program, Low-Volume Hospital Payment Adjustment, and Critical Access Hospital (CAH) Issues.
Michele Hudson, (410) 786-4487, Mark Luxton, (410) 786-4530, and Emily Lipkin, (410) 786-3633, Long-Term Care Hospital Prospective Payment System and MS-LTC-DRG Relative Weights Issues.
Siddhartha Mazumdar, (410) 786-6673, Rural Community Hospital Demonstration Program Issues.
Jeris Smith, (410) 786-0110, Frontier Community Health Integration Project Demonstration Issues.
Erin Patton, (410) 786-2437, Hospital Readmissions Reduction Program Administration Issues.
Lein Han, 410-786-0205, Hospital Readmissions Reduction Program—Measures Issues.
Michael Brea, (410) 786-4961, Hospital-Acquired Condition Reduction Program Issues.
Annese Abdullah-Mclaughlin, (410) 786-2995, Hospital-Acquired Condition Reduction Program—Measures Issues.
Grace Snyder, (410) 786-0700 and James Poyer, (410) 786-2261, Hospital Inpatient Quality Reporting and Hospital Value-Based Purchasing—Program Administration, Validation, and Reconsideration Issues.
Cindy Tourison, (410) 786-1093, Hospital Inpatient Quality Reporting and Hospital Value-Based Purchasing—Measures Issues Except Hospital Consumer Assessment of Healthcare Providers and Systems Issues.
Elizabeth Goldstein, (410) 786-6665, Hospital Inpatient Quality Reporting and Hospital Value-Based Purchasing—Hospital Consumer Assessment of Healthcare Providers and Systems Measures Issues.
Nekeshia McInnis, (410) 786-4486 and Ronique Evans, (410) 786-1000, PPS-Exempt Cancer Hospital Quality Reporting Issues.
Mary Pratt, (410) 786-6867, Long-Term Care Hospital Quality Data Reporting Issues.
Elizabeth Holland, (410) 786-1309, Dylan Podson (410) 786-5031, and Bryan Rossi (410) 786-065l, Promoting Interoperability Programs.
Benjamin Moll, (410) 786-4390, Provider Reimbursement Review Board Appeals Issues.
SUPPLEMENTARY INFORMATION:
Tables Available Through the Internet on the CMS Website
In the past, a majority of the tables referred to throughout this preamble and in the Addendum to the proposed rule and the final rule were published in the Federal Register, as part of the annual proposed and final rules. However, beginning in FY 2012, the majority of the IPPS tables and LTCH PPS tables are no longer published in the Federal Register. Instead, these tables, generally, will be available only through the internet. The IPPS tables for this FY 2020 final rule are available through the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. Click on the link on the left side of the screen titled, “FY 2020 IPPS Final Rule Home Page” or “Acute Inpatient—Files for Download.” The LTCH PPS tables for this FY 2020 final rule are available through the internet on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/LongTermCareHospitalPPS/index.html under the list item for Regulation Number CMS-1716-F. For further details on the contents of the tables referenced in this final rule, we refer readers to section VI. of the Addendum to this FY 2020 IPPS/LTCH PPS final rule.
Readers who experience any problems accessing any of the tables that are posted on the CMS websites, as previously identified, should contact Michael Treitel at (410) 786-4552.
Table of Contents
I. Executive Summary and Background
A. Executive Summary
B. Background Summary
C. Summary of Provisions of Recent Legislation Implemented in This Final Rule
D. Issuance of Notice of Proposed Rulemaking
E. Advancing Health Information Exchange
II. Changes to Medicare Severity Diagnosis-Related Group (MS-DRG) Classifications and Relative Weights
A. Background
B. MS-DRG Reclassifications
C. Adoption of the MS-DRGs in FY 2008
D. FY 2020 MS-DRG Documentation and Coding Adjustment
E. Refinement of the MS-DRG Relative Weight Calculation
F. Changes to Specific MS-DRG Classifications
G. Recalibration of the FY 2020 MS-DRG Relative Weights
H. Add-On Payments for New Services and Technologies for FY 2020
III. Changes to the Hospital Wage Index for Acute Care Hospitals
A. Background
B. Worksheet S-3 Wage Data for the FY 2020 Wage Index
C. Verification of Worksheet S-3 Wage Data
D. Method for Computing the FY 2020 Unadjusted Wage Index
E. Occupational Mix Adjustment to the FY 2020 Wage Index
F. Analysis and Implementation of the Occupational Mix Adjustment and the Final FY 2020 Occupational Mix Adjusted Wage Index
G. Application of the Rural Floor, Expired Imputed Floor Policy, and Application of the State Frontier Floor
H. FY 2020 Wage Index Tables
I. Revisions to the Wage Index Based on Hospital Redesignations and Reclassifications
J. Out-Migration Adjustment Based on Commuting Patterns of Hospital Employees
K. Reclassification From Urban to Rural Under Section 1886(d)(8)(E) of the Act Implemented at 42 CFR 412.103
L. Process for Requests for Wage Index Data Corrections
M. Labor-Related Share for the FY 2020 Wage Index
N. Final Policies To Address Wage Index Disparities Between High and Low Wage Index Hospitals
IV. Other Decisions and Changes to the IPPS for Operating Costs
A. Changes to MS-DRGs Subject to Postacute Care Transfer and MS-DRG Special Payment Policies
B. Changes in the Inpatient Hospital Updates for FY 2020 (§ 412.64(d))
C. Rural Referral Centers (RRCs) Annual Updates to Case-Mix Index and Discharge Criteria (§ 412.96)
D. Payment Adjustment for Low-Volume Hospitals (§ 412.101)
E. Indirect Medical Education (IME) Payment Adjustment (§ 412.105)
F. Payment Adjustment for Medicare Disproportionate Share Hospitals (DSHs) for FY 2020 (§ 412.106)
G. Hospital Readmissions Reduction Program: Updates and Changes (§§ 412.150 Through 412.154)
H. Hospital Value-Based Purchasing (VBP) Program: Policy Changes
I. Hospital-Acquired Condition (HAC) Reduction Program
J. Payments for Indirect and Direct Graduate Medical Education Costs (§§ 412.105 and 413.75 Through 413.83)
K. Rural Community Hospital Demonstration Program
V. Changes to the IPPS for Capital-Related Costs
A. Overview
B. Additional Provisions
C. Annual Update for FY 2020
VI. Changes for Hospitals Excluded From the IPPS
A. Rate-of-Increase in Payments to Excluded Hospitals for FY 2020
B. Methodologies and Requirements for TEFRA Adjustments to Rate-of-Increase Ceiling
C. Critical Access Hospitals (CAHs)
VII. Changes to the Long-Term Care Hospital Prospective Payment System (LTCH PPS) for FY 2020
A. Background of the LTCH PPS
B. Medicare Severity Long-Term Care Diagnosis-Related Group (MS-LTC-DRG) Classifications and Relative Weights for FY 2020
C. Payment Adjustment for LTCH Discharges That Do Not Meet the Applicable Discharge Payment Percentage
D. Changes to the LTCH PPS Payment Rates and Other Changes to the LTCH PPS for FY 2020
VIII. Quality Data Reporting Requirements for Specific Providers and Suppliers
A. Hospital Inpatient Quality Reporting (IQR) Program
B. PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program
C. Long-Term Care Hospital Quality Reporting Program (LTCH QRP)
D. Changes to the Medicare and Medicaid Promoting Interoperability Programs
IX. MedPAC Recommendations
X. Other Required Information
A. Publicly Available Data
B. Collection of Information Requirements
XI. Provider Reimbursement Review Board (PRRB) Appeals
Regulation Text
Addendum—Schedule of Standardized Amounts, Update Factors, and Rate-of-Increase Percentages Effective With Cost Reporting Periods Beginning on or After October 1, 2019 and Payment Rates for LTCHs Effective With Discharges Occurring on or After October 1, 2019
I. Summary and Background
II. Changes to the Prospective Payment Rates for Hospital Inpatient Operating Costs for Acute Care Hospitals for FY 2020
A. Calculation of the Adjusted Standardized Amount
B. Adjustments for Area Wage Levels and Cost-of-Living
C. Calculation of the Prospective Payment Rates
III. Changes to Payment Rates for Acute Care Hospital Inpatient Capital-Related Costs for FY 2020
A. Determination of Federal Hospital Inpatient Capital-Related Prospective Payment Rate Update
B. Calculation of the Inpatient Capital-Related Prospective Payments for FY 2020
C. Capital Input Price Index
IV. Changes to Payment Rates for Excluded Hospitals: Rate-of-Increase Percentages for FY 2020
V. Updates to the Payment Rates for the LTCH PPS for FY 2020
A. LTCH PPS Standard Federal Payment Rate for FY 2020
B. Adjustment for Area Wage Levels Under the LTCH PPS for FY 2020
C. LTCH PPS Cost-of-Living Adjustment (COLA) for LTCHs Located in Alaska and Hawaii
D. Adjustment for LTCH PPS High-Cost Outlier (HCO) Cases
E. Update to the IPPS Comparable/Equivalent Amounts To Reflect the Statutory Changes to the IPPS DSH Payment Adjustment Methodology
F. Computing the Adjusted LTCH PPS Federal Prospective Payments for FY 2020
VI. Tables Referenced in This FY 2020 IPPS/LTCH PPS Final Rule and Available Through the Internet on the CMS Website
Appendix A—Economic Analyses
I. Regulatory Impact Analysis
A. Statement of Need
B. Overall Impact
C. Objectives of the IPPS and the LTCH PPS
D. Limitations of Our Analysis
E. Hospitals Included in and Excluded From the IPPS
F. Effects on Hospitals and Hospital Units Excluded From the IPPS
G. Quantitative Effects of the Policy Changes Under the IPPS for Operating Costs
H. Effects of Other Policy Changes
I. Effects of Changes in the Capital IPPS
J. Effects of Payment Rate Changes and Policy Changes Under the LTCH PPS
K. Effects of Requirements for Hospital Inpatient Quality Reporting (IQR) Program
L. Effects of Requirements for the PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program
M. Effects of Requirements for the Long-Term Care Hospital Quality Reporting Program (LTCH QRP)
N. Effects of Requirements Regarding the Medicare Promoting Interoperability Program
O. Alternatives Considered
P. Reducing Regulation and Controlling Regulatory Costs
Q. Overall Conclusion
R. Regulatory Review Costs
II. Accounting Statements and Tables
A. Acute Care Hospitals
B. LTCHs
III. Regulatory Flexibility Act (RFA) Analysis
IV. Impact on Small Rural Hospitals
V. Unfunded Mandate Reform Act (UMRA) Analysis
VI. Executive Order 13175
VII. Executive Order 12866
Appendix B: Recommendation of Update Factors for Operating Cost Rates of Payment for Inpatient Hospital Services
I. Background
II. Inpatient Hospital Update for FY 2020
A. FY 2020 Inpatient Hospital Update
B. Update for SCHs and MDHs for FY 2020
C. FY 2020 Puerto Rico Hospital Update
D. Update for Hospitals Excluded From the IPPS
E. Update for LTCHs for FY 2020
III. Secretary's Recommendation
IV. MedPAC Recommendation for Assessing Payment Adequacy and Updating Payments in Traditional Medicare
I. Executive Summary and Background
A. Executive Summary
1. Purpose and Legal Authority
This FY 2020 IPPS/LTCH PPS final rule makes payment and policy changes under the Medicare inpatient prospective payment systems (IPPS) for operating and capital-related costs of acute care hospitals as well as for certain hospitals and hospital units excluded from the IPPS. In addition, it makes payment and policy changes for inpatient hospital services provided by long-term care hospitals (LTCHs) under the long-term care hospital prospective payment system (LTCH PPS). This final rule also makes policy changes to programs associated with Medicare IPPS hospitals, IPPS-excluded hospitals, and LTCHs. In this final rule, we are addressing wage index disparities impacting low wage index hospitals; providing for an alternative IPPS new technology add-on payment pathway for certain transformative new devices and qualified infectious disease products; revising the calculation of the IPPS new technology add-on payment; and making revisions and clarifications related to the substantial clinical improvement criterion under the IPPS.
We are establishing new requirements and revising existing requirements for quality reporting by specific providers (acute care hospitals, PPS-exempt cancer hospitals, and LTCHs) that are participating in Medicare. We also are establishing new requirements and revising existing requirements for eligible hospitals and CAHs participating in the Medicare and Medicaid Promoting Interoperability Programs. We are updating policies for the Hospital Value-Based Purchasing (VBP) Program, the Hospital Readmissions Reduction Program, and the Hospital-Acquired Condition (HAC) Reduction Program.
Under various statutory authorities, we are making changes to the Medicare IPPS, to the LTCH PPS, and to other related payment methodologies and programs for FY 2020 and subsequent fiscal years. These statutory authorities include, but are not limited to, the following:
- Section 1886(d) of the Social Security Act (the Act), which sets forth a system of payment for the operating costs of acute care hospital inpatient stays under Medicare Part A (Hospital Insurance) based on prospectively set rates. Section 1886(g) of the Act requires that, instead of paying for capital-related costs of inpatient hospital services on a reasonable cost basis, the Secretary use a prospective payment system (PPS).
- Section 1886(d)(1)(B) of the Act, which specifies that certain hospitals and hospital units are excluded from the IPPS. These hospitals and units are: Rehabilitation hospitals and units; LTCHs; psychiatric hospitals and units; children's hospitals; cancer hospitals; extended neoplastic disease care hospitals, and hospitals located outside the 50 States, the District of Columbia, and Puerto Rico (that is, hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa). Religious nonmedical health care institutions (RNHCIs) are also excluded from the IPPS.
- Sections 123(a) and (c) of the BBRA (Pub. L. 106-113) and section 307(b)(1) of the BIPA (Pub. L. 106-554) (as codified under section 1886(m)(1) of the Act), which provide for the development and implementation of a prospective payment system for payment for inpatient hospital services of LTCHs described in section 1886(d)(1)(B)(iv) of the Act.
- Sections 1814(l), 1820, and 1834(g) of the Act, which specify that payments are made to critical access hospitals (CAHs) (that is, rural hospitals or facilities that meet certain statutory requirements) for inpatient and outpatient services and that these payments are generally based on 101 percent of reasonable cost.
- Section 1866(k) of the Act, which provides for the establishment of a quality reporting program for hospitals described in section 1886(d)(1)(B)(v) of the Act, referred to as “PPS-exempt cancer hospitals.”
- Section 1886(a)(4) of the Act, which specifies that costs of approved educational activities are excluded from the operating costs of inpatient hospital services. Hospitals with approved graduate medical education (GME) programs are paid for the direct costs of GME in accordance with section 1886(h) of the Act.
- Section 1886(b)(3)(B)(viii) of the Act, which requires the Secretary to reduce the applicable percentage increase that would otherwise apply to the standardized amount applicable to a subsection (d) hospital for discharges occurring in a fiscal year if the hospital does not submit data on measures in a form and manner, and at a time, specified by the Secretary.
- Section 1886(o) of the Act, which requires the Secretary to establish a Hospital Value-Based Purchasing (VBP) Program, under which value-based incentive payments are made in a fiscal year to hospitals meeting performance standards established for a performance period for such fiscal year.
- Section 1886(p) of the Act, which establishes a Hospital-Acquired Condition (HAC) Reduction Program, under which payments to applicable hospitals are adjusted to provide an incentive to reduce hospital-acquired conditions.
- Section 1886(q) of the Act, as amended by section 15002 of the 21st Century Cures Act, which establishes the Hospital Readmissions Reduction Program. Under the program, payments for discharges from an applicable hospital as defined under section 1886(d) of the Act will be reduced to account for certain excess readmissions. Section 15002 of the 21st Century Cures Act requires the Secretary to compare hospitals with respect to the number of their Medicare-Medicaid dual-eligible beneficiaries (dual-eligibles) in determining the extent of excess readmissions.
- Section 1886(r) of the Act, as added by section 3133 of the Affordable Care Act, which provides for a reduction to disproportionate share hospital (DSH) payments under section 1886(d)(5)(F) of the Act and for a new uncompensated care payment to eligible hospitals. Specifically, section 1886(r) of the Act requires that, for fiscal year 2014 and each subsequent fiscal year, subsection (d) hospitals that would otherwise receive a DSH payment made under section 1886(d)(5)(F) of the Act will receive two separate payments: (1) 25 percent of the amount they previously would have received under section 1886(d)(5)(F) of the Act for DSH (“the empirically justified amount”), and (2) an additional payment for the DSH hospital's proportion of uncompensated care, determined as the product of three factors. These three factors are: (1) 75 percent of the payments that would otherwise be made under section 1886(d)(5)(F) of the Act; (2) 1 minus the percent change in the percent of individuals who are uninsured; and (3) a hospital's uncompensated care amount relative to the uncompensated care amount of all DSH hospitals expressed as a percentage.
- Section 1886(m)(6) of the Act, as added by section 1206(a)(1) of the Pathway for Sustainable Growth Rate (SGR) Reform Act of 2013 (Pub. L. 113-67) and amended by section 51005(a) of the Bipartisan Budget Act of 2018 (Pub. L. 115-123), which provided for the establishment of site neutral payment rate criteria under the LTCH PPS, with implementation beginning in FY 2016, and provides for a 4-year transitional blended payment rate for discharges occurring in LTCH cost reporting periods beginning in FYs 2016 through 2019. Section 51005(b) of the Bipartisan Budget Act of 2018 amended section 1886(m)(6)(B) by adding new clause (iv), which specifies that the IPPS comparable amount defined in clause (ii)(I) shall be reduced by 4.6 percent for FYs 2018 through 2026.
- Section 1899B of the Act, as added by section 2(a) of the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) (Pub. L. 113-185), which provides for the establishment of standardized data reporting for certain post-acute care providers, including LTCHs.
2. Summary of the Major Provisions
In this final rule, we provide a summary of the major provisions in this FY 2020 IPPS/LTCH PPS final rule. In general, these major provisions are part of the annual update to the payment policies and payment rates, consistent with the applicable statutory provisions. A general summary of the proposed changes that were included in the FY 2020 IPPS/LTCH PPS proposed rule is presented in section I.D. of the preamble of this final rule.
a. MS-DRG Documentation and Coding Adjustment
Section 631 of the American Taxpayer Relief Act of 2012 (ATRA, Pub. L. 112-240) amended section 7(b)(1)(B) of Public Law 110-90 to require the Secretary to make a recoupment adjustment to the standardized amount of Medicare payments to acute care hospitals to account for changes in MS-DRG documentation and coding that do not reflect real changes in case-mix, totaling $11 billion over a 4-year period of FYs 2014, 2015, 2016, and 2017. The FY 2014 through FY 2017 adjustments represented the amount of the increase in aggregate payments as a result of not completing the prospective adjustment authorized under section 7(b)(1)(A) of Public Law 110-90 until FY 2013. Prior to the ATRA, this amount could not have been recovered under Public Law 110-90. Section 414 of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) (Pub. L. 114-10) replaced the single positive adjustment we intended to make in FY 2018 with a 0.5 percent positive adjustment to the standardized amount of Medicare payments to acute care hospitals for FYs 2018 through 2023. (The FY 2018 adjustment was subsequently adjusted to 0.4588 percent by section 15005 of the 21st Century Cures Act.) Therefore, for FY 2020, we are making an adjustment of +0.5 percent to the standardized amount.
b. Revisions and Clarifications to the New Technology Add-On Payment Policy Substantial Clinical Improvement Criterion Under the IPPS
In the proposed rule, in addition to a broad request for public comments for potential rulemaking in future years, in order to respond to stakeholder feedback requesting greater understanding of CMS' approach to evaluating substantial clinical improvement, we solicited public comments on specific changes or clarifications to the IPPS and Outpatient Prospective Payment System (OPPS) substantial clinical improvement criterion used to evaluate applications for new technology add-on payments under the IPPS and the transitional pass-through payment for additional costs of innovative devices under the OPPS that CMS might consider making in this FY 2020 IPPS/LTCH PPS final rule for applications received beginning in FY 2020 for the IPPS and CY 2020 for the OPPS, to provide greater clarity and predictability.
In this final rule, after consideration of public comments, we are revising and clarifying certain aspects of our evaluation of the substantial clinical improvement criterion under the IPPS in 42 CFR 412.87.
c. Alternative Inpatient New Technology Add-On Payment Pathway for Transformative New Devices and Antimicrobial Resistant Products
As discussed in section III.H.8. of the preamble of this final rule, after consideration of public comments, given the Food and Drug Administration's (FDA's) expedited programs, and consistent with the Administration's commitment to addressing barriers to health care innovation and ensuring that Medicare beneficiaries have access to critical and life-saving new cures and technologies that improve beneficiary health outcomes, we are adopting an alternative pathway for the inpatient new technology add-on payment for certain transformative medical devices. In situations where a new medical device has received FDA marketing authorization (that is, the device has received pre-market approval (PMA); 510(k) clearance; or the granting of a De Novo classification request) and is the subject of the FDA's Breakthrough Devices Program, we are finalizing our proposal to create an alternative inpatient new technology add-on payment pathway to facilitate access to this technology for Medicare beneficiaries. In addition, after consideration of public comments and concerns related to antimicrobial resistance and its serious impact on Medicare beneficiaries and public health overall, we are finalizing an alternative inpatient new technology add-for Qualified Infectious Disease Products (QIDPs).
Specifically, we are establishing that, for applications received for IPPS new technology add-on payments for FY 2021 and subsequent fiscal years, if a medical device is the subject of the FDA's Breakthrough Devices Program or if a medical product technology receives the FDA's QIDP designation and received FDA marketing authorization, such a device or product will be considered new and not substantially similar to an existing technology for purposes of new technology add-on payment under the IPPS. We are also establishing that the medical device or product will not need to meet the requirement under 42 CFR 412.87(b)(1) that it represent an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
d. Revision of the Calculation of the Inpatient Hospital New Technology Add-On Payment
The current calculation of the new technology add-on payment is based on the cost to hospitals for the new medical service or technology. Under § 412.88, if the costs of the discharge (determined by applying cost-to-charge ratios (CCRs), as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 50 percent of the costs of the new medical service or technology; or (2) 50 percent of the amount by which the costs of the case exceed the standard DRG payment. Unless the discharge qualifies for an outlier payment, the additional Medicare payment is limited to the full MS-DRG payment plus 50 percent of the estimated costs of the new technology or medical service.
As discussed in section III.H.9. of the preamble of this final rule, after consideration of the concerns raised by commenters and other stakeholders, we agree that capping the add-on payment amount at 50 percent could, in some cases, not adequately reflect the costs of new technology or sufficiently support healthcare innovations.
After consideration of public comments, we are finalizing the proposed modification to the current payment amount to increase the maximum add-on payment amount to 65 percent of the costs of the new technology or medical service (except with respect to a medical product designated by the FDA as a QIDP). Therefore, we are establishing that, beginning with discharges occurring on or after October 1, 2019, for a new technology other than a medical product designated as a QIDP by the FDA, if the costs of a discharge involving a new medical service or technology exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 65 percent of the costs of the new medical service or technology; or (2) 65 percent of the amount by which the costs of the case exceed the standard DRG payment. In addition, after consideration of public comments and concerns related to antimicrobial resistance and its serious impact on Medicare beneficiaries and public health overall, we are establishing that, beginning with discharges occurring on or after October 1, 2019, for a new technology that is a medical product designated as a QIDP by the FDA, if the costs of a discharge involving a new medical service or technology exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 75 percent of the costs of the new medical service or technology; or (2) 75 percent of the amount by which the costs of the case exceed the standard DRG payment.
e. Finalized Policies To Address Wage Index Disparities
In the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20372), we invited the public to submit further comments, suggestions, and recommendations for regulatory and policy changes to the Medicare wage index. Many of the responses received from this request for information (RFI) reflect a common concern that the current wage index system perpetuates and exacerbates the disparities between high and low wage index hospitals. Many respondents also expressed concern that the calculation of the rural floor has allowed a limited number of States to manipulate the wage index system to achieve higher wages for many urban hospitals in those States at the expense of hospitals in other States, which also contributes to wage index disparities.
To help mitigate these wage index disparities, including those resulting from the inclusion of hospitals with rural reclassifications under 42 CFR 412.103 in the rural floor, in this final rule, we are reducing the disparity between high and low wage index hospitals by increasing the wage index values for certain hospitals with low wage index values and doing so in a budget neutral manner through an adjustment applied to the standardized amounts for all hospitals, as well as changing the calculation of the rural floor. We also are providing for a transition for hospitals experiencing significant decreases in their wage index values as compared to their final FY 2019 wage index. We are making these changes in a budget neutral manner.
In this final rule, we are increasing the wage index for hospitals with a wage index value below the 25th percentile wage index value for a fiscal year by half the difference between the otherwise applicable final wage index value for a year for that hospital and the 25th percentile wage index value for that year across all hospitals. Furthermore, this policy will be effective for at least 4 years, beginning in FY 2020, in order to allow employee compensation increases implemented by these hospitals sufficient time to be reflected in the wage index calculation. In order to offset the estimated increase in IPPS payments to hospitals with wage index values below the 25th percentile wage index value, we are applying a uniform budget neutrality factor to the standardized amount.
In addition, we are removing urban to rural reclassifications from the calculation of the rural floor, such that, beginning in FY 2020, the rural floor is calculated without including the wage data of hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented in the regulations at § 412.103). Also, for the purposes of applying the provisions of section 1886(d)(8)(C)(iii) of the Act, we are removing urban to rural reclassifications from the calculation of “the wage index for rural areas in the State in which the county is located” as referred to in the statute.
Lastly, for FY 2020, we are placing a 5-percent cap on any decrease in a hospital's wage index from the hospital's final wage index in FY 2019. We are applying a budget neutrality adjustment to the standardized amount so that our transition for hospitals that could be negatively impacted is implemented in a budget neutral manner.
f. DSH Payment Adjustment and Additional Payment for Uncompensated Care
Section 3133 of the Affordable Care Act modified the Medicare disproportionate share hospital (DSH) payment methodology, beginning in FY 2014. Under section 1886(r) of the Act, which was added by section 3133 of the Affordable Care Act, starting in FY 2014, DSHs receive 25 percent of the amount they previously would have received under the statutory formula for Medicare DSH payments in section 1886(d)(5)(F) of the Act. The remaining amount, equal to 75 percent of the amount that otherwise would have been paid as Medicare DSH payments, is paid as additional payments after the amount is reduced for changes in the percentage of individuals that are uninsured. Each Medicare DSH will receive an additional payment based on its share of the total amount of uncompensated care for all Medicare DSHs for a given time period.
In this FY 2020 IPPS/LTCH PPS final rule, we have updated our estimates of the three factors used to determine uncompensated care payments for FY 2020. We continue to use uninsured estimates produced by CMS' Office of the Actuary (OACT), as part of the development of the National Health Expenditure Accounts (NHEA) in the calculation of Factor 2. We also are using a single year of data on uncompensated care costs from Worksheet S-10 for FY 2015 to determine Factor 3 for FY 2020. In addition, we are continuing to use only data regarding low-income insured days (Medicaid days for FY 2013 and FY 2017 SSI days) to determine the amount of uncompensated care payments for Puerto Rico hospitals, and Indian Health Service and Tribal hospitals. We did not adopt specific Factor 3 polices for all-inclusive rate providers for FY 2020. In this final rule, we also are continuing to use the following established policies: (1) For providers with multiple cost reports, beginning in the same fiscal year, to use the longest cost report and annualize Medicaid data and uncompensated care data if a hospital's cost report does not equal 12 months of data; (2) in the rare case where a provider has multiple cost reports beginning in the same fiscal year, but one report also spans the entirety of the following fiscal year, such that the hospital has no cost report for that fiscal year, to use the cost report that spans both fiscal years for the latter fiscal year; and (3) to apply statistical trim methodologies to potentially aberrant cost-to-charge ratios (CCRs) and potentially aberrant uncompensated care costs reported on the Worksheet S-10.
g. Changes to the LTCH PPS
In this FY 2020 IPPS/LTCH PPS final rule, we set forth changes to the LTCH PPS Federal payment rates, factors, and other payment rate policies under the LTCH PPS for FY 2020. We also are establishing the payment adjustment for LTCH discharges when the LTCH does not meet the applicable discharge payment percentage and a reinstatement process, as required by section 1886(m)(6)(C) of the Act. An LTCH will be subject to this payment adjustment if, for cost reporting periods beginning in FY 2020 and subsequent fiscal years, the LTCH's percentage of Medicare discharges that meet the criteria for exclusion from the site neutral payment rate (that is, discharges paid the LTCH PPS standard Federal payment rate) of its total number of Medicare FFS discharges paid under the LTCH PPS during the cost reporting period is not at least 50 percent. We are adopting a probationary cure period as part of the reinstatement process.
h. Reduction of Hospital Payments for Excess Readmissions
We are making changes to policies for the Hospital Readmissions Reduction Program, which was established under section 1886(q) of the Act, as amended by section 15002 of the 21st Century Cures Act. The Hospital Readmissions Reduction Program requires a reduction to a hospital's base operating DRG payment to account for excess readmissions of selected applicable conditions. For FY 2017 and subsequent years, the reduction is based on a hospital's risk-adjusted readmission rate during a 3-year period for acute myocardial infarction (AMI), heart failure (HF), pneumonia, chronic obstructive pulmonary disease (COPD), elective primary total hip arthroplasty/total knee arthroplasty (THA/TKA), and coronary artery bypass graft (CABG) surgery. In this FY 2020 IPPS/LTCH PPS final rule, we are establishing the following policies: (1) A measure removal policy that aligns with the removal factor policies previously adopted in other quality reporting and quality payment programs; (2) an update to the Program's definition of “dual-eligible,” beginning with the FY 2021 program year to allow for a 1-month lookback period in data sourced from the State Medicare Modernization Act (MMA) files to determine dual-eligible status for beneficiaries who die in the month of discharge; (3) a subregulatory process to address any potential future nonsubstantive changes to the payment adjustment factor components; and (4) an update to the Program's regulations at 42 CFR 412.152 and 412.154 to reflect policies we are finalizing in this final rule and to codify additional previously finalized policies.
i. Hospital Value-Based Purchasing (VBP) Program
Section 1886(o) of the Act requires the Secretary to establish a Hospital VBP Program under which value-based incentive payments are made in a fiscal year to hospitals based on their performance on measures established for a performance period for such fiscal year. In this FY 2020 IPPS/LTCH PPS final rule, we are establishing that the Hospital VBP Program will use the same data used by the HAC Reduction Program for purposes of calculating the Centers for Disease Control and Prevention (CDC) National Health Safety Network (NHSN) Healthcare-Associated Infection (HAI) measures beginning with CY 2020 data collection, which is when the Hospital IQR Program will no longer collect data on those measures, and will rely on HAC Reduction Program validation to ensure the accuracy of CDC NHSN HAI measure data used in the Hospital VBP Program. We also are newly establishing certain performance standards.
j. Hospital-Acquired Condition (HAC) Reduction Program
Section 1886(p) of the Act establishes an incentive to hospitals to reduce the incidence of hospital-acquired conditions by requiring the Secretary to make an adjustment to payments to applicable hospitals, effective for discharges beginning on October 1, 2014. This 1-percent payment reduction applies to hospitals that rank in the worst-performing quartile (25 percent) of all applicable hospitals, relative to the national average, of conditions acquired during the applicable period and on all of the hospital's discharges for the specified fiscal year. As part of our agency-wide Patients over Paperwork and Meaningful Measures Initiatives, discussed in section I.A.2. of the FY 2019 IPPS/LTCH PPS final rule (83 FR 41147 and 41148), we are: (1) Adopting a measure removal policy that aligns with the removal factor policies previously adopted in other quality reporting and quality payment programs; (2) clarifying administrative policies for validation of the CDC NHSN HAI measures; (3) adopting the data collection periods for the FY 2022 program year; and (4) updating 42 CFR 412.172(f) to reflect policies finalized in the FY 2019 IPPS/LTCH PPS final rule.
k. Hospital Inpatient Quality Reporting (IQR) Program
Under section 1886(b)(3)(B)(viii) of the Act, subsection (d) hospitals are required to report data on measures selected by the Secretary for a fiscal year in order to receive the full annual percentage increase that would otherwise apply to the standardized amount applicable to discharges occurring in that fiscal year.
In this FY 2020 IPPS/LTCH PPS final rule, we are making several changes. We are: (1) Adopting the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination with a clarification and update; (2) adopting the Hybrid Hospital-Wide All-Cause Readmission (Hybrid HWR) measure (NQF #2879) in a stepwise fashion, beginning with two voluntary reporting periods which will run from July 1, 2021 through June 30, 2022, and from July 1, 2022 through June 30, 2023, before requiring reporting of the measure for the reporting period that will run from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination and for subsequent years; and (3) removing the Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure (NQF #1789) (HWR claims-only measure), beginning with the FY 2026 payment determination. We are not finalizing our proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM. We also are establishing reporting and submission requirements for eCQMs, including policies to: (1) Extend current eCQM reporting and submission requirements for both the CY 2020 reporting period/FY 2022 payment determination and CY 2021 reporting period/FY 2023 payment determination; (2) change the eCQM reporting and submission requirements for the CY 2022 reporting period/FY 2024 payment determination, such that hospitals will be required to report one, self-selected calendar quarter of data for three self-selected eCQMs and the Safe Use of Opioids—Concurrent Prescribing eCQM (NQF #3316e), for a total of four eCQMs; and (3) continue requiring that EHRs be certified to all available eCQMs used in the Hospital IQR Program for the CY 2020 reporting period/FY 2022 payment determination and subsequent years. These eCQM reporting and submission policies are in alignment with policies under the Promoting Interoperability Program. We also are establishing reporting and submission requirements for the Hybrid HWR measure. In addition, we are summarizing public comments we received on three measures we are considering for potential future inclusion in the Hospital IQR Program.
l. Medicare and Medicaid Promoting Interoperability Programs
For purposes of an increased level of stability, reducing the burden on eligible hospitals and CAHs, and clarifying certain existing policies, we are finalizing several changes to the Promoting Interoperability Program. Specifically, we are: (1) Eliminating the requirement that, for the FY 2020 payment adjustment year, for an eligible hospital that has not successfully demonstrated it is a meaningful EHR user in a prior year, the EHR reporting period in CY 2019 must end before and the eligible hospital must successfully register for and attest to meaningful use no later than the October 1, 2019 deadline; (2) establishing an EHR reporting period of a minimum of any continuous 90-day period in CY 2021 for new and returning participants (eligible hospitals and CAHs) in the Medicare Promoting Interoperability Program attesting to CMS; (3) requiring that the Medicare Promoting Interoperability Program measure actions must occur within the EHR reporting period, beginning with the EHR reporting period in CY 2020; (4) revising the Query of PDMP measure to make it an optional measure worth 5 bonus points in CY 2020, removing the exclusions associated with this measure in CY 2020, requiring a yes/no response instead of a numerator and denominator for CY 2019 and CY 2020, and clearly stating our intended policy that the measure is worth a full 5 bonus points in CY 2019 and CY 2020; (5) changing the maximum points available for the e-Prescribing measure from 5 points to 10 points beginning in CY 2020; (6) removing the Verify Opioid Treatment Agreement measure beginning in CY 2020 and clearly stating our intended policy that this measure is worth a full 5 bonus points in CY 2019; and (7) revising the Support Electronic Referral Loops by Receiving and Incorporating Health Information measure to more clearly capture the previously established policy regarding CEHRT use. We also are amending our regulations to incorporate several of these finalized policies.
For CQM reporting under the Medicare and Medicaid Promoting Interoperability Programs, we are generally aligning our requirements with requirements under the Hospital IQR Program. Specifically, we are: (1) Adopting one opioid-related CQM (Safe Use of Opioids—Concurrent Prescribing CQM beginning with the reporting period in CY 2021 (we are not finalizing our proposal to add the Hospital Harm—Opioid-Related Adverse Events CQM); (2) extending current CQM reporting and submission requirements for the reporting periods in CY 2020 and CY 2021; and (3) establishing CQM reporting and submission requirements for the reporting period in CY 2022, which will require all eligible hospitals and CAHs to report on the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the reporting period in CY 2022.
We sought public comments on whether we should consider proposing to adopt in future rulemaking the Hybrid Hospital-Wide All-Cause Readmission (Hybrid HWR) measure, beginning with the reporting period in CY 2023, a measure which we adopted under the Hospital IQR Program, and we sought information on a variety of issues regarding the future direction of the Medicare and Medicaid Promoting Interoperability Programs. We may use the input we received to inform further rulemaking.
3. Summary of Costs and Benefits
- Adjustment for MS-DRG Documentation and Coding Changes. Section 414 of the MACRA replaced the single positive adjustment we intended to make in FY 2018 once the recoupment required by section 631 of the ATRA was complete with a 0.5 percentage point positive adjustment to the standardized amount of Medicare payments to acute care hospitals for FYs 2018 through 2023. (The FY 2018 adjustment was subsequently adjusted to 0.4588 percentage point by section 15005 of the 21st Century Cures Act.) For FY 2020, we are making an adjustment of +0.5 percentage point to the standardized amount consistent with the MACRA.
- Alternative Inpatient New Technology Add-On Payment Pathway for Transformative New Devices: In this FY 2020 IPPS/LTCH PPS final rule, we are establishing an alternative inpatient new technology add-on payment pathway for a new medical device that is subject to the FDA Breakthrough Devices Program and has received FDA authorization (that is, received PMA approval, 510(k) clearance, or the granting of De Novo classification request). We are also establishing that, if a medical product is designated by the FDA as a Qualified Infectious Disease Product (QIDP) and received FDA market authorization. Under these alternative inpatient new technology add-on payment pathways, such a medical device or product will be considered new and not substantially similar to an existing technology for purposes of new technology add-on payment under the IPPS, and such a medical product or device will not need to meet the requirement under § 412.87(b)(1) that it represent an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
Given the relatively recent introduction of FDA's Breakthrough Devices Program, there have not been any medical devices that were part of the Breakthrough Devices Program and received FDA marketing authorization and for which the applicant applied for a new technology add-on payment under the IPPS and was not approved. If all of the future new medical devices that were part of the Breakthrough Devices Program and QIDPs that would have applied for new technology add-on payments would have been approved under the existing criteria, this policy has no impact. To the extent that there are future medical devices that were part of the Breakthrough Devices Program or QIDPs that are the subject of applications for new technology add-on payments, and those applications would have been denied under the current new technology add-on payment criteria, this policy is a cost, but that cost is not estimable. Therefore, it is not possible to quantify the impact of this policy.
Revisions to the Calculation of the Inpatient Hospital New Technology Add-On Payment: The current calculation of the new technology add-on payment is based on the cost to hospitals for the new medical service or technology. Under existing § 412.88, if the costs of the discharge exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare makes an add-on payment equal to the lesser of: (1) 50 percent of the estimated costs of the new technology or medical service; or (2) 50 percent of the amount by which the costs of the case exceed the standard DRG payment.
As discussed in section II.H.9. of the preamble of this final rule, we have modified the current payment mechanism to increase the amount of the maximum add-on payment amount to 65 percent (and 75 percent for QIDPs). Specifically, for technologies other than QIDPs, if the costs of a discharge (determined by applying CCRs as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 65 percent (or 75 percent for QIDPs) of the costs of the new medical service or technology; or (2) 65 percent (75 percent for QIDPs) of the amount by which the costs of the case exceed the standard DRG payment.
We estimate that for the nine technologies for which we are continuing to make new technology add on payments in FY 2020 and for the nine FY 2020 new technology add-on payment applications that we are approving for new technology add-on payments for FY 2020, these changes to the calculation of the new technology add-on payment will increase IPPS spending by approximately $94 million in FY 2020.
Technologies Approved for FY 2020 New Technology Add-On Payments: In section II.H.5. of the preamble to this final rule, we discuss 13 technologies for which we received applications for add-on payments for new medical services and technologies for FY 2020. We also discuss the status of the new technologies that were approved to receive new technology add-on payments in FY 2019 in section II.H.4. of the preamble to this final rule. As explained in the preamble to this final rule, add-on payments for new medical services and technologies under section 1886(d)(5)(K) of the Act are not required to be budget neutral. Based on those technologies approved for new technology add-on payments for FY 2020, new technology add-on payment are projected to increase approximately $162 million as compared to FY 2019 (which also reflects the estimated changes to the calculation of the inpatient new technology add-on payment described above).
- Changes To Address Wage Index Disparities. As discussed in section III.N. of the preamble of this final rule, to help mitigate wage index disparities, including those resulting from the inclusion of hospitals with rural reclassifications under 42 CFR 412.103 in the rural floor, we are reducing the disparity between high and low wage index hospitals by increasing the wage index values for certain hospitals with low wage index values (that is, hospitals with wage index values below the 25th percentile wage index value across all hospitals), as well as changing the calculation of the rural floor. In order to offset the estimated increase in IPPS payments to hospitals with wage index values below the 25th percentile wage index value, we have applied a uniform budget neutrality adjustment to the standardized amount. We also are establishing a transition for FY 2020 for hospitals experiencing significant decreases in their wage index values, and we are implementing this in a budget neutral manner by applying a budget neutrality adjustment to the standardized amount.
- Medicare DSH Payment Adjustment and Additional Payment for Uncompensated Care. For FY 2020, we are updating our estimates of the three factors used to determine uncompensated care payments. We are continuing to use uninsured estimates produced by OACT, as part of the development of the NHEA in the calculation of Factor 2. We also are using a single year of data on uncompensated care costs from Worksheet S-10 for FY 2015 to determine Factor 3 for FY 2020. To determine the amount of uncompensated care for purposes of calculating Factor 3 for Puerto Rico hospitals and Indian Health Service and Tribal hospitals, we are continuing to use only data regarding low-income insured days (Medicaid days for FY 2013 and FY 2017 SSI days).
We project that the amount available to distribute as payments for uncompensated care for FY 2020 will increase by approximately $78 million, as compared to our estimate of the uncompensated care payments that will be distributed in FY 2019. The payments have redistributive effects, based on a hospital's uncompensated care amount relative to the uncompensated care amount for all hospitals that are projected to be eligible to receive Medicare DSH payments, and the calculated payment amount is not directly tied to a hospital's number of discharges.
Update to the LTCH PPS Payment Rates and Other Payment Policies. Based on the best available data for the 384 LTCHs in our database, we estimate that the changes to the payment rates and factors that we presented in the preamble of and Addendum to this FY 2020 IPPS/LTCH PPS final rule, which reflect the end of the transition of the statutory application of the site neutral payment rate and the update to the LTCH PPS standard Federal payment rate for FY 2020, will result in an estimated increase in payments in FY 2020 of approximately $43 million.
- Changes to the Hospital Readmissions Reduction Program. For FY 2020 and subsequent years, the reduction is based on a hospital's risk-adjusted readmission rate during a 3-year period for acute myocardial infarction (AMI), heart failure (HF), pneumonia, chronic obstructive pulmonary disease (COPD), elective primary total hip arthroplasty/total knee arthroplasty (THA/TKA), and coronary artery bypass graft (CABG) surgery. Overall, in this FY 2020 IPPS/LTCH PPS final rule, we estimate that 2,583 hospitals would have their base operating DRG payments reduced by their determined proxy FY 2020 hospital-specific readmission adjustment. As a result, we estimate that the Hospital Readmissions Reduction Program will save approximately $563 million in FY 2020.
- Value-Based Incentive Payments Under the Hospital VBP Program. We estimate that there will be no net financial impact to participating hospitals under the Hospital VBP Program for the FY 2020 program year in the aggregate because, by law, the amount available for value-based incentive payments under the program in a given year must be equal to the total amount of base operating MS-DRG payment amount reductions for that year, as estimated by the Secretary. The estimated amount of base operating MS-DRG payment amount reductions for the FY 2020 program year and, therefore, the estimated amount available for value-based incentive payments for FY 2020 discharges is approximately $1.9 billion.
- Changes to the HAC Reduction Program. A hospital's Total HAC score and its ranking in comparison to other hospitals in any given year depend on several different factors. The FY 2020 program year is the first year in which we are implementing our equal measure weights scoring methodology. Any significant impact due to the HAC Reduction Program changes for FY 2020, including which hospitals will receive the adjustment, will depend on the actual experience of hospitals in the Program. We also are updating the hourly wage rate associated with burden for CDC NHSN HAI validation under the HAC Reduction Program.
- Changes to the Hospital Inpatient Quality Reporting (IQR) Program. Across 3,300 IPPS hospitals, we estimate that our changes for the Hospital IQR Program in this FY 2020 IPPS/LTCH PPS final rule would result in changes to the information collection burden compared to previously adopted requirements. The only policy that will affect the information collection burden for the Hospital IQR Program is the policy to adopt the Hybrid Hospital-Wide All-Cause Readmission (Hybrid HWR) measure (NQF #2879) in a stepwise fashion, beginning with two voluntary reporting periods which will run from July 1, 2021 through June 30, 2022, and from July 1, 2022 through June 30, 2023, before requiring reporting of the measure for the reporting period that will run from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination and for subsequent years. We estimate that the impact of this change is a total collection of information burden increase of 2,211 hours and a total cost increase of approximately $83,266 for all participating IPPS hospitals annually.
- Changes to the Medicare and Medicaid Promoting Interoperability Programs. We believe that, overall, the revised policies in this FY 2020 IPPS/LTCH PPS final rule will reduce burden, as described in detail in section X.B.9. of the preamble and Appendix A, section I.N. of this final rule.
B. Background Summary
1. Acute Care Hospital Inpatient Prospective Payment System (IPPS)
Section 1886(d) of the Social Security Act (the Act) sets forth a system of payment for the operating costs of acute care hospital inpatient stays under Medicare Part A (Hospital Insurance) based on prospectively set rates. Section 1886(g) of the Act requires the Secretary to use a prospective payment system (PPS) to pay for the capital-related costs of inpatient hospital services for these “subsection (d) hospitals.” Under these PPSs, Medicare payment for hospital inpatient operating and capital-related costs is made at predetermined, specific rates for each hospital discharge. Discharges are classified according to a list of diagnosis-related groups (DRGs).
The base payment rate is comprised of a standardized amount that is divided into a labor-related share and a nonlabor-related share. The labor-related share is adjusted by the wage index applicable to the area where the hospital is located. If the hospital is located in Alaska or Hawaii, the nonlabor-related share is adjusted by a cost-of-living adjustment factor. This base payment rate is multiplied by the DRG relative weight.
If the hospital treats a high percentage of certain low-income patients, it receives a percentage add-on payment applied to the DRG-adjusted base payment rate. This add-on payment, known as the disproportionate share hospital (DSH) adjustment, provides for a percentage increase in Medicare payments to hospitals that qualify under either of two statutory formulas designed to identify hospitals that serve a disproportionate share of low-income patients. For qualifying hospitals, the amount of this adjustment varies based on the outcome of the statutory calculations. The Affordable Care Act revised the Medicare DSH payment methodology and provides for a new additional Medicare payment beginning on October 1, 2013, that considers the amount of uncompensated care furnished by the hospital relative to all other qualifying hospitals.
If the hospital is training residents in an approved residency program(s), it receives a percentage add-on payment for each case paid under the IPPS, known as the indirect medical education (IME) adjustment. This percentage varies, depending on the ratio of residents to beds.
Additional payments may be made for cases that involve new technologies or medical services that have been approved for special add-on payments. To qualify, a new technology or medical service must demonstrate that it is a substantial clinical improvement over technologies or services otherwise available, and that, absent an add-on payment, it would be inadequately paid under the regular DRG payment.
The costs incurred by the hospital for a case are evaluated to determine whether the hospital is eligible for an additional payment as an outlier case. This additional payment is designed to protect the hospital from large financial losses due to unusually expensive cases. Any eligible outlier payment is added to the DRG-adjusted base payment rate, plus any DSH, IME, and new technology or medical service add-on adjustments.
Although payments to most hospitals under the IPPS are made on the basis of the standardized amounts, some categories of hospitals are paid in whole or in part based on their hospital-specific rate, which is determined from their costs in a base year. For example, sole community hospitals (SCHs) receive the higher of a hospital-specific rate based on their costs in a base year (the highest of FY 1982, FY 1987, FY 1996, or FY 2006) or the IPPS Federal rate based on the standardized amount. SCHs are the sole source of care in their areas. Specifically, section 1886(d)(5)(D)(iii) of the Act defines an SCH as a hospital that is located more than 35 road miles from another hospital or that, by reason of factors such as an isolated location, weather conditions, travel conditions, or absence of other like hospitals (as determined by the Secretary), is the sole source of hospital inpatient services reasonably available to Medicare beneficiaries. In addition, certain rural hospitals previously designated by the Secretary as essential access community hospitals are considered SCHs.
Under current law, the Medicare-dependent, small rural hospital (MDH) program is effective through FY 2022. Through and including FY 2006, an MDH received the higher of the Federal rate or the Federal rate plus 50 percent of the amount by which the Federal rate was exceeded by the higher of its FY 1982 or FY 1987 hospital-specific rate. For discharges occurring on or after October 1, 2007, but before October 1, 2022, an MDH receives the higher of the Federal rate or the Federal rate plus 75 percent of the amount by which the Federal rate is exceeded by the highest of its FY 1982, FY 1987, or FY 2002 hospital-specific rate. MDHs are a major source of care for Medicare beneficiaries in their areas. Section 1886(d)(5)(G)(iv) of the Act defines an MDH as a hospital that is located in a rural area (or, as amended by the Bipartisan Budget Act of 2018, a hospital located in a State with no rural area that meets certain statutory criteria), has not more than 100 beds, is not an SCH, and has a high percentage of Medicare discharges (not less than 60 percent of its inpatient days or discharges in its cost reporting year beginning in FY 1987 or in two of its three most recently settled Medicare cost reporting years).
Section 1886(g) of the Act requires the Secretary to pay for the capital-related costs of inpatient hospital services in accordance with a prospective payment system established by the Secretary. The basic methodology for determining capital prospective payments is set forth in our regulations at 42 CFR 412.308 and 412.312. Under the capital IPPS, payments are adjusted by the same DRG for the case as they are under the operating IPPS. Capital IPPS payments are also adjusted for IME and DSH, similar to the adjustments made under the operating IPPS. In addition, hospitals may receive outlier payments for those cases that have unusually high costs.
The existing regulations governing payments to hospitals under the IPPS are located in 42 CFR part 412, subparts A through M.
2. Hospitals and Hospital Units Excluded From the IPPS
Under section 1886(d)(1)(B) of the Act, as amended, certain hospitals and hospital units are excluded from the IPPS. These hospitals and units are: Inpatient rehabilitation facility (IRF) hospitals and units; long-term care hospitals (LTCHs); psychiatric hospitals and units; children's hospitals; cancer hospitals; extended neoplastic disease care hospitals, and hospitals located outside the 50 States, the District of Columbia, and Puerto Rico (that is, hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa). Religious nonmedical health care institutions (RNHCIs) are also excluded from the IPPS. Various sections of the Balanced Budget Act of 1997 (BBA, Pub. L. 105-33), the Medicare, Medicaid and SCHIP [State Children's Health Insurance Program] Balanced Budget Refinement Act of 1999 (BBRA, Pub. L. 106-113), and the Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 (BIPA, Pub. L. 106-554) provide for the implementation of PPSs for IRF hospitals and units, LTCHs, and psychiatric hospitals and units (referred to as inpatient psychiatric facilities (IPFs)). (We note that the annual updates to the LTCH PPS are included along with the IPPS annual update in this document. Updates to the IRF PPS and IPF PPS are issued as separate documents.) Children's hospitals, cancer hospitals, hospitals located outside the 50 States, the District of Columbia, and Puerto Rico (that is, hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa), and RNHCIs continue to be paid solely under a reasonable cost-based system, subject to a rate-of-increase ceiling on inpatient operating costs. Similarly, extended neoplastic disease care hospitals are paid on a reasonable cost basis, subject to a rate-of-increase ceiling on inpatient operating costs.
The existing regulations governing payments to excluded hospitals and hospital units are located in 42 CFR parts 412 and 413.
3. Long-Term Care Hospital Prospective Payment System (LTCH PPS)
The Medicare prospective payment system (PPS) for LTCHs applies to hospitals described in section 1886(d)(1)(B)(iv) of the Act, effective for cost reporting periods beginning on or after October 1, 2002. The LTCH PPS was established under the authority of sections 123 of the BBRA and section 307(b) of the BIPA (as codified under section 1886(m)(1) of the Act). During the 5-year (optional) transition period, a LTCH's payment under the PPS was based on an increasing proportion of the LTCH Federal rate with a corresponding decreasing proportion based on reasonable cost principles. Effective for cost reporting periods beginning on or after October 1, 2006 through September 30, 2015 all LTCHs were paid 100 percent of the Federal rate. Section 1206(a) of the Pathway for SGR Reform Act of 2013 (Pub. L. 113-67) established the site neutral payment rate under the LTCH PPS, which made the LTCH PPS a dual rate payment system beginning in FY 2016. Under this statute, based on a rolling effective date that is linked to the date on which a given LTCH's Federal FY 2016 cost reporting period begins, LTCHs are generally paid for discharges at the site neutral payment rate unless the discharge meets the patient criteria for payment at the LTCH PPS standard Federal payment rate. The existing regulations governing payment under the LTCH PPS are located in 42 CFR part 412, subpart O. Beginning October 1, 2009, we issue the annual updates to the LTCH PPS in the same documents that update the IPPS (73 FR 26797 through 26798).
4. Critical Access Hospitals (CAHs)
Under sections 1814(l), 1820, and 1834(g) of the Act, payments made to critical access hospitals (CAHs) (that is, rural hospitals or facilities that meet certain statutory requirements) for inpatient and outpatient services are generally based on 101 percent of reasonable cost. Reasonable cost is determined under the provisions of section 1861(v) of the Act and existing regulations under 42 CFR part 413.
5. Payments for Graduate Medical Education (GME)
Under section 1886(a)(4) of the Act, costs of approved educational activities are excluded from the operating costs of inpatient hospital services. Hospitals with approved graduate medical education (GME) programs are paid for the direct costs of GME in accordance with section 1886(h) of the Act. The amount of payment for direct GME costs for a cost reporting period is based on the hospital's number of residents in that period and the hospital's costs per resident in a base year. The existing regulations governing payments to the various types of hospitals are located in 42 CFR part 413.
C. Summary of Provisions of Recent Legislation That Are Implemented in This Final Rule
1. Pathway for SGR Reform Act of 2013 (Pub. L. 113-67)
The Pathway for SGR Reform Act of 2013 (Pub. L. 113-67) introduced new payment rules in the LTCH PPS. Under section 1206 of this law, discharges in cost reporting periods beginning on or after October 1, 2015, under the LTCH PPS, receive payment under a site neutral rate unless the discharge meets certain patient-specific criteria. In this FY 2020 IPPS/LTCH PPS final rule, we are continuing to update certain policies that implemented provisions under section 1206 of the Pathway for SGR Reform Act.
2. Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) (Pub. L. 113-185)
The Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) (Pub. L. 113-185), enacted on October 6, 2014, made a number of changes that affect the Long-Term Care Hospital Quality Reporting Program (LTCH QRP). In this final rule, we are continuing to implement portions of section 1899B of the Act, as added by section 2(a) of the IMPACT Act, which, in part, requires LTCHs, among other post-acute care providers, to report standardized patient assessment data, data on quality measures, and data on resource use and other measures.
3. The Medicare Access and CHIP Reauthorization Act of 2015 (Pub. L. 114-10)
Section 414 of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA, Pub. L. 114-10) specifies a 0.5 percent positive adjustment to the standardized amount of Medicare payments to acute care hospitals for FYs 2018 through 2023. These adjustments follow the recoupment adjustment to the standardized amounts under section 1886(d) of the Act based upon the Secretary's estimates for discharges occurring from FYs 2014 through 2017 to fully offset $11 billion, in accordance with section 631 of the ATRA. The FY 2018 adjustment was subsequently adjusted to 0.4588 percent by section 15005 of the 21st Century Cures Act.
4. The 21st Century Cures Act (Pub. L. 114-255)
The 21st Century Cures Act (Pub. L. 114-255), enacted on December 13, 2016, contained the following provision affecting payments under the Hospital Readmissions Reduction Program, which we are continuing to implement in this final rule:
- Section 15002, which amended section 1886(q)(3) of the Act by adding subparagraphs (D) and (E), which requires the Secretary to develop a methodology for calculating the excess readmissions adjustment factor for the Hospital Readmissions Reduction Program, based on cohorts defined by the percentage of dual-eligible patients (that is, patients who are eligible for both Medicare and full-benefit Medicaid coverage) cared for by a hospital. In this FY 2020 IPPS/LTCH PPS final rule, we are continuing to implement changes to the payment adjustment factor to assess penalties, based on a hospital's performance, relative to other hospitals treating a similar proportion of dual-eligible patients.
D. Issuance of Notice of Proposed Rulemaking
In the FY 2020 IPPS/LTCH PPS proposed rule appearing in the Federal Register on May 3, 2019 (84 FR 19158), we set forth proposed payment and policy changes to the Medicare IPPS for FY 2020 operating costs and capital-related costs of acute care hospitals and certain hospitals and hospital units that are excluded from IPPS. In addition, we set forth proposed changes to the payment rates, factors, and other payment and policy-related changes to programs associated with payment rate policies under the LTCH PPS for FY 2020.
In this final rule is a general summary of the changes that we proposed to make.
1. Proposed Changes to MS-DRG Classifications and Recalibrations of Relative Weights
In section II. of the preamble of the proposed rule, we included—
- Proposed changes to MS-DRG classifications based on our yearly review for FY 2020.
- Proposed adjustment to the standardized amounts under section 1886(d) of the Act for FY 2020 in accordance with the amendments made to section 7(b)(1)(B) of Public Law 110-90 by section 414 of the MACRA.
- Proposed recalibration of the MS-DRG relative weights.
- A discussion of the proposed FY 2020 status of new technologies approved for add-on payments for FY 2019 and a presentation of our evaluation and analysis of the FY 2020 applicants for add-on payments for high-cost new medical services and technologies (including public input, as directed by Pub. L. 108-173, obtained in a town hall meeting).
- A request for public comments on the substantial clinical improvement criterion used to evaluate applications for both the IPPS new technology add-on payments and the OPPS transitional pass-through payment for devices, and a discussion of potential revisions that we were considering adopting as final policies related to the substantial clinical improvement criterion for applications received beginning in FY 2020 for the IPPS (that is, for FY 2021 and later new technology add-on payments) and beginning in CY 2020 for the OPPS.
- A proposed alternative IPPS new technology add-on payment pathway for certain transformative new devices.
- Proposed changes to the calculation of the IPPS new technology add-on payment.
2. Proposed Changes to the Hospital Wage Index for Acute Care Hospitals
In section III. of the preamble to the proposed rule we proposed to make revisions to the wage index for acute care hospitals and the annual update of the wage data. Specific issues addressed included, but were not limited to, the following:
- The proposed FY 2020 wage index update using wage data from cost reporting periods beginning in FY 2016.
- Proposals to address wage index disparities between high and low wage index hospitals.
- Calculation, analysis, and implementation of the proposed occupational mix adjustment to the wage index for acute care hospitals for FY 2020 based on the 2016 Occupational Mix Survey.
- Proposed application of the rural floor and the frontier State floor.
- Proposed revisions to the wage index for acute care hospitals, based on hospital redesignations and reclassifications under sections 1886(d)(8)(B), (d)(8)(E), and (d)(10) of the Act.
- Proposed change to Lugar county assignments.
- Proposed adjustment to the wage index for acute care hospitals for FY 2020 based on commuting patterns of hospital employees who reside in a county and work in a different area with a higher wage index.
- Proposed labor-related share for the proposed FY 2020 wage index.
3. Other Decisions and Proposed Changes to the IPPS for Operating Costs
In section IV. of the preamble of the proposed rule, we discussed proposed changes or clarifications of a number of the provisions of the regulations in 42 CFR parts 412 and 413, including the following:
- Proposed changes to MS-DRGs subject to the postacute care transfer policy and special payment policy.
- Proposed changes to the inpatient hospital update for FY 2020.
- Proposed conforming changes to the regulations for the low-volume hospital payment adjustment policy.
- Proposed updated national and regional case-mix values and discharges for purposes of determining RRC status.
- The statutorily required IME adjustment factor for FY 2020.
- Proposed changes to the methodologies for determining Medicare DSH payments and the additional payments for uncompensated care.
- A request for public comments on PRRB appeals related to a hospital's Medicaid fraction in the DSH payment adjustment calculation.
- Proposed changes to the policies for payment adjustments under the Hospital Readmissions Reduction Program based on hospital readmission measures and the process for hospital review and correction of those rates for FY 2020.
- Proposed changes to the requirements and provision of value-based incentive payments under the Hospital Value-Based Purchasing Program.
- Proposed requirements for payment adjustments to hospitals under the HAC Reduction Program for FY 2020.
- Proposed changes related to CAHs as nonproviders for direct GME and IME payment purposes.
- Discussion of the implementation of the Rural Community Hospital Demonstration Program in FY 2020.
4. Proposed FY 2020 Policy Governing the IPPS for Capital-Related Costs
In section V. of the preamble to the proposed rule, we discussed the proposed payment policy requirements for capital-related costs and capital payments to hospitals for FY 2020.
5. Proposed Changes to the Payment Rates for Certain Excluded Hospitals: Rate-of-Increase Percentages
In section VI. of the preamble of the proposed rule, we discussed—
- Proposed changes to payments to certain excluded hospitals for FY 2020.
- Proposed change related to CAH payment for ambulance services.
- Proposed continued implementation of the Frontier Community Health Integration Project (FCHIP) Demonstration.
6. Proposed Changes to the LTCH PPS
In section VII. of the preamble of the is proposed rule, we set forth—
- Proposed changes to the LTCH PPS Federal payment rates, factors, and other payment rate policies under the LTCH PPS for FY 2020.
- Proposed payment adjustment for discharges of LTCHs that do not meet the applicable discharge payment percentage.
7. Proposed Changes Relating to Quality Data Reporting for Specific Providers and Suppliers
In section VIII. of the preamble of the proposed rule, we addressed—
- Proposed requirements for the Hospital Inpatient Quality Reporting (IQR) Program.
- Proposed changes to the requirements for the quality reporting program for PPS-exempt cancer hospitals (PCHQR Program).
- Proposed changes to the requirements under the LTCH Quality Reporting Program (LTCH QRP).
- Proposed changes to requirements pertaining to eligible hospitals and CAHs participating in the Medicare and Medicaid Promoting Interoperability Programs.
8. Provider Reimbursement Review Board Appeals
In section XI. of the preamble of the proposed rule, we discussed the growing number of Provider Reimbursement Review Board appeals made by providers and the action initiatives that are being implemented with the goal to: Decrease the number of appeals submitted; decrease the number of appeals in inventory; reduce the time to resolution; and increase customer satisfaction.
9. Determining Prospective Payment Operating and Capital Rates and Rate-of-Increase Limits for Acute Care Hospitals
In sections II. and III. of the Addendum to the proposed rule, we set forth the proposed changes to the amounts and factors for determining the proposed FY 2020 prospective payment rates for operating costs and capital-related costs for acute care hospitals. We proposed to establish the threshold amounts for outlier cases, including a proposed change to the methodology for calculating those threshold amounts for FY 2020 to incorporate a projection of outlier payment reconciliations. In addition, in section IV. of the Addendum to the proposed rule, we addressed the update factors for determining the rate-of-increase limits for cost reporting periods beginning in FY 2020 for certain hospitals excluded from the IPPS.
10. Determining Prospective Payment Rates for LTCHs
In section V. of the Addendum to the proposed rule, we set forth proposed changes to the amounts and factors for determining the proposed FY 2020 LTCH PPS standard Federal payment rate and other factors used to determine LTCH PPS payments under both the LTCH PPS standard Federal payment rate and the site neutral payment rate in FY 2020. We proposed to establish the adjustments for wage levels, the labor-related share, the cost-of-living adjustment, and high-cost outliers, including the applicable fixed-loss amounts and the LTCH cost-to-charge ratios (CCRs) for both payment rates.
11. Impact Analysis
In Appendix A of the proposed rule, we set forth an analysis of the impact the proposed changes would have on affected acute care hospitals, CAHs, LTCHs, and PCHs.
12. Recommendation of Update Factors for Operating Cost Rates of Payment for Hospital Inpatient Services
In Appendix B of the proposed rule, as required by sections 1886(e)(4) and (e)(5) of the Act, we provided our recommendations of the appropriate percentage changes for FY 2020 for the following:
- A single average standardized amount for all areas for hospital inpatient services paid under the IPPS for operating costs of acute care hospitals (and hospital-specific rates applicable to SCHs and MDHs).
- Target rate-of-increase limits to the allowable operating costs of hospital inpatient services furnished by certain hospitals excluded from the IPPS.
- The LTCH PPS standard Federal payment rate and the site neutral payment rate for hospital inpatient services provided for LTCH PPS discharges.
13. Discussion of Medicare Payment Advisory Commission Recommendations
Under section 1805(b) of the Act, MedPAC is required to submit a report to Congress, no later than March 15 of each year, in which MedPAC reviews and makes recommendations on Medicare payment policies. MedPAC's March 2019 recommendations concerning hospital inpatient payment policies addressed the update factor for hospital inpatient operating costs and capital-related costs for hospitals under the IPPS. We address these recommendations in Appendix B of this FY 2020 IPPS/LTCH PPS final rule. For further information relating specifically to the MedPAC March 2019 report or to obtain a copy of the report, contact MedPAC at (202) 220-3700 or visit MedPAC's website at: http://www.medpac.gov.
E. Advancing Health Information Exchange
The Department of Health and Human Services (HHS) has a number of initiatives designed to encourage and support the adoption of interoperable health information technology and to promote nationwide health information exchange to improve health care. The Office of the National Coordinator for Health Information Technology (ONC) and CMS work collaboratively to advance interoperability across settings of care, including post-acute care.
To further interoperability in post-acute care, we developed a Data Element Library (DEL) to serve as a publicly available centralized, authoritative resource for standardized data elements and their associated mappings to health IT standards. The DEL furthers CMS' goal of data standardization and interoperability. These interoperable data elements can reduce provider burden by allowing the use and exchange of health care data, support provider exchange of electronic health information for care coordination, person-centered care, and support real-time, data driven, clinical decision making. Standards in the Data Element Library (https://del.cms.gov/) can be referenced on the CMS website and in the ONC Interoperability Standards Advisory (ISA). The 2019 ISA is available at: https://www.healthit.gov/isa .
The 21st Century Cures Act (the Cures Act) (Pub. L. 114-255, enacted December 13, 2016) requires HHS to take new steps to enable the electronic sharing of health information ensuring interoperability for providers and settings across the care continuum. In an important provision, Congress defined “information blocking” as practices likely to interfere with, prevent, or materially discourage access, exchange, or use of electronic health information, and established new authority for HHS to discourage these practices. In March 2019, ONC and CMS published the proposed rules, “21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program” (84 FR 7424 through 7610) and “Interoperability and Patient Access” (84 FR 7610 through 7680), to promote secure and more immediate access to health information for patients and health care providers through the implementation of information blocking provisions of the Cures Act and the use of standardized application programming interfaces (APIs) that enable easier access to electronic health information. These two proposed rules extended their comment period by 30 days and closed on June 3, 2019. The proposed rules can be found at: www.regulations.gov.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19158), we invited providers to learn more about these important developments and how they are likely to affect hospitals paid under the IPPS and the LTCH PPS.
II. Changes to Medicare Severity Diagnosis-Related Group (MS-DRG) Classifications and Relative Weights
A. Background
Section 1886(d) of the Act specifies that the Secretary shall establish a classification system (referred to as diagnosis-related groups (DRGs)) for inpatient discharges and adjust payments under the IPPS based on appropriate weighting factors assigned to each DRG. Therefore, under the IPPS, Medicare pays for inpatient hospital services on a rate per discharge basis that varies according to the DRG to which a beneficiary's stay is assigned. The formula used to calculate payment for a specific case multiplies an individual hospital's payment rate per case by the weight of the DRG to which the case is assigned. Each DRG weight represents the average resources required to care for cases in that particular DRG, relative to the average resources used to treat cases in all DRGs.
Section 1886(d)(4)(C) of the Act requires that the Secretary adjust the DRG classifications and relative weights at least annually to account for changes in resource consumption. These adjustments are made to reflect changes in treatment patterns, technology, and any other factors that may change the relative use of hospital resources.
B. MS-DRG Reclassifications
For general information about the MS-DRG system, including yearly reviews and changes to the MS-DRGs, we refer readers to the previous discussions in the FY 2010 IPPS/RY 2010 LTCH PPS final rule (74 FR 43764 through 43766) and the FYs 2011 through 2019 IPPS/LTCH PPS final rules (75 FR 50053 through 50055; 76 FR 51485 through 51487; 77 FR 53273; 78 FR 50512; 79 FR 49871; 80 FR 49342; 81 FR 56787 through 56872; 82 FR 38010 through 38085, and 83 FR 41158 through 41258, respectively).
C. Adoption of the MS-DRGs in FY 2008
For information on the adoption of the MS-DRGs in FY 2008, we refer readers to the FY 2008 IPPS final rule with comment period (72 FR 47140 through 47189).
D. FY 2020 MS-DRG Documentation and Coding Adjustment
1. Background on the Prospective MS-DRG Documentation and Coding Adjustments for FY 2008 and FY 2009 Authorized by Public Law 110-90 and the Recoupment or Repayment Adjustment Authorized by Section 631 of the American Taxpayer Relief Act of 2012 (ATRA)
In the FY 2008 IPPS final rule with comment period (72 FR 47140 through 47189), we adopted the MS-DRG patient classification system for the IPPS, effective October 1, 2007, to better recognize severity of illness in Medicare payment rates for acute care hospitals. The adoption of the MS-DRG system resulted in the expansion of the number of DRGs from 538 in FY 2007 to 745 in FY 2008. By increasing the number of MS-DRGs and more fully taking into account patient severity of illness in Medicare payment rates for acute care hospitals, MS-DRGs encourage hospitals to improve their documentation and coding of patient diagnoses.
In the FY 2008 IPPS final rule with comment period (72 FR 47175 through 47186), we indicated that the adoption of the MS-DRGs had the potential to lead to increases in aggregate payments without a corresponding increase in actual patient severity of illness due to the incentives for additional documentation and coding. In that final rule with comment period, we exercised our authority under section 1886(d)(3)(A)(vi) of the Act, which authorizes us to maintain budget neutrality by adjusting the national standardized amount, to eliminate the estimated effect of changes in coding or classification that do not reflect real changes in case-mix. Our actuaries estimated that maintaining budget neutrality required an adjustment of −4.8 percentage points to the national standardized amount. We provided for phasing in this −4.8 percentage point adjustment over 3 years. Specifically, we established prospective documentation and coding adjustments of −1.2 percentage points for FY 2008, −1.8 percentage points for FY 2009, and −1.8 percentage points for FY 2010.
On September 29, 2007, Congress enacted the TMA [Transitional Medical Assistance], Abstinence Education, and QI [Qualifying Individuals] Programs Extension Act of 2007 (Pub. L. 110-90). Section 7(a) of Public Law 110-90 reduced the documentation and coding adjustment made as a result of the MS-DRG system that we adopted in the FY 2008 IPPS final rule with comment period to −0.6 percentage point for FY 2008 and −0.9 percentage point for FY 2009.
As discussed in prior year rulemakings, and most recently in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56780 through 56782), we implemented a series of adjustments required under sections 7(b)(1)(A) and 7(b)(1)(B) of Public Law 110-90, based on a retrospective review of FY 2008 and FY 2009 claims data. We completed these adjustments in FY 2013 but indicated in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53274 through 53275) that delaying full implementation of the adjustment required under section 7(b)(1)(A) of Public Law 110-90 until FY 2013 resulted in payments in FY 2010 through FY 2012 being overstated, and that these overpayments could not be recovered under Public Law 110-90.
In addition, as discussed in prior rulemakings and most recently in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38008 through 38009), section 631 of the ATRA amended section 7(b)(1)(B) of Public Law 110-90 to require the Secretary to make a recoupment adjustment or adjustments totaling $11 billion by FY 2017. This adjustment represented the amount of the increase in aggregate payments as a result of not completing the prospective adjustment authorized under section 7(b)(1)(A) of Public Law 110-90 until FY 2013.
2. Adjustments Made for FY 2018 and FY 2019 as Required Under Section 414 of Public Law 114-10 (MACRA) and Section 15005 of Public Law 114-255
As stated in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56785), once the recoupment required under section 631 of the ATRA was complete, we had anticipated making a single positive adjustment in FY 2018 to offset the reductions required to recoup the $11 billion under section 631 of the ATRA. However, section 414 of the MACRA (which was enacted on April 16, 2015) replaced the single positive adjustment we intended to make in FY 2018 with a 0.5 percentage point positive adjustment for each of FYs 2018 through 2023. In the FY 2017 rulemaking, we indicated that we would address the adjustments for FY 2018 and later fiscal years in future rulemaking. Section 15005 of the 21st Century Cures Act (Pub. L. 114-255), which was enacted on December 13, 2016, amended section 7(b)(1)(B) of the TMA, as amended by section 631 of the ATRA and section 414 of the MACRA, to reduce the adjustment for FY 2018 from a 0.5 percentage point positive adjustment to a 0.4588 percentage point positive adjustment. As we discussed in the FY 2018 rulemaking, we believe the directive under section 15005 of Public Law 114-255 is clear. Therefore, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38009) for FY 2018, we implemented the required +0.4588 percentage point adjustment to the standardized amount. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41157), consistent with the requirements of section 414 of the MACRA, we implemented a 0.5 percentage point positive adjustment to the standardized amount for FY 2019. We indicated that both the FY 2018 and FY 2019 adjustments were permanent adjustments to payment rates. We also stated that we plan to propose future adjustments required under section 414 of the MACRA for FYs 2020 through 2023 in future rulemaking.
3. Adjustment for FY 2020
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19170 through 19171) consistent with the requirements of section 414 of the MACRA, we proposed to implement a 0.5 percentage point positive adjustment to the standardized amount for FY 2020. We indicated that this would constitute a permanent adjustment to payment rates. We stated in the proposed rule that we plan to propose future adjustments required under section 414 of the MACRA for FYs 2021 through 2023 in future rulemaking.
Comment: Several commenters stated that in order to comply with ATRA requirements, CMS anticipated that a cumulative −3.2 percentage point adjustment to the standardized amount would achieve the mandated $11 billion recoupment. Commenters stated that CMS misinterpreted the relevant statutory authority, which they asserted explicitly assumes that recoupment under section 631 of the ATRA would result in an estimated −3.2 percentage point cumulative adjustment by FY 2017. Commenters asserted that the additional −0.7 percentage point adjustment made in FY 2017 has been improperly continued in FY 2018 and FY 2019, and failure to restore the additional 0.7 percentage point adjustment will make this reduction in hospital payments a permanent part of the baseline calculation of the IPPS rates, which, they contend, was not Congress's legislative intent in implementing the series of adjustments required under section 414 of the MACRA. Commenters urged CMS to use its exceptions and adjustments authority under section 1886(d)(5)(I) to restore an additional 0.7 percentage point payment adjustment in FY2020 to restore payment equity to hospitals and comply with what they asserted was Congressional intent. Other commenters suggested CMS implement an approximate positive adjustment of 1.0 percentage point by FY 2024 to fully and permanently restore the entire −3.9 percentage point recoupment adjustment to IPPS rates. A commenter requested that CMS provide its rationale for failing to do so. Finally, some of the commenters, while acknowledging that CMS may be bound by law, expressed opposition to the permanent reductions and requested that CMS refrain from making any additional coding adjustments in the future.
Response: As we discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19170 through 19171), and in response to similar comments in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41157), we believe section 414 of the MACRA and section 15005 of the 21st Century Cures Act set forth the levels of positive adjustments for FYs 2018 through 2023. We are not convinced that the adjustments prescribed by MACRA were predicated on a specific adjustment level estimated or implemented by CMS in previous rulemaking. While we had anticipated making a positive adjustment in FY 2018 to offset the reductions required to recoup the $11 billion under section 631 of the ATRA, section 414 of the MACRA required that we implement a 0.5 percentage point positive adjustment for each of FYs 2018 through 2023, and not the single positive adjustment we intended to make in FY 2018. As discussed in the FY 2017 IPPS/LTCH PPS final rule, by phasing in a total positive adjustment of only 3.0 percentage points, section 414 of the MACRA would not fully restore even the 3.2 percentage point adjustment originally estimated by CMS in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50515). Moreover, as discussed in the FY 2018 IPPS/LTCH PPS final rule, Public Law 114-255, which further reduced the positive adjustment required for FY 2018 from 0.5 percentage point to 0.4588 percentage point, was enacted on December 13, 2016, after CMS had proposed and finalized the final negative −1.5 percentage point adjustment required under section 631 of the ATRA. We see no evidence that Congress enacted these adjustments with the intent that CMS would make an additional +0.7 percentage point adjustment in FY 2018 to compensate for the higher than expected final ATRA adjustment made in FY 2017, nor are we persuaded that it would be appropriate to use the Secretary's exceptions and adjustments authority under section 1886(d)(5)(I) of the Act to adjust payments in FY 2020 to restore any additional amount of the original 3.9 percentage point reduction, given Congress' prescriptive adjustment levels under section 414 of the MACRA and section 15005 of the 21st Century Cures Act.
After consideration of the public comments we received, we are finalizing our proposal to implement a 0.5 percentage point adjustment to the standardized amount for FY 2020.
E. Refinement of the MS-DRG Relative Weight Calculation
1. Background
Beginning in FY 2007, we implemented relative weights for DRGs based on cost report data instead of charge information. We refer readers to the FY 2007 IPPS final rule (71 FR 47882) for a detailed discussion of our final policy for calculating the cost-based DRG relative weights and to the FY 2008 IPPS final rule with comment period (72 FR 47199) for information on how we blended relative weights based on the CMS DRGs and MS-DRGs. We also refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 56785 through 56787) for a detailed discussion of the history of changes to the number of cost centers used in calculating the DRG relative weights. Since FY 2014, we have calculated the IPPS MS-DRG relative weights using 19 CCRs, which now include distinct CCRs for implantable devices, MRIs, CT scans, and cardiac catheterization.
2. Discussion of Policy for FY 2020
Consistent with our established policy, we calculated the final MS-DRG relative weights for FY 2020 using two data sources: The MedPAR file as the claims data source and the HCRIS as the cost report data source. We adjusted the charges from the claims to costs by applying the 19 national average CCRs developed from the cost reports. The description of the calculation of the 19 CCRs and the MS-DRG relative weights for FY 2020 is included in section II.G. of the preamble to this FY 2020 IPPS/LTCH PPS final rule. As we did with the FY 2019 IPPS/LTCH PPS final rule, for this FY 2020 final rule, we are providing the version of the HCRIS from which we calculated these 19 CCRs on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. Click on the link on the left side of the screen titled “FY 2020 IPPS Final Rule Home Page” or “Acute Inpatient Files for Download.”
Comment: A commenter recommended that CMS work with stakeholders to update cost reporting instructions and improve the accuracy and validity of the national average CCRs. The commenter expressed concern that the differences between hospitals' use of nonstandard cost center codes and CMS' procedures for mapping and rolling up nonstandard codes to the standard cost centers will continue to result in invalid CCRs and inaccurate payments. The commenter stressed the need for flexibility in cost reporting, to accommodate any new or unique services that certain hospitals may provide, which may not be easily captured through the cost reporting software. Finally, the commenter again recommended, as it had done in response to prior IPPS rules, that CMS pay particular attention to data used for CT scan and MRI cost centers; the commenter believed that the hospital payment rates established by CMS from the CT scan and MRI CCRs simply do not correlate with resources used for these capital-intensive services.
Response: We have addressed similar public comments in prior rulemaking and refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 56787) for our response to these issues. We note that we will continue to explore ways in which we can improve the accuracy of the cost report data and calculated CCRs used in the cost estimation process.
F. Changes to Specific MS-DRG Classifications
1. Discussion of Changes to Coding System and Basis for FY 2020 MS-DRG Updates
a. Conversion of MS-DRGs to the International Classification of Diseases, 10th Revision (ICD-10)
As of October 1, 2015, providers use the International Classification of Diseases, 10th Revision (ICD-10) coding system to report diagnoses and procedures for Medicare hospital inpatient services under the MS-DRG system instead of the ICD-9-CM coding system, which was used through September 30, 2015. The ICD-10 coding system includes the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) for diagnosis coding and the International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS) for inpatient hospital procedure coding, as well as the ICD-10-CM and ICD-10-PCS Official Guidelines for Coding and Reporting. For a detailed discussion of the conversion of the MS-DRGs to ICD-10, we refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 56787 through 56789).
b. Basis for FY 2020 MS-DRG Updates
CMS has previously encouraged input from our stakeholders concerning the annual IPPS updates when that input was made available to us by December 7 of the year prior to the next annual proposed rule update. As discussed in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38010), as we work with the public to examine the ICD-10 claims data used for updates to the ICD-10 MS-DRGs, we would like to examine areas where the MS-DRGs can be improved, which will require additional time for us to review requests from the public to make specific updates, analyze claims data, and consider any proposed updates. Given the need for more time to carefully evaluate requests and propose updates, we changed the deadline to request updates to the MS-DRGs to November 1 of each year. This will provide an additional 5 weeks for the data analysis and review process. Interested parties had to submit any comments and suggestions for FY 2020 by November 1, 2018, and should submit any comments and suggestions for FY 2021 by November 1, 2019 via the CMS MS-DRG Classification Change Request Mailbox located at: MSDRGClassificationChange@cms.hhs.gov. The comments that were submitted in a timely manner for FY 2020 are discussed in this section of the preamble of this final rule. As discussed in the proposed rule and in the sections that follow, we may not be able to fully consider all of the requests that we receive for the upcoming fiscal year. We have found that, with the implementation of ICD-10, some types of requested changes to the MS-DRG classifications require more extensive research to identify and analyze all of the data that are relevant to evaluating the potential change. We note in the discussion that follows those topics for which further research and analysis are required, and which we will continue to consider in connection with future rulemaking.
Following are the changes that we proposed to the MS-DRGs for FY 2020 in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19171 through 19257). We invited public comments on each of the MS-DRG classification proposed changes, as well as our proposals to maintain certain existing MS-DRG classifications discussed in the proposed rule. In some cases, we proposed changes to the MS-DRG classifications based on our analysis of claims data and consultation with our clinical advisors. In other cases, we proposed to maintain the existing MS-DRG classifications based on our analysis of claims data and consultation with our clinical advisors. For the FY 2020 IPPS/LTCH PPS proposed rule, our MS-DRG analysis was based on ICD-10 claims data from the September 2018 update of the FY 2018 MedPAR file, which contains hospital bills received through September 30, 2018, for discharges occurring through September 30, 2018. In our discussion of the proposed MS-DRG reclassification changes, we referred to our analysis of claims data from the “September 2018 update of the FY 2018 MedPAR file.”
In this FY 2020 IPPS/LTCH PPS final rule, we summarize the public comments we received on our proposals, present our responses, and state our final policies. For this FY 2020 final rule, we generally did not perform any further MS-DRG analysis of claims data. Therefore, our MS-DRG analysis is based on ICD-10 claims data from the September 2018 update of the FY 2018 MedPAR file, which contains hospital bills received through September 30, 2018, for discharges occurring through September 30, 2018, except as otherwise noted.
As explained in previous rulemaking (76 FR 51487), in deciding whether to propose to make further modifications to the MS-DRGs for particular circumstances brought to our attention, we consider whether the resource consumption and clinical characteristics of the patients with a given set of conditions are significantly different than the remaining patients represented in the MS-DRG. We evaluate patient care costs using average costs and lengths of stay and rely on the judgment of our clinical advisors to determine whether patients are clinically distinct or similar to other patients represented in the MS-DRG. In evaluating resource costs, we consider both the absolute and percentage differences in average costs between the cases we select for review and the remainder of cases in the MS-DRG. We also consider variation in costs within these groups; that is, whether observed average differences are consistent across patients or attributable to cases that are extreme in terms of costs or length of stay, or both. Further, we consider the number of patients who will have a given set of characteristics and generally prefer not to create a new MS-DRG unless it would include a substantial number of cases.
In our examination of the claims data, we apply the following criteria established in FY 2008 (72 FR 47169) to determine if the creation of a new complication or comorbidity (CC) or major complication or comorbidity (MCC) subgroup within a base MS-DRG is warranted:
- A reduction in variance of costs of at least 3 percent;
- At least 5 percent of the patients in the MS-DRG fall within the CC or MCC subgroup;
- At least 500 cases are in the CC or MCC subgroup;
- There is at least a 20-percent difference in average costs between subgroups; and
- There is a $2,000 difference in average costs between subgroups.
In order to warrant creation of a CC or MCC subgroup within a base MS-DRG, the subgroup must meet all five of the criteria.
We are making the FY 2020 ICD-10 MS-DRG GROUPER and Medicare Code Editor (MCE) Software Version 37, the ICD-10 MS-DRG Definitions Manual files Version 37 and the Definitions of Medicare Code Edits Manual Version 37 available to the public on our CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html.
2. Pre-MDC
a. Peripheral ECMO
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41166 through 41169), we discussed a request we received to review cases reporting the use of extracorporeal membrane oxygenation (ECMO) in combination with the insertion of a percutaneous short-term external heart assist device. We also noted that a separate request to create a new ICD-10-PCS procedure code specifically for percutaneous ECMO was discussed at the March 6-7, 2018 ICD-10 Coordination and Maintenance Committee Meeting for which we finalized the creation of three new procedure codes to identify and describe different types of ECMO treatments currently being utilized. These three new procedure codes were included in the FY 2019 ICD-10-PCS procedure codes files (which are available via the internet on the CMS website at: https://www.cms.gov/Medicare/Coding/ICD10/2019-ICD-10-PCS.html) and were made publicly available in May 2018. We received recommendations from commenters on suggested MS-DRG assignments for the two new procedure codes that uniquely identify percutaneous (peripheral) ECMO, including assignment to MS-DRG 215 (Other Heart Assist System Implant), or to Pre-MDC MS-DRG 004 (Tracheostomy with Mechanical Ventilation >96 Hours or Principal Diagnosis Except Face, Mouth and Neck without Major O.R. Procedure) specifically for the new procedure code describing percutaneous veno-venous (VV) ECMO or an alternate MS-DRG within MDC 4 (Diseases and Disorders of the Respiratory System). In our response, we noted that because these codes were not finalized at the time of the proposed rule, there were no proposed MDC or MS-DRG assignments or O.R. and non-O.R. designations for these new procedure codes and they were not reflected in Table 6B.—New Procedure Codes (which is available via the internet on the CMS website at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) associated with the FY 2019 IPPS/LTCH PPS proposed rule.
We further noted that, consistent with our annual process of assigning new procedure codes to MDCs and MS-DRGs, and designating a procedure as an O.R. or non-O.R. procedure, we reviewed the predecessor procedure code assignment. For the reasons discussed in the FY 2019 IPPS/LTCH PPS final rule, our clinical advisors did not support assigning the new procedure codes for the percutaneous (peripheral) ECMO procedures to the same MS-DRG as the predecessor code for open (central) ECMO in pre-MDC MS-DRG 003.
Effective with discharges occurring on and after October 1, 2018, the three ECMO procedure codes and their corresponding MS-DRG assignments are as shown in the following table.

As noted in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19173), after publication of the FY 2019 IPPS/LTCH PPS final rule, we received comments and feedback from stakeholders expressing concern with the MS-DRG assignments for the two new procedure codes describing peripheral ECMO. Specifically, these stakeholders stated that: (1) The MS-DRG assignments for ECMO should not be based on how the patient is cannulated (open versus peripheral) because most of the costs for both central and peripheral ECMO can be attributed to the severity of illness of the patient; (2) there was a lack of opportunity for public comment on the finalized MS-DRG assignments; (3) patient access to ECMO treatment and programs is now at risk because of inadequate payment; and (4) CMS did not appear to have access to enough patient data to evaluate for appropriate MS-DRG assignment consideration. They also stated that the new procedure codes do not account for an open cut-down approach that may be performed on a peripheral vessel during a peripheral ECMO procedure. These stakeholders recommended that, consistent with the usual process of assigning new procedure codes to the same MS-DRG as the predecessor code, the MS-DRG assignment for peripheral ECMO procedures should be revised to allow assignment of peripheral ECMO procedures to Pre-MDC MS-DRG 003 (ECMO or Tracheostomy with Mechanical Ventilation >96 Hours or Principal Diagnosis Except Face, Mouth and Neck with Major O.R. Procedure). They stated that this revision would also allow for the collection of further claims data for patients treated with ECMO and assist in determining the appropriateness of any future modifications in MS-DRG assignment.
We also received feedback from a few stakeholders that, for some cases involving peripheral ECMO, the current designation provides compensation that these stakeholders believe is “reasonable” (for example, for peripheral ECMO in certain patients admitted with acute respiratory failure and sepsis). Some of these stakeholders agreed with CMS that once claims data become available, the volume, length of stay and cost data of claims with these new codes can be examined to determine if modifications to MS-DRG assignment or O.R. and non-O.R. designation are warranted. However, some of these stakeholders also expressed concerns that the current assignments and designation do not appropriately compensate for the resources used when peripheral ECMO is used to treat certain patients (for example, patients who are admitted with cardiac arrest and cardiogenic shock of known cause or patients admitted with a different principal diagnosis or patients who develop a diagnosis after admission that requires ECMO). These stakeholders stated that the current MS-DRG assignments for such cases involving peripheral ECMO do not provide sufficient payment and do not fully consider the severity of illness of the patient and the level of resources involved in treating such patients, such as surgical team, general anesthesia, and other ECMO support such as specialized monitoring.
We stated in the proposed rule that with regard to stakeholders' concerns that we did not allow the opportunity for public comment on the MS-DRG assignment for the three new procedure codes that describe central and peripheral ECMO, as noted above and as explained in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41168), these new procedure codes were not finalized at the time of the proposed rule. We noted that although there were no proposed MDC or MS-DRG assignment or O.R. and non-O.R. designations for these three new procedure codes, we did, in fact, review and respond to comments on the recommended MDC and MS-DRG assignments and O.R./non-O.R. designations in the final rule (83 FR 41168 through 41169). For FY 2019, consistent with our annual process of assigning new procedure codes to MDCs and MS-DRGs and designating a procedure as an O.R. or non-O.R. procedure, we reviewed the predecessor procedure code assignments. Upon completing the review, our clinical advisors did not support assigning the two new ICD-10-PCS procedure codes for peripheral ECMO procedures to the same MS-DRG as the predecessor code for open (central) ECMO procedures. Further, our clinical advisors also did not agree with designating peripheral ECMO procedures as O.R. procedures because they stated that these procedures are less resource intensive compared to open ECMO procedures.
As noted, our annual process for assigning new procedure codes involves review of the predecessor procedure code's MS-DRG assignment. However, this process does not automatically result in the new procedure code being assigned (or proposed for assignment) to the same MS-DRG as the predecessor code. There are several factors to consider during this process that our clinical advisors take into account. For example, in the absence of volume, length of stay, and cost data, they may consider the specific service, procedure, or treatment being described by the new procedure code, the indications, treatment difficulty, and the resources utilized. For FY 2020, as discussed in the FY 2020 IPPS/LTCH PPS proposed rule, we have continued to consider how these and other factors may apply in the context of classifying procedures under the ICD-10 MS-DRGs, including with regard to the specific concerns raised by stakeholders.
In the absence of claims data for the new ICD-10-PCS procedure codes describing peripheral ECMO, we analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for cases reporting the predecessor ICD-10-PCS procedure code 5A15223 (Extracorporeal membrane oxygenation, continuous) in Pre-MDC MS-DRG 003, including those cases reporting secondary diagnosis MCC and CC conditions, that were grouped under the ICD-10 MS-DRG Version 35 GROUPER. Our findings are shown in the table below.

The total number of cases reported in MS-DRG 003 was 14,456, with an average length of stay of 29.6 days and average costs of $122,168. For the cases reporting procedure code 5A15223 (Extracorporeal membrane oxygenation, continuous), there was a total of 2,086 cases, with an average length of stay of 20.2 days and average costs of $128,168. For the cases reporting procedure code 5A15223 with an MCC, there was a total 9 of 2,000 cases, with an average length of stay of 20.7 days and average costs of $131,305. For the cases reporting procedure 5A15223 with a CC, there was a total of 79 cases, with an average length of stay of 7.6 days and average costs of $58,231.
In the proposed rule, we stated that our clinical advisors reviewed these data and noted that the average length of stay for the cases reporting ECMO with procedure code 5A15223 of 20.2 days may not necessarily be a reliable indicator of resources that can be attributed to ECMO treatment. We also stated that our clinical advisors believed that a more appropriate measure of resource consumption for ECMO would be the number of hours or days that a patient was specifically receiving ECMO treatment, rather than the length of hospital stay. However, they noted that this information is not currently available in the claims data. Further, we noted that our clinical advisors also stated that the average costs of $128,168 for the cases reporting ECMO with procedure code 5A15223 are not necessarily reflective of the resources utilized for ECMO treatment alone, as the average costs represent a combination of factors, including the principal diagnosis, any secondary diagnosis CC and/or MCC conditions necessitating initiation of ECMO, and potentially any other procedures that may be performed during the hospital stay. Our clinical advisors recognized that patients who require ECMO treatment are severely ill and recommended we review the claims data to identify the number (frequency) and types of principal and secondary diagnosis CC and/or MCC conditions that were reported among the 2,086 cases reporting procedure code 5A15223. Our findings are shown in the following tables for the top 10 principal diagnosis codes, followed by the top 10 secondary diagnosis MCC and secondary diagnosis CC conditions that were reported within the claims data with procedure code 5A15223.



We stated in the proposed rule that these data show that the conditions reported for these patients requiring treatment with ECMO and reported with predecessor ICD-10-PCS procedure code 5A1223 represent a greater severity of illness, present greater treatment difficulty, have poorer prognoses, and have a greater need for intervention. While the data analysis was based on the conditions reported with the predecessor ICD-10-PCS procedure code 5A1223 (Extracorporeal membrane oxygenation, continuous), we stated that our clinical advisors believe the data may provide an indication of how cases reporting the new procedure codes describing peripheral (percutaneous) ECMO may be represented in future claims data with regard to indications for treatment, a patient's severity of illness, resource utilization, and treatment difficulty.
Based on the results of our data analysis and further review of the cases reporting ECMO, including consideration of the stakeholders' concerns that the MS-DRG assignments for ECMO procedures should not be based on the method of cannulation, we stated in the proposed rule that our clinical advisors agreed that resource consumption for both central and peripheral ECMO cases can be primarily attributed to the severity of illness of the patient, and that the method of cannulation is less relevant when considering the overall resources required to treat patients on ECMO. Specifically, we stated that our clinical advisors noted that consideration of resource consumption for cases reporting the use of ECMO may extend well beyond the duration of time that a patient was actively receiving ECMO treatment, which may range anywhere from less than 24 hours to 10 days or more. As noted in the proposed rule and above, in the absence of unique procedure codes that specify the duration of time that a patient was receiving ECMO treatment, we cannot ascertain from the claims data the resource use specifically attributable to treatment with ECMO during a hospital stay (84 FR 19175). However, when reviewing consumption of hospital resources for the cases in which ECMO was reported during a hospital stay, the claims data clearly show that the patients placed on ECMO typically have multiple MCC and CC conditions. These data provide additional information on the expanding indications for ECMO treatment as well as an indication of the complexities and the treatment difficulty associated with these patients. We also stated in the proposed rule that, while our clinical advisors continue to believe that central (open) ECMO may be more resource intensive and carries significant risks for complications, including bleeding, infection, and vessel injury because it requires an incision along the sternum (sternotomy) and is performed for open heart surgery, they believe that the subset of patients who require treatment with ECMO, regardless of the cannulation method, would be similar in terms of overall hospital resource consumption. We also noted that while we do not yet have Medicare claims data to evaluate the new peripheral ECMO procedure codes, review of limited registry data provided by stakeholders for patients treated with a reported peripheral ECMO procedure did not contradict that costs for peripheral ECMO appear to be similar to the costs of overall resources required to treat patients on ECMO (regardless of method of cannulation) and appear to be attributable to the severity of illness of the patient.
With regard to stakeholders who stated that the two new procedure codes do not account for an open cut-down approach that may be performed on a peripheral vessel during a peripheral ECMO procedure, we noted in the proposed rule that a request and proposal to create ICD-10-PCS codes to differentiate between peripheral vessel percutaneous and peripheral vessel open cutdown according to the indication (VA or VV) for ECMO was discussed at the March 5-6, 2019 ICD-10 Coordination and Maintenance Committee meeting. We refer readers to the website at: https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD-9-CM-C-and-M-Meeting-Materials.html for the committee meeting materials and discussion regarding this proposal. We also noted that, in this same proposal, another coding option to add duration values to allow the reporting of the number of hours or the number of days a patient received ECMO during the stay was also made available for public comment.
Upon further review and consideration of peripheral ECMO procedures, including the indications, treatment difficulty, and the resources utilized, for the reasons discussed above, in the FY 2020 IPPS/LTCH PPS proposed rule, we stated that our clinical advisors supported the assignment of the new ICD-10-PCS procedure codes for peripheral ECMO procedures to the same MS-DRG as the predecessor code for open (central) ECMO procedures for FY 2020. Therefore, based on our review, including consideration of the comments and input from our clinical advisors, we proposed to reassign the following procedure codes describing peripheral ECMO procedures from their current MS-DRG assignments to Pre-MDC MS-DRG 003 (ECMO or Tracheostomy with Mechanical Ventilation >96 Hours or Principal Diagnosis Except Face, Mouth and Neck with Major O.R. Procedure) as shown in the table below. We stated in the proposed rule that, if this proposal is finalized, we also would make conforming changes to the titles for MS-DRGs 207, 291, 296, and 870 to no longer reflect the “or Peripheral Extracorporeal Membrane Oxygenation (ECMO)” terminology in the title. We also noted in the proposed rule that this proposal included maintaining the designation of these peripheral ECMO procedures as non-O.R. Therefore, we stated in the proposed rule that, if finalized, the procedures would be defined as non-O.R. affecting the MS-DRG assignment for Pre-MDC MS-DRG 003.
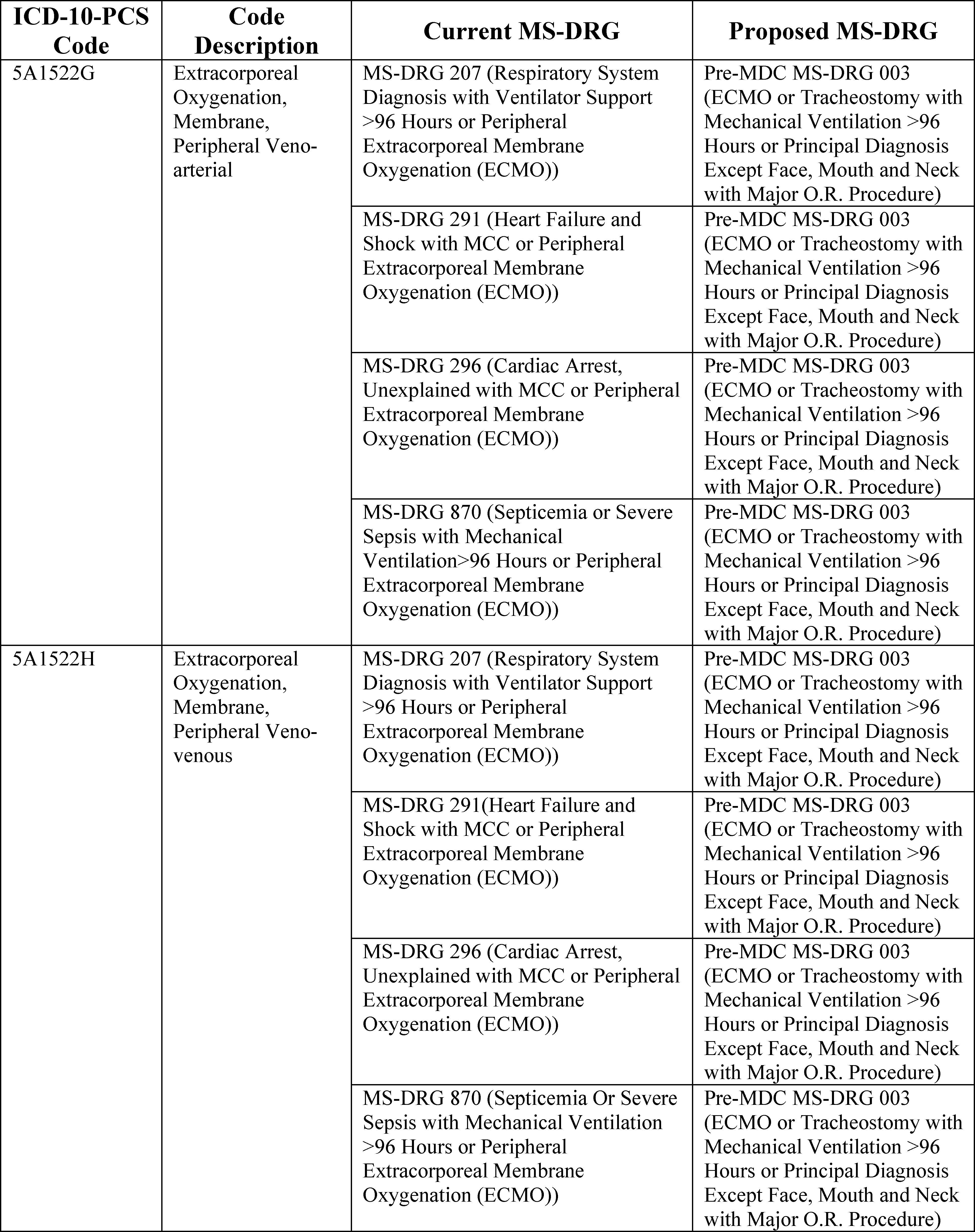
Comment: Several commenters expressed support for the proposal to reassign procedure codes 5A1522G and 5A1522H describing peripheral ECMO procedures from their current MS-DRG assignments to Pre-MDC MS-DRG 003 and to revise the titles for MS-DRGs 207, 291, 296 and 870 as shown in the table above. The commenters stated that this reassignment more appropriately reflects the resource utilization of patients requiring this treatment. A commenter also stated their appreciation of CMS' research for the proposal which they believe was needed to maintain the financial viability of ECMO programs. Another commenter stated they agreed with the non-O.R. designation of peripheral ECMO procedures noting these procedures are typically performed at the bedside or in an ICU setting due to the emergent condition of the patient. This commenter also stated that the delivery of ECMO support in a non-O.R. setting does not diminish the resource intensive nature of the treatment however, and therefore agreed with the designation of non-O.R. affecting Pre-MDC MS-DRG 003.
Response: We thank the commenters for their support.
Comment: A few commenters recommended that ICD-10-PCS procedure codes 5A1522G and 5A1522H be assigned to MS-DRG 215 (Other Heart Assist System Implant) as opposed to Pre-MDC MS-DRG 003. The commenters stated that MS-DRG 215 is the primary MS-DRG for peripheral heart assist pumps with similar patient conditions and clinical coherence. A commenter stated that assigning percutaneous (peripheral) ECMO into a different category for payment than percutaneous VAD (Ventricular Assist Device) creates a system of winners and losers by device.
Response: We thank the commenters for their recommendation. We note that as stated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41168), in cases where a percutaneous external heart assist device is utilized, in combination with a percutaneous ECMO procedure, effective October 1, 2018, the ICD-10 MS-DRG GROUPER logic results in a case assignment to MS-DRG 215 because the percutaneous external heart assist device procedure is designated as an O.R. procedure and assigned to MS-DRG 215. We also note that under the ICD-10-PCS classification, ECMO is not defined as a device. The procedure codes in Table 5A0, specifically any procedure code for ECMO, do not contain a device value for the sixth character, rather they contain a function value for the sixth character to identify oxygenation.
Comment: A commenter expressed concern with the proposal to continue designating peripheral ECMO procedures as non-O.R. procedures, however, the commenter acknowledged that these procedures may be performed in non-O.R. locations such as the ER or ICU. The commenter noted that the determining factor for the location where ECMO is initiated is typically dictated by the patient's situation. According to the commenter, for critically ill patients who require life-saving ECMO, cannulation and initiation of the ECMO circuit is usually done in an emergent manner. The commenter also noted that these patients are often at risk of imminent death and cannot safely be moved to another location for cannulation and ECMO initiation. The commenter requested that CMS review the designation of the ECMO codes and consider the unique nature of these procedures during the comprehensive review of the ICD-10-PCS procedure codes.
Response: We appreciate the commenter's feedback. As noted in the proposed rule and in section II.F.13.a. of the preamble of this final rule, we plan to conduct a comprehensive, systematic review of the ICD-10-PCS procedure codes, including the ECMO procedure codes, and as part of that comprehensive procedure code review, we will also review the process for determining when a procedure is considered an operating room procedure.
Comment: A commenter noted that the FY 2020 ICD-10-PCS codes were made publicly available in June 2019 and that new procedure codes describing intraoperative ECMO were created. The commenter requested that CMS provide guidance on the correct reporting of these procedure codes when performed in the cardiac catheterization lab, the electrophysiology lab or other inpatient places of service, including the O.R., since the designation of these new procedure codes is non-O.R.
Response: The commenter is correct that the FY 2020 ICD-10-PCS procedure code files were made publicly available in June 2019 (which are available via the internet on the CMS website at: https://www.cms.gov/Medicare/Coding/ICD10/2020-ICD-10-PCS.html) and that new procedure codes describing intraoperative ECMO have been created. As shown in Table 6B.—New Procedure Codes, associated with this final rule (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html), procedure codes 5A15A2F (Extracorporeal oxygenation, membrane, central, intraoperative), 5A15A2G (Extracorporeal oxygenation, membrane, peripheral veno-arterial, intraoperative) and 5A15A2H (Extracorporeal oxygenation, membrane, peripheral veno-venous, intraoperative) are effective with discharges on and after October 1, 2019 and are designated as non-O.R. procedures. We note that, historically, we have not provided coding advice in rulemaking with respect to policy. We collaborate with the American Hospital Association (AHA) through the Coding Clinic for ICD-10-CM and ICD-10-PCS to promote proper coding (81 FR 56841).
Comment: Some commenters suggested that CMS should assign the new procedure codes describing intraoperative peripheral ECMO procedures (as discussed above) to Pre-MDC MS-DRG 003 until claims data is available to analyze their impact on resource utilization.
Response: We appreciate the commenters' suggestion, however, as discussed at the ICD-10 Coordination and Maintenance Committee meeting held on March 5-6, 2019, the request (and subsequent finalization) for new procedure codes describing the intraoperative use of ECMO was specifically to address those situations in which the use of the ECMO was in support of a surgical (O.R.) procedure and the ECMO was discontinued at the conclusion of the procedure. For example, a patient who undergoes a lung transplant and receives ECMO support during the transplant procedure and the ECMO is discontinued at the conclusion of the lung transplant procedure. In this scenario, it is the lung transplant that is the surgical (O.R.) procedure and case assignment to MS-DRG 007 (Lung Transplant) by the GROUPER logic is what is appropriately reflected in the MedPAR claims data. As stated in the proposed rule and in this final rule, our annual process of assigning new procedure codes to MDCs and MS-DRGs, and designating a procedure as an O.R. or non-O.R. procedure involves review of the predecessor procedure code assignment. However, this process does not automatically result in the new procedure code being assigned to the same MS-DRG as the predecessor code. Consistent with our annual process of reviewing the MS-DRGs, we will continue to monitor cases to determine if any additional adjustments are warranted to account for changes in resource consumption.
Comment: A few commenters requested that CMS consider reprocessing claims for cases reporting procedure code 5A1522G or 5A1522H in MS-DRGs 207, 291, 296 or 870 in FY 2019 as a result of the financial impact it has had on providers and their belief that the codes were inappropriately classified. Specifically, commenters questioned if CMS would permit acute care hospitals to re-bill all FY 2019 ECMO cases under MS-DRG 003 to recoup lost revenues.
Response: As previously discussed, consistent with our annual process of assigning new procedure codes to MDCs and MS-DRGs, we reviewed the predecessor procedure code assignments, as well as other factors relevant to the MS-DRG assignment. As discussed in the proposed rule, after further consideration of these factors and review of these cases, including the data analysis described previously, CMS proposed to change the assignment of these cases beginning in FY 2020. As such, and consistent with our general approach to changes in MS-DRG assignment, the finalized policy we are adopting with regard to the assignment of cases reporting peripheral ECMO procedures is prospective, effective with discharges beginning in FY 2020 and is not applicable to discharges in FY 2019. We also note that section 1886(d)(5)(A) of the Act provides for Medicare payments to Medicare-participating hospitals in addition to the basic prospective payments for cases incurring extraordinarily high costs. To qualify for outlier payments, a case must have costs above a fixed-loss cost threshold amount (a dollar amount by which the costs of a case must exceed payments in order to qualify for outliers).
Comment: A commenter stated that Tables 7A and 7B associated with the proposed rule show a decline of the case counts in Pre-MDC MS-DRG 003 from Version 36 to Version 37 of the ICD-10 MS-DRG GROUPER (15,749 vs. 15,164). The commenter stated that under the current proposal to reassign cases reporting peripheral ECMO procedures, they would expect to see a shift in cases to Pre-MDC MS-DRG 003 from MS-DRGs 207, 291, 296, and 870 for the cases reporting procedures for peripheral ECMO. The commenter requested that CMS revisit these tables to provide insight and clarification concerning a potential issue with the surgical hierarchy given that the peripheral ECMO procedure codes are not recognized as O.R. procedures and the Version 36 volume of cases is higher than the Version 37 volume of cases based on the data within these tables.
Response: We reviewed the cases assigned to Pre-MDC MS-DRG 003 and found that the majority of the reduction in the case counts between Version 36 and Version 37 of the GROUPER was attributable to the proposed change in the designation of the ICD-10-PCS procedure codes describing bronchoalveolar lavage from O.R. to non-O.R. status, which is discussed in section II.F.13.b.1. of the preamble of this final rule. Since these procedures were the only operating room procedure reported for these cases, the proposed change in the O.R. status of these codes resulted in the reassignment or “shift” of these cases reporting these procedures from Pre-MDC MS-DRG 003 to Pre-MDC MS-DRG 004. As discussed in section II.F.13.b.1, we are finalizing this proposed change in designation for these procedure codes, and therefore Tables 7A and 7B associated with this final rule reflect similar “shifts” in the volume of cases reported to MS-DRG 003 between Version 36 and Version 37 of the GROUPER.
After consideration of the public comments we received, we are finalizing our proposal to reassign the procedure codes describing peripheral ECMO procedures from their current MS-DRG assignments to Pre-MDC MS-DRG 003 and maintain the designation of the peripheral ECMO procedures as non-O.R. We are also finalizing our proposal to make changes to the titles for MS-DRGs 207, 291, 296, and 870 to no longer reflect the “or Peripheral Extracorporeal Membrane Oxygenation (ECMO)” terminology in the title under the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
b. Allogeneic Bone Marrow Transplant
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19176), we received a request to create new MS-DRGs for cases that would identify patients who undergo an allogeneic hematopoietic cell transplant (HCT) procedure. The requestor asked us to split MS-DRG 014 (Allogeneic Bone Marrow Transplant) into two new MS-DRGs and assign cases to the recommended new MS-DRGs according to the donor source, with cases for allogeneic related matched donor source assigned to one MS-DRG and cases for allogeneic unrelated matched donor source assigned to the other MS-DRG. The requestor stated that by creating two new MS-DRGs for allogeneic related and allogeneic unrelated donor source, respectively, the MS-DRGs would more appropriately recognize the clinical characteristics and cost differences in allogeneic HCT cases.
The requestor stated that allogeneic related and allogeneic unrelated HCT cases are clinically different and have significantly different donor search and cell acquisition charges. According to the requestor, 70 percent of patients do not have a matched sibling donor (that is, an allogeneic related matched donor) in their family. The requestor also stated that this rate is higher for Medicare beneficiaries. According to the requestor, the current payment for allogeneic HCT cases is inadequate and affects patient's access to care.
The requestor performed its own analysis and stated that it found the average costs for HCT cases reporting revenue code 0815 (Stem cell acquisition) alone or revenue code 0819 (Other organ acquisition) in combination with revenue code 0815 with one of the ICD-10-PCS procedure codes for allogeneic unrelated donor source were significantly higher than the average costs for HCT cases reporting revenue code 0815 alone or both revenue codes 0815 and 0819 in combination with one of the ICD-10-PCS procedure codes for allogeneic related donor source. Further, the requestor reported that, according to its analysis, the average costs for HCT cases reporting revenue code 0815 alone or both revenue codes 0815 and 0819 in combination with one of the ICD-10-PCS procedure codes for unspecified allogeneic donor source were also significantly higher than the average costs for HCT cases reporting the ICD-10-PCS procedure codes for allogeneic related donor source. The requestor suggested that cases reporting the unspecified donor source procedure code are highly likely to represent unrelated donors, and recommended that, if the two new MS-DRGs are created as suggested, the cases reporting the procedure codes for unspecified donor source be included in the suggested new “unrelated donor” MS-DRG. The requestor also suggested that CMS apply a code edit through the inpatient Medicare Code Editor (MCE), similar to the edit in the Integrated Outpatient Code Editor (I/OCE) which requires reporting of revenue code 0815 on the claim with the appropriate procedure code or the claim may be subject to being returned to the provider.
As noted in the proposed rule, the ICD-10-PCS procedure codes assigned to MS-DRG 014 that identify related, unrelated and unspecified donor source for an allogeneic HCT are shown in the following table.

As noted in the FY 2020 IPPS/LTCH PPS proposed rule, we examined claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRG 014 and identified the subset of cases within MS-DRG 014 reporting procedure codes for allogeneic HCT related donor source, allogeneic HCT unrelated donor source, and allogeneic HCT unspecified donor source, respectively. Our findings are shown in the following table.

The total number of cases reported in MS-DRG 014 was 854, with an average length of stay of 28.2 days and average costs of $91,446. For the subset of cases reporting procedure codes for allogeneic HCT related donor source, there were a total of 292 cases with an average length of stay of 29.5 days and average costs of $87,444. For the subset of cases reporting procedure codes for allogeneic HCT unrelated donor source, there was a total of 466 cases with an average length of stay of 27.9 days and average costs of $95,146. For the subset of cases reporting procedure codes for allogeneic HCT unspecified donor source, there was a total of 90 cases with an average length of stay of 26.2 days and average costs of $90,945.
We stated in the proposed rule that based on the analysis described above, the current MS-DRG assignment for the cases in MS-DRG 014 that identify patients who undergo an allogeneic HCT procedure, regardless of donor source, appears appropriate. The data analysis reflects that each subset of cases reporting a procedure code for an allogeneic HCT procedure (that is, related, unrelated, or unspecified donor source) has an average length of stay and average costs that are comparable to the average length of stay and average costs of all cases in MS-DRG 014. We also noted that, in deciding whether to propose to make further modifications to the MS-DRGs for particular circumstances brought to our attention, we do not consider the reported revenue codes. Rather, as stated previously, we consider whether the resource consumption and clinical characteristics of the patients with a given set of conditions are significantly different than the remaining patients represented in the MS-DRG. We do this by evaluating the ICD-10-CM diagnosis and/or ICD-10-PCS procedure codes that identify the patient conditions, procedures, and the relevant MS-DRG(s) that are the subject of a request. Specifically, we stated that, for this request, as noted above, we analyzed the cases reporting the ICD-10-PCS procedure codes that identify an allogeneic HCT procedure according to the donor source. We then evaluated patient care costs using average costs and average lengths of stay (based on the MedPAR data) and rely on the judgment of our clinical advisors to determine whether the patients are clinically distinct or similar to other patients represented in the MS-DRG. We stated that because MS-DRG 014 is defined by patients who undergo an allogeneic HCT transplant procedure, our clinical advisors state they are all clinically similar in that regard. We also noted that the ICD-10-PCS procedure codes that describe an allogeneic HCT procedure were revised effective October 1, 2016 to uniquely identify the donor source in response to a request and proposal that was discussed at the March 9-10, 2016 ICD-10 Coordination and Maintenance Committee meeting. We refer readers to the website at: https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD-9-CM-C-and-M-Meeting-Materials.html for the committee meeting materials and discussion regarding this proposal.
In the proposed rule, in response to the requestor's statement that allogeneic related and allogeneic unrelated HCT cases are clinically different and have significantly different donor search and cell acquisition charges, we stated that our clinical advisors supported maintaining the current structure for MS-DRG 014 because they believe that MS-DRG 014 appropriately classifies all patients who undergo an allogeneic HCT procedures and, therefore, it is clinically coherent. While the requestor stated that there are clinical differences in the related and unrelated HCT cases, they did not provide any specific examples of these clinical differences. With regard to the donor search and cell acquisition charges, the requestor noted that the unrelated donor cases are more expensive than the related donor cases because of the donor search process, which includes a registry search to identify the best donor source, extensive donor screenings, evaluation, and cell acquisition and transportation services for the patient. The requestor appeared to base that belief according to the donor source and average charges reported with revenue code 0815. As noted in the proposed rule and above, we use MedPAR data and do not consider the reported revenue codes in deciding whether to propose to make further modifications to the MS-DRGs. Based on our analysis of claims data for MS-DRG 014, our clinical advisors stated that the resources are similar for patients who undergo an allogeneic HCT procedure regardless of the donor source.
In reviewing this request, we also reviewed the instructions on billing for stem cell transplantation in Chapter 3 of the Medicare Claims Processing Manual and found that there appears to be inadvertent duplication under Section 90.3.1 and Section 90.3.3 of Chapter 3, as both sections provide instructions on Billing for Stem Cell Transplantation. Therefore, in the proposed rule, we stated that we are further reviewing the Medicare Claims Processing Manual to identify potential revisions to address this duplication. However, we also noted that section 90.3.1 and section 90.3.3 provide different instruction regarding which revenue code should be reported. Section 90.3.1 instructs providers to report revenue code 0815 and Section 90.3.3 instructs providers to report revenue code 0819. We noted that we issued instructions as a One-Time Notification, Pub. No. 100-04, Transmittal 3571, Change Request 9674, effective January 1, 2017, which instructs that the appropriate revenue code to report on claims for allogeneic stem cell acquisition/donor services is revenue code 0815. Accordingly, in the proposed rule, we stated that we also are considering additional revisions as needed to conform the instructions for reporting these codes in the Medicare Claims Processing Manual.
With regard to the requestor's recommendation that we create a new code edit through the inpatient MCE similar to the edit in the I/OCE which requires reporting of revenue code 0815 on the claim, in the proposed rule we noted that the MCE is not designed to include revenue codes for claims editing purposes. Rather, as stated in section II.F.16. of the preamble of this final rule, it is a software program that detects and reports errors in the coding of Medicare claims data. The coding of Medicare claims data refers to diagnosis and procedure coding, as well as demographic information.
For the reasons described above, in the FY 2020 IPPS/LTCH PPS proposed rule, we did not propose to change the current structure of MS-DRG 014. In addition, we did not propose to split MS-DRG 014 into two new MS-DRGs that assign cases according to whether the allogeneic donor source is related or unrelated, as the requestor suggested.
In addition, while conducting our analysis of cases reporting ICD-10-PCS procedure codes for allogeneic HCT procedures that are assigned to MS-DRG 014, in the proposed rule, we noted that 8 procedure codes for autologous HCT procedures are currently included in MS-DRG 014, as shown in the following table. We stated that these codes are not properly assigned because MS-DRG 014 is defined by cases reporting allogenic HCT procedures.
In the proposed rule, we stated that the 8 ICD-10-PCS procedure codes for autologous HCT procedures were inadvertently included in MS-DRG 014 as a result of efforts to replicate the ICD-9-CM MS-DRGs. Under the ICD-9-CM MS-DRGs, procedure code 41.06 (Cord blood stem cell transplant) was used to identify these procedures and was also assigned to MS-DRG 014. As shown in the ICD-9-CM code description, the reference to “autologous” is not included. However, because the ICD-10-PCS autologous HCT procedure codes were considered as plausible translations of the ICD-9-CM procedure code (41.06), they were inadvertently included in MS-DRG 014. We also noted that, of these 8 procedure codes, there are 4 procedure codes that describe a transfusion via arterial access. As noted in the proposed rule and described in more detail below, because a transfusion procedure always uses venous access rather than arterial access, these codes are considered clinically invalid and were the subject of a proposal discussed at the March 5-6, 2019 ICD-10 Coordination and Maintenance Committee meeting to delete these codes effective October 1, 2019 (FY 2020).
The majority of ICD-10-PCS procedure codes specifying autologous HCT procedures are currently assigned to MS-DRGs 016 and 017 (Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy and Autologous Bone Marrow Transplant without CC/MCC, respectively). These codes are listed in the following table.

We stated in the proposed rule that, while we believe, as indicated, the cases reporting ICD-10-PCS procedure codes for autologous HCT procedures may be improperly assigned to MS-DRG 014, we also examined claims data for this subset of cases to determine the frequency with which they were reported and the relative resource use as compared with all cases assigned to MS-DRGs 016 and 017. Our findings are shown in the following table.

For the subset of cases in MS-DRG 014 reporting ICD-10-PCS codes for autologous HCT procedures, there was a total of 6 cases with an average length of stay of 23.5 days and average costs of $38,319. The total number of cases reported in MS-DRG 016 was 2,150, with an average length of stay of 18 days and average costs of $47,546. The total number of cases reported in MS-DRG 017 was 104, with an average length of stay of 11 days and average costs of $33,540.
As indicated in the FY 2020 IPPS/LTCH PPS proposed rule, the results of our analysis indicate that the frequency with which these autologous HCT procedure codes were reported in MS-DRG 014 is low and that average costs of cases reporting autologous HCT procedures assigned to MS-DRG 014 are more aligned with the average costs of cases assigned to MS-DRGs 016 and 017, with the average costs being lower than the average costs for all cases assigned to MS-DRG 016 and higher than the average costs for all cases assigned to MS-DRG 017. We further stated in the proposed rule that our clinical advisors also indicated that the procedure codes for autologous HCT procedures are more clinically aligned with cases that are assigned to MS-DRGs 016 and 017 that are comprised of autologous HCT procedures. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to reassign the following 4 procedure codes for HCT procedures specifying autologous cord blood stem cell as the donor source via venous access to MS-DRGs 016 and 017 for FY 2020.

As discussed in the proposed rule and earlier in this section, the 4 procedure codes for HCT procedures that describe an autologous cord blood stem cell transfusion via arterial access currently assigned to MS-DRG 014, as listed previously, are considered clinically invalid. These procedure codes were discussed at the March 5-6, 2019 ICD-10 Coordination and Maintenance Committee meeting, along with additional procedure codes that are also considered clinically invalid, as described in the section below.
We stated in the proposed rule that during our analysis of procedure codes that describe a HCT procedure, we identified 128 clinically invalid codes from the transfusion table (table 302) in the ICD-10-PCS classification identifying a transfusion using arterial access, as listed in Table 6P.1a. associated with the proposed rule (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html). As shown in Table 6P.1a., these 128 procedure codes describe transfusion procedures with body system/region values “5” Peripheral Artery and “6” Central Artery. Because a transfusion procedure always uses venous access rather than arterial access, these codes are considered clinically invalid and were proposed for deletion at the March 5-6, 2019 ICD-10 Coordination and Maintenance Committee meeting. We refer the reader to the website at: https://www.cms.gov/Medicare/Coding/ICD10/C-and-M-Meeting-Materials.html for the Committee meeting materials regarding this proposal.
As discussed in the proposed rule, we examined claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 014, 016, and 017 to determine if there were any cases that reported one of the 128 clinically invalid codes from the transfusion table in the ICD-10-PCS classification identifying a transfusion using arterial access, and as listed in Table 6P.1a. associated with the proposed rule. Our clinical advisors agreed that because a transfusion procedure always uses venous access rather than arterial access, these codes are considered invalid. We stated in the proposed rule that because these procedure codes describe clinically invalid procedures, we would not expect these codes to be reported in any claims data. Our findings are shown in the following table.

As shown in this table, we found a total of 3,108 cases across MS-DRGs 014, 016, and 017 with an average length of stay of 20.4 days and average costs of $59,140. We found a total of 31 cases (0.9 percent) reporting a procedure code for an invalid transfusion procedure, identifying the body system/region value “5” Peripheral Artery or “6” Central Artery, with an average length of stay of 19.6 days and average costs of $52,912.
The results of the data analysis demonstrate that these invalid transfusion procedures represent approximately 1 percent of all discharges across MS-DRGs 014, 016, and 017.
To summarize, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to: (1) Reassign the four ICD-10-PCS codes for HCT procedures specifying autologous cord blood stem cell as the donor source from MS-DRG 014 to MS-DRGs 016 and 017 (procedure codes 30230X0, 30233X0, 30240X0, 30243X0); and (2) delete the 128 clinically invalid codes from the transfusion table in the ICD-10-PCS Classification describing a transfusion using arterial access that were discussed at the March 5-6, 2019 ICD-10 Coordination and Maintenance Committee meeting and listed in Table 6P.1a associated with the proposed rule. As discussed previously, we did not propose to split MS-DRG 014 into the two requested new MS-DRGs that would assign cases according to whether the allogeneic donor source is related or unrelated.
Comment: Commenters supported the proposal to maintain the current structure of MS-DRG 014. Commenters also supported the proposals to (1) reassign the four ICD-10-PCS codes for HCT procedures specifying autologous cord blood stem cell as the donor source from MS-DRG 014 to MS-DRGs 016 and 017 (procedure codes 30230X0, 30233X0, 30240X0, 30243X0); and (2) delete the 128 clinically invalid codes from the transfusion table in the ICD-10-PCS Classification. A commenter specifically expressed their appreciation with CMS' diligence in ensuring the clinical appropriateness of the ICD-10 codes. This commenter also requested that CMS create an edit (similar to what was implemented in the CY 2017 Hospital Outpatient Prospective Payment System final rule, which states outpatient claims assigned to C-APC 5224 with CPT code 38240 must be reported with revenue code 0815, and if that code is missing, the claim is returned by an edit to the provider) for inpatient claims utilizing ICD-10-PCS codes and revenue code 0815. According to the commenter, this would better inform CMS future ratesetting and reimbursement, as well as provide access to the more robust data in revenue code 0815 which the commenter asserted would allow CMS to do a meaningful analysis on the differences between search and procurement costs for related versus unrelated transplants. The commenter also recommended that CMS look at bone marrow and stem cell transplant services holistically and consider the process that providers must follow in order to correctly code and submit a claim.
Response: We appreciate the commenters' support. With regard to the recommendation that we create a new code edit for ICD-10-PCS codes reported with revenue code 0815 on the claim, as we noted in the proposed rule, the MCE is not designed to include revenue codes for claims editing purposes. Rather, as stated in section II.F.16. of the preamble of this final rule, it is a software program that detects and reports errors in the coding of Medicare claims data. In response to the commenter's recommendation that we consider the process that providers must follow in order to correctly code and submit a claim, we note that, as stated in the proposed rule, and above, we issued instructions as a One-Time Notification, Pub. No. 100-04, Transmittal 3571, Change Request 9674, effective January 1, 2017, which instructs that the appropriate revenue code to report on claims for allogeneic stem cell acquisition/donor services is revenue code 0815. As indicated, we are considering additional revisions as needed to conform the instructions for reporting these codes in the Medicare Claims Processing Manual.
After consideration of the public comments we received, we are finalizing our proposal to (1) reassign the four ICD-10-PCS codes for HCT procedures specifying autologous cord blood stem cell as the donor source from MS-DRG 014 to MS-DRGs 016 and 017 (procedure codes 30230X0, 30233X0, 30240X0, 30243X0); and (2) delete the 128 clinically invalid codes from the transfusion table in the ICD-10-PCS Classification and listed in Table 6P.1a associated with the proposed rule and this final rule (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) under the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
c. Chimeric Antigen Receptor (CAR) T-Cell Therapies
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19180), we received a request to create a new MS-DRG for procedures involving CAR T-cell therapies. The requestor stated that creation of a new MS-DRG would improve payment for CAR T-cell therapies in the inpatient setting. According to the requestor, while cases involving CAR T-cell therapy may now be eligible for new technology add-on payments and outlier payments, there continue to be significant financial losses by providers. The requestor also suggested that CMS modify its existing payment mechanisms to use a CCR of 1.0 for charges associated with CAR T-cell therapy.
In addition, the requestor included technical and operational suggestions related to CAR T-cell therapy, such as the development of unique CAR T-cell therapy revenue and cost centers for billing and cost reporting purposes. In the proposed rule, we stated that we will consider these technical and operational suggestions in the development of future billing and cost reporting guidelines and instructions.
In the FY 2020 IPPS/LTCH PPS proposed rule, we noted that, currently, procedures involving CAR T-cell therapies are identified with ICD-10-PCS procedure codes XW033C3 (Introduction of engineered autologous chimeric antigen receptor t-cell immunotherapy into peripheral vein, percutaneous approach, new technology group 3) and XW043C3 (Introduction of engineered autologous chimeric antigen receptor t-cell immunotherapy into central vein, percutaneous approach, new technology group 3), which became effective October 1, 2017. In the FY 2019 IPPS/LTCH PPS final rule, we finalized our proposal to assign cases reporting these ICD-10-PCS procedure codes to Pre-MDC MS-DRG 016 for FY 2019 and to revise the title of this MS-DRG to “Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy”. We refer readers to section II.F.2.d. of the preamble of the FY 2019 IPPS/LTCH PPS final rule for a complete discussion of these final policies (83 FR 41172 through 41174).
As stated in the proposed rule and earlier, the current procedure codes for CAR T-cell therapies both became effective October 1, 2017. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41172 through 41174), we indicated we should collect more comprehensive clinical and cost data before considering assignment of a new MS-DRG to these therapies. We stated in the FY 2020 IPPS/LTCH PPS proposed rule that, while the September 2018 update of the FY 2018 MedPAR data file does contain some claims that include those procedure codes that identify CAR T-cell therapies, the number of cases is limited, and the submitted costs vary widely due to differences in provider billing and charging practices for this therapy. Therefore, while these claims could potentially be used to create relative weights for a new MS-DRG, we stated that we do not have the comprehensive clinical and cost data that we generally believe are needed to do so. Furthermore, we stated in the proposed rule that given the relative newness of CAR T-cell therapy and our proposal to continue new technology add-on payments for FY 2020 for the two CAR T-cell therapies that currently have FDA approval (KYMRIAHTM and YESCARTATM), as discussed in section II.G.4.d. of the preamble of the proposed rule and this final rule, at this time we believe it may be premature to consider creation of a new MS-DRG specifically for cases involving CAR T-cell therapy for FY 2020.
Therefore, we did not propose to modify the current MS-DRG assignment for cases reporting CAR T-cell therapies for FY 2020. We noted that cases reporting ICD-10-PCS codes XW033C3 and XW043C3 would continue to be eligible to receive new technology add-on payments for discharges occurring in FY 2020 if our proposal to continue such payments is finalized. We stated that currently, we expect that, in future years, we would have additional data that exhibit more stability and greater consistency in charging and billing practices that could be used to evaluate the potential creation of a new MS-DRG specifically for cases involving CAR T-cell therapies.
Comment: Several commenters supported our proposal not to modify the current MS-DRG assignment for cases reporting CAR T-cell therapies for FY 2020, stating that CMS should wait until more clinical and cost data are available. Commenters indicated that CMS should wait until claims are coded and billed in a uniform manner so that consistent and accurate claims data is available for rate-setting. MedPAC also stated that incorporating new technologies into the Medicare program by using an existing MS-DRG in conjunction with new technology add-on payments and outlier payments has created incentives for efficiency and risk-sharing between providers and the Medicare program.
Response: We appreciate the commenters' support for our proposal and agree that incorporating new technologies into the Medicare program by using an existing MS-DRG in conjunction with new technology add-on payments, and outlier payments if applicable, is consistent with our policies regarding how new technologies are incorporated into the IPPS.
Comment: Several other commenters encouraged CMS to develop a new MS-DRG for cases reporting CAR T-cell therapies for FY 2020 in order to adequately cover the costs of treatment and so as not to dis-incentivize hospitals from providing CAR T-cell therapies due to inadequate reimbursement. Most of these commenters recommended alternative payment approaches for the CAR T-cell product if a new MS-DRG were created.
A commenter stated that claims analyses from the FY 2019 IPPS/LTCH PPS proposed rule for the KYMRIAHTM and YESCARTATM new technology add-on payment applications found a significant number of patients who may be eligible for use of these therapies, which may be reflective of the potential growth of these therapies in the future. The commenter also stated that according to the FY 2018 MEDPAR update, other pre-MDC MS-DRGs contain fewer cases than the 386 CAR T-cell discharges that CMS estimated would qualify for new technology add-on payments. The commenter stated that this suggests that there are enough cases for CAR T-cell therapies to be considered for their own MS-DRG assignment. Another commenter stated that in the FY 2019 IPPS/LTCH PPS proposed rule, CMS expressed concern about the potential redistributive effects away from core hospital services over time toward specialized hospitals and how that may affect payment for core services if a new MS-DRG is created. The commenter stated they shared these concerns; however, believed they are mitigated to the extent that CMS creates a new MS-DRG during a time when the volume of CAR T-cell cases is very low. They also noted the technology will likely become less expensive, not more expensive over time, as commonly occurs with expensive new technologies. The commenter urged CMS to create a new MS-DRG specific to CAR T-cell cases for use in FY 2020. The commenter expressed concern that if CMS waits to make an MS-DRG change at a time when volume is higher, but before the CAR T-cell cases have become less expensive, the CAR T-cell cases will draw a higher amount of additional payments at the expense of all other cases.
Response: As discussed in the proposed rule, we continue to believe that we do not have the comprehensive clinical and cost data that we generally believe is needed to create a new MS-DRG. As stated earlier, we also continue to believe that incorporating new technologies into the Medicare program by using an existing MS-DRG in conjunction with new technology add-on payments, and outlier payments if applicable, is consistent with our policies regarding how new technologies are incorporated into the IPPS. We note that we address additional comments relating to the creation of a separate MS-DRG, including potential payment approaches, in the discussion of alternative payment for CAR T-cell therapy cases that follows.
With respect to the number of cases, we note that the new technology add-on payment estimate is a projection of future cases. Our standard practice in determining whether to create a new MS-DRG is to examine the number of cases, and the clinical and cost characteristics of those cases in the historical claims data. We do not have the clinical and cost data about these projected future FY 2020 cases available at this time.
With respect to the commenter who expressed concern that waiting to create a new MS-DRG would draw a higher amount of additional payments at the expense of all other cases, we are unclear as to the specific concern being raised by the commenter. Each year, we calculate the relative weights by dividing the average cost for cases within each MS-DRG by the average cost for cases across all MS-DRGs. Since the relative weight is recalculated each year, the implications for the payments for other cases do not differ based on when a new MS-DRG is created.
Therefore, after consideration of the comments we received, and for the reasons discussed, we are finalizing our proposal not to modify the MS-DRG assignment for cases reporting CAR-T cell therapies for FY 2020. As noted previously, we address additional comments we received relating to the creation of any potential new MS-DRG, including payment under any such MS-DRG, in the discussion that follows.
As part of our solicitation of public comment on the potential creation of a new MS-DRG for CAR-T cell therapy procedures, in the proposed rule we also invited comment on the most appropriate way to develop the relative weight if we were to finalize the creation of a new MS-DRG in future rulemaking. We stated that, while the data are limited, it may be operationally possible to create a relative weight by dividing the average costs of cases that include the CAR T-cell procedures by the average costs of all cases, consistent with our current methodology for setting the relative weights for FY 2020 and using the same applicable data sources used for other MS-DRGs (for FY 2020, the FY 2018 MedPAR data and FY 2016 HCRIS data). We invited public comments on whether this is the most accurate method for determining the relative weight, given the current variation in the claims data for these procedures, and also on how to address the significant number of cases involving clinical trials. We stated in the proposed rule that, while we do not typically exclude cases in clinical trials when developing the relative weights, in this case, the absence of the drug costs on claims for cases involving clinical trial claims could have a significant impact on the relative weight. We also stated that it is unclear whether a relative weight calculated using cases for which hospitals do and do not incur drug costs would accurately reflect the resource costs of caring for patients who are not involved in clinical trials. We stated that a different approach might be to develop a relative weight using an appropriate portion of the average sales price (ASP) for these drugs as an alternative way to reflect the costs involved in treating patients receiving CAR T-cell therapies. We requested public comments on these approaches or other approaches for setting the relative weight if we were to finalize a new MS-DRG. We noted that any such new MS-DRG would be established in a budget neutral manner, consistent with section 1886(d)(4)(C)(iii) of the Act, which specifies that the annual DRG reclassification and recalibration of the relative weights must be made in a manner that ensures that aggregate payments to hospitals are not affected.
Comment: We received many comments on the most appropriate way to develop the relative weight and modify rate setting trims if we were to finalize the creation of a new MS-DRG, including different ways to determine the cost of the CAR T-cell therapy product, such as the use of Average Sales Price data or acquisition cost data, and technical comments on claims inclusion and exclusion criteria related to clinical trials.
Response: As discussed previously in this section, we are finalizing our proposal not to modify the MS-DRG assignment for cases reporting CAR-T cell therapies for FY 2020. We will consider these comments in connection with any future rulemaking relating to the MS-DRG assignment for the CAR-T cell therapy cases.
As discussed further in section II.G.7. of the preamble to the proposed rule, we also requested public comment on payment alternatives for CAR T-cell cases, including eliminating the use of the CCR in calculating the new technology add-on payment for KYMRIAH® and YESCARTA® by making a uniform add-on payment that equals the proposed maximum add-on payment. We also requested public comments on whether we should consider utilizing a specific CCR for ICD-10-PCS procedure codes used to report the performance of procedures involving the use of CAR T-cell therapies; for example, a CCR of 1.0, when determining outlier payments, when determining the new technology add-on payments, and when determining payments to IPPS-excluded cancer hospitals for CAR T-cell therapies.
We invited public comments on how payment alternatives for CAR T-cell therapy would affect access to care, as well as how they would affect incentives to encourage lower drug prices, which is a high priority for this Administration. As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41172 through 41174) and the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19279), we are considering approaches and authorities to encourage value-based care and lower drug prices. We solicited public comments on how the effective dates of any potential payment methodology alternatives, if any were to be adopted, may intersect and affect future participation in any such alternative approaches.
Comment: Some commenters indicated that CMS should pay for CAR T-cell therapy products based on the Average Sales Price. Some commenters noted that CMS pays for hemophilia blood clotting factors in this manner. A commenter recognized that payment for blood clotting factors in this manner was established by statute, but suggested that CMS may have the statutory authority to pay using this approach, or CMS could seek statutory authority from Congress. Another commenter urged CMS to pay for CAR T-cell therapies at Wholesale Acquisition Cost (WAC) plus six percent. Some commenters suggested that CMS require hospitals to submit on the claim the particular CAR T-cell product's NDC code. Other commenters stated given the similarity of CAR T-cell therapies to solid organ transplants, in that they are high-cost, low-volume services, CMS should pay for CAR T-cell therapies on a reasonable cost basis. Some commenters indicated that CMS should require providers to report value code 86, the actual invoice/acquisition cost, on their claims and include the actual product acquisition cost on the claim for payment purposes.
Several commenters suggested that CMS adopt a CCR of 1.0 for CAR T-cell products for all payment purposes, including new technology add-on payments, outlier payments, and payments to IPPS-excluded cancer hospitals. These commenters stated that utilizing a CCR of 1.0 will ensure uniformity among providers, many of whom are currently marking up the CAR-T charge, which impacts CMS' ability to analyze claims data that are critical for rate setting. These commenters also stated that they believe the use of a CCR of 1.0 would ensure consistent billing practices and payment that would be mutually beneficial for CMS and providers, including eliminating the need for providers to mark-up the CAR T-cell product cost. MedPAC expressed concern about using a CCR of 1.0, which would presume the hospitals charged their actual costs despite what it stated was the clear financial incentive to increase charges. MedPAC also expressed concern that this could set a precedent for other items going forward, and instead recommended the use of a lagged ASP based payment. Another commenter stated that using a CCR of 1.0 is a radical departure from previous payment methods and CMS should carefully consider possible issues that may result.
Many commenters requested structural changes in new technology add-on payments for the drug therapy, including the use of a uniform add-on payment. Many commenters also requested a higher new technology add-on payment percentage for CAR T-cell therapy products, up to 100 percent, rather than our proposed 65 percent for all new technologies, indicating that the proposed 65 percent would result in inadequate payment.
Some commenters suggested that CMS develop and release for comment an outcomes-based payment model for CAR T-cell therapy payments in the future and encouraged CMS to consider a payment alternative for CAR T-cell therapy under which CMS would test a new payment model through the Innovation Center and would pay for these technologies based on outcome and value rather than service.
Response: After a review of the comments received, we continue to believe, similar to last year, that given the relative newness of CAR T-cell therapy, and our continued consideration of approaches and authorities to encourage value-based care and lower drug prices, it would be premature to adopt structural changes to our existing payment mechanisms, either under the IPPS or for IPPS-excluded cancer hospitals, specifically for CAR T-cell therapy. For these reasons, we disagree with the commenters' requested changes to our current payment mechanisms for FY 2020, including, but not limited to, the creation of a pass-through payment; structural changes in new technology add-on payments and/or a differentially higher new technology add-on payment percentage specifically for CAR T-cell products, and changes in the usual cost-to-charge ratios (CCRs) used in ratesetting and payment, including those used in determining new technology add-on payments, outlier payments, and payments to IPPS excluded cancer hospitals. However, as discussed elsewhere in this final rule, we are finalizing a maximum new technology add-on payment percentage of 65 percent of the costs of the new technology for FY 2020, a 30 percent ((0.65/0.50)-1) increase from the current 50 percent. This increase to 65 percent will apply to all approved new technologies (except products designated by the FDA as a Qualified Infectious Disease Products, for which the maximum add-on amount will be 75 percent of the costs of the new technology), including CAR T-cell therapy products.
We stated in the proposed rule that another potential consideration if we were to create a new MS-DRG is the extent to which it would be appropriate to geographically adjust the payment under any such new MS-DRG. Under the methodology for determining the Federal payment rate for operating costs under the IPPS, the labor-related proportion of the national standardized amounts is adjusted by the wage index to reflect the relative differences in labor costs among geographic areas. The IPPS Federal payment rate for operating costs is calculated as the MS-DRG relative weight × [(labor-related applicable standardized amount × applicable wage index) + (nonlabor-related applicable standardized amount × cost-of-living adjustment)]. Given our understanding that the costs for CAR T-cell therapy drugs do not vary among geographic areas, and given that costs for CAR T-cell therapy would likely be an extremely high portion of the costs for the MS-DRG, in the proposed rule we invited public comments on whether we should not geographically adjust the payment for cases assigned to any potential new MS-DRG for CAR-T cell therapy procedures. We also invited public comments on whether to instead apply the geographic adjustment to a lower proportion of payments under any potential new MS-DRG and, if so, how that lower proportion should be determined. We noted that while the prices of other drugs may also not vary significantly among geographic areas, generally speaking, those other drugs would not have estimated costs as high as those of CAR T-cell therapies, nor would they represent as significant a percentage of the average costs for the case. We invited public comments on the use of our exceptions and adjustments authority under section 1886(d)(5)(I) of the Act (or other relevant authorities) to implement any such potential changes.
Comment: Some commenters stated that CMS should include adjustments for the wage index in a potential future MS-DRG for CAR T-cell therapies, including commenters that expressed concern that not applying the wage index would increase provider losses on these services. Some commenters stated that they did not believe CMS had the statutory flexibility to selectively apply the wage index. Many other commenters stated that CMS should not apply the wage index to the cost of the drug, as the cost does not vary by location, and hospitals with a wage index greater than 1 would be overpaid for the drug, while hospitals with a wage index less than 1 would be underpaid.
Response: We appreciate the commenters' input on the application of the wage index to a potential future MS-DRG for CAR T-cell therapies. We will consider these comments should we develop a proposed MS-DRG for CAR T-cell therapies in the future.
As discussed in the proposed rule, section 1886(d)(5)(B) of the Act provides that prospective payment hospitals that have residents in an approved graduate medical education (GME) program receive an additional payment for a Medicare discharge to reflect the higher patient care costs of teaching hospitals relative to nonteaching hospitals. The regulations regarding the calculation of this additional payment, known as the indirect medical education (IME) adjustment, are located at 42 CFR 412.105. The formula is traditionally described in terms of a certain percentage increase in payment for every 10-percent increase in the resident-to-bed ratio. For some hospitals, this percentage increase can exceed an additional 25 percent or more of the otherwise applicable payment. Some hospitals, sometimes the same hospitals, can also receive a large percentage increase in payments due to the Medicare disproportionate hospital (DSH) adjustment provision under section 1886(d)(5)(F) of the Act. The regulations regarding the calculation of the additional DSH payment are located at 42 CFR 412.106.
In the proposed rule we stated that, given that the payment for cases assigned to a new MS-DRG for CAR T-cell therapy could significantly exceed the historical payment for any existing MS-DRG, these percentage add-on payments could arguably result in unreasonably high additional payments for CAR T-cell therapy cases unrelated in any significant empirical way to the costs of the hospital in providing care. For example, consider a teaching hospital that has an IME adjustment factor of 0.25, and a DSH adjustment factor of 0.10. If we were to create a new MS-DRG for CAR T-cell therapy procedures that resulted in an average IPPS Federal payment rate for operating costs of $400,000, under the current payment mechanism, the hospital would receive an IME payment of $100,000 ($400,000 × 0.25) and a DSH payment of $40,000 ($400,000 × 0.10), such that the total IPPS Federal payment rate for operating costs including IME and DSH payments would be $540,000 ($400,000 + $100,000 + $40,000). We invited public comments on whether the IME and DSH payments should not be made for cases assigned to any new MS-DRG for CAR T-cell therapy. We also invited public comments on whether we should instead reduce the applicable percentages used to determine these add-ons and, if so, how those lower percentages should be determined. We invited public comments on the use of our exceptions and adjustments authority under section 1886(d)(5)(I) of the Act (or other relevant authorities) to implement any potential changes.
Comment: Several commenters stated that CMS should include adjustments for DSH and IME in a potential future MS-DRG for CAR T-cell therapies (as described below); some commenters stated that they did not believe CMS had the statutory flexibility to selectively apply these adjustments. Commenters also expressed concern that not applying these adjustments would increases provider losses on these services. Several commenters stated that the IME adjustment is not based on a requirement that the costs for each service at a teaching hospital are greater than at a non-teaching hospital, but is instead due to the recognition that overall the costs are greater. A commenter stated that teaching hospitals are under considerable financial strain, that they will disproportionately shoulder the burdens of new, higher cost services, and that CMS should consider these costs and burdens before determining that the IME adjustment to CAR T-cell therapy cases would result in a payment that is too high. This commenter also stated that hospitals that receive DSH payments are less profitable than hospitals serving better-insured populations. Therefore, in order for these hospitals to access expensive new technologies, they need to receive a level of reimbursement that can support these services.
Many commenters stated that CMS should not apply the DSH and IME adjustments to the entire MS-DRG payment for CAR T-cell therapy cases, as this would result in a higher than appropriate payment. Several of these commenters also suggested that CMS consider “carving out” payment for CAR T-cell therapy cases to avoid this problem.
Response: We appreciate the commenters' input on the application of the DSH and IME adjustments to a potential future MS-DRG for CAR T-cell therapies. We will consider these comments should we develop a proposed MS-DRG for CAR T-cell therapies in the future.
3. MDC 1 (Diseases and Disorders of the Nervous System): Carotid Artery Stent Procedures
The logic for case assignment to MS-DRGs 034, 035, and 036 (Carotid Artery Stent Procedures with MCC, with CC, and without CC/MCC, respectively) as displayed in the ICD-10 MS-DRG Version 36 Definitions Manual (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html) is comprised of two lists of logic that include procedure codes for operating room (O.R.) procedures involving dilation of a carotid artery (common, internal or external) with intraluminal device(s). The first list of logic is entitled “Operating Room Procedures” and the second list of logic is entitled “Operating Room Procedures with Operating Room Procedures”. In the FY 2020 IPPS/LTCH PPS proposed rule, we identified 46 ICD-10-PCS procedure codes in the second logic list that do not describe dilation of a carotid artery with an intraluminal device. Of these 46 procedure codes, we identified 24 codes describing dilation of a carotid artery without an intraluminal device; 8 codes describing dilation of the vertebral artery; and 14 codes describing dilation of a vein (jugular, vertebral and face), as shown in the following table.

We examined claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 034, 035, and 036 and identified cases reporting any one of the 46 ICD-10-PCS procedure codes listed in the tables above. Our findings are shown in the following table.

As shown in the table above, we found a total of 863 cases with an average length of stay of 6.8 days and average costs of $27,600 in MS-DRG 034. There were 15 cases reporting at least one of the 46 procedure codes that do not describe dilation of the carotid artery with an intraluminal device in MS-DRG 034 with an average length of stay of 8.8 days and average costs of $36,596. For MS-DRG 035, we found a total of 2,369 cases with an average length of stay of 3 days and average costs of $16,731. There were 52 cases reporting at least one of the 46 procedure codes that do not describe dilation of the carotid artery with an intraluminal device in MS-DRG 035 with an average length of stay of 3.5 days and average costs of $17,815. For MS-DRG 036, we found a total of 3,481 cases with an average length of stay of 1.4 days and average costs of $12,637. There were 67 cases reporting at least one of the 46 procedure codes that do not describe dilation of the carotid artery with an intraluminal device in MS-DRG 036 with an average length of stay of 1.4 days and average costs of $12,621.
In the proposed rule, we noted that our clinical advisors stated that MS-DRGs 034, 035, and 036 are defined to include only those procedure codes that describe procedures that involve dilation of a carotid artery with an intraluminal device. Therefore, we proposed to remove the procedure codes listed in the table above from MS-DRGs 034, 035, and 036 that describe procedures which (1) do not include an intraluminal device; (2) describe procedures performed on arteries other than a carotid; and (3) describe procedures performed on a vein.
We also indicated in the proposed rule that the 46 ICD-10-PCS procedure codes listed in the table above are also assigned to MS-DRGs 037, 038, and 039 (Extracranial Procedures with MCC, with CC, and without CC/MCC, respectively). Therefore, we also examined claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 037, 038, and 039. Our findings are shown in the following table.
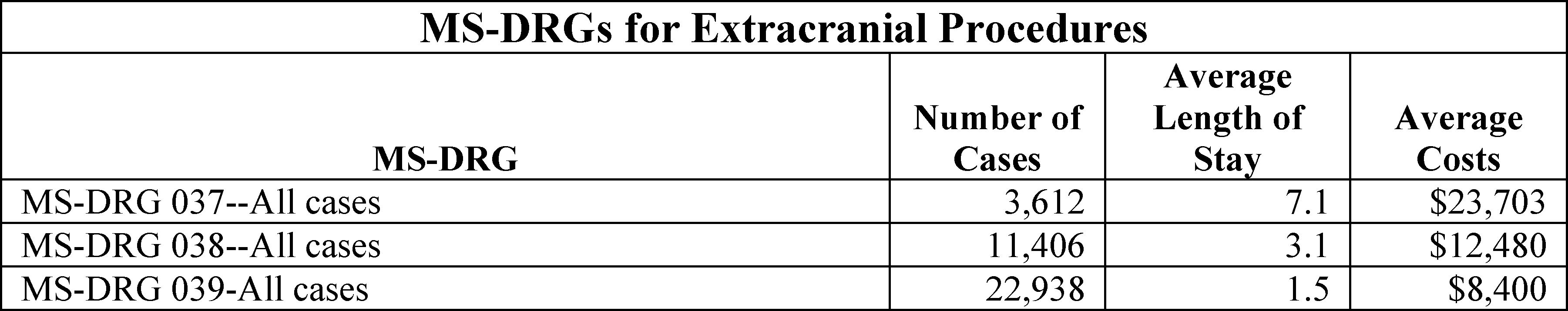
We found a total of 3,612 cases in MS-DRG 037 with an average length of stay of 7.1 days and average costs of $23,703. We found a total of 11,406 cases in MS-DRG 038 with an average length of stay of 3.1 days and average costs of $12,480. We found a total of 22,938 cases in MS-DRG 039 with an average length of stay of 1.5 days and average costs of $8,400.
In the proposed rule, we stated that during our review of claims data for MS-DRGs 037, 038, and 039, we also discovered 96 ICD-10-PCS procedure codes describing dilation of a carotid artery with an intraluminal device that were inadvertently included as a result of efforts to replicate the ICD-9 based MS-DRGs. These procedure codes are also included in the logic for MS-DRGs 034, 035, and 036. Under ICD-9-CM, procedure codes 00.61 (Percutaneous angioplasty of extracranial vessel(s)) and 00.63 (Percutaneous insertion of carotid artery stent(s)) are both required to be reported on a claim to identify that a carotid artery stent procedure was performed and for assignment of the case to MS-DRGs 034, 035, and 036. Procedure code 00.61 is designated as an O.R. procedure, while procedure code 00.63 is designated as a non-O.R. procedure. Under ICD-10-PCS, a carotid artery stent procedure is described by one unique code that includes both clinical concepts of the angioplasty (dilation) and the insertion of the stent (intraluminal device). This “combination code” under ICD-10-PCS is designated as an O.R. procedure. Under ICD-9-CM, procedure code 00.61 reported in the absence of procedure code 00.63 results in assignment to MS-DRGs 037, 038, and 039 according to the MS-DRG logic because procedure code 00.61 has an inclusion term for vertebral vessels, as well as for the carotid vessels. Therefore, when all of the comparable translations of procedure code 00.61 as an O.R. procedure were replicated from the ICD-9 based MS-DRGs to the ICD-10 based MS-DRGs, this replication inadvertently results in the assignment of ICD-10-PCS procedure codes that identify and describe a carotid artery stent procedure to MS-DRGs 037, 038, and 039. Therefore, we proposed to remove the 96 ICD-10-PCS procedure codes describing dilation of a carotid artery with an intraluminal device from MS-DRGs 037, 038, and 039.
We also found 6 procedure codes describing dilation of a carotid artery with an intraluminal device in MS-DRGs 037, 038, and 039 that are not currently assigned to MS-DRGs 034, 035, and 036. In the proposed rule, we stated that our clinical advisors recommended that these 6 procedure codes be reassigned from MS-DRGs 037, 038, and 039 to MS-DRGs 034, 035, and 036 because the 6 procedure codes are consistent with the other procedures describing dilation of a carotid artery with an intraluminal device that are currently assigned to MS-DRGs 034, 035, and 036. We refer readers to Table 6P.1b. associated with the proposed rule (which is available via the internet on the CMS website at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) for the complete list of procedure codes that we proposed to remove from MS-DRGs 037, 038, and 039.
We also noted that, as discussed in the proposed rule and section II.F.14.f. of the preamble of this final rule, we are deleting a number of codes that include the ICD-10-PCS qualifier term “bifurcation” as the result of the finalized proposal discussed at the September 11-12, 2018 ICD-10 Coordination and Maintenance Committee meeting. We refer readers to the website at: https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD-9-CM-C-and-M-Meeting-Materials.html for the committee meeting materials and discussion regarding this proposal. We noted in the proposed rule that, of the 96 procedure codes that we proposed to remove from the logic for MS-DRGs 037, 038, and 039, there are 48 procedure codes that include the qualifier term “bifurcation”. Therefore, we stated in the proposed rule that these 48 procedure codes will be deleted effective October 1, 2019. We stated that the 48 remaining valid procedure codes that do not include the term “bifurcation” that we proposed to remove from MS-DRGs 037, 038, and 039 will continue to be assigned to MS-DRGs 034, 035, and 036.
Lastly, we stated in the proposed rule that, if the applicable proposed MS-DRG changes are finalized, we would make a conforming change to the ICD-10 MS-DRG Version 37 Definitions Manual for FY 2020 by combining all the procedure codes identifying a carotid artery stent procedure within MS-DRGs 034, 035, and 036 into one list entitled “Operating Room Procedures” to better reflect the definition of these MS-DRGs based on the discussion and proposals described above.
Comment: Several commenters supported this proposal stating that only procedures involving dilation of a carotid artery using intraluminal devices should be included in MS-DRGs 034-036 and that procedures that do not involve both a carotid artery and an intraluminal device should be removed from MS-DRGs 034-036. Several commenters also supported our proposal to remove 96 ICD-10 PCS codes describing dilation of a carotid artery with intraluminal device from MS-DRGs 037, 038 and 039 and to delete the 48 procedure codes from MS-DRGs 037, 038, and 039 that include the qualifier term “bifurcation.
Response: We appreciate the commenters' support.
Comment: A commenter expressed concern and disagreed with the proposal to delete the procedure codes that include the qualifier term “bifurcation”. The commenter stated that in vascular surgery, use of the term bifurcation may be used to document when a procedure occurs in a branch vessel.
Response: We appreciate the commenter's suggestion, however, as discussed at the ICD-10 Coordination and Maintenance Committee meeting held on September 11-12, 2018, the qualifier value Bifurcation was proposed (and subsequently finalized) to be deleted from the following ICD-10-PCS tables—037 Dilation of Upper Arteries, 03C Extirpation of Upper Arteries, 047 Dilation of Lower Arteries, 04C Extirpation of Lower Arteries and 04V Restriction of Lower Arteries. The original proposal for the qualifier Bifurcation was intended to capture data specifically regarding procedures on coronary arteries. The term bifurcation describes diagnosis related information, and generally, under ICD-10 PCS we do not include diagnosis related information in the procedure classification.
After consideration of the public comments we received, we are finalizing our proposal to remove the procedure codes listed previously from MS-DRGs 034, 035, and 036 that describe procedures which (1) do not include an intraluminal device; (2) describe procedures performed on arteries other than a carotid; and (3) describe procedures performed on a vein. We are also finalizing our proposal to remove 96 ICD-10 PCS codes describing dilation of a carotid artery with intraluminal device from MS-DRGs 037, 038 and 039 and are finalizing our proposal to reassign the 6 procedure codes discussed above from MS-DRGs 037, 038, and 039 to MS-DRGs 034, 035, and 036 because the 6 procedure codes are consistent with the other procedures describing dilation of a carotid artery with an intraluminal device that are currently assigned to MS-DRGs 034, 035, and 036. We refer readers to Table 6P.1b. associated with this final rule (which is available via the internet on the CMS website at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) for the complete list of procedure codes that we removed from MS-DRGs 037, 038, and 039. Additionally, we are finalizing our proposal to delete the 48 procedure codes from MS-DRGs 037, 038, and 039 that include the qualifier term “bifurcation”. Finally, we are finalizing our proposal to make a conforming change to the ICD-10 MS-DRG Version 37 Definitions Manual for FY 2020 by combining all the procedure codes identifying a carotid artery stent procedure within MS-DRGs 034, 035, and 036 into one list entitled “Operating Room Procedures” to better reflect the definition of these MS-DRGs.
4. MDC 4 (Diseases and Disorders of the Respiratory System): Pulmonary Embolism
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19185), we discussed that we received a request to reassign three ICD-10-CM diagnosis codes for pulmonary embolism with acute cor pulmonale from MS-DRG 176 (Pulmonary Embolism without MCC) to the higher severity level MS-DRG 175 (Pulmonary Embolism with MCC). The three diagnosis codes are identified in the following table.

The requestor noted that, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41231 through 41234), we finalized the proposal to remove the special logic in the GROUPER for processing claims containing a code on the Principal Diagnosis Is Its Own CC or MCC Lists and deleted the relevant tables from the ICD-10 MS-DRG Definitions Manual Version 36, effective October 1, 2018. As a result of this change, cases reporting any one of the three ICD-10-CM diagnosis codes describing a pulmonary embolism with acute cor pulmonale were reassigned from MS-DRG 175 to MS-DRG 176, absent a secondary diagnosis code to trigger assignment to MS-DRG 175. The requestor stated that this change in the MS-DRG assignment for these cases resulted in a reduction in payment for cases involving pulmonary embolism with acute cor pulmonale and that the FY 2019 payment rate for MS-DRG 176 does not appropriately account for the costs and resource utilization associated with these cases because the subset of patients with pulmonary embolism with acute cor pulmonale often represents a more severe set of patients with pulmonary embolism.
The logic for case assignment to MS-DRGs 175 and 176 is displayed in the ICD-10 MS-DRG Version 36 Definitions Manual, which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html.
As indicated in the FY 2020 IPPS/LTCH PPS proposed rule, we analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 175 and 176 to identify cases reporting diagnosis codes describing pulmonary embolism with acute cor pulmonale as listed above (ICD-10-CM diagnosis codes I26.01, I26.02 or I26.09) as the principal diagnosis or as a secondary diagnosis. Our findings are shown in the following table.
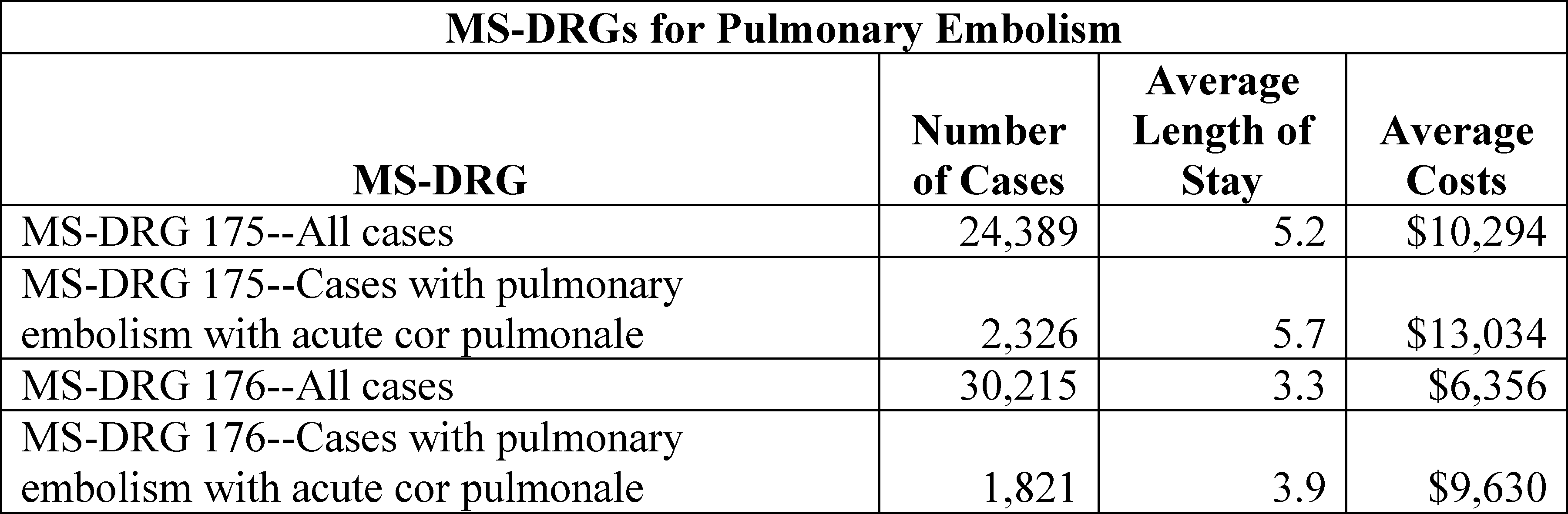
As shown in the table, for MS-DRG 175, there was a total of 24,389 cases with an average length of stay of 5.2 days and average costs of $10,294. Of these 24,389 cases, there were 2,326 cases reporting pulmonary embolism with acute cor pulmonale, with an average length of stay 5.7 days and average costs of $13,034. For MS-DRG 176, there was a total of 30,215 cases with an average length of stay of 3.3 days and average costs of $6,356. Of these 30,215 cases, there were 1,821 cases reporting pulmonary embolism with acute cor pulmonale with an average length of stay of 3.9 days and average costs of $9,630.
As stated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41231 through 41234), available ICD-10 data can now be used to evaluate other indicators of resource utilization and, as shown by our claims analysis, the data indicate that the average costs of cases reporting pulmonary embolism or saddle embolus with acute cor pulmonale ($9,630) in MS-DRG 176 are closer to the average costs for all pulmonary embolism cases in MS-DRG 175 ($10,294) as compared to the average costs for all cases in MS-DRG 176 ($6,356). We stated in the proposed rule that our clinical advisors also agreed that this subset of patients with acute cor pulmonale often represents a more severe set of patients and that these cases are more appropriately assigned to the higher severity level “with MCC” MS-DRG. Therefore, in the proposed rule, we proposed to reassign cases reporting diagnosis code I26.01, I26.02, or I26.09 to the higher severity level MS-DRG 175 and to revise the title for MS-DRG 175 to “Pulmonary Embolism with MCC or Acute Cor Pulmonale” to more accurately reflect the diagnoses assigned there.
Comment: Commenters supported our proposed reassignment of diagnosis codes I26.01, I26.02, and I26.09 to the higher severity level MS-DRG 175 and revision of the title for MS-DRG 175 to “Pulmonary Embolism with MCC or Acute Cor Pulmonale” to more accurately reflect the diagnoses.
Response: We thank the commenters for their support. After consideration of the public comments we received, we are finalizing our proposal to reassign cases reporting diagnosis code I26.01, I26.02, or I26.09 to the higher severity level MS-DRG 175 and to revise the title for MS-DRG 175 to “Pulmonary Embolism with MCC or Acute Cor Pulmonale”.
5. MDC 5 (Diseases and Disorders of the Circulatory System)
a. Transcatheter Mitral Valve Repair With Implant
As we did for the FY 2015 IPPS/LTCH PPS proposed rule (79 FR 28008 through 28010) and for the FY 2017 IPPS/LTCH PPS proposed rule (81 FR 24985 through 24989), for FY 2020, as discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19185 through 19193), we received a request to modify the MS-DRG assignment for transcatheter mitral valve repair (TMVR) with implant procedures. ICD-10-PCS procedure code 02UG3JZ (Supplement mitral valve with synthetic substitute, percutaneous approach) identifies and describes this procedure. This request also included the suggestion that CMS give consideration to reclassifying other endovascular cardiac valve repair procedures. Specifically, the requestor recommended that cases reporting procedure codes describing an endovascular cardiac valve repair with implant be reassigned to MS-DRGs 266 and 267 (Endovascular Cardiac Valve Replacement with and without MCC, respectively) and that the MS-DRG titles be revised to Endovascular Cardiac Valve Interventions with Implant with and without MCC, respectively. We refer readers to detailed discussions of the MitraClip® System (hereafter referred to as MitraClip®) for transcatheter mitral valve repair in previous rulemakings, including the FY 2012 IPPS/LTCH PPS proposed rule (76 FR 25822) and final rule (76 FR 51528 through 51529), the FY 2013 IPPS/LTCH PPS proposed rule (77 FR 27902 through 27903) and final rule (77 FR 53308 through 53310), the FY 2015 IPPS/LTCH PPS proposed rule (79 FR 28008 through 28010) and final rule (79 FR 49889 through 49892), the FY 2016 IPPS/LTCH PPS proposed rule (80 FR 24356 through 24359) and final rule (80 FR 49363 through 49367), and the FY 2017 IPPS/LTCH PPS proposed rule (81 FR 24985 through 24989) and final rule (81 FR 56809 through 56813), in response to requests for MS-DRG reclassification, as well as the FY 2014 IPPS/LTCH PPS proposed rule (78 FR 27547 through 27552), under the new technology add-on payment policy. In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50575), we were unable to consider further the application for a new technology add-on payment for MitraClip® because the technology had not received FDA approval by the July 1, 2013 deadline.
In the FY 2015 IPPS/LTCH PPS final rule, we finalized our proposal to not create a new MS-DRG or to reassign cases reporting ICD-9-CM procedure code 35.97 that described procedures involving the MitraClip® to another MS-DRG (79 FR 49889 through 49892). Under a new application, the request for new technology add-on payments for the MitraClip® System was approved for FY 2015 (79 FR 49941 through 49946). The new technology add-on payment for MitraClip® was subsequently discontinued effective FY 2017.
In the FY 2016 IPPS/LTCH PPS final rule (80 FR 49371), we finalized a modification to the MS-DRGs to which procedures involving the MitraClip® were assigned. For the ICD-10 based MS-DRGs to fully replicate the ICD-9-CM based MS-DRGs, ICD-10-PCS code 02UG3JZ (Supplement mitral valve with synthetic substitute, percutaneous approach), which identifies the MitraClip® technology and is the ICD-10-PCS code translation for ICD-9-CM procedure code 35.97 (Percutaneous mitral valve repair with implant), was assigned to new MS-DRGs 273 and 274 (Percutaneous Intracardiac Procedures with MCC and without MCC, respectively) and continued to be assigned to MS-DRGs 231 and 232 (Coronary Bypass with PTCA with MCC and without MCC, respectively).
In the FY 2017 IPPS/LTCH PPS proposed and final rules, we also discussed our analysis of MS-DRGs 228, 229, and 230 (Other Cardiothoracic Procedures with MCC, with CC, and without CC/MCC, respectively) with regard to the possible reassignment of cases reporting ICD-10-PCS procedure code 02UG3JZ (Supplement mitral valve with synthetic substitute, percutaneous approach). We finalized our proposal to collapse these MS-DRGs (228, 229, and 230) from three severity levels to two severity levels by deleting MS-DRG 230 and revising the structure of MS-DRG 229. We also finalized our proposal to reassign ICD-10-PCS procedure code 02UG3JZ (Supplement mitral valve with synthetic substitute, percutaneous approach) from MS-DRGs 273 and 274 to MS-DRG 228 and revised MS-DRG 229 (81 FR 56813).
As we discussed in the proposed rule, according to the requestor, there are substantial clinical and resource differences between the transcatheter mitral valve repair (TMVR) procedure and other procedures currently grouping to MS-DRGs 228 and 229. The requestor noted that, currently, ICD-10-PCS procedure code 02UG3JZ is the only endovascular valve intervention with implant procedure that maps to MS-DRGs 228 and 229. The requestor also noted that other ICD-10-PCS procedure codes describing procedures for endovascular (transcatheter) cardiac valve repair with implant map to MS-DRGs 273 and 274 or to MS-DRGs 216, 217, 218, 219, 220, and 221 (Cardiac Valve and Other Major Cardiothoracic Procedures with and without Cardiac Catheterization with MCC, with CC and without CC/MCC, respectively). The requestor further noted that all ICD-10-PCS procedure codes for endovascular cardiac valve replacement procedures map to MS-DRGs 266 (Endovascular Cardiac Valve Replacement with MCC) and 267 (Endovascular Cardiac Valve Replacement without MCC).
As noted in the proposed rule, the ICD-10-PCS procedure codes describing a transcatheter cardiac valve repair procedure with an implant are listed in the following table.

As also noted in the proposed rule, the ICD-10-PCS procedure codes describing a transcatheter cardiac valve replacement procedure are listed in the following table.

We noted in the proposed rule that the requestor performed its own analyses, first comparing TMVR procedures (ICD-10-PCS procedure code 02UG3JZ) to other procedures currently assigned to MS-DRGs 228 and 229, as well as to the transcatheter cardiac valve replacement procedures in MS-DRGs 266 and 267. We refer the reader to the ICD-10 MS-DRG Version 36 Definitions Manual for complete documentation of the logic for case assignment to MS-DRGs 228 and 229 (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html). According to the requestor, its findings indicate that TMVR is more closely aligned with MS-DRGs 266 and 267 than MS-DRGs 228 and 229 with regard to average length of stay and average [standardized] costs. The requestor also examined the impact of removing cases reporting a TMVR procedure (ICD-10-PCS procedure code 02UG3JZ) from MS-DRGs 228 and 229 and adding those cases to MS-DRGs 266 and 267. The requestor noted this movement would have minimal impact to MS-DRGs 266 and 267 based on its analysis. In addition, the requestor stated that its request is in alignment with CMS' policy goal of creating and maintaining clinically coherent MS-DRGs.
The requestor acknowledged that CMS has indicated in prior rulemaking that TMVR procedures are not clinically similar to endovascular cardiac valve replacement procedures, and the requestor agreed that they are distinct procedures. However, the requestor also believed that TMVR is more similar to the replacement procedures in MS-DRGs 266 and 267 compared to the other procedures currently assigned to MS-DRGs 228 and 229. The requestor provided the following table of procedures in volume order (highest to lowest) to illustrate the clinical differences between TMVR procedures and other procedures currently assigned to MS-DRGs 228 and 229.

The requestor noted that, among the procedures listed in the table, TMVR is the only procedure that involves treatment of a cardiac valve and is the only procedure that involves implanting a synthetic substitute.
To illustrate the similarities between TMVR procedures and endovascular cardiac valve replacements in MS-DRGs 266 and 267, the requestor provided the following table.

The requestor noted that both TMVR procedures and endovascular cardiac valve replacements use a percutaneous approach, treat cardiac valves, and use an implanted device for purposes of improving the function of the specified valve. The requestor believed that the analyses support the request to group TMVR procedures with endovascular cardiac valve replacements from a resource perspective and an improvement to clinical coherence could be achieved because TMVR procedures are more similar to the endovascular cardiac valve replacements compared to the other procedures in MS-DRGs 228 and 229, where TMVR is currently assigned.
As noted in the proposed rule and earlier in this section, the request also included the suggestion that CMS give consideration to reclassifying other endovascular cardiac valve repair with implant procedures to MS-DRGs 266 and 267; specifically, endovascular cardiac valve repair with implant procedures involving the aortic, pulmonary, tricuspid and other non-TMVR mitral valve procedures that currently group to MS-DRGs 273 and 274 or MS-DRGs 216, 217, 218, 219, 220 and 221. The requestor acknowledged that endovascular cardiac valve repair with implant procedures involving these other cardiac valves have lower volumes in comparison to the TMVR procedure (ICD-10-PCS procedure code 02UG3JZ), which makes analysis of these procedures a little more difficult. However, the requestor suggested that movement of these procedures to MS-DRGs 266 and 267 would enable the ability to maintain clinical coherence for all endovascular cardiac valve interventions. The requestor also stated that there is an anticipated increase in the volume of not only the TMVR procedure described by ICD-10-PCS procedure code 02UG3JZ (which has grown annually since the MitraClip® was approved for new technology add-on payment in FY 2015), but also for the other endovascular cardiac valve repair with implant procedures, such as those involving the tricuspid valve, which are currently under study in the United States and Europe. Based on this anticipated increase in volume for endovascular cardiac valve repair with implant procedures, the requestor believed that it would be advantageous to take this opportunity to restructure the MS-DRGs by moving all the endovascular cardiac valve repair with implant procedures to MS-DRGs 266 and 267 with revised titles as noted previously, to improve clinical consistency beginning in FY 2020. The requestor further noted that while the requestor believes its request reflects the best approach for appropriate MS-DRG assignment for TMVR and other endovascular cardiac valve repair with implant procedures, the requestor understands that CMS may consider other alternatives.
As indicated in the proposed rule, we analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for cases reporting ICD-10-PCS procedure code 02UG3JZ in MS-DRGs 228 and 229 as well as cases reporting one of the procedure codes listed above describing a transcatheter cardiac valve repair with implant procedure in MS-DRGs 216, 217, 218, 219, 220, 221, 273, and 274. Our findings are shown in the tables below.

As shown in the table, we found a total of 5,909 cases for MS-DRG 216 with an average length of stay of 16 days and average costs of $70,435. Of those 5,909 cases, there were 48 cases reporting a procedure code for a transcatheter cardiac valve repair with an average length of stay of 12.6 days and average costs of $72,556. We found a total of 2,166 cases for MS-DRG 217 with an average length of stay of 9.4 days and average costs of $47,299. Of those 2,166 cases, there was a total of 25 cases reporting a procedure for a transcatheter cardiac valve repair with an average length of stay of 3.4 days and average costs of $40,707. We found a total of 268 cases for MS-DRG 218 with an average length of stay of 6.8 days and average costs of $39,501. Of those 268 cases, there were 4 cases reporting a procedure code for a transcatheter cardiac valve repair with an average length of stay of 1.3 days and average costs of $45,903. We found a total of 15,105 cases for MS-DRG 219 with an average length of stay of 10.9 days and average costs of $55,423. Of those 15,105 cases, there were 55 cases reporting a procedure code for a transcatheter cardiac valve repair with an average length of stay of 7.1 days and average costs of $65,880. We found a total of 15,889 cases for MS-DRG 220 with an average length of stay of 6.6 days and average costs of $38,313. Of those 15,889 cases, there were 40 cases reporting a procedure code for a transcatheter cardiac valve repair with an average length of stay of 3 days and average costs of $38,906. We found a total of 2,652 cases for MS-DRG 221 with an average length of stay of 4.7 days and average costs of $33,577. Of those 2,652 cases, there were 13 cases reporting a procedure code for a transcatheter cardiac valve repair with an average length of stay of 2.2 days and average costs of $29,646.
For MS-DRG 228, we found a total of 5,583 cases with an average length of stay of 9.2 days and average costs of $46,613. Of those 5,583 cases, there were 1,688 cases reporting ICD-10-PCS procedure code 02UG3JZ (Supplement mitral valve with synthetic substitute, percutaneous approach) with an average length of stay of 5.6 days and average costs of $49,569. As noted previously and in the proposed rule, ICD-10-PCS procedure code 02UG3JZ is the only endovascular cardiac valve repair with implant procedure assigned to MS-DRGs 228 and 229. We found a total of 6,593 cases for MS-DRG 229 with an average length of stay of 4.3 days and average costs of $32,322. Of those 6,593 cases, there were 2,018 cases reporting ICD-10-PCS procedure code 02UG3JZ with an average length of stay of 1.7 days and average costs of $38,321.
For MS-DRG 273, we found a total of 7,785 cases with an average length of stay of 6.9 days and average costs of $27,200. Of those 7,785 cases, there were 6 cases reporting a procedure code for a transcatheter cardiac valve repair with an average length of stay of 7.5 days and average costs of $52,370. We found a total of 20,434 cases in MS-DRG 274 with an average length of stay of 2.3 days and average costs of $22,771. Of those 20,434 cases, there were 7 cases reporting a procedure code for a transcatheter cardiac valve repair with an average length of stay of 1.4 days and average costs of $28,152.
As also indicated in the proposed rule, we also analyzed cases reporting any one of the procedure codes listed above describing a transcatheter cardiac valve replacement procedure in MS-DRGs 266 and 267. Our findings are shown in the table below.

As shown in the table, there was a total of 15,079 cases with an average length of stay of 5.6 days and average costs of $51,402 in MS-DRG 266. For MS-DRG 267, there was a total of 20,845 cases with an average length of stay of 2.4 days and average costs of $41,891.
As stated previously and in the proposed rule, the requestor noted that ICD-10-PCS procedure code 02UG3JZ describing a transcatheter mitral valve repair with implant procedure is the only endovascular cardiac valve intervention with implant procedure assigned to MS-DRGs 228 and 229. The data analysis shows that for the cases reporting procedure code 02UG3JZ in MS-DRGs 228 and 229, the average length of stay and average costs are aligned with the average length of stay and average costs of cases in MS-DRGs 266 and 267, respectively.
The data also show that, for MS-DRGs 216, 217, 218, 219, 220, and 221 and for MS-DRG 274, the average length of stay for cases reporting a transcatheter cardiac valve with implant procedure is shorter than the average length of stay for all the cases in their assigned MS-DRG. For MS-DRG 273, the average length of stay for cases reporting a transcatheter cardiac valve with implant procedure is slightly longer (7.5 days versus 6.9 days). In addition, the average costs for the cases reporting a transcatheter cardiac valve with implant procedure are higher when compared to all the cases in their assigned MS-DRG with the exception of MS-DRG 217 ($40,707 versus $47,299) and MS-DRG 221($29,646 versus $33,577).
In the proposed rule, we stated that our clinical advisors continue to believe that transcatheter cardiac valve repair procedures are not the same as a transcatheter (endovascular) cardiac valve replacement. However, we stated that they agreed with the requestor and, based on our data analysis, that these procedures are more clinically coherent in that they also describe endovascular cardiac valve interventions with implants and are similar in terms of average length of stay and average costs to cases in MS-DRGs 266 and 267 when compared to other procedures in their current MS-DRG assignment. For these reasons, we stated that our clinical advisors agreed that we should propose to reassign the endovascular cardiac valve repair procedures (supplement procedures) listed previously to the endovascular cardiac valve replacement MS-DRGs.
We also analyzed the impact of grouping the endovascular cardiac valve repair with implant (supplement) procedures with the endovascular cardiac valve replacement procedures. The following table reflects our findings for the proposed revised endovascular cardiac valve (supplement) procedures with the endovascular cardiac valve replacement MS-DRGs with a 2-way severity level split.

As shown in the table, there was a total of 16,922 cases for the endovascular cardiac valve replacement and supplement procedures with MCC group, with an average length of stay of 5.7 days and average costs of $51,564. There was a total of 22,958 cases for the endovascular cardiac valve replacement and supplement procedures without MCC group, with an average length of stay of 2.4 days and average costs of $41,563. As indicated in the proposed rule, we applied the criteria to create subgroups for the two-way severity level split for the proposed revised MS-DRGs and found that all five criteria were met. For the proposed revised MS-DRGs, there is at least (1) 500 or more cases in the MCC group or in the without MCC subgroup; (2) 5 percent or more of the cases in the MCC group or in the without MCC subgroup; (3) a 20 percent difference in average costs between the MCC group and the without MCC group; (4) a $2,000 difference in average costs between the MCC group and the without MCC group; and (5) a 3-percent reduction in cost variance, indicating that the proposed severity level splits increase the explanatory power of the base MS-DRG in capturing differences in expected cost between the proposed MS-DRG severity level splits by at least 3 percent and thus improve the overall accuracy of the IPPS payment system.
As stated in the proposed rule, during our review of the transcatheter cardiac valve repair (supplement) procedures in MS-DRGs 216, 217, 218, 219, 220, and 221, MS-DRGs 228 and 229, and MS-DRGs 273 and 274, our clinical advisors recommended that we also analyze the claims data to identify other (non-supplement) transcatheter (endovascular) procedures that involve the cardiac valves and are assigned to those same MS-DRGs to determine if additional modifications may be warranted, consistent with our ongoing efforts to refine the ICD-10 MS-DRGs.
We analyzed the following ICD-10-PCS procedure codes that are currently assigned to MS-DRGs 216, 217, 218, 219, 220, and 221.
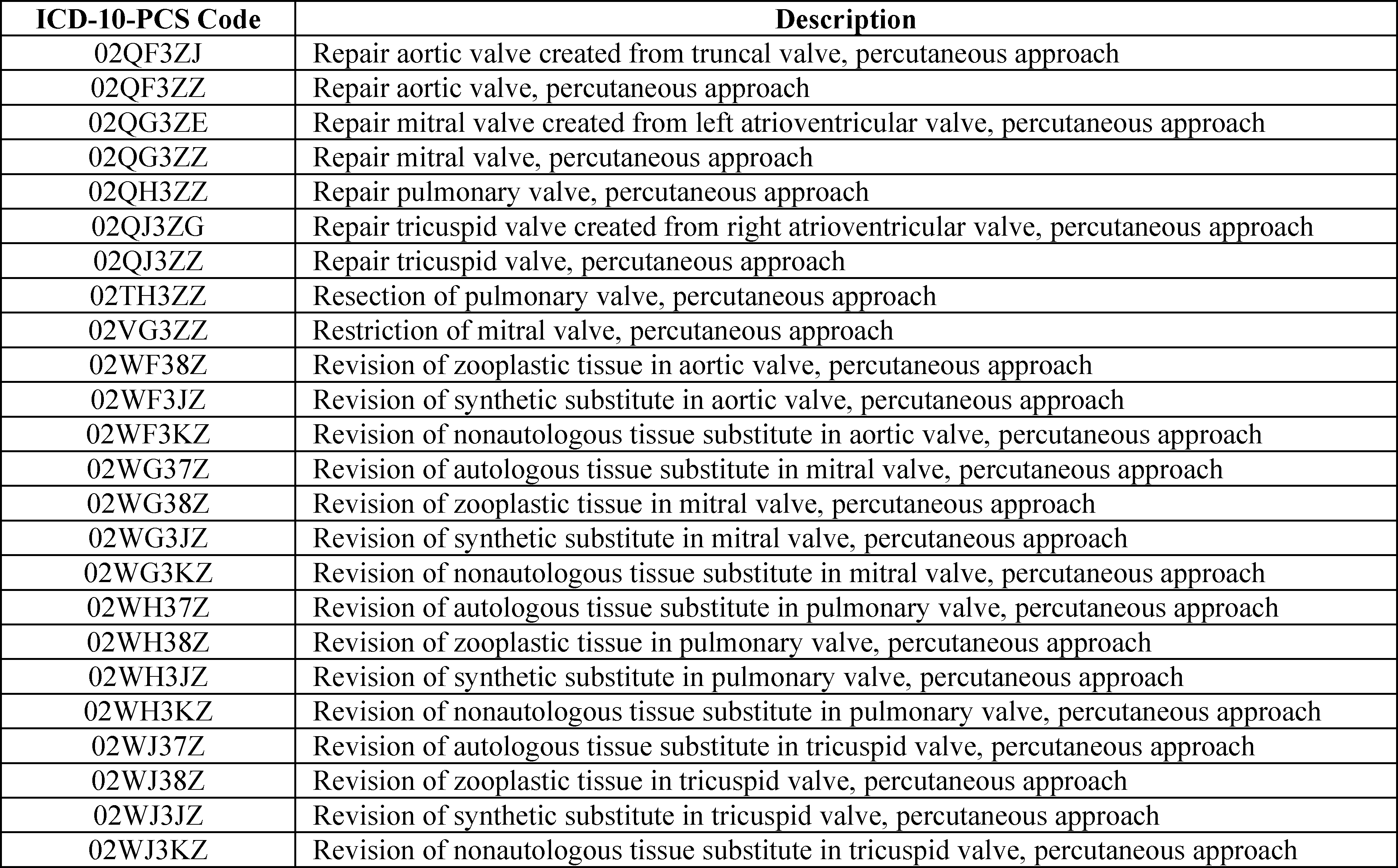
We also analyzed ICD-10-PCS procedure code 02TH3ZZ (Resection of pulmonary valve, percutaneous approach) that is currently assigned to MS-DRGs 228 and 229. Lastly, we analyzed the following ICD-10-PCS procedure codes that are currently assigned to MS-DRGs 273 and 274.

We analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for cases reporting any of the above listed procedure codes in MS-DRGs 216, 217, 218, 219, 220, and 221, MS-DRGs 228 and 229, and MS-DRGs 273 and 274. Our findings are shown in the following tables. We noted in the proposed rule that there were no cases found in MS-DRGs 228 and 229 reporting ICD-10-PCS procedure code 02TH3ZZ (Resection of pulmonary valve, percutaneous approach).


In the proposed rule, we stated we found that the overall frequency with which cases reporting at least one of the above ICD-10-PCS procedure codes were reflected in the claims data was 2,075 times with an average length of stay of 8.5 days and average costs of $27,838. ICD-10-PCS procedure code 027F3ZZ (Dilation of aortic valve, percutaneous approach) had the highest frequency of 1,720 times with an average length of stay of 8.6 days and average costs of $25,265. We also found that cases reporting ICD-10-PCS procedure code 02WF3KZ (Revision of nonautologous tissue substitute in aortic valve, percutaneous approach) had the highest average costs of $69,030 with an average length of stay of 1 day. While not displayed above, we also noted that, of the 7,785 cases found in MS-DRG 273, from the remaining procedure codes describing procedures other than those performed on a cardiac valve, there were 4,920 cases reporting ICD-10-PCS procedure code 02583ZZ (Destruction of conduction mechanism, percutaneous approach) with an average length of stay of 6.6 days and average costs of $26,800, representing approximately 63 percent of all the cases in that MS-DRG. In addition, of the 20,434 cases in MS-DRG 274, from the remaining procedure codes describing procedures other than those performed on a cardiac valve, there were 9,268 cases reporting ICD-10-PCS procedure code 02583ZZ (Destruction of conduction mechanism, percutaneous approach) with an average length of stay of 3.2 days and average costs of $21,689, and 8,775 cases reporting ICD-10-PCS procedure code 02L73DK (Occlusion of left atrial appendage with intraluminal device, percutaneous approach) with an average length of stay of 1.2 days and average costs of $25,476, representing approximately 88 percent of all the cases in that MS-DRG.
We stated in the proposed rule that after analyzing the claims data to identify the overall frequency with which the other (non-supplement) ICD-10-PCS procedure codes describing a transcatheter (endovascular) cardiac valve procedure were reported and assigned to MS-DRGs 216, 217, 218, 219, 220, and 221, MS-DRGs 228 and 229, and MS-DRGs 273 and 274, our clinical advisors suggested that these other cardiac valve procedures should be grouped together because the procedure codes are describing procedures performed on a cardiac valve with a percutaneous (transcatheter/endovascular) approach, they can be performed in a cardiac catheterization laboratory, they require that the interventional cardiologist have special additional training and skills, and often require additional ancillary procedures and equipment, such as trans-esophageal echocardiography, to be available at the time of the procedure. Our clinical advisors noted that these procedures are generally considered more complicated and resource-intensive, and form a clinically coherent group. They also noted that the majority of procedures currently being reported in MS-DRGs 273 and 274 are procedures other than those involving a cardiac valve and, therefore, believed that reassignment of the other (non-supplement) ICD-10-PCS procedure codes describing a transcatheter (endovascular) cardiac valve procedure would have minimal impact to those MS-DRGs.
We then analyzed the impact of grouping the other transcatheter cardiac valve procedures. The following table reflects our findings for the suggested other endovascular cardiac valve procedures MS-DRGs with a 2-way severity level split.

As shown in the table, there were 1,527 cases for the other endovascular cardiac valve procedures with MCC group, with an average length of stay of 9.7 days and average costs of $27,801. There was a total of 560 cases for the other endovascular cardiac valve procedures without MCC group, with an average length of stay of 3.9 days and average costs of $17,027. As stated in the proposed rule, we applied the criteria to create subgroups for the two-way severity level split for the suggested MS-DRGs and found that all five criteria were met. For the suggested MS-DRGs, there is at least (1) 500 or more cases in the MCC group or in the without MCC subgroup; (2) 5 percent or more of the cases in the MCC group or in the without MCC subgroup; (3) a 20 percent difference in average costs between the MCC group and the without MCC group; (4) at least a $2,000 difference in average costs between the MCC group and the without MCC group; and (5) a 3-percent reduction in cost variance, indicating that the proposed severity level splits increase the explanatory power of the base MS-DRG in capturing differences in expected cost between the proposed MS-DRG severity level splits by at least 3 percent and thus improve the overall accuracy of the IPPS payment system.
For FY 2020, we proposed to modify the structure of MS-DRGs 266 and 267 by reassigning the procedure codes describing a transcatheter cardiac valve repair (supplement) procedure from the list above and to revise the title of these MS-DRGs. We also proposed to revise the title of MS-DRGs 266 from “Endovascular Cardiac Valve Replacement with MCC” to “Endovascular Cardiac Valve Replacement and Supplement Procedures with MCC” and the title of MS-DRG 267 from “Endovascular Cardiac Valve Replacement without MCC” to “Endovascular Cardiac Valve Replacement and Supplement Procedures without MCC”, to reflect the proposed restructuring. In addition, we proposed to create two new MS-DRGs with a two-way severity level split for the remaining (non-supplement) transcatheter cardiac valve procedures listed above. These proposed new MS-DRGs are proposed new MS-DRG 319 (Other Endovascular Cardiac Valve Procedures with MCC) and proposed new MS-DRG 320 (Other Endovascular Cardiac Valve Procedures without MCC), which would also conform with the severity level split of MS-DRGs 266 and 267. We proposed to reassign the procedure codes from their current MS-DRGs to the proposed new MS-DRGs.
Comment: Several commenters agreed with the proposal to reassign the procedure codes describing a transcatheter cardiac valve repair (supplement) procedure from their current MS-DRG assignments as displayed and discussed above, to proposed revised MS-DRGs 266 and 267. Commenters also agreed with our proposal to revise the titles for MS-DRGs 266 and 267 to reflect the proposed restructuring. Commenters noted the procedural technique, skills, staff, equipment and average costs of the transcatheter cardiac valve repair (supplement) procedures closely correspond with other transcatheter valve procedures that are currently classified within MS-DRGs 266 and 267. Commenters stated the proposal ensures that the new MS-DRG assignments accurately capture the resource utilization and clinical coherence for these transcatheter cardiac valve procedures. Commenters stated that the procedure for transcatheter mitral valve repair (TMVR) with implant (e.g., Mitraclip®), identified by ICD-10-PCS procedure code 02UG3JZ (Supplement mitral valve with synthetic substitute, percutaneous approach) has demonstrated evidence-based clinical benefits and the proposal would allow effective treatment options for high risk patients where open heart surgery is not an option. Other commenters commended CMS for reviewing the MS-DRG assignment for transcatheter cardiac valve procedures and proposing to reassign the supplement procedures to MS-DRGs 266 and 267 since, according to the commenters, these MS-DRGs were specifically created to classify these kinds of patients. Commenters also stated that the proposal ensures more appropriate payment to providers for these procedures. A commenter who expressed support for the proposal encouraged CMS to continue to monitor these MS-DRGs as therapies continue to evolve and future modifications may be warranted.
Response: We appreciate the commenters' support. We agree the proposal would accurately capture the resource utilization and clinical coherence for these transcatheter cardiac valve procedures. Consistent with our annual process of reviewing the MS-DRGs, we will continue to monitor cases to determine if any additional adjustments are warranted.
Comment: Some commenters also agreed with the proposal to create new MS-DRGs 319 and 320 for the other transcatheter (non-supplement) cardiac valve procedures and stated this would better reflect the resource consumption for these patients. A commenter who supported the proposal requested that CMS clarify that the procedures can be performed by both interventional cardiologists, as well as cardiothoracic surgeons. This commenter agreed that, regardless of the provider performing the procedure, additional training and skills are required. The commenter also recommended that CMS continue to monitor the claims data for the affected procedure codes to ensure that unintended consequences do not occur and patient access is not at risk.
A few commenters recommended that CMS delay the proposed reassignment of non-supplement transcatheter cardiac valve procedures to proposed new MS-DRGs 319 and 320 until more data informing resource use for non-supplement percutaneous cardiac valve procedures becomes available and further consideration is given to clinical coherence. A commenter believed that reassignment of these procedures at this time is premature and that a decision by CMS to delay the implementation of this proposed policy specific to non-supplement valve procedures by percutaneous approach would have minimal impact on the adoption and implementation of the proposed separate policy related to the reassignment of transcatheter cardiac valve repair (supplement) procedures to MS-DRGs 266 and 267. Another commenter expressed concern that not all the procedure codes describing non-supplement transcatheter cardiac valve procedures included in the proposed reassignment to proposed new MS-DRGs 319 and 320 appear to be consistent with the rationale presented in the proposed rule nor did the analysis identify all the potentially impacted cases and therefore, according to the commenter, the analysis does not sufficiently estimate the impact on providers for FY 2020.
Response: We thank the commenters for their support and feedback. We wish to clarify that the transcatheter (non-supplement) cardiac valve procedures can be performed by both interventional cardiologists, as well as cardiothoracic surgeons. Our clinical advisors agree with the commenter that regardless of the provider performing the procedure, additional training and skills are required.
We disagree with delaying the proposed reassignment of non-supplement transcatheter cardiac valve procedures to proposed new MS-DRGs 319 and 320 and that reassignment of these procedures at this time is premature. We also disagree with the commenter who expressed concern that not all the procedure codes describing non-supplement transcatheter cardiac valve procedures included in the proposed reassignment to proposed new MS-DRGs 319 and 320 appear to be consistent with the rationale presented in the proposed rule. As discussed in the proposed rule and previously in this section, our clinical advisors, as well as several other commenters, supported grouping these other cardiac valve procedures together because the procedure codes are describing procedures performed on a cardiac valve with a percutaneous (transcatheter/endovascular) approach, they can be performed in a cardiac catheterization laboratory, they require special additional training and skills, and often require additional ancillary procedures and equipment. With regard to the commenter's concern that the analysis did not identify all the potentially impacted cases and therefore does not sufficiently estimate the impact on providers for FY 2020, we note that the analysis we provided was based on the MS-DRGs that were discussed under the proposal for cases that reported any of the non-supplement transcatheter cardiac valve procedures. (If no cases were found to report one of the listed procedure codes describing a non-supplement transcatheter cardiac valve procedure then that procedure code was not reflected in the data analysis table). As stated in the proposed rule, we presented the impact of grouping the transcatheter (non-supplement) cardiac valve procedures with a 2-way severity level split. The analysis was based on the September 2018 update of the FY 2018 MedPAR data and included the proposed changes to the CC/MCC severity level designations. While, as previously noted, we do not generally perform any further MS-DRG analysis of claims data for purposes of the final rule, in response to the commenter's concern regarding whether the analysis identified all potentially impacted cases, we further examined the proposed 2-way severity level split using the March 2019 update of the FY 2018 MedPAR data.

As shown in the table, there were 1,700 cases for the other endovascular cardiac valve procedures with MCC group, with an average length of stay of 10.1 days and average costs of $29,181. There was a total of 624 cases for the other endovascular cardiac valve procedures without MCC group, with an average length of stay of 3.9 days and average costs of $16,706. Similar to our process discussed in the proposed rule, we again applied the criteria to create subgroups for the two way severity level split for the proposed MS-DRGs and found that all five criteria were met. We note that, as discussed in section II.F.14.c.1. of the preamble of this final rule, we are generally not finalizing the proposed changes to the CC/MCC severity level designations that were considered under the comprehensive CC/MCC analysis. Therefore, the above updated analysis reflects the finalized policy.
For the reasons noted previously, we continue to believe it is appropriate to group all the non-supplement transcatheter cardiac valve procedures together, and the updated data analysis also continues to support the two way severity level split. In response to the commenter's recommendation that we monitor the claims data for the affected procedure codes to ensure that unintended consequences do not occur and patient access is not put at risk, consistent with our annual process of reviewing the MS-DRGs, we will continue to monitor cases to determine if any additional modifications are warranted. For the reasons described above and after consideration of the public comments we received, we are finalizing our proposal to modify the structure of MS-DRGs 266 and 267 by reassigning the procedure codes describing a transcatheter cardiac valve repair (supplement) procedure from the list above and to revise the title of MS-DRG 266 from “Endovascular Cardiac Valve Replacement with MCC” to “Endovascular Cardiac Valve Replacement and Supplement Procedures with MCC” and to revise the title of MS-DRG 267 from “Endovascular Cardiac Valve Replacement without MCC” to “Endovascular Cardiac Valve Replacement and Supplement Procedures without MCC”. In addition, we are finalizing our proposal to create new MS-DRG 319 (Other Endovascular Cardiac Valve Procedures with MCC) and new MS-DRG 320 (Other Endovascular Cardiac Valve Procedures without MCC) and reassigning the non-supplement transcatheter cardiac valve procedure codes displayed and discussed earlier in this section from their current MS-DRGs to these new MS-DRGs, under the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
b. Revision of Pacemaker Lead
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19193), in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41189 through 41190), we finalized our proposal to maintain the Version 35 ICD-10 MS-DRG GROUPER logic for the Version 36 ICD-10 MS-DRG GROUPER logic within MS-DRGs 260, 261, and 262 (Cardiac Pacemaker Revision Except Device Replacement with MCC, with CC and without CC/MCC, respectively) so that cases reporting any of the ICD-10-PCS procedure codes describing procedures involving pacemakers and related procedures and associated devices would continue to be assigned to those MS-DRGs under MDC 5 because they are reported when a pacemaker device requires revision and they have a corresponding circulatory system diagnosis. We also discussed and finalized the addition of ICD-10-PCS procedure codes 02H63MZ (Insertion of cardiac lead into right atrium, percutaneous approach) and 02H73MZ (Insertion of cardiac lead into left atrium, percutaneous approach) to the GROUPER logic as non-O.R. procedures that impact the MS-DRG assignment when reported as stand-alone codes for the insertion of a pacemaker lead within MS-DRGs 260, 261, and 262 in response to a commenter's suggestion.
After publication of the FY 2019 IPPS/LTCH PPS final rule, it was brought to our attention that ICD-10-PCS procedure code 02H60JZ (Insertion of pacemaker lead into right atrium, open approach) was inadvertently omitted from the GROUPER logic for MS-DRGs 260, 261, and 262. This procedure code is designated as a non-O.R. procedure. However, we note that, within MDC 5, in MS-DRGs 242, 243, and 244, this procedure code is part of a code pair that requires another procedure code (cluster). In the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to add procedure code 02H60JZ to the list of non-O.R. procedures that would impact MS-DRGs 260, 261, and 262 when reported as a stand-alone procedure code, consistent with ICD-10-PCS procedure codes 02H63JZ (Insertion of pacemaker lead into right atrium, percutaneous approach) and 02H64JZ (Insertion of pacemaker lead into right atrium, percutaneous endoscopic approach), which also describe the insertion of a pacemaker lead into the right atrium. We stated in the proposed rule that, if the proposal is finalized, we would make conforming changes to the ICD-10 MS-DRG Definitions Manual Version 37.
Comment: Commenters agreed with the proposal to add procedure code 02H60JZ to the list of non-O.R. procedures that would impact MS-DRGs 260, 261, and 262 when reported as a stand-alone procedure code.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add procedure code 02H60JZ to the list of non-O.R. procedures that would impact MS-DRGs 260, 261, and 262 when reported as a stand-alone procedure code under the ICD-10 MS-DRGs Version 37, effective October 1, 2019, and will make conforming changes to the ICD-10 MS-DRG Definitions Manual Version 37.
6. MDC 8 (Diseases and Disorders of the Musculoskeletal System and Connective Tissue)
a. Knee Procedures With Principal Diagnosis of Infection
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19193 through 19199), we received a request to add ICD-10-CM diagnosis codes M00.9 (Pyogenic arthritis, unspecified) and A54.42 (Gonococcal arthritis) to the list of principal diagnoses for MS-DRGs 485, 486, and 487 (Knee Procedure with Principal Diagnosis of Infection with MCC, with CC, and without CC/MCC, respectively) in MDC 8. The requestor believed that adding diagnosis code M00.9 is necessary to accurately recognize knee procedures that are performed with a principal diagnosis of infectious arthritis, including those procedures performed when the specific infectious agent is unknown. The requestor stated that, currently, only diagnosis codes describing infections caused by a specific bacterium are included in MS-DRGs 485, 486, and 487. The requestor stated that additional diagnosis codes such as M00.9 are indicated for knee procedures performed as a result of infection because pyogenic arthritis can reasonably be diagnosed based on the patient's history and clinical symptoms, even if a bacterial infection is not confirmed by culture. For example, the requestor noted that a culture may present negative for infection if a patient has been treated with antibiotics prior to knee surgery, but other clinical signs may indicate a principal diagnosis of joint infection. In the absence of a culture identifying an infection by a specific bacterium, the requestor stated that ICD-10-CM diagnosis code M00.9 should also be included as a principal diagnosis in MS-DRGs 485, 486, and 487.
The requestor also asserted that ICD-10-CM diagnosis code A54.42 should be added to the list of principal diagnoses for MS-DRGs 485, 486, and 487 because gonococcal arthritis is also an infectious type of arthritis that can be an indication for a knee procedure.
We noted in the proposed rule that, currently, cases reporting ICD-10-CM diagnosis codes M00.9 or A54.42 as a principal diagnosis group to MS-DRGs 488 and 489 (Knee Procedures without Principal Diagnosis of Infection with and without CC/MCC, respectively) when a knee procedure is also reported on the claim.
As indicated in the proposed rule, we analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for ICD-10-CM diagnosis codes M00.9 and A54.42, which are currently assigned to medical MS-DRGs 548, 549, and 550 (Septic Arthritis with MCC, with CC, and without CC/MCC, respectively) in the absence of a surgical procedure. Our findings are shown in the following table.

As shown in the table, we found a total of 2,172 cases in MS-DRGs 548, 549, and 550. A total of 601 cases were reported in MS-DRG 548, with an average length of stay of 8.1 days and average costs of $13,974. Cases in MS-DRG 548 with a principal diagnosis of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) accounted for 312 of these 601 cases, and reported an average length of stay of 7.6 days and average costs of $13,177. As we stated in the proposed rule, none of the cases in MS-DRG 548 had a principal diagnosis of gonococcal arthritis (ICD-10-CM diagnosis code A54.42).
The total number of cases reported in MS-DRG 549 was 1,169, with an average length of stay of 5 days and average costs of $8,547. Within this MS-DRG, 686 cases had a principal diagnosis described by ICD-10-CM diagnosis code M00.9, with an average length of stay of 4.7 days and average costs of $7,976. Two of the cases reported in MS-DRG 549 had a principal diagnosis described by ICD-10-CM diagnosis code A54.42. These 2 cases had an average length of stay of 8 days and average costs of $7,070.
The total number of cases reported in MS-DRG 550 was 402, with an average length of stay of 3.5 days and average costs of $6,317. Within this MS-DRG, 260 cases had a principal diagnosis described by ICD-10-CM diagnosis code M00.9 with an average length of stay of 3.2 days and average costs of $6,209. Three of the cases reported in MS-DRG 550 had a principal diagnosis described by ICD-10-CM diagnosis code A54.42. These 3 cases had an average length of stay of 2.3 days and average costs of $3,929.
In summary, for MS-DRGs 548, 549, and 550, there were 1,258 cases that reported ICD-10-CM diagnosis code M00.9 as the principal diagnosis and 5 cases that reported ICD-10-CM diagnosis code A54.42 as the principal diagnosis. We noted that, overall, our data analysis suggests that the MS-DRG assignment for cases reporting ICD-10-CM diagnosis codes M00.9 and A54.42 is appropriate based on the average costs and average length of stay. However, we stated in the proposed rule that it is unclear how many of these cases involved infected knee joints because neither ICD-10-CM diagnosis code M00.9 nor A54.42 is specific to the knee.
We then analyzed claims data for MS-DRGs 485, 486, and 487 (Knee Procedures with Principal Diagnosis of Infection with MCC, with CC, and without CC/MCC, respectively) and for MS-DRGs 488 and 489 (Knee Procedures without Principal Diagnosis of Infection with and without CC/MCC, respectively). For MS-DRGs 488 and 489, we also analyzed claims data for cases reporting a knee procedure with ICD-10-CM diagnosis code M00.9 or A54.42 as a principal diagnosis, as these are the MS-DRGs to which such cases would currently group. Our findings are shown in the following table.

As shown in the table, we found a total of 1,021 cases reported in MS-DRG 485, with an average length of stay of 9.7 days and average costs of $23,980. We found a total of 2,260 cases reported in MS-DRG 486, with an average length of stay of 6.0 days and average costs of $16,060. The total number of cases reported in MS-DRG 487 was 614, with an average length of stay of 4.2 days and average costs of $12,396. For MS-DRG 488, we found a total of 2,857 cases with an average length of stay of 4.8 days and average costs of $14,197. Of these 2,857 cases, we found 524 cases that reported a principal diagnosis of pyogenic arthritis (ICD-10-CM diagnosis code M00.9), with an average length of stay of 7.1 days and average costs of $16,894. There were no cases found that reported a principal diagnosis of gonococcal arthritis (ICD-10-CM diagnosis code A54.42). For MS-DRG 489, we found a total of 2,416 cases with an average length of stay of 2.4 days and average costs of $9,217. Of these 2,416 cases, we found 195 cases that reported a principal diagnosis of pyogenic arthritis (ICD-10-CM diagnosis code M00.9), with an average length of stay of 4.1 days and average costs of $9,526. We found 1 case that reported a principal diagnosis of gonococcal arthritis (ICD-10-CM diagnosis code A54.42) in MS-DRG 489, with an average length of stay of 8 days and average costs of $10,810.
Upon review of the data, we noted in the proposed rule that the average costs and average length of stay for cases reporting a principal diagnosis of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) in MS-DRG 488 are higher than the average costs and average length of stay for all cases in MS-DRG 488. We found similar results for MS-DRG 489 for the cases reporting diagnosis code M00.9 or A54.42 as the principal diagnosis.
As stated in the proposed rule and earlier, the requestor recommended that ICD-10-CM diagnosis codes M00.9 and A54.42 be added to the list of principal diagnoses in MS-DRGs 485, 486, and 487 to recognize knee procedures that are performed with a principal diagnosis of an infectious type of arthritis. As we stated in the proposed rule, because these diagnosis codes are not specific to the knee in the code description, we examined the ICD-10-CM Alphabetic Index to review the entries that refer and correspond to these diagnosis codes. Specifically, we searched the Index for codes M00.9 and A54.42 and found the following entries.

We stated in the proposed rule that our clinical advisors agreed that the results of our ICD-10-CM Alphabetic Index review combined with the data analysis results support the addition of ICD-10-CM diagnosis code M00.9 to the list of principal diagnoses of infection for MS-DRGs 485, 486, and 487. The entries for diagnosis code M00.9 include infection of the knee, and as discussed above, in our data analysis, we found cases reporting ICD-10-CM diagnosis code M00.9 as a principal diagnosis in MS-DRGs 488 and 489, indicating that knee procedures are, in fact, being performed for an infectious arthritis of the knee. In addition, the average costs for cases reporting a principal diagnosis code of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) in MS-DRG 488 are similar to the average costs of cases in MS-DRG 486 ($16,894 and $16,060, respectively). We stated in the proposed rule that, because MS-DRG 488 includes cases with a CC or an MCC, we reviewed how many of the 524 cases reporting a principal diagnosis code of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) were reported with a CC or an MCC. We found that there were 361 cases reporting a CC with an average length of stay of 6 days and average costs of $14,092 and 163 cases reporting an MCC with an average length of stay of 9.5 days and average costs of $23,100. Therefore, the cases in MS-DRG 488 reporting a principal diagnosis code of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) with an MCC have average costs that are consistent with the average costs of cases in MS-DRG 485 ($23,100 and $23,980, respectively), and the cases with a CC have average costs that are consistent with the average costs of cases in MS-DRG 486 ($14,092 and $16,060, respectively), as noted above. We also noted that the average length of stay for cases reporting a principal diagnosis code of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) with an MCC in MS-DRG 488 is similar to the average length of stay for cases in MS-DRG 485 (9.5 days and 9.7 days, respectively), and the cases with a CC have an average length of stay that is equivalent to the average length of stay for cases in MS-DRG 486 (6 days and 6 days, respectively). We further noted that the average length of stay for cases reporting a principal diagnosis code of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) in MS-DRG 489 is similar to the average length of stay for cases in MS-DRG 487 (4.1 days and 4.2 days, respectively). Lastly, the average costs for cases reporting a principal diagnosis code of pyogenic arthritis (ICD-10-CM diagnosis code M00.9) in MS-DRG 489 are consistent with the average costs for cases in MS-DRG 487 ($9,526 and $12,396, respectively), with a difference of $2,870. For these reasons, we proposed to add ICD-10-CM diagnosis code M00.9 to the list of principal diagnosis codes for MS-DRGs 485, 486, and 487.
Comment: Commenters agreed with CMS' proposal to add ICD-10-CM diagnosis code M00.9 to the list of principal diagnosis codes for assignment to MS-DRGs 485, 486 and 487. The commenters stated that the proposal was reasonable, given the ICD-10-CM diagnosis code and the information provided.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-CM diagnosis code M00.9 to the list of principal diagnosis codes for assignment to MS-DRGs 485, 486 and 487 in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
In the proposed rule, we stated that our clinical advisors did not support the addition of ICD-10-CM diagnosis code A54.42 to the list of principal diagnosis codes for MS-DRGs 485, 486, and 487 because ICD-10-CM diagnosis code A54.42 is not specifically indexed to include the knee or any infection in the knee. Therefore, we did not propose to add ICD-10-CM diagnosis code A54.42 to the list of principal diagnosis codes for these MS-DRGs.
Comment: Commenters did not support CMS' proposal to not add ICD-10-CM diagnosis code A54.42 to the list of codes for these MS-DRGs. Commenters noted that although A54.42 is not specific to the knee, the code is intended to be used for any joint, similar to code M00.9. Commenters also noted that the GROUPER logic for MS-DRGs 485, 486 and 487 that requires the combination of a principal diagnosis code and an ICD-10-PCS procedure code for a knee procedure will ensure that cases that report a principal diagnosis code of A54.42 and a knee procedure are clinically similar to other cases in MS-DRGs 485, 486 and 487.
Response: We agree with commenters that diagnosis code A54.42 would be the appropriate code for a diagnosis of gonococcal arthritis of the knee although the Index entry is not specific. Our clinical advisors reviewed this issue and the ICD-10-CM Alphabetic index and noted that there are no other diagnosis codes in the subcategory A54.- series (Gonococcal infection) that are more specific to the knee. Our clinical advisors noted that although there was only one case reporting gonococcal arthritis as the principal diagnosis with a knee procedure performed in the September 2018 update of the FY 2018 MedPAR file, they agreed that based on the result of further review, including consideration of the commenters' concerns, there is merit in adding A54.42 to MS-DRGs 485, 486 and 487 because diagnosis code A54.42 would be the appropriate code to report a diagnosis of gonococcal arthritis of the knee. We agree with commenters that this reassignment is consistent with the reassignment of ICD-10-CM diagnosis code M00.9 because, although the Index entries do not specifically include the knee or any infection of the knee, diagnosis code A54.42 would also be used to report an infection of the knee. Therefore, after consideration of the public comments that we received and for the reasons described, we are finalizing the assignment of ICD-10-CM diagnosis code A54.42 to the list of principal diagnosis codes for assignment to MS-DRGs 485, 486, and 487 (Knee Procedure with Principal Diagnosis of Infection with MCC, with CC, and without CC/MCC, respectively) in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
In the FY 2020 IPPS/LTCH PPS proposed rule, we stated that upon review of the existing list of principal diagnosis codes for MS-DRGs 485, 486, and 487, our clinical advisors recommended that we review the following ICD-10-CM diagnosis codes currently included on the list of principal diagnosis codes because the codes are not specific to the knee.

These ICD-10-CM diagnosis codes are currently assigned to medical MS-DRGs 559, 560, and 561 (Aftercare, Musculoskeletal System and Connective Tissue with MCC, with CC, and without CC/MCC, respectively) within MDC 8 in the absence of a surgical procedure. Similar to the process described above, in the proposed rule, we stated that we examined the ICD-10-CM Alphabetic Index to review the entries that refer and correspond to the diagnosis codes shown in the table above. We found the following entries.

The Index entries for the ICD-10-CM diagnosis codes listed above reflect terms relating to an infection. However, none of the entries is specific to the knee. In addition, in the proposed rule we noted that there are other diagnosis codes in the subcategory T84.5-series (Infection and inflammatory reaction due to internal joint prosthesis) that are specific to the knee. For example, ICD-10-CM diagnosis code T84.53X- (Infection and inflammatory reaction due to internal right knee prosthesis) or ICD-10-CM diagnosis code T84.54X- (Infection and inflammatory reaction due to internal left knee prosthesis) with the appropriate 7th digit character to identify initial encounter, subsequent encounter or sequela, would be reported to identify a documented infection of the right or left knee due to an internal prosthesis. We further noted that these ICD-10-CM diagnosis codes (T84.53X- and T84.54X-) with the 7th character “A” for initial encounter are currently already in the list of principal diagnosis codes for MS-DRGs 485, 486, and 487.
We stated in the proposed rule that our clinical advisors supported the removal of the above ICD-10-CM diagnosis codes from the list of principal diagnosis codes for MS-DRGs 485, 486, and 487 because they are not specifically indexed to include an infection of the knee and there are other diagnosis codes in the subcategory T84.5-series that uniquely identify an infection and inflammatory reaction of the right or left knee due to an internal prosthesis as noted above.
As indicated in the proposed rule, we also analyzed claims data for MS-DRGs 485, 486 and 487 to identify cases reporting one of the above listed ICD-10-CM diagnosis codes not specific to the knee as a principal diagnosis. Our findings are shown in the following table.

For MS-DRG 485, we found 13 cases reporting one of the diagnosis codes not specific to the knee as a principal diagnosis with an average length of stay of 11.2 days and average costs of $30,765. For MS-DRG 486, we found 43 cases reporting one of the diagnosis codes not specific to the knee as a principal diagnosis with an average length of stay of 6.5 days and average costs of $15,837. For MS-DRG 487, we found 7 cases reporting one of the diagnosis codes not specific to the knee as a principal diagnosis with an average length of stay of 2.6 days and average costs of $11,362.
We stated in the proposed rule that, overall, for MS-DRGs 485, 486, and 487, there were a total of 63 cases reporting one of the ICD-10-CM diagnosis codes not specific to the knee as a principal diagnosis with an average length of stay of 7 days and average costs of $18,421. Of those 63 cases, there were 32 cases reporting a principal diagnosis code from the ICD-10-CM subcategory T84.5-series (Infection and inflammatory reaction due to internal joint prosthesis); 23 cases reporting a principal diagnosis code from the ICD-10-CM subcategory T84.6-series (Infection and inflammatory reaction due to internal fixation device), with 22 of the 23 cases reporting ICD-10-CM diagnosis code T84.69XA (Infection and inflammatory reaction due to internal fixation device of other site, initial encounter) and 1 case reporting ICD-10-CM diagnosis code T84.63XA (Infection and inflammatory reaction due to internal fixation device of spine, initial encounter); and 8 cases reporting ICD-10-CM diagnosis code M86.9 (Osteomyelitis, unspecified) as a principal diagnosis.
We stated in the proposed rule that our clinical advisors believe that there may have been coding errors among the 63 cases reporting a principal diagnosis of infection not specific to the knee. For example, 32 cases reported a principal diagnosis code from the ICD-10-CM subcategory T84.5-series (Infection and inflammatory reaction due to internal joint prosthesis) that was not specific to the knee and, as stated previously and in the proposed rule, there are other codes in this subcategory that uniquely identify an infection and inflammatory reaction of the right or left knee due to an internal prosthesis.
Based on the results of our claims analysis and input from our clinical advisors, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to remove the following ICD-10-CM diagnosis codes that do not describe an infection of the knee from the list of principal diagnosis codes for MS-DRGs 485, 486, and 487: M86.9, T84.50XA, T84.51XA, T84.52XA, T84.59XA, T84.60XA, T84.63XA, and T84.69XA. We did not propose to change the current assignment of these diagnosis codes in MS-DRGs 559, 560, and 561.
Comment: Many commenters agreed with the proposal to remove the eight diagnosis codes that do not describe an infection specific to the knee from the list of principal diagnosis codes for MS-DRGs 485, 486, and 487, and to maintain their current assignment in MS-DRGs 559, 560, and 561. A commenter did not support the proposal and believed the diagnosis of osteomyelitis should continue to be included in MS-DRGs 485, 486 and 487 because osteomyelitis describes an infection of the knee which includes cartilage, ligaments, tendons and bones.
Response: We appreciate the commenters' support. We agree that osteomyelitis as a diagnostic term describes an infection which can include cartilage, ligaments, tendons and bones. However, as discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19196), the diagnosis codes that are the subject of this proposal, including diagnosis code M86.9 (Osteomyelitis, unspecified) are not specific to the knee. There are other diagnosis codes in the subcategory M86.-series (Osteomyelitis) that are specific to the knee and will continue to be included in MS-DRGs 485, 486 and 487.
Therefore, after consideration of the comments we received, we are finalizing our proposal to remove ICD-10-CM diagnosis codes M86.9, T84.50XA, T84.51XA, T84.52XA, T84.59XA, T84.60XA, T84.63XA, and T84.69XA from the list of principal diagnosis codes for MS-DRGs 485, 486, and 487, and maintain their current assignment in MS-DRGs 559, 560, and 561 in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
In addition, we stated in the proposed rule that our clinical advisors recommended that we add the following ICD-10-CM diagnosis codes as principal diagnosis codes for MS-DRGs 485, 486, and 487 because they are specific to the knee and describe an infection.

As indicated in the proposed rule, ICD-10-CM diagnosis code A18.02 (Tuberculous arthritis of other joints) is currently assigned to medical MS-DRGs 548, 549, and 550 (Septic Arthritis with MCC, with CC, and without CC/MCC, respectively) within MDC 8 and MS-DRGs 974, 975, and 976 (HIV with Major Related Condition with MCC, with CC, and without CC/MCC, respectively) within MDC 25 (Human Immunodeficiency Virus Infections) in the absence of a surgical procedure. ICD-10-CM diagnosis codes M01.X61 (Direct infection of right knee in infectious and parasitic diseases classified elsewhere), M01.X62 (Direct infection of left knee in infectious and parasitic diseases classified elsewhere), and M01.X69 (Direct infection of unspecified knee in infectious and parasitic diseases classified elsewhere) are currently assigned to medical MS-DRGs 548, 549, and 550 (Septic Arthritis with MCC, with CC, and without CC/MCC, respectively) within MDC 8 in the absence of a surgical procedure. ICD-10-CM diagnosis codes M71.061 (Abscess of bursa, right knee), M71.062 (Abscess of bursa, left knee), M71.069 (Abscess of bursa, unspecified knee), M71.161 (Other infective bursitis, right knee), M71.162 (Other infective bursitis, left knee), and M71.169 (Other infective bursitis, unspecified knee) are currently assigned to medical MS-DRGs 557 and 558 (Tendonitis, Myositis and Bursitis with and without MCC, respectively) within MDC 8 in the absence of a surgical procedure.
Similar to the process described above, in the proposed rule we examined the ICD-10-CM Alphabetic Index to review the entries that refer and correspond to the diagnosis codes shown in the table above. We found the following entries.


We noted that there were no Index entries specifically for ICD-10-CM diagnosis codes M71.061, M71.062, M71.069, M71.161, M71.162, and M71.169. Rather, there were Index entries at the subcategory levels of M71.06- and M71.16-. We found the following entries.

We stated that our clinical advisors agreed that the results of our review of the ICD-10-CM Alphabetic Index support the addition of these ICD-10-CM diagnosis codes to MS-DRGs 485, 486, and 487 because the Index entries and/or the code descriptions clearly describe or include an infection that is specific to the knee.
Therefore, we proposed to add the following ICD-10-CM diagnosis codes to the list of principal diagnosis codes for MS-DRGs 485, 486, and 487: A18.02, M01.X61, M01.X62, M01.X69, M71.061, M71.062, M71.069, M71.161, M71.162, and M71.169.
Comment: Commenters agreed with CMS' proposal to add 10 additional ICD-10-CM diagnosis codes that are specific to the knee and describe an infection to the list of principal diagnosis codes for assignment to MS-DRGs 485, 486 and 487. The commenters stated that the proposal was reasonable, given the ICD-10-CM diagnosis codes and the information provided.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-CM diagnosis codes A18.02, M01.X61, M01.X62, M01.X69, M71.061, M71.062, M71.069, M71.161, M71.162, and M71.169 to the list of principal diagnosis codes for assignment to MS-DRGs 485, 486 and 487 in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
b. Neuromuscular Scoliosis
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19201 through 19202), we received a request to add ICD-10-CM diagnosis codes describing neuromuscular scoliosis to the list of principal diagnosis codes for MS-DRGs 456, 457, and 458 (Spinal Fusion except Cervical with Spinal Curvature or Malignancy or Infection or Extensive Fusions with MCC, with CC, and without CC/MCC, respectively). As we stated in the proposed rule, excluding the ICD-10-CM diagnosis codes that address the cervical spine, the following ICD-10-CM diagnosis codes are used to describe neuromuscular scoliosis.

The requestor asserted that all levels of neuromuscular scoliosis, except cervical, should group to the non-cervical spinal fusion MS-DRGs for spinal curvature (MS-DRGs 456, 457, and 458). The requestor also noted that the current MS-DRG logic only groups cases reporting neuromuscular scoliosis to MS-DRGs 456, 457, and 458 when neuromuscular scoliosis is reported as a secondary diagnosis. The requestor contended that it would be rare for a diagnosis of neuromuscular scoliosis to be reported as a secondary diagnosis because there is not a “code first” note in the ICD-10-CM Tabular List of Diseases and Injuries indicating to “code first” the underlying cause. We stated in the proposed rule that, according to the requestor, when a diagnosis of neuromuscular scoliosis is the reason for an admission for non-cervical spinal fusion, neuromuscular scoliosis must be sequenced as the principal diagnosis because it is the chief condition responsible for the admission. However, this sequencing, which adheres to the ICD-10-CM Official Guidelines for Coding and Reporting, prevents the admission from grouping to the non-cervical spinal fusion MS-DRGs for spinal curvature caused by neuromuscular scoliosis.
As indicated in the proposed rule, we analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for cases reporting any of the ICD-10-CM diagnosis codes describing neuromuscular scoliosis (as listed previously) as a principal diagnosis with a non-cervical spinal fusion, which are currently assigned to MS-DRGs 459 and 460 (Spinal Fusion except Cervical with MCC and without MCC, respectively). Our findings are shown in the following table.

The data reveal that there was a total of 56,500 cases in MS-DRGs 459 and 460. We found 3,903 cases reported in MS-DRG 459, with an average length of stay of 8.6 days and average costs of $46,416. Of these 3,903 cases, 3 reported a principal diagnosis code of neuromuscular scoliosis, with an average length of stay of 15.3 days and average costs of $95,745. We found a total of 52,597 cases in MS-DRG 460, with an average length of stay of 3.3 days and average costs of $28,754. Of these 52,597 cases, 8 cases reported a principal diagnosis code describing neuromuscular scoliosis, with an average length of stay of 4.3 days and average costs of $71,406. We stated in the proposed rule that the data clearly demonstrate that the average costs and average length of stay for the small number of cases reporting a principal diagnosis of neuromuscular scoliosis are higher in comparison to all the cases in their assigned MS-DRG.
We also analyzed claims data for MS-DRGs 456, 457, and 458 (Spinal Fusion except Cervical with Spinal Curvature or Malignancy or Infection or Extensive Fusions with MCC, with CC, and without CC/MCC, respectively) to identify the spinal fusion cases reporting any of the ICD-10-CM codes describing neuromuscular scoliosis (as listed previously) as a secondary diagnosis. Our findings are shown in the following table.

As we noted in the proposed rule, the data indicate that there were 1,344 cases reported in MS-DRG 456, with an average length of stay of 12 days and average costs of $66,012. Of these 1,344 cases, 6 cases reported a secondary diagnosis code describing neuromuscular scoliosis, with an average length of stay of 18.2 days and average costs of $79,809. We found a total of 3,654 cases in MS-DRG 457, with an average length of stay of 6.2 days and average costs of $47,577. Twelve of these 3,654 cases reported a secondary diagnosis code describing neuromuscular scoliosis, with an average length of stay of 4.5 days and average costs of $31,646. Finally, the 1,245 cases reported in MS-DRG 458 had an average length of stay of 3.4 days and average costs of $34,179. Of these 1,245 cases, 6 cases reported neuromuscular scoliosis as a secondary diagnosis, with an average length of stay of 3.3 days and average costs of $31,117.
We reviewed the ICD-10-CM Tabular List of Diseases for subcategory M41.4 and confirmed there is a “Code also underlying condition” note. We also reviewed the ICD-10-CM Official Guidelines for Coding and Reporting for the “code also” note at Section 1.A.12.b., which states: “A `code also' note instructs that two codes may be required to fully describe a condition, but this note does not provide sequencing direction.” We stated in the proposed rule that our clinical advisors agreed that the sequencing of the ICD-10-CM diagnosis codes is determined by which condition leads to the encounter and is responsible for the admission. They also note that there may be instances in which the underlying cause of the diagnosis of neuromuscular scoliosis is not treated or responsible for the admission.
As discussed in the proposed rule and earlier, our review of the claims data shows that a small number of cases reported neuromuscular scoliosis either as a principal diagnosis in MS-DRGs 459 and 460 or as a secondary diagnosis in MS-DRGs 456, 457, and 458. We stated that our clinical advisors agreed that while the volume of cases is small, the average costs and average length of stay for the cases reporting neuromuscular scoliosis as a principal diagnosis with a non-cervical spinal fusion currently grouping to MS-DRGs 459 and 460 are more aligned with the average costs and average length of stay for the cases reporting neuromuscular scoliosis as a secondary diagnosis with a non-cervical spinal fusion currently grouping to MS-DRGs 456, 457, and 458. Therefore, for the reasons described above, we proposed to add the following ICD-10-CM codes describing neuromuscular scoliosis to the list of principal diagnosis codes for MS-DRGs 456, 457, and 458: M41.40, M41.44, M41.45, M41.46, and M41.47.
Comment: Commenters agreed with CMS' proposal to add ICD-10-CM diagnosis codes M41.40, M41.44, M41.45, M41.46, and M41.47 that describe neuromuscular scoliosis to the list of principal diagnosis codes for assignment to MS-DRGs 456, 457 and 458 (Spinal Fusion except Cervical with Spinal Curvature of Malignancy or Infection or Extensive Fusions with MCC, with CC, and without CC/MCC, respectively). The commenters stated that the proposal was reasonable, given the ICD-10-CM diagnosis codes and the information provided. A commenter specifically expressed appreciation for CMS' display of cost and length of stay data in the analysis, in addition to the clinical factors that support our decision making.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-CM diagnosis codes M41.40, M41.44, M41.45, M41.46, and M41.47 to the list of principal diagnosis codes for assignment to MS-DRGs 456, 457 and 458 in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
c. Secondary Scoliosis and Secondary Kyphosis
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19202 through 19204), we received a request to add ICD-10-CM diagnosis codes describing secondary scoliosis and secondary kyphosis to the list of principal diagnoses for MS-DRGs 456, 457, and 458 (Spinal Fusion except Cervical with Spinal Curvature or Malignancy or Infection or Extensive Fusions with MCC, with CC, and without CC/MCC, respectively). As we indicated in the proposed rule, excluding the ICD-10-CM diagnosis codes that address the cervical spine, the following ICD-10-CM diagnosis codes are used to describe secondary scoliosis.

Excluding the ICD-10-CM diagnosis codes that address the cervical spine, the following ICD-10-CM diagnosis codes are used to describe secondary kyphosis.

The requestor stated that generally in cases of diagnoses of secondary scoliosis or kyphosis, the underlying cause of the condition is not treated or is not responsible for the admission. If a patient is admitted for surgery to correct non-cervical spinal curvature, it is appropriate to sequence the diagnosis of secondary scoliosis or secondary kyphosis as principal diagnosis. However, reporting a diagnosis of secondary scoliosis or secondary kyphosis as the principal diagnosis with a non-cervical spinal fusion procedure results in the case grouping to MS-DRG 459 or 460 (Spinal Fusion except Cervical with MCC and without MCC, respectively), instead of the spinal fusion with spinal curvature MS-DRGs 456, 457, and 458.
As indicated in the proposed rule, we analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 459 and 460 to determine the number of cases reporting an ICD-10-CM diagnosis code describing secondary scoliosis or secondary kyphosis as the principal diagnosis. Our findings are shown in the following table.

As shown in the table, we found a total of 3,903 cases in MS-DRG 459, with an average length of stay of 8.6 days and average costs of $46,416. Of these 3,903 cases, we found 4 cases that reported a principal diagnosis of secondary scoliosis, with an average length of stay of 7.3 days and average costs of $56,024. We also found 4 cases that reported a principal diagnosis of secondary kyphosis, with an average length of stay of 5.8 days and average costs of $41,883. For MS-DRG 460, we found a total of 52,597 cases with an average length of stay of 3.3 days and average costs of $28,754. Of these 52,597 cases, we found 34 cases that reported a principal diagnosis of secondary scoliosis, with an average length of stay of 3.6 days and average costs of $34,424. We found 31 cases that reported a principal diagnosis of secondary kyphosis in MS-DRG 460, with an average length of stay of 4.6 days and average costs of $42,315.
We also analyzed claims data for MS-DRGs 456, 457, and 458 to determine the number of cases reporting an ICD-10-CM diagnosis code describing secondary scoliosis or secondary kyphosis as a secondary diagnosis. Our findings are shown in the following table.

As we stated in the proposed rule, the data indicate that there were 1,344 cases in MS-DRG 456, with an average length of stay of 12 days and average costs of $66,012. Of these 1,344 cases, there were 37 cases that reported a secondary diagnosis of secondary scoliosis, with an average length of stay of 7.7 days and average costs of $58,009. There were also 52 cases in MS-DRG 456 reporting a secondary diagnosis of secondary kyphosis, with an average length of stay of 12 days and average costs of $78,865. In MS-DRG 457, there was a total of 3,654 cases, with an average length of stay of 6.2 days and average costs of $47,577. Of these 3,654 cases, there were 187 cases that reported secondary scoliosis as a secondary diagnosis, with an average length of stay of 4.9 days and average costs of $37,655. In MS-DRG 457, there were also 114 cases that reported a secondary diagnosis of secondary kyphosis, with an average length of stay of 5.2 days and average costs of $37,357. Finally, there was a total of 1,245 cases in MS-DRG 458, with an average length of stay of 3.4 days and average costs of $34,179. Of these 1,245 cases, there were 190 cases that reported a secondary diagnosis of secondary scoliosis, with an average length of stay of 3 days and average costs of $29,052. There were 39 cases in MS-DRG 458 that reported a secondary diagnosis of secondary kyphosis, with an average length of stay of 3.7 days and average costs of $31,015.
We stated in the proposed rule that our clinical advisors agreed that the average length of stay and average costs for the small number of cases reporting secondary scoliosis or secondary kyphosis as a principal diagnosis with a non-cervical spinal fusion currently grouping to MS-DRGs 459 and 460 are generally more aligned with the average length of stay and average costs for the cases reporting secondary scoliosis or secondary kyphosis as a secondary diagnosis with a non-cervical spinal fusion currently grouping to MS-DRGs 456, 457, and 458. They also noted that there may be instances in which the underlying cause of the diagnosis of secondary scoliosis or secondary kyphosis is not treated or responsible for the admission. Therefore, for the reasons described above, we proposed to add the following ICD-10-CM diagnosis codes describing secondary scoliosis and secondary kyphosis to the list of principal diagnosis codes for MS-DRGs 456, 457, and 458: M40.10, M40.14, M40.15, M41.50, M41.54, M41.55, M41.56, and M41.57.
Comment: Commenters agreed with CMS' proposal to add ICD-10-CM diagnosis codes M40.10, M40.14, M40.15, M41.50, M41.54, M41.55, M41.56, and M41.57 that describe secondary scoliosis and secondary kyphosis to the list of principal diagnosis codes for assignment to MS-DRGs 456, 457 and 458 (Spinal Fusion except Cervical with Spinal Curvature of Malignancy or Infection or Extensive Fusions with MCC, with CC, and without CC/MCC, respectively). The commenters stated that the proposal was reasonable, given the ICD-10-CM diagnosis codes and the information provided.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-CM diagnosis codes M40.10, M40.14, M40.15, M41.50, M41.54, M41.55, M41.56, and M41.57 that describe secondary scoliosis and secondary kyphosis to the list of principal diagnosis codes for assignment to MS-DRGs 456, 457 and 458 in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
As also discussed in the proposed rule, during our review of MS-DRGs 456, 457, and 458, we found the following diagnosis codes that describe conditions involving the cervical region.

We stated that our clinical advisors noted that because the diagnosis codes shown in the table above describe conditions involving the cervical region, they are not clinically appropriate for assignment to MS-DRGs 456, 457, and 458, which are defined by non-cervical spinal fusion procedures (with spinal curvature or malignancy or infection or extensive fusions). Therefore, our clinical advisors recommended that these codes be removed from the MS-DRG logic for these MS-DRGs. As such, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to remove the diagnosis codes that describe conditions involving the cervical region as shown in the table above from MS-DRGs 456, 457, and 458.
Comment: Commenters agreed with the proposal to remove 34 diagnosis codes that describe conditions involving the cervical region from the list of principal diagnosis codes for MS-DRGs 456, 457, and 458, to improve clinical homogeneity and better reflect resource costs since these MS-DRGs are defined by non-cervical spinal fusion procedures. The commenters stated that the proposal was reasonable, given the ICD-10-CM diagnosis codes and the information provided.
Response: We appreciate the commenters' support. Therefore, we are finalizing our proposal to remove the ICD-10-CM diagnosis codes that describe conditions involving the cervical region as shown the table above from the list of principal diagnosis codes for MS-DRGs 456, 457, and 458 in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
7. MDC 11 (Diseases and Disorders of the Kidney and Urinary Tract): Extracorporeal Shock Wave Lithotripsy (ESWL)
As discussed in the FY 2020 IPPS/LTCH PPS (84 FR 19204 through 19210), we received two separate, but related requests to add ICD-10-CM diagnosis code N13.6 (Pyonephrosis) and ICD-10-CM diagnosis code T83.192A (Other mechanical complication of indwelling ureteral stent, initial encounter) to the list of principal diagnosis codes for MS-DRGs 691 and 692 (Urinary Stones with ESW Lithotripsy with CC/MCC and without CC/MCC, respectively) in MDC 11 so that cases are assigned more appropriately when an Extracorporeal Shock Wave Lithotripsy (ESWL) procedure is performed.
As noted in the proposed rule, ICD-10-CM diagnosis code N13.6 currently groups to MS-DRGs 689 and 690 (Kidney and Urinary Tract Infections with MCC and without MCC, respectively) and ICD-10-CM diagnosis code T83.192A currently groups to MS-DRGs 698, 699, and 700 (Other Kidney and Urinary Tract Diagnoses with MCC, with CC, and without CC/MCC, respectively).
As stated in the proposed rule, the ICD-10-PCS procedure codes for identifying procedures involving ESWL are designated as non-O.R. procedures and are shown in the following table.

Pyonephrosis can be described as an infection of the kidney with pus in the upper collecting system which can progress to obstruction. Patients with an obstruction in the upper urinary tract due to urinary stones (calculi), tumors, fungus balls or ureteropelvic obstruction (UPJ) may also have a higher risk of developing pyonephrosis. If pyonephrosis is not recognized and treated promptly, it can result in serious complications, including fistulas, septic shock, irreversible damage to the kidneys, and death.
As noted in the proposed rule and above, the requestor recommended that ICD-10-CM diagnosis codes N13.6 and T83.192A be added to the list of principal diagnosis codes for MS-DRGs 691 and 692. There are currently four MS-DRGs that group cases for diagnoses involving urinary stones, which are subdivided to identify cases with and without an ESWL procedure: MS-DRGs 691 and 692 (Urinary Stones with ESW Lithotripsy with and without CC/MCC, respectively) and MS-DRGs 693 and 694 (Urinary Stones without ESW Lithotripsy with and without MCC, respectively).
The requestor stated that when patients who have been diagnosed with hydronephrosis secondary to renal and ureteral calculus obstruction undergo an ESWL procedure, ICD-10-CM diagnosis code N13.2 (Hydronephrosis with renal and ureteral calculous obstruction) is reported and groups to MS-DRGs 691 and 692. However, if a patient with a diagnosis of hydronephrosis has a urinary tract infection (UTI) in addition to a renal calculus obstruction and undergoes an ESWL procedure, ICD-10-CM diagnosis code N13.6 must be coded and reported as the principal diagnosis, which groups to MS-DRGs 689 and 690. The requestor stated that ICD-10-CM diagnosis code N13.6 should be grouped to MS-DRGs 691 and 692 when reported as a principal diagnosis because this grouping will more appropriately reflect resource consumption for patients who undergo an ESWL procedure for obstructive urinary calculi, while also receiving treatment for urinary tract infections.
With regard to ICD-10-CM diagnosis code T83.192A, the requestor believed that when an ESWL procedure is performed for the treatment of calcifications within and around an indwelling ureteral stent, it is comparable to an ESWL procedure performed for the treatment of urinary calculi. Therefore, the requestor recommended adding ICD-10-CM diagnosis code T83.192A to MS-DRGs 691 and 692 when reported as a principal diagnosis and an ESWL procedure is also reported on the claim.
We stated in the proposed rule that, to analyze these separate, but related requests, we first reviewed the reporting of ICD-10-CM diagnosis code N13.6 within the ICD-10-CM classification. We noted that ICD-10-CM diagnosis code N13.6 is to be assigned for conditions identified in the code range N13.0-N13.5 with infection. (Codes in this range describe hydronephrosis with obstruction.) Infection may be documented by the patient's provider as urinary tract infection (UTI) or as specific as acute pyelonephritis. We agreed with the requestor that if a patient with a diagnosis of hydronephrosis has a urinary tract infection (UTI) in addition to a renal calculus obstruction and undergoes an ESWL procedure, ICD-10-CM diagnosis code N13.6 must be coded and reported as the principal diagnosis, which groups to MS-DRGs 689 and 690. In this case scenario, we stated that the ESWL procedure is designated as a non-O.R. procedure and does not impact the MS-DRG assignment when reported with ICD-10-CM diagnosis code N13.6.
The ICD-10-CM classification instructs that when both a urinary obstruction and a genitourinary infection co-exist, the correct code assignment for reporting is ICD-10-CM diagnosis code N13.6, which is appropriately grouped to MS-DRGs 689 and 690 (Kidney and Urinary Tract Infections with MCC and without MCC, respectively) because it describes a type of urinary tract infection. Therefore, in response to the requestor's suggestion that ICD-10-CM diagnosis code N13.6 be grouped to MS-DRGs 691 and 692 when reported as a principal diagnosis to more appropriately reflect resource consumption for patients who undergo an ESWL procedure for obstructive urinary calculi while also receiving treatment for urinary tract infections, we noted in the proposed rule that the ICD-10-CM classification provides instruction to identify the conditions reported with ICD-10-CM diagnosis code N13.6 as an infection, and not as urinary stones. We stated that our clinical advisors agreed with this classification and the corresponding MS-DRG assignment for diagnosis code N13.6. In addition, our clinical advisors noted that an ESWL procedure is a non-O.R. procedure and we stated that they do not believe that this procedure is a valid indicator of resource consumption for cases that involve an infection and obstruction. We stated that our clinical advisors believe that the resources used for a case that involves an infection and an obstruction are clinically distinct from the cases that involve an obstruction only in the course of treatment. Therefore, our clinical advisors did not agree with the request to add ICD-10-CM diagnosis code N13.6 to the list of principal diagnoses for MS-DRGs 691 and 692.
As also indicated in the proposed rule, we also performed various analyses of claims data to evaluate this request. We analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 689 and 690 to identify cases reporting ICD-10-CM diagnosis code N13.6 as the principal diagnosis with and without an ESWL procedure. Our findings are reflected in the table below.

For MS-DRG 689, we found a total of 68,020 cases with an average length of stay of 4.8 days and average costs of $7,873. Of those 68,020 cases, we found 1,024 cases reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a principal diagnosis with an average length of stay of 6.1 days and average costs of $13,809. Of those 1,024 cases reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a principal diagnosis, there were 6 cases that also reported an ESWL procedure with an average length of stay of 14.2 days and average costs of $45,489. For MS-DRG 690, we found a total of 131,999 cases with an average length of stay of 3.5 days and average costs of $5,692. Of those 131,999 cases, we found 4,625 cases reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a principal diagnosis with an average length of stay of 3.6 days and average costs of $5,483. Of those 4,625 cases reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a principal diagnosis, there were 24 cases that also reported an ESWL procedure with an average length of stay of 4.8 days and average costs of $14,837.
As we stated in the proposed rule, the data indicate that the 1,024 cases reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a principal diagnosis in MS-DRG 689 have a longer average length of stay (6.1 days versus 4.8 days) and higher average costs ($13,809 versus $7,873) compared to all the cases in MS-DRG 689. The data also indicate that the 6 cases reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a principal diagnosis that also reported an ESWL procedure have a longer average length of stay (14.2 days versus 4.8 days) and higher average costs ($45,489 versus $7,873) in comparison to all the cases in MS-DRG 689. We found similar results for cases reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a principal diagnosis with an ESWL procedure in MS-DRG 690, where the average length of stay was slightly longer (4.8 days versus 3.5 days) and the average costs were higher ($14,837 versus $5,692).
We then conducted further analysis for the six cases in MS-DRG 689 that reported a principal diagnosis of pyonephrosis with ESWL to determine what factors may be contributing to the longer lengths of stay and higher average costs. Specifically, we analyzed the MCC conditions that were reported across the six cases. Our findings are shown in the table below.

We found seven secondary diagnosis MCC conditions reported among the six cases in MS-DRG 689 that had a principal diagnosis of pyonephrosis with ESWL. We stated that these MCC conditions appear to have contributed to the longer lengths of stay and higher average costs for those six cases. As shown in the table above, the overall average length of stay for the cases reporting these conditions is 12.8 days with average costs of $39,069, which we stated in the proposed rule is consistent with the average length of stay of 14.2 days and average costs of $45,489 for the cases in MS-DRG 689 that had a principal diagnosis of pyonephrosis with ESWL.
We then analyzed the 24 cases in MS-DRG 690 that reported a principal diagnosis of pyonephrosis with ESWL to determine what factors may be contributing to the longer lengths of stay and higher average costs. Specifically, we analyzed the CC conditions that were reported across the 24 cases. Our findings are shown in the table below.


We found 37 secondary diagnosis CC conditions reported among the 24 cases in MS-DRG 690 that had a principal diagnosis of pyonephrosis with ESWL. We stated that these CC conditions appear to have contributed to the longer length of stay and higher average costs for those 24 cases. As shown in the table above, the overall average length of stay for the cases reporting these conditions is 6.6 days with average costs of $18,173, which we stated is higher, although comparable, to the average length of stay of 4.8 days and average costs of $14,837 for the cases in MS-DRG 690 that had a principal diagnosis of pyonephrosis with ESWL. We noted that it appears that 1 of the 24 cases had at least 4 secondary diagnosis CC conditions (F33.1, I48.1, I50.22, and J96.10) with an average length of stay of 12 days and average costs of $55,034, which we believed contributed greatly overall to the longer length of stay and higher average costs for those secondary diagnosis CC conditions reported among the 24 cases.
We stated that our clinical advisors agreed that the resource consumption for the 6 cases in MS-DRG 689 and the 24 cases in MS-DRG 690 that reported a principal diagnosis of pyonephrosis with ESWL cannot be directly attributed to ESWL and believe that it is the secondary diagnosis MCC and CC conditions that are the major contributing factors to the longer average length of stay and higher average costs for these cases.
As also indicated in the proposed rule, we also analyzed claims data for MS-DRGs 691 and 692 (Urinary Stones with ESW Lithotripsy with CC/MCC and without CC/MCC, respectively) and MS-DRGs 693 and 694 (Urinary Stones without ESW Lithotripsy with MCC and without MCC, respectively) to identify claims reporting pyonephrosis (ICD-10-CM diagnosis code N13.6) as a secondary diagnosis. Our findings are shown in the following table.

As shown in the table above, in MS-DRG 691, there was a total of 140 cases with an average length of stay of 3.9 days and average costs of $11,997. Of those 140 cases, there were 3 cases that reported pyonephrosis as a secondary diagnosis and an ESWL procedure with an average length of stay of 8.0 days and average costs of $24,280. There was a total of 124 cases found in MS-DRG 692 with an average length of stay of 2.1 days and average costs of $8,326. We stated in the proposed rule that there were no cases in MS-DRG 692 that reported pyonephrosis as a secondary diagnosis with an ESWL procedure. For MS-DRG 693, there was a total of 1,315 cases with an average length of stay of 5.1 days and average costs of $9,668. Of those 1,315 cases, there were 16 cases reporting pyonephrosis as a secondary diagnosis with an average length of stay of 5.5 days and average costs of $9,962. For MS-DRG 694, there was a total of 7,240 cases with an average length of stay of 2.7 days and average costs of $5,263. Of those 7,240 cases, there were 89 cases reporting pyonephrosis as a secondary diagnosis with an average length of stay of 3.5 days and average costs of $6,678.
Similar to the process described above, we then conducted further analysis for the three cases in MS-DRG 691 that reported a secondary diagnosis of pyonephrosis with ESWL to determine what factors may be contributing to the longer lengths of stay and higher average costs. Specifically, we analyzed what other MCC and CC conditions were reported across the three cases. We stated in the proposed rule that we found no other MCC conditions reported for those three cases. Our findings for the CC conditions reported for those three cases are shown in the table below.

We found six secondary diagnosis CC conditions reported among the three cases in MS-DRG 691 that had a secondary diagnosis of pyonephrosis with ESWL. We stated in the proposed rule that these CC conditions appear to have contributed to the longer lengths of stay and higher average costs for those three cases. As shown in the table above, the overall average length of stay for the cases reporting these conditions is 6.4 days with average costs of $20,181, which we stated is more consistent with the average length of stay of 8.0 days and average costs of $24,280 for the cases in MS-DRG 691 that had a secondary diagnosis of pyonephrosis with ESWL.
We stated in the proposed rule that our clinical advisors believe that the resource consumption for those three cases cannot be directly attributed to ESWL and that it is the secondary diagnosis CC conditions reported in addition to pyonephrosis, which is also designated as a CC condition, that are the major contributing factors for the longer average lengths of stay and higher average costs for these cases in MS-DRG 691.
As indicated in the proposed rule, we did not conduct further analysis for the 16 cases in MS-DRG 693 or the 89 cases in MS-DRG 694 that reported a secondary diagnosis of pyonephrosis because MS-DRGs 693 and 694 do not include ESWL procedures and the average length of stay and average costs for those cases were consistent with the data findings for all of the cases in their assigned MS-DRG.
As discussed earlier in this section and the proposed rule, the requestor suggested that ICD-10-CM diagnosis code N13.6 should be grouped to MS-DRGs 691 and 692 when reported as a principal diagnosis because this grouping will more appropriately reflect resource consumption for patients who undergo an ESWL procedure for obstructive urinary calculi, while also receiving treatment for urinary tract infections. However, as we stated in the proposed rule, based on the results of the data analysis and input from our clinical advisors, we believe that cases for which ICD-10-CM diagnosis code N13.6 was reported as a principal diagnosis or as a secondary diagnosis with an ESWL procedure should not be utilized as an indicator for increased utilization of resources based on the performance of an ESWL procedure. Rather, we stated that we believe that the resource consumption is more likely the result of secondary diagnosis CC and/or MCC diagnosis codes.
In the proposed rule, with respect to the requestor's concern that cases reporting ICD-10-CM diagnosis code T83.192A (Other mechanical complication of indwelling ureteral stent, initial encounter) and an ESWL procedure are not appropriately assigned and should be added to the list of principal diagnoses for MS-DRGs 691 and 692 (Urinary Stones with ESW Lithotripsy with CC/MCC and without CC/MCC, respectively), we stated that our clinical advisors note that ICD-10-CM diagnosis code T83.192A is not necessarily indicative of a patient having urinary stones. As such, they did not support adding ICD-10-CM diagnosis code T83.192A to the list of principal diagnosis codes for MS-DRGs 691 and 692.
As indicated in the proposed rule, we analyzed claims data to identify cases reporting ICD-10-CM diagnosis code T83.192A as a principal diagnosis with ESWL in MS-DRGs 698, 699, and 700 (Other Kidney and Urinary Tract Diagnoses with MCC, with CC, and without CC/MCC, respectively). Our findings are shown in the following table.
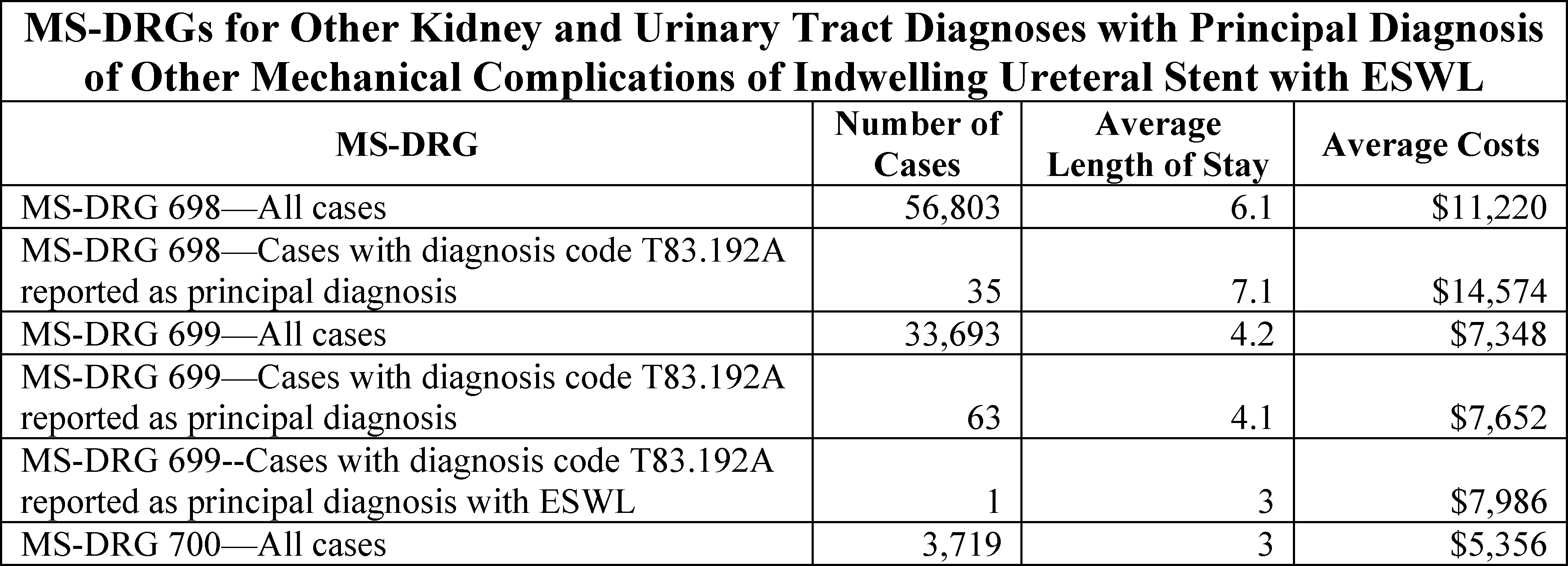
For MS-DRG 698, there was a total of 56,803 cases reported, with an average length of stay of 6.1 days and average costs of $11,220. Of these 56,803 cases, 35 cases reported ICD-10-CM diagnosis code T83.192A as the principal diagnosis, with an average length of stay of 7.1 days and average costs of $14,574. We stated that there were no cases that reported an ESWL procedure with ICD-10-CM diagnosis code T83.192A as the principal diagnosis in MS-DRG 698. For MS-DRG 699, there was a total of 33,693 cases reported, with an average length of stay of 4.2 days and average costs of $7,348. Of the 33,693 cases in MS-DRG 699, there were 63 cases that reported ICD-10-CM diagnosis code T83.192A as the principal diagnosis, with an average length of stay of 4.1 days and average costs of $7,652. We stated that there was only 1 case in MS-DRG 699 that reported ICD-10-CM diagnosis code T83.192A as the principal diagnosis with an ESWL procedure, with an average length of stay of 3 days and average costs of $7,986. For MS-DRG 700, there was a total of 3,719 cases reported, with an average length of stay of 3 days and average costs of $5,356. We stated that there were no cases that reported ICD-10-CM diagnosis code T83.192A as the principal diagnosis in MS-DRG 700. Of the 98 cases in MS-DRGs 698 and 699 that reported a principal diagnosis of other mechanical complication of indwelling ureteral stent (diagnosis code T83.192A), only 1 case also reported an ESWL procedure. Based on the results of our data analysis and input from our clinical advisors, we did not propose to add ICD-10-CM diagnosis code T83.192A to the list of principal diagnosis codes for MS-DRGs 691 and 692.
Comment: Commenters supported CMS' proposal to not add ICD-10-CM diagnosis codes N13.6 and T83.192A to the list of principal diagnosis codes for MS-DRGs 691 and 692. Commenters commended CMS for conducting the analysis and continuing to make further refinements to the MS-DRGs. The commenters stated that the proposal was reasonable, given the ICD-10-CM diagnosis codes and the information provided.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to not add ICD-10-CM diagnosis codes N13.6 and T83.192A to the list of principal diagnosis codes for MS-DRGs 691 and 692 in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule, in connection with these requests, our clinical advisors recommended that we evaluate the frequency with which ESWL is reported in the inpatient setting across all the MS-DRGs. Therefore, we also analyzed claims data from the September 2018 update of the FY 2018 MedPAR file to identify the other MS-DRGs to which claims reporting an ESWL procedure were reported. Our findings are shown in the following table.

As noted in the proposed rule, our findings with respect to the cases reporting an ESWL procedure in each of these MS-DRGs, as compared to all cases in the applicable MS-DRG, are shown in the table below.



We stated in the proposed rule that our data analysis indicates that, generally, the subset of cases reporting an ESWL procedure appear to have a longer average length of stay and higher average costs when compared to all the cases in their assigned MS-DRG. However, we noted in the proposed rule that this same subset of cases also reported at least one O.R. procedure and/or diagnosis designated as a CC or an MCC, which our clinical advisors believe are contributing factors to the longer average lengths of stay and higher average costs, with the exception of the case assigned to MS-DRG 700, which is a medical MS-DRG and has no CC or MCC conditions in the logic. Therefore, we stated that our clinical advisors do not believe that cases reporting an ESWL procedure should be considered as an indication of increased resource consumption for inpatient hospitalizations.
Our clinical advisors also suggested that we evaluate the reporting of ESWL procedures in the inpatient setting over the past few years. We analyzed claims data for MS-DRGs 691 and 692 from the FY 2012 through the FY 2016 MedPAR files, which were used in our analysis of claims data for MS-DRG reclassification requests effective for FY 2014 through FY 2018. We note that the analysis findings shown in the following table reflect ICD-9-CM, ICD-10-CM and ICD-10-PCS coded claims data.

As indicated in the proposed rule, the data show a steady decline in the number of cases reporting urinary stones with an ESWL procedure for the past 5 years. As previously noted, the total number of cases reporting urinary stones with an ESWL procedure for MS-DRGs 691 and 692 based on our analysis of the September 2018 update of the FY 2018 MedPAR file was 264, which again is a decline from the prior year's figures. As discussed throughout this section and in the proposed rule, an ESWL procedure is a non-O.R. procedure which currently groups to medical MS-DRGs 691 and 692. Therefore, we stated in the proposed rule that because an ESWL procedure is a non-O.R. procedure and due to decreased usage of this procedure in the inpatient setting for the treatment of urinary stones, our clinical advisors believe that there is no longer a clinical reason to subdivide the MS-DRGs for urinary stones (MS-DRGs 691, 692, 693, and 694) based on ESWL procedures.
Therefore, we proposed to delete MS-DRGs 691 and 692 and to revise the titles for MS-DRGs 693 and 694 from “Urinary Stones without ESW Lithotripsy with MCC” and “Urinary Stones without ESW Lithotripsy without MCC”, respectively to “Urinary Stones with MCC” and “Urinary Stones without MCC”, respectively.
Comment: Commenters supported the proposal to delete MS-DRGs 691 and 692 and to revise the titles for MS-DRGs 693 and 694 from “Urinary Stones without ESW Lithotripsy with MCC” and “Urinary Stones without ESW Lithotripsy without MCC”, respectively to “Urinary Stones with MCC” and “Urinary Stones without MCC”. Commenters agreed that deleting MS-DRGs 691 and 692 and revising the titles for MS-DRGs 693 and 694 will better reflect utilization of resources for cases reporting urinary stones with a EWSL procedure as well as provide for appropriate payment for the procedures. The commenters noted that the proposal was reasonable, given the data, the ICD-10-PCS procedure codes, and information provided.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to delete MS-DRGs 691 and 692 and to revise the titles for MS-DRGs 693 and 694 from “Urinary Stones without ESW Lithotripsy with MCC” and “Urinary Stones without ESW Lithotripsy without MCC”, respectively to “Urinary Stones with MCC” and “Urinary Stones without MCC”, in the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
8. MDC 12 (Diseases and Disorders of the Male Reproductive System): Diagnostic Imaging of Male Anatomy
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19210 through 10211), we received a request to review four ICD-10-CM diagnosis codes describing body parts associated with male anatomy that are currently assigned to MDC 5 (Diseases and Disorders of the Circulatory System) in MS-DRGs 302 and 303 (Atherosclerosis with MCC and Atherosclerosis without MCC, respectively). The four codes are listed in the following table.

The requestor recommended that the four diagnosis codes shown in this table be considered for assignment to MDC 12 (Diseases and Disorders of the Male Reproductive System), consistent with other diagnosis codes that include the male anatomy. However, the requestor did not suggest a specific MS-DRG assignment within MDC 12.
As indicated in the proposed rule, we examined claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 302 and 303 to identify any cases reporting a diagnosis code for abnormal radiologic findings on diagnostic imaging of the testicles. We did not find any such cases.
We stated in the proposed rule that our clinical advisors reviewed this request and determined that the assignment of diagnosis codes R93.811, R93.812, R93.813, and R93.819 to MDC 5 in MS-DRGs 302 and 303 was a result of replication from ICD-9-CM diagnosis code 793.2 (Nonspecific (abnormal) findings on radiological and other examination of other intrathoracic organs) which was assigned to those MS-DRGs. Therefore, we stated that our clinical advisors supported reassignment of these codes to MDC 12. Our clinical advisors agreed that this reassignment is clinically appropriate because these diagnosis codes are specific to the male anatomy, consistent with other diagnosis codes in MDC 12 that include the male anatomy. Specifically, we stated in the proposed rule that our clinical advisors suggested reassignment of the four diagnosis codes to MS-DRGs 729 and 730 (Other Male Reproductive System Diagnoses with CC/MCC and without CC/MCC, respectively). Therefore, we proposed to reassign ICD-10-CM diagnosis codes R93.811, R93.812, R93.813, and R93.819 from MDC 5 in MS-DRGs 302 and 303 to MDC 12 in MS-DRGs 729 and 730.
Comment: Commenters supported our proposed reassignment of ICD-10-CM diagnosis codes R93.811, R93.812, R93.813, and R93.819 from MDC 5 to MDC 12.
Response: We thank the commenters for their support. After consideration of the public comments we received, we are finalizing our proposal to reassign ICD-10-CM diagnosis codes R93.811, R93.812, R93.813, and R93.819 from MDC 5 in MS-DRGs 302 and 303 to MDC 12 in MS-DRGs 729 and 730.
9. MDC 14 (Pregnancy, Childbirth and the Puerperium): Reassignment of Diagnosis Code O99.89
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19211 through 19214), we received a request to review the MS-DRG assignment for cases reporting ICD-10-CM diagnosis code O99.89 (Other specified diseases and conditions complicating pregnancy, childbirth and the puerperium). The requestor stated that it is experiencing MS-DRG shifts to MS-DRG 769 (Postpartum and Post Abortion Diagnoses with O.R. Procedure) as a result of the new obstetric MS-DRG logic when ICD-10-CM diagnosis code O99.89 is reported as a principal diagnosis in the absence of a delivery code on the claim (to indicate the patient delivered during that hospitalization), or when there is no other secondary diagnosis code on the claim indicating that the patient is in the postpartum period. As we stated in the proposed rule, according to the requestor, claims reporting ICD-10-CM diagnosis code O99.89 as a principal diagnosis for conditions described as occurring during the antepartum period that are reported with an O.R. procedure are grouping to MS-DRG 769. In the example provided by the requestor, ICD-10-CM diagnosis code O99.89 was reported as the principal diagnosis, with ICD-10-CM diagnosis codes N13.2 (Hydronephrosis with renal and ureteral calculous obstruction) and Z3A.25 (25 weeks of gestation of pregnancy) reported as secondary diagnoses with ICD-10-PCS procedure code 0T68DZ (Dilation of right ureter with intraluminal device, endoscopic approach), resulting in assignment to MS-DRG 769. The requestor noted that, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41212), we stated “If there was not a principal diagnosis of abortion reported on the claim, the logic asks if there was a principal diagnosis of an antepartum condition reported on the claim. If yes, the logic then asks if there was an O.R. procedure reported on the claim. If yes, the logic assigns the case to one of the proposed new MS-DRGs 817, 818, or 819.” In the requestor's example, there were not any codes reported to indicate that the patient was in the postpartum period, nor was there a delivery code reported on the claim. Therefore, the requestor suggested that a more appropriate assignment for ICD-10-CM diagnosis code O99.89 may be MS-DRGs 817, 818, and 819 (Other Antepartum Diagnoses with O.R. Procedure with MCC, with CC and without CC/MCC, respectively).
As noted in the proposed rule, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41202 through 41216), we finalized our proposal to restructure the MS-DRGs within MDC 14 (Pregnancy, Childbirth and the Puerperium) which established new concepts for the GROUPER logic. We stated that, as a result of the modifications made, ICD-10-CM diagnosis code O99.89 was classified as a postpartum condition and is currently assigned to MS-DRG 769 (Postpartum and Post Abortion Diagnoses with O.R. Procedure) and MS-DRG 776 (Postpartum and Post Abortion Diagnoses without O.R. Procedure) under the Version 36 ICD-10 MS-DRGs. As also discussed and displayed in Diagram 2 in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41212 through 41213), we explained in the proposed rule that the logic asks if there was a principal diagnosis of a postpartum condition reported on the claim. If yes, the logic then asks if there was an O.R. procedure reported on the claim. If yes, the logic assigns the case to MS-DRG 769. If no, the logic assigns the case to MS-DRG 776. Therefore, we stated in the proposed rule that the MS-DRG assignment for the example provided by the requestor is grouping accurately according to the current GROUPER logic.
As indicated in the proposed rule, we analyzed claims data from the September 2018 update of the FY 2018 MedPAR file for cases reporting diagnosis code O99.89 in MS-DRGs 769 and 776 as a principal diagnosis or as a secondary diagnosis. Our findings are shown in the following table.
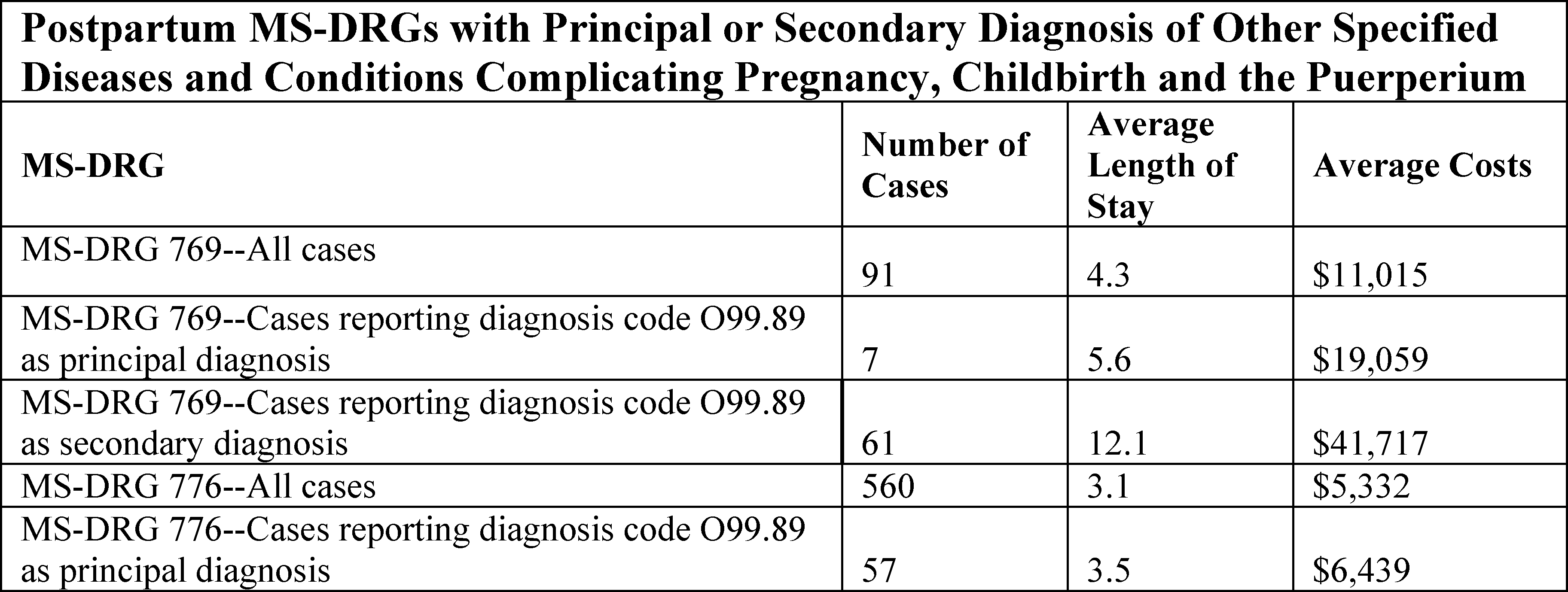
As shown in the table above, we found a total of 91 cases in MS-DRG 769 with an average length of stay of 4.3 days and average costs of $11,015. Of these 91 cases, 7 cases reported ICD-10-CM diagnosis code O99.89 as a principal diagnosis with an average length of stay of 5.6 days and average costs of $19,059, and 61 cases reported ICD-10-CM diagnosis code O99.89 as a secondary diagnosis with an average length of stay of 12.1 days and average costs of $41,717. For MS-DRG 776, we found a total of 560 cases with an average length of stay of 3.1 days and average costs of $5,332. Of these 560 cases, 57 cases reported ICD-10-CM diagnosis code O99.89 as a principal diagnosis with an average length of stay of 3.5 days and average costs of $6,439. We stated in the proposed rule that there were no cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis in MS-DRG 776.
For MS-DRG 769, the data show that the 68 cases reporting ICD-10-CM diagnosis code O99.89 as a principal or secondary diagnosis have a longer average length of stay and higher average costs compared to all the cases in MS-DRG 769. For MS-DRG 776, the data show that the 57 cases reporting a principal diagnosis of ICD-10-CM diagnosis code O99.89 have a similar average length of stay compared to all the cases in MS-DRG 776 (3.5 days versus 3.1 days) and average costs that are consistent with the average costs of all cases in MS-DRG 776 ($6,439 versus $5,332).
We noted in the proposed rule that the description for ICD-10-CM diagnosis code O99.89 “Other specified diseases and conditions complicating pregnancy, childbirth and the puerperium”, describes conditions that may occur during the antepartum period (pregnancy), during childbirth, or during the postpartum period (puerperium). In addition, in the ICD-10-CM Tabular List of Diseases, there is an inclusion term at subcategory O99.8- instructing users that the reporting of any diagnosis codes in that subcategory is intended for conditions that are reported in certain ranges of the classification. Specifically, the inclusion term states “Conditions in D00-D48, H00-H95, M00-N99, and Q00-Q99.” There is also an instructional note to “Use additional code to identify condition.” As a result, we stated that ICD-10-CM diagnosis code O99.89 may be reported to identify conditions that occur during the antepartum period (pregnancy), during childbirth, or during the postpartum period (puerperium). However, it is not restricted to the reporting of obstetric specific conditions only. In the example provided by the requestor, ICD-10-CM diagnosis code O99.89 was reported as the principal diagnosis with ICD-10-CM diagnosis code N13.2 (Hydronephrosis with renal and ureteral calculous obstruction) as a secondary diagnosis. In the proposed rule, we stated that ICD-10-CM diagnosis code N13.2 is within the code range referenced earlier in this section (M00-N99) and qualifies as an appropriate condition for reporting according to the instruction.
As noted in the proposed rule and earlier, ICD-10-CM diagnosis code O99.89 is intended to report conditions that occur during the antepartum period (pregnancy), during childbirth, or during the postpartum period (puerperium) and is not restricted to the reporting of obstetric specific conditions only. However, because the diagnosis code description includes three distinct obstetric related stages, we stated in the proposed rule that it is not clear what stage the patient is in by this single code. For example, upon review of subcategory O99.8-, we recognized that the other ICD-10-CM diagnosis code sub-subcategories are expanded to include unique codes that identify the condition as occurring or complicating pregnancy, childbirth or the puerperium. Specifically, sub-subcategory O99.81- (Abnormal glucose complicating pregnancy, childbirth, and the puerperium) is expanded to include the following ICD-10-CM diagnosis codes.

These codes specifically identify at what stage the abnormal glucose was a complicating condition. We stated in the proposed rule that, because each code uniquely identifies a stage, the code can be easily classified under MDC 14 as an antepartum condition (ICD-10-CM diagnosis code O99.810), occurring during a delivery episode (ICD-10-CM diagnosis code O99.814), or as a postpartum condition (ICD-10-CM diagnosis code O99.815). The same is not true for ICD-10-CM diagnosis code O99.89 because it includes all three stages in the single code.
Therefore, we examined the number and type of secondary diagnoses reported with ICD-10-CM diagnosis code O99.89 as a principal diagnosis for MS-DRGs 769 and 776 to identify how many secondary diagnoses were related to other obstetric conditions and how many were related to non-obstetric conditions.

As shown in the table above, there was a total of 59 secondary diagnoses reported with diagnosis code O99.89 as the principal diagnosis for MS-DRG 769. Of those 59 secondary diagnoses, 13 were obstetric (OB) related diagnosis codes (11 antepartum, 1 postpartum and 1 delivery) and 46 were non-obstetric (Non-OB) related diagnosis codes. For MS-DRG 776, there was a total of 376 secondary diagnoses reported with diagnosis code O99.89 as the principal diagnosis. Of those 376 secondary diagnoses, 113 were obstetric (OB) related diagnosis codes (88 antepartum, 19 postpartum and 6 delivery) and 263 were non-obstetric (Non-OB) related diagnosis codes.
The data reflect that, for MS-DRGs 769 and 776, the number of secondary diagnoses identified as OB-related antepartum diagnoses is greater than the number of secondary diagnoses identified as OB-related postpartum diagnoses (99 antepartum diagnoses versus 20 postpartum diagnoses). The data also indicate that, of the 435 secondary diagnoses reported with ICD-10-CM diagnosis code O99.89 as the principal diagnosis, 309 (71 percent) of those secondary diagnoses were non-OB-related diagnosis codes. Because there was a greater number of secondary diagnoses identified as OB-related antepartum diagnoses compared to the OB-related postpartum diagnoses within the postpartum MS-DRGs when ICD-10-CM diagnosis code O99.89 was reported as the principal diagnosis, we performed further analysis of diagnosis code O99.89 within the antepartum MS-DRGs.
Under the Version 35 ICD-10 MS-DRGs, diagnosis code O99.89 was classified as an antepartum condition and was assigned to MS-DRG 781 (Other Antepartum Diagnoses with Medical Complications). Therefore, we also analyzed claims data for MS-DRGs 817, 818 and 819 (Other Antepartum Diagnoses with O.R. Procedure with MCC, with CC and without CC/MCC, respectively) and MS-DRGs 831, 832, and 833 (Other Antepartum Diagnoses without O.R. Procedure with MCC, with CC and without CC/MCC, respectively) for cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis. We noted in the proposed rule that the analysis for the proposed FY 2020 ICD-10 MS-DRGs is based upon the September 2018 update of the FY 2018 MedPAR claims data that were grouped through the ICD-10 MS-DRG GROUPER Version 36. Our findings are shown in this table.
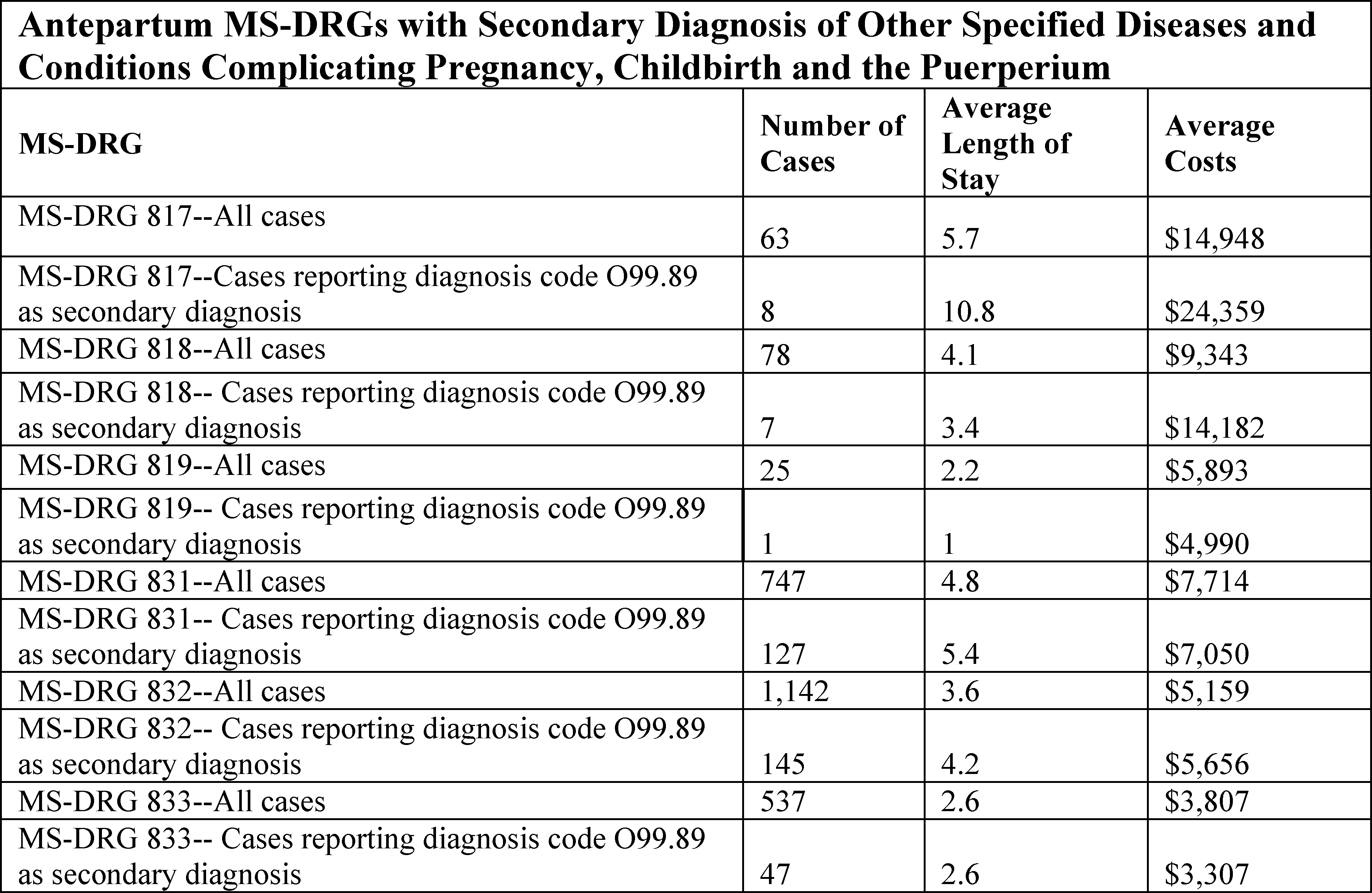
As shown in the table above, we found a total of 63 cases in MS-DRG 817 with an average length of stay of 5.7 days and average costs of $14,948. Of these 63 cases, there were 8 cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis with an average length of stay of 10.8 days and average costs of $24,359. For MS-DRG 818, we found a total of 78 cases with an average length of stay of 4.1 days and average costs of $9,343. Of these 78 cases, there were 7 cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis with an average length of stay of 3.4 days and average costs of $14,182. For MS-DRG 819, we found a total of 25 cases with an average length of stay of 2.2 days and average costs of $5,893. Of these 25 cases, there was 1 case reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis with an average length of stay of 1 day and average costs of $4,990.
For MS-DRG 831, we found a total of 747 cases with an average length of stay of 4.8 days and average costs of $7,714. Of these 747 cases, there were 127 cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis with an average length of stay of 5.4 days and average costs of $7,050. For MS-DRG 832, we found a total of 1,142 cases with an average length of stay of 3.6 days and average costs of $5,159. Of these 1,142 cases, there were 145 cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis with an average length of stay of 4.2 days and average costs of $5,656. For MS-DRG 833, we found a total of 537 cases with an average length of stay of 2.6 days and average costs of $3,807. Of these 537 cases, there were 47 cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis with an average length of stay of 2.6 days and average costs of $3,307.
As we stated in the proposed rule, overall, there was a total of 335 cases reporting ICD-10-CM diagnosis code O99.89 as a secondary diagnosis within the antepartum MS-DRGs. Of those 335 cases, 16 cases involved an O.R. procedure and 319 cases did not involve an O.R. procedure. The data indicate that ICD-10-CM diagnosis code O99.89 is reported more often as a secondary diagnosis within the antepartum MS-DRGs (335 cases) than it is reported as a principal or secondary diagnosis within the postpartum MS-DRGs (125 cases).
Further, we stated that our clinical advisors believe that, because ICD-10-CM diagnosis code O99.89 can be reported during the antepartum period (pregnancy), during childbirth, or during the postpartum period (puerperium), there is not a clear clinical indication as to which set of MS-DRGs (antepartum, delivery, or postpartum) would be the most appropriate assignment for this diagnosis code. They recommended that we collaborate with the National Center for Health Statistics (NCHS) at the Centers for Disease Control and Prevention (CDC), in consideration of a proposal to possibly expand ICD-10-CM diagnosis code O99.89 to become a sub-subcategory that would result in the creation of unique codes with a sixth digit character to specify which obstetric related stage the patient is in. For example, under subcategory O99.8-, a proposed new sub-subcategory for ICD-10-CM diagnosis code O99.89- could include the following proposed new diagnosis codes:
- O99.890 (Other specified diseases and conditions complicating pregnancy);
- O99.894 (Other specified diseases and conditions complicating childbirth); and
- O99.895 (Other specified diseases and conditions complicating the puerperium).
We noted in the proposed rule that, if such a proposal to create this new sub-subcategory and new diagnosis codes were approved and finalized, it would enable improved data collection and more appropriate MS-DRG assignment, consistent with the current MS-DRG assignments of the existing obstetric related diagnosis codes. We stated, for instance, a new diagnosis code described as “complicating pregnancy” would be clinically aligned with the antepartum MS-DRGs, a new diagnosis code described as “complicating childbirth” would be clinically aligned with the delivery MS-DRGs, and a new diagnosis code described as “complicating the puerperium” would be clinically aligned with the postpartum MS-DRGs. (We note that all requests for new diagnosis codes require that a proposal be approved for discussion at a future ICD-10 Coordination and Maintenance Committee meeting.)
We stated in the proposed rule that, while our clinical advisors could not provide a strong clinical justification for classifying ICD-10-CM diagnosis code O99.89 as an antepartum condition versus as a postpartum condition for the reasons described above, they did consider the claims data to be informative as to how the diagnosis code is being reported for obstetric patients. In analyzing both the postpartum MS-DRGs and the antepartum MS-DRGs discussed earlier in this section, they agreed that the data clearly show that ICD-10-CM diagnosis code O99.89 is reported more frequently as a secondary diagnosis within the antepartum MS-DRGs than it is reported as a principal or secondary diagnosis within the postpartum MS-DRGs.
Based on our analysis of claims data and input from our clinical advisors, we proposed to reclassify ICD-10-CM diagnosis code O99.89 from a postpartum condition to an antepartum condition under MDC 14. We stated in the proposed rule that, if finalized, ICD-10-CM diagnosis code O99.89 would follow the logic as described in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41212) which asks if there was a principal diagnosis of an antepartum condition reported on the claim. If yes, the logic then asks if there was an O.R. procedure reported on the claim. If yes, the logic assigns the case to MS-DRG 817, 818, or 819. If no (there was not an O.R. procedure reported on the claim), the logic assigns the case to MS-DRG 831, 832, or 833.
Comment: Commenters supported the proposal to reclassify ICD-10-CM diagnosis code O99.89 from a postpartum condition to an antepartum condition under MDC 14. Commenters also agreed with the recommendation to expand diagnosis code O99.89 to create a new sub-subcategory that would result in the creation of unique codes with a sixth digit character to specify which obstetric related stage the patient is in.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to reclassify ICD-10-CM diagnosis code O99.89 from a postpartum condition to an antepartum condition. For FY 2020, cases reporting diagnosis code O99.89 will follow the logic as previously described in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41212) which asks if there was a principal diagnosis of an antepartum condition reported on the claim. If yes, the logic then asks if there was an O.R. procedure reported on the claim. If yes, the logic assigns the case to MS-DRG 817, 818, or 819 (Other Antepartum Diagnoses with O.R. Procedure with MCC, with CC and without CC/MCC, respectively). If no (there was not an O.R. procedure reported on the claim), the logic assigns the case to MS-DRG 831, 832, or 833 (Other Antepartum Diagnoses without O.R. Procedure with MCC, with CC and without CC/MCC, respectively).
10. MDC 22 (Burns): Skin Graft to Perineum for Burn
As discussed in the FY 2020 IPPS/LTCH PPS (84 FR 19214 through 19215), we received a request to add seven ICD-10-PCS procedure codes that describe a skin graft to the perineum to MS-DRG 927 (Extensive Burns Or Full Thickness Burns with MV >96 Hours with Skin Graft) and MS-DRGs 928 and 929 (Full Thickness Burn with Skin Graft Or Inhalation Injury with CC/MCC and without CC/MCC, respectively) in MDC 22. The seven procedure codes are listed in the following table.
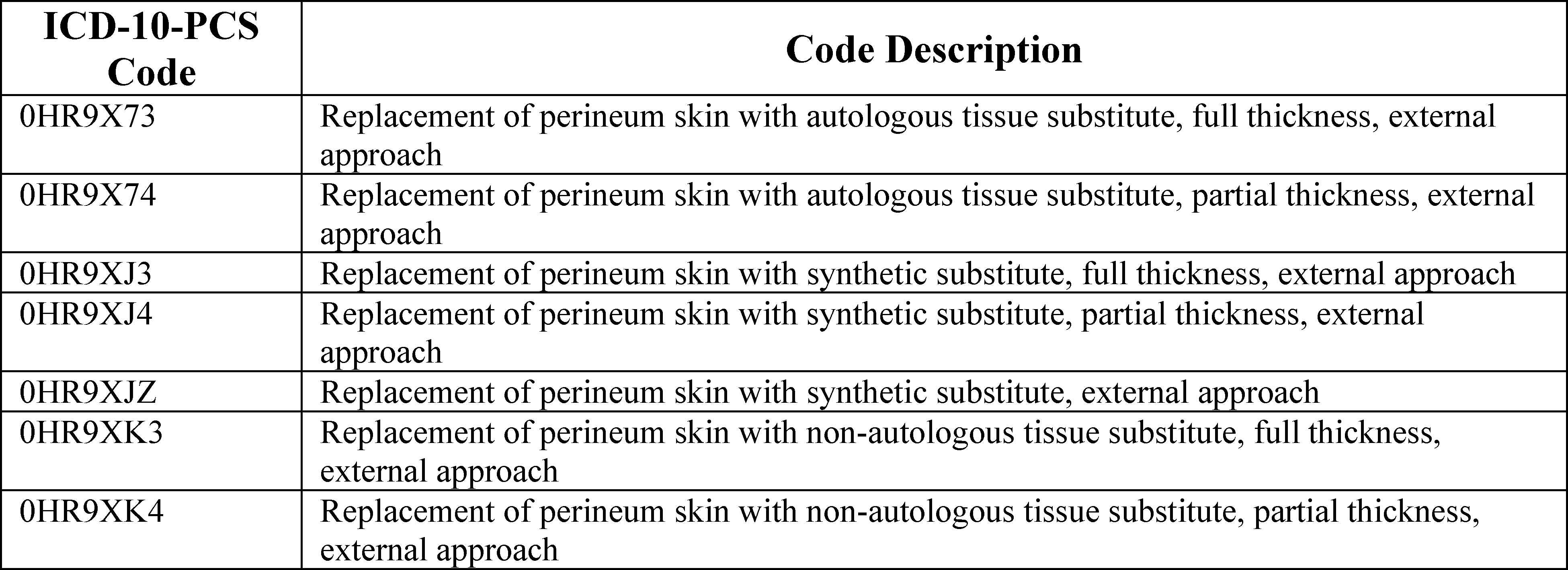
As indicated in the proposed rule, these seven procedure codes are currently assigned to MS-DRGs 746 and 747 (Vagina, Cervix and Vulva Procedures with CC/MCC and without CC/MCC, respectively). In addition, we stated in the proposed rule that when reported in conjunction with a principal diagnosis in MDC 21 (Injuries, Poisonings and Toxic Effects of Drugs), these codes group to MS-DRGs 907, 908, and 909 (Other O.R. Procedures For Injuries with MCC, with CC and without CC/MCC, respectively), and when reported in conjunction with a principal diagnosis in MDC 24 (Multiple Significant Trauma), these codes group to MS-DRGs 957, 958, and 959 (Other O.R. Procedures For Multiple Significant Trauma with MCC, with CC and without CC/MCC, respectively). In addition, we stated that these procedures are designated as non-extensive O.R. procedures and are assigned to MS-DRGs 987, 988 and 989 (Non-Extensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC, and without CC/MCC, respectively) when a principal diagnosis that is unrelated to the procedure is reported on the claim.
The requestor provided an example in which it identified one case where a patient underwent debridement and split thickness skin graft (STSG) to the perineum area (only), and expressed concern that the case did not route to MS-DRGs 928 and 929 to recognize operating room resources. (We note that the requestor did not specify the diagnosis associated with this case nor the MS-DRG to which this one case was grouped.) The requestor stated that providers may document various terminologies for this anatomic site, including perineum, groin, and buttocks crease; therefore, when a provider deems a burn to affect the perineum as opposed to the groin or buttock crease, cases should route to MS-DRGs which compensate hospitals for skin grafting operating room resources. Therefore, the requestor recommended that the cited seven ICD-10-PCS codes be added to the list of procedure codes for a skin graft within MS-DRGs 927, 928, and 929.
As noted in the proposed rule, we reviewed this request by analyzing claims data from the September 2018 update of the FY 2018 MedPAR file for cases reporting any of the above seven procedure codes in MS-DRGs 746, 747, 907, 908, 909, 957, 958, 959, 987, 988, and 989. Our findings are shown in the following table.

As shown in the table above, the overall volume of cases reporting a skin graft to the perineum procedure is low, with a total of 6 cases found. In MS-DRG 746, we found a total of 1,344 cases with an average length of stay of 5 days and average costs of $11,847. The single case reporting a skin graft to the perineum procedure in MS-DRG 746 had a length of stay of 2 days and a cost of $10,830. In MS-DRG 907, we found a total of 7,843 cases with an average length of stay of 10 days and average costs of $28,919. The single case reporting a skin graft to the perineum procedure in MS-DRG 907 had a length of stay of 8 days and a cost of $21,909. In MS-DRG 908, we found a total of 9,286 cases with an average length of stay of 5.3 days and average costs of $14,601. The single case reporting a skin graft to the perineum procedure in MS-DRG 908 had a length of stay of 6 days and a cost of $8,410. In MS-DRG 988, we found a total of 8,391 cases with an average length of stay of 5.7 days and average costs of $12,294. The 2 cases reporting a skin graft to the perineum procedure in MS-DRG 988 had an average length of stay of 3 days and average costs of $6,906. In MS-DRG 989, we found a total of 1,551 cases with an average length of stay of 3.1 days and average costs of $8,171. The single case reporting a skin graft to the perineum procedure in MS-DRG 989 had a length of stay of 7 day and a cost of $14,080. We stated that we found no cases reporting a skin graft to the perineum procedure in MS-DRG 747, 909, 957, 958, 959, or 987. Further, we stated that cases reporting a skin graft to the perineum procedure generally had shorter length of stays and lower average costs than those of their assigned MS-DRGs overall.
We then analyzed claims data for MS-DRGs 927, 928, and 929 (the MS-DRGs to which the requestor suggested that these cases group) for all cases reporting a procedure describing a skin graft to the perineum listed in the table above to consider how the resources involved in the cases reporting a procedure describing a skin graft to the perineum compared to those of all cases in MS-DRGs 927, 928, and 929. Our findings are shown in the following table.

As shown in the table above, for MS-DRG 927, we found a total of 146 cases with an average length of stay of 30.9 days and average costs of $147,903; no cases reporting a skin graft to the perineum procedure were found. For MS-DRG 928, we found a total of 1,149 cases with an average length of stay of 15.7 days and average costs of $45,523. We found 5 cases reporting a skin graft to the perineum procedure with an average length of stay of 39 days and average costs of $64,041. For MS-DRG 929, we found a total of 296 cases with an average length of stay of 7.9 days and average costs of $21,474; and no cases reporting a skin graft to the perineum procedure were found. We noted in the proposed rule that none of the 5 cases reporting a skin graft to the perineum in MS-DRGs 927, 928, and 929 reported a skin graft to the perineum procedure as the only operating room procedure. Therefore, we stated in the proposed rule that it is not possible to determine how much of the operating room resources for these 5 cases were attributable to the skin graft to the perineum procedure.
We further stated that our clinical advisors reviewed the claims data described above and noted that none of the cases reporting the seven identified procedure codes that grouped to MS-DRGs 746, 907, 908, 988, and 989 (listed in the table above) had a principal or secondary diagnosis of a burn, which suggests that these skin grafts were not performed to treat a burn. We stated that therefore, our clinical advisors believe that it would not be appropriate for these cases that report a skin graft to the perineum procedure to group to MS-DRGs 927, 928, and 929, which describe burns. Our clinical advisors state that the seven ICD-10-PCS procedure codes that describe a skin graft to the perineum are more clinically aligned with the other procedures in MS-DRGs 746 and 747, to which they are currently assigned. Therefore, we did not propose to add the seven identified procedure codes to MS-DRGs 927, 928, and 929 in the proposed rule.
Comment: Commenters did not support the proposal to not add ICD-10-PCS procedure codes 0HR9X73, 0HR9X74, 0HR9XJ3, 0HR9XJ4, 0HR9XJZ, 0HR9XK3, and 0HR9XK4 that describe a skin graft to the perineum to MS-DRGs 927, 928 and 929. The commenters noted that in the hypothetical scenario in which the principal diagnoses code T21.37XA, third degree burn of (female) perineum, or T21.36XA, third degree burn of the (male) perineum, is coded as the principal diagnosis in combination with ICD-10-PCS codes describing skin graft to the perineum, the case would group to MS-DRG 934 (Full Thickness Burn without Skin Graft or Inhalation Injury). A commenter stated that since CMS' DRG tables are referenced nationally by other payers, the GROUPER logic should change in spite of the fact that CMS's data reflects little or no volume for these cases.
Response: We appreciate the commenters' feedback.
In response to public comments, our clinical advisors reviewed the claims data in the September 2018 update of the FY 2018 MedPAR file and again noted that none of the cases reporting the seven identified procedure codes that grouped to MS-DRGs 746, 907, 908, 988, and 989 had a principal or secondary diagnosis of a burn. Therefore, our clinical advisors continue to believe that it would not be appropriate for these cases that report a skin graft to the perineum procedure to group to MS-DRGs 927, 928, and 929, which describe burns, in the absence of MedPAR data indicating that these skin grafts are performed to treat burns. Our clinical advisors believe that the seven ICD-10-PCS procedure codes that describe a skin graft to the perineum are more clinically aligned with the other procedures in MS-DRGs 746 and 747, to which they are currently assigned. As additional claims data becomes available, we can determine if future modifications to the assignment of these procedure codes are warranted at a later date.
Therefore, after consideration of the public comments we received, we are finalizing our proposal to maintain the current structure of MS-DRGs 927, 928 and 929 for FY 2020.
11. MDC 23 (Factors Influencing Health Status and Other Contacts With Health Services): Assignment of Diagnosis Code R93.89
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19216), we received a request to consider reassignment of ICD-10-CM diagnosis code R93.89 (Abnormal finding on diagnostic imaging of other specified body structures) from MDC 5 (Diseases and Disorders of the Circulatory System) in MS-DRGs 302 and 303 (Atherosclerosis with and without MCC and Atherosclerosis without MCC, respectively) to MDC 23 (Factors Influencing Health Status and Other Contact with Health Services), consistent with other diagnosis codes that include abnormal findings. However, the requestor did not suggest a specific MS-DRG assignment within MDC 23.
As indicated in the proposed rule, we examined claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 302 and 303 and identified cases reporting diagnosis code R93.89. Our findings are shown in the following table.

As shown in the table, for MS-DRG 302, there was a total of 3,750 cases with an average length of stay of 3.8 days and average costs of $7,956. Of these 3,750 cases, there were 3 cases reporting abnormal finding on diagnostic imaging of other specified body structures, with an average length of stay 7.7 days and average costs of $10,818. For MS-DRG 303, there was a total of 12,986 cases with an average length of stay of 2.3 days and average costs of $4,920. Of these 12,986 cases, there were 10 cases reporting abnormal finding on diagnostic imaging of other specified body structures, with an average length of stay 2 days and average costs of $3,416.
We stated in the proposed rule that our clinical advisors reviewed this request and determined that the assignment of diagnosis code R93.89 to MDC 5 in MS-DRGs 302 and 303 was a result of replication from ICD-9-CM diagnosis code 793.2 (Nonspecific (abnormal) findings on radiological and other examination of other intrathoracic organs), which was assigned to those MS-DRGs. Therefore, they supported reassignment of diagnosis code R93.89 to MDC 23. Our clinical advisors agree this reassignment is clinically appropriate as it is consistent with other diagnosis codes in MDC 23 that include abnormal findings from other nonspecified sites. Specifically, we stated in the proposed rule that our clinical advisors suggested reassignment of diagnosis code R89.93 to MS-DRGs 947 and 948 (Signs and Symptoms with and without MCC, respectively). Therefore, we proposed to reassign ICD-10-CM diagnosis code R93.89 from MDC 5 in MS-DRGs 302 and 303 to MDC 23 in MS-DRGs 947 and 948.
Comment: Commenters supported our proposed reassignment of ICD-10-CM diagnosis code R93.89 from MDC 5 to MDC 23.
Response: We thank the commenters for their support. After consideration of the public comments we received, we are finalizing our proposal to reassign ICD-10-CM diagnosis code R93.89 from MDC 5 in MS-DRGs 302 and 303 to MDC 23 in MS-DRGs 947 and 948.
12. Review of Procedure Codes in MS-DRGs 981 Through 983 and 987 Through 989
a. Adding Procedure Codes and Diagnosis Codes Currently Grouping to MS-DRGs 981 Through 983 or MS-DRGs 987 Through 989 Into MDCs
We annually conduct a review of procedures producing assignment to MS-DRGs 981 through 983 (Extensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC, and without CC/MCC, respectively) or MS-DRGs 987 through 989 (Nonextensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC, and without CC/MCC, respectively) on the basis of volume, by procedure, to see if it would be appropriate to move cases reporting these procedure codes out of these MS-DRGs into one of the surgical MS-DRGs for the MDC into which the principal diagnosis falls. The data are arrayed in two ways for comparison purposes. We look at a frequency count of each major operative procedure code. We also compare procedures across MDCs by volume of procedure codes within each MDC. We use this information to determine which procedure codes and diagnosis codes to examine.
We identify those procedures occurring in conjunction with certain principal diagnoses with sufficient frequency to justify adding them to one of the surgical MS-DRGs for the MDC in which the diagnosis falls. We also consider whether it would be more appropriate to move the principal diagnosis codes into the MDC to which the procedure is currently assigned. Based on the results of our review of the claims data from the September 2018 update of the FY 2018 MedPAR file, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19216 through 19224), we proposed to move the cases reporting the procedures and/or principal diagnosis codes described below from MS-DRGs 981 through 983 or MS-DRGs 987 through 989 into one of the surgical MS-DRGs for the MDC into which the principal diagnosis or procedure is assigned.
(1) Gastrointestinal Stromal Tumors With Excision of Stomach and Small Intestine
As discussed in the proposed rule, gastrointestinal stromal tumors (GIST) are tumors of connective tissue, and are currently assigned to MDC 8 (Diseases and Disorders of the Musculoskeletal System and Connective Tissue). The ICD-10-CM diagnosis codes describing GIST are listed in the table below.

We stated in the proposed rule that during our review of cases that group to MS-DRGs 981 through 983, we noted that when procedures describing open excision of the stomach or small intestine (ICD-10-PCS procedure codes 0DB60ZZ (Excision of stomach, open approach) and 0DB80ZZ (Excision of small intestine, open approach)) were reported with a principal diagnosis of GIST, the cases group to MS-DRGs 981 through 983. These two excision codes are assigned to several MDCs, as listed in the table below. We stated in the proposed rule that whenever there is a surgical procedure reported on the claim, which is unrelated to the MDC to which the case was assigned based on the principal diagnosis, it results in an MS-DRG assignment to a surgical class referred to as “unrelated operating room procedures”.

We first examined cases that reported a principal diagnosis of GIST and ICD-10-PCS procedure code 0DB60ZZ or 0DB80ZZ that currently group to MS-DRGs 981 through 983, as well as all cases in MS-DRGs 981 through 983. Our findings are shown in the table below.

Of the MDCs to which these gastrointestinal excision procedures are currently assigned, we stated that our clinical advisors indicated that cases with a principal diagnosis of GIST that also report an open gastrointestinal excision procedure code would logically be assigned to MDC 6 (Diseases and Disorders of the Digestive System). Within MDC 6, ICD-10-PCS procedures codes 0DB60ZZ and 0DB80ZZ are currently assigned to MS-DRGs 326, 327, and 328 (Stomach, Esophageal and Duodenal Procedures with MCC, CC, and without CC/MCC, respectively). To understand how the resources associated with the subset of cases reporting a principal diagnosis of GIST and procedure code 0DB60ZZ or 0DB80ZZ compare to those of cases in MS-DRGs 326, 327, and 328 as a whole, we examined the average costs and average length of stay for all cases in MS-DRGs 326, 327, and 328. Our findings are shown in the table below.

In the proposed rule, we stated that our clinical advisors reviewed these data and noted that the average length of stay and average costs of this subset of cases were similar to those of cases in MS-DRGs 326, 327, and 328 in MDC 6. To consider whether it was appropriate to move the GIST diagnosis codes from MDC 8, we examined the other procedure codes reported for cases that report a principal diagnosis of GIST and noted that almost all of the O.R. procedures most frequently reported were assigned to MDC 6 rather than MDC 8. Further, we stated that our clinical advisors believe that, given the similarity in resource use between this subset of cases and cases in MS-DRGs 326, 327, and 328, and that the GIST diagnosis codes are gastrointestinal in nature, they would be more appropriately assigned to MS-DRGs 326, 327, and 328 in MDC 6 than their current assignment in MDC 8. Therefore, we proposed to move the GIST diagnosis codes listed above from MDC 8 to MDC 6 within MS-DRGs 326, 327, and 328. We stated that, under our proposal, cases reporting a principal diagnosis of GIST would group to MS-DRGs 326, 327, and 328.
We note that every diagnosis code is assigned to a medical MS-DRG to define the logic of the MS-DRG either as a principal or secondary diagnosis. We also note that, as discussed in section II.F.13.a., certain procedure codes may affect the MS-DRG and result in a surgical MS-DRG assignment. We are clarifying that under this proposal, cases reporting a principal diagnosis of GIST would group to MS-DRGs 326, 327, and 328 only in the presence of a surgical procedure assigned to MS-DRGs 326, 327, and 328; in the absence of a surgical procedure, cases with a principal diagnosis of GIST would group to MS-DRGs 374, 375, and 376 (Digestive Malignancy with MCC, with CC, and without CC/MCC, respectively), which is the medical MS-DRG that contains digestive malignancies, and to which they would be assigned within MDC 6. We refer the reader to the ICD-10 MS-DRG Version 36 Definitions Manual for complete documentation of the logic for case assignment to surgical MS-DRGs 326, 327, and 328 and to medical MS-DRGs 374, 375, and 376 (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html).
Comment: Several commenters supported our proposal. A commenter stated that placing the ICD-10-CM diagnosis codes describing GIST in the proposed DRGs would better reflect the gastrointestinal nature of the underlying GIST disease and the resource use associated with this subset of cases relative to others within the same MDC/DRG groupings.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to move the GIST diagnosis codes listed above from MDC 8 to MDC 6, with the additional clarification that in the absence of a surgical procedure, these cases are assigned to the medical MS-DRGs 374, 375 and 376 under the ICD-10 MS-DRGs Version 37, effective October 1, 2019. As a result, cases reporting a principal diagnosis of GIST and a procedure code that is assigned to MS-DRGs 326, 327, and 328 (such as ICD-10-PCS codes 0DB60ZZ and 0DB80ZZ) will group to MS-DRGs 326, 327, and 328.
(2) Peritoneal Dialysis Catheter Complications
As discussed in the proposed rule, during our review of the cases currently grouping to MS-DRGs 981-983, we noted that cases reporting a principal diagnosis of complications of peritoneal dialysis catheters with procedure codes describing removal, revision, and/or insertion of new peritoneal dialysis catheters group to MS-DRGs 981 through 983. The ICD-10-CM diagnosis codes that describe complications of peritoneal dialysis catheters, listed in the table below, are assigned to MDC 21 (Injuries, Poisonings and Toxic Effects of Drugs). These principal diagnoses are frequently reported with the procedure codes describing removal, revision, and/or insertion of new peritoneal dialysis catheters.

The procedure codes in the table below describe removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes and are currently assigned to MDC 6 (Diseases and Disorders of the Digestive System) in MS-DRGs 356, 357, and 358 (Other Digestive System O.R. Procedures with MCC, with CC, and without CC/MCC, respectively).

As indicated in the proposed rule, we examined the claims data from the September 2018 update of the FY 2018 MedPAR file for the average costs and length of stay for cases that report a principal diagnosis of complications of peritoneal dialysis catheters with a procedure describing removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes. Our findings are shown in the table below. We noted in the proposed rule that we did not find any such cases in MS-DRG 983.

We stated that our clinical advisors indicated that, within MDC 21, the procedures describing removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes most suitably group to MS-DRGs 907, 908, and 909, which contain all procedures for injuries that are not specific to the hand, skin, and wound debridement. To determine how the resources for this subset of cases compared to cases in MS-DRGs 907, 908, and 909 as a whole, we examined the average costs and length of stay for cases in MS-DRGs 907, 908, and 909. Our findings are shown in the table below.

Further, we stated in the proposed rule that our clinical advisors considered these data and noted that the average costs and length of stay for this subset of cases, most of which group to MS-DRG 981, are lower than the average costs and length of stay for cases of the same severity level in MS-DRGs 907. However, we further stated that our clinical advisors believe that the procedures describing removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes are clearly related to the principal diagnosis codes describing complications of peritoneal dialysis catheters and, therefore, it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses. Therefore, we proposed to add the eight procedure codes listed in the table above that describe removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes to MDC 21 (Injuries, Poisonings & Toxic Effects of Drugs) in MS-DRGs 907, 908, and 909. As indicated in the proposed rule, under this proposal, cases reporting a principal diagnosis of complications of peritoneal dialysis catheters with a procedure describing removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes would group to MS-DRGs 907, 908, and 909.
Comment: Commenters supported our proposal to add the eight procedure codes listed in the table above that describe removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes to MDC 21.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add the eight procedure codes listed in the table above that describe removal, revision, and/or insertion of new peritoneal dialysis catheters or revision of synthetic substitutes to MDC 21.
(3) Bone Excision With Pressure Ulcers
As discussed in the proposed rule, during our review of the cases that group to MS-DRGs 981 through 983, we noted that when procedures describing excision of the sacrum, pelvic bones, and coccyx (ICD-10-PCS procedure codes 0QB10ZZ (Excision of sacrum, open approach), 0QB20ZZ (Excision of right pelvic bone, open approach), 0QB30ZZ (Excision of left pelvic bone, open approach), and 0QBS0ZZ (Excision of coccyx, open approach)) are reported with a principal diagnosis of pressure ulcers in MDC 9 (Diseases and Disorders of the Skin, Subcutaneous Tissue and Breast), the cases group to MS-DRGs 981 through 983. As noted in the proposed rule, the procedures describing excision of the sacrum, pelvic bones, and coccyx group to several MDCs, which are listed in the table below.
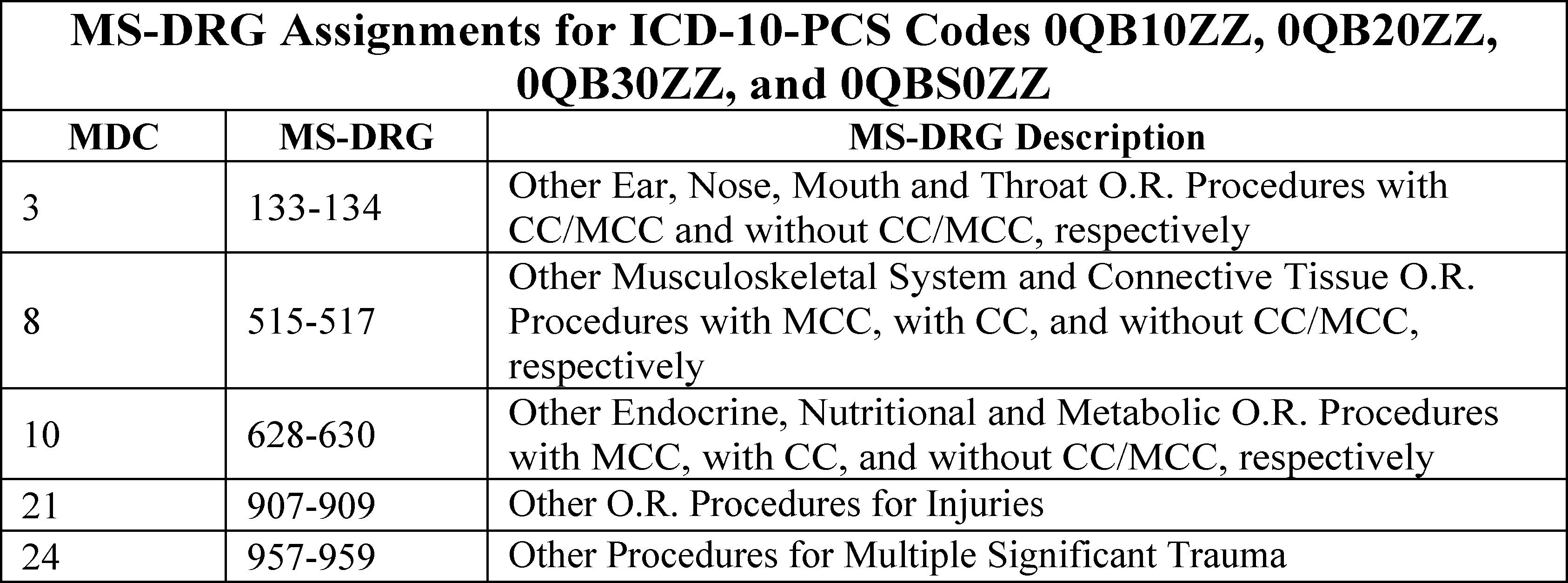
We stated in the proposed rule that, when cases reporting procedure codes describing excision of the sacrum, pelvic bones, and coccyx report a principal diagnosis from MDC 9, the ICD-10-CM diagnosis codes that are most frequently reported as principal diagnoses are listed below.
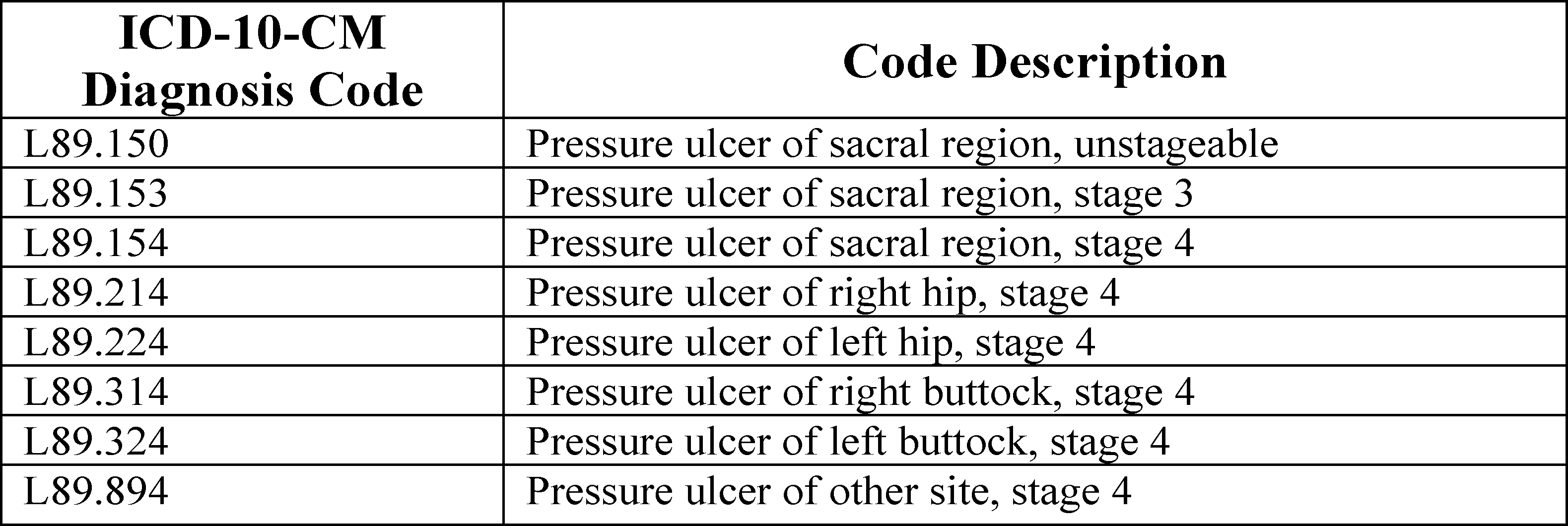
As indicated in the proposed rule, we examined the claims data from the September 2018 update of the FY 2018 MedPAR file for the average costs and length of stay for cases that report procedures describing excision of the sacrum, pelvic bones, and coccyx in conjunction with a principal diagnosis of pressure ulcers.

We stated that our clinical advisors indicated that, given the nature of these procedures, they could not be appropriately assigned to the specific surgical MS-DRGs within MDC 9, which are: Skin graft; skin debridement; mastectomy for malignancy; and breast biopsy, local excision, and other breast procedures. Therefore, we stated in the proposed rule that our clinical advisors believe that these procedures would most suitably group to MS-DRGs 579, 580, and 581 (Other Skin, Subcutaneous Tissue and Breast Procedures with MCC, with CC, and without CC/MCC, respectively), which contain procedures assigned to MDC 9 that do not fit within the specific surgical MS-DRGs in MDC 9. Therefore, as indicated in the proposed rule, we examined the claims data for the average length of stay and average costs for MS-DRGs 579, 580, and 581 in MDC 9. Our findings are shown in the table below.

We stated that our clinical advisors reviewed these data and noted that, in this subset of cases, most cases group to MS-DRGs 981 and 982 and have greater average length of stay and average costs than those cases of the same severity level in MS-DRGs 579 and 580. We further stated that the smaller number of cases that group to MS-DRG 983 have lower average costs than cases in MS-DRG 581. However, we stated that our clinical advisors believe that the procedure codes describing excision of the sacrum, pelvic bones, and coccyx are clearly related to the principal diagnosis codes describing pressure ulcers, as these procedures would be performed to treat pressure ulcers in the sacrum, hip, and buttocks regions. Therefore, we stated in the proposed rule that our clinical advisors believe that it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses. Therefore, we proposed to add the ICD-10-PCS procedure codes describing excision of the sacrum, pelvic bones, and coccyx to MDC 9 in MS-DRGs 579, 580, and 581. As noted in the proposed rule, under this proposal, cases reporting a principal diagnosis in MDC 9 (such as pressure ulcers) with a procedure describing excision of the sacrum, pelvic bones, and coccyx would group to MS-DRGs 579, 580, and 581.
Comment: Commenters did not support our proposal to add the ICD-10-PCS procedure codes describing excision of the sacrum, pelvic bones, and coccyx to MDC 9 in MS-DRGs 579, 580, and 581. Commenters stated that it is not appropriate for procedures performed on muscles to be grouped to MS-DRGs for skin and subcutaneous tissues. A commenter stated that once a pressure ulcer extends into the muscle or bone, it is no longer a disease of the skin and subcutaneous tissue, but a disease of the musculoskeletal tissue.
Response: We note that all pressure ulcers, including those that extend to the muscle or bone, are assigned to MDC 9, so that for purposes of DRG assignment, the GROUPER categorizes all pressure ulcers as diseases of the skin and subcutaneous tissue. As noted in the proposed rule, our clinical advisors believe that these procedures would be performed to treat pressure ulcers in the sacrum, hip, and buttocks regions. The surgical MS-DRGs within each MDC that include `other' procedures are intended to encompass procedures that, while not directly related to the MDC, can and do occur with principal diagnoses in that MDC with sufficient frequency.
Comment: A commenter stated that they recognize that CMS may have selected MDC 9 as it includes all pressure ulcers, but recommended that CMS consider MDC 8 instead. A commenter stated that if the debridement is performed to the level of the soft tissue, then the case should group to MS-DRGs 501, 502, and 503 (Soft tissue procedures with MCC, with CC, and without CC/MCC respectively). The commenter stated that they believe it should be the procedure that determines the MDC and DRG to which the case groups.
Response: As explained in the proposed rule, when conducting the review of procedures producing assignment to MS-DRGs 981 through 983 or MS-DRGs 987 through 989, the objective is to identify those procedures occurring in conjunction with certain principal diagnoses with sufficient frequency to justify adding them to one of the surgical MS-DRGs for the MDC in which the diagnosis falls, or to move the principal diagnosis codes to the MDC in which the procedure falls. During this analysis, we noted that procedures describing excision of the sacrum, pelvic bones, and coccyx group to MS-DRGs 981 through 983 when reported with a principal diagnosis in MDC 9. If we were to add these procedures to MDC 8, that would not address the matter of these procedures producing assignment to MS-DRGs 981 through 983. Since our clinical advisors believe that these procedures are clearly related to the principal diagnoses assigned to MDC 9, our clinical advisors believe that it is appropriate to add these procedures to MDC 9. We also note that, with the exception of the pre-MDC, assignment to MDCs is driven by the principal diagnosis and not by the procedure. Therefore, it is inconsistent with GROUPER logic to determine the MDC based on the procedure.
After consideration of the public comments we received, we are finalizing our proposal to add the ICD-10-PCS procedure codes describing excision of the sacrum, pelvic bones, and coccyx to MDC 9 in MS-DRGs 579, 580, and 581.
(4) Lower Extremity Muscle and Tendon Excision
As discussed in the proposed rule, during the review of the cases that group to MS-DRGs 981 through 983, we noted that when several ICD-10-PCS procedure codes describing excision of lower extremity muscles and tendons are reported in conjunction with ICD-10-CM diagnosis codes in MDC 10 (Endocrine, Nutritional and Metabolic Diseases and Disorders), the cases group to MS-DRGs 981 through 983. As indicated in the proposed rule, these ICD-10-PCS procedure codes are listed in the table below, and are assigned to several MS-DRGs, which are also listed below.


As noted in the proposed rule, the ICD-10-CM diagnosis codes in MDC 10 that are most frequently reported as the principal diagnosis with a procedure describing excision of lower extremity muscles and tendons are listed in the table below. We stated in the proposed rule that the combination indicates debridement procedures for more complex diabetic ulcers.

To understand the resource use for the subset of cases reporting procedure codes describing excision of lower extremity muscles and tendons that are currently grouping to MS-DRGs 981 through 983, as indicated in the proposed rule, we examined claims data for the average length of stay and average costs for these cases. Our findings are shown in the table below.

We stated in the proposed rule that our clinical advisors examined cases reporting procedures describing excision of lower extremity muscles and tendons with a principal diagnosis in the MS-DRGs within MDC 10 and determined that these cases would most suitably group to MS-DRGs 622, 623, and 624 (Skin Grafts and Wound Debridement for Endocrine, Nutritional and Metabolic Disorders with MCC, with CC, and without CC/MCC, respectively). Therefore, we examined the average length of stay and average costs for cases assigned to MS-DRGs 622, 623, and 624. Our findings are shown in the table below.

As indicated in the proposed rule, our clinical advisors reviewed these data and noted that most of the cases reporting procedures describing excision of lower extremity muscles and tendons group to MS-DRGs 981 and 982. For these cases, the average length of stay and average costs are lower than those of cases that currently group to MS-DRGs 622 and 623. However, our clinical advisors believe that these procedures are clearly related to the principal diagnoses in MDC 10, as they would be performed to treat skin-related complications of diabetes and, therefore, it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses. Therefore, we proposed to add the procedure codes listed previously describing excision of lower extremity muscles and tendons to MDC 10. We stated in the proposed rule that, under our proposal, cases reporting these procedure codes with a principal diagnosis in MDC 10 would group to MS-DRGs 622, 623, and 624.
Comment: A commenter supported our proposal to add the procedure codes describing excision of lower extremity muscles and tendons to MDC 10.
Response: We appreciate the commenter's support.
Comment: Other commenters did not support our proposal to add the procedure codes describing excision of lower extremity muscles and tendons to MDC 10. Commenters stated that muscle and tendon procedures are more resource intensive than skin procedures. A commenter stated that cases involving tendon excisions should group to MS-DRGs 501, 502, and 503 in MDC 8, and that cases involving excisions of muscle group to MS-DRGs 515, 516, and 517 in MDC 8. This commenter stated that the procedure should drive the MDC and DRGs to which the case is assigned.
Response: Our clinical advisors believe that these procedures are clearly related to the principal diagnoses assigned to MDC 10 with which they are most frequently reported (that is, codes describing diabetes with complications), and are therefore appropriately assigned to MDC 10, and specifically to MS-DRGs 622, 623, and 624, which describe wound debridement. We also note that, with the exception of the pre-MDC, assignment to MDCs is driven by the principal diagnosis and not by the procedure. Therefore, it is inconsistent with the GROUPER logic to determine the MDC based on the procedure.
After consideration of the public comments we received, we are finalizing our proposal to add the procedure codes listed previously describing excision of lower extremity muscles and tendons to MDC 10.
(5) Kidney Transplantation Procedures
As discussed in the proposed rule, during our review of the cases that group to MS-DRGs 981 through 983, we noted that when procedures describing transplantation of kidneys (ICD-10-PCS procedure codes 0TY00Z0 (Transplantation of right kidney, allogeneic, open approach) and 0TY10Z0 (Transplantation of left kidney, allogeneic, open approach)) are reported in conjunction with ICD-10-CM diagnosis codes in MDC 5 (Diseases and Disorders of the Circulatory System), the cases group to MS-DRGs 981 through 983. We stated that the ICD-10-CM diagnosis codes in MDC 5 that are reported with the kidney transplantation codes are I13.0 (Hypertensive heart and chronic kidney disease with heart failure and with stage 1 through stage 4 chronic kidney disease) and I13.2 (Hypertensive heart and chronic kidney disease with heart failure and with stage 5 chronic kidney disease), which group to MDC 5. Procedure codes describing transplantation of kidneys are assigned to MS-DRG 652 (Kidney Transplant) in MDC 11. As indicated in the proposed rule, we examined claims data to identify the average length of stay and average costs for cases reporting procedure codes describing transplantation of kidneys with a principal diagnosis in MDC 5, which are currently grouping to MS-DRGs 981 through 983. Our findings are shown in the table below. We stated in the proposed rule that we did not find any such cases in MS-DRG 983.

We further stated that our clinical advisors examined the MS-DRGs within MDC 5 and indicated that, given the nature of the procedures compared to the specific surgical procedures contained in the other surgical MS-DRGs in MDC 5, they could not be appropriately assigned to any of the specific surgical MS-DRGs. Therefore, they determined that these cases would most suitably group to MS-DRG 264 (Other Circulatory System O.R. Procedures), which contains a broader range of procedures related to MDC 5 diagnoses. As indicated in the proposed rule, we examined claims data to determine the average length of stay and average costs for cases assigned to MS-DRG 264. We found a total of 10,073 cases, with an average length of stay of 9.3 days and average costs of $22,643.
Our clinical advisors reviewed these data and noted that the average costs for cases reporting transplantation of kidney with a diagnosis from MDC 5 are similar to the average costs of cases in MS-DRG 264 ($22,643 in MS-DRG 264 compared to $25,340 in MS-DRG 981), while the average length of stay is shorter than that of cases in MS-DRG 264 (9.3 days in MS-DRG 264 compared to 6.8 days for this subset of cases in MS-DRG 981). We stated in the proposed rule that our clinical advisors noted that ICD-10-CM diagnosis codes describing hypertensive heart and chronic kidney disease without heart failure (I13.10 (Hypertensive heart and chronic kidney disease without heart failure, with stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease) and I13.11 (Hypertensive heart and chronic kidney disease without heart failure, with stage 5 chronic kidney disease, or end stage renal disease group) group to MS-DRG 652 (Kidney Transplant) in MDC 11 (Diseases and Disorders of the Kidney and Urinary Tract)). Our clinical advisors also noted that the counterpart codes describing hypertensive heart and chronic kidney disease with heart failure are as related to the kidney transplantation codes as the codes without heart failure, but because the codes with heart failure group to MDC 5, cases reporting a kidney transplant procedure with a diagnosis code of hypertensive heart and chronic kidney disease with heart failure currently group to MS-DRGs 981 through 983. Therefore, we proposed to add ICD-10-PCS procedure codes 0TY00Z0 and 0TY10Z0 to MS-DRG 264 in MDC 5. We stated in the proposed rule that, under this proposal, cases reporting a principal diagnosis in MDC 5 with a procedure describing kidney transplantation would group to MS-DRG 264 in MDC 5. We also noted in the proposed rule that, because MDC 5 covers the circulatory system and kidney transplants generally group to MDC 11, we invited public comments on whether the procedure codes should instead continue to group to MS-DRGs 981 through 983.
Comment: Commenters opposed our proposal to add ICD-10-PCS procedure codes 0TY00Z0 and 0TY10Z0 to MS-DRG 264 in MDC 5. A commenter stated that the proposed relative weight for MS-DRG 652, where most kidney transplant procedures are grouped, is 3.384, while the proposed weight for MS-DRG 264 is 3.2357. Some commenters stated that this proposal would reduce the reimbursement for kidney transplantation of recipients with serious cardiac conditions by 33 percent. Commenters stated that cases that involve both chronic kidney disease and heart failure should not be paid less than cases that involve patients without serious comorbid conditions. Commenters suggested that CMS instead assign these cases to MDC 652, noting that the length of stay for the vast majority of kidney transplant cases involving serious cardiac conditions approximates the length of stay for kidney transplants in general. Commenters also stated that assigning all kidney transplant cases to the same MS-DRG simplifies collection of cost data, stating that when cases are split among several MS-DRG “families” it complicates the analysis required to determine whether additional severity-based MS-DRGs would be appropriate. Commenters stated that if it was not possible to assign these cases to MS-DRG 652, then the cases should remain in MS-DRGs 981 through 983. Commenters disagreed with assigning these cases to a circulatory DRG because the procedure is performed on the urinary system.
Response: We appreciate the comments and concerns raised on our proposal. Our clinical advisors generally believe that it is preferable to assign these cases to a discrete MS-DRG within the GROUPER rather than allowing them to continue to group to MS-DRGs 981 through 983, which do not contain a group of clinically coherent principal diagnoses, but instead consist of cases from various MDCs that are unrelated to one another. However, we believe it would be appropriate to take additional time to review the concerns raised by commenters consistent with the President's recent Executive Order on Advancing American Kidney Health (see https://www.whitehouse.gov/presidential-actions/executive-order-advancing-american-kidney-health/). Therefore, after consideration of public comments, we are not finalizing our proposal to add ICD-10-PCS procedure codes 0TY00Z0 and 0TY10Z0 to MS-DRG 264 in MDC 5. Accordingly, cases reporting a principal diagnosis in MDC 5 with a procedure describing kidney transplantation (i.e., procedure code 0TY00Z0 or 0TY10Z0) will continue to group to MS-DRGs 981 through 983 under the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
(6) Insertion of Feeding Device
As discussed in the proposed rule, during our review of the cases that group to MS-DRGs 981 through 983, we noted that when ICD-10-PCS procedure code 0DH60UZ (Insertion of feeding device into stomach, open approach) is reported with ICD-10-CM diagnosis codes assigned to MDC 1 (Diseases and Disorders of the Nervous System) or MDC 10 (Endocrine, Nutritional and Metabolic Diseases and Disorders), the cases group to MS-DRGs 981 through 983. ICD-10-PCS procedure code 0DH60UZ is currently assigned to MDC 6 (Diseases and Disorders of the Digestive System) in MS-DRGs 326, 327, and 328 (Stomach, Esophageal and Duodenal Procedures) and MDC 21 (Injuries, Poisonings and Toxic Effects of Drugs) in MS-DRGs 907, 908, and 909 (Other O.R. Procedures for Injuries). We stated in the proposed rule that we also noticed that: (1) When ICD-10-PCS procedure code 0DH60UZ is reported with a principal diagnosis in MDC 1, the ICD-10-CM diagnosis codes reported with this procedure code describe cerebral infarctions of various etiology and anatomic locations and resulting complications; and (2) when ICD-10-PCS procedure code 0DH60UZ is reported with a principal diagnosis in MDC 10, the ICD-10-CM diagnosis codes reported with this procedure code pertain to dehydration, failure to thrive, and various forms of malnutrition.
As indicated in the proposed rule, we examined claims data to identify the average length of stay and average costs for cases in MS-DRGs 981 through 983 reporting ICD-10-PCS procedure code 0DH60UZ in conjunction with a principal diagnosis from MDC 1 or MDC 10. Our findings are shown in the table below.

In the proposed rule we stated that our clinical advisors determined that the feeding tube procedure was related to specific diagnoses within MDC 1 and MDC 10 and, therefore, could be assigned to both MDCs. Therefore, they reviewed the MS-DRGs within MDC 1 and MDC 10. We stated that they determined that the most suitable MS-DRG assignment within MDC 1 would be MS-DRGs 040, 041, and 042 (Peripheral, Cranial Nerve and Other Nervous System Procedures with MCC, with CC or Peripheral Neurostimulator, and without CC/MCC, respectively), which contain procedures assigned to MDC 1 that describe insertion of devices into anatomical areas that are not part of the nervous system. Our clinical advisors determined that the most suitable MS-DRG assignment within MDC 10 would be MS-DRGs 628, 629, and 630 (Other Endocrine, Nutritional and Metabolic O.R. Procedures with MCC, with CC, and without CC/MCC, respectively), which contain the most clinically similar procedures assigned to MDC 10, such as those describing insertion of infusion pump into subcutaneous tissue and fascia. Therefore, we examined claims data to identify the average length of stay and average costs for cases assigned to MDC 1 in MS-DRGs 040, 041, and 042 and MDC 10 in MS-DRGs 628, 629, and 630. Our findings are shown in the tables below.


Our clinical advisors reviewed these data and noted that the average length of stay and average costs for the subset of cases reporting ICD-10-PCS procedure code 0DH60UZ with a principal diagnosis assigned to MDC 1 are higher than those cases in MS-DRGs 040, 041, and 042. For example, the cases reporting ICD-10-PCS procedure code 0DH60UZ and a principal diagnosis in MDC 1 that currently group to MS-DRG 981 have an average length of stay of 19.3 days and average costs of $40,598, while the cases in MS-DRG 040 have an average length of stay of 10.2 days and average costs of $27,096. We stated in the proposed rule that our clinical advisors noted that the average length of stay and average costs for the subset of cases reporting ICD-10-PCS procedure code 0DH60UZ with a principal diagnosis assigned to MDC 10 are more closely aligned with those cases in MS-DRGs 628, 629, and 630. We stated that in both cases, our clinical advisors believe that the insertion of feeding device is clearly related to the principal diagnoses in MDC 1 and MDC 10 and, therefore, it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses. Therefore, we proposed to add ICD-10-PCS procedure code 0DH60UZ to MDC 1 and MDC 10. We stated in the proposed rule that, under this proposal, cases reporting procedure code 0DH60UZ with a principal diagnosis in MDC 1 would group to MS-DRGs 040, 041, and 042, while cases reporting ICD-10-PCS procedure code 0DH60UZ with a principal diagnosis in MDC 10 would group to MS-DRGs 628, 629, and 630.
Comment: Commenters supported our proposal to add ICD-10-PCS procedure code 0DH60UZ to MDC 1 and MDC 10.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-PCS procedure code 0DH60UZ to MDC 1 and MDC 10.
(7) Basilic Vein Reposition in Chronic Kidney Disease
As discussed in the proposed rule, during our review of the cases that group to MS-DRGs 981 through 983, we noted that when procedures codes describing reposition of basilic vein (ICD-10-PCS procedure codes 05SB0ZZ (Reposition right basilic vein, open approach), 05SB3ZZ (Reposition right basilic vein, percutaneous approach), 05SC0ZZ (Reposition left basilic vein, open approach), and 05SC3ZZ (Reposition left basilic vein, percutaneous approach)) are reported with a principal diagnosis in MDC 11 (Diseases and Disorders of the Kidney and Urinary Tract) (typically describing chronic kidney disease), the cases group to MS-DRGs 981 through 983. We stated in the proposed rule that this code combination suggests a revision of an arterio-venous fistula in a patient on chronic hemodialysis. As indicated in the proposed rule, we examined claims data to identify the average length of stay and average costs for cases reporting procedures describing reposition of basilic vein with a principal diagnosis in MDC 11, which are currently grouping to MS-DRGs 981 through 983. Our findings are shown in the table below.

We stated in the proposed rule that our clinical advisors examined claims data for cases in the MS-DRGs within MDC 11 and determined that cases reporting procedures describing reposition of basilic vein with a principal diagnosis in MDC 11 would most suitably group to MS-DRGs 673, 674, and 675 (Other Kidney and Urinary Tract Procedures with MCC, with CC, and without CC/MCC, respectively), to which MDC 11 procedures describing reposition of veins (other than renal veins) are assigned. Therefore, we examined claims data to identify the average length of stay and average costs for cases assigned to MS-DRGs 673, 674, and 675. Our findings are shown in the table below.

As indicated in the proposed rule, our clinical advisors reviewed these data and noted that the average length of stay and average costs for cases reporting procedures describing reposition of basilic vein with a principal diagnosis in MDC 11 with an MCC are significantly lower than for those cases in MS-DRG 673. The average length of stay and average costs are similar for those cases with a CC, while the single case without a CC or MCC had significantly lower costs than the average costs of cases in MS-DRG 675. However, we stated that our clinical advisors believe that when the procedures describing reposition of basilic vein are reported with a principal diagnosis describing chronic kidney disease, the procedure is likely related to arteriovenous fistulas for dialysis associated with the chronic kidney disease. Therefore, we stated in the proposed rule that our clinical advisors believe that it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses. Therefore, we proposed to add ICD-10-PCS procedures codes 05SB0ZZ, 05SB3ZZ, 05SC0ZZ, and 05SC3ZZ to MDC 11. We stated that, under our proposal, cases reporting procedure codes describing reposition of basilic vein with a principal diagnosis in MDC 11 would group to MS-DRGs 673, 674, and 675.
Comment: Commenters supported our proposal to add ICD-10-PCS procedures codes 05SB0ZZ, 05SB3ZZ, 05SC0ZZ, and 05SC3ZZ to MDC 11.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-PCS procedures codes 05SB0ZZ, 05SB3ZZ, 05SC0ZZ, and 05SC3ZZ to MDC 11.
(8) Colon Resection With Fistula
As discussed in the proposed rule, during our review of the cases that group to MS-DRGs 981 through 983, we noted that when ICD-10-PCS procedure code 0DTN0ZZ (Resection of sigmoid colon, open approach) is reported with a principal diagnosis in MDC 11 (Diseases and Disorders of the Kidney and Urinary Tract), the cases group to MS-DRGs 981 through 983. We stated that the principal diagnosis most frequently reported with ICD-10-PCS procedure code 0DTN0ZZ in MDC 11 is ICD-10-CM code N32.1 (Vesicointestinal fistula). As indicated in the proposed rule, ICD-10-PCS procedure code 0DTN0ZZ currently groups to several MDCs, which are listed in the table below.

As we stated in the proposed rule, we examined claims data to identify the average length of stay and average costs for cases reporting procedure code 0DTN0ZZ with a principal diagnosis in MDC 11, which are currently grouping to MS-DRGs 981 through 983. Our findings are shown in the table below.

Our clinical advisors examined the MS-DRGs within MDC 11 and determined that the cases reporting procedure code 0DTN0ZZ with a principal diagnosis in MDC 11 would most suitably group to MS-DRGs 673, 674, and 675, which contain procedures performed on structures other than kidney and urinary tract anatomy. We note that the claims data describing the average length of stay and average costs for cases in these MS-DRGs are included in a table earlier in this section. Because vesicointestinal fistulas involve both the bladder and the bowel, some procedures in both MDC 6 (Diseases and Disorders of the Digestive System) and MDC 11 (Diseases and Disorders of the Kidney and Urinary Tract) would be expected to be related to a principal diagnosis of vesicointestinal fistula (ICD-10-CM code N32.1). We stated in the proposed rule that our clinical advisors observed that procedure code 0DTN0ZZ is the second most common procedure reported in conjunction with a principal diagnosis of code N32.1, after ICD-10-PCS procedure code 0TQB0ZZ (Repair bladder, open approach), which is assigned to both MDC 6 and MDC 11. Our clinical advisors reviewed the data and noted that the average length of stay and average costs for this subset of cases are generally higher for this subset of cases than for cases in MS-DRGs 673, 674, and 675. However, we stated that our clinical advisors believe that when ICD-10-PCS procedure code 0DTN0ZZ is reported with a principal diagnosis in MDC 11 (typically vesicointestinal fistula), the procedure is related to the principal diagnosis. Therefore, we proposed to add ICD-10-PCS procedure code 0DTN0ZZ to MDC 11. We stated in the proposed rule that, under our proposal, cases reporting procedure code 0DTN0ZZ with a principal diagnosis of vesicointestinal fistula (diagnosis code N32.1) in MDC 11 would group to MS-DRGs 673, 674, and 675.
Comment: Some commenters supported our proposal to add ICD-10-PCS procedure code 0DTN0ZZ to MDC 11.
Response: We appreciate the commenters' support.
Comment: A commenter opposed our proposal to add ICD-10-PCS procedure code 0DTN0ZZ to MDC 11 in MS-DRGs 673, 674, and 675 because these MS-DRGs does not account for the organ in which the disease originates. This commenter stated that the disease process that causes the formation of a vesicointestinal fistula generally do not originate in the bladder. This commenter recommended that CMS instead consider assigning ICD-10-PCS procedure code 0DTN0ZZ to MS-DRGs 329, 330, and 331 (Major small and large bowel procedures with MCC, with CC, and without CC/MCC, respectively).
Response: As we stated in the proposed rule, ICD-10-PCS procedure code 0DTN0ZZ is already assigned to MDC 6 in MS-DRGs 329, 330, and 331. As described above, when conducting the review of procedures producing assignment to MS-DRGs 981 through 983 or MS-DRGs 987 through 989, the objective is to identify those procedures occurring in conjunction with certain principal diagnoses with sufficient frequency to justify adding them to one of the surgical MS-DRGs for the MDC in which the diagnosis falls, or to move the principal diagnosis codes to the MDC in which the procedure falls. During this analysis, we noted that ICD-10-PCS procedure code 0DTN0ZZ groups to MS-DRGs 981 through 983 when reported with a principal diagnosis in MDC 11. Given that the only way to address this grouping issue is to move or add the diagnosis code and procedure codes, in this case we proposed to add ICD-10-PCS procedure code 0DTN0ZZ to MDC 11. While the disease process that causes the formation of a vesicointestinal fistula may not originate in the bladder, our clinical advisors believe that when ICD-10-PCS procedure code 0DTN0ZZ is reported in conjunction with the vesicointestinal fistula, it is related to the diagnosis.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-PCS procedure code 0DTN0ZZ to MDC 11.
b. Reassignment of Procedures Among MS-DRGs 981 Through 983 and 987 Through 989
We also review the list of ICD-10-PCS procedures that, when in combination with their principal diagnosis code, result in assignment to MS-DRGs 981 through 983, or 987 through 989, to ascertain whether any of those procedures should be reassigned from one of those two groups of MS-DRGs to the other group of MS-DRGs based on average costs and the length of stay. We look at the data for trends such as shifts in treatment practice or reporting practice that would make the resulting MS-DRG assignment illogical. If we find these shifts, we would propose to move cases to keep the MS-DRGs clinically similar or to provide payment for the cases in a similar manner. Generally, we move only those procedures for which we have an adequate number of discharges to analyze the data.
Based on the results of our review of claims data in the September 2018 update of the FY 2018 MedPAR file, we did not propose to change the current structure of MS-DRGs 981 through 983 and MS-DRGs 987 through 989.
We did not receive any public comments on our maintaining the current structure of MS-DRGs 981 through 983 and MS-DRGs 987 through 989. Therefore, we are finalizing the current structure of MS-DRGs 981 through 983 and MS-DRGs 987 through 989 without modification.
c. Additions for Diagnosis and Procedure Codes to MDCs
As we did in the FY 2020 IPPS/LTCH PPS proposed rule, below we summarize the requests we received to examine cases found to group to MS-DRGs 981 through 983 or MS-DRGs 987 through 989 to determine if it would be appropriate to add procedure codes to one of the surgical MS-DRGs for the MDC into which the principal diagnosis falls or to move the principal diagnosis to the surgical MS-DRGs to which the procedure codes are assigned.
(1) Stage 3 Pressure Ulcers of the Hip
We received a request to reassign cases for a stage 3 pressure ulcer of the left hip when reported with procedures involving excision of pelvic bone or transfer of hip muscle from MS-DRGs 981, 982, and 983 (Extensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC, and without CC/MCC, respectively) to MS-DRG 579 (Other Skin, Subcutaneous Tissue and Breast Procedures with MCC) in MDC 9. ICD-10-CM diagnosis code L89.223 (Pressure ulcer left hip, stage 3) is used to report this condition and is currently assigned to MDC 9 (Diseases and Disorders of the Skin, Subcutaneous Tissue and Breast). We refer readers to section II.F.12.a. of the preamble of this final rule, where we address ICD-10-PCS procedure code 0QB30ZZ (Excision of left pelvic bone, open approach), which was reviewed as part of our ongoing analysis of the unrelated MS-DRGs and which we proposed, and are finalizing, to add to MS-DRGs 579, 580, and 581 in MDC 5. (While the requestor only referred to base MS-DRG 579, in the proposed rule we stated that we believe it is appropriate to assign the cases to MS-DRGs 579, 580, and 581 by severity level.) We stated that ICD-10-PCS procedure codes 0KXP0ZZ (Transfer left hip muscle, open approach) and 0KXN0ZZ (Transfer right hip muscle, open approach) may be reported to describe transfer of hip muscle procedures and are currently assigned to MDC 1 (Diseases and Disorders of the Nervous System) and MDC 8 (Diseases and Disorders of the Musculoskeletal System and Connective Tissue). We included ICD-10-PCS procedure code 0KXN0ZZ in our analysis because it describes the identical procedure on the right side.
Our analysis of this grouping issue confirmed that, when a stage 3 pressure ulcer of the left hip (ICD-10-CM diagnosis code L89.223) is reported as a principal diagnosis with ICD-10-PCS procedure code 0KXP0ZZ or 0KXN0ZZ, these cases group to MS-DRGs 981, 982, and 983. The reason for this grouping is because whenever there is a surgical procedure reported on a claim that is unrelated to the MDC to which the case was assigned based on the principal diagnosis, it results in an MS-DRG assignment to a surgical class referred to as “unrelated operating room procedures.” In the example provided, because ICD-10-CM diagnosis code L89.223 describing a stage 3 pressure ulcer of left hip is classified to MDC 9 and because ICD-10-PCS procedure codes 0KXP0ZZ and 0KXN0ZZ are classified to MDC 1 (Diseases and Disorders of the Nervous System) in MS-DRGs 040, 041, and 042 (Peripheral, Cranial Nerve and Other Nervous System Procedures with MCC, with CC or Peripheral Neurostimulator, and without CC/MCC, respectively) and MDC 8 (Diseases and Disorders of the Musculoskeletal System and Connective Tissue) in MS-DRGs 500, 501, and 502 (Soft Tissue Procedures with MCC, with CC, and without CC/MCC, respectively), the GROUPER logic assigns this case to the “unrelated operating room procedures” set of MS-DRGs.
For our review of this grouping issue and the request to have procedure code 0KXP0ZZ added to MDC 9, in the proposed rule we examined claims data for cases reporting procedure code 0KXP0ZZ or 0KXN0ZZ in conjunction with a diagnosis code that typically groups to MDC 9. Our findings are shown in the table below.

As indicated in the proposed rule and earlier, the requestor suggested that we move ICD-10-PCS procedure code 0KXP0ZZ to MS-DRG 579. However, we stated that our clinical advisors believe that, within MDC 9, these procedure codes are more clinically aligned with the procedure codes assigned to MS-DRGs 573, 574, and 575 (Skin Graft for Skin Ulcer or Cellulitis with MCC, with CC and without CC/MCC, respectively), which are more specific to the care of stage 3, 4 and unstageable pressure ulcers than MS-DRGs 579, 580, and 581. Therefore, as indicated in the proposed rule, we examined claims data to identify the average length of stay and average costs for cases assigned to MS-DRGs 573, 574, and 575. Our findings are shown in the table below.
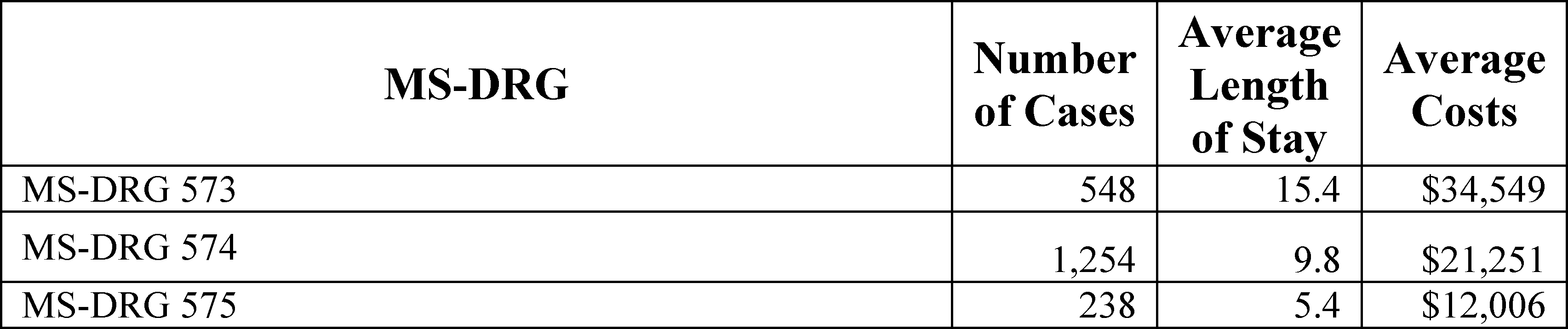
We noted in the proposed rule that the average costs for cases in MS-DRGs 573 and 574 are higher than the average costs of the subset of cases with the same severity reporting a hip muscle transfer and a principal diagnosis in MDC 9, while the average costs of those cases in MS-DRG 575 are similar to the average costs of those cases that are currently grouping to MS-DRG 983. However, we stated in the proposed rule that our clinical advisors believe that the cases of hip muscle transfer represent a distinct, recognizable clinical group similar to those cases in MS-DRGs 573, 574, and 575, and that the procedures are clearly related to the principal diagnosis codes. Therefore, we stated that they believe that it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses. Therefore, we proposed to add ICD-10-PCS procedure codes 0KXP0ZZ and 0KXN0ZZ to MDC 9. We stated in the proposed rule that, under our proposal, cases reporting ICD-10-PCS procedure code 0KXP0ZZ or 0KXN0ZZ with a principal diagnosis in MDC 9 would group to MS-DRGs 573, 574, and 575. We are clarifying that under our proposal, cases reporting ICD-10-PCS codes 0KXP0ZZ or 0KXN0ZZ would also group to MS-DRGs 576, 577, and 578 in the absence of a principal diagnosis of skin ulcer or cellulitis. The reason for this additional assignment is that under the GROUPER logic, all of the procedures assigned to MS-DRGs 573, 574, and 575 are also assigned to MS-DRGs 576, 577, and 578; the presence or absence of a principal diagnosis of skin ulcer or cellulitis determines whether the case groups to MS-DRGs 573, 574, and 575 or to MS-DRGs 576, 577, and 578. We refer the reader to the ICD-10 MS-DRG Version 36 Definitions Manual for complete documentation of the logic for case assignment to MS-DRGs 573, 574, 575, 576, 577, and 578 (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html).
Comment: A commenter supported our proposal to add ICD-10-PCS procedure codes 0KXP0ZZ and 0KXN0ZZ to MDC 9.
Response: We appreciate the commenter's support.
Comment: Other commenters did not support our proposal to add ICD-10-PCS procedure codes 0KXP0ZZ and 0KXN0ZZ to MDC 9. The commenters stated that it is not appropriate for procedures performed on muscles to group to MS-DRGs for skin and subcutaneous tissues. These commenters also stated that transfer procedures are more clinically significant and resource intensive than grafts to the skin and subcutaneous tissue.
Response: Our clinical advisors agree that procedures performed on muscles would not generally be expected to group to MS-DRGs for skin and subcutaneous tissues. However, while they believe that principal diagnoses from MDC 9 would not be the principal diagnoses most often reported with ICD-10-PCS procedure codes 0KXP0ZZ and 0KXN0ZZ, the claims data indicate that there are cases reporting a principal diagnosis assigned to MDC 9, as identified by the requestor. Our clinical advisors continue to believe that these cases involving hip muscle transfer represent a distinct, recognizable clinical group, which is similar to those cases in MS-DRGs 573, 574, and 575, and that the procedures are clearly related to the principal diagnosis codes. With respect to the comment that transfer procedures are more clinically significant and resource intensive than grafts to the skin and subcutaneous tissue, our clinical advisors believe that the transfer procedures are sufficiently similar to procedures involving grafts to the skin and subcutaneous tissue, particularly given that a review of the data presented in the proposed rule and described previously in this section demonstrate that the average costs for MS-DRGs 573, 574, and 575 are generally greater than those of the subset of cases involving hip muscle transfer with a diagnosis in MDC 9. Most of the cases that currently group to MS-DRGs 981 through 983 occur in MS-DRGs 981 and 982, which have average costs of $25,023 and $17,955 respectively, while the MS-DRGs with the same severity level, MS-DRGs 573 and 574, have average costs of $34,549 and $21,251, respectively. We also believe it is preferable to assign these cases to a discrete MS-DRG within the GROUPER logic rather than allowing them to continue to group to MS-DRGs 981 through 983, which do not contain a group of clinically coherent principal diagnoses. MS-DRGs 573, 574, 575, 576, 577, and 578, which are specific to the care of conditions that necessitate skin grafts, represent a group of clinically coherent principal diagnoses to which procedures describing transfer of muscles are more appropriately assigned than those in MS-DRGs 981 through 983.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-PCS procedure codes 0KXP0ZZ and 0KXN0ZZ to MDC 9.
(2) Gastrointestinal Stromal Tumor
We received a request to reassign cases for gastrointestinal stromal tumor of the stomach when reported with a procedure describing laparoscopic bypass of the stomach to jejunum from MS-DRGs 981, 982, and 983 to MS-DRGs 326, 327, and 328 (Stomach, Esophageal and Duodenal Procedures with MCC, with CC, and without CC/MCC, respectively) by adding ICD-10-PCS procedure code 0D164ZA (Bypass stomach to jejunum, percutaneous endoscopic approach) to MDC 6. ICD-10-CM diagnosis code C49.A2 (Gastrointestinal stromal tumor of stomach) is used to report this condition and is currently assigned to MDC 8. ICD-10-PCS procedure code 0D164ZA is used to report the stomach bypass procedure and is currently assigned to MDC 5 (Diseases and Disorders of the Circulatory System), MDC 6 (Diseases and Disorders of the Digestive System), MDC 7 (Diseases and Disorders of the Hepatobiliary System and Pancreas), MDC 10 (Endocrine, Nutritional and Metabolic Diseases and Disorders), and MDC 17 (Myeloproliferative Diseases and Disorders, Poorly Differentiated Neoplasms). We refer readers to section II.F.12.a. of the preamble of this final rule where we discuss our finalized policy to move the listed diagnosis codes describing gastrointestinal stromal tumors, including ICD-10-CM diagnosis code C49.A2, into MDC 6. Therefore, in the proposed rule, we stated that this proposal, if finalized, would address the cases grouping to MS-DRGs 981 through 983 by instead moving the diagnosis codes to MDC 6, which would result in the diagnosis code and the procedure code referenced by the requestor grouping to the same MDC.
We did not receive comments on our proposal to address this grouping issue by moving the diagnosis codes to MDC 6 rather than moving the procedure codes as requested. We refer the reader to section II.F.12.a. of this final rule for the comments regarding our proposal to move the GIST diagnosis codes to MDC 6, as well as our finalization of this proposal.
(3) Finger Cellulitis
We received a request to reassign cases for cellulitis of the right finger when reported with a procedure describing open excision of the right finger phalanx from MS-DRGs 981, 982, and 983 to MS-DRGs 579, 580, and 581 (Other Skin, Subcutaneous Tissue and Breast Procedures with MCC, with CC, and without CC/MCC, respectively). In the proposed rule, we stated that, currently, ICD-10-CM diagnosis code L03.011 (Cellulitis of right finger) is used to report this condition and is currently assigned to MDC 09 in MS-DRGs 573, 574, and 575 (Skin Graft for Skin Ulcer or Cellulitis with MCC, CC, and without CC/MCC, respectively), 576, 577, and 578 (Skin Graft except for Skin Ulcer or Cellulitis with MCC, CC, and without CC/MCC, respectively), and 602 and 603 (Cellulitis with MCC and without MCC, respectively). ICD-10-PCS procedure code 0PBT0ZZ (Excision of right finger phalanx, open approach) is used to identify the excision procedure, and is currently assigned to MDC 03 (Diseases and Disorders of the Ear, Nose, Mouth and Throat) in MS-DRGs 133 and 134 (Other Ear, Nose, Mouth and Throat O.R. Procedures with CC/MCC, and without CC/MCC, respectively); MDC 08 (Diseases and Disorders of the Musculoskeletal System and Connective Tissue) in MS-DRGs 515, 516, and 517 (Other Musculoskeletal System and Connective Tissue O.R. Procedures with MCC, with CC, and without CC/MCC, respectively); MDC 10 (Endocrine, Nutritional and Metabolic Diseases and Disorders) in MS-DRGs 628, 629, and 630 (Other Endocrine, Nutritional and Metabolic O.R. Procedures with MCC, with CC, and without CC/MCC, respectively); MDC 21 (Injuries, Poisonings and Toxic Effects of Drugs) in MS-DRGs 907, 908, and 909 (Other O.R. Procedures for Injuries with MCC, with CC, and without CC/MCC, respectively); and MDC 24 (Multiple Significant Trauma) in MS-DRGs 957, 958, and 959 (Other O.R. Procedures for Multiple Significant Trauma with MCC, with CC, and without CC/MCC, respectively).
Our analysis of this grouping issue confirmed that when a procedure such as open excision of right finger phalanx (ICD-10-PCS procedure code 0PBT0ZZ) is reported with a principal diagnosis from MDC 9, such as cellulitis of the right finger (ICD-10-CM diagnosis code L03.011), these cases group to MS-DRGs 981, 982, and 983. As we stated in the proposed rule, during our review of this issue, we also examined claims data for similar procedures describing excision of phalanges (which are listed in the table below) and noted the same pattern. We further noted that the ICD-10-PCS procedure codes describing excision of phalanx procedures with the diagnostic qualifier “X”, which are used to report these procedures when performed for diagnostic purposes, are already assigned to MS-DRGs 579, 580, and 581 (to which the requestor suggested these cases group). We stated in the proposed rule that our clinical advisors also believe that procedures describing resection of phalanges should be assigned to the same MS-DRG as the excisions, because the resection procedures would also group to MS-DRGs 981, 982, and 983 when reported with a principal diagnosis from MDC 9.

As noted in the previous discussion and the proposed rule, whenever there is a surgical procedure reported on the claim that is unrelated to the MDC to which the case was assigned based on the principal diagnosis, it results in an MS-DRG assignment to a surgical class referred to as “unrelated operating room procedures”.
We examined the claims data for the three codes describing cellulitis of the finger (ICD-10-CM diagnosis codes L03.011 (Cellulitis of the right finger), L03.012 (Cellulitis of left finger), and L03.019 (Cellulitis of unspecified finger)) to identify the average length of stay and average costs for cases reporting a principal diagnosis of cellulitis of the finger in conjunction with the excision of phalanx procedures listed in the table above. We also noted in the proposed rule that there were no cases reporting a principal diagnosis of cellulitis of the finger in conjunction with the resection of phalanx procedures listed in the table above.

We also examined the claims data to identify the average length of stay and average costs for all cases in MS-DRGs 579, 580, and 581. Our findings are shown in the table in section II.F.12.A.3.of the preamble of this final rule.
We stated in the proposed rule that while our clinical advisors noted that the average length of stay and average costs for cases in MS-DRGs 579, 580, and 581 are generally higher than the average length of stay and average costs for the subset of cases reporting a principal diagnosis of cellulitis of the finger and a procedure describing excision of phalanx, they believe that the procedures are clearly related to the principal diagnosis codes and, therefore, it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses, particularly given that procedures describing excision of phalanx with the diagnostic qualifier “X” are already assigned to these MS-DRGs. In addition, we stated that our clinical advisors believe it is clinically appropriate for the procedures describing resection of phalanx to be assigned to MS-DRGs 579, 580, and 581 as well. Therefore, we proposed to add the procedure codes describing excision and resection of phalanx listed above to MS-DRGs 579, 580, and 581. We stated that, under this proposal, cases reporting one of the excision or resection procedures listed in the table above in conjunction with a principal diagnosis from MDC 9 would group to MS-DRGs 579, 580, and 581.
Comment: A commenter supported our proposal to add the procedure codes describing excision and resection of phalanx listed above to MS-DRGs 579, 580, and 581 in MDC 9.
Response: We appreciate the commenter's support.
Comment: Other commenters did not support our proposal to add the procedure codes describing excision and resection of phalanx listed above to MS-DRGs 579, 580, and 581 in MDC 9. Commenters stated that it does not appear clinically appropriate for bone procedures to be grouped to skin and subcutaneous tissue MS-DRGs, and that the small number of cases suggests that this may be a coding issue.
Response: We note that MS-DRGs 579, 580, and 581 already contain many bone-related procedures, such as those beginning with 0PD, which describe extraction of bone. In addition, our clinical advisors believe that it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses, particularly given that procedures describing excision of phalanx with the diagnostic qualifier “X” are already assigned to these MS-DRGs.
After consideration of the public comments we received, we are finalizing our proposal to add procedure codes describing excision and resection of phalanx listed above to MS-DRGs 579, 580, and 581 in MDC 9.
(4) Multiple Trauma With Internal Fixation of Joints
We received a request to reassign cases involving multiple significant trauma with internal fixation of joints from MS-DRGs 981, 982, and 983 to MS-DRGs 957, 958, and 959 (Other O.R. Procedures for Multiple Significant Trauma with MCC, with CC, and without CC/MCC, respectively). The requestor provided an example of several ICD-10-CM diagnosis codes that together described multiple significant trauma in conjunction with ICD-10-PCS procedure codes in tables 0SH and 0RH that describe internal fixation of joints. The requestor provided several suggestions to address this assignment, including: adding all ICD-10-PCS procedure codes in MDC 8 (Diseases and Disorders of the Musculoskeletal System and Connective Tissue) with the exception of codes that group to MS-DRG 956 (Limb Reattachment, Hip and Femur Procedures for Multiple Significant Trauma) to MS-DRGs 957, 958, and 959; adding codes within the ICD-10-PCS tables 0SH and 0RH to MDC 24; and adding ICD-10-PCS procedure codes from all MDCs except those that currently group to MS-DRG 955 (Craniotomy for Multiple Significant Trauma) or MS-DRG 956 (Limb Reattachment, Hip and Femur Procedures for Multiple Significant Trauma) to MS-DRGs 957, 958, and 959.
We stated in the proposed rule that, while we understand the requestor's concern about these multiple significant trauma cases, we believe any potential reassignment of these cases requires significant analysis. We further stated that, similar to our analysis of MDC 14 (initially discussed at 81 FR 56854), there are multiple logic lists in MDC 24 that would need to be reviewed. For example, to satisfy the logic for multiple significant trauma, the logic requires a diagnosis code from the significant trauma principal diagnosis list and two or more significant trauma diagnoses from different body sites. The significant trauma logic lists for the other body sites (which include head, chest, abdominal, kidney, urinary system, pelvis or spine, upper limb, and lower limb) allow the extensive list of diagnosis codes included in the logic to be reported as a principal or secondary diagnosis. The analysis of the reporting of all the codes as a principal and/or secondary diagnosis within MDC 24, combined with the analysis of all of the ICD-10-PCS procedure codes within MDC 8, is anticipated to be a multi-year effort. Therefore, we stated that we plan to consider this issue for future rulemaking as part of our ongoing analysis of the unrelated procedure MS-DRGs.
(5) Totally Implantable Vascular Access Devices
We received a request to reassign cases for insertion of totally implantable vascular access devices (TIVADs) listed in the table below when reported with principal diagnoses in MDCs other than MDC 9 (Diseases and Disorders of the Skin, Subcutaneous Tissue and Breast) and MDC 11 (Diseases and Disorders of the Kidney and Urinary Tract) from MS-DRGs 981 through 983 to a surgical MS-DRG within the appropriate MDC based on the principal diagnosis. The requestor noted that the insertion of TIVAD procedures are newly designated as O.R. procedures, effective October 1, 2018, and are assigned to MDCs 9 and 11. The requestor stated that TIVADs can be placed for a variety of purposes and are used to treat a wide range of malignancies at various sites and, therefore, would likely have a relationship to the principal diagnosis within any MDC. The requestor suggested that procedures describing the insertion of TIVADs group to surgical MS-DRGs within every MDC (other than MDCs 2, 20, and 22, which do not contain surgical MS-DRGs). The requestor further stated that the surgical hierarchy should assign more significant O.R. procedures within each MDC to a higher position than procedures describing the insertion of TIVADs because these procedures consume less O.R. resources than more invasive procedures.

We stated in the proposed rule that, while we agreed that TIVAD procedures may be performed in connection with a variety of principal diagnoses, we note that because these procedures are newly designated as O.R. procedures effective October 1, 2018, we do not yet have sufficient data to analyze this request. We further stated that we plan to consider this issue in future rulemaking as part of our ongoing analysis of the unrelated procedure MS-DRGs.
(6) Gastric Band Procedure Complications or Infections
We received a request to reassign cases for infection or complications due to gastric band procedures when reported with a procedure describing revision of or removal of extraluminal device in/from the stomach from MS-DRGs 987, 988, and 989 (Non-Extensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC and without MCC/CC, respectively) to MS-DRGs 326, 327, and 328 (Stomach, Esophageal, and Duodenal Procedures with MCC, with CC, and without CC/MCC, respectively). We stated in the proposed rule that ICD-10-CM diagnosis codes K95.01 (Infection due to gastric band procedure) and K95.09 (Other complications of gastric band procedure) are used to report these conditions and are currently assigned to MDC 6 (Diseases and Disorders of the Digestive System). ICD-10-PCS procedure codes 0DW64CZ (Revision of extraluminal device in stomach, percutaneous endoscopic approach) and 0DP64CZ (Removal of extraluminal device from stomach, percutaneous endoscopic approach) are used to report the revision of, or removal of, an extraluminal device in/from the stomach and are currently assigned to MDC 10 (Endocrine, Nutritional and Metabolic Diseases and Disorders) in MS-DRGs 619, 620, and 621 (O.R. Procedures for Obesity with MCC with CC, and without CC/MCC, respectively).
Our analysis of this grouping issue confirmed that when procedures describing the revision of or removal of an extraluminal device in/from the stomach are reported with principal diagnoses in MDC 6 (such as ICD-10-CM diagnosis codes K95.01 and K95.09), in the absence of a procedure assigned to MDC 6, these cases group to MS-DRGs 987, 988, and 989. As noted in the previous discussion and in the proposed rule, whenever there is a surgical procedure reported on the claim that is unrelated to the MDC to which the case was assigned based on the principal diagnosis, it results in an MS-DRG assignment to a surgical class referred to as “unrelated operating room procedures”.
As indicated in the proposed rule, we examined the claims data to identify cases involving ICD-10-PCS procedure codes 0DW64CZ and 0DP64CZ reported with a principal diagnosis of K95.01 or K95.09 that are currently grouping to MS-DRGs 987, 988, and 989. Our findings are shown in the table below.
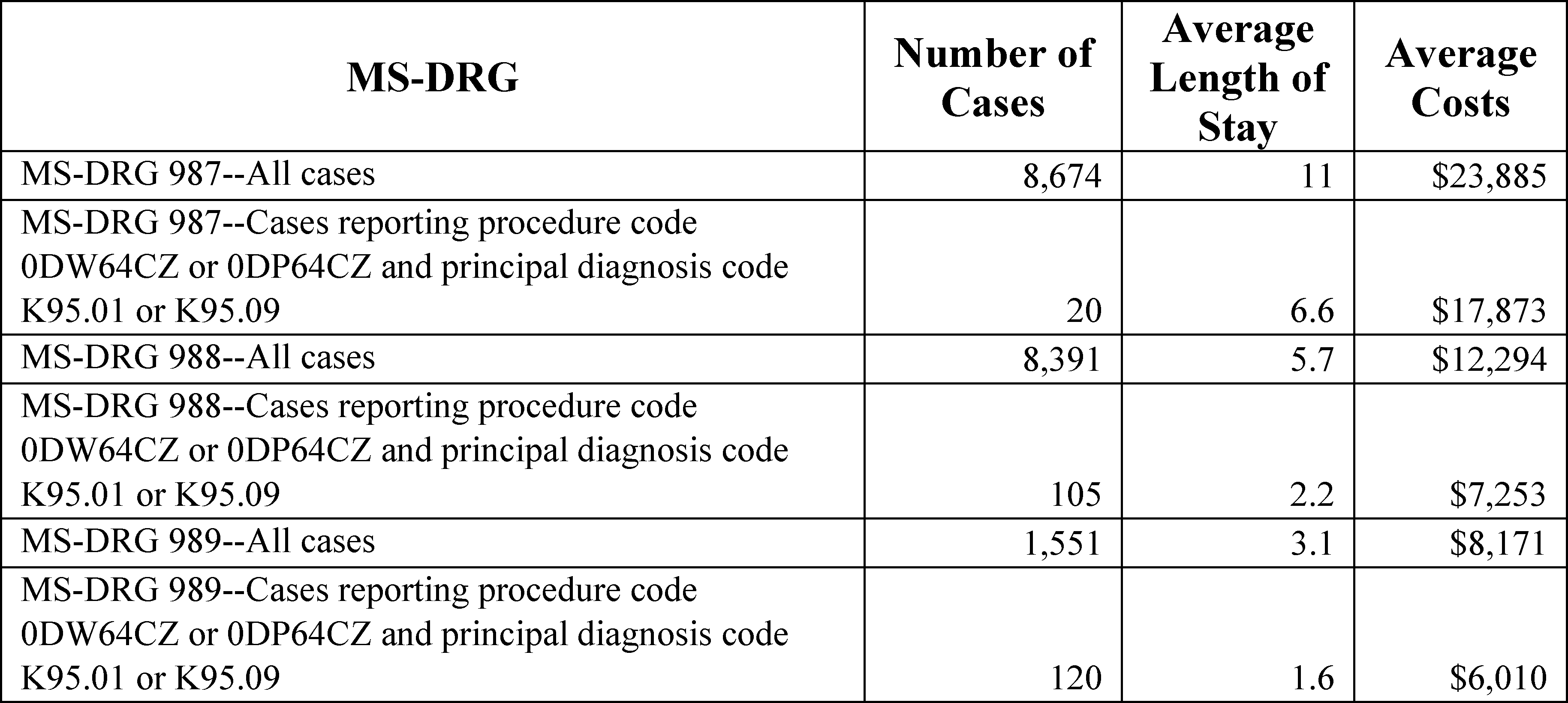
We also examined the data for cases in MS-DRGs 326, 327, and 328, and our findings are provided in a table presented in section II.F.12.a. of the preamble of this final rule. We stated in the proposed rule that, while our clinical advisors noted that the average length of stay and average costs of cases in MS-DRGs 326, 327, and 328 are significantly higher than the average length of stay and average costs for the subset of cases reporting procedure code 0DW64CZ or 0DP64CZ and a principal diagnosis code of K95.01 or K95.09, they believe that the procedures are clearly related to the principal diagnosis and, therefore, it is clinically appropriate for the procedures to group to the same MS-DRGs as the principal diagnoses. In addition, we stated that our clinical advisors believe that because these procedures are intended to treat a complication of a procedure related to obesity, rather than the obesity itself, they are more appropriately assigned to stomach, esophageal, and duodenal procedures (MS-DRGs 326, 327, and 328) in MDC 6 than to procedures for obesity (MS-DRGs 619, 620, and 621) in MDC 10.
Therefore, we proposed to add ICD-10-PCS procedure codes 0DW64CZ and 0DP64CZ to MDC 6 in MS-DRGs 326, 327, and 328. We stated in the proposed rule that, under this proposal, cases reporting procedure code 0DW64CZ or 0DP64CZ in conjunction with a principal diagnosis code of K95.01 or K95.09 would group to MS-DRGs 326, 327, and 328.
Comment: Commenters supported our proposal to add ICD-10-PCS procedure codes 0DW64CZ and 0DP64CZ to MDC 6 in MS-DRGs 326, 327, and 328.
Response: We appreciate the commenters' support.
After consideration of the public comments received, we are finalizing our proposal to add ICD-10-PCS procedure codes 0DW64CZ and 0DP64CZ to MDC 6 in MS-DRGs 326, 327, and 328.
(7) Peritoneal Dialysis Catheters
We received a request to reassign cases for complications of peritoneal dialysis catheters when reported with procedure codes describing removal, revision, and/or insertion of new peritoneal dialysis catheters from MS-DRGs 981 through 983 to MS-DRGs 356, 357, and 358 (Other Digestive System O.R. Procedures with MCC, with CC, and without CC/MCC, respectively) in MDC 6 by adding the diagnosis codes describing complications of peritoneal dialysis catheters to MDC 6. We stated in the proposed rule that our clinical advisors believe it is more appropriate to add the procedure codes describing removal, revision, and/or insertion of new peritoneal dialysis catheters to MS-DRGs 907, 908, and 909 than to move the diagnosis codes describing complications of peritoneal dialysis catheters to MDC 6 because the diagnosis codes describe complications, rather than initial placement, of peritoneal dialysis catheters, and therefore, are most clinically aligned with the diagnosis codes assigned to MDC 21 (where they are currently assigned). In section II.F.12.a. of the preamble of the proposed rule, we proposed, and as discussed in this final rule, are finalizing, to add procedures describing removal, revision, and/or insertion of peritoneal dialysis catheters to MS-DRGs 907, 908, and 909 in MDC 21. We refer readers to section II.F.12.a. of the preamble of this final rule in which we describe our analysis of this issue as part of our broader review of the unrelated MS-DRGs.
(8) Occlusion of Left Renal Vein
We received a request to reassign cases for varicose veins in the pelvic region when reported with an embolization procedure from MS-DRGs 981, 982 and 983 (Non-Extensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC, and without CC/MCC, respectively) to MS-DRGs 715 and 716 (Other Male Reproductive System O.R. Procedures for Malignancy with CC/MCC and without CC/MCC, respectively) and MS-DRGs 717 and 718 (Other Male Reproductive System O.R. Procedures Except Malignancy with CC/MCC and without CC/MCC, respectively) in MDC 12 (Diseases and Disorders of the Male Reproductive System) and to MS-DRGs 749 and 750 (Other Female Reproductive System O.R. Procedures with CC/MCC and without CC/MCC, respectively) in MDC 13 (Diseases and Disorders of the Female Reproductive System). We stated in the proposed rule that ICD-10-CM diagnosis code I86.2 (Pelvic varices) is reported to identify the condition of varicose veins in the pelvic region and is currently assigned to MDC 12 and to MDC 13. ICD-10-PCS procedure code 06LB3DZ (Occlusion of left renal vein with intraluminal device, percutaneous approach) may be reported to describe an embolization procedure performed for the treatment of pelvic varices and is currently assigned to MDC 5 (Diseases and Disorders of the Circulatory System) in MS-DRGs 270, 271, and 272 (Other Major Cardiovascular Procedures with MCC, with CC, and without CC/MCC, respectively), MDC 6 (Diseases and Disorders of the Digestive System) in MS-DRGs 356, 357, and 358 (Other Digestive System O.R. Procedures with MCC, with CC, and without CC/MCC, respectively), MDC 21 (Injuries, Poisonings and Toxic Effects of Drugs) in MS-DRGs 907, 908, and 909 (Other O.R. Procedures for Injuries with MCC, CC, without CC/MCC, respectively), and MDC 24 (Multiple Significant Trauma) in MS-DRGs 957, 958, 959 (Other O.R. Procedures for Multiple Significant Trauma with MCC, with CC, and without CC/MCC, respectively). The requestor also noted that when this procedure is performed on pelvic veins on the right side, such as the ovarian vein, (which is reported with ICD-10-PCS code 06L03DZ (Occlusion of inferior vena cava with intraluminal device, percutaneous approach)) for varicose veins in the right pelvic region, the case groups to MS-DRGs 715 and 716 and MS-DRGs 717 and 718 in MDC 12 (for male patients) or MS-DRGs 749 and 750 in MDC 13 (for female patients). We note that there was an inadvertent error in the proposed rule in which the term “renal vein” was referenced rather than “pelvic veins on the right side” or “ovarian vein”.
Our analysis of this grouping issue confirmed that when ICD-10-CM diagnosis code I86.2 (Pelvic varices) is reported with ICD-10-PCS procedure code 06LB3DZ, the case groups to MS-DRGs 981, 982, and 983. As noted above in previous discussions and in the proposed rule, whenever there is a surgical procedure reported on the claim that is unrelated to the MDC to which the case was assigned based on the principal diagnosis, it results in an MS-DRG assignment to a surgical class referred to as “unrelated operating room procedures.”
As indicated in the proposed rule, we examined the claims data to identify cases involving procedure code 06LB3DZ in MS-DRGs 981, 982, and 983 reported with a principal diagnosis code of I86.2. We found no cases in the claims data.
In the absence of data to examine, we indicated that our clinical advisors reviewed this request and agreed with the requestor that when the embolization procedure is performed on the left ovarian vein (reported with ICD-10-PCS procedure code 06LB3DZ), it should group to the same MS-DRGs as when it is performed on the right ovarian vein. Therefore, we proposed to add ICD-10-PCS procedure code 06LB3DZ to MDC 12 in MS-DRGs 715, 716, 717, and 718 and to MDC 13 in MS-DRGs 749 and 750. We stated in the proposed rule that, under this proposal, cases reporting ICD-10-CM diagnosis code I86.2 with ICD-10-PCS procedure code 06LB3DZ would group to MDC 12 (for male patients) or MDC 13 (for female patients).
Comment: A commenter stated that this issue should be reevaluated, because 06L03DZ is not the correct code to report procedures done on the right renal vein; rather, 06L93DZ (Occlusion of right renal vein with intraluminal device, percutaneous approach) would be reported instead.
Response: We appreciate the commenter's request for clarification. We wish to clarify that certain specific pelvic veins do not have their own body part value in the ICD-10-PCS, and the ICD-10-PCS Body Part Key instructs coders to assign the inferior vena cava body part for veins such as the right ovarian vein and the right testicular vein, and to assign the left renal vein body part for veins such as the left ovarian vein and the left testicular vein. Therefore, ICD-10-PCS codes 06L03DZ or 06LB3DZ indeed may be reported to describe an embolization procedure performed for the treatment of pelvic varices of these respective sites. As such, our clinical advisors believe that when the embolization procedure is performed on veins classified to the left renal vein, such as the left ovarian vein and the left testicular vein, it should group to the same MS-DRGs as when it is performed on veins classified to the inferior vena cava, such as the right ovarian vein and the right testicular vein.
After consideration of the public comments we received, we are finalizing our proposal to add ICD-10-PCS procedure code 06LB3DZ to MDC 12 in MS-DRGs 715, 716, 717, and 718 and to MDC 13 in MS-DRGs 749 and 750.
13. Operating Room (O.R.) and Non-O.R. Issues
a. Background
Under the IPPS MS-DRGs (and former CMS MS-DRGs), we have a list of procedure codes that are considered operating room (O.R.) procedures. Historically, we developed this list using physician panels that classified each procedure code based on the procedure and its effect on consumption of hospital resources. For example, generally the presence of a surgical procedure which required the use of the operating room would be expected to have a significant effect on the type of hospital resources (for example, operating room, recovery room, and anesthesia) used by a patient, and therefore, these patients were considered surgical. Because the claims data generally available do not precisely indicate whether a patient was taken to the operating room, surgical patients were identified based on the procedures that were performed. Generally, if the procedure was not expected to require the use of the operating room, the patient would be considered medical (non-O.R.).
Currently, each ICD-10-PCS procedure code has designations that determine whether and in what way the presence of that procedure on a claim impacts the MS-DRG assignment. First, each ICD-10-PCS procedure code is either designated as an O.R. procedure for purposes of MS-DRG assignment (“O.R. procedures”) or is not designated as an O.R. procedure for purposes of MS-DRG assignment (“non-O.R. procedures”). Second, for each procedure that is designated as an O.R. procedure, that O.R. procedure is further classified as either extensive or non-extensive. Third, for each procedure that is designated as a non-O.R. procedure, that non-O.R. procedure is further classified as either affecting the MS-DRG assignment or not affecting the MS-DRG assignment. We refer to these designations that do affect MS-DRG assignment as “non-O.R. affecting the MS-DRG.” For new procedure codes that have been finalized through the ICD-10 Coordination and Maintenance Committee meeting process and are proposed to be classified as O.R. procedures or non-O.R. procedures affecting the MS-DRG, our clinical advisors recommend the MS-DRG assignment which is then made available in association with the proposed rule (Table 6B.—New Procedure Codes) and subject to public comment. These proposed assignments are generally based on the assignment of predecessor codes or the assignment of similar codes. For example, we generally examine the MS-DRG assignment for similar procedures, such as the other approaches for that procedure, to determine the most appropriate MS-DRG assignment for procedures proposed to be newly designated as O.R. procedures. As discussed in section II.F.15. of the preamble of this final rule, we are making Table 6B.—New Procedure Codes—FY 2020 available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. We also refer readers to the ICD-10 MS-DRG Version 36 Definitions Manual at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html for detailed information regarding the designation of procedures as O.R. or non-O.R. (affecting the MS-DRG) in Appendix E—Operating Room Procedures and Procedure Code/MS-DRG Index.
In the FY 2020 IPPS/LTCH PPS proposed rule, we stated that, given the long period of time that has elapsed since the original O.R. (extensive and non-extensive) and non-O.R. designations were established, the incremental changes that have occurred to these O.R. and non-O.R. procedure code lists, and changes in the way inpatient care is delivered, we plan to conduct a comprehensive, systematic review of the ICD-10-PCS procedure codes. This will be a multi-year project during which we will also review the process for determining when a procedure is considered an operating room procedure. For example, we may restructure the current O.R. and non-O.R. designations for procedures by leveraging the detail that is now available in the ICD-10 claims data. We refer readers to the discussion regarding the designation of procedure codes in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38066) where we stated that the determination of when a procedure code should be designated as an O.R. procedure has become a much more complex task. This is, in part, due to the number of various approaches available in the ICD-10-PCS classification, as well as changes in medical practice. While we have typically evaluated procedures on the basis of whether or not they would be performed in an operating room, we believe that there may be other factors to consider with regard to resource utilization, particularly with the implementation of ICD-10. Therefore, as we stated in the proposed rule, we are again soliciting public comments on what factors or criteria to consider in determining whether a procedure is designated as an O.R. procedure in the ICD-10-PCS classification system for future consideration. Commenters should submit their recommendations to the following email address: MSDRGClassificationChange@cms.hhs.gov by November 1, 2019.
We stated in the proposed rule that, as a result of this planned review and potential restructuring, procedures that are currently designated as O.R. procedures may no longer warrant that designation, and conversely, procedures that are currently designated as non-O.R. procedures may warrant an O.R. type of designation. We intend to consider the resources used and how a procedure should affect the MS-DRG assignment. We may also consider the effect of specific surgical approaches to evaluate whether to subdivide specific MS-DRGs based on a specific surgical approach. We plan to utilize our available MedPAR claims data as a basis for this review and the input of our clinical advisors. As part of this comprehensive review of the procedure codes, we also intend to evaluate the MS-DRG assignment of the procedures and the current surgical hierarchy because both of these factor into the process of refining the ICD-10 MS-DRGs to better recognize complexity of service and resource utilization.
We will provide more detail on this analysis and the methodology for conducting this review in future rulemaking. As we noted in the proposed rule, as we continue to develop our process and methodology, as noted above, we are soliciting public comments on other factors to consider in our refinement efforts to recognize and differentiate consumption of resources for the ICD-10 MS-DRGs.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19231 through 19235), we addressed requests that we received regarding changing the designation of specific ICD-10-PCS procedure codes from non-O.R. to O.R. procedures, or changing the designation from O.R. procedure to non-O.R. procedure. Below we discuss the process that was utilized for evaluating the requests that were received for FY 2020 consideration. For each procedure, our clinical advisors considered:
- Whether the procedure would typically require the resources of an operating room;
- Whether it is an extensive or a nonextensive procedure; and
- To which MS-DRGs the procedure should be assigned.
We noted in the proposed rule that many MS-DRGs require the presence of any O.R. procedure. As a result, cases with a principal diagnosis associated with a particular MS-DRG would, by default, be grouped to that MS-DRG. Therefore, we do not list these MS-DRGs in our discussion below. Instead, we only discuss MS-DRGs that require explicitly adding the relevant procedures codes to the GROUPER logic in order for those procedure codes to affect the MS-DRG assignment as intended. In cases where we proposed to change the designation of procedure codes from non-O.R. procedures to O.R. procedures, we also proposed one or more MS-DRGs with which these procedures are clinically aligned and to which the procedure code would be assigned.
In addition, cases that contain O.R. procedures will map to MS-DRG 981, 982, or 983 (Extensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC, and without CC/MCC, respectively) or MS-DRG 987, 988, or 989 (Non-Extensive O.R. Procedure Unrelated to Principal Diagnosis with MCC, with CC, and without CC/MCC, respectively) when they do not contain a principal diagnosis that corresponds to one of the MDCs to which that procedure is assigned. These procedures need not be assigned to MS-DRGs 981 through 989 in order for this to occur. Therefore, if requestors included some or all of MS-DRGs 981 through 989 in their request or included MS-DRGs that require the presence of any O.R. procedure, we did not specifically address that aspect in summarizing their request or our response to the request in the section below.
For procedures that would not typically require the resources of an operating room, our clinical advisors determined if the procedure should affect the MS-DRG assignment.
As indicated in the proposed rule, we received several requests to change the designation of specific ICD-10-PCS procedure codes from non-O.R. procedures to O.R. procedures, or to change the designation from O.R. procedures to non-O.R. procedures. Below, as we did in the proposed rule, in this final rule, we detail and respond to some of those requests and, further, summarize and respond to the public comments we received in response to our proposals, if applicable. With regard to the remaining requests, as stated in the proposed rule, our clinical advisors believe it is appropriate to consider these requests as part of our comprehensive review of the procedure codes discussed above.
b. O.R. Procedures to Non-O.R. Procedures
(1) Bronchoalveolar Lavage
Bronchoalveolar lavage (BAL) is a diagnostic procedure in which a bronchoscope is passed through the patient's mouth or nose into the lungs. A small amount of fluid is squirted into an area of the lung and then collected for examination. Two requestors identified 13 ICD-10-PCS procedure codes describing BAL procedures that generally can be performed at bedside and would not require the resources of an operating room. In the ICD-10 MS-DRG Version 36 Definitions Manual, these 13 ICD-10-PCS procedure codes are currently recognized as O.R. procedures for purposes of MS-DRG assignment.
In the proposed rule, we stated that we agreed with the requestors that these procedures do not typically require the resources of an operating room. Therefore, we proposed to remove the following 13 procedure codes from the FY 2020 ICD-10 MS-DRGs Version 37 Definitions Manual in Appendix E—Operating Room Procedures and Procedure Code/MS-DRG Index as O.R. procedures. We stated in the proposed rule that, under this proposal, these procedures would no longer impact MS-DRG assignment.

Comment: Some commenters supported our proposal to designate the 13 procedure codes above as non-O.R. procedures.
Response: We appreciate the commenters' support.
Comment: Other commenters opposed our proposal to designate the 13 procedure codes above as non-O.R. procedures. A commenter stated that due to the complexity of the procedures being performed, they should continue to be designated as an O.R. procedure, while another commenter stated that CMS should not reassign any procedures as O.R. or non-O.R. until it has completed its comprehensive review.
Response: As indicated in the proposed rule, our clinical advisors believe that these procedures do not typically require the resources of an operating room. The commenter did not provide information to the contrary. We also do not agree with the commenter who stated that we should not reassign any procedures as O.R. or non-O.R; rather, while some requests may involve a broader review of additional ranges of ICD-10-PCS codes, such that we believe they are more appropriately considered as part of our comprehensive review of procedure codes, we generally believe it is more accurate to address requests to change the designation of procedures as OR or non-OR as they arise rather than waiting for the comprehensive review, which is a multiyear project.
After consideration of the public comments we received, we are finalizing our policy to designate the 13 codes above as non-O.R.
(2) Percutaneous Drainage of Pelvic Cavity
One requestor identified two ICD-10-PCS procedure codes that describe procedures involving percutaneous drainage of the pelvic cavity. The two ICD-10-PCS procedure codes are: 0W9J3ZX (Drainage of pelvic cavity, percutaneous approach, diagnostic) and 0W9J3ZZ (Drainage of pelvic cavity, percutaneous approach).
ICD-10-PCS procedure code 0W9J3ZX is currently recognized as an O.R. procedure for purposes of MS-DRG assignment, while the nondiagnostic ICD-10-PCS procedure code 0W9J3ZZ is not recognized as an O.R. procedure for purposes of MS-DRG assignment. The requestor stated that percutaneous drainage procedures of the pelvic cavity for both diagnostic and nondiagnostic purposes are not complex procedures and both types of procedures are usually performed in a radiology suite. The requestor stated that both procedures should be classified as non-O.R. procedures.
We stated in the proposed rule that we agreed with the requestor that these procedures do not typically require the resources of an operating room. Therefore, we proposed to remove procedure code 0W9J3ZX from the FY 2020 ICD-10 MS-DRG Version 37 Definitions Manual in Appendix E—Operating Room Procedures and Procedure Code/MS-DRG Index as an O.R. procedure. We stated that, under this proposal, this procedure would no longer impact MS-DRG assignment.
Comment: Commenters supported the proposal to change the designation of 0W9J3ZX to a non-O.R. procedure. The commenters stated that the proposal was reasonable, given the data and information provided.
A commenter stated that CMS should not consider any requests to modify the designation of procedures as O.R. or non-O.R. for FY 2020. As stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19230), CMS plans to conduct a comprehensive systematic review of the ICD-10-PCS procedure codes. The commenter suggested that reassignment requests should be held until the review has been completed.
Response: We appreciate the commenters' support. We do not agree with the commenter who stated that we should not reassign any procedures as O.R. or non-O.R; rather, while some requests may involve a broader review of additional ranges of ICD-10-PCS codes, such that we believe they are more appropriately considered as part of our comprehensive review of procedure codes, we generally believe it is more accurate to address requests to change the designation of procedures as OR or non-OR as they arise rather than waiting for the comprehensive review, which is a multiyear project. After consideration of the public comments we received, we are finalizing our proposal to change the designation of 0W9J3ZX from an O.R. procedure to non-O.R. procedure, effective October 1, 2019.
(3) Percutaneous Removal of Drainage Device
One requestor identified two ICD-10-PCS procedure codes that describe procedures involving the percutaneous placement and removal of drainage devices from the pancreas. These two ICD-10-PCS procedure codes are: 0FPG30Z (Removal of drainage device from pancreas, percutaneous approach) and 0F9G30Z (Drainage of pancreas with drainage device, percutaneous approach). ICD-10-PCS procedure code 0FPG30Z is currently recognized as an O.R. procedure for purposes of MS-DRG assignment, while ICD-10-PCS procedure code 0F9G30Z is not recognized as an O.R. procedure for purposes of MS-DRG assignment. The requestor stated that percutaneous placement of drains is typically performed in a radiology suite under image guidance and removal of a drain would not be more resource intensive than its placement.
We stated in the proposed rule that we agreed with the requestor that these procedures do not typically require the resources of an operating room. Therefore, we proposed to remove ICD-10-PCS procedure code 0FPG30Z from the FY 2020 ICD-10 MS-DRG Version 37 Definitions Manual in Appendix E—Operating Room Procedures and Procedure Code/MS-DRG Index as an O.R. procedure. We stated that, under this proposal, this procedure would no longer impact MS-DRG assignment.
Comment: Commenters supported the proposal to change the designation of 0FPG30Z to a non-O.R. procedure. The commenters stated that the proposal was reasonable, given the data and information provided.
A commenter stated that CMS should not consider any requests to modify the designation of procedures as O.R. or non-O.R. for FY 2020. As stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19230), CMS plans to conduct a comprehensive systematic review of the ICD-10-PCS procedure codes. The commenter suggested that reassignment requests should be held until the review has been completed.
Response: We appreciate the commenters' support. We do not agree with the commenter who stated that we should not reassign any procedures as O.R. or non-O.R; rather, while some requests may involve a broader review of additional ranges of ICD-10-PCS codes, such that we believe they are more appropriately considered as part of our comprehensive review of procedure codes, we generally believe it is more accurate to address requests to change the designation of procedures as OR or non-OR as they arise rather than waiting for the comprehensive review, which is a multiyear project. After consideration of the public comments we received, we are finalizing our proposal to change the designation of 0FPG30Z from an O.R. procedure to a non-O.R. procedure, effective October 1, 2019.
c. Non-O.R. Procedures to O.R. Procedures
(1) Percutaneous Occlusion of Gastric Artery
One requestor identified two ICD-10-PCS procedure codes that describe percutaneous occlusion and restriction of the gastric artery with intraluminal device, ICD-10-PCS procedure codes 04L23DZ (Occlusion of gastric artery with intraluminal device, percutaneous approach) and 04V23DZ (Restriction of gastric artery with intraluminal device, percutaneous approach), that the requestor stated are currently not recognized as O.R. procedures for purposes of MS-DRG assignment. The requestor noted that transcatheter endovascular embolization of the gastric artery with intraluminal devices uses comparable resources to transcatheter endovascular embolization of the gastroduodenal artery. The requestor stated that ICD-10-PCS procedure codes 04L33DZ (Occlusion of hepatic artery with intraluminal device, percutaneous approach) and 04V33DZ (Restriction of hepatic artery with intraluminal device, percutaneous approach) are recognized as O.R. procedures for purposes of MS-DRG assignment, and ICD-10-PCS procedure codes 04L23DZ and 04V23DZ should therefore also be recognized as O.R. procedures for purposes of MS-DRG assignment. We note that, contrary to the requestor's statement, ICD-10-PCS procedure code 04V23DZ is already recognized as an O.R. procedure for purposes of MS-DRG assignment.
We stated in the proposed rule that we agreed with the requestor that ICD-10-PCS procedure code 04L23DZ typically requires the resources of an operating room. Therefore, we proposed to add this code to the FY 2020 ICD-10 MS-DRG Version 37 Definitions Manual in Appendix E—Operating Room Procedures and Procedure Code/MS-DRG Index as an O.R. procedure assigned to MS-DRGs 270, 271, and 272 (Other Major Cardiovascular Procedures with MCC, CC, without CC/MCC, respectively) in MDC 05 (Diseases and Disorders of the Circulatory System); MS-DRGs 356, 357, and 358 (Other Digestive System O.R. Procedures, with MCC, CC, without CC/MCC, respectively) in MDC 06 (Diseases and Disorders of the Digestive System); MS-DRGs 907, 908, and 909 (Other O.R. Procedures for Injuries with MCC, CC, without CC/MCC, respectively) in MDC 21 (Injuries, Poisonings and Toxic Effects of Drugs); and MS-DRGs 957, 958, and 959 (Other O.R. Procedures for Multiple Significant Trauma with MCC, CC, without CC/MCC, respectively) in MDC 24 (Multiple Significant Trauma).
Comment: Commenters supported the proposal to change the designation of 04L23DZ from a non-O.R. to O.R. procedure. The commenters stated that the proposal was reasonable, given the data and information provided. A commenter noted that this change better reflects the resources required to perform the procedure and better aligns its designation with the designation of other procedures of similar technical difficulty.
A commenter stated that CMS should not consider any requests to modify the designation of procedures as O.R. or non-O.R. for FY 2020. As stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19230), CMS plans to conduct a comprehensive systematic review of the ICD-10-PCS procedure codes. The commenter suggested that reassignment requests should be held until the review has been completed.
Response: We appreciate the commenters' support. We do not agree with the commenter who stated that we should not reassign any procedures as O.R. or non-O.R; rather, while some requests may involve a broader review of additional ranges of ICD-10-PCS codes, such that we believe they are more appropriately considered as part of our comprehensive review of procedure codes, we generally believe it is more accurate to address requests to change the designation of procedures as OR or non-OR as they arise rather than waiting for the comprehensive review, which is a multiyear project. After consideration of the public comments we received, we are finalizing our proposal to change the designation of 04L23DZ from non-O.R. procedure to O.R. procedure, effective October 1, 2019.
(2) Endoscopic Insertion of Endobronchial Valves
As noted in the FY 2020 IPPS/LTCH PPS proposed rule, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41257), we discussed a comment we received in response to the FY 2019 IPPS/LTCH PPS proposed rule regarding eight ICD-10-PCS procedure codes that describe endobronchial valve procedures that the commenter believed should be designated as O.R. procedures. The codes are identified in the following table.

The commenter stated that these procedures are most commonly performed in the O.R., given the need for better monitoring and support through the process of identifying and occluding a prolonged air leak using endobronchial valve technology. The commenter also noted that other endobronchial valve procedures have an O.R. designation. We noted that, in the ICD-10 MS-DRGs Version 35, these eight ICD-10-PCS procedure codes are not recognized as O.R. procedures for purposes of MS-DRG assignment. The commenter requested that these eight procedure codes be assigned to MS-DRG 163 (Major Chest Procedures with MCC) due to similar cost and resource use. As discussed in the FY 2019 IPPS/LTCH PPS final rule, our clinical advisors disagreed with the commenter that the eight identified procedures typically require the use of an operating room, and believed that these procedures would typically be performed in an endoscopy suite. Therefore, we did not finalize a change to the eight procedure codes describing endoscopic insertion of an endobronchial valve listed in the table above for FY 2019 under the ICD-10 MS-DRGs Version 36.
After publication of the FY 2019 IPPS/LTCH PPS final rule, we received feedback from several stakeholders expressing continued concern with the designation of the eight ICD-10-PCS procedure codes describing the endoscopic insertion of an endobronchial valve listed in the table above, including requests to reconsider the designation of these codes for FY 2020. Some requestors stated that while they appreciated CMS' attention to the issue, they believed that important clinical and financial factors had been overlooked. The requestors noted that while the site of care is an important consideration for MS-DRG assignment, there are other clinical factors such as case complexity, patient health risk and the need for anesthesia that also affect hospital resource consumption and should influence MS-DRG assignment. With regard to complexity, the requestors stated that many of these patients are high-risk, often recovering from major lung surgery and have significantly compromised respiratory function. According to one requestor, these patients may have major comorbidities, such as cancer or emphysema contributing to longer lengths of stay in the hospital. This requestor acknowledged that procedures performed for the endoscopic insertion of an endobronchial valve are often, but not always, performed in the O.R., however, the requestor also noted this should not preclude the designation of these procedures as O.R. procedures since there have been other examples of reclassification requests where the combination of factors, such as treatment difficulty, resource utilization, patient health status, and anesthesia administration were considered in the decision to change the designation for a procedure from non-O.R. to O.R. Another requestor stated that CMS' current designation of a procedure involving the endoscopic insertion of an endobronchial valve as a non-O.R. procedure is not reflective of actual practice and this designation has payment consequences that may affect access to the treatment for a vulnerable patient population, with limited treatment options. The requestor recommended that procedures involving the endoscopic insertion of an endobronchial valve should be designated as O.R. procedures and assigned to MS-DRGs 163, 164, and 165 (Major Chest Procedures with MCC, with CC and without CC/MCC, respectively). In addition, a few of the requestors also conducted their own analyses and indicated that if procedures involving the endoscopic insertion of an endobronchial valve were to be assigned to MS-DRGs 163, 164, and 165, the average costs of the cases reporting a procedure code describing the endoscopic insertion of an endobronchial valve would still be higher compared to all the cases in the assigned MS-DRG.
As indicated in the FY 2020 IPPS/LTCH PPS proposed rule, we examined claims data from the September 2018 update of the FY 2018 MedPAR file for MS-DRGs 163, 164 and 165 to identify cases reporting any one of the eight procedure codes listed in the above table describing the endoscopic insertion of an endobronchial valve. We stated that cases reporting one of these procedure codes would be assigned to MS-DRG 163, 164, or 165 if at least one other procedure that is designated as an O.R. procedure and assigned to these MS-DRGs was also reported on the claim. In addition, cases reporting a procedure code describing the endoscopic insertion of an endobronchial valve with a different surgical approach are assigned to MS-DRGs 163, 164, and 165. Our findings are shown in the following table.

We found a total of 10,812 cases in MS-DRG 163 with an average length of stay of 11.6 days and average costs of $33,433. Of those 10,812 cases, we found 49 cases reporting a procedure for the endoscopic insertion of an endobronchial valve with an average length of stay of 21.1 days and average costs of $53,641. For MS-DRG 164, we found a total of 14,800 cases with an average length of stay of 5.6 days and average costs of $18,202. Of those 14,800 cases, we found 23 cases reporting a procedure for the endoscopic insertion of an endobronchial valve with an average length of stay of 14 days and average costs of $37,287. For MS-DRG 165, we found a total of 7,907 cases with an average length of stay of 3.3 days and average costs of $13,408. Of those 7,907 cases, we found 3 cases reporting a procedure for the endoscopic insertion of an endobronchial valve with an average length of stay of 18.3 days and average costs of $39,249.
We also examined claims data to identify any cases reporting any one of the eight procedure codes listed in the table above describing the endoscopic insertion of an endobronchial valve within MS-DRGs 166, 167, and 168 (Other Respiratory System O.R. Procedures with MCC, with CC, and without CC/MCC, respectively). We further stated that cases reporting one of these procedure codes would be assigned to MS-DRG 166, 167, or 168 if at least one other procedure that is designated as an O.R. procedure and assigned to these MS-DRGs was also reported on the claim. In addition, MS-DRGs 166, 167, and 168 are the other surgical MS-DRGs where cases reporting a respiratory diagnosis within MDC 4 would be assigned. Our findings are shown in the following table.

We found a total of 16,050 cases in MS-DRG 166 with an average length of stay of 10.6 days and average costs of $26,645. Of those 16,050 cases, we found 11 cases reporting a procedure for the endoscopic insertion of an endobronchial valve with an average length of stay of 25.7 days and average costs of $71,700. For MS-DRG 167, we found a total of 8,165 cases with an average length of stay of 5.3 days and average costs of $13,687. Of those 8,165 cases, we found 4 cases reporting a procedure for the endoscopic insertion of an endobronchial valve with an average length of stay of 10 days and average costs of $28,847. For MS-DRG 168, we found a total of 2,430 cases with an average length of stay of 2.8 days and average costs of $9,645. Of those 2,430 cases, we indicated that we did not find any cases reporting a procedure for the endoscopic insertion of an endobronchial valve.
The results of our data analysis indicate that cases reporting a procedure for the endoscopic insertion of an endobronchial valve in MS-DRGs 163, 164, 165, 166, and 167 have a longer length of stay and higher average costs when compared to all the cases in their assigned MS-DRG. We stated in the proposed rule that because the data are based on surgical MS-DRGs 163, 164, 165, 166 and 167, and the procedure codes for endoscopic insertion of an endobronchial valve are currently designated as non-O.R. procedures, there was at least one other O.R. procedure reported on the claim resulting in case assignment to one of those MS-DRGs. Our clinical advisors indicated that because there was another O.R. procedure reported, the insertion of the endobronchial valve procedure may or may not have been the main determinant of resource use for those cases. Therefore, we conducted further analysis to evaluate cases for which no other O.R. procedure was performed with the endoscopic insertion of an endobronchial valve and case assignment resulted in a medical MS-DRG. Our findings are shown in the following table.


We further stated in the proposed rule that the data indicate that there is a wide variation in the average length of stay and average costs for cases reporting a procedure for the endoscopic insertion of an endobronchial valve, with volume generally low across MS-DRGs. As shown in the table, for several of the medical MS-DRGs, there was only one case reporting a procedure for the endoscopic insertion of an endobronchial valve. The highest volume of cases reporting a procedure for the endoscopic insertion of an endobronchial valve was found in MS-DRG 199 (Pneumothorax with MCC) with a total of 28 cases with an average length of stay of 16.4 days and average costs of $38,384. The highest average costs and longest average length of stay for cases reporting a procedure for the endoscopic insertion of an endobronchial valve was $67,299 in MS-DRG 207 (Respiratory System Diagnosis with Ventilator Support >96 Hours or Peripheral Extracorporeal Membrane Oxygenation (ECMO)) where 4 cases were found with an average length of stay of 20 days. Overall, there was a total of 91 cases reporting the insertion of an endobronchial valve procedure with an average length of stay of 13.7 days and average costs of $33,377 across the medical MS-DRGs.
Our clinical advisors agreed that the subset of patients who undergo endoscopic insertion of an endobronchial procedure are complex and may have multiple comorbidities such as severe underlying lung disease that impact the hospital length of stay. We stated that they also believe that, as we begin the process of refining how procedure codes may be classified under ICD-10-PCS, including designation of a procedure as O.R. or non-O.R., we should take into consideration whether the procedure is driving resource use for the admission. (We refer the reader to section II.F.13.a. of the preamble of this final rule for the discussion of our plans to conduct a comprehensive review of the ICD-10-PCS procedure codes). Based on the claims data analysis, which show a wide variation in average costs for cases reporting endoscopic insertion of an endobronchial valve without an O.R. procedure, we stated that our clinical advisors are not convinced that endoscopic insertion of an endobronchial valve is a key contributing factor to the consumption of resources as reflected in the data. We stated that they also believe, in review of the procedures that are currently assigned to MS-DRGs 163, 164, 165, 166, 167, and 168, that further refinement of these MS-DRGs may be warranted. For these reasons, we stated in the proposed rule that, at this time, our clinical advisors do not support designating endoscopic insertion of an endobronchial valve as an O.R. procedure, nor do they support assignment of these procedures to MS-DRGs 163, 164, and 165 until additional analyses can be performed for this subset of patients as part of the comprehensive procedure code review.
For the reasons described above and in the proposed rule, we did not propose to change the current non-O.R. designation of the eight ICD-10-PCS procedure codes that describe endoscopic insertion of an endobronchial valve. However, we stated that because we agreed that endoscopic insertion of an endobronchial valve procedures are performed on clinically complex patients, we believe it may be appropriate to consider designating these procedures as non-O.R. affecting specific MS-DRGs for FY 2020. Therefore, we requested public comment on designating these procedure codes as non-O.R. procedures affecting the MS-DRG assignment, including the specific MS-DRGs that cases reporting the endoscopic insertion of an endobronchial valve should affect for FY 2020. As we noted in the proposed rule, it is not clear based on the claims data to what degree the endoscopic insertion of an endobronchial valve is a contributing factor for the consumption of resources for these clinically complex patients and given the potential refinement that may be needed for MS-DRGs 163, 164, 165, 166, 167, and 168, we solicited comment on whether cases reporting the endoscopic insertion of an endobronchial valve should affect any of these MS-DRGs or other MS-DRGs.
Comment: Several commenters disagreed with our proposal to not designate the eight procedure codes describing endoscopic insertion of an endobronchial valve procedure as an O.R. procedure until additional analyses can be performed as part of the comprehensive procedure code review. Commenters urged CMS to include the eight procedure codes discussed above in the GROUPER logic for MS-DRGs 163, 164, and 165 based on the analysis that was presented in the proposed rule effective FY 2020. A commenter noted that the analysis showed that cases in surgical MS-DRGs 163, 164, 165, 166 and 167 reporting the endoscopic insertion of an endobronchial valve had longer length of stays and higher average costs than other cases in those MS-DRGs. The commenter stated that the analysis showed that most cases in the medical MS-DRGs reporting the endoscopic insertion of an endobronchial valve had costs significantly higher than the relative weights of the medical DRGs. This commenter also stated that the skill level required for placement, anesthesia (even if performed outside the O.R.), and the severity level of the patient increase costs beyond that recognized within the medical MS-DRGs. The commenter further stated that because CMS's data supports a higher severity level, higher costs, and longer length of stays for patients who undergo endoscopic insertion of an endobronchial valve, they recommended reclassifying the eight procedure codes to O.R. status effective FY 2020, and grouping to MS-DRGs 163, 164 and 165 within MDC 4, to MS-DRG 853 when sepsis is principal diagnosis, and to MS-DRGs 981, 982, and 983 when there is an unrelated principal diagnosis. The commenter stated their belief that further delay of a relative weight increase for these procedures is not warranted nor supported. Another commenter commended CMS for soliciting comments on whether to consider any of the eight procedure codes describing the endoscopic insertion of an endobronchial valve procedure as non-O.R. impacting the MS-DRG assignment. This commenter recommended assigning all eight procedure codes identifying the endoscopic insertion of an endobronchial valve without another O.R. procedure to MS-DRGs 163, 164, and 165 for clinical coherence. According to the commenter, there are currently no medical MS-DRGs with clinically similar procedures or costs, therefore, assignment to MS-DRGs 163, 164 and 165 would ensure adequate payment to providers for these procedures. This commenter also stated that the costs associated with the endoscopic insertion of an endobronchial valve are a significant contributing factor to the higher average costs and length of stay in comparison to clinically similar cases that do not involve the endoscopic insertion of an endobronchial valve.
Response: We appreciate the commenters' feedback on the designation of the eight procedure codes describing the endoscopic insertion of an endobronchial valve. We agree with the commenter that the analysis in the proposed rule showed that cases reporting a procedure for the endoscopic insertion of an endobronchial valve in MS-DRGs 163, 164, 165, 166, and 167 have a longer length of stay and higher average costs when compared to all the cases in their assigned MS-DRG. As noted above, we stated in the proposed rule that because the data are based on surgical MS-DRGs 163, 164, 165, 166 and 167, there was at least one other O.R. procedure reported on the claim resulting in case assignment to one of those MS-DRGs. We also acknowledge that the analysis in the proposed rule showed that most cases in the medical MS-DRGs reporting the endoscopic insertion of an endobronchial valve demonstrated costs higher than the relative weights of the medical DRGs. While our clinical advisors continue to believe it is unclear (based on the claims data) to what degree the endoscopic insertion of an endobronchial valve is a contributing factor for the consumption of resources for these clinically complex patients, they agree, as noted in the proposed rule, that the subset of patients who undergo endoscopic insertion of an endobronchial procedure are complex and may have multiple comorbidities such as severe underlying lung disease that impact the hospital length of stay. Our clinical advisors also continue to believe that further refinement of surgical MS-DRGs 163, 164, 165, 166 and 167 may be warranted because there are other procedure codes describing the insertion of endobronchial valve procedures by various approaches that are currently assigned to MS-DRGs 163, 164, and 165 and are designated as O.R. procedures, which our clinical advisors believe may require further analysis with respect to utilization of resources and designation as O.R. versus non-O.R. There are also other procedure codes currently assigned to MS-DRGs 163, 164 and 165 that describe procedures being performed on body parts other than those related to the chest. For example, we found codes describing laser interstitial thermal therapy (LITT) of several gastrointestinal body parts that do not appear to be clinically coherent. With regard to MS-DRGs 166 and 167, our clinical advisors believe that these MS-DRGs may require further consideration for potential restructuring in connection with the ongoing evaluation of severity level designations and also as a result of the finalized policy (as discussed in section II.F.3. of the preamble of this final rule) regarding the deletion of several procedure codes that contain the qualifier “bifurcation” which are currently assigned to MS-DRGs 166 and 167 (as well as MS-DRG 168). For these reasons, our clinical advisors believe additional analysis of these surgical MS-DRGs is needed. In response to the commenter who suggested that cases reporting one of the eight procedure codes describing the endoscopic insertion of an endobronchial procedure should group to MS-DRG 853 (Infectious & Parasitic Diseases with O.R. Procedure with MCC) when sepsis is the principal diagnosis, and to MS-DRGs 981, 982, and 983 when there is an unrelated principal diagnosis, we note that, as shown in the proposed rule and above, our analysis of the cases reporting the endoscopic insertion of an endobronchial valve in a medical MS-DRG did not result in any cases being found in MS-DRG 853 and our clinical advisors do not agree with assignment of these procedures to that MS-DRG in the absence of further analysis. We also note that, because our clinical advisors continue to believe that endoscopic insertion of an endobronchial valve should not be designated as an O.R. procedure, they do not support the recommendation for assignment to MS-DRGs 981, 982, and 983 as those MS-DRGs are defined by procedures designated as extensive O.R. procedures. We refer the reader to section II.F.13.a. of the preamble in this final rule, for detailed information on how the designation of each ICD-10-PCS procedure code on a claim impacts the MS-DRG assignment.
In the proposed rule we stated that we agreed that endoscopic insertion of an endobronchial valve procedures are performed on clinically complex patients and that we believed it may be appropriate to consider designating these procedures as non-O.R. affecting specific MS DRGs for FY 2020. Our clinical advisors support the commenters' recommendation for the assignment of cases reporting the endoscopic insertion of an endobronchial valve to MS-DRGs 163, 164, and 165 under the current structure of the ICD-10 MS-DRGs for clinical coherence with the other insertion of endobronchial valve procedures currently assigned to those MS-DRGs and based on the data analysis. Our clinical advisors acknowledge that the data analysis presented in the proposed rule demonstrated that cases reporting a procedure for the endoscopic insertion of an endobronchial valve in MS-DRGs 163, 164, 165, 166, and 167 have a longer length of stay and higher average costs when compared to all the cases in their assigned MS-DRG, however, the average costs and length of stay for those cases are more aligned with MS-DRGs 163, 164 and 165 than MS- DRGs 166, 167, and 168 or any other MS-DRGs within MDC 4 at this time. (As noted in the proposed rule, we did not find any cases reporting a procedure for the insertion of an endobronchial valve in MS-DRG 168).
After consideration of the public comments we received and for the reasons described above, we are finalizing the designation of the eight procedure codes listed earlier in this section that describe the endoscopic insertion of an endobronchial valve as non-O.R. affecting MS-DRGs 163, 164 and 165 (Major Chest Procedures with MCC, with CC and without CC/MCC, respectively) under the ICD-10 MS-DRGs Version 37, effective October 1, 2019.
14. Changes to the MS-DRG Diagnosis Codes for FY 2020
a. Background of the CC List and the CC Exclusions List
Under the IPPS MS-DRG classification system, we have developed a standard list of diagnoses that are considered CCs. Historically, we developed this list using physician panels that classified each diagnosis code based on whether the diagnosis, when present as a secondary condition, would be considered a substantial complication or comorbidity. A substantial complication or comorbidity was defined as a condition that, because of its presence with a specific principal diagnosis, would cause an increase in the length-of-stay by at least 1 day in at least 75 percent of the patients. However, depending on the principal diagnosis of the patient, some diagnoses on the basic list of complications and comorbidities may be excluded if they are closely related to the principal diagnosis. In FY 2008, we evaluated each diagnosis code to determine its impact on resource use and to determine the most appropriate CC subclassification (non-CC, CC, or MCC) assignment. We refer readers to sections II.D.2. and 3. of the preamble of the FY 2008 IPPS final rule with comment period for a discussion of the refinement of CCs in relation to the MS-DRGs we adopted for FY 2008 (72 FR 47152 through 47171).
b. Overview of Comprehensive CC/MCC Analysis
In the FY 2008 IPPS/LTCH PPS final rule (72 FR 47159), we described our process for establishing three different levels of CC severity into which we would subdivide the diagnosis codes. The categorization of diagnoses as an MCC, a CC, or a non-CC was accomplished using an iterative approach in which each diagnosis was evaluated to determine the extent to which its presence as a secondary diagnosis resulted in increased hospital resource use. We refer readers to the FY 2008 IPPS/LTCH PPS final rule (72 FR 47159) for a complete discussion of our approach. Since this comprehensive analysis was completed for FY 2008, we have evaluated diagnosis codes individually when receiving requests to change the severity level of specific diagnosis codes. However, given the transition to ICD-10-CM and the significant changes that have occurred to diagnosis codes since this review, we stated in the proposed rule that we believe it is necessary to conduct a comprehensive analysis once again. We further stated that we had completed this analysis and we were discussing our findings in the proposed rule. We used the same methodology utilized in FY 2008 to conduct this analysis, as described below.
For each secondary diagnosis, we measured the impact in resource use for the following three subsets of patients:
(1) Patients with no other secondary diagnosis or with all other secondary diagnoses that are non-CCs.
(2) Patients with at least one other secondary diagnosis that is a CC but none that is an MCC.
(3) Patients with at least one other secondary diagnosis that is an MCC.
Numerical resource impact values were assigned for each diagnosis as follows:

Each diagnosis for which Medicare data were available was evaluated to determine its impact on resource use and to determine the most appropriate CC subclass (non-CC, CC, or MCC) assignment. In order to make this determination, the average cost for each subset of cases was compared to the expected cost for cases in that subset. The following format was used to evaluate each diagnosis:

Count (Cnt) is the number of patients in each subset and C1, C2, and C3 are a measure of the impact on resource use of patients in each of the subsets. The C1, C2, and C3 values are a measure of the ratio of average costs for patients with these conditions to the expected average cost across all cases. The C1 value reflects a patient with no other secondary diagnosis or with all other secondary diagnoses that are non-CCs. The C2 value reflects a patient with at least one other secondary diagnosis that is a CC but none that is a major CC. The C3 value reflects a patient with at least one other secondary diagnosis that is a major CC. A value close to 1.0 in the C1 field would suggest that the code produces the same expected value as a non-CC diagnosis. That is, average costs for the case are similar to the expected average costs for that subset and the diagnosis is not expected to increase resource usage. A higher value in the C1 (or C2 and C3) field suggests more resource usage is associated with the diagnosis and an increased likelihood that it is more like a CC or major CC than a non-CC. Thus, a value close to 2.0 suggests the condition is more like a CC than a non-CC but not as significant in resource usage as an MCC. A value close to 3.0 suggests the condition is expected to consume resources more similar to an MCC than a CC or non-CC. For example, a C1 value of 1.8 for a secondary diagnosis means that for the subset of patients who have the secondary diagnosis and have either no other secondary diagnosis present, or all the other secondary diagnoses present are non-CCs, the impact on resource use of the secondary diagnoses is greater than the expected value for a non-CC by an amount equal to 80 percent of the difference between the expected value of a CC and a non-CC (that is, the impact on resource use of the secondary diagnosis is closer to a CC than a non-CC).
These mathematical constructs are used as guides in conjunction with the judgment of our clinical advisors to classify each secondary diagnosis reviewed as an MCC, a CC, or a non-CC. Our clinical advisors reviewed the resource use impact reports and suggested modifications to the initial CC subclass assignments when clinically appropriate.
c. Changes to Severity Levels
(1) General
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19235 through 19246), the diagnosis codes for which we proposed a change in severity level designation as a result of the analysis described in that proposed rule were shown in Table 6P.1c. associated with that proposed rule (which is available via the internet on the CMS website at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html). Using the method described above to perform our comprehensive CC/MCC analysis, our clinical advisors recommended a change in the severity level designation for 1,492 ICD-10-CM diagnosis codes. As shown in Table 6P.1c. associated with the FY 2020 IPPS/LTCH PPS proposed rule, the proposed changes to severity level resulting from our comprehensive analysis moved some diagnosis codes to a higher severity level designation and other diagnosis codes to a lower severity level designation, as indicated in the two columns which display CMS' FY 2019 classification in column C and the proposed changes for FY 2020 in column D. We refer readers to the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19235 through 19246) for a complete discussion of our proposals, including a summary of the proposed changes and illustrations of proposed severity level changes.
We invited public comments on our proposed severity level designations for the diagnosis codes as shown in Table 6P.1c associated with the proposed rule. We received many comments on the proposals, with the majority of commenters requesting that the adoption of the proposed changes be delayed in order to provide additional time to evaluate given the broad scope of the proposed changes. As discussed in more detail below, after consideration of the public comments we received, we are generally not finalizing our proposed changes to the severity level designations for the ICD-10-CM diagnosis codes as shown in Table 6P.1c associated with the proposed rule, with the exception of the proposed changes to the codes related to antimicrobial resistance as discussed in greater detail below. Below we provide a summary of the comments we received and our response.
Comment: Commenters expressed support for a limited number of the proposed changes in severity level, including the proposed change in severity level designation for diagnosis codes E83.39 (Other disorders of phosphorus metabolism), E83.51 (Hypocalcemia), R62.7 (Adult failure to thrive), R63.3 (Feeding difficulties), Z16.12 (Extended spectrum beta lactamase (ESBL) resistance), Z16.21 (Resistance to vancomycin), Z16.24 (Resistance to multiple antibiotics), and Z16.39 (Resistance to other specified antimicrobial drug) from a non-CC to a CC. Commenters stated their belief that these proposals were reasonable and reflect the resource utilization for these diagnoses.
However, many commenters expressed concern with the proposed severity level designation changes overall and recommended CMS conduct further analysis prior to finalizing any proposals. Specifically, commenters expressed concern that the extensive changes proposed to the severity level designations for the ICD-10-CM diagnosis codes as shown in Table 6P.1c, the majority of which would be a lower severity level (for example, CC to a non-CC), would no longer appropriately reflect resource use for patient care and could have a significant unintended or improper adverse financial impact. In addition, some commenters believed there was not sufficient time to review the nearly 1,500 diagnosis codes for which a change to the severity designation was proposed, noting that CMS engaged in its analysis for over a year before making any comprehensive proposals, and because there have been significant changes that have occurred to diagnosis codes since the transition to ICD-10-CM, in particular the exponential increase in the number of codes. Other general themes reflected in the comments included desire for more transparency and stakeholder engagement, the belief that clinical severity was not consistently reflected in the proposed severity level designations, and concern regarding the impact on Medicaid and private payers, stating such payers often base their payment amount on Medicare.
Some commenters stated that the information provided was not sufficient to adequately explain the proposed changes in severity level designations for certain diagnosis codes or families of codes. Other commenters were concerned that CMS' stated criteria were not met for some of the proposed changes to severity designations and specifically noted instances where diagnoses that appear to be clinically less severe (and therefore require less resources) were proposed to be assigned a higher severity level designation than other diagnoses that they believe require more resources. Another commenter recommended that any changes be phased in to allow time to assess the impacts such modifications would have on hospitals and patients.
Response: We thank commenters for their comments on our proposed changes. After consideration of the public comments we received, and for the reasons discussed below, we agree it would be premature to adopt broad changes to the severity designations at this time. We agree with commenters that there have been significant changes to the scope and complexity of diagnosis codes since the transition to ICD-10-CM. We also believe that at this time it would be prudent to further examine the proposed severity designations to ensure they would appropriately reflect resource use based on review of the data as well as consideration of relevant clinical factors (for example, the clinical nature of each of the secondary diagnoses and the severity level of clinically similar diagnoses, as explained above) and improve the overall accuracy of the IPPS payments. Postponing the adoption of comprehensive changes in severity level designations will allow us to incorporate review of additional ICD-10 claims data as it becomes available and to fully consider the technical feedback provided from the public on the proposed rule. This would also allow further opportunity to provide additional background to the public on the methodology utilized and clinical rationale applied across diagnostic categories to assist the public in its review, such as making a test GROUPER publicly available to allow for impact testing. In addition, we can consider further whether it is appropriate to propose to make such comprehensive changes all at once or in phases, as suggested by some commenters.
Furthermore, this will afford an opportunity for us to explore additional means of eliciting feedback on the current severity level designations after the final rule and prior to the November 1, 2019 deadline for MS-DRG requests, comments and suggestions for FY 2021, such as holding an open door forum to solicit additional feedback. When providing additional feedback or comments, we encourage the public to provide a detailed explanation of why a specific severity level designation for a diagnosis code would ensure that designation appropriately reflects resource use. We also invite feedback regarding other possible ways we can approach the implementation of our proposed comprehensive changes to severity level designations, such as a phased-in approach or changes by specific code categories or MDCs. In summary, for the reasons discussed above, we are generally not finalizing our proposed changes to the severity designations for the ICD-10-CM diagnosis codes as shown in Table 6P.1c associated with the proposed rule, other than the changes to the severity level designations for the diagnosis codes in category Z16- (Resistance to antimicrobial drugs) from a non-CC to a CC, as discussed in more detail below.
Comment: As noted above, we received comments supporting our proposed change in severity level designation for diagnosis codes related to antimicrobial resistance (that is, Z16.12 (Extended spectrum beta lactamase (ESBL) resistance), Z16.21 (Resistance to vancomycin), Z16.24 (Resistance to multiple antibiotics), and Z16.39 (Resistance to other specified antimicrobial drug) from a non-CC to a CC. These commenters stated that they agree that patients with an ICD-10-CM secondary diagnosis code indicating that they were treated for an infection resistant to antibiotics should be, at a minimum, assigned a CC severity level designation. They asserted that the resources required to treat patients suffering from antimicrobial resistant infections should warrant a higher severity designation, and indicated that caring for patients with these complications is more resource intensive, including the need for stronger, different, or extra antibiotics. Commenters further indicated that the higher resources required to treat patients suffering from antimicrobial resistant infections are particularly relevant with respect to Medicare beneficiaries because they are vulnerable to drug-resistant infections due to greater exposure to resistant bacteria (e.g., via catheter infection or from other chronic diseases). These commenters expressed significant concerns related to the public health crisis represented by antimicrobial resistance and urged CMS to also apply the change in the severity level designation from non-CC to CC to the other ICD 10-CM diagnosis codes specifying antimicrobial drug resistance. A few of these commenters made recommendations for certain ICD-10-CM diagnosis codes that specify antimicrobial drug resistance either in addition to or in lieu of the codes included in our proposal. However, many of these commenters recommended that we also apply the change in the severity level designation from non-CC to CC to the other ICD-10-CM diagnosis codes specifying antimicrobial drug resistance (that is, the other diagnosis codes in category Z16-(Resistance to antimicrobial drugs).
Response: We understand the concerns expressed by commenters related to the public health crisis that antimicrobial resistance represents. Addressing these concerns is consistent with the Administration's key priorities, and we have taken into consideration their statements that it clinically requires greater resources to treat patients suffering from antimicrobial resistant infections. For example, antimicrobial resistance results in a substantial number of additional hospital days for Medicare beneficiaries (estimated to be more than 600,000 additional days in the hospital each year), resulting in additional costs and resources to care for these patients.[1] For these reasons, while we are continuing to examine the implementation of broader comprehensive changes to the CC/MCC designations, we believe it is appropriate to finalize the change in the severity level designations from non-CC to CC for the ICD-10-CM diagnosis codes specifying antimicrobial drug resistance. We also agree with the commenters that the change in severity level designation should also apply to the other ICD-10-CM diagnosis codes that specify antimicrobial drug resistance. We believe this would be consistent with our proposal because these codes, which identify the resistance and non-responsiveness of a condition to antimicrobial drugs, are in the same family of codes (Z16) as the previously listed diagnosis codes related to antimicrobial resistance (that is, Z16.12, Z16.21, Z16.24, and Z16.39). Therefore, we are finalizing a change to the severity level designation for all of the codes in category Z16- (Resistance to antimicrobial drugs), which are listed below, from a non-CC to a CC designation.
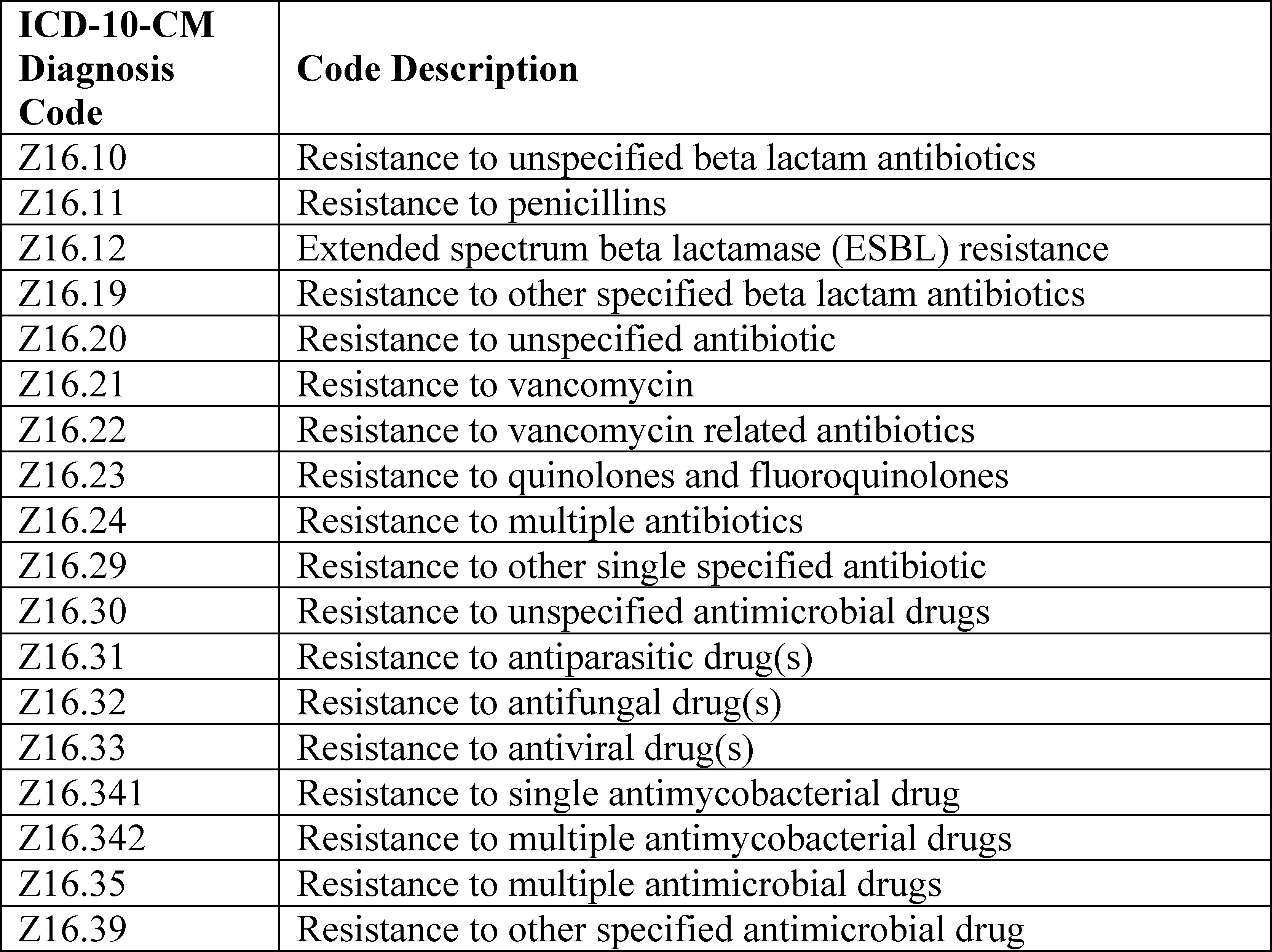
(We refer readers to sections II.H.8. and II.H.9. of the preamble of this final rule for a discussion of new technology add-on payment policies related to antimicrobial resistance.)
d. Requested Changes to Severity Levels
In the FY 2020 IPPS/LTCH PPS proposed rule (19246 through 19250) we discussed the external requests we received to make changes for the severity level designations of diagnosis codes in seven specific groups which included (1) Acute Right Heart Failure, (2) Chronic Right Heart Failure, (3) Ascites in Alcoholic Liver Disease and Toxic Liver Disease, (4) Factitious Disorder Imposed on Self, (5) Nonunion and Malunion of Physeal Metatarsal Fractures, (6) Other Encephalopathy, and (7) Obstetrics Chapter Codes. As these requests were external requests we discussed them separately from the comprehensive CC/MCC analysis, however, we utilized the same approach and methodology, consistent with our annual process of reviewing requested changes to severity levels. We note that, for the seven groups of external requests we received, we did not propose any changes to the severity levels of the diagnosis codes based on the results of our data analysis and the input of our clinical advisors, with the exception of group (7) Obstetrics Chapter Codes. We also note that we solicited comments on, but did not specifically propose changes for, the diagnosis codes discussed from group (1) Acute Right Heart Failure.
Some commenters disagreed with our decision not to propose changes in the severity level designation for certain groups of codes, for example the acute right heart failure and ascites codes, and recommended that we finalize changes to the severity levels, stating that the resources required are similar to the existing codes. Other commenters specifically recommended that we postpone any decisions related to the obstetrics chapter codes and work with a panel of provider stakeholders. As we indicated in the proposed rule, given the limited number of cases reporting ICD-10-CM obstetrical codes in the Medicare claims data, we are considering use of datasets other than MedPAR cost data for future evaluation of severity level designation for the ICD-10-CM diagnosis codes from the Obstetrics chapter of the ICD-10-CM classification.
As discussed above, after consideration of the public comments received, we are generally not finalizing our proposed changes to the severity level designations for the ICD-10-CM diagnosis codes that were reviewed as part of the comprehensive CC/MCC analysis and shown in Table 6P.1c associated with the proposed rule. Similarly, we are not finalizing any proposed changes to the obstetric chapter diagnosis codes for FY 2020, to allow for further consideration of these codes as part of our comprehensive analysis as well as further consideration of the use of additional data sets for these particular codes, given the limited number of cases reported in the Medicare claims data. We are also finalizing our proposals to maintain the current severity level designations for the remaining six groups of diagnosis codes listed above for FY 2020. We will continue to consider the public comments received on the external requests for changes to severity level designations as we review and consider the public comments on our comprehensive CC/MCC analysis.
e. Additions and Deletions to the Diagnosis Code Severity Levels for FY 2020
The following tables identify the additions and deletions to the diagnosis code MCC severity levels list and the additions and deletions to the diagnosis code CC severity levels list for FY 2020 and are available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
Table 6I.1—Additions to the MCC List—FY 2020;
Table 6I.2—Deletions to the MCC List—FY 2020;
Table 6J.1—Additions to the CC List—FY 2020; and
Table 6J.2—Deletions to the CC List—FY 2020.
f. CC Exclusions List for FY 2020
In the September 1, 1987 final notice (52 FR 33143) concerning changes to the DRG classification system, we modified the GROUPER logic so that certain diagnoses included on the standard list of CCs would not be considered valid CCs in combination with a particular principal diagnosis. We created the CC Exclusions List for the following reasons: (1) To preclude coding of CCs for closely related conditions; (2) to preclude duplicative or inconsistent coding from being treated as CCs; and (3) to ensure that cases are appropriately classified between the complicated and uncomplicated DRGs in a pair.
In the May 19, 1987 proposed notice (52 FR 18877) and the September 1, 1987 final notice (52 FR 33154), we explained that the excluded secondary diagnoses were established using the following five principles:
- Chronic and acute manifestations of the same condition should not be considered CCs for one another;
- Specific and nonspecific (that is, not otherwise specified (NOS)) diagnosis codes for the same condition should not be considered CCs for one another;
- Codes for the same condition that cannot coexist, such as partial/total, unilateral/bilateral, obstructed/unobstructed, and benign/malignant, should not be considered CCs for one another;
- Codes for the same condition in anatomically proximal sites should not be considered CCs for one another; and
- Closely related conditions should not be considered CCs for one another.
The creation of the CC Exclusions List was a major project involving hundreds of codes. We have continued to review the remaining CCs to identify additional exclusions and to remove diagnoses from the master list that have been shown not to meet the definition of a CC. We refer readers to the FY 2014 IPPS/LTCH PPS final rule (78 FR 50541 through 50544) for detailed information regarding revisions that were made to the CC and CC Exclusion Lists under the ICD-9-CM MS-DRGs.
The ICD-10 MS-DRGs Version 36 CC Exclusion List is included as Appendix C in the ICD-10 MS-DRG Definitions Manual, which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html, and includes two lists identified as Part 1 and Part 2. Part 1 is the list of all diagnosis codes that are defined as a CC or MCC when reported as a secondary diagnosis. If the code designated as a CC or MCC is allowed with all principal diagnoses, the phrase “NoExcl” (for no exclusions) follows the CC or MCC designation. For example, ICD-10-CM diagnosis code A17.83 (Tuberculous neuritis) has this “NoExcl” entry. For all other diagnosis codes on the list, a link is provided to a collection of diagnosis codes which, when used as the principal diagnosis, would cause the CC or MCC diagnosis to be considered as a non-CC. Part 2 is the list of diagnosis codes designated as a MCC only for patients discharged alive; otherwise, they are assigned as a non-CC. After publication of the proposed rule, we found inconsistencies in the assignment of this “NoExcl” entry to the diagnoses designated as a CC or MCC. Generally, each CC or MCC diagnosis excludes itself from acting as a CC or MCC diagnosis, however, there are approximately 229 diagnosis codes we identified in Appendix C that have the phrase “NoExcl” and should instead contain a link to exclude themselves from acting as a CC or MCC. Therefore, we have corrected the list of diagnosis codes for the ICD-10 MS-DRG Definitions Manual Version 37, Appendix C—Complications or Comorbidities Exclusion List by providing a link to a collection of diagnosis codes which, when used as the principal diagnosis, will cause the CC or MCC to be considered as only a non-CC, for each of the 229 diagnosis codes identified. We have also removed the sentence that states, “If the CC or MCC is allowed with all principal diagnoses, then the phrase NoExcl follows the CC/MCC indicator” as there are no longer any entries for which this phrase applies. We note that these corrections to Appendix C do not represent a change in MS-DRG assignment (or IPPS payment) and are being made to conform the appendix and tables to current policy. We also note these corrections are reflected for Table 6K.—Complete List of CC Exclusions—FY 2020.
In the FY 2020 IPPS/LTCH PPS proposed rule, for FY 2020, we proposed changes to the ICD-10 MS-DRGs Version 37 CC Exclusion List. Therefore, we developed Table 6G.1.—Proposed Secondary Diagnosis Order Additions to the CC Exclusions List—FY 2020; Table 6G.2.—Proposed Principal Diagnosis Order Additions to the CC Exclusions List—FY 2020; Table 6H.1.—Proposed Secondary Diagnosis Order Deletions to the CC Exclusions List—FY 2020; and Table 6H.2.—Proposed Principal Diagnosis Order Deletions to the CC Exclusions List—FY 2020. For Table 6G.1, each secondary diagnosis code proposed for addition to the CC Exclusion List is shown with an asterisk and the principal diagnoses proposed to exclude the secondary diagnosis code are provided in the indented column immediately following it. For Table 6G.2, each of the principal diagnosis codes for which there is a CC exclusion is shown with an asterisk and the conditions proposed for addition to the CC Exclusion List that will not count as a CC are provided in an indented column immediately following the affected principal diagnosis. For Table 6H.1, each secondary diagnosis code proposed for deletion from the CC Exclusion List is shown with an asterisk followed by the principal diagnosis codes that currently exclude it. For Table 6H.2, each of the principal diagnosis codes is shown with an asterisk and the proposed deletions to the CC Exclusions List are provided in an indented column immediately following the affected principal diagnosis. Tables 6G.1., 6G.2., 6H.1., and 6H.2. associated with the proposed rule are available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
The proposed CC Exclusions for a subset of the diagnosis codes as set forth in Tables 6G.1, 6G.2, 6H.1 and 6H.2 associated with the FY 2020 IPPS/LTCH PPS proposed rule reflected the proposed severity level designations as discussed in section II.F.14.c.1. of the preamble of the proposed rule which were based on our comprehensive CC/MCC analysis. As discussed in section II.F.14.c.1. of the preamble of this final rule, we are not finalizing the proposed changes to the severity level designations after consideration of the public comments received (with the exception of the specified ICD-10-CM diagnosis codes in category Z16-Resistance to antimicrobial drugs). Therefore, the finalized CC Exclusions List as displayed in Tables 6G.1, 6G.2, 6H.1, 6H.2. and 6K. associated with this final rule reflect the severity levels under Version 36 of the ICD-10 MS-DRGs for a subset of the diagnosis codes.
15. Changes to the ICD-10-CM and ICD-10-PCS Coding Systems
To identify new, revised and deleted diagnosis and procedure codes, for FY 2020, we have developed Table 6A.—New Diagnosis Codes, Table 6B.—New Procedure Codes, Table 6C.—Invalid Diagnosis Codes, Table 6D.—Invalid Procedure Codes, Table 6E.—Revised Diagnosis Code Titles, and Table 6F.—Revised Procedure Code Titles for this final rule.
These tables are not published in the Addendum to the proposed rule or final rule, but are available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html as described in section VI. of the Addendum to this final rule. As discussed in section II.F.18. of the preamble of this final rule, the code titles are adopted as part of the ICD-10 (previously ICD-9-CM) Coordination and Maintenance Committee process. Therefore, although we publish the code titles in the IPPS proposed and final rules, they are not subject to comment in the proposed or final rules.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19250) we proposed the MDC and MS-DRG assignments for the new diagnosis codes and procedure codes as set forth in Table 6A.—New Diagnosis Codes and Table 6B.—New Procedure Codes. We also stated that the proposed severity level designations for the new diagnosis codes were set forth in Table 6A. and the proposed O.R. status for the new procedure codes were set forth in Table 6B.
Comment: A commenter expressed support for the proposed MS-DRG assignments under MDC 5 (Diseases and Disorders of the Circulatory System) for new procedure codes describing the insertion, removal, and revision of subcutaneous defibrillator leads via open and percutaneous approaches as reflected in Table 6B.—New Procedure Codes, that was associated with the proposed rule. However, the commenter stated it was not clear why MS-DRGs 040 (Peripheral, Cranial Nerve and Other Nervous System Procedures with MCC), 041 (Peripheral, Cranial Nerve and Other Nervous System Procedures with CC or Peripheral Neurostimulator), and 042 (Peripheral, Cranial Nerve and Other Nervous System Procedures without CC/MCC) under MDC 1 (Diseases and Disorders of the Nervous System) were also proposed as MS-DRG assignments for the procedures describing removal and revision of subcutaneous defibrillator lead. The commenter requested that CMS provide information in the FY 2020 IPPS/LTCH PPS final rule regarding those proposed MS-DRG assignments, including the diagnosis and procedure codes that would result in assignment to those MS-DRGs. The commenter provided the following table to display the proposed MS-DRG assignments as reflected in Table 6B- New Procedure Codes that was associated with the proposed rule.

Response: We thank the commenter for their support. With regard to why MS-DRGs 040, 041, and 042 under MDC 1 were also proposed as MS-DRG assignments for the procedures describing removal and revision of subcutaneous defibrillator lead, we note that, as described in section II.F.2.a. of the preamble of this final rule, consistent with our annual process of assigning new procedure codes to MDCs and MS-DRGs, and designating a procedure as an O.R. or non-O.R. procedure, we reviewed the predecessor procedure code assignment. The predecessor procedure codes for the above listed removal and revision of subcutaneous defibrillator lead procedure codes are procedure codes 0JPT0PZ (Removal of cardiac rhythm related device from trunk subcutaneous tissue and fascia, open approach), 0JPT3PZ (Removal of cardiac rhythm related device from trunk subcutaneous tissue and fascia, percutaneous approach), 0JWT0PZ (Revision of cardiac rhythm related device in trunk subcutaneous tissue and fascia, open approach) and 0JWT3PZ (Revision of cardiac rhythm related device in trunk subcutaneous tissue and fascia, percutaneous approach) which are currently assigned to MS-DRGs 040, 041, and 042 under MDC 1. We also note that, in each MDC there is usually a medical and a surgical class referred to as “other medical diseases” and “other surgical procedures,” respectively. The “other” medical and surgical classes are not as precisely defined from a clinical perspective. The other classes would include diagnoses or procedures which were infrequently encountered or not well defined clinically. The “other” surgical category contains surgical procedures which, while infrequent, could still reasonably be expected to be performed for a patient in the particular MDC. Within MDC 1, MS-DRGs 040, 041, and 042 are defined as a set of the “other” surgical classes as indicated in their MS-DRG titles with the “Other Nervous System Procedures” terminology. With regard to the diagnosis codes, we note that the diagnoses in each MDC correspond to a single organ system or etiology and in general are associated with a particular medical specialty. As such, the diagnoses assigned to MDC 1 correspond to the central nervous system. While we agree that it would be rare for a diagnosis related to a disease or disorder of the nervous system to be reported with a procedure that involves the removal or revision of a subcutaneous defibrillator lead, we note that, as discussed and displayed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41184), cases with procedure codes that identify the insertion of a cardiac rhythm related device (the predecessor code for insertion of subcutaneous defibrillator lead procedures) were previously assigned to MS-DRGs 040, 041, and 042 and a small number of cases were found to be reported in those MS-DRGs, thus indicating that the combination of a diagnosis code from MDC 1 and one of the procedures describing the insertion of a cardiac rhythm related device did occur. While we did not specifically conduct analysis of claims data for the procedures describing a removal or revision of a cardiac rhythm related device, our clinical advisors continue to support assignment of the new procedure codes describing removal and revision of subcutaneous defibrillator lead procedures to MS-DRGs 040, 041, and 042 as reflected in Table 6B. New Procedure Codes, associated with this final rule.
Additionally, as discussed in section II.F.2.a. of the preamble of this final rule, in our discussion of the annual process for assigning new procedure codes to MS-DRGs, a similar process is also utilized for assigning new diagnosis codes to MS-DRGs that involves review of the predecessor diagnosis code's MDC and MS-DRG assignment and severity level designation. However, this process does not automatically result in the new diagnosis code being assigned (or proposed for assignment) to the same severity level and/or MS-DRG and MDC as the predecessor code. There are several factors to consider during this process that our clinical advisors take into account.
The proposed severity level designations for a subset of the new diagnosis codes as set forth in Table 6A associated with the FY 2020 IPPS/LTCH PPS proposed rule reflected the proposed severity level designations as discussed in section II.F.14.c.1. of the preamble of the proposed rule which were based on our comprehensive CC/MCC analysis. For example, new diagnosis codes in the category L89- series describing pressure-induced deep tissue damage of various anatomical sites were proposed to be designated at a CC severity level. However, as discussed in section II.F.14.c.1. of the preamble of this final rule, we are not finalizing the proposed changes to the severity level designations based on our comprehensive CC/MCC analysis after consideration of the public comments received (with the exception of the specified ICD-10-CM diagnosis codes in category Z16-Resistance to antimicrobial drugs). Therefore, consistent with our annual process for assigning new diagnosis codes to MDCs and MS-DRGs and designating a new diagnosis code as an MCC, a CC or a non-CC, we reviewed the predecessor code MDC and MS-DRG assignments and the severity level designations for for these new codes and determined the appropriate severity level designation for these codes is the same severity level as the predecessor code under Version 36 of the ICD-10 MS-DRGs. The finalized severity level designations for these new diagnosis codes as set forth in Table 6A associated with this final rule therefore reflect the same severity level as the predecessor code under Version 36 of the ICD-10 MS-DRGs.
We also note that after publication of the proposed rule we identified procedures identified by procedure codes beginning with the prefix 0D1 describing bypass procedures of the small and large intestines in Table 6B.—New Procedure Codes that were inadvertently proposed for assignment to MS-DRGs 829 and 830 (Myeloproliferative Disorders Or Poorly Differentiated Neoplasms with Other Procedure with CC/MCC and without CC/MCC, respectively). Assignment of these procedures to MS-DRGs 829 and 830 is not applicable because the procedures would not result in assignment to these MS-DRGs due to the logic of the surgical hierarchy. Therefore, we have removed MS-DRGs 829 and 830 from the list of MS-DRGs to which these bypass procedures of the small and large intestine are assigned for FY 2020 as reflected in Table 6B.—New Procedure Codes associated with this final rule.
We are finalizing the MDC and MS-DRG assignments for the new diagnosis and procedure codes as set forth in Table 6A.—New Diagnosis Codes and Table 6B.—New Procedure Codes. In addition, the finalized O.R. status for the new procedure codes are set forth in Table 6B. We are making available on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html the following tables associated with this final rule:
- Table 6A.—New Diagnosis Codes-FY 2020;
- Table 6B.—New Procedure Codes-FY 2020;
- Table 6C.—Invalid Diagnosis Codes-FY 2020;
- Table 6D.—Invalid Procedure Codes-FY 2020;
- Table 6E.—Revised Diagnosis Code Titles-FY 2020;
- Table 6F.—Revised Procedure Code Titles-FY 2020;
- Table 6G.1.—Secondary Diagnosis Order Additions to the CC Exclusions List-FY 2020;
- Table 6G.2.—Principal Diagnosis Order Additions to the CC Exclusions List-FY 2020;
- Table 6H.1.—Secondary Diagnosis Order Deletions to the CC Exclusions List-FY 2020;
- Table 6H.2.—Principal Diagnosis Order Deletions to the CC Exclusions List-FY 2020;
- Table 6I.—Complete MCC List-FY 2020;
- Table 6I.1.—Additions to the MCC List-FY 2020;
- Table 6I.2.-Deletions to the MCC List-FY 2020;
- Table 6J.—Complete CC List-FY 2020;
- Table 6J.1.—Additions to the CC List-FY 2020;
- Table 6J.2.—Deletions to the CC List-FY 2020; and
- Table 6K.—Complete List of CC Exclusions-FY 2020
16. Changes to the Medicare Code Editor (MCE)
The Medicare Code Editor (MCE) is a software program that detects and reports errors in the coding of Medicare claims data. Patient diagnoses, procedure(s), and demographic information are entered into the Medicare claims processing systems and are subjected to a series of automated screens. The MCE screens are designed to identify cases that require further review before classification into an MS-DRG.
As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41220), we made available the FY 2019 ICD-10 MCE Version 36 manual file. The link to this MCE manual file, along with the link to the mainframe and computer software for the MCE Version 36 (and ICD-10 MS-DRGs) are posted on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html.
In the FY 2020 IPPS/LTCH PPS proposed rule, we addressed the MCE requests we received by the November 1, 2018 deadline. We also discussed the proposals we were making based on internal review and analysis. In this FY 2020 IPPS/LTCH PPS final rule, we present a summation of the comments we received in response to the MCE requests and proposals presented based on internal reviews and analyses in the proposed rule, our responses to those comments, and our finalized policies.
In addition, as a result of new and modified code updates approved after the annual spring ICD-10 Coordination and Maintenance Committee meeting, we routinely make changes to the MCE. In the past, in both the IPPS proposed and final rules, we have only provided the list of changes to the MCE that were brought to our attention after the prior year's final rule. We historically have not listed the changes we have made to the MCE as a result of the new and modified codes approved after the annual spring ICD-10 Coordination and Maintenance Committee meeting. These changes are approved too late in the rulemaking schedule for inclusion in the proposed rule. Furthermore, although our MCE policies have been described in our proposed and final rules, we have not provided the detail of each new or modified diagnosis and procedure code edit in the final rule. However, we make available the finalized Definitions of Medicare Code Edits (MCE) file. Therefore, we are making available the FY 2020 ICD-10 MCE Version 37 Manual file, along with the link to the mainframe and computer software for the MCE Version 37 (and ICD-10 MS-DRGs), on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/MS-DRG-Classifications-and-Software.html.
a. Age Conflict Edit: Maternity Diagnoses
In the MCE, the Age conflict edit exists to detect inconsistencies between a patient's age and any diagnosis on the patient's record; for example, a 5-year-old patient with benign prostatic hypertrophy or a 78-year-old patient coded with a delivery. In these cases, the diagnosis is clinically and virtually impossible for a patient of the stated age. Therefore, either the diagnosis or the age is presumed to be incorrect. Currently, in the MCE, the following four age diagnosis categories appear under the Age conflict edit and are listed in the manual and written in the software program:
- Perinatal/Newborn—Age of 0 years only; a subset of diagnoses which will only occur during the perinatal or newborn period of age 0 (for example, tetanus neonatorum, health examination for newborn under 8 days old).
- Pediatric—Age is 0-17 years inclusive (for example, Reye's syndrome, routine child health exam).
- Maternity—Age range is 12-55 years inclusive (for example, diabetes in pregnancy, antepartum pulmonary complication).
- Adult—Age range is 15-124 years inclusive (for example, senile delirium, mature cataract).
Under the ICD-10 MCE, the maternity diagnoses category for the Age conflict edit considers the age range of 12 to 55 years inclusive. For that reason, the diagnosis codes on this Age conflict edit list would be expected to apply to conditions or disorders specific to that age group only.
We stated in the proposed rule that we received a request to reconsider the age range associated with the maternity diagnoses category for the Age conflict edit. According to the requestor, pregnancies can and do occur prior to age 12 and after age 55. The requestor suggested that a more appropriate age range would be from age 9 to age 64 for the maternity diagnoses category.
We agreed with the requestor that pregnancies can and do occur prior to the age of 12 and after the age of 55. We further stated in the proposed rule that we also agreed that the suggested range, age 9 to age 64, is an appropriate age range. Therefore, we proposed to revise the maternity diagnoses category for the Age conflict edit to consider the new age range of 9 to 64 years inclusive.
Comment: Commenters agreed with CMS' proposal to revise the maternity diagnoses category for the Age conflict edit by expanding the age range.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to revise the maternity diagnoses category for the Age conflict edit to consider the new age range of 9 to 64 years inclusive under the ICD-10 MCE Version 37, effective October 1, 2019.
b. Sex Conflict Edit: Diagnoses for Females Only Edit
In the MCE, the Sex conflict edit detects inconsistencies between a patient's sex and any diagnosis or procedure on the patient's record; for example, a male patient with cervical cancer (diagnosis) or a female patient with a prostatectomy (procedure). In both instances, the indicated diagnosis or the procedure conflicts with the stated sex of the patient. Therefore, the patient's diagnosis, procedure, or sex is presumed to be incorrect.
As discussed in section II.F.15. of the preamble of this final rule, Table 6A.—New Diagnosis Codes which is associated with this final rule (and is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) lists the new diagnosis codes that have been approved to date which will be effective with discharges on and after October 1, 2019. We stated in the proposed rule that ICD-10-CM diagnosis code N99.85 (Post endometrial ablation syndrome) is a new code that describes a condition consistent with the female sex. We proposed to add this diagnosis code to the Diagnoses for Females Only edit code list under the Sex conflict edit.
Comment: Commenters agreed with the proposal to add diagnosis code N99.85 to the Diagnoses for Females Only edit code list under the Sex conflict edit.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add diagnosis code N99.85 (Post endometrial ablation syndrome) to the Diagnoses for Females Only edit code list under the Sex conflict edit under the ICD-10 MCE Version 37, effective October 1, 2019.
c. Unacceptable Principal Diagnosis Edit
In the MCE, there are select codes that describe a circumstance that influences an individual's health status but does not actually describe a current illness or injury. There also are codes that are not specific manifestations but may be due to an underlying cause. These codes are considered unacceptable as a principal diagnosis. In limited situations, there are a few codes on the MCE Unacceptable Principal Diagnosis edit code list that are considered “acceptable” when a specified secondary diagnosis is also coded and reported on the claim.
In the proposed rule we stated that ICD-10-CM diagnosis codes I46.2 (Cardiac arrest due to underlying cardiac condition) and I46.8 (Cardiac arrest due to other underlying condition) are codes that clearly specify cardiac arrest as being due to an underlying condition. Also, in the ICD-10-CM Tabular List, there are instructional notes to “Code first underlying cardiac condition” at ICD-10-CM diagnosis code I46.2 and to “Code first underlying condition” at ICD-10-CM diagnosis code I46.8. Therefore, we proposed to add ICD-10-CM diagnosis codes I46.2 and I46.8 to the Unacceptable Principal Diagnosis Category edit code list.
As discussed in section II.F.15. of the preamble of this final rule, Table 6A.—New Diagnosis Codes associated with this final rule (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) lists the new diagnosis codes that have been approved to date that will be effective with discharges occurring on and after October 1, 2019.
As indicated in the proposed rule, we proposed to add the new ICD-10-CM diagnosis codes listed in the following table to the Unacceptable Principal Diagnosis Category edit code list, as these codes are consistent with other ICD-10-CM diagnosis codes currently included on the Unacceptable Principal Diagnosis Category edit code list.

Comment: Commenters agreed with our proposal to add diagnosis codes I46.2 and I46.8, as well as the new ICD-10-CM diagnosis codes listed in the table above, to the Unacceptable Principal Diagnosis Category edit code list.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to add diagnosis codes I46.2 and I46.8 to the Unacceptable Principal Diagnosis Category edit code list. We are also finalizing our proposal to add the new ICD-10-CM diagnosis codes previously listed in the table to the Unacceptable Principal Diagnosis Category edit code list under the ICD-10 MCE Version 37, effective October 1, 2019.
d. Non-Covered Procedure Edit
In the MCE, the Non-Covered Procedure edit identifies procedures for which Medicare does not provide payment. Payment is not provided due to specific criteria that are established in the National Coverage Determination (NCD) process. We refer readers to the website at: https://www.cms.gov/Medicare/Coverage/DeterminationProcess/howtorequestanNCD.html for additional information on this process. In addition, there are procedures that would normally not be paid by Medicare but, due to the presence of certain diagnoses, are paid.
As discussed in section II.F.15. of the preamble of this final rule, Table 6D.—Invalid Procedure Codes associated with this final rule (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) lists the procedure codes that are no longer effective as of October 1, 2019. Included in this table are the following ICD-10-PCS procedure codes listed on the Non-Covered Procedure edit code list.

In the proposed rule, we proposed to remove these codes from the Non-Covered Procedure edit code list.
In addition, as discussed in section II.F.2.b. of the preamble of the proposed rule, a number of ICD-10-PCS procedure codes describing bone marrow transplant procedures were the subject of a proposal discussed at the March 5-6, 2019 ICD-10 Coordination and Maintenance Committee meeting, to be deleted effective October 1, 2019. We proposed that if the applicable proposal is finalized, we would delete the subset of those ICD-10-PCS procedure codes that are currently listed on the Non-Covered Procedure edit code list as shown in the following table.

Comment: Commenters agreed with our proposal to remove the ICD-10-PCS procedure codes previously listed in the tables from the Non-Covered Procedure edit code list.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal to remove the ICD-10-PCS procedure codes previously listed in the tables that are no longer valid from the Non-Covered Procedure edit code list within the ICD-10 MCE Version 37 effective October 1, 2019. We note that the proposal involving ICD-10-PCS procedure codes describing bone marrow transplant procedures was finalized after the March 5-6, 2019 ICD-10 Coordination and Maintenance Committee meeting, as reflected in Table 6D.—Invalid Procedure Codes associated with this final rule (which is available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html).
e. Future Enhancement
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38053 through 38054), we noted the importance of ensuring accuracy of the coded data from the reporting, collection, processing, coverage, payment, and analysis aspects. We have engaged a contractor to assist in the review of the limited coverage and noncovered procedure edits in the MCE that may also be present in other claims processing systems that are utilized by our MACs. The MACs must adhere to criteria specified within the National Coverage Determinations (NCDs) and may implement their own edits in addition to what are already incorporated into the MCE, resulting in duplicate edits. The objective of this review is to identify where duplicate edits may exist and to determine what the impact might be if these edits were to be removed from the MCE.
We have noted that the purpose of the MCE is to ensure that errors and inconsistencies in the coded data are recognized during Medicare claims processing. As we indicated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41228), we are considering whether the inclusion of coverage edits in the MCE necessarily aligns with that specific goal because the focus of coverage edits is on whether or not a particular service is covered for payment purposes and not whether it was coded correctly.
As we continue to evaluate the purpose and function of the MCE with respect to ICD-10, we encourage public input for future discussion. As we have discussed in prior rulemaking, we recognize a need to further examine the current list of edits and the definitions of those edits. As noted in the FY 2020 IPPS/LTCH PPS proposed rule, we continue to encourage public comments on whether there are additional concerns with the current edits, including specific edits or language that should be removed or revised, edits that should be combined, or new edits that should be added to assist in detecting errors or inaccuracies in the coded data. Comments should be directed to the MS-DRG Classification Change Mailbox located at: MSDRGClassificationChange@cms.hhs.gov by November 1, 2019 for FY 2021 rulemaking.
17. Changes to Surgical Hierarchies
Some inpatient stays entail multiple surgical procedures, each one of which, occurring by itself, could result in assignment of the case to a different MS-DRG within the MDC to which the principal diagnosis is assigned. Therefore, it is necessary to have a decision rule within the GROUPER by which these cases are assigned to a single MS-DRG. The surgical hierarchy, an ordering of surgical classes from most resource-intensive to least resource-intensive, performs that function. Application of this hierarchy ensures that cases involving multiple surgical procedures are assigned to the MS-DRG associated with the most resource-intensive surgical class.
A surgical class can be composed of one or more MS-DRGs. For example, in MDC 11, the surgical class “kidney transplant” consists of a single MS-DRG (MS-DRG 652) and the class “major bladder procedures” consists of three MS-DRGs (MS-DRGs 653, 654, and 655). Consequently, in many cases, the surgical hierarchy has an impact on more than one MS-DRG. The methodology for determining the most resource-intensive surgical class involves weighting the average resources for each MS-DRG by frequency to determine the weighted average resources for each surgical class. For example, assume surgical class A includes MS-DRGs 001 and 002 and surgical class B includes MS-DRGs 003, 004, and 005. Assume also that the average costs of MS-DRG 001 are higher than that of MS-DRG 003, but the average costs of MS-DRGs 004 and 005 are higher than the average costs of MS-DRG 002. To determine whether surgical class A should be higher or lower than surgical class B in the surgical hierarchy, we would weigh the average costs of each MS-DRG in the class by frequency (that is, by the number of cases in the MS-DRG) to determine average resource consumption for the surgical class. The surgical classes would then be ordered from the class with the highest average resource utilization to that with the lowest, with the exception of “other O.R. procedures” as discussed in this final rule.
This methodology may occasionally result in assignment of a case involving multiple procedures to the lower-weighted MS-DRG (in the highest, most resource-intensive surgical class) of the available alternatives. However, given that the logic underlying the surgical hierarchy provides that the GROUPER search for the procedure in the most resource-intensive surgical class, in cases involving multiple procedures, this result is sometimes unavoidable.
We note that, notwithstanding the foregoing discussion, there are a few instances when a surgical class with a lower average cost is ordered above a surgical class with a higher average cost. For example, the “other O.R. procedures” surgical class is uniformly ordered last in the surgical hierarchy of each MDC in which it occurs, regardless of the fact that the average costs for the MS-DRG or MS-DRGs in that surgical class may be higher than those for other surgical classes in the MDC. The “other O.R. procedures” class is a group of procedures that are only infrequently related to the diagnoses in the MDC, but are still occasionally performed on patients with cases assigned to the MDC with these diagnoses. Therefore, assignment to these surgical classes should only occur if no other surgical class more closely related to the diagnoses in the MDC is appropriate.
A second example occurs when the difference between the average costs for two surgical classes is very small. We have found that small differences generally do not warrant reordering of the hierarchy because, as a result of reassigning cases on the basis of the hierarchy change, the average costs are likely to shift such that the higher-ordered surgical class has lower average costs than the class ordered below it.
Based on the changes that we proposed to make in the FY 2020 IPPS/LTCH PPS proposed rule, as discussed in section II.F.5.a. of the preamble of this final rule, in the proposed rule we proposed to revise the surgical hierarchy for MDC 5 (Diseases and Disorders of the Circulatory System) as follows: In MDC 5, we proposed to sequence proposed new MS-DRGs 319 and 320 (Other Endovascular Cardiac Valve Procedures with and without MCC, respectively) above MS-DRGs 222, 223, 224, 225, 226, and 227 (Cardiac Defibrillator Implant with and without Cardiac Catheterization with and without AMI/HF/Shock with and without MCC, respectively) and below MS-DRGs 266 and 267 (Endovascular Cardiac Valve Replacement with and without MCC, respectively). We also note that, as discussed in section II.F.5.a. of the preamble of this final rule, we proposed to revise the titles for MS-DRGs 266 and 267 to “Endovascular Cardiac Valve Replacement and Supplement Procedures with MCC” and “Endovascular Cardiac Valve Replacement and Supplement Procedures without MCC”, respectively.
Our proposal for Appendix D—MS-DRG Surgical Hierarchy by MDC and MS-DRG of the ICD-10 MS-DRG Definitions Manual Version 37 is illustrated in the following table.

Comment: Commenters supported our proposal to sequence proposed new MS-DRGs 319 and 320 above MS-DRGs 222, 223, 224, 225, 226, and 227, and below MS- DRGs 266 and 267. However, a commenter proposed an alternate option upon reviewing Table 5.—List Of Medicare Severity Diagnosis-Related Groups (MS-DRGs), Relative Weighting Factors, And Geometric And Arithmetic Mean Length Of Stay—FY 2020 associated with the proposed rule. The commenter noted that because multiple procedures may be performed during an encounter and MS-DRGs 215, 216, 217, 218, 219, 220, 221, 222, 223, 224, 225, 226, 227, 228, 229, 231, 232, 233, 234, 235, and 236 (MS-DRG 230 was deleted effective FY 2017) are weighted higher than the proposed new MS-DRGs 319 and 320, sequencing proposed new MS-DRGs 319 and 320 above MS-DRGs 239, 240, and 241 (Amputation for Circulatory System Disorders except Upper Limb & Toe with MCC, with CC, and without CC/MCC, respectively) and below MS-DRG 270, 271 and 272 (Other Major Cardiovascular Procedures with MCC, with CC, and without CC/MCC, respectively) appeared more appropriate to result in the most resource intensive MS-DRG assignment when multiple cardiac procedures are performed.
Response: We thank the commenters for their support. As discussed in section II.F.5.a. of the preamble of this final rule, we are finalizing our proposal to create new MS-DRGs 319 and 320. In response to the commenter's suggestion that we sequence new MS-DRGs 319 and 320 above MS-DRGs 239, 240, and 241 and below MS-DRGs 270, 271 and 272, we reviewed the surgical hierarchy once again. Upon our review, we agree that the initial proposed sequencing did not adequately account for the most resource intensive MS-DRG assignment. However, our clinical advisors also did not completely agree with the suggested alternative option offered by the commenter and recommended that new MS-DRGs 319 and 320 be sequenced above MS-DRGs 270, 271 and 272 and below MS-DRGs 268 and 269 (Aortic and Heart Assist Procedures Except Pulsation Balloon with and without MCC, respectively) because they believe this sequencing more appropriately reflects resource utilization when multiple cardiac procedures are performed and will result in the most suitable MS-DRG assignment.
After consideration of the public comments we received and the input of our clinical advisors, we are finalizing the below changes to the surgical hierarchy for new MS-DRGs 319 and 320 within Appendix D—MS-DRG Surgical Hierarchy by MDC and MS-DRG of the ICD-10 MS-DRG Definitions Manual Version 37 as illustrated in the following table.
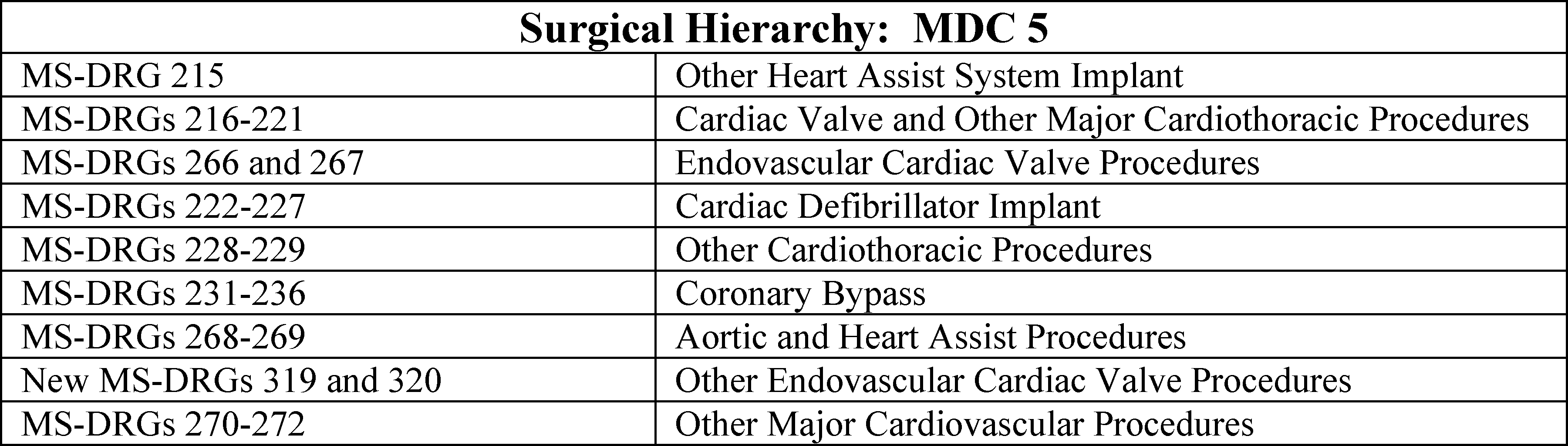
As with other MS-DRG related issues, we encourage commenters to submit requests to examine ICD-10 claims pertaining to the surgical hierarchy via the CMS MS-DRG Classification Change Request Mailbox located at: MSDRGClassificationChange@cms.hhs.gov by November 1, 2019 for consideration for FY 2021.
18. Maintenance of the ICD-10-CM and ICD-10-PCS Coding Systems
In September 1985, the ICD-9-CM Coordination and Maintenance Committee was formed. This is a Federal interdepartmental committee, co-chaired by the National Center for Health Statistics (NCHS), the Centers for Disease Control and Prevention (CDC), and CMS, charged with maintaining and updating the ICD-9-CM system. The final update to ICD-9-CM codes was made on October 1, 2013. Thereafter, the name of the Committee was changed to the ICD-10 Coordination and Maintenance Committee, effective with the March 19-20, 2014 meeting. The ICD-10 Coordination and Maintenance Committee addresses updates to the ICD-10-CM and ICD-10-PCS coding systems. The Committee is jointly responsible for approving coding changes, and developing errata, addenda, and other modifications to the coding systems to reflect newly developed procedures and technologies and newly identified diseases. The Committee is also responsible for promoting the use of Federal and non-Federal educational programs and other communication techniques with a view toward standardizing coding applications and upgrading the quality of the classification system.
The official list of ICD-9-CM diagnosis and procedure codes by fiscal year can be found on the CMS website at: http://cms.hhs.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html. The official list of ICD-10-CM and ICD-10-PCS codes can be found on the CMS website at: http://www.cms.gov/Medicare/Coding/ICD10/index.html.
The NCHS has lead responsibility for the ICD-10-CM and ICD-9-CM diagnosis codes included in the Tabular List and Alphabetic Index for Diseases, while CMS has lead responsibility for the ICD-10-PCS and ICD-9-CM procedure codes included in the Tabular List and Alphabetic Index for Procedures.
The Committee encourages participation in the previously mentioned process by health-related organizations. In this regard, the Committee holds public meetings for discussion of educational issues and proposed coding changes. These meetings provide an opportunity for representatives of recognized organizations in the coding field, such as the American Health Information Management Association (AHIMA), the American Hospital Association (AHA), and various physician specialty groups, as well as individual physicians, health information management professionals, and other members of the public, to contribute ideas on coding matters. After considering the opinions expressed at the public meetings and in writing, the Committee formulates recommendations, which then must be approved by the agencies.
The Committee presented proposals for coding changes for implementation in FY 2020 at a public meeting held on September 11-12, 2018, and finalized the coding changes after consideration of comments received at the meetings and in writing by November 13, 2018.
The Committee held its 2019 meeting on March 5-6, 2019. The deadline for submitting comments on these code proposals was April 5, 2019. It was announced at this meeting that any new diagnosis and procedure codes for which there was consensus of public support and for which complete tabular and indexing changes would be made by May 2019 would be included in the October 1, 2019 update to the ICD-10-CM diagnosis and ICD-10-PCS procedure code sets. As discussed in earlier sections of the preamble of this final rule, there are new, revised, and deleted ICD-10-CM diagnosis codes and ICD-10-PCS procedure codes that are captured in Table 6A.—New Diagnosis Codes, Table 6B.—New Procedure Codes, Table 6C.—Invalid Diagnosis Codes, Table 6D.—Invalid Procedure Codes, Table 6E.—Revised Diagnosis Code Titles, and Table 6F.—Revised Procedure Code Titles for this final rule, which are available via the internet on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. The code titles are adopted as part of the ICD-10 (previously ICD-9-CM) Coordination and Maintenance Committee process. Therefore, although we make the code titles available for the IPPS proposed rule, they are not subject to comment in the proposed rule. Because of the length of these tables, they are not published in the Addendum to the proposed rule. Rather, they are available via the internet as discussed in section VI. of the Addendum to the proposed rule.
Live Webcast recordings of the discussions of the diagnosis and procedure codes at the Committee's September 11-12, 2018 meeting can be obtained from the CMS website at: http://cms.hhs.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/index.html?redirect=/icd9ProviderDiagnosticCodes/03_meetings.asp. The live webcast recordings of the discussions of the diagnosis and procedure codes at the Committee's March 5-6, 2019 meeting can be obtained from the CMS website at: https://www.cms.gov/Medicare/Coding/ICD10/C-and-M-Meeting-Materials.html.
The materials for the discussions relating to diagnosis codes at the September 11-12, 2018 meeting and March 5-6, 2019 meeting can be found at: http://www.cdc.gov/nchs/icd/icd10cm_maintenance.html. These websites also provide detailed information about the Committee, including information on requesting a new code, attending a Committee meeting, and timeline requirements and meeting dates.
We encourage commenters to address suggestions on coding issues involving diagnosis codes to: Donna Pickett, Co-Chairperson, ICD-10 Coordination and Maintenance Committee, NCHS, Room 2402, 3311 Toledo Road, Hyattsville, MD 20782. Comments may be sent by Email to: nchsicd10cm@cdc.gov.
Questions and comments concerning the procedure codes should be submitted via Email to: ICDProcedureCodeRequest@cms.hhs.gov.
In the September 7, 2001 final rule implementing the IPPS new technology add-on payments (66 FR 46906), we indicated we would attempt to include proposals for procedure codes that would describe new technology discussed and approved at the Spring meeting as part of the code revisions effective the following October.
Section 503(a) of Public Law 108-173 included a requirement for updating diagnosis and procedure codes twice a year instead of a single update on October 1 of each year. This requirement was included as part of the amendments to the Act relating to recognition of new technology under the IPPS. Section 503(a) amended section 1886(d)(5)(K) of the Act by adding a clause (vii) which states that the Secretary shall provide for the addition of new diagnosis and procedure codes on April 1 of each year, but the addition of such codes shall not require the Secretary to adjust the payment (or diagnosis-related group classification) until the fiscal year that begins after such date. This requirement improves the recognition of new technologies under the IPPS by providing information on these new technologies at an earlier date. Data will be available 6 months earlier than would be possible with updates occurring only once a year on October 1.
While section 1886(d)(5)(K)(vii) of the Act states that the addition of new diagnosis and procedure codes on April 1 of each year shall not require the Secretary to adjust the payment, or DRG classification, under section 1886(d) of the Act until the fiscal year that begins after such date, we have to update the DRG software and other systems in order to recognize and accept the new codes. We also publicize the code changes and the need for a mid-year systems update by providers to identify the new codes. Hospitals also have to obtain the new code books and encoder updates, and make other system changes in order to identify and report the new codes.
The ICD-10 (previously the ICD-9-CM) Coordination and Maintenance Committee holds its meetings in the spring and fall in order to update the codes and the applicable payment and reporting systems by October 1 of each year. Items are placed on the agenda for the Committee meeting if the request is received at least 3 months prior to the meeting. This requirement allows time for staff to review and research the coding issues and prepare material for discussion at the meeting. It also allows time for the topic to be publicized in meeting announcements in the Federal Register as well as on the CMS website. A complete addendum describing details of all diagnosis and procedure coding changes, both tabular and index, is published on the CMS and NCHS websites in June of each year. Publishers of coding books and software use this information to modify their products that are used by health care providers. This 5-month time period has proved to be necessary for hospitals and other providers to update their systems.
A discussion of this timeline and the need for changes are included in the December 4-5, 2005 ICD-9-CM Coordination and Maintenance Committee Meeting minutes. The public agreed that there was a need to hold the fall meetings earlier, in September or October, in order to meet the new implementation dates. The public provided comment that additional time would be needed to update hospital systems and obtain new code books and coding software. There was considerable concern expressed about the impact this April update would have on providers.
In the FY 2005 IPPS final rule, we implemented section 1886(d)(5)(K)(vii) of the Act, as added by section 503(a) of Public Law 108-173, by developing a mechanism for approving, in time for the April update, diagnosis and procedure code revisions needed to describe new technologies and medical services for purposes of the new technology add-on payment process. We also established the following process for making these determinations. Topics considered during the Fall ICD-10 (previously ICD-9-CM) Coordination and Maintenance Committee meeting are considered for an April 1 update if a strong and convincing case is made by the requestor at the Committee's public meeting. The request must identify the reason why a new code is needed in April for purposes of the new technology process. The participants at the meeting and those reviewing the Committee meeting materials and live webcast are provided the opportunity to comment on this expedited request. All other topics are considered for the October 1 update. Participants at the Committee meeting are encouraged to comment on all such requests. We indicated in the proposed rule that there were not any requests approved for an expedited April l, 2019 implementation of a code at the September 11-12, 2018 Committee meeting. Therefore, there were not any new codes for implementation on April 1, 2019.
ICD-9-CM addendum and code title information is published on the CMS website at: http://www.cms.hhs.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/index.html?redirect=/icd9ProviderDiagnosticCodes/01overview.asp#TopofPage. ICD-10-CM and ICD-10-PCS addendum and code title information is published on the CMS website at: http://www.cms.gov/Medicare/Coding/ICD10/index.html. CMS also sends copies of all ICD-10-CM and ICD-10-PCS coding changes to its Medicare contractors for use in updating their systems and providing education to providers.
Information on ICD-10-CM diagnosis codes, along with the Official ICD-10-CM Coding Guidelines, can also be found on the CDC website at: http://www.cdc.gov/nchs/icd/icd10.htm. Additionally, information on new, revised, and deleted ICD-10-CM diagnosis and ICD-10-PCS procedure codes is provided to the AHA for publication in the Coding Clinic for ICD-10. AHA also distributes coding update information to publishers and software vendors.
The following chart shows the number of ICD-10-CM and ICD-10-PCS codes and code changes since FY 2016 when ICD-10 was implemented.

As mentioned previously, the public is provided the opportunity to comment on any requests for new diagnosis or procedure codes discussed at the ICD-10 Coordination and Maintenance Committee meeting.
19. Replaced Devices Offered Without Cost or With a Credit
a. Background
In the FY 2008 IPPS final rule with comment period (72 FR 47246 through 47251), we discussed the topic of Medicare payment for devices that are replaced without cost or where credit for a replaced device is furnished to the hospital. We implemented a policy to reduce a hospital's IPPS payment for certain MS-DRGs where the implantation of a device that subsequently failed or was recalled determined the base MS-DRG assignment. At that time, we specified that we will reduce a hospital's IPPS payment for those MS-DRGs where the hospital received a credit for a replaced device equal to 50 percent or more of the cost of the device.
In the FY 2012 IPPS/LTCH PPS final rule (76 FR 51556 through 51557), we clarified this policy to state that the policy applies if the hospital received a credit equal to 50 percent or more of the cost of the replacement device and issued instructions to hospitals accordingly.
b. Changes for FY 2020
As discussed in the FY 2020 IPPS/LTCH proposed rule (84 FR 19255 through 19257), for FY 2020, we proposed to create new MS-DRGs 319 and 320 (Other Endovascular Cardiac Valve Procedures with and without MCC, respectively) and to revise the title for MS-DRG 266 from “Endovascular Cardiac Valve Replacement with MCC” to “Endovascular Cardiac Valve Replacement and Supplement Procedures with MCC” and the title for MS-DRG 267 from “Endovascular Cardiac Valve Replacement without MCC” to “Endovascular Cardiac Valve Replacement and Supplement Procedures without MCC”.
We noted in the proposed rule, as stated in the FY 2016 IPPS/LTCH PPS proposed rule (80 FR 24409), we generally map new MS-DRGs onto the list when they are formed from procedures previously assigned to MS-DRGs that are already on the list. Currently, MS-DRGs 216 through 221 are on the list of MS-DRGs subject to the policy for payment under the IPPS for replaced devices offered without cost or with a credit as shown in the table below. A subset of the procedures currently assigned to MS-DRGs 216 through 221 was proposed for assignment to proposed new MS-DRGs 319 and 320. Therefore, we proposed that if the applicable proposed MS-DRG changes are finalized, we also would add proposed new MS-DRGs 319 and 320 to the list of MS-DRGs subject to the policy for payment under the IPPS for replaced devices offered without cost or with a credit and make conforming changes to the titles of MS-DRGs 266 and 267 as reflected in the table below. We also proposed to continue to include the existing MS-DRGs currently subject to the policy as also displayed in the table below.


As discussed in section II.F.5.a. of the preamble of this final rule, we are finalizing our proposal to add new MS-DRGs 319 and 320. We did not receive any public comments opposing our proposal to add MS-DRGs 319 and 320 to the policy for replaced devices offered without cost or with credit, make conforming changes to the titles of MS-DRGs 266 and 267 as reflected in the table above or to continue to include the existing MS-DRGs currently subject to the policy. Therefore, we are finalizing the list of MS-DRGs in the table included in the proposed rule and above that will be subject to the replaced devices offered without cost or with a credit policy effective October 1, 2019.
The final list of MS-DRGs subject to the IPPS policy for replaced devices offered without cost or with a credit will also be issued to providers in the form of a Change Request (CR).
20. Out of Scope Public Comments Received
We received public comments regarding a number of MS-DRG and related issues that were outside the scope of the proposals included in the FY 2020 IPPS/LTCH PPS proposed rule.
Because we consider these public comments to be outside the scope of the proposed rule, we are not addressing them in this final rule. As stated in section II.F.1.b. of the preamble of this final rule, we encourage individuals with comments about MS-DRG classification to submit these comments no later than November 1 of each year so that they can be considered for possible inclusion in the annual proposed rule. We will consider these public comments for possible proposals in future rulemaking as part of our annual review process.
G. Recalibration of the FY 2020 MS-DRG Relative Weights
1. Data Sources for Developing the Relative Weights
In developing the FY 2020 system of weights, we proposed to use two data sources: Claims data and cost report data. As in previous years, the claims data source is the MedPAR file. This file is based on fully coded diagnostic and procedure data for all Medicare inpatient hospital bills. The FY 2018 MedPAR data used in this final rule include discharges occurring on October 1, 2017, through September 30, 2018, based on bills received by CMS through March 31, 2019, from all hospitals subject to the IPPS and short-term, acute care hospitals in Maryland (which at that time were under a waiver from the IPPS). The FY 2018 MedPAR file used in calculating the relative weights includes data for approximately 9,514,788 Medicare discharges from IPPS providers. Discharges for Medicare beneficiaries enrolled in a Medicare Advantage managed care plan are excluded from this analysis. These discharges are excluded when the MedPAR “GHO Paid” indicator field on the claim record is equal to “1” or when the MedPAR DRG payment field, which represents the total payment for the claim, is equal to the MedPAR “Indirect Medical Education (IME)” payment field, indicating that the claim was an “IME only” claim submitted by a teaching hospital on behalf of a beneficiary enrolled in a Medicare Advantage managed care plan. In addition, the December 31, 2018 update of the FY 2018 MedPAR file complies with version 5010 of the X12 HIPAA Transaction and Code Set Standards, and includes a variable called “claim type.” Claim type “60” indicates that the claim was an inpatient claim paid as fee-for-service. Claim types “61,” “62,” “63,” and “64” relate to encounter claims, Medicare Advantage IME claims, and HMO no-pay claims. Therefore, the calculation of the relative weights for FY 2020 also excludes claims with claim type values not equal to “60.” The data exclude CAHs, including hospitals that subsequently became CAHs after the period from which the data were taken. We note that the FY 2020 relative weights are based on the ICD-10-CM diagnosis codes and ICD-10-PCS procedure codes from the FY 2018 MedPAR claims data, grouped through the ICD-10 version of the FY 2020 GROUPER (Version 37).
The second data source used in the cost-based relative weighting methodology is the Medicare cost report data files from the HCRIS. Normally, we use the HCRIS dataset that is 3 years prior to the IPPS fiscal year. Specifically, we used cost report data from the March 31, 2018 update of the FY 2017 HCRIS for calculating the FY 2020 cost-based relative weights.
2. Methodology for Calculation of the Relative Weights
As we explain in section II.E.2. of the preamble of this final rule, we calculated the FY 2020 relative weights based on 19 CCRs, as we did for FY 2019. The methodology we proposed to use to calculate the FY 2020 MS-DRG cost-based relative weights based on claims data in the FY 2018 MedPAR file and data from the FY 2017 Medicare cost reports is as follows:
- To the extent possible, all the claims were regrouped using the FY 2020 MS-DRG classifications discussed in sections II.B. and II.F. of the preamble of this final rule.
- The transplant cases that were used to establish the relative weights for heart and heart-lung, liver and/or intestinal, and lung transplants (MS-DRGs 001, 002, 005, 006, and 007, respectively) were limited to those Medicare-approved transplant centers that have cases in the FY 2018 MedPAR file. (Medicare coverage for heart, heart-lung, liver and/or intestinal, and lung transplants is limited to those facilities that have received approval from CMS as transplant centers.)
- Organ acquisition costs for kidney, heart, heart-lung, liver, lung, pancreas, and intestinal (or multivisceral organs) transplants continue to be paid on a reasonable cost basis. Because these acquisition costs are paid separately from the prospective payment rate, it is necessary to subtract the acquisition charges from the total charges on each transplant bill that showed acquisition charges before computing the average cost for each MS-DRG and before eliminating statistical outliers.
- Claims with total charges or total lengths of stay less than or equal to zero were deleted. Claims that had an amount in the total charge field that differed by more than $30.00 from the sum of the routine day charges, intensive care charges, pharmacy charges, implantable devices charges, supplies and equipment charges, therapy services charges, operating room charges, cardiology charges, laboratory charges, radiology charges, other service charges, labor and delivery charges, inhalation therapy charges, emergency room charges, blood and blood products charges, anesthesia charges, cardiac catheterization charges, CT scan charges, and MRI charges were also deleted.
- At least 92.3 percent of the providers in the MedPAR file had charges for 14 of the 19 cost centers. All claims of providers that did not have charges greater than zero for at least 14 of the 19 cost centers were deleted. In other words, a provider must have no more than five blank cost centers. If a provider did not have charges greater than zero in more than five cost centers, the claims for the provider were deleted.
- Statistical outliers were eliminated by removing all cases that were beyond 3.0 standard deviations from the geometric mean of the log distribution of both the total charges per case and the total charges per day for each MS-DRG.
- Effective October 1, 2008, because hospital inpatient claims include a POA indicator field for each diagnosis present on the claim, only for purposes of relative weight-setting, the POA indicator field was reset to “Y” for “Yes” for all claims that otherwise have an “N” (No) or a “U” (documentation insufficient to determine if the condition was present at the time of inpatient admission) in the POA field.
Under current payment policy, the presence of specific HAC codes, as indicated by the POA field values, can generate a lower payment for the claim. Specifically, if the particular condition is present on admission (that is, a “Y” indicator is associated with the diagnosis on the claim), it is not a HAC, and the hospital is paid for the higher severity (and, therefore, the higher weighted MS-DRG). If the particular condition is not present on admission (that is, an “N” indicator is associated with the diagnosis on the claim) and there are no other complicating conditions, the DRG GROUPER assigns the claim to a lower severity (and, therefore, the lower weighted MS-DRG) as a penalty for allowing a Medicare inpatient to contract a HAC. While the POA reporting meets policy goals of encouraging quality care and generates program savings, it presents an issue for the relative weight-setting process. Because cases identified as HACs are likely to be more complex than similar cases that are not identified as HACs, the charges associated with HAC cases are likely to be higher as well. Therefore, if the higher charges of these HAC claims are grouped into lower severity MS-DRGs prior to the relative weight-setting process, the relative weights of these particular MS-DRGs would become artificially inflated, potentially skewing the relative weights. In addition, we want to protect the integrity of the budget neutrality process by ensuring that, in estimating payments, no increase to the standardized amount occurs as a result of lower overall payments in a previous year that stem from using weights and case-mix that are based on lower severity MS-DRG assignments. If this would occur, the anticipated cost savings from the HAC policy would be lost.
To avoid these problems, we reset the POA indicator field to “Y” only for relative weight-setting purposes for all claims that otherwise have an “N” or a “U” in the POA field. This resetting “forced” the more costly HAC claims into the higher severity MS-DRGs as appropriate, and the relative weights calculated for each MS-DRG more closely reflect the true costs of those cases.
In addition, in the FY 2013 IPPS/LTCH PPS final rule, for FY 2013 and subsequent fiscal years, we finalized a policy to treat hospitals that participate in the Bundled Payments for Care Improvement (BPCI) initiative the same as prior fiscal years for the IPPS payment modeling and ratesetting process without regard to hospitals' participation within these bundled payment models (77 FR 53341 through 53343). Specifically, because acute care hospitals participating in the BPCI Initiative still receive IPPS payments under section 1886(d) of the Act, we include all applicable data from these subsection (d) hospitals in our IPPS payment modeling and ratesetting calculations as if the hospitals were not participating in those models under the BPCI initiative. We refer readers to the FY 2013 IPPS/LTCH PPS final rule for a complete discussion on our final policy for the treatment of hospitals participating in the BPCI initiative in our ratesetting process. For additional information on the BPCI initiative, we refer readers to the CMS' Center for Medicare and Medicaid Innovation's website at: http://innovation.cms.gov/initiatives/Bundled-Payments/index.html and to section IV.H.4. of the preamble of the FY 2013 IPPS/LTCH PPS final rule (77 FR 53341 through 53343).
The participation of hospitals in the BPCI initiative concluded on September 30, 2018. The participation of hospitals in the Bundled Payments for Care Improvement (BPCI) Advanced model started on October 1, 2018. The BPCI Advanced model, tested under the authority of section 3021 of the Affordable Care Act (codified at section 1115A of the Act), is comprised of a single payment and risk track, which bundles payments for multiple services beneficiaries receive during a Clinical Episode. Acute care hospitals may participate in BPCI Advanced in one of two capacities: As a model Participant or as a downstream Episode Initiator. Regardless of the capacity in which they participate in the BPCI Advanced model, participating acute care hospitals will continue to receive IPPS payments under section 1886(d) of the Act. Acute care hospitals that are Participants also assume financial and quality performance accountability for Clinical Episodes in the form of a reconciliation payment. For additional information on the BPCI Advanced model, we refer readers to the BPCI Advanced web page on the CMS Center for Medicare and Medicaid Innovation's website at: https://innovation.cms.gov/initiatives/bpci-advanced/. As noted in the proposed rule, consistent with our policy for FY 2019, and consistent with how we have treated hospitals that participated in the BPCI Initiative, for FY 2020, we continue to believe it is appropriate to include all applicable data from the subsection (d) hospitals participating in the BPCI Advanced model in our IPPS payment modeling and ratesetting calculations because, as noted above, these hospitals are still receiving IPPS payments under section 1886(d) of the Act.
The charges for each of the 19 cost groups for each claim were standardized to remove the effects of differences in area wage levels, IME and DSH payments, and for hospitals located in Alaska and Hawaii, the applicable cost-of-living adjustment. Because hospital charges include charges for both operating and capital costs, we standardized total charges to remove the effects of differences in geographic adjustment factors, cost-of-living adjustments, and DSH payments under the capital IPPS as well. Charges were then summed by MS-DRG for each of the 19 cost groups so that each MS-DRG had 19 standardized charge totals. Statistical outliers were then removed. These charges were then adjusted to cost by applying the national average CCRs developed from the FY 2017 cost report data.
The 19 cost centers that we used in the relative weight calculation are shown in the following table. The table shows the lines on the cost report and the corresponding revenue codes that we used to create the 19 national cost center CCRs. We stated in the proposed rule that, if stakeholders had comments about the groupings in this table, we may consider those comments as we finalize our policy. However, we did not receive any comments on the groupings in this table, and therefore, we are finalizing the groupings as proposed.
We invited public comments on our proposals related to recalibration of the FY 2020 relative weights and the changes in relative weights from FY 2019.
Comment: Several commenters expressed concern about significant reductions to the relative weight for MS-DRG 215. Commenters stated that the reduction in the proposed relative weight was 29 percent, which is the largest decrease of any MS-DRG; commenters also noted that the cumulative decrease to the relative weight for MS-DRG 215 would be 43% since FY 2017. Commenters stated that the proposed relative weights would result in significant underpayments to facilities, which would in turn limit access to heart assist devices.
Some commenters specifically referenced the Impella®, one of the heart assist devices used to provide ventricular support. Commenters also stated that the proposed reduction in the relative weight resulted from several coding changes and a new FDA indication for the Impella®, for the treatment of cardiomyopathy with cardiogenic shock. The commenters stated that these changes in coding guidance are still not reflected in claims for the FY 2020 proposed rule, and that 68% of claims for procedures utilizing the Impella® device did not have a charge for the Impella® in the Other Implants revenue center. Other commenters stated that 22% of claims did not have a charge for the device. Some commenters stated that they expect the future claims data to result in an increase to the relative weight for MS-DRG 215 for FY 2021.
Commenters requested that CMS maintain the relative weight at the FY 2018 relative weight for any MS-DRG that was held harmless last year and continues to face a 20% or greater reduction from its FY 2018 relative weight. Commenters stated that a hold harmless policy is consistent with prior rulemaking, in which CMS provided for transition periods for changes that have significant payment implications.
Response: As we indicated in the FY 2018 IPPS/LTCH final rule (82 FR 38103), and in response to similar comments in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41273), we do not believe it is normally appropriate to address relative weight fluctuations that appear to be driven by changes in the underlying data. Nevertheless, after reviewing the comments received and the data used in our ratesetting calculations, we acknowledge an outlier circumstance where the weight for an MS-DRG is seeing a significant reduction for each of the 3 years since CMS began using the ICD-10 data in calculating the relative weights. While we would ordinarily consider this weight change to be appropriately driven by the underlying data, given the comments received and the potential for these declines to be associated with the implementation of ICD-10, we are adopting a temporary one-time measure for FY 2020 for an MS-DRG where the FY 2018 relative weight declined by 20 percent from the FY 2017 relative weight and the FY 2020 relative weight would have declined by 20 percent or more from the FY 2019 relative weight, which was maintained at the FY 2018 relative weight. Specifically, for an MS-DRG meeting this criterion, we will continue the current policy of maintaining the relative weight at the FY 2018 level. In other words, the FY 2020 relative weight will be set equal to the FY 2019 relative weight, which was in turn set equal to the FY 2018 relative weight.
We believe this policy is consistent with our general authority to assign and update appropriate weighting factors under sections 1886(d)(4)(B) and (C) of the Act. We also believe that it appropriately addresses the situation in which the reduction to the FY 2020 relative weights may potentially continue to be associated with the implementation of ICD-10. We continue to believe that changes in relative weights that are not of this outlier magnitude over the 3 years since we first incorporated the ICD-10 data in our ratesetting are appropriately being driven by the underlying data and not associated with the implementation of ICD-10.


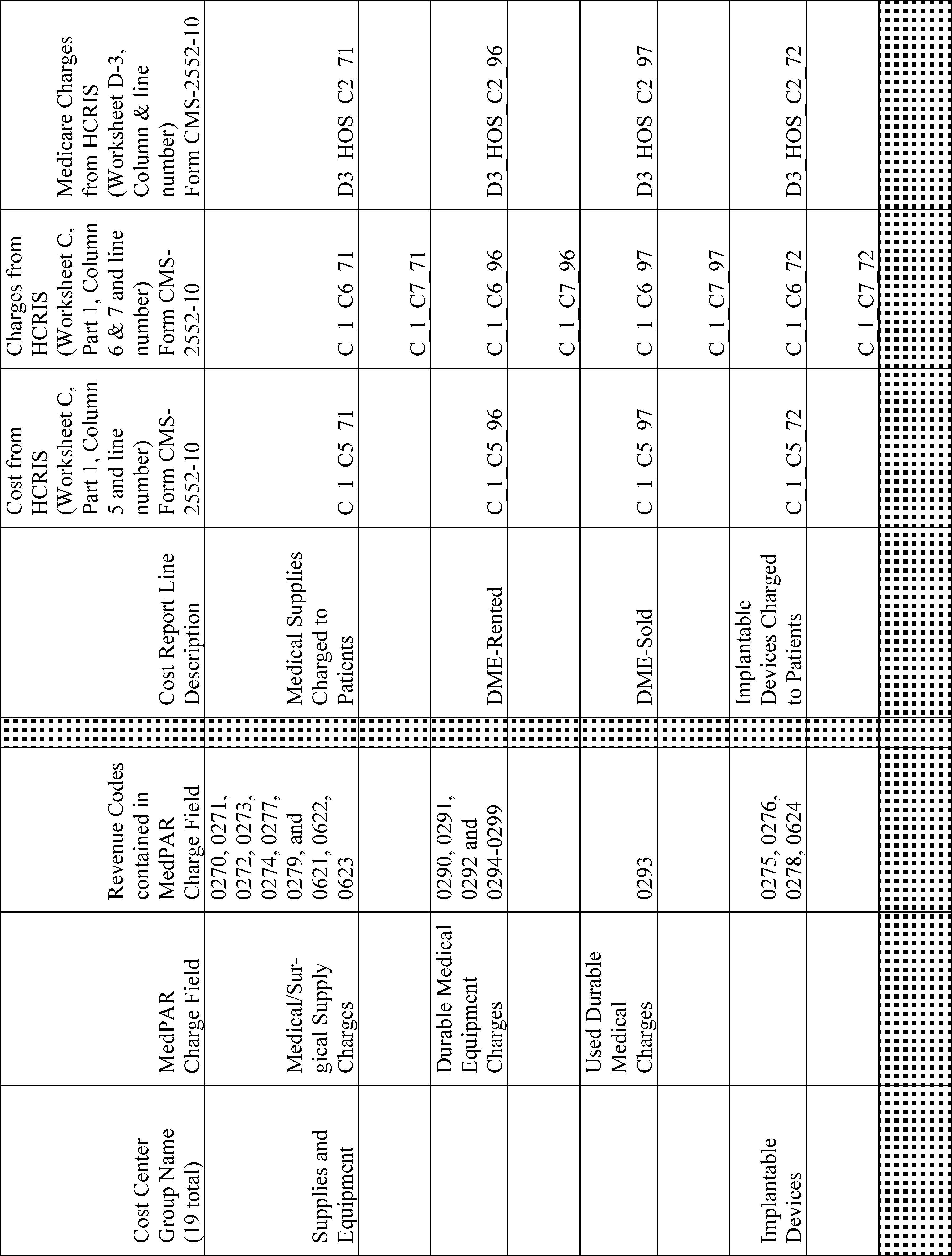




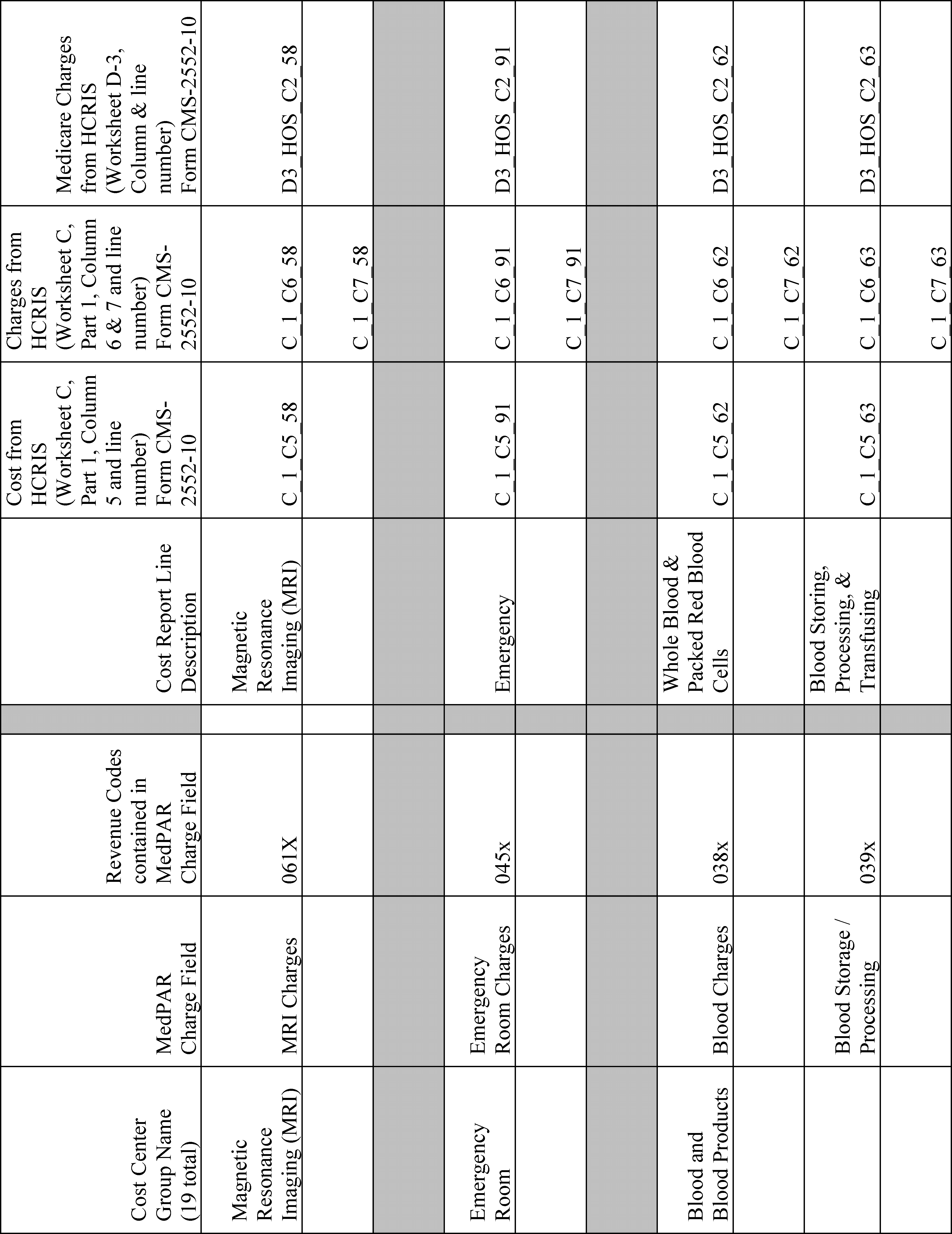



3. Development of National Average CCRs
We developed the national average CCRs as follows:
Using the FY 2017 cost report data, we removed CAHs, Indian Health Service hospitals, all-inclusive rate hospitals, and cost reports that represented time periods of less than 1 year (365 days). We included hospitals located in Maryland because we include their charges in our claims database. We then created CCRs for each provider for each cost center (see prior table for line items used in the calculations) and removed any CCRs that were greater than 10 or less than 0.01. We normalized the departmental CCRs by dividing the CCR for each department by the total CCR for the hospital for the purpose of trimming the data. We then took the logs of the normalized cost center CCRs and removed any cost center CCRs where the log of the cost center CCR was greater or less than the mean log plus/minus 3 times the standard deviation for the log of that cost center CCR. Once the cost report data were trimmed, we calculated a Medicare-specific CCR. The Medicare-specific CCR was determined by taking the Medicare charges for each line item from Worksheet D-3 and deriving the Medicare-specific costs by applying the hospital-specific departmental CCRs to the Medicare-specific charges for each line item from Worksheet D-3. Once each hospital's Medicare-specific costs were established, we summed the total Medicare-specific costs and divided by the sum of the total Medicare-specific charges to produce national average, charge-weighted CCRs.
After we multiplied the total charges for each MS-DRG in each of the 19 cost centers by the corresponding national average CCR, we summed the 19 “costs” across each MS-DRG to produce a total standardized cost for the MS-DRG. The average standardized cost for each MS-DRG was then computed as the total standardized cost for the MS-DRG divided by the transfer-adjusted case count for the MS-DRG. The average cost for each MS-DRG was then divided by the national average standardized cost per case to determine the relative weight.
The FY 2020 cost-based relative weights were then normalized by an adjustment factor of 1.789031 so that the average case weight after recalibration was equal to the average case weight before recalibration. The normalization adjustment is intended to ensure that recalibration by itself neither increases nor decreases total payments under the IPPS, as required by section 1886(d)(4)(C)(iii) of the Act.
The 19 national average CCRs for FY 2020 are as follows:
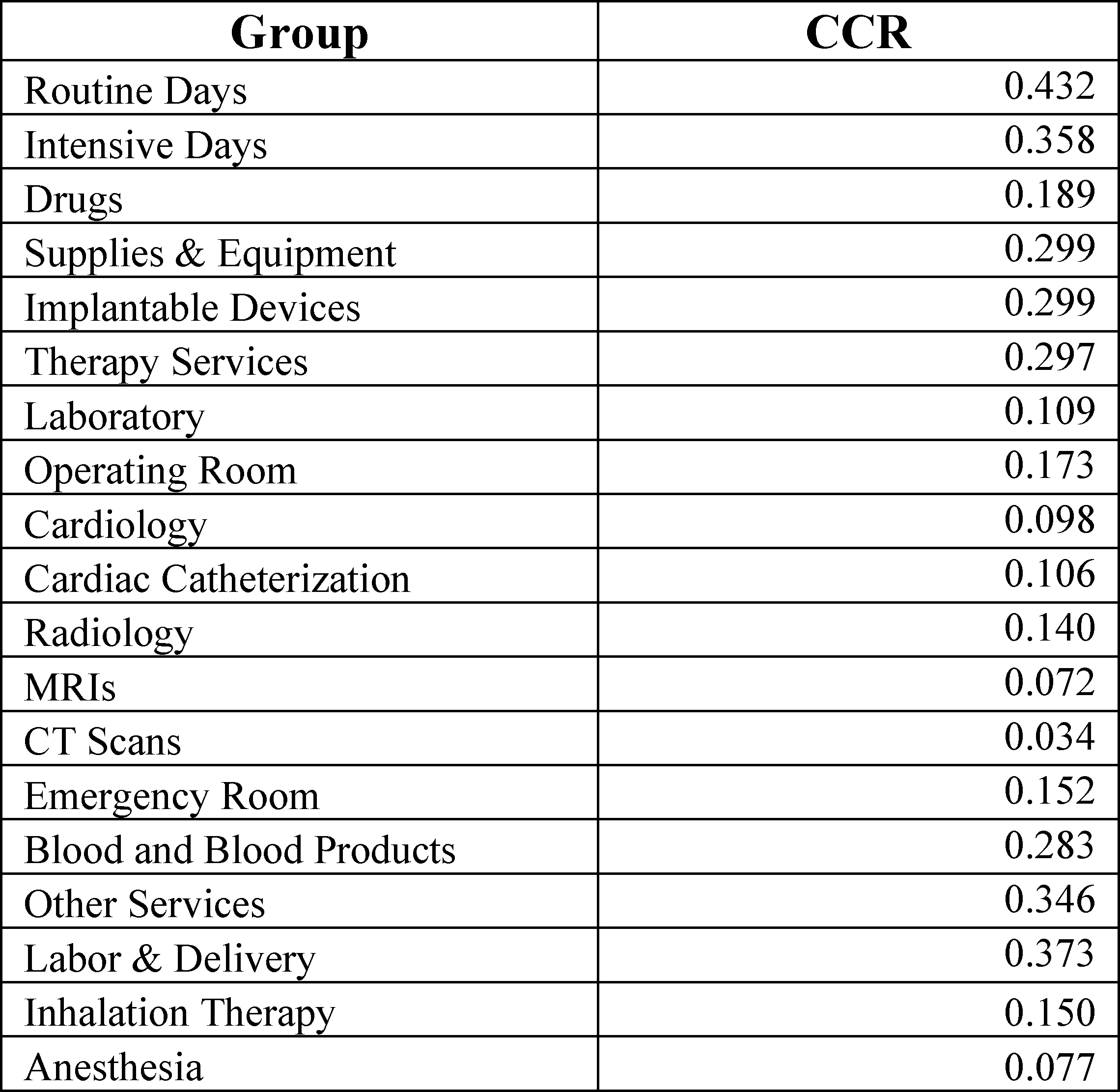
Since FY 2009, the relative weights have been based on 100 percent cost weights based on our MS-DRG grouping system.
When we recalibrated the DRG weights for previous years, we set a threshold of 10 cases as the minimum number of cases required to compute a reasonable weight. We proposed to use that same case threshold in recalibrating the MS-DRG relative weights for FY 2020. Using data from the FY 2018 MedPAR file, there were 8 MS-DRGs that contain fewer than 10 cases. For FY 2020, because we do not have sufficient MedPAR data to set accurate and stable cost relative weights for these low-volume MS-DRGs, we proposed to compute relative weights for the low-volume MS-DRGs by adjusting their final FY 2019 relative weights by the percentage change in the average weight of the cases in other MS-DRGs from FY 2019 to FY 2020. The crosswalk table is shown below.

After consideration of the comments we received, we are finalizing our proposals, with the modification for recalibrating the relative weights for FY 2020 for an MS-DRG where the FY 2018 relative weight declined by 20 percent from the FY 2017 relative weight and the FY 2020 relative weight would have declined by 20 percent or more from the FY 2019 relative weight, which was maintained at the FY 2018 relative weight.
H. Add-On Payments for New Services and Technologies for FY 2020
1. Background
Sections 1886(d)(5)(K) and (L) of the Act establish a process of identifying and ensuring adequate payment for new medical services and technologies (sometimes collectively referred to in this section as “new technologies”) under the IPPS. Section 1886(d)(5)(K)(vi) of the Act specifies that a medical service or technology will be considered new if it meets criteria established by the Secretary after notice and opportunity for public comment. Section 1886(d)(5)(K)(ii)(I) of the Act specifies that a new medical service or technology may be considered for new technology add-on payment if, based on the estimated costs incurred with respect to discharges involving such service or technology, the DRG prospective payment rate otherwise applicable to such discharges under this subsection is inadequate. We note that, beginning with discharges occurring in FY 2008, CMS transitioned from CMS- DRGs to MS-DRGs. The regulations at 42 CFR 412.87 implement these provisions and specify three criteria for a new medical service or technology to receive the additional payment: (1) The medical service or technology must be new; (2) the medical service or technology must be costly such that the DRG rate otherwise applicable to discharges involving the medical service or technology is determined to be inadequate; and (3) the service or technology must demonstrate a substantial clinical improvement over existing services or technologies. In this final rule, we highlight some of the major statutory and regulatory provisions relevant to the new technology add-on payment criteria, as well as other information. For a complete discussion on the new technology add-on payment criteria, we refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51572 through 51574).
Under the first criterion, as reflected in § 412.87(b)(2), a specific medical service or technology will be considered “new” for purposes of new medical service or technology add-on payments until such time as Medicare data are available to fully reflect the cost of the technology in the MS-DRG weights through recalibration. We note that we do not consider a service or technology to be new if it is substantially similar to one or more existing technologies. That is, even if a medical product receives a new FDA approval or clearance, it may not necessarily be considered “new” for purposes of new technology add-on payments if it is “substantially similar” to another medical product that was approved or cleared by FDA and has been on the market for more than 2 to 3 years. In the FY 2010 IPPS/RY 2010 LTCH PPS final rule (74 FR 43813 through 43814), we established criteria for evaluating whether a new technology is substantially similar to an existing technology, specifically: (1) Whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome; (2) whether a product is assigned to the same or a different MS-DRG; and (3) whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population. If a technology meets all three of these criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments. For a detailed discussion of the criteria for substantial similarity, we refer readers to the FY 2006 IPPS final rule (70 FR 47351 through 47352), and the FY 2010 IPPS/LTCH PPS final rule (74 FR 43813 through 43814).
Under the second criterion, § 412.87(b)(3) further provides that, to be eligible for the add-on payment for new medical services or technologies, the MS-DRG prospective payment rate otherwise applicable to discharges involving the new medical service or technology must be assessed for adequacy. Under the cost criterion, consistent with the formula specified in section 1886(d)(5)(K)(ii)(I) of the Act, to assess the adequacy of payment for a new technology paid under the applicable MS-DRG prospective payment rate, we evaluate whether the charges for cases involving the new technology exceed certain threshold amounts. The MS-DRG threshold amounts used in evaluating new technology add-on payment applications for FY 2020 are presented in a data file that is available, along with the other data files associated with the FY 2019 IPPS/LTCH PPS final rule and correction notice, on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2019-IPPS-Final-Rule-Home-Page-Items/FY2019-IPPS-Final-Rule-Data-Files.html?DLPage=1&DLEntries=10&DLSort=0&DLSortDir=ascending. As finalized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41275), beginning with FY 2020, we include the thresholds applicable to the next fiscal year (previously included in Table 10 of the annual IPPS/LTCH PPS proposed and final rules) in the data files associated with the prior fiscal year. Accordingly, the final thresholds for applications for new technology add-on payments for FY 2021 are presented in a data file that is available on the CMS website, along with the other data files associated with this FY 2020 final rule, by clicking on the FY 2020 IPPS Final Rule Home Page at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html.
In the September 7, 2001 final rule that established the new technology add-on payment regulations (66 FR 46917), we discussed the issue of whether the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule at 45 CFR parts 160 and 164 applies to claims information that providers submit with applications for new medical service or technology add-on payments. We refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51573) for complete information on this issue.
Under the third criterion, § 412.87(b)(1) of our existing regulations provides that a new technology is an appropriate candidate for an additional payment when it represents an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries. For example, a new technology represents a substantial clinical improvement when it reduces mortality, decreases the number of hospitalizations or physician visits, or reduces recovery time compared to the technologies previously available. (We refer readers to the September 7, 2001 final rule for a more detailed discussion of this criterion (66 FR 46902). We also refer readers to section II.H.8. of the preamble of this final rule for a discussion of our final policy regarding an alternative inpatient new technology add-on payment pathway for transformative new devices. We also refer readers to section II.H.10. of the preamble of this final rule for a discussion of our final policy regarding an alternative inpatient new technology add-on payment pathway for certain antimicrobials.)
The new medical service or technology add-on payment policy under the IPPS provides additional payments for cases with relatively high costs involving eligible new medical services or technologies, while preserving some of the incentives inherent under an average-based prospective payment system. The payment mechanism is based on the cost to hospitals for the new medical service or technology. Under § 412.88, if the costs of the discharge (determined by applying cost-to-charge ratios (CCRs) as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 50 percent of the estimated costs of the new technology or medical service (if the estimated costs for the case including the new technology or medical service exceed Medicare's payment); or (2) 50 percent of the difference between the full DRG payment and the hospital's estimated cost for the case. Unless the discharge qualifies for an outlier payment, the additional Medicare payment is limited to the full MS-DRG payment plus 50 percent of the estimated costs of the new technology or medical service. We refer readers to section II.H.9. of the preamble of this final rule for a discussion of our final policy regarding the change to the calculation of the new technology add-on payment beginning in FY 2020, including our finalized amendments to § 412.88 of the regulations.
Section 503(d)(2) of Public Law 108-173 provides that there shall be no reduction or adjustment in aggregate payments under the IPPS due to add-on payments for new medical services and technologies. Therefore, in accordance with section 503(d)(2) of Public Law 108-173, add-on payments for new medical services or technologies for FY 2005 and later years have not been subjected to budget neutrality.
In the FY 2009 IPPS final rule (73 FR 48561 through 48563), we modified our regulations at § 412.87 to codify our longstanding practice of how CMS evaluates the eligibility criteria for new medical service or technology add-on payment applications. That is, we first determine whether a medical service or technology meets the newness criterion, and only if so, do we then make a determination as to whether the technology meets the cost threshold and represents a substantial clinical improvement over existing medical services or technologies. We amended § 412.87(c) to specify that all applicants for new technology add-on payments must have FDA approval or clearance by July 1 of the year prior to the beginning of the fiscal year for which the application is being considered.
The Council on Technology and Innovation (CTI) at CMS oversees the agency's cross-cutting priority on coordinating coverage, coding and payment processes for Medicare with respect to new technologies and procedures, including new drug therapies, as well as promoting the exchange of information on new technologies and medical services between CMS and other entities. The CTI, composed of senior CMS staff and clinicians, was established under section 942(a) of Public Law 108-173. The Council is co-chaired by the Director of the Center for Clinical Standards and Quality (CCSQ) and the Director of the Center for Medicare (CM), who is also designated as the CTI's Executive Coordinator.
The specific processes for coverage, coding, and payment are implemented by CM, CCSQ, and the local Medicare Administrative Contractors (MACs) (in the case of local coverage and payment decisions). The CTI supplements, rather than replaces, these processes by working to assure that all of these activities reflect the agency-wide priority to promote high-quality, innovative care. At the same time, the CTI also works to streamline, accelerate, and improve coordination of these processes to ensure that they remain up to date as new issues arise. To achieve its goals, the CTI works to streamline and create a more transparent coding and payment process, improve the quality of medical decisions, and speed patient access to effective new treatments. It is also dedicated to supporting better decisions by patients and doctors in using Medicare-covered services through the promotion of better evidence development, which is critical for improving the quality of care for Medicare beneficiaries.
To improve the understanding of CMS' processes for coverage, coding, and payment and how to access them, the CTI has developed an “Innovator's Guide” to these processes. The intent is to consolidate this information, much of which is already available in a variety of CMS documents and in various places on the CMS website, in a user friendly format. This guide was published in 2010 and is available on the CMS website at: https://www.cms.gov/Medicare/Coverage/CouncilonTechInnov/Downloads/Innovators-Guide-Master-7-23-15.pdf.
As we indicated in the FY 2009 IPPS final rule (73 FR 48554), we invite any product developers or manufacturers of new medical services or technologies to contact the agency early in the process of product development if they have questions or concerns about the evidence that would be needed later in the development process for the agency's coverage decisions for Medicare.
The CTI aims to provide useful information on its activities and initiatives to stakeholders, including Medicare beneficiaries, advocates, medical product manufacturers, providers, and health policy experts. Stakeholders with further questions about Medicare's coverage, coding, and payment processes, or who want further guidance about how they can navigate these processes, can contact the CTI at CTI@cms.hhs.gov.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19274), we noted that applicants for add-on payments for new medical services or technologies for FY 2021 must submit a formal request, including a full description of the clinical applications of the medical service or technology and, as applicable, the results of any clinical evaluations demonstrating that the new medical service or technology represents a substantial clinical improvement, along with a significant sample of data to demonstrate that the medical service or technology meets the high-cost threshold. Complete application information, along with final deadlines for submitting a full application, will be posted on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/newtech.html. To allow interested parties to identify the new medical services or technologies under review before the publication of the proposed rule for FY 2021, the CMS website also will post the tracking forms completed by each applicant. We note that the burden associated with this information collection requirement is the time and effort required to collect and submit the data in the formal request for add-on payments for new medical services and technologies to CMS. The aforementioned burden is subject to the PRA; it is currently being revised based on the finalized policies discussed in this section of the final rule and approved under OMB control number 0938-1347, which expires on December 31, 2020.
2. Public Input Before Publication of a Notice of Proposed Rulemaking on Add-On Payments
Section 1886(d)(5)(K)(viii) of the Act, as amended by section 503(b)(2) of Public Law 108-173, provides for a mechanism for public input before publication of a notice of proposed rulemaking regarding whether a medical service or technology represents a substantial clinical improvement or advancement. The process for evaluating new medical service and technology applications requires the Secretary to—
- Provide, before publication of a proposed rule, for public input regarding whether a new service or technology represents an advance in medical technology that substantially improves the diagnosis or treatment of Medicare beneficiaries;
- Make public and periodically update a list of the services and technologies for which applications for add-on payments are pending;
- Accept comments, recommendations, and data from the public regarding whether a service or technology represents a substantial clinical improvement; and
- Provide, before publication of a proposed rule, for a meeting at which organizations representing hospitals, physicians, manufacturers, and any other interested party may present comments, recommendations, and data regarding whether a new medical service or technology represents a substantial clinical improvement to the clinical staff of CMS.
In order to provide an opportunity for public input regarding add-on payments for new medical services and technologies for FY 2020 prior to publication of the FY 2020 IPPS/LTCH PPS proposed rule, we published a notice in the Federal Register on October 5, 2018 (83 FR 50379), and held a town hall meeting at the CMS Headquarters Office in Baltimore, MD, on December 4, 2018. In the announcement notice for the meeting, we stated that the opinions and presentations provided during the meeting would assist us in our evaluations of applications by allowing public discussion of the substantial clinical improvement criterion for each of the FY 2020 new medical service and technology add-on payment applications before the publication of the FY 2020 IPPS/LTCH PPS proposed rule.
We stated in the FY 2020 IPPS/LTCH PPS proposed rule that approximately 100 individuals registered to attend the town hall meeting in person, while additional individuals listened over an open telephone line. We also live-streamed the town hall meeting and posted the morning and afternoon sessions of the town hall on the CMS YouTube web page at: https://www.youtube.com/watch?v=4z1AhEuGHqQ and https://www.youtube.com/watch?v=m26Xj1EzbIY, respectively. We considered each applicant's presentation made at the town hall meeting, as well as written comments submitted on the applications that were received by the due date of December 14, 2018, in our evaluation of the new technology add-on payment applications for FY 2020 in the development of the FY 2020 IPPS/LTCH PPS proposed rule.
In response to the published notice and the December 4, 2018 New Technology Town Hall meeting, we received written comments regarding the applications for FY 2020 new technology add-on payments. (We refer readers to section II.H.2. of the preamble of the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19275) for summaries of the comments we received in response to the published notice and the New Technology Town Hall meeting and our responses.) We also noted in the FY 2020 IPPS/LTCH PPS proposed rule that we do not summarize comments that are unrelated to the “substantial clinical improvement” criterion. As explained earlier and in the Federal Register notice announcing the New Technology Town Hall meeting (83 FR 50379 through 50381), the purpose of the meeting was specifically to discuss the substantial clinical improvement criterion in regard to pending new technology add-on payment applications for FY 2020. Therefore, we did not summarize those written comments in the proposed rule that are unrelated to the substantial clinical improvement criterion. In section II.H.5. of the preamble of the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19284 through 19367), we summarized comments regarding individual applications, or, if applicable, indicated that there were no comments received in response to the New Technology Town Hall meeting notice or New Technology Town Hall meeting, at the end of each discussion of the individual applications.
3. ICD-10-PCS Section “X” Codes for Certain New Medical Services and Technologies
As discussed in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49434), the ICD-10-PCS includes a new section containing the new Section “X” codes, which began being used with discharges occurring on or after October 1, 2015. Decisions regarding changes to ICD-10-PCS Section “X” codes will be handled in the same manner as the decisions for all of the other ICD-10-PCS code changes. That is, proposals to create, delete, or revise Section “X” codes under the ICD-10-PCS structure will be referred to the ICD-10 Coordination and Maintenance Committee. In addition, several of the new medical services and technologies that have been, or may be, approved for new technology add-on payments may now, and in the future, be assigned a Section “X” code within the structure of the ICD-10-PCS. We posted ICD-10-PCS Guidelines on the CMS website at: http://www.cms.gov/Medicare/Coding/ICD10/2016-ICD-10-PCS-and-GEMs.html, including guidelines for ICD-10-PCS Section “X” codes. We encourage providers to view the material provided on ICD-10-PCS Section “X” codes.
4. FY 2020 Status of Technologies Approved for FY 2019 New Technology Add-On Payments
a. Defitelio® (Defibrotide)
Jazz Pharmaceuticals submitted an application for new technology add-on payments for FY 2017 for defibrotide (Defitelio®), a treatment for patients who have been diagnosed with hepatic veno-occlusive disease (VOD) with evidence of multi-organ dysfunction. VOD, also known as sinusoidal obstruction syndrome (SOS), is a potentially life-threatening complication of hematopoietic stem cell transplantation (HSCT), with an incidence rate of 8 percent to 15 percent. Diagnoses of VOD range in severity from what has been classically defined as a disease limited to the liver (mild) and reversible, to a severe syndrome associated with multi-organ dysfunction or failure and death. Patients who have received treatment involving HSCT who develop VOD with multi-organ failure face an immediate risk of death, with a mortality rate of more than 80 percent when only supportive care is used. The applicant asserted that Defitelio® improves the survival rate of patients who have been diagnosed with VOD with multi-organ failure by 23 percent.
Defitelio® received Orphan Drug Designation for the treatment of VOD in 2003 and for the prevention of VOD in 2007. It has been available to patients as an investigational drug through an Expanded Access Program since 2006. The applicant's New Drug Application (NDA) for Defitelio® received FDA approval on March 30, 2016. The applicant confirmed that Defitelio® was not available on the U.S. market as of the FDA NDA approval date of March 30, 2016. According to the applicant, commercial packaging could not be completed until the label for Defitelio® was finalized with FDA approval, and that commercial shipments of Defitelio® to hospitals and treatment centers began on April 4, 2016. Therefore, we agreed that, based on this information, the newness period for Defitelio® begins on April 4, 2016, the date of its first commercial availability.
The applicant received approval to use unique ICD-10-PCS procedure codes to describe the use of Defitelio®, with an effective date of October 1, 2016. The approved ICD-10-PCS procedure codes are: XW03392 (Introduction of defibrotide sodium anticoagulant into peripheral vein, percutaneous approach); and XW04392 (Introduction of defibrotide sodium anticoagulant into central vein, percutaneous approach).
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for Defitelio® and consideration of the public comments we received in response to the FY 2017 IPPS/LTCH PPS proposed rule, we approved Defitelio® for new technology add-on payments for FY 2017 (81 FR 56906). With the new technology add-on payment application, the applicant estimated that the average Medicare beneficiary would require a dosage of 25 mg/kg/day for a minimum of 21 days of treatment. The recommended dose is 6.25 mg/kg given as a 2-hour intravenous infusion every 6 hours. Dosing should be based on a patient's baseline body weight, which is assumed to be 70 kg for an average adult patient. All vials contain 200 mg at a cost of $825 per vial. Therefore, we determined that cases involving the use of the Defitelio® technology would incur an average cost per case of $151,800 (70 kg adult × 25 mg/kg/day × 21 days = 36,750 mg per patient/200 mg vial = 184 vials per patient × $825 per vial = $151,800). Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment amount for a case involving the use of Defitelio® is $75,900 for FY 2019.
Our policy is that a medical service or technology may continue to be considered “new” for purposes of new technology add-on payments within 2 or 3 years after the point at which data begin to become available reflecting the inpatient hospital code assigned to the new service or technology. Our practice has been to begin and end new technology add-on payments on the basis of a fiscal year, and we have generally followed a guideline that uses a 6-month window before and after the start of the fiscal year to determine whether to extend the new technology add-on payment for an additional fiscal year. In general, we extend new technology add-on payments for an additional year only if the 3-year anniversary date of the product's entry onto the U.S. market occurs in the latter half of the fiscal year (70 FR 47362).
With regard to the newness criterion for Defitelio®, we considered the beginning of the newness period to commence on the first day Defitelio® was commercially available (April 4, 2016). Because the 3-year anniversary date of the entry of the Defitelio® onto the U.S. market (April 4, 2019) would occur during FY 2019, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19276), we proposed to discontinue new technology add-on payments for this technology for FY 2020. We invited public comments on our proposal to discontinue new technology add-on payments for Defitelio® for FY 2020.
Comment: A commenter supported CMS' proposal to discontinue new technology add-on payments for FY 2020 for Defitelio®.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to discontinue new technology add-on payments for Defitelio® for FY 2020.
b. Ustekinumab (Stelara®)
Janssen Biotech submitted an application for new technology add-on payments for the Stelara® induction therapy for FY 2018. Stelara® received FDA approval on September 23, 2016 as an intravenous (IV) infusion treatment for adult patients who have been diagnosed with moderately to severely active Crohn's disease (CD) who have failed or were intolerant to treatment using immunomodulators or corticosteroids, but never failed a tumor necrosis factor (TNF) blocker, or failed or were intolerant to treatment using one or more TNF blockers. Stelara® IV is intended for induction—subcutaneous prefilled syringes are intended for maintenance dosing. Stelara® must be administered intravenously by a health care professional in either an inpatient hospital setting or an outpatient hospital setting.
Stelara® for IV infusion is packaged in single 130 mg vials. Induction therapy consists of a single IV infusion dose using the following weight-based dosing regimen: Patients weighing 55 kg or less than (<) 55 kg are administered 260 mg of Stelara® (2 vials); patients weighing more than (>) 55 kg, but 85 kg or less than (<) 85 kg are administered 390 mg of Stelara® (3 vials); and patients weighing more than (>) 85 kg are administered 520 mg of Stelara® (4 vials). An average dose of Stelara® administered through IV infusion is 390 mg (3 vials). Maintenance doses of Stelara® are administered at 90 mg, subcutaneously, at 8-week intervals and may occur in the outpatient hospital setting.
CD is an inflammatory bowel disease of unknown etiology, characterized by transmural inflammation of the gastrointestinal (GI) tract. Symptoms of CD may include fatigue, prolonged diarrhea with or without bleeding, abdominal pain, weight loss and fever. CD can affect any part of the GI tract including the mouth, esophagus, stomach, small intestine, and large intestine. Most commonly used pharmacologic treatments for CD include antibiotics, mesalamines, corticosteroids, immunomodulators, tumor necrosis alpha (TNFα) inhibitors, and anti-integrin agents. Surgery may be necessary for some patients who have been diagnosed with CD in which conventional therapies have failed.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for Stelara® and consideration of the public comments we received in response to the FY 2018 IPPS/LTCH PPS proposed rule, we approved Stelara® for new technology add-on payments for FY 2018 (82 FR 38129). Cases involving Stelara® that are eligible for new technology add-on payments are identified by ICD-10-PCS procedure code XW033F3 (Introduction of other New Technology therapeutic substance into peripheral vein, percutaneous approach, new technology group 3). With the new technology add-on payment application, the applicant estimated that the average Medicare beneficiary would require a dosage of 390 mg (3 vials) at a hospital acquisition cost of $1,600 per vial (for a total of $4,800). Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment amount for a case involving the use of Stelara® is $2,400 for FY 2019.
With regard to the newness criterion for Stelara®, we considered the beginning of the newness period to commence when Stelara® received FDA approval as an IV infusion treatment for Crohn's disease (CD) on September 23, 2016. Because the 3-year anniversary date of the entry of Stelara® onto the U.S. market (September 23, 2019) will occur during FY 2019, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19276 through 19277), we proposed to discontinue new technology add-on payments for this technology for FY 2020. We invited public comments on our proposal to discontinue new technology add-on payments for Stelara® for FY 2020.
Comment: A commenter supported CMS' proposal to discontinue new technology add-on payments for FY 2020 for Stelara®.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to discontinue new technology add-on payments for Stelara® for FY 2020.
c. Bezlotoxumab (ZINPLAVATM)
Merck & Co., Inc. submitted an application for new technology add-on payments for ZINPLAVATM for FY 2018. ZINPLAVATM is indicated as a treatment to reduce recurrence of Clostridium difficile infection (CDI) in adult patients who are receiving antibacterial drug treatment for a diagnosis of CDI and who are at high risk for CDI recurrence. ZINPLAVATM is not indicated for the treatment of the presenting episode of CDI and is not an antibacterial drug. ZINPLAVATM should only be used in conjunction with an antibacterial drug treatment for CDI.
Clostridium difficile (C-diff) is a disease-causing anaerobic, spore forming bacterium that affects the gastrointestinal (GI) tract. Some people carry the C-diff bacterium in their intestines, but never develop symptoms of an infection. The difference between asymptomatic colonization and disease is caused primarily by the production of an enterotoxin (Toxin A) and/or a cytotoxin (Toxin B). The presence of either or both toxins can lead to symptomatic CDI, which is defined as the acute onset of diarrhea with a documented infection with toxigenic C-diff. The GI tract contains millions of bacteria, commonly referred to as “normal flora” or “good bacteria,” which play a role in protecting the body from infection. Antibiotics can kill these good bacteria and allow C-diff to multiply and release toxins that damage the cells lining the intestinal wall, resulting in a CDI. CDI is a leading cause of hospital-associated gastrointestinal illnesses. Persons at increased risk for CDI include people who are currently on or who have recently been treated with antibiotics, people who have encountered current or recent hospitalization, people who are older than 65 years, immunocompromised patients, and people who have recently had a diagnosis of CDI. CDI symptoms include, but are not limited to, diarrhea, abdominal pain, and fever. CDI symptoms range in severity from mild (abdominal discomfort, loose stools) to severe (profuse, watery diarrhea, severe abdominal pain, and high fevers). Severe CDI can be life-threatening and, in rare cases, can cause bowel rupture, sepsis and organ failure. CDI is responsible for 14,000 deaths per year in the United States.
C-diff produces two virulent, pro-inflammatory toxins, Toxin A and Toxin B, which target host colonic endothelial cells by binding to endothelial cell surface receptors via combined repetitive oligopeptide (CROP) domains. These toxins cause the release of inflammatory cytokines leading to intestinal fluid secretion and intestinal inflammation. The applicant asserted that ZINPLAVATM targets Toxin B sites within the CROP domain rather than the C-diff organism itself. According to the applicant, by targeting C-diff Toxin B, ZINPLAVATM neutralizes Toxin B, prevents large intestine endothelial cell inflammation, symptoms associated with CDI, and reduces the recurrence of CDI.
ZINPLAVATM received FDA approval on October 21, 2016, as a treatment to reduce the recurrence of CDI in adult patients receiving antibacterial drug treatment for CDI and who are at high risk of CDI recurrence. As previously stated, ZINPLAVATM is not indicated for the treatment of CDI. ZINPLAVATM is not an antibacterial drug, and should only be used in conjunction with an antibacterial drug treatment for CDI. ZINPLAVATM became commercially available on February 10, 2017. Therefore, the newness period for ZINPLAVATM began on February 10, 2017. The applicant submitted a request for a unique ICD-10-PCS procedure code and was granted approval for the following procedure codes: XW033A3 (Introduction of bezlotoxumab monoclonal antibody, into peripheral vein, percutaneous approach, new technology group 3) and XW043A3 (Introduction of bezlotoxumab monoclonal antibody, into central vein, percutaneous approach, new technology group 3).
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for ZINPLAVATM and consideration of the public comments we received in response to the FY 2018 IPPS/LTCH PPS proposed rule, we approved ZINPLAVATM for new technology add-on payments for FY 2018 (82 FR 38119). With the new technology add-on payment application, the applicant estimated that the average Medicare beneficiary would require a dosage of 10 mg/kg of ZINPLAVATM administered as an IV infusion over 60 minutes as a single dose. According to the applicant, the WAC for one dose is $3,800. Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment amount for a case involving the use of ZINPLAVATM is $1,900 for FY 2019.
With regard to the newness criterion for ZINPLAVATM, we considered the beginning of the newness period to commence on February 10, 2017. As discussed previously in this section, in general, we extend new technology add-on payments for an additional year only if the 3-year anniversary date of the product's entry onto the U.S. market occurs in the latter half of the upcoming fiscal year. Because the 3-year anniversary date of the entry of ZINPLAVATM onto the U.S. market (February 10, 2020) will occur in the first half of FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19277), we proposed to discontinue new technology add-on payments for this technology for FY 2020. We invited public comments on our proposal to discontinue new technology add-on payments for ZINPLAVATM technology for FY 2020.
Comment: A commenter supported CMS' proposal to discontinue new technology add-on payments for FY 2020 for ZINPLAVATM.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to discontinue new technology add-on payments for ZINPLAVATM for FY 2020.
d. KYMRIAH® (Tisagenlecleucel) and YESCARTA® (Axicabtagene Ciloleucel)
Two manufacturers, Novartis Pharmaceuticals Corporation and Kite Pharma, Inc., submitted separate applications for new technology add-on payments for FY 2019 for KYMRIAH® (tisagenlecleucel) and YESCARTA® (axicabtagene ciloleucel), respectively. Both of these technologies are CD-19-directed T-cell immunotherapies used for the purposes of treating patients with aggressive variants of non-Hodgkin lymphoma (NHL).
On May 1, 2018, Novartis Pharmaceuticals Corporation received FDA approval for KYMRIAH®'s second indication, the treatment of adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma. On October 18, 2017, Kite Pharma, Inc. received FDA approval for the use of YESCARTA® indicated for the treatment of adult patients with r/r large B-cell lymphoma after two or more lines of systemic therapy, including DLBCL not otherwise specified, primary mediastinal large B-cell lymphoma, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma.
Procedures involving the KYMRIAH® and YESCARTA® therapies are both reported using the following ICD-10-PCS procedure codes: XW033C3 (Introduction of engineered autologous chimeric antigen receptor t-cell immunotherapy into peripheral vein, percutaneous approach, new technology group 3); and XW043C3 (Introduction of engineered autologous chimeric antigen receptor t-cell immunotherapy into central vein, percutaneous approach, new technology group 3). In the FY 2019 IPPS/LTCH PPS final rule, we finalized our proposal to assign cases reporting these ICD-10-PCS procedure codes to Pre-MDC MS-DRG 016 for FY 2019 and to revise the title of this MS-DRG to Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy. We refer readers to section II.F.2.d. of the preamble of the FY 2019 IPPS/LTCH PPS final rule for a complete discussion of these final policies (83 FR 41172 through 41174).
With respect to the newness criterion, according to both applicants, KYMRIAH® and YESCARTA® are the first CAR T-cell immunotherapies of their kind. As discussed in the FY 2019 IPPS/LTCH PPS proposed and final rules, because potential cases representing patients who may be eligible for treatment using KYMRIAH® and YESCARTA® would group to the same MS-DRGs (because the same ICD-10-CM diagnosis codes and ICD-10-PCS procedures codes are used to report treatment using either KYMRIAH® or YESCARTA®), and we believed that these technologies are intended to treat the same or similar disease in the same or similar patient population, and are purposed to achieve the same therapeutic outcome using the same or similar mechanism of action, we believed these two technologies are substantially similar to each other and that it was appropriate to evaluate both technologies as one application for new technology add-on payments under the IPPS. For these reasons, we stated that we intended to make one determination regarding approval for new technology add-on payments that would apply to both applications, and in accordance with our policy, would use the earliest market availability date submitted as the beginning of the newness period for both KYMRIAH® and YESCARTA®.
As summarized in the FY 2019 IPPS/LTCH PPS final rule, we received comments from the applicants for KYMRIAH® and YESCARTA® regarding whether KYMRIAH® and YESCARTA® were substantially similar to each other. The applicant for YESCARTA® stated that it believed each technology consists of notable differences in the construction, as well as manufacturing processes and successes that may lead to differences in activity. The applicant encouraged CMS to evaluate YESCARTA® as a separate new technology add-on payment application and approve separate new technology add-on payments for YESCARTA®, effective October 1, 2018, and to not move forward with a single new technology add-on payment evaluation determination that covers both CAR T-cell therapies, YESCARTA® and KYMRIAH®. The applicant for KYMRIAH® indicated that, based on FDA's approval, it agreed with CMS that KYMRIAH® is substantially similar to YESCARTA®, as defined by the new technology add-on payment application evaluation criteria. We refer readers to the FY 2019 IPPS/LTCH PPS final rule for a more detailed summary of these and other public comments we received regarding substantial similarity for KYMRIAH® and YESCARTA®.
After consideration of the public comments we received and for the reasons discussed in the FY 2019 IPPS/LTCH PPS final rule, we stated that we believed that KYMRIAH® and YESCARTA® are substantially similar to one another. We also noted that for FY 2019, there was no payment impact regarding this determination of substantial similarity because the cost of the technologies is the same. However, we stated that we welcomed additional comments in future rulemaking regarding whether KYMRIAH® and YESCARTA® are substantially similar and intended to revisit this issue in the FY 2020 IPPS/LTCH PPS proposed rule. As stated in the FY 2020 IPPS/LTCH PPS proposed rule, for the reasons discussed in the FY 2019 IPPS/LTCH PPS final rule, we continue to believe that KYMRIAH® and YESCARTA® are substantially similar to each other for purposes of new technology add-on payments under the IPPS. As we noted in the FY 2020 IPPS/LTCH PPS proposed rule, for FY 2020, the pricing for KYMRIAH® and YESCARTA® remains the same and, therefore, for FY 2020, there would continue to be no payment impact regarding the determination that the two technologies are substantially similar to each other for purposes of new technology add-on payments under the IPPS. In the proposed rule, similar to last year, we welcomed public comments regarding whether KYMRIAH® and YESCARTA® are substantially similar to each other. We refer readers to the FY 2019 IPPS/LTCH PPS final rule for a complete discussion on newness and substantial similarity regarding KYMRIAH® and YESCARTA®.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for KYMRIAH® and YESCARTA® and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved new technology add-on payments for KYMRIAH® and YESCARTA® for FY 2019 (83 FR 41299). Cases involving KYMRIAH® or YESCARTA® that are eligible for new technology add-on payments are identified by ICD-10-PCS procedure codes XW033C3 or XW043C3. The applicants for both KYMRIAH® and YESCARTA® estimated that the average cost for an administered dose of KYMRIAH® or YESCARTA® is $373,000. Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, for FY 2019, the maximum new technology add-on payment for a case involving the use of KYMRIAH® or YESCARTA® is $186,500.
As previously stated, our policy is that a medical service or technology may continue to be considered “new” for purposes of new technology add-on payments within 2 or 3 years after the point at which data begin to become available reflecting the inpatient hospital code assigned to the new service or technology. With regard to the newness criterion for KYMRIAH® and YESCARTA®, as discussed in the FY 2019 IPPS/LTCH PPS final rule, according to the applicant for YESCARTA®, the first commercial shipment of YESCARTA® was received by a certified treatment center on November 22, 2017. As previously stated, we use the earliest market availability date submitted as the beginning of the newness period for both KYMRIAH® and YESCARTA®. Therefore, we consider the beginning of the newness period for both KYMRIAH® and YESCARTA® to commence November 22, 2017.
Because the 3-year anniversary date of the entry of the technology onto the U.S. market (November 22, 2020) will occur after FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19278 through 19279), we proposed to continue new technology add-on payments for KYMRIAH® and YESCARTA® for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of KYMRIAH® and YESCARTA® would be increased to $242,450 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving KYMRIAH® or YESCARTA® would remain at $186,500 for FY 2020.
For the reasons discussed in section II.F.2.c. of the proposed rule (84 FR 19180 through 19182), we proposed not to modify the current MS-DRG assignment for cases reporting CAR T-cell therapies for FY 2020. Alternatively, we stated that we were seeking public comments on payment alternatives for CAR-T cell therapies. We also invited public comments on how these payment alternatives would affect access to care, as well as how they affect incentives to encourage lower drug prices, which is a high priority for this Administration. As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41172 through 41174), we are considering approaches and authorities to encourage value-based care and lower drug prices. We solicited public comments on how the effective dates of any potential payment methodology alternatives, if any were to be adopted, may intersect and affect future participation in any such alternative approaches. In the proposed rule, we stated that such payment alternatives could include adjusting the CCRs used to calculate new technology add-on payments for cases involving the use of KYMRIAH® and YESCARTA®. We noted that we also considered this payment alternative for FY 2019, as discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41172 through 41174), and are revisiting this approach given the additional experience with CAR T-cell therapy being provided in hospitals paid under the IPPS and in IPPS-excluded cancer hospitals. We also requested public comments on other payment alternatives for these cases, including eliminating the use of CCRs in calculating the new technology add-on payments for cases involving the use of KYMRIAH® and YESCARTA® by making a uniform add-on payment that equals the proposed maximum add-on payment, that is, 65 percent of the cost of the technology (in accordance with the proposed increase in the calculation of the maximum new technology add-on payment amount), which in this instance would be $242,450; and/or using a higher percentage than the proposed 65 percent to calculate the maximum new technology add-on payment amount. We stated in the proposed rule that, if we were to finalize any such changes to the new technology add-on payment for cases involving the use of KYMRIAH® and YESCARTA®, we would also revise our proposed amendments to § 412.88 accordingly.
We refer readers to section II.F.2.c. of this final rule for discussion of the comments we received in response to the proposals and solicitations for public comment above.
After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for KYMRIAH® and YESCARTA®. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of KYMRIAH® and YESCARTA® will be $242,450 for FY 2020; that is, 65 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
e. VYXEOSTM (Cytarabine and Daunorubicin Liposome for Injection)
Jazz Pharmaceuticals, Inc. submitted an application for new technology add-on payments for the VYXEOSTM technology for FY 2019. VYXEOSTM was approved by FDA on August 3, 2017, for the treatment of adults with newly diagnosed therapy-related acute myeloid leukemia (t-AML) or AML with myelodysplasia-related changes (AML-MRC).
Treatment of AML diagnoses usually consists of two phases; remission induction and post-remission therapy. Phase one, remission induction, is aimed at eliminating as many myeloblasts as possible. The most common used remission induction regimens for AML diagnoses are the “7+3” regimens using an antineoplastic and an anthracycline. Cytarabine and daunorubicin are two commonly used drugs for “7+3” remission induction therapy. Cytarabine is continuously administered intravenously over the course of 7 days, while daunorubicin is intermittently administered intravenously for the first 3 days. The “7+3” regimen typically achieves a 70 to 80 percent complete remission (CR) rate in most patients under 60 years of age.
VYXEOSTM is a nano-scale liposomal formulation containing a fixed combination of cytarabine and daunorubicin in a 5:1 molar ratio. This formulation was developed by the applicant using a proprietary system known as CombiPlex. According to the applicant, CombiPlex addresses several fundamental shortcomings of conventional combination regimens, specifically the conventional “7+3” free drug dosing, as well as the challenges inherent in combination drug development, by identifying the most effective synergistic molar ratio of the drugs being combined in vitro, and fixing this ratio in a nano-scale drug delivery complex to maintain the optimized combination after administration and ensuring exposure of this ratio to the tumor.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for VYXEOSTM and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved VYXEOSTM for new technology add-on payments for FY 2019 (83 FR 41304). Cases involving VYXEOSTM that are eligible for new technology add-on payments are identified by ICD-10-PCS procedure codes XW033B3 (Introduction of cytarabine and caunorubicin liposome antineoplastic into peripheral vein, percutaneous approach, new technology group 3) or XW043B3 (Introduction of cytarabine and daunorubicin liposome antineoplastic into central vein, percutaneous approach, new technology group 3). In its application, the applicant estimated that the average cost of a single vial for VYXEOSTM is $7,750 (daunorubicin 44 mg/m2 and cytarabine 100 mg/m2). As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41305), we computed a maximum average of 9.4 vials used in the inpatient hospital setting with the maximum average cost for VYXEOSTM used in the inpatient hospital setting equaling $72,850 ($7,750 cost per vial * 9.4 vials). Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of VYXEOSTM is $36,425 for FY 2019.
With regard to the newness criterion for VYXEOSTM, we consider the beginning of the newness period to commence when VYXEOSTM was approved by the FDA (August 3, 2017). As discussed previously in this section, in general, we extend new technology add-on payments for an additional year only if the 3-year anniversary date of the product's entry onto the U.S. market occurs in the latter half of the upcoming fiscal year. Because the 3-year anniversary date of the entry of the VYXEOSTM onto the U.S. market (August 3, 2020) will occur in the second half of FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19279 through 19280), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of VYXEOSTM would be $47,353.50 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving VYXEOSTM would remain at $36,425 for FY 2020. We invited public comments on our proposals to continue new technology add-on payments for VYXEOSTM for FY 2020.
Comment: A commenter supported CMS' proposal to continue new technology add-on payments for FY 2020 for VYXEOSTM.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for VYXEOSTM for FY 2020. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of VYXEOSTM will be $47,352.50 for FY 2020; that is, 65 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
f. VABOMERETM (meropenem-vaborbactam)
Melinta Therapeutics, Inc., submitted an application for new technology add-on payments for VABOMERETM for FY 2019. VABOMERETM is indicated for use in the treatment of adult patients who have been diagnosed with complicated urinary tract infections (cUTIs), including pyelonephritis, caused by designated susceptible bacteria. VABOMERETM received FDA approval on August 29, 2017.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for VABOMERETM and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved VABOMERETM for new technology add-on payments for FY 2019 (83 FR 41311). We noted in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41311) that the applicant did not request approval for the use of a unique ICD-10-PCS procedure code for VABOMERETM for FY 2019 and that as a result, hospitals would be unable to uniquely identify the use of VABOMERETM on an inpatient claim using the typical coding of an ICD-10-PCS procedure code. We noted that in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53352), with regard to the oral drug DIFICIDTM, we revised our policy to allow for the use of an alternative code set to identify oral medications where no inpatient procedure is associated for the purposes of new technology add-on payments. We established the use of a NDC as the alternative code set for this purpose and described our rationale for this particular code set. This change was effective for payments for discharges occurring on or after October 1, 2012. In the FY 2019 IPPS/LTCH PPS final rule, we acknowledged that VABOMERETM is not an oral drug and is administered by IV infusion, but it was the first approved new technology aside from an oral drug with no uniquely assigned inpatient procedure code. Therefore, we believed that the circumstances with respect to the identification of eligible cases using VABOMERETM are similar to those addressed in the FY 2013 IPPS/LTCH PPS final rule with regard to DIFICIDTM because we did not have current ICD-10-PCS code(s) to uniquely identify the use of VABOMERETM to make the new technology add-on payment. We stated that because we have determined that VABOMERETM has met all of the new technology add-on payment criteria and cases involving the use of VABOMERETM would be eligible for such payments for FY 2019, we needed to use an alternative coding method to identify these cases and make the new technology add-on payment for use of VABOMERETM in FY 2019. Therefore, for the reasons discussed in the FY 2019 IPPS/LTCH PPS final rule and similar to the policy in the FY 2013 IPPS/LTCH PPS final rule, cases involving VABOMERETM that are eligible for new technology add-on payments for FY 2019 are identified by National Drug Codes (NDC) 65293-0009-01 or 70842-0120-01 (VABOMERETM Meropenem-Vaborbactam Vial).
According to the applicant, the cost of VABOMERETM is $165 per vial. A patient receives two vials per dose and three doses per day. Therefore, the per-day cost of VABOMERETM is $990 per patient. The duration of therapy, consistent with the Prescribing Information, is up to 14 days. Therefore, the estimated cost of VABOMERETM to the hospital, per patient, is $13,860. We stated in the FY 2019 IPPS/LTCH PPS final rule that based on the limited data from the product's launch, approximately 80 percent of VABOMERETM's usage would be in the inpatient hospital setting, and approximately 20 percent of VABOMERETM's usage may take place outside of the inpatient hospital setting. Therefore, the average number of days of VABOMERETM administration in the inpatient hospital setting is estimated at 80 percent of 14 days, or approximately 11.2 days. As a result, the total inpatient cost for VABOMERETM is $11,088 ($990 * 11.2 days). Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of VABOMERETM is $5,544 for FY 2019.
With regard to the newness criterion for VABOMERETM, we consider the beginning of the newness period to commence when VABOMERETM received FDA approval (August 29, 2017). As discussed previously in this section, in general, we extend new technology add-on payments for an additional year only if the 3-year anniversary date of the product's entry onto the U.S. market occurs in the latter half of the upcoming fiscal year. Because the 3-year anniversary date of the entry of VABOMERETM onto the U.S. market (August 29, 2020) will occur during the second half of FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19280 through 19281), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of VABOMERETM would be $7,207.20 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving VABOMERETM would remain at $5,544 for FY 2020.
As we previously noted in this rule and in the proposed rule, because there was no ICD-10-PCS code(s) to uniquely identify the use of VABOMERETM, we indicated in the FY 2019 IPPS/LTCH PPS final rule that FY 2019 cases involving the use of VABOMERETM that are eligible for the FY 2019 new technology add-on payments would be identified using an NDC code. Subsequent to the issuance of that final rule, new ICD-10-PCS codes XW033N5 (Introduction of Meropenem-vaborbactam Anti-infective into Peripheral Vein, Percutaneous Approach, New Technology Group 5) and XW043N5 (Introduction of Meropenem-vaborbactam Anti-infective into Central Vein, Percutaneous Approach, New Technology Group 5) were finalized to identify cases involving the use of VABOMERETM, effective October 1, 2019, as shown in Table 6B—New Procedure Codes, associated with the FY 2020 IPPS final rule and available via the internet on the CMS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html and then clicking on the link on the left titled “FY 2022 IPPS Final Rule Home Page”. Therefore, we stated in the proposed rule that, for FY 2020, we will use these two ICD-10-PCS codes (XW033N5 and XW043N5) to identify cases involving the use of VABOMERETM that are eligible for the new technology add-on payments.
While these newly approved ICD-10-PCS procedure codes can be used to uniquely identify cases involving the use of VABOMERETM for FY 2020, we stated in the proposed rule that we are concerned that limiting new technology add-on payments only to cases reporting these new ICD-10-PCS codes for FY 2020 could cause confusion because it is possible that some providers may inadvertently continue to bill some claims with the NDC codes rather than the new ICD-10-PCS codes. Therefore, for FY 2020, we proposed that in addition to using the new ICD-10-PCS codes to identify cases involving the use of VABOMERETM, we would also continue to use the NDC codes to identify cases and make the new technology add-on payments. As a result, we proposed that cases involving the use of VABOMERETM that are eligible for new technology add-on payments for FY 2020 would be identified by ICD-10-PCS codes XW033N5 or XW043N5 or NDCs 65293-0009-01 or 70842-0120-01. We invited public comments on our proposal to continue new technology add-on payments for VABOMERETM for FY 2020 and our proposals for identifying and making new technology add-on payments for cases involving the use of VABOMERETM.
Comment: A commenter supported CMS' proposal to continue new technology add-on payments for FY 2020 for VABOMERETM. This commenter also supported CMS' proposal to identify cases involving the use of VABOMERETM that are eligible for new technology add-on payments for FY 2020 using ICD-10-PCS codes XW033N5 or XW043N5 or NDCs 65293-0009-01 or 70842-0120-01.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for VABOMERETM for FY 2020, as well as our proposal to identify cases involving the use of VABOMERETM that are eligible for new technology add-on payments for FY 2020 using ICD-10-PCS codes XW033N5 or XW043N5 or NDCs 65293-0009-01 or 70842-0120-01. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of VABOMERETM will be $8,316 for FY 2020; that is, 75 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
g. remedē® System
Respicardia, Inc. submitted an application for new technology add-on payments for the remedē® System for FY 2019. According to the applicant, the remedē® System is indicated for use as a transvenous phrenic nerve stimulator in the treatment of adult patients who have been diagnosed with moderate to severe central sleep apnea (CSA). The remedē® System consists of an implantable pulse generator, and a stimulation and sensing lead. The pulse generator is placed under the skin, in either the right or left side of the chest, and it functions to monitor the patient's respiratory signals. A transvenous lead for unilateral stimulation of the phrenic nerve is placed either in the left pericardiophrenic vein or the right brachiocephalic vein, and a second lead to sense respiration is placed in the azygos vein. Both leads, in combination with the pulse generator, function to sense respiration and, when appropriate, generate an electrical stimulation to the left or right phrenic nerve to restore regular breathing patterns.
On October 6, 2017, the remedē® System was approved by the FDA as an implantable phrenic nerve stimulator indicated for the use in the treatment of adult patients who have been diagnosed with moderate to severe CSA. The device was available commercially upon FDA approval. Therefore, the newness period for the remedē® System is considered to begin on October 6, 2017.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for the remedē® System and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved the remedē® System for new technology add-on payments for FY 2019. Cases involving the use of the remedē® System that are eligible for new technology add-on payments are identified by ICD-10-PCS procedures codes 0JH60DZ and 05H33MZ in combination with procedure code 05H03MZ (Insertion of neurostimulator lead into right innominate vein, percutaneous approach) or 05H43MZ (Insertion of neurostimulator lead into left innominate vein, percutaneous approach). According to the application, the cost of the remedē® System is $34,500 per patient. Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of the remedē® System is $17,250 for FY 2019 (83 FR 41320).
With regard to the newness criterion for the remedē® System, we consider the beginning of the newness period to commence when the remedē® System was approved by the FDA on October 6, 2017. Because the 3-year anniversary date of the entry of the remedē® System onto the U.S. market (October 6, 2020) will occur after FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19281), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of the remedē® System would be $22,425 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving the remedē® System would remain at $17,250 for FY 2020. We invited public comments on our proposals to continue new technology add-on payments for the remedē® System for FY 2020.
Comment: Several commenters supported CMS' proposal to continue new technology add-on payments for FY 2020 for the remedē® System. A commenter, who was also the applicant, believed that the newness period for the remedē® System should start on February 1, 2018 instead of the FDA approval date of October 6, 2017. The commenter stated that due to the required build out of operational and commercial capabilities, the remedē® System was not commercially available upon FDA approval and the first case involving its use did not occur until February 1, 2018. The commenter asserted that the date of the first implant should mark the start of the newness period as before that the technology was not commercially available.
Several commenters asserted that the descriptor of one of the ICD-10-PCS procedure codes used to uniquely identify cases involving the use of the remedē® System is incorrect. Per the commenters, CMS indicated in the proposed rule that cases involving the use of the remedē® System that are eligible for new technology add-on payments are identified by ICD-10-PCS procedure codes 0JH60DZ and 05H33MZ in combination with procedure code 05H03MZ (Insertion of neurostimulator lead into right innominate vein, percutaneous approach) or 05H43MZ (Insertion of neurostimulator lead into left innominate vein, percutaneous approach). The commenters asserted that the descriptor of the code 05H03MZ was incorrectly stated in the proposed rule as involving the right innominate vein, whereas the correct body part for this code is the azygos vein.
Furthermore, the commenters noted that the codes listed for the remedē® System in the proposed rule do not match the advice that was published in the Fourth Quarter 2016 issue of Coding Clinic for ICD-10-CM/PCS regarding insertion of a phrenic neurostimulator. Per the commenters, the Coding Clinic advised assigning code 0JH60MZ for insertion of the stimulator generator into the chest subcutaneous tissue and fascia and code 05H032Z for the insertion of monitoring device into the azygos vein, plus the appropriate code for insertion of neurostimulator lead into either the left or right innominate vein. The commenters asserted that the device values for both the code for the stimulator generator and the code for the insertion of the lead in the azygos vein in the Coding Clinic advice were different than the ones indicated by CMS in the proposed rule. Commenters indicated that, according to Coding Clinic, for coding purposes, the sensing lead is designated as a monitoring device to differentiate between the sensing lead that monitors the respiratory activity and the electrode that delivers the electrical stimulation. The commenters requested that CMS revisit this topic and revise as applicable the stated codes to identify placement of the remedē® System to be consistent with the advice published in Coding Clinic for ICD-10-CM/PCS. A commenter requested that CMS also make the appropriate retroactive payments consistent with the revised codes.
Response: We appreciate the commenters' support. Regarding newness, we will consider the additional information the applicant provided when proposing whether to continue new technology add-on payments for the remedē® System for FY 2021.
Regarding codes, we acknowledge the error in our description of the ICD-10-PCS procedure code 05H03MZ in the Proposed Rule and agree with the commenters that the correct body part for this code is the azygos vein, not the innominate vein as stated in the Proposed Rule. We also acknowledge that the finalized codes used to identify cases involving the remedē® System that are eligible for the add-on payment differ from those that were published in the Fourth Quarter 2016 issue of Coding Clinic for ICD-10-CM/PCS regarding insertion of a phrenic neurostimulator. However, we believe that the finalized codes from the March 2018 Coordination & Maintenance Committee meeting supercede the Coding Clinic advice for the technology. Therefore, cases involving the remedē® System that are eligible for the add-on payment will continue to be identified with the procedure codes 0JH60DZ (Insertion of multiple array stimulator generator into chest subcutaneous tissue and fascia, open approach) and 05H03MZ (Insertion of neurostimulator lead into azygos vein, percutaneous approach) in combination with procedure code 05H33MZ (Insertion of neurostimulator lead into right innominate vein, percutaneous approach) or 05H43MZ (Insertion of neurostimulator lead into left innominate vein, percutaneous approach).
After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for the remedē® System for FY 2020. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of the remedē® System will be $22,425 for FY 2020; that is, 65 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
h. ZEMDRITM (Plazomicin)
Achaogen, Inc. submitted an application for new technology add-on payments for ZEMDRITM (Plazomicin) for FY 2019. According to the applicant, ZEMDRITM (Plazomicin) is a next-generation aminoglycoside antibiotic, which has been found in vitro to have enhanced activity against many multi-drug resistant (MDR) gram-negative bacteria. The applicant received approval from the FDA on June 25, 2018, for use in the treatment of adults who have been diagnosed with cUTIs, including pyelonephritis.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for ZEMDRITM and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved ZEMDRITM for new technology add-on payments for FY 2019 (83 FR 41334). Cases involving ZEMDRITM that are eligible for new technology add-on payments are identified by ICD-10-PCS procedure codes XW033G4 (Introduction of Plazomicin anti-infective into peripheral vein, percutaneous approach, new technology group 4) or XW043G4 (Introduction of Plazomicin anti-infective into central vein, percutaneous approach, new technology group 4). In its application, the applicant estimated that the average Medicare beneficiary would require a dosage of 15 mg/kg administered as an IV infusion as a single dose. According to the applicant, the WAC for one dose is $330, and patients will typically require 3 vials for the course of treatment with ZEMDRITM per day for an average duration of 5.5 days. Therefore, the total cost of ZEMDRITM per patient is $5,445. Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of ZEMDRITM is $2,722.50 for FY 2019.
With regard to the newness criterion for ZEMDRITM, we consider the beginning of the newness period to commence when ZEMDRITM was approved by the FDA on June 25, 2018. Because the 3-year anniversary date of the entry of ZEMDRITM onto the U.S. market (June 25, 2021) will occur after FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19281 through 19282), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of ZEMDRITM would be $3,539.25 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving ZEMDRITM would remain at $2,722.50 for FY 2020. We invited public comments on our proposals to continue new technology add-on payments for ZEMDRITM for FY 2020.
Comment: A commenter supported CMS' proposal to continue new technology add-on payments for FY 2020 for ZEMDRITM.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for ZEMDRITM for FY 2020. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of ZEMDRITM will be $4,083.75 for FY 2020; that is, 75 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
i. GIAPREZATM
The La Jolla Pharmaceutical Company submitted an application for new technology add-on payments for GIAPREZATM for FY 2019. GIAPREZATM, a synthetic human angiotensin II, is administered through intravenous infusion to raise blood pressure in adult patients who have been diagnosed with septic or other distributive shock.
GIAPREZATM was granted a Priority Review designation under FDA's expedited program and received FDA approval on December 21, 2017, for the use in the treatment of adults who have been diagnosed with septic or other distributive shock as an intravenous infusion to increase blood pressure.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for GIAPREZATM and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved GIAPREZATM for new technology add-on payments for FY 2019 (83 FR 41342). Cases involving GIAPREZATM that are eligible for new technology add-on payments are identified by ICD-10-PCS procedure codes XW033H4 (Introduction of synthetic human angiotensin II into peripheral vein, percutaneous approach, new technology, group 4) or XW043H4 (Introduction of synthetic human angiotensin II into central vein, percutaneous approach, new technology group 4). In its application, the applicant estimated that the average Medicare beneficiary would require a dosage of 20 ng/kg/min administered as an IV infusion over 48 hours, which would require 2 vials. The applicant explained that the WAC for one vial is $1,500, with each episode-of-care costing $3,000 per patient. Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of GIAPREZATM is $1,500 for FY 2019.
With regard to the newness criterion for GIAPREZATM, we consider the beginning of the newness period to commence when GIAPREZATM was approved by the FDA (December 21, 2017). Because the 3-year anniversary date of the entry of GIAPREZATM onto the U.S. market (December 21, 2020) would occur after FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19282), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of GIAPREZATM would be $1,950 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving GIAPREZATM would remain at $1,500 for FY 2020. We invited public comments on our proposals to continue new technology add-on payments for GIAPREZATM for FY 2020.
Comment: A commenter supported CMS' proposal to continue new technology add-on payments for FY 2020 for GIAPREZATM.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for GIAPREZATM for FY 2020. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of GIAPREZATM will be $4,083.75 for FY 2020; that is, 65 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
j. Cerebral Protection System (Sentinel® Cerebral Protection System)
Claret Medical, Inc. submitted an application for new technology add-on payments for the Cerebral Protection System (Sentinel® Cerebral Protection System) for FY 2019. According to the applicant, the Sentinel Cerebral Protection System is indicated for the use as an embolic protection (EP) device to capture and remove thrombus and debris while performing transcatheter aortic valve replacement (TAVR) procedures. The device is percutaneously delivered via the right radial artery and is removed upon completion of the TAVR procedure. The De Novo request for the Sentinel® Cerebral Protection System was granted by FDA on June 1, 2017 (DEN160043).
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for the Sentinel® Cerebral Protection System and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved the Sentinel® Cerebral Protection System for new technology add-on payments for FY 2019 (83 FR 41348). Cases involving the Sentinel® Cerebral Protection System that are eligible for new technology add-on payments are identified by ICD-10-PCS code X2A5312 (Cerebral embolic filtration, dual filter in innominate artery and left common carotid artery, percutaneous approach). In its application, the applicant estimated that the cost of the Sentinel® Cerebral Protection System is $2,800. Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of the Sentinel® Cerebral Protection System is $1,400 for FY 2019.
With regard to the newness criterion for the Sentinel® Cerebral Protection System, we consider the beginning of the newness period to commence when the FDA granted the De Novo request for the Sentinel® Cerebral Protection System (June 1, 2017). As discussed previously in this section, in general, we extend new technology add-on payments for an additional year only if the 3-year anniversary date of the product's entry onto the U.S. market occurs in the latter half of the upcoming fiscal year. Because the 3-year anniversary date of the entry of the Sentinel® Cerebral Protection System onto the U.S. market (June 1, 2020) will occur in the second half of FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19282 through 19283), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of the Sentinel® Cerebral Protection System would be $1,820 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving the Sentinel® Cerebral Protection System would remain at $1,400 for FY 2020. We invited public comments on our proposals to continue new technology add-on payments for the Sentinel® Cerebral Protection System for FY 2020.
Comment: Several commenters supported CMS' proposal to continue new technology add-on payments for FY 2020 for the Sentinel® Cerebral Protection System.
Response: We appreciate the commenters' support. After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for the Sentinel® Cerebral Protection System for FY 2020. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of the Sentinel® Cerebral Protection System will be $1,820 for FY 2020; that is, 65 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
k. The AQUABEAM System (Aquablation)
PROCEPT BioRobotics Corporation submitted an application for new technology add-on payments for the AQUABEAM System (Aquablation) for FY 2019. According to the applicant, the AQUABEAM System is indicated for the use in the treatment of patients experiencing lower urinary tract symptoms caused by a diagnosis of benign prostatic hyperplasia (BPH). The AQUABEAM System consists of three main components: A console with two high-pressure pumps, a conformal surgical planning unit with trans-rectal ultrasound imaging, and a single-use robotic hand-piece. The applicant reported that the AQUABEAM System provides the operating surgeon a multi-dimensional view, using both ultrasound image guidance and endoscopic visualization, to clearly identify the prostatic adenoma and plan the surgical resection area. The applicant stated that, based on the planning inputs from the surgeon, the system's robot delivers Aquablation, an autonomous waterjet ablation therapy that enables targeted, controlled, heat-free and immediate removal of prostate tissue used for the purpose of treating lower urinary tract symptoms caused by a diagnosis of BPH. Per the applicant, the combination of surgical mapping and robotically-controlled resection of the prostate is designed to offer predictable and reproducible outcomes, independent of prostate size, prostate shape or surgeon experience.
The FDA granted the AQUABEAM System's De Novo request on December 21, 2017, for use in the resection and removal of prostate tissue in males suffering from lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia. The applicant stated that the AQUABEAM System was made available on the U.S. market immediately after the FDA granted the De Novo request.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for the AQUABEAM System and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved the AQUABEAM System for new technology add-on payments for FY 2019 (83 FR 41355). Cases involving the AQUABEAM System that are eligible for new technology add-on payments are identified by ICD-10-PCS code XV508A4 (Destruction of prostate using robotic waterjet ablation, via natural or artificial opening endoscopic, new technology group 4). The applicant estimated that the average Medicare beneficiary would require the transurethral procedure of one AQUABEAM System per patient. According to the application, the cost of the AQUABEAM System is $2,500 per procedure. Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of the AQUABEAM System's Aquablation System is $1,250 for FY 2019.
With regard to the newness criterion for the AQUABEAM System, we consider the beginning of the newness period to commence on the date the FDA granted the De Novo request (December 21, 2017). As noted previously and in the FY 2019 rulemaking, the applicant stated that the AQUABEAM System was made available on the U.S. market immediately after the FDA granted the De Novo request.
We note that in the FY 2019 IPPS/LTCH PPS final rule, we inadvertently misstated the newness period beginning date as April 19, 2018 (83 FR 41351). As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41350), in its public comment in response to the FY 2019 IPPS/LTCH PPS proposed rule, the applicant explained that, while the AQUABEAM System received approval from the FDA for its De Novo request on December 21, 2017, local non-coverage determinations in the Medicare population resulted in the first case being delayed until April 19, 2018. Therefore, the applicant believed that the newness period should begin on April 19, 2018, instead of the date FDA granted the De Novo request. In the final rule, we responded that with regard to the beginning of the technology's newness period, as discussed in the FY 2005 IPPS final rule (69 FR 49003), the timeframe that a new technology can be eligible to receive new technology add-on payments begins when data begin to become available. While local non-coverage determinations may limit the use of a technology in different regions in the country, a technology may be available in regions where no local non-coverage decision existed (with data beginning to become available). We also explained that under our historical policy we do not consider how frequently the medical service or technology has been used in the Medicare population in our determination of newness (as discussed in the FY 2006 IPPS final rule (70 FR 47349)). We stated in the FY 2019 IPPS/LTCH PPS proposed rule that consistent with this response, and as indicated in the FY 2019 proposed rule and elsewhere in the final rule, we believe the beginning of the newness period to commence on the first day the AQUABEAM System was commercially available (December 21, 2017). As noted, the later statement that the newness period beginning date for the AQUABEAM System is April 19, 2018 was an inadvertent error. We stated in the FY 2020 IPPS/LTCH PPS proposed rule that, as we indicated in the FY 2019 IPPS/LTCH PPS final rule, we welcomed further information from the applicant for consideration regarding the beginning of the newness period.
Because the 3-year anniversary date of the entry of the AQUABEAM System onto the U.S. market (December 21, 2020) will occur after FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19283), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of the AQUABEAM System would be $1,625 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving the AQUABEAM System would remain at $1,250 for FY 2020. We invited public comments on our proposals to continue new technology add-on payments for the AQUABEAM System for FY 2020.
Comment: A few commenters supported CMS' proposal to continue new technology add-on payments for the AQUABEAM System for FY 2020.
Several commenters disagreed with CMS' belief that the newness period for the AQUABEAM System commenced on December 21, 2017, the day that FDA granted the De Novo request for the AQUABEAM System. These commenters, including the applicant, asserted that the American Medical Association assigned Aquablation therapy to a Category III CPT code prior to FDA clearance, and as a result Aquablation therapy was non-covered by all Medicare Administrative Contractors prior to the date of FDA clearance through to the present day. Per the commenters, this is equivalent to a uniform, non-coverage policy for the entire nation. The commenters further stated that CMS has consistently recognized that the start of the newness period can occur months after FDA approval if there are delays in availability—including nationwide non-coverage—as indicated in the FY 2005 IPPS Final Rule, the FY 2006 IPPS Final Rule, and the CY 2016 OPPS Final Rule. The commenters asserted that based on longstanding rules and policy statements, the appropriate beginning of the newness period for the AQUABEAM System should be April 19, 2018, or the date of the first procedure in a commercially-insured patient.
Response: We appreciate the commenters' support. With regard to newness, we note that Category III CPT codes are not recognized on inpatient claims. We continue to consider the beginning of the newness period for the AQUABEAM System to commence on December 21, 2017, or the date the FDA granted the applicant's De Novo request.
After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for the AQUABEAM System for FY 2020. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of the AQUABEAM System will be $1,625 for FY 2020; that is, 65 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
l. AndexXaTM (Andexanet alfa)
Portola Pharmaceuticals, Inc. (Portola) submitted an application for new technology add-on payments for FY 2019 for the use of AndexXaTM (Andexanet alfa).
AndexXaTM received FDA approval on May 3, 2018, and is indicated for use in the treatment of patients who are receiving treatment with rivaroxaban and apixaban, when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
After evaluation of the newness, costs, and substantial clinical improvement criteria for new technology add-on payments for AndexXaTM and consideration of the public comments we received in response to the FY 2019 IPPS/LTCH PPS proposed rule, we approved AndexXaTM for new technology add-on payments for FY 2019 (83 FR 41362). Cases involving the use of AndexXaTM that are eligible for new technology add-on payments are identified by ICD-10-PCS procedure codes XW03372 (Introduction of Andexanet alfa, Factor Xa inhibitor reversal agent into peripheral vein, percutaneous approach, new technology group 2) or XW04372 (Introduction of Andexanet alfa, Factor Xa inhibitor reversal agent into central vein, percutaneous approach, new technology group 2). The applicant explained that the WAC for 1 vial is $2,750, with the use of an average of 10 vials for the low dose and 18 vials for the high dose. The applicant noted that per the clinical trial data, 90 percent of cases were administered a low dose and 10 percent of cases were administered the high dose. The weighted average between the low and high dose is an average of 10.22727 vials. Therefore, the cost of a standard dosage of AndexXaTM is $28,125 ($2,750 × 10.22727). Under existing § 412.88(a)(2), we limit new technology add-on payments to the lesser of 50 percent of the average cost of the technology or 50 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of AndexXaTM is $14,062.50 for FY 2019.
With regard to the newness criterion for AndexXaTM, we consider the beginning of the newness period to commence when AndexXaTM received FDA approval (May 3, 2018). Because the 3-year anniversary date of the entry of AndexXaTM onto the U.S. market (May 3, 2021) will occur after FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19283 through 19284), we proposed to continue new technology add-on payments for this technology for FY 2020. In addition, under the proposed change to the calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of the proposed rule (84 FR 19373), we proposed that the maximum new technology add-on payment amount for a case involving the use of AndexXaTM would be $18,281.25 for FY 2020; that is, 65 percent of the average cost of the technology. However, we stated that if we did not finalize the proposed change to the calculation of the new technology add-on payment amount, we were proposing that the maximum new technology add-on payment for a case involving AndexXaTM would remain at $14,062.50 for FY 2020. We invited public comments on our proposals to continue new technology add-on payments for AndexXaTM for FY 2020.
Comment: A commenter supported CMS' proposal to continue new technology add-on payments for FY 2020 for AndexXaTM.
Response: We appreciate the commenter's support. After consideration of the public comments we received, we are finalizing our proposal to continue new technology add-on payments for AndexXaTM for FY 2020. Under the revised calculation of the new technology add-on payment amount discussed in section II.H.9. of the preamble of this final rule, the maximum new technology add-on payment amount for a case involving the use of AndexXaTM will be $18,281.25 for FY 2020; that is, 65 percent of the average cost of the technology. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
5. FY 2020 Applications for New Technology Add-On Payments
We received 18 applications for new technology add-on payments for FY 2020. In accordance with the regulations under § 412.87(c), applicants for new technology add-on payments must have FDA approval or clearance by July 1 of the year prior to the beginning of the fiscal year for which the application is being considered. One applicant withdrew its application prior to the issuance of the proposed rule.
Since the issuance of the FY 2020 IPPS/LTCH PPS proposed rule, three applicants, AbbVie Pharmaceuticals, Inc. (the applicant for VENCLEXTA®), Somahlution, Inc. (the applicant for DURAGRAFT®), and Nabriva Therapeutics U.S., Inc. (the applicant for CONTEPOTM), withdrew their applications. One applicant, Merck & Co., Inc (the applicant for Imipenem, Cilastatin, and Relebactam (IMI/REL) Injection), did not meet the deadline of July 1 for FDA approval or clearance of the technology and, therefore, the technology is not eligible for consideration for new technology add-on payments for FY 2020. A discussion of the remaining 13 applications is presented in this final rule.
a. AZEDRA® (Ultratrace® iobenguane Iodine-131) Solution
Progenics Pharmaceuticals, Inc. submitted an application for new technology add-on payments for AZEDRA® (Ultratrace® iobenguane Iodine-131) for FY 2020. (We note that Progenics Pharmaceuticals, Inc. previously submitted an application for new technology add-on payments for AZEDRA® for FY 2019, which was withdrawn prior to the issuance of the FY 2019 IPPS/LTCH PPS final rule.) AZEDRA® is a drug solution formulated for intravenous (IV) use in the treatment of patients who have been diagnosed with obenguane avid malignant and/or recurrent and/or unresectable pheochromocytoma and paraganglioma (PPGL). AZEDRA® contains a small molecule ligand consisting of meta-iodobenzylguanidine (MIBG) and131 Iodine (131 I) (hereafter referred to as “131 I-MIBG”). The applicant noted that iobenguane Iodine-131 is also known as131 I-MIBG.
The applicant reported that PPGLs are rare tumors with an incidence of approximately 2 to 8 people per million per year.[2 3] Both tumors are catecholamine-secreting neuroendocrine tumors, with pheochromocytomas being the more common of the two and comprising 80 to 85 percent of cases. While 10 percent of pheochromocytomas are malignant, whereby “malignant” is defined by the World Health Organization (WHO) as “the presence of distant metastases,” paragangliomas have a malignancy frequency of 25 percent.[4 5] Approximately one-half of malignant tumors are pronounced at diagnosis, while other malignant tumors develop slowly within 5 years.[6] Pheochromocytomas and paragangliomas tend to be indistinguishable at the cellular level and frequently at the clinical level. For example catecholamine-secreting paragangliomas often present clinically like pheochromocytomas with hypertension, episodic headache, sweating, tremor, and forceful palpitations.[7] Although pheochromocytomas and paragangliomas can share overlapping histopathology, epidemiology, and molecular pathobiology characteristics, there are differences between these two neuroendocrine tumors in clinical behavior, aggressiveness and metastatic potential, biochemical findings and association with inherited genetic syndrome differences, highlighting the importance of distinguishing between the presence of malignant pheochromocytoma and the presence of malignant paraganglioma. At this time, there is no curative treatment for malignant pheochromocytomas and paragangliomas. Successful management of these malignancies requires a multidisciplinary approach of decreasing tumor burden, controlling endocrine activity, and treating debilitating symptoms. According to the applicant, decreasing metastatic tumor burden would address the leading cause of mortality in this patient population, where the 5-year survival rate is 50 percent for patients with untreated malignant pheochromocytomas and paragangliomas.[8] The applicant stated that controlling catecholamine hypersecretion (for example, severe paroxysmal or sustained hypertension, palpitations and arrhythmias) would also mean decreasing morbidity associated with hypertension (for example, risk of stroke, myocardial infarction and renal failure), and begin to address the 30-percent cardiovascular mortality rate associated with malignant pheochromocytomas and paragangliomas.
The applicant reported that, prior to the introduction of AZEDRA®, controlling catecholamine activity in pheochromocytomas and paragangliomas was medically achieved with administration of combined alpha and beta-adrenergic blockade, and surgically with tumor tissue reduction. Because there is no curative treatment for malignant pheochromocytomas and paragangliomas, resecting both primary and metastatic lesions whenever possible to decrease tumor burden [9] provides a methodology for controlling catecholamine activity and lowering cardiovascular mortality risk. Besides surgical removal of tumor tissue for lowering tumor burden, there are other treatment options that depend upon tumor type (that is, pheochromocytoma tumors versus paraganglioma tumors), anatomic location, and the number and size of the metastatic tumors. These treatment options include: (1) Radiation therapy; (2) nonsurgical local ablative therapy with radiofrequency ablation, cryoablation, and percutaneous ethanol injection; (3) transarterial chemoembolization for liver metastases; and (4) radionuclide therapy using metaiodobenzylguanidine (MIBG) or somatostatin. Regardless of the method to reduce local tumor burden, periprocedural medical care is needed to prevent massive catecholamine secretion and hypertensive crisis.[10]
The applicant stated that AZEDRA® specifically targets neuroendocrine tumors arising from chromaffin cells of the adrenal medulla (in the case of pheochromocytomas) and from neuroendocrine cells of the extra-adrenal autonomic paraganglia (in the case of paragangliomas).[11] According to the applicant, AZEDRA® is a more consistent form of[131] I-MIBG compared to compounded formulations of[131] I-MIBG that are not approved by the FDA. AZEDRA® (iobenguane I 131) (AZEDRA) was approved by the FDA on July 30, 2018, and according to the applicant, is the first and only drug indicated for the treatment of adult and pediatric patients 12 years and older who have been diagnosed with iobenguane scan positive, unresectable, locally advanced or metastatic pheochromocytoma or paraganglioma who require systemic anticancer therapy. Among local tumor tissue reduction options, use of external beam radiation therapy (EBRT) at doses greater than 40 Gy can provide local pheochromocytoma and paraganglioma tumor control and relief of symptoms for tumors at a variety of sites, including the soft tissues of the skull base and neck, abdomen, and thorax, as well as painful bone metastases.[12] However, the applicant stated that EBRT irradiated tissues are unresponsive to subsequent treatment with[131] I- MIBG radionuclide.[13] MIBG was initially used for the imaging of paragangliomas and pheochromocytomas because of its similarity to noradrenaline, which is taken up by chromaffin cells. Conventional MIBG used in imaging expanded to off-label use in patients who had been diagnosed with malignant pheochromocytomas and paragangliomas. Because[131] I-MIBG is sequestered within pheochromocytoma and paraganglioma tumors, subsequent malignant cell death occurs from radioactivity. Approximately 50 percent of tumors are eligible for treatment involving[131] I-MIBG therapy based on having MIBG uptake with diagnostic imaging. According to the applicant, despite uptake by tumors, studies have also found that[131] I-MIBG therapy has been limited by total radiation dose, hematologic side effects, and hypertension. While the pathophysiology of total radiation dose and hematologic side effects are more readily understandable, hypertension is believed to be precipitated by large quantities of non-iodinated MIBG or “cold” MIBG being introduced along with radioactive[131] I-MIBG therapy.[14] The “cold” MIBG blocks synaptic reuptake of norepinephrine, which can lead to tachycardia and paroxysmal hypertension within the first 24 hours, the majority of which occur within 30 minutes of administration and can be dose-limiting.[15]
The applicant asserted that its new proprietary manufacturing process called Ultratrace® allows AZEDRA® to be manufactured without the inclusion of unlabeled or “cold” MIBG in the final formulation. The applicant also noted that targeted radionuclide MIBG therapy to reduce tumor burden is one of two treatments that have been studied the most. The other treatment is cytotoxic chemotherapy and, specifically, Carboplatin, Vincristine, and Dacarbazine (CVD). The applicant stated that cytotoxic chemotherapy is an option for patients who experience symptoms with rapidly progressive, non-resectable, high tumor burden, and that cytotoxic chemotherapy is another option for a large number of metastatic bone lesions.[16] According to the applicant, CVD was believed to have an effect on malignant pheochromocytomas and paragangliomas due to the embryonic origin being similar to neuroblastomas. The response rates to CVD have been variable between 25 percent and 50 percent.[17 18] These patients experience side effects consistent with chemotherapeutic treatment with CVD, with the added concern of the precipitation of hormonal complications such as hypertensive crisis, thereby requiring close monitoring during cytotoxic chemotherapy.[19] According to the applicant, use of CVD relative to other tumor burden reduction options is not an ideal treatment because of nearly 100 percent recurrence rates, and the need for chemotherapy cycles to be continually readministered at the risk of increased systemic toxicities and eventual development of resistance. Finally, there is a subgroup of patients that are asymptomatic and have slower progressing tumors where frequent follow-up is an option for care.[20] Therefore, the applicant believed that AZEDRA® offers cytotoxic radioactive therapy for the indicated population that avoids harmful side effects that typically result from use of low-specific activity products.
The applicant reported that the recommended AZEDRA® dosage and frequency for patients receiving treatment involving131 I-MIBG therapy for a diagnosis of avid malignant and/or recurrent and/or unresectable pheochromocytoma and paraganglioma tumors is:
- Dosimetric Dosing—5 to 6 micro curies (mCi) (185 to 222 MBq) for a patient weighing more than or equal to 50 kg, and 0.1 mCi/kg (3.7 MBq/kg) for patients weighing less than 50 kg. Each recommended dosimetric dose is administered as an IV injection.
- Therapeutic Dosing—500 mCi (18.5 GBq) for patients weighing more than 62.5 kg, and 8 mCi/kg (296 MBq/kg) for patients weighing less than or equal to 62.5 kg. Therapeutic doses are administered by IV infusion, in ~50 mL over a period of ~30 minutes (100 mL/hour), administered approximately 90 days apart.
With respect to the newness criterion, the applicant indicated that FDA granted Orphan Drug designation for AZEDRA® on January 18, 2006, followed by Fast Track designation on March 8, 2006, and Breakthrough Therapy designation on July 26, 2015. The applicant's New Drug Application (NDA) proceeded on a rolling basis, and was completed on November 2, 2017. AZEDRA® was approved by the FDA on July 30, 2018, for the treatment of adult and pediatric patients 12 years and older who have been diagnosed with iobenguane scan positive, unresectable, locally advanced or metastatic pheochromocytoma or paraganglioma who require systemic anticancer therapy through a New Drug Approval (NDA) filed under Section 505(b)(1) of the Federal Food, Drug and Cosmetic Act and 21 CFR 314.50. Currently, there are no approved ICD-10-PCS procedure codes to uniquely identify procedures involving the administration of AZEDRA®. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19286), we noted that the applicant submitted a request for approval for a unique ICD-10-PCS code for the administration of AZEDRA® beginning in FY 2020. The following ICD-10-PCS codes are now assigned for the use of AZEDRA®: XW033S5 (Introduction of Iobenguane I-131 Antineoplastic into Peripheral Vein, Percutaneous Approach, New Technology Group 5), and XW043S5 (Introduction of Iobenguane I-131 Antineoplastic into Central Vein, Percutaneous Approach, New Technology Group 5).
As discussed earlier, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or similar mechanism of action, the applicant stated that while AZEDRA® and low-specific activity conventional I-131 MIBG both target the same transporter sites on the tumor cell surface, the therapies' safety and efficacy outcomes are different. These differences in outcomes are because AZEDRA® is manufactured using the proprietary Ultratrace® technology, which maximizes the molecules that carry the tumoricidal component (I-131 MIBG) and minimizes the extraneous unlabeled component (MIBG, free ligands), which could cause cardiovascular side effects. Therefore, according to the applicant, AZEDRA® is designed to increase efficacy and decrease safety risks, whereas conventional I-131 MIBG uses existing technologies and results in a product that overwhelms the normal reuptake system with excess free ligands, which leads to safety issues as well as decreasing the probability of the131 I-MIBG binding to the tumor cells.
With regard to the second criterion, whether a product is assigned to the same or a different MS-DRG, the applicant noted that there are no specific MS-DRGs for the assignment of cases involving the treatment of patients who have been diagnosed with pheochromocytoma and paraganglioma. We stated in the proposed rule that we believed potential cases representing patients who may be eligible for treatment involving the administration of AZEDRA® would be assigned to the same MS-DRGs as cases representing patients who receive treatment for a diagnosis of iobenguane avid malignant and/or recurrent and/or unresectable pheochromocytoma and paraganglioma. We also refer readers to the cost criterion discussion in this final rule, which includes the applicant's list of the MS-DRGs to which potential cases involving treatment with the administration of AZEDRA® most likely would map.
With regard to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, according to the applicant, AZEDRA® is the only FDA-approved drug indicated for use in the treatment of patients who have been diagnosed with malignant pheochromocytoma and paraganglioma tumors that avidly take up131 I-MIBG and are recurrent and/or unresectable. The applicant stated that these patients face serious mortality and morbidity risks if left untreated, as well as potentially suffer from side effects if treated by available off-label therapies.
The applicant also contended that AZEDRA® can be distinguished from other currently available treatments because it potentially provides the following advantages:
- AZEDRA® will have a very limited impact on normal norepinephrine reuptake due to the negligible amount of unlabeled MIBG present in the dose. Therefore, AZEDRA® is expected to pose a much lower risk of acute drug-induced hypertension.
- There is minimal unlabeled MIBG to compete for the norepinephrine transporter binding sites in the tumor, resulting in more effective delivery of radioactivity.
- Current off-label therapeutic use of131 I is compounded by individual pharmacies with varied quality and conformance standards.
- Because of its higher specific activity (the activity of a given radioisotope per unit mass), AZEDRA® infusion times are significantly shorter than conventional131 I administrations.
Therefore, with these potential advantages, the applicant maintained that AZEDRA® represents an option for the treatment of patients who have been diagnosed with malignant and/or recurrent and/or unresectable pheochromocytoma and paraganglioma tumors, where there is a clear, unmet medical need.
For the reasons cited earlier, the applicant believed that AZEDRA® is not substantially similar to other currently available therapies and/or technologies and meets the “newness” criterion. We invited public comments on whether AZEDRA® is substantially similar to other currently available therapies and/or technologies and meets the “newness” criterion.
Comment: We received multiple comments in support of applicant's assertion that AZEDRA® is not substantially similar to other currently available therapies and/or technologies. A commenter described AZEDRA® as highly unique technology that is unlike any pre-existing treatment with a structure unlike any pre-existing treatment option given the use of the proprietary Ultratrace® technology, leading to increases in efficacy due to its unique “carrier-free” structure with less non-radioactive drug to compete for uptake by tumors. Commenters mentioned that prior to AZEDRA®'s approval, there was no FDA-approved drug treatment for advanced pheochromocytomas and paragangliomas patients. Commenters asserted that compared to other off-label treatments, AZEDRA provides an important new option with substantial clinical improvement in terms of both safety and efficacy for patients with metastatic and/or recurrent and/or unresectable PPGL.
Response: We thank commenters for their input. After consideration of the comments received, we agree that AZEDRA® utilizes a new mechanism of action from prior therapeutic uses of MIBG and therefore is not substantially similar to an existing technology and meets the criteria for “newness.”
With regard to the cost criterion, the applicant conducted an analysis using FY 2015 MedPAR data to demonstrate that AZEDRA® meets the cost criterion. The applicant searched for potential cases representing patients who may be eligible for treatment involving AZEDRA® that had one of the following ICD-9-CM diagnosis codes (which the applicant believed is indicative of diagnosis appropriate for treatment involving AZEDRA®): 194.0 (Malignant neoplasm of adrenal gland), 194.6 (Malignant neoplasm of aortic body and other paraganglia), 209.29 (Malignant carcinoid tumor of other sites), 209.30 (Malignant poorly differentiated neuroendocrine carcinoma, any site), 227.0 (Benign neoplasm of adrenal gland), 237.3 (Neoplasm of uncertain behavior of paraganglia)—in combination with one of the following ICD-9-CM procedure codes describing the administration of a radiopharmaceutical: 00.15 (High-dose infusion interleukin-2); 92.20 (Infusion of liquid brachytherapy radioisotope); 92.23 (Radioisotopic teleradiotherapy); 92.27 (Implantation or insertion of radioactive elements); 92.28 (Injection or instillation of radioisotopes). The applicant reported that the potential cases used for this analysis mapped to MS-DRGs 054 and 055 (Nervous System Neoplasms with and without MCC, respectively), MS-DRG 271 (Other Major Cardiovascular Procedures with CC), MS-DRG 436 (Malignancy of Hepatobiliary System or Pancreas with CC), MS-DRG 827 (Myeloproliferative Disorders or Poorly Differentiated Neoplasms with Major O.R. Procedure with CC), and MS-DRG 843 (Other Myeloproliferative Disorders or Poorly Differentiated Neoplastic Diagnosis with MCC). Due to patient privacy concerns, because the number of cases under each MS-DRG was less than 11 in total, the applicant assumed an equal distribution between these 6 MS-DRGs. Based on the FY 2019 IPPS/LTCH PPS final rule correction notice data file thresholds, the average case-weighted threshold amount was $60,136. Using the identified cases, the applicant determined that the average unstandardized charge per case ranged from $21,958 to $152,238 for the 6 evaluated MS-DRGs. After removing charges estimated to be associated with precursor agents, the applicant used a 3-year inflation factor of 1.1436 (a yearly inflation factor of 1.04574 applied over 3 years), based on the FY 2018 IPPS/LTCH PPS final rule (82 FR 38527), to inflate the charges from FY 2015 to FY 2018. The applicant provided an estimated average of $151,000 per therapeutic dose per patient, based on the wholesale acquisition cost of the drug and the average dosage amount for most patients, with a total cost per patient estimated to be approximately $980,000. After including the cost of the technology, the applicant determined an inflated average case-weighted standardized charge per case of $1,078,631.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19287), we stated that we were concerned with the limited number of cases the applicant analyzed. However, we acknowledged the difficulty in obtaining cost data for such a rare condition. We invited public comments on whether the AZEDRA® technology meets the cost criterion.
Comment: The applicant submitted a comment in response to CMS's concern, stating that although the number of cases under each MS-DRG identified for its analysis included fewer than 11 total cases, the information provided a meaningful and workable data set based on the MedPAR files and is consistent with a product used to treat an ultra-rare disease. Furthermore, the applicant stated that the cost information and analysis submitted with the application demonstrated that AZEDRA® will significantly exceed the relevant cost threshold for the MS-DRGs to which cases map, both in the aggregate (based on case-weighted threshold amounts), and for each individual MS-DRG.
Response: We appreciate the applicant's comment in response to our concerns. After consideration of the public comments we received, we believe that AZEDRA® meets the cost criterion.
With regard to substantial clinical improvement, the applicant maintained that the use of AZEDRA® has been shown to reduce the incidence of hypertensive episodes and use of antihypertensive medications, reduce tumor size, improve blood pressure control, and reduce secretion of tumor biomarkers. In addition, the applicant asserted that AZEDRA® provides a treatment option for those outlined in its indication patient population. The applicant asserted that AZEDRA® meets the substantial clinical improvement criterion based on the results from two clinical studies: (1) MIP-IB12 (IB12): A Phase I Study of Iobenguane (MIBG) I-131 in Patients With Malignant Pheochromocytoma/Paraganglioma; [21] and (2) MIP-IB12B (IB12B): A Study Evaluating Ultratrace® Iobenguane I-131 in Patients With Malignant Relapsed/Refractory Pheochromocytoma/Paraganglioma. The applicant explained that the IB12B study is similar to the IB12 study in that both studies evaluated two open-label, single-arm studies. The applicant reported that both studies included patients who had been diagnosed with malignant and/or recurrent and/or unresectable pheochromocytoma and paraganglioma tumors, and both studies assessed objective tumor response, biochemical tumor response, overall survival rates, occurrence of hypertensive crisis, and the long-term benefit of AZEDRA® treatment relative to the need for antihypertensives. However, according to the applicant, the study designs differed in dose regimens (1 dose administered to patients in the IB12 study, and 2 doses administered to patients in the IB12B study) and primary study endpoints. Differences in the designs of the studies prevented direct comparison of study endpoints and pooling of the data. In addition, the applicant stated that results from safety data from the IB12 study and the IB12B study were pooled and used to support substantial clinical improvement assertions. In the proposed rule, we noted that neither the IB12 study nor the IB12B study compared the effects of the use of AZEDRA® to any of the other treatment options to decrease tumor burden (for example, cytotoxic chemotherapy, radiation therapy, and surgical debulking).
Regarding the data results from the IB12 study, the applicant asserted that, based on the reported safety and tolerability, and primary endpoint of radiological response at 12 months, high-specific-activity I-131 MIBG may be an effective alternative therapeutic option for patients who have been diagnosed with iobenguane-avid, metastatic and/or recurrent pheochromocytoma and paraganglioma tumors for whom there are no other approved therapies and for those patients who have failed available treatment options. In addition, the applicant used the exploratory finding of decreased or discontinuation of anti-hypertensive medications relative to baseline medications as evidence that AZEDRA® has clinical benefit and positive impact on the long-term effects of hypertension induced norepinephrine producing malignant pheochromocytoma and paraganglioma tumors. In the proposed rule, we stated that we understand that the applicant used antihypertensive medications as a proxy to assess the long-term effects of hypertension such as renal, myocardial, and cerebral end organ damage. The applicant reported that it studied 15 of the original IB12 study's 21-patient cohort, and found 33 percent (n=5) had decreased or discontinuation of antihypertensive medications during the 12 months of follow-up. However, the applicant did not provide additional data on the incidence of renal insufficiency/failure, myocardial ischemic/infarction events, or transient ischemic attacks or strokes. Therefore, in the proposed rule, we stated that it is unclear to us if these five patients also had decreased urine metanephrines, changed their diet, lost significant weight, or if other underlying comorbidities that influence hypertension were resolved, making it difficult to understand the significance of this exploratory finding.
Regarding the applicant's assertion that the use of AZEDRA® is safer and more effective than alternative therapies, in the proposed rule we noted that the IB12 study was a dose-escalating study and did not compare current therapies with the use of AZEDRA®. We also noted the following: (1) The average age of the 21 enrolled patients in the IB12 study was 50.4 years old (a range of 30 to 72 years old); (2) the gender distribution was 61.9 percent (n=13) male and 38.1 percent (n=8) female; and (3) 76.2 percent (n=16) were white, 14.3 percent (n=3) were black or African American, and 9.5 percent (n=2) were Asian. We agreed with the study's conductor [22] that the size of the study is a limitation, and with a younger, predominately white, male patient population, generalization of study results to a more diverse population may be difficult. The applicant reported that one other aspect of the patient population indicated that all 21 patients received prior anti-cancer therapy for treatment of malignant pheochromocytoma and paraganglioma tumors, which included the following: 57.1 percent (n=12) received radiation therapy including external beam radiation and conventional MIBG; 28.6 percent (n=6) received cytotoxic chemotherapy (for example, CVD and other chemotherapeutic agents); and 14.3 percent (n=3) received Octreotide.[23] Although this study's patient population illustrates a population that has failed some of the currently available therapy options, which may potentially support a finding of substantial clinical improvement for those with no other treatment options, we stated in the proposed rule that we were unclear which patients benefited from treatment involving AZEDRA®, especially in view of the finding of a Fitzgerald, et al. study cited earlier [24] that concluded tissues previously irradiated by EBRT were found to be unresponsive to subsequent treatment with131 I-MIBG radionuclide. It was not clear in the application how previously EBRT-treated patients who failed EBRT fared with the Response Evaluation Criteria in Solid Tumors (RECIST) scores, biotumor marker results, and reduction in antihypertensive medications. We stated that we also lacked information to draw the same correlation between previously CVD-treated patients and their RECIST scores, biotumor marker results, and reduction in antihypertensive medications.
The applicant asserted that the use of AZEDRA® reduces tumor size and reduces the secretion of tumor biomarkers, thereby providing important clinical benefits to patients. The IB12 study assessed the overall best tumor response based on RECIST.[25] Tumor biomarker response was assessed as complete or partial response for serum chromogranin A and total metanephrines in 80 percent and 64 percent of patients, respectively. The applicant noted that both the overall best tumor response based on RECIST and tumor biomarker response favorable results are at doses higher than 500 mCi. In the proposed rule, we stated that we noticed that tumor burden improvement, as measured by RECIST criteria, showed that none of the 21 patients achieved a complete response. In addition, although 4 patients showed partial response, these 4 patients also experienced dose-limiting toxicity with hematological events, and all 4 patients received administered doses greater than 18.5 GBq (500mCi). We also noted that, regardless of total administered activity (for example, greater than or less than 18.5 GBq (500mCi)), 61.9 percent (n=13) of the 21 patients enrolled in the study had stable disease and 14.3 percent (n=2) of the 14 patients who received greater than administered doses of 18.5 GBq (500mCi) had progressive disease. Finally, we also stated that we noticed that, for most tumor biomarkers, there were no dose relationship trends. We stated that while we appreciate the applicant's contention that there is no other FDA-approved drug therapy for patients who have been diagnosed with131 I-MIBG avid malignant and/or recurrent and/or unresectable pheochromocytoma and paraganglioma tumors, we had questions as to whether the overall tumor best response and overall best tumor biomarker data results from the IB12 study support a finding that the use of the AZEDRA® technology represents a substantial clinical improvement.
Finally, regarding the applicant's assertion that, based on the IB12 study data, AZEDRA® provides a safe alternative therapy for those patients who have failed other currently available treatment therapies, we stated in the proposed rule that we noted none of the patients experienced hypertensive crisis, and that 76 percent (n=16) of the 21 patients enrolled in the study experienced Grade III or IV adverse events. Although the applicant indicated the adverse events were related to the study drug, the applicant also noted that there was no statistically significant difference between the greater than or less than 18.5 GBq administered doses; both groups had adverse events rates greater than 75 percent. Specifically, 5 of 7 patients (76 percent) who received less than or equal to 18.5 GBq administered doses, and 11 of 14 patients (79 percent) who received greater than 18.5 GBq administered doses experienced Grade III or IV adverse advents. The most common (greater than or equal to 10 percent) Grade III and IV adverse events were neutropenia, leukopenia, thrombocytopenia, nausea, and vomiting. We also noted that: (1) There were 5 deaths during the study that occurred from approximately 2.5 months up to 22 months after treatment and there was no detailed data regarding the 5 deaths, especially related to the total activity received during the study; (2) there was no information about which patients received prior radiation therapy with EBRT and/or conventional MIBG relative to those who experienced Grade III or IV adverse events; and (3) the total lifetime radiation dose was not provided by the applicant.
The applicant provided study data results from the IB12B study (MIP-IB12B), an open-label, prospective 5-year follow-up, single-arm, multi-center, Phase II pivotal study to evaluate the safety and efficacy of the use of AZEDRA® for the treatment of patients who have been diagnosed with malignant and/or recurrent pheochromocytoma and paraganglioma tumors to support the assertion of substantial clinical improvement. The applicant reported that the IB12B's primary endpoint is the proportion of patients with a reduction (including discontinuation) of all anti-hypertensive medication by at least 50 percent for at least 6 months. Seventy-four patients who received at least 1 dosimetric dose of AZEDRA® were evaluated for safety and 68 patients who received at least 1 therapeutic dose of AZEDRA®, each at 500 mCi (or 8 mCi/kg for patients weighing less than or equal to 62.5 kg), were assessed for specific clinical outcomes. The applicant asserted that results from this prospective study met the primary endpoint (reduction or discontinuation of anti-hypertensive medications), as well as demonstrated strong supportive evidence from key secondary endpoints (overall tumor response, tumor biomarker response, and overall survival rates) that confers important clinical relevance to patients who have been diagnosed with malignant pheochromocytoma and paraganglioma tumors. The applicant also indicated that the use of AZEDRA® was shown to be generally well tolerated at doses administered at 8 mCi/kg. In the proposed rule, we stated that we noted the data results from the IB12B study did not have a comparator arm, making it difficult to interpret the clinical outcome data relative to other currently available therapies.
As discussed for the IB12 study, the applicant reported that antihypertension treatment was a proxy for effectiveness of the use of AZEDRA® on norepinephrine induced hypertension producing tumors. In the IB12B study, 25 percent (17/68) of patients met the primary endpoint of having a greater than 50 percent reduction in anti-hypertensive agents for at least 6 months. The applicant further indicated that an additional 16 patients showed a greater than 50 percent reduction in anti-hypertensive agents for less than 6 months, and by pooling data results from these 33 patients the applicant concluded that 49 percent (33/68) of patients achieved a greater than 50 percent reduction at any time during the study's 12-month follow-up period. The study's primary endpoint data also revealed that 11 percent of the 88 patients who received a therapeutic dose of AZEDRA® experienced a worsening of preexisting hypertension defined as an increase in systolic blood pressure to ≥160 mmHg with an increase of 20 mmHg or an increase in diastolic blood pressure ≥100 mmHg with an increase of 10 mmHg. All changes in blood pressure occurred within the first 24 hours post infusion. The applicant further compared its data results from the IB12B study regarding antihypertension medication and the frequency of post-infusion hypertension with published studies on MIBG and CVD therapy. The applicant noted a retrospective analysis of CVD therapy of 52 patients who had been diagnosed with metastatic pheochromocytoma and paraganglioma tumors that found only 15 percent of CVD-treated patients achieved a 50-percent reduction in anti-hypertensive agents. The applicant also compared its data results for post-infusion hypertension with literature reporting on MIBG and found 14 and 19 percent (depending on the study) of patients receiving MIBG experience hypertension within 24 hours of infusion. Comparatively, the applicant stated that the use of AZEDRA® had no acute events of hypertension following infusion.
Regarding reduction in tumor burden (as defined by RECIST scores), the applicant indicated that at the conclusion of the IB12B study's 12-month follow-up period, 23.4 percent (n=15) of the 68 patients showed a partial response, 68.8 percent (n=44) of the 68 patients achieved stable disease, and 4.7 percent (n=3) of the 68 patients showed progressive disease. None of the patients showed completed response. The applicant maintained that achieving stable disease is important for patients who have been treated for malignant pheochromocytoma and paraganglioma tumors because this is a progressive disease without a cure at this time. The applicant also indicated that literature shows that stable disease is maintained in approximately 47 percent of treatment naïve patients who have been diagnosed with metastatic pheochromocytoma and paraganglioma tumors at 1 year due to the indolent nature of the disease.[26] In the IB12B study, the data results equated to 23 percent of patients achieving partial response and 69 percent of patients achieving stable disease. According to the applicant, this compares favorably to treatment with both conventional radiolabeled MIBG and CVD chemotherapy.
The applicant stated that the data results demonstrated effective tumor response rates. The applicant reported that the IB12 and IB12B study data showed overall tumor response rates of 80 percent and 92 percent, respectively. In addition, the applicant contended that the study data across both trials show that patients demonstrated improved blood pressure control, reductions in tumor biomarker secretion, and strong evidence in overall survival rates. The overall median time to death from the first dose was 36.7 months in all treated patients. Patients who received 2 therapeutic doses had an overall median survival rate of 48.7 months, compared to 17.5 months for patients who only received a single dose. In the proposed rule, we stated that we noted the IB12B study reported 12-month Kaplan-Meier estimate of survival of 91 percent, while the drug dosing study IB12 reported overall subject survival of 86 percent at 12 months, 62 percent at 24 months, 38 percent at 36 months, and 4.8 percent at 48 months. We also noted that only 45 of 68 patients who received at least 1 therapeutic dose completed the 12-month efficacy phase.
The applicant indicated that comparison of the IB12B study data regarding overall survival rate with historical data is difficult due to the differences in the retrospective nature of the published clinical studies and heterogeneous patient characteristics, especially when overall survival is calculated from the time of initial diagnosis. In the proposed rule, we stated that we agreed with the applicant regarding the difficulties in comparing the results of the published clinical studies, and also believed that the differences in these studies may make it more difficult to evaluate whether the use of the AZEDRA® technology improves overall survival rates relative to other therapies.
We stated that we acknowledge the challenges with constructing robust clinical studies due to the extremely rare occurrence of patients who have been diagnosed with pheochromocytoma and paraganglioma tumors. However, in the proposed rule, we stated we were concerned that because the data for both of these studies is mainly based upon retrospective studies and small, heterogeneous patient cohorts, it is difficult to draw precise conclusions regarding efficacy. We stated that only very limited nonpublished data from two, single-arm, noncomparative studies were available to evaluate the safety and effectiveness of AZEDRA®, leading to a comparison of outcomes with historical controls.
We invited public comments on whether the use of the AZEDRA® technology meets the substantial clinical improvement criterion, including with respect to the specific concerns we had raised, which included whether the safety data profile from the IB12 study supports a finding that the use of AZEDRA® represents a substantial clinical improvement for patients who received treatment with131 I-MIBG for a diagnosis of avid malignant and/or recurrent and/or unresectable PPGL tumors, and whether the data results regarding hypertension support a finding that the use of the AZEDRA® technology represents a substantial clinical improvement, and if anti-hypertensive medication reduction is an adequate proxy for improvement in renal, cerebral, and myocardial end organ damage.
Comment: We received multiple comments in support of AZEDRA®'s meeting the substantial clinical improvement criterion. Commenters stated that the clinical data demonstrates important benefits and meaningful clinical improvements for patients compared to other treatments that may be unavailable to patients with advanced PPGL. Commenters stated that certain drug treatments have been used that are not specifically approved by FDA, such as certain chemotherapy regimens or low specific-activity iobenguane I-131, are not effective and frequently lead to serious and harmful side effects, including chemical toxicity and acute hypertensive crisis. Another commenter encouraged CMS to consider the very rare nature of advanced PPGL when considering the sizes of the clinical study patient populations and other aspects of the information relating to AZEDRA®'s application, particularly when a therapy is for an orphan condition and/or is the first and only FDA approved treatment option for the relevant patient population.
The applicant also provided comments regarding substantial clinical improvement. The applicant highlighted AZEDRA®'s FDA “Breakthrough Therapy”, “Fast Track”, “Priority Review”, and “Orphan Drug” designations to demonstrate the meaningful efficacy and safety criteria that a product must meet to obtain these statuses. The applicant also reiterated its contention that AZEDRA® represents a substantial clinical improvement over currently available treatments because it (1) offers a treatment option for a patient population that is unresponsive to or ineligible for currently available treatments for advanced disease and (2) significantly improves clinical outcomes compared to existing treatments for patients who have advanced PPGL and require systemic anticancer treatment. The applicant also responded to some specific issues raised by CMS in the proposed rule. The applicant pointed out that at one point, CMS incorrectly described the IB12B and IB12 as “retrospective” studies, when in fact they were prospective in nature. The applicant clarified that, consistent with prospectively designed clinical trials, the protocol for IB12B included pre-specified endpoints that were statistically powered to demonstrate clinical benefit for patients with advanced PPGL. These endpoints and statistical analyses were used to define the study's success criteria prior to collecting any subject data to prevent the possibility of bias. As such, Study IB12B was a prospective study, specifically designed to demonstrate that AZEDRA® offers a treatment option for a patient population that is unresponsive to or ineligible for currently available treatments. The applicant also provided background to support its claim that the number of patients enrolled in IB12B was statistically meaningful and noteworthy for a last-line therapy study for an ultra-rare disease state.
In response to CMS's concern whether safety data from the IB12 study could provide relevant clinical improvement data, the applicant stated that while the IB12 study was prospectively designed to assess the safety, dosimetry, and preliminary efficacy for AZEDRA® in patients with advanced PPGL, it included several secondary efficacy endpoints that provide preliminary data such as overall tumor response (RECIST), biochemical tumor response, and survival time. The applicant stated that the overall tumor response endpoints were included in FDA's consideration of AZEDRA®'s efficacy, although it was not included in the final AZEDRA® prescribing information.
The applicant stated the primary endpoint of reduction in antihypertension medication was selected because a more traditional endpoint, such as overall survival, was not practical or possible given the nature of PPGL. The applicant stated: “PPGL may progress slowly, and overall have a variable natural history, which makes the use of a traditional endpoint such as overall survival difficult and time-consuming.” According to the applicant, the endpoint was chosen to evaluate a key cause of morbidity in PPGL and thereby reflect direct clinical benefit.
Response: We appreciate the additional information provided by the applicant, and the input from all commenters. After a review of the public comments we received, and upon review of all information provided by the applicant and review of the FDA Evaluation and Review of AZEDRA®'s NDA/BLA 209607 (https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/021200Orig1s015MultidisciplineR.pdf), we believe the technology offers a treatment option for the FDA indicated approved population for whom no other FDA approved treatment is available. Additionally, we note that, per the FDA's Multidisciplinary Evaluation and Review, use of the technology suggested a durable response in the reduction of hypertension as measured by the primary endpoint plus the confirmed overall tumor response measures of direct clinical benefit in this population of patients with serious, life threatening and rare disease (https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/021200Orig1s015MultidisciplineR.pdf pages 12, 20). CMS also notes FDA's adverse events of cytopenias, sialoadenitis and renal failure in those who received two doses of 131I-MIBG, as well as the most common adverse reactions of Myelosuppression and Gastrointestinal related adverse events. CMS notes FDA's postmarketing requirement (PMR) for the applicant to fully characterize the risk of developing secondary malignancies (i.e., development of myelodysplastic syndrome, acute leukemia, and other secondary malignancies) in patients treated with131 I-MIBG. Risk management will also include product labeling and routine pharmacovigilance to ensure the safe and effective use of131 I-MIBG (https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/021200Orig1s015MultidisciplineR.pdf page 21). Also, CMS will monitor any additional data as it becomes available.
In summary, we have determined that AZEDRA® meets all of the criteria for approval of new technology add-on payments, and we are approving new technology add-on payments for FY 2020.
Cases involving AZEDRA® that are eligible for new technology add-on payments will be identified by ICD-10-PCS code XW033S5 and XW043S5. In its application, the applicant stated that the price of AZEDRA (Wholesale Acquisition Cost) is $302.00 per millicurie (mCi) prescribed. Most patients (i.e., those weighing 62.5 kg or more) receive a therapeutic dose of 500 mCi. Accordingly, the applicant estimated an average cost of $302/mCi times 500 mCi, or approximately $151,000. Therefore, according to the applicant, the cost of AZEDRA® is $151,000. Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the average cost of the technology, or 65 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of AZEDRA® is $98,150 for FY 2020.
b. CABLIVI® (caplacizumab-yhdp)
The Sanofi Company submitted an application for new technology add-on payments for CABLIVI® (caplacizumab-yhdp) for FY 2020. The applicant described CABLIVI® as a humanized bivalent nanobody consisting of two identical building blocks joined by a tri alanine linker, which is administered through intravenous and subcutaneous injection to inhibit microclot formation in adult patients who have been diagnosed with acquired thrombotic thrombocytopenic purpura (aTTP). The applicant stated that aTTP is a life-threatening, immune-mediated thrombotic microangiopathy characterized by severe thrombocytopenia, hemolytic anemia, and organ ischemia with an estimated 3 to 11 cases per million per year in the U.K. and U.S.[27 28 29] Further, the applicant stated that aTTP is an ultra-orphan disease caused by inhibitory autoantibodies to von Willebrand Factor-cleaving protease (vWFCP) also known as “a disintegrin and metalloprotease with thrombospondin type 1 motif, member 13 (ADAMTS13),” resulting in a severe deficiency in WFCP. The applicant further explained that von Willebrand Factor (vWF) is a key protein in hemostasis and is an adhesive, multimeric plasma glycoprotein with a pivotal role in the recruitment of platelets to sites of vascular injury. According to the applicant, more than 90 percent of circulating vWF is expressed by endothelial cells and secreted into the systemic circulation as ultra-large von Willebrand Factor (ULvWF) multimers. The applicant stated that decreased ADAMTS13 activity leads to an accumulation of ULvWF multimers, which bind to platelets and induce platelet aggregation. According to the applicant, the consumption of platelets in these microthrombi causes severe thrombocytopenia, tissue ischemia and organ dysfunction (commonly involving the brain, heart, and kidneys) and may result in acute thromboembolic events such as stroke, myocardial infarction, venous thrombosis, and early death. The applicant indicated that the aforementioned tissue and organ damage resulting from the ischemia leads to increased levels of lactate dehydrogenase (LDH), troponins, and creatinine (organ damage markers) and that faster normalization of these organ damage markers and platelet counts is believed to be linked with faster resolution of the ongoing microthrombotic process and the associated tissue ischemia. According to the applicant, in diagnoses of aTTP there is no consensual, validated surrogate marker that defines the subpopulation at greatest risk of death or significant morbidity. Therefore, the applicant stated that all patients who have been diagnosed with aTTP should be considered severe cases and treated in order to prevent death and significant morbidity.
The applicant explained that the two standard-of-care (SOC) treatment options for a diagnosis of aTTP are plasma exchange (PE), in which a patient's blood plasma is removed through apheresis and is replaced with donor plasma, and immunosuppression (for example, corticosteroids and increasingly also rituximab), which is often administered as adjunct to plasma exchange in the treatment for a diagnosis of aTTP.[30 31] According to the applicant, despite the current SOC treatment options, acute aTTP episodes are still associated with a mortality rate of up to 20 percent, which generally occurs within the first weeks of diagnosis. The applicant asserted that, although the 20-percent mortality rate reflects substantial improvement because of PE treatment, in spite of greater understanding of disease pathogenesis and the use of newer immunosuppressants, the mortality rate has not been further improved.[32 33 34 35 36 37] The applicant also noted that another important limitation of the currently available therapies (PE and immunosuppression) is the delayed onset of effect of days to weeks of these therapies because such therapies do not directly address the pathophysiological platelet aggregation that leads to the formation of microthrombi, which is ultimately associated with death or with the severe outcomes reported with diagnoses of aTTP. The applicant explained that despite current treatment, exacerbation and relapse occur and frequently lead to hospitalization and the need to restart daily PE treatment and optimize immunosuppression. In addition, the applicant noted that patients may experience exacerbations after discontinuing plasma exchange treatment due to continuing formation of microthrombi as a result of unresolved underlying autoimmune disease, and patients remain at risk of thrombotic complications or early death until the episode is completely resolved.[38]
According to the information provided by the applicant, CABLIVI® is administered as an adjunct to PE treatment and immunosuppressive therapy immediately upon diagnosis of aTTP through a bolus intraveneous injection for the first dose and subcutaneous injection for all subsequent doses. The recommended treatment regimen and dosage of CABLIVI® consists of administering 10 mg on the first day of treatment via intravenous injection prior to the standard plasma exchange treatment. After completion of PE treatment on the first day, a 10 mg subcutaneous injection is administered. After the first day, and for the rest of the plasma exchange treatment period, a daily 10 mg subcutaneous injection is administered following each day's PE treatment. After the PE treatment period is completed, a daily 10 mg subcutaneous injection is administered for 30 days. If the underlying immunological disease (aTTP) is not resolved, the treatment period should be extended beyond 30 days and be accompanied by optimization of immunosuppression (another SOC treatment option, in addition to PE treatment). According to the applicant and as discussed later, the use of CABLIVI® produces faster normalization of platelet count response compared to that of SOC treatment options alone. The applicant indicated that this contributes to a decrease in the length of the SOC treatment period with respect to the number of days of PE treatment, the mean length of intensive care unit stays, and the mean length of hospitalizations.
With respect to the newness criterion, CABLIVI® received FDA approval on February 6, 2019, for the treatment of adult patients who have been diagnosed with aTTP, in combination with plasma exchange and immunosuppressive therapy. According to information provided by the applicant, CABLIVI® was previously granted Fast Track and Orphan Drug designations in the United States for the treatment of aTTP by the FDA and Orphan Drug designation in Europe for the treatment of aTTP. Currently, there are no ICD-10-PCS procedure codes to uniquely identify procedures involving CABLIVI®. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19291), we noted that the applicant submitted a request for approval for a unique ICD-10-PCS procedure code for the administration of CABLIVI® beginning in FY 2020. The applicant was granted approval for the following procedure codes: XW013W5 (Introduction of Caplacizumab into Subcutaneous Tissue, Percutaneous Approach, New Technology Group 5), XW033W5 (Introduction of Caplacizumab into Peripheral Vein, Percutaneous Approach, New Technology Group 5) and XW043W5 (Introduction of Caplacizumab into Central Vein, Percutaneous Approach, New Technology Group 5).
As previously discussed, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, according to the applicant, CABLIVI® is a first-in-class therapy with an innovative mechanism of action. The applicant explained that CABLIVI® binds to the A1 domain of vWF and specifically inhibits the interaction between vWF and platelets. Furthermore, the applicant indicated that in patients who have been diagnosed with aTTP, proteolysis of ULvWF multimers by ADAMTS13 is impaired due to the presence of inhibiting or clearing anti-ADAMTS13 auto-antibodies, resulting in the persistence of the constitutively active A1 domain and, as a consequence, platelets spontaneously bind to ULvWF and generate microvascular blood clots in high shear blood vessels. The applicant noted that CABLIVI® is able to interact with vWF in both its active (that is, ULvWF multimers or normal multimers activated through immobilization or shear stress) and inactive forms (that is, multimers prior to conformational change of the A1 domain), thereby immediately blocking the interaction of vWF with the platelet receptor (GPIb-IX-V) and further preventing spontaneous interaction of ULvWF with platelets that would lead to platelet microthrombi formation in the microvasculature, local schemia and platelet consumption. The applicant highlighted that this immediate platelet-protective effect differentiates CABLIVI® from slower-acting therapies, such as PE and immunosuppressants, which need days to exert their effect. The applicant explained that PE acts by removing ULvWF and the circulating auto-antibodies against ADAMTS13, thereby replenishing blood levels of ADAMTS13, while immunosuppressants aim to stop or reduce the formation of auto-antibodies against ADAMTS13.
With respect to the second criterion, whether a product is assigned to the same or a different MS-DRG, the applicant believed that potential cases representing patients who may be eligible for treatment involving CABLIVI® would be assigned to the same MS- DRGs as cases representing patients who receive SOC treatment for a diagnosis of aTTP. As explained in this final rule in the discussion of the cost criterion, the applicant believed that potential cases representing patients who may be eligible for treatment involving CABLIVI® would be assigned to MS-DRGs that contain cases representing patients who were diagnosed with aTTP and received therapeutic PE procedures during hospitalization.
With respect to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, according to the applicant, there are no other specific therapies approved for the treatment of patients diagnosed with aTTP. As stated earlier, according to the applicant, patients who have been diagnosed with aTTP have two currently available SOC treatment options: PE, in which a patient's blood plasma is removed through apheresis and is replaced with donor plasma, and immunosuppression (for example, corticosteroids and increasingly rituximab), which is administered as an adjunct to PE in the treatment of aTTP. The applicant further explained that immunosuppression consisting of glucocorticoids is often administered as adjunct to PE in the initial treatment of a diagnosis of aTTP,[39 40] but their use is based on historical evidence that some patients with limited symptoms might respond to corticosteroids alone.[41 42] The applicant noted that there have been no studies specifically comparing treatment involving the combination of PE with corticosteroids, versus PE alone; that they are not specifically approved for the treatment of a diagnosis of aTTP, and that other immunosuppressive agents used to treat a diagnosis of aTTP, such as rituximab, have not been studied in properly controlled, double-blind studies. The applicant also noted that rituximab, aside from not being licensed for the treatment of a diagnosis of aTTP, is not fully effective during the first 2 weeks of treatment, with a reported delay of onset of its effect that may extend up to 27 days, with at least 3 to 7 days needed to achieve adequate B-cell depletion (given the B-cells may also contain ADAMTS13 antibodies), and even longer to restore ADAMTS13 activity levels.[43 44]
Based on the applicant's statements as previously summarized, the applicant believes that CABLIVI® provides a new treatment option for patients who have been diagnosed with aTTP. However, we stated in the proposed rule that it is not clear that CABLIVI® would involve the treatment of a different type of disease or a different patient population. As stated earlier, according to the applicant, patients who have been diagnosed with aTTP have two SOC treatment options for a diagnosis of aTTP: PE, in which a patient's blood plasma is removed through apheresis and is replaced with donor plasma, and immunosuppression (for example, corticosteroids and increasingly also rituximab), which is administered as an adjunct to PE in the initial treatment for a diagnosis of aTTP. We stated that therefore, it appears that CABLIVI® is used to treat the same or similar type of disease (a diagnosis of aTTP) and a similar patient population as currently available treatment options.
We invited public comments on whether CABLIVI® is substantially similar to other technologies and whether CABLIVI® meets the newness criterion.
Comment: Several commenters stated that CABLIVI® is not substantially similar to other technologies and meets the newness criterion. Commenters stated that CABLIVI® is the only FDA approved therapy for aTTP and is a novel technological approach to the disease. Other commenters stated that CABLIVI® is a unique anti-vWF blocking nanobody and the first of its kind in treating acute TTP that should be used at the earliest possible time after presentation of patients with immune-mediated TTP. The commenters stated that they believe CABLIVI® to be potentially lifesaving because no other treatment modalities act in this specific manner. A commenter stated that CABLIVI® differs from the treatments currently available for aTTP because it immediately prevents platelets from binding to the abnormally large vWF molecules, a key abnormality of TTP. A commenter stated that CABLIVI® is a nanobody that directly and specifically targets the pathophysiologic interaction between vWF and platelets, thus rapidly halting the life-threatening process that causes morbidity and mortality in those with aTTP. According to this commenter, no other drug is capable of doing this. Finally, this commenter stated that CABLIVI® is a novel therapy against a rare but potentially fatal autoimmune disease, aTTP that has not had significant short-term developments in almost 30 years.
The applicant commented that CABLIVI® has been approved for the treatment of aTTP in a similar patient population as currently available treatment options. However the applicant also stated that CABLIVI® is a very different technology consisting of a different mode of action that results in improved outcomes with respect to platelet count response, recurrence, and other pre-specified clinical outcome endpoints. The applicant stated that CABLIVI® is the only FDA-approved therapy for treating aTTP in conjunction with PE and immunosuppressive therapy.
The applicant also re-iterated information previously submitted with its application, and previously summarized in this final rule, that CABLIVI® is the only therapeutic agent that is designed to rapidly and specifically reduce the microthrombi formation via reduction in platelet aggregation for patients with an acute aTTP episode. According to the applicant, CABLIVI®'s novel mechanism of action works by targeting the A1 domain of vWF, thus preventing the interaction between vWF and platelets and thereby reducing the subsequent microvascular thrombosis. Regarding the current SOC, the applicant stated that as no randomized controlled prospective clinical studies have been performed to evaluate the efficacy and safety of the immunosuppressive therapies currently used to treat aTTP, the safe and effective dosing regimens of these agents are not known. The applicant further stated that while PE can provide rapid replenishment of new platelets and new ADAMTS 13 to reduce large platelet string formation, it is suboptimal in efficacy with a remaining mortality of up to 20 percent and substantial patient burden and side effects.
Response: We appreciate the commenters' input and the additional detail regarding whether CABLIVI® is substantially similar to existing technologies.
After consideration of the public comments we received and information submitted by the applicant in its application, we believe that while potential cases representing patients who may be eligible for treatment involving CABLIVI® would be assigned to the same MS- DRGs as cases representing patients who receive SOC treatment for a diagnosis of aTTP, and that CABLIVI® is used to treat the same or similar type of disease (a diagnosis of aTTP) and a similar patient population as currently available treatment options, we agree with the applicant that CABLIVI® does not use the same or similar mechanism of action as other technologies used for the treatment of aTTP. We believe that CABLIVI®'s mechanism of action, which targets the A1 domain of vWF, thus preventing the interaction between vWF and platelets and thereby reducing the subsequent microvascular thrombosis, is unique and distinct from other available forms of treatment for aTTP and, therefore, we believe that CABLIVI® meets the newness criterion. We consider the beginning of the newness period to commence when CABLIVI® was approved by the FDA on February 6, 2019.
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that the technology meets the cost criterion. In order to identify the range of MS-DRGs that cases representing potential patients who may be eligible for treatment using CABLIVI® may map to, the applicant identified all MS- DRGs for patients who had been hospitalized for a diagnosis of aTTP. Specifically, the applicant searched the FY 2017 MedPAR file for Medicare fee-for-service inpatient hospital claims submitted between October 1, 2016 and September 30, 2017, and identified potential cases by ICD-10-CM diagnosis code M31.1 (Thrombotic microangiopathy) and ICD-10-PCS procedure codes 6A550Z3 (Pheresis of plasma, single) and 6A551Z3 (Pheresis of plasma, multiple). The applicant noted that it excluded cases with an ICD-10-CM diagnosis code of D59.3 (Hemolytic-uremic syndrome).
This resulted in 360 cases spanning 61 MS-DRGs, with approximately 67.2 percent of all potential cases mapping to the following 5 MS-DRGs:

Using the 242 identified cases that mapped to the top 5 MS-DRGs previously described, the applicant determined that the average case-weighted unstandardized charge per case was $188,765. The applicant then standardized the charges and then removed historic charges for items that are expected to be avoided for patients who receive treatment involving CABLIVI®. The applicant determined that 31 percent of historical routine bed charges, 65 percent of historical ICU charges, and 38 percent of historical blood administration charges (which includes charges for therapeutic PE) would be reduced because of the use of CABLIVI®, based on the findings from the Phase III clinical study HERCULES. The applicant indicated it used the FY 2017 MedPAR file to determine the appropriate amount of charges to remove. The applicant then inflated the adjusted standardized charges by 8.864 percent utilizing the 2-year inflation factor published by CMS in the FY 2019 IPPS/LTCH PPS final rule to adjust the outlier threshold (83 FR 41722). (In the FY 2020 IPPS/LTCH PPS proposed rule, we noted that this figure was revised in the FY 2019 IPPS/LTCH PPS final rule correction notice. The corrected final 2-year inflation factor is 1.08986 (83 FR 49844). We further noted that even when using the corrected final rule values to inflate the charges, the average case-weighted standardized charge per case exceeded the average case-weighted threshold amount.) The applicant explained that the anticipated price for CABLIVI®'s indication for the treatment of patients who have been diagnosed with aTTP, in combination with plasma exchange and immunosuppressive therapy, has yet to be determined and, therefore, no charges for CABLIVI® were added in the analysis. Based on the FY 2019 IPPS/LTCH PPS final rule correction notice data file thresholds for FY 2020, the applicant determined the average case-weighted threshold amount was $49,904. The final inflated average case-weighted standardized charge per case was $145,543. Because the final inflated average case-weighted standardized charge per case exceeds the average case-weighted threshold amount, the applicant maintained that the technology meets the cost criterion. We invited public comments on whether CABLIVI® meets the cost criterion.
Comment: The applicant submitted a revised analysis using the 2-year inflation factor of 1.08986 from the FY 2019 IPPS correction notice to inflate charges from FY 2017 to FY 2019. The applicant also added charges to reflect the current wholesale acquisition cost (WAC) price for CABLIVI®. According to the applicant, after changing the 2-year inflation factor from 8.864 percent to 8.986 percent and adding charges for the new technology, the inflated average case-weighted standardized charge per case was $413,246. Based on this analysis, the applicant determined that the inflated average case-weighted standardized charge per case for CABLIVI® exceeded the threshold amount of $49,904 and that CABLIVI® meets the cost criterion.
Response: We appreciate the applicant's input and revised analysis. After consideration of the public comments we received, we believe that CABLIVI® meets the cost criterion.
With respect to the substantial clinical improvement criterion, the applicant asserted that it believes that CABLIVI® represents a substantial clinical improvement compared to the use of currently available treatments (PE and immunosuppressants) because it: (1) Significantly reduces time to platelet count response, which is consistent with the halting of platelet consumption in microthrombi; (2) significantly reduces the number of patients with aTTP-related death, recurrence of aTTP-related episodes, or a major thromboembolic event; (3) reduces mortality; (4) reduces the proportion of patients with recurrence of aTTP diagnoses; (5) reduces the proportion of patients who develop refractory disease; (6) reduces the number of days of PE; (7) reduces the mean length of intensive care unit stay and the mean length of hospitalization; and (8) shows a trend of more rapid normalization of organ damage markers. The applicant provided further detail regarding these assertions, referencing the results of Phase II and Phase III studies and an integrated efficacy analysis of both studies.
The applicant reported that the Phase II study was a randomized, single-blind, placebo controlled study entitled ALX-0681-2.1/10 (TITAN) that examined the efficacy and safety of the use of CABLIVI® compared to a placebo, with the primary endpoint being achievement of a statistically significant reduction in time to platelet count response. Seventy-five patients, 66 of which were white, (19 to 72 years old, with a mean of 41.6 years old; 44 women and 31 men) with an episode of aTTP were randomized 1:1 to receive either CABLIVI® (n = 36) or placebo (n = 39), in addition to daily PE.[45] Patients received their first dose of CABLIVI® administered through intravenous injection prior to the first PE, followed by daily doses administered subcutaneously after each PE. After discontinuing PE, daily doses of CABLIVI® administered through subcutaneous injection were continued for 30 days. The median treatment duration with CABLIVI® was 36 days.
According to the applicant, significantly more patients in the treatment arm met the primary endpoint [95 percent Confidence Interval (CI) (3.78, 1.28)]. The applicant indicated that the time to platelet count response improvement constitutes a significant substantial clinical improvement because it demonstrated that patients treated with CABLIVI® were 2.2 times more likely to achieve an acceptable time to platelet count response than patients receiving treatment with the placebo. Additionally, the applicant noted that exacerbation of aTTP occurred in fewer patients who were treated with CABLIVI® (8.3 percent) than placebo (28.2 percent). During the 1-month follow-up period, 8 relapses (defined as a recurrence more than 30 days after discontinuing PE) occurred in the CABLIVI® group with 7 of the relapses occurring within 10 days of discontinuing the study drug. In all seven of the relapses, ADAMTS13 activity was still severely suppressed at the end of the treatment period, evidence of ongoing underlying immunological disease and indicating an imminent risk of another relapse. The applicant explained that according to post-hoc analyses, the group of patients who were treated with CABLIVI® compared to placebo showed a decrease in the percentage of patients with refractory disease (0 percent versus 10.8 percent), a reduction in the number of days of PE (7.7 days versus 11.7 days) and a trend to more rapid normalization of organ damage markers (lactate dehydrogenase, cardiac troponin I and serum creatinine). Finally, the applicant noted that there were no deaths in the group of patients who were treated with CABLIVI®. However, 2 of the 39 placebo-treated patients (5.1 percent) died.
The applicant explained that the Phase III study was a randomized, double-blind, placebo controlled study entitled ALX0681-C301 (HERCULES) that examined the efficacy and safety of the use of CABLIVI® compared to a placebo, with the primary endpoint being achievement of a statistically significant reduction in time to platelet count response. One hundred forty-five patients (18 to 79 years old, with a mean of 46 years old, 100 women and 45 men), with an episode of aTTP were randomized 1:1 to receive either CABLIVI® (n=72) or placebo (n=73) in addition to daily PE and immunosuppression.[46] The applicant explained that patients received a single 10 mg CABLIVI® intravenous injection or placebo prior to the first PE, followed by a daily CABLIVI® 10 mg subcutaneous injection or placebo after completion of PE, for the duration of the daily PE treatment period and for 30 days thereafter. According to the applicant, if at the end of this treatment period (daily PE treatment period and 30 days after) there was evidence of persistent underlying immunological disease activity (indicative of an imminent risk for recurrence), treatment could be extended weekly for a maximum of 4 weeks, together with optimization of immunosuppression. The applicant indicated that patients who experienced a recurrence while undergoing study drug treatment were switched to open-label CABLIVI® and they were again treated for the duration of daily PE treatment and for 30 days thereafter. If at the end of this treatment period (daily PE treatment period and 30 days after) there was evidence of ongoing underlying immunological disease, open-label treatment with CABLIVI® could be extended weekly for a maximum of 4 weeks, together with optimization of immunosuppression. Patients were followed for 28 days after discontinuation of treatment. Upon recurrence during the follow-up period (that is, after all study drug treatment had been discontinued), there was no re-initiation of the study drug because recurrence at this point was treated according to the SOC. The median treatment duration with CABLIVI® in the double-blind period was 35 days.
According to the applicant, patients in the treatment arm were more likely to achieve platelet count response at any given time point, compared to the placebo [95 percent CI (1.1, 2.2)]. The applicant believed that this constitutes a significant substantial clinical improvement because patients who were treated with CABLIVI® were 1.55 times more likely to achieve platelet count response at any given time point, compared to placebo. The applicant also indicated that, compared to placebo, treatment with CABLIVI® resulted in a 74 percent reduction in the number of patients with aTTP-related death, recurrence of aTTP diagnosis, or a major thromboembolic event, during the study drug treatment period (p<0.0001).
The applicant noted that the proportion of patients with a recurrence of an aTTP diagnosis in the Phase III study period (that is, the drug treatment period plus the 28-day follow-up after discontinuation of the drug treatment) was 67 percent lower in the CABLIVI® group (12.7 percent) compared to the placebo group (38.4 percent) (p<0.001). The applicant also indicated that in all 6 patients in the CABLIVI® group who experienced a recurrence of an aTTP diagnosis during the follow-up period (that is, a relapse), ADAMTS13 activity levels were less than 10 percent at the end of the study drug treatment, indicating that the underlying immunological disease was still active at the time CABLIVI® was discontinued. Furthermore, the applicant stated that there were no patients who were treated with CABLIVI® that had refractory disease (defined as absence of platelet count doubling after 4 days of standard treatment and elevated LDH), compared to 3 patients (4.2 percent) who had refractory disease that were treated with placebo. The applicant also explained that a trend to faster normalization of the organ damage markers lactate dehydrogenase, cardiac troponin I and serum creatinine was observed in patients who were treated with CABLIVI®. The applicant noted that during the study drug treatment, there were no deaths in patients who were treated with CABLIVI®, while 3 of the 73 placebo-treated patients (4.1 percent) died. Finally, the applicant stated that during the Phase III study drug treatment period, treatment with CABLIVI® resulted in a 38 percent reduction in the mean number of PE treatment days versus placebo (reduction of 3.6 days) and a 41 percent reduction in the mean volume of PE (reduction of 14.6L). Furthermore, treatment with CABLIVI® resulted in a 65 percent reduction in the mean length of ICU stay (reduction of 6.3 days) and a 31 percent reduction in the mean length of hospitalization (reduction of 4.5 days) during the Phase III study drug treatment period.
The applicant submitted integrated data from the blinded periods of the Phase II and Phase III studies that show a statistically significant difference in favor of CABLIVI® (n=108) in time to platelet count response compared to placebo (n=112). The applicant indicated that patients who were treated with CABLIVI® were 1.65 times more likely to achieve platelet count response at any given time point during the blinded period than patients who were treated with placebo (95 percent CI: 1.23, 2.20; p<0.001). Additionally, according to the applicant, integrated data from the blinded periods of the Phase II and Phase III studies showed that compared to placebo, treatment with CABLIVI® resulted in a 72.6 percent reduction in the percentage of patients with aTTP-related death, a recurrence of a aTTP diagnosis, or at least one treatment-emergent major thromboembolic event during the blinded treatment period (p<0.0001). More specifically, the applicant indicated that during the blinded treatment period no aTTP-related deaths occurred in the CABLIVI® group compared to 4 aTTP-related deaths in the placebo group (p<0.05), treatment with CABLIVI® resulted in an 84.0 percent reduction in the proportion of patients with a recurrence of a aTTP diagnosis (exacerbation, relapse) during the blinded treatment period (p<0.0001), and treatment with CABLIVI® resulted in a reduction of 40.8 percent in the proportion of patients with at least one treatment-emergent major thromboembolic event during the blinded treatment period.
According to the applicant, pooled data from the two studies showed that none of the patients who were treated with CABLIVI® developed refractory disease (that is, absence of platelet count doubling after 4 days of standard treatment and elevated LDH) compared to 7 patients (6.3 percent; 7/112) who were treated with placebo during the blinded period (p<0.01). Finally, the applicant noted that across both studies, treatment with CABLIVI® resulted in a 37.5 percent reduction in the mean number of days of PE treatment (reduction of 3.9 days).
In the FY 2020 IPPS/LTCH PPS proposed rule, we stated that although the applicant asserts that CABLIVI® represents a substantial clinical improvement compared to the use of currently available treatments (PE and immunosuppressants), we were concerned that the Phase II TITAN and Phase III HERCULES studies may not provide enough evidence to support that the use of CABLIVI® represents a substantial clinical improvement.
Regarding the Phase II TITAN study, we stated that we were concerned that because 66 of the 75 patients in the study population were white, the results of the study may not be generalizable to a more diverse population that may be at risk for diagnosis of aTTP. Additionally, we noted that CABLIVI® was associated with fewer aTTP exacerbations during therapy, but was associated with more aTTP exacerbations after therapy was discontinued, suggesting a lack of effect on long-term anti-ADAMTS13 antibody levels. Although this is consistent with CABLIVI®'s mechanism of action, we stated our concern in the proposed rule that without long-term data to determine the impact of adjunct use of CABLIVI® on exacerbations and relapse it may be difficult to determine if the use of CABLIVI® represents a substantial clinical improvement over existing therapy.
Based on data from the Oklahoma TTP-HUS Registry, the incidence of aTTP is approximately three cases per 1 million adults per year.[47] Additionally, the median age for a diagnosis of aTTP is 41, with a wide range between 9 years old and 78 years old. In the proposed rule, we acknowledged the challenges of constructing robust clinical studies due to the extremely rare occurrence of patients who have been diagnosed with aTTP. However, we stated that we were nonetheless concerned that the study population in the Phase III HERCULES study was small, 145 people. Additionally, we indicated that it was unclear if the response rate may differ in those who have a de novo diagnosis versus those with recurrent disease. We noted that PE treatment alone has been attributed to an 80 percent survival rate,[48] and because CABLIVI® is given in combination with or after SOC therapies, we stated in the proposed rule that we were concerned that we may not have sufficient information to determine the extent to which the study results were attributable to the use of CABLIVI®. Furthermore, we stated that with the follow-up period for the Phase III HERCULES study being only 28 days, we were concerned that there is a lack of long-term data. We further stated that, in the absence of long-term data, we were concerned about the impact of the use of CABLIVI® on the relapse rate beyond the overall study period, including the 28-day follow-up period.
Finally, although both the Phase II and III studies consisted of key secondary endpoints such as death or major thromboembolic events, in the proposed rule we indicated that we were concerned these endpoints were not clearly defined. We also stated that we were concerned the studies did not appear to account for other clearly defined endpoints such as heart attack, stroke, a bleeding episode, and power calculations for the expected differences in such endpoints that would be biologically important.
We invited public comments on whether CABLIVI® meets the substantial clinical improvement criterion.
Comment: Several commenters provided comments in support of CABLIVI®. A commenter stated that CABLIVI® utilizes a monoclonal antibody that binds to vWF, causing platelets to clump and clog up the microcirculation of patients and thereby reducing the number of plasma exchanges required to bring patients back to normal platelet counts. The commenter stated that the clinical benefit of reducing the amount of plasma exchanges include lowering the amount of plasma required to maintain the blood bank's supply, lessening the chance of TRALI, reducing time spent in the intensive care unit, reducing time in hospitalization, replacing many hours of expensive plasma exchange in the inpatient and outpatient settings with a subcutaneous injection, and tremendous increase in patient satisfaction in their overall care.
A commenter stated that CABLIVI® has the potential to save the lives of those individuals who do not respond to current conventional treatment, plasma exchange, corticosteroids, and rituximab. The commenter stated that without bound platelets, the thrombosis is prevented. Finally, the commenter stated that CABLIVI® blocks the tissue injury, but corticosteroids, rituximab, and plasma exchange are still needed to affect the cause of the disease.
Another commenter stated that with the pathophysiology of aTTP rapidly and durably crippled as long as CABLIVI® is administered, immunosuppression and other therapies such as plasma exchange can be provided to these patients to help obtain a prolonged remission after cessation of CABLIVI®. The commenter stated that CABLIVI® is a valuable tool for the treatment of aTTP that provides significantly improved clinical care compared to the current standard of care. According to the commenter, by creating a window period during CABLIVI® administration in which the pathophysiology of aTTP is crippled in a targeted fashion, patients with aTTP can be treated for existing organ damage (for example, injuries to heart, brain, gut, RBCs) and have an earlier opportunity for immunosuppression to begin working against this dangerous autoimmune disease. The commenter stated that in two randomized controlled trials, CABLIVI® has demonstrated the ability to rapidly normalize platelet count in a sustained manner while drug is being administered, as well as decrease the composite endpoint of death, disease recurrence, and thromboembolic events.
The applicant provided information in response to CMS' concerns regarding whether CABLIVI® meets the substantial clinical improvement criterion. The information provided by the applicant was in response to CMS' concerns regarding whether CABLIVI® meets the overall substantial clinical improvement criterion, the demographics of the Phase II TITAN study patient population, the need for longer-term studies to identify the effect of CABLIVI® on exacerbations and relapse, the small sample size included in the Phase III HERCULES study and the clinical trial design of the Phase II TITAN and Phase III HERCULES studies due to short follow-up period, unclear defined secondary endpoints and inclusion of biologically important endpoints.
The applicant stated that the multi-discipline review of CABLIVI® by the FDA concluded that the Phase III HERCULES study provided substantial evidence of CABLIVI®'s effectiveness when added to daily PE and immunosuppression compared to PE and immunosuppression alone. The applicant stated that the primary endpoint of the Phase III HERCULES study was time to platelet response in which the study produced a median time to platelet response of 2.7 days in the CABLIVI® treatment group compared to 2.9 days in the placebo treatment group. According to the applicant, other equally important clinical outcomes consist of the proportion of patients with aTTP-related death, recurrence of aTTP or at least one treatment emergent major thromboembolic event (a composite endpoint). The applicant stated that these outcomes were significantly lower in the CABLIVI® treatment group (9/72 (13 percent) compared to the placebo treatment group 36/73 (49 percent) (p<0.0001). The applicant further stated that the proportion of patients with a recurrence of aTTP in the overall study period was significantly lower in the CABLIVI® treatment group (9/72 (13 percent) patients) compared to the placebo treatment group (28/73 (38 percent) patients) (p<0.001). The applicant noted that in the 6 patients treated with CABLIVI® who experienced a recurrence of aTTP during the follow-up period (that is, a relapse defined as recurrent thrombocytopenia after initial recovery of platelet count (platelet count 2: 150,000/μL) that required re-initiation of daily plasma exchange, occurring after the 30-day post daily plasma exchange period), ADAMTS13 activity levels were <10 percent at the end of the study drug treatment suggesting that the underlying immunological disease was still active at the time CABLIVI® was stopped.
The applicant also stated that during the overall study drug treatment period, which included, for all patients, the period on double-blind treatment, as well as, for patients who had an exacerbation and were switched, the period on open-label CABLIVI®-treatment resulted in a 38 percent reduction in the number of PE days (average reduction 3.6 days) and a 41 percent reduction in the volume of plasma exchanged (average reduction 15 L). The applicant also stated that there was a 65 percent reduction in length of intensive care unit (ICU) stay (average reduction 6.3 days) and a 31 percent reduction in length of hospitalization (average reduction 4.5 days).
In response to CMS's concerns regarding the patient population demographics of the Phase II TITAN trial, the applicant stated that the FDA assessed the substantial clinical improvement of CABLIVI® based on the Phase III HERCULES study, whereas the Phase II TITAN trial was considered supportive evidence. The applicant also noted that it is important to understand that both the Phase II TITAN and Phase III HERCULES studies included US sites (8 sites/15 patients in TITAN and 10 sites/32 patients in HERCULES). According to the applicant the Phase III HERCULES study is the pivotal study for efficacy evaluation and was a study in which US patients represented overall 22 percent of the overall patient population. Also, the applicant stated that in the Phase III HERCULES study, 28 patients were black or African American (21.1 percent of the overall aTTP population and only 13.8 percent of the US population) and as such the applicant considers the results of the studies applicable to the US population. The applicant also stated that the FDA did not raise any concerns related to the demographics of the patient population during the Biologics License Application (BLA) review process.
Regarding the CMS concern on the need for longer-term studies to identify the effect of CABLIVI® on exacerbations and relapse the applicant re-iterated information previously submitted with its application and previously summarized. The applicant stated that the trial results show the proportion of patients with a recurrence of aTTP in the overall study period was significantly lower in the CABLIVI® group (9/72 (13 percent) patients) compared to the placebo group (28/73 (38 percent) patients) (p<0.001) and that in the 6 patients treated with CABLIVI® who experienced a recurrence of aTTP during the follow-up period, ADAMTS13 activity levels were <10 percent at the end of the study drug treatment suggesting that the underlying immunological disease was still active at the time CABLIVI® was stopped.
The applicant also acknowledged that long-term studies and clinical experiences are needed to better understand CABLIVI®'s effectiveness in preventing recurrences of aTTP episodes and as such it is conducting a 3 year follow-up study for those patients enrolled in the Phase III HERCULES study in which data will be available in the near future. In addition, the applicant stated they are working with the medical community to explore real world data generation opportunities, including registries.
In response to CMS' concerns regarding the small sample size included in the Phase III HERCULES study, the applicant stated that as aTTP is an ultra-rare blood disorder with a reported incidence of 4 to 5 cases per million in the US, enrolling a large number of patients in a clinical study is challenging. Furthermore, the applicant explained that the sample size calculation of the Phase III HERCULES study was assessed in the BLA review process by the FDA and described accurately as being based on superiority testing of CABLIVI® over placebo with respect to time to platelet response and satisfying the following criteria:
- 80 percent power;
- Log-rank test at 2-sided a = 0.05;
- Accrual period lasting 2.5 years;
- Time-to-event period set at 45 days (note: for the primary endpoint, a patient is censored if there is no platelet response by day 45);
- 40 percent reduction in time-platelet response. Assuming a median time-to-response of 7 days among placebo, this is tantamount to a median time-to-response of 4.2 days in the CABLIVI® arm; and
- Expected dropout rate of 10 percent in the first 10 days after first administration of study drug.
The applicant stated that under these criteria, 121 events are required resulting in a sample size of 132 patients and that the actual number of patients randomized in the study exceeded this threshold at 145. Also, according to the applicant, the FDA did not have any major comments or concerns about the sample size of Phase III HERCULES study, endpoint definition or other relevant methodological questions or concerns during the BLA review process. The applicant also stated that the Phase III HERCULES study was the largest study ever conducted in this rare condition in which the results were recently published in the New England Journal of Medicine with no significant questions or remarks from the editors on the sample size, endpoint definition or any other relevant methodological questions raised by journal editors or reviewers.
In response to CMS' concerns regarding the clinical trial design of the Phase II TITAN and Phase III HERCULES studies due to short follow-up period, the applicant stated that the 1-month follow-up period was defined based on current evidence that this is the period for which patients are at higher risk of recurrence for the presenting episode of a TTP. The applicant re-iterated information previously submitted with its application and previously summarized in this final rule stating that the proportion of patients with a recurrence of aTTP in the overall study period was significantly lower in the CABLIVI® group (9/72 (13 percent) patients) compared to the placebo group (28/73 (38 percent) patients) (p<0.001). Again, the applicant indicated that in the 6 patients treated with CABLIVI® who experienced a recurrence of aTTP during the follow-up period, ADAMTS13 activity levels were <10 percent at the end of the study drug treatment suggesting that the underlying immunological disease was still active at the time CABLIVI® was stopped.
In response to CMS' concerns regarding clinical trial design of the Phase II TITAN and Phase III HERCULES studies due to unclear defined secondary endpoints and inclusion of biologically important endpoints, the applicant stated that the Phase III HERCULES study was designed to understand the potential role of CABLIVI® in the treatment of aTTP by comparing CABLIVI® with placebo with respect to time to normalization of platelet count (primary endpoint) and the risk of death and complications caused by thrombotic events and organ damage (secondary and other endpoints). According to the applicant, the trial also evaluated the potential of CABLIVI® to reduce the risk of recurrence by allowing for treatment to continue until immunosuppressive therapy resolved the underlying autoimmune disease. The applicant noted that the endpoints of this study were defined a priori and detailed in the clinical study protocol.
The applicant re-iterated information previously submitted with its application and previously summarized in this final rule stating that primary outcome of the studies was the time to a response, which was defined as the time from the first intravenous administration of CABLIVI® or placebo to normalization of the platelet count (that is, a platelet count of at least 150,000 per cubic millimeter), with discontinuation of daily plasma exchange within 5 days thereafter. According to the applicant, the results showed a statistically significant shorter median time to normalization of platelet count in CABLIVI® group (p=0.01) comparing to placebo.
The applicant also referenced four key secondary outcomes of the studies, which were hierarchically ranked on the basis of clinical relevance, as the following:
1. A composite of TTP-related death, recurrence of TTP, or a major thromboembolic event (for example, myocardial infarction, stroke, bleeding episodes) during the trial treatment period. Results were statistically significant favoring CABLIVI® arm (p<0.001);
2. Recurrence of TTP at any time during the trial, including the follow-up period. Results were statistically significant favoring CABLIVI® arm (p<0.001);
3. Refractory TTP (defined by the lack of a doubling of the platelet count after 4 days of treatment and a lactate dehydrogenase level that remained above the upper limit of the normal range). Results were not statistically significant (p=0.06); and
4. The time to normalization (that is, to a level below the defined upper limit of the normal range) of three organ-damage markers (lactate dehydrogenase, cardiac troponin I, and serum creatinine). Not tested for statistical significance as prior endpoint was not statistically significant.
The applicant stated that a recurrence was defined as a new decrease in the platelet count that necessitated the re-initiation of plasma exchange after normalization of the platelet count had occurred, an exacerbation was defined as a recurrence that occurred within 30 days after the last plasma exchange and a relapse was defined as a recurrence that occurred more than 30 days after cessation of plasma exchange. Furthermore, the applicant conveyed that outcomes that were not part of the hierarchy included the number of days of PE and the volume of plasma exchanged, the duration of stay in an ICU and in the hospital, mortality rate, pharmacodynamic and pharmacokinetic variables, and immunogenicity. Finally, according to the applicant, safety assessments were performed throughout the course of the trial and included evaluation of vital signs, physical examinations, clinical laboratory testing, and 12-lead electrocardiography.
Response: We appreciate all the comments received related to CABLIVI®, including the applicant's submission of additional information to address the concerns presented in the proposed rule.
After consideration of the public comments we received, we believe that the applicant has addressed our concerns regarding whether CABLIVI® meets the substantial clinical improvement criterion, and that CABLIVI® represents a substantial clinical improvement over existing technologies (PE and immunosuppression alone) based on the results of the Phase II TITAN and Phase III HERCULES studies with respect to time to platelet count response, which is consistent with the halting of platelet consumption in microthrombi; the number of patients with aTTP-related death and recurrence of aTTP-related episodes or a major thromboembolic event, and mortality. Additionally, we note that CABLIVI® is the only FDA-approved therapy for treating aTTP in conjunction with PE and immunosuppressive therapy.
In summary, we have determined that CABLIVI® meets all of the criteria for approval of new technology add-on payments. Therefore, we are approving new technology add-on payments for CABLIVI® for FY 2020. Cases involving CABLIVI® that are eligible for new technology add-on payments will be identified by ICD-10-PCS procedure codes XW013W5, XW033W5 and XW043W5. In its application and subsequent public comment, the applicant estimated that the average Medicare beneficiary would require a dosage of 11 mg/kg administered as an intravenous injection as a single dose and of 10 mg/kg administered as a subcutaneous injection as a single dose. According to the applicant, the WAC for one dose of 10 mg/kg is $7,300, and patients will typically require 1.16 vials for the course of treatment with CABLIVI® per day for an average duration of 6 days for an average total of 7 vials. Therefore, the total cost of CABLIVI® per patient is $51,100. Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the average cost of the technology, or 65 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of CABLIVI® is $33,215 for FY 2020.
c. CivaSheet®
CivaTech Oncology, Inc. submitted an application for new technology add-on payments for CivaSheet® for FY 2020. CivaSheet® received FDA clearance of a 510(k) premarket notification on August 29, 2014. CivaSheet® was approved as a “sealed source” by the Nuclear Regulatory Commission (NRC) and added to the Registry of Radioactive Sealed Source and Devices on October 24, 2014. On May 9, 2018, CivaSheet® was registered by the American Association of Physicists in Medicine (AAPM) on the “Joint AAPM/IROC Houston Registry of Brachytherapy Sources Complying with AAPM Dosimetric Prerequisites.” According to the applicant, inclusion on this AAPM registry is a long-standing requirement imposed on brachytherapy sources used in all National Cancer Institute clinical trials and that all other available brachytherapy sources are included on this registry. According to the applicant, CivaSheet® was not commercially distributed among IPPS hospitals until May 2018, after meeting the requirements for inclusion in the AAPM registry. Therefore, according to the applicant the “newness” period for the CivaSheet®, if approved for FY 2020 new technology add-on payments, should commence on May 9, 2018. Based on this information, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19295), we stated that we believe the newness period for CivaSheet® would begin on May 9, 2018. However, we invited public comments on whether inclusion on the AAPM registry is an appropriate indicator of the first availability of the CivaSheet® brachytherapy sources on the U.S. market and whether the date of inclusion on the AAPM registry is appropriate to consider as the beginning of the newness period for CivaSheet®.
Comment: The applicant submitted public comments reiterating that CivaSheet was registered by the American Association of Physicists in Medicine (AAPM) on the Joint AAPM/IROC Houston Registry of Brachytherapy Sources Complying with AAPM Dosimetric Prerequisites. The applicant reiterated that while the CivaSheet was cleared by the Food and Drug Administration and approved by the Nuclear Regulatory Commission as a “sealed source” somewhat earlier, inclusion of a brachytherapy source on this Registry is essentially a prerequisite for commercial acceptance of such a source. For acceptance of a new brachytherapy source outside of essentially experimental contexts, completion of dosimetric studies is necessary. The applicant indicated that it is the AAPM's validation that the results of these studies indicate compliance with its prerequisites, rather than FDA clearance, that appropriately marks the readiness of a source for the market and the CivaSheet® was added to the registry, May 9, 2018.
Response: We appreciate the applicant's comments. After consideration of the comments we received, it appears that CivaSheet® was not commercially distributed among IPPS hospitals until May 2018, after meeting the requirements for inclusion in the AAPM registry. As we have stated in prior rulemaking (69 FR 28237), the 2-year to 3-year period of newness for a technology or medical service would ordinarily begin with FDA approval, unless there was some documented delay in bringing the product onto the market after that approval. Therefore, we believe that the newness period for the CivaSheet® would begin May 9, 2018. CivaSheet® is intended for medical purposes to be placed into a body cavity or tissue as a source for the delivery of radiation therapy. CivaSheet® is indicated for use as a permanent interstitial brachytherapy source for the treatment of selected localized tumors. The device may be used either for primary treatment or for the treatment of residual disease after excision of the primary tumor. CivaSheet® may be used concurrently, or sequentially, with other treatment modalities, such as external beam radiation therapy or chemotherapy. In the proposed rule, we noted that the applicant had submitted a request for approval for a unique ICD-10-PCS procedure code to describe procedures involving the use of the CivaSheet® device, beginning in FY 2020. Approval was granted for the following procedure codes effective October 1, 2019:



As discussed previously, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and, therefore, would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, according to the applicant, CivaSheet® does not have a similar mechanism of action in comparison to existing brachytherapy technologies. The applicant asserted that the unique construction and configuration of the CivaSheet® device permits delivery of radiation intra-operatively in a highly targeted fashion. The applicant explained that the CivaSheet® is cut to size in the operation room (OR) and conformed to the patient's anatomy and surgical site, which allows radiation to be delivered to the resected tumor bed margins at the time of the original surgery. The applicant further explained that, it is generally believed that “hot” spots should be avoided in the delivery of radiotherapy because they lead to complications, citing the finding that “[i]n brachytherapy, dose homogeneity is difficult to achieve, but efforts to minimize “hot” spots have been regarded as virtuous and implant-planning guidelines were developed to assist in this regard.” [49] The applicant stated that implants are rarely geometrically perfect and, to avoid under-dosing some parts of the target volume, it may be necessary to create “hot spots” in other parts of the anatomy. However, as a result, a “hotter” dose compared to that achievable with external beam technologies can be delivered to the intended area. In contrast, the applicant indicated that CivaSheet®'s unidirectional configuration substantially reduces the dose delivered to neighboring radiosensitive structures. The applicant further stated that other forms of radiation delivery do not have these capabilities, and no other shielded low-dose radiation (LDR) sources are currently available on the market. According to the applicant, external beam radiation generally cannot be delivered intra-operatively, partly because dosage requirements make this impractical and potentially risky and because appropriate aiming cannot be computed in the timeframe of a performed surgery.
The applicant believed that, in the absence of the use of the CivaSheet® device, a patient requiring radiation therapy to accompany surgery would most likely receive radiation therapy as an outpatient service following the inpatient hospitalization after surgery. Moreover, the applicant stated that not only does this typically require multiple, fractionated treatments, in some cases, outpatient external beam radiation may not be possible due to excessive toxicity to normal surrounding tissues. According to the applicant, radiation therapy can be delivered intra-operatively directly to surgical margins through use of a linear accelerator. However, the applicant stated that these technologies deliver radiation in a single “flash,” whereas the CivaSheet® device enables the delivery of radiation over time, increasing the efficacy of the radiation therapy.
Further, the applicant stated that external beam radiation devices have a fixed ball or cone-shaped applicator, which does not necessarily conform well to the irregular shapes of surgical cavities or permit effective screening of adjacent tissues. Additionally, the applicant stated that this form of radiation therapy requires a specialized linear accelerator and a specially shielded operating room, which the applicant believes restricts its use to IPPS-exempt cancer centers.
The applicant further stated that, in the past, cylindrical brachytherapy seeds have been used with various mesh products as a form of intra-operative radiation therapy (IORT). However, according to the applicant, the use of cylindrical brachytherapy seeds used with various mesh products has not developed as part of standard clinical practice. According to the applicant, patients treated with previous cylindrical brachytherapy seeds faced considerable challenges with toxicity from the unfocused, unshielded seed sources when placed in proximity of sensitive organs.[50] Additionally the surgical meshes previously used were not designed to maximize source orientation and spacing, and also ran the risk of source dispersion as the mesh degraded.[51] The applicant maintains that the CivaSheet® is the first low-dose radiation (LDR) brachytherapy device designed specifically for the delivery of IORT. CivaSheet®'s individual brachytherapy sources are flat with a gold shielding on one side of the seed, a design that focuses radiation in one direction, in contrast to the cylindrical shape of LDR brachytherapy seeds, which emit radiation in all directions. According to the applicant, properties of the flat, gold-shielded sources and the bioabsorbable polymer encapsulation make the CivaSheet® uniquely suited for intra-operative delivery. As such, the applicant asserted that the CivaSheet® does not have a similar mechanism of action when compared to existing LDR brachytherapies.
With regard to the second criterion, whether a product is assigned to the same or a different MS-DRG, the applicant asserted that patients who may be eligible for treatment using the CivaSheet® include hospitalized patients having tumors removed from the pancreas, colon and anus, pelvic area, head and neck, soft tissue sarcomas, non-small-cell lung cancer, ocular melanoma, atypical meningioma and retroperitoneum and that cases involving the use of the CivaSheet® would map primarily into the following MS-DRGs listed below. In the proposed rule, we indicated that we believe that cases involving the use of existing technologies would be assigned to these same MS-DRGs as previously listed.


With regard to the third criterion, whether the use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, according to the applicant, clinical conditions that may require use of the CivaSheet® include treatment of the same patient population as those who have been diagnosed with a variety of types of cancer, including pancreatic cancer, colorectal cancer, anal cancer, pelvic area/gynecological cancer, retroperitoneal sarcoma and head and neck cancers.
The applicant asserted that the CivaSheet® device is not substantially similar to any existing technology because it uses a unique mechanism of action, when compared to existing LDR brachytherapy technologies, to achieve a therapeutic outcome and, therefore, meets the newness criterion.
We invited public comments on whether the CivaSheet® device meets the newness criterion.
Comment: The applicant submitted public comments stating that it believes that the CivaSheet® meets CMS' newness criterion. The applicant stated that in particular, the CivaSheet® enables intraoperative delivery of radiation in circumstances where this was not previously possible, whether using brachytherapy or other forms of radiation, without adverse effects on neighboring, radiosensitive tissue. The applicant stated that the capability for one-directional delivery of radiation, attributable to the gold shielding on each source and the persisting matrix in which the sources are embedded and which maintains their orientation within the body as the surgical wound is closed and heals, is unique. The applicant further stated that the customizable, conformable, planar design allows positional stability, homogenous distribution of radiation in the surgical cavity, features not available in radioactive seed technology previously available. Response: We appreciate the applicant's comments with regard to the newness criterion. After consideration of the comments we received, we believe the mechanism of action of the CivaSheet® is unique from other brachytherapy technologies because of. the unidirectional delivery of intraoperatively applied radiation due to its shielded gold layer. Therefore, we believe the CivaSheet® is not substantially similar to existing technology and that it meets the newness criterion.
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that the technology meets the cost criterion. To determine the MS-DRGs that potential cases representing patients who may be eligible for treatment involving CivaSheet® would map to, the applicant identified all MS-DRGs for cases that included ICD-10-CM diagnosis codes for either pancreatic cancer, colorectal cancer, anal cancer, pelvic area/gynecological cancer, retroperitoneal sarcoma and head and neck cancers as a primary or secondary diagnosis. Based on the FY 2017 MedPAR Hospital Limited Data Set (LDS), the applicant identified a total of 22,835 potential cases. The applicant limited its analyses to the most relevant 32 MS-DRGs, which represented 80 percent of all the cases. The applicant excluded the following cases: statistical outliers which the applicant defined as 3 standard deviations from the geometric mean, HMO cases and claims submitted only for graduate medical education payments and cases at hospitals that were not included in the FY 2019 IPPS/LTCH PPS final rule impact file (the applicant noted that these are predominately cancer hospitals not subject to the IPPS). After applying the trims as previously described, the applicant identified 17,173 remaining cases.
Using the 17,173 cases, the applicant determined an average case-weighted unstandardized charge per case of $122,565. The applicant standardized the charges for each case and inflated each case's charges from FY 2017 to FY 2019 by applying the outlier charge inflation factor of 1.085868 from the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20581). The applicant indicated that the current average cost of the CivaSheet® device is $24,132.86. The applicant then added charges for CivaSheet® by taking the cost of the device and converting it to a charge by dividing the costs by the national average CCR of 0.309 for implants from the FY 2019 IPPS/LTCH PPS final rule (83 FR 41273). The applicant calculated an average case-weighted standardized charge per case of $188,897 using the percent distribution of MS-DRGs as case weights. Based on this analysis, the applicant determined that the final inflated average case-weighted standardized charge per case for CivaSheet® exceeded the average case-weighted threshold amount of $87,446 by $101,451.
In the proposed rule, we noted that the inflation factor used by the applicant was the proposed 2-year inflation factor, which was discussed in the FY 2019 IPPS/LTCH PPS final rule summation of the calculation of the FY 2019 IPPS outlier charge inflation factor for the proposed rule (83 FR 41718 through 41722). The final 2-year inflation factor published in the FY 2019 IPPS/LTCH PPS final rule was 1.08864 (83 FR 41722), which was revised in the FY 2019 IPPS/LTCH PPS final rule correction notice to 1.08986 (83 FR 49844). However, we noted that even when using either the final rule values or the corrected final rule values published in the correction notice to inflate the charges, the final inflated average case-weighted standardized charge per case for CivaSheet® would exceed the average case-weighted threshold amount. We invited public comments on whether the CivaSheet® meets the cost criterion.
Comment: The applicant submitted public comments reiterating its previously submitted cost analysis. The applicant further stated that it believes the technology meets the cost criterion.
Response: After consideration of the public comments we received, we agree that the CivaSheet® meets the cost criterion.
With regard to the substantial clinical improvement criterion, the applicant asserted that CivaSheet® represents a substantial clinical improvement over existing technologies because it provides the following: (1) Improved local control of different cancers; [52] (2) reduced rate of device-related complications; [53] (3) reduced rate of radiation toxicity; [54] (4) decreased future hospitalizations; [55] (5) decreased rate of subsequent therapeutic interventions; [56] (6) improvement in back pain and appetite in pancreatic cancer patients [57] and (7) improved local control for pancreatic cancer patients.[58]
With regard to improved local control of different cancers, the applicant provided the clinical outcomes results of a 20-month report of a patient who had been diagnosed with leiomyosarcoma of the pelvic sidewall.[59] According to the report, the purpose of the report was to document the experience of using the CivaSheet® implant as adjuvant intraoperative treatment in a patient who had been diagnosed with locally advanced leiomyosarcoma of the lateral pelvic sidewall. The patient analyzed in this report is a 62-year-old African American male who was found to have a mass incidentally in the left pelvic sidewall. The patient presented with lower abdominal pain, hematuria, and lower left flank pain radiating to the left groin. A CT scan revealed a mass in the left pelvic sidewall that measured 8.1 x 6.4 x 3.7 cm, with encasement of the left common iliac vein and no distant metastasis. A biopsy revealed a high-grade leiomyosarcoma. Given his advanced clinical stage and iliac vein encasement, neoadjuvant pelvic radiotherapy with IMRT, surgical resection with reconstruction, and a boost with intraoperative LDR brachytherapy were performed. The patient was treated with pelvic IMRT (50.4 Gy/28 fractions). The patient then underwent gross total resection and the CivaSheet® was implanted intraoperatively. The patient recovered well from the interventions, according to the report. At 20 months after implantation of the LDR brachytherapy device, clinical evaluations and CT imaging surveillance demonstrated no evidence of residual disease, according to the report.
With regard to reducing the rate of device-related complications, the applicant summarized four case series. In the four case series, the CivaSheet® device was used to treat: (1) Axillary squamous cell carcinoma; [60] (2) retroperitoneal sarcoma; [61 62 63] (3) gastric signet ring adenocarcinoma; (4) pancreatic cancer; and (5) other abdominal malignancies. There were 13 patients associated with these 4 case series.
Seneviratne, et al.'s case series report documented experience with the use of the CivaSheet® device in a 78 year old male patient who had been diagnosed with axillary squamous cell carcinoma. According to the case series report, prior to surgery a dose of 58 Gy, prescribed to the 95 percent isodose line (±5 percent), was delivered in 2 Gy fractions with 3-dimensional conformal EBRT with concurrent weekly administration of cisplatin 40 mg/m2 at an outside facility. Magnetic resonance imaging scans obtained 3 months post-treatment revealed that the mass had decreased in size to 3.8 cm × 2.5 cm × 3.9 cm, but maintained encasement of the axillary artery, axillary vein, and several inferior branches of the brachial plexus. Concerns with regard to increased toxicity to the axillary structures discouraged further EBRT, and the CivaSheet® device was implanted immediately post tumor resection. Given that microscopic disease within formerly irradiated tissue was being treated, a prescription dose of 20 Gy at 5 mm from the surface of the mesh was considered adequate because of its delivery of a biologically effective dose (BED)-10 of 39.8 Gy and equivalent dose (EQD)-2 of 33.2 Gy to the tumor bed, while limiting the D2cc for the brachial plexus to a BED3 of 27.9 Gy and EQD2 of 16.7 Gy, based on post implant analysis. According to the Seneviratne, et al. analysis, this approach allowed for a significantly limited dose to be delivered to the brachial plexus. A composite dose constraint of D2cc of 75 Gy was selected on the basis of recent data showing elevated clinical brachial plexopathy rates beyond this threshold. This constraint was met with an estimated composite EQD2 of 74.7 Gy, which, according to the applicant, would not have been obtainable with EBRT to a tumor bed EQD2 of greater than or equal to 30 Gy. The patient was discharged on the same day with instructions on wound care and radiation safety. According to the applicant, the incision healed well, with no signs of infection, seroma, or lymphadenopathy during monthly follow-up visits. At the 8-month follow-up visit, the patient was documented to only have minor shoulder pain. Seneviratne, et al., also discussed their views on the advantages of the use of the CivaSheet® device, which include its bio-absorbability, ease of visualization with imaging, potential for intra-operative customization, ability to complement various treatment approaches including EBRT and surgical resection, and ease of implantation with minimal training.
To further substantiate its assertions of a reduced rate of device-related complications regarding the CivaSheet® device, the applicant stated that its malleability is likely to be particularly useful in treating irregularly shaped surgical cavities, such as those created after breast lumpectomies or pelvic side wall resections. According to the applicant, the CivaSheet® device also overcomes several shortcomings observed even among those LDR mesh devices that use the same isotope. According to the applicant, as the vicryl sutures of traditional LDR mesh devices bend and curve around irregular surfaces during placement, the spacing and orientation of the radioactive seeds may be altered, leading to unpredictable variations in isodose geometry. The applicant stated that, in contrast, the polymer encapsulation of the Pd-103 Civa seeds before embedding within the membrane allows the sources to maintain their orientation in space and deliver radiation in accordance with the predetermined geometry. According to the applicant, additionally, unlike older LDR mesh devices that run the risk of source dispersion after mesh degradation, the polymer encapsulation allows the seeds to maintain their placement even as the membrane is absorbed over time. In this same case study, Seneviratne, et al., stated that a 3-month post implantation imaging of the CivaSheet® device demonstrated that the radioactive source geometry had remained stable since the initial implantation.
The applicant also provided Howell, et al.'s case series results of six patients diagnosed with recurrent retroperitoneal sarcoma who had been treated with the use of the CivaSheet® device to support its claims of reduced rate of toxicity and improved local control. Similar to the Seneviratne, et al. case series report, Howell, et al.'s case series' report also noted concerns regarding prior EBRT, costs associated with intra-operative radiation therapy both for the patient and the hospital, and concerns of at-risk surrounding anatomic structures. Given these concerns, Howell, et al.'s case series report also investigated LDR brachytherapy using CivaSheet®. Amongst the six patients observed, five patients had diagnoses of recurrent disease in the retroperitoneum or pelvic side wall; one patient had a diagnosis of locally-advanced leiomyosarcoma with no previous treatment. Regarding prior treatment, two patients had prior EBRT at first diagnosis. Four patients received neoadjuvant EBRT prior to surgery in addition to treatment involving CivaSheet® brachytherapy. The LDR brachytherapy dose was determined using radiobiological calculations of biological effective dose (BED) based on the linear-quadratic model and EQD2 values. An LDR brachytherapy dose of 20 to 60 Gy (36 Gy mean) was administered, corresponding to BED values of 15 to 53 Gy (29 Gy mean) and EQD2 values of 12 to 43 Gy (23 Gy mean). Because the goal was to provide a conformal radiation boost for an additional 15 to 20 Gy EQD2, the prescribed absorbed doses were considered appropriate. All patients were followed by CT scan to assess implant migration, observed radiation-related toxicities, and evidence for local recurrence between 2.5 weeks and 3 months. No evidence of implant migration or radiation-related toxicities was found. Based on these results, the study concluded that LDR directional brachytherapy delivered a targeted dose distribution that was successfully used to treat retroperitoneal sarcoma, and that the utilized device is an important option for the treatment of patients who have been diagnosed with retroperitoneal sarcoma having close/positive surgical margins and/or in combination with EBRT to optimize local control.
Two other case series, by Zhen, H. et al.,[64] and Turian, et al.,[65] were submitted by the applicant to support the assertion of reduced rate of device-related complications. Both case series assessed the use of LDR brachytherapy using the CivaSheet® device in the tumor bed given the same clinical challenges outlined in case series observed and investigated in the Seneviratne, et al., and Howell, et al. analyses in patients previously treated with chemoradiation protocols and in patients who had been diagnosed with recurrent tumors close to important functional tissues. Both case series assessed LDR brachytherapy using the CivaSheet® device in the treatment of different cancers like retroperitoneal sarcomas, pancreatic cancers, and gastric singnet ring adenocarcinoma or other abdominal carcinomas. Both case series followed the patients with CT imaging sometime between 2.5 weeks and 86 weeks. Both case series' study concluded that LDR brachytherapy with the use of the CivaSheet® device was a feasible alternative treatment modality for the cancers treated in each case series. According to Zhen, et al., an advantage of using the CivaSheet® device is that the CivaDot sheets can be easily cut to any size and shape at the time of implant. The author further stated that the CivaDot sheet is malleable and can conform to curved surfaces. This device characteristic, according to the author, gives the physician more flexibility to treat tumor beds with irregular shapes and surface curvatures compared with electron beam cylindrical applicators, thereby reducing the rate of device-related complications. However, the analysis by Zhen, et al. also indicated that a limitation in dosimetric evaluation using CT imaging is related to the inability to identify the orientation of the individual CivaDot mainly because of limited resolution and metal artifact caused by the gold plating. CivaDot orientation is inferred from the fact that all dots are embedded in a membrane that is sutured to the tumor bed and because the post-implant CT scan shows the shape of the CivaSheet® seeds being maintained. Also, Zhen, et al. noted that surgical clips could be mistakenly identified as CivaDots. The analysis by Zhen, et al. recommended that the use of surgical clips should be minimized.
With regard to the reduced rate of toxicity, the applicant provided a clinical case series by Howell, et al.[66] to show that shielding healthy tissues while irradiating the tumor bed after surgical resection was achieved by providing a conformal radiotherapy, a novel Pd-103 low-dose rate (LDR) brachytherapy device. Methods and materials of the case include the following: the LDR brachytherapy device was considered for patients who had been diagnosed with recurrent retroperitoneal sarcoma, had received prior radiotherapy to the area, and/or had anatomy concerning for high-risk margins predicted for recurrence after resection. The case series included the clinical conclusions for five patients who had been diagnosed with recurrent disease in the retroperitoneum or pelvic side wall, one patient who had been diagnosed with locally-advanced leiomyosarcoma with no previous treatment, two patients who had prior EBRT at first diagnosis, and four patients who received neoadjuvant EBRT prior to surgery in combination with brachytherapy. The LDR brachytherapy dose was determined using radiobiological calculations of biological effective dose (BED) based on the linear-quadratic model and EQD2 values. An LDR brachytherapy dose of 20 to 60 Gy (36 Gy mean) was administered, corresponding to BED values of 15 to 53 Gy (29 Gy mean) and EQD2 values of 12 to 43 Gy (23 Gy mean). Because the goal was to provide a conformal radiation boost for an additional 15 to 20 Gy EQD2, the prescribed absorbed doses were considered appropriate. According to the applicant, results showed that radiation was delivered to the at-risk tissues with minimal irradiation of adjacent healthy structures or structures occupying the surgical cavity after tumor resection. According to the applicant, clinical outcomes indicated feasibility for surgical implantation and promising results in comparison to current standards-of-care. The device did not migrate over the course of follow-up and there were no observed radiation-related toxicities.
The Howell, et al. clinical case series concluded that LDR directional brachytherapy delivered a targeted dose distribution that was successfully used to treat retroperitoneal sarcoma and that the utilized device is an important option for the treatment of patients who have been diagnosed with retroperitoneal sarcoma having close/positive surgical margins and/or in combination with EBRT to optimize local control.
The applicant also cited three additional case series to support their assertions of reduced rate of device-related complications and reduced rate of radiation toxicity. The first is on file at CivaTech in which they indicated that more than 60 patients, since 2015, had CivaSheet® implanted with no reported device-related toxicity in patients previously treated with maximal EBRT. No other details were provided by the applicant. The second case series by Taunk, et al.[67] assessed the use of CivaSheet® in three patients who had been diagnosed with colorectal adenocarcinoma who had undergone prior induction chemotherapy and neoadjuvant chemoradiation. CivaSheet® was placed in the tumor bed and patients were followed with CT imaging to assess implant migration, 30- and 90-day radiation toxicity and local recurrence. One patient was deemed not a feasible candidate because the CivaSheet® could not be uniformly opposed to the sacrum due to the degree of concavity. The other two patients underwent successful CivaSheet® implantation, and at 30 days showed stability of the device and no apparent toxicity. In the final additional case series from Rivard, et al.,[68] a single patient who had been diagnosed with pelvic side wall cancer (type not indicated) was implanted with CivaSheet® and the CivaSheet® dose distributions were compared to those of conventional low-dose rate, low-energy photon-emitting brachytherapy seeds (that is, palladium 103, Iodine-125, and Cesium-131). According to the applicant, results suggest gold-shielding CivaDots attenuate radiation for directional brachytherapy and CivaSheet® provides a therapeutic target dose, while substantially minimizing critical structure doses. In this specific case study, the applicant stated that the use of CivaSheet® showed decreased radiation to adjacent organs, such as the bowel and the bladder.
With regard to decreasing the number of future hospital visits, the applicant provided a poster presentation presented at the American Brachytherapy Society 2017 Annual Meeting. The purpose of this study was to investigate the feasibility of using intra-operative directional brachytherapy for the treatment of squamous cell carcinoma of the oropharynx. The study included a single patient who had received a prior course of external beam radiation therapy of 70 Gy in 2015. Due to positive margins near the carotid after the resection, and the increased risk of additional external radiation, brachytherapy was considered as a treatment option. CivaSheet® was used for the implant. The Pd-103 sources were spaced 8 mm apart on a rectangular grid. Unidirectional dose was achieved by a 0.05 mm thick gold disk-shaped foil on the reverse side of each source. A dose of 120 Gy at 5 mm depth was prescribed. After the resection, the entire polymer sheet was placed on the treatment area to determine the needed dimensions. The CivaSheet® device was then removed and cut to size with scissors leaving 26 Pd-103 sources remaining. The surgeon used 3.0 vicryl sutures for attachment in a concave shape over the carotid artery, where there was a positive margin. The gold foil was positioned to protect the neck flap and closure. The surgical team completed the procedure and the patient recovered without any complications.
Results of the study showed that the sources remained in position in a concave array pattern. Due to the dose fall-off of Pd-103, the calculated dose to critical structures was minimized. Because the surgical implant of the CivaDot sheet proceeded as expected with no complications and the post-implant plan indicated that the CivaSheet® remained in position with the radioactive side contacting the treatment area, the applicant asserts that future hospital visits will be decreased because the patient will not return for EBRT.
With regard to decreases in the rate of subsequent therapeutic interventions, the applicant stated that the standard-of-care for most patients undergoing surgery is typically preceded or followed by a form of external beam radiation therapy. A typical course of intensity modulated radiation therapy (IMRT) is 25 to 30 fractions (separate treatments) delivered over the course of 3 to 6 weeks. The applicant stated that, for some patients, CivaSheet® will be the only form of radiation therapy they will receive. CivaSheet® is implanted in one procedure and radiation is locally delivered over the course of several weeks, while the sources provide a continuous dose and later decay. The device is not removed and no additional follow-up visits are required for the patient to receive therapeutic intervention. According to the applicant, use of CivaSheet® can avoid the time and expense of dozens of radiation therapy visits over the course of several weeks as compared to EBRT. The applicant further stated that the published clinical data provided with its application [69] shows that the use of CivaSheet® is an effective and safe combinational treatment to external beam radiation therapy. According to the applicant, radiation oncologists can use CivaSheet® to increase the dose of radiation that can be delivered to a tumor margin, without increasing toxicity and that this may reduce the odds that a patient experiences cancer recurrence.[70 71 72] The applicant also asserted that the targeted radiation approach has demonstrated no toxic effects for patients. The applicant further stated that other forms of radiation have a known rate of complications and toxicity that result in the need for additional therapies and interventions (for example, topical creams for skin reddening, and medicine for pain). The applicant indicated that there has been no change in concomitant medications prescribed because of the use of the CivaSheet® implant either on or off trial. The applicant did not link these claims to any of the studies provided with its application. In addition, the applicant asserts that, of the case studies they provided, there have been no instances of therapeutic interventions to resolve an issue that was induced by the use of the CivaSheet® device to deliver radiation.[73 74 75]
With regard to improvement in back pain and appetite (compared to baseline) in pancreatic cancer patients, the applicant asserted that patients answered standardized, international questionnaire EORTC QLQ-C30 and PANC26 and that these results are on file at CivaTech. The applicant provided the baseline, 70 days post-operative and 98 days postoperative patient responses to “Have you ever had back pain?” Baseline response: 1.5; 70 days post-operative response: 1.0 and 98 days post-operative response: 1.0. The applicant also provided baseline, 70 days post-operative and 98 days post-operative patient responses to “Were you restricted in the amounts of food you could eat as a result of your disease or treatment?” Baseline response: 2.5; 70 days postoperative response: 1.0 and 98 days postoperative response: 1.0. (Response Values: 1.0 = “Not at all”; 2.0 = “A little”; 3.0 = “Quite a bit”; 4.0 = “Very much”).
With regard to improved local control for pancreatic cancer patients, the applicant provided the results of a dosimetric study entitled, “Widening the Therapeutic Window Using an Implantable, Uni-directional LDR Brachytherapy Sheet as a Boost in Pancreatic Cancer Case Series,” a poster presented at the ASTRO 2018 Annual Meeting. According to background information in the applicant's poster, pancreatic patients often undergo neoadjuvant chemotherapy and chemoradiation in preparation for surgical resection of the tumor. In addition, oftentimes after neoadjuvant therapy there are inflammatory changes that, unfortunately, hinder pre-operative imaging and create the potential for unreliable determination of tumor resection. Accompanying the potentially unreliable determination of tumor resectability are patient concerns when positive retroperitoneal margins have close proximity to major vasculature. The applicant noted that additional EBRT boost, initiated post operatively, is an option, but difficult given bowel constraints and the difficulty in identifying the area at highest risk. Given these constraints associated with treating pancreatic cancers, the purpose of this study was to demonstrate the ability of the LDR brachytherapy CivaSheet® device to deliver a focal high-dose boost, targeted to the area at highest risk in patients who received neoadjuvant chemoradiation. This dosimetric case series consisted of four patients who had been diagnosed with borderline resectable pancreatic cancer who received neoadjuvant FOLFIRINOX followed by gemcitabine-based chemoradiotherapy (chemoRT) to 50.4 Gy in 28 fractions with dose prescribed to the gross tumor plus a 1 cm margin. According to the poster provided by the applicant, after neoadjuvant therapy, the multidisciplinary team was concerned for close or positive margin resection. Using the CivaSheet® device, a 38 Gy EQD2 dose to 5 mm depth was implanted in these patients and a total dose of 88.4 Gy was delivered to the targeted tissue. Post-operatively, patients had a CT scan to identify the tumor bed contour, as well as the contour of surrounding at-risk organs; the small bowel (SB) was contoured as the bowel bag and included the entire peritoneal cavity. Following the CT scan, brachytherapy plans, as well as EBRT boost plans, were created for each patient. A dose-volume histogram (DVH) from initial 3D treatment plans for all patients showed the SB volume receiving 45 Gy (V45) was a median of 78.2 cc (range 61.7-107.1 ccs) and maximum bowel doses were a median of 53.2 Gy, range 53.1-53.6 Gy. According to the applicant, the V45 for SB should be less than 195 cc, with a maximum of less than or equal to 58 Gy to prevent SB obstruction, fistula and perforation. According to the applicant, with the CivaSheet® device, the boost dose was dramatically increased while SB exposure was marginal at about 1/10th of the prescription dose. For the target, the CivaSheet® delivered the prescription dose to 5 mm depth with a large inhomogeneous dose throughout the tumor bed with the minimum dose of 38 Gy. Dosimetric comparison of a CivaSheet® tumor bed boost and a Stereotactic Body Radiation Therapy (SBRT) tumor bed boost to the SB was 9.6 Gy compared to 24 Gy for external beam plan. According to the applicant, the conclusions from this case series are that applying a brachytherapy uni-directional source to the area at highest risk can serve to improve the therapeutic index by improving the local control and minimizing toxicities in pancreatic cancer patients after neoadjuvant therapy.
With regard to whether CivaSheet® represents a substantial clinical improvement relative to other brachytherapy technologies currently available, in the proposed rule we stated that we were concerned that all of the supporting data appear to be feasibility studies substantiating the use of the CivaSheet® in different cancers and difficult anatomic locations. We also we stated that we were concerned that there do not appear to be any comparisons to other current treatments, nor any long-term follow-up with comparisons to currently available therapies. We invited public comments on whether CivaSheet® meets the substantial clinical improvement criterion.
Comment: The applicant submitted public comments regarding CMS' concerns. With regard to our concern that the supporting data provided by the applicant appear to be feasibility studies, the applicant stated that the feasibility studies substantiate the experience with such uses. The applicant further stated that it believes that CMS' characterization fails to reflect other aspects of these studies as they are not limited to investigating whether intraoperative radiation therapy can be delivered with the CivaSheet®, but also show positive outcomes, including providing information following patients for periods that range up to 24 or even 35 months. The applicant further stated that in the case of radiation therapy, the likely effects in the body of specific doses on target tumors and on healthy tissues are well known and can be quantified with well-developed treatment planning systems. The applicant stated that the major research questions at this stage of the product's development are not focused on either the safety or efficacy of the treatment (since the product is already cleared by the FDA) but on whether physicians in clinical practice can position it appropriately in the surgical field and on the effects of the localized, unidirectional delivery of intraoperatively applied radiation that CivaSheet® provides on outcomes of interest, including indications of toxicity and recurrence.
With regard to CMS' concern that there do not appear to be any comparisons to other current treatments, or any long-term follow-up with comparison to currently available therapies, the applicant stated that it believes that the results detailed in the following categories for CivaSheet® patients compare favorably with the results presented in the clinical literature regarding the toxicity rates for EBRT and with historical recurrence rates for patients receiving common adjunctive therapies:
- Reduced radiation toxicity—None of the patients in the associated clinical literature whose treatments have included CivaSheet® have suffered nausea, vomiting, diarrhea, constipation or fatigue, all side effects that are common with other forms of radiation therapy, due to the CivaSheet® treatment. The applicant stated that the company keeps records of all patients treated, and to date has not received any reports or complaints of acute or chronic radiation toxicity attributable to the CivaSheet® in any of the 78 patients who have received the therapy. The applicant believes this record compares favorably with the rates for toxicity for EBRT.
- Fewer therapeutic interventions and hospitalizations—The applicant stated that for the same group of patients, the local recurrence rate for disease in the treatment field of the device for patients treated with CivaSheet® is none, regardless of site of the cancer treated. The applicant stated that comparison with information drawn from the clinical literature regarding the local recurrence rate by site that would be expected if the patient were treated by the existing standards of care following surgery, including the common adjunctive procedures, external beam radiation and chemotherapy, reveals the extent of local recurrence is more favorable for CivaSheet® patients. The applicant believes that because of the absence of local recurrence in the treatment fields, patients have not required additional procedures following the primary cancer surgery, on either outpatient or inpatient basis, related to treating disease recurrence in the area treated by CivaSheet®. The applicant further stated that in addition, patients have not required further interventions or hospitalizations to treat radiation related side effects, as none have been recorded.
The applicant also provided information, by indication, to studies involving CivaSheet® and on which they have information on file. These include the literature cited in their FY 2020 new technology add-on payment application and the ongoing clinical trials. The applicant also provided an appendix summarizing key information for comparison available in the clinical literature. For each cancer type treated with CivaSheet, the applicant displayed the toxicity rates for EBRT, the most common and widely available alternative, with references cited. These range from 1.1 percent (gastrointestinal following prostatectomy) to as high as 80 percent for retroperitoneal sarcoma. According to the applicant, the comparative rates for CivaSheet treatments are zero in the published literature presented to CMS, and the company has received no reports of local recurrence or toxicity for patients treated outside of a clinical trial setting. The appendix also showed similar information for local recurrence rates. According to the applicant, in the literature, these range from 6 percent for breast cancer to as high as 60 percent for gynecogical cancers.
The applicant provided a second appendix, Appendix 2, to provide links of the claims noted in the studies provided with its application. Appendix 2 presented information, by indication, to studies involving CivaSheet® and on which the applicant has information on file to include the literature cited in its application and the ongoing clinical trials.
The applicant believes that the data it provided demonstrates a substantial clinical improvement for the treatment of Medicare patients with cancer.
We also received a public comment stating that CivaSheet provides a targeted and high enough dose to the surgical margin to control local disease without inducing side effect and that CivaSheet® has benefits for pancreatic, sarcoma and colorectal patients. The commenter did not provide additional data in support of these statements.
Response: We appreciate the public comments we received regarding whether the CivaSheet meets the substantial clinical improvement criterion, including the comments submitted by the applicant. While the applicant provided additional references and a summary of the clinical trials underway, we believe the data remains limited as most of the clinical trials will not complete enrollment until 2020. Further, the majority of the evidence submitted to date still focuses on limited numbers of patients who participated in feasibility studies with no comparator arms nor clinical outcome results. Finally, the single clinical trial that has been completed is not anticipated to have data available until third quarter 2019. For these reasons, we are unable to determine that the CivaSheet® represents a substantial clinical improvement over existing therapies. Therefore, we are not approving new technology add-on payments for the CivaSheet® for FY 2020.
d. EluviaTM Drug-Eluting Vascular Stent System
Boston Scientific Corporation submitted an application for new technology add-on payments for the EluviaTM Drug-Eluting Vascular Stent System for FY 2020. EluviaTM, a drug-eluting stent for the treatment of lesions in the femoropopliteal arteries, received FDA premarket approval (PMA) on September 18, 2018.
According to the applicant, the EluviaTM system is a sustained-release drug-eluting stent indicated for improving luminal diameter in the treatment of peripheral artery disease (PAD) with symptomatic de novo or restenotic lesions in the native superficial femoral artery (SFA) and or proximal popliteal artery (PPA) with reference vessel diameters (RVD) ranging from 4.0 to 6.0 mm and total lesion lengths up to 190 mm.
The applicant stated that PAD is a circulatory condition in which narrowed arteries reduce blood flow to the limbs, usually in the legs. Symptoms of PAD may include lower extremity pain due to varying degrees of ischemia, claudication which is characterized by pain induced by exercise and relieved with rest. According to the applicant, risk factors for PAD include individuals who are age 70 years old and older; individuals who are between the ages of 50 years old and 69 years old with a history of smoking or diabetes; individuals who are between the ages of 40 years old and 49 years old with diabetes and at least one other risk factor for atherosclerosis; leg symptoms suggestive of claudication with exertion, or ischemic pain at rest; abnormal lower extremity pulse examination; known atherosclerosis at other sites (for example, coronary, carotid, renal artery disease); smoking; hypertension, hyperlipidemia, and homocysteinemia.[76] PAD is primarily caused by atherosclerosis—the buildup of fatty plaque in the arteries. PAD can occur in any blood vessel, but it is more common in the legs than the arms. Approximately 8.5 million people in the United States have PAD, including 12 to 20 percent of individuals who are age 60 years old and older.[77]
A diagnosis of PAD is established with the measurement of an ankle-brachial index (ABI) less than or equal to 0.9. The ABI is a comparison of the resting systolic blood pressure at the ankle to the higher systolic brachial pressure. Duplex ultrasonography is commonly used, in conjunction with the ABI, to identify the location and severity of arterial obstruction.[78]
Management of the disease is aimed at improving symptoms, improving functional capacity, and preventing amputations and death. Management of patients who have been diagnosed with lower extremity PAD may include medical therapies to reduce the risk for future cardiovascular events related to atherosclerosis, such as myocardial infarction, stroke, and peripheral arterial thrombosis. Such therapies may include antiplatelet therapy, smoking cessation, lipid-lowering therapy, and treatment of diabetes and hypertension. For patients with significant or disabling symptoms unresponsive to lifestyle adjustment and pharmacologic therapy, intervention (percutaneous, surgical) may be needed. Surgical intervention includes angioplasty, a procedure in which a balloon-tip catheter is inserted into the artery and inflated to dilate the narrowed artery lumen. The balloon is then deflated and removed with the catheter. For patients with limb-threatening ischemia (for example, pain while at rest and or ulceration), revascularization is a priority to reestablish arterial blood flow. According to the applicant, treatment of the SFA is problematic due to multiple issues including high rate of restenosis and significant forces of compression.
The applicant describes EluviaTM Drug-Eluting Vascular Stent System as a sustained-release drug-eluting self-expanding, nickel titanium alloy (nitinol) mesh stent used to reestablish blood flow to stenotic arteries. According to the applicant, the EluviaTM stent is coated with the drug paclitaxel, which helps prevent the artery from restenosis. The applicant stated that EluviaTM's polymer-based drug delivery system is uniquely designed to sustain the release of paclitaxel beyond 1 year to match the restenotic process in the SFA. According to the applicant, the EluviaTM Stent System is comprised of: (1) The implantable endoprosthesis; and (2) the stent delivery system (SDS). On both the proximal and distal ends of the stent, radiopaque markers made of tantalum increase visibility of the stent to aid in placement. The tri-axial designed delivery system consists of an outer shaft to stabilize the stent delivery system, a middle shaft to protect and constrain the stent, and an inner shaft to provide a guide wire lumen. The delivery system is compatible with 0.035 in (0.89 mm) guide wires. The EluviaTM stent is available in a variety of diameters and lengths. The delivery system is offered in 2 working lengths (75 cm and 130 cm).
As discussed previously, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would, therefore, not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, according to the applicant, EluviaTM uses a unique mechanism of action which has not been utilized by previously available medical devices for treating stenotic lesions in the SFA. The applicant asserted that the EluviaTM Drug-Eluting Vascular Stent System is a device/drug combination product composed of an implantable stent, combined with a polybutyl methacrylate (PBMA) primer layer, a paclitaxel/polyvinylidene difluoride (PVDF) polymer, and a stent delivery system. According to the applicant, the polymer carries and protects the drug before and during the procedure and ensures that the drug is released into the tissue in a controlled, sustained manner to prevent restenosis of the vessel. According to the applicant, the EluviaTM system continues to deliver paclitaxel to combat restenosis for 12 to 15 months, which involves a novel and distinct mechanism of action different than other drug-coated balloons or drug-coated stents that only deliver the drug to the artery for about 2 months. According to the applicant, the PBMA polymer is clinically proven to permit the sustained release of paclitaxel to achieve a therapeutic outcome. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19313), we noted that, the applicant submitted a request for consideration for approval at the March 2019 ICD-10 Coordination and Maintenance Committee Meeting for a unique ICD-10-PCS procedure code to describe procedures which use the EluviaTM stent system. Approval was granted for the following procedure codes effective October 1, 2019:




With regard to the second criterion, whether a technology is assigned to the same or a different MS-DRG, the applicant asserted that patients who may be eligible for treatment using the EluviaTM system include hospitalized patients who have been diagnosed with PAD. According to the applicant, these potential cases may map to multiple MS-DRGs, the most likely being MS-DRGs 252 (Other Vascular Procedures With MCC), 253 (Other Vascular Procedures With CC) and 254 (Other Vascular Procedures Without CC/MCC). In the proposed rule, we stated that potential cases representing patients who may be eligible for treatment using the EluviaTM system would be assigned to the same MS-DRGs as cases representing hospitalized patients who have been diagnosed with PAD and treated with currently available technologies.
With regard to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population when compared to an existing technology, according to the applicant, clinical conditions that may require use of the EluviaTM stent system include treatment of the same patient population as cases identified with a variety of diagnosis codes from the ICD-10-CM category I70 (Atherosclerosis) as listed in this table:


The applicant asserted that the EluviaTM stent is not substantially similar to any existing technology because it uses a unique mechanism of action, when compared to existing technologies to achieve a therapeutic outcome and, therefore, meets the newness criterion.
In the proposed rule, we stated that we were concerned as to whether the polymer drug carrier system that the EluviaTM system uses is, in fact, a new mechanism of action as compared to stents that contain paclitaxel without the carrier polymer. We stated that we were concerned that the EluviaTM device may have a mechanism of action similar to the paclitaxel-coated Zilver® Drug-Eluting Peripheral Stent, which is indicated for improving luminal diameter for the treatment of de novo or restenotic symptomatic lesions in native vascular disease of the above-the-knee femoropopliteal arteries having reference vessel diameter from 4 mm to 7 mm and total lesion lengths up to 300 mm per patient. We invited public comments on whether the EluviaTM system is substantially similar to existing technology and whether it meets the newness criterion, including with respect to the concerns we raised.
Comment: The applicant commented that the EluviaTM device's mechanism of action is different from that of the paclitaxel-coated Zilver PTX (Zilver® Drug-Eluting Peripheral Stent) because the EluviaTM device's polymer matrix layer allows for targeted, localized, sustained, low-dose amorphous paclitaxel delivery to peripheral artery lesions over the course of the peripheral restenotic cascade with minimal systemic distribution or particulate loss. The applicant provided a comparison of the polymer matrix stent vs. the paclitaxel-coated stent. According to the applicant, the polymer matrix stent is encased in a polymer matrix, the paclitaxel-coated stent is not. The dose density of paclitaxel for the polymer matrix vs the paclitaxel coated stent is 0.167ug/mm2 vs 3ug/mm2. Paclitaxel is delivered to the lesion via a diffusion gradient with the polymer matrix stent whereas the paclitaxel-coated stent has no diffusion gradient. Paclitaxel is released directly to the target lesion with the polymer matrix stent. Paclitaxel release is non-specific to the target lesion with paclitaxel-coated stent. Paclitaxel is released over approximately 12-15 months with the polymer matrix stent. Paclitaxel release is complete at two months with paclitaxel coated stents.
Response: We appreciate the applicant's comments and comparison of the polymer matrix EluviaTM vs the paclitaxel-coated Zilver PTX with regard to the mechanism of action. After consideration of the applicant's comments, we believe that the EluviaTM device uses a unique mechanism of action to achieve a therapeutic outcome when compared to existing technologies such as the paclitaxel-coated stent. Therefore the EluviaTM device meets the newness criterion.
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that the technology meets the cost criterion.
As noted in the proposed rule and earlier, the applicant asserted that cases involving the treatment of PAD, involving treatment of lesions in the femoropopliteal arteries typically, map to MS-DRGs 252, 253, and 254. The applicant searched the FY 2017 MedPAR data file in MS-DRGs 252, 253 and 254 for cases reporting an ICD-10-PCS procedure code for the treatment of Peripheral BMS or DES, which the applicant believed would represent cases potentially eligible for the use of the EluviaTM stent system. The applicant identified 109,747 claims for cases representing patients who may be eligible for treatment involving the EluviaTM stent system. The applicant applied the following trims: Claims paid under GHO (that is, Medicare beneficiaries enrolled in a Medicare Advantage managed care plan), claims for CAHs, IPFs, IRFs, LTCHs, Children's, Cancer, and RHNCI hospitals excluding Maryland acute-care hospitals, claims with total charges or lengths-of-stay of less than or equal to zero, claims with total charge differing from sum of charges of the 19 cost groups by greater than $30, providers that do not have charges greater than $0 for at least 14 of the 19 cost groups, claims with total charges for the MS-DRG +/− 3 standard deviations from the log mean total charges or charges per day, “IME only” claims submitted by a teaching hospital on behalf of a beneficiary enrolled in a Medicare Advantage plan, claims with claim types “61 to 64” (that is, claim types that refer to encounter claims, Medicare Advantage IME, and HMO no-pay claims), and claims for which the applicant was unable to calculate standardized charges (because the Provider Number associated with the claim does not appear in the FY 2017 impact file). This resulted in 73,861 claims across MS-DRGs 252, 253, and 254.
Using the 73,861 claims, the applicant determined an average case-weighted unstandardized charge per case of $96,232. The applicant removed all device-related charges and then standardized the charges for each case and inflated each case's charges by applying the FY 2019 IPPS/LTCH PPS final rule outlier charge inflation factor of 1.08864 (83 FR 41722). (In the proposed rule, we noted that the 2-year charge inflation factor was revised in the FY 2019 IPPS/LTCH PPS final rule correction notice to 1.08986 (83 FR 49844). We further noted that even when using the corrected final rule values to inflate the charges, the average case-weighted standardized charge per case for each scenario exceeded the average case-weighted threshold amount.) The applicant then added charges for EluviaTM by taking the cost of the device and converting it to a charge by dividing the costs by the national average CCR of 0.309 for devices from the FY 2019 IPPS/LTCH PPS final rule (83 FR 41273). The applicant calculated an average case-weighted standardized charge per case of $86,950 using the percent distribution of MS-DRGs as case-weights. Based on this analysis, the applicant determined that the final inflated average case-weighted standardized charge per case for EluviaTM exceeded the average case-weighted threshold of $81,518 by $5,432.
The applicant conducted additional analyses to demonstrate it meets the cost criterion. In these analyses, the applicant repeated the cost analysis, as previously described, with one analysis of cases reporting the ICD-10-PCS procedures codes for Peripheral DES procedures and the other analysis with cases reporting the ICD-10-PCS procedures codes for Peripheral BMS procedures. In each of these additional sensitivity analyses, the final inflated average case-weighted standardized charge per case exceeded the average case-weighted cost threshold amount. We invited public comments on whether EluviaTM meets the cost criterion.
Comment: The applicant submitted public comments reiterating the various cost analyses results. The applicant maintained that the technology meets the cost criterion.
Response: We appreciate the applicant's comments concerning the cost criterion. After consideration of the public comments we received, we agree that the EluviaTM device meets the cost criterion.
With regard to the substantial clinical improvement criterion, the applicant asserted that the EluviaTM Drug-Eluting Vascular Stent System represents a substantial clinical improvement over existing technologies because it achieves superior primary patency; reduces the rate of subsequent therapeutic interventions; decreases the number of future hospitalizations or physician visits; reduces hospital readmission rates; reduces the rate of device-related complications; and achieves similar functional outcomes and EQ-5D index values while associated with half the rate of target lesion revascularizations (TLRs).
The applicant submitted the results of the MAJESTIC study, a single-arm, first-in-human study of EluviaTM. The MAJESTIC [79] study is a prospective, multi-center, single-arm, open-label study. According to the applicant, the MAJESTIC study demonstrated long-term treatment durability among patients whose femoropopliteal arteries were treated with the EluviaTM stent. The applicant asserts that the MAJESTIC study demonstrates the sustained impact of the EluviaTM stent on primary patency. The MAJESTIC study enrolled 57 patients who had been diagnosed with symptomatic lower limb ischemia and lesions in the superficial femoral artery or proximal popliteal artery. Efficacy measures at 2 years included primary patency, defined as duplex ultrasound peak systolic velocity ratio of less than 2.5 and the absence of target lesion revascularization (TLR) or bypass. Safety monitoring through 3 years included adverse events and TLR. The 24-month clinic visit was completed by 53 patients; 52 had Doppler ultrasound evaluable by the core laboratory, and 48 patients had radiographs taken for stent fracture analysis. The 3-year follow-up was completed by 54 patients. At 2 years, 90.6 percent (48/53) of the patients had improved by 1 or more Rutherford categories as compared with the pre-procedure level without the need for TLR (when those with TLR were included, 96.2 percent sustained improvement); only 1 patient exhibited a worsening in level, 66.0 percent (35/53) of the patients exhibited no symptoms (category 0) and 24.5 percent (13/53) had mild claudication (category 1) at the 24-month visit. Mean ABI improved from 0.73 ± 0.22 at baseline to 1.02 ± 0.20 at 12 months and 0.93 ± 0.26 at 24 months. At 24 months, 79.2 percent (38/48) of the patients had an ABI increase of at least 0.1 compared with baseline or had reached an ABI of at least 0.9. The applicant also noted that at 12 months the Kaplan-Meier estimate of primary patency was 96.4 percent.
With regard to the EluviaTM stent achieving superior primary patency, the applicant submitted the results of the IMPERIAL [80] study in which the EluviaTM stent is compared, head-to-head, to the Zilver® PTX Drug-Eluting stent. The IMPERIAL study is a global, multi-center, randomized controlled trial consisting of 465 subjects. Eligible patients were aged 18 years old or older and had a diagnosis of symptomatic lower-limb ischaemia, defined as Rutherford Category 2, 3, or 4 and stenotic, restenotic (treated with a drug-coated balloon greater than 12 months before the study or standard percutaneous transluminal angioplasty only), or occlusive lesions in the native superficial femoral artery or proximal popliteal artery, with at least 1 infrapopliteal vessel patent to the ankle or foot. Patients had to have stenosis of 70 percent or more (via angiographic assessment), vessel diameter between 4 mm and 6 mm, and total lesion length between 30 mm and 140 mm.
Patients who had previously stented target lesion/vessels treated with drug-coated balloon less than 12 months prior to randomization/enrollment and patients who had undergone prior surgery of the SFA/PPA in the target limb to treat atherosclerotic disease were excluded from the study. Two concurrent single-group (EluviaTM only) sub-studies were done: A non-blinded, non-randomized pharmacokinetic sub-study and a non-blinded, non-randomized study of patients who had been diagnosed with long lesions (greater than 140 mm in diameter). The IMPERIAL study is a prospective, multi-center, single-blinded randomized, controlled (RCT) non-inferiority trial. Patients were randomized (2:1) to implantation of either a paclitaxel-eluting polymer stent (EluviaTM) or a paclitaxel-coated stent (Zilver® PTX) after the treating physician had successfully crossed the target lesion with a guide wire. The primary endpoints of the study are Major Adverse Events defined as all causes of death through 1 month, Target Limb Major Amputation through 12 months and/or Target Lesion Revascularization (TLR) through 12 months and primary vessel patency at 12 months post-procedure. Secondary endpoints included the Rutherford categorization, Walking Impairment Questionnaire, and EQ-5D assessments at 1 month and 6 months post-procedure. Patient demographic and characteristics were balanced between EluviaTM stent and Zilver® PTX stent groups.
The applicant noted that lesion characteristics for the patients in the EluviaTM stent versus the Zilver® PTX stent arms were comparable. Clinical follow-up visits related to the study were scheduled for 1 month, 6 months, and 12 months after the procedure, with follow-up planned to continue through 5 years, including clinical visits at 24 months and 5 years and clinical or telephone follow-up at 3 and 4 years.
The applicant asserted that in the IMPERIAL study the EluviaTM stent demonstrated superior primary patency over the Zilver® PTX stent, 86.8 percent versus 77.5 percent, respectively (p=0.0144). The non-inferiority primary efficacy endpoint was also met. The applicant asserts that the SFA presents unique challenges with respect to maintaining long-term patency. There are distinct pathological differences between the SFA and coronary arteries. The SFA tends to have higher levels of calcification and chronic total occlusions when compared to coronary arteries. Following an intervention within the SFA, the SFA produces a healing response which often results in restenosis or re-narrowing of the arterial lumen. This cascade of events leading to restenosis starts with inflammation, followed by smooth muscle cell proliferation and matrix formation.[81] Because of the unique mechanical forces in the SFA, this restenotic process of the SFA can continue well beyond 300 days from the initial intervention. Results from the IMPERIAL study showed that primary patency at 12 months, by Kaplan-Meier estimate, was significantly greater for EluviaTM than for Zilver® PTX, 88.5 percent and 79.5 percent, respectively (p=0.0119). According to the applicant, these results are consistent with the 96.4 percent primary patency rate at 12 months in the MAJESTIC study.
The IMPERIAL study included two concurrent single-group (EluviaTM only) sub-studies: A non-blinded, non-randomized pharmacokinetic sub-study and a non-blinded, non-randomized study of patients with long lesions (greater than 140 mm in diameter). For the pharmacokinetic sub-study, patients had venous blood drawn before stent implantation and at intervals ranging from 10 minutes to 24 hours post implantation, and again at either 48 hours or 72 hours post implantation. The pharmacokinetics sub-study confirmed that plasma paclitaxel concentrations after EluviaTM stent implantation were well below thresholds associated with toxic effects in studies in patients who had been diagnosed with cancer (0·05 μM or ~43 ng/mL).
The IMPERIAL sub-study long lesion subgroup consisted of 50 patients with average lesion length of 162.8 mm that were each treated with two EluviaTM stents. According to the applicant, 12-month outcomes for the long lesion subgroup are 87 percent primary patency and 6.5 percent Target Lesion Revascularization (TLR). According to the applicant, in a separate subgroup analysis of patients 65 years old and older (Medicare population), the primary patency rate in the EluviaTM stent group is 92.6 percent, compared to 75.0 percent for the Zilver® PTX stent group (p=0.0386).
With regard to reducing the rate of subsequent therapeutic interventions, secondary outcomes in the IMPERIAL study included repeat re-intervention on the same lesion, target lesion revascularization (TLR). The rate of subsequent interventions, or TLRs, in the EluviaTM stent group was 4.5 percent compared to 9.0 percent in the Zilver® PTX stent group. The applicant asserted that the TLR rate in the EluviaTM group represents a substantial reduction in re-intervention on the target lesion compared to that of the Zilver® PTX stent group.
With regard to decreasing the number of future hospitalizations or physician visits, the applicant asserted that the substantial reduction in the lesion revascularization rate led to a reduced need to provide additional intensive care, distinguishing the EluviaTM group from the Zilver® PTX stent group. In the IMPERIAL study, EluviaTM-treated patients required fewer days of re-hospitalization. Patients in the EluviaTM group averaged 13.9 days of re-hospitalization for all adverse events compared to 17.7 days of re-hospitalization for patients in the Zilver® PTX stent group. Patients in the EluviaTM group were re-hospitalized for 2.8 days for TLR/Total Vessel Revascularization (TVR) compared to 7.1 days in the Zilver® PTX stent group. And lastly, patients in the EluviaTM group were re-hospitalized for 2.7 days for procedure/device-related adverse events compared to 4.5 days from the Zilver® PTX stent group.
With regard to reducing hospital readmission rates, the applicant asserted that patients treated in the EluviaTM group experienced reduced rates of hospital readmission following the index procedure compared to those in the Zilver® PTX stent group. Hospital readmission rates at 12 months were 3.9 percent for the EluviaTM group compared to 7.1 percent for the Zilver® PTX stent group. Similar results were noted at 1 and 6 months; 1.0 percent versus 2.6 percent and 2.4 percent versus 3.8 percent, respectively.
With regard to reducing the rate of device-related complications, the applicant asserted that while the rates of adverse events were similar in total between treatment arms in the IMPERIAL study, there were measurable differences in device-related complications. Device-related adverse-events were reported in 8 percent of the patients in the EluviaTM group compared to 14 percent of the patients in the Zilver® PTX stent group.
Lastly, with regard to achieving similar functional outcomes and EQ-5D index values, while associated with half the rate of TLRs, the applicant asserted that narrowed or blocked arteries within the SFA can limit the supply of oxygen-rich blood throughout the lower extremities, causing pain or discomfort when walking (claudication). The applicant further asserted that performing physical activities is often challenging because of decreased blood supply to the legs, typically causing symptoms to become more challenging over time unless treated. While functional outcomes appear similar between the EluviaTM and Zilver® PTX stent groups at 12 months, these improvements for the Zilver® PTX stent group are associated with twice as many TLRs to achieve similar EQ-5D index values.[82] Secondary endpoints improved after stent implantation and were generally similar between the groups. At 12 months, of the patients with complete Rutherford assessment data, 241 (86 percent) of 281 patients in the EluviaTM group and 120 (85 percent) of 142 patients in the Zilver® PTX group had symptoms reported as Rutherford Category 0 or 1 (none to mild claudication). The mean ankle-brachial index was 1·0 (SD 0·2) in both groups at 12 months (baseline mean ankle-brachial index 0·7 [SD 0·2] for EluviaTM; 0·8 [0·2] for Zilver® PTX), with sustained hemodynamic improvement for approximately 80 percent of the patients in both groups. Walking function improved significantly from baseline to 12 months in both groups, as measured with the Walking Impairment Questionnaire and the 6-minute walk test. In both groups, the majority of patients had sustained improvement in the mobility dimension of the EQ-5D and roughly half had sustained improvement in the pain or discomfort dimension. No significant between-group differences were observed in the Walking Impairment Questionnaire, 6-minute walk test, or EQ-5D. Secondary endpoint results for the EluviaTM stent and Zilver® PTX stent groups are as follows:
- Hemodynamic improvement in walking—80.8 percent versus 78.7 percent;
- Walking impairment questionnaire scores (change from baseline)—40.8 (36.5) versus 35.8 (39.5);
- Distance (change from baseline)—33.2 (38.3) versus 29.5 (38.2);
- Speed (change from baseline)—18.3 (29.5) versus 18.1 (28.7);
- Stair climbing (change from baseline)—19.4 (36.7) versus 21.1 (34.6); and
- 6- Minute walk test distance (m) (change from baseline)—44.5 (119.5) versus 51.8 (130.5).
In the proposed rule, we stated that we were concerned that the IMPERIAL study, which showed significant differences in primary patency at 12 months, was designed for non-inferiority and not superiority. We also noted the results of a recently published meta-analysis of randomized controlled trials of the risk of death associated with the use of paclitaxel-coated balloons and stents in the femoropopliteal artery of the leg, which found that there is increased risk of death following application of paclitaxel-coated balloons and stents in the femoropopliteal artery of the lower limbs and that further investigations are urgently warranted,[83] although the EluviaTM system was not included in the meta-analysis. We invited public comments on whether the EluviaTM system meets the substantial clinical improvement criterion, including the implications of the conclusion of the meta-analysis results with respect to a finding of substantial clinical improvement for EluviaTM.
Comment: The applicant submitted public comments regarding CMS' concerns. With regard to our concern that the IMPERIAL study was designed for non-inferiority and not superiority, the applicant stated that superiority testing was performed after the 12-month follow-up window for all enrolled subjects had closed. The applicant also stated that from a statistical perspective, the pre-specified success criteria for superiority used the same logic as the pre-specified success criteria for non-inferiority: “ELUVIA will be concluded to be superior to Zilver PTX for device effectiveness if the one-sided lower 95 percent confidence bound on the difference between treatment groups in 12-month primary patency is greater than zero.” The applicant stated that a more stringent one-sided lower 97.5 percent confidence bound (shown as two-sided 95 percent confidence interval) on the difference between treatment groups was observed to be greater than zero and the corresponding p-value was 0.0144.
In addition to the internal analysis performed by the applicant, the applicant stated that the data were published in The Lancet [84] following its rigorous peer-review process. The applicant quoted the following from The Lancet: “The superiority analysis of primary patency in the full-analysis cohort was a pre-specified post-hoc analysis” and “In this head-to-head randomized trial, the primary non-inferiority endpoints for efficacy and safety at 12 months were met, and post-hoc analysis of the 12-month patency rate showed superiority for Eluvia over Zilver PTX.”
According to the applicant, clinical trial guidelines support performing a pre-specified post-hoc superiority analysis in this situation, provided “(1) the trial has been properly designed and carried out in accordance with the strict requirements of a non-inferiority trial. (2) actual p-values for superiority are presented to allow independent assessment of the strength of the evidence and (3) analysis according to the intention-to-treat (ITT) principle is given greatest emphasis.”[85] The applicant contends that the IMPERIAL trial met all those requirements.
With respect to the results of the recently published meta-analysis of randomized controlled trials of the risk of death associated with the use of paclitaxel-coated balloons and stents in the femoropopliteal artery of the leg, which found that there is increased risk of death following application of paclitaxel-coated balloons and stents in the femoropopliteal artery of the lower limbs, in its public comment, the applicant maintained that the EluviaTM device is different from the devices evaluated in the meta-analysis. The applicant also noted that the EluviaTM device was not addressed in the meta-analysis and that the EluviaTM device delivers paclitaxel in much lower doses than the products discussed in the meta-analysis. The applicant contends that the EluviaTM device is the only peripheral device to deliver paclitaxel through a sustained-release mechanism of action where delivery of paclitaxel is controlled and focused on the target lesion. The applicant believes that the suggestion in the meta-analysis of a late-term mortality risk associated with paclitaxel coated devices is not directly applicable to the EluviaTM device. The applicant further stated that they submitted information (available at https://www.fda.gov/media/127704/download) to the FDA on paclitaxel relative to the EluviaTM device in advance of FDA's June 19-20 Circulatory System Devices Panel of the Medical Devices Advisory Committee Meeting. Consequently, the applicant does not believe that the findings of limited generalizability suggested in the meta-analysis should inhibit CMS from determining that the EluviaTM satisfies the substantial clinical improvement criterion.
In addition to the applicant's public comments, we also received several public comments supporting the EluviaTM Drug-Eluting Stent System's application for New Technology Add-on Payment in FY2020. Commenters expressed that it is important for PAD patients to have access to this technology.
We also received a comment expressing safety concerns with paclitaxel devices used to treat PAD. The commenter stated they were aware of an FDA alert concerning paclitaxel devices. The commenter stated the applicant and other manufacturers of devices using paclitaxel should consider an alternative to paclitaxel.
Response: We appreciate the applicant's and other public comments. We are aware of the FDA's March 15, 2019 Letter to healthcare providers regarding the “Treatment of Peripheral Arterial Disease with Paclitaxel-Coated Balloons and Paclitaxel-Eluting Stents Potentially Associated with Increased Mortality” and that on June 19-20, 2019, the FDA convened a public meeting of the Circulatory System Devices Panel of the Medical Devices Advisory Committee to share information and perspectives from all interested parties on a potential late mortality signal associated with the use of paclitaxel-coated balloons and paclitaxel-eluting stents in patients with peripheral arterial disease.
In March 2019, the FDA conducted a preliminary analysis of long-term follow-up data (up to five years in some studies) of the pivotal premarket randomized trials for paclitaxel-coated products indicated for PAD. While the analyses are ongoing, according to the FDA, the preliminary review of the data has identified a potentially concerning signal of increased long-term mortality in study subjects treated with paclitaxel-coated products compared to patients treated with uncoated devices.[86] Of the three trials with 5-year follow-up data, each showed higher mortality in subjects treated with paclitaxel-coated products than subjects treated with uncoated devices. In total, among the 975 subjects in these 3 trials, there was an approximately 50 percent increased risk of mortality in subjects treated with paclitaxel-coated devices versus those treated with control devices (20.1 percent versus 13.4 percent crude risk of death at 5 years).
The FDA stated that the data should be interpreted with caution for several reasons. First, there is large variability in the risk estimate of mortality due to the limited amount of long-term data. Second, the studies were not originally designed to be pooled, introducing greater uncertainty in the results. Third, the specific cause and mechanism of the increased mortality is unknown.
Based on the preliminary review of available data, the FDA made the following recommendations regarding the use of paclitaxel-coated balloons and paclitaxel-eluting stents: That health care providers consider the following until further information is available; continue diligent monitoring of patients who have been treated with paclitaxel-coated balloons and paclitaxel-eluting stents; when making treatment recommendations and as part of the informed consent process, consider that there may be an increased rate of long-term mortality in patients treated with paclitaxel-coated balloons and paclitaxel-eluting stents; discuss the risks and benefits of all available PAD treatment options with your patients; for most patients, alternative treatment options to paclitaxel-coated balloons and paclitaxel-eluting stents should generally be used until additional analysis of the safety signal has been performed; for some individual patients at particularly high risk for restenosis, clinicians may determine that the benefits of using a paclitaxel-coated product may outweigh the risks; ensure patients receive optimal medical therapy for PAD and other cardiovascular risk factors as well as guidance on healthy lifestyles including weight control, smoking cessation, and exercise.
The FDA further stated that paclitaxel-coated balloons and stents are known to improve blood flow to the legs and decrease the likelihood of repeat procedures to reopen blocked blood vessels. However, because of this concerning safety signal, the FDA stated that it believes alternative treatment options should generally be used for most patients while the FDA continues to further evaluate the increased long-term mortality signal and its impact on the overall benefit-risk profile of these devices. The FDA stated it intends to conduct additional analyses to determine whether the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use. The FDA stated it will also evaluate whether these analyses impact the safety of patients treated with these devices for other indications, such as treatment of arteriovenous access stenosis or critical limb ischemia.
Because of concerns regarding this issue, the FDA convened an Advisory Committee meeting of the Circulatory System Devices Panel on June 19-20, 2019 to: Facilitate a public, transparent, and unbiased discussion on the presence and magnitude of a long-term mortality signal; discuss plausible reasons, including any potential biological mechanisms, for a long-term mortality signal; re-examine the benefit-risk profile of this group of devices; consider modifications to ongoing and future US clinical trials evaluating devices containing paclitaxel, including added surveillance, updated informed consent, and enhanced adjudication for drug-related adverse events and deaths; and guide other regulatory actions, as needed. The June 19-20, 2019 Advisory Committee meeting of the Circulatory System Devices Panel concluded that analyses of available data from FDA-approved devices show an increase in late mortality (between two and five years) associated with paclitaxel-coated devices intended to treat femoropopliteal disease. However, causality for the late mortality rate increase could not be determined. Additional data may be needed to further assess the magnitude of the late mortality signal, determine any potential causes, identify patient sub-groups that may be at greater risk, and to update benefit-risk considerations of this device class.[87]
The FDA continues to recommend that health care providers report any adverse events or suspected adverse events experienced with the use of paclitaxel-coated balloons and paclitaxel-eluting stents. The FDA stated that it will keep the public informed as any new information or recommendations become available.
After consideration of the public comments we received and the latest available information from the FDA advisory panel, we note the FDA panel's preliminary review of the data that has identified a potentially concerning signal of increased long-term mortality in study subjects treated with paclitaxel-coated products compared to patients treated with uncoated devices. Additionally, since the FDA has stated that it believes alternative treatment options should generally be used for most patients while the FDA continues to further evaluate the increased long-term mortality signal and its impact on the overall benefit-risk profile of these devices, we remain concerned that we do not have enough information to determine that the EluviaTM device represents a substantial clinical improvement over existing technologies. Therefore, we are not approving the EluviaTM device for FY 2020 new technology add-on payments. We will monitor any new information or recommendations as they become available.
e. ELZONRISTM (tagraxofusp, SL-401)
Stemline Therapeutics submitted an application for new technology add-on payments for ELZONRISTM for FY 2020. ELZONRISTM (tagraxofusp, SL-401) is a targeted therapy for the treatment of blastic plasmacytoid dendritic cell neoplasm (BPDCN) administered via infusion. The applicant stated that BPDCN, previously known as blastic natural killer (NK) cell leukemia/lymphoma, is a rare, highly aggressive hematologic malignancy with a median overall survival of 8 to 14 months from diagnosis that occurs predominantly in the elderly (median age at diagnosis is 67 years old) and in male patients (75 percent). The applicant cited data from the Surveillance, Epidemiology, and End Results Program (SEER) registry that the estimated incidence of BPDCN is less than 100 new cases per year in the U.S. However, the applicant believes that registries likely underestimate the true incidence of BPDCN due to changing nomenclature and lack of a standardized disease characterization prior to 2008, and that additional patients may be eligible for treatment.
According to the applicant, ELZONRISTM is a targeted therapy directed to the interleukin-3 receptor (IL-3 receptor). The IL-3 receptor is composed of two chains: An alpha chain, also known as CD123, and a β chain. Together, the two chains form a high-affinity cell surface receptor for interleukin-3 (IL-3). The binding of IL-3 to the IL-3 receptor initiates signaling that stimulates the proliferation and differentiation of certain hematopoietic cells. The alpha unit of the IL-3 receptor (also known as CD123) has also been found to be expressed in a variety of cancers, including BPDCN, a malignancy derived from plasmacytoid dendrite cells (pDCs).
The applicant explained that ELZONRISTM is a recombinant protein composed of human IL-3 genetically fused to a truncated diphtheria toxin (DT) payload. The applicant stated that ELZONRISTM binds with high affinity to the IL-3 receptor and is engineered such that IL-3 replaces the native receptor-binding domain of DT and thereby acts like a homing device, targeting the DT cytotoxic payload specifically to CD123-expressing cells. Upon binding to the IL-3 receptor, ELZONRISTM is internalized into endosomes, where the low pH environment enables proteolytic cleavage and release of the catalytic domain of DT into the cytoplasm. The target of DT's catalytic domain is elongation factor 2 (EF-2), a key protein involved in protein translation. Inactivation of EF-2 leads to termination of protein synthesis, which ultimately results in cell death. The applicant asserted that ELZONRISTM is engineered such that IL-3 targets the cytotoxic payload specifically to CD123-expressing cells.
The applicant indicated that the regimens historically employed for the treatment of patients who have been diagnosed with BPDCN have generally consisted of those regimens, or modified versions of those regimens, used for aggressive hematologic malignancies, including regimens normally used in the treatment of acute lymphoblastic leukemia, acute myeloid leukemia, and lymphoma. The applicant summarized the mechanisms of various drugs and regimens currently used to treat BPDCN, including:
- Etoposide, which the applicant explained works by inhibiting topoisomerase II, which in turn disrupts the ligation step of the cell cycle, leading to apoptosis and cell death.
- Hyper CVAD, which the applicant explained is a regimen consisting of cyclophosphamide, vincristine and doxorubicin, dexamethasone, methotrexate, and cytarabine. Cyclophosphamide damages DNA by binding to it and causing the formation of cross-links. Vincristine prevents cell duplication by binding to the protein tubulin. Dexamethasone is a steroid to counteract side effects. Methotrexate is an antimetabolite that competitively inhibits an enzyme that is used in in folate synthesis, arresting cell reproduction.
- CHOP, which the applicant explained is a regimen of cyclophosphamide, doxorubicin, vincristine, and prednisone.
- AspaMetDex L-asparaginase, Methotrexate, Dexamethasone. The applicant explained that L-asparaginase catalyzes the conversion of L-asparagine to aspartic acid and ammonia, depriving leukemic cells of L-asparagine, leading to cell death.
- Ara-C regimen (cytarabine), which the applicant explained interferes with synthesis of DNA by altering the sugar component of nucleosides.
The applicant stated that there are no approved therapies or established standards of care for the treatment of patients who have been diagnosed with BPDCN, either for treatment-naive or previously-treated patients. The applicant asserted that current treatments for patients who have been diagnosed with BPDCN might temporarily help to slow disease progression, but they fail to eradicate cancer stem cells (CSCs), and no specific treatment regimen has been shown to be effective or is recommended. According to the applicant, only half of reported patients show initial response to the regimens historically employed for treatment of a diagnosis of BPDCN, and these reported responses do not generally appear to be durable, with many patients experiencing a quick relapse. Overall survival is typically low, ranging from 8 to 14 months across various treatment regimens.
With respect to the newness criterion, according to the applicant, the FDA accepted the applicant's Biologics License Application (BLA) filing for ELZONRISTM in August 2018 for the treatment of patients who have been diagnosed with blastic plasmacytoid dendritic cell neoplasm. The FDA granted this application Breakthrough Therapy, Priority Review, and Orphan Drug designations, and on December 21, 2018, approved ELZONRISTM for the treatment of blastic plasmacytoid dendritic cell neoplasm in adults and in pediatric patients 2 years old and older. The applicant submitted a request for approval for a unique ICD-10-PCS code for the administration of ELZONRISTM beginning in FY 2020 and was granted approval for the following procedure codes effective October 1, 2019: XW033Q5 (Introduction of Tagraxofusp-erzs Antineoplastic into peripheral vein, percutaneous approach, new technology, group 5) and XW043Q5 (Introduction of Tagraxofusp-erzs Antineoplastic into central vein, percutaneous approach, new technology group 5).
As previously discussed, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, according to the applicant, ELZONRISTM treats BPDCN via target antigen specificity, attacking cells with the IL-3 receptor (CD123) overexpressed in cancer stem cells (CSCs) and tumor bulk, but minimally expressed or absent on normal hematopoietic stem cells. The applicant indicated that ELZONRISTM's mechanism of action involves a receptor-mediated endocytosis, inhibition of protein synthesis, and interference with IL-3 signal transduction pathways, leading to growth arrest and apoptosis in leukemia blasts and CSCs. The applicant asserted that current BPDCN treatments are not targeted, and their mechanisms of action aim to arrest quickly-dividing cells through DNA alkylation and intercalation, as well as through protein binding to prevent cell duplication. The applicant also asserted that current treatments for patients who have been diagnosed with BPDCN might temporarily help to slow disease progression, but they fail to eradicate CSCs. The applicant stated that in contrast, ELZONRISTM utilizes a payload that is not cell cycle-dependent and, therefore, it is able to kill not just highly proliferative tumor bulk, but also the relatively quiescent CSCs. The applicant noted that there are similar targeted therapies currently under investigation, although the applicant asserted that these other therapies are all in much earlier stages of development. Therefore, the applicant asserted that ELZONRISTM utilizes a different mechanism of action than currently available treatment options.
With respect to the second criterion, whether a product is assigned to the same or a different MS-DRG, the applicant stated that because BPDCN is a distinct and rare hematologic malignancy and there are no other approved therapies or established standard-of-care, cases representing patients receiving treatment involving ELZONRISTM would not be assigned to the same MS-DRG(s) when compared to cases representing patients receiving treatment involving existing technologies. In the proposed rule, we noted that, as explained in the discussion of the cost criterion, the applicant stated that potential cases representing patients who may be eligible for treatment involving ELZONRISTM would be assigned to MS-DRGs that contain cases representing patients who are receiving chemotherapy without acute leukemia as a secondary diagnosis.
With respect to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, according to the applicant, the use of ELZONRISTM would involve treatment of a dissimilar patient population as compared to other therapies. The applicant stated that the World Health Organization standardized the current name and specific category of disease for BPDCN in 2016, designating it as a distinct entity within the acute myeloid neoplasms and acute leukemias. The applicant indicated that no BPDCN standard-of-care has been established and currently patients who have been diagnosed with BPDCN are being treated with therapies used for other diseases. Therefore, the applicant asserted that ELZONRISTM would be used in the treatment of a new patient population because the patient population in question is distinguishable from others by the ICD-10-CM diagnosis code specific to BPDCN: C86.4 (Blastic NK-cell lymphoma), for which there is no specific treatment regimen that has been shown to be effective or is recommended, as previously stated.
As presented in the proposed rule and previously summarized, the applicant maintains that ELZONRISTM meets the newness criterion and is not substantially similar to existing technologies because it has a unique mechanism of action; potential cases representing patients who may be eligible for treatment involving the use of ELZONRISTM would be assigned to a different MS-DRG when compared to existing technologies; and the use of the technology would treat a new patient population. We invited public comments on whether ELZONRISTM is substantially similar to any existing technologies and whether ELZONRISTM meets the newness criterion.
Comment: The applicant submitted a comment reiterating that ELZONRISTM is the first approved treatment for patients with BPDCN and the first approved CD123-targeted therapy.
Response: Based on the applicant's comment and information submitted by the applicant as part of its FY 2020 new technology add-on payment application for ELZONRISTM, as discussed in the proposed rule (84 FR 19319) and previously summarized, we believe that ELZONRISTM has a unique mechanism of action and the use of the technology would treat a new patient population. Therefore, we believe ELZONRISTM is not substantially similar to existing treatment options and meets the newness criterion. We consider the beginning of the newness period to commence when ELZONRISTM was approved by the FDA on December 21, 2018.
With regard to the cost criterion, the applicant used the FY 2017 MedPAR Hospital Limited Data Set (LDS) to assess the MS-DRGs to which cases representing potential patient hospitalizations that may be eligible for treatment involving ELZONRISTM would most likely be assigned. The applicant identified these potential cases using the ICD-10-CM diagnosis code C86.4 (Blastic NK-cell lymphoma), which the applicant stated is another name for BPDCN. The applicant identified 65 cases reporting ICD-10-CM diagnosis code C86.4 spanning 28 different MS-DRGs. The applicant asserted that cases representing patients hospitalized who may be eligible to receive treatment involving ELZONRISTM would most likely appear in MS-DRGs 847 (Chemotherapy without Acute Leukemia as Secondary Diagnosis with CC) and 846 (Chemotherapy without Acute Leukemia as Secondary Diagnosis with MCC). Therefore, the applicant limited the analysis to the cases in MS-DRG 847 and MS-DRG 846 that also reported the ICD-10-CM diagnosis code C86.4. The cases identified in these two MS-DRGs accounted for 24 (37 percent) of the 65 cases reporting ICD-10-CM diagnosis code C86.4.
The applicant indicated that because the number of cases reporting ICD-10-CM diagnosis code C86.4 is so low and it was difficult to discern the costs of the predecessor therapies that would be replaced by the use of ELZONRISTM, the applicant performed the cost criterion analysis under two different scenarios. Both scenarios use the 24 cases identified in the FY 2017 MedPAR data and increase the sample size by using an additional 18 cases identified in the FY 2016 MedPAR data mapping to the same MS-DRGs and reporting the same ICD-10-CM diagnosis code, for a combined total of 42 cases with an average case-weighted unstandardized charge per case of $67,947. For the first scenario, because the applicant was unable to determine the appropriate costs for the predecessor therapies, the applicant did not remove any predecessor charges from the cases analyzed, although the applicant noted that it might be extreme to assume that no products or services would be replaced if ELZONRISTM were used. For the second scenario, the applicant removed all charges from the cases so that only ELZONRISTM was used as the cost of the case. The applicant characterized this as a conservative assumption, as it assumes that the only charges related to these cases would be the cost of ELZONRISTM.
The applicant then standardized the FY 2017 charges using the FY 2017 impact file and then inflated the charges to FY 2019 using the 2-year inflation factor of 8.59 percent (1.085868) that the applicant indicated was published in the FY 2019 IPPS/LTCH PPS final rule. The applicant standardized FY 2016 charges using the FY 2016 impact file and then inflated the charges to FY 2019 using a 3-year inflation factor of 13.15 percent (1.131529), which was calculated based on the 1-year inflation factor (1.04205) that the applicant indicated was listed in the FY 2019 IPPS/LTCH PPS final rule. In the proposed rule, we noted that the inflation factors used by the applicant were the proposed 1-year and 2-year inflation factors, which were published in the FY 2019 IPPS/LTCH PPS final rule in the summary of FY 2019 IPPS proposals (83 FR 41718). The final 1-year and 2-year inflation factors published in the FY 2019 IPPS/LTCH PPS final rule are 1.04338 and 1.08864, respectively (83 FR 41722), and a 3-year inflation factor calculated based on these numbers is 1.13587. We further noted that these figures were revised in the FY 2019 IPPS/LTCH PPS final rule correction notice. The corrected final 1-year and 2-year inflation factors are 1.04396 and 1.08986, respectively (83 FR 49844), and a 3-year inflation factor calculated based on the corrected final numbers is 1.13776.
The applicant then added charges for ELZONRISTM in both scenarios. To determine the charges for ELZONRISTM, the applicant calculated the average per discharge cost of ELZONRISTM inflated by the inverse of the national average CCR for pharmacy costs of 0.191. The applicant then calculated an average case-weighted standardized charge per case for each scenario and compared it with the average case-weighted threshold amount. The applicant stated that ELZONRISTM exceeded the average-case-weighted threshold amount under each scenario and, therefore, meets the cost criterion. Results of the analyses of both scenarios are summarized in this table:

In the proposed rule, we noted that the applicant used the proposed rule values to inflate the standardized charges. However, we further noted that even when using either the final rule values or corrected final rule values to inflate the charges, the average case-weighted standardized charge per case for each scenario exceeded the average case-weighted threshold amount. We invited public comments on whether ELZONRISTM meets the cost criterion.
We did not receive any public comments on whether ELZONRISTM meets the cost criterion. Based on the information submitted by the applicant as part of its FY 2020 new technology add-on payment application for ELZONRISTM, as discussed in the proposed rule (84 FR 19319 through 19320) and previously summarized, the average case-weighted standardized charge per case exceeded the average case-weighted threshold amount. Therefore, ELZONRISTM meets the cost criterion.
With respect to the substantial clinical improvement criterion, the applicant stated that it believes ELZONRISTM represents a substantial clinical improvement because: (1) ELZONRISTM is the only treatment indicated specifically for the treatment of patients who have been diagnosed with BPDCN, a disease without a defined standard-of-care; (2) ELZONRISTM offers a treatment option for a patient population ineligible for aggressive chemotherapy regimens used to treat BPDCN; (3) ELZONRISTM exhibits high complete remission rates, potentially superior to other regimens used to treat a diagnosis of BPDCN; (4) ELZONRISTM significantly improves overall survival (OS) in the treatment of patients diagnosed with BPDCN as compared to currently available treatment regimens; (5) ELZONRISTM significantly improves clinical outcomes in the BPDCN patient population because it may allow more patients to bridge to stem cell transplantation, an effective treatment not currently administered to most patients due to their inability to tolerate the requisite conditioning therapies; (6) ELZONRISTM exhibits a manageable profile that is consistent over increasing patient exposure and experience, demonstrating a well-tolerated targeted therapy suitable for the majority of patients who are unable to receive intensive chemotherapy; and (7) ELZONRISTM is more efficient than other chemotherapeutic drugs at killing BPDCN in preclinical studies, suggesting clinical benefit would also be exhibited if head-to-head comparison was pursued.
In support of the claim that ELZONRIS[TM] is the only treatment indicated specifically for the treatment of patients who have been diagnosed with BPDCN, the applicant submitted a 2016 review article which indicated that no standardized therapeutic approach has been established yet for the treatment of BPDCN, and the optimal therapy remains to be defined.[88]
Second, in support of the claim that ELZONRIS[TM] offers a treatment option for a patient population ineligible for aggressive chemotherapy regimens used to treat BPDCN, the applicant submitted a 2016 review of treatment modalities for patients who have been diagnosed with BPDCN to establish that there is a clear unmet need for targeted treatment. The study reported that seven BPDCN patients treated with Hyper-CVAD, an aggressive chemotherapy regimen, achieved an overall response of 86 percent and complete remission of 67 percent; [89] however, the applicant noted that the evidence is limited to a small number of patients. Another 2016 review article indicated that supportive care or palliative chemotherapy is used in the treatment of many patients who have been diagnosed with BPDCN because of their age or comorbidities, and may be the only option for elderly patients with a low performance status or characterized by the presence of relevant co-morbidities, suggesting that targeted therapy has the potential for improving patient outcomes.[90]
Third, the applicant maintained that ELZONRIS[TM] exhibits high complete remission rates, potentially superior to other regimens used to treat patients who have been diagnosed with BPDCN. The applicant submitted a 2013 retrospective case study of patients who had been diagnosed with BPDCN, in which 15/41 (37 percent) of evaluable patients achieved CR with induction therapies; 2 partial responders subsequently became complete responders with consolidation therapy (17/41: 41 percent). This study noted a high death rate of 17 percent following induction treatment.[91] The applicant reported prospective clinical trial data from ELZONRIS[TM] 's pivotal trial (ELZONRIS[TM] 12µg/kg/day), which observed a complete response plus a complete clinical response of 72 percent in treatment-naive patients (21/29 patients).[92]
Fourth, the applicant maintained that ELZONRIS[TM] significantly improves overall survival (OS) in patients who have been diagnosed with BPDCN as compared to currently available treatment regimens. The applicant submitted a 2013 retrospective case study of patients who have been diagnosed with BPDCN, which found that the median overall survival was just 8.7 months in 43 patients.[93] The applicant reported prospective clinical trial data from ELZONRIS[TM] 's pivotal trial (ELZONRIS[TM] 12µg/kg/day), which found that median overall survival has not yet been reached, with a median follow-up of 23 months [0.2−41 + months].[94]
Fifth, the applicant maintained that ELZONRISTM significantly improves clinical outcomes in the treatment of the BPDCN patient population because it may allow more patients to bridge to stem cell transplantation, an effective treatment not currently administered to most patients due to their inability to tolerate the requisite conditioning therapies. The applicant submitted a 2011 retrospective study that included 6 cases of elderly patients who had been diagnosed with BPDCN in which 4 patients underwent allogenic stem cell transplantation (SCT) following moderately reduced intensity of conditioning chemotherapy regimens; 2 patients who received stem cell transplant while in remission lived disease free 57 months and 16 months post-SCT, and 2 patients transplanted with active disease achieved complete remission but relapsed 6 and 18 months after transplantation. Conditioning chemotherapy regimens were reduced in intensity due to the patients' elderly age.[95] The applicant also submitted a 2015 retrospective study of 25 BPDCN cases in which patients were treated with SCT. Of 11 BPDCN patients treated with autologous SCT and 14 patients treated with allogenic SCT, overall survival (OS) at 4 years was 82 percent and 69 percent, respectively, and no relapses were observed.[96] The applicant also submitted a 2013 retrospective study of 43 BPDCN cases in which only 6 out of 43 patients (14 percent) received allogenic SCT.[97] The applicant submitted a 2010 retrospective study of BPDCN cases in which only 10 out of 47 patients (21 percent) received SCT.[98] The applicant submitted a 2016 review article which concluded that early results from clinical trials for ELZONRISTM indicate that it could be used to consolidate the effects of first-line chemotherapy and/or reduce minimal residual disease before allogenic SCT.[99] The applicant reported prospective clinical trial data from ELZONRISTM's pivotal trial (ELZONRISTM 12 μg/kg/day), for which the median age among the patients with BPDCN who received treatment involving ELZONRISTM was 70 years old, in which 45 percent (13/29) of treatment-naive patients treated with ELZONRISTM (12 μg/kg/day) were bridged to SCT in remission.[100]
Sixth, the applicant maintained that ELZONRISTM exhibits a manageable profile that demonstrates a well-tolerated targeted therapy suitable for the majority of patients who are unable to receive intensive chemotherapy. The prospective clinical trial data from ELZONRISTM's pivotal trial (ELZONRISTM 12 μg/kg/day) found that ELZONRISTM's side effect profile remained consistent over increasing patient exposure and experience. No evidence of cumulative toxicity was seen over multiple cycles of ELZONRISTM. Myelosuppression (thrombocytopenia, anemia, neutropenia) was modest, reversible, and was not dose-limiting for any patient. The most common treatment-related adverse events included increased alanine aminotransferase levels, increased aspartate aminotransferase levels and hypoalbuminemia, mostly restricted to the first cycle of therapy. The most serious side effect was capillary leak syndrome; most reports were Grade II in severity.[101]
Lastly, the applicant asserts that ELZONRISTM is more efficient than other chemotherapeutic drugs at killing BPDCN in preclinical studies, suggesting clinical benefit would also be exhibited if head-to-head comparison to cytotoxic agents commonly used for the treatment of hematologic malignancies was pursued. The applicant submitted a 2015 preclinical study that found malignant cells from patients who had been diagnosed with BPDCN were more sensitive to ELZONRISTM than to a wide variety of cytotoxic agents commonly used for treatment of hematologic malignancies, including drugs such as cytosine arabinoside, cyclophosphamide, vincristine, dexamethasone, methotrexate, Erwinia L-asparaginase, and asparaginase.[102]
After reviewing the information submitted by the applicant as part of its FY 2020 new technology add-on payment application for ELZONRISTM, in the FY 2020 IPPS/LTCH PPS proposed rule, we stated we were concerned that some of the evidence submitted by the applicant to demonstrate substantial clinical improvement over existing technologies is based on preclinical studies. We also stated that we were unsure if the study populations in the 2013 retrospective study that the applicant used to compare remission rates are composed of treatment-naive, previously-treated, or a mix of patients.
In addition, the applicant reported that the interim results of the Phase II trial of treatment of BPDCN with ELZONRISTM demonstrated high response rates in BPDCN, including: 90 percent overall response in treatment naive patients (26/29) and 69 percent overall response in relapse/refractory patients (9/13); 72 percent complete response plus complete clinical response in treatment naive patients (21/29) and 38 percent complete response plus complete clinical response in relapse/refractory patients (5/13); and 45 percent of patients treated in first-line setting were bridged to stem cell transplant in remission (13/29).[103] However, we stated that we were concerned that the small number of patients in the study and the lack of baseline data against which to compare this technology may make it more difficult to determine whether these interim results support a finding of substantial clinical improvement. We also noted that because the clinical trial is ongoing and the final outcomes are not available, we stated we were concerned that there may not be enough information on the efficacy to determine substantial clinical improvement at this time. We also noted that the applicant's December 2018 New Technology Town Hall meeting presentation included information that differs slightly from the application materials, and we were not clear whether the study results submitted with the application reflect the most current information available. We invited public comments on whether ELZONRISTM meets the substantial clinical improvement criterion, including with respect to the concerns we have raised.
Comment: The applicant submitted comments in response to CMS's concerns in the proposed rule regarding whether ELZONRISTM meets the substantial clinical improvement criterion.
With respect to the concern that some of the evidence submitted by the applicant to demonstrate substantial clinical improvement over existing technologies is based on preclinical studies, the applicant stated that at the time of the new technology add-on payment application submission (December 2018), the peer reviewed publications of ELZONRISTM (tagraxofusp-erzs) included preclinical studies by Angelot-Delettre (2015) and Delettre (2013) and initial prospective evidence of the clinical activity of ELZONRISTM in patients with BPDCN (Frankel 2014). The applicant stated that since the new technology add-on payment application submission, ELZONRISTM was approved by the FDA for the treatment of BPDCN in adults and pediatric patients two years and older on December 21, 2018, and the efficacy and safety data from the pivotal study of ELZONRISTM that formed the basis for the FDA approval was published in the April 25th issue of the New England Journal of Medicine (NEJM). The applicant stated that Study STML-401-0114 (ELZONRISTM BPDCN Clinical Trial), the subject of the NEJM article, was a multicenter, multistage study of ELZONRISTM in patients with BPDCN and the largest prospective clinical trial designed to evaluate outcomes in patients with BPDCN. The applicant submitted the 2019 study as part of its comment, which reported that among the 29 previously untreated patients receiving ELZONRISTM at a dose of 12 µg/kg/day, the overall response rate was 90 percent, 72 percent (21/29) achieved a complete response plus a complete clinical response, and 45 percent (13/29) bridged to SCT. Survival rates at 18 and 24 months were 59 percent and 52 percent, respectively. Among the 15 previously-treated patients, the overall response rate was 67 percent, and the median overall survival was 8.5 months. The study concluded that in adult patients with untreated or relapsed BPDCN, the use of ELZONRISTM led to clinical responses, though serious adverse events were common.[104]
With respect to the concern that we were unsure if the study populations in the 2013 retrospective study that the applicant used to compare remission rates are composed of treatment-naïve, previously-treated, or a mix of patients, the applicant stated that the 2013 Pagano et al. study was a multi-center retrospective study that evaluated 43 treatment-naïve BPDCN patients from 2005-2011 who received traditional chemotherapy. The applicant noted that the results included 41 percent of patients achieving a CR; a median overall survival of 8.7 months, and 14 percent of patients bridged to receive a SCT.[105] In contrast, the ELZONRISTM clinical trial consisted of a mix of patients (N=47), of which 32 were receiving ELZONRISTM as first-line treatment. The applicant stated that among the 29 treatment-naive patients who received ELZONRIS at a dose of 12 mcg/kg, 72 percent of patients (21/29) achieved a CR; survival rates at 18 and 24 months were 59 percent and 52 percent, respectively; and 45 percent of patients (13/29) bridged to receive a SCT.[106]
With respect to the concern that the small number of patients in the clinical trial and the lack of baseline data against which to compare this technology may make it more difficult to determine whether these interim results support a finding of substantial clinical improvement, the applicant stated that BPDCN is a very rare and highly aggressive hematologic malignancy, with an estimated incidence of 0.41/1,000,000 patients age-adjusted to the 2000 US standard population, corresponding to less than 100 new cases per year. The applicant stated that the ELZONRISTM BPDCN Clinical Trial was the first study prospectively designed to assess the safety and efficacy of a therapy in patients with BPDCN, including a pre-defined cohort for confirmation of efficacy. The applicant stated that to date, it is considered the largest prospective study of patients with BPDCN ever conducted (N=47); a cohort that is sizeable and adequately represents the `real-world' population in terms of demographics and baseline characteristics. The applicant stated that as such, this study, for the first time, provided prospectively acquired data for any therapy in this patient population and are therefore considered to be more robust and reliable than previously reported retrospective data. The applicant stated further that in the absence of available therapies for patients with BPDCN, empirical chemotherapies have been employed in the past for both treatment-naïve and previously treated BPDCN, and the published literature regarding BPDCN treatment consists primarily of case reports and retrospective data reviews with limited published data from prospective clinical studies. The applicant stated that the accuracy and ability to interpret the response rates reported in the literature is limited, given the general lack of well-defined response criteria, especially related to measurement of the extent of cutaneous disease and other extramedullary sites of disease. As such, the applicant stated that published response rates should be viewed with caution and may represent artificially high response rates in some instances.
With respect to the concern that there may not be enough information on the efficacy of ELZONRISTM to determine substantial clinical improvement at this time given that the clinical trial is ongoing and the final outcomes are not available, the applicant stated that FDA approval was based on the efficacy and safety results from the ELZONRISTM BPDCN Clinical Trial in patients with treatment-naive or previously treated BPDCN. The applicant explained that the clinical trial was a multi-stage study, with each study stage featuring its own objectives and design elements. The applicant stated that Stage 1 (dose escalation), Stage 2 (expansion), and Stage 3 (pivotal, confirmatory for efficacy) are complete and the results were published in the NEJM on April 25th, 2019. The applicant stated that patients were also enrolled in an additional cohort (Stage 4) to enable ongoing access to ELZONRISTM in a clinical study.
With respect to the concern that the applicant's December 2018 New Technology Town Hall meeting presentation included information that differs slightly from the application materials, and we were not clear whether the study results submitted with the application reflect the most current information available, the applicant stated that the most current ELZONRISTM data was reported by Pemmaraju and colleagues and published in the April 25th, 2019 issue of the NEJM,[107] and the applicant submitted a copy of the article as part of its comment.
Response: We appreciate the additional information and analysis provided by the applicant and the applicant's input in response to our concerns regarding substantial clinical improvement. After reviewing the information submitted by the applicant addressing our concerns raised in the proposed rule, we agree with the applicant that ELZONRISTM represents a substantial clinical improvement over existing technologies because, based on the information provided by the applicant, the technology offers a treatment option for a patient population unresponsive to, or ineligible for, currently available treatments and substantially improves response rates and clinical outcomes for patients with BPDCN.
After consideration of the public comments we received, we have determined that ELZONRISTM meets all of the criteria for approval for new technology add-on payments. Therefore, we are approving new technology add-on payments for ELZONRISTM for FY 2020. Cases involving the use of ELZONRISTM that are eligible for new technology add-on payments will be identified by ICD-10-PCS procedure codes XW033Q5 and XW043Q5.
In its application, the applicant stated that ELZONRISTM is supplied as a non-preserved, sterile, single-use liquid dosage in 2 mL glass vials containing 1 mL of solution at a concentration of 1 mg/mL (1 mg/vial). It is administered by intravenous infusion at 12µg/kg/day over 15 minutes once daily on days 1-5 of a 21 day cycle. The dosing period may be extended for dose delays up to day 10 of the cycle. The applicant stated that the first administration cycle should occur in the inpatient setting; subsequent cycles may be administered in the inpatient or appropriate outpatient setting. The applicant stated that in clinical studies, roughly 70 percent of treatment-naive patients received 2 vials per dose (the remaining patients received 1 vial per dose). Relapsed/refractory patients were more likely to have 1 vial per dose (70 percent vs. 30 percent). In all, about 70 percent of patients are treatment naive, and 30 percent are relapsed/refractory. Using this information, the applicant calculated that the average inpatient hospitalization would require 7.9 vials. According to the applicant, the WAC per vial is $24,430. Therefore, the average total cost of ELZONRISTM per patient is $192,997. Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the costs of the new medical service or technology, or 65 percent of the amount by which the costs of the case exceed the MS-DRG payment. As a result, the maximum new technology add-on payment for a case involving the use of ELZONRISTM is $125,448.05 for FY 2020. (As discussed in section II.H.9. of the preamble of this final rule, we are revising the maximum new technology add-on payment to 65 percent, or 75 percent for certain antimicrobial products, of the average cost of the technology.)
f. BalversaTM (Erdafitinib)
Johnson & Johnson Health Care Systems, Inc. (on behalf of Janssen Oncology, Inc.) submitted an application for new technology add-on payments for BalversaTM for FY 2020. BalversaTM is indicated for the second-line treatment of adult patients who have been diagnosed with locally advanced or metastatic urothelial carcinoma whose tumors exhibit certain fibroblast growth factor receptor (FGFR) genetic alterations as detected by an FDA-approved test, and who have disease progression during or following at least one line of prior chemotherapy including within 12 months of neoadjuvant or adjuvant chemotherapy.
According to the applicant, BalversaTM is an oral pan-fibroblast growth factor receptor (FGFR) tyrosine kinase inhibitor being evaluated in Phase II and III clinical trials in patients who have been diagnosed with advanced urothelial cancer. FGFRs are a family of receptor tyrosine kinases, which may be upregulated in various tumor cell types and may be involved in tumor cell differentiation and proliferation, tumor angiogenesis, and tumor cell survival. BalversaTM is a pan-fibroblast FGFR inhibitor with potential antineoplastic activity. Upon oral administration, BalversaTM binds to and inhibits FGFR, which may result in the inhibition of FGFR-related signal transduction pathways and, therefore, the inhibition of tumor cell proliferation and tumor cell death in FGFR-overexpressing tumor cells.
The applicant indicated that urothelial cancer (also known as transitional cell cancer or bladder cancer) is the sixth most common type of cancer diagnosed in the U.S. In 2018, an estimated 81,190 new cases of bladder cancer were expected to be diagnosed (approximately 62,380 in men and 18,810 in women), and result in 17,240 deaths (approximately 1 out of 5 diagnosed men and 1 out of 4 diagnosed women).[108] According to the applicant, for patients with metastatic disease, outcomes can be dire due to the often rapid progression of the tumor and the lack of efficacious treatments, especially in cases of relapsed or refractory disease. The applicant further stated that the relative 5-year survival rate for patients with metastatic disease is 5 percent.
According to the applicant, in regard to current second-line treatment, patients who have been diagnosed with locally advanced or metastatic urothelial cancer have limited options and favor anti-programmed death ligand 1/anti-programmed death 1 (anti-PD-L1/anti-PD-1) therapies (also known as checkpoint inhibitors) as opposed to conventional cytotoxic chemotherapy. With objective response rates ranging from approximately 20 to 25 percent with currently approved therapies and treatments, the applicant stated that new effective treatment options are needed for this patient population. Although there are five FDA-approved immune checkpoint inhibitors, the applicant stated that studies have shown that not all patients benefit from PD-1 blockade. The applicant explained that patients harboring FGFR alternates, which occurs at a frequency of approximately 20 percent, are believed to have immunologically “cold tumors” that are less likely to benefit from PD-1 blockade therapy.
The applicant noted that BalversaTM was granted Breakthrough Therapy designation by the FDA on March 15, 2018, for the treatment of patients who have been diagnosed and treated for urothelial cancer whose tumors have certain FGFR genetic alterations. BalversaTM received accelerated FDA approval on April 12, 2019. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19322), we noted that the applicant submitted a request for approval at the March 2019 ICD-10 Coordination and Maintenance Committee Meeting for a unique ICD-10-PCS procedure code to specifically identify cases involving the administration of BalversaTM. BalversaTM was granted approval for the ICD-10-PCS procedure code XW0DXL5 (Introduction of Erdafitinib Antineoplastic into Mouth and Pharynx, External Approach, New Technology Group 5), with an effective date of October 1, 2019.
As previously discussed, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, the applicant asserted that BalversaTM is not substantially similar to any existing treatment options because its inhibitory mechanism of action is novel. Specifically, the applicant stated that BalversaTM is a pan-fibroblast FGFR inhibitor with potential antineoplastic activity. Upon oral administration, BalversaTM binds to and inhibits FGFR, which may result in the inhibition of FGFR-related signal transduction pathways and, therefore, the inhibition of tumor cell proliferation and tumor cell death in FGFR-overexpressing tumor cells. The applicant stated that BalversaTM is a potent pan-FGFR (1-4) tyrosine kinase inhibitor with IC50 (drug concentration at which 50 percent of target enzyme activity is inhibited) in the single-digit nanomolar range. According to the applicant, BalversaTM will, therefore, represent a first-in-class FGFR inhibitor because of its novel mechanism of action.
With respect to the second criterion, whether a product is assigned to the same or a different MS-DRG, the applicant stated that potential cases representing patients who may be eligible for treatment involving BalversaTM are likely to be assigned to a wide variety of MS-DRGs because patients who may receive treatment involving BalversaTM in the inpatient setting would likely be hospitalized due to other conditions than urothelial cancer. The applicant stated that potential cases representing patients who may be eligible for treatment involving the use of BalversaTM may be assigned to the same MS-DRGs as cases representing patients treated with currently available treatment options for urothelial cancer.
With respect to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, the applicant asserted that the treatment involving BalversaTM is specific to a select subset of patients who have been diagnosed with locally advanced or metastatic urothelial carcinoma and previously treated, but subsequently present with FGFR alterations. According to the applicant, while patients who have been diagnosed with metastatic or unresectable urothelial cancer may be offered second-line therapy options of a checkpoint inhibitor or systemic chemotherapy, treatment involving BalversaTM is specific to a subset of patients with certain FGFR-genetic alterations. Therefore, the applicant believes that BalversaTM treats a different patient population than currently available treatments.
We invited public comments on whether BalversaTM is substantially similar to any existing technology and whether it meets the newness criterion.
Comment: The applicant noted that CMS did not object to the assertion that BalversaTM meets the newness criterion because BalversaTM is not substantially similar to existing technologies and because it is the first drug with its mechanism of action approved by the FDA.
Response: We agree with the applicant that BalversaTM meets the newness criterion. We agree that BalversaTM is not substantially similar to existing treatment options because it has a unique mechanism of action. We consider April 12, 2019 as the beginning of the newness period for BalversaTM.
With regard to the cost criterion, the applicant conducted the following analysis. The applicant searched the FY 2017 MedPAR Hospital Limited Data Set (LDS) for inpatient hospital claims for potential cases representing patients who may be eligible for treatment using BalversaTM. The applicant noted that because the inpatient admission for the potential cases identified would likely be unrelated to the proposed indication for the use of BalversaTM, it is unlikely that the administration of BalversaTM would be initiated during an inpatient hospitalization. In addition, the applicant assumed that most hospitals would not utilize BalversaTM for short-stay inpatient hospitalization, and the applicant therefore eliminated all identified potential cases representing inpatient hospitalizations of 3 days or fewer from its analysis. The applicant also assumed that any inpatient hospitalization of 4 days or longer would involve the daily administration of BalversaTM and calculated the drug's costs on a case-by-case basis, multiplying the length-of-stay times the cost of the drug.
The applicant used a combination of ICD-10-CM diagnosis codes to identify these potential cases. The applicant first identified claims with one of the following ICD-10-CM diagnosis codes listed in this table.

The applicant then searched the MedPAR data file for inpatient hospital claims that also had one of the following ICD-10-CM diagnosis codes listed in this table to identify a combination of applicable codes.

Based on this search, the applicant identified 2,844 cases mapping to a wide range of MS-DRGs. The applicant identified and used in its analysis those MS-DRGs to which more than 1 percent of the total identified cases were assigned, as listed in this table.


Using 100 percent of the cases assigned to these MS-DRGs, the applicant determined an average case-weighted unstandardized charge per case of $86,302. The applicant did not remove any charges for prior therapies because the applicant indicated that the use of BalversaTM would not replace any other therapies. The applicant standardized the charges for each case and inflated each case's charges by applying the FY 2019 IPPS/LTCH PPS final rule outlier charge inflation factor of 1.08864 (83 FR 41722). (In the proposed rule, we noted that the 2-year charge inflation factor was revised in the FY 2019 IPPS/LTCH PPS final rule correction notice. The revised factor is 1.08986 (83 FR 49844). However, we further noted that even when using either the revised final rule values or the corrected final rule values published in the correction notice to inflate the charges, the final inflated average case-weighted standardized charge per case for BalversaTM would exceed the average case-weighted threshold amount.) The applicant then added the charges for the cost of BalversaTM. To determine the charges for the cost of BalversaTM, the applicant used the inverse of the FY 2019 IPPS/LTCH PPS final rule pharmacy national average CCR of 0.191. The applicant's reported average case-weighted threshold amount was $62,435 and its reported final inflated average case-weighted standardized charge per case was $111,713. Based on this analysis, the applicant believes BalversaTM meets the cost criterion because the final inflated average case-weighted standardized charge per case exceeds the average case-weighted threshold amount. We invited public comments on whether BalversaTM meets the cost criterion.
Comment: The applicant submitted a comment stating that CMS did not object to its assertion that BalversaTM meets the cost criterion. The applicant also submitted an updated analysis. The applicant stated that in the analysis presented to CMS for the proposed rule, the average case-weighted threshold amount was $62,435 and the final inflated average case-weighted standardized charge per case was $111,713. After BalversaTM received FDA approval, the analysis was updated with charges added to reflect the wholesale acquisition cost for BalversaTM, resulting in a final inflated average case-weighted standardized charge per case $109,211. The applicant noted that this remains above the case-weighted threshold amount of $62,435 and that BalversaTM therefore continues to meet the cost criterion.
Response: We appreciate the additional information provided by the applicant regarding whether BalversaTM meets the cost criterion. We agree that BalversaTM meets the cost criterion.
The applicant asserted that BalversaTM represents a substantial clinical improvement over existing technologies because it offers a treatment option for a patient population unresponsive to or ineligible for currently available treatments. The applicant stated that BalversaTM provides a substantial clinical improvement for a select group of patients who have been diagnosed with locally advanced or metastatic urothelial carcinoma who have failed first-line treatment and have limited second-line treatment options, despite the recent introduction of checkpoint inhibitors. The applicant further stated that the use of BalversaTM will be the first available treatment option specific for the subset of patients who have certain fibroblast growth factor receptor (FGFR) genetic alterations that are detected by an FDA-approved test. The applicant also believes that BalversaTM represents a significant clinical improvement because the technology reduces mortality, decreases pain, and reduces recovery time.
To support its assertions of substantial clinical improvement, the applicant submitted the results of a Phase I dose-escalation study for the use of BalversaTM in the target patient population for which the applicant asserts BalversaTM would be the first available treatment option and represents a substantial clinical improvement, which is patients who had been diagnosed with advanced solid tumors for which standard curative treatment appeared no longer effective. With a sample size of 65 patients, patients received escalating oral doses of BalversaTM ranging from 0.5 mg to 12 mg, administered continuously daily, or oral doses of BalversaTM of 10 mg or 12 mg administered on a 7-days-on/7-days-off intermittent schedule. The study intended to identify the Recommended Phase II Dose (RP2D) and investigate the safety and pharmacodynamics of the drug. The applicant stated that the initial RP2D was considered 9 mg continuous daily dosing and 10 mg for intermitted dosing on the basis of improved tolerability.
The applicant also provided data from a multi-center, open-label Phase II study of 99 patients, ages 36 years old to 87 years old, with the median age being 68 years old, who had been diagnosed with metastatic or unresectable urothelial carcinoma that had specific FGFR alterations and were treated with a starting daily dose of BalversaTM of 8 mg. The applicant noted the study included 87 patients who progressed after at least or more than 1 line of prior chemotherapy or within 12 months of (neo) adjuvant chemotherapy. According to the applicant, the objective response rate (ORR) measured by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 criteria was 40.4 percent (95 percent confidence interval [CI], 30.7 percent to 50.1 percent; 3.0 percent complete responses and 37.4 percent partial responses). The disease control rate (complete responses, partial responses, and stable disease) was 79.8 percent. The ORRs were similar in chemotherapy-naïve patients versus patients who progressed/relapsed after chemotherapy (41.7 percent versus 40.2 percent) and in patients who had visceral metastases versus those who did not (38.5 percent versus 47.6 percent). The median time to response was 1.4 months, and the median duration of response was 5.6 months (95 percent CI, 4.2 months to 7.2 months). The applicant noted that the results demonstrated a median progression-free survival of 5.5 months (95 percent CI, 4.2 months to 6.0 months) and a median overall survival of 13.8 months (95 percent CI, 9.8 months-not estimable). In an exploratory analysis of 22 patients previously treated with immunotherapy, the ORR was 59 percent; response to prior immunotherapy (per investigator) in these patients was 5 percent.[109 110]
The applicant also referenced an ongoing Phase III study, but indicated that the data was not available at the time of the application's submission.
In the proposed rule, we stated that we have the following concerns with regard to whether the technology meets the substantial clinical improvement criterion. First, we stated that the applicant did not provide substantial data comparing BalversaTM to existing therapies. Additionally, the studies that were provided were based on small sample sizes, open-labeled, and presented without a complete comparison to existing therapies. Due to the limited nature of available data, we stated we have concerns that we may not have enough information to determine if BalversaTM represents a substantial clinical improvement over existing technologies.
We invited public comments on whether BalversaTM meets the substantial clinical improvement criterion.
Comment: The applicant submitted a comment in response to CMS' concerns about the limited nature of available data. The applicant referenced the Phase II study (n=87) previously detailed in the proposed rule. The applicant stated that an objective response rate (ORR) of 32.2 percent (95 percent confidence interval [CI]: 22.4-42.0) was observed. The applicant also noted that among the majority of patients (n=64) enrolled with FGFR 3 point mutations, the ORR was 40.6 percent (95 percent CI: 28.6-52.7).
In response to CMS' concern about the lack of comparison of BalversaTM to existing therapies, the applicant stated that in the absence of head-to-head data, effectiveness comparisons can be made based on approved therapies in metastatic urothelial carcinoma for which BalversaTM is approved. Per the applicant, FDA-approved systemic therapies for locally advanced or mUC following platinum-based chemotherapy include KEYTRUDA® (pembrolizumab), TECENTRIQ® (atezolizumab), BAVENCIO® (avelumab), IMFINZI® (durvalumab), and OPDIVO® (nivolumab). The applicant noted that of the five approved checkpoint inhibitors, pembrolizumab observed the highest ORR of 21 percent in their registration trial.[111] Furthermore, the applicant noted that in the United States, docetaxel is an acceptable systemic chemotherapy following progression after platinum-based chemotherapy. The applicant stated that although docetaxel is not approved for the treatment of mUC in the US, a Phase 2 study conducted in 30 patients demonstrated a partial response in 4 (13.3 percent) patients.[112]
Response: We appreciate the additional information and analysis provided by the applicant in response to our concerns regarding substantial clinical improvement, including the additional information on data trends supporting an improved ORR for BalversaTM when compared to other FDA approved medications. We note that in the cited study regarding the ORR for pembrolizumab, ORRs of 33 percent and 21 percent were achieved in two separate efficacy randomized trials with sample sizes of 834 and 540 respectively.[113] These are independent studies with varying sample and study characteristics and lacking unifying statistical testing. However, in light of the severity of the disease and patient population with limited treatment options, and the results provided by the applicant from its Phase II study, which featured an objective response rate of 40.4 percent, a disease control of 79.8 percent, and a median progression-free survival of 5.5 months, we agree with the applicant that BalversaTM meets the substantial clinical improvement criterion.
After consideration of the public comment we received, we have determined that BalversaTM meets all of the criteria for approval of new technology add-on payments. Therefore, we are approving new technology add-on payments for BalversaTM for FY 2020. Cases involving BalversaTM that are eligible for new technology add-on payments will be identified by ICD-10-PCS procedure code XW0DXL5. In its application, the applicant stated that BalversaTM will be supplied as 3 mg, 4 mg and 5 mg tablets with a recommended starting dose of 8 mg daily. According to the applicant, the WAC for one dose of BalversaTM is $613.20 per day for an average duration of 8.9 days. Therefore, the total cost of BalversaTM per patient is $5,481.89. Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the costs of the new medical service or technology, or 65 percent of the amount by which the costs of the case exceed the MS-DRG payment. As a result, the maximum new technology add-on payment for a case involving the use of BalversaTM is $3,563.23 for FY 2020.
g. ERLEADATM (Apalutamide)
Johnson & Johnson Health Care Systems Inc., on behalf of Janssen Products, LP, Inc., submitted an application for new technology add-on payments for ERLEADATM (apalutamide) for FY 2020. ERLEADATM received FDA approval on February 14, 2018. This oral drug is an androgen receptor inhibitor indicated for the treatment of patients who have been diagnosed with non-metastatic castration-resistant prostate cancer (nmCRPC).
Prostate cancer is the second leading cause of cancer death in men.[114] Androgens, a type of hormone that includes testosterone, can promote tumor growth. Androgen-deprivation therapy (ADT) is initially an effective way to treat prostate cancer. However, almost all men with prostate cancer eventually develop castration-resistant disease, or cancer that continues to grow despite treatment with hormone therapy or surgical castration.[115] Non-metastatic castration-resistant prostate cancer (nmCRPC) is a clinical state in which cancer has not spread to other parts of the body, but continues to grow despite treatment with ADT, either medical or surgical, that lowers testosterone levels. Delaying metastases, or extending metastasis-free survival (MFS), may delay symptomatic progression, morbidity, mortality, and healthcare resource utilization. According to the applicant, nearly all men who die from prostate cancer have antecedent metastases to bone or other sites. ERLEADATM blocks the effect of androgens on the tumor in order to delay metastases, a major cause of complications and death among men with prostate cancer. Prior to ERLEADATM, there were no FDA-approved treatments for nmCRPC to delay the onset of metastatic castration-resistant prostate cancer (mCRPC).[116] The U.S. incidence of nmCRPC is estimated to be 50,000 to 60,000 cases per year.[117]
With respect to the newness criterion, ERLEADATM (apalutamide) was granted Fast Track and Priority Review designations under FDA's expedited programs, and received FDA approval on February 14, 2018 for the treatment of patients who have been diagnosed with non-metastatic castration-resistant prostate cancer. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19325), we noted that the applicant submitted a request for approval for a unique ICD-10-PCS code for the administration of ERLEADATM beginning in FY 2020. Approval was granted for the following procedure code effective October 1, 2019: XW0DXJ5 (Introduction of Apalutamide Antineoplastic into Mouth and Pharynx, External Approach, New Technology Group 5).
As previously discussed, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, the applicant maintained that ERLEADATM is new because it was the first drug approved by the FDA with its mechanism of action. Specifically, ERLEADATM is an androgen receptor (AR) inhibitor that binds directly to the ligand-binding domain of the AR. It has a trifold mechanism of action. Apalutamide inhibits AR nuclear translocation, inhibits DNA binding, and impedes AR-mediated transcription, which together inhibit tumor cell growth.[118] According to the applicant, in non-clinical studies, apalutamide administration caused decreased tumor cell proliferation and increased apoptosis leading to decreased tumor volume in mouse xenograft models of prostate cancer. Furthermore, the applicant asserted that in additional non-clinical studies, apalutamide was shown to have a higher binding affinity to the androgen receptor than bicalutamide (CASODEX), a first-generation anti-androgen that has been used in clinical practice for the treatment of nmCRPC. However, the applicant noted that bicalutamide is not FDA-approved for this indication nor is there Phase III data available on its use in this population. In addition, according to the applicant, apalutamide has a different mechanism of action than bicalutamide because it does not show antagonist-to-antagonist switch like bicalutamide.
With regard to the second criterion, whether a product is assigned to the same or different MS-DRG, the applicant noted that patients who may be eligible to receive treatment involving ERLEADATM in the inpatient setting will likely be hospitalized due to other conditions. Therefore, the applicant explained that potential cases eligible to receive treatment involving ERLEADATM are likely to be assigned to a wide variety of MS-DRGs, and ERLEADATM is similar to existing technologies in this respect.
With regard to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, the applicant maintained that ERLEADATM was the first FDA-approved treatment option for patients who have been diagnosed with nmCRPC. According to the applicant, there are a number of therapies currently available for patients who have been diagnosed with mCRPC, including chemotherapy, continuous ADT, immunotherapy, radiation therapy, radiopharmaceutical therapy, and androgen pathway treatments, including secondary hormonal therapies and supportive care. However, prior to ERLEADATM, there were no FDA-approved treatment options for patients who have been diagnosed with nmCRPC to delay the onset of mCRPC. Therefore, according to the applicant, ERLEADATM provides a treatment option to patients who have been diagnosed with a stage of prostate cancer that previously had no other approved treatment options available, and the standard approach was “watch and wait/observation.” The applicant stated that both the National Comprehensive Cancer Network® (NCCN®) guidelines for prostate cancer and American Urological Association (AUA) guidelines for castration-resistant prostate cancer note the limited treatment options for nmCRPC as compared to mCRPC. The applicant pointed out that apalutamide is highly recommended, as one of the two treatments with a Category 1 recommendation included in the NCCN® guidelines and standard treatment options for asymptomatic nmCRPC based on evidence level Grade A in the AUA guidelines.[119 120] Therefore, the applicant posited that ERLEADATM involves the treatment of a new patient population because it is a new treatment option for patients who have been diagnosed with nmCRPC and have limited available treatment options.
As noted in the proposed rule and previously summarized, the applicant maintained that ERLEADATM meets the newness criterion and is not substantially similar to existing technologies because it has a unique mechanism of action and offers an effective treatment option to a new patient population with limited available treatment options. We invited public comments on whether ERLEADATM meets the newness criterion.
Comment: The applicant commented that CMS did not express concern about the newness criterion, and reiterated that ERLEADATM is not substantially similar to existing technologies and qualifies as new because it was the first drug with its mechanism of action approved by the FDA to treat patients with nmCRPC.
Response: We agree that ERLEADATM is not substantially similar to existing technologies and that it meets the newness criterion because it was the first drug with its mechanism of action approved by the FDA to treat patients with nmCRPC. We consider February 14, 2018 as the beginning of the newness period for ERLEADATM.
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that the technology meets the cost criterion. In order to identify the range of MS-DRGs to which cases representing potential patients who may be eligible for treatment using ERLEADATM may map, the applicant identified cases that would be eligible for use of ERLEADATM by the presence of two ICD-10-CM diagnosis code combinations: C61 (Malignant meoplasm of prostate) in combination with R97.21 (Rising PSA following treatment for malignant neoplasm of prostate); or C61 in combination with Z19.2 (Hormone resistant malignancy status). The applicant searched the FY 2017 MedPAR final rule file (claims from FY 2015) for claims with the presence of these two code combinations. Cases identified mapped to a wide variety of MS-DRGs. The applicant eliminated all hospital stays of fewer than 4 days from its analysis because of its assumption that most hospitals would not provide ERLEADATM for short-stay inpatients. The applicant also assumed that any hospital stay 4 days or longer would involve the daily provision of ERLEADATM. This resulted in 493 cases across 152 MS-DRGs, with approximately 33 percent of all cases mapping to the following 9 MS-DRGs: MS-DRG 871 (Septicemia or Severe Sepsis without MV >96 Hours with MCC); MS-DRG 543 (Pathological Fractures and Musculoskeletal and Connective Tissue Malignancy with CC); MS-DRG 683 (Renal Failure with CC); MS-DRG 723 (Malignancy, Male Reproductive System with CC); MS-DRG 722 (Malignancy, Male Reproductive System with MCC); MS-DRG 698 (Other Kidney and Urinary Tract Diagnoses with MCC); MS-DRG 699 (Other Kidney and Urinary Tract Diagnoses with CC); MS-DRG 682 (Renal Failure with MCC); and MS-DRG 948 (Signs and Symptoms without MCC).
For the 493 identified cases, the average case-weighted unstandardized charge per case was $66,559. The applicant then standardized the charges using the FY 2017 IPPS/LTCH PPS final rule Impact file. Because ERLEADATM would not replace any other therapies occurring during the inpatient stay, the applicant did not remove any charges for the current treatment. The applicant then applied the 2-year inflation factor of 8.59 percent (1.085868) published in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41718) to inflate the charges from FY 2017 to FY 2019. In the proposed rule, we noted that the inflation factors were revised in the FY 2019 IPPS/LTCH PPS final rule correction notice. The corrected final 2-year inflation factor is 1.08986 (83 FR 49844). The applicant converted the costs of ERLEADATM to charges using the inverse of the FY 2019 IPPS/LTCH PPS final rule pharmacy national average CCR of 0.191 (83 FR 41273) to include the charges in its estimate. Based on the FY 2019 IPPS/LTCH PPS final rule correction notice data file thresholds, the average case-weighted threshold amount was $52,362. The average case-weighted standardized charge per case was $76,901. Because the average case-weighted standardized charge per case exceeds the average case-weighted threshold amount, the applicant maintained that the technology meets the cost criterion.
The applicant submitted an additional cost analysis including hospital stays shorter than 4 days to demonstrate that ERLEADATM also meets the cost criterion using all discharges in the analysis, regardless of length of stay. While the applicant maintained that ERLEADATM is unlikely to be administered by the hospital for inpatient stays fewer than 4 days, the applicant demonstrated that the average case-weighted standardized charge per case ($57,150) continues to exceed the average case-weighted threshold amount ($50,225) using all discharges (932 cases).
In the proposed rule, we noted that the applicant used the proposed rule values to inflate the previously discussed standardized charges. However, we further noted that even when using either the final rule values or the corrected final rule values to inflate the charges, the average case-weighted standardized charge per case exceeded the average case-weighted threshold amount in each analysis. We invited public comments on whether ERLEADATM meets the cost criterion.
Comment: The applicant commented that the average case-weighted standardized charge per case was above the average case-weighted threshold amount in both the initial and second analysis.
Response: We agree that ERLEADATM meets the cost criterion.
With respect to the substantial clinical improvement criterion, the applicant asserted that ERLEADATM represents a substantial clinical improvement because: (1) The technology offers a treatment option for a patient population previously ineligible for treatments, because ERLEADATM is the first FDA-approved treatment for patients who have been diagnosed with nmCRPC; and (2) use of the technology significantly improves clinical outcomes for a patient population because ERLEADATM was shown to significantly improve a number of clinical outcomes in the randomized Phase III SPARTAN trial,[121] including significant improvement in metastasis-free survival (MFS).
First, the applicant stated that there were no FDA-approved treatments to delay metastasis for patients who have been diagnosed with nmCRPC, a small but important clinical state within the spectrum of prostate cancer, prior to the FDA approval of ERLEADATM. The applicant emphasized that until the FDA approved the use of ERLEADATM, Medicare patients who have been diagnosed with nmCRPC had extremely limited treatment options, and the standard approach was “watch and wait/observation.” The applicant asserted that ERLEADATM offers a promising new treatment option and has been shown to improve MFS in a Phase III trial [122] with a demonstrated safety and tolerability profile and no negative impact to health-related quality of life based on patient-reported outcomes. Therefore, the applicant stated that the “robust results” of the clinical trial demonstrate that ERLEADATM is a substantial clinical improvement over existing technologies because it provides an effective treatment option for a patient population previously ineligible for treatments.
Second, the applicant maintained that ERLEADATM is a substantial clinical improvement because ERLEADATM was shown to significantly improve a number of clinical outcomes, most notably MFS. Metastases are a major cause of complications and death among men with prostate cancer. Therefore, according to the applicant, delaying metastases may delay symptomatic progression, morbidity, mortality, and healthcare resource utilization. ERLEADATM was approved by the FDA based on a prostate cancer trial using the primary endpoint of MFS, with overall survival used as a secondary endpoint.
The SPARTAN trial was a randomized, double-blind, placebo-controlled, Phase III trial which included men who had been diagnosed with nmCRPC and a prostate-specific antigen doubling time of 10 months or less. Patients were randomly assigned, in a 2:1 ratio, to receive apalutamide (240 mg per day) or placebo. A total of 1,207 men underwent randomization (806 to the apalutamide group and 401 to the placebo group). All of the patients continued to receive androgen-deprivation therapy. The primary end point of MFS was defined as the time from randomization to the first detection of distant metastasis on imaging or death. The study team calculated that a sample of 1,200 patients with 372 primary end-point events would provide the trial with 90 percent power to detect a hazard ratio for metastasis or death in the apalutamide group versus the placebo group of 0.70, at a two-sided significance level of 0.05. The Kaplan-Meier method was used to estimate medians for each trial group. The primary statistical method of comparison for time-to-event end points was a log-rank test with stratification according to the pre-specified factors. Cox proportional-hazards models were used to estimate the hazard ratios and 95 percent confidence intervals.
According to the applicant, results of the primary endpoint analysis for MFS were both statistically significant and clinically meaningful. Median MFS was 40.5 months in the apalutamide group as compared with 16.2 months in the placebo group (hazard ratio [HR] = 0.28; 95 percent confidence interval [CI]: 0.23, 0.35; P<0.0001). In other words, ERLEADATM significantly prolonged MFS by 2 years in men who had been diagnosed with nmCRPC. In a multi-variate analysis, treatment with ERLEADATM was an independent predictor for longer MFS (HR: 0.26; 95 percent CI: 0.21-0.32; P<0.0001). The treatment effect of ERLEADATM on MFS was consistently favorable across pre-specified subgroups, including patients with Prostate Specific Antigen doubling time (PSADT) of less than 6 months versus more than 6 months (short PSA doubling time is a predictor of metastasis), use of bone-sparing agents, and local-regional disease.
Additionally, the applicant stated that the validity of the primary endpoint results is supported by improvements in all secondary endpoints, with significant improvement observed in time to metastasis, progression-free survival (PFS), and time to symptomatic progression (all P<0.001) for ERLEADATM compared to placebo.
According to the applicant, treatment with ERLEADATM significantly extended time to metastasis by almost 2 years (40.5 months versus 16.6 months, P<0.001). In addition, time to bone metastasis and nodal metastasis in particular were both significantly longer (P<0.0001) in the ERLEADATM group compared to the placebo group.
According to the applicant, ERLEADATM was also associated with a significant improvement in the secondary endpoint of PFS, at 40.5 months for the ERLEADATM group versus 14.7 months for the placebo group (P<0.001). In a multi-variate analysis of patients treated in the SPARTAN study, treatment with ERLEADATM was an independent predictor for longer time to symptomatic progression (reached versus not reached; P<0.001).
The applicant also included the results of additional secondary endpoints for CMS consideration as evidence of substantial clinical improvement, including a suggested overall survival (OS) benefit; demonstrated safety profile; maintained quality of life; and decreased prostate specific antigen (PSA) levels.
While OS data were not mature at the time of final MFS analysis (only 24 percent of the required number of OS events were available for analysis), the applicant asserted that OS results suggested a benefit of treatment using ERLEADATM as compared to placebo. The applicant explained that, according to a statistical analysis model correlating the proportion of variability of OS attributable to the variability of MFS, patients who developed metastases at 6, 9, and 12 months had significantly shorter median OS compared with those patients without metastasis.
The applicant also stated that treatment using ERLEADATM provides an effective option with a demonstrated safety profile and tolerability for patients who have been diagnosed with nmCRPC. The safety of the use of ERLEADATM was assessed in the SPARTAN trial, and adverse events (AEs) that occurred at ≥15 percent in either group included: Fatigue, hypertension, rash, diarrhea, nausea, weight loss, arthralgia, and falls. The applicant asserted that in considering the risks and benefits of treatment involving the use of ERLEADATM for patients who have been diagnosed with nmCRPC, the FDA noted that there were no FDA-approved treatments for the indication and that ERLEADATM had a favorable risk-benefit profile.
Next, the applicant stated that the use of ERLEADATM also has a substantial clinical improvement benefit of maintaining quality of life. According to the applicant, patients who have been diagnosed with nmCRPC are generally asymptomatic, so it is a positive outcome if the addition of a therapy does not cause degradation of health-related quality of life. The applicant maintained that in asymptomatic men who have been diagnosed with high-risk nmCRPC, health-related quality of life (HRQOL) was maintained after initiation of the use of ERLEADATM.[123] According to the applicant, patient-reported outcomes using the Functional Assessment of Cancer Therapy-Prostate [FACT-P] questionnaire and European Quality of Life-5 Dimensions-3 Levels [EQ-5D-3L] questionnaire results indicated that patients who received treatment involving ERLEADATM maintained stable overall HRQOL outcomes over time from both treatment groups.
Additionally, the applicant discussed prostate specific antigen (PSA) outcomes as another secondary result demonstrating substantial clinical improvement. PSA, a protein produced by the prostate gland, is often present at elevated levels in men who have been diagnosed with prostate cancer and PSA tests are used to monitor the progression of the disease. According to the applicant, at 12 weeks after randomization, the median PSA level had decreased by 89.7 percent in the ERLEADATM group versus an increase of 40.2 percent in the placebo group. In an exploratory analysis performed by the applicant of patients treated in the SPARTAN study, the use of ERLEADATM decreased the risk of PSA progression by 94 percent compared with the patients in the placebo group (not reached vs 3.71 months; HR: 0.064; 95 percent CI: 0.052-0.080; P<0.0001). Overall, a ≥90 percent maximum decline in PSA from baseline at any time during the study was reported in 66 percent of the patients in the ERLEADATM group and 1 percent of the patients in the placebo group, according to the applicant. The applicant noted that increase in time to PSA progression is relevant from a clinical standpoint for clinicians and patients alike because PSA monitoring, rather than the use of regularly scheduled surveillance imaging, as was the case with SPARTAN, is often the most practical method of screening for progression of nmCRPC.
In the proposed rule, we stated that we had the following concerns regarding the applicant's assertions of substantial clinical improvement:
- Regarding the SPARTAN trial design, we stated we were concerned that the study enrollment may not be representative of the U.S. population considering that North American enrollment was only 35 percent of patients overall, and only approximately 6 percent of enrolled patients were black. Underrepresentation of black patients is of particular concern considering that, in the United States, African-American patients are disproportionately affected by prostate cancer. According to the CDC,[124] the rate of new prostate cancers by race is 158.3 per 100,000 men for African-Americans, compared to 90.2 for whites, 78.8 for Hispanics, 51.0 for Asian/Pacific Islanders, and 49.6 for American Indians/Alaska Natives. We stated that we were concerned that, based on an exploratory subgroup analysis performed by the applicant, black patients may not have performed better in the treatment group; while the hazard ratio of 0.63 (95 percent confidence interval: 0.23, 1.72) suggests a benefit to the group treated with ERLEADATM, the median MFS for this subgroup was reported as shorter for the ERLEADATM group at 25.8 months than for the placebo group, at 36.8 months.[125] Additionally, we noted that 23 percent of the patients in the SPARTAN trial did not have definitive local therapy at baseline for their diagnosis of prostate cancer, which is accepted standard-of-care in the United States.
In response to this concern about low North American enrollment and subgroup underrepresentation, the applicant submitted additional information claiming a consistent treatment effect across all subpopulations and regions. The applicant also pointed to the low hazard ratio for the subgroup of black patients as support for the benefit of the use of ERLEADATM. In the proposed rule, we welcomed additional information and public comments on whether the SPARTAN trial results are generalizable to the U.S. population, and in particular, African-American patients.
- We also noted regarding the SPARTAN trial that a total of 7.0 percent of the patients in the ERLEADATM group and 10.6 percent of the patients in the placebo group withdrew consent from the trial. In the proposed rule, we stated that additional explanation from the applicant of how those that withdrew were considered in the analysis, and whether there was any analysis of potential impact of withdrawals on the study results would be helpful.
- We also stated in the proposed rule that we had concerns about the primary endpoint used for the SPARTAN trial, MFS. The applicant explained that MFS was determined to be a reasonable end point for patients who have been diagnosed with nmCRPC because of the difficulty in using OS as a primary endpoint; multiple drugs can be used sequentially for advanced disease, necessitating larger and longer trials and potentially confounding interpretation of results if attempting to prove that a prostate cancer drug lengthens OS. Nevertheless, because MFS is not identical to OS and data on OS was not mature at the time of the study's results, we noted that it may be difficult to conclude based on the current data whether the use of ERLEADATM improves OS.
To address this concern, the applicant submitted additional information on MFS as a surrogate clinical endpoint for OS, including a recent study by the International Clinical Endpoints for Cancer of the Prostate (ICECaP) Working Group showing a correlation between MFS and OS in several prostate cancer studies.[126] The applicant explained that based on review of 19 randomized, controlled trials evaluating 21 study units in 12,712 men with localized prostate cancer, the correlation between OS and MFS was 0.91 (95 percent CI: 0.91-0.91) at the patient level, as measured by Kendall's τ. To demonstrate that MFS is closely linked with OS, the applicant cited a retrospective analysis of electronic health record database for patients who have been diagnosed with nmCRPC in which MFS independently predicted mortality risk; patients developing metastasis within 1 year had 4.4-fold greater risk for mortality (95 percent CI: 2.2-8.8) than those who remained metastasis-free at year 3.[127] The applicant also reiterated that a significant positive correlation between MFS and OS was observed in the SPARTAN trial (Pearson's correlation coefficient = 0.66; Spearman's correlation coefficient = 0.62, P<0.0001; and Kendall τ statistic = 0.52, parametric Fleischer's statistical model correlation coefficient of 0.69 (standard error, 0.002; 95 percent CI: 0.69-0.70)).
We invited public comments on whether ERLEADATM meets the substantial clinical improvement criterion for patients who have been diagnosed with nmCRPC.
Comment: The applicant submitted comments in response to concerns about the applicability of the data from the SPARTAN study to the US population, including African-American patients. The applicant stated that ERLEADATM treatment benefit was evaluated by region (North America, Europe, Asia-Pacific), and the treatment effect showing benefit from ERLEADATM in each region was consistent with the overall population. Also, the applicant pointed to the additional data summarized in the proposed rule (84 FR 19328) supplied in response to this concern, and reiterated that analyses by race also indicate that the SPARTAN study results are generalizable to the US patient population with nmCRPC, including African-Americans.
The applicant also responded to our request for additional explanation of how those that withdrew were considered in the analysis and the potential impact of withdrawals on the study results. According to the applicant, the small proportion of subjects who withdrew consent for the study are not expected to affect the analysis' conclusions; all subjects randomized to treatment were included in the Intention-to-Treat analysis for efficacy, including subjects who withdrew consent. The applicant stated that only 1.7 percent (n = 14) of subjects in the ERLEADATM group and 2.7 percent (n = 11) of subjects in the placebo group were censored due to withdrawal of consent, and that small proportion is not expected to impact the conclusion of the MFS analysis.
Finally, in response to our concern about the SPARTAN study primary endpoint, MFS, the applicant submitted information to demonstrate that MFS is accepted as a study endpoint by the FDA and the oncologic community. The applicant described draft guidance from the FDA [128] as stating that the prolonged disease course and assessment period for patients with nmCRPC may make the use of overall survival (OS) impractical as a primary endpoint to support approval of treatments, and that endpoints that can be measured earlier in the course of disease, including MFS, are useful and clinically relevant assessments.
Additionally, the applicant commented further on the clinical relevance of MFS and the correlation of metastasis with morbidity and the need for additional medical interventions. The applicant discussed the International Clinical Endpoints for Cancer of the Prostate (ICECaP) Working Group's review of 19 randomized controlled trials evaluating 21 study units in 12,712 patients with localized prostate cancer, in which the correlation between OS and MFS was 0.91 (95 percent CI: 0.91-0.91) at the patient level, as measured by Kendall's τ. At the trial level, R 2 was 0.83 (95 percent CI: 0.71-0.88) from weighted linear regression of 8-year OS rates vs 5-year MFS rates. The applicant asserted that the treatment effect (measured by log HR) for MFS and OS was well correlated (R2, 0.92 [95 percent CI: 0.81-0.95]).[129] The applicant also referred to the study of an electronic health record database in patients with nmCRPC in which MFS independently predicted mortality risk: Metastasis within 1 year had 4.4-fold greater risk for mortality (95 percent CI: 2.2-8.8) than those who remained metastasis-free at year 3.[130] The applicant also stated that the correlational analysis between MFS and OS in patients with nmCRPC included in the SPARTAN study showed that patients who developed metastases at 6, 9, and 12 months had significantly shorter median OS compared with those patients without metastasis. Finally, the applicant commented that the clinical benefit of MFS was further supported by an analysis of the SPARTAN study performed after one year of additional follow up, which assessed the time from randomization to the start of the next subsequent therapy after discontinuation of the study medication, known as second progression free survival (PFS2). According to the applicant, that analysis supported treating patients with nmCRPC with ERLEADATM provides a significantly longer response than ADT alone followed by a second therapy and support treatment of these patients with ERLEADATM.
Response: We appreciate the additional information and analysis provided by the applicant in response to our concerns regarding substantial clinical improvement. After reviewing the information submitted by the applicant addressing our concerns raised in the proposed rule, we agree that ERLEADATM represents a substantial clinical improvement because it significantly delays metastasis in patients with nmCRPC.
After consideration of the public comment we received, we have determined that ERLEADATM meets all of the criteria for approval for new technology add-on payments. Therefore, we are approving new technology add-on payments for ERLEADATM for FY 2020. Cases involving the use of ERLEADATM that are eligible for new technology add-on payments will be identified by ICD-10-PCS procedure code XW0DXJ5. In its application, the applicant estimated that the average Medicare beneficiary would require a dosage of 4 tablets per day. The applicant explained that the WAC is $10,920 for a thirty day supply, or $91.00 per tablet. Typical dosage for ERLEADATM is 4 tablets per day, resulting in a daily cost of $364. Because the drug is administered daily, the cost to the hospital would depend on the patient's length of stay. The applicant's MedPAR analysis determined an average length of stay of approximately 7.854 days. Multiplying the length of stay of 7.854 by the daily cost of $364 resulted in an average cost per patient of $2,858.84. Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the costs of the new medical service or technology, or 65 percent of the amount by which the costs of the case exceed the MS-DRG payment. As a result, the maximum new technology add-on payment for a case involving the use of ERLEADATM is $1,858.25 for FY 2020.
h. SPRAVATO (Esketamine)
Johnson & Johnson Health Care Systems, Inc., on behalf of Janssen Pharmaceuticals, Inc., submitted an application for new technology add-on payments for SPRAVATO (Esketamine) nasal spray for FY 2020. The FDA indication for SPRAVATO is treatment-resistant depression (TRD).
According to the applicant, major depressive disorder affects nearly 300 million people of all ages globally and is the leading cause of disability worldwide. People with major depressive disorder (MDD) suffer from a serious, biologically-based disease which has a significant negative impact on all aspects of life, including quality of life and function.[131] Although currently available anti-depressants are effective for many of these patients, approximately one-third do not respond to treatment.[132] Patients who have not responded to at least two different anti-depressant treatments of adequate dose and duration for their current depressive episode are considered to have been diagnosed with TRD. MDD in older age is marked by lower response and remission rates, greater disability and functional decline, decreased quality of life, and greater mortality from suicide.[133 134 135]
According to the applicant, currently available pharmacologic treatments for depression include Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), tricyclic anti-depressants (TCAs), other atypical anti-depressants, and adjunctive atypical antipsychotics. In addition to SPRAVATO, the only pharmacologic treatment currently approved for treatment-resistant depression is a combination of two drugs: An antipsychotic and an SSRI (fluoxetine/olanzapine combination). Currently available non-pharmacological medical treatments include electroconvulsive therapy, vagal nerve stimulation, deep brain stimulation (DBS), transcranial direct current stimulation (tDCS), and repetitive transcranial magnetic stimulation (rTMS).
According to the applicant, SPRAVATO is a non-competitive, subtype non-selective, activity-dependent glutamate receptor modulator. The applicant indicates that SPRAVATO works through increased glutamate release resulting in downstream neurotrophic signaling facilitating synaptic plasticity, thereby bringing about rapid and sustained improvement in people who have been diagnosed with TRD. The applicant explained that, through glutamate receptor modulation, SPRAVATO helps to restore connections between brain cells in people who have been diagnosed with TRD.[136]
According to the applicant, the nasal spray device is a single-use device that delivers a total of 28 mg of SPRAVATO in two sprays (one spray per nostril). The applicant has approved dosages of 56 mg (two devices) or 84 mg (three devices), with a 28 mg (one device) available for patients 65 years old and older. The treatment session consists of the patient's self-administration of SPRAVATO under healthcare supervision to ensure proper usage and post-administration observation to ensure patient stability. Specifically, clinicians will need to monitor blood pressure and mental status changes. The applicant states that monitoring will be required at every administration session.
With respect to the newness criterion, the applicant submitted a New Drug Application (NDA) for SPRAVATO Nasal Spray based on a recently completed Phase III clinical development program for treatment-resistant depression. According to the applicant, SPRAVATO was granted a Breakthrough Therapy designation in 2013. SPRAVATO Nasal Spray was approved by the FDA with an effective date of March 5, 2019. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19329), we noted that the applicant had submitted a request to the ICD-10 Coordination and Maintenance Committee for approval for a unique ICD-10-PCS procedure code to specifically identify cases involving the use of SPRAVATO, beginning in FY 2020. As of the time of the development of this final rule, a unique ICD-10-PCS procedure code to specifically identify cases involving the use of SPRAVATO has not yet been finalized in response to the applicant's request. Therefore, cases reporting SPRAVATO will be identified by ICD-10-PCS procedure code 3E097GC (Introduction of Other Therapeutic Substance into Nose, Via Natural or Artificial Opening) for FY 2020.
As previously discussed, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or similar mechanism of action, the applicant asserts that SPRAVATO has a unique mechanism of action. The applicant stated that SPRAVATO is the first new approach in 30 years for the treatment of major depressive disorder, including treatment-resistant depression.[137 138] According to the applicant, unlike existing approved anti-depressant pharmacotherapies, SPRAVATO's anti-depressant activity does not primarily modulate monoamine systems (norepinephrine, serotonin, or dopamine). The applicant asserts that SPRAVATO restores connections between brain cells in people with treatment-resistant depression through glutamate receptor modulation, which results in downstream neurotropic signaling.[139]
With regard to the second criterion, whether the technology is assigned to the same or different MS-DRG, the applicant asserts that it is likely that potential cases representing patients who may be eligible for treatment involving the use of SPRAVATO Nasal Spray would be assigned to the same MS-DRGs as patients who receive treatment involving currently available anti-depressants (AD).
With regard to the third criterion, whether the technology treats the same or a similar disease or the same or similar patient population, the applicant asserts that potential patients who may be eligible to receive treatment involving SPRAVATO will be comprised of a subset of patients who are receiving treatment involving currently available anti-depressants. The applicant did not specifically address the application of this criterion to SPRAVATO.
We invited public comments on whether SPRAVATO is substantially similar to any existing technologies and whether it meets the newness criterion.
Comment: The applicant submitted a public comment in response to the proposed rule. The applicant stated that SPRAVATO is not substantially similar to existing technologies and qualifies as new because it is the first new antidepressant mechanism of action in decades to treat Treatment Resistant Depression (TRD).[140 141] The applicant stated that unlike existing pharmacotherapies for depression, the primary antidepressant activity of SPRAVATO is not believed to directly involve inhibition of serotonin, norepinephrine, or dopamine reuptake.[142 143 144]
With regard to SPRAVATO treating the same or a similar disease or the same or similar patient population as existing technologies, the applicant reiterated that SPRAVATO treats, in conjunction with an oral antidepressant, TRD. According to the applicant, even with currently available antidepressant treatments, an estimated one-third of people in the U.S. who suffer with MDD fail to respond to treatment.[145] The applicant stated that TRD has no universally accepted definition; however, one definition consists of those patients with major depressive disorder (MDD) who have not responded to at least two different antidepressants of adequate dose and duration in the current depressive episode.[146]
Response: We appreciate the additional information provided by the applicant regarding whether SPRAVATO meets the newness criterion. After consideration of the public comments we received and information submitted by the applicant in its application, we believe that SPRAVATO uses a unique mechanism of action to achieve a therapeutic outcome because it works differently than currently available therapies, through glutamate receptor modulation rather than the inhibition of serotonin, norepinephrine, or dopamine reuptake. Therefore, we believe SPRAVATO is not substantially similar to existing treatment options and meets the newness criterion. We consider the beginning of the newness period to commence when SPRAVATO was approved by the FDA on March 5, 2019.
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that the technology meets the cost criterion. To identify cases eligible for SPRAVATO, the applicant searched the FY 2017 MedPAR data file for claims with the presence of one of the following ICD-10-CM diagnosis codes: F33 (Major depressive disorder, recurrent), F33.2 (Major depressive disorder, recurrent severe without psychotic features), F33.3 (Major depressive disorder, recurrent, severe with psychotic symptoms), and F33.9 (Major depressive disorder, recurrent, unspecified). Claims from the FY 2017 MedPAR data file with the presence of one of these ICD-10-CM diagnosis codes mapped to a wide variety of MS-DRGs. The applicant excluded claims if they had one or more diagnoses from the following list: (1) Aneurysmal vascular disease; (2) intracerebral hemorrhage; (3) dementia; (4) hyperthyroidism; (5) pulmonary insufficiency; (6) uncontrolled brady- or tachyarrhythmias; (7) history of brain injury; (8) hypertensive; (9) encephalopathy; (10) other conditions associated with increased intracranial pressure; and (10) pregnancy. The applicant believed that these conditions would preclude the use of SPRAVATO. The applicant also assumed that hospitals would not allow administration of SPRAVATO for short-stay inpatient hospitalizations and, therefore, excluded all hospitalizations of fewer than 5 days. The applicant assumed that patients would be allowed to administer their first dose on the 5th day and every 7 days thereafter. Lastly, the applicant assumed that, based on clinical data, patients would use 2.5 spray devices per treatment, once a week.
After applying the inclusion and exclusion criteria as previously described, the applicant identified a total of 3,437 potential cases mapping to 439 MS-DRGs, with approximately 54.7 percent of cases mapping to MS-DRGs 885 (Psychoses), 871 (Septicemia or Severe Sepsis without MV >96 Hours with MCC), 917 (Poisoning & Toxic Effects of Drugs with MCC), 897 (Alcohol/Drug Abuse or Dependence without Rehabilitation Therapy without MCC), 291 (Heart Failure & Shock with MCC or Peripheral Extracorporeal Membrane Oxygenation (ECMO)), 918 (Poisoning & Toxic Effects of Drugs without MCC), 190 (Chronic Obstructive Pulmonary Disease with MCC), 853 (Infectious & Parasitic Diseases with O.R. Procedure with MCC), 683 (Renal Failure with CC), and 682 (Renal Failure with MCC). The applicant further defined the potential cases representing patients who may be eligible for treatment involving the use of SPRAVATO in the cost criterion analysis by reducing the number of cases in each MS-DRG by one-third due to clinical data indicating that approximately one-third of patients who have been diagnosed with MDD also have been diagnosed with TRD.[147, 148]
The applicant calculated the average case-weighted unstandardized charge per case to be $73,119. Because the use of SPRAVATO is not expected to replace prior treatments, the applicant did not remove any charges for the prior technology. The applicant then standardized the charges and applied a 2-year inflation factor of 1.08986 obtained from the FY 2019 IPPS/LTCH PPS final rule correction notice (83 FR 49844). The applicant then added charges for the new technology to the inflated average case-weighted standardized charges per case. No other related charges were added to the cases. The applicant calculated a final inflated average case-weighted standardized charge per case of $74,738 and an average case-weighted threshold amount of $48,864. Because the final inflated average case-weighted standardized charge per case exceeded the average case-weighted threshold amount, the applicant maintained that the technology met the cost criterion.
With regard to the previous analysis, in the FY 2020 IPPS/LTCH PPS proposed rule we stated that we were concerned whether it is appropriate to reduce the number of cases to one-third of the total potential cases identified. While the supporting statistical data provided by the applicant suggest that one-third of patients who have been diagnosed with MDD often also receive diagnoses of TRD, we stated that it is unclear which cases representing patients should be removed. We further stated that it is possible that patients who have been diagnosed with MDD are covered by all 439 MS-DRGs, but patients who have been diagnosed with TRD only exist in a certain subset of these same MS-DRGs. Further, those patients who have been diagnosed with TRD could account for the most costly of patients who have been diagnosed with MDD. We noted in the proposed rule that, ultimately, without further evidence, we may not be able to verify that the assumption that patients who have been diagnosed with TRD comprise one-third of the identified cases representing patients who have been diagnosed with MDD and are evenly distributed across all of the MS-DRG identified cases is appropriate. We invited public comments on this issue and whether the SPRAVATO Nasal Spray meets the cost criterion.
Comment: The applicant submitted a comment in regard to our concerns on the cost criterion. The applicant reiterated that there are no ICD-10 codes with which to identify patients with TRD and about 1/3 of people with MDD have TRD. The applicant then stated that in its original cost analysis they found cases with diagnosis codes signifying MDD and randomly selected 1/3 of those cases for the cost analysis. In response to CMS' concerns, the applicant updated the analysis selecting the 1/3 of cases with the highest charges. This choice was made in response to a study comparing Medicare beneficiaries with TRD and Medicare beneficiaries without TRD which found that the cost of the inpatient hospitalizations for the TRD cohort were clearly higher (average $9,947 vs. $5,426).[149] With this new sample selection the applicant performed the cost analysis using the inverse of the FY 2019 pharmacy national average CCR of 0.191 to determine the charges for SPRAVATO, and a 2-year inflation factor of 1.08986 from the FY 2019 IPPS final rule correction notice to inflate the charges from FY 2017 to FY 2019. The applicant stated that with the new selection methodology, SPRAVATO meets the cost criterion, with an inflated average case-weighted standardized charge per case of $165,669 that exceeds the average case-weighted threshold amount of $74,682.
Response: We appreciate the comment and additional information provided by the applicant. After consideration of the public comment we received, we agree that SPRAVATO meets the cost criterion.
With respect to the substantial clinical improvement criterion, the applicant asserted that SPRAVATO Nasal Spray represents a substantial clinical improvement over existing treatments because it provides a treatment option for a patient population that failed available treatments and who have shown inadequate response to at least two anti-depressants in their current episode of MDD.[150] According to the applicant, in addition to SPRAVATO, there is currently only one other pharmacotherapy used for the treatment for diagnoses of TRD that is approved by the FDA (Symbyax®, a fluoxetine-olanzapine combination), but its use is limited by tolerability concerns.[151] In support of its assertions of substantial clinical improvement, the applicant provided several studies regarding SPRAVATO.
The first study is a Phase II, double-blind, doubly-randomized, placebo-controlled, multi-center study in adults aged 20 years old to 64 years old.[152] This study consisted of the following four phases: The screening, double-blind treatment, the optional open-label treatment, and post-treatment follow-up. During the treatment phase, two periods of treatment occurred between the 1st and the 8th day and the 8th and the 15th day. At the beginning of first treatment period, participants were randomized 3:1:1:1 to an intranasal placebo, SPRAVATO 28 mg, 56 mg, or 84 mg twice weekly, respectively. During the second treatment period, patients who were initially randomized to treatment groups remained on the treatment regimen until the 15th day. Patients initially assigned to the placebo group and who had moderate to severe symptoms (as measured by the 16-item quick inventory of depressive symptomatology-self report total score) were re-randomized 1:1:1:1 to placebo, SPRAVATO 28 mg, 56 mg, or 84 mg twice weekly groups, respectively.
Of the 126 patients screened, 67 were randomized at the beginning of the first treatment period, with 33 patients receiving placebo, 11 patients receiving 28 mg of SPRAVATO, 11 patients receiving 56 mg of SPRAVATO, and 12 patients receiving 84 mg of SPRAVATO in dosages. At the beginning of the second treatment period, those in the treated group remained on the same treatment regimen, while the 33 placebo patients were re-randomized. Of the placebo group in the first treatment period, 6 patients were added to the 4 who remained on placebo, 8 patients received 28 mg of SPRAVATO, 9 patients received 56 mg of SPRAVATO, and 5 patients received 84 mg SPRAVATO in dosages. Of the 67 respondents randomized, 63 (94 percent) completed the first treatment phase and 60 (90 percent) completed the first and second treatment phases. During both treatment phases patients were assessed at baseline, 2 hours, 24 hours, and at the study period endpoints for the Montgomery-Asberg Depression Rating Scale (MADRS) score, Clinical Global Impression of Severity scale score, adverse events and other safety assessments including the Clinician Administered Dissociative States Scale (CADSS). The primary efficacy endpoint, change from baseline to endpoint in MADRS total score, was analyzed using the analysis of covariance model including treatment and country as factors and period baseline MADRS total score as a covariate.[153]
At the end of the first treatment period, the least square mean change (standard error) for the placebo group was −4.9 (1.74). As compared to the placebo, the least square mean difference from placebo (standard error) for the SPRAVATO treatment groups was −5.0 (2.99) for 28 mg of SPRAVATO in dosage, −7.6 (2.91) for 56 mg of SPRAVATO in dosage, and −10.5 (2.79) for 84 mg of SPRAVATO in dosage; these differences were statistically significant at or beyond p < 0.05. Similar differences were seen at 2 hours and 24 hours for these groups with the only non-significant difference occurring for 56 mg of SPRAVATO in dosage at 2 hours as compared to baseline. At the end of the second treatment period, the least square mean change (standard error) for the placebo group was −4.5 (2.92), for the SPRAVATO-treated groups was −3.1 (2.99) from the placebo for 28 mg of SPRAVATO in dosage, −4.4 (3.06) from the placebo for 56 mg of SPRAVATO in dosage, and −6.9 (3.41) from the placebo for 84 mg of SPRAVATO in dosage. Only the 84 mg of SPRAVATO dosage difference from the mean was statistically significant (p<0.05). When the results from the first and second treatment periods were pooled, all three groups had statistically significant differences from the placebo. Based on these results, the applicant asserts that all three SPRAVATO treatment groups were superior to the placebo.
When considering the safety profile of the use of SPRAVATO, the study reports that 3 (5 percent) of the treated patients and 1 (2 percent) open-label patient experienced adverse events leading to discontinuation (syncope, headache, dissociative syndrome, ectopic pregnancy). There was a noted dose response for the adverse events of dizziness and nausea only. Most of the treated patients experienced transient elevations in blood pressure and heart rate on dosing days, as well as perceptual changes and/or dissociate symptoms (as measured by CADSS) that began shortly after dosing and typically resolved by 2 hours.[154]
The study titled Transform One submitted by the applicant is a Phase III, randomized, double-blind, active controlled, multi-center study which enrolled patients 18 years old to 64 years old who had been diagnosed with treatment-resistant depression for 28 days.[155] Patients were randomized (1:1:1) to receive SPRAVATO 56 mg, 84 mg, or a placebo nasal spray administered twice weekly combined with a newly initiated, open-label oral anti-depressant (AD) administered daily (duloxetine, escitalopram, sertraline, or venlafaxine extended release), which was dosed according to a fixed titration schedule. Patients were assessed on the MADRS, CADSS, and discharge readiness as measured by overall clinical status and the Global Assessment of Discharge Readiness (CGADR). Discharge status was assessed at 1 and 1.5 hours. MADRS was assessed at 24 hours post initial dose and weekly thereafter. CADSS was assessed at baseline and all dosing visits.
Three hundred and fifteen patients of the 346 were randomized and completed the treatment phase; 115 patients were randomized to the 56 mg of SPRAVATO dosage group along with 114 to the 84 mg of SPRAVATO dosage group and 113 to the placebo group. The withdrawal rate was 3-fold higher in the 84 mg of SPRAVATO dosage group (16.4 percent) than the 56 mg of SPRAVATO dosage group (5.1 percent) and the placebo group (5.3 percent). Eleven of the 19 84 mg of SPRAVATO dosage withdrawals withdrew after only receiving the first 56 mg SPRAVATO dose; the withdrawal rate was not a dose-related safety finding. Baseline statistics show few differences between groups: The 56 mg of SPRAVATO dosage group has a higher proportion of patients who have 1 or 2 previous AD medications (69 percent) as compared to the patients in the 84 mg of SPRAVATO dosage group (51.8 percent) and placebo group (59.3 percent), and the placebo group (193.1) has a notably shorter duration of the current episode of depression in weeks as compared to the 56 mg of SPRAVATO dosage group (202.8) and 84 mg of SPRAVATO dosage group (212.7). The MADRS score was assessed by a mixed model for repeated measures with change from baseline as the response variable and the fixed effect model terms for treatment dosage, day, region, class of oral AD, a treatment-by-day moderating effect, and baseline value as a covariate.
The primary efficacy measure was assessed by change in MADRS score from baseline at 28 days. At the end of the study the 56 mg and 84 mg of SPRAVATO dosage groups had a difference of least square means of −4.1 and −3.2, respectively. Neither of these were statistically significant differences as compared to the placebo. The least square mean treatment difference of MADRS score as compared to the placebo were also assessed longitudinally at baseline and the 2nd day (−3.0 for the 56 mg of SPRAVATO dosage group and −2.2 for the 84 mg of SPRAVATO dosage group), the 8th day (−3.0 for the 56 mg of SPRAVATO dosage group and −2.7 for the 84 mg of SPRAVATO dosage group), the 15th day (−3.8 for the 56 mg of SPRAVATO dosage group and −3.6 for the 84 mg of SPRAVATO dosage group), the 22nd day (−5.0 for the 56 mg of SPRAVATO dosage group and −3.7 for the 84 mg of SPRAVATO dosage group), and the 28th day (−4.0 for the 56 mg of SPRAVATO dosage group and −3.6 for the 84 mg of SPRAVATO dosage group). In a graph provided by the applicant, the lines plus standard errors plotted for the 56 mg and 84 mg of SPRAVATO dosage groups overlap with each other at each time point, but do not appear to overlap with the placebo group (calculated confidence intervals would necessarily be wider and would possibly overlap).
A secondary efficacy measure was the rate of patients who are responders and remitters. Response is defined as greater than or equal to 50 percent improvement on MADRS from baseline. Remission is defined as a MADRS total score less than or equal to 12. The 56 mg and 84 mg of SPRAVATO dosage treatment groups, 54.1 percent and 53.1 percent, respectively, had higher response rates than the placebo treatment group at 38.9 percent. The 56 mg and 84 mg of SPRAVATO dosage treatment groups, 36.0 percent and 38.8 percent, had higher remission rates than the placebo treatment group at 30.6 percent.
Lastly, safety was assessed by adverse events and CADSS. Both the 56 mg and 84 mg of SPRAVATO dosage treatment groups had spikes of CADSS scores, which spiked approximately 40 minutes post dose and resolved at 90 minutes. These post dose spikes gradually decreased from day 1 to day 25, but remained higher than the placebo group. The 84 mg of SPRAVATO dosage treatment group had higher CADSS score spikes than the 56 mg of SPRAVATO dosage treatment group at all periods except day 1. The top 5 of 12 pooled treatment group adverse events and percentages experienced are as follows: Nausea (29.4 percent), dissociation (26.8 percent), dizziness (25.1 percent), vertigo (20.8 percent), and headache (20.3 percent).
The study titled Transform Two is a Phase III, randomized (1:1), control trial, multi-center study enrolling patients 18 years old to 64 years old who had been diagnosed with treatment-resistant depression.[156] One hundred and fourteen patients were randomized to the treatment group and 109 to the control group; 101 and 100 of the treated and control groups respectively finished the study. For the treatment group, doses of SPRAVATO began at 56 mg on the 1st day, with potential increases up to 84 mg until the 15th day at which point the dose remained stable. Two-thirds of the SPRAVATO-treated patients were receiving the 84 mg dosage at the end of the study. For both the placebo and treatment groups, a newly-initiated AD was assigned by the investigator (duloxetine, escitalopram, sertraline, and venlafaxine extended release) following a fixed titration dosing.
The primary efficacy endpoint was the change from baseline at day 28 in MADRS total score, which was analyzed using a mixed-effects model using repeated measures (MMRM). The model included baseline MADRS total score as a covariate, and treatment, country, class of AD (SNRI or SSRI), day, and day-by-treatment moderator as fixed effects, and a random patient effect. The key secondary efficacy endpoints were as follows: The proportion of patients showing onset of clinical response by the 2nd day that was maintained for the duration of the treatment phase, the change from baseline in socio-occupational disability using the Sheehan Disability Scale (SDS) using the MMRM model, and the change from baseline in depressive symptoms using the patient health questionnaire 9-item (PHQ-9) using the MMRM model.
There were no apparent differences between the SPRAVATO treatment and placebo groups at baseline. At day 28, the difference of least square means (standard error) for the SPRAVATO-treated group was −4.0 (1.69) as compared to the placebo-treated group (p<0.05). Similar to Transform One, the difference of least square means for the SPRAVATO-treated group as compared to the placebo-treated group were plotted for baseline and the 2nd, 8th, 15th, 22nd, and 28th day. At all treatment periods, except baseline and the 15th day, the SPRAVATO treatment group had statistically significant lower scores than the placebo-treated group as indicated by 95 percent confidence intervals. The difference between the SPRAVATO-treated and placebo-treated groups for the early onset of sustained clinical response was substantively similar and not statistically different. The difference of least square means (standard error) in socio-occupational disability as measured by SDS was −4.0 (1.17) for those in the SPRAVATO-treated group as compared to the placebo-treated group (p<0.05). The difference of least square means (standard error) for the PHQ-9 total score for the SPRAVATO-treated group compared to the placebo-treated group was −2.4 (0.88) (p<0.05). Lastly, 69.3 percent of the SPRAVATO-treated patients as compared to 52.0 percent of the placebo-treated patients were considered responders and 52.5 percent of the SPRAVATO-treated patients as compared to 31.0 percent of the placebo patients were considered remitters. The adverse events list, post dosing blood pressure increase, and post dosing CADSS spike were similar to those seen in the previous Transform One study.[157]
A post-hoc analysis based on Transform Two, which included 46 SPRAVATO-treated and 44 placebo-treated patients was conducted to assess for differences in efficacy and safety between the U.S. population and the overall study population.[158] Efficacy was again assessed by MADRS, SDS, and PHQ-9 scores using the MMRM and with safety assessments for treatment-emergent adverse events (TEAEs), serious adverse events (SAEs), CADSS and other measures. At baseline the treated group of SPRAVATO plus an AD was similar to the placebo-treated group who took only an AD on most measures to include average age, sex, race, class of oral ADs, MADRS, CGI-S, SDS, and PHQ-9 scores. The placebo-treated group had a longer average duration of current episode at 177.6 days as compared to 132.2 days for the SPRAVATO-treated group; the placebo-treated group had a higher proportion of patients having 3 or more previous AD medications (50.1 percent) as compared to the SPRAVATO treatment group (32.7 percent).
Both the SPRAVATO-treated and placebo-treated groups showed improvement on the efficacy measures after 28 days. At the endpoint of 28 days, the SPRAVATO treatment group had a statistically significant MADRS total score least square mean difference of −5.5 (p < 0.05) from the placebo treatment group. At the endpoint the median scores on the clinician-rated severity of depressive illness as measured by CGI-S were −1.5 and −1.0 for the SPRAVATO-treated and placebo-treated groups respectively (one-sided p value > 0.07). For the measure of patient-rated severity of depressive illness, the SPRAVATO treatment group had a least square mean difference in PHQ-9 of −3.1 (p<0.05) as compared to the placebo treatment group. On the measure of functional impairment, the SPRAVATO treatment group had a least square mean difference in SDS of −5.2 (p<0.01) as compared to the placebo treatment group. Overall treatment-emergent adverse events were observed in 91.3 percent of SPRAVATO-treated patients and 77.3 percent of placebo-treated patients. One SPRAVATO-treated patient experienced a serious adverse event of cerebral hemorrhage. Lastly, the top five most common adverse events were dizziness, nausea, headache, dysgeusia, and throat irritation.
The study titled Transform Three is a randomized (1:1), double-blind, active-controlled, multi-center study in elderly patients 65 years old and older who had been diagnosed with TRD.[159] Randomization was stratified by country and class of oral AD (SNRI and SSRI). All treatment patients started on a 28 mg dosage of SPRAVATO and flexibly increased dosages of 56 mg or 84 mg based on investigator's determination of efficacy and tolerability. Both SPRAVATO-treated (n = 72) and placebo-treated (n = 66) patients were started on a newly initiated AD (duloxetine, escitalopram, sertraline, and venlafaxine extended release). One hundred and twenty-two patients completed the double-blind phase, with 63 patients in the SPRAVATO-treated group and 60 patients in the placebo-treated group.
The primary endpoint was the change in MADRS total score from the 1st day to the 28th day. Secondary endpoints included the evaluation of response and remission rates by group and the Clinical Global Impression—Severity (CGI-S) scores. The safety endpoints were evaluated by adverse event occurrence, laboratory tests, vital sign measurements, physical exams, and other exams.
At baseline, there were substantive differences between the placebo-treated and SPRAVATO treatment groups in three measures. Patients from the SPRAVATO treatment group (48.6 percent) were more likely to be from the European Union as compared to the placebo-treated group (36.9 percent). Patients from the SPRAVATO treatment group were more likely to have 1 (20.8 percent versus 9.2 percent) to 4 (16.7 percent versus 6.2 percent) previous ADs as compared to the placebo-treated group. On the measure of duration of current episode of depression in weeks, the SPRAVATO-treated group had an average (standard deviation) of 163.1 (277.04) as compared to the placebo-treated group with 274.1 (395.47). The primary endpoint, the change from baseline to Day 28 of MADRS score difference of least square means (95 percent CI) for the SPRAVATO treatment group was −3.6 (−7.20,0.07) as compared to the placebo group. As with previous studies, the longitudinal change in MADRS total score is presented for baseline and at the 8th, 15th, 22nd, and 28th day. The results for the SPRAVATO-treated group overlap with the placebo-treated group at each time point. At Day 28, 27.0 percent of the SPRAVATO-treated patients as compared to 13.3 percent of the placebo-treated patients were considered responders and 17.5 percent of the SPRAVATO-treated patients as compared to 6.7 percent of the placebo-treated patients were considered remitters. At baseline and the end of the study, 83.4 percent and 38.1 percent, respectively, of the SPRAVATO-treated patients were rated as experiencing severe or marked symptoms on the CGI-S scale as compared to 66.1 percent and 54.4 percent, respectively, for those on the placebo.
Of the 72 patients who were treated with SPRAVATO, 51 (70.8 percent) experienced a treatment-emergent adverse event (TEAE) as compared to 39 of the 65 (60.0 percent) placebo-treated patients. Five patients reported serious adverse events during the double-blind phase, three of whom were SPRAVATO-treated patients and two of whom were placebo-treated patients. The top 5 of the 16 adverse events among the treated patients are dizziness (20.8 percent), nausea (18.1 percent), blood pressure increase (12.5 percent), fatigue (12.5 percent), and headache (12.5 percent).
A post-hoc analysis, which included 34 SPRAVATO-treated patients and 36 placebo-treated patients from the Transform Three study, was performed to examine the response and remission associated with treatments in a subset of respondents 65 years old and older in the United States.[160] The MADRS, CGI-S, PHQ-9, and adverse event data were utilized to assess clinical outcomes. Remission was defined as a 50 percent or greater decrease in MADRS baseline score and remission was defined as a MADRS score of 12 or lower or a PHQ-9 score of less than 5. At baseline the SPRAVATO-treated and placebo-treated groups were similar on the measures of age, sex, race, class of oral AD, age at major depressive disorder diagnosis, MADRS score, and CGI-S score. The SPRAVATO treatment group differed from the placebo treatment group on the measures of mean duration of current depressive episode in weeks (187.6 versus 420.9) and mean PHQ-9 score (15.2 versus 18.2).
At the 28-day endpoint, response rates based on MADRS scores were 26.7 percent (n = 30) for the SPRAVATO-treated group and 14.7 percent (n = 34) for the placebo-treated group. At the endpoint, remission rates based on MADRS scores were 16.7 percent (n = 30) for the SPRAVATO-treated group and 2.9 percent (n = 34) for the placebo-treated group. Patient remission rates based on the PHQ-9 scores for SPRAVATO-treated and placebo-treated patients were 9.4 percent (n = 32) and 22.6 percent (n = 31), respectively. Clinically meaningful response as measured by a one point or greater decrease in the CGI-S score was 63.3 percent (n = 30) for the SPRAVATO-treated group and 29.4 percent (n = 34) for those on the placebo. Clinically significant response as measured by a decrease of two or greater on the CGI-S scale was 43.3 percent (n = 30) for the SPRAVATO-treated group and 11.8 percent (n = 34) for those on the placebo. Lastly, 67.7 percent of the SPRAVATO-treated patients and 58.3 percent of placebo-treated patients experienced a treatment-emergent adverse event. There was one serious adverse event in the SPRAVATO-treated group (hip fracture) and placebo-treated group (dizziness) each. The top 5 most common adverse events in the 34 SPRAVATO-treated patients were dysphoria (11.8 percent), fatigue (11.8 percent), headache (11.8 percent), insomnia (11.8 percent), and nausea (11.8 percent).
The study titled Sustain One concerns a double-blind, randomized withdrawal, multi-center study entering either directly or after completing the double-blind phase of an acute, short-term study.[161] A total of 705 patients were enrolled in this study of which 437 entered directly into the study and the remainder transferred from one of two short-term SPRAVATO studies (fixed dose, n = 150; flexible dose, n = 118). During the maintenance phase of this study, analyses were performed on two mutually exclusive groups: (1) On the stable remitters who were those randomized patients who were in stable remission at the end of the optimization phase and who received at least one dose of the study drug with one dose of an AD; and (2) on the stable responders who were those randomized patients who were stable responders at the end of optimization and who received at least one dose of the study drug with one dose of an AD. A relapse was defined as a MADRS total score of 22 or greater for 2 consecutive assessments separated by 5 to 15 days or hospitalization for worsening depression or any other clinically relevant event suggestive of relapse.
Of those classified in stable remission, 90 patients were receiving treatment with SPRAVATO in combination with an AD and 86 patients were receiving treatment with the placebo in combination with an AD. Of those classified in stable response, 62 patients were receiving treatment with SPRAVATO in combination with an AD and 59 patients were receiving treatment with the placebo in combination with an AD. At baseline, between group and within group randomization seems substantively successful, except for a lower proportion of placebo-treated stable responders being male (28.8 percent) as compared to SPRAVATO-treated stable responders (38.7 percent), placebo-treated stable remitters (31.4 percent), and SPRAVATO-treated stable remitters (35.6 percent).
Kaplan-Meier estimates of patients who remained relapse free were performed for both study groups. For both remitters and responders, the SPRAVATO-treated had a higher percent of patients without relapse for longer than the control group. Overall, among the stable remitters, 24 (26.7 percent) of the patients in the SPRAVATO-treated group and 39 (45.3 percent) of the patients in the placebo-treated group experienced a relapse event during the maintenance phase; among stable responders, 16 (25.8 percent) of the patients and 34 (57.6 percent) of the patients in the respective groups relapsed. Treatment with SPRAVATO in combination with an AD decreased the risk of relapse by 51 percent (estimated hazard ratio = 0.49; 95 percent CI: 0.29, 0.84) among stable remitters and by 70 percent (hazard ratio = 0.30; 95 percent CI: 0.16, 0.55) among stable responders, as compared to the placebo.
Safety and adverse events were presented similarly to the previously discussed study data. The top 5 of the 22 adverse events were dysgeusia (27.0 percent), vertigo (25.0 percent), dissociation (22.4 percent), somnolence (21.1 percent), and dizziness (20.4 percent). The applicant stated that most adverse events were mild to moderate, observed post dose on dosing days, and generally resolved in the same day. Serious adverse events considered related to the study drug were reported for six patients in the SPRAVATO treatment group (disorientation, hypothermia, lacunar stroke, sedation, and suicidal ideation for one patient each, and autonomic nervous system imbalance and simple partial seizure for one patient). The investigator considered the lacunar infarct as probably related to the treatment, while the sponsor considered the events of lacunar infarct and hypothermia as doubtfully related to the treatment. As with the previous studies, present-state dissociative symptoms and transient perceptual effects measured by the CADSS total score began shortly after the start of SPRAVATO dosing, peaked at 40 minutes, and resolved by 1.5 hours.
The next study presented by the applicant titled Sustain Two concerns an open-label, long-term (up to 1 year of exposure), multi-center, single-arm, Phase III study for patients who had been diagnosed with TRD who entered into the study as either direct-entry or transferred-entry (patients who completed the double-blind, randomized, 4-week, Phase III, efficacy and safety study in elderly patients).[162] A total of 802 patients were enrolled; 779 entered in the induction phase (691 as direct-entry and 88 as transferred-entry non-responders). A total of 603 patients entered the optimization/maintenance phase (580 from the induction phase and 23 were transferred-entry responders). A total of 150 (24.9 percent) of the patients completed the optimization/maintenance phase. At that time, the predefined total patient exposure was met and the study was stopped by the sponsor; 331 (54.9 percent) of the patients were still receiving treatment and, therefore, discontinued the study. Patients treated had a starting dose of 56 mg of SPRAVATO, or 28 mg for patients who were 65 years old or older, followed by flexible dosing increases (28 mg to 84 mg per clinical judgment) twice a week for 4 weeks. Dosages became stable at 15 days for those under 65 years old, and at 18 days for those 65 years old and older.
At baseline, 802 respondents had an average age of 52.2 years old, 62.6 percent were women, 85.5 percent were white, an average BMI of 27.9 percent, and 43.1 percent with a family history of depression. The anti-depressants prescribed to these respondents were duloxetine (31.1 percent), escitalopram (29.6 percent), sertraline (19.6 percent), and venlafaxine extended release (19.5 percent). Of the respondents at baseline, 39.9 percent had used 3 or more ADs prior to the study with no response. Safety measures were reported at 4 weeks, 48 weeks, and pooled. For TEAEs, 83.8 percent of patients experienced at least one at 4 weeks and 85.6 percent at 48 weeks. TEAEs occurred in 90.1 percent (n = 723) of all patients and led to discontinuation in 9.5 percent of both the pooled 4 and 48 week patient samples. TEAEs caused 2 deaths (acute respiratory and cardiac failure, and completed suicide; neither death considered as related by investigator) at 48 weeks. The top 5 most common TEAEs for the 4-week and 48-week time points were dizziness (29.3 percent and 22.4 percent), dissociation (23.1 percent and 18.6 percent), nausea (20.2 percent and 13.9 percent), headache (17.6 percent and 18.9 percent), and somnolence (12.1 percent and 14.1 percent). At 4 weeks, 2.2 percent of the patients experienced at least 1 serious adverse event and 6.3 percent at 48 weeks. Of the 68 serious adverse events, 63 were assessed as not related or doubtfully related to treatment involving SPRAVATO by the investigator. Five of the serious adverse events (anxiety, delusion, delirium, suicidal ideation and suicide attempt) were considered as treatment related. Overall, performance on multiple cognitive domains including visual learning and memory, as well as spatial memory/executive function either improved or remained stable post baseline in both elderly and younger patients.
Based on all of the previous discussion, the applicant concluded that the use of SPRAVATO represents a substantial clinical improvement over existing technologies. In the proposed rule, we stated the following concerns regarding whether SPRAVATO meets the substantial clinical improvement criterion.
First, we stated we were concerned that the use of the placebo in combination with a newly prescribed anti-depressant may not be the most appropriate comparator when assessing the clinical improvement of the use of SPRAVATO as compared to existing therapies. In its application, the applicant listed multiple treatment options aside from the use of anti-depressants, which are currently available to treat diagnoses of TRD. It is possible that other treatments approved for diagnoses of TRD may obtain better treatment outcomes than changing to a new single anti-depressant (as was the method used in the studies submitted in support of this application). We stated that comparisons with existing treatments for treatment-resistant major depressive disorders would help us better evaluate the clinical improvements offered by the use of SPRAVATO.
Second, we stated that we were not certain that the results in the studies submitted consistently show that the use of SPRAVATO represents a substantial clinical improvement when compared to existing therapies. We stated that there does not appear to be a consistent statistically significant positive primary efficacy outcome for SPRAVATO-treated patients compared to placebo-treated patients. Based on the data provided, we stated that we also were uncertain of the extent to which the findings from the submitted studies apply to the broader Medicare population. We further stated that we were particularly concerned that there are few substantive and statistically significant improvements in depression outcomes with SPRAVATO treatment among the Medicare-aged participants of the study samples. In addition, we stated that the studies which limit their analyses to Medicare-aged study participants have limited racial diversity amongst small samples. In addition, we noted that the submitted studies excluded patients with significant medical and psychiatric comorbidities through exclusion criteria. However, we noted the likelihood of having multiple chronic comorbid conditions is increased amongst those with a mental health disorder [163 164] and for the elderly.[165 166] The existence of comorbidities increases the likelihood that the negative effects of poly-pharmacy and drug-drug interactions could be experienced among the Medicare population. Given that the provided studies utilized exclusion criteria, which excluded those with serious comorbidities, we stated that we were concerned that the limited results did not adequately represent the average or even the majority of the Medicare population.
Third, we indicated that we had concerns regarding the primary and secondary endpoints for several of these studies. We stated that it was unclear whether the primary endpoint of these studies (change in baseline MADRS) was the most appropriate endpoint to assess substantial clinical improvement, particularly as it was unclear what threshold degree of change was defined as meeting the definition of change from baseline in the analyses, and whether this degree of change translated to clinical improvement (for example, response and remissions rates). In addition, we stated that we had concerns regarding the potential for physician behavior to have introduced bias, which could impact the study results. The studies state that anti-depressants are physician assigned and not randomized. Some of the provided studies control for the type of anti-depressant prescribed (SSRI and SNRI). We stated that we believed there was the potential for an interaction effect between the prescribed anti-depressant and SPRAVATO. We stated that it was possible that one particular anti-depressant (of the anti-depressants used in the studies)/SPRAVATO combination accounts for the entirety of the differences seen between the treated groups and the control groups. We further stated that without consistently controlling for the specific anti-depressants prescribed in multivariate analyses, we may not be able to parse this potentially complex relation apart.
Fourth, given that SPRAVATO is comprised of the drug ketamine, we stated in the proposed rule that we were concerned with the potential for abuse. Ketamine is accepted as a medication for which there is a strong possibility for abuse.[167 168 169] As one publication finds, current abuse of intravenous ketamine occurs intranasally.[170] While clinical trials assess the short-term benefits of ketamine treatment, there exists a paucity of long-term studies to assess whether chronic usage of this product may increase the likelihood of abuse.[171] In light of the potential for addictive behavior, we stated we were concerned that despite any demonstrated short-term clinical benefits, there may be potential negatives for the use of this drug in the longer term.
We invited public comments on whether SPRAVATO meets the substantial clinical improvement criterion.
Comment: The applicant submitted a comment addressing concerns raised by CMS in the proposed rule regarding whether SPRAVATO meets the substantial clinical improvement criterion. In response to CMS' concern that a placebo may be an insufficient comparator for SPRAVATO, the applicant stated that the use of a placebo was an appropriate method to assess clinical improvements in TRD. According to the applicant, two treatments (Symbyax [olanzapine and fluoxetine hydrochloride]) and electroconvulsive therapy) are available for use in place of a placebo but are not appropriate comparators due to tolerability concerns [172] for the former and poor side effects and limited availability for the latter.[173 174]
In response to CMS' concern that the results of studies did not consistently show substantial clinical improvement of SPRAVATO when compared to existing therapies, the applicant referenced previously submitted studies, Transform-2 and Sustain-1. According to the applicant, in the Transform-2 trial, patients with TRD achieved clinically meaningful and statistically significant improvement in depressive symptoms after being switched to SPRAVATO vs. a placebo [175] which resulted in a group treatment difference which exceeded minimum clinically important difference thresholds reported elsewhere.[176 177] Similarly the applicant asserted that, for Sustain-1, SPRAVATO demonstrated a significantly delayed time to relapse versus those treated with a placebo after 16 weeks of treatment with SPRAVATO.[178] The applicant further added that in a recent publication in the New England Journal of Medicine, data from the SPRAVATO Phase 3 studies provided evidence of clinically meaningful efficacy when SPRAVATO is used in combination with a newly initiated oral antidepressant.[179] The applicant concluded that SPRAVATO consistently shows efficacy at both the short and long-term time points.
In regard to CMS' concern about SPRAVATO's applicability to the Medicare population, the applicant reiterated results from the Transform-3 and Sustain-2 studies which included samples targeting ages 65 years of age and older. The applicant stated in their comment that they acknowledge the limitations of the clinical trials given the inclusion and exclusion criteria of the studies. The applicant also recognized that people under 65 years of age with long-term disabilities are also included in the Medicare population. Although the applicant did not capture in the trials whether or not patients were on disability, it indicated that many of the patients enrolled were not working because of their depression. In the Transform-2 and Sustain-1 studies 30.9 percent and 25.5 percent respectively of patients were unemployed; the applicant stated that many of the patients enrolled were not working because of their depression and therefore the percent unemployed was used as a proxy for chronically disabled.
In response to CMS' concern regarding studies lacking data to show efficacy across various racial groups, the applicant conceded that there is limited racial diversity amongst the Phase 3 clinical trials for TRD, and that their intent is to continue gathering evidence based on real world data as available. However, the applicant noted that based on the limited sample size, there did not appear to be any difference in efficacy for this variable.
In response to CMS' concern that studies provided exclude patients with certain medical and psychiatric comorbidities, the applicant stated that patients with other comorbid anxiety disorders, post-traumatic stress disorder, and certain chronic medical conditions were included. The applicant provided data from the Transform-3 study and pooled studies (Transform-1, Transform-2, and Sustain-1) showing the incidence of common psychiatric comorbidities upon enrollment in the phase three trials in adults 18-64 treated with SPRAVATO.

In response to CMS' concern that the primary endpoint (change in baseline MADRS) may not be the most appropriate for evaluating SPRAVATO success, the applicant stated the MADRS is a 10 item, clinician-administered scale designed to measure overall severity of depressive symptoms in subjects with MDD. The applicant stated that the scale was selected because it is validated, reliable, and acceptable to regulatory health authorities as a primary efficacy endpoint in a patient population with MDD. Each item is scored between 0-6, leading to a total score 0-60. The 10 items include the following symptoms: apparent sadness; reported sadness; inner tension; reduced sleep; reduced appetite; concentration difficulties; lassitude; inability to feel; pessimistic thoughts; suicidal thoughts. Cutoffs generally used for severity include: 0-6 normal; 7-19 mild depression; 20-34 moderate depression; >34 severe depression.[180] A “clinically meaningful” change from baseline on the MADRS (within-patient change) has been reported to range between a 6-9 point reduction in total score. Change in total scores is dependent, in part, on baseline MDD severity.[181 182] In contrast, when groups are compared to each other at the conclusion of a trial, a 2-point difference between groups has been found to be clinically meaningful.[183 184]
In response to CMS' concern about the potential for bias from clinical staff, the applicant commented that as SPRAVATO has known transient dissociative effects that are difficult to blind, potentially biasing the research staff who observed these adverse events (AEs), the MADRS was performed prior to dosing throughout the DB studies by independent remote (by phone) blinded raters using the Structured Interview Guide for the MADRS. Blinded, independent raters were specifically trained not to inquire about AEs, and study subjects were reminded not to discuss AEs with the MADRS raters. To enhance remote rating quality and reliability, and to prevent rater drift, audio-recording of the remote MADRS assessments was implemented.[185] As an additional measure to enhance blinding, a bittering agent was added to the placebo nasal spray to simulate the taste of SPRAVATO nasal spray.[186 187]
In response to CMS' concern about the potential for medication interactions between the newly prescribed antidepressant and SPRAVATO, the applicant provided subgroup analyses in a pooled adult population with TRD from the Transform-1 and -2 studies which showed no major differences in the MADRS total score from baseline to day 28 by class of antidepressant. Further, the applicant stated that the rate of treatment-emergent adverse events reported in subjects from the SSRI subgroup (87.4 percent) was similar to the rate in subjects from the SNRI subgroup (86.7 percent).
In response to CMS' concern for the potential abuse of SPRAVATO the applicant stated that the medication is mandated by the FDA to be accompanied by a Risk Evaluation and Mitigation Strategy (REMS) program and other procedures to mitigate potential risk for misuse and abuse in longer term use patients.[188] The applicant states that additional safeguards, such as safety surveillance using aggregate data from external sources and the restricted distribution of SPRAVATO to a limited number of wholesalers and distributers, are aimed at minimizing the risk of misuse. Finally, the applicant stated that the Phase 3 programs assessed for evidence of withdrawal or rebound symptoms after the cessation of SPRAVATO [189] and found no evidence up to four weeks later.
Response: We appreciate the thorough response and additional information provided by the applicant in response to our concerns regarding substantial clinical improvement. We agree with the applicant that due to difficulties arising from treatment with Symbyax or electroconvulsive therapy that it may be clinically challenging to use these current treatments for TRD as comparators for SPRAVATO. We also agree that SPRAVATO shows evidence of clinically meaningful efficacy based on the additional information provided by the applicant's comment regarding change in baseline MADRS score as an appropriate measure to assess substantial clinical improvement. We also appreciate the applicant's efforts to address clinical bias and the potential for abuse of SPRAVATO. In light of this information we agree that SPRAVATO meets the substantial clinical improvement criterion.
After consideration of the public comments we received, we have determined that Spravato meets all of the criteria for approval of new technology add-on payments. Therefore, we are approving new technology add-on payments for Spravato for FY 2020. Cases involving Spravato that are eligible for new technology add-on payments will be identified by ICD-10-PCS procedure code 3E097GC (Introduction of Other Therapeutic Substance into Nose, Via Natural or Artificial Opening). According to the applicant, the cost for one dose of SPRAVATO is $295, and patients will typically require 2.5 nasal spray units per treatment for a cost per day of $737.50. The applicant states that patients undergoing induction typically receive treatment twice per week while those undergoing maintenance receive treatment once per week or every two weeks. Because the applicant assumed that hospitals would not provide Spravato for stays shorter than 5 days the applicant assumed a dosage schedule where the 1st dosage is administered on day 5, the 2nd dosage is administered on day 12, and the 3rd dosage is administered on day 19, and so forth. The applicant found that there would be an average dosage of 2.1169 nasal spray units per discharge. The applicant therefore estimates that the average total cost of Spravato per patient per discharge is $1,561.21 ($737.50 × 2.1169). Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the average cost of the technology, or 65 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of Spravato is $1,014.79 for FY 2020.
i. XOSPATA® (gilteritinib)
Astellas Pharma U.S., Inc. submitted an application for new technology add-on payments for XOSPATA® (gilteritinib) for FY 2020. XOSPATA® received FDA approval November 28, 2018, and is indicated for the treatment of adult patients who have been diagnosed with relapsed or refractory acute myeloid leukemia (AML) with a FMS-like tyrosine kinase 3 (FLT3) mutation as detected by an FDA-approved test.
According to the applicant, XOSPATA® is an oral, small molecule FMS-like tyrosine kinase 3 (FLT3). The applicant states that XOSPATA® inhibits FLT3 receptor signaling and proliferation in cells exogenously expressing FLT3, including FLT3 internal tandem duplication (ITD), tyrosine kinase domain mutations (TKD) FLT3D835Y and FLT3-ITD-D835Y and that it induces apoptosis in leukemic cells expressing FLT3-ITD. FLT3 is a member of the class III receptor tyrosine kinase family that is normally expressed on the surface of hematopoietic progenitor cells, but it is over expressed in the majority of AML cases.
The applicant states that AML is a type of cancer in which the bone marrow makes abnormal myeloblasts (a type of white blood cell), red blood cells, or platelets. According to the applicant, AML is a rare and rapidly progressing form of cancer of the blood and bone marrow, characterized by the proliferation of immature white blood cells known as blast cells. The applicant states that while the specific cause of AML is unknown, AML is generally characterized by aberrant differentiation and increased proliferation of malignantly transformed myeloid progenitor cells. It is considered a heterogeneous disease state with various molecular and genetic abnormalities, which result in variable clinical outcomes. When untreated or refractory to available treatments, AML results in the accumulation of these transformed cells within the bone marrow and suppression of the production of normal blood cells (resulting in severe neutropenia and/or thrombocytopenia). AML may be associated with infiltration of these cells into other organs and tissues and can be rapidly fatal.
Almost 90 percent of leukemia cases are diagnosed in adults 20 years of age and older, among whom the most common types are chronic lymphocytic leukemia and AML.[190] AML accounts for approximately 80 percent of acute leukemias diagnosed in adults, with a median age at diagnosis of 66 years old. It has been estimated that 19,520 people are diagnosed annually with AML in the United States.[191] In general, the incidence of AML increases with advancing age; the prognosis is poorer in older patients, and the tolerability of the currently available standard-of-care treatment for patients who have been diagnosed with AML is much poorer for older patients.[192]
According to the applicant, approximately 30 percent of adult patients who have been diagnosed with AML are refractory, meaning unresponsive, to induction therapy. Furthermore, of those who achieve complete response (CR), approximately 75 percent will relapse. These patients are then determined to have relapsed/refractory (R/R) AML. According to the applicant, several chemotherapy regimens have been used for the treatment of patients who have been diagnosed with resistant or relapsed disease; however, the chemotherapy combinations are universally dose-intensive and cannot always be easily administered to older patients because of a high-risk of unacceptable toxicity. The applicant indicated that, while these regimens may generate second remission rates of up to 50 percent in patients with a first remission of more than 1 year, toxicity is high in most patients who are frail or over 60 years old.[193 194 195] Additionally, the applicant stated that if patients (including younger patients) relapse within 6 months of their initial CR, the chance of attaining a second remission is less than 20 percent with chemotherapy alone.[196] Furthermore, 5-year survival after first relapse is approximately 10 percent, demonstrating the lack of an effective cure for patients who have been diagnosed with relapsed AML.[197] Salvage therapy utilizing low-dose chemotherapy provides a therapy that is more tolerable; however, the low response rates (17 to 21 percent) makes the benefit of these agents limited.[198 199] Patients who are in second relapse or are refractory to first salvage, meaning unresponsive to both the preferred treatment, as well as the secondary choice of treatment, have an extremely poor prognosis, with survival measured in weeks.[200] Additionally, patients who have been diagnosed with R/R AML have poor quality of life, higher hospitalization and total resource use burden, and higher total healthcare costs.[201 202 203 204]
The applicant indicated that patients who have been diagnosed with AML with FLT3 positive mutations are a well-established subpopulation of AML patients, but there are no approved therapies for patients who have been diagnosed with R/R AML with FLT3 mutations. Approximately 30 percent of patients newly diagnosed with AML have mutations in the FLT3 gene.[205 206] FLT3 is a member of the class III receptor tyrosine kinase family that is normally expressed on the surface of hematopoietic progenitor cells. FLT3 and its ligand play an important role in proliferation, survival, and differentiation of multipotent stem cells. The applicant explained that FLT3 is overexpressed in the majority of patients diagnosed with AML. In addition, activated FLT3 with internal tandem duplication (ITD) or tyrosine kinase domain (TKD) mutations at around D835 in the activation loop are present in 20 percent to 25 percent and 5 percent to 10 percent of AML cases, respectively.[207] These activated mutations in FLT3 are oncogenic and show transforming activity in cells.[208]
Compared to patients with wild-type FLT3, AML patients with FLT3 mutation experience shorter remission duration at 2 years, according to the applicant. Approximately 30 percent of FLT3-ITD patients relapse versus approximately 16 percent of other AML patients.[209] Additionally, these patients experience poorer survival outcomes. The estimated median OS for patients who have been newly diagnosed with FLT3 mutations is 15.2 to 15.5 months compared to 19.3 to 28.6 months for patients with wild-type FLT3.[210] Patients who have been diagnosed with R/R FLT3 mutation positive AML have lower remission rates with salvage chemotherapy, shorter durations of remission to second relapse and decreased overall survival relative to FLT3 mutation negative patients.[211, 212, 213] According to the applicant, patients who have been diagnosed with FLT3 mutation positive R/R AML have a substantial unmet medical need for treatment.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19337), we noted that the applicant had submitted a request to the ICD-10 Coordination and Maintenance Committee for approval for a unique ICD-10-PCS code to identify procedures involving the use of XOSPATA®, beginning in FY 2020. Approval was granted for the following ICD-10-PCS procedure code effective October 1, 2019: XW0DXV5 (Introduction of Gilteritinib Antineoplastic into Mouth and Pharynx, External Approach, New Technology Group 5).
As discussed earlier, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and, therefore, would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, the applicant asserted that XOSPATA® has a unique mechanism of action and, therefore, should be considered new under this criterion. The applicant stated that XOSPATA® is an oral, small molecule FMS-like tyrosine kinase 3 (FLT3) inhibitor. According to the applicant, XOSPATA® inhibits FLT3 receptor signaling and proliferation in cells exogenously expressing FLT3, including FLT3 internal tandem duplication (ITD), tyrosine kinase domain mutations (TKD) FLT3-D835Y and FLT3-ITD D835Y, and it induces apoptosis in leukemic cells expressing FLT3-ITD. The applicant asserted that XOSPATA® is the only FLT3-targeting agent approved by the FDA for the treatment of relapsed or refractory FLT3mut+ AML.
With regard to the second criterion, whether a product is assigned to the same or a different MS-DRG, the applicant asserted that cases involving patients being medically treated for the type of AML indicated for XOSPATA® would map to the following MS-DRGs: 834 (Acute Leukemia without Major O.R. Procedure with MCC), 835 (Acute Leukemia without Major O.R. Procedure with CC), and 836 (Acute Leukemia without Major O.R. Procedure without CC/MCC). In the proposed rule, we indicated that under current coding conventions it appeared likely that cases involving treatment with the use of XOSPATA® would map to the same MS-DRGs as existing therapies.
With regard to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population when compared to an existing technology, the applicant stated that XOSPATA® is FDA-approved for the treatment of adult patients who have relapsed or refractory AML with a FLT3 mutation. Cases representing potential patients that may be eligible for treatment involving XOSPATA® would be identified by ICD-10-CM diagnostic codes C92.02 (Acute myeloblastic leukemia, in relapse) and C92.A2 (Acute myeloid leukemia with multilineage dysplasia, in relapse). The applicant further asserted that there are currently no other FLT3-targeting agents approved for the treatment of patients who have been diagnosed with relapsed or refractory FLT3mut+ AML. Therefore, the applicant asserted that XOSPATA® is indicated to treat a new patient population for which there are no other technologies currently available.
We invited public comments on whether XOSPATA® is substantially similar to any existing technologies, and whether it meets the newness criterion.
We did not receive any public comments concerning whether XOSPATA® meets the newness criterion.
After consideration of the information provided by the applicant, we believe that XOSPATA® has a unique mechanism of action and treats a new patient population for which there are no other technologies currently available, and therefore is not substantially similar to existing technologies and meets the newness criterion. .
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that the technology meets the cost criterion.
The applicant searched the FY 2017 MedPAR data file for cases reporting ICD-10-CM diagnosis codes C92.02 (Acute myeloblastic leukemia, in relapse) and C92.A2 (Acute myeloid leukemia with multilineage dysplasia, in relapse) listed as a primary or secondary diagnosis that mapped to MS-DRGs 834, 835, and 836. The applicant applied the following trims to the cases:
- Excluded Health Maintenance Organization (HMO) and IME Only claims;
- Excluded cases for bone marrow transplant because potential eligible patients who may receive treatment involving XOSPATA® would not receive a bone marrow transplant during the same admission as they received chemotherapy;
- Excluded cases indicating an O.R. procedure;
- Excluded cases treated at 8 providers that were not listed in the FY 2019 IPPS/LTCH PPS final rule correction notice impact file (these are predominately cancer hospitals).
After applying the previously discussed trims, 407 potential cases remained. The applicant noted that it used only departmental charges that are used by CMS for rate setting.
Using the 407 cases, the applicant determined an average case-weighted unstandardized charge per case of $166,389. The applicant then removed all pharmacy charges because the applicant believed that patients would typically receive other pharmaceuticals such as anti-emetics during the hospital stay and patients receiving treatment involving the use of XOSPATA® would continue to receive those other pharmaceuticals. Additionally, according to the applicant, blood charges were reduced because some patients receiving treatment involving the use of XOSPATA® became infusion independent in the clinical trial. The applicant standardized the charges for each case and inflated each case's charges by applying the proposed outlier charge inflation factor of 1.085868 (included in the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20581)). The applicant calculated an average case-weighted standardized charge per case of $157,034 using the percent distribution of MS-DRGs as case-weights. Based on this analysis, the applicant determined that the technology met the cost criterion because the final inflated average case-weighted standardized charge per case for XOSPATA® exceeded the average case-weighted threshold amount of $88,479 by $68,555. As noted in the FY 2020 IPPS/LTCH PPS proposed rule, the inflation factor used by the applicant was the proposed 2-year inflation factor, which was discussed in the FY 2019 IPPS/LTCH PPS final rule summation of the calculation of the FY 2019 IPPS outlier charge inflation factor for the proposed rule (83 FR 41718 through 41722). The final 2-year inflation factor published in the FY 2019 IPPS/LTCH PPS final rule was 1.08864 (83 FR 41722), which was revised in the FY 2019 IPPS/LTCH PPS final rule correction notice to 1.08986 (83 FR 49844).
We further noted that, although the applicant used the proposed rule value to inflate the standardized charges, even when using the final rule value or the corrected final rule value revised in the correction notice to inflate the charges, the final inflated average case-weighted standardized charge per case for XOSPATA® would exceed the average case-weighted threshold amount. We invited public comments on whether XOSPATA® meets the cost criterion.
We did not receive any comments on whether XOSPATA® meets the cost criterion. Based on the analysis described previously, we believe that XOSPATA® meets the cost criterion.
With regard to substantial clinical improvement, the applicant submitted one central study to support its assertion that XOSPATA® represents a substantial clinical improvement over existing technologies because it offers a treatment option for FLT3mut+ AML patients ineligible for currently available treatments. The applicant also asserted that XOSPATA® represents a substantial clinical improvement because the technology reduces mortality, decreases the number of subsequent diagnostic or therapeutic interventions, and reduces the number of future hospitalizations due to adverse events as shown by its studies.[214]
According to the applicant, the efficacy of XOSPATA® in the treatment of patients who have been diagnosed with R/R AML has been demonstrated in a U.S.-based, multi-national, active-controlled, Phase III study (ADMIRAL, 2215-CL-0301). This study was designed to determine the clinical benefit of the use of XOSPATA® in patients who have been diagnosed with FMS-like tyrosine kinase (FLT3) mutated AML who are refractory to, or have relapsed, after first-line AML therapy as shown with overall survival (OS) compared to salvage chemotherapy, and to determine the efficacy of the use of XOSPATA® as assessed by the rate of complete remission and complete remission with partial hematological recovery (CR/CRh) in these patients.[215]
In the ADMIRAL (2215-CL-0301) study, the applicant noted that XOSPATA® demonstrated clinically meaningful CR and CRh rates, as well as a clinically meaningful duration of CR/CRh in the patients studied. The CR/CRh rate was 21.8 percent, with 31/142 patients achieving a CR/CRh, 18/142 patients achieving CR (12.7 percent) and 13/142 patients achieving a CRh (9.2 percent). Of the 31 patients (21.8 percent) who achieved CR/CRh, the median duration of remission was 4.5 months. For the 18 patients who achieved CR and the 13 patients who achieved CRh, the median duration of response was 8.7 months and 2.9 months, respectively.[216]
The safety evaluation of XOSPATA® is based on 292 patients who had been diagnosed with relapsed or refractory AML treated with 120 mg of XOSPATA® daily. The applicant noted that when looking at the ADMIRAL study, the most common serious adverse events (SAEs) (Grade III or above) were lab abnormalities of elevation of liver transaminases in 43 (15 percent) of patients, fatigue in 14 (5 percent) of patients, myalgia or arthralgia in 13 (5 percent) of patients, and gastrointestinal disorders of diarrhea in 8 (3 percent) of patients and nausea in 4 (1 percent) of patients. Due to the number and type of SAEs reported, the applicant believed that XOSPATA® has the potential to decrease the number of subsequent future hospitalizations or physician visits as a result of management of adverse events, in particular serious adverse events.
Transfusion dependence was also evaluated in the XOSPATA®-treated patients. In some hematologic disorders, becoming transfusion independent or receiving fewer transfusions over a specified interval is defined as improvement or response depending on whether therapy is given.[217]
In the ADMIRAL study, at baseline prior to therapy initiation, 34 patients in the XOSPATA® arm were classified as transfusion independent and 107 patients were classified as transfusion dependent. Of these transfusion dependent patients, 34 (31.8 percent) patients became transfusion independent during XOSPATA® treatment. Of the 34 patients who were transfusion independent at baseline, 18 (52.9 percent) patients maintained transfusion independence during XOSPATA® treatment.
The applicant asserted that the use of XOSPATA® addresses a medical need in a patient population that has been difficult to manage in the past due to limited treatment options. In the ADMIRAL study, the applicant provided data specific to reduced mortality rate compared to historical data. Because of the small number of SAEs, the applicant stated that it anticipates reduction of subsequent diagnostic and therapeutic interventions, as well as decreased number of future physician visits and hospitalization as noted previously. However, we stated in the proposed rule the applicant did not provide direct numbers for the comparator arm of the ADMIRAL study in its application. Because of this, we further stated we were concerned that it may be difficult to determine XOSPATA®'s comparative effectiveness. We noted that the ADMIRAL study was designed to evaluate efficacy and head-to-head trials were lacking. We indicated in the proposed rule that until the comparative data for both randomized arms were available, we were concerned that there may be insufficient evidence to determine that XOSPATA® provides a substantial clinical improvement over existing technologies.
We invited public comments on whether XOSPATA® meets the substantial clinical improvement criterion.
Comment: The applicant provided updated information on the results of the Phase 3 ADMIRAL trial. As noted above, patients in the ADMIRAL trial with relapsed or refractory AML were randomized to receive either XOSPATA® or salvage chemotherapy. The applicant provided additional information that the median overall survival for patients who received XOSPATA® was 9.3 months compared to 5.6 months for patients who received salvage chemotherapy. Hazard ratio was 0.64 with 95 percent confidence levels of 0.49 to 0.83. The p-value was 0.0004. The applicant also provided information showing that the ADMIRAL trial showed a decrease of 34.5 percent in number of patients requiring the transfusion with RBC or platelets.
Response: We appreciate the comments and additional data submitted by the applicant in response to our concerns. After consideration of the additional data provided, which shows an improvement in median overall survival for patients who received XOSPATA® compared to patients who received salvage chemotherapy, we believe XOSPATA® meets the substantial clinical improvement criterion.
After consideration of the public comments we received, we have determined that XOSPATA® meets all of the criteria for approval of new technology add-on payments. Therefore, we are approving new technology add-on payments for FY 2020. Cases involving XOSPATA® that are eligible for new technology add-on payments will be identified by ICD-10-PCS code XW0DXV5 (Introduction of Gilteritinib Antineoplastic into Mouth and Pharynx, External Approach, New Technology Group 5). In its application, the applicant estimated that the average Medicare beneficiary would require a dosage of 120mg/day administered as oral tablets in three divided doses. According to the applicant, the WAC for one dose is $250, and patients will typically require 3 tablets for the course of treatment with XOSPATA® per day for an average duration of 15 days. Therefore, the total cost of XOSPATA® per patient is $11,250. Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the average cost of the technology, or 65 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of XOSPATA® is $7,312.50 for FY 2020.
j. GammaTile TM
GT Medical Technologies, Inc. submitted an application for new technology add-on payments for FY 2020 for the GammaTile TM. We note that Isoray Medical, Inc. and GammaTile, LLC previously submitted an application for new technology add-on payments for GammaTile TM for FY 2018, which was withdrawn, and also for FY 2019, however the technology did not receive FDA approval or clearance by July 1, 2018 and, therefore, was not eligible for consideration for new technology add-on payments for FY 2019. The GammaTile TM is a brachytherapy device for use in the treatment of patients who have been diagnosed with recurrent intracranial neoplasms, which uses cesium-131 radioactive sources embedded in a collagen matrix. GammaTile TM is designed to provide adjuvant radiation therapy to eliminate remaining tumor cells in patients who required surgical resection of recurrent brain tumors. According to the applicant, the GammaTile TM technology is a new vehicle of delivery for and inclusive of cesium-131 brachytherapy sources embedded within the product. The applicant stated that the technology has been manufactured for use in the setting of a craniotomy resection site where there is a high chance of local recurrence of a CNS or dual-based tumor. The applicant asserted that the use of the GammaTile TM technology provides a new, unique modality for treating patients who require radiation therapy to augment surgical resection of malignancies of the brain. By offsetting the radiation sources with a 3mm gap of a collagen matrix, the applicant asserted that the use of the GammaTile TM technology resolves issues with “hot” and “cold” spots associated with brachytherapy, improves safety, and potentially offers a treatment option for patients with limited, or no other, available options. The GammaTile TM is biocompatible and bioabsorbable, and is left in the body permanently without need for future surgical removal. The applicant asserted that the commercial manufacturing of the product will significantly improve on the process of constructing customized implants with greater speed, efficiency, and accuracy than is currently available, and requires less surgical expertise in placement of the radioactive sources, allowing a greater number of surgeons to utilize brachytherapy techniques in a wider variety of hospital settings. The GammaTile TM technology received FDA clearance as a Class II medical device on July 6, 2018. The cleared indications for use state that GammaTile TM is intended to deliver radiation therapy (brachytherapy) in patients who have been diagnosed with recurrent intercranial neoplasms. The applicant submitted a request for approval for a unique ICD-10-PCS code for the use of the GammaTile TM technology, which was approved effective October 1, 2017 (FY 2018). The ICD-10-PCS procedure code used to identify procedures involving the use of the GammaTile TM technology is 00H004Z (Insertion of radioactive element, cesium-131 collagen implant into brain, open approach).
As discussed earlier, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, the applicant stated that when compared to treatment using external beam radiation therapy, GammaTile TM uses a new and unique mechanism of action to achieve a therapeutic outcome. The applicant explained that the GammaTile TM technology is fundamentally different in structure, function, and safety from all external beam radiation therapies, and delivers treatment through a different mechanism of action. In contrast to external beam radiation modalities, the applicant further explained that the GammaTile TM is a form of internal radiation termed brachytherapy. According to the applicant, brachytherapy treatments are performed using radiation sources positioned very close to the area requiring radiation treatment and deliver radiation to the tissues that are immediately adjacent to the margin of the surgical resection. Conversely, external beam radiation therapy travels inward and typically exposes radiation to a large volume of normal brain tissue. As a result, the common clinical practice to avoid radiation toxicity is to reduce dosage ranges, limiting overall efficacy.
Due to the custom positioning of the radiological sources and the use of the cesium-131 isotope, the applicant noted that the GammaTile TM technology focuses therapeutic levels of radiation on an extremely small area of the brain. Unlike all external beam techniques, the applicant stated that this radiation does not pass externally inward through the skull and healthy areas of the brain to reach the targeted tissue and, therefore, may limit neurocognitive deficits seen with the use of external beam techniques. Because of the rapid reduction in radiation intensity that is characteristic of cesium-131, the applicant asserted that the GammaTile TM technology can target the margin of the excision with greater precision than any alternative treatment option, while sparing healthy brain tissue from unnecessary and potentially damaging radiation exposure.
The applicant also stated that, when compared to other types of brain brachytherapy, GammaTile TM uses a new and unique mechanism of action to achieve a therapeutic outcome. The applicant explained that cancerous cells at the margins of a tumor resection cavity can also be irradiated with the placement of brachytherapy sources in the tumor cavity. However, the applicant asserted that the GammaTile TM technology is a pioneering form of brachytherapy for the treatment of brain tumors that uses the isotope cesium-131 embedded in a collagen implant that is customized to the geometry of the brain cavity. According to the applicant, the use of cesium-131 and the custom distribution of seeds offset in a three-dimensional collagen matrix results in a unique and highly effective delivery of radiation therapy to brain tissue. Specifically, the applicant asserted that the offset radiation source permits only a prescribed radiation dose to reach the target surface, reducing the potential for radiation induced necrosis and the need for reoperation. Additionally, the applicant stated that because the half-life of cesium-131 used in GammaTile TM is shorter compared to other brachytherapy isotopes, this results in a more rapid and effective energy deposition than other isotopes with longer half-lives. Therefore, applicant believes that GammaTile TM is unique due to the greater relative biological effectiveness compared to other brachytherapy options.
With regard to the second criterion, whether a product is assigned to the same or a different MS-DRG, the GammaTile TM technology is a treatment option for patients who have been diagnosed with brain tumors that progress locally after initial treatment with external beam radiation therapy, and cases involving this technology are assigned to the same MS-DRG (MS-DRG 023 (Craniotomy with Major Device Implant/Acute Complex CNS PDX with MCC or Chemotherapy Implant)) as other current treatment forms of brachytherapy and external beam radiation therapy.
With regard to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, the applicant stated that the GammaTile TM technology offers a treatment option for a patient population with limited, or no other, available treatment options. The applicant explained that treatment options for patients who have been diagnosed with brain tumors that progress locally after initial treatment with external beam radiation therapy are limited, and there is no current standard-of-care in this setting. According to the applicant, surgery alone for recurrent tumors may provide symptom relief, but does not remove all of the cancerous cells. The applicant further stated that repeating external beam radiation therapy for adjuvant treatment is hampered by an increasing risk of brain injury because additional external beam radiation therapy will increase the total dose of radiation to brain tissue, as well as increase the total volume of irradiated brain tissue. Secondary treatment with external beam radiation therapy is often performed with a reduced and, therefore less effective, dose. The applicant stated that the technique of implanting cesium-131 seeds in a collagen matrix is currently only available to patients in one location and requires a high degree of expertise to implant. The manufacturing process of the GammaTile TM will greatly expand the availability of treatment beyond research programs at highly specialized cancer treatment centers.
Based on the previous discussion, the applicant concluded that the GammaTile TM technology is not substantially similar to other existing technologies and meets the newness criterion.
However, in the proposed rule we stated that we were concerned that the mechanism of action of the GammaTile TM may be the same or similar to current forms of radiation therapy or brachytherapy. Specifically, we stated that while the placement of the cesium-131 source (or any radioactive source) in a collagen matrix offset may constitute a new delivery vehicle, we were concerned that this sort of improvement in brachytherapy for the use in the salvage treatment of radiosensitive malignancies of the brain may not represent a new mechanism of action. We also questioned whether the technology treats a new patient population, as maintained by the applicant, because of the availability of other implantable treatment devices that treat the same patient population as the patients treated by the GammaTile TM.
We invited public comments on whether the GammaTile TM technology is substantially similar to any existing technologies and whether it meets the newness criterion.
Comment: We received multiple comments in support of the claim that GammaTile TM is not substantially similar to existing technologies. A commenter stated that GammaTile TM was designed to provide a fundamentally new mechanism, permitting cells within the targeted area surrounding the tumor excision cavity to receive therapeutic levels of radiation while eliminating hot spots that have occurred with traditional brachytherapy. Commenters stated that due to the consistency of construction and relative ease of placement, GammaTile TM would provide a promising therapeutic treatment to patients nationwide. The applicant also provided additional information to support its assertion that GammaTile TM meets the newness criterion. Specifically, the applicant stated that the GammaTileTM is the only brachytherapy implant device with an indication cleared by the U.S. FDA that specifies an indication for treating recurrent brain tumors. The applicant stated that it is the only brachytherapy implant device designed to realign and retarget radiation in a three-dimensional surgical excision using a new mechanism of action with the integration of a geometric spacer to offset the brachytherapy sources from the tissues. According to the applicant, this focused radiation therapy is not possible either with external-beam radiation therapy (EBRT) using photons, electrons, protons, or other forms of external beam radiation, or with other brachytherapy sources or delivery devices. The applicant also asserted that GammaTileTM should not be disqualified from new technology add-on payments due to having the same or similar mechanism of action because it is a type of radiation therapy. The applicant stated that many pharmaceutical technologies utilize similar microscopic chemical effects, yet may yield differing macroscopic effects, and have been considered to utilize new mechanisms of action. The applicant asserts that radiation therapy agents should be similarly evaluated, asserting that otherwise, it could be argued that there can be no new mechanisms of action for either drugs or radiation sources, and that such a conclusion would be inconsistent with Congressional intent and efforts to promote patient access to innovation, or the overall mission of CMS. The applicant stated that GammaTileTM provides a new mechanism of action when compared to existing technologies and this new mechanism plays a primary role in achieving the positive therapeutic outcomes seen in the clinical data.
Response: We appreciate the information provided by the applicant and commenters. After consideration of comments, we believe that the GammaTileTM mechanism of action is different from current forms of radiation therapy and brachytherapy as it is the first FDA cleared device to use a manufactured collagen matrix which offsets radiation sources for use for the treatment of recurrent intracranial neoplasms. Therefore, the GammaTileTM is not substantially similar to existing brachytherapy technology and meets the newness criterion.
With regard to the cost criterion, the applicant conducted the following analysis. The applicant worked with the Barrow Neurological Institute at St. Joseph's Hospital and Medical Center (St. Joseph's) to obtain actual claims from mid-2015 through mid-2016 for craniotomies that did not involve placement of the GammaTile TM technology. The cases were assigned to MS-DRGs 025 through 027 (Craniotomy and Endovascular Intracranial Procedures with MCC, with CC, and without CC/MCC, respectively). For the 460 claims, the average case-weighted unstandardized charge per case was $143,831. The applicant standardized the charges for each case and inflated each case's charges by applying the outlier charge inflation factor of 1.04205 included in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41718) by the age of each case (that is, the factor was applied to 2015 claims 3 times and 2016 claims 2 times). The applicant then calculated an estimate for ancillary charges associated with placement of the GammaTile TM device, as well as standardized charges for the GammaTile TM device itself. The applicant determined it meets the cost criterion because the final inflated average case-weighted standardized charge per case (including the charges associated with the GammaTile TM device) of $253,876 exceeds the average case-weighted threshold amount of $143,749 for MS-DRG 023, the MS-DRG that would be assigned for cases involving the GammaTile TM device.
As indicated in the proposed rule, the applicant also noted, in response to a concern expressed by CMS in the FY 2018 IPPS/LTCH PPS proposed rule, that its analysis does not include a reduction in costs due to reduced operating room times. The applicant stated that, while the use the device will reduce operating times relative to the freehand placement of seeds in other brain brachytherapy procedures, none of the claims in the cost analysis involve such freehand placement. We invited public comments on whether the GammaTile TM technology meets the cost criterion.
We received no comments on whether the GammaTile TM technology meets the cost criterion. Based on the analysis above, we believe that GammaTile TM meets the cost criterion.
With regard to substantial clinical improvement, the applicant stated that the GammaTile TM technology offers a treatment option for a patient population unresponsive to, or ineligible for, currently available treatments for recurrent CNS malignancies and significantly improves clinical outcomes when compared to currently available treatment options. The applicant explained that therapeutic options for patients who have been diagnosed with large or recurrent brain metastases are limited (for example, stereotactic radiotherapy, additional EBRT, or systemic immunochemotherapy). However, according to the applicant, the GammaTile TM technology provides a treatment option for patients who have been diagnosed with radiosensitive recurrent brain tumors that are not eligible for treatment with any other currently available treatment option. Specifically, the applicant stated that the GammaTile TM device may provide the only radiation treatment option for patients who have been diagnosed with tumors located close to sensitive vital brain sites (for example, brain stem) and patients who have been diagnosed with recurrent brain tumors who may not be eligible for additional treatment involving the use of external beam radiation therapy. There is a lifetime limit for the amount of radiation therapy a specific area of the body can receive. Patients whose previous treatment includes external beam radiation therapy may be precluded from receiving high doses of radiation associated with subsequent external beam radiation therapy, and the GammaTile TM technology can also be used to treat tumors that are too large for treatment with external beam radiation therapy. Patients who have been diagnosed with these large tumors are not eligible for treatment with external beam radiation therapy because the radiation dose to healthy brain tissue would be too high.
The applicant summarized how the GammaTileTM technology improves clinical outcomes compared to existing treatment options, including external beam radiation therapy and other forms of brain brachytherapy as: (1) Providing a treatment option for patients with no other available treatment options; (2) reducing the rate of mortality compared to alternative treatment options; (3) reducing the rate of radiation necrosis; (4) reducing the need for re-operation; (5) reducing the need for additional hospital visits and procedures; and (6) providing more rapid beneficial resolution of the disease process treatment.
The applicant cited several sources of data to support these assertions. The applicant referenced a paper by Brachman, Dardis et al., which was published in the Journal of Neurosurgery on December 21, 2018.[218] This study, a follow-up on the progress of 20 patients with recurrent previously irradiated meningiomasis, is a feasibility or superior progression-free survival study comparing the patient's own historical control rate against subsequent treatment with GammaTileTM.
An additional source of clinical data is from Gamma Tech's internal review of data from two centers treating brain tumors with GammaTileTM; the two centers are the Barrow Neurological Institute (BNI) at St. Joseph's Hospital and St. Joseph's Medical Center, Phoenix, AZ, and this internal review is referred to herein as the “BNI” study.[219] The BNI study summarized Gamma Tech's experience with the GammaTileTM technology. Another source of data that the applicant cited to support its assertions regarding substantial clinical improvement is an abstract by Pinnaduwage, D., et al. Also submitted in the application were abstracts from 2014 through 2018 in which updates from the progression-free survival study and the BNI study were presented at specialty society clinical conferences. The following summarizes the findings cited by the applicant to support its assertions regarding substantial clinical improvement.
Regarding the assertion of local control, the 2018 article which was published in the Journal of Neurosurgery found that, with a median follow-up of 15.4 months (range 0.03-47.5 months), there were 2 reported cases of recurrence out of 20 meningiomas, with median treatment site progression time after surgery and brachytherapy with the GammaTileTM precursor and prototype devices not yet being reached, compared to 18.3 months in prior instances. Median overall survival after resection and brachytherapy was 26 months, with 9 patient deaths. In a presentation at the Society for Neuro-Oncology in November 2014,[220] the outcomes of 20 patients who were diagnosed with 27 tumors covering a variety of histological types treated with the GammaTileTM prototype were presented. The applicant noted the following with regard to the patients: (1) All tumors were intracranial, supratentorial masses and included low and high-grade meningiomas, metastases from various primary cancers, high-grade gliomas, and others; (2) all treated masses were recurrent following treatment with surgery and/or radiation and the group averaged two prior craniotomies and two prior courses of external beam radiation treatment; and (3) following surgical excision, the prototype GammaTileTM were placed in the resection cavity to deliver a dose of 60 Gray to a depth of 5 mm of tissue; and (4) all patients had previously experienced regrowth of their tumors at the site of treatment and the local control rate of patients entering the study was 0 percent.
With regard to outcomes, the applicant stated that, after their initial treatment, patients had a median progression-free survival time of 5.8 months; post treatment with the prototype GammaTileTM, at the time of this analysis, only 1 patient had progressed at the treatment site, for a local control rate of 96 percent; and median progression-free survival time, a measure of how long a patient lives without recurrence of the treated tumor, had not been reached (as this value can only be calculated when more than 50 percent of treated patients have failed the prescribed treatment).
The applicant also cited the findings from Brachman, et al. to support local control of recurrent brain tumors. At the Society for Neuro-Oncology Conference on Meningioma in June 2016 [221] , a second set of outcomes on the prototype GammaTileTM was presented. This study enrolled 16 patients with 20 recurrent Grade II or III meningiomas, who had undergone prior surgical excision external beam radiation therapy. These patients underwent surgical excision of the tumor, followed by adjuvant radiation therapy with the prototype GammaTileTM. The applicant noted the following outcomes: (1) Of the 20 treated tumors, 19 showed no evidence of radiographic progression at last follow-up, yielding a local control rate of 95 percent; 2 of the 20 patients exhibited radiation necrosis (1 symptomatic, 1 asymptomatic); and (2) the median time to failure from the prior treatment with external beam radiation therapy was 10.3 months and after treatment with the prototype GammaTileTM only 1 patient failed at 18.2 months. Therefore, the median treatment site progression-free survival time after the prototype GammaTileTM treatment had not yet been reached (average follow-up of 16.7 months, range 1 to 37 months).
A third prospective study was accepted for presentation at the November 2016 Society for Neuro-Oncology annual meeting.[222] In this study, 13 patients who were diagnosed with recurrent high-grade gliomas (9 with glioblastoma and 4 with Grade III astrocytoma) were treated in an identical manner to the cases previously described. Previously, all patients had failed the international standard treatment for high-grade glioma, a combination of surgery, radiation therapy, and chemotherapy referred to as the “Stupp regimen.” For the prior therapy, the median time to failure was 9.2 months (range 1 to 40 months). After therapy with a prototype GammaTileTM, the applicant noted the following: (1) The median time to same site local failure had not been reached and 1 failure was seen at 18 months (local control 92 percent); and (2) with a median follow-up time of 8.1 months (range 1 to 23 months) 1 symptomatic patient (8 percent) and 2 asymptomatic patients (15 percent) had radiation-related MRI changes. However, no patients required re-operation for radiation necrosis or wound breakdown. Dr. Youssef was accepted to present at the 2017 Society for Neuro-Oncology annual meeting, where he provided an update of 58 tumors treated with the GammaTileTM technology. At a median whole group follow-up of 10.8 months, 12 patients (20 percent) had a local recurrence at an average of 11.33 months after implant. Six and 18 month recurrence free survival was 90 percent and 65 percent, respectively. Five patients had complications, at a rate that was equal to or lower than rates previously published for patients without access to the GammaTileTM technology.
In support of its assertion of a reduction in radiation necrosis, the applicant also included discussion of a presentation by D.S. Pinnaduwage, Ph.D., at the August 2017 annual meeting of the American Association of Physicists in Medicine. Dr. Pinnaduwage compared the brain radiation dose of the GammaTileTM technology with other radioactive seed sources. Iodine-125 and palladium-103 were substituted in place of the cesium-131 seeds. The study reported findings that other radioactive sources reported higher rates of radiation necrosis and that “hot spots” increased with larger tumor size, further limiting the use of these isotopes. The study concluded that the larger high-dose volume with palladium-103 and iodine-125 potentially increases the risk for radiation necrosis, and the inhomogeneity becomes more pronounced with increasing target volume. The applicant also cited a presentation by Dr. Pinnaduwage at the August 2018 annual meeting of the American Association of Physicists in Medicine, in which research findings demonstrated that seed migration in collagen tile implantations was relatively small for all tested isotopes, with Cesium-13 showing the least amount of seed migration.
The applicant asserted that, when considered in total, the data reported in these presentations and studies and the intermittent data presented in their abstracts support the conclusion that a significant therapeutic effect results from the addition of GammaTileTM radiation therapy to the site of surgical removal. According to the applicant, the fact that these patients had failed prior best available treatments (aggressive surgical and adjuvant radiation management) presents the unusual scenario of a salvage therapy outperforming the current standard-of-care. The applicant noted that follow-up data continues to accrue on these patients.
Regarding the assertion that GammaTileTM reduces mortality, the applicant stated that the use of the GammaTileTM technology reduces rates of mortality compared to alternative treatment options. The applicant explained that studies on the GammaTileTM technology have shown improved local control of tumor recurrence. According to the applicant, the results of these studies showed local control rates of 92 percent to 96 percent for tumor sites that had local control rates of 0 percent from previous treatment. The applicant noted that these studies also have not reached median progression-free survival time with follow-up times ranging from 1 to 37 months. Previous treatment at these same sites resulted in median progression-free survival times of 5.8 to 10.3 months.
The applicant further stated that the use of the GammaTileTM technology reduces rates of radiation necrosis compared to alternative treatment options. The applicant explained that the rate of symptomatic radiation necrosis in the GammaTileTM clinical studies of 5 to 8 percent is substantially lower than the 26 percent to 57 percent rate of symptomatic radiation necrosis requiring re-operation historically associated with brain brachytherapy, and lower than the rates reported for initial treatment of similar tumors with modern external beam and stereotactic radiation techniques. The applicant indicated that this is consistent with the customized and ideal distribution of radiation therapy provided by the GammaTileTM technology.
The applicant also asserted that the use of the GammaTileTM technology reduces the need for re-operation compared to alternative treatment options. The applicant explained that patients receiving a craniotomy, followed by external beam radiation therapy or brachytherapy, could require re-operation in the following three scenarios:
- Tumor recurrence at the excision site could require additional surgical removal;
- Symptomatic radiation necrosis could require excision of the affected tissue; and
- Certain forms of brain brachytherapy require the removal of brachytherapy sources after a given period of time.
However, according to the applicant, because of the high local control rates, low rates of symptomatic radiation necrosis, and short half-life of cesium-131, the GammaTileTM technology will reduce the need for re-operation compared to external beam radiation therapy and other forms of brain brachytherapy.
Additionally, the applicant stated that the use of the GammaTileTM technology reduces the need for additional hospital visits and procedures compared to alternative treatment options. The applicant noted that the GammaTileTM technology is placed during surgery, and does not require any additional visits or procedures. The applicant contrasted this improvement with external beam radiation therapy, which is often delivered in multiple fractions that must be administered over multiple days. The applicant provided an example where whole brain radiotherapy (WBRT) is delivered over 2 to 3 weeks, while the placement of the GammaTileTM technology occurs during the craniotomy and does not add any time to a patient's recovery.
Based on consideration of all of the previously presented data, the applicant believed that the use of the GammaTileTM technology represents a substantial clinical improvement over existing technologies. In the proposed rule, we stated a concern that the clinical efficacy and safety data provided by the applicant may be limited. We indicated that the findings presented appear to be derived from relatively small case-studies and not data from clinical trials conducted under an FDA-approved investigational device exemption application. We further stated that, while the applicant described increases in median time to disease recurrence in support of clinical improvement, we were concerned with the lack of analysis, meta-analysis, or statistical tests that indicated that seeded brachytherapy procedures represented a statistically significant improvement over alternative treatments, such as external beam radiation or other forms of brachytherapy. We also were concerned that many of the studies involved the use of prototype devices, and not the actual manufactured device. Finally, while the FDA cleared the 510(k) submission for GammaTileTM authorizing marketing of the device for the cleared indications for use, we noted in the proposed rule that the FDA's issuance of a “substantial equivalence determination” for the GammaTile did not indicate a review of any specific superiority claims to a predicate device.
We invited public comments on whether the GammaTileTM technology meets the substantial clinical improvement criterion.
Comment: Multiple commenters wrote in support that GammaTileTM meets the substantial clinical improvement criterion. A commenter stated that GammaTileTM provides a meaningful benefit to a vulnerable population of patients, and promises substantial clinical improvement over the management options currently available for the treatment of recurrent brain tumors. Another stated that there was growing evidence that that patients are living longer without tumor recurrence, and with less associated morbidity and an improved quality of life.
The applicant also provided additional information, including in response to several of CMS's concerns. First, they stated that the data are not limited and the data do not come from relatively small studies. The applicant stated that most of the clinical data come from a robust, comprehensive study. The applicant included a reference to its study, described on ClinicalTrials.gov under NCT03088579, which included 79 recurrent, previously irradiated intracranial neoplasms. The applicant clarified that over the course of previous submissions to CMS, they presented interim data which may have given the impression that the data came from smaller, disconnected studies, which was not the case. The applicant stated that they received two peer-reviewed awards for comprehensive clinical trial reporting on the treatment of 79 recurrent brain tumors treated with GammaTile.TM
The applicant noted CMS's statement that the data did not appear to come from “FDA approved trials” and CMS's statement that the FDA review did not indicate a review of superiority claims. The applicant responded that in its initial review of the GammaTileTM, the FDA required information regarding the effect of radiation exposure on the collagen tile and extensive animal model implant testing, including brain implantation, and that the applicant also provided to FDA information regarding the Gamma TileTM clinical trial data involving 79 consecutive recurrent brain tumors. The applicant further noted that the Gamma TileTM is the only brachytherapy implant device with an indication cleared or approved by the U.S. Food and Drug Administration that specifies an indication for treating recurrent brain tumors.
In response to CMS's concern as to whether additional analysis, meta-analysis, or statistical tests are needed to compare the GammaTileTM to other treatment modalities, such as external beam radiation or other forms of brachytherapy, the applicant commented that there is ample information and data available to conclude that the GammaTileTM is a substantial clinical improvement over existing options. The applicant stated that they collaborated with a biostatistics firm to advise to ensure the analysis of their data meets the highest standards. Specifically, they stated that in the clinical trial involving 79 recurrent brain tumors, each patient served as their own control. The applicant asserted that this minimized the potential influence of confounding variables such as age, gender, and treatment team. The clinical endpoints included time to tumor progression and survival, which the applicant states provided objective, clinically important measures. The median local control after GammaTileTM therapy versus prior treatment was 12.0 versus 9.5 months for high-grade glioma patients and 48.8 months versus 23.3 months for menigioma patients. For the metastasis patients, the median local control had not been reached versus 5.1 months with prior treatment. The median overall survival was 12.0 months for high grade glioma patients, 12.0 months for brain metastasis patients, and 49.2 months for the meningioma patients.
Additionally, the applicant pointed out that the majority of patients in the studies had failed a course of treatment that included external beam radiation. The applicant stated that most had already reached the maximum allowable amount of external beam radiation, and repeating more of the same treatment as a control arm could not be justified. The applicant reiterated that multiple studies demonstrated that GammaTileTM performed in a superior manner compared to adverse event rates for other therapies. In response to CMS's concern that studies were performed with prototype devices, not commercially-manufactured final products, the applicant stated that in the manufacturing process, the assembly of the GammaTileTM is reproduced to exacting specifications that are highly consistent with the process used with the prototype and from patient to patient.
Finally, the applicant provided study data with updated analysis of patient outcome data to CMS. The applicant provided a recent summary presentation on the 79 cases at The American Brachytherapy Society.[223] The applicant stated that these data demonstrate dramatic, clinically meaningful difference in Kaplan-Meier curves comparing time to local recurrence at same site in the same patients. The applicant stated that GammaTileTM is significantly outperforming the initial therapies attempted in this patient population and the pattern in findings is consistent across all three sub-groups of patients (recurrent meningiomas, recurrent gliomas, and recurrent brain metastases). The applicant stated that the data demonstrate reduced complication rates compared to external beam radiation and standard brachytherapy.
Response: After further review, CMS continues to have concerns with respect to whether GammaTileTM meets the substantial clinical improvement criterion to be approved for new technology add-on payments. In particular, we note that the study performed on 79 patients was a single-arm and single-institution study, where each patient functioned as their own control and the study goal was to compare the time to local recurrence after GammaTileTM treatment to the time of local recurrence after initial treatment of intracranial tumors. That is, the control arm were patients treated for initial intracranial brain tumors, and the treatment arm or the GammaTileTM treatment arm were the same control patients now experiencing local recurrent intracranial brain tumors in the same site with the same brain tumor type. In this clinical trial, the applicant compared the time from initial treatment to first local recurrence (control arm) vs. time from GammaTileTM treatment of first local recurrence to second local recurrence of the same brain tumor site and tumor type. Based on the data, there was no statistically significant difference between the control arm treatment and GammaTileTM treatment.
Additionally, the applicant also shared the data on the initial 20 of 79 patients which was published (Brachman D, Youssef E, Dardis CJ, et al. “Resection and permanent intracranial brachytherapy using modular, biocompatible cesium-131 implants: results in 20 recurrent, previously irradiated meningiomas” J Neurosurg Dec212018 pp1-10). The authors of this published article identified the following potential study limitations related to a single-arm, single-institution trial design: (1) Potential confounding, due to a lack of a control group, from the possibility that some tumors may have achieved local control due to repeat surgery alone and not necessarily from GammaTileTM intraoperative placement; (2) a lack of technical generalizability since all the initial patients were treated in a single center; and (3) reporting on a subset of a study's enrolled patients can either overestimate or underestimate the utility of the reported therapy. While we acknowledge the difficulty in establishing randomized control groups in studies involving recurrent brain tumors, after careful review of all data received to date, we find the data did not show a statistically significant difference between the time to first recurrence in the control arm in comparison to the time to second recurrence in the GammaTileTM treatment arm. Based on the information stated above, we are unable to make a determination that GammaTileTM technology represents a substantial clinical improvement over existing therapies. Therefore, we are not approving new technology add-on payments for the GammaTileTM for FY 2020.
k. JAKAFITM (ruxolitinib)
Incyte Corporation submitted an application for new technology add-on payments for JAKAFITM (ruxolitinib) for FY 2020. JAKAFITM is an oral kinase inhibitor that inhibits Janus-associated kinases 1 and 2 (JAK1/JAK2). The JAK pathway, which includes JAK1 and JAK2, is involved in the regulation of immune cell maturation and function. According to the applicant, JAK inhibition represents a novel therapeutic approach for the treatment of acute graft-versus-host disease (GVHD) in patients who have had an inadequate response to corticosteroids.
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a treatment option for patients who have been diagnosed with hematologic cancers, some solid tumors, and some non-malignant hematologic disorders. According to the applicant, approximately 9,000 allo-HSCTs were performed in the U.S. in 2017. The most common cause of death in allo-HSCT recipients within the first 100 days is relapsed disease (29 percent), infection (16 percent), and GVHD (9 percent).[224] GVHD is a condition where donor immunocompetent cells attack the host tissue. GVHD can be acute (aGVHD), which generally occurs prior to day 100, or chronic (cGVHD). aGVHD results in systemic inflammation and tissue destruction affecting multiple organs. Systemic corticosteroids are used as first-line therapy for the treatment of a diagnosis of aGVHD, with response rates between 40 percent and 60 percent. However, the response is often not durable, and there is no consensus on optimal second-line treatment.[225] The applicant stated that it envisioned the use of JAKAFITM as second-line treatment (that is, first-line steroid treatment failures) for the treatment of a diagnosis of steroid-refractory aGVHD.
In its application for new technology add-on payments, the applicant reported that there are no FDA-approved treatments for patients who have been diagnosed with steroid-refractory aGVHD, and despite available treatment options, according to the applicant, patients do not always achieve a positive response, underscoring the need for new and innovative treatments for these patients. The applicant states that patients who develop steroid-refractory aGVHD can progress to severe disease, with 1-year mortality rates of 70 to 80 percent. A number of combination treatment approaches are being investigated as second-line therapy in patients who have been diagnosed with steroid-refractory aGVHD, including methotrexate, mycophenolate mofetil, extracorporeal photopheresis, IL-2R targeting agents (basiliximab, daclizumab, denileukin, and diftitox), alemtuzumab, horse antithymocyte globulin, etancercept, infliximab, and sirolimus. According to the applicant, the American Society for Blood and Marrow Transplantation (ASBMT) does not provide any recommendations for second-line therapy for patients who have been diagnosed with steroid-refractory aGVHD, nor suggest avoidance of any specific agent.
JAKAFITM received FDA approval in 2011 for the treatment of patients who have been diagnosed with intermediate or high-risk myelofibrosis (MF). In addition, JAKAFITM received FDA approval in December 2014 for the treatment of patients who have been diagnosed with polycythemia vera (PV) who have had an inadequate response to, or are intolerant of hydroxyurea. JAKAFITM is primarily prescribed in the outpatient setting for these indications. The applicant submitted a supplemental new drug application (sNDA) (with Orphan Drug and Breakthrough Therapy designations) seeking FDA's approval for a new indication for JAKAFITM for the treatment of patients who have been diagnosed with steroid-refractory aGVHD who have had an inadequate response to treatment with corticosteroids and received FDA approval on May 24, 2019 for the treatment of steroid-refractory aGVHD in adult and pediatric patients 12 years and older [226 227] . The applicant asserts that for this new indication, JAKAFITM is expected to be used in the inpatient setting, during either hospital admission for allo-HSCT, or upon need for hospital re-admission for treating patients who have been diagnosed with aGVHD who have had an inadequate response to treatment with corticosteroids.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19347), we noted that the applicant submitted a request for approval for a unique ICD-10-PCS procedure code to describe procedures involving the administration of JAKAFITM beginning in FY 2020. The applicant was approved for an ICD-10-PCS code, XW0DXT5 (Introduction of ruxolitinib into mouth and pharynx, external approach, new technology group 5), effective October 1, 2019.
As previously stated, if a technology meets all three of the substantial similarity criteria as previously described, it would be considered substantially similar to an existing technology and, therefore, would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, the applicant asserts that there are no products that utilize the same or similar mechanism of action (that is, JAK inhibition) to achieve the same therapeutic outcome for the treatment of acute steroid-resistant GVHD. The applicant further explained that JAKAFITM functions to inhibit the JAK pathway, and has been shown in pre-clinical and clinical trials to reduce GVHD. The applicant explained that JAKs are intracellular, non-receptor tyrosine kinases that relay the signaling of inflammatory cytokines. The applicant stated that, based on their role in immune cell development and function, JAKs might affect all phases of aGVHD pathogenesis, including cell activation, expansion, and destruction. Specifically, JAKs regulate activities of immune cells involved in aGVHD etiology, including antigen-presenting cells, T-cells, and B-cells, and function downstream of many cytokines relevant to GVHD-mediated tissue damage. Inhibition of JAK1/JAK2 signaling in aGVHD could be expected to block signal transduction from proinflammatory cytokines that activate antigen-presenting cells, expansion and differentiation of T-cells, suppression of regulatory T-cells, and inflammation and tissue destruction mediated by infiltrating cytotoxic T-cells.[228] The applicant stated that other agents that are being investigated as second-line treatments for patients who have been diagnosed with steroid-resistant aGVHD, such as methotrexate, mycophenolate mofetil, extracorporeal photopheresis, IL-2R targeting agents (basiliximab, daclizumab, denileukin, and diftitox), alemtuzumab, horse antithymocyte globulin, etancercept, infliximab, and sirolimus, use a different mechanism of action than that of JAKAFITM. The applicant believes that the mechanism of action of JAKAFITM differs from that of existing technologies used to achieve the same therapeutic outcome.
With regard to the second criterion, whether a product is assigned to the same or a different MS-DRG, in its application for new technology add-on payments, the applicant asserted that there are currently no FDA-approved medicines for the treatment of patients who have been diagnosed with steroid-refractory aGVHD who have had an inadequate response to corticosteroids and, therefore, JAKAFITM would not be assigned to the same MS-DRG as existing technologies.
With respect to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, the applicant stated that there are no existing treatment options for patients who have been diagnosed with steroid-refractory aGVHD who have had an inadequate response to corticosteroids and, therefore, JAKAFITM represents a new treatment option for a patient population without existing or alternative options. The applicant stated that, based on its knowledge, there are no other prospective studies evaluating the effects of treatment with JAK inhibitors for the treatment of aGVHD in this patient population, and there are no FDA-approved agents for the treatment of patients who have been diagnosed with steroid-refractory aGVHD who have inadequately responded to treatment with corticosteroids.
For the reasons summarized in the proposed rule and in this final rule, the applicant maintained that JAKAFITM is not substantially similar to any existing technology. We noted in the proposed rule, however, that there are a number of available second-line treatment options for a diagnosis of aGVHD that treat the same patient population. We also noted that a number of these treatment options use a method of immunomodulation and suppress the body's immune response similar to the mechanics and goals of JAKAFITM and stated that, therefore, we believed that JAFAKITM may have a similar mechanism of action as existing therapies. Finally, we stated in the proposed rule that for patients receiving treatment involving any current second-line therapies for a diagnosis of steroid-refractory aGVHD, CMS would expect these patient cases to be generally assigned to the same MS-DRGs as a diagnosis for aGVHD, as would cases representing patients who may be eligible for treatment involving JAKAFITM. We invited public comments on whether JAKAFITM is substantially similar to any existing technologies, including with respect to the concerns we raised, and whether the technology meets the newness criterion.
Comment: In its public comment, the applicant stated that CMS is incorrectly comparing JAKAFITM to other therapies that treat similar patient populations and utilize the same MS-DRG for the diagnosis of aGVHD. They stated that JAKAFITM is the first and only FDA-approved medicine for the aGVHD patient population and has a novel mechanism of action that is distinct from the unapproved treatment options that attempt to suppress the body's immune response in patients with steroid-refractory aGVHD. Furthermore, they stated that JAKAFITM, a kinase inhibitor, inhibits Janus Associated Kinases (JAKs) JAK1 and JAK2, which mediate the signaling of a number of cytokines and growth factors that are important for hematopoiesis and immune function.[229] They also stated that JAK signaling involves recruitment of signal transducers and activators of transcription (STATs) to cytokine receptors, activation and subsequent localization of STATs to the nucleus leading to modulation of gene expression and that JAK-STAT signaling pathways play a key role in regulating the development, proliferation, and activation of several immune cell types important for GVHD pathogenesis. The commenter further stated that JAKAFITM has been extensively evaluated in preclinical models in steroid-refractory acute GVHD and that in a mouse model of acute GVHD, oral administration of JAKAFITM was associated with decreased expression of inflammatory cytokines in colon homogenates and reduced immune-cell infiltration in the colon. Additionally, they stated that in this study, significant improvements in body weight were observed in JAKAFITM-treated mice and that in the same mouse model, steroids were shown to not be as effective in ameliorating disease severity, as compared to JAKAFITM and steroid-treated animals had shown significant disease improvement upon switching to JAKAFITM. Lastly they stated that, treatment with JAKAFITM was shown to significantly enhance survival in the major histocompatibility (MHC)-mismatched mouse model of aGVHD as compared to vehicle control.
The applicant also asserted that MS-DRGs are broad payment groupings that are organized based on diagnosis and/or procedures performed during an inpatient hospitalization (for example, Allogeneic Bone Marrow Transplantation; Major Hematological and Immunological Diagnoses Except Sickle Cell Crisis and Coagulation Disorders) and that MS-DRGs do not provide a relevant means to determine newness. Per the applicant, the fact that JAKAFITM and the unapproved treatment options overlap in the same MS-DRG does not acknowledge the clinical benefit that JAKAFITM offers patients with aGVHD.
Another commenter expressed support for JAKAFITM. They stated that aGVHD remains the most important barrier to successful outcomes of an allogeneic stem cell transplant and that only ~50 percent of patients respond to corticosteroids. They stated that those who do not, have a 1 year mortality of ~70 percent to 80 percent. They also stated that prior to the FDA approval of JAKAFITM on May 24, 2019, this remained an unmet need since most of the available off-label therapies are non-targeted in their approach. They asserted that the mechanism of JAKAFITM is well-defined, and novel. They stated that none of the alternative “best available therapies”, which are all off-label, have a well-defined mechanism of action or targeted approach. Thus, the commenter believed that JAKAFITM represents a first-in kind approach to steroid-refractory acute GVHD and that it meets the threshold for “newness” as defined by CMS.
Response: We appreciate the commenters' input on whether JAKAFITM meets the newness criterion. Upon review of the public comments and the clinical information presented by the applicant, we agree with the commenters that JAKAFITM meets the newness criterion. As noted by the applicant, JAKAFITM inhibits JAK1 and JAK2, which mediate the signaling of a number of cytokines and growth factors that are important for hematopoiesis and immune function and these signaling pathways play a key role in regulating the development, proliferation, and activation of several immune cell types important for GVHD pathogenesis, whereby other treatments that are used for aGVHD suppress the body's immune response in patients with steroid-refractory aGVHD. We believe this is a unique mechanism of action and therefore JAKAFITM is not substantially similar to other drug therapies used to treat steroid-refractory aGVHD and may provide treatment options for certain patients with steroid-refractory aGVHD who have not responded to other therapies. We consider May 24, 2019 the beginning of the newness period for JAKAFITM.
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that the technology meets the cost criterion. To identify cases representing patients who may be eligible for treatment involving JAKAFITM, the applicant searched the FY 2017 MedPAR Limited Data Set (LDS) for cases reporting ICD-10-CM diagnosis codes for acute or unspecified GVHD in combination with either ICD-10-CM diagnosis codes for associated complications of bone marrow transplant or ICD-10-PCS procedure codes for transfusion of allogeneic bone marrow, as identified in this table. The applicant used this methodology to capture patients who developed aGVHD during their initial stay for allo-HSCT treatment, as well as those patients who were discharged and needed to be readmitted for a diagnosis of aGVHD.
The applicant submitted the following table displaying a complete list of the ICD-10-CM diagnosis codes and ICD-10-PCS procedure codes it used to identify cases representing patients who may be eligible for treatment with JAKAFITM.


The applicant identified a total of 210 cases mapping to MS-DRGs 014 (Allogeneic Bone Marrow Transplant), 808 (Major Hematological and Immunological Diagnoses except Sickle Cell Crisis and Coagulation Disorders with MCC), 809 (Major Hematological and Immunological Diagnoses except Sickle Cell Crisis and Coagulation Disorders with CC), and 871 (Septicemia or Severe Sepsis without MV > 96 hours with MCC). The applicant indicated that, because it is difficult to determine the realistic amount of drug charges to be replaced or avoided as a result of the use of JAKAFITM, it provided two scenarios to demonstrate that JAKAFITM meets the cost criterion. In the first scenario, the applicant removed 100 percent of pharmacy charges to conservatively estimate the charges for drugs that potentially may be replaced or avoided by the use of JAKAFITM. The applicant then standardized the charges and applied a 2-year inflation factor of 8.864 percent, which is the same inflation factor used by CMS to update the outlier threshold in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41722). (In the proposed rule, we noted that this figure was revised in the FY 2019 IPPS/LTCH PPS final rule correction notice. The corrected final 2-year inflation factor is 1.08986 (83 FR 49844).) The applicant then added charges for JAKAFITM to the inflated average case-weighted standardized charges per case. No other related charges were added to the cases.
Under the assumption of 100 percent of historical drug charges removed, the applicant calculated the inflated average case-weighted standardized charge per case to be $261,512 and the average case-weighted threshold amount to be $172,493. Based on this analysis, the applicant believed that JAKAFITM meets the cost criterion because the inflated average case-weighted standardized charge per case exceeds the average case-weighted threshold amount.
As noted in the proposed rule and this final rule, the applicant also submitted a second scenario to demonstrate that JAKAFITM meets the cost criterion. The applicant indicated that removing all charges for previous technologies as demonstrated in the first scenario is unlikely to reflect the actual case because many drugs are used in treating a diagnosis of aGVHD, especially during the initial bone marrow transplant. Therefore, the applicant also provided a sensitivity analysis where it did not remove any pharmacy charges or any other historical charges, which it indicated could be a more realistic assumption. Under this scenario, the final average case-weighted standardized charge per case is $377,494, which exceeds the average case-weighted threshold amount of $172,493. The applicant maintained that JAKAFITM also meets the cost criterion under this scenario.
We invited public comments on whether JAKAFITM meets the cost criterion.
Comment: The applicant submitted a revised analysis of the two scenarios used to demonstrate that JAKAFITM meets the cost criterion. The applicant used a 2-year inflation factor of 1.08986 from the FY 2019 IPPS/LTCH PPS final rule correction notice to inflate the charges in both scenarios from FY 2017 to FY 2019. The applicant also added charges for the new technology. Under the first scenario, in which 100 percent of pharmacy charges were removed, the inflated average case-weighted standardized charge per case increased from $261,512 to $263,002. Under the second scenario, in which the applicant did not remove any pharmacy charges, the inflated average case-weighted standardized charge per case increased from $377,494 to $379,114. Based on this revised analysis, for both scenarios, the applicant determined that the inflated average case-weighted standardized charge per case for JAKAFITM exceeds the average case-weighted threshold amount of $172,493, and that JAKAFITM meets the cost criterion.
Response: We appreciate the applicant's input and additional analysis. After consideration of the public comments we received, we agree with the applicant that JAKAFITM meets the cost criterion.
With respect to the substantial clinical improvement criterion, in its application for new technology add-on payments, the applicant asserted that JAKAFITM represents a substantial clinical improvement because: (1) The technology offers a treatment option for a patient population previously ineligible for treatments because JAKAFITM would be the first FDA-approved treatment option for patients who have been diagnosed with GVHD who have had an inadequate response to corticosteroids; and (2) use of the technology significantly improves clinical outcomes in patients with steroid-refractory aGVHD, which the applicant asserts is supported by the results from REACH1, a prospective, open-label, single-cohort Phase II study of the use of JAKAFITM, in combination with corticosteroids, for the treatment of Grade II to IV steroid-refractory aGVHD.
The applicant stated that there are very few prospective studies evaluating second-line therapy for a diagnosis of steroid-refractory aGVHD, and interpretation of these studies is hampered by the heterogeneity of the patient population, small sample sizes, and lack of standardization in the study design (including timing of the response, different response criteria, and absence of validated endpoints). Agents that have been investigated over the last 2 decades in these studies include low-dose methotrexate, mycophenolate mofetil, extracorporeal photopheresis, IL-2R targeting (that is, basiliximab, daclizumab, denileukin, and diftitox), alemtuzumab, horse antithymocyte globulin, etanercept, infliximab, and sirolimus. The applicant stated that second-line treatments, especially those associated with suppression of T-cells, are associated with increased infection and viral reactivation (including cytomegalovirus (CMV), Epstein-Barr virus, human herpes virus 6, adenovirus, and polyoma). Numerous combination approaches (for example, antibodies directed against IL-2 receptor, mammalian target of rapamycin inhibitors, or other immunosuppressive agents) also have been studied for the treatment of steroid-refractory aGVHD, but the applicant indicated that data do not support the recommendation or exclusion of any particular regimen. The applicant also asserted that such treatment combination approaches have been associated with significant toxicities, high failure rates, and an average 6-month survival rate of 49 percent.[230] Therefore, the applicant maintains that therapeutic options are limited for patients who are refractory to corticosteroid treatment for a diagnosis of aGVHD.
The applicant asserted that the clinical benefit of the use of JAKAFITM in patients who have been diagnosed with steroid-refractory aGVHD is supported by the results from five clinical studies, including a mixture of prospective and retrospective studies.
The first study is REACH1, a prospective, open-label, single-cohort Phase II study of the use of JAKAFITM, in combination with corticosteroids, for the treatment of Grade II to IV steroid-refractory aGVHD. REACH1 included 71 patients who had been diagnosed with steroid-refractory aGVHD. Included eligible patients were those that were 12 years old or older, had undergone at least one allogeneic hematopoietic stem cell transplantation from any donor source and donor type and were diagnosed with Grade II to IV steroid-refractory aGVHD, and presented evidence of myeloid engraftment. The patients' median age was 58 years old (ages 18 years old to 73 years old); 66 patients were white and 36 patients were female. The majority of patients had peripheral blood stem cells as the graft source (57 patients or 80.3 percent). The starting dose of JAKAFITM was 5 mg twice daily (BID). The dose could be increased to 10 mg BID after 3 days, if hematologic parameters were stable and in the absence of any treatment-related toxicities. Methylprednisolone (or prednisone equivalent) was administered at a starting dose of 2 mg/kg/day on the first day of treatment and tapered as appropriate. Patients receiving calcineurin inhibitors or other medications for GVHD prophylaxis were permitted to continue at the investigator's discretion. The primary endpoint was overall response rate (ORR) at Day 28, which the applicant indicated has been shown to be predictive of non-relapse mortality (NRM). No description of the statistical methods used in the REACH1 study was provided by the applicant.
The applicant stated that the ORR at Day 28 was achieved by 54.9 percent of patients; nearly half (48.7 percent) of the responding patients achieved a complete response (CR). The best ORR was 73.2 percent. Median time to first response for all responders was 7 days. Median duration of response was 345 days for both Day 28 responders (lower limit, 159 days) and for other responders (lower limit, 106 days). Event-free probability estimates for Day 28 responders at 3 and 6 months were 81.6 percent and 65.2 percent, respectively. Among all patients, median (95 percent CI) overall survival was 232.0 (93.0-not evaluable) days. Mean survival rates for the 39 responders at Day 28 were 73.2 percent at 6 months, 69.9 percent at 9 months, and 66.2 percent at 12 months with non-relapsed mortality of 21.2 percent at 6 months, 24.5 percent at 9 months, and 28.2 percent at 12 months. Mean survival rates for the 13 other responders were 35.9 percent at 6 and 9 months and were not evaluable at 12 months with non-relapsed mortality at 64.1 percent at 6 and 9 months and not evaluable at 12 months. Mean survival rates for non-responders were 15.8 percent at 6 months and 10.5 percent at 9 months and 12 months with non-relapsed mortality at 78.9 percent at 6 months and 84.2 percent at 9 and 12 months. Most patients (55.8 percent) had a greater than or equal to 50 percent reduction from baseline in corticosteroid dose.
The applicant stated that the additional use of JAKAFITM to corticosteroid-based treatment did not result in unexpected toxicities or exacerbation of known toxicities related to high-dose corticosteroids or aGVHD. Cytopenias were among the most common treatment-emergent adverse events. The applicant indicated that JAKAFITM was well tolerated, and the adverse event profile was consistent with the observed safety profiles of the use of JAKAFITM and that of patients who had been diagnosed with steroid-refractory aGVHD. The most common treatment emergent adverse events in the REACH1 study were anemia (64.8 percent), hypokalemia (49.3 percent), peripheral edema (45.1 percent), decreased platelet count (45.1 percent), decreased neutrophil count (39.4 percent), muscular weakness (33.8 percent), dyspnea (32.4 percent), hypomagnesaemia (32.4 percent), hypocalcemia (31 percent), and nausea (31 percent). The most common treatment emergent infections were sepsis (12.7 percent) and bacteremia (9.9 percent).
All patients who had a CMV event (n=14) had a positive CMV donor or recipient serostatus or both at baseline. No deaths were attributed to CMV events. The applicant asserted that the results of the prospective REACH1 study demonstrate the potential of the use of JAKAFITM to meaningfully improve the outcomes of allo-HSCT patients who develop steroid-refractory aGVHD, and further underscore the promise of JAK inhibition to advance the treatment of this potentially-devastating condition. Longer term follow-up analyses from REACH1 are expected to yield additional insights into the long-term efficacy and safety profile of the use of JAKAFITM in this patient population.
In a second prospective, open-label study, 14 patients who had been diagnosed with acute or chronic GVHD that were refractory to corticosteroids and at least 2 other lines of treatment were treated with JAKAFITM at a dose of 5 mg twice a day and increased to 10 mg twice a day. Of the 14 patients, 13 responded with respect to clinical GVHD symptoms and serum levels of pro-inflammatory cytokines. Three patients with histologically-proven acute skin or intestinal GVHD Grade I, achieved a CR. One non-responder discontinued use of JAKAFITM after 1 week because of lack of efficacy. In all other patients, corticosteroids could be reduced after a median treatment period of 1.5 weeks. CMV reactivation was observed in 4 out of the 14 patients, and they responded well to antiviral therapy. Until last follow-up, no patient experienced a relapse of GVHD.
The applicant asserted that the efficacy and safety of the use of JAKAFITM for the treatment of steroid-refractory aGVHD is further supported by the results from a third study, a retrospective, multi-center study of 95 patients who received JAKAFITM as salvage therapy for corticosteroid-refractory GVHD. In the 54 patients who had been diagnosed with aGVHD, the median number of GVHD therapies received was 3. The (best) ORR was 81.5 percent. A CR and partial response (PR) was achieved in 46.3 percent and 35.2 percent of patients, respectively. Median time to response was 1.5 weeks (range 1 to 11 weeks). Cytopenias and cytomegalovirus reactivation were seen in 55.5 percent (Grade III or IV) and 33.3 percent of patients who had been diagnosed with aGVHD, respectively. Of those patients responding to treatment with JAKAFITM, with either CR or PR (n=44), the rate of GVHD-relapse was 6.8 percent (3/44). The 6-month-survival was 79 percent (67.3 percent to 90.7 percent, 95 percent CI). The median follow-up time was 26.5 weeks (range 3 to 106 weeks). Underlying malignancy relapse occurred in 9.2 percent of patients who had been diagnosed with aGVHD.
A fourth retrospective study evaluated data from the same 95 patients in 19 stem cell transplant centers in Europe and the United States. For long-term results, CR was defined as the absence of any symptoms related to GVHD; PR was defined as the improvement of greater than or equal to 1 in stage severity in one organ, without deterioration in any other organ. A response had to last for at least or more than 3 weeks. Of the 54 patients who had been diagnosed with aGVHD, the 1-year overall survival (OS) rate was 62.4 percent (CI: 49.4 percent to 75.4 percent). The estimated median OS (50 percent death) was 18 months for aGVHD patients. The median duration of JAKAFITM treatment was 5 months. At follow-up, 22/54 (41 percent) of the patients had an ongoing response and were free of any immunosuppression. Cytopenias (any grade) and CMV-reactivation were observed during JAKAFITM-treatment (30/54, 55.6 percent and 18/54, 33.3 percent, respectively).
A fifth retrospective study evaluated 79 patients who received treatment using JAKAFITM for refractory GVHD at 13 centers in Spain. Twenty-two patients had a diagnosis of aGVHD (Grades II to IV) and received a median of 2 previous GVHD therapies (range, 1 to 5 therapies). The median daily dose of JAKAFITM was 20 mg. The overall response rate was 68.2 percent, which was obtained after a median of 2 weeks of treatment, and 18.2 percent (4/22) of the patients reached CR. Overall, steroid doses were tapered in 72 percent of the patients who had been diagnosed with aGVHD. Cytomegalovirus reactivation was reported in 54.5 percent of the patients who had been diagnosed with aGVHD. Overall, 26 patients (32.9 percent) discontinued treatment using JAKAFITM due to: Lack of response (14), cytopenias (3 patients had thrombocytopenia, 3 had anemia, and 3 had both); infections (1 patient); other causes (2 patients). Ten deaths occurred in patients who had been diagnosed with aGVHD.
In the proposed rule, we noted the following concerns with respect to whether JAKAFITM represents a substantial clinical improvement. First, we stated that while the applicant has submitted data from several clinical studies to support the efficacy of the use of JAKAFITM in treatment of patients who have been diagnosed with steroid-resistant aGVHD, including an overall response rate at Day 28 for 54.9 percent of the patients enrolled in one study, with nearly half of the responding patients achieving CR, the applicant has not provided any data directly comparing the use of JAKAFITM to any second-line treatments. As noted previously in the proposed rule and this final rule, a number of different agents can be used for second-line treatment as described by recommendations from the American Society of Blood and Marrow Transplantation (ASBMT).[231] Numerous combination approaches have been investigated for second-line therapy for diagnoses of steroid-refractory aGVHD in allo-HSCT patients. These studied agents include methotrexate, mycophenolate mofetil, extracorporeal photopheresis, IL-2R targeting agents (basiliximab, daclizumab, denileukin, and diftitox), alemtuzumab, horse antithymocyte globulin, etancercept, infliximab, and sirolimus. In addition, we stated that recommendations from professional societies for the treatment of diagnoses of aGVHD describe the lack of data demonstrating superior efficacy of any single agent as second-line therapy for patients who have been diagnosed with steroid-resistant aGVHD and, therefore, suggest that choice of second-line treatment be guided by clinical considerations.[232] We stated that, because the applicant has not provided any data directly comparing the use of JAKAFITM to any other second-line treatments (for example, current standard-of-care), it may make it difficult to directly assess whether the use of JAKAFITM provides a substantial clinical improvement compared to these existing therapies.
Second, we stated that we have concerns regarding the methodologic approach of the studies submitted by the applicant in support of its assertions regarding substantial clinical improvement. While two of the clinical studies provided by the applicant are prospective in nature, the other three clinical studies provided in support of the application are retrospective studies and, therefore, provide a weaker basis of evidence for making conclusions of the causative effects of the drug compared to prospective studies. Additionally, we noted that no blinding or randomization occurred to minimize potential biases from the lack of a control group, and no Phase III study data were submitted by the applicant, to assist in our evaluation of substantial clinical improvement. Although we acknowledged that the patient population that would be eligible for treatment involving JAKAFITM under its proposed indication is likely relatively small because it is a subset of the patient population receiving allo-HSCTs, we stated that it may be difficult to evaluate the impact of the technology on longer term outcomes, such as overall survival and durability of response based on the studies submitted because the clinical studies are based on relatively small sample sizes.
Third, we stated that given the variable amount of detail provided on the studies generally (for example, the number of patients from the United States, how many are Medicare eligible and the results for these Medicare-eligible patients, what specific first-line treatments enrolled patients received and for what duration, how CRs and PRs were defined and assessed, statistical methods and assumptions), it was more difficult to fully assess the generalizability of the applicant's assertions to the Medicare population.
Fourth, we noted that several patients enrolled in each of the studies provided by the applicant had safety-related complications, including cytopenias and CMV reactivation. We stated that these complications were concerning because the target population is already immunocompromised and at risk of serious infections.
We invited public comments on whether JAKAFITM meets the substantial clinical improvement criterion, including with respect to the concerns we raised.
Comment: The applicant submitted a comment addressing our concerns regarding substantial clinical improvement as indicated in the proposed rule. With respect to our concern that the applicant did not provide any data directly comparing the use of JAKAFITM to any second-line treatments, the applicant stated that no head-to-head, multicenter, randomized, well-controlled studies have been carried out to assess the efficacy and safety of second-line therapy for aGVHD and that clinicians rely on reports of retrospective studies and single-arm phase II studies to evaluate the merits of any given treatment [233] . They stated that comparison of results between these studies is complicated by the lack of standardized endpoints and the small numbers of patients included in most reports.
With respect to our concern regarding the methodologic approach of the studies submitted by the applicant in support of its assertions regarding substantial clinical improvement, the applicant stated that the FDA granted JAKAFITM Breakthrough Therapy Designation and Priority Review for aGVHD and asserted that these designations indicate that the FDA believes the product offers a significant and substantial clinical improvement when compared to standard therapies. The applicant also referred to the prospective, open-label, single-arm, multicenter, pivotal study (REACH1) that was the basis for the FDA's approval of JAKAFITM for treatment of steroid-refractory acute GVHD in adults and pediatric patients 12 years and older. The applicant reiterated that the primary endpoint in the REACH1 study was Day 28 overall response rate (ORR) (complete response, very good partial response or partial response) as defined by Center for International Blood and Marrow Transplant Research (CIBMTR) criteria, and that the ORR at Day 28 in the patients who were refractory to steroids alone and evaluable for efficacy was 57.1 percent (28/49). The applicant stated that the majority of these 28 patients had achieved a CR (53.6 percent, 15/28) and that Day 28 ORR was 100 percent for Grade II aGVHD, 40.7 percent for Grade III aGVHD, and 44.4 percent for Grade IV2 aGVHD.
The applicant also stated that the key secondary endpoint in REACH1 was duration of response. The duration of response, at the time of the 3-month data cutoff, was calculated using two measures:
- From Day-28 response to progression, new salvage therapy for acute GVHD or death from any cause (with progression being defined as worsening by one stage in any organ without improvement in other organs in comparison to prior response assessment). The median duration of response by this definition was 16 days (95 percent CI 9, 83).
- From Day-28 response to either death or need for new therapy for aGVHD (additional salvage therapy or increase in steroids). The median duration of response by this definition was 173 days (95 percent CI 66, NE).
The applicant further stated that, as described in its initial application, patients who develop steroid-refractory aGVHD can progress to severe disease, with 1-year mortality rates of 70-80 percent; the weighted average 6-month survival estimate across 25 studies that reported 6-month overall survival was 49 percent; the overall distribution of 6-month survival rates was similar for prospective and retrospective studies; the largest study tested horse antithymocyte globulin (ATG) in 79 patients, and reported a 6-month survival estimate of 44 percent; and hence, this study has previously been used as a reference point for the interpretation of survival results in other studies.
With respect to our concerns about the generalizability of the applicant's assertions to the Medicare population, the applicant stated that of the 49 patients that were evaluable for efficacy, the mean age was 57 (range, 18-72 years). They also stated that the exploratory subgroup analysis shows that 12 percent were of Medicare-eligible age (that is, ≥ 65 years) and that the exploratory subgroup analysis showed that JAKAFITM demonstrates clinical activity across patients <65 and ≥ 65 years. Lastly they stated that of all patients enrolled in REACH1 (n = 71), 18 percent were of Medicare-eligible age, and is supportive of the Medicare patient population of 25 percent estimated in their new technology add-on payment application.
Finally, with respect to our concern that several patients enrolled in each of the studies provided by the applicant had safety-related complications, including cytopenias and CMV reactivation, which is concerning because the target population is already immunocompromised and at risk of serious infections, the applicant stated that in the REACH1 study, the adverse event profile was consistent with the observed safety profiles of JAKAFITM and that of patients with steroid-refractory acute GVHD. They also stated that hematologic laboratory abnormalities were evaluated in the REACH1 study during JAKAFITM treatment and based on laboratory parameters, all grade anemia, thrombocytopenia, and neutropenia were reported in 75 percent, 75 percent, and 58 percent of patients, respectively. They also presented the following information: Anemia, thrombocytopenia, and neutropenia were reported as Grade 3 or 4 (worst grade during treatment) in 45 percent, 61 percent, and 40 percent of patients, respectively; treatment-emergent cytopenias led to discontinuation of Jakafi in 2 patients; infections occurred in 55 percent of enrolled patients, with 41 percent being Grade 3/4 in severity; infections led to treatment discontinuation in 10 percent of patients; related to cytomegalovirus (CMV), all patients who had a CMV event (n = 14, 19.7%; includes CMV infection [n = 10, 14.1%] and recurrent CMV viremia [n = 4, 5.6%]) had a positive CMV donor or recipient serostatus or both at baseline. They stated that no deaths were attributed to CMV events in the study.
Another commenter stated that steroid-refractory aGVHD has a dismal outcome with currently “best-available therapy” that are all off-label, and the 1 year survival rate of these patients is less than 20 percent to 30 percent. The commenter stated that in the REACH1 study, among the 49 patients evaluable for efficacy, the median survival was 333 days (95 percent CI, 93-NE) at the time of the 3-month data cutoff. The estimated 6-month and 12-month survival for Day 28 responders was 70.6 percent (95 percent CI, 47.3 percent-85 percent) for both time points. The commenter concluded that a significant proportion of patients are impacted favorably. Regarding the risk of infections, the commenter provided the following information: There is global immune dysfunction in patients with corticosteroid refractory acute GVHD; in the setting of a clinical trial for this subset of patients, it is tough to assess the impact of the intervention versus the baseline risk of infection; and in the REACH-1 study, it was noted that there were no treatment emergent fatal events related to CMV, which is an important viral infection in patients undergoing allogeneic stem cell transplant. The commenter stated that as a clinical investigator, they believe that early intervention with JAKAFITM (in patients meeting criteria of steroid-refractory aGVHD) will further decrease the risk of global immune-dysfunction, and lead to further decrease in infection in responders, as clinicians will be able to spare corticosteroids.
Response: We appreciate the commenters' input. After consideration of the public comments we received, we agree that JAKAFITM is a treatment option which offers a substantial clinical improvement over standard therapies for patients who have been diagnosed with steroid-refractory aGVHD. We agree that current treatment options for patients with steroid-refractory aGVHD have a poor outcome and that the one year survival rate is not favorable. Additionally, the data cited by the applicant in its public comments from the Phase II REACH1 study demonstrated improved outcomes, including the following: Overall response rate at Day 28 in the patients who were refractory to steroids alone and evaluable for efficacy was 57.1 percent (28/49); the majority of the 28 patients who were refractory to steroids alone and evaluable for efficacy had achieved a CR (53.6 percent, 15/28); Day 28 ORR was 100 percent for Grade II aGVHD, 40.7 percent for Grade III aGVHD, and 44.4 percent for Grade IV2 aGVHD. In terms of safety, there were no treatment emergent fatal events related to CMV, which is an important viral infection in patients undergoing allogeneic stem cell transplant. Additionally, the REACH1 study included patients (18 percent) that were of Medicare-eligible age demonstrating the effectiveness of JAKAFITM in the Medicare population. Finally, the clinical information for JAKAFITM presented by the applicant demonstrates that certain patients with steroid-refractory aGVHD have better clinical outcomes than those who were not treated with JAKAFITM. Therefore, we believe that JAKAFITM meets the substantial clinical improvement criterion.
After consideration of the public comments we received, we have determined that JAKAFITM meets all of the criteria for approval of new technology add-on payments. Therefore, we are approving new technology add-on payments for JAKAFITM for FY 2020. Cases involving JAKAFITM that are eligible for new technology add-on payments will be identified by ICD-10-PCS procedure code XW0DXT5, Introduction of ruxolitinib into mouth and pharynx, external approach, new technology group 5. According to the applicant, JAKAFITM has a WAC of $13,111 for 60 tablets/30 day supply (or approximately $218.52) per tablet, and patients will take JAKAFITM orally, twice per day, with an anticipated duration of treatment of 14 days. Therefore, the total cost of JAKAFITM per patient is $6,118.56. Under § 412.88(a)(2 (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the costs of the new medical service or technology, or 65 percent of the amount by which the costs of the case exceed the MS-DRG payment. As a result, the maximum new technology add-on payment for a case involving the use of JAKAFITM is $3,977.06 for FY 2020.
l. Supersaturated Oxygen (SSO2) Therapy (DownStream® System)
TherOx, Inc. submitted an application for new technology add-on payments for Supersaturated Oxygen (SSO2) Therapy (the TherOx DownStream® System) for FY 2020. We note that the applicant previously submitted an application for new technology add-on payments for FY 2019, which was withdrawn prior to the issuance of the FY 2019 IPPS/LTCH PPS final rule. The DownStream® System is an adjunctive therapy that creates and delivers superoxygenated arterial blood directly to reperfused areas of myocardial tissue which may be at risk after an acute myocardial infarction (AMI), or heart attack. Per the FDA, SSO2 Therapy is indicated for the preparation and delivery of SuperSaturated Oxygen Therapy (SSO2 Therapy) to targeted ischemic regions perfused by the patient's left anterior descending coronary artery immediately following revascularization by means of percutaneous coronary intervention (PCI) with stenting that has been completed within 6 hours after the onset of anterior acute myocardial infarction (AMI) symptoms caused by a left anterior descending artery infarct lesion. The applicant stated that the net effect of the SSO2 Therapy is to reduce the size of the infarction and, therefore, lower the risk of heart failure and mortality, as well as improve quality of life for STEMI patients.
SSO2 Therapy consists of three main components: The DownStream® System; the DownStream cartridge; and the SSO2 delivery catheter. The DownStream® System and cartridge function together to create an oxygen-enriched saline solution called SSO2 solution from hospital-supplied oxygen and physiologic saline. A small amount of the patient's blood is then mixed with the SSO2 solution, producing oxygen-enriched hyperoxemic blood, which is delivered to the left main coronary artery (LMCA) via the delivery catheter at a flow rate of 100 ml/min. The duration of the SSO2 Therapy is 60 minutes and the infusion is performed in the catheterization laboratory. The oxygen partial pressure (pO2) of the infusion is elevated to ~1,000 mmHg, therefore providing oxygen locally to the myocardium at a hyperbaric level for 1 hour. After the 60-minute SSO2 infusion is complete, the cartridge is unhooked from the patient and discarded per standard practice. Coronary angiography is performed as a final step before removing the delivery catheter and transferring the patient to the intensive care unit (ICU).
The applicant for the SSO2 Therapy received premarket approval from the FDA on April 2, 2019. The applicant stated that use of the SSO2 Therapy can be identified by the ICD-10-PCS procedure codes 5A0512C (Extracorporeal supersaturated oxygenation, intermittent) and 5A0522C (Extracorporeal supersaturated oxygenation, continuous).
As discussed earlier, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments. The applicant identified three treatment options currently available to restore coronary artery blood flow in AMI patients. These options are fibronolytic therapy (plasminogen activators) with or without glycoprotein IIb/IIIa inhibitors, percutaneous coronary intervention (PCI) with or without stent placement, and coronary artery bypass graft (CABG). The applicant noted that all of these therapies restore blood flow at the macrovascular level by targeting the coronary artery thrombosis that is the direct cause of the AMI. The applicant also noted that PCI with stenting is the preferred treatment for STEMI patients. The applicant asserted that SSO2 Therapy is not substantially similar to these existing treatment options and, therefore, meets the newness criterion. In this final rule, as in the proposed rule, we summarize the applicant's assertions with respect to whether the SSO2 Therapy meets each of the three substantial similarity criteria.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, the applicant asserted that SSO2 Therapy is a unique therapy designed to deliver localized hyperbaric oxygen equivalent to the coronary arteries immediately after administering the standard-of-care, PCI with stenting. The applicant describes SSO2 Therapy's mechanism of action as two-fold: (1) First, the increased oxygen levels act to re-open the microcirculatory system within the infarct zone, which has experienced ischemia during the occlusion period, and (2) second, once the microcirculatory system is re-opened, the blood flow containing the additional oxygen re-starts metabolic processes within the stunned myocardium. According to the applicant, the net result is to reduce the extent of necrosis as measured by infarct size in the myocardium post-AMI and thereby improve left ventricular function, leading to improved patient outcomes. The applicant maintained that this mechanism of action is not comparable to that of any existing treatment because no other therapy has demonstrated an infarct size reduction over and above the routine delivery of PCI. As previously mentioned, the applicant asserted that currently available therapies restore blood flow at the macrovascular level by targeting the coronary artery thrombosis that is the direct cause of the AMI.
With respect to the second criterion, whether a product is assigned to the same or a different MS-DRG, the applicant reiterated that the standard procedure for treating patients with AMI is PCI with stent placement, and that these cases are typically assigned to MS-DRG 246 (Percutaneous Cardiovascular Procedures with Drug-Eluting Stent with MCC or 4+ Arteries/Stents), MS-DRG 247 (Percutaneous Cardiovascular Procedures with Drug-Eluting Stent without MCC), MS-DRG 248 (Percutaneous Cardiovascular Procedures with Non-Drug-Eluting Stent with MCC or 4+ Arteries/Stents), MS-DRG 249 (Percutaneous Cardiovascular Procedures with Non-Drug-Eluting Stent without MCC), MS-DRG 250 (Percutaneous Cardiovascular Procedures without Coronary Artery Stent with MCC), or MS-DRG 251 (Percutaneous Cardiovascular Procedures without Coronary Artery Stent without MCC). The applicant maintained that because no other technologies exist that can deliver localized hyperbaric oxygen in the acute care setting, SSO2 Therapy has no analogous MS-DRG assignment. However, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19353), we noted that potential cases that may be eligible for treatment involving SSO2 Therapy may be assigned to the same MS-DRG(s) as other cases involving PCI with stent placement also used to treat patients who have been diagnosed with AMI.
With respect to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, according to the applicant, the target patient population of SSO2 Therapy is patients who are receiving treatment after a diagnosis of AMI and specifically ST-segment elevation myocardial infarction (STEMI) where the anterior wall infarction impacts the left ventricle (LV). The applicant acknowledged that, because SSO2 Therapy is administered following completion of successful PCI, its target patient population includes a subset of patients with the same or similar type of disease process as patients treated with PCI with stent placement. However, the applicant also asserted that, while PCI with stenting achieves the goal of re-opening a blocked artery, SSO2 Therapy delivers localized hyperbaric oxygen to reduce the extent of the myocardial necrosis that occurs as a consequence of experiencing AMI. Therefore, the applicant believed that SSO2 Therapy offers a treatment option for a different type of disease than currently available treatments.
We invited public comments on whether SSO2 Therapy is substantially similar to existing technologies and whether it meets the newness criterion.
We did not receive any public comments on whether SSO2 Therapy is substantially similar to existing technologies and whether it meets the newness criterion. However, based on the information submitted by the applicant as part of its FY 2020 new technology add-on payment application for SSO2 Therapy, as discussed in the proposed rule (84 FR 19353) and as previously summarized in this final rule, we believe that SSO2 Therapy has a unique mechanism of action as it delivers a localized hyperbaric oxygen equivalent to the coronary arteries immediately after administering the standard-of-care, PCI with stenting, in order to restart metabolic processes within the stunned myocardium and reduce infarct size. Therefore, we believe SSO2 Therapy is not substantially similar to existing technologies and meets the newness criterion. We consider the beginning of the newness period to commence when SSO2 Therapy was approved by the FDA on April 2, 2019.
With regard to the cost criterion, the applicant conducted the following analysis to demonstrate that SSO2 Therapy meets the cost criterion. The applicant searched the FY 2017 MedPAR file for claims reporting diagnoses of anterior STEMI by ICD-10-CM diagnosis codes I21.0 (ST elevation myocardial infarction of anterior wall), I21.01 (ST elevation (STEMI) myocardial infarction involving left main coronary artery), I21.02 (ST elevation (STEMI) myocardial infarction involving left anterior descending coronary artery), or I21.09 (ST elevation (STEMI) myocardial infarction involving other coronary artery of anterior wall) as a primary diagnosis, which the applicant believed would describe potential cases representing potential patients who may be eligible for treatment involving the SSO2 Therapy. The applicant identified 11,668 cases mapping to 4 MS-DRGs, with approximately 91 percent of all potential cases mapping to MS-DRG 246 (Percutaneous Cardiovascular Procedures with Drug-Eluting Stent with MCC or 4+ Arteries/Stents) and MS-DRG 247 (Percutaneous Cardiovascular Procedures with Drug-Eluting Stent without MCC). The remaining 9 percent of potential cases mapped to MS-DRG 248 (Percutaneous Cardiovascular Procedures with Non-Drug-Eluting Stent with MCC or 4+ Arteries/Stents) and MS-DRG 249 (Percutaneous Cardiovascular Procedures with Non-Drug-Eluting Stent without MCC).
The applicant determined that the average case-weighted unstandardized charge per case was $98,846. The applicant then standardized the charges. The applicant did not remove charges for the current treatment because, as previously discussed, SSO2 Therapy would be used as an adjunctive treatment option following successful PCI with stent placement. The applicant then added charges for the technology, which accounts for the use of 1 cartridge per patient, to the average charges per case. The applicant did not apply an inflation factor to the charges for the technology. The applicant also added charges related to the technology, to account for the additional supplies used in the administration of SSO2 Therapy, as well as 70 minutes of procedure room time, including technician labor and additional blood tests. The applicant inflated the charges related to the technology. Based on the FY 2019 IPPS/LTCH PPS final rule correction notice data file thresholds, the average case-weighted threshold amount was $96,267. In the applicant's analysis, the inflated average case-weighted standardized charge per case was $144,364. Because the inflated average case-weighted standardized charge per case exceeds the average case-weighted threshold amount, the applicant maintained that the technology meets the cost criterion.
We invited public comments on whether the SSO2 Therapy meets the cost criterion.
We did not receive any public comments on whether SSO2 Therapy meets the cost criterion. Based on the information submitted by the applicant as part of its FY 2020 new technology add-on payment application for SSO2 Therapy, as discussed in the proposed rule (84 FR 19353 through 19354) and as previously summarized in this final rule, the average case-weighted standardized charge per case exceeded the average case-weighted threshold amount. Therefore, SSO2 Therapy meets the cost criterion.
With regard to the substantial clinical improvement criterion, the applicant asserted that SSO2 Therapy represents a substantial clinical improvement over existing technologies because it improves clinical outcomes for STEMI patients as compared to the currently available standard-of-care treatment, PCI with stenting alone. Specifically, the applicant asserted that: (1) Infarct size reduction improves mortality outcomes; (2) infarct size reduction improves heart failure outcomes; (3) SSO2 Therapy significantly reduces infarct size; (4) SSO2 Therapy prevents left ventricular dilation; and (5) SSO2 Therapy reduces death and heart failure at 1 year. The applicant highlighted the importance of the SSO2 Therapy's mechanism of action, which treats hypoxemic damage at the microvascular or microcirculatory level. Specifically, the applicant noted that microvascular impairment in the myocardium is irreversible and leads to a greater extent of infarction. According to the applicant, the totality of the data on myocardial infarct size, ventricular remodeling, and clinical outcomes strongly supports the substantial clinical benefit of SSO2 Therapy administration over the standard-of-care.
To support the claims that infarct size reduction improves mortality and heart failure outcomes, the applicant cited an analysis of the Collaborative Organization for RheothRx Evaluation (CORE) trial and a pooled patient-level analysis.
- The CORE trial was a prospective, randomized, double-blinded, placebo-controlled trial of Poloxamer 188, a novel therapy adjunctive to thrombolysis at the time the study was conducted.[234] The applicant sought to relate left ventricular ejection fraction (EF), end-systolic volume index (ESVI) and infarct size (IS), as measured in a single, randomized trial, to 6-month mortality after myocardial infarction treated with thrombolysis. According to the applicant, subsets of clinical centers participating in CORE also participated in one or two radionuclide sub-studies: (1) Angiography for measurement of EF and absolute, count-based LV volumes; and (2) single-photon emission computed tomographic sestamibi measurements of IS. These sub-studies were performed in 1,194 and 1,181 patients, respectively, of the 2,948 patients enrolled in the trial. Furthermore, ejection fraction, ESVI, and IS, as measured by central laboratories in these sub-studies, were tested for their association with 6-month mortality. According to the applicant, the results of the study showed that ejection fraction (n = 1,137; p = 0.0001), ESVI (n = 945; p=0.055) and IS (n = 1,164; p = 0.03) were all associated with 6-month mortality, therefore, demonstrating the relationship between these endpoints and mortality.[235]
- The pooled patient-level analysis was performed from 10 randomized, controlled trials (with a total of 2,632 patients) that used primary PCI with stenting.[236] The analysis assessed infarct size within 1 month after randomization by either cardiac magnetic resonance (CMR) imaging or technetium-99m sestamibi single-photon emission computed tomography (SPECT), with clinical follow-up for 6 months. Infarct size was assessed by CMR in 1,889 patients (71.8 percent of patients) and by SPECT in 743 patients (28.2 percent of patients) including both inferior wall and more severe anterior wall STEMI patients. According to the applicant, median infarct size (or percent of left ventricular myocardial mass) was 17.9 percent and median duration of clinical follow-up was 352 days. The Kaplan-Meier estimated 1-year rates of all-cause mortality, re-infarction, and HF hospitalization were 2.2 percent, 2.5 percent, and 2.6 percent, respectively. The applicant noted that a strong graded response was present between infarct size (per 5 percent increase) and the 2 outcome measures of subsequent mortality (Cox-adjusted hazard ratio: 1.19 [95 percent confidence interval: 1.18 to 1.20]; p<0.0001) and hospitalization for heart failure (adjusted hazard ratio: 1.20 [95 percent confidence interval: 1.19 to 1.21]; p<0.0001), independent of other baseline factors.[237] The applicant concluded from this study that infarct size, as measured by CMR or technetium-99m sestamibi SPECT within 1 month after primary PCI, is strongly associated with all-cause mortality and hospitalization for heart failure within 1 year.
Next, to support the claim that SSO2 Therapy significantly reduces infarct size, the applicant cited the AMIHOT I and II studies.
- The AMIHOT I clinical trial was designed as a prospective, randomized evaluation of patients who had been diagnosed with AMI, including both anterior and inferior patients, and received treatment with either PCI with stenting alone or with SSO2 Therapy as an adjunct to successful PCI within 24 hours of symptom onset.[238] The study included 269 randomized patients and 3 co-primary endpoints: Infarction size reduction, regional wall motion score improvement at 3 months, and reduction in ST segment elevation. The study was designed to demonstrate superiority of the SSO2 Therapy group as compared to the control group for each of these endpoints, as well as to demonstrate non-inferiority of the SSO2 Therapy group with respect to 30-day Major Adverse Cardiac Event (MACE). The applicant stated that results for the control versus SSO2 Therapy group comparisons for the three co-primary effectiveness endpoints demonstrated a nominal improvement in the test group, although this nominal improvement did not achieve clinical and statistical significance in the entire population. The applicant further stated that a pre-specified analysis of the SSO2 Therapy patients who were revascularized within 6 hours of AMI symptom onset and who had anterior wall infarction showed a marked improvement in all 3 co-primary endpoints as compared to the control group.[239] Key safety data revealed no statistically significant differences in the composite primary endpoint of 1-month (30 days) MACE rates between the SSO2 Therapy and control groups. MACE includes the combined incidence of death, re-infarction, target vessel revascularization, and stroke. In total, 9/134 (6.7 percent) of the patients in the SSO2 Therapy group and 7/135 (5.2 percent) of the patients in the control group experienced 30-day MACE (p = 0.62).[240]
- The AMIHOT II trial randomized 301 patients who had been diagnosed with and receiving treatment for anterior AMI with either PCI plus the SSO2 Therapy or PCI alone.[241] The AMIHOT II trial had a Bayesian statistical design that allows for the informed borrowing of data from the previously completed AMIHOT I trial. The primary efficacy endpoint of the study required proving superiority of the infarct size reduction, as assessed by Tc-99m Sestamibi SPECT imaging at 14 days post PCI/stenting, with the use of SSO2 Therapy as compared to patients who were receiving treatment involving PCI with stenting alone. The primary safety endpoint for the AMIHOT II trial required a determination of non-inferiority in the 30-day MACE rate, comparing the SSO2 Therapy group with the control group, within a safety delta of 6.0 percent.[242] Endpoint evaluation was performed using a Bayesian hierarchical model that evaluated the AMIHOT II result conditionally in consideration of the AMIHOT I 30-day MACE data. According to the applicant, the results of the AMIHOT II trial showed that the use of SSO2 therapy, together with PCI and stenting, demonstrated a relative reduction of 26 percent in the left ventricular infarct size and absolute reduction of 6.5 percent compared to PCI and stenting alone.[243]
Next, to support the claim that SSO2 Therapy prevents left ventricular dilation, the applicant cited the Leiden study, which represents a single-center, sub-study of AMIHOT I patients treated at Leiden University in the Netherlands. The study describes outcomes of randomized selective treatment with intracoronary aqueous oxygen (AO), the therapy delivered by SSO2 Therapy, versus standard care in patients who had acute anterior wall myocardial infarction within 6 hours of onset. Of the 50 patients in the sub-study, 24 received treatment using adjunctive AO and 26 were treated according to standard care after PCI, with no significant differences in baseline characteristics between groups. LV volumes and function were assessed by contrast echocardiography at baseline and 1 month. According to the applicant, the results demonstrated that treatment with aqueous oxygen prevents LV remodeling, showing a reduction in LV volumes (3 percent decrease in LV end-diastolic volume and 11 percent decrease in LV end-systolic volume) at 1 month as compared to baseline in AO-treated patients, as compared to increasing LV volumes (14 percent increase in LV end diastolic volume and 18 percent increase in LV end-systolic volume) at 1 month in control patients.[244] The results also show that treatment using AO preserves LV ejection fraction at 1 month, with AO-treated patients experiencing a 10 percent increase in LV ejection fraction as compared to a 2 percent decrease in LV ejection fraction among patients in the control group.[245]
Finally, to support the claim that SSO2 Therapy reduces death and heart failure at 1 year, the applicant submitted the results from the IC- HOT clinical trial, which was designed to confirm the safety and efficacy of the use of the SSO2 Therapy in those individuals presenting with a diagnosis of anterior AMI who have undergone successful PCI with stenting of the proximal and/or mid left anterior descending artery within 6 hours of experiencing AMI symptoms. It is an IDE, nonrandomized, single arm study. The study primarily focused on safety, utilizing a composite endpoint of 30-day Net Adverse Clinical Events (NACE). A maximum observed event rate of 10.7 percent was established based on a contemporary PCI trial of comparable patients who had been diagnosed with anterior wall STEMI. The results of the IC-HOT trial exhibited a 7.1 percent observed NACE rate, meeting the study endpoint. Notably, no 30-day mortalities were observed, and the type and frequency of 30-day adverse events occurred at similar or lower rates than in contemporary STEMI studies of PCI-treated patients who had been diagnosed with anterior AMI.[246] Furthermore, according to the applicant, the results of the IC-HOT study supported the conclusions of effectiveness established in AMIHOT II with a measured 30-day median infarct size = 19.4 percent (as compared to the AMIHOT II SSO2 Therapy group infarct size = 20.0 percent).[247] The applicant stated that notable measures include 4-day microvascular obstruction (MVO), which has been shown to be an independent predictor of outcomes, 4-day and 30-day left ventricular end diastolic and end systolic volumes, and 30-day infarct size.[248] The applicant also stated that the IC-HOT study results exhibited a favorable MVO as compared to contemporary trial data, and decreasing left ventricular volumes at 30 days, compared to contemporary PCI populations that exhibit increasing left ventricular size.[249] The applicant asserted that the IC-HOT clinical trial data continue to demonstrate the substantial clinical benefit of the use of SSO2 Therapy as compared to the standard-of-care, PCI with stenting alone.
The applicant also performed controlled studies in both porcine and canine AMI models to determine the safety, effectiveness, and mechanism of action of the SSO2 Therapy.[250 251] According to the applicant, the key summary points from these animal studies are:
- SSO2 Therapy administration post-AMI acutely improves heart function as measured by left ventricular ejection fraction (LVEF) and regional wall motion as compared with non-treated control subjects.
- SSO2 Therapy administration post-AMI results in tissue salvage, as determined by post-sacrifice histological measurements of the infarct size. Control animals exhibit larger infarcts than the SSO2-treated animals.
- SSO2 Therapy has been shown to be non-toxic to the coronary arteries, myocardium, and end organs in randomized, controlled swine studies with or without induced acute myocardial infarction.
- SSO2 Therapy administration post-AMI has exhibited regional myocardial blood flow improvement in treated animals as compared to controls.
- A significant reduction in myeloperoxidase (MPO) levels in the SSO2-treated animals versus controls, which indicate improvement in underlying myocardial hypoxia.
- Transmission electron microscopy (TEM) photographs showing amelioration of endothelial cell edema and restoration of capillary patency in ischemic zone cross-sectional histological examination of the SSO2- treated animals, while non-treated controls exhibit significant edema and vessel constriction at the microvascular level.
In the proposed rule, we stated that we had the following concerns regarding whether the technology meets the substantial clinical improvement criterion. We noted that the standard-of-care for STEMI had evolved since the AMIHOT I and AMIHOT II studies were conducted, such that it is unclear whether use of SSO2 Therapy would demonstrate the same clinical improvement as compared to the current standard-of-care. We also noted that the AMIHOT II study used SPECT infarct size data 14 days post-MI for efficacy and MACE events (including death, re-infarction, revascularization, and stroke) by 30 days post-MI for safety. Therefore, we stated that we were concerned that there is no long-term data to demonstrate the validity of these statistics, and that infarct size has not been completely validated as a surrogate marker for the combination of PCI plus SSO2. With respect to the IC-HOT study, we stated that we were concerned that the lack of a control may limit the interpretation of the data. We also were concerned that the safety data (death, re-infarction, re-vascularization, stent thrombosis, severe heart failure, and bleeding) for the IC-HOT study were limited to the 30 days post-MI, with no long-term data being available.
We invited public comments on whether the SSO2 Therapy meets the substantial clinical improvement criterion, including with respect to whether the results of the AMIHOT I and AMIHOT II studies remain valid given the advancements in STEMI care since these trials were conducted, and the availability of long-term data to validate the efficacy and safety data of the AMIHOT II and IC-HOT studies.
Comment: Several commenters submitted comments regarding CMS's concerns about whether SSO2 Therapy meets the substantial clinical improvement criterion. Many of these commenters summarized the history of STEMI care, beginning with the first breakthrough of thrombolytic therapy followed by interventional procedures with balloon angioplasty and subsequent stenting of the coronary blockage, which became widely accepted as the standard of care. These commenters affirmed the relationship between myocardial infarct size and long term clinical outcomes such as heart failure, rehospitalization and mortality. Several commenters referenced the CORE trial in which the size of the measured infarct was directly correlated with the rates of 6-month death in 1,164 STEMI patients treated with thrombolytic therapy. The CORE trial found that every reduction in infarct size by an absolute 5 percent of the left ventricle correlated with a 17-18 percent improvement in survival). The commenters also referenced a recent meta-analysis of 2,632 patients from 10 randomized controlled trials with STEMI who underwent PCI and then had their infarct size measured within the next several days. The meta-analysis showed that myocardial infarction size was strongly associated with 1-year hospitalization for heart failure and all-cause mortality, and that for every 5 percent increase in MI size, there was a 20 percent increase in relative hazard ratio for 1-year hospitalization for heart failure and all-cause mortality. A commenter emphasized that the relationship between infarct size and outcomes is not dependent on the mode of therapy delivered during patient treatment; reduced infarct size, no matter how it is accomplished, has been associated with improved survival and reduced heart failure and rehospitalization.
With respect to the validity of the AMIHOT I and AMIHOT II studies given the advancements in STEMI care since the trials were conducted, the commenters believed that the treatment of STEMI patients had not changed since the AMIHOT II study was conducted, and that no new adjunct pharmacology or device had been proven clinically beneficial until SSO2 Therapy. Several commenters asserted that SSO2 Therapy is the first treatment (adjunctive or otherwise) in three decades of trials to significantly reduce myocardial infarct size and that it has not been superseded by any recent strategies or devices. Another commenter explained that the evolution in STEMI care since the advent of stenting can be attributed to improvement in the stents' material (for instance, the introduction of drug coating) and the organization of medical care, including reducing time from symptom onset to first medical contact, door-to-balloon time, total ischemic time, and improved antithrombotic therapy. The commenter acknowledged that these developments improved clinical outcomes and reduced mortality, but that they all occur in the clinical workflow prior to the therapeutic intervention, which has remained unchanged since the advent of drug-eluting stents. A commenter noted that short term 30 day mortality for STEMI patients has dropped steadily from 10-20 percent to under 5 percent with the latest generation drug eluting stents. However, another commenter pointed out that the mortality rate has not changed in recent years for STEMI treated with PCI. Another commenter noted that large infarctions still occur in spite of the advances in PCI, and that many therapies have failed to demonstrate better outcomes beyond that obtained from timely reperfusion alone.
A commenter stated that until the development of the SSO2 Downstream System there was no practicable method available for treating critically ill STEMI patients with hyperoxemic coronary perfusion. The commenter stated that even with rapid treatment of AMI itself by PCI, the infarct size and loss of heart muscle is often substantial, resulting in heart failure. The commenter also stated that numerous drugs and devices have been studied to reduce heart failure after STEMI, including fluosol, magnesium, RheothRx, trimetazidine, hSOD, cylexin, adenosine, anti-CD18 antibodies, eniporide, pexelizumab, tilarginine, EPO, sodium nitrate, cyclosporine, TRO40303, delcasertib, metformin, bendavia, aspiration thrombectomy, distal embolic protection, hypothermia, pre- and post-conditioning, cell therapy and others. According to the commenter, none have been convincingly effective, and most have been costly and have had side-effects.
With respect to the availability of long-term data to validate the efficacy and safety data of the AMIHOT II and IC-HOT studies, many of the commenters reiterated the results of these studies as presented in the original application and as previously summarized in this final rule. Specifically, the commenters highlighted (1) the 26 percent relative and 6.5 percent absolute reduction in median infarct size compared to the control group (p = 0.02) in the AMIHOT II study, and (2) the 0 percent mortality and 1 percent incidence of congestive heart failure at both 30 days and at 1 year in the IC-HOT study. A commenter noted that the relatively low, median infarct size by CMR at 30 days in the IC- HOT trial was nearly identical to the median value at 2 weeks by perfusion imaging in the AMIHOT II trial. The commenter stated that infarct size remained unchanged over the 30 day follow up period, and asserted that further changes in infarct size are therefore extremely unlikely. The same commenter noted that the very low percentage of microvascular occlusion that was found in the IC-HOT trial at day 30 also portends a favorable long term outcome.
Most commenters also referred to a formal analysis comparing the clinical outcomes in SSO2 treated patients to those of a case-matched historical control population. This analysis compared the 1-year clinical outcomes from the IC-HOT study to a propensity score-matched population from a similar patient cohort of high-risk anterior STEMI patients enrolled in the INFUSE-AMI trial (n=83 patients per arm for the matched analysis). Per the commenters, statistically significant reductions in mortality and heart failure were observed at one year post treatment. At 1 year after PCI, mortality was 7.6 percent in the control group from the INFUSE-AMI trial vs. 0.0 percent in the SSO2 therapy group (p = 0.01). Furthermore, new onset heart failure or heart failure readmissions occurred in 7.4 percent in the INFUSE-AMI group vs. 0.0 percent in the SSO2 Therapy group (p = 0.01). A commenter noted that because these results are non-randomized, were drawn from 2 separate studies, are from a modest number of patients, and the effect size is better than would be expected in a large trial (noting that no therapy will completely eliminate death and HF after anterior STEMI), they should be considered hypothesis generating. Nonetheless, the commenter stated that they do suggest long-term clinical improvement with SSO2 Therapy, consistent with the proven reduction in infarct size.
Response: We thank the commenters for their input. We appreciate the additional background on the evolution of STEMI care and agree with the commenters that infarct size can be strongly correlated with outcomes such as heart failure, rehospitalization, and mortality. We agree that the results of the AMIHOT I, AMIHOT II, and IC-HOT studies are promising and suggest the potential for long term clinical improvement with SSO2 Therapy consistent with the reduction in infarct size demonstrated by imaging. However, we are uncertain if the clinical improvement seen in these studies is necessarily a result of infarct size reduction after SSO2 Therapy use, or other developments in STEMI care delivery. That is, it is unclear, based on the information provided, the incremental effect of SSO2 Therapy on clinical outcomes as compared to the current standard of care, PCI with stenting but without the SSO2 Therapy as an adjunctive treatment.
After consideration of all the information from the applicant, as well as the public comments we received, we are unable to determine that SSO2 Therapy represents a substantial clinical improvement over the currently available therapies used to treat STEMI patients. We remain concerned that the current data does not adequately support a sufficient association between the outcome measures of heart failure, rehospitalization, and mortality with the use of SSO2 Therapy specifically to determine that the technology represents a substantial clinical improvement over existing available options. Therefore, we are not approving new technology add-on payments for SSO2 Therapy for FY 2020.
m. T2Bacteria® Panel (T2 Bacteria Test Panel)
T2 Biosystems, Inc. submitted an application for new technology add-on payments for the T2 Bacteria Test Panel (T2Bacteria® Panel) for FY 2020. According to the applicant, the T2Bacteria® Panel is indicated as an aid in the diagnosis of bacteremia, bacterial presence in the blood which is a precursor for sepsis. Per the FDA cleared indication, results from the T2Bacteria Panel are not intended to be used as the sole basis for diagnosis, treatment, or other patient management decisions in patients with suspected bacteremia. Concomitant blood cultures are necessary to recover organisms for susceptibility testing or further identification, and for organisms not detected by the T2Bacteria Panel. However, the applicant noted that the T2 Bacteria Panel is a multiplex diagnostic panel that detects five major bacterial pathogens (Enterococcus faecium, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Staphylococcus aureus) associated with sepsis. According to the applicant, the T2Bacteria® Panel is capable of detecting bacterial pathogens directly in whole blood more rapidly and with greater sensitivity as compared to the current standard-of-care, blood culture. The applicant noted that the T2Bacteria® Panel's major detected species are five of the most common and virulent sepsis-causing organisms.[252 253] The applicant asserted that, by enabling the rapid administration of species-specific antimicrobial therapies, the T2Bacteria® Panel helps to reduce patients' hospital lengths-of-stay and substantially improves clinical outcomes. Furthermore, the applicant asserted that the T2Bacteria® Panel helps to reduce the overuse of ineffective or unnecessary antimicrobial therapy, reducing patient side effects, lowering hospital costs, and potentially counteracting the growing resistance to antimicrobial therapy.
The applicant stated that the T2Bacteria® Panel runs on the T2Dx Instrument, which is a bench-top diagnostic instrument that utilizes developments in magnetic resonance and nanotechnology to detect pathogens directly in whole blood, plasma, serum, saliva, sputum and urine at limits of detection as low as one colony forming unit per milliliter. The applicant explained that the T2Dx breaks down red blood cells, concentrates microbial cells and cellular debris, amplifies DNA using a thermostable polymerase and target-specific primers, and detects amplified product by amplicon-induced agglomeration of supermagnetic particles and T2MR measurement.[254] To perform a diagnostic test, the patient's sample tube is snapped onto the disposable test cartridge, which is pre-loaded with all necessary reagents. The cartridge is then inserted into the T2Dx, which automatically processes the sample and then delivers a diagnostic test result. The applicant asserted that each test panel is comprised of a test cartridge and a reagent tray and that each are required to run the T2Bacteria® Test Panel.
As stated in the FY 2020 IPPS/LTCH PPS proposed rule and as previously stated in this final rule, the current standard-of care for identifying bacterial bloodstream infections that cause sepsis is a blood culture. The applicant explained that blood culture diagnostics have many limitations, beginning with a series of time and labor intensive analyses. According to the applicant, completing a blood culture requires typically 20 mLs or more of a patient's blood, which is obtained in two 10 mL draws and placed into two blood culture bottles containing nutrients formulated to grow bacteria. The applicant explained that before the blood culture indicates if a patient is infected, pathogens typically must reach a concentration of 1,000,000 to 100,000,000 CFU/mL in the blood specimen. This growth process typically takes 1 to 6 or more days because the pathogen's initial concentration in the blood specimen is often less than 10 CFU/mL.- The applicant stated that a typical blood culture provides a result in a 2 to 4 day timeframe for species ID and yields 50 to 65 percent clinical sensitivity.[255 256] According to the applicant, a recent retrospective analysis of 13 U.S. hospitals and over 150,000 cultures found a median blood culture time for species ID of 43 hours.[257]
According to the applicant, blood cultures provide results at multiple stages. A negative test result requires a minimum of 5 days for blood cultures. A positive blood culture typically means that some pathogen is present, but additional steps must be performed to identify the specific pathogen and provide targeted therapy. The applicant submitted data stating that during the T2Bacteria® Panel's pivotal study, blood cultures took an average of 63.2 hours (off T2Bacteria® Panel) and 38.5 hours (on T2Bacteria® Panel) to obtain positive results and 96.0 hours (off T2Bacteria® Panel) and 71.7 hours (on T2Bacteria® Panel) to achieve species identification.[258] The applicant stated that, given this length of time to species identification, the first therapy for a patient at risk of sepsis is often broad-spectrum antibiotics, which treats some, but not all bacteria types. In addition, the applicant indicated that the time to species identification in blood culture diagnostics causes delays in administration of species-specific targeted therapies, increasing hospital lengths-of-stay and risk of death.
With respect to the newness criterion, the applicant received FDA 510(k) clearance on May 24, 2018, based on a determination of substantial equivalence to a legally marketed predicate device. The applicant noted that the T2Bacteria® Panel has a very broad application in the inpatient hospital setting and, as a result, potential cases available for use of the T2Bacteria® Panel may be identified by thousands of ICD-10-CM diagnosis codes. In the proposed rule (84 FR 19357), we noted that the applicant had submitted a request to the ICD-10 Coordination and Maintenance Committee for approval for a unique ICD-10-PCS procedure code, effective in FY 2020, to describe procedures which use the T2Bacteria® Panel. T2Bacteria® Panel was granted approval for the ICD-10-PCS code XXE5XM5 (Measurement of Infection, Whole Blood Nucleic Acid-base Microbial Detection, New Technology Group 5), effective October 1, 2019.
As previously discussed, if a technology meets all three of the substantial similarity criteria, it would be considered substantially similar to an existing technology and would not be considered “new” for purposes of new technology add-on payments.
With regard to the first criterion, whether a product uses the same or a similar mechanism of action to achieve a therapeutic outcome, the applicant asserted that the T2Bacteria® Panel: (1) Has a different mechanism of action when compared to the current standard-of-care for the diagnosis of bacterial pathogens directly from whole blood; and (2) is designed to achieve a different therapeutic outcome when compared to the other diagnostic test panel that is based on the same technological diagnostic platform. Specifically, the applicant asserted that the standard-of-care blood culture is a laboratory test in which blood, taken from the patient, is inoculated into bottles containing culture media and incubated over a period of time to determine whether infection-causing micro-organisms (bacteria or fungi) are present in the patient's bloodstream. In contrast, the applicant stated that the T2Bacteria® Panel relies on developments in magnetic resonance and nanotechnology to determine the presence of bacterial pathogens in a patient's blood by exploiting the physics of magnetic resonance. Furthermore, the applicant indicated that the only other product on the U.S. market that uses the same or similar mechanism of action as the T2Bacteria® Panel is the T2Candida Panel, which detects five clinically relevant species of Candida, a fungal pathogen known to cause sepsis. However, the applicant noted that the T2Candida Panel is a diagnostic aid in the treatment of sepsis caused by fungal infections in the blood and thus achieves a different therapeutic outcome than the T2Bacteria® Panel.
With regard to the second criterion, whether the technology is assigned to the same or different MS-DRG, the applicant did not comment. However, we stated in the proposed rule that we believed cases involving the use of the technology would be assigned to the same MS-DRGs as cases involving the current standard-of-care of laboratory blood cultures.
With respect to the third criterion, whether the new use of the technology involves the treatment of the same or similar type of disease and the same or similar patient population, according to the applicant, the T2Bacteria® Panel would be used as a diagnostic aid in the treatment of similar diseases and patient populations as the current standard-of-care, laboratory blood cultures.
In the proposed rule, we stated our concern that the mechanism of action of the T2Bacteria® Test Panel may be similar to the mechanism of action used by laboratory blood cultures or other available diagnostic tests that are the current standard of care. While the applicant stated that the T2Bacteria® Test Panel has a unique mechanism of action, we noted that like other available diagnostic tests, the T2Bacteria® Test Panel uses DNA to identify bacterial species. Similarly, in order to obtain species identification from the current standard-of-care, blood cultures, a DNA test is also required. Therefore, we stated that we were concerned with the similarity of this mechanism of action. We invited public comments on whether the T2Bacteria® Test Panel is substantially similar to the standard-of-care laboratory blood cultures or other diagnostic tests and whether this technology meets the newness criterion.
Comment: A commenter submitted a comment in response to CMS' concern that the T2Bacteria® Test Panel has a mechanism of action which is similar to currently available diagnostic tests. The commenter stated that while it is the case that the T2Bacteria® Test Panel uses DNA to identify bacteria species, its unique feature is the rapid identification of bacteria without the requirement for blood culture and/or other diagnostic techniques. The commenter stated that they knew of no other FDA cleared diagnostics for which this is the case.
Two commenters stated that the T2Bacteria® Test Panel detects bacterial-associated DNA differently than all other FDA cleared products because it does not depend on a positive blood culture and bacterial cell growth to detect pathogens. The commenters added that this innovation is due to magnetic resonance detection used by the T2Bacteria® Test Panel.
The applicant submitted a comment stating that the T2Bacteria® Test Panel does not use the same or similar mechanism of action compared to an existing technology. The applicant stated that all other bloodstream pathogen identification methods require a positive blood culture and that the T2Bacteria® Test Panel has a limit of detection greater than 1,000 times lower than any bloodstream pathogen identification method, allowing it to be used directly on patient blood samples without culturing. Lastly the applicant stated that while the T2Bacteria Panel does identify species with DNA, the differences from direct and independent detection, lack of growth, and lack of interference from antibiotics and competitive growth relative to all other FDA cleared diagnostics distinguishes the T2Bacteria Panel as a novel technology.
In response to CMS' concern that the T2Bacteria® Test Panel was similar to the blood cultures in that they both require DNA tests to identify bacterial species, a commenter stated that DNA tests are not required to identify bacteria from blood cultures. The commenter stated that most institutions still use traditional microbiology techniques (for example, biochemical reaction tests) to identify bacterial species.
Response: We appreciate the commenters' input and the additional information provided by the applicant in response to our concerns in the proposed rule. After consideration of the public comments we received and information submitted by the applicant in its application, we believe that the T2Bacteria® Test Panel uses a unique mechanism of action to achieve a therapeutic outcome because it works differently than currently available therapies through magnetic resonance detection to detect bacterial DNA directly from patient blood samples. Therefore, we believe T2Bacteria® Test Panel is not substantially similar to existing technologies and meets the newness criterion.
With regard to the cost criterion, the applicant provided the following analysis. To identify the MS-DRGs to which potential cases available for use of the T2Bacteria® Panel would most likely map, a selection of ICD-10-CM diagnosis codes associated with the clinical presence of the on-panel sepsis-causing bacteria for which the T2Bacteria® Test Panel tests was identified.[259 260 261 262 263] The applicant asserted that the T2Bacteria® Test Panel can identify three Gram-negative blood stream infections (Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa) and two Gram-positive bloodstream infection species (Staphylococcus aureus, and Enterococcus faecium). A total of 67 ICD-10-CM diagnosis codes were identified and segmented by two categories, infections (39 codes) and sepsis (28 codes). The applicant asserted that the former category represents potential cases available to be diagnosed by the T2Bacteria® Panel for patients who are at risk for sepsis and the latter represents potential cases available for use of the T2Bacteria® Panel for patients who have been diagnosed with a confirmed sepsis. The applicant stated that distinguishing between the two was necessary due to the varying costs associated with the treatment of patients at risk for sepsis versus confirmed cases of sepsis.
After the identification of the 39 infection and 28 sepsis diagnosis codes, both selections were refined by the applicant with the removal of cases identified by a total of 15 codes that represent pathogens not within the spectrum of blood infections that the T2Bacteria® Panel has been tested with and/or has been confirmed to detect. From the infection diagnosis codes, cases identified by two ICD-10-CM diagnosis codes: A021 (Salmonella sepsis); and A227 (Anthrax sepsis) were removed. From the sepsis diagnosis codes, cases identified by 13 diagnosis codes were removed: A021 (Salmonella sepsis); A227 (Anthrax sepsis); A400 (Sepsis due to streptococcus, group A); A401 (Sepsis due to streptococcus, group B); A403 (Sepsis due to streptococcus pneumonia); A408 (Other streptococcal sepsis); A409 (Streptococcal sepsis, unspecified); A413 (Sepsis due to hemophilus influenza); A414 (Sepsis due to anaerobes); A4153 (Sepsis due to serratia); A427 (Actinomycotic sepsis); A5486 (Gonococcal sepsis); and B377 (Candidal sepsis). The remaining infection and sepsis diagnosis codes were then used to query the FY 2017 MedPAR database to identify inpatient discharges reporting these diagnosis codes under the primary and secondary position.
According to the applicant, the resulting sets of MS-DRGs from both diagnosis code selection queries had visible commonalities when looking at only the MS-DRGs that contained potential cases which represented at least 1 percent of the discharge volume for the specific diagnoses. According to the applicant, due to the high volume of cases pulled and visible trends, provider-specific discharges at the MS-DRG level with fewer than 11 discharges were omitted from the analysis. In reconciling the list of MS-DRGs containing potential cases identified for the specific infection and sepsis codes, the applicant stated that MS-DRGs 853 (Infectious & Parasitic Diseases with O.R. Procedure with MCC), 870 (Septicemia or Severe Sepsis with Mechanical Ventilation > 96 Hours), 871 (Septicemia or Severe Sepsis without Mechanical Ventilation > 96 Hours with MCC) and 872 (Septicemia or Severe Sepsis without Mechanical Ventilation > 96 Hours without MCC) contain at least 1 percent of the potential case volume under both scenarios and are the MS-DRGs to which these potential cases available for use of the T2Bacteria® Test Panel would most closely map.
The applicant provided multiple cost analysis scenarios to demonstrate that the T2Bacteria® Test Panel meets the cost criterion. Eight scenarios were provided for the Sepsis and Infection diagnosis codes, separately, using the ICD-10-CM selections and based on the following methodologies: (1) Applicable discharges for the potential cases contained in 4 MS-DRGs (853, 870, 871 and 872); (2) applicable discharges for cases inclusive of all identified MS-DRGs; (3) applicable discharges with ICU usage for potential cases contained in 4 MS-DRGs (853, 870, 871 and 872); (4) applicable discharges with ICU usage for potential cases inclusive of all identified MS-DRGs; (5) applicable discharges for cases contained in 4 MS-DRGs (853, 870, 871 and 872) with removal of 50 percent of pharmacy charges for prior technology; (6) applicable discharges for potential cases inclusive of all identified MS-DRGs with removal of 50 percent of pharmacy charges for prior technology; (7) applicable discharges with ICU usage for potential cases contained in 4 MS-DRGs (853, 870, 871 and 872) with removal of 75 percent of pharmacy charges for prior technology; and (8) applicable discharges with ICU usage for potential cases contained inclusive of all identified MS-DRGs with removal of 75 percent of pharmacy charges for prior technology.
The applicant's order of operations used for each analysis is as follows: (1) Using the 15 sepsis or 37 infection diagnosis codes; (2) using the complete set of cases or those who had an ICU stay; (3) removing pharmacy charges at 0 percent, 50 percent, or 75 percent (for ICU patients only); and (4) standardizing the charges per cases using the Impact File published with the FY 2019 IPPS/LTCH PPS final rule correction notice data file. After removing the charges for the prior technology and standardizing charges, the applicant applied an inflation factor of 1.08986, which is the 2-year inflation factor from the FY 2019 IPPS/LTCH PPS final rule correction notice (83 FR 49844) to update the charges from FY 2017 to FY 2019. The applicant then added charges for the T2Bacteria® Panel. Under each scenario, the applicant stated that the inflated average case-weighted standardized charge per case exceeded the average case-weighted threshold amount. In this final rule, as in the proposed rule, we provide a table depicting the applicant's results for all 16 scenarios that the applicant indicated demonstrates that the technology meets the cost criterion.


The applicant noted that, in all 16 scenarios, the average case-weighted standardized charge per case for potential cases available for aid by use of the T2Bacteria® Test Panel would exceed the average case-weighted threshold amounts in the FY 2019 IPPS/LTCH PPS final rule correction notice data file by between $803.87 and $33,488.82. Supplementary analyses were provided by the applicant, which included eight additional scenarios that combined the 15 sepsis and 37 infection diagnosis codes into one set of 52 diagnosis codes. The applicant again utilized an inflation factor of 1.08986 and followed the same methodology as the previously discussed cost analyses. The applicant again noted that the final inflated average case-weighted standardized charge per case exceeded the average case-weighted threshold amounts in all scenarios, ranging between $1,083.67 and $32,430.57.
We invited public comments on whether the T2Bacteria® Panel meets the cost criterion.
Comment: A commenter stated that cost remains a major impediment to the use of the T2Bacteria technology despite its vital importance. In addition, the applicant submitted a statement reaffirming that the T2Bacteria Test Panel fulfills the cost criterion as demonstrated by multiple cost analysis scenarios presented in their original application and as previously summarized in this final rule.
Response: We thank the commenter for their input. After consideration of the comments received and the analyses described previously we agree that the T2Bacteria® Panel meets the cost criterion.
With respect to the substantial clinical improvement criterion, the applicant asserted that the T2Bacteria® Panel represents a substantial clinical improvement over existing technologies. According to the applicant, the T2Bacteria® Panel is the only FDA cleared-diagnostic aid that has the ability to rapidly and accurately identify sepsis-causing bacteria species directly from whole blood within 3 to 5 hours, instead of the 1 to 5 days required by current standard-of-care laboratory blood cultures or other diagnostic technology. The applicant also asserted that the use of the T2Bacteria® Panel provides more rapid beneficial resolution of the disease process due to enabling faster treatment. Several studies provided by the applicant suggest that effective detection prior to therapy can lead to a reduction in hospital lengths-of-stay and likelihood of death.[264 265] According to the applicant, in these studies for every hour reduction in time to effective therapy or species ID, the length-of-stay decreased by 2.7 hours.
The applicant stated that the T2Bacteria® pivotal trial that it submitted to support FDA clearance enrolled 11 hospitals in the United States and 1,427 patients with a blood culture ordered as the standard-of-care, with species ID determined by MALDI-TOF or Vitek2.[266] Furthermore, due to the low prevalence of panel specific organisms, an additional 250 contrived specimens were evaluated. The T2Bacteria® Panel result was blinded to the managing staff and did not influence care. Blood samples were drawn for culture and T2Bacteria® Panel from the same line at the same time. The mean time to blood culture positivity was 51.0 ± 43.0 hours (mean ± SD) and the mean time to species ID was 83.7 ± 47.6 hours (mean ± SD). In contrast, the mean time to T2Bacteria® Panel result was 6.5 ± 1.9 hours, where a full load of 7 samples completed in 7.70 ± 1.4 hours and a single sample completed in 3.6 ± 0.02 hours. Therefore, the difference in mean time to result between blood culture and the T2Bacteria® Panel assay was 77.2 hours or 3.2 days (p < 0.001). Compared to the matched draw blood culture and contrived samples, the overall sensitivity ranged from 81.3 percent to 100 percent and specificity ranged from 95.0 percent to 100 percent, respectively. Of the 190 positive T2Bacteria® Panel results, 35 had matching blood culture results and 155 were potentially false positive. Of these 155, 35 had a positive blood culture at another blood draw within 14 days; 30 had positive results by amplification and gene sequencing; and 23 had other positive non-blood specimens for the same organism. Sixty-three of the 190 (33 percent) positive results were not associated with evidence of infection. Later testing by the applicant confirmed that reagent contamination caused the high false positive rates specifically for E. coli of 1.7 percent and P. aeruginosa (1.7 percent) in stored blood samples. Compared to blood culture results for species identified with the T2Bacteria® Panel, the assay detected 3.2-times more positives associated with infection.
Nguyen, et al., a submitted publication manuscript based on the pivotal study data, found that the species identification of the T2Bacteria® Panel took an average mean time of 3.61 ± 0.2 hours up to 7.70 ± 1.38 hours (mean time dependent on the number of samples loaded, 1 to 7), which was shorter than that of the standard-of-care blood culture with a mean time of 71.7 ± 39.3 hours.[267] In addition to faster species identification, the applicant asserted that the T2Bacteria® Panel identifies more infection-positive cases than blood cultures when verified by non-concurrent test results [268] or when verified with proven, probably, or possible criteria (concurrent blood culture positive results, non-concurrent blood culture results with positive culture results from another site within 21 days, and no culture match, but the T2Bacteria® Panel bacteria was a plausible cause of disease, respectively). In this study, 66 percent of patients with concomitant blood culture results and T2Bacteria® Panel positive results were not on active antibiotics at the time of the blood draw, while 24 percent of patients with probable or possible blood stream infections that were positive by T2Bacteria® Panel alone were not on effective therapy.
In another study submitted by the applicant, 137 blood cultures and T2Bacteria® Panel tests were obtained from participants in the emergency department.[269] T2Bacteria® Panel results were verified with concordant blood culture results, or when discordant with blood cultures from another location drawn within 14 days of the matched draw, or with the whole blood Sanger sequencing method. No samples generated an invalid result for the T2Bacteria® assay. The T2Bacteria® Panel identified 15 positives for which blood cultures had concordant matches for 12. The three unmatched positives were verified via other means. As compared to blood cultures, the T2Bacteria® Panel had an overall positive percent agreement of 100 percent (12/12) and a negative percent agreement of 98.4 percent (662/673). The negative percent agreement is shown to be due to blood culture results that are indeterminate, or false positive.
In the same study [270] , the T2Bacteria® Panel results relative to standard-of-care blood culture identification were classified into four impact level categories: (1) Minimal impact results have negative blood culture results with no evidence of infection for which results would have little to no impact; (2) some impact results occur for patients who have an effective therapy at the time of results, but the number of antibiotics administered could have been reduced; (3) moderate impact results are for those on effective therapy at the time of results, but were switched to species-directed therapy within 12 hours of a standard-of-care blood culture identification; and (4) direct impact results relate to those who could have been placed on effective therapy earlier based on the results of the T2Bacteria® Panel.[271] The study identified 7 “minimal impact” incidents, 8 “some impact” incidents, 4 “moderate impact” incidents, and 4 “direct impact” incidents, indicating that 16/23 (69.6 percent) of positive test results could have potentially influenced patient care.
In articles provided by the applicant which concerned separate studies, the T2Bacteria® Panel was found to have a shorter time to species identification than blood cultures.[272 273] The study analysis by De Angelis, et al., 2018, an international, prospective observational study involving 129 patients (144 enrolled) 18 years of age and older who had a blood culture and for whom a T2Bacteria® Panel was also obtained, showed that the T2Bacteria® Panel provided a mean time to species identification and negative result of 5.5 ± 1.4 hours and 6.1 ± 1.5 hours, respectively as compared to 25.2 ± 15.2 hours and 120 ± 0.0 hours resulting from the standard-of-care blood culture method, respectively.[274] There were a total of 10 concordantly identified micro-organisms, 2 identified by standard-of-care blood culture only, and 20 detected by the T2Bacteria® Panel only. As compared to the results from the standard-of-care blood culture method, the results from the T2Bacteria® Panel had a sensitivity that ranged from 50 percent to 100 percent across the 5 detection channels, with an aggregate of 83.3 percent and a specificity that ranged from 94.8 percent to 100 percent, with an aggregate of 97.6 percent. For patients who had a matched blood culture positive (n=8) and who met the criterion of infection (n=6), a total of 36 percent (5/14) of the patients were receiving inappropriate antimicrobial therapy at the time of the T2Bacteria® Panel result. The results of this study are again discussed in another article submitted by the applicant, which states that these results may have the potential to rapidly identify the five on-panel pathogens that may include cases missed by results of the standard-of-care blood culture.[275]
The applicant further asserted that the T2Bacteria® Panel provides a decreased rate of subsequent diagnostic or therapeutic interventions. The applicant discussed the results of a meta-analysis of 70 studies, in which the proportion of patients on an inappropriate empiric therapy was 46.5 percent.[276] The applicant indicated that the results show that amongst patients with a blood culture draw, typical antibiotic administration rates range from 50 to 70 percent.[277 278 279] The applicant asserted that based on the results of the analysis by the Voigt, et al., manuscript, 35 percent (8/23) of the patients, receiving 3.6 ± 1.1 (mean ± SD) unique antibiotics per patient, could have potentially seen a reduction in the number of administered antibiotics.[280] The applicant further stated via a supplementary presentation to CMS that the use of the T2Bacteria® Panel allows for earlier species directed therapy than that allowed for by standard-of-care blood cultures. The applicant believed that the use of the T2Bacteria® Panel may allow the provider to move from broad potentially unnecessary empiric to species-targeted therapy. The applicant stated that using hospital antibiograms and being informed of the species by the T2Bacteria® Panel, the physician is able to use species-directed therapy and place up to 90 percent of patients on an effective therapy in a few hours instead of 2 to 3 days.
According to the applicant, the practice of antibiotic de-escalation was recently evaluated across 23 studies and found to be safe and effective.[281] Given the toxicity associated with antibiotics, where some antibiotics cause encephalopathies including seizures[282] and in extreme cases show up to a 4.5 percent mortality rate due to the antibiotic itself,[283] the applicant asserted that judicious use of antibiotics is necessary. The applicant further stated that rapid diagnostics such as that able to be accomplished by the use of the T2Bacteria® Panel assay, due to its negative predictive value (NPV) of 99.7 percent,[284] will enable physicians to focus therapy and reduce the use of unnecessary drugs, where a targeted therapy is possible in 3.8 hours instead of 2 days, reducing toxicity and development of resistance.[285]
The applicant stated that the use of the T2Bacteria® Panel will result in reduced mortality. The applicant indicated that the results of large retrospective analyses show that every hour delaying time to appropriate antibiotic therapy increased odds of death by 4 percent or reduced survival by 7.6 percent.[286 287 288] The applicant stated that the results of the T2Bacteria® Panel Pivotal trial show that out of 23 positive patients, 4 (17 percent) could have seen a reduction in time to effective therapy, with mean time of 28.0 hours. An additional 4 (17 percent) could have seen a reduction in time to species-directed therapy, with mean time reduction of 52.6 hours. The applicant stated that by using the T2Bacteria® Panel assay relative to standard-of-care blood cultures, they expect a potential reduction in the odds of death to be 52.8 percent. According to the applicant, this factor of 2 difference is consistent with a two-time higher odds of death in patients given inappropriate empiric antibiotics relative to appropriate empiric antibiotics.[289] The applicant indicated that this result suggests that employing the use of the T2Bacteria® Panel assay should reduce mortality in bacteremia patients who are not immediately on appropriate therapy.
In the form of supplementary information, the applicant stated that the use of the T2Bacteria® Panel covers 5 species, which account for 50 percent to 70 percent of all blood stream infections, depending on local epidemiology. According to the applicant, the remaining 30 percent to 50 percent of patients would continue to need standard-of-care blood cultures for species identification. Based on all of the previous discussions, the applicant believed that the T2Bacteria® Test Panel represents a substantial clinical improvement over existing technologies.
In the proposed rule, we stated that we have the following concerns regarding whether the T2Bacteria® Panel meets the substantial clinical improvement criterion. First, we stated that we were not certain that the applicant had provided sufficient evidence to demonstrate that the early identification without antibiotic susceptibility provided by the use of the T2 Bacteria® Panel is enough to prevent unnecessary empiric therapy because specific identification and antibiotic susceptibilities may still be required by blood cultures to adequately treat sepsis. For instance, if an on-panel bacteria were identified it remains possible that this species could be resistant to the standard-of-care treatment for such bacteria used in a hospital. In addition, we stated that we believe that not only is it possible for an identified species to be resistant to typical empiric therapy, therefore diminishing the utility of its early identification, it also is possible for off-panel organisms to be present and also not be affected by species-targeted empiric treatment. The applicant provided supplemental information in which it stated that, consistent with its labeling, the use of the T2Bacteria® Test Panel would not replace blood cultures for specific organisms. Given this information, we stated that we were concerned that the use of the T2Bacteria® Panel may not be a substantial clinical improvement over standard-of-care blood cultures, the existing comparator.
Second, the applicant provided research and analyses which suggest that the use of the T2Bacteria® Test Panel may lead to decreased hospital lengths-of-stay, and decreased mortality. Specifically, these analyses and articles show that there is a possibility for a correlated relationship between the T2Bacteria® Panel's time to species ID and these identified outcomes. The applicant addressed this issue in a qualitative manuscript analysis involving identification of potential impacts of the T2Bacteria® Test Panel.[290] In the proposed rule, we stated that we recognized that this qualitative analysis is informative, but we were concerned that the low number of cases (under 10) may limit generalizability of these results. Given this information, we stated that we were concerned that in lieu of direct testing, these suggestive findings may not show a causative relationship.
Third, we stated that we were concerned that in all of the studies provided, the comparator for the T2Bacteria® Panel is a single blood culture draw. It is well established that blood culture sensitivity and specificity increase with repeat blood draws. According to research provided by the applicant, a single set of blood cultures should not be drawn, but rather surveillance blood cultures, involving multiple draws over time, should be practiced.[291] Therefore, in the proposed rule, we stated that we believed initial blood cultures followed by repeated blood draws would have been a better comparator. Furthermore, we stated that we believed an even stronger comparator for the T2Bacteria® Test Panel would be other DNA based tests, such as polymerase chain reaction (PCR), which also utilize DNA to identify bacterial infections.
Ultimately, we stated that we were concerned that the use of the T2Bacteria® Test Panel may not alter the clinical course of treatment. We stated that we believed that the variable sensitivity and specificity for the T2Bacteria® Panel may be of concern if these results do not compare favorably to other available DNA tests. We stated that while some of the false positives in the pivotal trial were explained by reagent contamination (43 of the 63 false positives),[292] the high false positive rate seen in the applicant's literature, (for example, 13 of 32 positives (40.6 percent),[293] 58 of 146 positives (39.7 percent),[294] and a potential 20 of 63 (31.7 percent) from the pivotal trial) may result in unnecessary treatment of patients. Furthermore, we stated that use of a contrived arm in the pivotal trial and low overall incidence of these five specific sepsis-causing organisms may make it difficult to determine a substantial clinical improvement in the complex clinical setting. Lastly, we stated that it seemed that blood cultures may still be necessary to identify species susceptibility because the T2Bacteria® Test Panel does not identify susceptibility and subsequent treatment based upon its results will still require empiric treatment. We stated that if these points are true, then the inferred decreased hospital lengths-of-stay, decreased mortality, and better clinical outcomes may not be achieved with the use of the T2Bacteria® Test Panel.
We invited public comments on whether the T2Bacteria® Test Panel technology meets the substantial clinical improvement criterion, including with respect to the specific concerns we have raised.
Comment: Several commenters responded to our concern that early identification without antibiotic susceptibility of a bacteria may not be enough to prevent unnecessary empiric therapy. These commenters stated that the T2Bacteria Test Panel is a favorable complement to blood cultures that can rapidly identify sick patients given the limitations of the current standard of care, with a commenter stating that the Test Panel should not be considered a comparator to blood cultures.
A commenter stated that even without susceptibility results the T2Bacteria Test Panel enables the tailoring of therapy faster than any other technology, especially in patients known to be infected but with negative blood cultures. A second commenter stated that the Test Panel has the potential to impact both skin and urinary tract infections without the need for susceptibility testing. The commenter stated that a negative test result for patients with cellulitis could provide strong evidence against the need for vancomycin in certain patients and could also potentially facilitate the de-escalation of treatment. The commenter added as an example that in urinary tract infections which are primarily caused by E. coli and K. pneumonia, a positive test along with an institutional antibiogram can help shape therapy, while a negative for P. aeruginosa can lead to the reduced use of a key driver of antimicrobial resistance.
The applicant submitted a comment stating that the vast majority of bacteremia episodes are correctly treated after a positive species identification[295 296 297] and physicians acknowledge the value of species ID without susceptibility.[298] The applicant acknowledged that the T2Bacteria Test Panel is not a replacement for blood cultures but asserted that a diagnostic does not need to replace another to improve patient outcomes. According to the applicant, depending on the patient population and hospital ward, the T2Bacteria Panel will cover 50 to 70 percent of all bacteremia, including 90 percent of bacteremia by ESKAPE pathogens that are at particularly high risk of resisting broad spectrum antibiotics and could benefit from a species-directed change in therapy.[299 300 301 302 303] The applicant further noted that with a mean time difference between blood cultures and T2Bacteria Test Panel species identification of 77.2 hours,[304] clinicians could escalate or de-escalate therapy based on species ID 3 days in advance of the current standard of care. Lastly the applicant stated that a recent and independent economic analysis of direct-from-sample molecular diagnostic assays in an emergency department showed cost savings with technologies similar to the T2Bacteria Panel.[305]
Response: We appreciate the commenters' input and the applicant's response, including the additional information provided by the applicant and commenter in regards to the potential for early species identification to impact care provided by physicians.
Comment: Several commenters provided comments in response to our concern that the T2Bacteria Test Panel may not lead to decreased hospital lengths-of-stay and mortality due to a lack of supportive data. A commenter stated that the panel obviates the need for waiting for cells to grow as clinicians still face the challenge of selecting therapy while waiting for a positive blood culture, and that a major predictor of mortality in sepsis and septic shock is time to appropriate therapy. The commenter added that the T2Bacteria Test Panel helps place patients on appropriate therapy earlier than previously possible, leading to faster resolution and shorter lengths of stay.
The applicant reiterated results from an observational study summarized in the proposed rule in which 70 percent of patients with positive results from the T2Bacteria Test Panel may have realized benefits in their care. The applicant stated that a meta-analysis of 70 studies found the proportion of patients not on appropriate empiric antibiotic therapy was found to be 46.5 percent.[306] The applicant asserted, given these observations, that the T2Bacteria Panel has potential to substantially reduce the proportion of patients on inappropriate therapy, which for a significant proportion of patients will reduce unnecessary use of antibiotics and time to effective therapy. The applicant stated that to date a total of 125 patients in seven studies have been found to benefit from the T2Bacteria Test Panel, with 28.6 percent of patients benefitting after a T2Bacteria positive result, 53.7 percent benefitting after a T2Bacteria negative result, and 41.8 percent of patients benefitting overall. Finally, the applicant emphasized that the T2Bacteria Test Panel was cleared by the FDA less than one year ago and interventional studies are ongoing.
A commenter stated that they collaborated with T2 Biosystems in the study of the T2Bacteria Test panel on patients with leukemia and those undergoing hematopoietic cell transplantation. The commenter stated that among 84 patients, 4.8 percent and 13.1 percent were positive for an infection as identified by blood cultures and the T2Bacteria Test Panel respectively. Of seven patients, five had organisms detected that would have altered antibacterial therapy. The commenter added that the median time to detection for the T2Bacteria Test Panel as compared to blood cultures was 3.7 hours as compared to 12.5 hours respectively.
Response: We thank both commenter and applicant for their input, and appreciate the additional information regarding the correlation between T2Bacteria Test Panel, hospital length-of-stay, and mortality.
Comment: Regarding our concern that the single blood culture draw used in the applicant's pivotal trial may be a poor comparator to the T2Bacteria Test Panel in light of the well-established, increasing sensitivity and specificity involved in repeated blood draws, a commenter stated that a major advantage of the T2Bacteria Test Panel is the ability to potentially obviate multiple blood draws for blood culture. The commenter added that since the T2Bacteria Test Panel is the only FDA cleared direct-from-blood test for bacteremia it is well positioned to have a major impact on the clinical workflow.
The applicant stated since no other direct-from-blood, culture-independent DNA based tests are FDA cleared, they were required to use blood cultures as a comparator. The applicant maintained that the purpose of the comparator in the prospective arm of the T2Bacteria pivotal study was to demonstrate that the T2Bacteria assay can detect clinical infections. The applicant also maintained that comparator selection for an FDA diagnostic accuracy study has no impact on the clinical utility of the T2Bacteria Panel, as clinical impact analyses evaluate clinical diagnoses, patient outcomes, and the timing of effective antibiotic therapy. Finally, the applicant agreed with our statement in the proposed rule that repeat blood draws are the standard of care; however, the applicant stated that they also present a problem for comparative analyses. Per the applicant, bacteria may enter and exit the bloodstream for short durations over time during the course of disease and effective antibiotics can have a strong influence on the ability of bacteria to grow in culture. According to the applicant, by using repeat blood draws as the comparator, the applicant would record an inflated number of apparent false negatives from the effects of antibiotics and transient bacteremia.
Response: We thank the commenter and the applicant for their input. We appreciate the additional information regarding the use of repeat blood draws as a comparator to the T2Bacteria Test Panel.
Comment: In response to CMS' concern that the use of the T2Bacteria Test Panel may not alter the clinical course of treatment, the applicant stated that there are two dimensions to this concern, the impact on therapy escalations and de-escalations. First the applicant noted the T2Bacteria Test Panel has a specificity of 96 percent and therefore false positives would raise unnecessary treatment by 1 to 2 percent. The applicant added that this increase represents a worst case estimate because it assumes blind adherence to the T2Bacteria Panel result, with no consideration of the clinical course of the patient.
Second, the applicant stated that the increase in unnecessary treatment from false positive results ignores the potential for de-escalation. Per the applicant, within the context of the clinical course, a negative T2 Bacteria result could be an opportunity to reduce unnecessary antibiotic use, particularly due to a 99.7 percent negative predictive value. For example, vancomycin is frequently prescribed empirically; reported vancomycin empiric therapy rates include 23 percent [307] , 54 percent [308] , 65 percent [309] , and 67 percent [310] . The applicant stated that if clinicians de-escalated vancomycin based on clinical indicators and a negative T2Bacteria result, a major reduction in vancomycin administration could be realized, which would likely more than compensate for the additional unnecessary therapy from the panel.
A commenter stated that the ability to know if a patient is infected with an ESKAPE pathogen within three to five hours of a blood draw is a major clinical advantage. They added that the test will reduce unnecessary use of antibiotics, save hospitals money, and save lives. When addressing the concern for false positives, the commenter stated that the likelihood of infection is significantly higher with a T2Bacteria positive than without. They added that the current overuse of antibiotics is driven by a lack of information for time-critical patients and that with the T2Bacteria Test Panel this issue is addressed.
Response: We appreciate the commenter's and applicant's input regarding the potential of the T2Bacteria Test Panel to alter the clinical workflow of treating infections and impact on antibiotic resistance.
After consideration of the public comments we received, we agree that the T2Bacteria Test Panel represents a substantial clinical improvement over existing technologies because it reduces the proportion of patients on inappropriate therapy, thus reducing the rate of subsequent diagnostic or therapeutic intervention as well as length of stay and mortality rates caused by sepsis causing bacterial infections. In summary, we have determined that the T2Bacteria test panel meets all of the criteria for approval for new technology add-on payments. Therefore, we are approving new technology add-on payments for the T2Bacteria test panel for FY 2020. Cases involving the use of the T2Bacteria test panel that are eligible for new technology add-on payments will be identified by ICD-10-PCS procedure code XXE5XM5. In its application, the applicant estimated that the cost of the T2Bacteria test panel is $150. Under § 412.88(a)(2) (revised as discussed in this final rule), we limit new technology add-on payments to the lesser of 65 percent of the average cost of the technology, or 65 percent of the costs in excess of the MS-DRG payment for the case. As a result, the maximum new technology add-on payment for a case involving the use of the T2Bacteria test panel is $97.50 for FY 2020.
6. Request for Information on the New Technology Add-On Payment Substantial Clinical Improvement Criterion
Under the Hospital Inpatient Prospective Payment System (IPPS), CMS has established policies to provide additional payment for new medical services and technologies. Similarly, under the Hospital Outpatient Prospective Payment System (OPPS), CMS has established policies to provide separate payment for innovative medical devices, drugs and biologicals. Sections 1886(d)(5)(K) and (L) of the Act require the Secretary to establish a mechanism to recognize the costs of new medical services and technologies under the IPPS, and section 1833(t)(6) of the Act requires the Secretary to provide an additional payment amount, known as a transitional pass-through payment, for the additional costs of innovative medical devices, drugs, and biologicals under the OPPS.
Under the IPPS, the regulations at § 412.87 implement these provisions and specify three criteria for a new medical service or technology to receive the additional payment: (1) The medical service or technology must be new; (2) the medical service or technology must be costly such that the DRG rate otherwise applicable to discharges involving the medical service or technology is determined to be inadequate; and (3) the service or technology must demonstrate a substantial clinical improvement over existing services or technologies. Under this third criterion, § 412.87(b)(1) of our existing regulations provides that a new technology is an appropriate candidate for an additional payment when it represents an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries (we refer readers to the September 7, 2001 final rule for a more detailed discussion of this criterion (66 FR 46902)). For more background on add-on payments for new medical services and technologies under the IPPS, we refer readers to the FY 2009 IPPS/LTCH PPS final rule (73 FR 48552). Similar regulations exists for the OPPS; we refer interested readers to the FY 2020 IPPS/LTCH PPS proposed rule discussion of those regulations (84 FR 19367).
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19368), we stated that we understood that greater clarity regarding what would substantiate the requirements of the substantial clinical improvement criterion would help the public, including innovators, better understand how CMS evaluates new technology applications for add-on payments and provide greater predictability about which applications will meet the criterion for substantial clinical improvement. Therefore, in the proposed rule, we announced that we were considering potential revisions to the substantial clinical improvement criteria under the IPPS new technology add-on payment policy, and the OPPS transitional pass-through payment policy for devices, and invited public comments on the type of additional detail and guidance that the public and applicants for new technology add-on payments would find useful. The request for public comments was intended to be broad in scope and provide a foundation for potential rulemaking in future years. We refer readers to the FY 2020 IPPS/LTCH PPS proposed rule for additional detail regarding this request for public comments (84 FR 19367 through 19369).
CMS appreciates the many comments received in response to our request for information on longer term changes to the substantial clinic improvement criteria. CMS remains committed to helping ensure that Medicare beneficiaries have access to potentially life-saving diagnostics and therapies that improve beneficiary health outcomes. The comments received from the public will help us achieve these goals. In addition to the policies that we are finalizing in this FY 2020 final rule with respect to new medical services and technologies, we intend to continue to review the comments received in response to our Request for Information in order to continue our work in this area and inform our future rulemaking.
7. Revisions and Clarifications to the New Technology Add-On Payment Substantial Clinical Improvement Criterion Under the IPPS
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19369) we also announced that we were considering adopting, in the FY 2020 IPPS/LTCH PPS final rule, the following potential regulatory changes to the substantial clinical improvement criteria for applications received beginning in FY 2020 for IPPS (that is, for FY 2021 and subsequent new technology add-on payment) and beginning in CY 2020 for OPPS, after consideration of the public comments we receive in response to the proposed rule. We also invited public comments on whether any or all of these potential regulatory changes might be more appropriate as changes in guidance rather than or in addition to changes to our regulations.
- Adopting a policy in regulation or sub-regulatory guidance that explicitly specifies that the requirement for substantial clinical improvement can be met if the applicant demonstrates that new technology would be broadly adopted among applicable providers and patients. A broad adoption criterion would reflect the choices of patients and providers, and thus the marketplace, in determining whether a technology represents a substantial clinical improvement. This patient-centered approach would acknowledge that patients and providers can together determine the potential for substantial clinical improvement on an individual basis. As part of the policy being considered, we would add a provision at § 412.87(b)(1) and § 419.66(c)(2) stating that “substantially improves” means, inter alia, broad adoption by applicable providers and patients. We invited public comments on whether, if such a provision is finalized, it should specify that a “majority” is the appropriate way to further define and specify “broad adoption”, or if some other measure of “broad” (for example, more than the current standard-of-care, more than a particular percentage) is more appropriate. Furthermore, we invited public comments on whether to further specify that “broad adoption” is in the context of applicable providers and patients for the technology, and does not mean broadly adopted across the entire IPPS or OPPS. We stated that we were interested in whether commenters have particular suggestions regarding how, in implementing such a provision, CMS could provide other helpful regulatory clarification or sub-regulatory guidance regarding how “broad adoption” could be measured and demonstrated prospectively as a basis for substantial clinical improvement. We stated that if adopted, such a policy would establish, by regulation, predictability and clarity regarding the meaning and application of substantial clinical improvement by providing a specific and clear path to one way substantial clinical improvement can be established.
- Adopting in regulations or through sub-regulatory guidance a definition that the term “substantially improves” means, inter alia, that the new technology has demonstrated positive clinical outcomes that are different from existing technologies. As part of the policy being considered, we would specify that the term “improves” can always be met by comparison to existing technology. Then, we would further specify that such improvement may always be demonstrated by reference and comparison to diagnosis or treatment achieved by existing technology. We stated that this would provide a standard for innovators that is predictable and based on comparison to outcomes from existing technologies, and would reflect that an evaluation of “improvement” involves a comparison relative to existing technology. We stated that if adopted, such a policy, would establish, by regulation or through sub-regulatory guidance, predictability and clarity regarding the meaning and application of substantial clinical improvement by clarifying how existing and new technologies are compared.
- Adopting a policy in regulation or through sub-regulatory guidance that specifies that “substantially improves” can be met through real-world data and evidence, including a non-exhaustive list of such data and evidence, but that such evidence is not a requirement. Real-world evidence reflects usage in everyday settings outside of a clinical trial, which is the majority of care delivered in the United States. For example, between 3 percent and 5 percent of patients with cancer are enrolled in a clinical trial.[311]
As part of the policy being considered, the regulation or sub-regulatory guidance would list the kinds of data and evidence and particular findings that CMS would consider in determining whether the technology meets the substantial clinical improvement criterion and that such kinds of data can be sufficient to meet that standard. Then, we would provide a non-exhaustive list of such kinds of data and findings, including: A decreased mortality rate; a reduction in length of stay; a reduced recovery time; a reduced rate of at least one significant complication; a decreased rate of at least one subsequent diagnostic or therapeutic intervention; a reduction in at least one clinically significant adverse event; a decreased number of future hospitalizations or physician visits; a more rapid beneficial resolution of the disease process treatment; an improvement in one or more activities of daily living; or, an improved quality of life. We stated that outcomes relating to quality of life, length of stay, and activities of daily living may reflect meaningful endpoints not often captured by clinical trials or other pivotal trials designed primarily for regulatory purposes. We invited public comments on whether we should adopt such a policy and list, and if so, what the list should contain. We also invited comments on whether, as a general matter, data exists on patients' experience with new medical devices outside of the clinician's office, on the effects of a treatment on patients' activities of daily living, or on any of the other areas as previously listed. We stated that these comments would at least inform our adoption of a policy in regulations or sub-regulatory guidance. We stated that if adopted, such a policy, would establish, by regulation or guidance, predictability and clarity regarding the meaning and application of substantial clinical improvement by providing a specific and clear path to one way substantial clinical improvement can be established.
- To address the impression that a peer-reviewed journal article is required for the agency to find that a new technology meets the requirement for substantial clinical improvement, explicitly adopting a policy in regulations or sub-regulatory guidance that the relevant information for purposes of a finding of substantial clinical improvement may not require a peer-reviewed journal article. We stated that we recognize the value of both academic and other traditional and non-traditional emerging sources of information in determining substantial clinical improvement. We invited public comments on whether, in addition to making clear that a peer-reviewed journal article is not required, types of relevant information that could be helpful should be specified in such a regulation or guidance to include but not be limited to other particular formats or sources of information, such as consensus statements, white papers, patient surveys, editorials and letters to the editor, systematic reviews, meta-analyses, inferences from other literature or evidence, and case studies, reports or series, in addition to randomized clinical trials, study results, or letters from major associations, whether published or not. We stated that if adopted, such a policy, would establish, by regulation or guidance, predictability and clarity that the agency is open, in every case, to all types of information in considering whether a new technology meets the substantial clinical improvement criterion, consistent with our current practice of not requiring any particular type of information.
- Adopting a policy in regulations or sub-regulatory guidance that, if there is a demonstrated substantial clinical improvement based on the use of a new medical service or technology for any subset of beneficiaries, the substantial clinical improvement criterion may be met regardless of the size of that subset patient population. Substantial clinical improvement may be confounded by comorbidities, patient factors, or other concomitant therapies which are not readily controlled in research studies. This potential change recognizes that subset populations may have unique needs. As part of the policy being considered, we would include a statement in regulation or guidance that a technology may meet the “substantial clinical improvement” criterion by demonstrating a substantial improvement for any subset of beneficiaries regardless of size. We stated that this potential change would reflect that many medical technologies are designed for limited subset populations. Many personalized and precision medicine approaches aspire for “n=1 therapy.”
We invited public comments on whether, in adopting such a policy, we should also specify that the add-on payment would be limited to use in that subset of patient population. If not, why not? For example, if a new technology that treats cancer only demonstrates substantial clinical improvement for a select subset of patients with that diagnosis, should the additional inpatient payments for use of the new technology be limited to only when that new technology is used in the treatment of that select subset of Medicare beneficiaries, and, if so, how could that subset of patient population be defined in advance, and in what circumstances should there be an exception to any such limitation? If such a policy were adopted, how could it be constructed or written to not create new limitations or obstacles to innovation that are not present in our regulations today?
We also invited public comments as to whether there are special approaches that CMS should adopt in regulations or through sub-regulatory guidance for new technologies that treat low-prevalence medical conditions in which substantial clinical improvement may be more challenging to evaluate. Specifically, we invited comment on how to categorize and specify these conditions, including how to define “low-prevalence”, whether CMS should adopt any of the potential changes under consideration in this section which are not adopted more broadly, or any special approaches suggested by commenters. We stated that the goal is to establish, by regulation or guidance, predictability and clarity that the substantial clinical improvement criterion can be met, either in all cases or for cases involving low-prevalence medical conditions, regardless of the size of the patient population which would benefit.
- Adopting a policy in regulations or sub-regulatory guidance that specifically addresses that the substantial clinical improvement criterion can be met without regard to the FDA pathway for the technology. We indicated that as part of the policy being considered, we would clarify in regulation that the notion of “improvement” includes situations where there is an extant technology such as a predicate device for 510(k) purposes, and explicitly state that the agency will not require a device to receive an FDA marketing authorization other than a 510(k) clearance in order for the device to be considered a substantial clinical improvement. We stated that if adopted, the policy described here, would establish, by regulation or guidance, predictability and clarity by clarifying that the substantial clinical improvement criterion can be met without regard to the FDA pathway for the technology, consistent with our current practice.
We solicited comments on the potential revisions and regulatory or sub-regulatory changes as previously described, and also welcomed suggestions on other information that would help us clarify and/or modify in the FY 2020 IPPS/LTCH PPS final rule or through sub-regulatory guidance CMS' expectations regarding substantial clinical improvement for payments for new technologies.
Comments: With respect to the use of “broad adoption” in evaluating substantial clinical improvement, some commenters urged CMS to proceed cautiously through additional rulemaking. Some of these comments stated that “broad adoption” should not be a prerequisite for new technology add on payment eligibility. MedPAC indicated it did not equate substantial clinical improvement with broad adoption, and that it is not appropriate for the Medicare program to provide higher payment for services that have not been proven to have a clinical advantage over existing treatment options. MedPAC indicated that it has written extensively about items and services provided to Medicare beneficiaries that lack evidence of comparative clinical effectiveness, yet are broadly used.
With respect to indicating that “substantially improves” means that the new technology has demonstrated positive clinical outcomes that are different from existing technologies, some commenters were concerned that such a standard might restrict alternative study designs or impose standards that exceed realistic requirements. These commenters noted that for many novel technologies, there may be no existing technologies that could appropriately serve as a comparator. Some commenters indicated that such a comparison should not be a requirement for meeting the substantial clinical improvement criterion. If CMS decides to advance a comparison to existing technologies as a standard for demonstrating substantial clinical improvement, these commenters indicated that it is important to note that the comparator should be the standard of care, which may be a procedure or no intervention, rather than existing technology.
With respect to indicating that “substantially improves” can be met through real-world data and evidence, many commenters supported the continued development of real-world data as evidence to demonstrate substantial clinical improvement. Some commenters indicated that would allow applicants greater flexibility to gather evidence in support of new technology add on payment or pass-through either in conjunction with or as a part of their data collection for FDA approval purposes. These commenters indicated that data registries that collect real world data are an important part of modern product development and monitoring. Some commenters supported a non-exhaustive list of the data and findings, including the following: A decreased mortality rate, a reduction in length of stay, a reduced recovery time, a reduced rate of at least one significant complication, a decreased rate of at least one subsequent diagnostic or therapeutic intervention, a reduction in at least one clinically significant adverse event, a decreased number of future hospitalizations or physician visits, a more rapid beneficial resolution of the disease process treatment, an improvement in one or more activities of daily living, or an improved quality of life. Some commenters indicated that CMS should consider other outcomes or findings that would positively impact patient care, and that one such outcome would be anticipated greater medication adherence or compliance. Some commenters indicated that real-world evidence should not be required for meeting the substantial clinical improvement criterion since it may not necessarily be available when a new technology is first approved or cleared by the FDA. Some commenters indicated that if CMS allows real-world evidence to be used for demonstrating substantial clinical improvement, CMS should also consider real-world evidence obtained from markets outside the U.S. since U.S.-based real-world evidence may not be available. Some commenters indicated that while in certain instances real world evidence would be appropriate to supplement other evidence, it would not be appropriate to only rely on the use of real world data. Some commenters indicated that CMS should consider how the FDA and the National Evaluation System for health Technology (NEST) consider real world data.
With respect to indicating that the relevant information for purposes of a finding of substantial clinical improvement may not require a peer-reviewed journal article, many commenters supported this. These commenters indicated that the peer-review process used for publications in medical journals often suffers from long timelines that are often out of the control of the new technology add on payment applicants. These commenters indicated that these lengthy processes can sometimes jeopardize a new technology add on payment or pass-through application, both of which have time limits based on the newness criterion. These commenters believed that peer-reviewed journal articles do play an important role by having studies evaluated through the peer-review process and through the dissemination of the information to the medical community, but peer-review publication should not be a requirement for submission of studies or data for new technology add on payment or pass-through. Some commenters indicated that CMS should accept the documents that evaluate and summarize the clinical study data that is submitted to FDA for review as a part of the FDA approval or clearance process. They indicated that this information and its format are sufficient for FDA to conduct its review and CMS should be able to evaluate the evidence in a similar manner. These commenters indicated that CMS should explicitly state that peer-reviewed publications are not required and that other forms of evidence submission are acceptable for substantial clinical improvement evaluation.
Many commenters supported an approach that if there is a demonstrated substantial clinical improvement based on the use of a new medical service or technology for any subset of beneficiaries, the substantial clinical improvement criterion may be met regardless of the size of that subset patient population. These commenters believed that this is consistent with several of the other policies discussed in the proposed rule, especially to allow for the submission of real-world evidence. These commenters indicated that subgroup analysis is often a key aspect of clinical investigation, and sometimes substantial clinical improvements will apply to a subset of patients. The commenters further indicated that these subsets are sometimes populations without currently adequate treatment options for which a new technology would be particularly beneficial. Some commenters noted that this policy could also help incentivize the development of new anti-infective drugs because new anti-infectives, or anti-infectives that are investigated for new indications, are often studied for particular subpopulations in which there are gaps among the currently available drugs.
Response: As with the comments on longer term changes, CMS appreciates the many comments received regarding potential revisions and clarifications to the substantial clinical improvement criterion beginning with applications received beginning in FY 2020 for IPPS (that is, for FY 2021 and subsequent new technology add-on payment).
We agree with the commenters who indicated that it may be premature to incorporate “broad adoption” into our evaluation of substantial clinical improvement. However, we also believe that many of the ideas supported by commenters are consistent with the principles underlying our existing approach for evaluating substantial clinical improvement. After reviewing the comments we have received, we believe it would helpful to prospectively codify in our regulations at § 412.87 the following aspects of how we evaluate substantial clinical improvement for purposes of new technology add-on payments under the IPPS.
First, and most importantly, the totality of the circumstances is considered when making a determination that a new medical service or technology represents an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
Second, a determination that a new medical service or technology represents an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of Medicare beneficiaries means:
- The new medical service or technology offers a treatment option for a patient population unresponsive to, or ineligible for, currently available treatments; or
- The new medical service or technology offers the ability to diagnose a medical condition in a patient population where that medical condition is currently undetectable, or offers the ability to diagnose a medical condition earlier in a patient population than allowed by currently available methods, and there must also be evidence that use of the new medical service or technology to make a diagnosis affects the management of the patient; or
- The use of the new medical service or technology significantly improves clinical outcomes relative to services or technologies previously available as demonstrated by one or more of the following: A reduction in at least one clinically significant adverse event, including a reduction in mortality or a clinically significant complication; a decreased rate of at least one subsequent diagnostic or therapeutic intervention; a decreased number of future hospitalizations or physician visits; a more rapid beneficial resolution of the disease process treatment including, but not limited to, a reduced length of stay or recovery time; an improvement in one or more activities of daily living; an improved quality of life; or, a demonstrated greater medication adherence or compliance; or,
- The totality of the circumstances otherwise demonstrates that the new medical service or technology substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
Third, evidence from the following published or unpublished information sources from within the United States or elsewhere may be sufficient to establish that a new medical service or technology represents an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of Medicare beneficiaries: Clinical trials, peer reviewed journal articles; study results; meta-analyses; consensus statements; white papers; patient surveys; case studies; reports; systematic literature reviews; letters from major healthcare associations; editorials and letters to the editor; and public comments. Other appropriate information sources may be considered. This is consistent with our current approach, as discussed in the proposed rule, in which we accept a wide range of data and other evidence to support the conclusion of substantial clinical improvement.
Fourth, the medical condition diagnosed or treated by the new medical service or technology may have a low prevalence among Medicare beneficiaries. This is consistent with our current approach, in which we do not require a certain prevalence among Medicare beneficiaries.
Fifth, the new medical service or technology may represent an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of a subpopulation of patients with the medical condition diagnosed or treated by the new medical service or technology. This is consistent with our current approach, in which the medical service or technology may be a substantial clinical improvement for a subpopulation of patients.
In addition to codifying these at § 412.87, we will consider the other suggestions made by commenters along with review of the comments received in response to our Request for Information in order to continue our critical work in this area and inform our future rulemaking.
8. Alternative Inpatient New Technology Add-On Payment Pathway for Transformative New Devices
Under section 1886(d)(5)(K)(vi) of the Act, a medical service or technology will be considered a “new medical service or technology” if the service or technology meets criteria established by the Secretary after notice and an opportunity for public comment. For a more complete discussion of the establishment of the current criteria for the new technology add-on payment, we refer readers to the September 7, 2001 final rule (66 FR 46913), where we finalized the “substantial improvement” criterion to limit new technology add-on payments under the IPPS to those technologies that afford clear improvements over the use of previously available technologies. Specifically, we stated that we would evaluate a request for new technology add-on payments against the following criteria to determine if the new medical service or technology would represent a substantial clinical improvement over existing technologies:
- The device offers a treatment option for a patient population unresponsive to, or ineligible for, currently available treatments.
- The device offers the ability to diagnose a medical condition in a patient population where that medical condition is currently undetectable or offers the ability to diagnose a medical condition earlier in a patient population than allowed by currently available methods. There must also be evidence that use of the device to make a diagnosis affects the management of the patient.
- Use of the device significantly improves clinical outcomes for a patient population as compared to currently available treatments. We also noted examples of outcomes that are frequently evaluated in studies of medical devices. (We note our codification of certain aspects of our evaluation of the substantial clinical improvement criterion as discussed in section II.H.7. of this preamble.)
In the September 7, 2001 final rule (66 FR 46913), we stated that we believed the special payments for new technology should be limited to those new technologies that have been demonstrated to represent a substantial improvement in caring for Medicare beneficiaries, such that there is a clear advantage to creating a payment incentive for physicians and hospitals to utilize the new technology. We also stated that where such an improvement is not demonstrated, we continued to believe the incentives of the DRG system would provide a useful balance to the introduction of new technologies. In that regard, we also pointed out that various new technologies introduced over the years have been demonstrated to have been less effective than initially believed, or in some cases even potentially harmful. We stated that we believe that it is in the best interest of Medicare beneficiaries to proceed very carefully with respect to the incentives created to quickly adopt new technology.
Since 2001 when we first established the substantial clinical improvement criterion, the FDA programs for helping to expedite the development and review of transformative new technologies that are intended to treat serious conditions and address unmet medical needs (referred to as FDA's expedited programs) have continued to evolve in tandem with advances in medical innovations and technology. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19371), we noted that at the time of the development of the September 7, 2001 final rule, devices were the predominant new technology entering the market and, therefore, the substantial clinical improvement criterion was developed with innovative new devices as a focus. At the time, the FDA had three expedited programs (Priority Review, Accelerated Approval, and Fast Track) for drugs and biologicals and no expedited programs for devices. Now, as described in FDA guidance (available on the website at: https://www.fda.gov/downloads/Drugs/Guidances/UCM358301.pdf and https://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM581664.pdf), there are four expedited FDA programs for drugs (the three expedited FDA programs named above and a fourth, Breakthrough Therapy, which was established in 2012) and one expedited FDA program for devices, the Breakthrough Devices Program. The 21st Century Cures Act (Cures Act) (Pub. L. 144-255) established the Breakthrough Devices Program to expedite the development of, and provide for priority review of, medical devices and device-led combination products that provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions and which meet one of the following four criteria: That represent breakthrough technologies; for which no approved or cleared alternatives exist; that offer significant advantages over existing approved or cleared alternatives, including the potential, compared to existing approved alternatives, to reduce or eliminate the need for hospitalization, improve patient quality of life, facilitate patients' ability to manage their own care (such as through self-directed personal assistance), or establish long-term clinical efficiencies; or the availability of which is in the best interest of patients.
In the proposed rule, we explained that some stakeholders over the years have requested that new technologies that receive marketing authorization and are part of an FDA expedited program be deemed as representing a substantial clinical improvement for purposes of the inpatient new technology add-on payments, even in the initial rulemaking on this issue. We understand this request would arguably create administrative efficiency because some stakeholders currently view the two sets of criteria as the same, overlapping, similar, or otherwise duplicative or unnecessary. As discussed in the September 7, 2001 final rule in which we initially adopted the requirement that a new technology must represent a substantial clinical improvement, we proposed to consult a Federal panel of experts in evaluating new technology under the “substantial improvement” criterion. A commenter believed the panel would be unnecessary and that CMS should automatically deem drugs and biologicals approved by FDA that were included in its expedited programs (which the commenter referred to as “fast track” processes) as new technology (66 FR 46914). We stated in response that the panel would consider all relevant information (including FDA expedited program approval) in making its determinations. However, we stated that we did not envision an automatic approval process.
Since 2001, we have continued to receive similar comments. More recently, in response to the FY 2019 New Technology Town Hall meeting notice (83 FR 50379) and the meeting, a commenter stated that the Food and Drug Administration Modernization Act of 1997 authorized a category of medical devices that are eligible for FDA Priority Review designation (83 FR 20278). The commenter explained that, to qualify, products must be designated by the FDA as offering the potential for significant improvements in the diagnosis or treatment of the most serious illnesses, including those that are life-threatening or irreversibly debilitating. The commenter indicated that the processes by which products meeting the statutory standard for priority review are considered by the FDA are specified in greater detail in FDA's Expedited Access Pathway Program, and in the 21st Century Cures Act. The commenter believed that the criteria for FDA Priority Review designation of devices are very similar to the substantial clinical improvement criteria and, therefore, devices used in the inpatient setting determined to be eligible for expedited review and approved by the FDA should automatically be considered as meeting the substantial clinical improvement criterion, without further consideration by CMS.
As we discussed in the proposed rule, the Administration is committed to addressing barriers to healthcare innovation and ensuring Medicare beneficiaries have access to critical and life-saving new cures and technologies that improve beneficiary health outcomes. As detailed in the President's FY 2020 Budget, HHS is pursuing several policies that will instill greater transparency and consistency around how Medicare covers and pays for innovative technology.
Therefore, given the FDA programs for helping to expedite the development and review of transformative new drugs and devices that meet expedited program criteria (that is, new drugs and devices that treat serious or life-threatening diseases or conditions for which there is an unmet medical need), we considered whether it would also be appropriate to similarly facilitate access to these transformative new technologies for Medicare beneficiaries taking into consideration that marketing authorization (that is, Premarket Approval (PMA); 510(k) clearance; the granting of a De Novo classification request; or approval of a New Drug Application (NDA)) for a product that is the subject of one of FDA's expedited programs could lead to situations where the evidence base for demonstrating substantial clinical improvement in accordance with CMS' current standard has not fully developed at the time of FDA marketing authorization (that is, PMA; 510(k) clearance; the granting of a De Novo classification request; or approval of a NDA) (as applicable). (We note a biological product can be the subject of an expedited program as the subject of the FDA's Biologics License Application (BLA).) We also considered whether FDA marketing authorization of a product that is part of an FDA expedited program is evidence that the product is sufficiently different from existing products for purposes of newness.
After consideration of these issues, and consistent with the Administration's commitment to addressing barriers to healthcare innovation and ensuring Medicare beneficiaries have access to critical and life-saving new cures and technologies that improve beneficiary health outcomes, we concluded that it would be appropriate to develop an alternative pathway for transformative medical devices. In situations where a new medical device is part of the Breakthrough Devices Program and has received FDA marketing authorization (that is, the device has received PMA; 510(k) clearance; or the granting of a De Novo classification request), we proposed an alternative inpatient new technology add-on payment pathway to facilitate access to this technology for Medicare beneficiaries (84 FR 19372).
Specifically, we proposed that, for applications received for new technology add-on payments for FY 2021 and subsequent fiscal years, if a medical device is part of the FDA's Breakthrough Devices Program and received FDA marketing authorization, it would be considered new and not substantially similar to an existing technology for purposes of the new technology add-on payment under the IPPS. In light of the criteria applied under the FDA's Breakthrough Device Program, and because the technology may not have a sufficient evidence base to demonstrate substantial clinical improvement at the time of FDA marketing authorization, we also proposed that the medical device would not need to meet the requirement under § 412.87(b)(1) that it represent an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries. We proposed to add a new paragraph (c) under § 412.87 to codify this proposed policy; existing paragraph (c) would be redesignated as paragraph (d) and amendments would be made to proposed redesignated paragraph (d) to reflect this proposed alternative pathway and to make clear that a new medical device may only be approved under § 412.87(b) or proposed new § 412.87(c). Under this proposed alternative pathway, a medical device that has received FDA marketing authorization (that is, has been approved or cleared by, or had a De Novo classification request granted by, the FDA) and that is part of the FDA's Breakthrough Devices Program would need to meet the cost criterion under § 412.87(b)(3), as reflected in proposed new § 412.87(c)(3), and would be considered new as reflected in proposed § 412.87(c)(2).
Given the lack of an evidence base to demonstrate substantial clinical improvement at the time of FDA marketing authorization, we solicited public comment on how CMS should weigh the benefits of this proposed alternative pathway to facilitate beneficiary access to transformative new medical devices, including the benefits of mitigating potential delayed access to innovation and adoption, against any potential risks, such as the risk of adverse events or negative outcomes that might come to light later.
As discussed in the proposed rule (84 FR 19373), for the reasons discussed in section I.O. of Appendix A to the proposed rule, we did not propose an alternative inpatient new technology add-on payment pathway for drugs at this time. In that section, we stated that while we continue to work on these initiatives for drug affordability, we believed that it was appropriate to distinguish between drugs and devices in our consideration of a proposed policy change for transformative new technologies (84 FR 19672).
Comment: The majority of commenters supported our proposed alternative new technology add-on payment pathway for a new medical device that is part of the Breakthrough Devices Program and has received FDA marketing authorization. In general, these commenters agreed that this policy will afford an opportunity to gather evidence to demonstrate substantial clinical improvement while enhancing hospital adoption, which will increase beneficiary access to new technologies that improve health outcomes. Some of the other reasons cited by commenters who supported this proposed policy include reduced burden and redundancy, improved administrative efficiency, greater transparency, predictability and certainty in the regulatory and reimbursement processes, and consistency across federal programs, including support of greater interagency collaboration between CMS and FDA. In particular, some of the commenters who expressed support for this policy indicated that they believe that the FDA's Breakthrough Device program is designed to appropriately balance benefits to patients with life threatening illnesses against potential risks for devices that receive marketing authorization.
Some commenters urged CMS not to adopt this proposed alternative new technology add-on payment pathway for certain transformative medical devices. These commenters believe that devices that receive market authorization through FDA's Breakthrough Device program are unlikely to include data applicable to the Medicare beneficiary population, and have more uncertainty of benefit than the current evidence standard under the current new technology add-on payment policy. As such they believe this proposed policy, if finalized, would offer a financial incentive for the use of such transformative medical devices without improving clinical outcomes for beneficiaries.
A few commenters, notwithstanding their general support for the proposal, expressed uncertainty about adopting the proposed policy, because the FDA's Breakthrough Device program is still relatively new. These commenters recommend that CMS continue to work jointly with FDA to understand the achievements and challenges of this program as it progresses. A few other commenters conditionally supported the adoption of the proposal, indicating that they believe an expansion of the evidence standard for establishing substantial clinical improvements could be preferable to eliminating the substantial clinical improvement criterion for medical devices that have received FDA market authorization and are subject to the Breakthrough Device Program. In contrast, another commenter indicated because new technology add-on payments result in an additional cost to the Medicare program, CMS should ensure that clinical benefit is clearly established before approving any technology under the new technology add-on payment policy.
Other commenters also expressed concerns about the proposed policy. Specifically, with respect to a medical device that receives a 510(k) clearance, some commenters stated it would not be appropriate to consider a product “new and not substantially similar” to an existing technology when the 510(k) clearance process is based on a predicate device and can be met by demonstrating that it is substantially equivalent to a medical device already on the market. Most of these same commenters, however, did support that devices that receive either a PMA approval or for which FDA has granted a De Novo classification request would be considered new, stating their belief that such FDA designations indicate that such a medical device would not be substantially similar to an existing technology.
We also received comments requesting that CMS extend or develop similar alternative new technology add-on payment pathways for all expedited FDA pathways (for example, Fast Track, Accelerated Approval, Breakthrough Therapy, and Priority Review, including Qualified Infectious Disease Products (QIDPs)), as well as other categories of technologies such as those with a Regenerative Medicine Advanced Therapy (RMAT) designation, devices granted a Humanitarian Device Exemption (HDE), and those that do not currently fit into existing CMS benefit categories, such as Software as a Medical Device (SaMD). In particular, many of these commenters explicitly urged CMS to expand the proposed policy to include drugs that have also received Breakthrough Therapy designation from the FDA, arguing that the rationale to and CMS's stated goal of the proposal to facilitate access to technology for Medicare beneficiaries applies equally to all technologies that receive market authorization under an expedited FDA pathway. Some of these commenters stated their belief that contrary to CMS's assumptions, the current drug-pricing system does not provide generous incentives for innovation, and argued that instead costly innovative drugs, which are not separately or adequately reimbursed in inpatient settings, can lead to a significant barrier to access for new treatment options for beneficiaries. Other commenters argued that CMS should have a consistent new technology add-on payment policy for all “breakthrough” technologies, that is, devices and drugs that have received FDA marketing authorization and are subject to an expedited FDA program. These commenters indicated that there is no reason for CMS to adopt inconsistent reimbursement policies for technologies that are market authorized as the subject of an expedited FDA program just because one technology is a device and the other is a drug. They believe the data and requirements needed to support a Breakthrough Therapy designation are as sufficient for new technology add-on payment purposes for drugs as the Breakthrough Device Program requirements are for devices. In advocating that CMS consider expanding the proposal to include drugs that receive market authorization as part of an expedited FDA program, it was suggested that CMS could also consider including additional criteria to qualify under an alternative pathway; for example, if a drug improves patient quality of life, produces long-term clinical treatment efficiencies, or such other criteria as specified by the Secretary.
Several commenters urged CMS to extend the proposed alternative new technology add-on payment pathway to a product that is designated by the FDA as a QIDP. The commenters expressed significant concerns related to the public health crisis represented by antimicrobial resistance, which occurs when germs like bacteria and fungi develop the ability to resist drugs designed to kill them. The Federal Food, Drug, and Cosmetic Act defines QIDPs as “an antibacterial or antifungal drug for human use intended to treat serious or life-threatening infections, including those caused by (1) an antibacterial or antifungal resistant pathogen, including novel or emerging infectious pathogens; or (2) qualifying pathogens listed by the Secretary . . . .” [312] These commenters asserted that timely access to appropriate antimicrobial therapy is key to clinical success and improved patient outcomes. They further maintained that resistant infections result in higher costs to healthcare systems, including Medicare, because patients experience illnesses of a longer duration, require additional tests, and require the use of more expensive drugs and related services. These commenters believed extending the proposed alternative new technology add-on payment pathway to QIDPs would be one way to address regulatory barriers and payment disincentives to innovation related to antimicrobial resistance, while improving Medicare beneficiaries' access to new treatments that improve health outcomes and save lives.
Some commenters who supported the proposal also encouraged CMS to consider other changes to the new technology add-on payment policy, such as further revising and clarifying the substantial clinical improvement criteria (as also discussed in the proposed rule), updating or eliminating the “substantial similarity” criteria (stating those criteria are not required by statute), and adopting a policy to automatically assess new MS-DRG creation or assignment for new technologies when their new technology add-on payment status expires.
Lastly, several commenters that supported this proposal also recommended that CMS likewise expedite beneficiary access to “breakthrough” devices in the outpatient hospital setting by adopting a similar pathway to obtain OPPS pass-through device status.
Response: We appreciate the commenters' support of the proposed alternative new technology add-on payment pathway for a new medical device that is part of the Breakthrough Devices Program and has received FDA marketing authorization. As discussed in the proposed rule and as previously discussed in this final rule, after considering that the evidence base to demonstrate substantial clinical improvement may not be fully developed at the time of FDA marketing authorization, we proposed an alternative inpatient new technology add on payment pathway to facilitate access for Medicare beneficiaries to new medical devices that are part of the Breakthrough Devices Program and have received FDA marketing authorization. It is for this reason that we believe that with respect to these technologies, even though, as some commenters assert, there may be less certainty of clinical benefit or data representing the Medicare beneficiary population as compared to the evidence standard for substantial clinical improvement under the current new technology add-on payment policy, we believe the benefits of providing early access to critical and life-saving new cures and technologies that improve beneficiary health outcomes support establishing this alternative pathway. While we appreciate the commenter's concern regarding additional Medicare program expenditures, for the previously stated reasons, we believe it is appropriate to facilitate beneficiary access to transformative new medical devices by establishing an alternative pathway for a device that receives FDA marketing authorization and is subject to the FDA's Breakthrough Devices Program that does not require substantial clinical improvement be demonstrated as a condition of approval because the evidence base to demonstrate substantial clinical improvement may not be fully developed at the time of FDA marketing authorization for such devices.
We agree with commenters that this policy supports greater interagency collaboration between CMS and FDA, and CMS is committed to continue to work collaboratively with the FDA as the FDA's expedited programs, including the Breakthrough Devices Program, evolve. We refer commenters that conditionally supported the adoption of the proposed alternative pathway, but preferred that the evidence standard for establishing substantial clinical improvement be expanded, to the discussion of substantial clinical improvement in section II.H.7. of this final rule. With respect to commenters that expressed concern regarding the “newness” criterion for a medical device that receives a 510(k) clearance under the proposed alternative new technology add-on payment pathway for transformative medical devices, we do not agree that such a product cannot be “new and not substantially similar” to an existing technology for purposes of the new technology add-on payment policy. FDA's clearance of a 510(k) is based on a determination that the device at issue is “substantially equivalent” to a legally marketed (predicate) device, which is not subject to PMA. As we have discussed in prior rulemakings, under our current policy, a new technology, including a device that receives a 510k clearance, can be considered “new” for purposes of the new technology add-on payment if it does not meet at least one of the three substantial similarity criteria (and therefore would not be considered substantially similar to an existing technology). (For a detailed discussion of the criteria for substantial similarity, we refer readers to the FY 2006 IPPS final rule (70 FR 47351 through 47352) and the FY 2010 IPPS/LTCH PPS final rule (74 FR 43813 through 43814).) Therefore, we believe it is appropriate to include a device that has received PMA, 510(k) clearance, or has been granted a De Novo classification request for FDA marketing authorization under the alternative inpatient new technology add-on payment pathway for transformative new devices.
In response to comments that requested that the proposed alternative inpatient new technology add-on payment pathway be extended to, or an alternative pathway similarly be created for, drugs and biologicals (that is, Priority Review, Accelerated Approval, Fast Track, and Breakthrough Therapy), we recognize that the goal of facilitating access to new technologies for Medicare beneficiaries could also apply to these designations. However, as we discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19373 and 19672), we believed that making this policy applicable to drugs would further incentives for innovation but without decreasing cost, a key priority of this Administration. As we also stated in the proposed rule, while we continue to work on initiatives for drug affordability, we believe that it is appropriate to distinguish between drugs and devices in our consideration of a proposed policy change for transformative new technologies, and therefore we disagree with commenters that there is no reason to adopt different new technology add-on payment policies for devices and drugs that receive market authorization and are subject to an expedited FDA pathway. We continue to believe that it is appropriate to distinguish between drugs and devices in our consideration of a policy change for transformative new technologies while we continue to work on these initiatives for drug affordability for the reasons stated in the proposed rule. Therefore we are not applying this alternative inpatient new technology add-on payment pathway in situations where a new drug designated for or approved under an FDA expedited program for drugs has received FDA marketing authorization. We will continue to consider this issue for future rulemaking, including the suggestion to develop additional criteria to qualify under an alternative pathway for technologies that receive FDA marketing authorization under or are designated for an FDA expedited program for drugs.
While we are not applying this alternative inpatient new technology add-on payment pathway to new drugs more generally, we understand and share commenters' concerns related to antimicrobial resistance and its serious impact on Medicare beneficiaries and public health overall. The Center for Disease Control and Prevention (CDC) describes antimicrobial resistance as “one of the biggest public health challenges of our time.” [313] We believe Medicare beneficiaries may be disproportionately impacted by antimicrobial resistance due in large part to the elderly's unique vulnerability to drug-resistant infections (e.g., due to age-related and/or disease-related immunosuppression, greater pathogen exposure from via catheter use). Medicare beneficiaries account for the majority of cases of both new diagnoses of antimicrobial resistant infections (approximately 62 percent) and the resulting deaths (approximately 65 percent) in hospitals in the United States.[314] Antimicrobial resistance results in a substantial number of additional hospital days for Medicare beneficiaries (estimated to be more than 600,000 additional days each year), resulting in significant unnecessary health care expenditures.[315] While we continue to believe, for the reasons stated, that it is appropriate to distinguish between drugs and devices in the application of an alternative new technology add-on payment pathway, after consideration of these specific concerns and consistent with the Administration's commitment to address issues related to antimicrobial resistance, in order to help secure access to antibiotics, and improve health outcomes for Medicare beneficiaries in a manner that is as expeditious as possible, at this time we believe it would be appropriate to extend the proposed alternative new technology add-on payment pathway to a product that is designated by the FDA as a QIDP. Therefore, under our finalized policy we are providing that for applications received for new technology add-on payments for FY 2021 and subsequent fiscal years, if a technology receives the FDA's QIDP designation and received FDA marketing authorization, it will be considered new and not substantially similar to an existing technology for purposes of new technology add-on payments and will not need to meet the requirement that it represent an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
Regarding the requests to develop an alternative pathway for new technology add-on payments for other special designations (other than those that receive market authorization under an expedited FDA pathway as previously discussed), while we recognize that the goal of facilitating access to new technologies for Medicare beneficiaries could also apply to other designations, in general we believe it is prudent to gain experience under this new alternative pathway for certain transformative new devices before expanding it to other special designations to allow us to evaluate the benefits of this proposed alternative pathway to facilitate beneficiary access to transformative new medical devices as well as any other considerations that may come to light after application of this new pathway. We will keep these suggestions in mind for consideration in future rulemaking.
With respect to the commenters that recommended other changes to the IPPS new technology add-on payment policy, we appreciate these suggestions and will take them into consideration for future rulemaking. In addition, we note that we are proposing to adopt a similar pathway to obtain OPPS pass-through status for medical devices that receive FDA marketing authorization and are part of the FDA's Breakthrough Devices Program in the CY 2020 OPPS/ASC proposed rule.
Therefore, after consideration of public comments, we are finalizing our proposed alternative new technology add-on payment pathway for certain medical devices and, for the reasons discussed above, we are also extending that alternative new technology add-on payment pathway to a product that is designated by the FDA as a QIDP. Therefore, for applications received for new technology add-on payments for FY 2021 and subsequent fiscal years, if a medical device is part of the FDA's Breakthrough Devices Program or a product is designated by the FDA as a QIDP, and received FDA marketing authorization, it will be considered new and not substantially similar to an existing technology for purposes of the new technology add-on payment under the IPPS, and not need to meet the requirement that it represent an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries. We are also adopting our proposed changes to § 412.87 to codify this proposed policy, as modified to reflect the finalized alternative pathway for QIDPs.
Specifically, to codify this final policy, under § 412.87 we are adding new paragraphs (c) and (d) and redesignating existing paragraph (c) as paragraph (e); redesignated paragraph (e) is being amended to reflect these alternative pathways and to make clear that a new medical service or technology may only be approved under § 412.87(b), new § 412.87(c), or new § 412.87(d). Under this alternative pathway for QIDPs, a medical product that has received FDA marketing authorization and is designated by the FDA as a QIDP will need to meet the cost criterion under § 412.87(b)(3), as reflected in new § 412.87(d)(3), and will be considered new as reflected in new § 412.87(d)(2).
In the proposed rule, we further noted that section 1886(d)(5)(K)(ii)(II) of the Act provides for the collection of data with respect to the costs of a new medical service or technology described in subclause (I) for a period of not less than 2 years and not more than 3 years beginning on the date on which an inpatient hospital code is issued with respect to the service or technology. We also invited public comments on whether the newness period under the proposed alternative new technology add-on payment pathway for transformative new medical devices should be limited to a period of time sufficient for the evidence base for the new transformative medical device to develop to the point where a substantial clinical improvement determination can be made (for example, 1 to 2 years after approval, depending on whether the transformative new medical device would be eligible for a third year of new technology add-on payments). We noted that, if we were to adopt such a policy in the future, the proposed amended regulation text would be revised accordingly. We further noted that the newness period for a transformative new medical device cannot exceed 3 years, regardless of whether it is approved under the current eligibility criteria, the proposed alternative pathway, or potentially first under the proposed alternative pathway, and subsequently under the current eligibility criteria later in its newness period.
Comment: Some commenters supported limiting the duration of the payment under the alternative new technology add-on payment pathway for transformative new medical devices to 2 years. These commenters believed that revaluation of available evidence of substantial clinical improvement for the third year achieves an appropriate balance of potential risks with access for new treatment options for beneficiaries.
In contrast, other commenters recommend that the timeframe align with the full eligibility period available under the existing new technology add-on payment policy. That is, the new technology add-on payment should be applicable for not less than 2 years and not more than 3 years to allow sufficient time for CMS to collect hospital cost and claims data to inform MS-DRG assignment and relative weights. These commenters indicated that re-evaluating a device that received marketing authorization as part of the FDA's Breakthrough Devices Program 1 or 2 years after approval may not provide adequate time to collect and evaluate data needed to demonstrate substantial clinical improvement, and believed the full new technology add-on payment policy eligibility period is necessary to ensure Medicare beneficiaries have access to the latest innovations. Commenters also stated that establishing different eligibility timelines for devices approved for new technology add-on payments through the traditional and alternative pathways could limit the development and adoption of devices that are part of the FDA's Breakthrough Devices Program.
Response: We appreciate the feedback and recommendations provided by commenters on limiting the newness period under the proposed alternative new technology add-on payment pathway for transformative new medical devices. We will take these comments in consideration, and may consider adopting such a policy in the future through rulemaking.
9. Change to the Calculation of the Inpatient New Technology Add-On Payment
As noted in the proposed rule and earlier, section 1886(d)(5)(K)(ii)(I) of the Act specifies that a new medical service or technology may be considered for a new technology add-on payment if, based on the estimated costs incurred with respect to discharges involving such service or technology, the DRG prospective payment rate otherwise applicable to such discharges under this subsection is inadequate. As discussed in the September 7, 2001 final rule, in deciding which treatment is most appropriate for any particular patient, it is expected that physicians would balance the clinical needs of patients with the efficacy and costliness of particular treatments. In the May 4, 2001 proposed rule (66 FR 22695), we stated that we believed it is appropriate to limit the additional payment to 50 percent of the additional cost of the new technology to appropriately balance the incentives. We stated that this proposed limit would provide hospitals an incentive for continued cost-effective behavior in relation to the overall costs of the case. In addition, we stated that we believed hospitals would face an incentive to balance the desirability of using the new technology versus the old; otherwise, there would be a large and perhaps inappropriate incentive to use the new technology.
As such, the current calculation of the new technology add-on payment is based on the cost to hospitals for the new medical service or technology. Specifically, under § 412.88, if the costs of the discharge (determined by applying CCRs as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 50 Percent of the costs of the new medical service or technology; or (2) 50 percent of the amount by which the costs of the case exceed the standard DRG payment. Unless the discharge qualifies for an outlier payment, the additional Medicare payment is limited to the full MS-DRG payment plus 50 percent of the estimated costs of the new technology or medical service.
We stated in the FY 2020 IPPS/LTCH PPS proposed rule that since the 50-percent limit to the new technology add-on payment was first established, we have received feedback from stakeholders that our current policy does not adequately reflect the costs of new technology and does not sufficiently support healthcare innovations. For example, stakeholders have stated that a maximum add-on payment of 50 percent does not allow for accurate payment of a new technology with an unprecedented high cost, such as the CAR T-cell technologies KYMRIAH® and YESCARTA® (83 FR 41173).
After consideration of the concerns raised by commenters and other stakeholders, and consistent with the Administration's commitment to addressing barriers to healthcare innovation and ensuring Medicare beneficiaries have access to critical and life-saving new cures and technologies that improve beneficiary health outcomes, we stated in the proposed rule that we agree that there may be merit to the recommendations to increase the maximum add-on amount, and that capping the add-on payment amount at 50 percent could in some cases no longer provide a sufficient incentive for the use of a new technology. Costs of new medical technologies have increased over the years to the point where 50 percent of the estimated cost may not be adequate, and we have received feedback that hospitals may potentially choose not to provide certain technologies for that reason alone.
At the same time, we continue to believe that it is important to preserve the incentives inherent under an average-based prospective payment system through the use of a percentage of the estimated costs of a new technology or service. We stated in the September 7, 2001 final rule (66 FR 46919) that we do not believe it is appropriate to pay an add-on amount equal to 100 percent of the costs of new technology because there is no similar methodology to reduce payments for cost-saving technology. For example, as new technologies permit the development of less-invasive surgical procedures, the total costs per case may begin to decline as patients recover and leave the hospital sooner. Finally, we stated our concern that, because these payments are linked to charges submitted by hospitals, there is the potential that hospitals may adapt their charge structure to maximize payments for DRGs that include eligible new technologies. The higher the marginal cost factor, the greater the incentive hospitals face in this regard.
As noted in the FY 2020 IPPS/LTCH PPS proposed rule, it is challenging to determine empirically a precise payment percentage between the current 50 percent and 100 percent payment that would be the most appropriate. However, we stated that we believed that 65 percent would be an incremental increase that would reasonably balance the need to maintain the incentives inherent to the prospective payment system while also encouraging the development and use of new technologies.
Therefore, in the proposed rule, we proposed that, beginning with discharges on or after October 1, 2019, if the costs of a discharge involving a new technology (determined by applying CCRs as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 65 Percent of the costs of the new medical service or technology; or (2) 65 percent of the amount by which the costs of the case exceed the standard DRG payment. Unless the discharge qualifies for an outlier payment, the additional Medicare payment would be limited to the full MS-DRG payment plus 65 percent of the estimated costs of the new technology or medical service. We also proposed to revise paragraphs (a)(2) and (b) under § 412.88 to reflect these proposed changes to the calculation of the new technology add-on payment amount beginning in FY 2020.
Comment: The vast majority of the comments we received supported an increase in the new technology add-on payment percentage, citing reasons such as providing more adequate payments to hospitals on a per case basis; increased efficacy, effectiveness, and overall quality of patient care; reduction in price barriers that previously may have disincentivized the use of the most innovative technology; and to the extent that more hospitals are able to adopt technologies approved for new technology add-on payments as a result of higher Medicare payments, the more claims data will be available to fully reflect the costs of these technologies in and improve the accuracy of MS-DRG weights. Some commenters indicated that they remained concerned that hospitals will continue to endure a significant shortfall between their costs and their payments when using technologies approved for new technology add-on payments, even with the proposed increase to 65 percent. These commenters believed that even if the payment percentage were increased to 65 percent, a hospital that provides a costly medical service or technology that qualifies for a for new technology add-on payment would still lose money on the case regardless of how efficient it is. Therefore, these commenters stated that an increase to only 65 percent would not be adequate to accomplish CMS's stated goals of addressing barriers to healthcare innovation and ensuring Medicare beneficiaries have access to critical and life-saving new cures and technologies that improve beneficiary health outcomes.
While commenters generally supported the proposed increase in the new technology add-on payment percentage, many indicated that a percentage between 80 and 100 percent would be more appropriate to sufficiently incentivize the use of new technologies and ensure Medicare beneficiaries' access to innovations in care and improved health outcomes. A few commenters stated that the proposal to increase the new technology add-on payment percentage from 50 percent to 65 percent was consistent with CMS's stated goals of addressing barriers to healthcare innovation and ensuring Medicare beneficiaries access to new technologies. Similarly, MedPAC indicated that a percentage up to 65 should be sufficient to achieve access given the continued growth in the number of new technology applications.
Many commenters stated that a strong case could be made that the new technology add-on payment percentage should be higher than 65 percent. Some commenters encouraged CMS to consider setting the percentage as close to 100 percent as possible, indicating that any percentage that is less than 100 percent would continue to provide a disincentive for appropriate use of a new technology. The majority of commenters suggested that the most appropriate new technology add-on payment amount increase would be 80 percent; however, there were also commenters that suggested new technology add-on payment amount increases of 75, 85 and 100 percent. Commenters who supported an increase to 80 percent indicated a variety of reasons, including that 80 percent strikes an appropriate balance of including a cost sharing element with the hospitals for new technologies, alleviates enough of the financial disincentive to allow hospitals to provide greater access to Medicare patients who may benefit from these innovative technologies, preserves the incentives inherent under the MS-DRG payment system without creating an undue financial burden, and encourages more swift adoption of new technologies. Several commenters indicated that increasing the new technology add-on payment percentage to 80 percent would be consistent with other CMS shared-risk mechanisms, and in particular it would align with the IPPS outlier payment, under which hospitals are reimbursed based on a marginal cost factor equal to 80 percent of the combined operating and capital costs in excess of the fixed-loss threshold.
Some commenters also pointed to an analysis by Avalere Health LLC that they state found that despite receiving $40.5 million in new technology add-on payments between FY 2006 and FY 2013, hospitals also received $23.2 million in outlier payments on these same cases. These commenters believe that the fact that so many new technology add-on payment cases also qualify for outlier payments underscores how inadequate the new technology add-on payment is, and they state that for this reason they believe that an 80 percent level would mitigate those losses, further encourage adoption of new technologies, and continue to provide incentives for hospitals to act as prudent purchasers. A few commenters also indicated that although an 80 percent new technology add-on payment percentage would not fully compensate all hospitals for the cost of using new technologies, it would bring CMS closer to fulfilling the statutory obligation to make payments in “an amount that adequately reflects the estimated average cost of such service or technology.”
While most commenters indicated that the percentage should be raised uniformly for all technologies approved for new technology add-on payments, some commenters indicated that the percentage for certain technologies (for example, CAR T-cell therapy) needed to be higher, up to 100 percent, due to the high cost of the therapy, while other commenters pointed to other specific types of new technologies where they indicated that the new technology add-on payment percentage should be higher. In particular, several commenters urged CMS to adopt a new technology add-on payment percentage of 100 percent for products designated by the FDA as QIDPs given the significant concerns they expressed related to the public health crisis represented by antimicrobial resistance (as further described in section II.H.8. of this preamble). Some of these commenters further urged CMS to at least finalize a policy that would provide for an increased percentage for QIDPs above the proposed 65 percent, for example, 80 percent or 90 percent, if a maximum percentage of 100 percent for QIDPs was not adopted. As discussed in section II.H.8. of this preamble where we discuss our finalized policy to extend the alternative new technology add-on payment pathway for certain transformative medical devices to QIDPs, these commenters asserted that timely access to appropriate antimicrobial therapy is key to clinical success and improved patient outcomes. In addition, they maintained that resistant infections result in higher costs to healthcare systems, including Medicare, because patients experience illnesses of a longer duration, require additional tests, and require the use of more expensive drugs and related services. These commenters asserted that further increasing the new technology add-on payment percentage for QIDPs above the proposed 65 percent (and specifically, to between 80 to 100 percent) would address regulatory barriers and payment disincentives to innovation related to antimicrobial resistance, while improving Medicare beneficiaries' access to new treatments that improve health outcomes and save lives.
Commenters also suggested CMS consider other modifications to the new technology add-on payment policy, such as no longer using the current “lesser of” methodology and instead making a uniform add-on payment for all new technology cases, using the acquisition cost reported on the claim as the basis for the add-on payment amount, and establishing a more frequent inpatient new technology add-on payment policy approval process.
Response: We appreciate the commenters' support for the proposed increase in the new technology add-on payment percentage. As discussed in the proposed rule and previously in this final rule, it is challenging to determine empirically a precise payment percentage between the current 50 percent and 100 percent payment that would reasonably balance the need to maintain the incentives inherent to the prospective payment system while also encouraging the development and use of new technologies. In response to commenters that encouraged CMS to consider setting the percentage as close to 100 percent as possible, indicating that any percentage that is less than 100 percent would continue to provide a disincentive for appropriate use of a new technology, we strongly disagree. Setting the percentage as close to 100 percent as possible maintains very little of the incentives inherent to the prospective payment system. In response to commenters who suggested that the most appropriate new technology add-on payment amount increase would be in the 75 or 80 percent range, while we agree this would better maintain the incentives for cost-effective behavior than a 100 percent payment, we do not believe there is evidence that a payment in this range is required to ensure appropriate access to new technologies. We also disagree that the new technology add-on payment amount should necessarily align with the IPPS outlier payment methodology. We note that there are different policy considerations for new technology payments and outlier payments. We also disagree that the existence of outlier payments for some new technology cases is evidence that those payments are necessarily inadequate, as there may be unrelated reasons why a hospital would receive outlier payments. There may also be circumstances where new technology payments and outlier payments work in a complimentary manner for related reasons, that do not necessarily mean the appropriate policy is to increase new technology payments; for example, we note that MedPAC in its comment letter recommended that CAR T-cell therapy continue to be paid in FY 2020 using a combination of new technology add-on payments and outlier payments. Lastly, we generally disagree that our proposed 65 percent payment does not adequately reflect the estimated average cost of a new technology. Commenters did not cite evidence that our proposed 65 percent payment, a 30 percent increase (= (0.65/0.50)−1)) over the current 50 percent payment, would generally be an insufficient incremental increase to ensure appropriate access to new technologies.
However, while we generally disagree with commenters that our proposed 65 percent new technology add-on payment would be inadequate, as noted earlier in section II.H.8, we understand and share commenters' concerns related to antimicrobial resistance and its serious impact on Medicare beneficiaries and public health overall. As we noted in that section, the Center for Disease Control and Prevention (CDC) describes antimicrobial resistance as “one of the biggest public health challenges of our time.” We believe Medicare beneficiaries may be disproportionately impacted by antimicrobial resistance due in large part to the elderly's unique vulnerability to drug-resistant infections (e.g., due to age-related and/or disease-related immunosuppression, greater pathogen exposure from via catheter use). As such, antimicrobial resistance results in a substantial number of additional hospital days for Medicare beneficiaries, resulting in significant unnecessary health care expenditures. Although we continue to believe, for the reasons discussed, that our proposed new technology add-on payment percentage of 65 percent is generally appropriate, after consideration of these specific concerns and consistent with the Administration's commitment to address issues related to antimicrobial resistance, in order to help secure access to antibiotics, and improve health outcomes for Medicare beneficiaries in a manner that is as expeditious as possible, at this time we believe it would be appropriate to apply a higher new technology add-on payment of 75 percent for a product that is designated by the FDA as a QIDP and receives FDA marketing authorization.
With regard to the comments that requested an increase to the new technology add-on payment percentage for CAR T-cell therapy, as we discuss in greater detail in section II.F.2.c. of this preamble, after a review of the comments received, we continue to believe, similar to last year, that given the relative newness of CAR T-cell therapy, and our continued consideration of approaches and authorities to encourage value-based care and lower drug prices, it would be premature to adopt structural changes to our existing payment mechanisms, either under the IPPS or for IPPS-excluded cancer hospitals, specifically for CAR T-cell therapy. For these reasons, we are not adopting the commenters' requested changes to our current payment mechanisms for FY 2020, including, but not limited to, structural changes in new technology add-on payments and/or a differentially higher new technology add-on payment percentage specifically for CAR T-cell therapy products. (For additional details on the comments we received in response to our request for public comment on payment alternatives for CAR T-cell cases that was included in the proposed rule, and our responses, refer to section II.F.2.c. of the preamble of this final rule.)
We appreciate the commenters' suggestions for other modifications to the new technology add-on payment policy, such as making a uniform add-on payment, using the acquisition cost reported on the claim as the basis for the add-on payment, and developing a more frequent approval process, and will consider them for future rule-making.
After consideration of public comments, we are finalizing an increase in the new technology add-on payment percentage. Specifically, for a new technology other than a medical product designated by the FDA as a QIDP, beginning with discharges on or after October 1, 2019, if the costs of a discharge involving a new technology (determined by applying CCRs as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 65 percent of the costs of the new medical service or technology; or (2) 65 percent of the amount by which the costs of the case exceed the standard DRG payment. For a new technology that is a medical product designated by the FDA as a QIDP, beginning with discharges on or after October 1, 2019, if the costs of a discharge involving a new technology (determined by applying CCRs as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 75 percent of the costs of the new medical service or technology; or (2) 75 percent of the amount by which the costs of the case exceed the standard DRG payment. Under this finalized policy, unless the discharge qualifies for an outlier payment, the additional Medicare payment will be limited to the full MS-DRG payment plus 65 percent (or 75 percent for a medical product designated by the FDA as a QIDP) of the estimated costs of the new technology or medical service. We are also finalizing our proposed revisions to paragraphs (a)(2) and (b) under § 412.88 to reflect these changes to the calculation of the new technology add-on payment amount beginning in FY 2020, as modified to reflect the finalized percentage for a medical product designated by the FDA as a QIDP.
II. Changes to the Hospital Wage Index for Acute Care Hospitals
A. Background
1. Legislative Authority
Section 1886(d)(3)(E) of the Act requires that, as part of the methodology for determining prospective payments to hospitals, the Secretary adjust the standardized amounts for area differences in hospital wage levels by a factor (established by the Secretary) reflecting the relative hospital wage level in the geographic area of the hospital compared to the national average hospital wage level. We currently define hospital labor market areas based on the delineations of statistical areas established by the Office of Management and Budget (OMB). A discussion of the FY 2020 hospital wage index based on the statistical areas appears under section III.A.2. of the preamble of this final rule.
Section 1886(d)(3)(E) of the Act requires the Secretary to update the wage index annually and to base the update on a survey of wages and wage-related costs of short-term, acute care hospitals. (CMS collects these data on the Medicare cost report, CMS Form 2552-10, Worksheet S-3, Parts II, III, and IV. The OMB control number for approved collection of this information is 0938-0050, which expires on March 31, 2022.) This provision also requires that any updates or adjustments to the wage index be made in a manner that ensures that aggregate payments to hospitals are not affected by the change in the wage index. The adjustment for FY 2020 is discussed in section II.B. of the Addendum to this final rule.
As discussed in section III.I. of the preamble of this final rule, we also take into account the geographic reclassification of hospitals in accordance with sections 1886(d)(8)(B) and 1886(d)(10) of the Act when calculating IPPS payment amounts. Under section 1886(d)(8)(D) of the Act, the Secretary is required to adjust the standardized amounts so as to ensure that aggregate payments under the IPPS after implementation of the provisions of sections 1886(d)(8)(B), (d)(8)(C), and (d)(10) of the Act are equal to the aggregate prospective payments that would have been made absent these provisions. The budget neutrality adjustment for FY 2020 is discussed in section II.A.4.b. of the Addendum to this final rule.
Section 1886(d)(3)(E) of the Act also provides for the collection of data every 3 years on the occupational mix of employees for short-term, acute care hospitals participating in the Medicare program, in order to construct an occupational mix adjustment to the wage index. A discussion of the occupational mix adjustment that we are applying to the FY 2020 wage index appears under sections III.E.3. and F. of the preamble of this final rule.
2. Core-Based Statistical Areas (CBSAs) for the FY 2020 Hospital Wage Index
The wage index is calculated and assigned to hospitals on the basis of the labor market area in which the hospital is located. Under section 1886(d)(3)(E) of the Act, beginning with FY 2005, we delineate hospital labor market areas based on OMB-established Core-Based Statistical Areas (CBSAs). The current statistical areas (which were implemented beginning with FY 2015) are based on revised OMB delineations issued on February 28, 2013, in OMB Bulletin No. 13-01. OMB Bulletin No. 13-01 established revised delineations for Metropolitan Statistical Areas, Micropolitan Statistical Areas, and Combined Statistical Areas in the United States and Puerto Rico based on the 2010 Census, and provided guidance on the use of the delineations of these statistical areas using standards published in the June 28, 2010 Federal Register (75 FR 37246 through 37252). We refer readers to the FY 2015 IPPS/LTCH PPS final rule (79 FR 49951 through 49963) for a full discussion of our implementation of the OMB labor market area delineations beginning with the FY 2015 wage index.
Generally, OMB issues major revisions to statistical areas every 10 years, based on the results of the decennial census. However, OMB occasionally issues minor updates and revisions to statistical areas in the years between the decennial censuses through OMB Bulletins. On July 15, 2015, OMB issued OMB Bulletin No. 15-01, which provided updates to and superseded OMB Bulletin No. 13-01 that was issued on February 28, 2013. The attachment to OMB Bulletin No. 15-01 provided detailed information on the update to statistical areas since February 28, 2013. The updates provided in OMB Bulletin No. 15-01 were based on the application of the 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas to Census Bureau population estimates for July 1, 2012 and July 1, 2013. In the FY 2017 IPPS/LTCH PPS final rule (81 FR 56913), we adopted the updates set forth in OMB Bulletin No. 15-01 effective October 1, 2016, beginning with the FY 2017 wage index. For a complete discussion of the adoption of the updates set forth in OMB Bulletin No. 15-01, we refer readers to the FY 2017 IPPS/LTCH PPS final rule. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38130), we continued to use the OMB delineations that were adopted beginning with FY 2015 to calculate the area wage indexes, with updates as reflected in OMB Bulletin No. 15-01 specified in the FY 2017 IPPS/LTCH PPS final rule.
On August 15, 2017, OMB issued OMB Bulletin No. 17-01, which provided updates to and superseded OMB Bulletin No. 15-01 that was issued on July 15, 2015. The attachments to OMB Bulletin No. 17-01 provide detailed information on the update to statistical areas since July 15, 2015, and are based on the application of the 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas to Census Bureau population estimates for July 1, 2014 and July 1, 2015. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41362 through 41363), we adopted the updates set forth in OMB Bulletin No. 17-01 effective October 1, 2018, beginning with the FY 2019 wage index. For a complete discussion of the adoption of the updates set forth in OMB Bulletin No. 17-01, we refer readers to the FY 2019 IPPS/LTCH PPS final rule.
For FY 2020, we are continuing to use the OMB delineations that were adopted beginning with FY 2015 (based on the revised delineations issued in OMB Bulletin No. 13-01) to calculate the area wage indexes, with updates as reflected in OMB Bulletin Nos. 15-01 and 17-01.
3. Codes for Constituent Counties in CBSAs
CBSAs are made up of one or more constituent counties. Each CBSA and constituent county has its own unique identifying codes. There are two different lists of codes associated with counties: Social Security Administration (SSA) codes and Federal Information Processing Standard (FIPS) codes. Historically, CMS has listed and used SSA and FIPS county codes to identify and crosswalk counties to CBSA codes for purposes of the hospital wage index. As we discussed in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38129 through 38130), we have learned that SSA county codes are no longer being maintained and updated. However, the FIPS codes continue to be maintained by the U.S. Census Bureau. We believe that using the latest FIPS codes will allow us to maintain a more accurate and up-to-date payment system that reflects the reality of population shifts and labor market conditions.
The Census Bureau's most current statistical area information is derived from ongoing census data received since 2010; the most recent data are from 2015. The Census Bureau maintains a complete list of changes to counties or county equivalent entities on the website at: https://www.census.gov/geo/reference/county-changes.html. We believe that it is important to use the latest counties or county equivalent entities in order to properly crosswalk hospitals from a county to a CBSA for purposes of the hospital wage index used under the IPPS.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38129 through 38130), we adopted a policy to discontinue the use of the SSA county codes and began using only the FIPS county codes for purposes of crosswalking counties to CBSAs. In addition, in the same rule, we implemented the latest FIPS code updates which were effective October 1, 2017, beginning with the FY 2018 wage indexes. These updates have been used to calculate the wage indexes in a manner generally consistent with the CBSA-based methodologies finalized in the FY 2005 IPPS final rule and the FY 2015 IPPS/LTCH PPS final rule.
For FY 2020, we are continuing to use only the FIPS county codes for purposes of crosswalking counties to CBSAs. For FY 2020, Tables 2 and 3 associated with this final rule and the County to CBSA Crosswalk File and Urban CBSAs and Constituent Counties for Acute Care Hospitals File posted on the CMS website reflect these county changes.
B. Worksheet S-3 Wage Data for the FY 2020 Wage Index
The FY 2020 wage index values are based on the data collected from the Medicare cost reports submitted by hospitals for cost reporting periods beginning in FY 2016 (the FY 2019 wage indexes were based on data from cost reporting periods beginning during FY 2015).
1. Included Categories of Costs
The FY 2020 wage index includes all of the following categories of data associated with costs paid under the IPPS (as well as outpatient costs):
- Salaries and hours from short-term, acute care hospitals (including paid lunch hours and hours associated with military leave and jury duty).
- Home office costs and hours.
- Certain contract labor costs and hours, which include direct patient care, certain top management, pharmacy, laboratory, and nonteaching physician Part A services, and certain contract indirect patient care services (as discussed in the FY 2008 final rule with comment period (72 FR 47315 through 47317)).
- Wage-related costs, including pension costs (based on policies adopted in the FY 2012 IPPS/LTCH PPS final rule (76 FR 51586 through 51590)) and other deferred compensation costs.
2. Excluded Categories of Costs
Consistent with the wage index methodology for FY 2019, the wage index for FY 2020 also excludes the direct and overhead salaries and hours for services not subject to IPPS payment, such as skilled nursing facility (SNF) services, home health services, costs related to GME (teaching physicians and residents) and certified registered nurse anesthetists (CRNAs), and other subprovider components that are not paid under the IPPS. The FY 2020 wage index also excludes the salaries, hours, and wage-related costs of hospital-based rural health clinics (RHCs), and Federally qualified health centers (FQHCs) because Medicare pays for these costs outside of the IPPS (68 FR 45395). In addition, salaries, hours, and wage-related costs of CAHs are excluded from the wage index for the reasons explained in the FY 2004 IPPS final rule (68 FR 45397 through 45398). For FY 2020 and subsequent years, other wage-related costs are also excluded from the calculation of the wage index. As discussed in the FY 2019 IPPS/LTCH final rule (83 FR 41365 through 41369), other wage-related costs reported on Worksheet S-3, Part II, Line 18 and Worksheet S-3, Part IV, Line 25 and subscripts, as well as all other wage-related costs, such as contract labor costs, are excluded from the calculation of the wage index.
3. Use of Wage Index Data by Suppliers and Providers Other Than Acute Care Hospitals Under the IPPS
Data collected for the IPPS wage index also are currently used to calculate wage indexes applicable to suppliers and other providers, such as SNFs, home health agencies (HHAs), ambulatory surgical centers (ASCs), and hospices. In addition, they are used for prospective payments to IRFs, IPFs, and LTCHs, and for hospital outpatient services. We note that, in the IPPS rules, we do not address comments pertaining to the wage indexes of any supplier or provider except IPPS providers and LTCHs. Such comments should be made in response to separate proposed rules for those suppliers and providers.
C. Verification of Worksheet S-3 Wage Data
The wage data for the FY 2020 wage index were obtained from Worksheet S-3, Parts II and III of the Medicare cost report (Form CMS-2552-10, OMB Control Number 0938-0050 with expiration date March 31, 2022) for cost reporting periods beginning on or after October 1, 2015, and before October 1, 2016. For wage index purposes, we refer to cost reports during this period as the “FY 2016 cost report,” the “FY 2016 wage data,” or the “FY 2016 data.” Instructions for completing the wage index sections of Worksheet S-3 are included in the Provider Reimbursement Manual (PRM), Part 2 (Pub. 15-2), Chapter 40, Sections 4005.2 through 4005.4. The data file used to construct the FY 2020 wage index includes FY 2016 data submitted to us as of June 19, 2019. As in past years, we performed an extensive review of the wage data, mostly through the use of edits designed to identify aberrant data.
We asked our MACs to revise or verify data elements that result in specific edit failures. For the proposed FY 2020 wage index, we identified and excluded 81 providers with aberrant data that should not be included in the wage index, although we stated in the FY 2020 IPPS/LTCH PPS proposed rule that if data elements for some of these providers are corrected, we intend to include data from those providers in the final FY 2020 wage index (84 FR 19375). We also adjusted certain aberrant data and included these data in the proposed wage index. For example, in situations where a hospital did not have documentable salaries, wages, and hours for housekeeping and dietary services, we imputed estimates, in accordance with policies established in the FY 2015 IPPS/LTCH PPS final rule (79 FR 49965 through 49967). We instructed MACs to complete their data verification of questionable data elements and to transmit any changes to the wage data no later than March 22, 2019. In addition, as a result of the April and May appeals processes, and posting of the April 30, 2019 PUF, we have made additional revisions to the FY 2020 wage data, as described further below. The revised data are reflected in this FY 2020 IPPS/LTCH PPS final rule.
Among the hospitals we identified with aberrant data and excluded from the proposed rule wage index were eight hospitals that are part of a health care delivery system that is unique in several ways. As we explained in the proposed rule, (84 FR 19375), the vast majority of the system's hospitals (38) are located in a single State, with one union representing most of their hospital employees in the “northern” region of the State, while another union represents most of their hospital employees in the “southern” region of the State. The salaries negotiated do not reflect competitive local labor market salaries; rather, the salaries reflect negotiated salary rates for the “northern” and “southern” regions of the State respectively. For example, all medical assistants in the “northern” region start at $24.31 per hour, and medical assistants in the “southern” region start at $20.36 per hour. Thus, all salaries for similar positions and levels of experience in the northern region, for example, are the same regardless of prevailing labor market conditions in the area in which the hospital is located. In addition, this chain is part of a managed care organization and an integrated delivery system wherein the hospitals rely on the system's health care plans for funding. For the FY 2020 proposed wage index calculation, we identified and excluded eight of the hospitals that are part of this health care system. The average hourly wages of these eight hospitals differ most from their respective CBSA average hourly wages, and there is a large gap between the average hourly wage of each of the eight hospitals and the next closest average hourly wage in their respective CBSAs. In the proposed rule (84 FR 19376), we stated that we do not believe that the average hourly wages of these eight hospitals accurately reflect the economic conditions in their respective labor market areas during the FY 2016 cost reporting period. Therefore, we stated that we believe the inclusion of the wage data for these eight hospitals in the proposed wage index would not ensure that the FY 2020 wage index represents the relative hospital wage level in the geographic area of the hospital as compared to the national average of wages. Rather, the inclusion of these data would distort the comparison of the average hourly wage of each of these hospitals' labor market areas to the national average hourly wage. We stated that we believe that under section 1886(d)(3)(E) of the Act, which requires the Secretary to establish an adjustment factor (the wage index) reflecting the relative hospital wage level in the geographic area of a hospital compared to the national average hospital wage level, we have the discretion to remove hospital data from the wage index that is not reflective of the relative hospital wage level in the hospitals' geographic area. In previous rulemaking (80 FR 49491), we explained that we remove hospitals from the wage index because their average hourly wages are either extraordinarily high or extraordinarily low compared to their labor market areas, even though their data were properly documented. For this reason, we have removed the data of other hospitals in the past; for example, data from government-owned hospitals and hospitals providing unique or niche services which affect their average hourly wages. In the proposed rule (84 FR 19376), we noted that we are considering removing all of the hospitals in this health care system from the FY 2021 and subsequent wage index calculations, not because they are failing edits due to inaccuracy, but because of the uniqueness of this chain of hospitals, in particular, the fact that the salaries of their employees are not based on local labor market rates.
In constructing the proposed FY 2020 wage index, we included the wage data for facilities that were IPPS hospitals in FY 2016, inclusive of those facilities that have since terminated their participation in the program as hospitals, as long as those data did not fail any of our edits for reasonableness. We stated in the proposed rule that we believe including the wage data for these hospitals is, in general, appropriate to reflect the economic conditions in the various labor market areas during the relevant past period and to ensure that the current wage index represents the labor market area's current wages as compared to the national average of wages. However, we excluded the wage data for CAHs as discussed in the FY 2004 IPPS final rule (68 FR 45397 through 45398); that is, any hospital that is designated as a CAH by 7 days prior to the publication of the preliminary wage index public use file (PUF) is excluded from the calculation of the wage index. For the proposed rule, we removed 4 hospitals that converted to CAH status on or after January 26, 2018, the cut-off date for CAH exclusion from the FY 2019 wage index, and through and including January 24, 2019, the cut-off date for CAH exclusion from the FY 2020 wage index. Since issuance of the proposed rule, we learned of 3 more CAHs that converted to CAH status on or after January 26, 2018, through and including January 24, 2019, for a total of 7 CAH exclusions. Also, since issuance of the proposed rule and in preparation for the April 30, 2019 PUF, we identified and deleted 2 more hospitals (one whose data changed since the January PUF and became aberrant, and the other whose data did not change, but it became evident for the first time that it was aberrantly low), while restoring 17 hospitals (including 1 hospital that is part of the unique healthcare chain discussed in the proposed rule at 84 FR 19375-6) whose data improved. After the April 30, 2019 PUF we identified and deleted 1 more hospital (whose data did not change, but it became evident for the first time that it was aberrantly low), while restoring the wage data of the 7 hospitals that are part of the unique health care chain. That is, we have restored to the final rule wage index calculation for FY 2020 the wage data of the 8 hospitals that are part of the unique health care chain discussed in the proposed rule (84 FR 19375-6), as discussed further below. In summary, in the calculation of the FY 2020 final wage index, we have restored the wage data of the 8 hospitals that are part of the unique health care chain referenced above plus the wage data of 16 additional hospitals, while deleting the wage data of 3 additional hospitals and 3 additional CAHs. Consequently, we calculated the proposed wage index using the Worksheet S-3, Parts II and III wage data of 3,239 hospitals.
For the final FY 2020 wage index, we allotted the wages and hours data for a multicampus hospital among the different labor market areas where its campuses are located in the same manner that we allotted such hospitals' data in the FY 2019 wage index (83 FR 41364 through 41365); that is, using campus full-time equivalent (FTE) percentages as originally finalized in the FY 2012 IPPS/LTCH PPS final rule (76 FR 51591). Table 2, which contains the final FY 2020 wage index associated with this final rule (available via the internet on the CMS website), includes separate wage data for the campuses of 17 multicampus hospitals. The following chart lists the multicampus hospitals by CSA certification number (CCN) and the FTE percentages on which the wages and hours of each campus were allotted to their respective labor market areas:

We note that, in past years, in Table 2, we have placed a “B” to designate the subordinate campus in the fourth position of the hospital CCN. However, for the FY 2019 IPPS/LTCH PPS proposed and final rules and subsequent rules, we have moved the “B” to the third position of the CCN. Because all IPPS hospitals have a “0” in the third position of the CCN, we believe that placement of the “B” in this third position, instead of the “0” for the subordinate campus, is the most efficient method of identification and interferes the least with the other, variable, digits in the CCN.
Comment: Several commenters strongly opposed the exclusion of seven hospitals' wage data (we note that as previously stated, the data for one of the eight hospitals excluded from the proposed rule PUF was included in the April 30, 2019 PUF due to improved data). These commenters stated that excluding accurate and verified data is inconsistent with the extensive process established by CMS to ensure the accuracy and reliability of hospital wage index data. In addition, commenters specifically raised the following concerns: Section 1395ww(d)(3)(E) of the Statute does not provide the authority for CMS to delete accurately-reported wage data; excluding hospitals without any definable standards is an abuse of discretion, creates uncertainty, and is arbitrary and capricious; the proposed exclusion is procedurally improper without formal notice-and-comment rulemaking in accordance with the Administrative Procedures Act (APA); excluding accurate wage data disregards labor costs and improperly substitutes CMS' judgment of reasonable wage levels for actual, free-market wage data; and singling out a health system due to its collective bargaining practices undermines the National Labor Relations Act (NLRA).
Several commenters stated that high labor costs are a true reflection of the challenging labor markets in California and the fact that wages are influenced by labor negotiations does not render them any less valid. A commenter stated that the exclusion of these seven hospitals raises constitutional concerns as it would impermissibly apply a rule that is directed at and penalizes a single party.
Commenters also expressed concern regarding the far-reaching effects of excluding the seven hospitals' wage data. A few commenters stated that excluding the wage data for the seven hospitals will decrease payments to hospitals in those CBSAs significantly, jeopardizing access to care for Medicare beneficiaries across California. Many commenters stated that excluding the seven hospitals' wage data will also harm inpatient psychiatric facilities, inpatient rehabilitation facilities, skilled nursing facilities, and other provider types whose payments are impacted by the wage index, and noted that CMS did not identify the fiscal impacts of the exclusions in its respective regulatory impact analyses for the IPF, IRF, SNF, and the IPPS proposed rules.
Additionally, commenters strongly opposed removing all 38 of the Health System's hospitals from the wage index data beginning in FY 2021.
Response: In consideration of comments received, and to allow more time to consider the appropriateness of including or excluding the wage data of this unique health care chain, the wage data of all eight hospitals in this health care chain that were deleted from the proposed rule calculation (84 FR 19375 through 19376) are included in the FY 2020 final rule wage index.
D. Method for Computing the FY 2020 Unadjusted Wage Index
In the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 41365), we indicated we were committed to transforming the health care delivery system, including the Medicare program, by putting an additional focus on patient-centered care and working with providers, physicians, and patients to improve outcomes. One key to that transformation is ensuring that the Medicare payment rates are as accurate and appropriate as possible, consistent with the law. We invited the public to submit comments, suggestions, and recommendations for regulatory and policy changes to address wage index disparities. Our proposals for FY 2020 to address wage index disparities, to the extent permitted under current law, are discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19393 through 19399). We stated in the proposed rule that we continue to believe that broader statutory wage index reform is needed.
1. Methodology for FY 2020
The method used to compute the proposed FY 2020 wage index without an occupational mix adjustment follows the same methodology that we used to compute the proposed wage indexes without an occupational mix adjustment since FY 2012 (76 FR 51591 through 51593), except as discussed in this final rule. Typically, we do not restate all of the steps of the methodology to compute the wage indexes in each proposed and final rulemaking; instead, we refer readers to the FY 2012 IPPS/LTCH PPS final rule. However, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19377 through 19379), we (1) restated the steps of the methodology in order to update outdated references to certain cost report lines which were then reflected on Medicare CMS Form 2552-96 but are now reflected on Medicare CMS Form 2552-10; (2) proposed to change the calculation of the Overhead Rate in Step 4; (3) proposed to modify our methodology with regard to how dollar amounts, hours, and other numerical values in the wage index calculation are rounded; and (4) proposed a methodology for calculating the wage index for urban areas without wage data. We otherwise did not propose to make any other policy changes in this section to the methodology set forth in the FY 2012 IPPS/LTCH PPS proposed rule (76 FR 51591 through 51593) for computing the proposed wage index without an occupational mix adjustment. Our methodology, including our proposals (as set forth above), is discussed below. Unless otherwise specified, all cost report line references in this section of this final rule refer to CMS Form 2552-10.
Step 1.—We gathered data from each of the non-Federal, short-term, acute care hospitals for which data were reported on the Worksheet S-3, Parts II and III of the Medicare cost report for the hospital's cost reporting period relevant to the proposed wage index (in this case, for FY 2020, these were data from cost reports for cost reporting periods beginning on or after October 1, 2015, and before October 1, 2016). In addition, we included data from some hospitals that had cost reporting periods beginning before October 2015 and reported a cost reporting period covering all of FY 2016. These data were included because no other data from these hospitals would be available for the cost reporting period as previously described, and because particular labor market areas might be affected due to the omission of these hospitals. However, we generally describe these wage data as FY 2016 data. We note that, if a hospital had more than one cost reporting period beginning during FY 2016 (for example, a hospital had two short cost reporting periods beginning on or after October 1, 2015, and before October 1, 2016), we include wage data from only one of the cost reporting periods, the longer, in the wage index calculation. If there was more than one cost reporting period and the periods were equal in length, we included the wage data from the later period in the wage index calculation.
Step 2.—Salaries.—The method used to compute a hospital's average hourly wage excludes certain costs that are not paid under the IPPS. (We note that, beginning with FY 2008 (72 FR 47315), we included what were then Lines 22.01, 26.01, and 27.01 of Worksheet S-3, Part II of CMS Form 2552-96 for overhead services in the wage index. Currently, these lines are lines 28, 33, and 35 on CMS Form 2552-10. However, we note that the wages and hours on these lines are not incorporated into Line 101, Column 1 of Worksheet A, which, through the electronic cost reporting software, flows directly to Line 1 of Worksheet S-3, Part II. Therefore, the first step in the wage index calculation is to compute a “revised” Line 1, by adding to the Line 1 on Worksheet S-3, Part II (for wages and hours respectively) the amounts on Lines 28, 33, and 35.) In calculating a hospital's Net Salaries (we note that we previously used the term “average” salaries in the FY 2012 IPPS/LTCH PPS final rule (76 FR 51592), but we now use the term “net” salaries) plus wage-related costs, we first compute the following: Subtract from Line 1 (total salaries) the GME and CRNA costs reported on CMS Form 2552-10, Lines 2, 4.01, 7, and 7.01, the Part B salaries reported on Lines 3, 5 and 6, home office salaries reported on Line 8, and exclude salaries reported on Lines 9 and 10 (that is, direct salaries attributable to SNF services, home health services, and other subprovider components not subject to the IPPS). We also subtract from Line 1 the salaries for which no hours were reported. Therefore, the formula for Net Salaries (from Worksheet S-3, Part II) is the following: ((Line 1 + Line 28 + Line 33 + Line 35)−(Line 2 + Line 3 + Line 4.01 + Line 5 + Line 6 + Line 7 + Line 7.01 + Line 8 + Line 9 + Line 10)).
To determine Total Salaries plus Wage-Related Costs, we add to the Net Salaries the costs of contract labor for direct patient care, certain top management, pharmacy, laboratory, and nonteaching physician Part A services (Lines 11, 12 and 13), home office salaries and wage-related costs reported by the hospital on Lines 14.01, 14.02, and 15, and nonexcluded area wage-related costs (Lines 17, 22, 25.50, 25.51, and 25.52). We note that contract labor and home office salaries for which no corresponding hours are reported are not included. In addition, wage-related costs for nonteaching physician Part A employees (Line 22) are excluded if no corresponding salaries are reported for those employees on Line 4.
The formula for Total Salaries plus Wage-Related Costs (from Worksheet S-3, Part II) is the following: ((Line 1 + Line 28 + Line 33 + Line 35)−(Line 2 + Line 3 + Line 4.01 + Line 5 + Line 6 + Line 7 + Line 7.01 + Line 8 + Line 9 + Line 10)) + (Line 11 + Line 12 + Line 13 + Line 14.01 + 14.02 + Line 15) + (Line 17 + Line 22 + 25.50 + 25.51 + 25.52).
Step 3.—Hours.—With the exception of wage-related costs, for which there are no associated hours, we compute total hours using the same methods as described for salaries in Step 2.
The formula for Total Hours (from Worksheet S-3, Part II) is the following: ((Line 1 + Line 28 + Line 33 + Line 35)−(Line 2 + Line 3 + Line 4.01 + Line 5 + Line 6 + Line 7 + Line 7.01 + Line 8 + Line 9 + Line 10)) + (Line 11 + Line 12 + Line 13 + Line 14.01 + 14.02 + Line 15).
Step 4.—For each hospital reporting both total overhead salaries and total overhead hours greater than zero, we then allocate overhead costs to areas of the hospital excluded from the wage index calculation. First, we determine the “excluded rate”, which is the ratio of excluded area hours to Revised Total Hours (from Worksheet S-3, Part II) with the following formula: (Line 9 + Line 10)/(Line 1 + Line 28 + Line 33 + Line 35)−(Lines 2, 3, 4.01, 5, 6, 7, 7.01, and 8 and Lines 26 through 43).
We then compute the amounts of overhead salaries and hours to be allocated to excluded areas by multiplying the above ratio by the total overhead salaries and hours reported on Lines 26 through 43 of Worksheet S-3, Part II. Next, we compute the amounts of overhead wage-related costs to be allocated to excluded areas using three steps:
(1) We determine the “overhead rate” (from Worksheet S-3, Part II), which is the ratio of overhead hours (Lines 26 through 43 minus the sum of Lines 28, 33, and 35) to revised hours excluding the sum of lines 28, 33, and 35 (Line 1 minus the sum of Lines 2, 3, 4.01, 5, 6, 7, 7.01, 8, 9, 10, 28, 33, and 35). We note that, for the FY 2008 and subsequent wage index calculations, we have been excluding the overhead contract labor (Lines 28, 33, and 35) from the determination of the ratio of overhead hours to revised hours because hospitals typically do not provide fringe benefits (wage-related costs) to contract personnel. Therefore, it is not necessary for the wage index calculation to exclude overhead wage-related costs for contract personnel. Further, if a hospital does contribute to wage-related costs for contracted personnel, the instructions for Lines 28, 33, and 35 require that associated wage-related costs be combined with wages on the respective contract labor lines.
The formula for the Overhead Rate (from Worksheet S-3, Part II) has been the following: (Lines 26 through 43−Lines 28, 33 and 35) / ((((Line 1 + Lines 28, 33, 35)−(Lines 2, 3, 4.01, 5, 6, 7, 7.01, 8, 26 through 43))−(Lines 9, 10, 28, 33, and 35)) + (Lines 26 through 43−Lines 28, 33, and 35)).
We stated in the proposed rule that, for the calculation for FY 2020 and subsequent fiscal years, we were reexamining this step as previously described regarding removal of the sum of overhead contract labor hours on Lines 28, 33, and 35. In the denominator of this calculation of the overhead rate, we have been subtracting out the sum of the overhead contract labor hours from Revised Total Hours. However, we stated in the proposed rule that this requires modification because Revised Total Hours do not include these overhead contract labor hours. We proposed to modify this step of the calculation of the overhead rate as follows:
The formula for the Overhead Rate (from Worksheet S-3, Part II) would be the following: (Lines 26 through 43−Lines 28, 33 and 35) / ((((Line 1 + Lines 28, 33, 35)−(Lines 2, 3, 4.01, 5, 6, 7, 7.01, 8, and 26 through 43))−(Lines 9 and 10)) + (Lines 26 through 43−Lines 28, 33, and 35)).
(2) We compute overhead wage-related costs by multiplying the overhead hours ratio by wage-related costs reported on Part II, Lines 17, 22, 25.50, 25.51, and 25.52.
(3) We multiply the computed overhead wage-related costs by the previously described excluded area hours ratio.
Finally, we subtract the computed overhead salaries, wage-related costs, and hours associated with excluded areas from the total salaries (plus wage-related costs) and hours derived in Steps 2 and 3.
Step 5.—For each hospital, we adjust the total salaries plus wage-related costs to a common period to determine total adjusted salaries plus wage-related costs. To make the wage adjustment, we estimate the percentage change in the employment cost index (ECI) for compensation for each 30-day increment from October 14, 2015 through April 15, 2017, for private industry hospital workers from the BLS' Compensation and Working Conditions. We use the ECI because it reflects the price increase associated with total compensation (salaries plus fringes) rather than just the increase in salaries. In addition, the ECI includes managers as well as other hospital workers. This methodology to compute the monthly update factors uses actual quarterly ECI data and assures that the update factors match the actual quarterly and annual percent changes. We also note that, since April 2006 with the publication of March 2006 data, the BLS' ECI uses a different classification system, the North American Industrial Classification System (NAICS), instead of the Standard Industrial Codes (SICs), which no longer exist. We have consistently used the ECI as the data source for our wages and salaries and other price proxies in the IPPS market basket, and we did not propose to make any changes to the usage for FY 2020. The factors used to adjust the hospital's data were based on the midpoint of the cost reporting period, as indicated in this final rule.
Step 6.—Each hospital is assigned to its appropriate urban or rural labor market area before any reclassifications under section 1886(d)(8)(B), 1886(d)(8)(E), or 1886(d)(10) of the Act. Within each urban or rural labor market area, we add the total adjusted salaries plus wage-related costs obtained in Step 5 for all hospitals in that area to determine the total adjusted salaries plus wage-related costs for the labor market area.
Step 7.—We divide the total adjusted salaries plus wage-related costs obtained under Step 6 by the sum of the corresponding total hours (from Step 4) for all hospitals in each labor market area to determine an average hourly wage for the area.
Step 8.—We add the total adjusted salaries plus wage-related costs obtained in Step 5 for all hospitals in the Nation and then divide the sum by the national sum of total hours from Step 4 to arrive at a national average hourly wage.
Step 9.—For each urban or rural labor market area, we calculate the hospital wage index value, unadjusted for occupational mix, by dividing the area average hourly wage obtained in Step 7 by the national average hourly wage computed in Step 8.
Step 10.—For each urban labor market area for which we do not have any hospital wage data (either because there are no IPPS hospitals in that labor market area, or there are IPPS hospitals in that area but their data are either too new to be reflected in the current year's wage index calculation, or their data are aberrant and are deleted from the wage index), we proposed that, for FY 2020 and subsequent years' wage index calculations, such CBSA's wage index would be equal to total urban salaries plus wage-related costs (from Step 5) in the State, divided by the total urban hours (from Step 4) in the State, divided by the national average hourly wage from Step 8. We stated in the proposed rule (84 FR 19378) that we believe that, in the absence of wage data for an urban labor market area, it is reasonable to propose to use a statewide urban average, which is based on actual, acceptable wage data of hospitals in that State, rather than impute some other type of value using a different methodology.
For calculation of the proposed FY 2020 wage index, we noted there are 2 urban CBSAs for which we do not have IPPS hospital wage data. In Table 3 associated with the proposed rule (which is available via the internet on the CMS website) which contains the proposed area wage indexes, we included a footnote to indicate to which CBSAs this proposed policy would apply. We proposed that these CBSAs' wage indexes would be equal to total urban salaries plus wage-related costs (from Step 5) in the respective State, divided by the total urban hours (from Step 4) in the respective State, divided by the national average hourly wage (from Step 8). Under this step, we also proposed to apply our proposed policy with regard to how dollar amounts, hours, and other numerical values in the wage index calculations are rounded.
We referred readers to section II. of the Appendix of the proposed rule for the policy regarding rural areas that do not have IPPS hospitals.
Step 11.—Section 4410 of Public Law 105-33 provides that, for discharges on or after October 1, 1997, the area wage index applicable to any hospital that is located in an urban area of a State may not be less than the area wage index applicable to hospitals located in rural areas in that State. The areas affected by this provision were identified in Table 2 which was listed in section VI. of the Addendum to the proposed rule and available via the internet on the CMS website.
As we noted previously in this section, we proposed to modify our methodology with regard to how dollar amounts, hours, and other numerical values in the unadjusted and adjusted wage index calculation are rounded, in order to help ensure consistency in the calculation. For example, we have received questions from stakeholders who use data printed in our proposed and final rules and online in our public use files (PUFs) to calculate the wage indexes, and as we noted in the proposed rule, it has come to our attention that, due in part to occasional inconsistencies in rounding of data, CMS' calculations and stakeholders' calculations may not match. Therefore, to help ensure consistency in the calculation, we proposed to modify how the wage data numbers are rounded, as follows. For data that we consider to be “raw data,” such as the cost report data on Worksheets S-3, Parts II and III, and the occupational mix survey data, we proposed to use such data “as is,” and not round any of the individual line items or fields. However, for any dollar amounts within the wage index calculations, including any type of summed wage amount, average hourly wages, and the national average hourly wage (both the unadjusted and adjusted for occupational mix), we proposed to round the dollar amounts to 2 decimals. For any hour amounts within the wage index calculations, we proposed to round such hour amounts to the nearest whole number. For any numbers not expressed as dollars or hours within the wage index calculations, which could include ratios, percentages, or inflation factors, we proposed to round such numbers to 5 decimals. However, we proposed to continue rounding the actual unadjusted and adjusted wage indexes to 4 decimals, as we have done historically.
As discussed in the FY 2012 IPPS/LTCH PPS final rule, in “Step 5,” for each hospital, we adjust the total salaries plus wage-related costs to a common period to determine total adjusted salaries plus wage-related costs. To make the wage adjustment, we estimate the percentage change in the employment cost index (ECI) for compensation for each 30-day increment from October 14, 2015, through April 15, 2017, for private industry hospital workers from the BLS' Compensation and Working Conditions. We have consistently used the ECI as the data source for our wages and salaries and other price proxies in the IPPS market basket, and we did not propose any changes to the usage of the ECI for FY 2020. The factors used to adjust the hospital's data were based on the midpoint of the cost reporting period, as indicated in the following table.

For example, the midpoint of a cost reporting period beginning January 1, 2016, and ending December 31, 2016, is June 30, 2016. An adjustment factor of 1.01585 was applied to the wages of a hospital with such a cost reporting period.
Previously, we also would provide a Puerto Rico overall average hourly wage. As discussed in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56915), prior to January 1, 2016, Puerto Rico hospitals were paid based on 75 percent of the national standardized amount and 25 percent of the Puerto Rico-specific standardized amount. As a result, we calculated a Puerto Rico-specific wage index that was applied to the labor-related share of the Puerto Rico-specific standardized amount. Section 601 of the Consolidated Appropriations Act, 2016 (Pub. L. 114-113) amended section 1886(d)(9)(E) of the Act to specify that the payment calculation with respect to operating costs of inpatient hospital services of a subsection (d) Puerto Rico hospital for inpatient hospital discharges on or after January 1, 2016, shall use 100 percent of the national standardized amount. As we stated in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56915 through 56916), because Puerto Rico hospitals are no longer paid with a Puerto Rico-specific standardized amount as of January 1, 2016, under section 1886(d)(9)(E) of the Act, as amended by section 601 of the Consolidated Appropriations Act, 2016, there is no longer a need to calculate a Puerto Rico-specific average hourly wage and wage index. Hospitals in Puerto Rico are now paid 100 percent of the national standardized amount and, therefore, are subject to the national average hourly wage (unadjusted for occupational mix) and the national wage index, which is applied to the national labor-related share of the national standardized amount. Therefore, for FY 2020, there is no Puerto Rico-specific overall average hourly wage or wage index.
Based on the previously described methodology, we stated that the proposed unadjusted national average hourly wage was the following:
| Proposed FY 2020 Unadjusted National Average Hourly Wage | $44.03 |
Comment: A commenter appreciated and supported CMS's proposal to provide more transparency and consistency by clarifying the rules of rounding data in the wage index calculation. However, the commenter suggested that average hourly wages be treated as a ratio rather than a dollar amount, and alleged that average hourly wages are actually imputed ratios and not actual dollar figures. The commenter believed that rounding average hourly wages to two decimal places as proposed, rather than the previous method of rounding to 5 decimals, decreases the precision and accuracy of the wage indexes. The commenter provided a hypothetical example to support their assertion.
Response: In the proposed rule (84 FR 19379 and 19380), we proposed to modify our methodology with regard to how dollar amounts, hours, and other numerical values in the unadjusted and adjusted wage index calculation are rounded, in order to help ensure consistency in the calculation. For data that we consider to be “raw data,” such as the cost report data on Worksheets S-3, Parts II and III, and the occupational mix survey data, we proposed to use such data “as is,” and not round any of the individual line items or fields. However, for any dollar amounts within the wage index calculations, including any type of summed wage amount, average hourly wages, and the national average hourly wage (both the unadjusted and adjusted for occupational mix), we proposed to round the dollar amounts to 2 decimals. For any hour amounts within the wage index calculations, we proposed to round such hour amounts to the nearest whole number. For any numbers not expressed as dollars or hours within the wage index calculations, which could include ratios, percentages, or inflation factors, we proposed to round such numbers to 5 decimals. We proposed to continue rounding the actual unadjusted and adjusted wage indexes to 4 decimals, as we have done historically.
We appreciate the commenter's careful review of our proposal on rounding, but we disagree with the commenter that average hourly wages are actually imputed ratios and not actual dollar figures. While the average hourly wage for each CBSA and the national average hourly wage are computed by dividing summed wages in the numerator by summed hours in the denominator, similar to a ratio, the purpose of this division is to calculate a dollar amount, not a ratio, that is representative of a typical wage per hour in that CBSA and nationally. Because dollar amounts, if not expressed in whole numbers, are typically expressed with 2 decimal places, we believe it is appropriate to compute average hourly wages with 2 decimals. Regarding the commenter's concern that average hourly wages rounded to 2 decimals may result in less precise wage indexes, we note that our proposal to round to 2 decimals is not inherently biasing any wage indexes to be artificially too high or too low; neither is one wage index biased against another, since, as a relative system, all wage indexes are rounded to 2 decimals. Therefore, we believe that average hourly wages rounded to 2 decimals can and do result in wage indexes for each CBSA that are an appropriate gage of the wages in that area, which is an important feature of the wage index adjustment.
Comment: We received a couple of other comments about home office/related organization wages and hours reported on Worksheet S-3, Part II, lines 14.01 and 14.02, and that these lines may improperly include wages and hours for Part B and nonreimbursable areas of the hospital. The commenters requested clarification of the cost report instructions for these line items.
Response: Because we consider these comment to be outside the scope of the FY 2020 wage index proposals, we are not directly responding to these comments in this final rule. However, we will take that commenter's concerns into consideration for future cost report clarifications.
After consideration of public comments received, we are finalizing without modification our proposed methodology as discussed above for computing the FY 2020 unadjusted wage index, including our proposals with respect to—(1) rounding dollar amounts, hours, and other numerical values used in the wage index calculation; (2) revising the Overhead Rate in Step 4; and (3) the methodology for calculating the wage index for urban areas without wage data.
Based on the methodology finalized above, the final unadjusted national average hourly wage is the following:
| Final FY 2020 Unadjusted National Average Hourly Wage | $44.19 |
2. Policies Regarding Rural Reclassification and Special Statuses for Multicampus Hospitals
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41369 through 41374), we codified policies regarding rural reclassification and special statuses for multicampus hospitals in the regulations at § 412.92 for sole community hospitals (SCHs), § 412.96 for rural referral centers (RRCs), § 412.103 for rural reclassification, and § 412.108 for Medicare-dependent, small rural hospitals (MDHs).
We stated that these policies apply to hospitals that have a main campus and one or more remote locations under a single provider agreement where services are provided and billed under the IPPS and that meet the provider-based criteria at § 413.65 as a main campus and a remote location of a hospital, also referred to as multicampus hospitals or hospitals with remote locations. As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41369), a main campus of a hospital cannot obtain an SCH, RRC, or MDH status or rural reclassification independently or separately from its remote location(s), and vice versa. Rather, if the criteria are met in the regulations at § 412.92 for SCHs, § 412.96 for RRCs, § 412.103 for rural reclassification, or § 412.108 for MDHs, the hospital (that is, the main campus and its remote location(s)) will be granted the special treatment or rural reclassification afforded by the aforementioned regulations.
We stated that, to qualify for rural reclassification or SCH, RRC, or MDH status, a hospital with remote locations must demonstrate that both the main campus and its remote location(s) satisfy the relevant qualifying criteria. If the regulations at § 412.92, § 412.96, § 412.103, and § 412.108 require data, such as bed count, number of discharges, or case-mix index, for example, to demonstrate that the hospital meets the qualifying criteria, the combined data from the main campus and its remote location(s) are to be used.
For other qualifying criteria set forth in the regulations at §§ 412.92, 412.96, 412.103, and 412.108 that do not involve data that can be combined, specifically qualifying criteria related to location, mileage, travel time, and distance requirements, a hospital would need to demonstrate that the main campus and its remote location(s) each independently satisfy those requirements in order for the entire hospital, including its remote location(s), to be reclassified or obtain a special status.
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41369 through 41374) for a detailed discussion of our policies for multicampus hospitals.
Comment: A few commenters referred to CMS' statement in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41373 and 41374) that it will take the feedback received regarding multicampus hospitals and SCH determinations into consideration for potential future rulemaking. The commenters “wholeheartedly agreed” with CMS' reasoning behind the use of remote campus locations for purposes of determining whether the distance criteria is met when evaluating SCH status criteria, but stated that they had hoped for clarification in the FY 2020 Medicare IPPS rulemaking regarding the definition of a remote location to be used in this determination. The commenters stated that there remains the potential that facilities that would otherwise qualify as a SCH may be precluded from doing so by the presence of a remote location that does not offer services originally intended in the creation of the SCH framework. Specifically, the commenters requested that CMS consider the following two policy clarifications:
- CMS should define a remote location as one that provides general acute care services to the community. If the remote location does not offer general acute care services reasonably available to the entire community, the campus should not be considered a remote location for purposes of determining SCH mileage criteria under 412.92(a)(4). For example, a facility providing only inpatient psychiatric services, inpatient OB/GYN women's services, or a provider-based Rural Health Clinic should not considered a remote location, according to the commenters.
- CMS should define a remote location as one that also meets the criteria of § 412.92(c)(2) which states, “the term like hospital means a hospital furnishing short term, acute care. CMS will not consider the nearby hospital to be a like hospital if the total inpatient days attributable to units of the nearby hospital that provides a level of care characteristic of the level of care payable under the acute care hospital inpatient prospective payment system are less than or equal to 8 percent of the similarly calculated total inpatient days of the hospital seeking sole community hospital designation.”
Response: We appreciate the commenters input. However, because we consider these comments to be outside the scope of the FY 2020 wage index proposals, we are not finalizing any changes to these policies in this final rule, but may consider these comments for future rulemaking.
E. Occupational Mix Adjustment to the FY 2020 Wage Index
As stated earlier, section 1886(d)(3)(E) of the Act provides for the collection of data every 3 years on the occupational mix of employees for each short-term, acute care hospital participating in the Medicare program, in order to construct an occupational mix adjustment to the wage index, for application beginning October 1, 2004 (the FY 2005 wage index). The purpose of the occupational mix adjustment is to control for the effect of hospitals' employment choices on the wage index. For example, hospitals may choose to employ different combinations of registered nurses, licensed practical nurses, nursing aides, and medical assistants for the purpose of providing nursing care to their patients. The varying labor costs associated with these choices reflect hospital management decisions rather than geographic differences in the costs of labor.
1. Use of 2016 Medicare Wage Index Occupational Mix Survey for the FY 2019, FY 2020, and FY 2021 Wage Indexes
Section 304(c) of the Consolidated Appropriations Act, 2001 (Pub. L. 106-554) amended section 1886(d)(3)(E) of the Act to require CMS to collect data every 3 years on the occupational mix of employees for each short-term, acute care hospital participating in the Medicare program. We collected data in 2013 to compute the occupational mix adjustment for the FY 2016, FY 2017, and FY 2018 wage indexes. As discussed in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 19903) and final rule (82 FR 38137), a new measurement of occupational mix (the 2016 survey) was required for FY 2019, FY 2020, and FY 2021.
The FY 2020 occupational mix adjustment is based on the calendar year (CY) 2016 survey. Hospitals were required to submit their completed 2016 surveys (Form CMS-10079, OMB Control Number 0938-0907 with expiration date 09/30/2019) to their MACs by July 3, 2017. The preliminary, unaudited CY 2016 survey data were posted on the CMS website on July 12, 2017. As with the Worksheet S-3, Parts II and III cost report wage data, as part of the FY 2020 desk review process, the MACs revised or verified data elements in hospitals' occupational mix surveys that resulted in certain edit failures.
2. Calculation of the Occupational Mix Adjustment for FY 2020
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19380), for FY 2020, we proposed to calculate the occupational mix adjustment factor using the same methodology that we have used since the FY 2012 wage index (76 FR 51582 through 51586) and to apply the occupational mix adjustment to 100 percent of the FY 2020 wage index. As we explained in the proposed rule (84 FR 19378 through 19380), we proposed to modify our methodology with regard to how dollar amounts, hours, and other numerical values in the unadjusted and adjusted wage index calculation are rounded, in order to ensure consistency in the calculation. For data that we consider to be “raw data,” such as the cost report data on Worksheets S-3, Parts II and III, and the occupational mix survey data, we proposed to use these data “as is”, and not round any of the individual line items or fields. However, for any dollar amounts within the wage index calculations, including any type of summed wage amount, average hourly wages, and the national average hourly wage (both the unadjusted and adjusted for occupational mix), we proposed to round such dollar amounts to 2 decimals. We proposed to round any hour amounts within the wage index calculations to the nearest whole number. We proposed to round any numbers not expressed as dollars or hours in the wage index calculations, which could include ratios, percentages, or inflation factors, to 5 decimals. However, we proposed to continue rounding the actual unadjusted and adjusted wage indexes to 4 decimals, as we have done historically.
Similar to the method we use for the calculation of the wage index without occupational mix, salaries and hours for a multicampus hospital are allotted among the different labor market areas where its campuses are located. Table 2 associated with this final rule (which is available via the internet on the CMS website), which contains the final FY 2020 occupational mix adjusted wage index, includes separate wage data for the campuses of multicampus hospitals. We refer readers to section III.C. of the preamble of this final rule for a chart listing the multicampus hospitals and the FTE percentages used to allot their occupational mix data.
Because the statute requires that the Secretary measure the earnings and paid hours of employment by occupational category not less than once every 3 years, all hospitals that are subject to payments under the IPPS, or any hospital that would be subject to the IPPS if not granted a waiver, must complete the occupational mix survey, unless the hospital has no associated cost report wage data that are included in the FY 2020 wage index. For the proposed FY 2020 wage index, we used the Worksheet S-3, Parts II and III wage data of 3,221 hospitals, and we used the occupational mix surveys of 3,119 hospitals for which we also have Worksheet S-3 wage data, which represented a “response” rate of 97 percent (3,119/3,221). For the proposed FY 2020 wage index, we applied proxy data for noncompliant hospitals, new hospitals, or hospitals that submitted erroneous or aberrant data in the same manner that we applied proxy data for such hospitals in the FY 2012 wage index occupational mix adjustment (76 FR 51586). As a result of applying this methodology, the proposed FY 2020 occupational mix adjusted national average hourly wage was the following:
| Proposed FY 2020 Occupational Mix Adjusted National Average Hourly Wage | $43.99 |
Comment: A commenter stated that all hospitals should be obligated to submit the occupational mix survey because failure to complete the survey jeopardizes the accuracy of the wage index. The commenter suggested that a penalty be instituted for nonsubmitters. This commenter also requested that, pending CMS' analysis of the Commuting Based Wage Index and given the Institute of Medicine's study on geographic variation in hospital wage costs, CMS eliminate the occupational mix survey and the significant reporting burden it creates.
Response: We appreciate the commenter's concern about the accuracy of the wage index. We have continually requested that all hospitals complete and submit the occupational mix surveys, although we did not establish a penalty for hospitals that did not submit the surveys. We did not establish a penalty for hospitals that did not submit the 2016 surveys. However, we are continuing to consider for future rulemaking various options for ensuring full compliance with future occupational mix surveys. Regarding the commenter's concern about the administrative burden of the occupational mix survey and the suggestion that we eliminate it, this survey is necessary to meet the provisions of section 1886(d)(3)(E) of the Act which requires us to measure the earnings and paid hours of employment by occupational category.
After consideration of the public comments we received, for the reasons discussed in the final rule and the proposed rule, for FY 2020, we are adopting as final our proposal to calculate the occupational mix adjustment factor using the same methodology that we have used since the FY 2012 wage index. In addition, as proposed, we are modifying our methodology with regard to how dollar amounts, hours, and other numerical values in the unadjusted and adjusted wage index calculation are rounded, in order to ensure greater consistency in the calculation. For data that we consider to be “raw data,” such as the cost report data on Worksheets S-3, Parts II and III, and the occupational mix survey data, we will use these data “as is”, and not round any of the individual line items or fields. However, for any dollar amounts within the wage index calculations, including any type of summed wage amount, average hourly wages, and the national average hourly wage (both the unadjusted and adjusted for occupational mix), we will round such dollar amounts to 2 decimals. We will round any hour amounts within the wage index calculations to the nearest whole number. We will round any numbers not expressed as dollars or hours in the wage index calculations, which could include ratios, percentages, or inflation factors, to 5 decimals. However, we will continue rounding the actual unadjusted and adjusted wage indexes to 4 decimals, as we have done historically.
For the final rule FY 2020 wage index, we used the Worksheet S-3, Parts II and III wage data of 3,239 hospitals, and we used the occupational mix surveys of 3,136 hospitals for which we also have Worksheet S-3 wage data, which represented a “response” rate of 97 percent (3,136/3,239). (We note that the number of occupational mix surveys in this final rule differs from that of the proposed rule because for this final rule we have generally been able to include the occupational mix surveys of hospitals whose wage data were aberrant for the proposed rule but have since been improved and were used for this final rule. However, since a proportional number of occupational mix surveys to the number of hospitals included in the wage index are included, the response rate remains the same. For the final FY 2020 wage index, we applied proxy data for noncompliant hospitals, new hospitals, or hospitals that submitted erroneous or aberrant data in the same manner that we applied proxy data for such hospitals in the FY 2012 wage index occupational mix adjustment (76 FR 51586). As a result of applying this methodology, the final FY 2020 occupational mix adjusted national average hourly wage is the following:
| Final FY 2020 Occupational Mix Adjusted National Average Hourly Wage | $44.15 |
F. Analysis and Implementation of the Occupational Mix Adjustment and the FY 2020 Occupational Mix Adjusted Wage Index
As discussed in section III.E. of the preamble of this final rule, for FY 2020, we are applying the occupational mix adjustment to 100 percent of the FY 2020 wage index. We calculated the occupational mix adjustment using data from the 2016 occupational mix survey data, using the methodology described in the FY 2012 IPPS/LTCH PPS final rule (76 FR 51582 through 51586).
The FY 2020 national average hourly wages for each occupational mix nursing subcategory as calculated in Step 2 of the occupational mix calculation are as follows. (We note that the average hourly wage figures are rounded to two decimal places as we are finalizing in section III.D. of the preamble of this final rule.)

The national average hourly wage for the entire nurse category is computed in Step 5 of the occupational mix calculation. Hospitals with a nurse category average hourly wage (as calculated in Step 4) of greater than the national nurse category average hourly wage receive an occupational mix adjustment factor (as calculated in Step 6) of less than 1.0. Hospitals with a nurse category average hourly wage (as calculated in Step 4) of less than the national nurse category average hourly wage receive an occupational mix adjustment factor (as calculated in Step 6) of greater than 1.0.
Based on the 2016 occupational mix survey data, we determined (in Step 7 of the occupational mix calculation) that the national percentage of hospital employees in the nurse category is 42 percent, and the national percentage of hospital employees in the all other occupations category is 58 percent. At the CBSA level, the percentage of hospital employees in the nurse category ranged from a low of 27 percent in one CBSA to a high of 82 percent in another CBSA.
We compared the FY 2020 occupational mix adjusted wage indexes for each CBSA to the unadjusted wage indexes for each CBSA. Applying the occupational mix adjustment to the wage data resulted in the following:

These results indicate that a larger percentage of urban areas (56.6 percent) would benefit from the occupational mix adjustment than would rural areas (48.9 percent).
G. Application of the Rural Floor, Summary of Expired Imputed Floor Policy, and Application of the State Frontier Floor
1. Rural Floor
Section 4410(a) of Public Law 105-33 provides that, for discharges on or after October 1, 1997, the area wage index applicable to any hospital that is located in an urban area of a State may not be less than the area wage index applicable to hospitals located in rural areas in that State. This provision is referred to as the “rural floor”. Section 3141 of Public Law 111-148 also requires that a national budget neutrality adjustment be applied in implementing the rural floor. Based on the FY 2020 wage index associated with this final rule (which is available via the internet on the CMS website) and, as discussed in section III.N. of the preamble of this final rule, based on the calculation of the rural floor without the wage data of hospitals that have reclassified as rural under § 412.103, we estimate that 166 hospitals will receive an increase in their FY 2020 wage index due to the application of the rural floor.
2. Summary of Expired Imputed Floor Policy
As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41376 through 41380), the imputed floor under both the original methodology and the alternative methodology expired on September 30, 2018. As such, the wage index and impact tables associated with this FY 2020 IPPS/LTCH PPS final rule (which are available on the internet via the CMS website) do not reflect the imputed floor policy, and we are not applying a national budget neutrality adjustment for the imputed floor for FY 2020. For a complete discussion, we refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41376 through 41380). As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19393 through 19399), we sought public comments on proposals to help address wage index disparities under the IPPS. We refer readers to section III.N of this final rule for a summary of these public comments and our responses. We also sought public comments on how the expiration of the imputed floor has impacted hospitals in FY 2019.
Comment: Multiple commenters stated that hospitals in all-urban states are subject to financial and competitive disadvantage as they face unique conditions including close proximity to some of the most competitive and densely populated labor markets in the country. Commenters stated that residents of all-urban states have a multitude of options in employment opportunities and, as such, competition further drives up the cost of labor in the region. Multiple commenters stated that without the imputed floor policy, all-urban states lack the protection for hospitals located outside of predominant labor markets. Commenters also stated that rural and urban populations have unique health needs and access issues which should be addressed equitably to ensure that all patients have sufficient access to care and that all physicians are compensated fairly for their work. Multiple commenters also stated that they support a permanent fix to the geographic disadvantage faced by hospitals in all-urban states and that they urge CMS look at ways to maintain the rural floor for urban hospitals while also addressing the needs of rural hospitals. Commenters further stated that CMS should maintain the imputed floor policy, just as it had for more than a decade, since the policy was effective at addressing the competitive disadvantage suffered by all-urban states in the absence of an imputed floor index. Finally, multiple commenters urged CMS to consider the significant negative impact of discontinuing the imputed floor policy, and urged the agency to consider how this action has impacted the ability of hospitals within all-urban states to compete in high-wage labor markets while providing high-quality services to patients.
A commenter stated that prior to the expiration of the imputed floor policy, hospitals in Rhode Island had some of the slimmest operating margins in the nation and the immediate impact of the elimination of the imputed floor to hospitals in Rhode Island was a 9.5 percent reduction in Medicare payments resulting in a direct loss of $28 million in fee-for-service Medicare payments and an additional loss of approximately $12 million in Medicare managed care payments. This commenter stated that it is without question that the expiration of the imputed floor policy has already had a dramatic impact on the financial solvency of every hospital in Rhode Island that is evidenced by the negative hospital operating margins reported in the first and second quarter of FY 2019. According to the commenter, the decision to eliminate the imputed floor policy did not consider the unique characteristics of Rhode Island that exist in the labor market in Southeastern New England which contributes to strong competition for healthcare workers. The commenter stated that the hospitals in Rhode Island operate and compete for workforce within a short distance of the high wage labor markets in Massachusetts and Connecticut that currently benefit from higher reimbursement rates due to their state's rural floor. The commenter stated that every Rhode Island resident lives within 30 minutes of either Massachusetts or Connecticut and the commuter rail runs from Providence, Rhode Island to Boston, Massachusetts and takes less than one hour resulting in thousands of Rhode Island residents commuting to jobs in Massachusetts and Connecticut every day. The commenter further stated that the Medicare wage index policies in effect today placed their hospitals at a distinct labor market disadvantage with Massachusetts and Connecticut evidenced by the fact that Rhode Island currently exports 22 percent of its nurses to Massachusetts and Connecticut, while Massachusetts exports 3.5 percent to Connecticut and Rhode Island and Connecticut exports 4.7 percent to Massachusetts and Rhode Island. The commenter stated that if Rhode Island is unable to compete for skilled healthcare professionals, it will ultimately impact the access to care for Medicare beneficiaries and all Rhode Islanders. Finally the commenter stated that they request that CMS restore the imputed floor policy retroactively to October 1, 2018 in a non-budget neutral manner, due to the tremendous immediate impact on the hospitals in Rhode Island.
Multiple commenters stated that it is important to note that the discontinuation of the imputed floor policy for all-urban states further exacerbates the disproportionate impact of the wage index disparities proposals on hospitals within all-urban states. A commenter stated that the imputed floor policy addressed the inequities in the wage index, which CMS' FY 2020 wage index disparities proposals will compound. A commenter explained that in FY 2019 CMS stated, “By allowing the imputed rural floor to expire for all urban states . . . CMS has begun the process of making the wage index more equitable.” The commenter explained, however, that in FY 2020, CMS recognized that the FY 2020 wage index disparities proposals will have significant adverse financial impacts on hospitals. More specifically, the commenter stated that CMS' elimination of the imputed floor policy did not account for the immediate impact to hospitals in Rhode Island; however, CMS acknowledged with the FY 2020 wage index disparities proposal that it is aware of and attempting to account for potential impact of that proposal by proposing to cap any wage index decreases for FY 2020 (including wage index decreases experienced by hospitals with wage indexes in the top 25th percentile) at 5 percent under the reasoning that hospitals so harmed should not face such immediate and drastic cuts. The commenter stated that it is unfortunate that CMS did not act with this same deliberation when it summarily eliminated the imputed rural floor in FY 2019.
According to the commenter, as CMS continues to address what it considers to be disparities in the wage index and how it is implemented, it unfortunately creates yet another disparity for Rhode Island hospitals. The commenter stated that if CMS is unable to develop a reasonable alternative methodology, then the elimination of the imputed floor policy should be considered as part of the broader Medicare wage index disparities proposal which recognizes and includes protection from significant losses in one year. The commenter also requested consideration for reinstatement of the imputed floor policy in FY 2020, and that the imputed floor policy be applied to the FY 2020 wage index.
A commenter stated that the expiration of the imputed floor policy resulted in a loss of approximately $11 million for New Jersey hospitals in areas that receive a lower overall wage index than hospitals classified into major metropolitan areas. Another commenter stated they estimated that the imputed floor policy's benefit to New Jersey in FY 2019 would have been approximately $13 million. According to commenters, the elimination of this policy is added to the total tally of cuts and disadvantageous policies from which hospitals in high wage and all-urban states suffer. According to a commenter, New Jersey's geographic location bordering the first and sixth largest cities in the country and the compact size of the state, along with numerous commuting options, put further strain on the labor market. A commenter stated that due to the expiration of the imputed floor policy, their hospitals are now receiving $5.5 million less in payments from Medicare that could have been used to benefit patient care in myriad ways, particularly in the underserved areas, such as: Employment of additional physicians including primary care and specialists to ensure continued access to care; expansion of programs to provide needed services such as addressing food insecurity and childhood early intervention; and expansion of the numerous health programs already subsidized by their hospitals. The commenter stated not just one program was negatively affected by the elimination of the imputed floor policy, as there are numerous programs and opportunities to provide essential care in the communities they serve.
Response: We thank the commenters for their comments regarding how the expiration of the imputed floor has impacted hospitals in FY 2019. As discussed in the FY 2019 final rule (83 FR 41378), we have expressed reservations about the imputed floor considering that the imputed rural floor methodology creates a disadvantage in the application of the wage index to hospitals in States with rural hospitals but no urban hospitals receiving the rural floor. As we discussed in the FY 2008 IPPS/LTCH PPS final rule (72 FR 47322), the FY 2012 IPPS/LTCH PPS final rule (76 FR 51593), the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 19905), and the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20363), the application of the rural and imputed floors requires transfer of payments from hospitals in States with rural hospitals but where the rural floor is not applied to hospitals in States where the rural or imputed floor is applied. While we continue to have such reservations about the application of an imputed floor, we are summarizing the comments we received in this final rule for the public's information.
3. State Frontier Floor for FY 2020
Section 10324 of Public Law 111-148 requires that hospitals in frontier States cannot be assigned a wage index of less than 1.0000. (We refer readers to the regulations at 42 CFR 412.64(m) and to a discussion of the implementation of this provision in the FY 2011 IPPS/LTCH PPS final rule (75 FR 50160 through 50161).) In the FY 2020 IPPS/LTCH PPS proposed rule, we did not propose any changes to the frontier floor policy for FY 2020. We stated in the proposed rule that 45 hospitals would receive the frontier floor value of 1.0000 for their FY 2020 wage index. These hospitals are located in Montana, Nevada, North Dakota, South Dakota, and Wyoming.
We did not receive any public comments on the application of the State frontier floor for FY 2020. In this final rule, 45 hospitals will receive the frontier floor value of 1.0000 for their FY 2020 wage index. These hospitals are located in Montana, Nevada, North Dakota, South Dakota, and Wyoming.
The areas affected by the final rural and frontier floor policies for the final FY 2020 wage index are identified in Table 2 associated with this final rule, which is available via the internet on the CMS website.
H. FY 2020 Wage Index Tables
In the FY 2016 IPPS/LTCH PPS final rule (80 FR 49498 and 49807 through 49808), we finalized a proposal to streamline and consolidate the wage index tables associated with the IPPS proposed and final rules for FY 2016 and subsequent fiscal years. Prior to FY 2016, the wage index tables had consisted of 12 tables (Tables 2, 3A, 3B, 4A, 4B, 4C, 4D, 4E, 4F, 4J, 9A, and 9C) that were made available via the internet on the CMS website. Effective beginning FY 2016, with the exception of Table 4E, we streamlined and consolidated 11 tables (Tables 2, 3A, 3B, 4A, 4B, 4C, 4D, 4F, 4J, 9A, and 9C) into 2 tables (Tables 2 and 3). As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41380), beginning with FY 2019, we added Table 4 which is titled and includes a “List of Counties Eligible for the Out-Migration Adjustment under Section 1886(d)(13) of the Act” for the relevant fiscal year. We refer readers to section VI. of the Addendum to this final rule for a discussion of the final wage index tables for FY 2020.
I. Revisions to the Wage Index Based on Hospital Redesignations and Reclassifications
1. General Policies and Effects of Reclassification and Redesignation
Under section 1886(d)(10) of the Act, the Medicare Geographic Classification Review Board (MGCRB) considers applications by hospitals for geographic reclassification for purposes of payment under the IPPS. Hospitals must apply to the MGCRB to reclassify not later than 13 months prior to the start of the fiscal year for which reclassification is sought (usually by September 1). Generally, hospitals must be proximate to the labor market area to which they are seeking reclassification and must demonstrate characteristics similar to hospitals located in that area. The MGCRB issues its decisions by the end of February for reclassifications that become effective for the following fiscal year (beginning October 1). The regulations applicable to reclassifications by the MGCRB are located in 42 CFR 412.230 through 412.280. (We refer readers to a discussion in the FY 2002 IPPS final rule (66 FR 39874 and 39875) regarding how the MGCRB defines mileage for purposes of the proximity requirements.) The general policies for reclassifications and redesignations and the policies for the effects of hospitals' reclassifications and redesignations on the wage index are discussed in the FY 2012 IPPS/LTCH PPS final rule for the FY 2012 final wage index (76 FR 51595 and 51596). In addition, in the FY 2012 IPPS/LTCH PPS final rule, we discussed the effects on the wage index of urban hospitals reclassifying to rural areas under 42 CFR 412.103. Hospitals that are geographically located in States without any rural areas are ineligible to apply for rural reclassification in accordance with the provisions of 42 CFR 412.103.
On April 21, 2016, we published an interim final rule with comment period (IFC) in the Federal Register (81 FR 23428 through 23438) that included provisions amending our regulations to allow hospitals nationwide to have simultaneous § 412.103 and MGCRB reclassifications. For reclassifications effective beginning FY 2018, a hospital may acquire rural status under § 412.103 and subsequently apply for a reclassification under the MGCRB using distance and average hourly wage criteria designated for rural hospitals. In addition, we provided that a hospital that has an active MGCRB reclassification and is then approved for redesignation under § 412.103 will not lose its MGCRB reclassification; such a hospital receives a reclassified urban wage index during the years of its active MGCRB reclassification and is still considered rural under section 1886(d) of the Act and for other purposes.
We discussed that when there is both a § 412.103 redesignation and an MGCRB reclassification, the MGCRB reclassification controls for wage index calculation and payment purposes. We exclude hospitals with § 412.103 redesignations from the calculation of the reclassified rural wage index if they also have an active MGCRB reclassification to another area. That is, if an application for urban reclassification through the MGCRB is approved, and is not withdrawn or terminated by the hospital within the established timelines, we consider the hospital's geographic CBSA and the urban CBSA to which the hospital is reclassified under the MGCRB for the wage index calculation. We refer readers to the April 21, 2016 IFC (81 FR 23428 through 23438) and the FY 2017 IPPS/LTCH PPS final rule (81 FR 56922 through 56930) for a full discussion of the effect of simultaneous reclassifications under both the § 412.103 and the MGCRB processes on wage index calculations.
2. MGCRB Reclassification and Redesignation Issues for FY 2020
a. FY 2020 Reclassification Application Requirements and Approvals
As previously stated, under section 1886(d)(10) of the Act, the MGCRB considers applications by hospitals for geographic reclassification for purposes of payment under the IPPS. The specific procedures and rules that apply to the geographic reclassification process are outlined in regulations under 42 CFR 412.230 through 412.280.
At the time this final rule was constructed, the MGCRB had completed its review of FY 2020 reclassification requests. Based on such reviews, there are 294 hospitals approved for wage index reclassifications by the MGCRB starting in FY 2020. Because MGCRB wage index reclassifications are effective for 3 years, for FY 2020, hospitals reclassified beginning in FY 2018 or FY 2019 are eligible to continue to be reclassified to a particular labor market area based on such prior reclassifications for the remainder of their 3-year period. There were 290 hospitals approved for wage index reclassifications in FY 2018 that will continue for FY 2020, and 275 hospitals approved for wage index reclassifications in FY 2019 that will continue for FY 2020. Of all the hospitals approved for reclassification for FY 2018, FY 2019, and FY 2020, based upon the review at the time of this final rule, 859 hospitals are in a MGCRB reclassification status for FY 2020 (with 30 of these hospitals reclassified back to their geographic location).
Under the regulations at 42 CFR 412.273, hospitals that have been reclassified by the MGCRB are permitted to withdraw their applications if the request for withdrawal is received by the MGCRB any time before the MGCRB issues a decision on the application, or after the MGCRB issues a decision, provided the request for withdrawal is received by the MGCRB within 45 days of the date that CMS' annual notice of proposed rulemaking is issued in the Federal Register concerning changes to the inpatient hospital prospective payment system and proposed payment rates for the fiscal year for which the application has been filed. For information about withdrawing, terminating, or canceling a previous withdrawal or termination of a 3-year reclassification for wage index purposes, we refer readers to § 412.273, as well as the FY 2002 IPPS final rule (66 FR 39887 through 39888) and the FY 2003 IPPS final rule (67 FR 50065 through 50066). Additional discussion on withdrawals and terminations, and clarifications regarding reinstating reclassifications and “fallback” reclassifications were included in the FY 2008 IPPS final rule (72 FR 47333) and the FY 2018 IPPS/LTCH PPS final rule (82 FR 38148 through 38150).
Changes to the wage index that result from withdrawals of requests for reclassification, terminations, wage index corrections, appeals, and the Administrator's review process for FY 2020 are incorporated into the wage index values published in this FY 2020 IPPS/LTCH PPS final rule. These changes affect not only the wage index value for specific geographic areas, but also the wage index value that redesignated/reclassified hospitals receive; that is, whether they receive the wage index that includes the data for both the hospitals already in the area and the redesignated/reclassified hospitals. Further, the wage index value for the area from which the hospitals are redesignated/reclassified may be affected.
Applications for FY 2021 reclassifications (OMB Control Number 0938-0573, expiration date January 31, 2021) are due to the MGCRB by September 3, 2019 (the first working day of September 2019). We note that this is also the deadline for canceling a previous wage index reclassification withdrawal or termination under 42 CFR 412.273(d). Applications and other information about MGCRB reclassifications may be obtained beginning in mid-July 2019, via the internet on the CMS website at: https://www.cms.gov/Regulations-and-Guidance/Review-Boards/MGCRB/index.html, or by calling the MGCRB at (410) 786-1174.
b. Elimination of Copy Requirement to CMS
Under regulations in effect prior to FY 2018 (42 CFR 412.256(a)(1)), applications for reclassification were required to be mailed or delivered to the MGCRB, with a copy to CMS, and were not allowed to be submitted through the facsimile (FAX) process or by other electronic means. Because we believed this previous policy was outdated and overly restrictive and to promote ease of application for FY 2018 and subsequent years, in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56928), we revised this policy to require applications and supporting documentation to be submitted via the method prescribed in instructions by the MGCRB, with an electronic copy to CMS.
We stated in the proposed rule (84 FR 19383) that, beginning with applications from hospitals to reclassify for FY 2020, the MGCRB requires applications, supporting documents, and subsequent correspondence to be filed electronically through the MGCRB module of the Office of Hearings Case and Document Management System (“OH CDMS”). Also, we stated that the MGCRB issues all of its notices and decisions via email and these documents are accessible electronically through OH CDMS. Registration instructions and the system user manual are available at: https://www.cms.gov/Regulations-and-Guidance/Review-Boards/MGCRB/Electronic-Filing.html.
Filing a reclassification application using OH CDMS entails completing required fields electronically and uploading supporting documentation. We stated in the proposed rule that we believe the requirement for hospitals to submit a copy of the application to CMS would now require hospitals to compile their application information in a different format than what is required by the MGCRB, which would result in additional burden for hospitals. Furthermore, we stated that we believe CMS can forgo the copy of applications provided by hospitals because the MGCRB's electronic module will facilitate CMS' verification of reclassification statuses during the wage index development process. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19383), we proposed to reduce burden for hospitals by eliminating the requirement to copy CMS. Specifically, we proposed to revise § 412.256(a)(1) to delete the requirement that an electronic copy of the application be sent to CMS, so that this section would specify that an application must be submitted to the MGCRB according to the method prescribed by the MGCRB.
Comment: Many commenters supported our proposal to no longer require that a copy of the application be submitted to CMS. The commenters stated that it will be less of a burden on hospitals. A few commenters applauded the proposal as a positive effort by CMS toward reducing administrative burden and duplication for hospitals, and encouraged CMS to continue seeking ways to modernize processes.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, for the reasons discussed in this final rule and the proposed rule, we are finalizing as proposed, without modification, our revisions to § 412.256(a)(1) to delete the requirement that an electronic copy of the application be sent to CMS, so that this section specifies that an application must be submitted to the MGCRB according to the method prescribed by the MGCRB.
c. Revision To Clarify Criteria for a Hospital Seeking Reclassification to Another Rural Area or Urban Area
Section 412.230(a)(4) of our regulations currently specifies that the rounding of numbers to meet certain mileage or qualifying percentage standards is not permitted when an individual hospital seeks wage index reclassification through the MGCRB. In this section, the regulation specifically cites paragraphs (b)(1), (b)(2), (d)(1)(iii), and (d)(1)(iv)(A) and (B). The qualifying percentage standards included in these paragraphs have been periodically updated, and additional paragraphs have been added in § 412.230 to reflect these changes. Specifically, paragraphs (d)(1)(iv)(C), (D), and (E) have been added to § 412.230 to reflect changes in the percentage standards implemented in FY 2002, FY 2010, and FY 2011, respectively. Although we have continued to apply the policy set forth at § 412.230(a)(4) to the updated percentage standards set forth in paragraphs (d)(1)(iv)(C), (D), and (E) in § 412.230, conforming changes to § 412.230(a)(4) were not made to reflect these new paragraphs. This oversight has caused some confusion. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19383), we proposed to revise § 412.230(a)(4) to clarify that the policy prohibiting the rounding of qualifying percentage standards applies to paragraphs (d)(1)(iv)(C), (D), and (E) in § 412.230. Specifically, we proposed to remove specific references to paragraphs (d)(1)(iv)(A) and (B) and instead cite paragraph (d)(1)(iv) as a more general reference to the specific standards.
We did not receive any public comments regarding this proposal. For the reasons discussed in this final rule and the proposed rule, we are finalizing the proposal, without modification, to revise § 412.230(a)(4) by removing specific references to paragraphs (d)(1)(iv)(A) and (B) and instead cite paragraph (d)(1)(iv) as a more general reference to the specific standards.
3. Redesignations Under Section 1886(d)(8)(B) of the Act
a. Lugar Status Determinations
In the FY 2012 IPPS/LTCH PPS final rule (76 FR 51599 through 51600), we adopted the policy that, beginning with FY 2012, an eligible hospital that waives its Lugar status in order to receive the out-migration adjustment has effectively waived its deemed urban status and, thus, is rural for all purposes under the IPPS effective for the fiscal year in which the hospital receives the out-migration adjustment. In addition, in that rule, we adopted a minor procedural change that would allow a Lugar hospital that qualifies for and accepts the out-migration adjustment (through written notification to CMS within 45 days from the publication of the proposed rule) to waive its urban status for the full 3-year period for which its out-migration adjustment is effective. By doing so, such a Lugar hospital would no longer be required during the second and third years of eligibility for the out-migration adjustment to advise us annually that it prefers to continue being treated as rural and receive the out-migration adjustment. In the FY 2017 IPPS/LTCH PPS final rule (81 FR 56930), we further clarified that if a hospital wishes to reinstate its urban status for any fiscal year within this 3-year period, it must send a request to CMS within 45 days of publication of the proposed rule for that particular fiscal year. We indicated that such reinstatement requests may be sent electronically to wageindex@cms.hhs.gov. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38147 through 38148), we finalized a policy revision to require a Lugar hospital that qualifies for and accepts the out-migration adjustment, or that no longer wishes to accept the out-migration adjustment and instead elects to return to its deemed urban status, to notify CMS within 45 days from the date of public display of the proposed rule at the Office of the Federal Register. These revised notification timeframes were effective beginning October 1, 2017. In addition, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38148), we clarified that both requests to waive and to reinstate “Lugar” status may be sent to wageindex@cms.hhs.gov. To ensure proper accounting, we request hospitals to include their CCN, and either “waive Lugar” or “reinstate Lugar”, in the subject line of these requests.
b. Clarification Regarding Accepting the Out-Migration Adjustment When the Out-Migration Adjustment Changes After Reclassification
Section 1886(d)(8)(B) of the Act provides that for purposes of a reclassification under this subsection, the Secretary shall treat a hospital located in a rural county adjacent to one or more urban areas as being located in the urban metropolitan statistical area to which the greatest number of workers in the county commute if certain criteria are met. Rural hospitals in these counties are commonly known as “Lugar” hospitals. This statutory provision specifies that Lugar status is mandatory (not optional) if the statutory criteria are met. However, as discussed in the FY 2012 IPPS/LTCH PPS proposed and final rules (76 FR 25885 through 25886 and 51599), Lugar hospitals located in counties that qualify for the out-migration adjustment are required to waive their Lugar urban status in its entirety in order to receive the out-migration adjustment. We stated our belief that this represents one permissible reading of the statute, given that section 1886(d)(13)(G) of the Act states that a hospital in a county that has an out-migration adjustment and that has not waived that adjustment under section 1886(d)(13)(F) of the Act is not eligible for reclassification under section 1886(d)(8) or (10) of the Act. Therefore, a hospital may opt to receive either its county's out-migration adjustment or the wage index determined by its Lugar reclassification.
We stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19384) that we have become aware of a potential issue with the current election process that requires further clarification. As discussed in the following section, the out-migration adjustment is calculated to provide a positive adjustment to the wage index for hospitals located in certain counties that have a relatively high percentage of hospital employees who reside in the county but work in a different county (or counties) with a higher wage index. When a county is determined to qualify for an out-migration adjustment, the final adjustment value is determined in accordance with section 1886(d)(13)(D) of the Act and is fixed by statute for a 3-year period under section 1886(d)(13)(F) of the Act. CMS performs an annual analysis to evaluate all counties without current out-migration adjustment values assigned, including counties where the out-migration adjustment value will be expiring after a 3-year period. Initial out-migration adjustment values are published in Table 4 associated with the IPPS proposed and final rules (which are available via the internet on the CMS website). We stated in the proposed rule that, due to various factors, including hospitals withdrawing or terminating MGCRB reclassifications, obtaining § 412.103 rural reclassifications, or corrections to hospital wage data, the amount of newly proposed (1st year) out-migration adjustment values may fluctuate between the proposed rule and the final rule (and subsequent correction notices). We stated that these fluctuations are typically minimal. However, we explained that in certain circumstances, after processing varying forms of reclassification, wage index values may change so that a county would no longer qualify for an out-migration adjustment. In particular, when changes in wage index reclassification status alter the State rural floor so that multiple CBSAs would be assigned the same wage index value, an out-migration adjustment may no longer be indicated for a county as there would be little, if any, differential in nearby wage index values. We stated in the proposed rule that this can lead to a situation where a hospital has opted to receive a nonexistent out-migration adjustment. We further stated that we believe this situation is not compatible with longstanding CMS policy preventing a hospital from waiving its deemed urban Lugar status outside the prescribed out-migration adjustment election process as previously described. Section 1886(d)(13)(G) of the Act specifies that a hospital in a county that has a wage index increase under section 1886(d)(13)(F) of the Act (the out-migration adjustment) and that has not waived such increase under section 1886(d)(13)(F) of the Act is not eligible for reclassification under section 1886(d)(8) or (10) of the Act during that period. As we discussed in the proposed rule, if there is no out-migration adjustment available to provide a wage index increase, the fact pattern for which CMS established the process for a hospital to opt to receive a county out-migration adjustment in lieu of its “Lugar” reclassification no longer applies, and the hospital must be assigned its deemed urban status. Therefore, in the proposed rule, we clarified that, in circumstances where an eligible hospital elects to receive the out-migration adjustment within 45 days of the public display date of the proposed rule at the Office of the Federal Register in lieu of its Lugar wage index reclassification, and the county in which the hospital is located would no longer qualify for an out-migration adjustment when the final rule (or a subsequent correction notice) wage index calculations are completed, the hospital's request to accept the out-migration adjustment would be denied, and the hospital would be automatically assigned to its deemed urban status under section 1886(d)(8)(B) of the Act. Final rule wage index values would be recalculated to reflect this reclassification, and in some instances, after taking into account this reclassification, the out-migration adjustment for the county in question could be restored in the final rule. However, as the hospital is assigned a Lugar reclassification under section 1886(d)(8)(B) of the Act, it would be ineligible to receive the county out-migration adjustment under section 1886(d)(13)(G) of the Act. Because the out-migration adjustment, once finalized, is locked for a 3-year period under section 1886(d)(13)(F) of the Act, the hospital would be eligible to accept its out-migration adjustment in either the second or third year.
c. Change to Lugar County Assignments
Section 1886(d)(8)(B) of the Act establishes a wage index reclassification process by which the Secretary is required to treat a hospital located in a rural county adjacent to one or more urban areas as being located in the urban metropolitan statistical area (MSA), or core based statistical area (CBSA), to which the greatest number of workers in the county commute if certain criteria are met. Rural hospitals in these counties are known as “Lugar” hospitals and the counties themselves are often referred to as “Lugar” counties. These Lugar counties are not located in any urban area, but are adjacent to one or more urban CBSAs. In determining whether a county qualifies as a Lugar county, sections 1886(d)(8)(B)(i) and (ii) of the Act require us to use the standards for designating MSAs published in the Federal Register by OMB based on the most recent available decennial population data. Based on OMB definitions (75 FR 37246 through 37252), a CBSA is composed of “central” counties and “outlying” counties. While “central” counties meet certain population density requirements and other urban characteristics, a county qualifies as an “outlying” county of a CBSA if it meets one of the following commuting requirements: (a) At least 25 percent of the workers living in the county work in the central county or counties of the CBSA; or (b) at least 25 percent of the employment in the county is accounted for by workers who reside in the central county or counties of the CBSA. Given the OMB standards, as previously discussed, when a county is located between two or more urban centers, these “central” county commuting patterns may be split between two or more CBSAs, and the 25-percent thresholds to qualify as an outlying county for any single CBSA may not be met. In such situations, the county would be considered rural according to CMS, based on the OMB definitions as previously discussed, as it would not be part of an urban CBSA. Section 1886(d)(8)(B) of the Act addresses this issue where a county would have qualified as an outlying urban county if all its central county commuting data to adjacent urban CBSAs were combined. Specifically, section 1886(d)(8)(B)(i) of the Act requires CMS to consider a rural county to be part of an adjacent CBSA if the rural county would otherwise be considered part of an urban area under the OMB standards for designating MSAs if the commuting rates used in determining outlying counties were determined on the basis of the aggregate number of resident workers who commute to (and, if applicable under the standards, from) the central county or counties of all contiguous MSAs. Section 1886(d)(8)(B)(i) of the Act further requires CMS to assign these Lugar counties to the CBSA to which the greatest number of workers in the county commute. We stated in the proposed rule (84 FR 19385) that since the implementation of section 1886(d)(8)(B) of the Act for discharges occurring after October 1, 1988, CMS' policy has been that, once a county qualifies as Lugar, the proper methodology for determining the CBSA to which the greatest number of workers in the county commute should be based on the same OMB dataset used to determine whether a county qualifies as an “outlying” county of a CBSA. These data are a summary of commuting patterns between the noncentral county being evaluated and the “central” county or counties of an urban metropolitan area (without taking into account outlying counties). We stated in the proposed rule that section 1886(d)(8)(B) of the Act clearly instructs CMS to use the OMB criteria for determining “outlying” counties when determining the list of qualifying Lugar counties. These criteria are limited to assessing commuting patterns to and from central counties. Further, we further stated that we do not believe the statute requires that CMS perform an additional and separate community analysis, taking into account outlying counties, to determine to which CBSA a Lugar county should be assigned. We explained that when CMS updated the OMB labor market delineations based on the 2010 decennial census in FY 2015, we were made aware that a hospital in Henderson County, TX (a Lugar county) disagreed with CMS' interpretation of the statute. In particular, the hospital stated that section 1886(d)(8)(B)(i) of the Act requires that CMS assign a qualified Lugar county to “the urban metropolitan statistical area to which the greatest number of workers in the county commute,” and that this instruction does not distinguish between an urban CBSA's central counties and outlying counties. The hospital claimed that the assignment of a Lugar county to a CBSA should not be based solely on commuting data and commuting patterns to and from the central county or counties of a CBSA, but should consider outlying counties as well.
We stated in the proposed rule that after consideration of this matter, we continue to believe that CMS' methodology is a reasonable interpretation of the statute. However, we stated that upon further consideration and analysis, we have determined that the Henderson, TX hospital's interpretation of section 1886(d)(8)(B) of the Act is a reasonable alternative. We explained that, after reanalyzing the commuting data used when developing the FY 2015 IPPS/LTCH PPS final rule (the American Community Survey commuting data for 2006 to 2010), we identified 10 instances where a rural county would have been assigned to a different CBSA if we had considered outlying counties in our analysis of the urban metropolitan statistical area to which the greatest number of workers in the county commute, as shown in the table in this section of this final rule.

Of these 10 counties, currently only 3 counties (Talladega, AL, Pearl River, MS, and Henderson, TX) contain IPPS hospitals (4 hospitals in total). We explained in the proposed rule (84 FR 19386) that when including “outlying” counties in the commuting analysis, the analysis suggests that generally (but not always) the revised CBSA assignment would be to a larger CBSA, which would be expected as larger CBSAs generally include a greater number of “outlying” counties. We stated in the proposed rule (84 FR 19887 through 19387) that after further consideration of this issue, we believe that inclusion of outlying counties in the commuting analysis for purposes of assigning counties that qualify as Lugar counties (the second step of the Lugar analysis), although not unambiguously required by statute, is a reasonable, and arguably more natural, reading of the language in section 1886(d)(8)(B)(i) of the Act. Accordingly, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19387), we proposed to modify the assigned CBSA for the 10 Lugar counties specified in the table set forth in the proposed rule for FY 2020. We stated in the proposed rule that we also planned to fully reevaluate this proposed policy and underlying methodologies, if finalized, when CMS updates Lugar county assignments, which typically occurs after OMB labor market delineations are updated in response to the next decennial census.
Comment: A commenter supported CMS' proposal to modify the assigned CBSA for the 10 Lugar counties. The commenter concurred that inclusion of both “central” and “outlying” counties in the commuting analysis for purposes of assigning counties that qualify as Lugar counties is a reasonable interpretation of section 1886(d)(8)(B)(i) of the Act.
Response: We appreciate the commenter's support of our proposal.
After consideration of the public comments we received, for the reasons discussed in this final rule and the proposed rule, we are finalizing as proposed, without modification, the revised CBSA assignments as described in the table set forth in the proposed rule (84 FR 19386) and as reflected in the table in this final rule. We further intend to reevaluate this policy and underlying methodologies when CMS updates Lugar county assignments after OMB labor market delineations are updated in response to the next decennial census.
J. Out-Migration Adjustment Based on Commuting Patterns of Hospital Employees
In accordance with section 1886(d)(13) of the Act, as added by section 505 of Public Law 108-173, beginning with FY 2005, we established a process to make adjustments to the hospital wage index based on commuting patterns of hospital employees (the “out-migration” adjustment). The process, outlined in the FY 2005 IPPS final rule (69 FR 49061), provides for an increase in the wage index for hospitals located in certain counties that have a relatively high percentage of hospital employees who reside in the county but work in a different county (or counties) with a higher wage index.
Section 1886(d)(13)(B) of the Act requires the Secretary to use data the Secretary determines to be appropriate to establish the qualifying counties. When the provision of section 1886(d)(13) of the Act was implemented for the FY 2005 wage index, we analyzed commuting data compiled by the U.S. Census Bureau that were derived from a special tabulation of the 2000 Census journey-to-work data for all industries (CMS extracted data applicable to hospitals). These data were compiled from responses to the “long-form” survey, which the Census Bureau used at that time and which contained questions on where residents in each county worked (69 FR 49062). However, the 2010 Census was “short form” only; information on where residents in each county worked was not collected as part of the 2010 Census. The Census Bureau worked with CMS to provide an alternative dataset based on the latest available data on where residents in each county worked in 2010, for use in developing a new out-migration adjustment based on new commuting patterns developed from the 2010 Census data beginning with FY 2016.
To determine the out-migration adjustments and applicable counties for FY 2016, we analyzed commuting data compiled by the Census Bureau that were derived from a custom tabulation of the American Community Survey (ACS), an official Census Bureau survey, utilizing 2008 through 2012 (5-year) Microdata. The data were compiled from responses to the ACS questions regarding the county where workers reside and the county to which workers commute. As we discussed in the FYs 2016, 2017, 2018, and 2019 IPPS/LTCH PPS final rules (80 FR 49501, 81 FR 56930, 82 FR 38150, and 83 FR 41384, respectively), the same policies, procedures, and computation that were used for the FY 2012 out-migration adjustment were applicable for FYs 2016 through 2019, and in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19387), we proposed to use them again for FY 2020. We have applied the same policies, procedures, and computations since FY 2012, and we believe they continue to be appropriate for FY 2020. We refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49500 through 49502) for a full explanation of the revised data source.
For FY 2020, the out-migration adjustment will continue to be based on the data derived from the custom tabulation of the ACS utilizing 2008 through 2012 (5-year) Microdata. For future fiscal years, we may consider determining out-migration adjustments based on data from the next Census or other available data, as appropriate. For FY 2020, we did not propose any changes to the methodology or data source that we used for FY 2016 (81 FR 25071). (We refer readers to a full discussion of the out-migration adjustment, including rules on deeming hospitals reclassified under section 1886(d)(8) or section 1886(d)(10) of the Act to have waived the out-migration adjustment, in the FY 2012 IPPS/LTCH PPS final rule (76 FR 51601 through 51602).) We did not receive any public comments on this proposed policy for FY 2020. Therefore, for FY 2020, we are finalizing our proposal, without modification, to continue using the same policies, procedures, and computation that were used for the FY 2012 outmigration adjustment and that were applicable for FY 2016, FY 2017, FY 2018, and FY 2019.
Table 2 associated with this final rule (which is available via the internet on the CMS website) includes the final out-migration adjustments for the FY 2020 wage index. In addition, as discussed in the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20367), we have added a Table 4, “List of Counties Eligible for the Out-Migration Adjustment under Section 1886(d)(13) of the Act.” For this final rule, Table 4 consists of the following: A list of counties that are eligible for the out-migration adjustment for FY 2020 identified by FIPS county code, the final FY 2020 out-migration adjustment, and the number of years the adjustment will be in effect. We believe this table makes this information more transparent and provides the public with easier access to this information. We note that we intend to make the information available annually via Table 4 associated with the IPPS/LTCH PPS proposed and final rules, and are including it among the tables associated with this FY 2020 IPPS/LTCH PPS final rule that are available via the internet on the CMS website.
K. Reclassification From Urban to Rural Under Section 1886(d)(8)(E) of the Act, Implemented at 42 CFR 412.103
1. Application for Rural Status and Lock-In Date
Under section 1886(d)(8)(E) of the Act, a qualifying prospective payment hospital located in an urban area may apply for rural status for payment purposes separate from reclassification through the MGCRB. Specifically, section 1886(d)(8)(E) of the Act provides that, not later than 60 days after the receipt of an application (in a form and manner determined by the Secretary) from a subsection (d) hospital that satisfies certain criteria, the Secretary shall treat the hospital as being located in the rural area (as defined in paragraph (2)(D)) of the State in which the hospital is located. We refer readers to the regulations at 42 CFR 412.103 for the general criteria and application requirements for a subsection (d) hospital to reclassify from urban to rural status in accordance with section 1886(d)(8)(E) of the Act. The FY 2012 IPPS/LTCH PPS final rule (76 FR 51595 through 51596) includes our policies regarding the effect of wage data from reclassified or redesignated hospitals.
Hospitals must meet the criteria to be reclassified from urban to rural status under § 412.103, as well as fulfill the requirements for the application process. There may be one or more reasons that a hospital applies for the urban to rural reclassification, and the timeframe that a hospital submits an application is often dependent on those reason(s). Because the wage index is part of the methodology for determining the prospective payments to hospitals for each fiscal year, we stated in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56931) that we believed there should be a definitive timeframe within which a hospital should apply for rural status in order for the reclassification to be reflected in the next Federal fiscal year's wage data used for setting payment rates.
Therefore, after notice of proposed rulemaking and consideration of public comments, in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56931 through 56932), we revised § 412.103(b) by adding paragraph (6) to specify that, in order for a hospital to be treated as rural in the wage index and budget neutrality calculations under §§ 412.64(e)(1)(ii), (e)(2), (e)(4), and (h) for payment rates for the next Federal fiscal year, the hospital's filing date (the lock-in date) must be no later than 70 days prior to the second Monday in June of the current Federal fiscal year and the application must be approved by the CMS Regional Office in accordance with the requirements of § 412.103.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41384 through 41386), we changed the lock-in date to provide for additional time in the ratesetting process and to match the lock-in date with another existing deadline, the usual public comment deadline for the IPPS proposed rule. We revised § 412.103(b)(6) to specify that, in order for a hospital to be treated as rural in the wage index and budget neutrality calculations under §§ 412.64(e)(1)(ii), (e)(2), (e)(4), and (h) for payment rates for the next Federal fiscal year, the hospital's application must be approved by the CMS Regional Office in accordance with the requirements of § 412.103 no later than 60 days after the public display date at the Office of the Federal Register of the IPPS proposed rule for the next Federal fiscal year.
The lock-in date does not affect the timing of payment changes occurring at the hospital-specific level as a result of reclassification from urban to rural under § 412.103. As we discussed in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56931) and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41385 through 41386), this lock-in date also does not change the current regulation that allows hospitals that qualify under § 412.103(a) to request, at any time during a cost reporting period, to reclassify from urban to rural. A hospital's rural status and claims payment reflecting its rural status continue to be effective on the filing date of its reclassification application, which is the date the CMS Regional Office receives the application, in accordance with § 412.103(d). The hospital's IPPS claims will be paid reflecting its rural status beginning on the filing date (the effective date) of the reclassification, regardless of when the hospital applies.
Comment: A commenter stated that denying rural reclassifications based on an arbitrary date would have significant negative impacts on the financial operations on many hospitals. The commenter also stated that section 1886(d)(8)(E) of the Act and the regulation at § 412.103 enable urban hospitals that meet certain criteria to reclassify as rural, and that the hospital needs to submit the reclassification request during the last quarter of a hospital's fiscal year.
Response: We reiterate that the lock-in date does not change the current regulation that allows hospitals that qualify under § 412.103(a) to request, at any time during a cost reporting period, to reclassify from urban to rural. In other words, we will not deny rural reclassifications after the lock-in date. Rather, the lock-in date is for ratesetting purposes only. With regard to the comment that hospitals need to submit a reclassification request during the last quarter of a hospital's fiscal year, we believe the commenter may be referring to the requirement at section 1886(d)(5)(C)(i) of the Act pursuant to which a hospital must submit its application for rural referral center (RRC) status during the last quarter of its cost reporting period. No such timing requirement applies to rural reclassifications under § 412.103, even those applications meeting the criteria at § 412.103(a)(3).
2. Change to the Regulations To Allow for Electronic Submission of Applications for Reclassification From Urban to Rural Status
The application requirements at § 412.103(b)(3) for reclassification from urban to rural status currently state that an application must be mailed to the CMS Regional Office by the requesting hospital and may not be submitted by facsimile or other electronic means. We stated in the proposed rule (84 FR 19388) that we believe that this policy is outdated and overly restrictive. In the interest of burden reduction and to promote ease of application, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19388), we proposed to eliminate the restriction on submitting an application by facsimile or other electronic means so that hospitals may also submit applications to the CMS Regional Office electronically. Accordingly, we proposed to revise § 412.103(b)(3) to allow a requesting hospital to submit an application to the CMS Regional Office by mail or by facsimile or other electronic means.
Comment: Many commenters supported this proposal to change the rural reclassification application requirements to allow for electronic submission. Commenters specifically expressed appreciation for the added flexibility and applauded CMS' effort to reduce burden and promote ease of application. A commenter stated that this proposal signifies a positive effort by CMS toward reducing administrative burden and duplication for hospitals, and encouraged the agency to continue to seek ways to modernize processes. Commenters urged CMS to finalize this proposed change to the regulations at § 412.103(b)(3).
Response: We appreciate the commenters' support of our proposal.
After consideration of the public comments we received, for the reasons discussed in this final rule and the proposed rule, we are finalizing as proposed, without modification, our change to the regulations at § 412.103(b)(3) to allow a requesting hospital to submit an application to the CMS Regional Office by mail or by facsimile or other electronic means.
3. Changes to Cancellation Requirements for Rural Reclassifications
Under current regulations at § 412.103(g)(1), hospitals, other than those hospitals that are rural referral centers (RRCs), may cancel a rural reclassification by submitting a written request to the CMS Regional Office not less than 120 days before the end of its current cost reporting period, effective beginning with the next full cost reporting period. Under the current regulations at § 412.103(g)(2), a hospital that was classified as an RRC under § 412.96 based on rural reclassification under § 412.103 may cancel its rural reclassification by submitting a written request to the CMS Regional Office not less than 120 days prior to the end of the Federal fiscal year and after being paid as rural for at least one 12-month cost reporting period. The RRC's cancellation of a § 412.103 rural reclassification is not effective until it has been paid as rural for at least one 12-month cost reporting period, and not until the beginning of the Federal fiscal year following both the request for cancellation and the 12-month cost reporting period.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19388), we proposed to revise the rural reclassification cancellation requirements at § 412.103(g) for hospitals classified as RRCs. Currently, § 412.103(g)(2) requires that, for a hospital that has been classified as an RRC based on rural reclassification under § 412.103, cancellation of a § 412.103 rural reclassification is not effective until the hospital that is classified as an RRC has been paid as rural for at least one 12-month cost reporting period, and not until the beginning of the Federal fiscal year following both the request for cancellation and the 12-month cost reporting period. We stated in the FY 2008 IPPS final rule (72 FR 47371 through 47373) that the goal of creating this minimum time period was to disincentivize hospitals from receiving a rural redesignation, obtaining RRC status to take advantage of special MGCRB reclassification rules, and then terminating their rural status. However, we stated in the proposed rule that, as suggested by a commenter in response to the April 22, 2016 interim final rule with comment period (81 FR 56926), this disincentive is no longer necessary now that hospitals can have simultaneous MGCRB and § 412.103 reclassifications. Accordingly, in the proposed rule, we proposed to revise § 412.103(g)(2)(iii) to specify that the provisions set forth at § 412.103(g)(2)(i) and (ii) are effective for all written requests submitted by hospitals on or after October 1, 2007 and before October 1, 2019 to cancel rural reclassifications. Therefore, we stated in the proposed rule that the reclassification cancellation requirements specific to RRCs at § 412.103(g)(2) would no longer apply for cancellation requests submitted on or after October 1, 2019. In addition, as further discussed below, we proposed to revise § 412.103(g) to include uniform reclassification cancellation requirements that would be applied to all hospitals effective for cancellation requests submitted on or after October 1, 2019.
As further discussed below, we proposed to revise the regulations at § 412.103(g) to set forth uniform requirements applicable to all hospitals for cancelling rural reclassifications. Currently, for non-RRCs, the cancellation of rural status is effective beginning with the hospital's next cost reporting period. A hospital that has a § 412.103 rural reclassification and that does not have an additional MGCRB or “Lugar” reclassification is assigned the rural wage index value for its State. We stated in the proposed rule (84 FR 19389) that because wage index values are determined and assigned to hospitals on a Federal fiscal year basis, when such an aforementioned hospital cancels its rural reclassification, the wage index value must be manually updated by the MAC to its appropriate urban wage index value. We further started that because the end dates of cost reporting periods vary among hospitals, this process can be cumbersome and some cancellation requests may not be processed in time to be accurately reflected in the IPPS final rule appendix tables. We stated that because there is no apparent advantage to continuing to link the rural reclassification cancellation date to a hospital's cost reporting period, we believe that, in the interests of reducing overall complexity and administrative burden, the cancellation of rural reclassification should be effective for all hospitals beginning with the next Federal fiscal year (that is, the Federal fiscal year following the cancellation request). In addition, we explained in the proposed rule that, similar to the current requirements at § 412.103(g)(2), we believe it would be appropriate to require hospitals to request cancellation not less than 120 days prior to the end of a Federal fiscal year. We stated that we believe this proposed 120-day timeframe would provide hospitals adequate time to assess and review reclassification options, and provide CMS adequate time to incorporate the cancellation in the wage index development process. As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41384 through 41386), we finalized a lock-in date for a new rural reclassification to be approved in order for a hospital to be treated as rural in the wage index and budget neutrality calculations under §§ 412.64(e)(1)(ii), (e)(2), (e)(4), and (h) for payment rates for the next Federal fiscal year. We stated that we considered using this deadline, which is 60 days after the public display date at the Office of the Federal Register of the IPPS proposed rule for the next Federal fiscal year, as the deadline to submit cancellation requests effective for the next Federal fiscal year. We explained that, while we see certain advantages with aligning various wage index deadlines to the same date, based on the public display date of the proposed rule, we believe the proposed deadline of not less than 120 days prior to the end of the Federal fiscal year would give hospitals adequate time to assess and review reclassification options, and CMS adequate time to incorporate the cancellation in the wage index and budget neutrality calculations under §§ 412.64(e)(1)(ii), (e)(2), (e)(4), and (h) for payment rates for the next Federal fiscal year. In addition, we stated that this proposed 120-day deadline is already familiar to many hospitals because it is similar to the current deadline under § 412.103(g)(2), and therefore, we believe implementation of the proposed deadline may pose less of a burden overall for many hospitals. For these reasons, we proposed to add paragraph (g)(3) to § 412.103 to specify that, for all written requests submitted by hospitals on or after October 1, 2019 to cancel rural reclassifications, a hospital may cancel its rural reclassification by submitting a written request to the CMS Regional Office not less than 120 days prior to the end of a Federal fiscal year, and the hospital's cancellation of the classification would be effective beginning with the next Federal fiscal year. In addition, we proposed to add paragraph (g)(1)(iii) to § 412.103 to specify that the provisions of paragraphs (g)(1)(i) and (ii) of § 412.103 are effective only for written requests submitted by hospitals before October 1, 2019 to cancel rural reclassification.
In addition, we proposed to codify into regulations a longstanding CMS policy regarding canceling a § 412.103 reclassification when a hospital opts to accept and receives its county out-migration adjustment in lieu of its “Lugar” reclassification. As discussed in the proposed rule (84 FR 19383), a hospital may opt to receive either its “Lugar” county reclassification established under section 1886(d)(8)(B) of the Act, or the county out-migration adjustment determined under section 1886(d)(13) of the Act. Such requests may be submitted to CMS by email to wageindex@cms.hhs.gov within 45 days of the public display date of the proposed rule for the next Federal fiscal year. We established this process because section 1886(d)(13)(G) of the Act prohibits a hospital from having both an out-migration wage index adjustment and reclassification under section 1886(d)(8) or (10) of the Act. Because § 412.103 reclassifications were established under section 1886(d)(8)(E) of the Act, a hospital cannot simultaneously have an out-migration adjustment and be reclassified as rural under § 412.103. In the FY 2012 IPPS/LTCH PPS final rule (76 FR 51600), we addressed a commenter's concern regarding timing issues for some hospitals that wish to receive their county out-migration adjustment, but would not have adequate time to also cancel their rural reclassification. In that rule, we stated that “we will allow the act of waiving Lugar status for the out-migration adjustment to simultaneously waive the hospital's deemed urban status and cancel the hospital's acquired rural status, thus treating the hospital as a rural provider effective on October 1.” We explained in the proposed rule (84 FR 19389) that, while this policy modification was initially discussed in the FY 2012 IPPS/LTCH PPS final rule in the context of hospitals wishing to obtain or maintain sole community hospital (SCH) or Medicare-dependent hospital (MDH) status, its application has not been limited to current or potential SCHs or MDHs. We stated that we continue to believe this policy of automatically canceling rural reclassifications when a hospital waives its Lugar reclassification to receive its out-migration adjustment reduces overall burden on hospitals by not requiring them to file a separate rural reclassification cancellation request. We also stated that we believe this policy reduces overall complexity for CMS, avoiding the need to track and process multiple cancellation requests. Accordingly, we stated that we believe this policy should be codified in the regulations at § 412.103.
Therefore, we proposed to add paragraph (g)(4) to § 412.103 to specify that a rural reclassification will be considered cancelled effective for the next Federal fiscal year when a hospital opts (by submitting a request to CMS within 45 days of the date of public display of the proposed rule for the next Federal fiscal year at the Office of the Federal Register in accordance with the procedure described in section III.I.3. of the preamble of the FY 2020 proposed rule) to accept and receives its county out-migration wage index adjustment determined under section 1886(d)(13) of the Act in lieu of its geographic reclassification described under section 1886(d)(8)(B) of the Act. We stated that if the hospital wishes to once again obtain a § 412.103 rural reclassification, it would have to reapply through the CMS Regional Office in accordance with § 412.103, and the hospital would once again be ineligible to receive its out-migration adjustment. We noted that, in a case where a hospital reclassified as rural under § 412.103 wishes to receive its out-migration adjustment but does not qualify for a “Lugar” reclassification, the hospital would need to formally cancel its § 412.103 rural reclassification by written request to the CMS Regional Office within the timeframe specified at § 412.103. Finally, in order to address the scenario described in section III.I.3.b. of the preamble of the proposed rule (84 FR 19384), we noted that, in proposed § 412.103(g)(4), we were providing that the hospital must not only opt to accept, but also receive, its county out-migration wage index adjustment to trigger cancellation of rural reclassification under that provision. We stated that in such cases where an out-migration adjustment is no longer applicable based on the wage index in the final rule, a hospital's rural reclassification remains in effect (unless otherwise cancelled by written request to the CMS Regional Office within the timeframe specified at § 412.103).
Comment: Many commenters supported the proposal to apply uniform cancellation requirements that would allow all hospitals to cancel reclassifications 120 days before the end of the federal fiscal year, without having to be paid as rural for one 12 month cost reporting period. Some commenters specifically applauded CMS' efforts to reduce administrative burden.
Response: We appreciate the commenters' support and the acknowledgment of CMS' administrative burden reduction efforts.
After consideration of the public comments we received, for the reasons discussed in this final rule and in the proposed rule, we are finalizing, without modification, our proposed revisions discussed above with respect to cancellation of rural reclassification. Specifically, as proposed, our reclassification cancellation requirements specific to RRCs at § 412.103(g)(2) will no longer apply for cancellation requests submitted on or after October 1, 2019. As proposed, we are revising § 412.103(g)(2)(iii) to specify that the provisions set forth at § 412.103(g)(2)(i) and (ii) are effective for all written requests submitted by hospitals on or after October 1, 2007 and before October 1, 2019 to cancel rural reclassifications. In addition, as proposed, we are finalizing uniform reclassification cancellation requirements that will be applied to all hospitals effective for cancellation requests submitted on or after October 1, 2019. Specifically, we are adding paragraph (g)(3) to § 412.103 to specify that, for all written requests submitted by hospitals on or after October 1, 2019 to cancel rural reclassifications, a hospital may cancel its rural reclassification by submitting a written request to the CMS Regional Office not less than 120 days prior to the end of a Federal fiscal year, effective beginning with the next Federal fiscal year. Furthermore, as proposed, we are adding paragraph (g)(1)(iii) to § 412.103 to specify that the provisions of paragraphs (g)(1)(i) and (ii) of § 412.103 are effective only for written requests submitted by hospitals before October 1, 2019 to cancel rural reclassification.
We are also finalizing our proposal, without modification, to add paragraph (g)(4) to § 412.103 to codify our longstanding policy that a rural reclassification will be considered cancelled effective for the next Federal fiscal year when a hospital opts (by submitting a request to CMS within 45 days of the date of public display of the proposed rule for the next Federal fiscal year at the Office of the Federal Register in accordance with the procedure described in section III.I.3. of the preamble of the FY 2020 proposed rule) to accept and receives its county out-migration wage index adjustment determined under section 1886(d)(13) of the Act in lieu of its geographic reclassification described under section 1886(d)(8)(B) of the Act.
When these changes go into effect, there will not be a minimum period that a hospital must maintain its rural reclassification before it is eligible to cancel it. Currently, RRCs are required to maintain a rural reclassification for at least 1 year. As previously described above, this policy was finalized in the FY 2008 IPPS final rule (72 FR 47371 through 47373) to disincentivize hospitals from receiving a rural redesignation to obtain a certain benefit, and then immediately cancel the rural redesignation. While we no longer believe it is necessary to retain this specific policy to maintain acquired rural status for 1 year, we are aware of other potential situations where hospitals may attempt to exploit the rural reclassification process in order to obtain higher wage index values. For example, a hospital may obtain a rural reclassification with the intention of receiving its State's rural wage index. If the application is approved by the CMS Regional Office after our ratesetting “lock-in date”, the final rule rural wage index value would most likely not include the data for this hospital in the ratesetting calculation. This may incentivize relatively low wage index hospitals to time their applications to avoid reducing the State's rural wage index. These hospitals could then conceivably cancel their rural reclassifications (effective for next FY), and then reapply again after the “lock date.” We plan to monitor this situation over the course of FY 2020, and determine if it is necessary to take action to prevent this type of gaming in future rulemaking.
L. Process for Requests for Wage Index Data Corrections
1. Process for Hospitals To Request Wage Index Data Corrections
The preliminary, unaudited Worksheet S-3 wage data files and the preliminary CY 2016 occupational mix data files for the proposed FY 2020 wage index were made available on June 5, 2018 through the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/FY2020-Wage-Index-Home-Page.html.
On January 31, 2019, we posted a public use file (PUF) at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/FY2020-Wage-Index-Home-Page.html containing FY 2020 wage index data available as of January 30, 2019. This PUF contains a tab with the Worksheet S-3 wage data (which includes Worksheet S-3, Parts II and III wage data from cost reporting periods beginning on or after October l, 2015 through September 30, 2016; that is, FY 2016 wage data), a tab with the occupational mix data (which includes data from the CY 2016 occupational mix survey, Form CMS-10079), a tab containing the Worksheet S-3 wage data of hospitals deleted from the January 31, 2019 wage data PUF, and a tab containing the CY 2016 occupational mix data of the hospitals deleted from the January 31, 2019 occupational mix PUF. In a memorandum dated January 18, 2019, we instructed all MACs to inform the IPPS hospitals that they service of the availability of the January 31, 2019 wage index data PUFs, and the process and timeframe for requesting revisions in accordance with the FY 2020 Wage Index Timetable.
In the interest of meeting the data needs of the public, beginning with the proposed FY 2009 wage index, we post an additional PUF on the CMS website that reflects the actual data that are used in computing the proposed wage index. The release of this file does not alter the current wage index process or schedule. We notify the hospital community of the availability of these data as we do with the current public use wage data files through our Hospital Open Door Forum. We encourage hospitals to sign up for automatic notifications of information about hospital issues and about the dates of the Hospital Open Door Forums at the CMS website at: http://www.cms.gov/Outreach-and-Education/Outreach/OpenDoorForums/index.html.
In a memorandum dated April 20, 2018, we instructed all MACs to inform the IPPS hospitals that they service of the availability of the preliminary wage index data files and the CY 2016 occupational mix survey data files posted on May 18, 2018, and the process and timeframe for requesting revisions.
In a memorandum dated June 6, 2018, we corrected and reposted the preliminary wage file on our website because we realized that the PUF originally posted on May 18, 2018 did not include new line items that were first included in cost reports for cost reporting periods beginning on or after October 1, 2015 (and will be used for the first time in the FY 2020 wage index). Specifically, the lines are: Worksheet S-3, Part II, lines 14.01 and 14.02, and 25.50, 25.51, 25.52, and 25.53; and Worksheet S-3, Part IV, lines 8.01, 8.02, 8.03. In the same memorandum, we instructed all MACs to inform the IPPS hospitals that they service of the availability of the corrected and reposted preliminary wage index data files and the CY 2016 occupational mix survey data files posted on June 6, 2018, and the process and timeframe for requesting revisions.
If a hospital wished to request a change to its data as shown in the June 6, 2018 preliminary wage and occupational mix data files, the hospital had to submit corrections along with complete, detailed supporting documentation to its MAC by September 4, 2018. Hospitals were notified of this deadline and of all other deadlines and requirements, including the requirement to review and verify their data as posted in the preliminary wage index data files on the internet, through the letters sent to them by their MACs. November 16, 2018 was the deadline for MACs to complete all desk reviews for hospital wage and occupational mix data and transmit revised Worksheet S-3 wage data and occupational mix data to CMS.
November 6, 2018 was the date by when MACs notified State hospital associations regarding hospitals that failed to respond to issues raised during the desk reviews. Additional revisions made by the MACs were transmitted to CMS throughout January 2019. CMS published the wage index PUFs that included hospitals' revised wage index data on January 31, 2019. Hospitals had until February 15, 2019, to submit requests to the MACs to correct errors in the January 31, 2019 PUF due to CMS or MAC mishandling of the wage index data, or to revise desk review adjustments to their wage index data as included in the January 31, 2019 PUF. Hospitals also were required to submit sufficient documentation to support their requests.
After reviewing requested changes submitted by hospitals, MACs were required to transmit to CMS any additional revisions resulting from the hospitals' reconsideration requests by March 22, 2019. Under our current policy as adopted in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38153), the deadline for a hospital to request CMS intervention in cases where a hospital disagreed with a MAC's handling of wage data on any basis (including a policy, factual, or other dispute) was April 4, 2019. Data that were incorrect in the preliminary or January 31, 2019 wage index data PUFs, but for which no correction request was received by the February 15, 2019 deadline, are not considered for correction at this stage. In addition, April 4, 2019 was the deadline for hospitals to dispute data corrections made by CMS of which the hospital is notified after the January 31, 2019 PUF and at least 14 calendar days prior to April 4, 2019 (that is, March 21, 2018), that do not arise from a hospital's request for revisions. We note that, as with previous years, for the proposed FY 2020 wage index, in accordance with the FY 2020 wage index timeline posted on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/FY2020-Wage-Index-Home-Page.html, the April appeals had to be sent via mail and email. We refer readers to the wage index timeline for complete details.
Hospitals were given the opportunity to examine Table 2 associated with the proposed rule, which was listed in section VI. of the Addendum to the proposed rule and available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/FY2020-Wage-Index-Home-Page.html. Table 2 associated with the proposed rule contained each hospital's proposed adjusted average hourly wage used to construct the wage index values for the past 3 years, including the FY 2016 data used to construct the proposed FY 2020 wage index. We noted in the proposed rule (84 FR 19390) that the proposed hospital average hourly wages shown in Table 2 only reflected changes made to a hospital's data that were transmitted to CMS by early February 2019.
We posted the final wage index data PUFs on April 30, 2019 via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/FY2020-Wage-Index-Home-Page.html. The April 2019 PUFs were made available solely for the limited purpose of identifying any potential errors made by CMS or the MAC in the entry of the final wage index data that resulted from the correction process previously described (the process for disputing revisions submitted to CMS by the MACs by March 21, 2019, and the process for disputing data corrections made by CMS that did not arise from a hospital's request for wage data revisions as discussed earlier).
After the release of the April 2019 wage index data PUFs, changes to the wage and occupational mix data could only be made in those very limited situations involving an error by the MAC or CMS that the hospital could not have known about before its review of the final wage index data files. Specifically, neither the MAC nor CMS will approve the following types of requests:
- Requests for wage index data corrections that were submitted too late to be included in the data transmitted to CMS by the MACs on or before March 21, 2018.
- Requests for correction of errors that were not, but could have been, identified during the hospital's review of the January 31, 2019 wage index PUFs.
- Requests to revisit factual determinations or policy interpretations made by the MAC or CMS during the wage index data correction process.
If, after reviewing the April 2019 final wage index data PUFs, a hospital believed that its wage or occupational mix data were incorrect due to a MAC or CMS error in the entry or tabulation of the final data, the hospital was given the opportunity to notify both its MAC and CMS regarding why the hospital believed an error exists and provide all supporting information, including relevant dates (for example, when it first became aware of the error). The hospital was required to send its request to CMS and to the MAC no later than May 30, 2019. May 30, 2019 was also the deadline for hospitals to dispute data corrections made by CMS of which the hospital was notified on or after 13 calendar days prior to April 4, 2019 (that is, March 22, 2019), and at least 14 calendar days prior to May 30, 2019 (that is, May 16, 2019), that did not arise from a hospital's request for revisions. (Data corrections made by CMS of which a hospital was notified on or after 13 calendar days prior to May 30, 2019 (that is, May 17, 2019) may be appealed to the Provider Reimbursement Review Board (PRRB).) Similar to the April appeals, beginning with the FY 2015 wage index, in accordance with the FY 2020 wage index timeline posted on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Wage-Index-Files-Items/FY2020-Wage-Index-Home-Page.html, the May appeals were required to be sent via mail and email to CMS and the MACs. We refer readers to the wage index timeline for complete details.
Verified corrections to the wage index data received timely (that is, by May 30, 2019) by CMS and the MACs were incorporated into the final FY 2020 wage index, which is effective October 1, 2019.
We created the processes previously described to resolve all substantive wage index data correction disputes before we finalize the wage and occupational mix data for the FY 2020 payment rates. Accordingly, hospitals that did not meet the procedural deadlines set forth earlier will not be afforded a later opportunity to submit wage index data corrections or to dispute the MAC's decision with respect to requested changes. Specifically, our policy is that hospitals that do not meet the procedural deadlines previously set forth (requiring requests to MACs by the specified date in February and, where such requests are unsuccessful, requests for intervention by CMS by the specified date in April) will not be permitted to challenge later, before the PRRB, the failure of CMS to make a requested data revision. We refer readers also to the FY 2000 IPPS final rule (64 FR 41513) for a discussion of the parameters for appeals to the PRRB for wage index data corrections. As finalized in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38154 through 38156), this policy also applies to a hospital disputing corrections made by CMS that do not arise from a hospital's request for a wage index data revision. That is, a hospital disputing an adjustment made by CMS that did not arise from a hospital's request for a wage index data revision would be required to request a correction by the first applicable deadline. Hospitals that do not meet the procedural deadlines set forth earlier will not be afforded a later opportunity to submit wage index data corrections or to dispute CMS' decision with respect to requested changes.
Again, we believe the wage index data correction process described earlier provides hospitals with sufficient opportunity to bring errors in their wage and occupational mix data to the MAC's attention. Moreover, because hospitals had access to the final wage index data PUFs by late April 2019, they had the opportunity to detect any data entry or tabulation errors made by the MAC or CMS before the development and publication of the final FY 2020 wage index by August 2019, and the implementation of the FY 2020 wage index on October 1, 2019. Given these processes, the wage index implemented on October 1 should be accurate. Nevertheless, in the event that errors are identified by hospitals and brought to our attention after May 30, 2019, we retain the right to make midyear changes to the wage index under very limited circumstances.
Specifically, in accordance with 42 CFR 412.64(k)(1) of our regulations, we make midyear corrections to the wage index for an area only if a hospital can show that: (1) The MAC or CMS made an error in tabulating its data; and (2) the requesting hospital could not have known about the error or did not have an opportunity to correct the error, before the beginning of the fiscal year. For purposes of this provision, “before the beginning of the fiscal year” means by the May deadline for making corrections to the wage data for the following fiscal year's wage index (for example, May 30, 2019 for the FY 2020 wage index). This provision is not available to a hospital seeking to revise another hospital's data that may be affecting the requesting hospital's wage index for the labor market area. As indicated earlier, because CMS makes the wage index data available to hospitals on the CMS website prior to publishing both the proposed and final IPPS rules, and the MACs notify hospitals directly of any wage index data changes after completing their desk reviews, we do not expect that midyear corrections will be necessary. However, under our current policy, if the correction of a data error changes the wage index value for an area, the revised wage index value will be effective prospectively from the date the correction is made.
In the FY 2006 IPPS final rule (70 FR 47385 through 47387 and 47485), we revised 42 CFR 412.64(k)(2) to specify that, effective on October 1, 2005, that is, beginning with the FY 2006 wage index, a change to the wage index can be made retroactive to the beginning of the Federal fiscal year only when CMS determines all of the following: (1) The MAC or CMS made an error in tabulating data used for the wage index calculation; (2) the hospital knew about the error and requested that the MAC and CMS correct the error using the established process and within the established schedule for requesting corrections to the wage index data, before the beginning of the fiscal year for the applicable IPPS update (that is, by the May 30, 2019 deadline for the FY 2020 wage index); and (3) CMS agreed before October 1 that the MAC or CMS made an error in tabulating the hospital's wage index data and the wage index should be corrected.
In those circumstances where a hospital requested a correction to its wage index data before CMS calculated the final wage index (that is, by the May 30, 2019 deadline for the FY 2020 wage index), and CMS acknowledges that the error in the hospital's wage index data was caused by CMS' or the MAC's mishandling of the data, we believe that the hospital should not be penalized by our delay in publishing or implementing the correction. As with our current policy, we indicated that the provision is not available to a hospital seeking to revise another hospital's data. In addition, the provision cannot be used to correct prior years' wage index data; and it can only be used for the current Federal fiscal year. In situations where our policies would allow midyear corrections other than those specified in 42 CFR 412.64(k)(2)(ii), we continue to believe that it is appropriate to make prospective-only corrections to the wage index.
We note that, as with prospective changes to the wage index, the final retroactive correction will be made irrespective of whether the change increases or decreases a hospital's payment rate. In addition, we note that the policy of retroactive adjustment will still apply in those instances where a final judicial decision reverses a CMS denial of a hospital's wage index data revision request.
2. Process for Data Corrections by CMS After the January 31 Public Use File (PUF)
The process set forth with the wage index timeline discussed in section III.L.1. of the preamble of this final rule allows hospitals to request corrections to their wage index data within prescribed timeframes. In addition to hospitals' opportunity to request corrections of wage index data errors or MACs' mishandling of data, CMS has the authority under section 1886(d)(3)(E) of the Act to make corrections to hospital wage index and occupational mix data in order to ensure the accuracy of the wage index. As we explained in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49490 through 49491) and the FY 2017 IPPS/LTCH PPS final rule (81 FR 56914), section 1886(d)(3)(E) of the Act requires the Secretary to adjust the proportion of hospitals' costs attributable to wages and wage-related costs for area differences reflecting the relative hospital wage level in the geographic areas of the hospital compared to the national average hospital wage level. We believe that, under section 1886(d)(3)(E) of the Act, we have discretion to make corrections to hospitals' data to help ensure that the costs attributable to wages and wage-related costs in fact accurately reflect the relative hospital wage level in the hospitals' geographic areas.
We have an established multistep, 15-month process for the review and correction of the hospital wage data that is used to create the IPPS wage index for the upcoming fiscal year. Since the origin of the IPPS, the wage index has been subject to its own annual review process, first by the MACs, and then by CMS. As a standard practice, after each annual desk review, CMS reviews the results of the MACs' desk reviews and focuses on items flagged during the desk review, requiring that, if necessary, hospitals provide additional documentation, adjustments, or corrections to the data. This ongoing communication with hospitals about their wage data may result in the discovery by CMS of additional items that were reported incorrectly or other data errors, even after the posting of the January 31 PUF, and throughout the remainder of the wage index development process. In addition, the fact that CMS analyzes the data from a regional and even national level, unlike the review performed by the MACs that review a limited subset of hospitals, can facilitate additional editing of the data that may not be readily apparent to the MACs. In these occasional instances, an error may be of sufficient magnitude that the wage index of an entire CBSA is affected. Accordingly, CMS uses its authority to ensure that the wage index accurately reflects the relative hospital wage level in the geographic area of the hospital compared to the national average hospital wage level, by continuing to make corrections to hospital wage data upon discovering incorrect wage data, distinct from instances in which hospitals request data revisions.
We note that CMS corrects errors to hospital wage data as appropriate, regardless of whether that correction will raise or lower a hospital's average hourly wage. For example, as discussed in section III.C. of the preamble of the FY 2019 IPPS/LTCH PPS final rule (83 FR 41364), in situations where a hospital did not have documentable salaries, wages, and hours for housekeeping and dietary services, we imputed estimates, in accordance with policies established in the FY 2015 IPPS/LTCH PPS final rule (79 FR 49965 through 49967). Furthermore, if CMS discovers after conclusion of the desk review, for example, that a MAC inadvertently failed to incorporate positive adjustments resulting from a prior year's wage index appeal of a hospital's wage-related costs such as pension, CMS would correct that data error and the hospital's average hourly wage would likely increase as a result.
While we maintain CMS' authority to conduct additional review and make resulting corrections at any time during the wage index development process, in accordance with the policy finalized in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38154 through 38156) and as first implemented with the FY 2019 wage index (83 FR 41389), hospitals are able to request further review of a correction made by CMS that did not arise from a hospital's request for a wage index data correction. Instances where CMS makes a correction to a hospital's data after the January 31 PUF based on a different understanding than the hospital about certain reported costs, for example, could potentially be resolved using this process before the final wage index is calculated. We believe this process and the timeline for requesting such corrections (as described earlier and in the FY 2018 IPPS/LTCH PPS final rule) promote additional transparency to instances where CMS makes data corrections after the January 31 PUF, and provide opportunities for hospitals to request further review of CMS changes in time for the most accurate data to be reflected in the final wage index calculations. These additional appeals opportunities are described earlier and in the FY 2020 Wage Index Development Time Table, as well as in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38154 through 38156).
M. Labor-Related Share for the FY 2020 Wage Index
Section 1886(d)(3)(E) of the Act directs the Secretary to adjust the proportion of the national prospective payment system base payment rates that are attributable to wages and wage-related costs by a factor that reflects the relative differences in labor costs among geographic areas. It also directs the Secretary to estimate from time to time the proportion of hospital costs that are labor-related and to adjust the proportion (as estimated by the Secretary from time to time) of hospitals' costs that are attributable to wages and wage-related costs of the DRG prospective payment rates. We refer to the portion of hospital costs attributable to wages and wage-related costs as the labor-related share. The labor-related share of the prospective payment rate is adjusted by an index of relative labor costs, which is referred to as the wage index.
Section 403 of Public Law 108-173 amended section 1886(d)(3)(E) of the Act to provide that the Secretary must employ 62 percent as the labor-related share unless this would result in lower payments to a hospital than would otherwise be made. However, this provision of Public Law 108-173 did not change the legal requirement that the Secretary estimate from time to time the proportion of hospitals' costs that are attributable to wages and wage-related costs. Thus, hospitals receive payment based on either a 62-percent labor-related share, or the labor-related share estimated from time to time by the Secretary, depending on which labor-related share resulted in a higher payment.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38158 through 38175), we rebased and revised the hospital market basket. We established a 2014-based IPPS hospital market basket to replace the FY 2010-based IPPS hospital market basket, effective October 1, 2017. Using the 2014-based IPPS market basket, we finalized a labor-related share of 68.3 percent for discharges occurring on or after October 1, 2017. In addition, in FY 2018, we implemented this revised and rebased labor-related share in a budget neutral manner (82 FR 38522). However, consistent with section 1886(d)(3)(E) of the Act, we did not take into account the additional payments that would be made as a result of hospitals with a wage index less than or equal to 1.0000 being paid using a labor-related share lower than the labor-related share of hospitals with a wage index greater than 1.0000. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41389 and 41390), for FY 2019, we continued to use a labor-related share of 68.3 percent for discharges occurring on or after October 1, 2018.
The labor-related share is used to determine the proportion of the national IPPS base payment rate to which the area wage index is applied. We include a cost category in the labor-related share if the costs are labor intensive and vary with the local labor market. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19393), for FY 2020, we did not propose to make any further changes to the national average proportion of operating costs that are attributable to wages and salaries, employee benefits, professional fees: Labor-related, administrative and facilities support services, installation, maintenance, and repair services, and all other labor-related services. Therefore, for FY 2020, we proposed to continue to use a labor-related share of 68.3 percent for discharges occurring on or after October 1, 2019.
As discussed in section IV.B. of the preamble of this final rule, prior to January 1, 2016, Puerto Rico hospitals were paid based on 75 percent of the national standardized amount and 25 percent of the Puerto Rico-specific standardized amount. As a result, we applied the Puerto Rico-specific labor-related share percentage and nonlabor-related share percentage to the Puerto Rico-specific standardized amount. Section 601 of the Consolidated Appropriations Act, 2016 (Pub. L. 114-113) amended section 1886(d)(9)(E) of the Act to specify that the payment calculation with respect to operating costs of inpatient hospital services of a subsection (d) Puerto Rico hospital for inpatient hospital discharges on or after January 1, 2016, shall use 100 percent of the national standardized amount. Because Puerto Rico hospitals are no longer paid with a Puerto Rico-specific standardized amount as of January 1, 2016, under section 1886(d)(9)(E) of the Act as amended by section 601 of the Consolidated Appropriations Act, 2016, there is no longer a need for us to calculate a Puerto Rico-specific labor-related share percentage and nonlabor-related share percentage for application to the Puerto Rico-specific standardized amount. Hospitals in Puerto Rico are now paid 100 percent of the national standardized amount and, therefore, are subject to the national labor-related share and nonlabor-related share percentages that are applied to the national standardized amount. Accordingly, for FY 2020, we did not propose a Puerto Rico-specific labor-related share percentage or a nonlabor-related share percentage.
We did not receive any public comments on our proposals related to the labor-related share percentage. Therefore, we are finalizing our proposals, without modification, to continue to use a labor-related share of 68.3 percent for discharges occurring on or after October 1, 2019 for all hospitals (including Puerto Rico hospitals) whose wage indexes are greater than 1.0000.
Tables 1A and 1B, which are published in section VI. of the Addendum to this FY 2020 IPPS/LTCH PPS final rule and available via the internet on the CMS website, reflect the national labor-related share, which is also applicable to Puerto Rico hospitals. For FY 2020, for all IPPS hospitals (including Puerto Rico hospitals) whose wage indexes are less than or equal to 1.0000, we are applying the wage index to a labor-related share of 62 percent of the national standardized amount. For all IPPS hospitals (including Puerto Rico hospitals) whose wage indexes are greater than 1.000, for FY 2020, we are applying the wage index to a labor-related share of 68.3 percent of the national standardized amount.
N. Policies To Address Wage Index Disparities Between High and Low Wage Index Hospitals
In the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20372), we invited the public to submit further comments, suggestions, and recommendations for regulatory and policy changes to the Medicare wage index. Many of the responses received from this request for information (RFI) reflect a common concern that the current wage index system perpetuates and exacerbates the disparities between high and low wage index hospitals. Many respondents also expressed concern that the calculation of the rural floor has allowed a limited number of States to manipulate the wage index system to achieve higher wages for many urban hospitals in those states at the expense of hospitals in other states, which also contributes to wage index disparities. For a summary of these comments and public comments received on wage index disparities in previous rules, see the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19393 through 19394) and the references therein.
To help mitigate these wage index disparities, including those resulting from the inclusion of hospitals with rural reclassifications under 42 CFR 412.103 in the calculation of the rural floor, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19393), we proposed to reduce the disparity between high and low wage index hospitals by increasing the wage index values for certain hospitals with low wage index values and decreasing the wage index values for certain hospitals with high wage index values to maintain budget neutrality, and changing the calculation of the rural floor, as further discussed below. We also proposed a transition for hospitals experiencing significant decreases in their wage index values.
1. Policies To Address Wage Index Disparities
a. Providing an Opportunity for Low Wage Index Hospitals To Increase Employee Compensation
As CMS and other entities have stated in the past, comprehensive wage index reform would require both statutory and regulatory changes, and could require new data sources. We stated in the proposed rule (84 FR 19394) that notwithstanding the challenges associated with comprehensive wage index reform, we agree with respondents to the request for information who indicated that some current wage index policies create barriers to hospitals with low wage index values from being able to increase employee compensation due to the lag between when hospitals increase the compensation and when those increases are reflected in the calculation of the wage index. (We noted that this lag results from the fact that the wage index calculations rely on historical data.) We also agreed that addressing this systemic issue does not need to wait for comprehensive wage index reform given the growing disparities between low and high wage index hospitals, including rural hospitals that may be in financial distress and facing potential closure. Therefore, in response to these concerns, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19395), we proposed a policy that would provide certain low wage index hospitals with an opportunity to increase employee compensation without the usual lag in those increases being reflected in the calculation of the wage index.
In general terms, we proposed to increase the wage index values for hospitals with a wage index value in the lowest quartile of the wage index values across all hospitals. As we discussed in the proposed rule, quartiles are a common way to divide a distribution, and therefore, we stated in the proposed rule we believe it is appropriate to divide the wage indexes into quartiles for this purpose. For example, the interquartile range is a common measure of variability based on dividing data into quartiles. Furthermore, quartiles are used to divide distributions for other purposes under the Medicare program. For example, when determining Medicare Advantage benchmarks, excluding quality bonuses, counties are organized into quartiles based on their Medicare fee-for-service (FFS) spending. Also, Congress chose the worst performing quartile of hospitals for the Hospital-Acquired Condition Reduction Program penalty. (We refer readers to section IV.J. of the preamble of this final rule for a discussion of the Hospital-Acquired Condition Reduction Program.) Having determined that quartiles are a reasonable method of dividing the distribution of hospitals' wage index values, we stated in the proposed rule that we believe that identifying hospitals in the lowest quartile as low wage index hospitals, hospitals in the second and third “middle” quartiles as hospitals with wages index values that are neither low nor high, and hospitals in the highest quartile as hospitals with high wage index values, is then a reasonable method of determining low wage index and high wage index hospitals for purposes of our proposals (discussed below) addressing wage index disparities. We stated that while we acknowledge there is no set standard for identifying hospitals as having low or high wage index values, we believe our proposed quartile approach is reasonable for this purpose, given that, as previously discussed, quartiles are a common way to divide distributions, and that our proposed approach is consistent with approaches used in other areas of the Medicare program.
We stated in the proposed rule that, based on the data for the proposed rule, for FY 2020, the 25th percentile wage index value across all hospitals was 0.8482. We stated in the proposed rule that if this policy is adopted in the final rule, this number would be updated in the final rule based on the final wage index values.
Under our proposed methodology, we proposed to increase the wage index for hospitals with a wage index value below the 25th percentile wage index. In the proposed rule (84 FR 19395), we proposed that the increase in the wage index for these hospitals would be equal to half the difference between the otherwise applicable final wage index value for a year for that hospital and the 25th percentile wage index value for that year across all hospitals. For example, as described in the proposed rule, assume the otherwise applicable final FY 2020 wage index value for a geographically rural hospital in Alabama is 0.6663, and the 25th percentile wage index value for FY 2020 is 0.8482. Half the difference between the otherwise applicable wage index value and the 25th percentile wage index value is 0.0910 (that is, (0.8482−0.6663)/2). Under our proposal, the FY 2020 wage index value for such a hospital would be 0.7573 (that is, 0.6663 + 0.0910).
We explained in the proposed rule (84 FR 19395) that some respondents to the request for information had indicated that CMS should establish a wage index floor for hospitals with low wage index values. However, as stated in the proposed rule, we believe that it is important to preserve the rank order of the wage index values under the current policy and, therefore, we proposed to increase the wage index for the low-wage index hospitals previously described by half the difference between the otherwise applicable final wage index value and the 25th percentile wage index value. We stated that we believe the rank order generally reflects meaningful distinctions between the employee compensation costs faced by hospitals in different geographic areas. We noted that although wage index value differences between areas may be artificially magnified by the current wage index policies, we do not believe those differences are nonexistent. For example, if we were to instead create a floor to address the lag issue previously discussed, it does not seem likely that hospitals in Puerto Rico and Alabama would have the same wage index value after hospitals in both areas have had the opportunity increase their employee compensation costs. We stated that we believe a distinction between their wage index values would remain because hospitals in these areas face different employee compensation costs in their respective labor market areas.
We proposed that this policy would be effective for at least 4 years, beginning in FY 2020, in order to allow employee compensation increases implemented by these hospitals sufficient time to be reflected in the wage index calculation. For the FY 2020 wage index, we proposed to use data from the FY 2016 cost reports. We stated in the proposed rule (84 FR 19395) that 4 years is the minimum time before increases in employee compensation included in the Medicare cost report could be reflected in the wage index data, and additional time may be necessary. We stated in the proposed rule that we intend to revisit the issue of the duration of the policy in future rulemaking as we gain experience under the policy if adopted.
The following are summaries of the comments we received regarding our proposal to provide an opportunity for low wage index hospitals to increase employee compensation, and our responses.
Comment: Many commenters expressed their support of our proposal to provide an opportunity for low wage index hospitals to increase employee compensation and indicated the negative impact low wage index values have on their local hospital's ability to attract and maintain a sufficient labor force. Many commenters indicated that the increase in wage index would allow employee compensation at low wage hospitals to rise to more competitive levels to help attract and retain skilled health care workers. Many commenters indicated that although the increase in the wage index is not permanent, it would still allow low wage hospitals to increase compensation and must be in place for 4 years to allow the employee compensation changes to be reflected in the wage index data. Many low wage index hospitals indicated that they have long desired to increase wages for employees and reinvest in their communities, and our proposal will give them the opportunity to do so.
Response: We appreciate the commenters' support of our proposal to provide an opportunity for low wage index hospitals to increase employee compensation. We agree with the commenters that in order to attract and maintain a sufficient labor force a hospital must provide adequate employee compensation. As further discussed later in this section, we believe our proposal to increase the wage index for low wage index hospitals will increase the accuracy of the wage index by appropriately reflecting the increased employee compensation that would occur (to attract and maintain a sufficient labor force) if not for the lag in the process between when a hospital increases its employee compensation and when that increase is reflected in the calculation of the wage index.
Comment: Some commenters who supported our proposal to provide an opportunity for low wage index hospitals to increase employee compensation also requested the proposal be expanded to address other hospitals, such as hospitals that have seen a significant decrease in their wage index over the past twenty years. In particular, some commenters argued that hospitals in eight specific CBSAs struggle to raise employee wages for many of the same reasons hospitals in low wage index areas struggle to raise employee wages. These commenters requested that over the next 4 years, for CBSAs meeting all of the following criteria:
- The CBSA does not benefit from implementation of our adjustment to the lowest quartile of wage index values.
- The CBSAs' wage index is less than 1.0000.
- The CBSA's wage index has fallen more than 10 percent from FY 2000 to FY 2019.
CMS increase the wage index in those CBSAs by half of the difference of the twenty year decline (that is, half of the difference in the FY 2000 wage index and the FY 2020 wage index).
Response: We disagree with these commenters. Raising the wage index values of certain hospitals above the 25th percentile and not other hospitals with similar wage index values distorts the rank order of the wage index, which for the reasons discussed above is a critical aspect of our proposal.
Comment: Many commenters objected to our proposal to provide an opportunity for low wage index hospitals to increase employee compensation. Such commenters generally noted that since we did not propose any method to ensure such hospitals increase employee compensation, there is no guarantee benefiting hospitals will increase employee compensation. Other commenters argued against the notion that a lag in wage data suppresses a hospital's ability to increase wages, and stated that any potential impact of this lag on a given hospital is mitigated by other factors, including the presence of other hospitals in their labor market area, and our proposal would therefore have little impact on the average hourly wage rates of low wage hospitals. Other commenters asserted that doing this through an increase in the wage index for low wage index hospitals removes the wage index's ability to provide a relative measure for wages across different geographic regions.
Response: We disagree with these commenters. In response to commenters who indicated that there is no method to ensure that hospitals increase their employee compensation, we note the policy is intended to provide an opportunity for low wage hospitals to increase their employee compensation, and we expect them to do so based on responses received to the request for information indicating that the lag between when hospitals increase the compensation and when those increases are reflected in the calculation of the wage index creates barriers to hospitals with low wage index values from being able to increase employee compensation as well as comments received on our proposal as summarized previously. However, as we indicated in the proposed rule, this was not proposed as a permanent policy. Once there has been sufficient time for that increased employee compensation to be reflected in the wage data, there should not be a continuing need for this policy. At the expiration of the policy, hospitals that have not increased their employee compensation in response to the wage index increase may experience a reduction in their wage index compared to when the policy was in effect. Conversely, at the expiration of the policy, hospitals that have increased their employee compensation may experience relatively little change in their wage index compared to when the policy was in effect. The future wage data from those hospitals will help us assess our reasonable expectation based on comments received in response to the request for information as well as proposal that low wage hospitals would increase employee compensation as a result of our proposal. This wage data will also help us and the public to assess the assertion by some commenters opposed to our proposal that any potential impact of the wage index data lag on a given hospital is mitigated by other factors and our proposal would have little impact on the average hourly wage rates of low wage hospitals. We disagree with these commenters. Based on the comments received from the low wage hospitals, we do expect them to increase their employee compensation and this increased compensation is expected to increase their average hourly wages.
In response to commenters who asserted that increasing the wage index for low wage index hospitals removes the wage index's ability to provide a relative measure for wages across different geographic regions, we believe, as noted earlier, that our proposal increases the accuracy of the wage index as a relative measure. As we discussed in the proposed rule (84 FR 19394 through 19395), under our current cost reporting process, there is a lag between the time a hospital makes employee compensation adjustments and the time these adjustments are reflected in the wage index. As we stated in the proposed rule, 4 years is the minimum time before increases in employee compensation included in the Medicare cost report could be reflected in the wage index data. We believe that if the lag did not exist and employee compensation increases could be more quickly reflected in the wage index values, low wage index hospitals would have been able to increase employee compensation. Our proposal will increase the accuracy of the wage index as a relative measure because it allows low wage index hospitals to increase their employee compensation in ways that we would expect if there were no lag in reflecting compensation adjustments in the wage index. Furthermore, as we stated in the proposed rule (84 FR 19395), our proposal to increase the wage index values for low wage index hospitals continues to preserve the rank order of wage index values and thus continues to reflect meaningful distinctions between the employee compensation costs faced by hospitals in different geographic areas. Based on comments received in response to our request for information and comments received on our proposed policy, we expect low wage hospitals to increase their employee compensation as a result of our proposed wage index increase. Our proposed policy will allow these expected increases to be more timely reflected in the wage index.
Comment: Some commenters indicated that the proposal is not consistent with the quartile system used in the Hospital-Acquired Condition Reduction Program as referenced in the proposed rule, noting that the Hospital-Acquired Condition Reduction Program uses quartiles based on ranking hospital performance against a particular metric. Commenters stated that in programs such as the Hospital-Acquired Condition Reduction Program, quartiles are used to incentivize or decentivize certain behaviors, but they do not augment or replace existing measures.
Response: As we noted in the proposed rule, the reference to the Hospital-Acquired Condition Reduction Program was intended just to show that quartiles are a common way to divide distributions, as the Hospital-Acquired Condition Reduction Program is a program that divides a distribution based on quartiles. It is immaterial that the Hospital-Acquired Condition Reduction Program itself serves a different purpose than our wage index proposal, in the same way it is immaterial the Medicare Advantage program serves a different purpose. The main point is not any commonality of purpose of the underlying programs, but that those programs use quartiles as a way a dividing a distribution. As we stated in the proposed rule, while we acknowledge there is no set standard for identifying hospitals as having low or high wage index values, we believe this quartile approach is reasonable for this purpose because it is a common way to divide distributions and is consistent with approaches used in other areas of the Medicare program.
Comment: Many commenters asserted that the rationale for our proposal was to address non-wage issues related to rural hospitals, the overall financial health of hospitals in low wage areas, or the broader issue of wage index reform. These commenters critiqued our proposal according to its effect on these issues and indicated that CMS should pursue alternative means to address these issues rather than the policy under consideration here.
Response: The wage index is a technical payment adjustment. The intent of our proposal is to increase the accuracy of the wage index as a technical adjustment, and not to use the wage index as a policy tool to address non-wage issues related to rural hospitals, or the laudable goals of the overall financial health of hospitals in low wage areas or broader wage index reform. As noted earlier, our proposal increases the accuracy of the wage index as a relative measure because it allows low wage index hospitals to increase their employee compensation in ways that we would expect if there were no lag between the time a hospital increases employee compensation and the time these increases are reflected in the wage index, and allows those increases to be more timely reflected in the wage index. While one effect of our proposal may be to improve the overall well-being of low wage hospitals, and we would welcome that effect, that is not the primary rationale for our proposal.
Comment: While many commenters were supportive of CMS' proposal to make this policy effective for 4 years, many other commenters objected. Some commenters pointed to the difficulty in sunsetting a policy that has been in effect for a number of years. Others argued there is no certainty that wage data 4 years from implementation would show that benefiting hospitals have raised wages (that is, the data may show benefiting hospitals gradually raised wages or not at all). Some argued that not all low wage hospitals will be able to raise wages immediately.
Response: As noted earlier, our proposal to increase the wage index for low wage index hospitals is intended to provide an opportunity for low wage hospitals to increase their employee compensation, which we believe, based on responses to the request for information as well as comments received on this proposal, that low wage index hospitals have been prevented from doing because of the lag between the time hospitals increase employee compensation and the time these increases are reflected in the wage index. Based on responses to the request for information as well as comments received on our proposal, we expect such hospitals to increase employee compensation as a result of this policy as noted previously. Once that increased employee compensation is reflected in the wage data, there may be no need for the continuation of the policy, given that we would expect the resulting increases in the wage index to continue after the temporary policy is discontinued.
We still intend to revisit the issue of the duration of the policy in future rulemaking as we gain experience under the policy. In response to commenters who indicated that it is difficult to sunset a policy that has been in effect for a number of years, we have routinely allowed transition policies related to changes in the wage index as a result of updated labor market areas to expire, and in the FY 2019 IPPS final rule we allowed the temporary imputed floor policy to expire. Just as it is within our rulemaking authority to adopt this policy, it also lies within our authority to discontinue it after it no longer serves to increase the accuracy of the wage index.
After consideration of the public comments we received, for the reasons discussed in this final rule and in the proposed rule, we are finalizing our proposal to increase the wage index for hospitals with a wage index value below the 25th percentile wage index by half the difference between the otherwise applicable final wage index value for a year for that hospital and the 25th percentile wage index value for that year across all hospitals, as proposed without modification. Based on the data for this final rule, for FY 2020, the 25th percentile wage index value across all hospitals is 0.8457. As proposed, this policy will be in effect for at least 4 fiscal years beginning October 1, 2019. As discussed above, we intend to revisit the issue of the duration of this policy in future rulemaking as we gain experience under the policy.
b. Budget Neutrality for Providing an Opportunity for Low Wage Index Hospitals To Increase Employee Compensation
As noted earlier and discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19393 through 19399), in response to the request for information on wage index disparities in the FY 2019 IPPS/LTCH PPS proposed rule, some respondents recommended that CMS create a wage index floor for low wage index hospitals, and that, in order to maintain budget neutrality, CMS reduce the wage index values for high wage index hospitals through the creation of a wage index ceiling.
In the proposed rule (84 FR 19395 through 19396), we stated our belief that while it would not be appropriate to create a wage index floor or a wage index ceiling as suggested in the previously summarized comment, we believed the suggestion that we provide a mechanism to increase the wage index of low wage index hospitals (as finalized in section III.N.2.a. of this final rule) while maintaining budget neutrality for that increase through an adjustment to the wage index of high wage index hospitals has two key merits. First, by compressing the wage index for hospitals on the high and low ends, that is, those hospitals with a low wage index and those hospitals with a high wage index, such a methodology increases the impact on existing wage index disparities more than by simply addressing one end. Second, such a methodology ensures those hospitals in the middle, that is, those hospitals whose wage index is not considered high or low, do not have their wage index values affected by this proposed policy. Thus, given the growing disparities between low wage index hospitals and high wage index hospitals, consistent with the previously summarized comment, we stated in the proposed rule our belief that it would be appropriate to maintain budget neutrality for the low wage index policy proposed in section III.N.3.a. of the preamble of the proposed rule by adjusting the wage index for high wage index hospitals.
As discussed earlier, we believe it is important to preserve the rank order of wage index values because the rank order generally reflects meaningful distinctions between the employee compensation costs faced by hospitals in different geographic areas. As indicated in the proposed rule, although wage index value differences between areas (including areas with high wage index hospitals) may be artificially magnified by the current wage index policies, we do not believe those differences are nonexistent, and therefore, we do not believe it would be appropriate to set a wage index ceiling or floor. Accordingly, in order to offset the estimated increase in IPPS payments to hospitals with wage index values below the 25th percentile under our proposal in section III.N.3.a. of the preamble of the proposed rule, we proposed to decrease the wage index values for hospitals with high wage index values, but preserve the rank order among those values, as further discussed in this final rule.
As discussed in section III.N.3.a. of the preamble of the proposed rule, we believe it is reasonable to divide all hospitals into quartiles based on their wage index value whereby we identify hospitals in the lowest quartile as low wage index hospitals, hospitals in the second and third “middle” quartiles as hospitals with wage index values that are neither high nor low, and hospitals in the highest quartile as hospitals with high wage index values. We stated in the proposed rule we believe our proposed quartile approach is reasonable for this purpose, given that, as previously discussed, quartiles are a common way to divide distributions, and this proposed approach is consistent with approaches used in other areas of the Medicare program. Therefore, we proposed to identify high wage index hospitals as hospitals in the highest quartile, and in the budget neutrality discussion that follows, we refer to hospitals with wage index values above the 75th percentile wage index value across all hospitals for a fiscal year as “high wage index hospitals.”
To ensure our proposal in section III.N.3.a. of the preamble of the proposed rule is budget neutral, we proposed to reduce the wage index values for high wage index hospitals using a methodology analogous to the methodology used to increase the wage index values for low wage index hospitals described in section III.N.3.a. of the preamble of the proposed rule; that is, we proposed to decrease the wage index values for high wage index hospitals by a uniform factor of the distance between the hospital's otherwise applicable wage index and the 75th percentile wage index value for a fiscal year across all hospitals.
We stated in the proposed rule that we believe we have authority to implement our lowest quartile wage index proposal in section III.N.3.a. of the preamble of the proposed rule and our budget neutrality proposal in section III.N.3.b. of the preamble of the proposed rule under section 1886(d)(3)(E) of the Act (which gives the Secretary broad authority to adjust for area differences in hospital wage levels by a factor (established by the Secretary) reflecting the relative hospital wage level in the geographic area of the hospital compared to the national average hospital wage level, and requires those adjustments to be budget neutral), and under our exceptions and adjustments authority under section 1886(d)(5)(I) of the Act.
Comment: The vast majority of commenters believed CMS should not apply budget neutrality at all to our proposed increase in the wage index for low wage hospitals as there are strong policy reasons not to do so, CMS does not have the statutory authority to do so, and/or it is not required by law. Many commenters specifically objected to our proposal to reduce the wage index values for hospitals in the top quartile indicating that it arbitrarily results in an inaccurate wage index for high wage hospitals, and it ignores the CMS audited wage data from high wage hospitals reflecting the actual labor costs of these hospitals. These commenters indicated that our proposed reduction to high wage hospitals undermines and is inconsistent with a wage index that is required to reflect real differences in labor costs based on data collected from IPPS hospitals.
Some commenters indicated that while they appreciate CMS' recognition of the fact that certain hospitals, including rural hospitals, may be in financial distress, facing potential closure, and in need of relief, there are high wage hospitals that have negative margins and also are struggling financially. Therefore, these commenters questioned whether a link can be made between the level of the Medicare wage index and hospitals' financial performance. These commenters stated that CMS has conducted no analysis or study establishing such a link, making the proposal a poorly researched, expensive, redistributive experiment. These commenters indicated our proposal effectively means that a struggling community hospital in a high-wage area would have to sustain Medicare payment cuts in order to subsidize arbitrary and possibly unfounded positive payment adjustments for hospitals in low-wage areas. These commenters questioned whether the Medicare wage index is the appropriate mechanism to attempt to improve the financial performance of low-wage index hospitals at the expense of high wage index hospitals.
Many commenters indicated that there is a high and increasing cost of living in high wage areas, and that high cost of living is reflected in the compensation provided to hospitals employees in those areas. These commenters indicated that our proposed budget neutrality adjustment targeted on high wage hospitals arbitrarily disregards these actual cost of living differences.
Many commenters indicated that the agency should not apply budget neutrality at all given the below-cost reimbursement that all inpatient PPS hospitals face and the lack of evidence to justify reductions to wage index values. Specifically, many of these commenters stated that Medicare currently reimburses IPPS hospitals less than the cost of care as evidenced both by survey data and declining Medicare margins over time. Many also stated that CMS did not indicate or provide evidence to show that wage index values above the 75th percentile are inaccurate or that those values do not reflect the wages paid by those hospitals. They indicated that CMS did not make any claims that these higher wage hospitals have wage index values that are unrepresentative of real wage information. They indicated that a policy that penalizes certain hospitals simply because of where they fall in the wage index distribution is not based on evidence and is arbitrary. They indicated that our proposed budget neutrality on high wage hospitals contradicts the efforts that both hospitals and CMS make in order to have consistent and accurate wage data reporting, including regular data submissions, revisions and audits.
Some commenters asserted that CMS has acknowledged that it is not required to increase the wage index values for low wage hospitals budget neutrally. Rather, CMS stated that “it would be appropriate to maintain budget neutrality” for the policy.
Some commenters indicated that our proposed budget neutrality adjustment on high wage hospitals penalizes certain rural hospitals. Specifically, these commenters indicated that the 75th percentile policy would reduce payments to 5 percent of rural IPPS hospitals, putting them at even more financial risk and likely worsening financial health and access concerns in certain rural areas. Other commenters indicated that it would negatively impact some safety net hospitals. A few commenters indicated that the proposal would negatively impact hospitals in all-urban states already suffering from the expiration of the imputed floor policy.
Commenters disagreed as to the budget neutrality approach CMS should take if our proposed increase in the wage index for low wage hospitals was implemented in a budget neutral manner. Some commenters supported our proposed budget neutrality adjustment on the top quartile indicating that hospitals in the middle two quartiles should not be impacted by increases in the lowest quartile. Other commenters, however, indicated that CMS should fund the increase through a national budget neutrality adjustment as is CMS's usual policy. (We note national budget neutrality on the standardized amount was one of the alternatives considered in the proposed rule (84 FR 19672)). These commenters claimed “selective” budget neutrality, as proposed by CMS, whereby a small subset of hospitals bears the entire burden of budget neutrality for a given CMS policy change is unprecedented, and it violates both the statutory purpose of the wage index and CMS' own long-standing policy of ensuring budget neutrality by spreading the cost of payment adjustments across all hospitals equally.
Similar to some comments made regarding our increase of the wage index values of hospitals in the lowest quartile, many commenters stated that the law does not provide CMS with the authority to reduce the wage index values of the high wage index hospitals and/or any wage index values to offset the increase in payments to the hospitals in the lowest quartile. Many of these commenters discussed both our authority under section 1886(d)(3)(E) and (d)(5)(I) of the Act. The legal comments included the following arguments.
With respect to our authority under 1886(d)(3)(E) of the Act, these commenters asserted that CMS states, but does not explain why, the statute setting forth the wage index provision gives it broad authority to institute a wage compression policy that, in essence, makes inaccurate the wage data values for half of the nation's hospitals. These commenters indicated that section 1886(d)(3)(E) of the Act provides a process for the adjustment of hospital payments to account “for area differences in hospital wage levels by a factor (established by the Secretary) reflecting the relative hospital wage level in the geographic area of the hospital compared to the national average hospital wage level[,]” and requires those adjustments to be budget neutral. These commenters indicated that the wage compression proposal violates the plain language of the statute because it will not result in an adjustment to the payment rates that reflect the actual wage data difference between the relative hospital wage levels in a geographic area compared to the national average, subject only to those adjustments that have been specifically set forth by Congress. The commenters indicated that our proposal clearly contradicts Congress' mandate.
Some commenters indicated that while certain of the details of the creation and implementation of the wage index may have been delegated by Congress to the agency, the statute nevertheless requires the Secretary to develop a mechanism to remove the effects of local wage differences. These commenters indicated that the payment adjustments to reflect area wage differences must be accurate. These commenters indicated that CMS' wage compression proposal does not remove the effects of local wage differences, but instead disregards accurately reported wage data for 50% of the nation's hospitals. These commenters asserted this is beyond the authority delegated to the agency and ignores the text of the statute whereby CMS is to adjust IPPS payments by a factor “reflecting the relative hospital wage level in the geographic area of the hospital compared to the national average hospital wage level.”
These commenters indicated that Congress instituted this statutory provision to identify actual differences in geographic labor costs relative to the national average and to account for them in the payments to hospitals, subject only to those adjustments that Congress has specifically authorized. These commenters indicated that Congress has authorized several adjustments in section 1886(d)(3)(E) of the Act to the hospital wage index adjustment, such as a budget neutrality adjustment, an adjustment to fix the wage-related portion at 62 percent, and a floor for frontier hospitals. These commenters stated that CMS has acted consistently with Congress' directives in the past, and has calculated the wage index based on actual wage data, subject only to those modifications specifically permitted by Congress and Congress has not authorized the wage compression adjustment. Moreover, these commenters asserted that CMS has instituted a process—the Wage Index Development Timetable—with detailed instructions for the sole purpose of ensuring that CMS has accurate wage index data from all IPPS hospitals. These commenters also noted that the data reported on Worksheet S-3 of the Medicare cost report are the only section of the cost report that is subject to a Medicare administrative contractor (MAC) review every single year. In addition to the MAC review, there is a subsequent additional secondary auditor with oversight of the MACs to ensure data are reported accurately. They indicated CMS has invested significant resources to ensure that the data reported and reflected in each year's cost reports are reliable and valid for the purposes of payment.
However, these commenters believe CMS is now proposing a policy that would use the wage data in a manner to rank the various hospitals so that the data of 25 percent of hospitals will be inaccurately and artificially pushed downwards to allow the data of a different 25 percent of hospitals to be inaccurately and artificially pushed upwards. They indicated that nothing in section 1886(d)(3)(E) of the Act suggests that Congress authorized CMS to institute a policy whereby half of the hospitals would receive wage index values that did not accurately match their actual values. Thus, these commenters asserted that CMS' proposal is beyond the authority granted by Congress, and CMS cannot lawfully institute our proposal under section 1886(d)(3)(E) of the Act.
These commenters also asserted that CMS' proposed action is ultra vires. They indicated that section 1886(d)(3)(E) of the Act contains only two exceptions. They indicated that Congress writes rules as well as exceptions. They stated that in section 1886(d)(3)(E) of the Act, Congress did both, establishing the basic rule in clause (i), and exceptions in clauses (ii) and (iii). Commenters stated these are the only exceptions that Congress has made, and that. Congress has not made any type of special exception to the first clause that would allow CMS to institute the wage compression policy. Thus, these commenters asserted that Congress did not give CMS the authority to implement the wage compression policy. As such, these commenters stated that the CMS-proposed action is ultra vires, and that the agency could not institute this proposal in conformance with section 1886(d)(3)(E) of the Act. These commenters further stated that, if Congress wanted to change the wage index in the manner proposed by CMS, it could have.
With respect to our exceptions and adjustments authority under section 1886(d)(5)(I) of the Act, these commenters stated—(1) this “catchall” cannot be used in a manner that vitiates the language and purpose of the rest of the statute, including section 1886(d)(5)(A) through (H) of the Act, as there must be limits to the authority granted to CMS under this section; (2) CMS is not acting by regulation, and, therefore, is not following 1886(d)(5)(I); and (3) if CMS does have the authority to make this change, this special authority is not required to be done in a budget neutral manner, as is clear from the statute where paragraph (d)(5)(I)(ii) references budget neutrality, but paragraph (d)(5)(I)(i) does not, and as is clear from relevant case law.
Response: As noted earlier, the intent of our proposal to increase the wage index for low wage hospitals is to increase the accuracy of the wage index as a technical adjustment, and not to use the wage index as a policy tool to address non-wage issues related to rural hospitals, or the laudable goals of the overall financial health of hospitals in low wage areas or broader wage index reform. As discussed previously, our proposal to increase the wage index for low wage index hospitals increases the accuracy of the wage index as a relative measure because it will allow low wage index hospitals to increase their employee compensation in ways that we would expect if there were no lag in reflecting compensation adjustments in the wage index. As we noted previously, we believe that many low wage index hospitals have been prevented from increasing compensation because of the lag under our cost reporting process between the time hospitals increase employee compensation and the time these increases are reflected in the wage index. Thus, under our proposal, we believe the wage index for low wage index hospitals will appropriately reflect the relative hospital wage level in those areas compared to the national average hospital wage level. Because our proposal is based on the actual wages that we expect low wage hospitals to pay, it falls within the scope of the authority of section 1886(d)(3)(E) of the Act. In particular, since our proposal will increase the accuracy of the wage index, we disagree with commenters' assertions that our proposal does not remove the effects of local wage differences, that it disregards accurately reported wage data, or that our proposal is beyond the authority granted to the agency under section 1886(d)(3)(E) of the Act whereby CMS is to adjust IPPS payments by a factor “reflecting the relative hospital wage level in the geographic area of the hospital compared to the national average hospital wage level.”
Under section 1886(d)(3)(E) of the Act, the wage index adjustment is required to be implemented in a budget neutral manner. However, even if the wage index were not required to be budget neutral under section 1886(d)(3)(E) of the Act, we would consider it inappropriate to use the wage index to increase or decrease overall IPPS spending. As noted above, the wage index not a policy tool but rather a technical adjustment designed to be a relative measure of the wages and wage-related costs of subsection (d) hospitals in the United States. As a result, if it is determined that section 1886(d)(3)(E) of the Act does not require the wage index to be budget neutral, we invoke our authority at 1886(d)(5)(I) of the Act in support of such a budget neutrality adjustment. Contrary to the suggestions of many commenters, we believe we could use our broad authority under that provision to promulgate such an adjustment to the extent it was determined that section 1886(d)(3)(E) of the Act was not available for that purpose.
We acknowledge, however, that some commenters have presented reasonable policy arguments that we should consider further regarding the relationship between our proposed budget neutrality adjustment targeting high wage hospitals and the design of the wage index to be a relative measure of the wages and wage-related costs of subsection (d) hospitals in the United States. Therefore, given that budget neutrality is required under section 1886(d)(3)(E) of the Act, given that even if it were not required, we believe it would be inappropriate to use the wage index to increase or decrease overall IPPS spending, and given that we wish to consider further the policy arguments raised by commenters regarding our budget neutrality proposal, we are finalizing a budget neutrality adjustment for our low wage hospital policy, but we are not finalizing our proposal to target that budget neutrality adjustment on high wage hospitals. Instead, consistent with CMS's current methodology for implementing wage index budget neutrality under section 1886(d)(3)(E) of the Act and the alternative approach we considered in the proposed rule (84 FR 19672), we are finalizing a budget neutrality adjustment to the national standardized amount for all hospitals so that the increase in the wage index for low wage index hospitals, as finalized in this rule, is implemented in a budget neutral manner.
As discussed above, some commenters asserted that the only adjustments to the wage index that are permitted under section 1886(d) of the Act are those specified by Congress in the statute (commenters specifically referred to the budget neutrality adjustment, the adjustment to set an alternative wage-related portion of 62 percent, and the floor for frontier hospitals). As we discussed in the proposed rule (84 FR 19396), section 1886(d)(3)(E) of the Act gives the Secretary broad authority to adjust for area differences in hospital wage levels by a factor (established by the Secretary) reflecting the relative hospital wage level in the geographic area of the hospital compared to the national average hospital wage level. The fact that section 1886(d) of the Act sets forth certain adjustments to the wage index calculation, such as those referred to by commenters, does not limit the exercise of our discretion under section 1886(d)(3)(E) of the Act in other respects.
After consideration of the public comments received, for the reasons discussed in this final rule and in the proposed rule, we are finalizing a budget neutrality adjustment for our low wage index hospital policy finalized in section III.N.2.a. of this final rule, but we are not finalizing our proposal to target that budget neutrality adjustment on high wage hospitals as we proposed (84 FR 19395 through 19396). Instead, consistent with CMS's current methodology for implementing wage index budget neutrality under section 1886(d)(3)(E) of the Act, and consistent with the alternative we considered in the proposed rule, we are finalizing a budget neutrality adjustment to the national standardized amount for all hospitals so that the increase in the wage index for low wage index hospitals, as finalized in this rule, is implemented in a budget neutral manner.
c. Preventing Inappropriate Payment Increases Due to Rural Reclassifications Under the Provisions of 42 CFR 412.103
We stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19396 through 19399) that we also agree with respondents to the request for information who indicated that another contributing systemic factor to wage index disparities is the rural floor. As discussed in the proposed rule, section 4410(a) of Public Law 105-33 provides that, for discharges on or after October 1, 1997, the area wage index applicable to any hospital that is located in an urban area of a State may not be less than the area wage index applicable to hospitals located in rural areas in that State. Section 3141 of Public Law 111-148 also requires that a national budget neutrality adjustment be applied in implementing the rural floor.
As we explained in the proposed rule, the rural floor policy was addressed by the Office of the Inspector General (OIG) in its recent November 2018 report, “Significant Vulnerabilities Exist in the Hospital Wage Index System for Medicare Payment” (A-01-17-00500), which is available on the OIG website at: https://oig.hhs.gov/oas/reports/region1/11700500.pdf. The OIG stated (we note that the footnote references included here are in the original document but are not carried here):
“The stated legislative intent of the rural floor was to correct the `anomaly' of `some urban hospitals being paid less than the average rural hospital in their States.' 9 However, we noted that MedPAC, an independent congressional advisory board, has since stated that it is `not aware of any empirical support for this policy,10 and that the policy is built on the false assumption that hospital wage rates in all urban labor markets in a State are always higher than the average hospital wage rate in rural areas of that State.” 11
As one simplified example that we presented in the proposed rule, for purposes of illustrating the rural floor policy, assume that the rural wage index for a State is 1.1000. Therefore, as we stated in the proposed rule, under current policy, the rural floor for that State would be 1.1000. Any urban hospital with a wage index value below 1.1000 in that State would have its wage index value raised to 1.1000. We further explained that the additional Medicare payments to those urban hospitals in that State increase the national budget neutrality adjustment for the rural floor provision.
As we discussed in the proposed rule (84 FR 19397), for a real world example of the impact of the rural floor policy, we point to FY 2018, in which 366 urban hospitals benefitted from the rural floor. The increase in the wage indexes of urban hospitals receiving the rural floor was offset by a nationwide decrease in all hospitals' wage indexes of approximately 0.67 percent. In Massachusetts, that meant that 36 urban hospitals received a wage index based on hospital wages in Nantucket, an island that is home to the only rural hospital contributing to the State's rural floor wage index. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38557), we estimated that those 36 hospitals would receive an additional $44 million in inpatient payments for the year. These increased payments were offset by decreased payments to hospitals nationwide, and those decreases were not based on actual local wage rates but on the current rural floor calculation.
We stated that as acknowledged by the OIG, CMS has long recognized the disparate impacts and unintended outcomes of the rural floor. We have stated that the rural floor creates a benefit for a minority of States that is then funded by a majority of States, including States that are overwhelmingly rural in character (73 FR 23528 and 23622). We also have stated that “as a result of hospital actions not envisioned by Congress, the rural floor is resulting in significant disparities in wage index and, in some cases, resulting in situations where all hospitals in a State receive a wage index higher than that of the single highest wage index urban hospital in the State” (76 FR 42170 and 42212).
As explained in the proposed rule, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41748), we indicated that wage index disparities associated with the rural floor significantly increased in FY 2019 with the urban to rural reclassification of an urban hospital in Massachusetts. We also noted that Massachusetts is not the only State where urban hospitals reclassified as rural under § 412.103 have a significant impact on the State's rural floor. We stated that this also occurs, for example, in Arizona and Connecticut. As discussed in the proposed rule, the rural floor policy was meant to address anomalies of some urban hospitals being paid less than the average rural hospital in their States, not to raise the payments of many hospitals in a State to the high wage level of a geographically urban hospital.
We noted in the proposed rule that, for FY 2020, the urban Massachusetts hospital reclassified as rural under § 412.103 has an approved MGCRB reclassification back to its geographic location, and, therefore, its MGCRB reclassification was used for wage index calculation and payment purposes in the proposed rule (that is, this hospital was not considered rural for wage index purposes). However, we stated in the proposed rule that under our current wage index policy as of the time of the FY 2020 proposed rule, the hospital would be able to influence the Massachusetts rural floor by withdrawing or terminating its MGCRB reclassification in accordance with the regulation at § 412.273 for FY 2020 or subsequent years. We note that this hospital did in fact withdraw its MGCRB reclassification back to its geographic location for the FY 2020 final rule, so absent our proposal, the Massachusetts rural floor would have been calculated using the high wages of this hospital.
Returning to our simplified example presented in the proposed rule, for purposes of illustrating the impact of an urban to rural reclassification on the calculation of the rural floor under current policy as of the time of the FY 2020 proposed rule, again assume that the rural wage index for a State is 1.1000. Therefore, under current policy, the rural floor for that State would be 1.1000. Any urban hospital with a wage index value below 1.1000 in that State would have its wage index value raised to 1.1000. However, now assume that one urban hospital in that State subsequently reclassifies from urban to rural and raises the rural wage index from 1.1000 to 1.2000. Now, solely because of a geographically urban hospital, the rural floor in that State would go from 1.1000 to 1.2000 under current policy.
As previously noted by OIG in the November 2018 report referenced, the stated legislative intent of the rural floor was to correct the “anomaly” of “some urban hospitals being paid less than the average rural hospital in their States.” (Report 105-149 of the Committee on the Budget, House of Representatives, to Accompany H.R. 2015, June 24, 1997, section 10205, page 1305.) We stated in the proposed rule that we believe that urban to rural reclassifications have stretched the rural floor provision beyond a policy designed to address such anomalies. We explained that, rather than raising the payment of some urban hospitals to the level of the average rural hospital in their State, urban hospitals may have their payments raised to the relatively high level of one or more geographically urban hospitals reclassified as rural. We further stated that the current state of affairs with respect to urban to rural reclassifications goes beyond the general criticisms of the rural floor policy by MedPAC, CMS, OIG, and many stakeholders. We stated in the proposed rule we believe an adjustment is necessary to address the unanticipated effects of urban to rural reclassifications on the rural floor and the resulting wage index disparities, including the inappropriate wage index disparities caused by the manipulation of the rural floor policy by some hospitals.
Therefore, given the circumstances, as previously described, the comments received on the request for information, and that urban to rural reclassifications have stretched the rural floor provision beyond a policy designed to address anomalies of some urban hospitals being paid less than the average rural hospital in their States, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19397), we proposed to remove urban to rural reclassifications from the calculation of the rural floor. In other words, we stated that under our proposal, beginning in FY 2020, the rural floor would be calculated without including the wage data of urban hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented at § 412.103). We stated in the proposed rule we believe our proposed calculation methodology is permissible under section 1886(d)(8)(E) of the Act and the rural floor statute (section 4410 of Pub. L. 105-33). We stated that section 1886(d)(8)(E) of the Act does not specify where the wage data of reclassified hospitals must be included. Therefore, we stated that we believe we have discretion to exclude the wage data of such hospitals from the calculation of the rural floor. Furthermore, we explained that the rural floor statute does not specify how the rural floor wage index is to be calculated or what data are to be included in the calculation. Therefore, we stated that we also believe we have discretion under the rural floor statute to exclude the wage data of hospitals reclassified under section 1886(d)(8)(E) of the Act from the calculation of the rural floor. We stated that we believe this proposed policy is necessary and appropriate to address the unanticipated effects of rural reclassifications on the rural floor and the resulting wage index disparities, including the effects of the manipulation of the rural floor by certain hospitals. As discussed in the proposed rule, the inclusion of reclassified hospitals in the rural floor calculation has had the unforeseen effect of exacerbating the wage index disparities between low and high wage index hospitals. Therefore, we explained that under our proposal, in the case of Massachusetts, for example, the geographically rural hospital in Nantucket would still be included in the calculation of the rural floor for Massachusetts, but a geographically urban hospital reclassified under § 412.103 would not.
Returning to our simplified example presented in the proposed rule for purposes of illustrating the impact of the proposed policy, again assume that the rural wage index for a State is 1.1000 without any hospital in the State having reclassified from urban to rural. Therefore, the rural floor for that State would be 1.1000. Any urban hospital with a wage index value below 1.1000 in that State would have its wage index value raised to 1.1000. However, again assume that one urban hospital in that State subsequently reclassifies from urban to rural and raises the rural wage index from 1.1000 to 1.2000. We stated that under our proposed policy, the rural floor in that State would not go from 1.1000 to 1.2000, but would remain at 1.1000 because urban to rural reclassifications would no longer impact the rural floor.
As we discussed earlier, we stated in the proposed rule that the purpose of our proposal to calculate the rural floor without including the wage data of urban hospitals reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented at § 412.103) was to address wage index disparities that result when urban hospitals may have their payments raised to the relatively high level of one or more geographically urban hospitals reclassified as rural. In particular, we stated in the proposed rule we believe that no urban hospital not reclassified as rural should have its payments raised to the relatively high level of one or more geographically urban hospitals reclassified as rural, and we believe it would be inappropriate to prevent this for one class of urban hospitals not reclassified as rural (that is, under the rural floor provision) but allow this for another. As such, for consistent treatment of urban hospitals not reclassified as rural, we also proposed to apply the provisions of section 1886(d)(8)(C)(iii) of the Act without including the wage data of urban hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented at § 412.103). We stated that because section 1886(d)(8)(C)(iii) of the Act provides that reclassifications under section 1886(d)(8)(B) of the Act and section 1886(d)(10) of the Act may not reduce any county's wage index below the wage index for rural areas in the State, we made this proposal to help ensure no urban hospitals not reclassified as rural, including those hospitals with no reclassification as well as those hospitals reclassified under section 1886(d)(8)(B) of the Act or section 1886(d)(10) of the Act, have their payments raised to the relatively high level of one or more geographically urban hospitals reclassified as rural. Specifically, for purposes of applying the provisions of section 1886(d)(8)(C)(iii) of the Act, we proposed to remove urban to rural reclassifications from the calculation of “the wage index for rural areas in the State in which the county is located” referred to in section 1886(d)(8)(C)(iii) of the Act.
Comment: Many commenters, including MedPAC, supported our proposal to remove urban to rural reclassifications from the calculation of the rural floor wage index. Some commenters asserted that CMS has the regulatory authority to determine how it calculates the rural floor, and the calculation should mirror the spirit and intent of law resulting in only the natural rural providers in a state to be considered when calculating a rural floor. Commenters strongly commended CMS for curbing the manipulative practice of some hospitals abusing the rural floor provision to inappropriately influence the rural floor wage index value, which many commenters stated exacerbates the wage index disparity between urban and rural hospitals. Commenters agreed with CMS that the use of urban to rural reclassifications to artificially inflate the rural floor has stretched the rural floor provision beyond its original intent. They stated that hospitals should not be penalized and bear the burden of declining reimbursement due to other hospitals manipulating their state wage index.
Many commenters stated that, in particular, the three states cited as examples in the proposed rule have benefitted to the detriment of hospitals in every other state due to budget neutrality. Commenters also stated they hope CMS will not be swayed by comments from hospitals that have been “unjustly enriched” by this policy over a number of years.
Several commenters stated that including urban to rural reclassifications in the rural floor calculation especially disadvantaged small, more rural states and financially distraught, struggling rural hospitals. In the words of a commenter, this “egregious loophole” has consistently disadvantaged rural and low wage hospitals.
Commenters stated that geographically urban hospitals should have no impact on the rural floor, and the proposal fairly achieves CMS' intent to address wage index disparities. Similarly, several commenters stated that the proposal allows hospitals to still seek designations requiring rural status and keeps the rural floor concept intact while preventing improper influencing of the area wage index. A commenter stated that removing the wage data of urban hospitals that have reclassified as rural from the rural floor is a “step in the right direction” to have the wage index reflect local labor prices.
A commenter stated that the proposal seems reasonable, but suggested that CMS monitor its impacts and reassess whether it accomplishes the intended policy goals.
Response: We appreciate the many comments in support of our proposal to remove the wage data of hospitals reclassified under § 412.103 from the rural floor calculation. As stated in the proposed rule, we believe this proposed policy is necessary and appropriate to address the unanticipated effects of rural reclassifications on the rural floor and the resulting wage index disparities, including the effects of the manipulation of the rural floor by certain hospitals. We intend to monitor whether the proposal accomplishes the aforementioned policy goals.
Comment: We also received many comments in opposition of this proposal. Many commenters requested that CMS continue to consider the wage data of hospitals reclassified under § 412.103 in the rural floor calculation. A few commenters requested CMS leave the current calculation of the rural floor in place until there is a broader solution resulting from CMS working with Congress. A commenter stated the proposal would actually penalize many rural states, rather than support them because many hospitals in states that are mostly rural in character benefit from the inclusion of urban hospitals reclassified as rural in the wage index rural floor. Commenters also stated that excluding reclassified hospitals from the rural floor is plainly inconsistent with the statutory language. Commenters stated that the statute does not draw any distinction between the “rural areas” used to calculate the rural floor under section 4410(a) of the Balanced Budget Act of 1997 and the “rural areas” that reclassified hospitals are to be treated as located in under section 1886(d)(8)(E) of the Act. According to these commenters, Congress intended the term “rural area” to have the same definition when applied to the rural floor and section 1886(d)(8)(E) of the Act. A commenter specifically stated that Congress did not create a subcategory of rural hospitals that are eligible for the rural wage index, but whose wages are not included in the calculation of a state's rural floor. Furthermore, this commenter stated that the precedent set by two cases, Geisinger Community Medical Center v. Burwell, and Lawrence + Memorial Hospital v. Burwell establishes that a reclassified hospital should be treated as a rural hospital for all purposes under IPPS, including wage reclassification.
Response: In the absence of broader wage index reform from Congress, we believe it is appropriate to revise the rural floor calculation as part of an effort to reduce wage index disparities. In response to the comment that many hospitals in states that are mostly rural benefit from the inclusion of urban hospitals in the wage index rural floor, the volume of comments that we received from stakeholders in mostly rural states supporting our proposal indicate that hospitals in such states were hurt more than helped by including hospitals with urban to rural reclassifications in the calculation of the rural floor. While urban hospitals in mostly rural states may benefit from an increase in the rural floor due to urban to rural reclassification, as the commenters suggest, other states with high wage urban hospitals using § 412.103 reclassifications to raise the rural floor can mitigate those gains for mostly rural states, due to budget neutrality.
Regarding CMS' statutory authority, as stated in the proposed rule, we believe our proposed calculation methodology is permissible under section 1886(d)(8)(E) of the Act (as implemented in § 412.103) and the rural floor statute (section 4410 of Pub. L. 105-33). Section 1886(d)(8)(E) of the Act does not specify where the wage data of reclassified hospitals must be included. Therefore, we believe we have discretion to exclude the wage data of such hospitals from the calculation of the rural floor. Furthermore, the rural floor statute does not specify how the rural floor wage index is to be calculated or what data are to be included in the calculation. Therefore, we also believe we have discretion under the rural floor statute to exclude the wage data of hospitals reclassified under section 1886(d)(8)(E) of the Act from the calculation of the rural floor. We note that under our proposal we would continue to calculate the rural floor based on the physical non-MSA area of a state, which is the same rural area to which a hospital is reclassified under section 1886(d)(8)(E) of the Act. However, for purposes of calculating the rural floor wage index for a state, we would not include in the rural area the data of hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act. As we discussed in the proposed rule (84 FR 19397), the stated legislative intent of the rural floor was to correct the “anomaly” of “some urban hospitals being paid less than the average rural hospital in their States.” (Report 105-149 of the Committee on the Budget, House of Representatives, to Accompany H.R. 2015, June 24, 1997, section 10205, page 1305). Under the current rural floor wage index calculation, rather than raising the payment of some urban hospitals to the level of the average rural hospital in their State, urban hospitals may have their payments raised to the relatively high level of one or more geographically urban hospitals reclassified as rural. We believe excluding the data of hospitals that reclassify as rural under section 1886(d)(8)(E) of the Act from the rural floor wage index is necessary and appropriate to address these unanticipated effects of rural reclassifications on the rural floor and the resulting wage index disparities, and is consistent with our authority under section 1886(d)(8)(E) of the Act and the rural floor statute.
We also note that our proposal is consistent with the decisions in Geisinger Community Medical Center v. Secretary, United States Department of Health and Human Services, 794 F.3d 383 (3d Cir. 2015) and Lawrence + Memorial Hospital v. Burwell, 812 F.3d 257 (2d Cir. 2016) in which the courts found that hospitals reclassified under § 412.013 must be considered rural for all purposes. Accordingly, it is CMS policy to consider hospitals reclassified as rural under § 412.103 as having rural status. For example, a hospital with a § 412.103 rural reclassification would receive the rural wage index and would use the rural mileage and wage criteria when applying for an MGCRB reclassification. But the issue whether to include the hospital's wage data for purposes of calculating the rural floor is separate from issues of the treatment of the hospital itself. The hospital is being treated as rural for section 1886(d) purposes regardless of whether its data is included for purposes of calculating the rural floor. We do not believe that the decisions in Geisinger and Lawrence+Memorial require any particular treatment of the wage data of hospitals reclassified under § 412.103 for purposes of calculating the rural floor. Those hospitals are being treated as rural because they are being allowed to reclassify through the MGCRB based on their rural designation under § 412.103, regardless of the treatment of their wage data for purposes of calculating the rural floor.
We believe that the strict reading of “rural for all purposes” to which the commenters subscribe is neither required by the text of the court decisions they cite nor appropriate from a policy perspective. For example, the wage data of a hospital with a § 412.103 rural redesignation is considered in its home geographic area in addition to the rural area to which it is reclassified for purposes of calculating the wage index. We believe that the commenters' reading would inappropriately require that the wage data for hospitals reclassified under § 412.103 be excluded from the wage index calculation of their geographic locations. Similarly, we believe that the commenters' reading that hospitals redesignated under § 412.103 must be treated as rural for all purposes could, if taken to its logical extreme, mean we must treat those hospitals as geographically located in the rural area. That could in turn potentially reduce a State's rural wage index value. The rural area wage index is held harmless from decreases due to any effect of wage index reclassification, but the hold harmless protection does not apply to the effect on the area wage index of hospitals geographically located in the area.
Comment: A commenter stated that rather than eliminating the benefit of gaming, CMS has created a competitive advantage for large, high cost urban hospitals that are able to reclassify as rural and receive the benefit of an increased rural area wage index while their lower cost competitors in their urban home geographic area that are not reclassified as rural are left with a reduced area wage index. Another commenter suggested reducing the potential for gaming by applying the rural floor only to rural hospitals in primarily urban states with only one or two rural facilities. Similarly, a commenter stated that any proposal should not disincentivize hospitals from reporting accurate data. Another commenter expressed understanding for CMS' concerns about the potential for gaming by engineering a rural floor for a state that is not reflective of the overall labor market for the state, but believed that the proposed solution “swings the pendulum too far in the other direction” by failing to recognize the unique healthcare skillset that requires urban and rural hospitals to compete in the same labor market. This commenter suggested the following alternative solutions:
- Allow urban hospitals to apply for reclassification to rural under the MGCRB for wage index purposes only. To prevent inflating the reclassified wage index, threshold criteria to show that the hospital operates in the same labor market as the State's rural hospitals could include an additional test that the hospital's average hourly wage is not more than 108 percent of the statewide rural average hourly wage.
- Set the floor for both urban and rural hospitals at the statewide average hourly wage. The commenter stated that state licensure of healthcare professions promotes a statewide healthcare labor market, and that this would therefore be a more realistic concept for a floor than a rural floor (even if comprised solely of geographically rural hospitals) which perpetuates the possibly erroneous perception that urban wages should not be lower than rural wages.
Another commenter requested that CMS calculate each rural reclassified wage index independently, by excluding all other reclassified hospitals from the calculation.
Response: We appreciate the commenters' recognition of our efforts to address gaming. In response to the first commenter who was concerned that CMS is creating a competitive advantage for large, high cost urban hospitals that are able to reclassify as rural and receive the benefit of an increased rural area wage index while their lower cost competitors in the home urban geographic area that are not reclassified as rural are left with a reduced area wage index, we note that the wage data of reclassified hospitals are included in both the hospital's geographic CBSA and the CBSA to which the hospital is reclassified for the wage index calculation. Accordingly, the wage data for a hospital with a § 412.103 redesignation are included in the wage index for its home geographic area and are also included in its State rural wage index (if including wage data for hospitals with a reclassification to a rural area raises the state's rural wage index). Therefore, we are unsure why the commenter believes that lower cost competitors are left with a reduced area wage index when a hospital reclassifies out of the urban area. In response to the second commenter, we do not believe we can apply the rural floor to rural hospitals because section 4410(a) of Public Law 105-33 provides that the area wage index applicable to any hospital that is located in an urban (emphasis added) area of a State may not be less than the area wage index applicable to hospitals located in rural areas in that State. With regard to the third comment, we agree that any proposal should not disincentivize hospitals from reporting accurate data and do not believe that our proposal disincentivizes accurate data reporting. Finally, with regard to the commenters' suggested alternatives, because we consider these comments to be outside the scope of the FY 2020 wage index proposals, we are not addressing them in this final rule but may consider them in future rulemaking.
Comment: A commenter requested that CMS completely eliminate the national budget neutral impact of the rural floor policy, but recognized this may be difficult to achieve absent legislative action.
Response: We agree with the commenter that this would be difficult to achieve without legislative action, as section 3141 of Public Law 111-148 requires that a national budget neutrality adjustment be applied in implementing the rural floor.
Comment: A commenter specifically supported CMS' proposed “thoughtful changes” to the rural floor wage index methodology so that the wage index of a State rural area could be differentiated from the state rural floor wage index. Several other commenters requested that CMS clarify the examples given in the proposed rule to confirm that the urban hospital reclassified as rural does obtain a wage index inclusive of that hospital's wage data.
Response: We appreciate the first commenter's support. In response to the commenters requesting clarification, we are confirming that an urban hospital reclassified as rural would obtain a wage index inclusive of that hospital's wage data under the proposed rural floor wage index policy. In the example in the proposed rule referred to by the commenter, where one urban hospital in a State reclassifies from urban to rural and raises the rural wage index from 1.1000 to 1.2000, the rural floor in that State would not go from 1.1000 to 1.2000, but would remain at 1.1000 because urban to rural reclassifications would no longer impact the rural floor. The rural wage index, however, would be raised to 1.2000 for the geographically rural hospitals and for hospitals reclassified as rural.
Comment: A commenter stated that hospitals that are reclassified as rural hospitals by CMS did so under allowable HHS authority and should not be penalized. Another commenter stated CMS' proposal will adversely impact urban hospitals that have made decisions to reclassify as rural under current policy and urged CMS to consider a three-year hold harmless period during which urban hospitals that have already reclassified as rural would be counted in each state's rural floor.
Response: We do not believe that this proposal penalizes or adversely impacts urban hospitals that have reclassified as rural. Hospitals reclassified as rural under § 412.103 would continue to maintain the benefits conferred by rural reclassification, as well as receive the rural wage index calculated including their data (provided that the hospital does not also have an MGCRB reclassification under section 1886(d)(10) of the Act or Lugar status under section 1886(d)(8)(B) of the Act).
After consideration of the public comments we received, for the reasons discussed in this final rule and in the proposed rule, we are finalizing without modification our proposal to calculate the rural floor without including the wage data of urban hospitals reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented at § 412.103). Additionally, we are finalizing without modification our proposal, for purposes of applying the provisions of section 1886(d)(8)(C)(iii) of the Act, to remove the wage data of urban hospitals reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented at § 412.103) from the calculation of “the wage index for rural areas in the State in which the county is located” referred to in section 1886(d)(8)(C)(iii) of the Act.
d. Transition for Hospitals Negatively Impacted
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19398), we stated we recognize that, absent further adjustments, the combined effect of the proposed changes to the FY 2020 wage index could lead to significant decreases in the wage index values for some hospitals depending on the data for the final rule. In the past, we have proposed and finalized budget neutral transition policies to help mitigate any significant negative impacts on hospitals of certain wage index proposals, and we stated in the proposed rule we believe it would be appropriate to propose a transition policy here for the same purpose. For example, in the FY 2015 IPPS/LTCH PPS final rule (79 FR 49957 through 49963), we finalized a budget neutral transition to address certain wage index changes that occurred under the new OMB CBSA delineations.
Therefore, for FY 2020, we proposed a transition wage index to help mitigate any significant decreases in the wage index values of hospitals compared to their final wage indexes for FY 2019. Specifically, for FY 2020, we proposed to place a 5-percent cap on any decrease in a hospital's wage index from the hospital's final wage index in FY 2019. In other words, we proposed that a hospital's final wage index for FY 2020 would not be less than 95 percent of its final wage index for FY 2019. We stated that this proposed transition would allow the effects of our proposed policies to be phased in over 2 years with no estimated reduction in the wage index of more than 5 percent in FY 2020 (that is, no cap would be applied the second year). We stated in the proposed rule we believe 5 percent is a reasonable level for the cap because it would effectively mitigate any significant decreases in the wage index for FY 2020. However, we sought public comments on alternative levels for the cap and accompanying rationale. We stated that, under the proposed transition policy, we would compute the proposed FY 2020 wage index for each hospital as follows.
Step 1.—Compute the proposed FY 2020 “uncapped” wage index that would result from the implementation of proposed changes to the FY 2020 wage index.
Step 2.—Compute a proposed FY 2020 “capped” wage index which would equal 95 percent of that provider's FY 2019 final wage index.
Step 3.—The proposed FY 2020 wage index is the greater of the “uncapped” wage index computed in Step 1 or the “capped” wage index computed in Step 2.
Comment: Commenters, including MedPAC, commended CMS for proposing the 5 percent cap to help transition providers through the proposed wage index changes. A commenter specifically agreed that the cap should only be applied for one year, while other commenters requested that hospitals negatively impacted should be given a longer transition to support hospitals continuing to experience a significant decrease, so as not to inflict financial harm on community hospitals.
Several commenters stated that the funding cliff created by the proposed policies for impacted hospitals is of sufficient magnitude that it will not be mitigated by a 5 percent cap. A commenter specifically recommended that the cap be extended for the entire proposal and that a cumulative cap be added as well to ensure no hospital loses more than 10 percent of its current cap overall. Another commenter stated that even a reduction of 5 percent could create significant financial problems for rural IPPS hospitals and that the cap does not provide long-term protection from reductions after one year, so CMS should exempt rural IPPS hospitals from any wage index reduction for FY 2020 and subsequent years. Additionally, MedPAC stated that the cap on wage index movements of more than 5 percent in one year should also be applied to increases in the wage index.
Some commenters indicated that there should be no transition policy because the transition policy benefits hospitals that have historically seen increases in their wage index due to one or more urban hospital in a state reclassifying as rural and increasing the rural floor in that state.
Response: We appreciate the commenters' input. We agree that a transition policy to help mitigate significant negative impacts on hospitals would be appropriate here. We believe that the proposed transition, which caps a hospital's final wage index for FY 2020 at not less than 95 percent of its final wage index for FY 2019, is sufficient to allow the effects of our proposed policies to be phased in over 2 years (that is, no cap would be applied the second year). As we stated in the proposed rule, we believe that 5 percent is a reasonable level for the cap because it would effectively mitigate any significant decreases in the wage index for FY 2020. We note that commenters did not suggest any alternate levels for the cap that they believed would be more appropriate. Regarding the commenter advocating for an additional cumulative cap, it is unclear what is meant by “10 percent of the current cap overall”. We are unsure what the commenter intended or how the commenter believes such a cumulative cap would work. As we stated above, we believe the 5 percent cap would effectively mitigate significant decreases in the wage index for FY 2020 and provide sufficient time for hospitals to adapt to the wage index policies that will be effective October 1, 2019.
Additionally, we do not believe it would be necessary or appropriate to have a longer transition. We believe a one year cap provides hospitals with declining payments sufficient time to plan appropriately for FY 2021 and future years, especially because some hospitals may be able to make reclassification choices to mitigate the decline. Furthermore, we disagree that there should be no transition. Because we are finalizing wage index changes that have significant payment implications, and consistent with our provision of transition periods in the past to mitigate large negative impacts on hospitals, we believe it would be appropriate to provide a wage index transition as proposed for FY 2020.
In response to the commenter requesting that CMS exempt IPPS rural hospitals from any wage index reduction for FY 2020 and subsequent years, we do not believe that such an exemption for all IPPS rural hospitals from any wage index reduction would promote an accurate wage index. Such an exemption for all IPPS rural hospitals would ignore the reality that average hourly wages may sometimes decline relative to the national average. Furthermore, such an exemption is not necessary as we believe that a 5 percent cap on wage index decreases for one year is sufficient to allow such hospitals to adjust to the wage index policies that will be effective October 1, 2019.
Finally, we appreciate MedPAC's suggestion that the cap on wage index movements of more than 5 percent should also be applied to increases in the wage index. However, as we discussed in the proposed rule, the purpose of the proposed transition policy, as well as those we have implemented in the past, is to help mitigate the significant negative impacts of certain wage index changes, not to curtail the positive impacts of such changes, and thus we do not think it would be appropriate to apply the 5 percent cap on wage index increases as well.
Comment: A few commenters sought clarification whether the 5 percent cap will be applied to all hospitals experiencing a wage index decrease from FY 2019 to FY 2020 regardless of circumstance, not just as a result of the proposals to address wage index disparities. The commenters specifically questioned whether hospitals that experience a wage index decrease for reasons such as losing an MGCRB reclassification, reclassifying from urban to rural under § 412.103, or changes to their wage index data would also have any decrease in their FY 2020 wage indexes compared to their final FY 2019 wage indexes capped at 5 percent. A commenter suggested that CMS move the budget neutrality computation and comparison earlier in the calculation so that it is only comparing the changes resulting from the proposed modifications to address wage index disparities, to eliminate the unintended consequences of the “flawed” approach in the proposed rule which limits losses even from normal, anticipated changes in the wage index calculations.
A few commenters also requested clarification regarding the applicability of the 5 percent cap on the wage index of a provider if it changes from urban to rural reclassification after the FY 2020 final rule is issued. For example, commenters questioned whether the hospital's wage index decrease would also be capped at a −5 percent change from their FY 2019 wage index if a decrease to a hospital's wage index occurs midyear during FY 2020 due to an urban to rural reclassification under § 412.103.
Additionally, a few commenters requested that CMS define the term “the hospital's final wage index in FY 2019” to clarify whether that refers to the final amount published in the FY 2019 IPPS final rule, the wage index paid to the hospital on the final day of FY 2019, or something else.
Response: We are clarifying that all hospitals will have any decrease in their wage indexes capped at 5 percent for FY 2020, regardless of circumstance causing the decline. With regard to the commenter who suggested that CMS only apply the transition to changes resulting from the proposed modifications to address wage index disparities, we note that it would be difficult to isolate changes due to the wage index disparities proposals because these proposals influence wage index and rural floor values, which may change hospitals' reclassification decisions as a result. Therefore, we believe that it is preferable in the interest of administrative simplicity, ease of implementation, and hospital financial planning, to apply the cap universally to all decreases in the wage index that occur during FY 2020, not just those resulting from our proposals to address wage index disparities.
In response to the commenters' requests for clarification regarding how the cap would be applied to midyear wage index changes, we will also apply this transition policy for FY 2020 to decreases in the FY 2020 final wage indexes that occur after FY 2020 final rule ratesetting. For example, a decrease in a hospital's wage index caused by a midyear FY 2020 wage index change would also be capped at a −5 percent change from FY 2019.
In response to the commenters who requested that we define the term “the hospital's final wage index in FY 2019”, we are clarifying that this refers to the final amount published in the FY 2019 IPPS final rule. We believe that using the publicly available wage indexes from the FY 2019 IPPS final rule facilitates transparency. A hospital can contact its MAC for assistance if it believes the incorrect wage index value was used as the basis for its transition and the MAC can make any appropriate correction.
After consideration of the public comments we received, for the reasons discussed in this final rule and the proposed rule, we are finalizing without modification our proposal, as clarified previously, to place a 5 percent cap on any decrease in a hospital's wage index from the hospital's final wage index in FY 2019 so that a hospital's final wage index for FY 2020 will not be less than 95 percent of its final wage index for FY 2019.
e. Transition Budget Neutrality
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19398), we proposed to apply a budget neutrality adjustment to the standardized amount so that our proposed transition (as previously described and in section III.N.3.d. of the preamble of the proposed rule (84 FR 19398)) for hospitals that could be negatively impacted is implemented in a budget neutral manner under our authority in section 1886(d)(5)(I) of the Act. We noted that implementing the proposed transition wage index in a budget neutral manner is consistent with past practice (for example, 79 FR 50372) where CMS has used its exceptions and adjustments authority under section 1886(d)(5)(I)(i) of the Act to budget neutralize transition wage index policies when such policies allow for the application of a transitional wage index only when it benefits the hospital. We stated that we believed, and continue to believe, that it would be appropriate to ensure that such policies do not increase estimated aggregate Medicare payments beyond the payments that would be made had we never proposed these transition policies (79 FR 50732). Therefore, for FY 2020, we proposed to use our exceptions and adjustments authority under section 1886(d)(5)(I)(i) of the Act to apply a budget neutrality adjustment to the standardized amount so that our proposed transition (described previously and in section III.N.3.d. of the preamble of the proposed rule) for hospitals negatively impacted is implemented in a budget neutral manner.
Specifically, we proposed to apply a budget neutrality adjustment to ensure that estimated aggregate payments under our proposed transition (as previously described in section III.N.3.d. of the preamble of the proposed rule) for hospitals negatively impacted by our proposed wage index policies would equal what estimated aggregate payments would have been without the proposed transition for hospitals negatively impacted. To determine the associated budget neutrality factor, we compared estimated aggregate IPPS payments with and without the proposed transition. To achieve budget neutrality for the proposed transition policy, we proposed to apply a budget neutrality adjustment factor of 0.998349 to the FY 2020 standardized amount, as further discussed in the Addendum to the proposed rule (84 FR 19398). We stated in the proposed rule that if this policy is adopted in the final rule, this number would be updated based on the final rule data.
We noted in the proposed rule (84 FR 19398 through 19399) that our proposal, discussed in section III.N.3.c. of the preamble of the proposed rule (84 FR 19396 through 19398), to prevent inappropriate payment increases due to rural reclassifications under § 412.103 would also be budget neutral, but this budget neutrality would occur through the proposed budget neutrality adjustments for geographic reclassifications and the rural floor that were discussed in the Addendum to the proposed rule.
Comment: MedPAC agreed that the 5 percent cap should be applied in a budget-neutral manner. Another commenter requested that CMS budget neutralize the impact of the 5 percent cap transition by reducing the wage indexes of the upper quartile rather than the standardized amount. The commenter stated that it would be much more appropriate to increase the upper quartile budget neutrality factor to whatever factor would be necessary to fund the 5 percent cap.
Response: We appreciate MedPAC and the commenter's input. As discussed previously, in order to further consider policy arguments raised by commenters, we are not finalizing our proposal to apply an adjustment to the wage index of high wage index hospitals to budget neutralize the wage index increase for low wage index hospitals (finalized in section III.N.3.b. of this final rule). We would need to further consider the same policy arguments before applying an adjustment to the wage indexes of high wage index hospitals to budget neutralize the transition policy finalized in this final rule. However, we continue to believe that it is appropriate and consistent with past practice (for example, 79 FR 50372) to budget neutralize this transition wage index policy by applying an adjustment to the standardized amount for all hospitals.
After consideration of the public comments we received, for the reasons discussed in this final rule and the proposed rule, we are finalizing our proposal, without modification, to apply a budget neutrality adjustment factor to the FY 2020 standardized amount for all hospitals to achieve budget neutrality for the transition policy, as further discussed in the Addendum of this final rule. Based on the final rule data, the budget neutrality adjustment factor to achieve budget neutrality for the transition policy is 0.998838. We refer readers to the Addendum of this final rule for further information regarding this budget neutrality calculation.
f. Alternatives Considered in the Proposed Rule
In the proposed rule (84 FR 19672), we considered a number of alternatives to our proposed policies to address wage index disparities. First, as an alternative to the proposed approach to budget neutralize the wage index increase for low wage index hospitals, we considered applying a budget neutrality adjustment factor to the standardized amount rather than focusing the adjustment on the wage index of high wage index hospitals. Second, we also considered mirroring our proposed approach of raising the wage index for low wage index hospitals by reducing the wage index values for high wage index hospitals by half the difference between the otherwise applicable final wage index value for these hospitals and the 75th percentile wage index value across all hospitals. We stated we would then make the estimated net effect on payments of—(1) the increase in the wage index for low wage index hospitals; and (2) the decrease in the wage index for high wage index hospitals budget neutral through an adjustment to the standardized amount. Finally, we considered creating a single national rural wage index area and rural wage index value, as further described in the proposed rule (84 FR 19672). We considered whether there currently exists a national rural labor market for hospital labor and, if not, whether we should facilitate the creation of such a national rural labor market through the establishment of this national rural wage index area.
Comments: In section III.N.2.b. of the preamble of this final rule, we summarized comments regarding the first alternative considered to budget neutralize the wage index increase for low wage index hospitals by applying a budget neutrality adjustment factor to the standardized amount rather than focusing the adjustment on the wage index of high wage index hospitals.
A few commenters provide feedback on the other two alternatives to CMS' wage index disparities proposals discussed in the proposed rule, namely (1) mirroring CMS' approach of raising the wage index for low wage index hospitals by reducing the wage index values for high wage index hospitals by half the difference between the otherwise applicable final wage index value for these hospitals and the 75th percentile wage index value, and (2) creating a national rural wage index area and national rural wage index. Some commenters who indicated that they supported a national rural wage index area indicated that they compete with bordering states for labor, or that a national rural wage index area would result in a higher wage index for many hospitals in their state. There was little support for the other alternative considered regarding reducing the wage index values for high wage index hospitals by half the difference between the otherwise applicable final wage index value for these hospitals and the 75th percentile wage index value due to the substantial redistributive effects of this alternative.
Response: In section III.N.2.b. of the preamble of this final rule, we address comments regarding the first alternative considered to budget neutralize the wage index increase for low wage index hospitals by applying a budget neutrality adjustment factor to the standardized amount rather than focusing the adjustment on the wage index of high wage index hospitals. For the reasons discussed in section III.N.2.b. of the preamble to this final rule, we are adopting this alternative considered in this final rule.
We appreciate the comments supporting the creation of a national rural wage index area and national rural wage index, but as we do not have evidence a national rural labor market exists or would be created if we were to adopt this alternative, this alternative would not increase the accuracy of the wage index. With respect to the comments we received on the alternative of reducing the wage index values for high wage index hospitals by half the difference between the otherwise applicable final wage index value for these hospitals and the 75th percentile wage index value, we believe the commenters' concerns regarding this alternative merit further consideration.
IV. Other Decisions and Changes to the IPPS for Operating System
A. Changes to MS-DRGs Subject to Postacute Care Transfer Policy and MS-DRG Special Payments Policies (§ 412.4)
1. Background
Existing regulations at 42 CFR 412.4(a) define discharges under the IPPS as situations in which a patient is formally released from an acute care hospital or dies in the hospital. Section 412.4(b) defines acute care transfers, and § 412.4(c) defines postacute care transfers. Our policy set forth in § 412.4(f) provides that when a patient is transferred and his or her length of stay is less than the geometric mean length of stay for the MS-DRG to which the case is assigned, the transferring hospital is generally paid based on a graduated per diem rate for each day of stay, not to exceed the full MS-DRG payment that would have been made if the patient had been discharged without being transferred.
The per diem rate paid to a transferring hospital is calculated by dividing the full MS-DRG payment by the geometric mean length of stay for the MS-DRG. Based on an analysis that showed that the first day of hospitalization is the most expensive (60 FR 45804), our policy generally provides for payment that is twice the per diem amount for the first day, with each subsequent day paid at the per diem amount up to the full MS-DRG payment (§ 412.4(f)(1)). Transfer cases also are eligible for outlier payments. In general, the outlier threshold for transfer cases, as described in § 412.80(b), is equal to the fixed-loss outlier threshold for nontransfer cases (adjusted for geographic variations in costs), divided by the geometric mean length of stay for the MS-DRG, and multiplied by the length of stay for the case, plus 1 day.
We established the criteria set forth in § 412.4(d) for determining which DRGs qualify for postacute care transfer payments in the FY 2006 IPPS final rule (70 FR 47419 through 47420). The determination of whether a DRG is subject to the postacute care transfer policy was initially based on the Medicare Version 23.0 GROUPER (FY 2006) and data from the FY 2004 MedPAR file. However, if a DRG did not exist in Version 23.0 or a DRG included in Version 23.0 is revised, we use the current version of the Medicare GROUPER and the most recent complete year of MedPAR data to determine if the DRG is subject to the postacute care transfer policy. Specifically, if the MS-DRG's total number of discharges to postacute care equals or exceeds the 55th percentile for all MS-DRGs and the proportion of short-stay discharges to postacute care to total discharges in the MS-DRG exceeds the 55th percentile for all MS-DRGs, CMS will apply the postacute care transfer policy to that MS-DRG and to any other MS-DRG that shares the same base MS-DRG. The statute directs us to identify MS-DRGs based on a high volume of discharges to postacute care facilities and a disproportionate use of postacute care services. As discussed in the FY 2006 IPPS final rule (70 FR 47416), we determined that the 55th percentile is an appropriate level at which to establish these thresholds. In that same final rule (70 FR 47419), we stated that we will not revise the list of DRGs subject to the postacute care transfer policy annually unless we are making a change to a specific MS-DRG.
To account for MS-DRGs subject to the postacute care policy that exhibit exceptionally higher shares of costs very early in the hospital stay, § 412.4(f) also includes a special payment methodology. For these MS-DRGs, hospitals receive 50 percent of the full MS-DRG payment, plus the single per diem payment, for the first day of the stay, as well as a per diem payment for subsequent days (up to the full MS-DRG payment (§ 412.4(f)(6)). For an MS-DRG to qualify for the special payment methodology, the geometric mean length of stay must be greater than 4 days, and the average charges of 1-day discharge cases in the MS-DRG must be at least 50 percent of the average charges for all cases within the MS-DRG. MS-DRGs that are part of an MS-DRG severity level group will qualify under the MS-DRG special payment methodology policy if any one of the MS-DRGs that share that same base MS-DRG qualifies (§ 412.4(f)(6)).
Prior to the enactment of the Bipartisan Budget Act of 2018 (Pub. L. 115-123), under section 1886(d)(5)(J) of the Act, a discharge was deemed a “qualified discharge” if the individual was discharged to one of the following postacute care settings:
- A hospital or hospital unit that is not a subsection (d) hospital.
- A skilled nursing facility.
- Related home health services provided by a home health agency provided within a timeframe established by the Secretary (beginning within 3 days after the date of discharge).
Section 53109 of the Bipartisan Budget Act of 2018 amended section 1886(d)(5)(J)(ii) of the Act to also include discharges to hospice care provided by a hospice program as a qualified discharge, effective for discharges occurring on or after October 1, 2018. Accordingly, effective for discharges occurring on or after October 1, 2018, if a discharge is assigned to one of the MS-DRGs subject to the postacute care transfer policy and the individual is transferred to hospice care by a hospice program, the discharge is subject to payment as a transfer case. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41394), we made conforming amendments to § 412.4(c) of the regulation to include discharges to hospice care occurring on or after October 1, 2018 as qualified discharges. We specified that hospital bills with a Patient Discharge Status code of 50 (Discharged/Transferred to Hospice—Routine or Continuous Home Care) or 51 (Discharged/Transferred to Hospice, General Inpatient Care or Inpatient Respite) are subject to the postacute care transfer policy in accordance with this statutory amendment. Consistent with our policy for other qualified discharges, CMS claims processing software has been revised to identify cases in which hospice benefits were billed on the date of hospital discharge without the appropriate discharge status code. Such claims will be returned as unpayable to the hospital and may be rebilled with a corrected discharge code.
2. Changes for FY 2020
As discussed in section II.F. of the preamble of the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19399 through 19401), based on our analysis of FY 2018 MedPAR claims data, we proposed to make changes to a number of MS-DRGs, effective for FY 2020. Specifically, we proposed to:
- Reassign procedure codes from MS-DRGs 216 through 218 (Cardiac Valve and Other Major Cardiothoracic Procedures with Cardiac Catheterization with MCC, CC and without CC/MCC, respectively), MS-DRGs 219 through 221 (Cardiac Valve and Other Major Cardiothoracic Procedures without Cardiac Catheterization with MCC, CC and without CC/MCC, respectively), and MS-DRGs 273 and 274 (Percutaneous Intracardiac Procedures with and without MCC, respectively) and create new MS-DRGs 319 and 320 (Other Endovascular Cardiac Valve Procedures with and without MCC, respectively); and
- Delete MS-DRGs 691 and 692 (Urinary Stones with ESW Lithotripsy with CC/MCC and without CC/MCC, respectively) and revise the titles for MS-DRGs 693 and 694 to “Urinary Stones with MCC” and “Urinary Stones without MCC”, respectively.
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19400), in light of the proposed changes to these MS-DRGs for FY 2020, according to the regulations under § 412.4(d), we evaluated these MS-DRGs using the general postacute care transfer policy criteria and data from the FY 2018 MedPAR file. If an MS-DRG qualified for the postacute care transfer policy, we also evaluated that MS-DRG under the special payment methodology criteria according to regulations at § 412.4(f)(6). We stated in the proposed rule that we continue to believe it is appropriate to reassess MS-DRGs when proposing reassignment of procedure codes or diagnosis codes that would result in material changes to an MS-DRG. We noted that MS-DRGs 216, 217, 218, 219, 220, and 221 are currently subject to the postacute care transfer policy. We stated that as a result of our review, these MS-DRGs, as proposed to be revised, would continue to qualify to be included on the list of MS-DRGs that are subject to the postacute care transfer policy. In addition, we noted that MS-DRGs 273 and 274 are also currently subject to the postacute care transfer policy and MS-DRGs 693 and 694 are currently not subject to the postacute care transfer policy. We stated that as a result of our review, these MS-DRGs, as proposed to be revised, would not qualify to be included on the list of MS-DRGs that are subject to the postacute care transfer policy. We noted that proposed new MS-DRGs 319 and 320 also would not qualify to be included on the list of MS-DRGs that are subject to the postacute care transfer policy. Therefore, we proposed to remove MS-DRGs 273 and 274 from the list of MS-DRGs that are subject to the postacute care transfer policy. We note that, as discussed in section II.F. of the preamble of this final rule, we are finalizing these proposed changes to the MS-DRGs.
We note that MS-DRGs that are subject to the postacute care transfer policy for FY 2019 and are not revised will continue to be subject to the policy in FY 2020. Using the December 2018 update of the FY 2018 MedPAR file, we developed a chart for the proposed rule (84 FR 19400) which set forth the analysis of the postacute care transfer policy criteria completed for the proposed rule with respect to each of these proposed new or revised MS-DRGs. We stated that, for the FY 2020 final rule, we intended to update this analysis using the most recent available data at that time. The following chart reflects our updated analysis for the finalized new and revised MS-DRGs using the postacute care transfer policy criteria and the March 2019 update of the FY 2018 MedPAR file.

During our annual review of proposed new or revised MS-DRGs and analysis of the December 2018 update of the FY 2018 MedPAR file, we reviewed the list of proposed revised or new MS-DRGs that qualify to be included on the list of MS-DRGs subject to the postacute care transfer policy for FY 2020 to determine if any of these MS-DRGs would also be subject to the special payment methodology policy for FY 2020. Based on our analysis of proposed changes to MS-DRGs included in the proposed rule, we determined that proposed revised MS-DRGs 216, 217, 218, 219, 220, and 221 would continue to meet the criteria for the MS-DRG special payment methodology. Because we proposed to remove MS-DRGs 273 and 274 from the list of MS-DRGs subject to the postacute care transfer policy, we also proposed to remove these MS-DRGs from the list of MS-DRGs subject to the MS-DRG special payment methodology, effective FY 2020 (84 FR 19400).
In the proposed rule, we indicated that, for the FY 2020 final rule, we intended to update this analysis using the most recent available data at that time. The following chart reflects our updated analysis for the finalized new and revised MS-DRGs using our criteria and the March 2019 update of the FY 2018 MedPAR file.

Comment: A commenter stated that CMS has applied the postacute care transfer policy criteria consistently with the regulation and agreeing with the assignment of post-acute care transfer policy and special payment policy status for the proposed new or revised MS-DRGs under the proposed rule.
Response: We appreciate the commenter's support.
After consideration of the public comments we received, and review of updated MedPAR data, we are finalizing the proposal to remove MS-DRGs 273 and 274 from the list of MS-DRGs that are subject to the postacute care transfer policy and the special payment policy.
The postacute care transfer and special payment policy status of these MS-DRGs is reflected in Table 5 associated with this final rule, which is listed in section VI. of the Addendum to this final rule and available via the internet on the CMS website.
B. Changes in the Inpatient Hospital Update for FY 2020 (§ 412.64(d))
1. FY 2020 Inpatient Hospital Update
In accordance with section 1886(b)(3)(B)(i) of the Act, each year we update the national standardized amount for inpatient hospital operating costs by a factor called the “applicable percentage increase.” For FY 2020, we are setting the applicable percentage increase by applying the adjustments listed in this section in the same sequence as we did for FY 2019. (We note that section 1886(b)(3)(B)(xii) of the Act required an additional reduction each year only for FYs 2010 through 2019.) Specifically, consistent with section 1886(b)(3)(B) of the Act, as amended by sections 3401(a) and 10319(a) of the Affordable Care Act, we are setting the applicable percentage increase by applying the following adjustments in the following sequence. The applicable percentage increase under the IPPS for FY 2020 is equal to the rate-of-increase in the hospital market basket for IPPS hospitals in all areas, subject to—
- A reduction of one-quarter of the applicable percentage increase (prior to the application of other statutory adjustments; also referred to as the market basket update or rate-of-increase (with no adjustments)) for hospitals that fail to submit quality information under rules established by the Secretary in accordance with section 1886(b)(3)(B)(viii) of the Act;
- A reduction of three-quarters of the applicable percentage increase (prior to the application of other statutory adjustments; also referred to as the market basket update or rate-of-increase (with no adjustments)) for hospitals not considered to be meaningful EHR users in accordance with section 1886(b)(3)(B)(ix) of the Act; and
- An adjustment based on changes in economy-wide productivity (the multifactor productivity (MFP) adjustment).
Section 1886(b)(3)(B)(xi) of the Act, as added by section 3401(a) of the Affordable Care Act, states that application of the MFP adjustment may result in the applicable percentage increase being less than zero.
In compliance with section 404 of the MMA, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38158 through 38175), we replaced the FY 2010-based IPPS operating market basket with the rebased and revised 2014-based IPPS operating market basket, effective with FY 2018.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19401), we proposed to base the proposed FY 2020 market basket update used to determine the applicable percentage increase for the IPPS on IHS Global Inc.'s (IGI's) fourth quarter 2018 forecast of the 2014-based IPPS market basket rate-of-increase with historical data through third quarter 2018, which was estimated to be 3.2 percent. We also proposed that if more recent data subsequently became available (for example, a more recent estimate of the market basket and the MFP adjustment), we would use such data, if appropriate, to determine the FY 2020 market basket update and the MFP adjustment in the final rule.
Based on the most recent data available for this FY 2020 IPPS/LTCH PPS final rule (that is, IGI's second quarter 2019 forecast of the 2014-based IPPS market basket rate-of-increase with historical data through the first quarter of 2019), we estimate that the FY 2020 market basket update used to determine the applicable percentage increase for the IPPS is 3.0 percent.
For FY 2020, depending on whether a hospital submits quality data under the rules established in accordance with section 1886(b)(3)(B)(viii) of the Act (hereafter referred to as a hospital that submits quality data) and is a meaningful EHR user under section 1886(b)(3)(B)(ix) of the Act (hereafter referred to as a hospital that is a meaningful EHR user), there are four possible applicable percentage increases that can be applied to the standardized amount.
Based on the most recent data available as previously described, we determined final applicable percentage increases to the standardized amount for FY 2020, as specified in the table that appears later in this section.
In the FY 2012 IPPS/LTCH PPS final rule (76 FR 51689 through 51692), we finalized our methodology for calculating and applying the MFP adjustment. As we explained in that rule, section 1886(b)(3)(B)(xi)(II) of the Act, as added by section 3401(a) of the Affordable Care Act, defines this productivity adjustment as equal to the 10-year moving average of changes in annual economy-wide, private nonfarm business MFP (as projected by the Secretary for the 10-year period ending with the applicable fiscal year, calendar year, cost reporting period, or other annual period). The Bureau of Labor Statistics (BLS) publishes the official measure of private nonfarm business MFP. We refer readers to the BLS website at http://www.bls.gov/mfp for the BLS historical published MFP data.
MFP is derived by subtracting the contribution of labor and capital input growth from output growth. The projections of the components of MFP are currently produced by IGI, a nationally recognized economic forecasting firm with which CMS contracts to forecast the components of the market baskets and MFP. As we discussed in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49509), beginning with the FY 2016 rulemaking cycle, the MFP adjustment is calculated using the revised series developed by IGI to proxy the aggregate capital inputs. Specifically, in order to generate a forecast of MFP, IGI forecasts BLS aggregate capital inputs using a regression model. A complete description of the MFP projection methodology is available on the CMS website at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareProgramRatesStats/MarketBasketResearch.html. As discussed in the FY 2016 IPPS/LTCH PPS final rule, if IGI makes changes to the MFP methodology, we will announce them on our website rather than in the annual rulemaking.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19402), for FY 2020, we proposed an MFP adjustment of 0.5 percentage point. Similar to the market basket update, for the proposed rule, we used IGI's fourth quarter 2018 forecast of the MFP adjustment to compute the proposed FY 2020 MFP adjustment. As noted previously, we proposed that if more recent data subsequently became available, we would use such data, if appropriate, to determine the FY 2020 market basket update and the MFP adjustment for the final rule.
Based on the most recent data available for this FY 2020 IPPS/LTCH PPS final rule (that is, IGI's second quarter 2019 forecast of the MFP adjustment), the current estimate of the MFP adjustment for FY 2020 is 0.4 percentage point.
We did not receive any public comments on our proposal to use the most recent available data to determine the final market basket update and the MFP adjustment. Therefore, for this final rule, we are finalizing a market basket update of 3.0 percent and an MFP adjustment of 0.4 percentage point for FY 2020 based on the most recent available data.
Based on these most recent data available, for this final rule, we have determined four applicable percentage increases to the standardized amount for FY 2020, as specified in the following table:

In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19402), we proposed to revise the existing regulations at 42 CFR 412.64(d) to reflect the current law for the update for FY 2020 and subsequent fiscal years. Specifically, in accordance with section 1886(b)(3)(B) of the Act, we proposed to add paragraph (viii) to § 412.64(d)(1) to set forth the applicable percentage increase to the operating standardized amount for FY 2020 and subsequent fiscal years as the percentage increase in the market basket index, subject to the reductions specified under § 412.64(d)(2) for a hospital that does not submit quality data and § 412.64(d)(3) for a hospital that is not a meaningful EHR user, less an MFP adjustment. (As previously noted, section 1886(b)(3)(B)(xii) of the Act required an additional reduction each year only for FYs 2010 through 2019.)
We did not receive any public comments on our proposal and therefore, we are finalizing our proposed changes to § 412.64(d) as proposed.
Section 1886(b)(3)(B)(iv) of the Act provides that the applicable percentage increase to the hospital-specific rates for SCHs and MDHs equals the applicable percentage increase set forth in section 1886(b)(3)(B)(i) of the Act (that is, the same update factor as for all other hospitals subject to the IPPS). Therefore, the update to the hospital-specific rates for SCHs and MDHs also is subject to section 1886(b)(3)(B)(i) of the Act, as amended by sections 3401(a) and 10319(a) of the Affordable Care Act. (Under current law, the MDH program is effective for discharges on or before September 30, 2022, as discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41429 through 41430).)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19402), for FY 2020, we proposed the following updates to the hospital-specific rates applicable to SCHs and MDHs: a proposed update of 2.7 percent for a hospital that submits quality data and is a meaningful EHR user; a proposed update of 1.9 percent for a hospital that fails to submit quality data and is a meaningful EHR user; a proposed update of 0.3 percent for a hospital that submits quality data and is not a meaningful EHR user; and a proposed update of -0.5 percent for a hospital that fails to submit quality data and is not a meaningful EHR user. As noted previously, for the FY 2020 IPPS/LTCH PPS proposed rule, we used IGI's fourth quarter 2018 forecast of the 2014-based IPPS market basket update with historical data through third quarter 2018. Similarly, we used IGI's fourth quarter 2018 forecast of the MFP adjustment. We proposed that if more recent data subsequently became available (for example, a more recent estimate of the market basket increase and the MFP adjustment), we would use such data, if appropriate, to determine the update in the final rule.
We did not receive any public comments on our proposal. Therefore are finalizing the proposal to determine the update to the hospital-specific rates for SCHs and MDHs in this final rule using the most recent available data.
For this final rule, based on the most recent available data, we are finalizing the following updates to the hospital specific rates applicable to SCHs and MDHs: An update of 2.6 percent for a hospital that submits quality data and is a meaningful EHR user; an update of 1.85 percent for a hospital that fails to submit quality data and is a meaningful EHR user; an update of 0.35 percent for a hospital that submits quality data and is not a meaningful EHR user; and an update of -0.4 percent for a hospital that fails to submit quality data and is not a meaningful EHR user.
2. FY 2020 Puerto Rico Hospital Update
As discussed in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56937 through 56938), prior to January 1, 2016, Puerto Rico hospitals were paid based on 75 percent of the national standardized amount and 25 percent of the Puerto Rico-specific standardized amount. Section 601 of Public Law 114-113 amended section 1886(d)(9)(E) of the Act to specify that the payment calculation with respect to operating costs of inpatient hospital services of a subsection (d) Puerto Rico hospital for inpatient hospital discharges on or after January 1, 2016, shall use 100 percent of the national standardized amount. Because Puerto Rico hospitals are no longer paid with a Puerto Rico-specific standardized amount under the amendments to section 1886(d)(9)(E) of the Act, there is no longer a need for us to determine an update to the Puerto Rico standardized amount. Hospitals in Puerto Rico are now paid 100 percent of the national standardized amount and, therefore, are subject to the same update to the national standardized amount discussed under section IV.B.1. of the preamble of this final rule. Accordingly, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19402 through 19403), for FY 2020, we proposed an applicable percentage increase of 2.7 percent to the standardized amount for hospitals located in Puerto Rico.
We did not receive any public comments on our proposal.
Based on the most recent data available for this final rule (as discussed previously in section IV.B.1. of the preamble of this final rule), we are finalizing an applicable percentage increase of 2.6 percent to the standardized amount for hospitals located in Puerto Rico.
We note that section 1886(b)(3)(B)(viii) of the Act, which specifies the adjustment to the applicable percentage increase for “subsection (d)” hospitals that do not submit quality data under the rules established by the Secretary, is not applicable to hospitals located in Puerto Rico.
In addition, section 602 of Public Law 114-113 amended section 1886(n)(6)(B) of the Act to specify that Puerto Rico hospitals are eligible for incentive payments for the meaningful use of certified EHR technology, effective beginning FY 2016, and also to apply the adjustments to the applicable percentage increase under section 1886(b)(3)(B)(ix) of the Act to Puerto Rico hospitals that are not meaningful EHR users, effective FY 2022. Accordingly, because the provisions of section 1886(b)(3)(B)(ix) of the Act are not applicable to hospitals located in Puerto Rico until FY 2022, the adjustments under this provision are not applicable for FY 2020.
C. Rural Referral Centers (RRCs) Annual Updates to Case-Mix Index and Discharge Criteria (§ 412.96)
Under the authority of section 1886(d)(5)(C)(i) of the Act, the regulations at § 412.96 set forth the criteria that a hospital must meet in order to qualify under the IPPS as a rural referral center (RRC). RRCs receive some special treatment under both the DSH payment adjustment and the criteria for geographic reclassification.
Section 402 of Public Law 108-173 raised the DSH payment adjustment for RRCs such that they are not subject to the 12-percent cap on DSH payments that is applicable to other rural hospitals. RRCs also are not subject to the proximity criteria when applying for geographic reclassification. In addition, they do not have to meet the requirement that a hospital's average hourly wage must exceed, by a certain percentage, the average hourly wage of the labor market area in which the hospital is located.
Section 4202(b) of Public Law 105-33 states, in part, that any hospital classified as an RRC by the Secretary for FY 1991 shall be classified as such an RRC for FY 1998 and each subsequent fiscal year. In the August 29, 1997 IPPS final rule with comment period (62 FR 45999), we reinstated RRC status for all hospitals that lost that status due to triennial review or MGCRB reclassification. However, we did not reinstate the status of hospitals that lost RRC status because they were now urban for all purposes because of the OMB designation of their geographic area as urban. Subsequently, in the August 1, 2000 IPPS final rule (65 FR 47089), we indicated that we were revisiting that decision. Specifically, we stated that we would permit hospitals that previously qualified as an RRC and lost their status due to OMB redesignation of the county in which they are located from rural to urban, to be reinstated as an RRC. Otherwise, a hospital seeking RRC status must satisfy all of the other applicable criteria. We use the definitions of “urban” and “rural” specified in Subpart D of 42 CFR part 412. One of the criteria under which a hospital may qualify as an RRC is to have 275 or more beds available for use (§ 412.96(b)(1)(ii)). A rural hospital that does not meet the bed size requirement can qualify as an RRC if the hospital meets two mandatory prerequisites (a minimum case-mix index (CMI) and a minimum number of discharges), and at least one of three optional criteria (relating to specialty composition of medical staff, source of inpatients, or referral volume). (We refer readers to § 412.96(c)(1) through (c)(5) and the September 30, 1988 Federal Register (53 FR 38513) for additional discussion.) With respect to the two mandatory prerequisites, a hospital may be classified as an RRC if—
- The hospital's CMI is at least equal to the lower of the median CMI for urban hospitals in its census region, excluding hospitals with approved teaching programs, or the median CMI for all urban hospitals nationally; and
- The hospital's number of discharges is at least 5,000 per year, or, if fewer, the median number of discharges for urban hospitals in the census region in which the hospital is located. The number of discharges criterion for an osteopathic hospital is at least 3,000 discharges per year, as specified in section 1886(d)(5)(C)(i) of the Act.
1. Case-Mix Index (CMI)
Section 412.96(c)(1) provides that CMS establish updated national and regional CMI values in each year's annual notice of prospective payment rates for purposes of determining RRC status. The methodology we used to determine the national and regional CMI values is set forth in the regulations at § 412.96(c)(1)(ii). The national median CMI value for FY 2020 is based on the CMI values of all urban hospitals nationwide, and the regional median CMI values for FY 2020 are based on the CMI values of all urban hospitals within each census region, excluding those hospitals with approved teaching programs (that is, those hospitals that train residents in an approved GME program as provided in § 413.75). These values are based on discharges occurring during FY 2018 (October 1, 2017 through September 30, 2018), and include bills posted to CMS' records through March 2019.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19403), we proposed that, in addition to meeting other criteria, if rural hospitals with fewer than 275 beds are to qualify for initial RRC status for cost reporting periods beginning on or after October 1, 2019, they must have a CMI value for FY 2018 that is at least—
- 1.68555 (national—all urban); or
- The median CMI value (not transfer-adjusted) for urban hospitals (excluding hospitals with approved teaching programs as identified in § 413.75) calculated by CMS for the census region in which the hospital is located.
The proposed median CMI values by region were set forth in a table in the proposed rule (84 FR 19403). We stated in the proposed rule that we intended to update the proposed CMI values in the FY 2020 final rule to reflect the updated FY 2018 MedPAR file, which will contain data from additional bills received through March 2019.
We did not receive any public comments on our proposals. Based on the latest available data (FY 2018 bills received through March 2019), in addition to meeting other criteria, if rural hospitals with fewer than 275 beds are to qualify for initial RRC status for cost reporting periods beginning on or after October 1, 2019, they must have a CMI value for FY 2018 that is at least:
- 1.68645 (national—all urban); or
- The median CMI value (not transfer-adjusted) for urban hospitals (excluding hospitals with approved teaching programs as identified in § 413.75) calculated by CMS for the census region in which the hospital is located.
The final CMI values by region are set forth in the following table.

A hospital seeking to qualify as an RRC should obtain its hospital-specific CMI value (not transfer-adjusted) from its MAC. Data are available on the Provider Statistical and Reimbursement (PS&R) System. In keeping with our policy on discharges, the CMI values are computed based on all Medicare patient discharges subject to the IPPS MS-DRG-based payment.
2. Discharges
Section 412.96(c)(2)(i) provides that CMS set forth the national and regional numbers of discharges criteria in each year's annual notice of prospective payment rates for purposes of determining RRC status. As specified in section 1886(d)(5)(C)(ii) of the Act, the national standard is set at 5,000 discharges. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19404), for FY 2020, we proposed to update the regional standards based on discharges for urban hospitals' cost reporting periods that began during FY 2017 (that is, October 1, 2016 through September 30, 2017), which were the latest cost report data available at the time the proposed rule was developed. Therefore, we proposed that, in addition to meeting other criteria, a hospital, if it is to qualify for initial RRC status for cost reporting periods beginning on or after October 1, 2019, must have, as the number of discharges for its cost reporting period that began during FY 2017, at least—
- 5,000 (3,000 for an osteopathic hospital); or
- If less, the median number of discharges for urban hospitals in the census region in which the hospital is located. (We refer readers to the table set forth in the FY 2020 IPPS/LTCH PPS proposed rule at 84 FR 19404.) In the proposed rule, we stated we intended to update these numbers in the FY 2020 final rule based on the latest available cost report data.
We did not receive any public comments on our proposals.
Based on the latest discharge data available at this time, that is, for cost reporting periods that began during FY 2017, the final median number of discharges for urban hospitals by census region are set forth in the following table.

We note that because the median number of discharges for hospitals in each census region is greater than the national standard of 5,000 discharges, under this final rule, 5,000 discharges is the minimum criterion for all hospitals, except for osteopathic hospitals for which the minimum criterion is 3,000 discharges.
D. Payment Adjustment for Low-Volume Hospitals (§ 412.101)
1. Background

We note that because the median number of discharges for hospitals in each census region is greater than the national standard of 5,000 discharges, under this final rule, 5,000 discharges is the minimum criterion for all hospitals, except for osteopathic hospitals for which the minimum criterion is 3,000 discharges.
D. Payment Adjustment for Low-Volume Hospitals (§ 412.101)
1. Background
Section 1886(d)(12) of the Act provides for an additional payment to each qualifying low-volume hospital under the IPPS beginning in FY 2005. The additional payment adjustment to a low-volume hospital provided for under section 1886(d)(12) of the Act is in addition to any payment calculated under section 1886 of the Act. Therefore, the additional payment adjustment is based on the per discharge amount paid to the qualifying hospital under section 1886 of the Act. In other words, the low-volume hospital payment adjustment is based on total per discharge payments made under section 1886 of the Act, including capital, DSH, IME, and outlier payments. For SCHs and MDHs, the low-volume hospital payment adjustment is based in part on either the Federal rate or the hospital-specific rate, whichever results in a greater operating IPPS payment.
As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41398 through 41399), section 50204 of the Bipartisan Budget Act of 2018 (Pub. L. 115-123) modified the definition of a low-volume hospital and the methodology for calculating the payment adjustment for low-volume hospitals for FYs 2019 through 2022. (Section 50204 also extended prior changes to the definition of a low-volume hospital and the methodology for calculating the payment adjustment for low-volume hospitals through FY 2018.) Beginning with FY 2023, the low-volume hospital qualifying criteria and payment adjustment will revert to the statutory requirements that were in effect prior to FY 2011. (For additional information on the low-volume hospital payment adjustment prior to FY 2018, we refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 56941 through 56943). For additional information on the low-volume hospital payment adjustment for FY 2018, we refer readers to the FY 2018 IPPS notice (CMS-1677-N) that appeared in the Federal Register on April 26, 2018 (83 FR 18301 through 18308).) In section IV.D.2. of the preamble of this final rule, we discuss the low-volume hospital payment adjustment policies for FY 2020.
2. Temporary Changes to the Low-Volume Hospital Definition and Payment Adjustment Methodology for FYs 2019 Through 2022
As discussed earlier, section 50204 of the Bipartisan Budget Act of 2018 further modified the definition of a low-volume hospital and the methodology for calculating the payment adjustment for low-volume hospitals for FYs 2019 through 2022. Specifically, the qualifying criteria for low-volume hospitals under section 1886(d)(12)(C)(i) of the Act were amended to specify that, for FYs 2019 through 2022, a subsection (d) hospital qualifies as a low-volume hospital if it is more than 15 road miles from another subsection (d) hospital and has less than 3,800 total discharges during the fiscal year. Section 1886(d)(12)(D) of the Act was also amended to provide that, for discharges occurring in FYs 2019 through 2022, the Secretary shall determine the applicable percentage increase using a continuous, linear sliding scale ranging from an additional 25 percent payment adjustment for low-volume hospitals with 500 or fewer discharges to a zero percent additional payment for low-volume hospitals with more than 3,800 discharges in the fiscal year. Consistent with the requirements of section 1886(d)(12)(C)(ii) of the Act, the term “discharge” for purposes of these provisions refers to total discharges, regardless of payer (that is, Medicare and non-Medicare discharges).
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41399), to implement this requirement, we specified a continuous, linear sliding scale formula to determine the low-volume hospital payment adjustment for FYs 2019 through 2022 that is similar to the continuous, linear sliding scale formula used to determine the low-volume hospital payment adjustment originally established by the Affordable Care Act and implemented in the regulations at § 412.101(c)(2)(ii) in the FY 2011 IPPS/LTCH PPS final rule (75 FR 50240 through 50241). Consistent with the statute, we provided that qualifying hospitals with 500 or fewer total discharges will receive a low-volume hospital payment adjustment of 25 percent. For qualifying hospitals with fewer than 3,800 discharges but more than 500 discharges, the low-volume payment adjustment is calculated by subtracting from 25 percent the proportion of payments associated with the discharges in excess of 500. As such, for qualifying hospitals with fewer than 3,800 total discharges but more than 500 total discharges, the low-volume hospital payment adjustment for FYs 2019 through 2022 is calculated using the following formula:
Low-Volume Hospital Payment Adjustment = 0.25−[0.25/3300] × (number of total discharges−500) = (95/330)−(number of total discharges/13,200).
For this purpose, we specified that the “number of total discharges” is determined as total discharges, which includes Medicare and non-Medicare discharges during the fiscal year, based on the hospital's most recently submitted cost report. The low-volume hospital payment adjustment for FYs 2019 through 2022 is set forth in the regulations at 42 CFR 412.101(c)(3).
Comment: Commenters expressed continued support of the low-volume hospital adjustment changes included in the Bipartisan Budget Act of 2018.
Response: While these changes are statutory, we appreciate commenters' support.
3. Process for Requesting and Obtaining the Low-Volume Hospital Payment Adjustment
In the FY 2011 IPPS/LTCH PPS final rule (75 FR 50238 through 50275 and 50414) and subsequent rulemaking (for example, the FY 2019 IPPS/LTCH PPS final rule (83 FR 41399 through 41401)), we discussed the process for requesting and obtaining the low-volume hospital payment adjustment. Under this previously established process, a hospital makes a written request for the low-volume payment adjustment under § 412.101 to its MAC. This request must contain sufficient documentation to establish that the hospital meets the applicable mileage and discharge criteria. The MAC will determine if the hospital qualifies as a low-volume hospital by reviewing the data the hospital submits with its request for low-volume hospital status in addition to other available data. Under this approach, a hospital will know in advance whether or not it will receive a payment adjustment under the low-volume hospital policy. The MAC and CMS may review available data such as the number of discharges, in addition to the data the hospital submits with its request for low-volume hospital status, in order to determine whether or not the hospital meets the qualifying criteria. (For additional information on our existing process for requesting the low-volume hospital payment adjustment, we refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41399 through 41401)).
As explained earlier, for FY 2019 and subsequent fiscal years, the discharge determination is made based on the hospital's number of total discharges, that is, Medicare and non-Medicare discharges, as was the case for FYs 2005 through 2010. Under § 412.101(b)(2)(i) and § 412.101(b)(2)(iii), a hospital's most recently submitted cost report is used to determine if the hospital meets the discharge criterion to receive the low-volume payment adjustment in the current year. As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41399 and 41400), we use cost report data to determine if a hospital meets the discharge criterion because this is the best available data source that includes information on both Medicare and non-Medicare discharges. (For FYs 2011 through 2018, the most recently available MedPAR data were used to determine the hospital's Medicare discharges because non-Medicare discharges were not used to determine if a hospital met the discharge criterion for those years.) Therefore, a hospital should refer to its most recently submitted cost report for total discharges (Medicare and non-Medicare) in order to decide whether or not to apply for low-volume hospital status for a particular fiscal year.
As also discussed in the FY 2019 IPPS/LTCH PPS final rule, in addition to the discharge criterion, for FY 2019 and for subsequent fiscal years, eligibility for the low-volume hospital payment adjustment is also dependent upon the hospital meeting the applicable mileage criterion specified in § 412.101(b)(2)(i) or § 412.101(b)(2)(iii) for the fiscal year. Specifically, to meet the mileage criterion to qualify for the low-volume hospital payment adjustment for FY 2020, as was the case for FY 2019, a hospital must be located more than 15 road miles from the nearest subsection (d) hospital. (We define in § 412.101(a) the term “road miles” to mean “miles” as defined in § 412.92(c)(1) (75 FR 50238 through 50275 and 50414).) For establishing that the hospital meets the mileage criterion, the use of a web-based mapping tool as part of the documentation is acceptable. The MAC will determine if the information submitted by the hospital, such as the name and street address of the nearest hospitals, location on a map, and distance from the hospital requesting low-volume hospital status, is sufficient to document that it meets the mileage criterion. If not, the MAC will follow up with the hospital to obtain additional necessary information to determine whether or not the hospital meets the applicable mileage criterion.
In accordance with our previously established process, a hospital must make a written request for low-volume hospital status that is received by its MAC by September 1 immediately preceding the start of the Federal fiscal year for which the hospital is applying for low-volume hospital status in order for the applicable low-volume hospital payment adjustment to be applied to payments for its discharges for the fiscal year beginning on or after October 1 immediately following the request (that is, the start of the Federal fiscal year). For a hospital whose request for low-volume hospital status is received after September 1, if the MAC determines the hospital meets the criteria to qualify as a low-volume hospital, the MAC will apply the applicable low-volume hospital payment adjustment to determine payment for the hospital's discharges for the fiscal year, effective prospectively within 30 days of the date of the MAC's low-volume status determination.
Consistent with this previously established process, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19405), for FY 2020, we proposed that a hospital must submit a written request for low-volume hospital status to its MAC that includes sufficient documentation to establish that the hospital meets the applicable mileage and discharge criteria (as described earlier). Consistent with historical practice, for FY 2020, we proposed that a hospital's written request must be received by its MAC no later than September 1, 2019 in order for the low-volume hospital payment adjustment to be applied to payments for its discharges beginning on or after October 1, 2019. If a hospital's written request for low-volume hospital status for FY 2020 is received after September 1, 2019, and if the MAC determines the hospital meets the criteria to qualify as a low-volume hospital, the MAC would apply the low-volume hospital payment adjustment to determine the payment for the hospital's FY 2020 discharges, effective prospectively within 30 days of the date of the MAC's low-volume hospital status determination. We noted in the proposed rule that this proposal was consistent with the process for requesting and obtaining the low-volume hospital payment adjustment for FY 2019 (83 FR 41399 through 41400).
Under this process, a hospital receiving the low-volume hospital payment adjustment for FY 2019 may continue to receive a low-volume hospital payment adjustment for FY 2020 without reapplying if it continues to meet the applicable mileage and discharge criteria (which, as discussed previously, are the same qualifying criteria that apply for FY 2019). In this case, a hospital's request can include a verification statement that it continues to meet the mileage criterion applicable for FY 2020. (Determination of meeting the discharge criterion is discussed earlier in this section.) We noted in the proposed rule that a hospital must continue to meet the applicable qualifying criteria as a low-volume hospital (that is, the hospital must meet the applicable discharge criterion and mileage criterion for the fiscal year) in order to receive the payment adjustment in that fiscal year; that is, low-volume hospital status is not based on a “one-time” qualification (75 FR 50238 through 50275). Consistent with historical policy, a hospital must submit its request, including this written verification, for each fiscal year for which it seeks to receive the low-volume hospital payment adjustment, and in accordance with the timeline described earlier.
Comment: A commenter suggested we alter our previously established process for requesting and obtaining the low-volume hospital payment adjustment for providers who have previously qualified for the low-volume hospital payment adjustment with the process used for sole community hospitals whereby hospitals would be required to notify the MAC within 30 days of any changes as opposed to a yearly verification statement.
Response: We appreciate the comment and will consider this suggestion for future rulemaking.
After consideration of the public comments we received, we are finalizing our proposals relating to the process for requesting and obtaining the low-volume hospital payment adjustment as previously described, without modification.
4. Conforming Changes To Codify Certain Changes to the Low-Volume Hospital Payment Adjustment for FYs 2011 Through 2017 Provided by Section 429 of the Consolidated Appropriations Act, 2018
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38188 through 38189), for the reasons discussed in that rule, we adopted a parallel adjustment in the regulations at § 412.101(e) which specifies that, for discharges occurring in FY 2018 and subsequent years, only the distance between Indian Health Service (IHS) and Tribal hospitals (collectively referred to here as “IHS hospitals”) will be considered when assessing whether an IHS hospital meets the mileage criterion under § 412.101(b)(2), and similarly, only the distance between non-IHS hospitals would be considered when assessing whether a non-IHS hospital meets the mileage criterion under § 412.101(b)(2). Section 429 of the Consolidated Appropriations Act, 2018, which was enacted on March 23, 2018, subsequently amended section 1886(d)(12)(C) of the Act by adding a new clause (iii) specifying that, for purposes of determining whether an IHS or a non-IHS hospital meets the mileage criterion under section 1886(d)(12)(C)(i) of the Act with respect to FY 2011 or a succeeding year, the Secretary shall apply the policy described in the regulations at § 412.101(e) (as in effect on the date of enactment). In other words, under this statutory change, the special treatment with respect to the proximities between IHS and non-IHS hospitals as set forth in § 412.101(e) for discharges occurring in FY 2018 and subsequent fiscal years is also applicable for purposes of applying the mileage criterion for the low-volume hospital payment adjustment for FYs 2011 through 2017. We refer readers to the notice that appeared in the Federal Register on August 23, 2018 (83 FR 42596 through 42600) for further detail on the process for requesting the low-volume hospital payment adjustment for any applicable fiscal years between FY 2011 and FY 2017 under the provisions of section 429 of the Consolidated Appropriations Act, 2018, including the details on the limitations under the reopening rules at 42 CFR 405.1885.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19406), we proposed to make conforming changes to the regulatory text at § 412.101(e) to reflect the changes to the low-volume hospital payment adjustment policy in accordance with the amendments made by section 429 of the Consolidated Appropriations Act, 2018. Specifically, we proposed to revise § 412.101(e) to specify that, subject to the reopening rules at 42 CFR 405.1885, a qualifying hospital may request the application of the policy set forth in proposed amended § 412.101(e)(1) for FYs 2011 through 2017. As noted previously, the process for requesting the low-volume hospital payment adjustment for any applicable fiscal years between FY 2011 and FY 2017 under the provisions of section 429 of the Consolidated Appropriations Act, 2018, as well as further discussion on the limitations under the reopening rules at 42 CFR 405.1885, are described in the August 23, 2018 Federal Register notice (83 FR 42596 through 42600). We noted that proposed amended § 412.101(e) would apply to discharges occurring in FY 2011 through FY 2017, consistent with the provisions of section 429 of the Consolidated Appropriations Act, 2018. We stated that to the extent that these proposed revisions could be viewed as retroactive rulemaking, they would be authorized under section 1871(e)(1)(A)(i) of the Act as the Secretary has determined that these changes are necessary to comply with the statute as amended by the Consolidated Appropriations Act, 2018.
We did not receive any public comments on our proposal. Therefore, we are finalizing, without modification, our proposed conforming changes to paragraph (e) of § 412.101 as previously discussed.
E. Indirect Medical Education (IME) Payment Adjustment Factor (§ 412.105)
Under the IPPS, an additional payment amount is made to hospitals with residents in an approved graduate medical education (GME) program in order to reflect the higher indirect patient care costs of teaching hospitals relative to nonteaching hospitals. The payment amount is determined by use of a statutorily specified adjustment factor. The regulations regarding the calculation of this additional payment, known as the IME adjustment, are located at § 412.105. We refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51680) for a full discussion of the IME adjustment and IME adjustment factor. Section 1886(d)(5)(B)(ii)(XII) of the Act provides that, for discharges occurring during FY 2008 and fiscal years thereafter, the IME formula multiplier is 1.35. Accordingly, for discharges occurring during FY 2020, the formula multiplier is 1.35. We estimate that application of this formula multiplier for the FY 2020 IME adjustment will result in an increase in IPPS payment of 5.5 percent for every approximately 10 percent increase in the hospital's resident-to-bed ratio.
Comment: A commenter stated they agreed with and supported the proposal regarding the IME adjustment factor.
Response: We appreciate the commenter's support. As previously noted, the IME adjustment factor is statutory. Accordingly, for discharges occurring during FY 2020, the IME formula multiplier is 1.35.
F. Payment Adjustment for Medicare Disproportionate Share Hospitals (DSHs) for FY 2020 (§ 412.106)
1. General Discussion
Section 1886(d)(5)(F) of the Act provides for additional Medicare payments to subsection (d) hospitals that serve a significantly disproportionate number of low-income patients. The Act specifies two methods by which a hospital may qualify for the Medicare disproportionate share hospital (DSH) adjustment. Under the first method, hospitals that are located in an urban area and have 100 or more beds may receive a Medicare DSH payment adjustment if the hospital can demonstrate that, during its cost reporting period, more than 30 percent of its net inpatient care revenues are derived from State and local government payments for care furnished to needy patients with low incomes. This method is commonly referred to as the “Pickle method.” The second method for qualifying for the DSH payment adjustment, which is the most common, is based on a complex statutory formula under which the DSH payment adjustment is based on the hospital's geographic designation, the number of beds in the hospital, and the level of the hospital's disproportionate patient percentage (DPP). A hospital's DPP is the sum of two fractions: The “Medicare fraction” and the “Medicaid fraction.” The Medicare fraction (also known as the “SSI fraction” or “SSI ratio”) is computed by dividing the number of the hospital's inpatient days that are furnished to patients who were entitled to both Medicare Part A and Supplemental Security Income (SSI) benefits by the hospital's total number of patient days furnished to patients entitled to benefits under Medicare Part A. The Medicaid fraction is computed by dividing the hospital's number of inpatient days furnished to patients who, for such days, were eligible for Medicaid, but were not entitled to benefits under Medicare Part A, by the hospital's total number of inpatient days in the same period.
Because the DSH payment adjustment is part of the IPPS, the statutory references to “days” in section 1886(d)(5)(F) of the Act have been interpreted to apply only to hospital acute care inpatient days. Regulations located at 42 CFR 412.106 govern the Medicare DSH payment adjustment and specify how the DPP is calculated as well as how beds and patient days are counted in determining the Medicare DSH payment adjustment. Under § 412.106(a)(1)(i), the number of beds for the Medicare DSH payment adjustment is determined in accordance with bed counting rules for the IME adjustment under § 412.105(b).
Section 3133 of the Patient Protection and Affordable Care Act, as amended by section 10316 of the same Act and section 1104 of the Health Care and Education Reconciliation Act (Pub. L. 111-152), added a section 1886(r) to the Act that modifies the methodology for computing the Medicare DSH payment adjustment. (For purposes of this final rule, we refer to these provisions collectively as section 3133 of the Affordable Care Act.) Beginning with discharges in FY 2014, hospitals that qualify for Medicare DSH payments under section 1886(d)(5)(F) of the Act receive 25 percent of the amount they previously would have received under the statutory formula for Medicare DSH payments. This provision applies equally to hospitals that qualify for DSH payments under section 1886(d)(5)(F)(i)(I) of the Act and those hospitals that qualify under the Pickle method under section 1886(d)(5)(F)(i)(II) of the Act.
The remaining amount, equal to an estimate of 75 percent of what otherwise would have been paid as Medicare DSH payments, reduced to reflect changes in the percentage of individuals who are uninsured, is available to make additional payments to each hospital that qualifies for Medicare DSH payments and that has uncompensated care. The payments to each hospital for a fiscal year are based on the hospital's amount of uncompensated care for a given time period relative to the total amount of uncompensated care for that same time period reported by all hospitals that receive Medicare DSH payments for that fiscal year.
As provided by section 3133 of the Affordable Care Act, section 1886(r) of the Act requires that, for FY 2014 and each subsequent fiscal year, a subsection (d) hospital that would otherwise receive DSH payments made under section 1886(d)(5)(F) of the Act receives two separately calculated payments. Specifically, section 1886(r)(1) of the Act provides that the Secretary shall pay to such subsection (d) hospital (including a Pickle hospital) 25 percent of the amount the hospital would have received under section 1886(d)(5)(F) of the Act for DSH payments, which represents the empirically justified amount for such payment, as determined by the MedPAC in its March 2007 Report to Congress. We refer to this payment as the “empirically justified Medicare DSH payment.”
In addition to this empirically justified Medicare DSH payment, section 1886(r)(2) of the Act provides that, for FY 2014 and each subsequent fiscal year, the Secretary shall pay to such subsection (d) hospital an additional amount equal to the product of three factors. The first factor is the difference between the aggregate amount of payments that would be made to subsection (d) hospitals under section 1886(d)(5)(F) of the Act if subsection (r) did not apply and the aggregate amount of payments that are made to subsection (d) hospitals under section 1886(r)(1) of the Act for such fiscal year. Therefore, this factor amounts to 75 percent of the payments that would otherwise be made under section 1886(d)(5)(F) of the Act.
The second factor is, for FY 2018 and subsequent fiscal years, 1 minus the percent change in the percent of individuals who are uninsured, as determined by comparing the percent of individuals who were uninsured in 2013 (as estimated by the Secretary, based on data from the Census Bureau or other sources the Secretary determines appropriate, and certified by the Chief Actuary of CMS), and the percent of individuals who were uninsured in the most recent period for which data are available (as so estimated and certified), minus 0.2 percentage point for FYs 2018 and 2019.
The third factor is a percent that, for each subsection (d) hospital, represents the quotient of the amount of uncompensated care for such hospital for a period selected by the Secretary (as estimated by the Secretary, based on appropriate data), including the use of alternative data where the Secretary determines that alternative data are available which are a better proxy for the costs of subsection (d) hospitals for treating the uninsured, and the aggregate amount of uncompensated care for all subsection (d) hospitals that receive a payment under section 1886(r) of the Act. Therefore, this third factor represents a hospital's uncompensated care amount for a given time period relative to the uncompensated care amount for that same time period for all hospitals that receive Medicare DSH payments in the applicable fiscal year, expressed as a percent.
For each hospital, the product of these three factors represents its additional payment for uncompensated care for the applicable fiscal year. We refer to the additional payment determined by these factors as the “uncompensated care payment.”
Section 1886(r) of the Act applies to FY 2014 and each subsequent fiscal year. In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50620 through 50647) and the FY 2014 IPPS interim final rule with comment period (78 FR 61191 through 61197), we set forth our policies for implementing the required changes to the Medicare DSH payment methodology made by section 3133 of the Affordable Care Act for FY 2014. In those rules, we noted that, because section 1886(r) of the Act modifies the payment required under section 1886(d)(5)(F) of the Act, it affects only the DSH payment under the operating IPPS. It does not revise or replace the capital IPPS DSH payment provided under the regulations at 42 CFR part 412, subpart M, which were established through the exercise of the Secretary's discretion in implementing the capital IPPS under section 1886(g)(1)(A) of the Act.
Finally, section 1886(r)(3) of the Act provides that there shall be no administrative or judicial review under section 1869, section 1878, or otherwise of any estimate of the Secretary for purposes of determining the factors described in section 1886(r)(2) of the Act or of any period selected by the Secretary for the purpose of determining those factors. Therefore, there is no administrative or judicial review of the estimates developed for purposes of applying the three factors used to determine uncompensated care payments, or the periods selected in order to develop such estimates.
2. Eligibility for Empirically Justified Medicare DSH Payments and Uncompensated Care Payments
As explained earlier, the payment methodology under section 3133 of the Affordable Care Act applies to “subsection (d) hospitals” that would otherwise receive a DSH payment made under section 1886(d)(5)(F) of the Act. Therefore, hospitals must receive empirically justified Medicare DSH payments in a fiscal year in order to receive an additional Medicare uncompensated care payment for that year. Specifically, section 1886(r)(2) of the Act states that, in addition to the payment made to a subsection (d) hospital under section 1886(r)(1) of the Act, the Secretary shall pay to such subsection (d) hospitals an additional amount. Because section 1886(r)(1) of the Act refers to empirically justified Medicare DSH payments, the additional payment under section 1886(r)(2) of the Act is limited to hospitals that receive empirically justified Medicare DSH payments in accordance with section 1886(r)(1) of the Act for the applicable fiscal year.
In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50622) and the FY 2014 IPPS interim final rule with comment period (78 FR 61193), we provided that hospitals that are not eligible to receive empirically justified Medicare DSH payments in a fiscal year will not receive uncompensated care payments for that year. We also specified that we would make a determination concerning eligibility for interim uncompensated care payments based on each hospital's estimated DSH status for the applicable fiscal year (using the most recent data that are available). We indicated that our final determination on the hospital's eligibility for uncompensated care payments will be based on the hospital's actual DSH status at cost report settlement for that payment year.
In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50622) and in the rulemaking for subsequent fiscal years, we have specified our policies for several specific classes of hospitals within the scope of section 1886(r) of the Act. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19408), we discussed our specific policies for FY 2020 with respect to the following hospitals:
- Subsection (d) Puerto Rico hospitals that are eligible for DSH payments also are eligible to receive empirically justified Medicare DSH payments and uncompensated care payments under the new payment methodology (78 FR 50623 and 79 FR 50006).
- Maryland hospitals are not eligible to receive empirically justified Medicare DSH payments and uncompensated care payments under the payment methodology of section 1886(r) of the Act because they are not paid under the IPPS. As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41402 through 41403), CMS and the State have entered into an agreement to govern payments to Maryland hospitals under a new payment model, the Maryland Total Cost of Care (TCOC) Model, which began on January 1, 2019. Under the Maryland TCOC Model, Maryland hospitals will not be paid under the IPPS in FY 2020, and will be ineligible to receive empirically justified Medicare DSH payments and uncompensated care payments under section 1886(r) of the Act.
- Sole community hospitals (SCHs) that are paid under their hospital-specific rate are not eligible for Medicare DSH payments. SCHs that are paid under the IPPS Federal rate receive interim payments based on what we estimate and project their DSH status to be prior to the beginning of the Federal fiscal year (based on the best available data at that time) subject to settlement through the cost report, and if they receive interim empirically justified Medicare DSH payments in a fiscal year, they also will receive interim uncompensated care payments for that fiscal year on a per discharge basis, subject as well to settlement through the cost report. Final eligibility determinations will be made at the end of the cost reporting period at settlement, and both interim empirically justified Medicare DSH payments and uncompensated care payments will be adjusted accordingly (78 FR 50624 and 79 FR 50007).
- Medicare-dependent, small rural hospitals (MDHs) are paid based on the IPPS Federal rate or, if higher, the IPPS Federal rate plus 75 percent of the amount by which the Federal rate is exceeded by the updated hospital-specific rate from certain specified base years (76 FR 51684). The IPPS Federal rate that is used in the MDH payment methodology is the same IPPS Federal rate that is used in the SCH payment methodology. Section 50205 of the Bipartisan Budget Act of 2018 (Pub. L. 115-123), enacted on February 9, 2018, extended the MDH program for discharges on or after October 1, 2017, through September 30, 2022. Because MDHs are paid based on the IPPS Federal rate, they continue to be eligible to receive empirically justified Medicare DSH payments and uncompensated care payments if their DPP is at least 15 percent, and we apply the same process to determine MDHs' eligibility for empirically justified Medicare DSH and uncompensated care payments as we do for all other IPPS hospitals. Due to the extension of the MDH program, MDHs will continue to be paid based on the IPPS Federal rate or, if higher, the IPPS Federal rate plus 75 percent of the amount by which the Federal rate is exceeded by the updated hospital-specific rate from certain specified base years. Accordingly, we will continue to make a determination concerning eligibility for interim uncompensated care payments based on each hospital's estimated DSH status for the applicable fiscal year (using the most recent data that are available). Our final determination on the hospital's eligibility for uncompensated care payments will be based on the hospital's actual DSH status at cost report settlement for that payment year. In addition, as we do for all IPPS hospitals, we will calculate a numerator for Factor 3 for all MDHs, regardless of whether they are projected to be eligible for Medicare DSH payments during the fiscal year, but the denominator for Factor 3 will be based on the uncompensated care data from the hospitals that we have projected to be eligible for Medicare DSH payments during the fiscal year.
- IPPS hospitals that elect to participate in the Bundled Payments for Care Improvement Advanced Initiative (BPCI Advanced) model starting October 1, 2018, will continue to be paid under the IPPS and, therefore, are eligible to receive empirically justified Medicare DSH payments and uncompensated care payments. For further information regarding the BPCI Advanced model, we refer readers to the CMS website at: https://innovation.cms.gov/initiatives/bpci-advanced/.
- IPPS hospitals that are participating in the Comprehensive Care for Joint Replacement Model (80 FR 73300) continue to be paid under the IPPS and, therefore, are eligible to receive empirically justified Medicare DSH payments and uncompensated care payments.
- Hospitals participating in the Rural Community Hospital Demonstration Program are not eligible to receive empirically justified Medicare DSH payments and uncompensated care payments under section 1886(r) of the Act because they are not paid under the IPPS (78 FR 50625 and 79 FR 50008). The Rural Community Hospital Demonstration Program was originally authorized for a 5-year period by section 410A of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) (Pub. L. 108-173), and extended for another 5-year period by sections 3123 and 10313 of the Affordable Care Act (Pub. L. 114-255). The period of performance for this 5-year extension period ended December 31, 2016. Section 15003 of the 21st Century Cures Act (Pub. L. 114-255), enacted December 13, 2016, again amended section 410A of Public Law 108-173 to require a 10-year extension period (in place of the 5-year extension required by the Affordable Care Act), therefore requiring an additional 5-year participation period for the demonstration program. Section 15003 of Public Law 114-255 also required a solicitation for applications for additional hospitals to participate in the demonstration program. At the time of issuance of the proposed rule, there were 29 hospitals participating in the demonstration program. At the time of development of this final rule, there are 28 hospitals participating in the demonstration program. Under the payment methodology that applies during the second 5 years of the extension period under the demonstration program, participating hospitals do not receive empirically justified Medicare DSH payments, and they are also excluded from receiving interim and final uncompensated care payments.
We received a comment in response to the discussion in the proposed rule concerning eligibility for interim uncompensated care payments based on each hospital's estimated DSH status for the applicable fiscal year (using the most recent data that are available).
Comment: A commenter stated that CMS had wrongly calculated its disproportionate patient percentage due to a “slight shift in the SSI percent and a delay in the pending Medicaid approvals,” which contributed to the determination of DSH eligible “NO” in Table 18 from the FY 2020 IPPS/LTCH proposed rule. The commenter urged CMS to consider its history of meeting the DSH threshold and reverse the “NO” to a “YES” for FY 2020 DSH payments, further noting that the DSH payment calculation for FY 2020 combines Medicaid utilization and an SSI percent from 2 years prior. The commenter noted that its amended Medicare cost report shows an increased disproportionate patient percentage ratio.
Response: In response to the comment concerning the hospital's projection of DSH eligibility, we note that regulations located at 42 CFR 412.106 govern the Medicare DSH payment adjustment and specify how the disproportionate patient percentage is calculated. Further, a hospital's eligibility to receive empirically justified DSH payments, can change throughout the year as the MACs receive and review updated data. Consistent with historical policy, an estimate of DSH eligibility is used to determine eligibility to receive interim uncompensated care payments prior to the start of the fiscal year based on each hospital's estimated DSH status for the applicable fiscal year (using the most recent data that are available at the time of the development of the proposed and final rules). The final determination on the hospital's eligibility for uncompensated care payments will be based on the hospital's actual DSH status at cost report settlement for that payment year.
3. Empirically Justified Medicare DSH Payments
As we have discussed earlier, section 1886(r)(1) of the Act requires the Secretary to pay 25 percent of the amount of the Medicare DSH payment that would otherwise be made under section 1886(d)(5)(F) of the Act to a subsection (d) hospital. Because section 1886(r)(1) of the Act merely requires the program to pay a designated percentage of these payments, without revising the criteria governing eligibility for DSH payments or the underlying payment methodology, we stated in the FY 2014 IPPS/LTCH PPS final rule that we did not believe that it was necessary to develop any new operational mechanisms for making such payments. Therefore, in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50626), we implemented this provision by advising MACs to simply adjust the interim claim payments to the requisite 25 percent of what would have otherwise been paid. We also made corresponding changes to the hospital cost report so that these empirically justified Medicare DSH payments can be settled at the appropriate level at the time of cost report settlement. We provided more detailed operational instructions and cost report instructions following issuance of the FY 2014 IPPS/LTCH PPS final rule that are available on the CMS website at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2014-Transmittals-Items/R5P240.html.
4. Uncompensated Care Payments
a. Calculation of Factor 1 for FY 2020
Section 1886(r)(2)(A) of the Act establishes Factor 1 in the calculation of the uncompensated care payment. Section 1886(r)(2)(A) of the Act states that this factor is equal to the difference between: (1) The aggregate amount of payments that would be made to subsection (d) hospitals under section 1886(d)(5)(F) of the Act if section 1886(r) of the Act did not apply for such fiscal year (as estimated by the Secretary); and (2) the aggregate amount of payments that are made to subsection (d) hospitals under section 1886(r)(1) of the Act for such fiscal year (as so estimated). Therefore, section 1886(r)(2)(A)(i) of the Act represents the estimated Medicare DSH payments that would have been made under section 1886(d)(5)(F) of the Act if section 1886(r) of the Act did not apply for such fiscal year. Under a prospective payment system, we would not know the precise aggregate Medicare DSH payment amount that would be paid for a Federal fiscal year until cost report settlement for all IPPS hospitals is completed, which occurs several years after the end of the Federal fiscal year. Therefore, section 1886(r)(2)(A)(i) of the Act provides authority to estimate this amount, by specifying that, for each fiscal year to which the provision applies, such amount is to be estimated by the Secretary. Similarly, section 1886(r)(2)(A)(ii) of the Act represents the estimated empirically justified Medicare DSH payments to be made in a fiscal year, as prescribed under section 1886(r)(1) of the Act. Again, section 1886(r)(2)(A)(ii) of the Act provides authority to estimate this amount.
Therefore, Factor 1 is the difference between our estimates of: (1) The amount that would have been paid in Medicare DSH payments for the fiscal year, in the absence of the new payment provision; and (2) the amount of empirically justified Medicare DSH payments that are made for the fiscal year, which takes into account the requirement to pay 25 percent of what would have otherwise been paid under section 1886(d)(5)(F) of the Act. In other words, this factor represents our estimate of 75 percent (100 percent minus 25 percent) of our estimate of Medicare DSH payments that would otherwise be made, in the absence of section 1886(r) of the Act, for the fiscal year.
As we did for FY 2019, in the FY 2020 IPPS/LTCH PPS proposed rule, in order to determine Factor 1 in the uncompensated care payment formula for FY 2020, we proposed to continue the policy established in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50628 through 50630) and in the FY 2014 IPPS interim final rule with comment period (78 FR 61194) of determining Factor 1 by developing estimates of both the aggregate amount of Medicare DSH payments that would be made in the absence of section 1886(r)(1) of the Act and the aggregate amount of empirically justified Medicare DSH payments to hospitals under 1886(r)(1) of the Act. These estimates will not be revised or updated after we know the final Medicare DSH payments for FY 2020.
Therefore, in order to determine the two elements of proposed Factor 1 for FY 2020 (Medicare DSH payments prior to the application of section 1886(r)(1) of the Act, and empirically justified Medicare DSH payments after application of section 1886(r)(1) of the Act), for the proposed rule, we used the most recently available projections of Medicare DSH payments for the fiscal year, as calculated by CMS' Office of the Actuary using the most recently filed Medicare hospital cost reports with Medicare DSH payment information and the most recent Medicare DSH patient percentages and Medicare DSH payment adjustments provided in the IPPS Impact File. The determination of the amount of DSH payments is partially based on the Office of the Actuary's Part A benefits projection model. One of the results of this model is inpatient hospital spending. Projections of DSH payments require projections for expected increases in utilization and case-mix. The assumptions that were used in making these projections and the resulting estimates of DSH payments for FY 2017 through FY 2020 are discussed in the table titled “Factors Applied for FY 2017 through FY 2020 to Estimate Medicare DSH Expenditures Using FY 2016 Baseline.”
For purposes of calculating our proposal for Factor 1 and modeling the impact of the FY 2020 IPPS/LTCH PPS proposed rule, we used the Office of the Actuary's December 2018 Medicare DSH estimates, which were based on data from the September 2018 update of the Medicare Hospital Cost Report Information System (HCRIS) and the FY 2019 IPPS/LTCH PPS final rule IPPS Impact File, published in conjunction with the publication of the FY 2019 IPPS/LTCH PPS final rule. Because SCHs that are projected to be paid under their hospital-specific rate are excluded from the application of section 1886(r) of the Act, these hospitals also were excluded from the December 2018 Medicare DSH estimates. Furthermore, because section 1886(r) of the Act specifies that the uncompensated care payment is in addition to the empirically justified Medicare DSH payment (25 percent of DSH payments that would be made without regard to section 1886(r) of the Act), Maryland hospitals, which are not eligible to receive DSH payments, were also excluded from the Office of the Actuary's December 2018 Medicare DSH estimates. The 29 hospitals that are participating in the Rural Community Hospital Demonstration Program were also excluded from these estimates because, under the payment methodology that applies during the second 5 years of the extension period, these hospitals are not eligible to receive empirically justified Medicare DSH payments or interim and final uncompensated care payments.
For the proposed rule, using the data sources that were previously discussed, the Office of the Actuary's December 2018 estimate for Medicare DSH payments for FY 2020, without regard to the application of section 1886(r)(1) of the Act, was approximately $16.857 billion. Therefore, also based on the December 2018 estimate, the estimate of empirically justified Medicare DSH payments for FY 2020, with the application of section 1886(r)(1) of the Act, was approximately $4.214 billion (or 25 percent of the total amount of estimated Medicare DSH payments for FY 2020). Under § 412.l06(g)(1)(i) of the regulations, Factor 1 is the difference between these two estimates of the Office of the Actuary. Therefore, in the proposed rule, we proposed that Factor 1 for FY 2020 would be $12,643,011,209.74, which is equal to 75 percent of the total amount of estimated Medicare DSH payments for FY 2020 ($16,857,348,279.65 minus $4,214,337,069.91).
Comment: A few commenters discussed our proposals regarding Factor 1 in their FY 2020 IPPS/LTCH PPS public comment submissions. A common theme, carrying over from comments in previous years, was the request for greater transparency in the methodology used by CMS and the OACT. This request was made with respect to the calculation of estimated Medicare DSH payments for purposes of determining Factor 1, and in particular the “Other” factor that is used to estimate Medicare DSH expenditures. Some commenters believed that the lack of opportunity afforded to hospitals to review the data used to develop our estimate is in violation of the Administrative Procedure Act.
Some commenters requested that CMS use the traditional payment reconciliation process to calculate final Medicare uncompensated care payments. A commenter asserted that reconciliation of Factor 1 and Factor 3 was necessary as a result of underestimates of Factor 1 in FY 2017 and FY 2018, resulting in underpayment of uncompensated care payments for those years. The commenter asserted that the section 1886(r)(2) of the Act allows for the Factors 1, 2, and 3 to be based on actual data for the specific fiscal year. The commenter stated using actual data from the specific fiscal year in which those costs are incurred, would result in more accurate estimates of these factors, instead of projections from prior-period figures.
Some commenters expressed concern about whether underreporting of Medicaid coverage was factored into the calculation of Factor 1, as it was for Factor 2. However, others noted that, from the FY 2020 proposed rule, it can be presumed that the Medicaid population decreased because the “Other” adjustment is less than 1.0. However, these commenters urged CMS to provide a detailed explanation, including calculations, of the assumptions used to make these projections.
A commenter noted that the adjustments made by CMS include an adjustment to account for the estimated effects of Medicaid expansion, but do not include the impact of including days for individuals who are entitled to benefits under Part A but received Medicare benefits through enrollment in a Medicare Advantage plan under Part C (Part C days) in the Part A/SSI fraction, thus leaving Factor 1 substantially understated. This commenter referenced the recent Supreme Court decision in which the Court held that the question of how to count Part C enrollees had to be addressed through notice and comment rulemaking. The commenter asserted that the inclusion of these Part C days in the Part A/SSI fraction could materially impact the DSH reimbursement used for Factor 1 by nearly 10 percent. The commenter suggested that CMS should estimate and adjust for the impact of removing Part C days from the Part A/SSI fraction. Similarly, another commenter asserted that, since FY 2014, hospitals have been deprived of DSH funding because of what the commenter perceives to be underestimates of Factor 1.
Response: We thank the commenters for their input. Regarding the comments referencing the Administrative Procedure Act, we note that under the Administrative Procedure Act, a proposed rule is required to include either the terms or substance of the proposed rule or a description of the subjects and issues involved. In this case, the FY 2020 IPPS/LTCH PPS proposed rule did include a detailed discussion of our proposed Factor 1 methodology and the data sources that would be used in making our estimate. Furthermore, we have been, and continue to be, transparent with respect to the methodology and data used to estimate Factor 1 and we disagree with commenters who assert otherwise. To provide context, we first note that Factor 1 is not estimated in isolation from other OACT projections. The Factor 1 estimates for proposed rules are generally consistent with the economic assumptions and actuarial analysis used to develop the President's Budget estimates under current law, and the Factor 1 estimates for the final rule are generally consistent with those used for the Midsession Review of the President's Budget. As we have in the past, for additional information on the development of the President's Budget, we refer readers to the Office of Management and Budget website at: https://www.whitehouse.gov/omb/budget. For additional information on the specific economic assumptions used in the Midsession Review of the President's FY 2020 Budget, we refer readers to the “Midsession Review of the President's FY 2020 Budget” available on the Office of Management and Budget website at: https://www.whitehouse.gov/omb/budget. We recognize that our reliance on the economic assumptions and actuarial analysis used to develop the President's Budget and the Midsession Review of the President's Budget in estimating Factor 1 has an impact on stakeholders who wish to replicate the Factor 1 calculation, such as modelling the relevant Medicare Part A portion of the budget, but we believe commenters are able to meaningfully comment on our proposed estimate of Factor 1 without replicating the budget.
For a general overview of the principal steps involved in projecting future inpatient costs and utilization, we refer readers to the “2019 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds” available on the CMS website at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/index.html under “Downloads.” We note that the annual reports of the Medicare Boards of Trustees to Congress represent the Federal Government's official evaluation of the financial status of the Medicare Program. The actuarial projections contained in these reports are based on numerous assumptions regarding future trends in program enrollment, utilization and costs of health care services covered by Medicare, as well as other factors affecting program expenditures. In addition, although the methods used to estimate future costs based on these assumptions are complex, they are subject to periodic review by independent experts to ensure their validity and reasonableness.
We also refer the public to the Actuarial Report on the Financial Outlook for Medicaid for a discussion of general issues regarding Medicaid projections.
Second, as described in more detail later in this section, in the FY 2020 IPPS/LTCH PPS proposed rule, we included information regarding the data sources, methods, and assumptions employed by the actuaries in determining the OACT's estimate of Factor 1. In summary, we indicated the historical HCRIS data update OACT used to identify Medicare DSH payments, explained that the most recent Medicare DSH payment adjustments provided in the IPPS Impact File were used, and provided the components of all the update factors that were applied to the historical data to estimate the Medicare DSH payments for the upcoming fiscal year, along with the associated rationale and assumptions. This discussion also included a description of the “Other” and “Discharges” assumptions, and also provided additional information regarding how we address the Medicaid and CHIP expansion.
In response to the commenters' assertion that Medicaid expansion is not adequately accounted for in the “Other” column, we note that the discussion in the proposed rule made clear that, based on data from the Midsession Review of the President's Budget, the OACT assumed per capita spending for Medicaid beneficiaries who enrolled due to the expansion to be 50 percent of the average per capita expenditures for a pre-expansion Medicaid beneficiary due to the better health of these beneficiaries. Taken as a whole, this description of our proposed methodology for estimating Factor 1 and the data sources used in making this estimate was entirely consistent with the requirements of the Administrative Procedure Act, and gave stakeholders adequate notice of, and a meaningful opportunity to comment on, the proposed estimate of Factor 1.
Regarding the commenters' assertion that, similar to the adjustment for Medicaid underreporting on survey data in the estimation of Factor 2, we should also account for this underreporting in our estimate of Factor 1, we note that the Factor 1 calculation uses Medicaid enrollment data and estimates and does not require the adjustment because it does not use survey data.
Regarding commenters' assertion that Factor 1 would be higher if Part C days were treated different, and their suggestion that CMS should estimate and adjust for the impact of removing Part C days from the Medicare/SSI fraction, we note that in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50614 through 50620), we readopted the policy of counting Medicare Advantage days in the SSI ratio for FY 2014 and all subsequent fiscal years (79 FR 50012). Accordingly, the rulemaking required by Azar v. Allina Health Services was completed for FY 2014 and all subsequent fiscal years in the FY 2014 IPPS/LTCH final rule. Thus, consistent with the policy adopted in that final rule, our estimate of Factor 1 for FY 2020 appropriately accounts for Medicare Advantage days by including them in the SSI ratio.
Lastly, regarding the commenters' perception that Factor 1 has been underestimated and their suggestion that CMS consider reconciling the estimates of Factors 1, 2, and 3, we continue to believe that applying our best estimates prospectively is most conducive to administrative efficiency, finality, and predictability in payments (78 FR 50628; 79 FR 50010; 80 FR 49518; 81 FR 56949; and 82 FR 38195). We believe that, in affording the Secretary the discretion to estimate the three factors used to determine uncompensated care payments and by including a prohibition against administrative and judicial review of those estimates in section 1886(r)(3) of the Act, Congress recognized the importance of finality and predictability under a prospective payment system. As a result, we do not agree with the commenters' suggestion that we should establish a process for reconciling our estimates of the three factors, which would be contrary to the notion of prospectivity. We also address comments specifically requesting that we establish procedures for reconciling Factor 3 later in this section, as part of the discussion of the comments received on the proposed methodology for Factor 3.
After consideration of the public comments we received, we are finalizing, as proposed, the methodology for calculating Factor 1 for FY 2020. We discuss the resulting Factor 1 amount for FY 2020 in this final rule. For this final rule, the OACT used the most recently submitted Medicare cost report data from the March 2019 update of HCRIS to identify Medicare DSH payments and the most recent Medicare DSH payment adjustments provided in the Impact File published in conjunction with the publication of the FY 2019 IPPS/LTCH PPS final rule and applied update factors and assumptions for future changes in utilization and case-mix to estimate Medicare DSH payments for the upcoming fiscal year. The June 2019 OACT estimate for Medicare DSH payments for FY 2020, without regard to the application of section 1886(r)(1) of the Act, was approximately $16.583 billion. This estimate excluded Maryland hospitals participating in the Maryland All-Payer Model, hospitals participating in the Rural Community Hospital Demonstration, and SCHs paid under their hospital-specific payment rate. Therefore, based on the June 2019 estimate, the estimate of empirically justified Medicare DSH payments for FY 2020, with the application of section 1886(r)(1) of the Act, was approximately $4.146 billion (or 25 percent of the total amount of estimated Medicare DSH payments for FY 2020). Under § 412.106(g)(1)(i) of the regulations, Factor 1 is the difference between these two estimates of the OACT. Therefore, in this final rule, Factor 1 for FY 2020 is $12,437,591,742.69, which is equal to 75 percent of the total amount of estimated Medicare DSH payments for FY 2020 ($16,583,455,656.92 minus $4,145,863,914.23).
The Office of the Actuary's final estimates for FY 2020 began with a baseline of $13.981 billion in Medicare DSH expenditures for FY 2016. The following table shows the factors applied to update this baseline through the current estimate for FY 2020:

In this table, the discharges column shows the increase in the number of Medicare fee-for-service (FFS) inpatient hospital discharges. The figures for FY 2017 and FY 2018 are based on Medicare claims data that have been adjusted by a completion factor. The discharge figure for FY 2019 is based on preliminary data for 2019. The discharge figure for FY 2020 is an assumption based on recent trends recovering back to the long-term trend and assumptions related to how many beneficiaries will be enrolled in Medicare Advantage (MA) plans. The case-mix column shows the increase in case-mix for IPPS hospitals. The case-mix figures for FY 2017 and FY 2018 are based on actual data adjusted by a completion factor. The FY 2019 increase is based on preliminary data. The FY 2020 increase is an estimate based on the recommendation of the 2010-2011 Medicare Technical Review Panel. The “Other” column shows the increase in other factors that contribute to the Medicare DSH estimates. These factors include the difference between the total inpatient hospital discharges and the IPPS discharges, and various adjustments to the payment rates that have been included over the years but are not reflected in the other columns (such as the change in rates for the 2-midnight stay policy). In addition, the “Other” column includes a factor for the Medicaid expansion due to the Affordable Care Act. The factor for Medicaid expansion was developed using public information and statements for each State regarding its intent to implement the expansion. Based on this information, it is assumed that 50 percent of all individuals who were potentially newly eligible Medicaid enrollees in 2016 resided in States that had elected to expand Medicaid eligibility and, for 2017 and thereafter, that 55 percent of such individuals would reside in expansion States. In the future, these assumptions may change based on actual participation by States. For a discussion of general issues regarding Medicaid projections, we refer readers to the 2017 Actuarial Report on the Financial Outlook for Medicaid, which is available on the CMS website at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2017.pdf. We note that, in developing their estimates of the effect of Medicaid expansion on Medicare DSH expenditures, our actuaries have assumed that the new Medicaid enrollees are healthier than the average Medicaid recipient and, therefore, use fewer hospital services. Specifically, based on data from the President's Budget, the OACT assumed per capita spending for Medicaid beneficiaries who enrolled due to the expansion to be 50 percent of the average per capita expenditures for a pre-expansion Medicaid beneficiary due to the better health of these beneficiaries. This assumption is consistent with recent internal estimates of Medicaid per capita spending pre-expansion and post-expansion.
This table shows the factors that are included in the “Update” column of the previous table:

b. Calculation of Factor 2 for FY 2020
(1) Background
Section 1886(r)(2)(B) of the Act establishes Factor 2 in the calculation of the uncompensated care payment. Section 1886(r)(2)(B)(ii) of the Act provides that, for FY 2018 and subsequent fiscal years, the second factor is 1 minus the percent change in the percent of individuals who are uninsured, as determined by comparing the percent of individuals who were uninsured in 2013 (as estimated by the Secretary, based on data from the Census Bureau or other sources the Secretary determines appropriate, and certified by the Chief Actuary of CMS) and the percent of individuals who were uninsured in the most recent period for which data are available (as so estimated and certified), minus 0.2 percentage point for FYs 2018 and 2019. In FY 2020 and subsequent fiscal years, there is no longer a reduction. We note that, unlike section 1886(r)(2)(B)(i) of the Act, which governed the calculation of Factor 2 for FYs 2014, 2015, 2016, and 2017, section 1886(r)(2)(B)(ii) of the Act permits the use of a data source other than the CBO estimates to determine the percent change in the rate of uninsurance beginning in FY 2018. In addition, for FY 2018 and subsequent years, the statute does not require that the estimate of the percent of individuals who are uninsured be limited to individuals who are under 65 years of age.
As we discussed in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38197), in our analysis of a potential data source for the rate of uninsurance for purposes of computing Factor 2 in FY 2018, we considered the following: (1) The extent to which the source accounted for the full U.S. population; (2) the extent to which the source comprehensively accounted for both public and private health insurance coverage in deriving its estimates of the number of uninsured; (3) the extent to which the source utilized data from the Census Bureau; (4) the timeliness of the estimates; (5) the continuity of the estimates over time; (6) the accuracy of the estimates; and (7) the availability of projections (including the availability of projections using an established estimation methodology that would allow for calculation of the rate of uninsurance for the applicable Federal fiscal year). As we explained in the FY 2018 IPPS/LTCH PPS final rule, these considerations are consistent with the statutory requirement that this estimate be based on data from the Census Bureau or other sources the Secretary determines appropriate and help to ensure the data source will provide reasonable estimates for the rate of uninsurance that are available in conjunction with the IPPS rulemaking cycle. In the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to use the same methodology as was used in FY 2018 and FY 2019 to determine Factor 2 for FY 2020.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38197 and 38198), we explained that we determined the source that, on balance, best meets all of these considerations is the uninsured estimates produced by CMS' Office of the Actuary (OACT) as part of the development of the National Health Expenditure Accounts (NHEA). The NHEA represents the government's official estimates of economic activity (spending) within the health sector. The information contained in the NHEA has been used to study numerous topics related to the health care sector, including, but not limited to, changes in the amount and cost of health services purchased and the payers or programs that provide or purchase these services; the economic causal factors at work in the health sector; the impact of policy changes, including major health reform; and comparisons to other countries' health spending. Of relevance to the determination of Factor 2 is that the comprehensive and integrated structure of the NHEA creates an ideal tool for evaluating changes to the health care system, such as the mix of the insured and uninsured because this mix is integral to the well-established NHEA methodology. In the FY 2020 IPPS/LTCH PPS proposed rule, we described some aspects of the methodology used to develop the NHEA that were particularly relevant in estimating the percent change in the rate of uninsurance for FY 2018 and FY 2019 that we believe continue to be relevant in developing the estimate for FY 2020. A full description of the methodology used to develop the NHEA is available on the CMS website at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/DSM-15.pdf.
The NHEA estimates of U.S. population reflect the Census Bureau's definition of the resident-based population, which includes all people who usually reside in the 50 States or the District of Columbia, but excludes residents living in Puerto Rico and areas under U.S. sovereignty, members of the U.S. Armed Forces overseas, and U.S. citizens whose usual place of residence is outside of the United States, plus a small (typically less than 0.2 percent of population) adjustment to reflect Census undercounts. In past years, the estimates for Factor 2 were made using the CBO's uninsured population estimates for the under 65 population. For FY 2018 and subsequent years, the statute does not restrict the estimate to the measurement of the percent of individuals under the age of 65 who are uninsured. Accordingly, as we explained in the FY 2018 IPPS/LTCH PPS proposed and final rules, we believe it is appropriate to use an estimate that reflects the rate of uninsurance in the United States across all age groups. In addition, we continue to believe that a resident-based population estimate more fully reflects the levels of uninsurance in the United States that influence uncompensated care for hospitals than an estimate that reflects only legal residents. The NHEA estimates of uninsurance are for the total U.S. population (all ages) and not by specific age cohort, such as the population under the age of 65.
The NHEA includes comprehensive enrollment estimates for total private health insurance (PHI) (including direct and employer-sponsored plans), Medicare, Medicaid, the Children's Health Insurance Program (CHIP), and other public programs, and estimates of the number of individuals who are uninsured. Estimates of total PHI enrollment are available for 1960 through 2017, estimates of Medicaid, Medicare, and CHIP enrollment are available for the length of the respective programs, and all other estimates (including the more detailed estimates of direct-purchased and employer-sponsored insurance) are available for 1987 through 2017. The NHEA data are publicly available on the CMS website at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/index.html.
In order to compute Factor 2, the first metric that is needed is the proportion of the total U.S. population that was uninsured in 2013. In developing the estimates for the NHEA, OACT's methodology included using the number of uninsured individuals for 1987 through 2009 based on the enhanced Current Population Survey (CPS) from the State Health Access Data Assistance Center (SHADAC). The CPS, sponsored jointly by the U.S. Census Bureau and the U.S. Bureau of Labor Statistics (BLS), is the primary source of labor force statistics for the population of the United States. (We refer readers to the website at: http://www.census.gov/programs-surveys/cps.html.) The enhanced CPS, available from SHADAC (available at: http://datacenter.shadac.org) accounts for changes in the CPS methodology over time. OACT further adjusts the enhanced CPS for an estimated undercount of Medicaid enrollees (a population that is often not fully captured in surveys that include Medicaid enrollees due to a perceived stigma associated with being enrolled in the Medicaid program or confusion about the source of their health insurance).
To estimate the number of uninsured individuals for 2010 through 2014, the OACT extrapolates from the 2009 CPS data using data from the National Health Interview Survey (NHIS). The NHIS is one of the major data collection programs of the National Center for Health Statistics (NCHS), which is part of the Centers for Disease Control and Prevention (CDC). The U.S. Census Bureau is the data collection agent for the NHIS. The NHIS results have been instrumental over the years in providing data to track health status, health care access, and progress toward achieving national health objectives. For further information regarding the NHIS, we refer readers to the CDC website at: https://www.cdc.gov/nchs/nhis/index.htm.
The next metrics needed to compute Factor 2 are projections of the rate of uninsurance in both calendar years 2019 and 2020. On an annual basis, OACT projects enrollment and spending trends for the coming 10-year period. Those projections (currently for years 2018 through 2027) use the latest NHEA historical data, which presently run through 2017. The NHEA projection methodology accounts for expected changes in enrollment across all of the categories of insurance coverage previously listed. The sources for projected growth rates in enrollment for Medicare, Medicaid, and CHIP include the latest Medicare Trustees Report, the Medicaid Actuarial Report, or other updated estimates as produced by OACT. Projected rates of growth in enrollment for private health insurance and the uninsured are based largely on OACT's econometric models, which rely on the set of macroeconomic assumptions underlying the latest Medicare Trustees Report. Greater detail can be found in OACT's report titled “Projections of National Health Expenditure: Methodology and Model Specification,” which is available on the CMS website at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/ProjectionsMethodology.pdf.
The use of data from the NHEA to estimate the rate of uninsurance is consistent with the statute and meets the criteria we have identified for determining the appropriate data source. Section 1886(r)(2)(B)(ii) of the Act instructs the Secretary to estimate the rate of uninsurance for purposes of Factor 2 based on data from the Census Bureau or other sources the Secretary determines appropriate. The NHEA utilizes data from the Census Bureau; the estimates are available in time for the IPPS rulemaking cycle; the estimates are produced by OACT on an annual basis and are expected to continue to be produced for the foreseeable future; and projections are available for calendar year time periods that span the upcoming fiscal year. Timeliness and continuity are important considerations because of our need to be able to update this estimate annually. Accuracy is also a very important consideration and, all things being equal, we would choose the most accurate data source that sufficiently meets our other criteria.
(2) Factor 2 for FY 2020
Using these data sources and the methodologies as previously described, the OACT has estimated that the uninsured rate for the historical, baseline year of 2013 was 14 percent and for CYs 2019 and 2020 is 9.4 percent and 9.4 percent, respectively.[316] As required by section 1886(r)(2)(B)(ii) of the Act, the Chief Actuary of CMS has certified these estimates.
As with the CBO estimates on which we based Factor 2 in prior fiscal years, the NHEA estimates are for a calendar year. In the rulemaking for FY 2014, many commenters noted that the uncompensated care payments are made for the fiscal year and not on a calendar year basis and requested that CMS normalize the CBO estimate to reflect a fiscal year basis. Specifically, commenters requested that CMS calculate a weighted average of the CBO estimate for October through December 2013 and the CBO estimate for January through September 2014 when determining Factor 2 for FY 2014. We agreed with the commenters that normalizing the estimate to cover FY 2014 rather than CY 2014 would more accurately reflect the rate of uninsurance that hospitals would experience during the FY 2014 payment year. Accordingly, we estimated the rate of uninsurance for FY 2014 by calculating a weighted average of the CBO estimates for CY 2013 and CY 2014 (78 FR 50633). We have continued this weighted average approach in each fiscal year since FY 2014.
We continue to believe that, in order to estimate the rate of uninsurance during a fiscal year more accurately, Factor 2 should reflect the estimated rate of uninsurance that hospitals will experience during the fiscal year, rather than the rate of uninsurance during only one of the calendar years that the fiscal year spans. Accordingly, we proposed to continue to apply the weighted average approach used in past fiscal years in order to estimate the rate of uninsurance for FY 2020. The OACT has certified this estimate of the fiscal year rate of uninsurance to be reasonable and appropriate for purposes of section 1886(r)(2)(B)(ii) of the Act.
The calculation of the proposed Factor 2 for FY 2020 using a weighted average of the OACT's projections for CY 2019 and CY 2020 was as follows:
- Percent of individuals without insurance for CY 2013: 14 percent.
- Percent of individuals without insurance for CY 2019: 9.4 percent.
- Percent of individuals without insurance for CY 2020: 9.4 percent.
- Percent of individuals without insurance for FY 2020 (0.25 times 0.094) + (0.75 times 0.094): 9.4 percent.
1−|((0.094−0.14)/0.14)| = 1−0.3286 = 0.6714 (67.14 percent).
For FY 2020 and subsequent fiscal years, section 1886(r)(2)(B)(ii) of the Act no longer includes any reduction to the above calculation. Therefore, we proposed that Factor 2 for FY 2020 would be 67.14 percent.
The proposed FY 2020 uncompensated care amount was $12,643,011,209.74 × 0.6714 = $8,488,517,726.22.
Proposed FY 2020 Uncompensated Care Amount: $8,488,517,726.22.
We invited public comments on our proposed methodology for calculating Factor 2 for FY 2020.
Comment: A few commenters asserted that CMS did not adequately explain how the OACT derived the estimates that were used in calculating Factor 2. According to commenters, the coverage level and underlying assumptions used by the agency resulted in the underestimation of Factor 2, which in turn diminished uncompensated care payments for hospitals. Commenters also expressed concerns generally about the amount of money available to make uncompensated payments and noted that the amount of money available for overall Medicare DSH payments, including both empirically justified DSH payments and uncompensated care payments, drastically changed under the new methodology established in the Affordable Care Act. They pointed out that as the number of uninsured people in the country increases, it is imperative that hospitals receive adequate Medicare DSH payments to cover the costs of increasing numbers of underinsured and uninsured patients. A commenter requested that CMS either revise Factor 2 to account for the estimated reduction in Medicaid enrollment as suggested by the 0.9932 “Other” adjustment in determining Factor 1 or explain why such a revision is unnecessary.
Response: We have been and continue to be transparent with respect to the methodology and data used to estimate Factor 2, and we disagree with commenters who assert otherwise. The FY 2020 IPPS/LTCH PPS proposed rule included a detailed discussion of our proposed Factor 2 methodology and the data sources that would be used in making our estimate. Section 1886(r)(2)(B)(ii) of the Act permits us to use a data source other than CBO estimates to determine the percent change in the rate of uninsurance beginning in FY 2018. As we explained in the proposed rule, we believe that the NHEA data, on balance, best meets all of our considerations, including the statutory requirement that the estimate be based on data from the Census Bureau or other sources the Secretary determines appropriate, and will allow reasonable estimates of the rate of uninsurance to be available in conjunction with the IPPS rulemaking cycle.
In response to the commenter that requested that CMS either revise Factor 2 to account for the estimated reduction in Medicaid enrollment as suggested by the 0.9932 “Other” adjustment in determining Factor 1 or explain why such a revision is unnecessary, we note that the “Other” adjustment relates to a number of factors, and does not represent only the effects of Medicaid expansion under the Affordable Care Act. As discussed in the proposed rule, the “Other” column shows the increase or decrease in certain other factors that also contribute to the estimate of Medicare DSH payments. These factors include the difference between total inpatient hospital discharges and IPPS discharges (particularly those in DSH hospitals) and various adjustments to the payment rates that have been included over the years but are not picked up in the other columns (such as the increase in rates for the two midnight policy). We note that the “Other” factor used in determining Factor 1 in this FY 2020 final rule is 1.0012.
After consideration of the public comments we received, we are finalizing the calculation of Factor 2 for FY 2020 as proposed. The estimates of the percent of uninsured individuals have been certified by the Chief Actuary of CMS, as discussed in the proposed rule. The calculation of the final Factor 2 for FY 2020 using a weighted average of OACT's projections for CY 2019 and CY 2020 is as follows:
- Percent of individuals without insurance for CY 2013: 14 percent.
- Percent of individuals without insurance for CY 2019: 9.4 percent.
- Percent of individuals without insurance for CY 2020: 9.4 percent.
- Percent of individuals without insurance for FY 2020 (0.25 times 0.094).
- Percent of individuals without insurance for FY 2020 (0.25 times 0.094) + (0.75 times 0.094): 9.4 percent.
1−|((0.094−0.14)/0.14)| = 1−0.3286 = 0.6714 (67.14 percent).
Therefore, the final Factor 2 for FY 2020 is 67.14 percent.
The final FY 2020 uncompensated care amount is $12,437,591,742.69 × 0.6714 = $8,350,599,096.04.
FY 2020 Uncompensated Care Amount: $8,350,599,096.04.
c. Calculation of Factor 3 for FY 2020
(1) General Background
Section 1886(r)(2)(C) of the Act defines Factor 3 in the calculation of the uncompensated care payment. As we have discussed earlier, section 1886(r)(2)(C) of the Act states that Factor 3 is equal to the percent, for each subsection (d) hospital, that represents the quotient of: (1) The amount of uncompensated care for such hospital for a period selected by the Secretary (as estimated by the Secretary, based on appropriate data (including, in the case where the Secretary determines alternative data are available that are a better proxy for the costs of subsection (d) hospitals for treating the uninsured, the use of such alternative data)); and (2) the aggregate amount of uncompensated care for all subsection (d) hospitals that receive a payment under section 1886(r) of the Act for such period (as so estimated, based on such data).
Therefore, Factor 3 is a hospital-specific value that expresses the proportion of the estimated uncompensated care amount for each subsection (d) hospital and each subsection (d) Puerto Rico hospital with the potential to receive Medicare DSH payments relative to the estimated uncompensated care amount for all hospitals estimated to receive Medicare DSH payments in the fiscal year for which the uncompensated care payment is to be made. Factor 3 is applied to the product of Factor 1 and Factor 2 to determine the amount of the uncompensated care payment that each eligible hospital will receive for FY 2014 and subsequent fiscal years. In order to implement the statutory requirements for this factor of the uncompensated care payment formula, it was necessary to determine: (1) The definition of uncompensated care or, in other words, the specific items that are to be included in the numerator (that is, the estimated uncompensated care amount for an individual hospital) and the denominator (that is, the estimated uncompensated care amount for all hospitals estimated to receive Medicare DSH payments in the applicable fiscal year); (2) the data source(s) for the estimated uncompensated care amount; and (3) the timing and manner of computing the quotient for each hospital estimated to receive Medicare DSH payments. The statute instructs the Secretary to estimate the amounts of uncompensated care for a period based on appropriate data. In addition, we note that the statute permits the Secretary to use alternative data in the case where the Secretary determines that such alternative data are available that are a better proxy for the costs of subsection (d) hospitals for treating individuals who are uninsured.
In the course of considering how to determine Factor 3 during the rulemaking process for FY 2014, the first year this provision was in effect, we considered defining the amount of uncompensated care for a hospital as the uncompensated care costs of that hospital and determined that Worksheet S-10 of the Medicare cost report potentially provides the most complete data regarding uncompensated care costs for Medicare hospitals. However, because of concerns regarding variations in the data reported on Worksheet S-10 and the completeness of these data, we did not use Worksheet S-10 data to determine Factor 3 for FY 2014, or for FYs 2015, 2016, or 2017. Instead, we believed that the utilization of insured low-income patients, as measured by patient days, would be a better proxy for the costs of hospitals in treating the uninsured and therefore appropriate to use in calculating Factor 3 for these years. Of particular importance in our decision making was the relative newness of Worksheet S-10, which went into effect on May 1, 2010. At the time of the rulemaking for FY 2014, the most recent available cost reports would have been from FYs 2010 and 2011, which were submitted on or after May 1, 2010, when the new Worksheet S-10 went into effect. We believed that concerns about the standardization and completeness of the Worksheet S-10 data could be more acute for data collected in the first year of the Worksheet's use (78 FR 50635). In addition, we believed that it would be most appropriate to use data elements that have been historically publicly available, subject to audit, and used for payment purposes (or that the public understands will be used for payment purposes) to determine the amount of uncompensated care for purposes of Factor 3 (78 FR 50635). At the time we issued the FY 2014 IPPS/LTCH PPS final rule, we did not believe that the available data regarding uncompensated care from Worksheet S-10 met these criteria and, therefore, we believed they were not reliable enough to use for determining FY 2014 uncompensated care payments. For FYs 2015, 2016, and 2017, the cost reports used for calculating uncompensated care payments (that is, FYs 2011, 2012, and 2013) were also submitted prior to the time that hospitals were on notice that Worksheet S-10 could be the data source for calculating uncompensated care payments. Therefore, we believed it was also appropriate to use proxy data to calculate Factor 3 for these years. We indicated our belief that Worksheet S-10 could ultimately serve as an appropriate source of more direct data regarding uncompensated care costs for purposes of determining Factor 3 once hospitals were submitting more accurate and consistent data through this reporting mechanism.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38202), we stated that we could no longer conclude that alternative data to the Worksheet S-10 are available for FY 2014 that are a better proxy for the costs of subsection (d) hospitals for treating individuals who are uninsured. Hospitals were on notice as of FY 2014 that Worksheet S-10 could eventually become the data source for CMS to calculate uncompensated care payments. Furthermore, hospitals' cost reports from FY 2014 had been publicly available for some time, and CMS had analyses of Worksheet S-10, conducted both internally and by stakeholders, demonstrating that Worksheet S-10 accuracy had improved over time. Analyses performed by MedPAC had already shown that the correlation between audited uncompensated care data from 2009 and the data from the FY 2011 Worksheet S-10 was over 0.80, as compared to a correlation of approximately 0.50 between the audited uncompensated care data and 2011 Medicare SSI and Medicaid days. Based on this analysis, MedPAC concluded that use of Worksheet S-10 data was already better than using Medicare SSI and Medicaid days as a proxy for uncompensated care costs, and that the data on Worksheet S-10 would improve over time as the data are actually used to make payments (81 FR 25090). In addition, a 2007 MedPAC analysis of data from the Government Accountability Office (GAO) and the American Hospital Association (AHA) had suggested that Medicaid days and low-income Medicare days are not an accurate proxy for uncompensated care costs (80 FR 49525).
Subsequent analyses from Dobson/DaVanzo, originally commissioned by CMS for the FY 2014 rulemaking and updated in later years, compared Worksheet S-10 and IRS Form 990 data and assessed the correlation in Factor 3s derived from each of the data sources. Our analyses on balance led us to believe that we had reached a tipping point in FY 2018 with respect to the use of the Worksheet S-10 data. We refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38201 through 38203) for a complete discussion of these analyses.
We found further evidence for this tipping point when we examined changes to the FY 2014 Worksheet S-10 data submitted by hospitals following the publication of the FY 2017 IPPS/LTCH PPS final rule. In the FY 2017 IPPS/LTCH PPS final rule, as part of our ongoing quality control and data improvement measures for the Worksheet S-10, we referred readers to Change Request 9648, Transmittal 1681, titled “The Supplemental Security Income (SSI)/Medicare Beneficiary Data for Fiscal Year 2014 for Inpatient Prospective Payment System (IPPS) Hospitals, Inpatient Rehabilitation Facilities (IRFs), and Long Term Care Hospitals (LTCHs),” issued on July 15, 2016 (available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R1681OTN.pdf). In this transmittal, as part of the process for ensuring complete submission of Worksheet S-10 by all eligible DSH hospitals, we instructed MACs to accept amended Worksheets S-10 for FY 2014 cost reports submitted by hospitals (or initial submissions of Worksheet S-10 if none had been submitted previously) and to upload them to the Health Care Provider Cost Report Information System (HCRIS) in a timely manner. The transmittal stated that, for revisions to be considered, hospitals were required to submit their amended FY 2014 cost report containing the revised Worksheet S-10 (or a completed Worksheet S-10 if no data were included on the previously submitted cost report) to the MAC no later than September 30, 2016. For the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 19949 through 19950), we examined hospitals' FY 2014 cost reports to see if the Worksheet S-10 data on those cost reports had changed as a result of the opportunity for hospitals to submit revised Worksheet S-10 data for FY 2014. Specifically, we compared hospitals' FY 2014 Worksheet S-10 data as they existed in the first quarter of CY 2016 with data from the fourth quarter of CY 2016. We found that the FY 2014 Worksheet S-10 data had changed over that time period for approximately one quarter of hospitals that receive uncompensated care payments. The fact that the Worksheet S-10 data changed for such a significant number of hospitals following a review of the cost report data they originally submitted and that the revised Worksheet S-10 information is available to be used in determining uncompensated care costs contributed to our belief that we could no longer conclude that alternative data are available that are a better proxy than the Worksheet S-10 data for the costs of subsection (d) hospitals for treating individuals who are uninsured.
We also recognized commenters' concerns that, in using Medicaid days as part of the proxy for uncompensated care, it would be possible for hospitals in States that choose to expand Medicaid to receive higher uncompensated care payments because they may have more Medicaid patient days than hospitals in a State that does not choose to expand Medicaid. Because the earliest Medicaid expansions under the Affordable Care Act began in 2014, the 2011, 2012, and 2013 Medicaid days used to calculate uncompensated care payments in FYs 2015, 2016, and 2017 are the latest available data on Medicaid utilization that do not reflect the effects of these Medicaid expansions. Accordingly, if we had used only low-income insured days to estimate uncompensated care in FY 2018, we would have needed to hold the time period of these data constant and use data on Medicaid days from 2011, 2012, and 2013 in order to avoid the risk of any redistributive effects arising from the decision to expand Medicaid in certain States. As a result, we would have been using older data that may provide a less accurate proxy for the level of uncompensated care being furnished by hospitals, contributing to our growing concerns regarding the continued use of low-income insured days as a proxy for uncompensated care costs in FY 2018.
In summary, as we stated in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38203), when weighing the new information regarding the correlation between the Worksheet S-10 data and IRS 990 data that became available to us after the FY 2017 rulemaking in conjunction with the information regarding Worksheet S-10 data and the low-income days proxy that we analyzed as part of our consideration of this issue in prior rulemaking, we determined that we could no longer conclude that alternative data to the Worksheet S-10 are available for FY 2014 that are a better proxy for the costs of subsection (d) hospitals for treating individuals who are uninsured. We also stated that we believe that continued use of Worksheet S-10 will improve the accuracy and consistency of the reported data, especially in light of CMS' concerted efforts to allow hospitals to review and resubmit their Worksheet S-10 data for past years and the use of trims for potentially aberrant data (82 FR 38207, 38217, and 38218). We also committed to continue to work with stakeholders to address their concerns regarding the accuracy of the reporting of uncompensated care costs through provider education and refinement of the instructions to Worksheet S-10.
For FY 2019, as discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41413), we continued to monitor the reporting of Worksheet S-10 data in anticipation of using Worksheet S-10 data from hospitals' FY 2014 and FY 2015 cost reports in the calculation of Factor 3. We acknowledged the concerns that had been raised regarding the instructions for Worksheet S-10. In particular, commenters had expressed concerns that the lack of clear and concise line-level instructions prevented accurate and consistent data from being reported on Worksheet S-10. We noted that, in November 2016, CMS issued Transmittal 10, which clarified and revised the instructions for the Worksheet S-10, including the instructions regarding the reporting of charity care charges. Transmittal 10 is available for download on the CMS website at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R10P240.pdf. In Transmittal 10, we clarified that hospitals may include discounts given to uninsured patients who meet the hospital's charity care criteria in effect for that cost reporting period. This clarification applied to cost reporting periods beginning prior to October 1, 2016, as well as cost reporting periods beginning on or after October 1, 2016. As a result, nothing prohibits a hospital from considering a patient's insurance status as a criterion in its charity care policy. A hospital determines its own financial criteria as part of its charity care policy. The instructions for the Worksheet S-10 set forth that hospitals may include discounts given to uninsured patients, including patients with coverage from an entity that does not have a contractual relationship with the provider, who meet the hospital's charity care criteria in effect for that cost reporting period. In addition, we revised the instructions for the Worksheet S-10 for cost reporting periods beginning on or after October 1, 2016, to provide that charity care charges must be determined in accordance with the hospital's charity care criteria/policy and written off in the cost reporting period, regardless of the date of service.
During the FY 2018 rulemaking, commenters pointed out that, in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56963), CMS agreed to institute certain additional quality control and data improvement measures prior to moving forward with incorporating Worksheet S-10 data into the calculation of Factor 3. However, the commenters indicated that, aside from a brief window in 2016 for hospitals to submit corrected data on their FY 2014 Worksheet S-10 by September 30, 2016, and the issuance of revised instructions (Transmittal 10) in November 2016 that are applicable to cost reports beginning on or after October 1, 2016, CMS had not implemented any additional quality control and data improvement measures. We stated in the FY 2018 IPPS/LTCH PPS final rule that we would continue to work with stakeholders to address their concerns regarding the reporting of uncompensated care through provider education and refinement of the instructions to the Worksheet S-10 (82 FR 38206).
On September 29, 2017, we issued Transmittal 11, which clarified the definitions and instructions for uncompensated care, non-Medicare bad debt, non-reimbursed Medicare bad debt, and charity care, as well as modified the calculations relative to uncompensated care costs and added edits to ensure the integrity of the data reported on Worksheet S-10. Transmittal 11 is available for download on the CMS website at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2017Downloads/R11p240.pdf. We further clarified that full or partial discounts given to uninsured patients who meet the hospital's charity care policy or financial assistance policy/uninsured discount policy (hereinafter referred to as Financial Assistance Policy or FAP) may be included on Line 20, Column 1 of Worksheet S-10. These clarifications apply to cost reporting periods beginning on or after October 1, 2013. We also modified the application of the CCR. We specified that the CCR will not be applied to the deductible and coinsurance amounts for insured patients approved for charity care and non-reimbursed Medicare bad debt. The CCR will be applied to the charges for uninsured patients approved for charity care or an uninsured discount, non-Medicare bad debt, and charges for noncovered days exceeding a length of stay limit imposed on patients covered by Medicaid or other indigent care programs.
We also provided another opportunity for hospitals to submit revisions to their Worksheet S-10 data for FY 2014 and FY 2015 cost reports. We refer readers to Change Request 10378, Transmittal 1981, titled “Fiscal Year (FY) 2014 and 2015 Worksheet S-10 Revisions: Further Extension for All Inpatient Prospective Payment System (IPPS) Hospitals,” issued on December 1, 2017 (available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2017Downloads/R1981OTN.pdf). In this transmittal, we instructed MACs to accept amended Worksheets S-10 for FY 2014 and FY 2015 cost reports submitted by hospitals (or initial submissions of Worksheet S-10 if none had been submitted previously) and to upload them to the Health Care Provider Cost Report Information System (HCRIS) in a timely manner. The transmittal included the deadlines by which hospitals needed to submit their amended FY 2014 and FY 2015 cost reports containing the revised Worksheet S-10 (or a completed Worksheet S-10 if no data were included on the previously submitted cost report) to the MAC, as well as the dates by which MACs must have accepted these data and uploaded the revised cost report to the HCRIS, in order for the data to be considered for purposes of the FY 2019 rulemaking.
(2) Background on the Methodology Used To Calculate Factor 3 for FY 2019
Section 1886(r)(2)(C) of the Act governs both the selection of the data to be used in calculating Factor 3, and also allows the Secretary the discretion to determine the time periods from which we will derive the data to estimate the numerator and the denominator of the Factor 3 quotient. Specifically, section 1886(r)(2)(C)(i) of the Act defines the numerator of the quotient as the amount of uncompensated care for such hospital for a period selected by the Secretary. Section 1886(r)(2)(C)(ii) of the Act defines the denominator as the aggregate amount of uncompensated care for all subsection (d) hospitals that receive a payment under section 1886(r) of the Act for such period. In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50638), we adopted a process of making interim payments with final cost report settlement for both the empirically justified Medicare DSH payments and the uncompensated care payments required by section 3133 of the Affordable Care Act. Consistent with that process, we also determined the time period from which to calculate the numerator and denominator of the Factor 3 quotient in a way that would be consistent with making interim and final payments. Specifically, we must have Factor 3 values available for hospitals that we estimate will qualify for Medicare DSH payments and for those hospitals that we do not estimate will qualify for Medicare DSH payments but that may ultimately qualify for Medicare DSH payments at the time of cost report settlement.
In the FY 2017 IPPS/LTCH PPS final rule, in order to mitigate undue fluctuations in the amount of uncompensated care payments to hospitals from year to year and smooth over anomalies between cost reporting periods, we finalized a policy of calculating a hospital's share of uncompensated care based on an average of data derived from three cost reporting periods instead of one cost reporting period. As explained in the preamble to the FY 2017 IPPS/LTCH PPS final rule (81 FR 56957 through 56959), instead of determining Factor 3 using data from a single cost reporting period as we did in FY 2014, FY 2015, and FY 2016, we used data from three cost reporting periods (Medicaid data for FYs 2011, 2012, and 2013 and SSI days from the three most recent available years of SSI utilization data (FYs 2012, 2013, and 2014)) to compute Factor 3 for FY 2017. Furthermore, instead of determining a single Factor 3 as we had done since the first year of the uncompensated care payment in FY 2014, we calculated an individual Factor 3 for each of the three cost reporting periods, which we then averaged by the number of cost reporting years with data to compute the final Factor 3 for a hospital. Under this policy, if a hospital had merged, we would combine data from both hospitals for the cost reporting periods in which the merger was not reflected in the surviving hospital's cost report data to compute Factor 3 for the surviving hospital. Moreover, to further reduce undue fluctuations in a hospital's uncompensated care payments, if a hospital filed multiple cost reports beginning in the same fiscal year, we combined data from the multiple cost reports so that the hospital could have a Factor 3 calculated using more than one cost report within a cost reporting period. We codified these changes for FY 2017 by amending the regulation at § 412.106(g)(1)(iii)(C).
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38213 through 38214), to address the issue of both long and short cost reporting periods, we finalized a policy of annualizing cost reports that do not have 12 months of data. As stated in the FY 2018 IPPS/LTCH PPS final rule, if the time between the start date of a hospital's cost reporting year and the end date of its cost reporting year is less than 12 months, we annualize the data so that the hospital has 12 months of data included in its Factor 3 calculation. Conversely, if the time between the aforementioned start date and the end date is greater than 12 months, we annualize the Medicaid days to achieve 12 months of Medicaid day's data. Under the policy adopted in the FY 2018 IPPS/LTCH PPS final rule, if a hospital filed more than one cost report beginning in the same fiscal year, we would first combine the data across the multiple cost reports before determining the difference between the start date and the end date to see if annualization is needed.
To address the effects of averaging Factor 3s calculated for three separate fiscal years, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38214 through 38215), we finalized a policy under which we apply a scaling factor to the Factor 3 values of all DSH eligible hospitals so that total uncompensated care payments will be consistent with the estimated amount available to make uncompensated care payments for the fiscal year. Specifically, we adopted a policy under which we divide 1 (the expected sum of all eligible hospitals' Factor 3 values) by the actual sum of all eligible hospitals' Factor 3 values and multiply the quotient by each hospital's total uncompensated care payment to obtain scaled uncompensated care payment amounts whose sum is consistent with the estimate of the total amount available to make uncompensated care payments.
As we stated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41414), with the additional steps we had taken to ensure the accuracy and consistency of the data reported on Worksheet S-10 since the publication of the FY 2018 IPPS/LTCH PPS final rule, we continued to believe that we can no longer conclude that alternative data to the Worksheet S-10 are currently available for FY 2014 that are a better proxy for the costs of subsection (d) hospitals for treating individuals who are uninsured. Similarly, the actions that we have taken to improve the accuracy and consistency of the Worksheet S-10 data, including the opportunity for hospitals to resubmit Worksheet S-10 data for FY 2015, led us to conclude that there are no alternative data to the Worksheet S-10 data currently available for FY 2015 that are a better proxy for the costs of subsection (d) hospitals for treating uninsured individuals. As such, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41428), we finalized our proposal to advance the time period of the data used in the calculation of Factor 3 forward by 1 year and to use data from FY 2013, FY 2014, and FY 2015 cost reports to determine Factor 3 for FY 2019. For the reasons we described earlier, we stated that we continue to believe it is inappropriate to use Worksheet S-10 data for periods prior to FY 2014. Rather, for cost reporting periods prior to FY 2014, we indicated that we believe it is appropriate to continue to use low-income insured days. Accordingly, with a time period that includes 3 cost reporting years consisting of FY 2013, FY 2014, and FY 2015, we used Worksheet S-10 data for the FY 2014 and FY 2015 cost reporting periods and the low-income insured days proxy data for the earliest cost reporting period. As in previous years, in order to perform this calculation for the FY 2019 final rule, we drew three sets of data (1 year of Medicaid utilization data and 2 years of Worksheet S-10 data) from the most recent available HCRIS extract, which was the June 30, 2018 update of HCRIS, due to the unique circumstances related to the impact of the hurricanes in 2017 (Harvey, Irma, Maria, and Nate) and the extension of the deadline to resubmit Worksheet S-10 data through January 2, 2018, and the subsequent impact on the MAC review timeline (83 FR 41421).
Accordingly, for FY 2019, in addition to the Worksheet S-10 data for FY 2014 and FY 2015, we used Medicaid days from FY 2013 cost reports and FY 2016 SSI ratios. We noted that cost report data from Indian Health Service and Tribal hospitals are included in HCRIS beginning in FY 2013 and no longer need to be incorporated from a separate data source. We also continued the policies that were finalized in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50020) to address several specific issues concerning the process and data to be employed in determining Factor 3 in the case of hospital mergers. In addition, we continued the policies that were finalized in the FY 2018 IPPS/LTCH PPS final rule to address technical considerations related to the calculation of Factor 3 and the incorporation of Worksheet S-10 data (82 FR 38213 through 38220). In that final rule, we adopted a policy, for purposes of calculating Factor 3, under which we annualize Medicaid days data and uncompensated care cost data reported on the Worksheet S-10 if a hospital's cost report does not equal 12 months of data. As in FY 2018, for FY 2019, we did not annualize SSI days because we do not obtain these data from hospital cost reports in HCRIS. Rather, we obtained these data from the latest available SSI ratios posted on the Medicare DSH homepage (https://www.cms.gov/Medicare/Medicare-fee-for-service-payment/AcuteInpatientPPS/dsh.html), which were aggregated at the hospital level and did not include the information needed to determine if the data should be annualized. To address the effects of averaging Factor 3s calculated for 3 separate fiscal years, we continued to apply a scaling factor to the Factor 3 values of all DSH eligible hospitals such that total uncompensated care payments are consistent with the estimated amount available to make uncompensated care payments for the applicable fiscal year. With respect to the incorporation of data from Worksheet S-10, we indicated that we believe that the definition of uncompensated care adopted in FY 2018 is still appropriate because it incorporates the most commonly used factors within uncompensated care as reported by stakeholders, including charity care costs and non-Medicare bad debt costs, and correlates to Line 30 of Worksheet S-10. Therefore, for purposes of calculating Factor 3 and uncompensated care costs in FY 2019, we again defined “uncompensated care” as the amount on Line 30 of Worksheet S-10, which is the cost of charity care (Line 23) and the cost of non-Medicare bad debt and nonreimbursable Medicare bad debt (Line 29).
We noted that we were discontinuing the policy finalized in the FY 2017 IPPS/LTCH PPS final rule concerning multiple cost reports beginning in the same fiscal year (81 FR 56957). Under this policy, we would first combine the data across the multiple cost reports before determining the difference between the start date and the end date to determine if annualization was needed. This policy was developed in response to commenters' concerns regarding the unique circumstances of hospitals that file cost reports that are shorter or longer than 12 months. As we explained in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56957 through 56959) and in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 19953), we believed that, for hospitals that file multiple cost reports beginning in the same year, combining the data from these cost reports had the benefit of supplementing the data of hospitals that filed cost reports that are less than 12 months, such that the basis of their uncompensated care payments and those of hospitals that filed full-year 12-month cost reports would be more equitable. As we stated in the FY 2019 IPPS/LTCH PPS proposed and final rules, we now believe that concerns about the equitability of the data used as the basis of hospital uncompensated care payments are more thoroughly addressed by the policy finalized in the FY 2018 IPPS/LTCH PPS final rule, under which CMS annualizes the Medicaid days and uncompensated care cost data of hospital cost reports that do not equal 12 months of data. Based on our experience, we stated that we believe that in many cases where a hospital files two cost reports beginning in the same fiscal year, combining the data across multiple cost reports before annualizing would yield a similar result to choosing the longer of the two cost reports and then annualizing the data if the cost report is shorter or longer than 12 months. Furthermore, even in cases where a hospital files more than one cost report beginning in the same fiscal year, it is not uncommon for one of those cost reports to span exactly 12 months. In this case, if Factor 3 is determined using only the full 12-month cost report, annualization would be unnecessary as there would already be 12 months of data. Therefore, for FY 2019, we stated that we believed it was appropriate to eliminate the additional step of combining data across multiple cost reports if a hospital filed more than one cost report beginning in the same fiscal year. Instead, for purposes of calculating Factor 3, we used data from the cost report that is equivalent to 12 months or, if no such cost report existed, the cost report that was closest to 12 months, and annualized the data. Furthermore, we acknowledged that, in rare cases, a hospital may have more than one cost report beginning in one fiscal year, where one report also spans the entirety of the following fiscal year, such that the hospital has no cost report beginning in that fiscal year. For instance, a hospital's cost reporting period may have started towards the end of FY 2012 but cover the duration of FY 2013. In these rare situations, we would use data from the cost report that spans both fiscal years in the Factor 3 calculation for the latter fiscal year as the hospital would already have data from the preceding cost report that could be used to determine Factor 3 for the previous fiscal year.
In FY 2019, we also continued to apply statistical trims to anomalous hospital CCRs using a similar methodology to the one adopted in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38217 through 38219), where we stated our belief that, just as we apply trims to hospitals' CCRs to eliminate anomalies when calculating outlier payments for extraordinarily high cost cases (§ 412.84(h)(3)(ii)), it is appropriate to apply statistical trims to the CCRs on Worksheet S-10, Line 1, that are considered anomalies. Specifically, § 412.84(h)(3)(ii) states that the Medicare contractor may use a statewide CCR for hospitals whose operating or capital CCR is in excess of 3 standard deviations above the corresponding national geometric mean (that is, the CCR “ceiling”). The geometric means for purposes of the Worksheet S-10 trim of CCRs and for purposes of § 412.84(h)(3)(ii) are separately calculated annually by CMS and published in the applicable sections of the proposed and final IPPS rules each year. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41415) for a detailed description of the CCR trim methodology for purposes of the Worksheet S-10 trim of CCRs, which included calculating 3 standard deviations above the national geometric mean CCR for each of the applicable cost report years (FY 2014 and FY 2015) that were part of the Factor 3 methodology for FY 2019.
Similar in concept to the policy that we adopted for FY 2018, for FY 2019, we stated that we continued to believe that uncompensated care costs that represent an extremely high ratio of a hospital's total operating expenses (such as the ratio of 50 percent used in the FY 2018 IPPS/LTCH PPS final rule) may be potentially aberrant, and that using the ratio of uncompensated care costs to total operating costs to identify potentially aberrant data when determining Factor 3 amounts has merit. We noted that we had instructed the MACs to review situations where a hospital has an extremely high ratio of uncompensated care costs to total operating costs with the hospital, but also indicated that we did not intend to make the MACs' review protocols public (83 FR 41416). Similarly, we believe that situations where there were extremely large dollar increases or decreases in a hospital's uncompensated care costs when it resubmitted its FY 2014 Worksheet S-10 or FY 2015 Worksheet S-10 data, or when the data it had previously submitted were reprocessed by the MAC, may reflect potentially aberrant data and warrant further review. In the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20399), we noted that our calculation of Factor 3 for the final rule would be contingent on the results of the ongoing MAC reviews of hospitals' Worksheet S-10 data, and in the event those reviews necessitate supplemental data edits, we would incorporate such edits in the final rule for the purpose of correcting aberrant data. After the completion of the MAC reviews, we did not incorporate any additional edits to the Worksheet S-10 data that we did not propose in the FY 2019 IPPS/LTCH PPS proposed rule. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41416) for a detailed discussion of our policies for trimming aberrant data. In brief summary, in cases where a hospital's uncompensated care costs for FY 2014 or FY 2015 were an extremely high ratio of its total operating costs, and the hospital could not justify the amount it reported, we determined the ratio of uncompensated care costs to the hospital's total operating costs from another available cost report, and applied that ratio to the total operating expenses for the potentially aberrant fiscal year to determine an adjusted amount of uncompensated care costs. For example, if the FY 2015 cost report was determined to include potentially aberrant data, data from the FY 2016 cost report would be used for the ratio calculation. In this case, the hospital's uncompensated care costs for FY 2015 would be trimmed by multiplying its FY 2015 total operating costs by the ratio of uncompensated care costs to total operating costs from the hospital's FY 2016 cost report to calculate an estimate of the hospital's uncompensated care costs for FY 2015 for purposes of determining Factor 3 for FY 2019.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41416), for Indian Health Service and Tribal hospitals, subsection (d) Puerto Rico hospitals, and all-inclusive rate providers, we continued the policy we first adopted for FY 2018 of substituting data regarding FY 2013 low-income insured days for the Worksheet S-10 data when determining Factor 3. As we discussed in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38209), the use of data from Worksheet S-10 to calculate the uncompensated care amount for Indian Health Service and Tribal hospitals may jeopardize these hospitals' uncompensated care payments due to their unique funding structure. With respect to Puerto Rico hospitals, we indicated that we continue to agree with concerns raised by commenters that the uncompensated care data reported by these hospitals need to be further examined before the data are used to determine Factor 3 (82 FR 38209). Finally, we acknowledged that the CCRs for all-inclusive rate providers are potentially erroneous and still in need of further examination before they can be used in the determination of uncompensated care amounts for purposes of Factor 3 (82 FR 38212). For the reasons described earlier related to the impact of the Medicaid expansion beginning in FY 2014, we stated that we also continue to believe that it is inappropriate to calculate a Factor 3 using FY 2014 and FY 2015 low-income insured days. Because we did not believe it was appropriate to use the FY 2014 or FY 2015 uncompensated care data for these hospitals and we also did not believe it was appropriate to use the FY 2014 or FY 2015 low-income insured days, we stated that the best proxy for the costs of Indian Health Service and Tribal hospitals, subsection (d) Puerto Rico hospitals, and all-inclusive rate providers for treating the uninsured continues to be the low-income insured days data for FY 2013. Accordingly, for these hospitals, we determined Factor 3 only on the basis of low-income insured days for FY 2013. We stated our belief that this approach was appropriate as the FY 2013 data reflect the most recent available information regarding these hospitals' low-income insured days before any expansion of Medicaid. In addition, because we continued to use 1 year of insured low-income patient days as a proxy for uncompensated care and residents of Puerto Rico are not eligible for SSI benefits, we continued to use a proxy for SSI days for Puerto Rico hospitals consisting of 14 percent of the hospital's Medicaid days, as finalized in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56953 through 56956).
Therefore, for FY 2019, we computed Factor 3 for each hospital by—
Step 1: Calculating Factor 3 using the low-income insured days proxy based on FY 2013 cost report data and the FY 2016 SSI ratio (or, for Puerto Rico hospitals, 14 percent of the hospital's FY 2013 Medicaid days);
Step 2: Calculating Factor 3 based on the FY 2014 Worksheet S-10 data;
Step 3: Calculating Factor 3 based on the FY 2015 Worksheet S-10 data; and
Step 4: Averaging the Factor 3 values from Steps 1, 2, and 3; that is, adding the Factor 3 values from FY 2013, FY 2014, and FY 2015 for each hospital, and dividing that amount by the number of cost reporting periods with data to compute an average Factor 3 (or for Puerto Rico hospitals, Indian Health Service and Tribal hospitals, and all-inclusive rate providers, using the Factor 3 value from Step 1).
We also amended the regulations at § 412.106(g)(1)(iii)(C) by adding a new paragraph (5) to reflect the previously discussed methodology for computing Factor 3 for FY 2019.
In the FY 2019 IPPS/LTCH PPS final rule, we noted that if a hospital does not have both Medicaid days for FY 2013 and SSI days for FY 2016 available for use in the calculation of Factor 3 in Step 1, we would consider the hospital not to have data available for the fiscal year, and would remove that fiscal year from the calculation and divide by the number of years with data. A hospital would be considered to have both Medicaid days and SSI days data available if it reported zero days for either component of the Factor 3 calculation in Step 1. However, if a hospital was missing data due to not filing a cost report in one of the applicable fiscal years, we would divide by the remaining number of fiscal years.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41417), we noted that we did not make any proposals with respect to the development of Factor 3 for FY 2020 and subsequent fiscal years. However, we noted that the previously discussed methodology would have the effect of fully transitioning the incorporation of data from Worksheet S-10 into the calculation of Factor 3 if used in FY 2020, and therefore, the use of low-income insured days would be phased out by FY 2020 if the same methodology were to be proposed and finalized for that year. We also indicated that it was possible that when we examine the FY 2016 Worksheet S-10 data, we might determine that the use of multiple years of Worksheet S-10 data is no longer necessary in calculating Factor 3 for FY 2020. We stated that, given the efforts hospitals have already undertaken with respect to reporting their Worksheet S-10 data and the subsequent reviews by the MACs that had already been conducted prior to the development of the FY 2019 IPPS/LTCH PPS final rule, along with additional review work that might take place following the issuance of the FY 2019 final rule, we might consider using 1 year of Worksheet S-10 data as the basis for calculating Factor 3 for FY 2020.
For new hospitals that did not have data for any of the three cost reporting periods used in the Factor 3 calculation for FY 2019, we continued to apply the new hospital policy finalized in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50643). That is, the hospital would not receive either interim empirically justified Medicare DSH payments or interim uncompensated care payments. However, if the hospital is later determined to be eligible to receive empirically justified Medicare DSH payments based on its FY 2019 cost report, the hospital would also receive an uncompensated care payment calculated using a Factor 3, where the numerator is the uncompensated care costs reported on Worksheet S-10 of the hospital's FY 2019 cost report, and the denominator is the sum of the uncompensated care costs reported on Worksheet S-10 of the FY 2015 cost reports for all DSH eligible hospitals (that is, the most recent year of the 3-year time period used in the development of Factor 3 for FY 2019). We noted that, given the time period of the data used to calculate Factor 3, any hospitals with a CCN established after October 1, 2015, would be considered new and subject to this policy.
(3) Methodology for Calculating Factor 3 for FY 2020
(a) Use of Audited FY 2015 Data
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19418 through 19419), since the publication of the FY 2019 IPPS/LTCH PPS final rule, we have continued to monitor the reporting of Worksheet S-10 data in order to determine the most appropriate data to use in the calculation of Factor 3 for FY 2020. As stated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41424), due to the overwhelming feedback from commenters emphasizing the importance of audits in ensuring the accuracy and consistency of data reported on the Worksheet S-10, we expected audits of the Worksheet S-10 to begin in the Fall of 2018. The audit protocol instructions were still under development at the time of the FY 2019 IPPS/LTCH PPS final rule; yet, we noted the audit protocols would be provided to the MACs in advance of the audit. Once the audit protocol instructions were complete, we began auditing the Worksheet S-10 data for selected hospitals in the Fall of 2018 so that the audited uncompensated care data from these hospitals would be available in time for use in the FY 2020 proposed rule. We chose to audit 1 year of data (that is, FY 2015) in order to maximize the available audit resources and not spread those audit resources over multiple years, potentially diluting their effectiveness. We chose to focus the audit on the FY 2015 cost reports primarily because this was the most recent year of data that we had broadly allowed to be resubmitted by hospitals, and many hospitals had already made considerable efforts to amend their FY 2015 reports for the FY 2019 rulemaking. We also considered that we had previously used the FY 2015 data as part of the calculation of the FY 2019 uncompensated care payments; therefore, the data had previously been subject to public comment and scrutiny.
Given that we have conducted audits of the FY 2015 Worksheet S-10 data and have previously used the FY 2015 data to determine uncompensated care payments, and the fact that the FY 2015 data are the most recent data that we have allowed to be resubmitted to date, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19419), we stated that we believe, on balance, that the FY 2015 Worksheet S-10 data are the best available data to use for calculating Factor 3 for FY 2020. However, as discussed in more detail later in the next section, we also considered using the FY 2017 data. In the proposed rule, we sought public comments on this alternative and stated that, based on the public comments we received, we could adopt this alternative in the FY 2020 final rule.
In the FY 2020 proposed rule, we recognized that, in FY 2019, we used 3 years of data in the calculation of Factor 3 in order to smooth over anomalies between cost reporting periods and to mitigate undue fluctuations in the amount of uncompensated care payments from year to year. However, we stated that, for FY 2020, we believe mixing audited and unaudited data for individual hospitals by averaging multiple years of data could potentially lead to a less smooth result, which is counter to our original goal in using 3 years of data. As we stated in the proposed rule, to the extent that the audited FY 2015 data for a hospital are relatively different from its unaudited FY 2014 data and/or its unaudited FY 2016 data, we potentially would be diluting the effect of our considerable auditing efforts and introducing unnecessary variability into the calculation if we continued to use 3 years of data to calculate Factor 3. As an example, we noted that approximately 10 percent of audited hospitals have more than a $20 million difference between their audited FY 2015 data and their unaudited FY 2016 data.
Accordingly, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19419), we proposed to use a single year of Worksheet S-10 data from FY 2015 cost reports to calculate Factor 3 in the FY 2020 methodology. We also noted that the proposed uncompensated care payments to hospitals whose FY 2015 Worksheet S-10 data were audited represented approximately half of the proposed total uncompensated care payments for FY 2020. For purposes of the FY 2020 proposed rule, we used the most recent available HCRIS extract available, which was the HCRIS data updated through February 15, 2019. We stated in the proposed rule that we expected to use the March 2019 update of HCRIS for the final rule.
Comment: Many commenters expressed support for CMS' proposal to utilize FY 2015 Worksheet S-10 data to determine each hospital's share of overall uncompensated care costs (UCC) in FY 2020. These commenters argued that data from the FY 2015 Worksheet S-10 are most appropriate for calculating Factor 3 because the data have been at least partially audited, and the audits result in data that are appropriate for use in determining uncompensated care payments. These commenters reiterated the discussion in the proposed rule, in which we explained that the audited hospitals were projected to receive approximately 50 percent of the total amount of the uncompensated care payments, and that CMS has afforded hospitals several opportunities to revise and resubmit FY 2015 Worksheet S-10 data to make it more accurate. To this end, a commenter indicated that uncompensated care costs calculated from the FY 2015 cost reports for DSH-eligible hospitals had declined nearly 18 percent between last year and this year as a result of amended data reported on the Worksheet S-10. These commenters believe that the corrective actions resulting from the FY 2015 Worksheet S-10 data audits outweigh the improved cost reporting instructions for the FY 2017 Worksheet S-10.
Conversely, many commenters opposed the proposed policy of using 1 year of FY 2015 Worksheet S-10 data to determine UCC. These commenters asserted that the instructions for completing the FY 2015 Worksheet S-10 were unclear and confusing, resulting in incomplete and inaccurate uncompensated care data. They believe that since the audited hospitals represent only half of the proposed total uncompensated care payments for FY 2020, the remaining half is highly susceptible to errors, due to the concerns with the instructions for the FY 2015 Worksheet S-10. In addition, many commenters voiced concerns with the auditing of the FY 2015 Worksheet S-10 data and opposed its use as a result of these concerns. Some commenters asserted that as a result of selective and inconsistent audits the FY 2015 Worksheet S-10 data may not be reliable for some providers. Additionally, some commenters stated that the mixing of data from audited and unaudited hospitals results in an uneven playing field, harming those hospitals that were audited to the benefit of those that were not. Finally, some commenters believed that the FY 2015 Worksheet S-10 data have already been used for FY 2019 uncompensated care payments and that more updated information needs to be used for FY 2020. These commenters also stated that continuing to use FY 2015 Worksheet S-10 data as the source of UCC creates a substantial lag in compensating hospitals for charity care that was provided in prior years.
Response: We thank commenters for their support of our proposal to use the FY 2015 Worksheet S-10 data to determine each hospital's share of UCC in FY 2020. We also appreciate the input from commenters who disagreed with the proposal. Given that we have conducted audits of the FY 2015 Worksheet S-10 data and have previously used the FY 2015 data to determine uncompensated care payments and the fact that the proposed uncompensated care payments to hospitals whose FY 2015 Worksheet S-10 data were audited represent approximately half of the total proposed uncompensated care payments for FY 2020, we believe that, on balance, the FY 2015 Worksheet S-10 data are the best available data to use for calculating Factor 3 for FY 2020. In response to the comment that the FY 2015 Worksheet S-10 data are outdated, we note that at the time we began auditing the FY 2015 Worksheet S-10 data in the Fall of 2018, the FY 2017 Worksheet S-10 data were incomplete as some hospitals were still submitting their cost reports. We chose to focus the audit on the FY 2015 cost reports primarily because this was the most recent year of data that we had broadly allowed to be resubmitted by hospitals, and many hospitals had already made considerable efforts to amend their FY 2015 reports prior to the FY 2019 rulemaking. We acknowledge that FY 2015 Worksheet S-10 data has not been audited for all hospitals . To the extent commenters believe that all hospitals' Worksheet S-10 data must be audited for there to be “level playing field” and for the data to be appropriate to use for FY 2020, we do not agree. We note that it was not feasible to audit all hospitals' FY 2015 report data for the FY 2020 rulemaking. The selection of hospitals for the FY 2015 Worksheet S-10 audits was based on a risk-based assessment process, which we believe was effective and appropriate. Regarding the commenter's assertion that the FY 2015 Worksheet S-10 data became unreliable as a result of the audit selection, process and/or adjustments, we refer readers to the discussion below. With respect to the commenters' concerns with Worksheet S-10 instructions for the FY 2015 cost reporting period, we refer readers to the discussion of these instructions in the later section on methodological considerations, where we address the comments related to the Worksheet S-10 instructions. We note that we will consider further commenters' concerns regarding data lag in future rulemaking in the determination of the best available data to calculate Factor 3 for future years.
Comment: A great number of commenters, whether in support of or in opposition to the proposed policy and the alternative considered, stated that as CMS moves from using a 3-year average to a single year of Worksheet S-10 data, the potential for anomalies and undue fluctuations in uncompensated care payments increases. Commenters stated that bad debt and charity write-offs can vary significantly from year to year for a given hospital, even if data are clean and accurate, and can cause large variations in uncompensated care payments. Several of these commenters questioned whether the proposal to move to a single year of the Worksheet S-10 data is a permanent decision by CMS, and many commenters recommended that CMS continue using a 3-year average to mitigate year-over-year volatility in uncompensated care payments, either now or in the future when additional years of audited Worksheet S-10 data become available. Some commenters remarked that the proposed CMS policy of relying on data from a single year increases the possibility of aberrant data from any 1 year or any one provider skewing the distribution of uncompensated care payments. They stated that a 3-year average could offer a stop-gap approach by providing a transition to a major change in the distribution of uncompensated care payments. A number of commenters requested that, if CMS does move to using 1 year of Worksheet S-10 data to calculate Factor 3, it also implement a stop-loss policy to protect hospitals that have a decrease of 5 to 10 percent in uncompensated care payments for any given year. Additionally, some commenters stated that there is variability in the amount of the per-discharge uncompensated care payment among hospitals, with the amount of the uncompensated care payment being higher than all other inpatient payments combined for some hospitals. These commenters recommended placing a limit on per-discharge uncompensated care payments, regardless of a hospital's Factor 3.
At the same time, other commenters stated that mixing audited and unaudited data is counterintuitive and would result in a poorly constructed 3-year average, in which the audited data would be diluted. Thus, many commenters believe that CMS should ultimately strive to average three years of audited data to determine hospitals' UCC. In contrast, other commenters supported the use of 1 year of data rather than a 3-year average. A commenter stated that if a provider has UCC that are rapidly changing, a 3-year average makes for a slow response. Additionally, the commenter believed that using a 3-year average hurts the newest of providers that don't have a full complement of data to report.
Response: We appreciate the commenters' support for our proposal to use 1 year of Worksheet S-10 data, as well as the requests from some commenters that we continue to use a 3-year average in the calculation of Factor 3 for FY 2020. Our primary reason for using a 3-year average in the past was to provide assurance that hospitals' uncompensated care payments would remain reasonably stable and predictable, and less subject to unpredictable swings and anomalies in a hospital's low-income insured days or reported uncompensated care costs between reporting periods. However, as we stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19419), we believe that, for FY 2020, mixing audited and unaudited data for individual hospitals by averaging multiple years of data could potentially lead to a less smooth result, which is counter to our original goal in using 3 years of data. To the extent that the audited FY 2015 data for a hospital are relatively different from its unaudited FY 2014, FY 2016, and/or FY 2017 data, we potentially would be diluting the effect of our considerable auditing efforts and introducing unnecessary variability into the calculation if we were to continue to use three years of data to calculate Factor 3. Still, given concerns raised by commenters regarding our proposal to use 1 year of data from the FY 2015 Worksheet S-10 to calculate Factor 3 for FY 2020, CMS may consider returning to the use of a 3-year average in rulemaking for future years, if appropriate.
Regarding commenters' recommendation that we adopt a stop-loss policy, we note that section 1886(r) does not provide CMS with authority to implement a stop-loss policy. Rather, section 1886(r)(2)(C) requires that we determine Factor 3 for each hospital based upon the ratio of the amount of uncompensated care furnished by the hospital compared to the uncompensated care furnished by all DSH-eligible hospitals, and there is no authority under section 1886(r) to adjust this amount. In the absence of such authority, we believe that the use of three years of data to determine Factor 3 for FYs 2018 and 2019, as discussed in the FY 2018 and FY 2019 IPPS/LTCH PPS final rules, provided a mechanism that had the effect of smoothing the transition from the use of low-income insured days to the use of Worksheet S-10 data. However, as we explained in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19419), for FY 2020, we believe mixing audited and unaudited data for individual hospitals by averaging multiple years of data could potentially lead to a less smooth result, which is counter to our original goal in using 3 years of data. When more years of audited data are available, we may consider returning to the use an average of more than 1 year (for example, a 3-year average), in rulemaking for future years. Regarding the comments recommending that CMS place a cap on the amount of per-discharge uncompensated care payments, we may consider the issue of per-discharge uncompensated care payments in future rulemaking including whether modifying the amount of interim uncompensated care payments would be administratively feasible in specific situations.
Comment: Many commenters proposed alternative ways to blend prior years' data for purposes of incorporating Worksheet S-10 data into the calculation of Factor 3. These alternative methodologies included suggestions to use data from the FY 2014, FY 2015, FY 2016, and FY 2017 Worksheet S-10 averaged together in various 3-year combinations, as well as suggestions to use later years when available. In addition to these suggestions, there were also commenters who supported the use of the FY 2015 Worksheet S-10 data, or the FY 2017 Worksheet S-10 data, but only in the context of an approach that also involved sources of data other than the Worksheet S-10. For example, some commenters recommended that CMS implement a blend utilizing low-income insured days, FY 2014 Worksheet S-10 data, and audited FY 2015 Worksheet S-10 data to calculate uncompensated care payments in FY 2020. A number of commenters suggested using a blend consisting of two-thirds of the uncompensated care payments hospitals received in FY 2019 and one third of hospitals' share of UCC based on the FY 2017 Worksheet S-10 data. Similarly, other commenters suggested using a blend of one-third low-income days and two-thirds UCC, including but not limited to using updated SSI days or FY 2019 Factor 3 shares, to calculate Factor 3 for FY 2020, in order to reduce payment variability. Some commenters believed a SSI day based proxy would produce a better estimate of uncompensated care costs Although these alternative methodologies were not proposed by CMS, commenters believe that CMS would have the authority to adopt one of the blends proposed by commenters as a logical outgrowth of the policies discussed in the proposed rule. Some commenters believed that ultimately, CMS should develop a review process similar to the one used to determine the hospital wage index, under which by FY 2023, CMS would utilize fully audited Worksheet S-10 data from FY 2017, FY 2018, and FY 2019 to determine Factor 3.
Response: We appreciate the comments regarding alternative ways to blend prior years' data for purposes of incorporating Worksheet S-10 data into the calculation of Factor 3 and the suggestions for alternative methods for computing proxies for uncompensated care costs. However, as we stated in the FY 2020 IPPS/LTCH PPS proposed rule, we can no longer conclude that alternative data to the Worksheet S-10 are available that are a better proxy for the costs of subsection (d) hospitals for treating individuals who are uninsured. As stated previously, we also believe that the FY 2015 Worksheet S-10 data are the best available data to use for calculating Factor 3 for FY 2020. As we continue to audit additional years of the Worksheet S-10 data and monitor the stability of uncompensated care payments, we may consider the use of multiple years of audited Worksheet S-10 data in rulemaking for future years. Regarding the comments recommending that CMS develop an audit process similar to hospital wage index reviews, we refer readers to the discussion below, which addresses the comments and suggestions on the audit process.
Comment: The auditing process for the FY 2015 Worksheet S-10 was a common topic within the public comments, and many commenters raised concerns regarding the audit process, in general, as well as with specific adjustments. Some commenters believed that auditing FY 2016 data would have been more effective than auditing FY 2015 data, because hospitals would have had an additional year of experience in understanding the reporting requirements and refining their data, resulting in fewer occasions for subjective audit differences. Another commenter expressed concern that the roughly 600 providers that were audited represented only approximately 25 percent of those eligible to receive Medicare DSH. Although some commenters acknowledged that these roughly 600 providers represented a large share of the total amount of uncompensated care payments, others observed that this sample of audited hospitals resulted in the proposed use of both audited and unaudited data for FY 2020. Some commenters believed that our proposal to use a mix of audited and unaudited FY 2015 data to be “arbitrary and capricious” and beyond the agency's legal authority. Other commenters believe that this mixture of data was disadvantageous to audited hospitals, to the benefit of those not audited.
A commenter believed that the auditing process for the FY 2015 Worksheet S-10 data was subjective and biased against providers with either high uncompensated care costs or with uncompensated care costs that may have changed significantly for good reason. Some commenters asserted that the audits lacked standardization, and that there were inconsistencies in the review adjustments made by the MACs and/or subcontractors, as well as variation across MACs in documentation requirements. According to these commenters, MACs made inconsistent adjustments across audited hospitals' UCC because they did not apply CMS's audit guidelines in a standardized and comprehensive manner. In addition, some commenters stated that cost report instructions still need to be clarified for issues that were addressed in the guidance included in the Worksheet S-10 Q&A issued following the FY 2018 final rule and in the audit protocols, and stated that the data elements needed for the audits should also be spelled out, like those required for bad debt logs.
Many commenters asserted that the audits of the FY 2015 Worksheet S-10 data were intense and rushed. Some commenters asserted that audit adjustments seemed inconsistent with the Worksheet S-10 instructions and were beyond the scope of the audit and the authority of the MACs. Examples of the types of concerns raised regarding the adjustments, include assertions that the adjustments were made under tight deadlines without providing hospitals the opportunity to review or appeal MAC decisions and that MACs made adjustments based on their own interpretation of language in hospitals' financial assistance policies, including disallowing discounts given to uninsured patients under the hospital's own financial assistance policy. The commenters believed these issues were a result of the MACs' lack of training and/or understanding of the charity care process. The issue of adjustments to charity care amounts for copayments was also prevalent among the comments related to adjustments. Commenters also described MAC adjustments related to increases made to expected patient payment amounts in Line 22 of Worksheet S-10 such that expected payments for patients provided with uninsured discounts exceeded the computed cost for charity care, in contradiction of what providers actually experience. (For example, some hospitals believed the expected payment amount would usually become bad debt in a future cost report.) Commenters also raised a concern that sizeable adjustments to the uncompensated care costs reported by a hospital were often based on extrapolations from small samples of hospital data.
Despite these perceived audit-related concerns and issues, many commenters were supportive of CMS' efforts in the continued auditing of Worksheet S-10 data and applauded the efforts to improve the data accuracy and integrity. Many commenters also recommended auditing the FY 2017 Worksheet S-10 data for use in FY 2021 rulemaking. Commenters also provided recommendations for future audits. They suggested that CMS audit all hospitals and utilize a single auditor, or at least establish and enforce a formal and uniform audit process, similar to the desk reviews conducted for the purposes of the wage index. Commenters requested that the standardized audit process include standardized timelines for information submission with adequate lead time, standardized documentation to meet information requirements, and adequate communication about expectations. Several commenters also urged CMS to consider targeting specific data elements, reducing the scope of the audits to reduce the burden placed on providers, and making audit instructions publicly available to improve accuracy in reporting and make the interpretation of audit guidelines by the MACs and providers more consistent. These commenters claimed that not making audit instructions public only results in the various MACs and providers taking different interpretations of CMS audit guidance, which results in inconsistent reporting.
In addition, some commenters requested that CMS make public the results of the audits of the FY 2015 Worksheet S-10 data so that all providers might benefit from the lessons learned. Other commenters suggested using findings from the audits to develop outreach and educational materials for providers. Some commenters requested that CMS provide examples of acceptable language for financial assistance policies to increase the reliability of provider reporting and MAC review, in light of the adjustments that have been made as a result of MAC interpretation of language in some hospitals' financial assistance policies.
Many commenters, particularly those that believed that claims sampling, extrapolations, determination of adjustments, and the impact of adjustments were different across hospitals subject to review of the FY 2015 Worksheet S-10 data, recommended that CMS consider statistical relevance and apply standard extrapolation in finding thresholds to ensure audit consistency across all providers.
Finally, a number of commenters expressed the need for an appeals process and recommended the use of an experienced third party to mediate audit adjustment disputes.
Response: We thank commenters for their feedback on the audits of the FY 2015 Worksheet S-10 data. As we stated in the FY 2019 IPPS/LTCH PPS final rule, due to the overwhelming feedback from commenters emphasizing the importance of audits in ensuring the accuracy and consistency of data reported on the Worksheet S-10, we expected audits of the Worksheet S-10 to begin in the Fall of 2018. The audit protocol instructions were still under development at the time of the FY 2019 IPPS/LTCH PPS final rule; yet, we noted the audit protocols would be provided to the MACs in advance of the audit. Once the audit protocol instructions were complete, we began auditing the Worksheet S-10 data for selected hospitals in the Fall of 2018 so that the audited uncompensated care data from these hospitals would be available in time for use in the FY 2020 proposed rule. As discussed in the FY 2020 IPPS/LTCH PPS proposed rule, we chose to audit 1 year of data (that is, FY 2015) in order to maximize the available audit resources and not spread those audit resources over multiple years, potentially diluting their effectiveness. At that time, the FY 2016 Worksheet S-10 data and the FY 2017 Worksheet S-10 data were incomplete, as not all providers would necessarily have submitted those cost reports. We therefore chose to focus the audit on the FY 2015 cost reports primarily because this was the most recent year of data that we had broadly allowed to be resubmitted by hospitals, and many hospitals had already made considerable efforts to amend their FY 2015 reports prior to their use for the FY 2019 rulemaking. We also considered that we had previously used the FY 2015 data as part of the calculation of the FY 2019 uncompensated care payments; therefore, the data had previously been subject to public comment and scrutiny. We note again that, while limited resources meant that auditing all hospitals was not feasible, the proposed uncompensated care payments to hospitals whose FY 2015 Worksheet S-10 data were audited represented a significant portion (approximately half) of the total proposed uncompensated care payments for FY 2020. As a result, we have more confidence in the accuracy of the FY 2015 data, as a whole, from the combined efforts from hospitals, who may not have been part of audit selection but resubmitted cost reports, as well as the results of the audits of the FY 2015 reports, in contrast to the data for later years which have not yet been audited, at this time.
As acknowledged by some commenters, we believe that the audits of the FY 2015 Worksheet S-10 data have resulted in improvements to the accuracy and integrity of reported hospital uncompensated care costs. We acknowledge that some hospitals have raised concerns with the audit process for Worksheet S-10 of the FY 2015 cost reports. With respect to the comments raising concerns regarding the timeframe of audits, it is not generally possible for providers to have extensions for additional time, during the audit process, as that would lead to excessive administrative inefficiencies and potentially delay the timeline for completing the audits across all audited providers. We strive for increased standardization as MACs continue to gain experience with these audits. Regarding the adjustments made by MACs during audits, when a provider has no documentation or insufficient documentation to support the information reported on its Worksheet S-10, then the MAC must adjust the information reported on the applicable lines to reflect only those uncompensated care costs that can be documented. This approach is necessary in order to be equitable to other hospitals that did maintain adequate documentation to support their reported uncompensated care information.
Regarding comments on the instructions for reporting on the Worksheet S-10 in effect for FY 2015, especially compared to the reporting instructions that were effective for cost reporting periods beginning on or after October 1, 2016, and how some of the FY 2015 report adjustments would not have been necessary if CMS had chosen as an alternative to audit the FY 2017 reports, we recognize that there were many comments and suggestions on the cost report instructions and/or auditing process of Worksheet S-10 data for FY 2015 reports. CMS strives to use the lessons learned from the audits of the FY 2015 data to improve the instructions and/or audits of Worksheet S-10 data in the future. For example, in recognition of the importance of additional audits and to allow for additional lead time, the audits of the FY 2017 Worksheet S-10 data have already begun and are currently in progress.
Regarding commenters' requests that CMS release the audit instructions, as noted in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56964), we stated that we do not make the MACs' review protocol public, as all CMS desk review and audit protocols are confidential and are for CMS and MAC use only. However, we will continue to work with stakeholders to address their concerns regarding the accuracy and consistency of data reported on the Worksheet S-10 through provider education and further refinement of the instructions for the Worksheet S-10 as appropriate. Regarding the comments requesting that we establish an appeal process, we note that for the reasons discussed previously, we have confidence in the reviews of FY 2015 reports. Moreover, we believe that the audit process will continue to improve. As a result, we do not believe, on balance, that the creation of an appeals process justifies an additional delay in the use of an entire year's Worksheet S-10 data at this time. We may consider this topic further in the future as we gain more experience with the use of Worksheet S-10 data in determining uncompensated care payments.
After consideration of the public comments we received, we are finalizing our proposal to use the FY 2015 Worksheet S-10 cost report data in the methodology of Factor 3, as discussed further in later sections.
(b) Alternative Considered to Use FY 2017 Data
Although we proposed to use Worksheet S-10 data from the FY 2015 cost reports, in the proposed rule we acknowledged that some hospitals raised concerns regarding some of the adjustments made to the FY 2015 cost reports following the audits of these reports (for example, adjustments made to Line 22 of Worksheet S-10). These hospitals contend that there are issues regarding the instructions in effect for FY 2015, especially compared to the reporting instructions that were effective for cost reporting periods beginning on or after October 1, 2016, and certain adjustments would not have been made if CMS had chosen as an alternative to audit the FY 2017 reports.
Accordingly, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19419), we sought public comments on whether the changes in the reporting instructions between the FY 2015 cost reports and the FY 2017 cost reports have resulted in a better common understanding among hospitals of how to report uncompensated care costs and improved relative consistency and accuracy across hospitals in reporting these costs. We also sought public comments on whether, due to the changes in the reporting instructions, we should use a single year of uncompensated care cost data from the FY 2017 reports, instead of the FY 2015 reports, to calculate Factor 3 for FY 2020. We note that we did not propose to use FY 2016 reports because the reporting instructions for that year were similar to the reporting instructions for the FY 2015 reports. In the proposed rule, we stated that if, based on the public comments received, we were to adopt a final policy in which we use Worksheet S-10 data from the FY 2017 cost reports to determine Factor 3 for FY 2020, we would also expect to use the March 2019 update of HCRIS for the final rule.
Under the alternative on which we sought public comment, the FY 2017 Worksheet S-10 data would be used instead of the FY 2015 Worksheet S-10 data, but, in general, the proposed Factor 3 methodology would be unchanged. In the proposed rule, we explained that the limited circumstances where the methodology would need to differ from the proposed methodology using FY 2015 data, if we were to adopt the alternative of using FY 2017 data in the final rule based on the public comments received, were outlined in section IV.F.4.c.(3)(d) of the preamble of the proposed rule (Methodological Considerations for Calculating Factor 3). We specified that if an aspect of the proposed methodology did not specifically indicate that we would modify it under the alternative considered, that aspect of the methodology would be unchanged, regardless of whether we were to use FY 2015 data or FY 2017 data. We note that in the proposed rule we provided all of the same public information regarding the alternative considered, including the Factor 3 values for each hospital and the impact information, that we provided for our proposal to use FY 2015 data.
Comment: Many commenters who opposed the use of FY 2015 Worksheet S-10 data supported the use of the alternative approach of using FY 2017 Worksheet S-10 data to determine Factor 3 for FY 2020. In general, supporters of the alternative policy believe that the increased clarity in the cost reporting instructions in place for the FY 2017 Worksheet S-10 outweighs the benefit derived from the audit work performed on a subset of the FY 2015 data. These commenters believe that FY 2017 Worksheet S-10 data were reported based on revised and improved instructions established through Transmittal 11, which some commenters indicated were easier to follow and improved providers' reporting of UCC. Specifically, commenters stated that the new instructions to report charity care based on write-off dates, consistent with reporting of bad debt based write-off dates, are less confusing and use hospital financial data that are more commonly available to hospital personnel. These commenters provided analyses which indicated that there are fewer reporting errors using the FY 2017 Worksheet S-10 instructions than the FY 2015 Worksheet S-10 instructions, in particular regarding reporting of high amounts of charity care coinsurance and deductibles. Specifically, a commenter asserted that fewer hospitals reported coinsurance and deductible amounts greater than 25 percent of total charity care charges on the FY 2017 Worksheet S-10 than on the FY 2015 Worksheet S-10. Other commenters believe that using data from the FY 2017 Worksheet S-10 would better address the issue of data lag, which could be a concern with the FY 2015 data.
In contrast, other commenters stated that FY 2017 Worksheet S-10 data may benefit from improvements in cost reporting instructions but with unknown precision. That is, the commenters stated that the FY 2017 data have not yet been audited, pointed to analyses that identify cases in which hospitals' uncompensated care costs account for more than 50 percent of their total operating expenses, and suggested that these data aberrancies indicate that the use of unaudited data is not appropriate. Furthermore, these commenters stated that there is no indication that providers whose FY 2015 Worksheet S-10 data were not audited would have been given the guidance necessary to improve the accuracy of their FY 2017 data, nor is there any indication that providers whose FY 2015 data were audited had the time to make corrections when filing their FY 2017 cost reports. Furthermore, a commenter expressed concern that the instructions for Worksheet S-10 had changed for FY 2017 in a way that created an incentive for hospitals to inflate charges, while other commenters stated that implementing new instructions is problematic as a general matter, as providers have varied interpretations of how to report data every time instructions change.
Some commenters further reflected that the Worksheet S-10 instructions have been revised several times in the last few years, and so the use of data from the FY 2017 Worksheet S-10 should be delayed until there are final and consistent instructions and the data have been reviewed. These commenters pointed specifically to problems with the reporting of coinsurance and deductibles in FY 2017, as well as significant increases in uncompensated care costs for some hospitals between FY 2015 and FY 2017. The commenters believe that these problems provide an example of the residual misreporting of data that remains even after the issuance of improved cost reporting instructions for FY 2017. Furthermore, commenters stated that only trims and some recent requests to some hospitals for additional information regarding potentially aberrant data had occurred for the FY 2017 data, and it was unclear to the commenters whether CMS would receive a timely response to these requests for use as part of this rulemaking. However, many commenters believed that the FY 2017 Worksheet S-10 data, once audited, would be appropriate for use in calculating Factor 3. These commenters recommended that CMS begin the auditing process as soon as possible and incorporate audited FY 2017 data into the methodology for FY 2021.
Response: We appreciate the input from commenters who expressed their support for the alternative policy of using the FY 2017 Worksheet S-10 data to determine each hospital's share of UCC in FY 2020. As noted in the FY 2019 IPPS/LTCH PPS final rule, on September 29, 2017, we issued Transmittal 11, which clarified the definitions and instructions for reporting uncompensated care, non-Medicare bad debt, non-reimbursed Medicare bad debt, and charity care, as well as modified the calculations relative to uncompensated care costs and added edits to improve the integrity of the data reported on Worksheet S-10. We agree that these revisions have improved the reporting of uncompensated care costs. However, due to the feedback from commenters in response to last year's proposed rule and also in response to the FY 2020 IPPS/LTCH PPS proposed rule, emphasizing the importance of audits in ensuring the accuracy and consistency of data reported on the Worksheet S-10, we believe that the FY 2017 Worksheet S-10 data should be audited before they are used in determining Factor 3. To this end, we began auditing the FY 2017 Worksheet S-10 data in July 2019, with the goal having the FY 2017 audited data available for future rulemaking.
(c) Definition of “Uncompensated Care”
We continue to believe that the definition of “uncompensated care” first adopted in FY 2018 when we started to incorporate data from Worksheet S-10 into the determination of Factor 3 and used again in FY 2019 is appropriate, as it incorporates the most commonly used factors within uncompensated care as reported by stakeholders, namely, charity care costs and bad debt costs, and correlates to Line 30 of Worksheet S-10. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19419), we proposed that, for purposes of determining uncompensated care costs and calculating Factor 3 for FY 2020, “uncompensated care” would continue to be defined as the amount on Line 30 of Worksheet S-10, which is the cost of charity care (Line 23) and the cost of non-Medicare bad debt and non-reimbursable Medicare bad debt (Line 29).
Comment: Several commenters supported the proposed definition of uncompensated care as charity care plus non-Medicare bad debt and non-reimbursable Medicare bad debt. However, as in the past, some commenters suggested that uncompensated care should include shortfalls from Medicaid, CHIP, and State and local indigent care programs, as the commenters believed these inclusions would make the distribution of uncompensated care payments more equitable. As a result, several of these commenters urged CMS to use Worksheet S-10, Line 31 to identify a hospital's share of uncompensated care costs rather than Line 30, as Line 31 includes Medicaid unreimbursed costs. The commenters stated that the purpose of uncompensated care payments is to partially subsidize unmet costs for treating low-income patients and the exclusion of Medicaid shortfalls exacerbates the problems faced by hospitals in states with lower Medicaid rates and locks in financing inequities that currently exist.
Furthermore, commenters stated their view that excluding Medicaid shortfalls from the definition of uncompensated care severely penalizes hospitals that care for large numbers of Medicaid patients because many States do not fully cover the costs associated with newly insured Medicaid recipients. Commenters believed that patients covered by Medicaid may still have uncompensated care costs. Some commenters believe that under the proposed policy, which did not include Medicaid shortfalls in the definition of uncompensated care costs, Medicare would significantly subsidize those States with Medicaid payment rates that cover the cost of care relative to those with lower Medicaid payment rates that do not cover the cost of care. The commenters indicated that this concern is further compounded if a state has higher Medicaid enrollment either because it has expanded its Medicaid program under the Affordable Care Act, has more permissive Medicaid eligibility criteria, or simply has a high proportion of its citizens that qualify for Medicaid. Finally, some commenters believed that Worksheet S-10 provides an incomplete picture of Medicaid shortfalls and should be revised to instruct hospitals to deduct inter-governmental transfers, certified public expenditures, and provider taxes from their Medicaid revenue.
Response: In response to the comments regarding Medicaid shortfalls, we recognize commenters' concerns but continue to believe there are compelling arguments for excluding Medicaid shortfalls from the definition of uncompensated care, including the fact that several key stakeholders, such as MedPAC, do not consider Medicaid shortfalls in their definition of uncompensated care, and that it is most consistent with section 1886(r)(2) of the Act for Medicare uncompensated care payments to target hospitals that incur a disproportionate share of uncompensated care for patients with no insurance coverage. Conceptual issues aside, we note that even if we were to adjust the definition of uncompensated care to include Medicaid shortfalls, this would not be a feasible option at this time due to computational limitations. Specifically, computing such shortfalls is operationally problematic because Medicaid pays hospitals a single DSH payment that in part covers the hospital's costs in providing care to the uninsured and in part covers estimates of the Medicaid “shortfalls.” Therefore, it is not clear how CMS would determine how much of the “shortfall” is left after the Medicaid DSH payment is made. In addition, in some States, hospitals return a portion of their Medicaid revenues to the State via provider taxes, making the computation of “shortfalls” even more complex.
We refer readers to the next section for our responses to additional comments on the Worksheet S-10 cost report instructions. In general, we will attempt to address commenters' concerns through future cost report clarifications to further improve and refine the information that is reported on Worksheet S-10 in order to support collection of the information necessary to implement section 1886(r)(2) of the Act.
Accordingly, after consideration of the public comments we received and for the reasons discussed in the proposed rule and previously in this final rule, we are finalizing our proposal to define uncompensated care costs as the amount on Line 30 of Worksheet S-10, which is the cost of charity care (Line 23) and the cost of non-Medicare bad debt and non-reimbursable Medicare bad debt (Line 29).
(d) Methodological Considerations for Calculating Factor 3
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19419 through 19422), we proposed to continue the merger policies that were finalized in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50020). In addition, we proposed to continue the policy that was finalized in the FY 2018 IPPS/LTCH PPS final rule of annualizing uncompensated care cost data reported on the Worksheet S-10 if a hospital's cost report does not equal 12 months of data.
We proposed to modify the new hospital policy first adopted in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50643) and continued through the FY 2019 IPPS/LTCH PPS final rule (83 FR 41417), for new hospitals that do not have data for the cost reporting period(s) used in the proposed Factor 3 calculation. As we discussed in the proposed rule, for FY 2020, new hospitals that are projected to be eligible for Medicare DSH will receive interim empirically justified DSH payments. Generally, new hospitals do not yet have available data to project their eligibility for DSH payments because there is a lag until the SSI ratio and the Medicaid ratio become available. However, we noted that there are some new hospitals (that is, hospitals with CCNs established after October 1, 2015) that have a preliminary projection of being eligible for DSH payments based on their most recent available DSH percentages. Because these hospitals do not have a FY 2015 cost report to use in the Factor 3 calculation and the projection of eligibility for DSH payments is still preliminary, we proposed that the MAC would make a final determination concerning whether the hospital is eligible to receive Medicare DSH payments at cost report settlement based on its FY 2020 cost report. We stated if the hospital is ultimately determined to be eligible for Medicare DSH payments for FY 2020, the hospital would receive an uncompensated care payment calculated using a Factor 3, where the numerator is the uncompensated care costs reported on Worksheet S-10 of the hospital's FY 2020 cost report, and the denominator is the sum of the uncompensated care costs reported on Worksheet S-10 of the FY 2015 cost reports for all DSH-eligible hospitals. This denominator would be the same denominator that is determined prospectively for purposes of determining Factor 3 for all DSH-eligible hospitals, excluding Puerto Rico hospitals and Indian Health Service and Tribal hospitals. The new hospital would not receive interim uncompensated care payments before cost report settlement because we would have no FY 2015 uncompensated care data on which to determine what those interim payments should be. We noted that, given the time period of the data we proposed to use to calculate Factor 3, any hospitals with a CCN established on or after October 1, 2015, would be considered new and subject to this policy. However, we stated that under the alternative policy considered of using FY 2017 data, we would modify the new hospital policy, such that any hospital with a CCN established on or after October 1, 2017, would be considered new and subject to this policy with conforming changes to provide for the use of FY 2017 uncompensated care data.
As discussed in the proposed rule, we have received questions regarding the new hospital policy for new Puerto Rico hospitals. In FY 2018 and FY 2019, Factor 3 for all Puerto Rico hospitals, including new Puerto Rico hospitals, was based on the low-income insured proxy data. Under this approach, the MAC will calculate a Factor 3 for new Puerto Rico hospitals at cost report settlement for the applicable fiscal year using the Medicaid days from the hospital's cost report and the SSI day proxy (that is, 14 percent of the hospital's Medicaid days) divided by the low-income insured proxy data denominator that was established for that fiscal year. For FY 2020, we proposed that Puerto Rico hospitals that do not have a FY 2013 report would be considered new hospitals and would be subject to the proposed new hospital policy, as previously discussed. Specifically, the numerator would be the uncompensated care costs reported on Worksheet S-10 of the hospital's FY 2020 cost report and the denominator would be the same denominator that is determined prospectively for purposes of determining Factor 3 for all DSH-eligible hospitals. As we stated in the proposed rule, we believe the notice of our intent in the proposed rule will provide sufficient time for all new Puerto Rico hospitals to take the steps necessary to ensure that their uncompensated care costs for FY 2020 are accurately reported on their FY 2020 Worksheet S-10. In addition, we indicated that we expect MACs to review FY 2020 reports from new hospitals, as necessary, which will address past commenters' concerns regarding the need for further review of Puerto Rico hospitals' uncompensated care data before the data are used to determine Factor 3. Therefore, we stated our belief that the uncompensated care costs reported on the FY 2020 Worksheet S-10 for new Puerto Rico hospitals are the best available and most appropriate data to use to calculate Factor 3 for these hospitals. We indicated this proposal would also allow our new hospital policy to be more uniform, given that Worksheet S-10 would be the source of the uncompensated care cost data across all new hospitals.
For Indian Health Service and Tribal hospitals and subsection (d) Puerto Rico hospitals that have a FY 2013 cost report, we proposed to adapt the policy first adopted for the FY 2018 rulemaking regarding FY 2013 low-income insured days when determining Factor 3. As we discussed in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38209), the use of data from Worksheet S-10 to calculate the uncompensated care amount for Indian Health Service and Tribal hospitals may jeopardize these hospitals' uncompensated care payments due to their unique funding structure. With respect to Puerto Rico hospitals that would not be subject to the proposed new hospital policy, we explained that we continue to agree with concerns raised by commenters that the uncompensated care data reported by these hospitals need to be further examined before the data are used to determine Factor 3. Accordingly, for these hospitals, we proposed to determine Factor 3 based on Medicaid days from FY 2013 and the most recent update of SSI days. The aggregate amount of uncompensated care that is used in the Factor 3 denominator for these hospitals would continue to be based on the low-income patient proxy; that is, the aggregate amount of uncompensated care determined for all DSH eligible hospitals using the low-income insured days proxy. We indicated that we believe this approach is appropriate because the FY 2013 data reflect the most recent available information regarding these hospitals' Medicaid days before any expansion of Medicaid. At the time of development of the proposed rule, for modeling purposes, we computed Factor 3 for these hospitals using FY 2013 Medicaid days and the most recent available FY 2017 SSI days. In addition, because we proposed to continue to use 1 year of insured low-income patient days as a proxy for uncompensated care for Puerto Rico hospitals and residents of Puerto Rico are not eligible for SSI benefits, we proposed to continue to use a proxy for SSI days for Puerto Rico hospitals, consisting of 14 percent of a hospital's Medicaid days, as finalized in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56953 through 56956).
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41417), we noted that further examination of the CCRs for all-inclusive rate providers was necessary before we considered incorporating Worksheet S-10 into the Factor 3 calculation for these hospitals. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19420), we stated that we had examined the CCRs from the FY 2015 cost reports and believe the risk that all-inclusive rate providers will have aberrant CCRs and, consequently, aberrant uncompensated care data, is mitigated by the proposal to apply trim methodologies for potentially aberrant uncompensated care costs for all hospitals. Therefore, we stated that we believe it is no longer necessary to propose specific Factor 3 policies for all-inclusive rate providers.
As discussed in the proposed rule, because we proposed to use 1 year of cost report data, as opposed to averaging 3 cost report years, it is also no longer necessary to propose to apply a scaling factor to the Factor 3 of all DSH eligible hospitals similar to the scaling factor that was finalized in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38214) and also applied in the FY 2019 IPPS/LTCH PPS final rule. The primary purpose of the scaling factor was to account for the averaging effect of the use of 3 years of data on the Factor 3 calculation.
However, in the FY 2020 IPPS/LTCH PPS proposed rule, we did propose to continue certain other policies finalized in the FY 2019 IPPS/LTCH PPS final rule, specifically: (1) For providers with multiple cost reports, beginning in the same fiscal year, using the longest cost report and annualizing Medicaid data and uncompensated care data if a hospital's cost report does not equal 12 months of data; (2) in the rare case where a provider has multiple cost reports, beginning in the same fiscal year, but one report also spans the entirety of the following fiscal year, such that the hospital has no cost report for that fiscal year, using the cost report that spans both fiscal years for the latter fiscal year; and (3) applying statistical trim methodologies to potentially aberrant CCRs and potentially aberrant uncompensated care costs reported on the Worksheet S-10. Thus, if a hospital's uncompensated care costs for FY 2015 are an extremely high ratio of its total operating costs, and the hospital cannot justify the amount it reported, we proposed to determine the ratio of uncompensated care costs to the hospital's total operating costs from another available cost report, and apply that ratio to the total operating expenses for the potentially aberrant fiscal year to determine an adjusted amount of uncompensated care costs. For example, if the FY 2015 cost report is determined to include potentially aberrant data, data from the FY 2016 cost report would be used for the ratio calculation. In this case, similar to the trim methodology used for FY 2019, the hospital's uncompensated care costs for FY 2015 would be trimmed by multiplying its FY 2015 total operating costs by the ratio of uncompensated care costs to total operating costs from the hospital's FY 2016 cost report to calculate an estimate of the hospital's uncompensated care costs for FY 2015 for purposes of determining Factor 3 for FY 2020.
In support of the alternative policy considered of using uncompensated care data from FY 2017 and to improve the quality of the Worksheet S-10 data generally, we explained in the proposed rule that we were then in the process of outreach to hospitals related to potentially aberrant data reported in their FY 2017 cost reports. For example, a significant positive or negative difference in the percent of total uncompensated care costs to total operating costs when comparing the hospital's FY 2015 cost report to its FY 2017 cost report may indicate potentially aberrant data. While hospitals may have uncompensated care cost fluctuations from year to year, if a hospital experiences a significant change compared to other comparable hospitals, this could be an indication of potentially aberrant data. A hospital with such changes would have the opportunity to justify its reporting fluctuation to the MAC and, if necessary, to amend its FY 2017 cost report. If a hospital's FY 2017 cost report remains unchanged without an acceptable response or explanation from the provider, under the alternative policy considered, we stated we would trim the data in the provider's FY 2017 cost report using data from the provider's FY 2015 cost report in order to determine Factor 3 for purposes of the final rule.
We stated in the proposed rule that while we expect all providers will have FY 2017 cost reports in HCRIS by the time that any data would be taken from HCRIS for the final rule, if such data are not reflected in HCRIS for an unforeseen reason unrelated to any inappropriate action or improper reporting on the part of the hospital, we would substitute the Worksheet S-10 data from its FY 2015 cost report for the data from the FY 2017 cost report.
Similar to the process used in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38217 through 38218) and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41415 and 41416) for trimming CCRs, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19421 through 19422), we proposed the following steps:
Step 1: Remove Maryland hospitals. In addition, we would remove all-inclusive rate providers because their CCRs are not comparable to the CCRs calculated for other IPPS hospitals.
Step 2: For FY 2015 cost reports, calculate a CCR “ceiling” with the following data: For each IPPS hospital that was not removed in Step 1 (including non-DSH eligible hospitals), we would use cost report data to calculate a CCR by dividing the total costs on Worksheet C, Part I, Line 202, Column 3 by the charges reported on Worksheet C, Part I, Line 202, Column 8. (Combining data from multiple cost reports from the same fiscal year is not necessary, as the longer cost report would be selected.) The ceiling would be calculated as 3 standard deviations above the national geometric mean CCR for the applicable fiscal year. This approach is consistent with the methodology for calculating the CCR ceiling used for high-cost outliers. Remove all hospitals that exceed the ceiling so that these aberrant CCRs do not skew the calculation of the statewide average CCR. (For the proposed rule, this trim would have removed 8 hospitals that have a CCR above the calculated ceiling of 0.925 for FY 2015 cost reports.) (Under the alternative policy considered, the trim would have removed 13 hospitals that have a CCR above the calculated ceiling of 0.942 for FY 2017 cost reports.)
Step 3: Using the CCRs for the remaining hospitals in Step 2, determine the urban and rural statewide average CCRs for FY 2015 for hospitals within each State (including non-DSH eligible hospitals), weighted by the sum of total inpatient discharges and outpatient visits from Worksheet S-3, Part I, Line 14, Column 14.
Step 4: Assign the appropriate statewide average CCR (urban or rural) calculated in Step 3 to all hospitals, excluding all-inclusive rate providers, with a CCR for FY 2015 greater than 3 standard deviations above the national geometric mean for that fiscal year (that is, the CCR “ceiling”). For the proposed rule, the statewide average CCR would therefore have been applied to 8 hospitals, of which 4 hospitals had FY 2015 Worksheet S-10 data. (Under the alternative policy considered, the statewide average CCR would have been applied to 13 hospitals, of which 5 hospitals had FY 2017 Worksheet S-10 data.). We note that in the proposed rule, we inadvertently omitted the information noted earlier regarding the exclusion of all-inclusive rate providers from this calculation, but have corrected this omission in the description of Step 4 in this final rule to clarify that the CCR trim methodology excludes all-inclusive rate providers.
For providers that did not report a CCR on Worksheet S-10, Line 1, we would assign them the statewide average CCR in step 4.
After applying the applicable trims to a hospital's CCR as appropriate, we proposed that we would calculate a hospital's uncompensated care costs for the applicable fiscal year as being equal to Line 30, which is the sum of Line 23, Column 3, and Line 29 determined using the hospital's CCR or the statewide average CCR (urban or rural), if applicable.
Therefore, for FY 2020, we proposed to compute Factor 3 for each hospital by—
Step 1: Selecting the provider's longest cost report from its Federal fiscal year (FFY) 2015 cost reports. (Alternatively, in the rare case when the provider has no FFY 2015 cost report because the cost report for the previous Federal fiscal year spanned the FFY 2015 time period, the previous Federal fiscal year cost report would be used in this step.)
Step 2: Annualizing the uncompensated care costs (UCC) from Worksheet S-10 Line 30, if the cost report is more than or less than 12 months. (If applicable, use the statewide average CCR (urban or rural) to calculate uncompensated care costs.)
Step 3: Combining annualized uncompensated care costs for hospitals that merged.
Step 4: Calculating Factor 3 for Indian Health Service and Tribal hospitals and Puerto Rico hospitals using the low-income insured days proxy based on FY 2013 cost report data and the most recent available SSI ratio (or, for Puerto Rico hospitals, 14 percent of the hospital's FY 2013 Medicaid days). The denominator is calculated using the low-income insured days proxy data from all DSH eligible hospitals.
Step 5: Calculating Factor 3 for the remaining DSH eligible hospitals using annualized uncompensated care costs (Worksheet S-10 Line 30) based on FY 2015 cost report data (from Step 3). The hospitals for which Factor 3 was calculated in Step 4 are excluded from this calculation.
We also proposed to amend the regulations at § 412.106(g)(1)(iii)(C) by adding a new paragraph (6) to reflect the proposed methodology for computing Factor 3 for FY 2020.
In the FY 2020 IPPS/LTCH PPS proposed rule, we proposed that if a hospital does not have Worksheet S-10 data for FY 2015 and the hospital is not a new hospital (that is, its CCN was established before October 1, 2015) nor has the rare case of no FY 2015 cost report, we would apply the steps as previously discussed with uncompensated care costs of zero for the hospital. In addition, if, in the course of the Worksheet S-10 reviews by MACs, a hospital is unable to provide sufficient documentation or is unwilling to justify its cost report, which subsequently results in the hospital's Worksheet S-10 being adjusted to zero, we also proposed to use the previously discussed steps to calculate Factor 3. We recognized that, under this proposal, these hospitals would be treated as having reported no uncompensated care costs on the Worksheet S-10 for FY 2015, which would result in their not receiving uncompensated care payments for FY 2020. However, we explained our belief that this proposal would be equitable to other hospitals because all short-term acute care hospitals are required to report Worksheet S-10 and must maintain sufficient documentation to support the information reported. In addition, we noted that hospitals have been on notice since the beginning of FY 2014 that Worksheet S-10 could eventually become the data source for CMS to calculate uncompensated care payments. Furthermore, we have previously given hospitals the opportunity to amend their Worksheet S-10 for FY 2015 cost reports (or to submit a Worksheet S-10 for FY 2015 if none had been submitted previously).
As we have done for every proposed and final rule beginning in FY 2014, we stated that in conjunction with both the FY 2020 IPPS/LTCH PPS proposed rule and final rule, we will publish on the CMS website a table listing Factor 3 for all hospitals that we estimate would receive empirically justified Medicare DSH payments in FY 2020 (that is, those hospitals that would receive interim uncompensated care payments during the fiscal year), and for the remaining subsection (d) hospitals and subsection (d) Puerto Rico hospitals that have the potential of receiving a Medicare DSH payment in the event that they receive an empirically justified Medicare DSH payment for the fiscal year as determined at cost report settlement. For purposes of the proposed rule, the table published on the CMS website included Factor 3 computed using both the proposed methodology and the potential alternative methodology. We noted that, at the time of development of the proposed rule, the FY 2017 SSI ratios were available. Accordingly, for purposes of the proposed rule, we computed Factor 3 for Indian Health Service and Tribal hospitals and Puerto Rico hospitals using the most recent available data regarding SSI days from the FY 2017 SSI ratios. We stated that we would also publish in the supplemental data file a list of the mergers that we were aware of and the computed uncompensated care payment for each merged hospital.
Hospitals had 60 days from the date of public display of the FY 2020 IPPS/LTCH PPS proposed rule to review the table and supplemental data file published on the CMS website in conjunction with the proposed rule and to notify CMS in writing of any inaccuracies. We stated that comments that are specific to the information included in the table and supplemental data file could be submitted to the CMS inbox at Section3133DSH@cms.hhs.gov. We indicated we would address these comments as appropriate in the table and the supplemental data file that we publish on the CMS website in conjunction with the publication of the FY 2020 IPPS/LTCH PPS final rule. After the publication of this FY 2020 IPPS/LTCH PPS final rule, hospitals will have until August 31, 2019, to review and submit comments on the accuracy of the table and supplemental data file published in conjunction with this final rule. Comments may be submitted to the CMS inbox at Section3133DSH@cms.hhs.gov through August 31, 2019, and any changes to Factor 3 will be posted on the CMS website prior to October 1, 2019.
We invited public comments on our proposed methodology for calculating Factor 3 for FY 2020, including, but not limited to, our proposed use of the FY 2015 Worksheet S-10 data and the alternative policy considered of using the FY 2017 Worksheet S-10 data instead of the FY 2015 Worksheet S-10 data.
We also note that, consistent with the policy adopted in FY 2014 and applied in each subsequent fiscal year, a 3-year average of discharges is used to produce an estimate of the amount of the uncompensated care payment per discharge. Specifically, the hospital's total uncompensated care payment amount from Factor 3, is divided by the hospital's historical 3-year average of discharges computed using most recent available data. The result of that calculation for each projected DSH eligible hospital is used to make interim uncompensated care payments through a per discharge payment amount. The interim uncompensated care payments made to the hospital during the fiscal year are reconciled following the end of the year to ensure that the final payment amount is consistent with the hospital's prospectively determined uncompensated care payment for the Federal fiscal year.
Comment: A commenter recommended that CMS apply a growth factor, such as the CBO's projected average monthly Part A fee-for-service enrollment, to the claims average in the FY 2020 proposed rule DSH Public Use File. The commenter notes that the 3-year discharge average, does not currently consider the growth of Medicare eligibility due to the aging of baby boomers since 2018. As a result, approximately 7.3-8 million new Medicare beneficiaries will be incurring additional inpatient claims by the end of FY 2020. To mitigate these risks, the commenter recommended CMS incorporate a growth factor designed to adjust for the increase in Medicare discharges caused by the growth in the number of Medicare eligible beneficiaries between 2018 and 2020 and apply this factor to the 3-year claims average for each hospital. The commenter stated that, in their view, discharge growth discrepancies create the risk of overpayments of uncompensated care payments and unstable cash flows for CMS, hospitals, and MA plans.
Response: We thank the commenter for their suggestions related to the 3-year discharge average. Although we did not propose any new policy related to determination of the discharge average for FY 2020, this is a topic we may consider in future rulemaking. For FY 2020, we will continue to calculate the interim uncompensated care payments on a per discharge basis using historical 3-year average of discharges without a growth factor. Consistent with the cost report settlement process that we have used since FY 2014, we note that a hospital's total amount of interim uncompensated care payments for the cost reporting period will be reconciled, in order to ensure consistency with the hospital's prospectively determined uncompensated care payment for the Federal fiscal year.
Comment: Some commenters recommended that CMS use the traditional payment reconciliation process to calculate final payments for uncompensated care costs pursuant to section 1886(r)(2) of the Act. In general, commenters did not object to CMS using prospective estimates, derived from the best data available, to calculate interim payments for uncompensated care costs in a Federal fiscal year after 2013. However, some commenters stated that these interim payments should be subject to later reconciliation based on estimates derived from actual data from the Federal fiscal year.
Response: Consistent with the position that we have taken in the rulemaking for previous years, we continue to believe that applying our best estimates prospectively is most conducive to administrative efficiency, finality, and predictability in payments (78 FR 50628; 79 FR 50010; 80 FR 49518; 81 FR 56949; and 82 FR 38195). We believe that, in affording the Secretary the discretion to estimate the three factors used to determine uncompensated care payments and by including a prohibition against administrative and judicial review of those estimates in section 1886(r)(3) of the Act, Congress recognized the importance of finality and predictability under a prospective payment system. As a result, we do not agree with the commenters' suggestion that we should establish a process for reconciling our estimates of uncompensated care payments, as this would be contrary to the overall framework of a prospective payment system like the IPPS.
The following comments relate to the Worksheet S-10 instructions:
Comment: Many commenters acknowledged the efforts CMS has taken to improve the guidance and the instructions for Worksheet S-10. Commenters commended the instructional clarifications implemented via Transmittals 10 and 11, and recognized that these improved instructions have allowed hospitals to better understand the intent of CMS' guidelines. In addition, some commenters stated that the information requested by auditors in reviewing the FY 2015 Worksheet S-10 data and the corresponding clarifications in the instructions have given facilities a better understanding of reporting requirements, which has led to more accurate reporting. Conversely, some commenters recognized that there are remaining issues with Worksheet S-10 and requested that CMS continue to revise the instructions to ensure additional clarity going forward.
Some commenters provided general suggestions to improve the Worksheet S-10 instructions. For example, several commenters urged CMS to implement fatal edits to ensure that the information reported on Worksheet S-10 is complete and internally consistent, and to instruct the MAC to audit negative, missing or suspicious information. A commenter requested that CMS provide further guidance regarding the Worksheet S-10 reporting requirements so as to avoid leaving the interpretation of the cost report instructions to the discretion of hospital reimbursement staff and/or MAC auditors, which would ultimately lead to inconsistent treatment of uncompensated care costs across hospitals. According to the commenter, CMS' clarification on this issue would also improve the comparability of uncompensated care cost data collected across hospitals. Similarly, another commenter noted that there remains hospital variation in the interpretation of a bad debt “write-off.” While the commenter recognized that all bad debt amounts should be net of recovery, in the absence a standard definition of what a “write-off” is, it is in the hands of individual provider accounting practices to arrive at such determination. Other commenters also requested that CMS release further clarification and guidance regarding its expectations as to what is charity care as opposed to other uncompensated care costs that may not match the spirit of the DSH program, and stated that this clarification is important as some providers may have an incentive to report other forms of cost as uncompensated care. Lastly, a commenter requested confirmation of whether the wording, “total facility, except physician and other professional services,” in relation to charity care and bad debt write-offs includes acute inpatient, exempt inpatient, outpatient, and long-term care services.
A few commenters stated that the instructions still need to be revised to clarify the issues that were addressed in the Worksheet S-10 Q&A issued following the FY 2018 final rule and in the audit protocols. To this end, a commenter asserted that several such issues, including expected patient payments and the definition of “uninsured,” were not included or clarified in Worksheet S-10 instructions nor, in the commenters' view, had CMS addressed these issues in rulemaking. A commenter specifically stated that one of the audit adjustments that was made during its audit was moving charity write-offs from Insured charity care in Worksheet S-10, Line 20, Column 2, to Uninsured charity care in Line 20, Column 1, when an insurance payment had not been made on the account. In this case, the commenter stated that definition of “uninsured” being used in Worksheet S-10 is different from the definition of “uninsured” that is used for the hospital-specific DSH limit at 42 CFR 447.295(c) which states that, “individuals who have no source of third party coverage for specific inpatient or outpatient hospital services must be considered, for purposes of that service, to be uninsured. This determination is not dependent on the receipt of payment by the hospital from the third party.”
Another area of concern raised by commenters was the potential for gaming of costs related to charity care and partial discounts. To ameliorate this problem, a commenter suggested that CMS develop more specific definitions of “uninsured” and “non-covered” in the reporting instructions as well as a standard format for providers to submit more detailed data about their charity care write-offs and non-Medicare bad debt. The commenter further stated that additional specificity could also be helpful in the determination of which costs are and are not allowable as part of future audits.
Some commenters also requested that CMS provide specific guidance, either regulatory or subregulatory, regarding the treatment of costs associated with patients insured under a third-party insurance. Commenters requested that CMS provide guidance both for patients with coverage from third-party companies that have a contractual relationship with the hospital, and patients with coverage from third-party companies that do not have a contractual relationship with the hospital. Commenters also requested clarification regarding the treatment of costs associated with patients that have a responsibility related to noncovered charges under a third-party insurance company, and patients covered under a catastrophic plan or limited benefit plan with a limited amount covered daily. A commenter posed questions regarding comprehensive examples of multiple coverage scenarios.
In addition to these concerns, many commenters had more specific suggestions, which would require column and line level modifications to Worksheet S-10. One of the most prevalent suggestions among commenters involved the application of the CCR to non-reimbursed Medicare bad debt and non-Medicare bad debt, which commenters classified as “unjustifiable” since Medicare bad debt and insured bad debt should be recorded at the full amount of the deductibles and/or coinsurance written-off. Specifically, commenters explained that applying a provider's CCR to Line 28 understates the cost of bad debt because “deductibles, coinsurances based on the negotiated payment rate, and the portion of allowable, non-reimbursable Medicare bad debt are not marked up to reflect the charged amount.” Given this, attempting to arrive at the cost of bad debt expense from “multiplying uncollectable deductibles, coinsurance based on the negotiated rate, and the portion of allowable Medicare bad debt that is non-reimbursable times a hospital's cost-to-charge ratio” is inappropriate and understates the “true cost of forgone revenue resulting from uncollectible accounts.” Commenters' general recommendation to resolve this issue was for CMS to create separate columns for insured and uninsured patients, with the column for “uninsured patients being multiplied by a hospital's cost-to-charge ratio to arrive at the cost of bad debt . . . and the column for insured patients (which should include amounts related to Medicare allowable, non-reimbursable bad debt) not being multiplied by the CCR.” In connection with these recommendations regarding the structure of Worksheet S-10, another commenter suggested that CMS add two new columns in the charity care section, before Column 2, so that hospitals can separately report charges subject to adjustment by the CCR (currently Line 25) and charges that are not subject to adjustment by the CCR. The commenter suggested similar changes to the bad debt section, creating two columns before the total column in which hospitals would separately report bad debt charges that should be adjusted by the CCR and bad debt write offs for cost-sharing that should not be multiplied by the CCR.
A topic broadly raised by commenters was the clarification of charity care, such as in the context of public programs, especially Medicaid, as well as third-party insurance. A commenter specifically requested clarification of which types of denials by state Medicaid FFS and managed care payers can be included as charity care, also asking if “charity care eligibility [can] be inferred by enrollment in Medicaid manage care plan?” The commenter also requested clarification of whether discounts or reductions to the standard managed care rate can be reported as charity care or an uninsured discount for patients who are eligible for discounts under a given hospital's charity care policy. In addition, the commenter sought clarification of the definition of “non-covered” charges related to days exceeding the length of stay limit and with respect to Medicare, Medicaid, Workers' Compensation/No Fault, and commercial plans with which the hospital has a contractual relationship, but for which it is not allowed to pursue patient collections for losses (for example unpaid claims). The commenter questioned whether a hospital is permitted to include such losses on Line 20 of Worksheet S-10, if it includes them in its financial assistance policy (FAP).
Several commenters perceived that there appears to be a general misunderstanding regarding non-covered Medicaid charges. A commenter pointed out that hospitals rely on different sources of information to report non-covered Medicaid services; for example, sources can primarily be patient transaction detail from hospital records or remittance advice (R/A) reports provided by Medicaid Fee for Service and Managed Care payers. The commenter believed that each source comes with a set of limitations, and stated it is important that the definition of uncompensated care for non-covered Medicaid services be further clarified. Given this, the commenter suggested that CMS provide definitive guidance to prevent inconsistent provider reporting of non-covered Medicaid charges, which can ultimately impact uncompensated care payment distributions.
A commenter specifically suggested that reporting charges from Medicaid days beyond the length of stay limit with insured patient coinsurance and deductibles may cause erroneous reporting (those three items are currently reported in Line 20 Column 2), such as when providers inadvertently do not report these same charges in Worksheet S-10 Line 25, where the CCR applies. According to the commenter, the instruction to report these charges on Worksheet S-10 Line 25 appears to be unnecessary; and they recommend that CMS could avoid misreporting of this information by requesting that providers report Medicaid days exceeding the length of stay limit with the rest of non-covered charges for Medicaid patients on Line 20 Column 1 to ensure the CCR is applied.
A commenter requested that CMS clarify recent guidance on Medicaid cross over bad debt and confirm the commenter's understanding regarding hospitals claiming Medicaid cross over bad debt for an unpaid Medicare deductible or coinsurance amount. The commenter stated that currently the deductible or coinsurance amount must be written-off to a bad debt expense account. According to the commenter, hospitals have historically written-off Medicare cross over bad debts to contractual allowance accounts because they considered these amounts an adjustment to the Medicaid allowed amount. Accordingly, the commenter perceived the CMS guidance on Medicare crossover bad debt as requiring hospitals to modify their own current patient account practices.
Finally, several commenters requested that CMS clarify whether there are implications for Worksheet S-10 from the recent Financial Accounting Standards Board Topic 606 on Medicare bad debt reporting.
Response: We appreciate commenters' concerns regarding the need for further clarification of the Worksheet S-10 instructions, as well as their suggestions on how to revise the form to continue improving provider reporting. As noted by some commenters, our continued efforts to refine the instructions and guidance have improved provider understanding of the Worksheet S-10. We also recognize that there are always continuing opportunities for further improvement, and to the extent that commenters have raised new questions and concerns, we will attempt to address them through future refinements to the Worksheet S-10 and the accompanying instructions. Nevertheless, we continue to believe that the Worksheet S-10 instructions are sufficiently clear to allow hospitals to accurately complete Worksheet S-10.
Regarding the commenter who referenced the Medicaid definition of “uninsured” used for purposes of the hospital-specific DSH limit at 42 CFR 447.295(c), we note the Medicare cost report instructions do not reference a Medicaid definition of uninsured patient.
As a general matter, hospitals have the discretion to design their charity care policies as they deem appropriate. However, we note that hospitals are not permitted to report Medicaid shortfalls (that is, situations where Medicaid payment is made for the patient care, but that reimbursement may be less than the actual cost of care or the billed amount) as charity care on line 20 column 1 or as bad debt on line 26, as that would not comply with the Worksheet S-10 cost reporting instructions nor the definition of uncompensated care we are adopting in this final rule and that has applied for every fiscal year starting with the FY 2014, even if under the hospitals' charity care policy a Medicaid shortfall would be considered charity care. We refer the reader to the earlier section for further discussion of the finalized definition of uncompensated care. In general, Medicaid patient charges should be reported on Worksheet S-10 line 6. However, charges for non-covered services provided to patients eligible for Medicaid or other indigent care programs may be reported on line 20, if such inclusion is specified in the hospital's charity care policy or FAP and the patient meets the hospital's charity care or FAP criteria. Additionally, non-covered charges for days exceeding a length-of-stay limit for patients covered by Medicaid or other indigent care program may be reported on line 25 and line 20 column 2, if such inclusion is specified in the hospital's charity care policy or FAP. We note a stay that exceeds the length-of-stay limit imposed on patients covered by Medicaid or other indigent care program does not mean a length of stay that just happens to be longer than an individual hospital's average length of stay, but is one that exceeds a Medicaid or other indigent care program's length of stay limit. In addition, a DRG-based Medicaid payment that is less than the cost of the services furnished to a Medicaid patient is considered a Medicaid shortfall and would not be for a non-covered service or charity care; therefore, the related charges must not be reported as charity care on line 20 column 1 of Worksheet S-10. As previously explained, a Medicaid shortfall, or a Medicaid contractual allowance, must not be re-characterized as charity care.
In conclusion, we note that the comments recommending structural changes to Worksheet S-10 fall outside the scope of this final rule. We therefore refer commenters to the forthcoming Paper Reduction Act (PRA) package for Form CMS 2552-10 approved OMB No. 0938-0050 expiring March 31, 2022. The forthcoming PRA package includes proposed changes to the Worksheet S-10 instructions, which will provide for a public comment period and is the appropriate forum for questions about and suggestions for modifications to Worksheet S-10.
Comment: Many commenters expressed concerns about the accuracy and integrity of the FY 2015 Worksheet S-10 data. A commenter noted that, for FY 2015, some hospitals incorrectly reported charity care transaction amounts based on write-off date, and that reporting of bad debts often duplicated charity care charges. The commenter stated that this duplication occurs because under the Worksheet S-10 instructions for FY 2015, charity care is reported as the total charge, while bad debt is reported as the write-off amount. This issue, according to the commenter, is not as prevalent in the FY 2017 data, because charity care is reported using a separate transaction (write-off) amount as opposed to total charges.
On a separate issue, a commenter asserted that in the FY 2015 Worksheet S-10 data, charity care amounts related to coinsurance and deductible amounts are overstated for more than 20 percent of eligible DSH hospitals. The commenter observed that in some cases, the overstating of such amounts can be attributed to the header in Worksheet S-10, Line 20, Column 2, which states, “Charity Care for Insured Patients.” Such description, according to the commenter, has caused several hospitals to inadvertently report other types of charges on this line, commonly for non-covered Medicaid services. The commenter noted that this issue has improved in the FY 2017 data due to increased provider education and cited analytic results in support of this notion. However, several commenters expressed concern regarding continued misreporting of coinsurance and deductibles in the FY 2017 Worksheet S-10. These commenters stated that it may be possible that the reported amounts of deductibles and coinsurance are excessive for some hospitals now that CMS has issued Transmittals 10 and 11, and the CCR is not being applied. Commenters provided analytic results which demonstrated an increase in the amounts of deductibles and coinsurance reported on the Worksheet S-10 between FY 2015 and FY 2017, as well as an increase in the number of hospitals reporting deductibles and coinsurance that exceeded the costs of uninsured patients. The commenter stated that the significant problems with reporting of deductibles and coinsurance in FY 2017 provide an example of continued misreporting of data, even after the issuance of improved cost reporting instructions for FY 2017.
Many commenters provided suggestions to enhance the accuracy and integrity of the Worksheet S-10 data. Several commenters urged that CMS continue its work to accurately capture hospital uncompensated care costs in its allocation of Medicare DSH payments. According to some commenters, this work could include providing ample opportunity for stakeholder feedback and education before issuing substantive revisions to Worksheet S-10, as well as conducting additional educational outreach to hospitals. A commenter encouraged CMS to invest resources in developing educational forums and opportunities for ongoing dialogue between CMS, MACs and hospitals prior to releasing significant revisions to guidance on cost report instructions. Commenters also suggested that CMS build infrastructure and look to the field for technology solutions, which could produce an industry standard for how data should be prepared and submitted to the MACs and CMS itself.
Response: We thank commenters for their continued concern and constructive feedback regarding the accuracy of Worksheet S-10 data. We believe that continued use of Worksheet S-10 will improve the accuracy and consistency of the reported data. In addition, we intend to continue with and further refine our efforts to review the Worksheet S-10 data submitted by hospitals based on what we have learned from the review and audit process we conducted for the FY 2020 rulemaking period. We also intend to consider the various issues raised by the commenters specifically related to the reporting of charity care and bad debt costs on Worksheet S-10 as we continue to review the Worksheet S-10 data.
We agree with commenters that continuing our ongoing educational effort is appropriate, including provider education that may occur during Worksheet S-10 reviews. We also appreciate the suggestions provided by commenters regarding areas for further education. We reiterate that we will continue the education efforts undertaken in the past as well as our collaboration with stakeholders to address their concerns regarding the accuracy and consistency of reporting of uncompensated care costs.
Comment: Several commenters urged CMS to allow hospitals to submit revisions to their cost reports in order to improve the accuracy of the data. Related to the FY 2015 Worksheet S-10 data, a commenter requested that CMS address and allow for corrections of what the commenter asserted were MAC adjustment errors made during the audits so that hospitals are allowed an opportunity to resubmit corrected Worksheet S-10 data in an expedited fashion for use in the final rule. The commenter stated that if CMS believes such corrected Worksheet S-10 data must be reviewed and/or approved before they can be used, then it must provide for an expedited review process that allows for high level agency review in order to overrule the MAC, and only permit disallowances to stand if applied consistently and uniformly to all providers.
Some commenters stated that CMS afforded hospitals several opportunities to improve FY 2015 data, but these opportunities have not been offered with respect to FY 2017 data. Commenters believe that many hospitals that might desire to reopen their FY 2017 cost report based on their FY 2015 audit findings have not had time to start that process. Finally, a commenter recommended that CMS indicate in the FY 2020 final rule that it intends to use FY 2017 Worksheet S-10 data to calculate uncompensated care payments for FY 2021 in order to provide sufficient notice to allow providers to begin amending their unaudited FY 2017 data before these data are used to determine payments.
Response: We acknowledge commenters' requests regarding the opportunity to resubmit cost reports for purposes of calculating FY 2020 uncompensated care payments. However, we do not agree that we should continue to offer hospitals multiple opportunities to amend their cost reports outside of the normal process. We expect a hospital to submit correct cost report data to its MAC and to use the normal timelines and procedures in place to amend its cost report, if appropriate. With respect to the commenter who recommended that we indicate in the FY 2020 final rule that we intend to use FY 2017 Worksheet S-10 data to calculate uncompensated care payments for FY 2021, we note that we will address proposed policies for FY 2021 in the FY 2021 IPPS/LTCH proposed rule.
Comment: Several commenters voiced concern that their most recent Worksheet S-10 data were not reflected in the data used for the proposed rule, and some were concerned that their most recent data would not be included in the final rule data file if CMS decides to use the March HCRIS extract, as proposed. For example, some commenters noted that the public use file from the proposed rule did not include audit adjustment reversals for the FY 2015 Worksheet S-10. Some commenters noted that because CMS had not given a directive as to the deadline for amending FY 2017 Worksheet S-10 data, many providers were still in the process of correcting their data and did not have enough time to submit the corrected data for use in the proposed rule, while other commenters stated that their amended cost report for FY 2017 had been accepted well after the cut-off for the proposed March HCRIS extract. Thus, commenters requested that CMS use the latest HCRIS extract possible, to allow providers and CMS to correct aberrant data identified for potential revision, as well as account for any hospital that voluntarily submitted Worksheet S-10 revisions. Some commenters attached copies of their updated Worksheet S-10 for CMS to consider on the record.
Response: We appreciate the commenters' diligence in checking that their own reports and data were properly processed. We recognize that some hospitals' data in the March HCRIS update may not have reflected all corrections and/or adjustments made to Worksheet S-10 data in response to our hospital outreach and auditing efforts. Given those circumstances and consistent with our historical practice of using the best data available, we are using a June 30, 2019 HCRIS extract, which is the most recent available data at the time of development of this final rule, to calculate Factor 3 for this FY 2020 IPPS/LTCH PPS final rule. We note that we expect to able to use the March HCRIS in future rulemaking, which is generally a more appropriate data source for a number of reasons, including that the data is available to the public to review for a longer period of time prior to the publication of the final rule, and the use of the June 30th extract presents ratesetting challenges for CMS to incorporate the data in time for the statutory publication of the final rule.
Following the publication of this final rule, hospitals will have until August 31, 2019, to review and submit comments on the accuracy of the table and supplemental data file published in conjunction with this final rule. We believe the supplemental data file reflects the most recent available data in HCRIS at the time of development of this final rule. We have not considered information from any revised Worksheets S-10 that were submitted as attachments to comments. We do not believe it would be appropriate to allow a hospital to use the rulemaking process to circumvent the requirement that cost report data need to be submitted to the MAC or the requirement that requests to reopen cost reports need to be submitted to the MAC. Otherwise we would have multiple potentially conflicting sources of information about a hospital's uncompensated care data or, more broadly, any cost report data that might be submitted during the rulemaking process. In addition, there are validity checks and other safeguards incorporated into the cost report submission process that would not be automatically applied to cost reports only submitted through rulemaking.
Comment: A few commenters also noted that the February 15, 2019 HCRIS extract used for the proposed rule may have misled some providers choosing between the proposed and alternative methodologies for calculating Factor 3 because certain changes to the FY 2015 data, such as audit corrections, would only be reflected when CMS uses the March HCRIS extract, as proposed for the final rule. Similarly, another commenter asserted that CMS has used different data and calculations in the final rules without the opportunity for hospitals to comment, that is, hospitals do not see their final DSH payment amounts until the final rule, in violation of the Administrative Procedural Act.
Response: Regarding the concerns related to the Administrative Procedure Act, we note that, under the Administrative Procedure Act, a proposed rule is required to include either the terms or substance of the proposed rule or a description of the subjects and issues involved. In this case, the FY 2020 IPPS/LTCH PPS proposed rule included a detailed discussion of our proposed methodology for calculating Factor 3 and the data that would be used. We made public the best data available at the time of the proposed rule, in order to allow hospitals to understand the anticipated impact of the proposed methodology. Moreover, following the publication of the proposed rule, we continued our efforts to ensure that information hospitals had properly submitted to their MAC in the prescribed timeframes would be available to be used in this final rule in the event we finalized our proposed methodology. We believe the fact that we provided data with the proposed rule, while concurrently continuing to review that data with individual hospitals is entirely consistent with the Administrative Procedure Act and established CMS practice. There is no requirement under either the Administrative Procedure Act or the Medicare statute that CMS make the actual data that will be used in a final rule available as part of the notice of proposed rulemaking. Rather, it is sufficient that we provide stakeholders with notice of our proposed methodology and the data sources that will be used, so that they may have a meaningful opportunity to submit their views on the proposed methodology and the adequacy of the data for the intended purpose. This requirement for notice and comment does not, however, extend to a requirement that we make all data that will be used to compute payments available to the public, so that they may have an opportunity to comment on accuracy of the data reported for individual hospitals. Similarly, there is no requirement that we provide an opportunity for comment on the actual payment amounts determined for each hospital.
Comment: Several commenters supported CMS' proposal to trim hospitals' uncompensated care costs to control for anomalies. However, many of these commenters recommended that CMS substitute aberrant data from the FY 2015 Worksheet S-10 with data from FY 2014, since the FY 2014 data have been previously available for public scrutiny and utilized in determining uncompensated care payments. A few commenters also voiced concerns regarding the agency's proposed policy for trimming uncompensated care costs. A commenter considered that it is unnecessary to substitute 1 year of Worksheet S-10 data for another, unless there has been some inappropriate action or improper reporting by the provider. Other commenters stated that CMS has not clarified how hospitals with high uncompensated care costs, which are subject to the trimming policy, are identified. The commenter added that CMS has failed to account for situations in which a hospital might legitimately have high uncompensated care costs for reasons such payer mix composition. The commenter suggested that CMS must take steps to discern when high uncompensated care costs arise from erroneous data rather than from a legitimate cause by ensuring that MACs work collaboratively with hospitals to distinguish inaccurate uncompensated care values from legitimately high values. According to the commenter, if a hospital can justify its high values, its uncompensated care costs should not be subject to the substitution.
Response: We appreciate the comments and suggestions regarding our policy for trimming uncompensated care costs that are an extremely high ratio of a hospital's total operating costs for the same year. We believe the proposed approach balances our desire to exclude potentially aberrant data with our concern regarding inappropriately reducing FY 2020 uncompensated care payments to a hospital that may have a legitimately high ratio. We note that no hospitals exceeded the 50 percent trim threshold for the FY 2015 Worksheet S-10. We will continue to consider the commenters' recommendations for the aberrant UCC data trim in future rulemaking.
Comment: Several commenters stated that the current Worksheet S-10 does not account for all patient care costs when converting charges to costs. These commenters stated that the current worksheet ignores substantial costs hospitals incur in training medical residents, supporting physician and professional services, and paying provider taxes associated with Medicaid revenue. Thus, these commenters requested that CMS refine the Worksheet S-10 to incorporate all patient care costs into the CCR. Commenters most often recommended that the CCR include the cost of graduate medical education (GME) to account for the costs associated with the training of interns and residents. The commenters stated that GME represents a significant portion of the overhead costs of teaching hospitals, where a large number of interns and residents treat patients from all financial backgrounds, including the uninsured. Therefore, the commenters believed that including GME costs in the CCR calculation and then using this adjusted CCR for Worksheet S-10 would more accurately represent the true uncompensated care costs for teaching hospitals. A commenter also stated that including GME cost in determining the CCR used on the Worksheet S-10 will better align with the Medicaid DSH program, as well as with the approach used by the IRS in calculating the hospital community benefit provided by non-profit hospitals.
In addition, commenters provided several suggestions for revising the CCR on Worksheet S-10. One suggestion was for CMS to use the total of Worksheet S, Column 3, Lines 1 through 117, reduced by the amount on Worksheet A-8, Line 10, as the cost component, and Worksheet C, Column 8, Line 200 as the charge component. Another commenter stated that GME costs can be included in the formula for calculating the CCR for Worksheet S-10 by using costs from Worksheet B, Part 1, Column 24, line 118, and by removing the reasonable compensation equivalency (RCE) limits from Worksheet S-10.
Response: As we have stated previously in response to this issue (83 FR 41425), we believe that the purpose of uncompensated care payments is to provide additional payment to hospitals for treating the uninsured, not for the costs incurred in training residents. In addition, because the CCR on Line 1 of Worksheet S-10 is pulled from Worksheet C, Part I, and is also used in other IPPS ratesetting contexts (such as high-cost outliers and the calculation of the MS-DRG relative weights) from which it is appropriate to exclude GME because GME is paid separately from the IPPS, we hesitate to adjust the CCR in the narrower context of calculating uncompensated care costs. Therefore, we continue to believe that it is not appropriate to modify the calculation of the CCR on Line 1 of Worksheet S-10 to include GME costs in the numerator. With regard to the comment that the CCRs on Worksheet S-10 are reported with the reasonable compensation equivalent (RCE) limits applied, we believe the commenter is mistaken. Line 1 of Worksheet S-10 instructs hospitals to compute the CCR by dividing the costs from Worksheet C, Part I, Line 202, Column 3, by the charges on Worksheet C, Part I, Line 202, Column 8. The RCE limits are applied in Column 4, not in Column 3; thus, the RCE limits do not affect the CCR on line 1 of Worksheet S-10.
Comment: Several commenters supported the proposal to use one cost report beginning in each fiscal year to derive the uncompensated care costs for that year, and to annualize Medicaid days and uncompensated care data for hospitals with less than 12 months of data. In addition, several commenters supported the proposed policy of allowing new hospitals that appear to be eligible for empirical DSH payments to receive empirically justified DSH payments but not interim uncompensated care payments.
Response: We appreciate the support for our proposal to use one cost report beginning in each fiscal year to derive the uncompensated care costs for that year, to annualize cost reports that do not equal 12 months of data, and to allow new hospitals that appear to be eligible for empirical DSH payments to receive interim empirically justified DSH payments but not interim uncompensated care payments.
Comment: Many commenters from Puerto Rico expressed their general support for the DSH policies proposed for FY 2020, and urged that CMS implement these policies as proposed. More specifically, several commenters supported the proposed policy for Puerto Rico, Indian Health Service, and Tribal hospitals, under which low-income patient days would continue to be utilized instead of the Worksheet S-10 UCC data to determine each hospital's share of uncompensated care payments. In addition, these commenters supported the proposal to continue to use 14 percent of Medicaid days as a proxy for Medicare SSI days when determining Factor 3 of the uncompensated care payment methodology for hospitals located in Puerto Rico. These commenters stated that the continued use of these proxies is appropriate, adding that they agree with CMS and other stakeholders that uncompensated care data reported by these hospitals need to be further examined before the data are used in calculating uncompensated care payments.
Response: We appreciate the support for our proposal to use low-income insured days as a proxy for UCC for Puerto Rico, Indian Health Service, and Tribal hospitals, as well as for our proposal to use 14 percent of a Puerto Rico hospital's Medicaid days as a proxy for SSI days. Because we are continuing to use insured low-income insured patient days as a proxy for uncompensated care for these hospitals in determining Factor 3 for FY 2020, and residents of Puerto Rico are not eligible for SSI benefits, we believe it is important to create a proxy for SSI days for Puerto Rico hospitals in the Factor 3 calculation.
The following comments address the proposed CCR trimming methodology:
Comment: A few commenters stated that the current CCR trimming methodology is not adequate to address the CCR anomalies in the Worksheet S-10 data reported by certain hospitals. Other commenters supported the current methodology. Some commenters also stated that hospitals that have been identified as potential outliers should have the opportunity to explain their data and correct errors before the trim methodology is applied, which would facilitate data validity. In addition, other commenters requested that the trimming methodology not be finalized until an audit of the data has been conducted, and that hospitals with extremely high CCRs be audited and an appropriate CCR determined instead of applying an arbitrary trim to a statewide average. For example, a number of commenters proposed that the four-step methodology for trimming CCRs should be used as an outlier identification process to alert auditors, not as a policy in and of itself. These commenters expect that as CMS continues to work on the Worksheet S-10 audit process, the proposed CCR trims would become an audit tool rather than a mechanism to trim what appears to be aberrant data.
A commenter stated that CMS should focus on understanding the underlying reason for varying CCRs, and that if CMS intends to require hospitals to revise their charge structures and cost apportionment methodologies, CMS should give the hospitals sufficient time to bring their systems into line with these requirements. Similarly, several commenters expressed concern over the proposed trim methodology because hospitals that are considered “all-inclusive rate providers” are not required to complete Worksheet C, Part I, which is used for reporting the CCR on Line 1 of the Worksheet S-10. As a result, these commenters believed that the proposed trim methodology would inappropriately modify their uncompensated care costs, and that a high CCR could be accurate if the hospital's charges are close to costs, as is usually the case for all-inclusive rate hospitals. These commenters recommended that CMS assess how the current CCR trim methodology affects all-inclusive rate providers, or work with MACs to derive an appropriate CCR.
In addition, commenters encouraged CMS to engage with hospitals in determining the best way to use Worksheet S-10 data to distribute uncompensated care payments to all-inclusive rate providers in the future, and some suggested that CMS continue to use the low-income patient days proxy to distribute Medicare DSH uncompensated care payments to these providers. A commenter stated that there was a contradiction in the proposed rule because CMS indicated that it was no longer necessary to propose specific Factor 3 policies for all-inclusive providers, yet later indicated that CMS would remove all-inclusive providers from the CCR trimming methodology because their CCRs are not comparable to the CCRs calculated for other IPPS hospitals. The commenter requested that CMS take a consistent approach in the final rule, and encouraged CMS to revisit its trimming methodology in the final rule and to also focus its audit activity for the FY 2017 Worksheet S-10 data on whether high CCR hospitals, particularly those that use an all-inclusive rate structure, are generating an accurate portrayal of uncompensated care costs.
Response: We appreciate the additional information provided by the commenters related to our proposed methodology for applying trims to the CCRs. We intend to further explore which trims are most appropriate to apply to the CCRs on Line 1 of Worksheet S-10, including whether it would be appropriate to apply a unique trim for certain subsets of hospitals, such as all-inclusive rate providers. We note that all-inclusive rate providers have the ability to compute and enter their appropriate information (for example, departmental cost statistics) on Worksheet S-10, Line 1, by answering “Yes” to the question on Worksheet S-2, Part I, Line 115, rather than having it computed using information from Worksheet C, Part I. We also intend to give additional consideration to the utilization of statewide averages in place of outlier CCRs, and will also consider other approaches that could ensure the validity of the trim methodology, while not penalizing hospitals that use alternative methods of cost apportionment. We may consider incorporating these alternative approaches through rulemaking for future years.
However, as discussed in the FY 2020 IPPS/LTCH PPS proposed rule, we have examined the CCRs from the FY 2015 cost reports and believe that the risk that all-inclusive rate providers will have aberrant CCRs and, consequently, aberrant uncompensated care data, is mitigated by the proposal to apply trim methodologies for potentially aberrant uncompensated care costs for all hospitals. As outlined in the proposed rule, we remove all-inclusive rate providers from the CCR trim in Step 1 of the trimming methodology because their CCRs are not comparable to the CCRs calculated for other IPPS hospitals. Thus, the CCRs for all-inclusive rate providers are excluded from the CCR trimming process. Regarding the commenters' view that CCR trims should not take place before we give providers further opportunities to explain or amend their data, we agree that, under ideal circumstances, CCR trims without audits would not be needed. However, providers have had sufficient time to amend their data and/or contact CMS to explain that the FY 2020 DSH Supplemental Data File posted in conjunction with FY 2020 IPPS/LTCH PPS proposed rule had incorrect data. As a result, we consider CCRs greater than 3 standard deviations above the national geometric mean CCR for the applicable fiscal year to be aberrant CCRs.
After consideration of the public comments we received, and for the reasons discussed in the proposed rule and in this final rule, we are finalizing our proposal to use 1 year of Worksheet S-10 data from FY 2015 cost reports to determine Factor 3 of the uncompensated care methodology.
Therefore, for FY 2020, we are finalizing the following methodology to compute Factor 3 for each hospital by—
Step 1: Selecting the provider's longest cost report from its Federal fiscal year (FFY) 2015 cost reports. (Alternatively, in the rare case when the provider has no FFY applicable cost report because the cost report for the previous Federal fiscal year spanned the time period, the previous Federal fiscal year cost report would be used in this step.)
Step 2: Annualizing the uncompensated care costs (UCC) from Worksheet S-10 Line 30, if the cost report is more than or less than 12 months. (If applicable, use the statewide average CCR (urban or rural) to calculate uncompensated care costs.)
Step 3: Combining annualized uncompensated care costs for hospitals that merged.
Step 4: Calculating Factor 3 for Indian Health Service and Tribal hospitals and Puerto Rico hospitals using the annualized low-income insured days proxy based on FY 2013 cost report data and the most recent available SSI ratio (or, for Puerto Rico hospitals, 14 percent of the hospital's FY 2013 Medicaid days). (Alternatively, in the rare case when the provider has no FFY applicable cost report because the cost report for the previous Federal fiscal year spanned the time period, the previous Federal fiscal year cost report would be used in this step.) We combine low-income insured days for hospitals that merged. The denominator is calculated using the low-income insured days proxy data from all DSH eligible hospitals. We note, that consistent with the policy adopted in the FY 2019 IPPS/LTCH final rule, if a hospital does not have both Medicaid days for FY 2013 and SSI days for FY 2017 available for use in the calculation of Factor 3 in Step 4, we would consider the hospital not to have data available for Step 4.
Step 5: Calculating Factor 3 for the remaining DSH-eligible hospitals using annualized uncompensated care costs (Worksheet S-10 Line 30) based on FY 2015 cost report data (from Step 3). The hospitals for which Factor 3 was calculated in Step 4 are excluded from this calculation.
We also are finalizing the following proposals: (1) For providers with multiple cost reports beginning in the same fiscal year, to use the longest cost report and annualize Medicaid data and uncompensated care data if a hospital's cost report does not equal 12 months of data; (2) where a provider has multiple cost reports beginning in the same fiscal year, but one report also spans the entirety of the following fiscal year such that the hospital has no cost report for that fiscal year, to use the cost report that spans both fiscal years for the latter fiscal year; and (3) to apply statistical trim methodologies to potentially aberrant CCRs and potentially aberrant uncompensated care costs.
For this FY 2020 IPPS/LTCH PPS final rule, we are finalizing a HCRIS cutoff of June 30, 2019, for purposes of calculating Factor 3. We are also finalizing our proposal to amend the regulations at § 412.106(g)(1)(iii)(C) by adding a new paragraph (6) to reflect the methodology for computing Factor 3 for FY 2020.
5. Request for Public Comments on Ways to Reduce Provider Reimbursement Review Board (PRRB) Appeals Related to a Hospital's Medicaid Fraction Used in the Disproportionate Share Hospital (DSH) Payment Adjustment Calculation
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19422 through 19423), as part of our ongoing efforts to reduce regulatory burden on providers, we are examining the backlog of appeals cases at the Provider Reimbursement Review Board (PRRB). A large number of appeals before the PRRB relate to the calculation of a hospital's disproportionate patient percentage (DPP) used in the calculation of the DSH payment adjustment. (We refer readers to section IV.F.1. of the preamble of this final rule for a discussion of the calculation of a hospital's DPP.) Many of these appeals before the PRRB focus on the calculation of a hospital's Medicaid fraction, which is one of the two fractions comprising the DPP, particularly the data used to determine an individual's Medicaid eligibility in the calculation. Specifically, it is possible that updated data on Medicaid eligibility are available following cost report submission. As a result, many hospitals annually appeal their cost reports to the PRRB in an effort to try and use updated State Medicaid eligibility data to calculate the Medicaid fraction. We believe it is in both CMS' and the providers' interest to seek a solution to issues related to the Medicaid fraction that appear to have led to a large volume and backlog of PRRB appeals. Therefore, we believe it is appropriate to explore options that may prevent the need for such appeals. We note that the Provider Reimbursement Review Board Rules, Version 2.0, August 29, 2018, contain revisions in Rules 46 and 47 pertaining to “Withdrawal of an Appeal or Issue Within an Appeal” and “Reinstatement”, respectively. These changes may lower the number of tracked PRRB appeals. In exploring possible solutions, we are concerned about balancing the competing interests of administrative finality, ease of implementation for both CMS and providers, and the use of the most appropriate data.
As stated in the proposed rule, we believe one such solution might be to develop regulations governing the timing of the data for determining Medicaid eligibility, somewhat similar to our existing policy on entitlement to SSI benefits which is determined at a specific time. For more information on this policy, we refer readers to the FY 2011 IPPS/LTCH PPS final rule (75 FR 50276). Under this possible solution, a provider would submit a cost report with Medicaid days based on the best available Medicaid eligibility data at the time of filing and could request a “reopening” when the cost report is settled without filing an appeal. CMS would issue directives to the MACs requiring them to reopen those cost reports for this issue at a specific time and set a realistic period during which the provider could submit updated data. This would be an expansion of the preamble instructions finalized in the CY 2016 OPPS/ASC final rule with comment period issued on November 13, 2015 (80 FR 70563 and 70564) which requires the MACs to accept one amended cost report submitted within 12 months after the due date of the cost report solely for the purpose of revising Medicaid days. (We note that an amendment of the cost report is initiated by the provider prior to final settlement of the cost report, while a reopening of the cost report occurs after final settlement and can be requested by the provider or initiated by the MAC.) Under this possible expansion, we would require MACs to reopen cost reports for the purpose of revising the Medicaid fraction near the end of the 3-year reopening window and use the Medicaid data at that time to settle the cost report. We believe the 3 years of the reopening period could provide adequate time to update the Medicaid data used to determine an individual's Medicaid eligibility for purposes of calculating a hospital's Medicaid fraction. However, as indicated in the proposed rule, we were generally interested in public comments on using reopenings as a mechanism to use updated Medicaid eligibility data and reduce the filing of PRRB appeals—in particular, the optimal time for review of data to occur taking into account the hospital's desire to receive accurate payment and CMS' and the MACs' desire to settle cost reports in a timely manner (for example, whether it makes sense to review data 2 years after cost report submission, near the end of the 3 years mentioned in the reopening regulations, or at some other time).
We stated in the proposed rule that we also are considering allowing hospitals, for a one-time option, to resubmit a cost report with updated Medicaid eligibility information, somewhat similar to our existing DSH policy allowing hospitals a one-time option to have their SSI ratios calculated based on their cost reporting period rather than the Federal fiscal year under 42 CFR 412.106(a)(3). Under this option, we would undertake rulemaking to determine the timeframe for exercising the option (which may be a maximum allowable time after the close of a cost reporting period or a specific window during which the request could be made). We indicated in the proposed rule we were interested in feedback and comments concerning the viability of these options, as well as any alternative approaches, that could help reduce the number of DSH-related appeals and inform our future rulemaking efforts.
Comment: We received several comments in response to this request for information. Commenters were generally supportive of the options presented.
Response: We thank commenters for responding to this request for information. We will take these comments into consideration for future rulemaking.
G. Hospital Readmissions Reduction Program: Updates and Changes (§§ 412.150 through 412.154)
1. Statutory Basis for the Hospital Readmissions Reduction Program
Section 1886(q) of the Act, as amended by section 15002 of the 21st Century Cures Act, establishes the Hospital Readmissions Reduction Program. Under the Hospital Readmissions Reduction Program, Medicare payments under the acute inpatient prospective payment system for discharges from an applicable hospital, as defined under section 1886(d) of the Act, may be reduced to account for certain excess readmissions. Section 15002 of the 21st Century Cures Act requires the Secretary to compare hospitals with respect to the proportion of beneficiaries who are dually eligible for Medicare and full-benefit Medicaid (dual eligibles) in determining the extent of excess readmissions. We refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49530 through 49531) and the FY 2018 IPPS/LTCH PPS final rule (82 FR 38221 through 38240) for a detailed discussion of and additional information on the statutory history of the Hospital Readmissions Reduction Program.
2. Regulatory Background
We refer readers to the following final rules for detailed discussions of the regulatory background and descriptions of the current policies for the Hospital Readmissions Reduction Program:
- FY 2012 IPPS/LTCH PPS final rule (76 FR 51660 through 51676).
- FY 2013 IPPS/LTCH PPS final rule (77 FR 53374 through 53401).
- FY 2014 IPPS/LTCH PPS final rule (78 FR 50649 through 50676).
- FY 2015 IPPS/LTCH PPS final rule (79 FR 50024 through 50048).
- FY 2016 IPPS/LTCH PPS final rule (80 FR 49530 through 49543).
- FY 2017 IPPS/LTCH PPS final rule (81 FR 56973 through 56979).
- FY 2018 IPPS/LTCH PPS final rule (82 FR 38221 through 38240).
- FY 2019 IPPS/LTCH PPS final rule (83 FR 41431 through 41439).
These rules describe the general framework for the implementation of the Hospital Readmissions Reduction Program, including: (1) The selection of measures for the applicable conditions/procedures; (2) the calculation of the excess readmission ratio (ERR), which is used, in part, to calculate the payment adjustment factor; (3) beginning in FY 2019, the calculation of the proportion of “dually eligible” Medicare beneficiaries which is used to stratify hospitals into peer groups and establish the peer group median ERRs; (4) the calculation of the payment adjustment factor, specifically addressing the base operating DRG payment amount, aggregate payments for excess readmissions (including calculating the peer group median ERRs), aggregate payments for all discharges, and the neutrality modifier; (5) the opportunity for hospitals to review and submit corrections using a process similar to what is currently used for posting results on Hospital Compare; (6) the adoption of an extraordinary circumstances exception policy to address hospitals that experience a disaster or other extraordinary circumstance; (7) the clarification that the public reporting of ERRs will be posted on an annual basis to the Hospital Compare website as soon as is feasible following the review and corrections period; and (8) the specification that the definition of “applicable hospital” does not include hospitals and hospital units excluded from the IPPS, such as LTCHs, cancer hospitals, children's hospitals, IRFs, IPFs, CAHs, and hospitals in United States territories and Puerto Rico.
We also have codified certain requirements of the Hospital Readmissions Reduction Program at 42 CFR 412.152 through 412.154. In section IV.G.12. of the preamble of this final rule, we are finalizing our proposals to update the regulatory text to reflect both the proposed policies that we are finalizing in this final rule as well as previously finalized policies.
The Hospital Readmissions Reduction Program strives to put patients first by ensuring they are empowered to make decisions about their own healthcare along with their clinicians, using information from data-driven insights that are increasingly aligned with meaningful quality measures. We believe the Hospital Readmissions Reduction Program incentivizes hospitals to improve health care quality and value, while giving patients the tools and information needed to make the best decisions for them. To that end, we are committed to monitoring the efficacy of the program to ensure that the Hospital Readmissions Reduction Program improves the lives of patients and reduces cost.
We note that we received public comments on the effectiveness and design of the Hospital Readmissions Reduction Program in response to the FY 2020 IPPS/LTCH PPS proposed rule. While we appreciate the commenters' feedback, because we did not include in the proposed rule any proposals related to these topics, we consider the public comments to be out of the scope of the proposed rule. Therefore, we are not addressing most of these comments in this final rule. However, all topics that we consider to be out of scope of the proposed rule will be taken into consideration when developing policies and program requirements for future years.
Comment: Several commenters urged CMS to work with a range of stakeholders—including hospitals, patients and health services researchers—to assess whether the Hospital Readmissions Reduction Program has had a negative impact on hospital mortality rates and other unintended consequences, and noted that some emerging research may suggest that the Hospital Readmissions Reduction Program's strong incentive to reduce readmissions could be associated with higher mortality rates.
Response: We believe that the Hospital Readmissions Reduction Program has successfully reduced readmissions, which are both harmful to patients and costly for the health care system. In June 2018, the Medicare Payment Advisory Commission also stated that “Readmission rates clearly declined from 2010 to 2016. Given the totality of the evidence and the findings in the literature, it appears that at least some of this reduction was due to the incentives in the HRRP. The exact share that is due to the HRRP and the share due to other factors is difficult to disentangle.” [317] Keeping patients healthy is one of our highest priorities, and we welcome any research reports pertaining to the unintended consequences of the program. We will continue to monitor literature that discusses the Program, and take this information into account during future policymaking. We are committed to monitoring any unintended consequences over time, such as the inappropriate shifting of care or increased patient morbidity and mortality, to ensure that the Hospital Readmissions Reduction Program improves the lives of patients and reduces cost.
3. Summary of Policies for the Hospital Readmissions Reduction Program
In the FY 2020 IPPS/LTCH PPS proposed rule, we proposed the following policies: (1) A measure removal policy that aligns with the removal factor policies previously adopted in other quality reporting and quality payment programs; (2) an update to the program's definition of “dual-eligible”, beginning with the FY 2021 program year, to allow for a 1-month lookback period in data sourced from the State Medicare Modernization Act (MMA) files to determine dual-eligible status for beneficiaries who die in the month of discharge; (3) a subregulatory process to address any potential future nonsubstantive changes to the payment adjustment factor components; and (4) an update to the regulations at 42 CFR 412.152 and 412.154 to reflect proposed policies and to codify additional previously finalized policies.
In this final rule, we are finalizing our proposals as proposed. We discuss these finalized proposals in greater detail below.
4. Current Measures and Newly Finalized Measure Policies for FY 2020 and Subsequent Years
a. Current Measures
The Hospital Readmissions Reduction Program currently includes six applicable conditions/procedures: Acute myocardial infarction (AMI); heart failure (HF); pneumonia; elective primary total hip arthroplasty/total knee arthroplasty (THA/TKA); chronic obstructive pulmonary disease (COPD); and coronary artery bypass graft (CABG) surgery. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41431 through 41439) for more information about how the Hospital Readmissions Reduction Program supports CMS' goal of bringing quality measurement, transparency, and improvement together with value-based purchasing to the hospital inpatient care setting through the Meaningful Measures Initiative. We continue to believe the measures we have adopted adequately meet the goals of the Hospital Readmissions Reduction Program. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19424), we did not propose to remove or adopt any additional measures at this time.
b. Measure Removal Factors Policy
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19424), while we did not propose to remove any measures from the Hospital Readmissions Reduction Program, we proposed to adopt a measure removal factors policy as part of our efforts to ensure that the Hospital Readmissions Reduction Program measure set continues to promote improved health outcomes for beneficiaries while minimizing the overall burden and costs associated with the program. The adoption of measure removal factors would align the Hospital Readmissions Reduction Program with our other quality reporting and quality payment programs and help ensure consistency in our measure evaluation methodology across programs.
In the FY 2019 IPPS/LTCH PPS final rule, we updated a number of CMS programs' considerations for removing measures from the respective programs. Specifically, we finalized eight measure removal factors for the Hospital IQR Program (83 FR 41540 through 41544), the Hospital VBP Program (83 FR 41441 through 41446), the PCHQR Program (83 FR 41609 through 41611), and the LTCH QRP (83 FR 41625 through 41627).
We believe these removal factors are also appropriate for the Hospital Readmissions Reduction Program, and we believe that alignment between CMS quality programs is important to provide stakeholders with a clear, consistent, and transparent process. Therefore, to align with our other quality reporting and quality payment programs, we proposed to adopt the following removal factors for the Hospital Readmissions Reduction Program:
- Factor 1. Measure performance among hospitals is so high and unvarying that meaningful distinctions and improvements in performance can no longer be made (“topped-out” measures);
- Factor 2. Measure does not align with current clinical guidelines or practice;
- Factor 3. Measure can be replaced by a more broadly applicable measure (across settings or populations) or a measure that is more proximal in time to desired patient outcomes for the particular topic;
- Factor 4. Measure performance or improvement does not result in better patient outcomes;
- Factor 5. Measure can be replaced by a measure that is more strongly associated with desired patient outcomes for the particular topic;
- Factor 6. Measure collection or public reporting leads to negative unintended consequences other than patient harm; [318]
- Factor 7. Measure is not feasible to implement as specified; and
- Factor 8. The costs associated with a measure outweigh the benefit of its continued use in the program.[319]
We note that these factors are considerations taken into account when deciding whether or not to remove measures, not firm requirements, and that we will propose to remove measures based on these factors on a case-by-case basis. We continue to believe that there may be circumstances in which a measure that meets one or more factors for removal should be retained regardless, because the benefits of a measure can outweigh its drawbacks. Our goal is to move the program forward in the least burdensome manner possible, while maintaining a parsimonious set of meaningful quality measures and continuing to incentivize improvement in the quality of care provided to patients.
We received several public comments on our proposed measure removal factors.
Comment: Many commenters supported the adoption of the eight measure removal factors previously adopted by the Hospital IQR Program and the Hospital VBP Program into the Hospital Readmissions Reduction Program. A few commenters stated that adoption of these factors would allow for consistency and alignment in measure evaluation methodology across programs. Some commenters also believed that the factors are well-established and ensure that a variety of valid reasons to remove a measure are considered by CMS. A few commenters also believed the proposal would reduce burden and increase efficiency.
Response: We thank the commenters for their support.
Comment: Some commenters encouraged CMS to be transparent in how these factors are applied when a measure is considered for removal and urged CMS to use the factors as a guide to removal rather than an automatic process.
Response: As we stated in the proposed rule and as described above, we consider these removal factors as considerations for removal, not firm requirements. We value transparency in our processes, and plan to seek stakeholder input through education and outreach, rulemaking and other stakeholder engagement before removing measures.
Comment: One commenter opposed the adoption of the removal criteria because this commenter believed the criteria lack specificity and empirical support. The commenter believed that CMS should include more detail on how the removal factors would apply to beneficiaries, and develop and publicly share how the terminology in each criterion would be applied. The commenter requested transparency around how such terms were tested and what results will empirically determine whether the criterion is met or not.
Response: We thank the commenter for these recommendations. As we discussed in the proposed rule, the removal factors are intended to be considerations that we take into account when deciding whether or not to remove measures. There may be circumstances in which we decide that a measure that meets one or more factors for removal should be retained regardless of the criteria, because any benefit of removing a measure could be outweighed by the benefits of retaining it. We intend to take multiple considerations and stakeholder feedback into account when determining whether to propose a measure for removal under any of the removal factors.
Comment: Several commenters supported removal Factor 1: “measure performance among hospitals is so high and unvarying that meaningful distinctions and improvement in performance can no longer be made (“topped-out” measures),” but encouraged CMS to enhance the removal factor by adding quantitative criteria or empirical criteria similar to the criteria adopted by Hospital IQR and Hospital VBP Programs. Some commenters specifically recommended adding the “topped out” definition adopted by the Hospital IQR and Hospital VBP Programs (79 FR 50055):
- The difference in performance between the 75th and 90th percentile is statistically indistinguishable. In general, this means that the 75th and 90th percentile scores differ by less than two standard deviations.
- The truncated coefficient of variation (TCV) is less or equal to 0.10. CMS's definition of “truncated” is to remove the top and bottom 5% of hospitals before calculating the CV. Applying these two criteria to current data shows that the program's measure set may already be “topped out” in performance.
Response: We thank the commenters for these recommendations. Because the Hospital Readmissions Reduction Program focuses on improved coordination and communication to prevent readmissions that are harmful to patients and costly to Medicare, the empirical criteria developed for the Hospital IQR and Hospital VBP Programs may not be appropriate for all readmissions. The Hospital Readmissions Reduction Program strives to encourage hospitals to reduce excess readmissions, not within a statistical standard, but to as close to zero as possible. While we do not believe that the Hospital IQR Program or Hospital VBP Programs' empirical standards are appropriate for the Hospital Readmissions Reduction Program at this time, we will consider whether other statistical standards may be more appropriate for the Hospital Readmissions Reduction Program in the future. Therefore, we believe adding quantitative or empirical criteria at this time would not be appropriate.
Comment: A few commenters opposed adoption of measure removal Factor 1: “measure performance among hospitals is so high and unvarying that meaningful distinctions and improvement in performance can no longer be made (“topped out” measures).” One commenter believed that removal of a measure immediately upon a “topped out” analysis would eliminate the ability to determine whether performance regresses or that the removal of the measure may result in lower quality of care over the long term. The commenter recommended CMS either consolidate measures that meet the “topped out” criteria but are still considered meaningful to stakeholders into a composite measure or include them as an evidence-based standard in a verification program. One commenter expressed its belief that the policy would eliminate many important measures and would therefore not address true quality improvement. Another commenter believed that many measures are “never events” and a low prevalence still can be unacceptably high. The commenter also believed the quantitative criteria CMS uses for determining topped out status is problematic, as beneficiaries and payers often avoid the lowest performers, and that CMS's topped out methodology does not account for variation in lower performing percentiles; additionally, a potential high degree of variation outside of the narrow 75th-90th percentiles is unaccounted for.
Response: We thank the commenters for these recommendations. As we discussed in the proposed rule, the removal factors are intended to be considerations taken into account when deciding whether or not to remove measures but are not firm requirements. There may be circumstances in which a measure that meets one or more factors for removal should be retained regardless, because any benefit of removing a measure could be outweighed by other benefits to retaining the measure. We intend to take multiple considerations into account when determining whether to propose a measure for removal under Factor 1 or any of the other removal factors. Additionally, we note that we have intentionally not provided numerical guidelines for Factor 1 in order to retain flexibility when assessing measures.
Comment: Several commenters expressed concern that retaining “topped out” measures could detract from quality improvements because hospitals might expend more resources trying to improve measures that have limited opportunity for improvement rather than focusing on measures that could provide greater opportunities for improvement. Another expressed concern that CMS might retire measures using the “topped-out” criteria before identifying and adopting replacement measures, and urged CMS to be thoughtful before removing measures.
Response: We thank the commenters for sharing their concerns. The removal factors are intended to be considerations that we take into account when deciding whether or not to remove measures as part of a holistic review of the program's measure set. There may be circumstances in which a measure that meets one or more factors for removal should be retained regardless of the criteria because any benefit of removing a measure could be outweighed by benefits of retaining the measure. We intend to take multiple considerations and stakeholder feedback into account when determining whether to propose a measure for removal under any of the removal factors.
Comment: Several commenters supported the adoption of Factor 8: “costs associated with a measure outweigh the benefit of its continued use in the program.”
Response: We thank the commenters for the support.
Comment: A few commenters raised specific concerns regarding Factor 8: “the costs associated with the measure outweigh the benefit of its continued use in the program.” A commenter supported the addition of Factor 8, but suggested that CMS seek stakeholder input specifically each time Factor 8 is considered for application. Another commenter opposed the adoption of Factor 8 unless “costs” and “benefits” are defined as “costs to Medicare beneficiaries and the public” and “benefits to Medicare beneficiaries and the public.” A few commenters expressed the belief that CMS should develop empirical criteria to determine whether this factor has been met. A few commenters strongly opposed Factor 8 because of their belief that it is extremely subjective, lacks clear criteria and guidelines, and that costs should not be the driving factor when deciding whether to remove a measure. A few commenters also argued that the other criteria were sufficient.
Response: We thank the commenters for sharing these concerns regarding Factor 8. We value transparency in our process and will seek stakeholder input prior to removing any measures from the Hospital Readmissions Reduction Program. We intend to be transparent in our assessment of measures under this measure removal factor. There are various considerations of costs and benefits that we will evaluate in applying removal Factor 8, and we will take into consideration the perspectives of multiple stakeholders. However, because we intend to evaluate each measure on a case-by-case basis, and each measure has been adopted to fill different needs in the Hospital Readmissions Reduction Program, we do not believe it would be meaningful to identify a specific set of assessment criteria to apply to all measures. We believe costs include costs to stakeholders such as patients, caregivers, providers, CMS, and other entities. In addition, we note that the benefits we will consider center on benefits to patients and caregivers as the primary beneficiaries of our quality reporting and value-based payment programs. When we propose to remove a measure under this measure removal factor, we will provide information on the costs and benefits we considered in evaluating the measure.
Comment: One commenter recommended that CMS adopt an additional measure removal factor, considering “whether the measure is important to beneficiaries or the public at large.” The commenter believed that the measure removal policy should center on the best interests of Medicare beneficiaries and Medicaid recipients and then the best interests of the public at large. The commenter recommended that the additional measure removal factor be Factor 1 to denote its primary importance, and the proposed measure removal factors be renumbered accordingly.
Response: We thank the commenter for this recommendation. We will consider the perspectives of all stakeholders when applying any of the measure removal factors, and importance to beneficiaries and the public at large are certainly part of this consideration. Additionally, we proposed these measure removal factors to support alignment with our other quality programs, and we do not believe that adopting additional measure removal factors for the Hospital Readmissions Reduction Program and renumbering the factors would facilitate alignment and could result in confusion when stakeholders review our programs' measure removal proposals in the future.
Comment: Another commenter recommended the loss of NQF-endorsement as an additional criterion for removal and encouraged CMS to remove measures that fail to pass NQF requirements or are replaced by more appropriate competing measures.
Response: We thank the commenter for this recommendation. As previously noted, our goal is to move the program forward in the least burdensome manner possible, while maintaining a parsimonious set of meaningful quality measures and continuing to incentivize improvement in the quality of care provided to patients. We review the Program's measure set on a regular basis and will continue to review and monitor the program's measure set, newly developed measures, and NQF guidance to ensure the program's measures remain evidence based. Additionally, we proposed these measure removal factors to support alignment with our other quality programs, and we do not believe that adopting additional measure removal factors for the Hospital Readmissions Reduction Program would facilitate alignment and could result in confusion when stakeholders review our programs' measure removal proposals in the future.
We intend to be transparent in our assessment of measures under the finalized measure removal factor. As mentioned in a previous comment response, because we intend to evaluate each measure on a case-by-case basis, and each measure has been adopted to fill different needs in the Hospital Readmissions Reduction Program, we do not believe it would be meaningful to identify a specific set of assessment criteria to apply to all measures.
After consideration of the public comments we received, we are finalizing our proposals to adopt for the Hospital Readmissions Reduction Program the eight measure removal factors currently in the Hospital IQR Program and Hospital VBP Program beginning with the FY 2020 program year.
5. Updated Definition of “Dual-Eligible” Beginning in FY 2021
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38226 through 38229), as part of implementing the 21st Century Cures Act, we finalized the definition of dual-eligible as follows: “Dual-eligible is a patient beneficiary who has been identified as having full benefit status in both the Medicare and Medicaid programs in the State Medicare Modernization Act (MMA) files for the month the beneficiary was discharged from the hospital.” In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41437 through 41438), we finalized our proposal to codify this definition at 42 CFR 412.152 along with other definitions pertinent to dual-eligibility calculations for assigning hospitals into peer groups.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19424 through 19425), we proposed to update our previously finalized definition of “dual-eligible” to specify that, for the payment adjustment factors beginning with the FY 2021 program year, “dual-eligible” is a patient beneficiary who has been identified as having full benefit status in both the Medicare and Medicaid programs in data sourced from the State MMA files for the month the beneficiary was discharged from the hospital, except for those patient beneficiaries who die in the month of discharge, who will be identified using the previous month's data sourced from the State MMA files.[320]
The updated definition is necessary to account for misidentification of the dual-eligible status of patient beneficiaries who die in the month of discharge, which can occur under the current definition. We were not aware at the time we finalized our current definition of “dual-eligible” that there are times when the data sourced from the State MMA files may underreport the number of beneficiaries with dual-eligibility status for the month in which the beneficiary dies, and, therefore, these data are not fully accurate reflections of dual-eligible status for the month in which a beneficiary dies. We have identified two situations that lead to the underreporting of dual-eligible patients: (1) The dual-eligible status is not recorded in the month of death; and (2) the dual-eligible status changes from dual in the months prior to death to non-dual in the month of death. We estimated that the number of misidentified patient beneficiaries is very small. We currently predict a 0.2% total increase in dual eligible beneficiaries admitted across all participating hospitals. Our analysis shows that this very small total increase did not have a large impact on peer grouping assignments or payment adjustments. Only 20 hospitals (less than 1 percent of open subsection (d) hospitals included in the Hospital Readmissions Reduction Program with measure results) would change peer group assignments under the proposed definition of dual-eligible stays. Of those 20 hospitals, 18 hospitals would receive a penalty under either definition of dual-eligible stays, and two hospitals would not receive a penalty under either definition. Nine of those 18 hospitals would have a slightly higher payment adjustment factor (PAF) and the largest increase would be 0.0023. Eight hospitals would have a slightly lower PAF and the largest decrease would be 0.0023. One hospital would have the same PAF under the revised definition. Based on our analysis, we believe that using the most accurate information available is the most appropriate policy for the program and consistent with our initial rationale for using the State MMA files as the source to identify dual-eligibles. When we adopted the current definition of “dual-eligible” in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38226), we stated, and many commenters agreed, that the State MMA file is considered the most current and most accurate source of data for identifying dual-eligible beneficiaries because the data are also used for operational purposes related to the administration of Medicare Part D benefits.
Our intent was, and remains, to use the most accurate data available to determine “dual-eligible” status in the hospital grouping portion of the payment adjustment. Through our analysis, we believe using a 1-month lookback period within the data sourced from the State MMA files to determine dual-eligible status for beneficiaries who die in the month of discharge will improve the accuracy of the number of beneficiaries identified as having dual-eligible status. We note that we proposed to update this definition for FY 2021 instead of FY 2020 because the time associated with updates to the data systems is inconsistent with our ability to finalize this proposal in time for FY 2020 and the lack of a subregulatory policy, which would allow us to make nonsubstantive changes outside of the rulemaking schedule.
We also proposed to revise the definition of “dual-eligible” codified at 42 CFR 412.152 to incorporate this update.
We received several public comments on our proposed modification to the definition of “dual-eligible” beginning in FY 2021.
Comment: Many commenters supported our proposal to modify the definition of a “dual eligible” beginning with the FY 2021 program year, to allow for a 1-month lookback period in data sourced from the State Medicare Modernization Act (MMA) files to determine dual-eligible status for beneficiaries who die in the month of discharge. Many commenters noted their beliefs that this update will more accurately reflect a hospital's dual eligible population and improve data reliability. Some commenters noted their understanding that only a small number of dual eligible beneficiaries' status would change as a result of the definition modification.
Response: We thank the commenters for their support. We would also like to provide additional information regarding the number of beneficiaries' statuses that are expected to change as a result of the definition modification. We anticipate about a 0.2% increase in dual eligible stays due to the definition modification based on the FY 2019 performance period (July 1, 2014 through June 30, 2017), or an increase from 8,769,611 dual stays under the previous definition to 8,786,367 dual stays under the modified definition, an increase of 16,756 dual eligible stays.
After consideration of the public comments we received, we are finalizing, without modification, that beginning in FY 2021, a “dual-eligible” is a patient beneficiary who has been identified as having full benefit status in both the Medicare and Medicaid programs in data sourced from the State MMA files for the month the beneficiary was discharged from the hospital, except for those patient beneficiaries who die in the month of discharge, who will be identified using the previous month's data sourced from the State MMA files.
6. Adoption of a Subregulatory Process for Changes to Payment Adjustment Factor Components
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41434), we reiterated our policy regarding the maintenance of technical specifications for quality measures. In adopting our policy for the maintenance of technical specifications in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50039), we stated that it is important to have in place a subregulatory process to incorporate nonsubstantive updates required by the National Quality Forum into the measure specifications we have adopted for the Hospital Readmissions Reduction Program, so that these measures remain up to date. We also stated that we would continue to use notice and comment rulemaking for any substantive changes to measure specification. We continue to believe this process is the most expeditious manner possible to ensure that quality measures remain fully up to date while preserving the public's ability to comment on updates that so fundamentally change a measure that it is no longer the same measure that we originally adopted. When we adopted this policy, we received commenter support for our policy of handling substantive and nonsubstantive changes to measures. The policy allows CMS two mechanisms to address measure updates: (1) The use of future proposed rules and public comment periods for substantive changes; and (2) subregulatory processes for nonsubstantive changes which also preserve CMS' autonomy and flexibility, in order to rapidly implement nonsubstantive updates to measures (79 FR 50039). We now believe it is important for the Hospital Readmissions Reduction Program to adopt an analogous subregulatory process for changes to the payment adjustment factor components to provide similar flexibility to rapidly implement nonsubstantive updates to implement previously finalized data components and other minor changes when payment adjustment factor components are impacted.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19425 through 19426), we proposed to adopt a policy under which we would use a subregulatory process to make nonsubstantive changes to the payment adjustment factor components used for the Hospital Readmissions Reduction Program. We previously adopted our payment adjustment factor components policies through the notice and comment rulemaking process. The Hospital Readmissions Reduction Program relies on these payment adjustment factor components, including, but not limited to, the proportion of dual-eligibles, peer group assignment, peer group median ERR, neutrality modifier, and ratio of DRG payments to total payments, to determine hospital payments in each fiscal year. Each year, we provide details on most of that information in the Hospital Specific Report (HSR) User Guide located on QualityNet website at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228772412669. However, there are times when data sourcing from previously finalized data sources and files and other technical aspects of the payment adjustment factor components change and require updating, even when those changes do not alter the intent of our previously finalized policies. Because the updates to data sourcing and technical aspects of the components are not always linked to the timing of regulatory actions, we believe this proposed policy is prudent to allow for the use of the most up-to-date, accurate information. We reiterate that we would continue to consider all changes to the framework of the components themselves as substantive changes that we would propose through the notice-and-comment rulemaking process.
Most recently, as discussed earlier, we identified an issue with data accuracy for determining dual-eligible status from data sourced from the State MMA files for beneficiaries who die in the same month as discharge. In section IV.G.5. of the preamble of this final rule, we are finalizing our proposal to amend the definition of “dual-eligible” to account for this data issue. However, we would like to clarify that the finalized proposal is not altering the intent of our previously finalized policy. Instead, the updated definition of “dual-eligible” allows for the use of the month preceding discharge for identifying dual-eligibles who died during the discharge month after learning that the current files misidentified the dual eligibility status of certain patient beneficiaries who die in the month of discharge. Although we have identified this issue, and do not believe that it is a substantive change to our policy for determining dual-eligibles, we believe that we should utilize the notice and comment rulemaking process to address this clarification because we do not currently have a subregulatory policy in place to address this type of data issue. However, we believe that a subregulatory process for addressing nonsubstantive data issues like the dual-eligible update could be used for similar situations in the future. Additionally, we would like to specify that decisions regarding substantive and nonsubstantive changes will be made in accordance with the recent Supreme Court ruling in Azar v. Allina Health Services, 587 U.S. ___, 139 S.Ct. 1804 (2019). We would publish these nonsubstantive data changes in the HSR User Guide annually. We note that we would continue to use notice and comment rulemaking for substantive changes.
With respect to what constitutes substantive changes versus nonsubstantive changes, we expect to make this determination on a case-by-case basis. In other quality reporting and quality payment programs (77 FR 53504), we stated that substantive changes are those that are so significant that the measures could no longer be considered the same measure. For this proposed policy, we would utilize the same principle; we would deem a change to be substantive and to require notice-and-comment rulemaking when the impact of the change to the payment adjustment factor component was so significant that it could no longer be considered to be the same as the previously finalized component. Examples of nonsubstantive changes would include, but not be limited to, updated naming or locations of data files and/or other minor discrepancies that do not change the intent of the policy. Examples of substantive changes to data might include use of different methodologies to use data than finalized for the payment adjustment factor component or the use of a different component in the methodology for payment calculations.
We received several public comments on our proposed subregulatory process for nonsubstantive updates to the payment adjustment factor components.
Comment: Several commenters supported our proposal to adopt a subregulatory process that would allow us to administer the Hospital Readmissions Reduction Program efficiently and address nonsubstantive requirements such as updating file names and or locations, the use of improved data files, or responses to unintended consequences of technical programmatic changes.
Response: We thank the commenters for their support.
Comment: Several commenters requested that CMS provide additional clarity on the proposed subregulatory process, including providing further definition of “nonsubstantive” and the criteria CMS would use to determine if something was nonsubstantive. A few other commenters urged CMS to better articulate the circumstances under which nonsubstantive changes can be made without formal review and comment from public stakeholders to ensure appropriate transparency.
Response: The proposed subregulatory process is intended to establish a mechanism to address nonsubstantive changes to the payment adjustment factor components used for the Program. Nonsubstantive updates are those that are technical in nature and include, but are not limited to, updates to file names or their locations, data processing through standard procedures and/or the correction of other minor discrepancies in data preparation that are required to implement the program, but do not change the intent of the previously finalized policies. We believe this subregulatory process is necessary because updates to previously finalized data sourcing and technical aspects of the components are not always linked to the timing of regulatory actions, such as rulemaking. Therefore, this policy will allow for the Program to use the most up-to-date, accurate files and data in payment adjustment calculations.
We believe this policy is particularly important as we are providing additional transparency into the Program's payment adjustment calculations. Beginning in FY 2020, we will begin providing additional details regarding the payment adjustment factors in the technical appendix of the HSR User Guide to provide greater insight and detail about the payment methodology, including information on how non-ERR components of the payment adjustment factor are calculated, such as information on the data processing used to prepare the analytic files for the payment adjustment factor calculations. This information includes details about our standard processing rules to produce clean data, such as the removal of duplicate stays, and the files used to produce aspects of the final payment adjustment factors. Depending on the state of the data received, or if files received by the program change due to factors outside of the program's control, the program would hope for flexibility to amend and update the nonsubstantive standard processing rules and data processing to ensure quality data are used for the payment adjustment calculations, rather than stall the program for lack of a mechanism to improve the data. We would similarly expect to use subregulatory policy to address other nonsubstantive updates that could have an impact on program operation.
Comment: Many commenters agreed that CMS should be able to make minor program changes without notice-and-comment rulemaking but urged CMS to develop safeguards that would require any programmatic changes impacting hospital performance or payment to be communicated in advance of implementation. These commenters suggested that the annual IPPS rulemaking process provides hospitals with a predictable opportunity to review and provide input on policy changes that could affect their performance in the program. Several commenters also noted that they believed that the proposal to change to the “dual-eligible” definition to allow for a one-month look back was a substantive change and would not have been appropriate to implement through the proposed subregulatory process.
Response: We thank the commenters for their support of the subregulatory process to address minor, nonsubstantive changes to the program, and acknowledge their desire for safeguards to ensure we do not use the policy to effect policy change. The proposed subregulatory policy is intended to serve as a mechanism to address nonsubstantive changes and ensure that the Program can rapidly implement updates to technical issues. It is not intended to address substantive policy changes outside of notice-and-comment rulemaking, nor would we use it in such a manner. As stated in our proposal, we intend to use the subregulatory policy for nonsubstantive changes that are purely technical in nature. When making determinations on whether to use the subregulatory process or not, we intend to adopt a conservative approach and ensure that the subregulatory policy is not used to alter or amend policies in a manner inconsistent with any previously finalized policy.
Additionally, we understand commenters' concerns about using the proposal to update the definition of “dual-eligible” in FY 2021 to allow for a one-month lookback as an example use case for the subregulatory process. We continue to believe that when minor, previously unknown discrepancies in data are discovered and those discrepancies frustrate but do not change the stated intent of our policies, a subregulatory process may be the best approach to address them in a timely manner. We will make those determinations on a case by case basis. We will take commenters' feedback into consideration for any future consideration of the application of the subregulatory process.
Comment: Several commenters expressed concerns that some nonsubstantive regulatory changes may result in significant changes for hospitals, such as programming measure changes, which could impact hospitals' internal monitoring systems. They encouraged CMS to establish a process for obtaining stakeholder input prior to making any changes to ensure the change is not substantive and to identify any burden or unintended consequences that may result from changes using the subregulatory process.
Response: We thank the commenters for this feedback. We plan to communicate any subregulatory changes to the payment adjustment factors via our standard outreach channels, most notably the HSR User Guides, which hospitals receive annually with their HSRs at the start of the review and correction period. Additionally, the HSR User Guide is posted on QualityNet at the start of the review and correction period. Because the subregulatory policy is intended to facilitate technical aspects of the program calculations, we expect that subregulatory changes will only impact internal CMS processes and do not expect these updates to impact hospitals' internal monitoring systems or create additional burden for hospitals.
After consideration of the public comments we received, we are finalizing our policy to adopt a subregulatory process to make nonsubstantive updates to payment adjustment factor components to facilitate the program's operation when minor changes are required, but do not substantively impact the program's previously finalized policies.
7. Applicable Period for FY 2022
We refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51671) and the FY 2013 IPPS/LTCH PPS final rule (77 FR 53675) for discussion of our previously finalized policy for defining applicable periods. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41434 through 41435), we finalized the following “applicable periods” to calculate the readmission payment adjustment factor for FY 2019, FY 2020, and FY 2021, respectively:
- The 3-year time period of July 1, 2014 through June 30, 2017 for FY 2019;
- The 3-year time period of July 1, 2015 through June 30, 2018 for FY 2020; and
- The 3-year time period of July 1, 2016 through June 30, 2019 for FY 2021.
These are the 3-year periods from which data are being collected in order to calculate ERRs and payment adjustment factors for the fiscal year; this includes aggregate payments for excess readmissions and aggregate payments for all discharges used in the calculation of the payment adjustment. The “applicable period” for dual-eligibles is the same as the “applicable period” that we otherwise adopt for purposes of the Hospital Readmissions Reduction Program.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19426), we proposed, for FY 2022, consistent with the definition specified at § 412.152, that the “applicable period” for the Hospital Readmissions Reduction Program would be the 3-year period from July 1, 2017 through June 30, 2020. The applicable period for dual-eligibles for FY 2022 would similarly be the 3-year period from July 1, 2017 through June 30, 2020.
We received one comment on the proposed applicable period for FY 2022.
Comment: A commenter supported CMS's proposal to continue using a three-year performance period for the Program.
Response: We thank the commenter for the support.
After consideration of the public comments that we received, we are finalizing the applicable periods for the Hospital Readmissions Reduction Program as proposed.
8. Identification of Aggregate Payments for Each Condition/Procedure and All Discharges for FY 2020
When calculating the numerator (aggregate payments for excess readmissions), we determine the base operating DRG payment amount for an individual hospital for the applicable period for such condition/procedure, using Medicare inpatient claims from the MedPAR file with discharge dates that are within the applicable period. Under our established methodology, we use the update of the MedPAR file for each Federal fiscal year, which is updated 6 months after the end of each Federal fiscal year within the applicable period, as our data source.
In identifying discharges for the applicable conditions/procedures to calculate the aggregate payments for excess readmissions, we apply the same exclusions to the claims in the MedPAR file as are applied in the measure methodology for each of the applicable conditions/procedures. For the FY 2020 applicable period, this includes the discharge diagnoses for each applicable condition/procedure based on a list of specific ICD-9-CM or ICD-10-CM and ICD-10-PCS code sets, as applicable, for that condition/procedure, because diagnoses and procedure codes for discharges occurring prior to October 1, 2015 were reported under the ICD-9-CM code set, while discharges occurring on or after October 1, 2015 (FY 2016), were reported under the ICD-10-CM and ICD-10-PCS code sets.
We identify Medicare fee-for-service (FFS) claims that meet the criteria previously described for each applicable condition/procedure to calculate the aggregate payments for excess readmissions (that is, claims paid for under Medicare Part C (Medicare Advantage) are not included in this calculation). This policy is consistent with the methodology to calculate ERRs based solely on admissions and readmissions for Medicare FFS patients. Therefore, consistent with our established methodology, for FY 2020, we proposed to continue to exclude admissions for patients enrolled in Medicare Advantage, as identified in the Medicare Enrollment Database.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19426 through 19427), for FY 2020, we proposed to determine aggregate payments for excess readmissions, aggregate payments for all discharges using data from MedPAR claims with discharge dates that are on or after July 1, 2015, and not later than June 30, 2018. As we stated in FY 2018 IPPS/LTCH PPS final rule (82 FR 38232), we will determine the neutrality modifier using the most recently available full year of MedPAR data. However, we note that, for the purpose of modeling the estimated FY 2020 readmissions payment adjustment factors for this final rule, we used the proportion of dual-eligibles, excess readmission ratios, and aggregate payments for each condition/procedure and all discharges for applicable hospitals from the FY 2020 Hospital Readmissions Reduction Program applicable period. For the FY 2020 program year, applicable hospitals will have the opportunity to review and correct calculations based on the proposed FY 2020 applicable period of July 1, 2015 to June 30, 2018, before they are made public under our policy regarding reporting of hospital-specific information. Again, we reiterate that this period is intended to review the program calculations, and not the underlying data. For more information on the review and corrections process, we refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53399 through 53401).
In the proposed rule, for FY 2020, we proposed to use MedPAR data from July 1, 2015 through June 30, 2018 for the FY 2020 Hospital Readmissions Reduction Program calculations. Specifically—
- The March 2016 update of the FY 2015 MedPAR file to identify claims within FY 2015 with discharges dates that are on or after July 1, 2015;
- The March 2017 update of the FY 2016 MedPAR file to identify claims within FY 2016;
- The March 2018 update of the FY 2017 MedPAR file to identify claims within FY 2017; and
- The March 2019 update of the FY 2018 MedPAR file to identify claims within FY 2018 with discharge dates that are on or before June 30, 2018.
We did not receive any public comments on our proposal to use the MedPAR data from July 1, 2015 through June 30, 2018 for the FY 2020 Hospital Readmissions Reduction Program calculations. Therefore, we are finalizing the use of the MedPAR data from July 1, 2015 through June 30, 2018 for FY 2020 as proposed.
9. Calculation of Payment Adjustment Factors for FY 2020
As we discussed in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38226), section 1886(q)(3)(D) of the Act requires the Secretary to group hospitals and apply a methodology that allows for separate comparisons of hospitals within peer groups in determining a hospital's adjustment factor for payments applied to discharges beginning in FY 2019.
To implement this provision, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38226 through 38237), we finalized several changes to the payment adjustment methodology for FY 2019. First, we finalized that an individual would be counted as a full-benefit dual-eligible patient if the beneficiary was identified as full benefit- dual status in the State Medicare Modernization Act (MMA) files for the month he or she was discharged from the hospital (82 FR 38226 through 38228). Second, we finalized our policy to define the proportion of full benefit dual-eligible beneficiaries as the proportion of dual-eligible patients among all Medicare FFS and Medicare Advantage stays (82 FR 38226 through 38228). Third, we finalized our policy to define the data period for determining dual-eligibility as the 3-year data period corresponding to the Program's applicable period (82 FR 38229). Fourth, we finalized our policy to stratify hospitals into quintiles, or five peer groups, based on their proportion of dual-eligible patients (82 FR 38229 through 38231). Finally, we finalized our policy to use the median ERR for the hospital's peer group in place of 1.0 in the payment adjustment formula and apply a uniform modifier to maintain budget neutrality (82 FR 38231 through 38237). The payment adjustment formula would then be:

where dx is AMI, HF, pneumonia, COPD, THA/TKA or CABG and payments refers to the base operating DRG payments. The payment reduction (1-P) resulting from use of the median ERR for the peer group is scaled by a neutrality modifier to achieve budget neutrality. We refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38226 through 38237) for a detailed discussion of the payment adjustment methodology. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19427), we did not propose any changes to this payment adjustment calculation methodology for FY 2020.
10. Calculation of Payment Adjustment for FY 2020
Section 1886(q)(3)(A) of the Act defines the payment adjustment factor for an applicable hospital for a fiscal year as “equal to the greater of: (i) The ratio described in subparagraph (B) for the hospital for the applicable period (as defined in paragraph (5)(D)) for such fiscal year; or (ii) the floor adjustment factor specified in subparagraph (C).” Section 1886(q)(3)(B) of the Act, in turn, describes the ratio used to calculate the adjustment factor. Specifically, it states that the ratio is equal to 1 minus the ratio of (i) the aggregate payments for excess readmissions, and (ii) the aggregate payments for all discharges, scaled by the neutrality modifier. The calculation of this ratio is codified at § 412.154(c)(1) of the regulations and the floor adjustment factor is codified at § 412.154(c)(2) of the regulations. Section 1886(q)(3)(C) of the Act specifies the floor adjustment factor at 0.97 for FY 2015 and subsequent fiscal years.
Consistent with section 1886(q)(3) of the Act, codified in our regulations at § 412.154(c)(2), for FY 2020, the payment adjustment factor will be either the greater of the ratio or the floor adjustment factor of 0.97. Under our established policy, the ratio is rounded to the fourth decimal place. In other words, for FY 2020, a hospital subject to the Hospital Readmissions Reduction Program would have an adjustment factor that is between 1.0 (no reduction) and 0.9700 (greatest possible reduction).
For additional information on the FY 2020 payment calculation, we refer readers to the QualityNet website at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776124112.
11. Confidential Reporting of Stratified Data for Hospital Quality Measures
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19427 through 19128), we noted that beginning as early as the spring of 2020, CMS plans to include in confidential hospital-specific reports (HSR) data stratified by patient dual eligible status for the six readmissions measures included in the Hospital Readmissions Reduction Program. These data will include two disparity methodologies designed to illuminate potential disparities within individual hospitals and across hospitals nationally and will supplement the measure data currently publicly reported on the Hospital Compare website. The first methodology, the Within-Hospital Disparity Method highlights differences in outcomes for dual eligible versus non-dual eligible patients within an individual hospital, while the second methodology, the Dual Eligible Outcome Method, allows for a comparison of performance in care for dual-eligible patients across hospitals (82 FR 38405 through 38407; 83 FR 41598). These two disparity methods are separate from the stratified methodology used by the Hospital Readmissions Reduction Program, and we emphasize that the two disparity methods would not be used in payment adjustment factors calculations under the Hospital Readmissions Reduction Program. We believe that providing the results of both disparity methods alongside a hospital's measure data as a point of reference allows for a more meaningful comparison and comprehensive assessment of the quality of care for patients with social risk factors and the identification of providers where disparities in health care may exist. We also believe the two disparity methods provide additional perspectives on health care equity (83 FR 41598).
We believe hospitals can use their results from the disparity methods to identify and develop strategies to reduce disparities in the quality of care for patients through targeted improvement efforts (83 FR 41598). The two disparity methods and the stratified methodology used by the Hospital Readmissions Reduction Program are part of CMS' broader effort to account for social risk factors in quality measurement and quality payment programs. We refer readers to section VIII.A.9. of the preamble of this final rule for more information on confidential reporting of stratified data for hospital quality measures. We further refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 57167 through 57168), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38324 through 38326; 82 FR 38403 through 38409), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41597 through 41601) for detailed discussions on disparity reporting.
We note that the two disparity methods do not place any additional collection or reporting burden on hospitals because dual-eligibility data are readily available in claims data. In addition, we reiterate that these confidential hospital-specific reports data do not impact the calculation of hospital payment adjustment factors under the Hospital Readmissions Reduction Program.
We received a number of public comments on our decision to provide hospitals with information from two disparity methods through confidential hospital-specific reports.
Comment: Many commenters supported CMS' plan to continue to provide hospitals with confidential hospital specific reports on the Pneumonia Readmission measure using the two disparity methods and to expand that effort to include five additional readmission measures. Several of these commenters specifically believed the effort would be useful to hospitals. Some commenters noted that it would help hospitals recognize potential disparities in care, implement targeted improvement efforts, and reduce disparities in the quality of care for this vulnerable population. A commenter specifically noted that differences in care based on beneficiaries' dual-eligible status is a reasonable social risk factor to begin assessing for disparities in care for quality measurement and value-based purchasing programs.
Response: We thank the commenters for their support for our efforts to provide data on disparities to hospitals. At present, dual-eligible status is the only social risk factor used for assessing disparities in hospital outcomes. We continue to explore the use of additional social risk factors for the hospital disparity methods.
Comment: Several commenters requested that CMS provide enough opportunity to review and understand the stratified performance and methodology used to develop these reports. They appreciated CMS's intention to remain engaged with stakeholders and to solicit feedback on hospital experiences and recommendations, including the format and usefulness of these reports. One commenter requested that CMS provide educational materials to help stakeholders interpret the information.
Response: We thank the commenters for their feedback. We intend to continue to provide educational resources for stakeholders as they continue to become familiar with the data provided from the two disparity methods provided in the confidential reports, including measure methodology overview, fact sheet, and frequently asked questions resources.[321] For additional information on the reliability of the measure data using the two disparity methods, we refer readers to the Hospital IQR Program's discussion in section VIII.A.9. of the preamble of this final rule.
Comment: A commenter suggested that attribution details for each measure be included within the respective programs' measures' technical specifications guides before publicly reporting data using the two disparity methods because they believed it is important to be clear about who is responsible for the reported outcomes and performance rates.
Response: To minimize the possibility of confusion, the attribution used when applying the disparity methods mirror those used by the corresponding measure in the Hospital Readmissions Reduction Program. Attribution details and other technical specifications for the readmission measures are publicly available in Measure Methodology Reports on our QualityNet website.[322]
Comment: A commenter expressed the belief that additional information in the confidential HSRs will help CMS make appropriate decisions as it considers disparity and risk-adjustment. A commenter encouraged CMS to study the differences between the disparity methodologies and Hospital Readmissions Reduction Program methodology.
Response: We thank the commenters for their feedback. We intend to continue to engage with hospitals and relevant stakeholders about their experiences with and recommendations for the data from the two disparity methods and to ensure the reliability of such data. We appreciate commenter's feedback regarding the harmonization with existing quality programs including the Hospital Readmission Reduction Program. We believe these two disparity methods complement each other in that they use the same social risk factor and serve two complementary purposes. The Hospital Readmissions Reduction Program stratifies hospitals based on dual-eligible proportion and compares a hospital's excess readmissions to other hospitals in its peer group to assess a hospital's performance, as mandated by the 21st Century Cures Act, whereas the disparities methods discussed in this section highlight opportunities to close the gap in performance among different patient groups. We also reiterate that the confidential reporting of disparity factors does not impact the payment adjustment factors for the Hospital Readmissions Reduction Program. We will continue to engage with hospitals and relevant stakeholders about their experiences with the two disparity methods.
Comment: Several commenters urged CMS to seek recommendations on the measure data and ensure that the data is reliable and easily understandable before any future proposals to publicly report the information. A commenter strongly supported sharing confidential HSR reports with the public for both the within-hospital and across-hospital disparity information because it believes this data should be available and transparent to the public and further stated its opposition to the use of any social risk-adjustment in measures. Another commenter believed this information should only be made public after the hospitals have had time to review and correct their data and that unadjusted data should be publicly available to enable communities to study and improve interventions to address disparities. A few commenters discouraged the use of any unadjusted data in public reporting or pay-for-performance measures.
Response: We thank the commenters for their feedback. We have not yet determined future plans with respect to publicly reporting data using the two disparity methods and intend to continue to engage with hospitals and relevant stakeholders about their experiences with and recommendations for the data from the two disparity methods and to ensure the reliability of such data before proposing to publicly display results from the two disparity methods in the future.
Comment: A few commenters expressed concern with stratifying measure data based only on dual eligible status. A commenter noted that dual eligibility may be sensitive to differences in state coverage and benefit policies, and may not fully reflect the level of poverty in communities.
Response: At present, dual eligibility is the only social risk factor used in the disparity methods. We have focused our initial efforts on providing disparity results based on dual eligible status because of strong evidence demonstrating worse health outcomes among dual eligible Medicare beneficiaries, and because reliable information is readily available in CMS administrative claims data. Because dual eligible status is available in CMS administrative data, it also does not require any additional reporting by hospitals for the purposes of applying the disparity methods. With respect to commenter's concern about the differences in state policies, the disparity methods evaluate differences in hospital quality only for adults 65 years and older. Federal minimum standards for allowable income and assets exist for older adults, contributing to more uniformity in Medicaid eligibility status across states relative to other groups, although state-level differences in eligibility standards for optional coverage pathways and benefits are noted. Our internal analyses accounting for state Medicaid eligibility policies reveal no substantive differences in the disparity method results. We continue to examine the impact of state Medicaid policies on the disparity methods.
We thank the commenters for their feedback and suggestions. We will take them into account and consider commenters' views as we develop future policies regarding the confidential reporting of disparity data. For additional information on the confidential reporting of stratified data for hospital quality measures, we refer readers to the Hospital IQR Program's discussion in section VIII.A.9. of the preamble of this final rule.
12. Revisions of Regulatory Text
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19428), we proposed to revise 42 CFR 412.152 to reflect our proposed policies and to codify previously finalized policies. Specifically, we proposed to revise the definition of “aggregate payments for excess readmissions”, as discussed earlier, to specify that it means the sum of the product for each applicable condition, among others, of “the excess readmission ratio for the hospital for the applicable period minus the peer group median excess readmission ratio” (instead of minus 1) (proposed paragraph (3) of the definition) and to include the neutrality modifier—a multiplicative factor that equates total Medicare savings under the current stratified methodology to the previous non-stratified methodology (proposed paragraph (4) of the definition).
We proposed to revise the definition of “applicable condition” to include other conditions and procedures as determined appropriate by the Secretary. In expanding the applicable conditions, the Secretary will seek endorsement of the entity with a contract under section 1890(a) of the Act, but may apply such measures without such an endorsement in the case of a specified area or medical topic determined appropriate by the Secretary for which a feasible and practical measure has not been endorsed by the entity with a contract under section 1890(a) of the Act as long as due consideration is given to measures that have been endorsed or adopted by a consensus organization identified by the Secretary.
We proposed to revise the definition of “base operating DRG payment amount”, with respect to a sole community hospital that receives payments under § 412.92(d) or a Medicare-dependent, small rural hospital that receives payments under § 412.108(c), to remove the applicability date of FY 2013, and to specify that this amount also includes the difference between the hospital-specific payment rate and the Federal payment rate determined under the subpart for a Medicare-dependent, small rural hospital that receives payments under § 412.108(c) and does not include the difference between the hospital-specific payment rate and the Federal payment rate determined under the subpart for a sole community hospital that receives payment under § 412.92(d).[323] This proposal was intended to align the regulatory text with section 1886(q)(2)(B)(i) of the Act by specifying the differential treatment following the expiration of the special treatment for Medicare-dependent, small rural hospitals for FY 2013 in the statute.
We proposed to revise the definition of “dual-eligible” to specify that, for payment adjustment factors beginning in FY 2021, dual-eligible is a patient beneficiary who has been identified as having full benefit status in both the Medicare and Medicaid programs in data sourced from the State MMA files for the month the beneficiary was discharged from the hospital except for those patient beneficiaries who die in the month of discharge, which will be identified using the previous month's data as sourced from the State MMA files, as discussed earlier.
We proposed to revise § 412.154(e) to specify that the limitations on administrative or judicial review would include the neutrality modifier and the proportion of dual-eligibles as discussed earlier (proposed new paragraphs (e)(4) and (5); existing paragraph (e)(4) would be redesignated as paragraph (e)(6)).
As discussed in section IV.G.5. of the preamble of this final rule, we received a number of supportive comments on our proposal to update the definition of “dual-eligible” beginning in FY 2021, which we addressed previously in this rule. We did not receive any public comments on our other proposals to update the regulatory text to align with previously finalized policies.
After consideration of the public comments we received, we are finalizing our proposal to update the regulatory text as proposed.
H. Hospital Value-Based Purchasing (VBP) Program: Policy Changes
1. Background
a. Statutory Background and Overview of Past Program Years
Section 1886(o) of the Act requires the Secretary to establish a hospital value-based purchasing program (the Hospital VBP Program) under which value-based incentive payments are made in a fiscal year (FY) to hospitals that meet performance standards established for a performance period for such fiscal year. Both the performance standards and the performance period for a fiscal year are to be established by the Secretary.
For more of the statutory background and descriptions of our current policies for the Hospital VBP Program, we refer readers to the Hospital Inpatient VBP Program final rule (76 FR 26490 through 26547); the FY 2012 IPPS/LTCH PPS final rule (76 FR 51653 through 51660); the CY 2012 OPPS/ASC final rule with comment period (76 FR 74527 through 74547); the FY 2013 IPPS/LTCH PPS final rule (77 FR 53567 through 53614); the FY 2014 IPPS/LTCH PPS final rule (78 FR 50676 through 50707); the CY 2014 OPPS/ASC final rule (78 FR 75120 through 75121); the FY 2015 IPPS/LTCH PPS final rule (79 FR 50048 through 50087); the FY 2016 IPPS/LTCH PPS final rule (80 FR 49544 through 49570); the FY 2017 IPPS/LTCH PPS final rule (81 FR 56979 through 57011); the CY 2017 OPPS/ASC final rule with comment period (81 FR 79855 through 79862); the FY 2018 IPPS/LTCH PPS final rule (82 FR 38240 through 38269); and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41440 through 41472).
We also have codified certain requirements for the Hospital VBP Program at 42 CFR 412.160 through 412.167.
b. FY 2020 Program Year Payment Details
Section 1886(o)(7)(B) of the Act instructs the Secretary to reduce the base operating DRG payment amount for a hospital for each discharge in a fiscal year by an applicable percent. Under section 1886(o)(7)(A) of the Act, the sum total of these reductions in a fiscal year must equal the total amount available for value-based incentive payments for all eligible hospitals for the fiscal year, as estimated by the Secretary. We finalized details on how we would implement these provisions in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53571 through 53573), and we refer readers to that rule for further details.
Under section 1886(o)(7)(C)(v) of the Act, the applicable percent for the FY 2020 program year is 2.00 percent. Using the methodology we adopted in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53571 through 53573), we estimate that the total amount available for value-based incentive payments for FY 2020 is approximately $1.9 billion, based on the March 2019 update of the FY 2018 MedPAR file.
As finalized in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53573 through 53576), we will utilize a linear exchange function to translate this estimated amount available into a value-based incentive payment percentage for each hospital, based on its Total Performance Score (TPS). Then, we will calculate a value-based incentive payment adjustment factor that will be applied to the base operating DRG payment amount for each discharge occurring in FY 2020, on a per-claim basis. We published proxy value-based incentive payment adjustment factors in Table 16 associated with the FY 2020 IPPS/LTCH PPS proposed rule (which is available via the internet on the CMS website). We are publishing updated proxy value-based incentive payment adjustment factors in Table 16A associated with this final rule (which is available via the internet on the CMS website). The proxy factors are based on the TPSs from the FY 2019 program year. These FY 2019 performance scores are the most recently available performance scores hospitals have been given the opportunity to review and correct. The updated slope of the linear exchange function used to calculate the proxy value-based incentive payment adjustment factors in Table 16A is 2.8392502375. This slope, along with the estimated amount available for value-based incentive payments, has been updated based on the March 2019 update to the FY 2018 MedPAR file and is also published in Table 16A (which is available via the internet on the CMS website).
After hospitals have been given an opportunity to review and correct their actual TPSs for FY 2020, we will post Table 16B (which will be available via the internet on the CMS website) to display the actual value-based incentive payment adjustment factors, exchange function slope, and estimated amount available for the FY 2020 program year. We expect Table 16B will be posted on the CMS website in the fall of 2019.
2. Retention and Removal of Quality Measures
a. Retention of Previously Adopted Hospital VBP Program Measures and Relationship Between the Hospital IQR and Hospital VBP Program Measure Sets
In the FY 2013 IPPS/LTCH PPS final rule (77 FR 53592), we finalized a policy to retain measures from prior program years for each successive program year, unless otherwise proposed and finalized. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41440 through 41441), we finalized a revision to our regulations at 42 CFR 412.164(a) to clarify that once we have complied with the statutory prerequisites for adopting a measure for the Hospital VBP Program (that is, we have selected the measure from the Hospital IQR Program measure set and included data on that measure on Hospital Compare for at least 1 year prior to its inclusion in a Hospital VBP Program performance period), the Hospital VBP Program statute does not require that the measure continue to remain in the Hospital IQR Program. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19429), we did not propose any changes to these policies.
b. Measure Removal Factors for the Hospital VBP Program
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41441 through 41446), in alignment with the Hospital IQR Program, we finalized all of the following measure removal factors for the Hospital VBP Program:
- Factor 1. Measure performance among hospitals is so high and unvarying that meaningful distinctions and improvements in performance can no longer be made (“topped out” measures), defined as: Statistically indistinguishable performance at the 75th and 90th percentiles; and truncated coefficient of variation ≤0.10.[324]
- Factor 2. A measure does not align with current clinical guidelines or practice.
- Factor 3. The availability of a more broadly applicable measure (across settings or populations), or the availability of a measure that is more proximal in time to desired patient outcomes for the particular topic.
- Factor 4. Performance or improvement on a measure does not result in better patient outcomes.
- Factor 5. The availability of a measure that is more strongly associated with desired patient outcomes for the particular topic.
- Factor 6. Collection or public reporting of a measure leads to negative unintended consequences other than patient harm.
- Factor 7. It is not feasible to implement the measure specifications.
- Factor 8. The costs associated with a measure outweigh the benefit of its continued use in the program.
We noted that these removal factors will be considerations taken into account when deciding whether or not to remove measures, not firm requirements. We continue to believe that there may be circumstances in which a measure that meets one or more factors for removal should be retained regardless, because the drawbacks of removing a measure could be outweighed by other benefits to retaining the measure. In addition, to further align with policies adopted in the Hospital IQR Program (74 FR 43864), in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41446), we finalized a policy that if we believe continued use of a measure poses specific patient safety concerns, we may promptly remove the measure from the program without rulemaking and notify hospitals and the public of the removal of the measure along with the reasons for its removal through routine communication channels and then confirm the removal of the measure from the Hospital VBP Program measure set in rulemaking. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19429), we did not propose any changes to these policies.
c. Summary of Previously Adopted Measures for the FY 2022 and FY 2023 Program Years
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41454 through 41456) and to the tables in this section showing summaries of previously adopted measures for the FY 2022 and FY 2023 program years. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19429 through 19431), we did not propose to add new measures to or remove measures from the Hospital VBP Program.


3. Previously Adopted Baseline and Performance Periods
a. Background
Section 1886(o)(4) of the Act requires the Secretary to establish a performance period for the Hospital VBP Program that begins and ends prior to the beginning of such fiscal year. We refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 56998 through 57003) for baseline and performance periods that we have adopted for the FY 2019, FY 2020, FY 2021, and FY 2022 program years. In the same final rule, we finalized a schedule for all future baseline and performance periods for previously adopted measures. We refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38256 through 38261) and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41466 through 41469) for additional baseline and performance periods that we have adopted for the FY 2022, FY 2023, and subsequent program years.
b. Person and Community Engagement Domain
Since the FY 2015 program year, we have adopted a 12-month baseline period and a 12-month performance period for measures in the Person and Community Engagement domain (previously referred to as the Patient- and Caregiver-Centered Experience of Care/Care Coordination domain) (77 FR 53598; 78 FR 50692; 79 FR 50072; 80 FR 49561). In the FY 2017 IPPS/LTCH PPS final rule (81 FR 56998), we finalized our proposal to adopt a 12-month performance period for the Person and Community Engagement domain that runs on the calendar year 2 years prior to the applicable program year and a 12-month baseline period that runs on the calendar year 4 years prior to the applicable program year, for the FY 2019 program year and subsequent years.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19431), we did not propose any changes to these policies.
c. Clinical Outcomes Domain
For the FY 2020 and FY 2021 program years, we adopted a 36-month baseline period and a 36-month performance period for measures in the Clinical Outcomes domain (previously referred to as the Clinical Care domain) (79 FR 50073; 80 FR 49563 through 49564). In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57001), we also adopted a 22-month performance period and a 36-month baseline period specifically for the MORT-30-PN (updated cohort) measure for the FY 2021 program year.
In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57000), we adopted a 36-month performance period and a 36-month baseline period for the FY 2022 program year for each of the previously finalized measures in the Clinical Outcomes domain—that is, the MORT-30-AMI, MORT-30-HF, MORT-30-COPD, COMP-HIP-KNEE, and MORT-30-CABG measures. In the same final rule, we adopted a 34-month performance period and a 36-month baseline period for the MORT-30-PN (updated cohort) measure for the FY 2022 program year.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38259), we adopted a 36-month performance period and a 36-month baseline period for the MORT-30-AMI, MORT-30-HF, MORT-30-COPD, MORT-30-CABG, MORT-30-PN (updated cohort), and COMP-HIP-KNEE measures for the FY 2023 program year and subsequent years. Specifically, for the mortality measures (MORT-30-AMI, MORT-30-HF, MORT-30-COPD, MORT-30-CABG, and MORT-30-PN (updated cohort)), the performance period runs for 36 months from July 1, 5 years prior to the applicable fiscal program year, to June 30, 2 years prior to the applicable fiscal program year, and the baseline period runs for 36 months from July 1, 10 years prior to the applicable fiscal program year, to June 30, 7 years prior to the applicable fiscal program year. For the COMP-HIP-KNEE measure, the performance period runs for 36 months from April 1, 5 years prior to the applicable fiscal program year, to March 31, 2 years prior to the applicable fiscal program year, and the baseline period runs for 36 months from April 1, 10 years prior to the applicable fiscal program year, to March 31, 7 years prior to the applicable fiscal program year.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19431), we did not propose any changes to the length of these performance or baseline periods.
d. Safety Domain
In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57000), we finalized our proposal to adopt a performance period for all measures in the Safety domain—with the exception of the CMS Patient Safety and Adverse Events Composite (CMS PSI 90) measure—that runs on the calendar year 2 years prior to the applicable program year and a baseline period that runs on the calendar year 4 years prior to the applicable program year for the FY 2019 program year and subsequent program years.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38258), for the FY 2023 program year, we adopted a 21-month baseline period (October 1, 2015 to June 30, 2017) and a 24-month performance period (July 1, 2019 to June 30, 2021) for the CMS PSI 90 measure. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38258 through 38259), we adopted a 24-month performance period and a 24-month baseline period for the CMS PSI 90 measure for the FY 2024 program year and subsequent years. Specifically, the performance period runs from July 1, 4 years prior to the applicable fiscal program year, to June 30, two years prior to the applicable fiscal program year, and the baseline period runs from July 1, 8 years prior to the applicable fiscal program year, to June 30, 6 years prior to the applicable fiscal program year.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19431), we did not propose any changes to these policies.
e. Efficiency and Cost Reduction Domain
Since the FY 2016 program year, we have adopted a 12-month baseline period and a 12-month performance period for the MSPB measure in the Efficiency and Cost Reduction domain (78 FR 50692; 79 FR 50072; 80 FR 49562). In the FY 2017 IPPS/LTCH PPS final rule (81 FR 56998), we finalized our proposal to adopt a 12-month performance period for the MSPB measure that runs on the calendar year 2 years prior to the applicable program year and a 12-month baseline period that runs on the calendar year 4 years prior to the applicable program year for the FY 2019 program year and subsequent years.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19431 through 19432), we did not propose any changes to these policies.
f. Summary of Previously Adopted Baseline and Performance Periods for the FY 2022 Through FY 2025 Program Years
These tables summarize the baseline and performance periods that we have previously adopted.




4. Performance Standards for the Hospital VBP Program
a. Background
Section 1886(o)(3)(A) of the Act requires the Secretary to establish performance standards for the measures selected under the Hospital VBP Program for a performance period for the applicable fiscal year. The performance standards must include levels of achievement and improvement, as required by section 1886(o)(3)(B) of the Act, and must be established no later than 60 days before the beginning of the performance period for the fiscal year involved, as required by section 1886(o)(3)(C) of the Act. We refer readers to the Hospital Inpatient VBP Program final rule (76 FR 26511 through 26513) for further discussion of achievement and improvement standards under the Hospital VBP Program.
In addition, when establishing the performance standards, section 1886(o)(3)(D) of the Act requires the Secretary to consider appropriate factors, such as: (1) Practical experience with the measures, including whether a significant proportion of hospitals failed to meet the performance standard during previous performance periods; (2) historical performance standards; (3) improvement rates; and (4) the opportunity for continued improvement.
We refer readers to the FY 2013, FY 2014, and FY 2015 IPPS/LTCH PPS final rules (77 FR 53599 through 53605; 78 FR 50694 through 50699; and 79 FR 50077 through 50081, respectively) for a more detailed discussion of the general scoring methodology used in the Hospital VBP Program. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41469 through 41470) for previously established performance standards for the FY 2021 program year.
We note that the performance standards for all of the following measures are calculated with lower values representing better performance:
- CDC NHSN HAI measures (CLABSI, CAUTI, CDI, MRSA Bacteremia, and Colon and Abdominal Hysterectomy SSI).
- CMS PSI 90 measure.
- COMP-HIP-KNEE measure.
- MSPB measure.
This distinction is made in contrast to other measures—HCAHPS and the mortality measures, which use survival rates rather than mortality rates—for which higher values indicate better performance. As discussed further in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50684), the performance standards for the Colon and Abdominal Hysterectomy SSI measure are computed separately for each procedure stratum, and we first award achievement and improvement points to each stratum separately, and then compute a weighted average of the points awarded to each stratum by predicted infections.
b. Previously Established and Newly Established Performance Standards for the FY 2022 Program Year
In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57009), we established performance standards for the FY 2022 program year for the Clinical Outcomes domain measures (MORT-30-AMI, MORT-30-HF, MORT-30-PN (updated cohort), MORT-30-COPD, MORT-30-CABG, and COMP-HIP-KNEE) and the Efficiency and Cost Reduction domain measure (MSPB). We note that the performance standards for the MSPB measure are based on performance period data. Therefore, we are unable to provide numerical equivalents for the standards at this time.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19435 through 19437), in accordance with our methodology for calculating performance standards discussed more fully in the Hospital Inpatient VBP Program final rule (76 FR 26511 through 26513) and codified at 42 CFR 412.160, we estimated additional performance standards for the FY 2022 program year. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19436), we noted that the numerical values for the performance standards for the Safety and Person and Community Engagement domains for the FY 2022 program year were estimates based on the most recently available data, and that we intended to update the numerical values in the FY 2020 IPPS/LTCH PPS final rule.
The previously established and newly established performance standards for the measures in the FY 2022 program year are set out in these tables.

The eight dimensions of the HCAHPS measure are calculated to generate the HCAHPS Base Score. For each of the eight dimensions, Achievement Points (0-10 points) and Improvement Points (0-9 points) are calculated, the larger of which is then summed across the eight dimensions to create the HCAHPS Base Score (0-80 points). Each of the eight dimensions is of equal weight; therefore, the HCAHPS Base Score ranges from 0 to 80 points. HCAHPS Consistency Points are then calculated, which range from 0 to 20 points. The Consistency Points take into consideration the scores of all eight Person and Community Engagement dimensions. The final element of the scoring formula is the summation of the HCAHPS Base Score and the HCAHPS Consistency Points, which results in the Person and Community Engagement Domain score that ranges from 0 to 100 points.

c. Previously Established Performance Standards for Certain Measures for the FY 2023 Program Year
We have adopted certain measures for the Safety domain, Clinical Outcomes domain, and Efficiency and Cost Reduction domain for future program years in order to ensure that we can adopt baseline and performance periods of sufficient length for performance scoring purposes. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38264 through 38265), we established performance standards for the FY 2023 program year for the Clinical Outcomes domain measures (MORT-30-AMI, MORT-30-HF, MORT-30-PN (updated cohort), MORT-30-COPD, MORT-30-CABG, and COMP-HIP-KNEE) and for the Efficiency and Cost Reduction domain measure (MSPB). In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41471 through 41472), we established, for the FY 2023 program year, the performance standards for the Safety domain measure, CMS PSI 90. We note that the performance standards for the MSPB measure are based on performance period data. Therefore, we are unable to provide numerical equivalents for the standards at this time. The previously established performance standards for these measures are set out in these tables.

d. Previously Established and Newly Established Performance Standards for Certain Measures for the FY 2024 Program Year
We have adopted certain measures for the Safety domain, Clinical Outcomes domain, and Efficiency and Cost Reduction domain for future program years in order to ensure that we can adopt baseline and performance periods of sufficient length for performance scoring purposes. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41472), we established performance standards for the FY 2024 program year for the Clinical Outcomes domain measures (MORT-30-AMI, MORT-30-HF, MORT-30-PN (updated cohort), MORT-30-COPD, MORT-30-CABG, and COMP-HIP-KNEE) and the Efficiency and Cost Reduction domain measure (MSPB). We note that the performance standards for the MSPB measure are based on performance period data. Therefore, we are unable to provide numerical equivalents for the standards at this time.
In accordance with our methodology for calculating performance standards discussed more fully in the Hospital Inpatient VBP Program final rule (76 FR 26511 through 26513) and codified at 42 CFR 412.160, we are establishing performance standards for the CMS PSI 90 measure for the FY 2024 program year. The previously established and newly established performance standards for these measures are set out in this table.

e. Newly Established Performance Standards for Certain Measures for the FY 2025 Program Year
As previously discussed, we have adopted certain measures for the Clinical Outcomes domain (MORT-30-AMI, MORT-30-HF, MORT-30-PN (updated cohort), MORT-30-COPD, MORT-30-CABG, and COMP-HIP-KNEE) and the Efficiency and Cost Reduction domain (MSPB) for future program years in order to ensure that we can adopt baseline and performance periods of sufficient length for performance scoring purposes. In accordance with our methodology for calculating performance standards discussed more fully in the Hospital Inpatient VBP Program final rule (76 FR 26511 through 26513), and our performance standards definitions codified at 42 CFR 412.160, we are establishing the following performance standards for the FY 2025 program year for the Clinical Outcomes domain and the Efficiency and Cost Reduction domain. We note that the performance standards for the MSPB measure are based on performance period data. Therefore, we are unable to provide numerical equivalents for the standards at this time. The newly established performance standards for these measures are set out in this table.

5. Scoring Methodology and Data Requirements
a. Domain Weighting for the FY 2022 Program Year and Subsequent Years for Hospitals That Receive a Score on All Domains
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38266), we finalized our proposal to retain the equal weight of 25 percent for each of the four domains in the Hospital VBP Program for the FY 2020 program year and subsequent years for hospitals that receive a score in all domains. In FY 2019 IPPS/LTCH PPS rulemaking (83 FR 20416 through 20420; 41459 through 41464), we proposed, but did not adopt, any changes to the Hospital VBP Program domains and weighting. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19439), we did not propose any changes to these domain weights.
b. Domain Weighting for the FY 2022 Program Year and Subsequent Years for Hospitals Receiving Scores on Fewer Than Four Domains
In the FY 2015 IPPS/LTCH PPS final rule (79 FR 50084 through 50085), for the FY 2017 program year and subsequent years, we adopted a policy that hospitals must receive domain scores on at least three of four quality domains in order to receive a TPS, and hospitals with sufficient data on only three domains will have their TPSs proportionately reweighted. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19439), we did not propose any changes to these domain weights.
c. Minimum Numbers of Measures for Hospital VBP Program Domains
Based on our previously finalized policies (82 FR 38266), for a hospital to receive domain scores for the FY 2021 program year and subsequent years:
- A hospital must report a minimum number of 100 completed HCAHPS surveys for a hospital to receive a Person and Community Engagement domain score.
- A hospital must receive a minimum of two measure scores within the Clinical Outcomes domain to receive a Clinical Outcomes domain score.
- A hospital must receive a minimum of two measure scores within the Safety domain to receive a Safety domain score.
- A hospital must receive a minimum of one measure score within the Efficiency and Cost Reduction domain to receive an Efficiency and Cost Reduction domain score.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19439), we did not propose any changes to these policies.
d. Minimum Numbers of Cases for Hospital VBP Program Measures
(1) Background
Section 1886(o)(1)(C)(ii)(IV) of the Act requires the Secretary to exclude for the fiscal year hospitals that do not report a minimum number (as determined by the Secretary) of cases for the measures that apply to the hospital for the performance period for the fiscal year. For additional discussion of the previously finalized minimum numbers of cases for measures under the Hospital VBP Program, we refer readers to the Hospital Inpatient VBP Program final rule (76 FR 26527 through 26531); the CY 2012 OPPS/ASC final rule (76 FR 74532 through 74534); the FY 2013 IPPS/LTCH PPS final rule (77 FR 53608 through 53610); the FY 2015 IPPS/LTCH PPS final rule (79 FR 50085 through 50086); the FY 2016 IPPS/LTCH PPS final rule (80 FR 49570); the FY 2017 IPPS/LTCH PPS final rule (81 FR 57011); the FY 2018 IPPS/LTCH PPS final rule (82 FR 38266 through 38267); and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41465 through 41466). In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19439), we did not propose any changes to these policies.
(2) Summary of Previously Adopted Minimum Numbers of Cases
The previously adopted minimum numbers of cases for these measures are set forth in this table.

e. Administrative Policies for NHSN Healthcare-Associated Infection (HAI) Measure Data
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41553), beginning with the CY 2020 reporting period, the Hospital IQR Program finalized removal of the five CDC NHSN HAI measures that are used in both the Hospital VBP and HAC Reduction Programs (CAUTI, CLABSI, Colon and Abdominal Hysterectomy SSI, MRSA Bacteremia, and CDI). Since these measures were adopted in the Hospital VBP Program, the Hospital VBP Program has used the same data to calculate the CDC NHSN HAI measures that are used by the Hospital IQR Program. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41475 through 41478), the HAC Reduction Program adopted data collection policies for the CDC NHSN HAI measures, beginning on January 1, 2020 with CY 2020 submissions, which will use the same process as the Hospital IQR Program for hospitals to report, review, and correct CDC NHSN HAI measure data. Furthermore, the HAC Reduction Program also adopted processes to validate the CDC NHSN HAI measures used in the HAC Reduction Program beginning with 3rd quarter 2020 discharges (83 FR 41478 through 41483). These processes are intended to reflect, to the greatest extent possible, the processes previously established for the Hospital IQR Program in order to aid continued hospital reporting through clear and consistent requirements. In section IV.I.7. of the preamble of this final rule, the HAC Reduction Program is finalizing additional refinements to its validation process for the CDC NHSN HAI measures in the HAC Reduction Program and discusses clarifications regarding validation processes.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19440), in order to streamline and simplify processes across hospital programs, we proposed that the Hospital VBP Program will use the same data to calculate the CDC NHSN HAI measures that the HAC Reduction Program uses for purposes of calculating the measures under that program, beginning on January 1, 2020 for CY 2020 data collection, which would apply to the Hospital VBP Program starting with data for the FY 2022 program year performance period. We stated that this proposed start date would align with the effective date of the removal of the measures from the Hospital IQR Program and the date when data on those measures will begin to be reported for the HAC Reduction Program, allowing for a seamless transition. We noted that the data used by the HAC Reduction Program will be the same data previously used by the Hospital IQR Program, and therefore, we do not anticipate any changes in the use of such data for the Hospital VBP Program.
We also proposed that the Hospital VBP Program would use the same processes adopted by the HAC Reduction Program for hospitals to review and correct data for the CDC NHSN HAI measures and will rely on HAC Reduction Program validation to ensure the accuracy of CDC NHSN HAI measure data used in the Hospital VBP Program. We noted that the processes for hospitals to submit, review, and correct their data for these measures are the same processes previously used by the Hospital IQR Program. We stated our belief that using the HAC Reduction Program review and correction process would satisfy the requirement in section 1886(o)(10)(A)(ii) of the Act to allow hospitals to review and submit corrections for Hospital VBP Program information that will be made public with respect to each hospital. In addition, as we noted earlier, the HAC Reduction Program's validation processes are intended to reflect, to the greatest extent possible, the processes previously established for the Hospital IQR Program. We referred readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41478 through 41483) for a discussion of those processes in the HAC Reduction Program.[325] We stated our belief that relying on the HAC Reduction Program's validation process would be sufficient for purposes of ensuring the accuracy of CDC NHSN HAI measure data under the Hospital VBP Program. We also stated our belief that these policies will ensure that the use of the same data for the Hospital VBP Program will result in accurate measure scores under the Hospital VBP Program.
We referred readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41475 through 41484) for additional details on the HAC Reduction Program's data collection, review and correction, validation, and data accuracy policies for the CDC NHSN HAI measures. We also refer readers to sections IV.I.6. and IV.I.7. of the preamble of this final rule for additional information about HAC Reduction Program data collection, review and correction, and refinements to validation policies for the CDC NHSN HAI measures.
Comment: Several commenters supported using the same HAI measure administrative requirements for the Hospital VBP Program as used in the HAC Reduction Program. Several commenters specifically supported our proposal to use the same data to calculate the CDC NHSN HAI measures that the HAC Reduction Program uses for purposes of calculating the measures under that program. A few commenters specifically supported using the same policies and processes as the HAC Reduction Program for submitting, reviewing, correcting, and validating the HAI data within the Hospital VBP Program.
A few commenters believed using the same administrative requirements for the CDC NHSN HAI measures across the two programs would bring more consistency across programs. A few commenters believed using the same administrative requirements used in the HAC Reduction Program will help reduce administrative burden associated with the programs. A commenter believed that removing redundancy will lead to more focused quality reporting and targets for hospitals.
A few commenters supported adopting the HAC Reduction Program processes for validating the CDC NHSN HAI measures in the Hospital VBP Program because they believed the validation process under the HAC Reduction Program is sufficient for ensuring data integrity. A commenter supported relying on the HAC Reduction Program validation process and data to ensure the accuracy of the CDC NHSN HAI measure data in the Hospital VBP Program to avoid any duplication of validation processes and efforts since the HAI measures continue to remain in two payment programs.
Response: We thank commenters for their support.
Comment: A few commenters requested clarification on the proposal for the Hospital VBP Program to use the same data to calculate the CDC NHSN HAI measures that the HAC Reduction Program uses for purposes of calculating the measures under that program does not affect the previously adopted and differing measurement periods used for calculating performance under the Hospital VBP and HAC Reduction Programs. Such commenters noted that the measurement period for the CDC NHSN HAI measures is 2 calendar years for the HAC Reduction Program and 1 calendar year for the Hospital VBP Program.
Response: We did not propose any changes to the previously adopted baseline or performance periods of the CDC NHSN HAI measures for the Hospital VBP Program. In the FY 2017 IPPS/LTCH PPS final rule, we adopted a performance period for the CDC NHSN HAI measures in the Safety domain that runs on the calendar year 2 years prior to the applicable program year and a baseline period that runs on the calendar year 4 years prior to the applicable program year for the FY 2019 program year and subsequent program years (81 FR 57000). We also refer readers to section IV.H.3.f of the preamble of this final rule for a summary of previously adopted baseline and performance periods for the FY 2022 through FY 2025 Hospital VBP Program years.
Comment: Several commenters requested that CMS clarify how the results of the HAI measure validation in the HAC Reduction Program would affect hospital scoring and ability to participate in the Hospital VBP Program. Several commenters noted that hospitals that do not meet HAI measure validation requirements will receive the lowest possible HAC Reduction Program score for the measure(s) on which they do not meet validation requirements, that the Hospital VBP Program has both baseline and performance periods, and the Hospital VBP Program statute expressly excludes from participation in the Hospital VBP Program hospitals that do not meet Hospital IQR Program administrative requirements. A commenter expressed a belief that even though the process is the same across programs, CMS should evaluate compliance separately for each program. One commenter expressed concern that using the same measure or a variation of it in multiple quality-based programs would inappropriately penalize hospitals multiple times for the same issue. Several commenters urged CMS to engage with stakeholders to determine a process for scoring hospitals that fail HAI measure validation in the Hospital VBP Program.
Response: While there is no statutory provision that automatically excludes a hospital from participation in the Hospital VBP Program if it does not meet HAC Reduction Program measure validation requirements, we intend to look closely at the issue of whether a hospital not meeting HAI validation requirements in the HAC Reduction Program has unintended consequences for its participation in the Hospital VBP Program and if so, whether we should consider the feasibility of changes to the Hospital VBP scoring methodology that would address those unintended consequences. Any such changes to the Hospital VBP Program policies would be proposed in future rulemaking. We appreciate commenters' questions and concerns and will review the Hospital VBP Program policies accordingly.
Comment: A few commenters expressed concern with the proposal for the Hospital VBP Program to rely on the HAC Reduction Program validation of the CDC NHSN HAI measures, expressing concern with the adequacy of the HAC Reduction Program methods for validation of the data quality and noting that the changes proposed by the HAC Reduction Program in the FY 2019 IPPS/LTCH PPS proposed rule were solely on the selection process of hospitals for validation and not the methods for validation of the data elements.
Response: As noted in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19440), the validation processes adopted for the CDC NHSN HAI measures in the HAC Reduction Program are intended to reflect, to the greatest extent possible, the processes previously established for the Hospital IQR Program, therefore, we continue to believe the validation processes adopted for the CDC NHSN HAI measures in the HAC Reduction Program are sufficient for purposes of ensuring the accuracy of CDC NHSN HAI measure data under the Hospital VBP Program. We also note in section IV.I.7. of the preamble of this final rule, the HAC Reduction Program is finalizing additional refinements to its validation selection methodology for the CDC NHSN HAI measures in the HAC Reduction Program and discusses clarifications regarding validation processes. We refer readers to section IV.I.7. of the preamble of this final rule for further discussion of the CDC NHSN HAI measure validation under the HAC Reduction Program.
Comment: A few commenters expressed concern with using the same measures in both the Hospital VBP Program and HAC Reduction Program because of redundancy and a belief that it is inappropriate to penalize hospitals multiple times for the same issue, with a commenter requesting that CMS consider consolidating the programs to reduce duplication.
Response: In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41449 through 41452), we describe our previous proposal to de-duplicate the five HAI measures and the CMS PSI 90 measure from the Hospital VBP Program to reduce program complexity for hospitals, and our decision in response to stakeholder concerns to not finalize removal of these measures from the Hospital VBP Program. We stated that these measures cover topics of critical importance to quality improvement and patient safety in the inpatient hospital setting, and track infections and adverse events that could cause significant health risks and other costs to Medicare beneficiaries, and therefore, it is appropriate and important to provide appropriate incentives for hospitals to avoid them through inclusion in more than one program (83 FR 41450). We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FY 41449 through 41452) for further information regarding the decision to not remove the CDC NHSN HAI measures and CMS PSI 90 measure from the Hospital VBP Program. We also note that the Hospital VBP Program and HAC Reduction Program are each separately required by the Act. The Hospital VBP Program, required under section 1886(o) of the Act, is an incentive program that redistributes a portion of the Medicare payments made to hospitals under the IPPS based on their performance on a variety of measures. The HAC Reduction Program, as outlined in section 1886(p) of the Act, reduces payments to the lowest quartile of hospitals for excess hospital-acquired conditions in order to increase patient safety in hospitals.
Comment: A commenter urged CMS to provide greater detail on the future public reporting of the CDC NHSN HAI measures on Hospital Compare, specifically with regard to data refresh, reporting frequency, and display of hospital performance that is evaluable and consumer friendly.
Response: Section 1886(o)(10)(A) of the Act requires the Hospital VBP Program to make information available to the public regarding the performance of individual hospitals, including performance with respect to each measure that applies to the hospital, on the Hospital Compare website in an easily understandable format. We also note that section 1886(p)(6) of the Act requires the HAC Reduction Program to make information available to the public regarding hospital-acquired conditions of each applicable hospital on the Hospital Compare website in an easily understandable format. As discussed in the FY 2019 IPPS/LTCH PPS final rule, we intend to maintain as much consistency as possible in how the measures are currently reported on the Hospital Compare website, including how they are displayed and the frequency of reporting. We intend to continue making CDC NHSN HAI measure data available to the public on a quarterly basis as soon as it is feasible on CMS websites such as the Hospital Compare website and through downloadable files at: https://data.medicare.gov/, after a 30-day preview period. We appreciate commenters' feedback and will consider it as we continue to evaluate the presentation of information on the Hospital Compare website.
After consideration of the public comments we received, we are finalizing, as proposed, that the Hospital VBP Program will use the same data to calculate the CDC NHSN HAI measures that the HAC Reduction Program uses for purposes of calculating the measures under that program, beginning on January 1, 2020 for CY 2020 data collection, which would apply to the Hospital VBP Program starting with data for the FY 2022 program year performance period, and to use the same processes adopted by the HAC Reduction Program for hospitals to review and correct data for the CDC NHSN HAI measures and rely on HAC Reduction Program validation to ensure the accuracy of CDC NHSN HAI measure data used in the Hospital VBP Program.
I. Hospital-Acquired Condition (HAC) Reduction Program
1. Background
We refer readers to the FY 2014 IPPS/LTCH PPS final rule (78 FR 50707 through 50708) for a general overview of the HAC Reduction Program and to the same final rule (78 FR 50708 through 50709) for a detailed discussion of the statutory basis for the Program. For additional descriptions of our previously finalized policies for the HAC Reduction Program, we also refer readers to the FY 2014 IPPS/LTCH PPS final rule (78 FR 50707 through 50729), the FY 2015 IPPS/LTCH PPS final rule (79 FR 50087 through 50104), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49570 through 49581), the FY 2017 IPPS/LTCH PPS final rule (81 FR 57011 through 57026), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38269 through 38278), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41472 through 41492). These policies describe the general framework for the HAC Reduction Program's implementation, including: (1) The relevant definitions applicable to the program; (2) the payment adjustment under the program; (3) the measure selection process and conditions for the program, including a risk adjustment and scoring methodology; (4) performance scoring; (5) data collection; (6) validation; (7) the process for making hospital-specific performance information available to the public, including the opportunity for a hospital to review the information and submit corrections; and (8) limitation of administrative and judicial review. We remind readers that data collection and validation policies (items (5) and (6)) were newly finalized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41472 through 41492).
We have also codified certain requirements of the HAC Reduction Program at 42 CFR 412.170 through 412.172. In section IV.I.12. of the preamble of this final rule, we are finalizing our proposal to update 42 CFR 412.172(f) to reflect policies that we finalized in the FY 2019 IPPS/LTCH PPS final rule.
2. Implementation of the HAC Reduction Program for FY 2020
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41472 through 41492), we reviewed the HAC Reduction Program in the context of our Meaningful Measures Initiative. The HAC Reduction Program addresses the priority areas of making care safer by reducing harm caused in the delivery of care. The measures in the Program generally represent “never events” [326] and often, if not always, assess the incidence of preventable conditions. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41547 through 41553), for the Hospital IQR Program, as part of the Meaningful Measures Initiative, we deduplicated the CMS Patient Safety and Adverse Events Composite (CMS PSI 90) beginning with the Hospital IQR Program's FY 2020 payment determination, and the Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) Healthcare-Associated Infection (HAI) measures (CDC NHSN HAI measures) from the Hospital IQR Program beginning in CY 2020/FY 2022 payment determination. However, we retained these measures in the HAC Reduction Program because we believe these measures will continue to encourage hospitals to address the serious harm caused by these adverse events while still using the most parsimonious measure set available. To that end, however, we needed to adopt numerous HAC Reduction Program-specific CDC NHSN HAI measure policies, including data collection, validation requirements, and scoring associated with data completeness, timeliness, and accuracy, to transition the administrative processes on which the HAC Reduction Program had historically relied on the Hospital IQR Program to support. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41475 through 41484), for the HAC Reduction Program, we formally adopted analogous processes to manage these administrative processes independently and to receive CDC NHSN data beginning in CY 2020, with validation beginning with Q3 CY 2020 infectious events.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19440 through 19446), we proposed to clarify policies that we finalized for the HAC Reduction Program in the FY 2019 IPPS/LTCH PPS final rule so that they are implemented as intended. We specifically proposed to: (1) Adopt a measure removal policy that aligns with the removal factor policies previously adopted in other quality reporting and quality payment programs; (2) clarify administrative policies for validation of the CDC NHSN HAI measures; (3) adopt the data collection periods for the FY 2022 program year; and (4) update regulations for the HAC Reduction Program at 42 CFR 412.172(f) to reflect policies finalized in the FY 2019 IPPS/LTCH PPS final rule.
3. Current Measures for FY 2020 and Subsequent Years
The HAC Reduction Program has adopted six measures to date. In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50717), we finalized the use of five CDC NHSN HAI measures: (1) CAUTI; (2) CDI; (3) CLABSI; (4) Colon and Abdominal Hysterectomy SSI; and (5) MRSA Bacteremia. In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57014), we also finalized the use of the CMS PSI 90 measure. These previously finalized measures, with their full measure names, are shown in this table.[327]

In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19441 through 19442), we did not propose to add or remove any measures. However, we received several comments regarding the HAC Reduction Program's measure set. We would like to reassure stakeholders that we review the HAC Reduction Program's measure set on an ongoing basis to ensure that the program continues to maintain a parsimonious set of meaningful quality measures. While we consider these comments out of scope, we will take these comments into consideration for future policy making.
4. Measures Specification and Technical Specifications
As we stated in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50100 through 50101) and reiterated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41475), we will use a subregulatory process to make nonsubstantive updates to measures used for the HAC Reduction Program and use notice-and-comment rulemaking to adopt substantive updates to measures.
We did not propose to adopt any substantive changes to the measures this year. Technical specifications for the CMS PSI 90 measure can be found on the QualityNet website at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetBasic&cid=1228695355425. Technical specifications for the CDC NHSN HAI measures can be found at CDC's NHSN website at: http://www.cdc.gov/nhsn/acute-care-hospital/index.html. Both websites provide measure updates and other information necessary to guide hospitals participating in the collection of HAC Reduction Program data.
5. Measure Removal Factors
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19442), while we did not propose to remove any measures, we proposed to adopt a removal factor policy as part of our ongoing efforts to ensure that the HAC Reduction Program measure set continues to promote improved health outcomes for beneficiaries while minimizing the overall burden and costs associated with the program. In addition, the adoption of measure removal factors would align the HAC Reduction Program with our other quality reporting and quality payment programs and help ensure consistency in our measure evaluation methodology across programs.
In the FY 2019 IPPS/LTCH PPS final rule, we updated considerations for removing measures from several CMS quality reporting and quality payment programs. Specifically, we finalized eight measure removal factors for the Hospital IQR Program (83 FR 41540 through 41544), the Hospital VBP Program (83 FR 41441 through 41446), the PCHQR Program (83 FR 41609 through 41611), and the LTCH QRP (83 FR 41625 through 41627).
We believe these removal factors are also appropriate for the HAC Reduction Program, and we believe that alignment among CMS quality programs is important to provide stakeholders with a clear, consistent, and transparent process. Therefore, to align with our other quality reporting and quality payment programs, we proposed to adopt the following removal factors for the HAC Reduction Program:
- Factor 1. Measure performance among hospitals is so high and unvarying that meaningful distinctions and improvements in performance can no longer be made (“topped-out” measures).
- Factor 2. Measure does not align with current clinical guidelines or practice.
- Factor 3. Measure can be replaced by a more broadly applicable measure (across settings or populations) or a measure that is more proximal in time to desired patient outcomes for the particular topic.
- Factor 4. Measure performance or improvement does not result in better patient outcomes.
- Factor 5. Measure can be replaced by a measure that is more strongly associated with desired patient outcomes for the particular topic.
- Factor 6. Measure collection or public reporting leads to negative unintended consequences other than patient harm.[328]
- Factor 7. Measure is not feasible to implement as specified.
- Factor 8. The costs associated with a measure outweigh the benefit of its continued use in the program.[329]
We note that these removal factors are considerations taken into account when deciding whether or not to remove measures, not firm requirements, and that we will propose to remove measures based on these factors on a case-by-case basis. We continue to believe that there may be circumstances in which a measure that meets one or more factors for removal should be retained regardless because the benefits of a measure can outweigh its drawbacks. Our goal is to move the program forward in the least burdensome manner possible, while maintaining a parsimonious set of meaningful quality measures and continuing to incentivize improvement in the quality of care provided to patients.
We received several public comments on our proposed measure removal factors.
Comment: Several commenters supported the adoption of the eight measure removal factors previously adopted by the Hospital IQR Program and the Hospital VBP Program into the HAC Reduction Program. A few commenters stated that adoption of these factors would allow for consistency and alignment in measure evaluation methodology across programs. Some commenters also believed that the factors are well-established and ensure that a variety of valid reasons to remove a measure are considered by CMS. A few commenters also believed the proposal would reduce burden and increase efficiency.
Response: We thank the commenters for their support.
Comment: Some commenters encouraged CMS be transparent in how these factors are applied when a measure is considered for removal and urged CMS to use the factors as a guide to removal rather than an automatic process.
Response: As we stated in the proposed rule and as previously described, we consider these removal factors as considerations for removal, not firm requirements. We value transparency in our processes, and plan to seek stakeholder input through education and outreach, rulemaking, and other stakeholder engagement before removing measures.
Comment: A commenter opposed the adoption of the removal criteria because this commenter believed the criteria lack specificity and empirical support. The commenter believed that CMS should include more detail on how the removal factors apply to beneficiaries and develop and publicly share how the terminology in each criterion is operationalized. The commenter requested transparency around how such terms are tested and what results will empirically determine whether the criterion is met or not.
Response: As we discussed in the proposed rule, the removal factors are intended to be considerations that we take into account when deciding whether or not to remove measures. There may be circumstances in which a measure that meets one or more factors for removal should be retained regardless of the criteria because any benefit of removing a measure could be outweighed by benefits of retaining the measure. We intend to take multiple considerations and stakeholder feedback into account when determining whether to propose a measure for removal under any of the removal factors.
Comment: Several commenters supported removal Factor 1: “Measure performance among hospitals is so high and unvarying that meaningful distinctions and improvement in performance can no longer be made (“topped-out” measures),” but encouraged CMS to enhance the removal factor by adding quantitative criteria or empirical criteria similar to the criteria adopted by Hospital IQR and Hospital VBP Programs. Some commenters specifically recommended adding the “topped out” definition adopted by the Hospital IQR and Hospital VBP Programs (79 FR 50055):
- The difference in performance between the 75th and 90th percentile is statistically indistinguishable. In general, this means that the 75th and 90th percentile scores differ by less than two standard deviations.
- The truncated coefficient of variation (TCV) is less or equal to 0.10. Our definition of “truncated” is to remove the top and bottom 5 percent of hospitals before calculating the CV. Applying these two criteria to current data shows that the program's measure set may already be “topped out” in performance.
Response: Because the HAC Reduction Program focuses on patient safety and “never events,” the empirical criteria developed for the Hospital IQR and Hospital VBP Programs may not be appropriate for hospital-acquired conditions. The HAC Reduction Program strives to encourage hospitals to reduce HACs, not within a statistical standard, but to as close to zero as possible. While we do not believe that the Hospital IQR Program or Hospital VBP Programs' empirical standards are appropriate for HAC Reduction Program at this time, we will consider whether other statistical standards may be more appropriate for the HAC Reduction Program in the future. Therefore, we believe adding quantitative or empirical criteria at this time would be contrary to our holistic approach.
Comment: A few commenters opposed adoption of measure removal Factor 1, “measure performance among hospitals is so high and unvarying that meaningful distinctions and improvement in performance can no longer be made (“topped out” measures).” A commenter believed that removal of a measure immediately upon a “topped out” analysis would eliminate the ability to determine whether performance regresses or that the removal of the measure may result in lower quality of care over the long term. The commenter recommended CMS either consolidate measures that meet the “topped out” criteria but are still considered meaningful to stakeholders into a composite measure or include them as an evidence-based standard in a verification program. Another commenter believed that many measures are “never events” and a low prevalence still can be unacceptably high. The commenter also believed the quantitative criteria CMS uses for determining topped out status is problematic, as beneficiaries and payers often avoid the lowest performers, and that CMS's topped out methodology does not account for variation in lower performing percentiles; additionally, a potential high degree of variation outside of the narrow 75th to 90th percentiles is unaccounted for.
Response: As we discussed in the proposed rule, the removal factors are intended to be considerations taken into account when deciding whether or not to remove measures but are not firm requirements. There may be circumstances in which a measure that meets one or more factors for removal should be retained regardless, because any benefit of removing a measure could be outweighed by other benefits to retaining the measure. We intend to take multiple considerations into account when determining whether to propose a measure for removal under Factor 1 or any of the other removal factors. Additionally, we note that we have intentionally not provided numerical guidelines for Factor 1 to retain flexibility when assessing measures.
Comment: Several commenters supported the adoption of Factor 8 (“costs associated with a measure outweigh the benefit of its continued use in the program”).
Response: We thank the commenters for the support.
Comment: A few commenters raised specific concerns regarding Factor 8 (“the costs associated with the measure outweigh the benefit of its continued use in the program”). A commenter supported the addition of Factor 8, but asked CMS to seek stakeholder input specifically each time Factor 8 is considered for application. Another commenter opposed the adoption of Factor 8 unless “costs” and “benefits” are defined as “costs to Medicare beneficiaries and the public” and “benefits to Medicare beneficiaries and the public.” A few commenters expressed the belief that CMS should develop empirical criteria to determine whether this factor has been met. A few commenters strongly opposed Factor 8 because of their belief that it is extremely subjective, lacks clear criteria and guidelines, and that costs should not be the driving factor when deciding to remove a measure. A few commenters opposed Factor 8, noting their belief that cost should not be a factor in whether measures should be in a quality reporting program and that the other criteria were sufficient.
Response: We thank the commenters for sharing these concerns regarding Factor 8. We value transparency in our process and will seek stakeholder input prior to removing any measures from the HAC Reduction Program. We intend to be transparent in our assessment of measures under this measure removal factor. There are various considerations of costs and benefits, direct and indirect, financial and otherwise, that we will evaluate in applying removal Factor 8, and we will take into consideration the perspectives of multiple stakeholders. However, because we intend to evaluate each measure on a case-by-case basis, and each measure has been adopted to fill different needs in the HAC Reduction Program, we do not believe it would be meaningful to identify a specific set of assessment criteria to apply to all measures. We believe costs include costs to stakeholders such as patients, caregivers, providers, CMS, and other entities. In addition, we note that the benefits we will consider center on benefits to patients and caregivers as the primary beneficiaries of our quality reporting and value-based payment programs. When we propose to remove a measure under this measure removal factor, we will provide information on the costs and benefits we considered in evaluating the measure.
Comment: A commenter recommended that CMS adopt an additional measure removal factor, considering “whether the measure is important to beneficiaries or the public at large.” The commenter believed that the measure removal policy should center on the best interests of Medicare beneficiaries and Medicaid recipients and then the best interests of the public at large. The commenter recommended that the additional measure removal factor be Factor 1 to denote its primary importance, and the proposed measure removal factors be renumbered.
Response: We will consider the perspectives of all stakeholders when applying any of the measure removal factors, and importance to beneficiaries and the public at large are certainly part of this consideration.
We intend to be transparent in our assessment of measures under the finalized measure removal factor. As mentioned in a previous comment response, because we intend to evaluate each measure on a case-by-case basis, and each measure has been adopted to fill different needs in the HAC Reduction Program, we do not believe it would be meaningful to identify a specific set of assessment criteria to apply to all measures. Additionally, we proposed these measure removal factors in alignment with our other quality programs, and we do not believe that adopting an additional measure removal factor for HAC Reduction Program and renumbering the factors would facilitate that alignment and could result in confusion when stakeholders review our programs' measure removal factors in the future.
After consideration of the public comments we received, we are finalizing our proposals to adopt for the HAC Reduction Program the eight measure removal factors currently in the Hospital IQR Program and Hospital VBP Program beginning with the FY 2020 program year.
6. Administrative Policies for the HAC Reduction Program for FY 2020 and Subsequent Years
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41475 through 41485), we discussed our previously finalized administrative policies for the HAC Reduction Program and adopted several HAC Reduction Program-specific policies for CDC NHSN HAI data collection and validation.
a. Data Collection Beginning CY 2020
As finalized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41475 through 41477), the HAC Reduction Program will assume responsibility for receiving CDC NHSN HAI data from the CDC beginning with CY 2020 (January 1, 2020) submissions. All reporting requirements, including, but not limited to, quarterly frequency, CDC collection system and deadlines, will remain constant from the current Hospital IQR Program requirements to aid continued hospital reporting through clear and consistent requirements. We refer readers to the Hospital IQR Program's prior years' rules for additional discussion of these requirements [330] and to QualityNet for the current reporting requirements and deadlines.
Hospitals will continue to submit data through the CDC NHSN portal by selecting “NHSN Reporting” after signing in at: https://sams.cdc.gov. The HAC Reduction Program will receive the CDC NHSN data directly from the CDC instead of through the Hospital IQR Program as an intermediary. We note that some hospitals may not have locations that meet the CDC NHSN criteria for CLABSI or CAUTI reporting, and that some hospitals may perform so few procedures requiring surveillance under the Colon and Abdominal Hysterectomy SSI measure that the data may not be meaningful for public reporting or sufficiently reliable to be utilized for a program year. If a hospital does not have adequate locations or procedures, it should submit the Measure Exception Form to the HAC Reduction Program beginning on January 1, 2020. The IPPS Quality Reporting Programs Measure Exception Form can be found using the link located on the QualityNet website under the Hospitals Inpatient > Hospital Inpatient Quality Reporting Program tab at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1228760487021. As has been the case under the Hospital IQR Program, hospitals seeking an exception would submit this form at least annually to be considered.
We reiterate that no additional collection mechanisms are required for the CMS PSI 90 measure because it is a claims-based measure calculated using data submitted to CMS by hospitals for Medicare payment, and therefore imposes no additional administrative or reporting requirements on participating hospitals.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19442 through 19443), we did not propose any updates to our previously finalized data collection processes.
b. Review and Correction of Claims Data and Chart-Abstracted CDC NHSN HAI Data Used in the HAC Reduction Program for FY 2020 and Subsequent Years
For the review and correction of claims data, hospitals are encouraged to ensure that their claims are accurate prior to the snapshot date, which is taken after the 90-day period following the last date of discharge used in the applicable period. In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50726 through 50727) and FY 2019 IPPS/LTCH PPS final rule (83 FR 41477 through 41478), we detailed the process for the review and correction of claims-based data, and we refer readers to those rules for more information on the process for the review and correction of claims-based data.
For the review and correction of chart-abstracted CDC NHSN HAI measures, we reiterate that hospitals can submit, review, and correct any of the chart-abstracted information for the full 41/2 months after the end of the reporting quarter. We refer readers to the FY 2014 IPPS/LTCH PPS final rule (78 FR 50726), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38270 through 38271), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41477 through 41478) for more information.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19443), we did not propose any change to our current administrative policies regarding the review and correction of claims data or chart-abstracted CDC NHSN HAI data.
7. Change to Validation Targeting Methodology and Clarifications Regarding Validation Processes
a. Summary of Existing Validation Processes
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41478 through 41484), we adopted processes to validate the CDC NHSN HAI measure data used in the HAC Reduction Program, because the Hospital IQR Program finalized its proposals to remove CDC NHSN HAI measures from its program. We finalized the HAC Reduction Program's processes to reflect, to the greatest extent possible, the processes previously established under the Hospital IQR Program. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41478 through 41484), for detailed information on the all of the following HAC Reduction Program validation processes:
- Measures Subject to Validation.
- Educational Review Process.
- Calculation of Confidence Intervals.
- Application of Validation Scoring and Penalty.
- Validation Period.
- Data Accuracy and Completeness Acknowledgement.
We also refer readers to the QualityNet website for more information regarding measure abstraction: https://www.qualitynet.org/dcs/ContentServer?cid=%201228776288808&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page.
We would also like to remind stakeholders of the finalized validation periods for the HAC Reduction Program.

In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19443 through 19445), we proposed to change the number of hospitals selected under the validation targeting methodology and provided two clarifications to this validation process.
b. Change to the Previously Finalized Validation Selection Methodology
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41480), we finalized our policy to select 200 additional hospitals for targeted validation and five targeting criteria.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19444), while we retained the same targeting criteria that we finalized last year, we proposed to change the number of hospitals targeted from exactly 200 hospitals to “up to 200 hospitals.” We believe this change is necessary to provide flexibility in the selection process for the HAC Reduction Program so that we can implement a targeting process for validation of chart-abstracted measures in both the Hospital IQR Program and HAC Reduction Program in a manner that does not unnecessarily subject hospitals to selection just to meet the 200 hospital target. This proposed policy would allow us to select only hospitals that meet the targeting criteria and allow us to remove hospitals that do not have the requisite number of CDC NHSN HAI events from the targeted validation pool. We note that this will not affect the statistical reliability of the validation sample because statistical methodologies are only applied to data within hospitals for validation.
Comment: Several commenters supported the change in number of hospitals selected for targeted validation from exactly 200 hospitals to “up to 200 hospitals.” The commenters cited reasons such as increased flexibility, neutral effect on statistical reliability, avoidance of duplicative efforts, and avoidance of arbitrary selection.
Response: We thank the commenters for the support.
After consideration of the public comments we received, we are finalizing our proposal to change the number of hospitals selected for targeted validation from “200” to “up to 200.”
c. Clarifications to the Validation Selection Methodology
As discussed in section IV.I.7.a. of the preamble of this final rule, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41478 through 41484), we finalized several proposals to implement validation of the CDC NHSN HAI measures in the HAC Reduction Program, in as similar a manner to the validation process used by the Hospital IQR Program as was prudent. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19444), in addition to proposing to change the number of targeted hospitals from “200” to “up to 200”, we also clarified our selection process for both the random and targeted sample of subsection (d) hospitals subject to HAC Reduction Program validation.
During the comment period for the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 41479), some commenters expressed concern that hospitals could now be selected for validation under both the Hospital IQR Program and the HAC Reduction Program during the same reporting period, thereby increasing the burden to selected hospitals. As we stated last year, one of the goals of our deduplication efforts has been and continues to be a reduction in provider burden. To that end, and to allay stakeholder concerns, we are clarifying the provider selection process and reassuring providers that we will work to reduce validation burden to the greatest extent possible.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19444), we clarified that the HAC Reduction Program, in conjunction with the Hospital IQR Program, will use an aggregated random sample selection methodology through which the validation team would select one pool of 400 subsection (d) hospitals for validation of chart-abstracted measures in both the Hospital IQR Program and HAC Reduction Program. The pool of 400 hospitals will be selected randomly and validated for both the CDC NHSN HAI measures for the HAC Reduction Program and the Hospital IQR Program's chart-abstracted measures. The HAC Reduction Program will include all subsection (d) hospitals in the sample, whereas the Hospital IQR Program will remove from the sample any subsection (d) hospital without an active notice of participation in the Hospital IQR Program (83 FR 41479).
This approach will ensure that the Programs' validation samples are selected at random and would avoid any perception associated with the selection of one program's sample before the other program's sample. We will begin using this selection process with Q3 CY 2020 infectious events, which is when the HAC Reduction Program is scheduled to begin its validation process. We refer readers to section VIII.A.11. of the preamble of this final rule for more information on the Hospital IQR Program's validation policies.
After the random selection process, an additional targeted [332] aggregated sample of up to 200 hospitals will be selected for the HAC Reduction and Hospital IQR Programs' validation processes using existing targeting criteria.
We also note that any nonsubstantive updates to the specifications for validation of chart-abstracted measures will be provided on the QualityNet website at:
https://www.qualitynet.org/dcs/ContentServer?cid=%201228776288808&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page. Further, any substantive changes, such as the measures validated, changes to passing confidence intervals, and the number of providers selected, will be proposed through notice-and-comment rulemaking.
We believe this clarification of our approach to the random selection of one pool of 400 hospitals and our finalized proposal to select up to 200 targeted hospitals will avoid increasing provider burden, because the total number of hospitals selected for validation is not increasing, nor is the number of measures that are subject to validation for the selected hospitals prior to deduplication.
Moreover, we do not anticipate any increased burden to hospitals, because we are not increasing the number of cases selected for validation. For HAC Reduction Program validation, we will continue to select up to 40 cases annually from each hospital selected for validation (four CAUTI, four CLABSI, and two Colon and Abdominal Hysterectomy SSI per quarter; or four CDI, four MRSA, and two Colon and Abdominal Hysterectomy SSI per quarter). As we stated in the FY 2019 IPPS/LTCH PPS rulemaking, we intend this process to be as efficient as possible and we believe this clarification and our finalized proposal help meet that expectation.
We received a number of comments on our validation policy proposals.
Comment: A few commenters supported the proposal to create a combined HAC Reduction Program and Hospital IQR Program pool of hospitals for validation selection to ensure that hospitals do not incur duplicative validation requirements during the same validation period.
Response: We reiterate that selected hospitals will be validated for both the CDC NHSN HAI measures for the HAC Reduction Program and the Hospital IQR Program's chart-abstracted measures, but this clarification avoids increasing provider burden because the total number of hospitals selected for validation is not increasing, nor is the number of measures and cases that are subject to validation for the selected hospitals prior to deduplication.
Comment: A few commenters believed that the proposal does not extend far enough to ensure that hospitals do not incur duplicative validation requirements. The commenters cited the excess burden of validation for separate programs with overlapping timeframes, specifically for Inpatient Quality Reporting Program validation and Outpatient Quality Reporting Program validation. Another commenter suggested that CMS also consider state validation policies and the associated burden in these policies.
Response: The Hospital Inpatient Quality Reporting Program and the Hospital Outpatient Quality Reporting Program are separate Programs with separate validation requirements. We continue to believe that validation is important to both programs and the states but will keep the recommendations under consideration when considering future policies for the HAC Reduction Program.
After consideration of the public comments we received, we are finalizing our proposal to use a combined HAC Reduction Program and Hospital IQR Program validation pool of subsection (d) hospitals and use an aggregated random sample selection methodology.
d. Clarification to Validation Filtering Methodology
As we discussed for the Hospital IQR Program in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53542), CMS has the option to target the sample selection to cases, referred to as candidate events, that are more likely to be true CDC NHSN HAI events, or those that meet CDC NHSN HAI criteria. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19444), in order to better target true events for CDC NHSN HAI validation, we proposed to clarify our approach for selecting CLABSI and CAUTI cases for chart-abstracted validation when CDC NHSN HAI validation that is currently performed under the Hospital IQR Program migrates to the HAC Reduction Program, beginning with the reporting of Q3 CY 2020 infections events. To date, our experience has shown that many candidate cases selected for validation have all their positive cultures collected during the first or second day following admission and, as such, would be considered community onset events (or non-hospital acquired) for CLABSI and CAUTI.[333] Therefore, we proposed to clarify that we would eliminate these candidate CLABSI and CAUTI cases from the CDC NHSN HAI selection process prior to random case selection via a filtering method. The filtering method would eliminate any cases from the validation pool for which all positive blood or urine cultures were collected during the first or second day following admission. We estimate that, by implementing this proposed filtering method, the number of true events validated for CLABSI and CAUTI will increase without increasing the sample size, which will help us better understand the overreporting and underreporting of such events. This proposed approach is also in support of the recommendations provided by a recent HHS Office of Inspector General (OIG) report, which recommended that we make better use of analytics to ensure the integrity of hospital-reported quality data and the resulting payment adjustments by identifying potential gaming or other inaccurate reporting of quality data.[334]
A key rationale for this proposed approach is that we have found that the yield rate for CLABSI and CAUTI, which is defined as the ratio of the number of true CDC NHSN HAI events to the total sample size of candidate events, is low (13 percent for CLABSI and 9 percent for CAUTI, based on the FY 2017 validation sample). After applying the proposed filtering method to the FY 2017 sample, we estimated that the yield rate increased from 13 percent to 24 percent for CLABSI and from 9 percent to 17 percent for CAUTI. This increase will help CMS better understand the number of overreporting and underreporting of such events. A higher yield rate improves the power of the validation methodology, meaning that CMS could potentially select fewer cases for validation while still increasing the predictive power of the validation methodology. A potential reduction in the amount of cases selected for validation would decrease burden for hospitals.
In addition, because hospitals may now have fewer than four events each of CLABSI and CAUTI that meet validation filtering requirements, we expect a reduction in burden from some hospitals being required to submit three or fewer medical records as part of the validation process. We anticipate this filtering method to allow for both a richer data sample and reduced provider burden.
We received several public comments on this topic.
Comment: Many commenters supported the proposed filtering methodology for CLABSI/CAUTI, with most citing reduced provider burden and a focus on true hospital-acquired infections rather than community-acquired or community-onset infections.
Response: We thank the commenters for the support.
Comment: A few commenters expressed concerns about potential unintended consequences from the filtering methodology. A commenter agreed that the new filtering methodology will help CMS better understand over and under reporting of CLABSI and CAUTI but expressed concern that accurate clinical designation of both community-onset and hospital acquired infections are important. A few commenters expressed concern that the potential for even less validation samples may negatively impact smaller hospitals with very few HAIs despite the new equal weighting methodology.
Response: We understand the commenters' concerns about how a filter could potentially impact the MRSA/CDI sample if only `Hospital Onset' are selected to be validated. However, for CLABSI/CAUTI validation, this is not a concern, because CLABSI/CAUTI measures are validated differently than MRSA/CDI measures. For CLABSI/CAUTI validation, there are no `Hospital Onset' vs. `Community Onset' conditions and/or restrictions, whereas for MRSA/CDI, there are. CMS will continue to monitor validation and how it may impact hospitals differently. However, CMS does not currently have reason to believe that the proposed validation process for the HAC Reduction Program will change the validation performance of smaller hospitals relative to the previous validation process. CMS also notes that the proposed filtering option will only affect the cases subject to validation among hospitals selected for validation and will not impact the sample of HAIs that hospitals report to NHSN and that are used in the HAC Reduction Program scoring.
Comment: A commenter encouraged CMS to consider additional validation improvements to improve data quality and cited a number of studies and reports, specifically MedPAC's March 2019 Report to Congress and OIG Report, “CMS Validated Hospital Inpatient Quality Reporting Program Data, But Should Use Additional Tools to Identify Gaming,” which highlight the potential for improving reliability and accuracy for reporting infections and patient safety issues and encourage better analytics for validation.
Response: We thank the commenter for the suggestions and will take them into account during future policy planning.
After consideration of the public comments we received, we are finalizing the proposed CLABSI and CAUTI validation filtering methodology to remove cases in which all positive blood or urine cultures were collected during the first or second day following admission.
We also note that the agreement rates between hospital-reported MRSA and CDI events compared to events identified as infections by a trained CMS abstractor using a standardized protocol (77 FR 53548) have been lower than the agreement rates for CLABSI and CAUTI. Unlike the true event rate issue for CLABSI and CAUTI, we have determined that the lower overall agreement rates for MRSA and CDI is due to the overreporting of such events. This overreporting appears to be caused by missing or incomplete laboratory record information submitted by hospitals on the validation templates. As a result, we will provide additional training to hospitals regarding template completion and medical record submission with the hope of increasing hospital validation performance on MRSA and CDI measures.
Comment: A commenter believed that the disagreement between the trained CMS abstractors and case reports may be due to differences between LabID criteria and clinical criteria and believed that LabID criteria over report cases of MRSA and CDI.
Response: We use the CDC measure protocol for abstracting the validation infection measure records. The CDC measures experts utilize most current and evidence-based criteria for the MRSA and CDI measure specifications. We encourage the commenter to submit any specific measure specification questions to the CDC NHSN Help Desk for additional clarification.
Comment: A commenter sought clarification on what is meant by “the lower overall agreement rates for MRSA and CDI is due to over reporting of such events.” The commenter is concerned that this could increase hospital risk, and the proposed filtering methodology may create undue burden.
Response: We have determined that the disagreement rate between trained CMS abstractors and hospital reported MRSA and CDI is due to hospitals erroneously classifying community onset infections as hospital-acquired infections. At this time, we are not proposing or finalizing any filtering methodology for MRSA and CDI. We are only increasing our educational efforts on this topic, which will not create burden for hospitals.
Colon and Abdominal Hysterectomy SSI has a similarly low yield rate, and we have begun testing a filtering option to apply to Colon and Abdominal Hysterectomy SSI cases to increase the yield rate for that measure as well. We anticipate providing further guidance for Colon and Abdominal Hysterectomy SSI in future rulemaking cycles. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19445), we did not propose any changes to the validation of Colon and Abdominal Hysterectomy SSI events.
Comment: A commenter supports CMS's development of a filtering method for SSI to increase yield rate and improve the power of the validation methodology.
Response: We thank the commenter for the support.
8. HAC Reduction Program Scoring Methodology
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41485 through 41489), we finalized our proposal to remove domains from the HAC Reduction Program and simply assign equal weight to each measure for which a hospital has a measure score. As a result of this policy, we calculate each hospital's Total HAC Score as the equally weighted average of the hospital's measure scores. The table in this section of this final rule displays the weights applied to each measure under this approach. All other aspects of the HAC Reduction Program scoring methodology remained the same, including the calculation of measure scores as Winsorized z-scores (FY 2017 IPPS/LTCH PPS final rule 81 FR 57022 through 57025), the determination of the 75th percentile Total HAC Score (83 FR 41480), and the determination of the worst-performing quartile (83 FR 41481 through 41482). In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19445), we did not propose any changes to this methodology.

9. Scoring Calculations Review and Correction Period
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41484), we renamed the annual 30-day review and correction period to the “Scoring Calculations Review and Correction Period.” The purpose of the annual 30-day review and corrections period is to allow hospitals to review the calculation of their HAC Reduction Program scores.
The HAC Reduction Program will continue to provide hospitals with annual confidential hospital-specific reports and discharge level information used in the calculation of their Total HAC Scores via the QualityNet Secure Portal. Hospitals must register at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1138115992011 for a QualityNet Secure Portal account in order to access their annual hospital-specific reports.
As we stated in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50725 through 50728), hospitals have a period of 30 days after the information is posted to the QualityNet Secure Portal to review their HAC Reduction Program scores, submit questions about the calculation of their results, and request corrections for their HAC Reduction Program scores prior to public reporting. Hospitals may use the 30-day Scoring Calculations Review and Correction Period to request corrections to the all of the following information prior to public reporting:
- CMS PSI 90 measure score.
- CMS PSI 90 measure result and Winsorized measure result.
- CLABSI measure score.
- CAUTI measure score.
- Colon and Abdominal Hysterectomy SSI measure score.
- MRSA Bacteremia measure score.
- CDI measure score.
- Total HAC Score.
As we clarified in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38270 through 38271), this 30-day period is not an opportunity for hospitals to submit additional corrections related to the underlying claims data for the CMS PSI 90, or to add new claims to the data extract used to calculate the results. Hospitals have an opportunity to review and correct claims and CDC NHSN HAI data used in the HAC Reduction Program as detailed in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50726 through 50727), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38270 through 38271), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41477 through 41478).
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19445 through 19446), we did not propose any changes to our policies regarding the scoring calculations review and correction period.
10. Applicable Period for FY 2022 Program Year
In the FY 2018 IPPS/LTCH PPS final rule, we finalized the applicable period for the CMS PSI 90 as the 24-month period from July 1, 2016 through June 30, 2018. Additionally, we finalized the applicable period for the CDC NHSN HAI measures (CLABSI, CAUTI, Colon and Abdominal Hysterectomy SSI, MRSA Bacteremia, and CDI), as the 24-month period from January 1, 2017 through December 31, 2018, or CY 2017 and 2018. These two 24-month applicable periods apply to payments for FY 2020, and set the timelines for subsequent applicable periods.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19446), consistent with the definition specified at § 412.170, we proposed to adopt the applicable period for the FY 2022 HAC Reduction Program for the CMS PSI 90 as the 24-month period from July 1, 2018 through June 30, 2020, and the applicable period for CDC NHSN HAI measures as the 24-month period from January 1, 2019 through December 31, 2020.
We did not receive any public comments on this topic. Therefore, we are finalizing the applicable period for the FY 2022 Program year as proposed.
11. Limitation on Administrative and Judicial Review
Section 1886(p)(7) of the Act, as codified at 42 CFR 412.172(g), provides that there will be no administrative or judicial review under section 1869 of the Act, under section 1878 of the Act, or otherwise for any of the following:
- The criteria describing an applicable hospital in paragraph 1886(p)(2)(A) of the Act.
- The specification of hospital acquired conditions under paragraph 1886(p)(3) of the Act.
- The specification of the applicable period under paragraph 1886(p)(4) of the Act;
- The provision of reports to applicable hospitals under paragraph 1886(p)(5) of the Act.
- The information made available to the public under paragraph 1886(p)(6) of the Act.
For additional information, we refer readers to the FY 2014 IPPS/LTCH PPS final rule (78 FR 50729) and the FY 2015 IPPS/LTCH PPS final rule (79 FR 50100).
12. Regulatory Updates (42 CFR 412.172)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19446), we proposed to update 42 CFR 412.172(f)(2) and (4) to reflect current policies and align across our quality programs. We proposed these updates to remove references to domains, which were removed from the scoring methodology beginning with the FY 2020 calculation. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41485 through 41489) for a discussion of the removal of domains from the HAC Reduction Program and more information about the equal weighting scoring methodology.
We did not receive any public comments on this topic. Therefore, we are finalizing the updates to the Program's regulatory text as proposed.
J. Payments for Indirect and Direct Graduate Medical Education Costs (§§ 412.105 and 413.75 Through 413.83)
1. Background
Section 1886(h) of the Act, as added by section 9202 of the Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985 (Pub. L. 99-272), establishes a methodology for determining Medicare payments to hospitals for the direct costs of approved graduate medical education (GME) programs. Section 1886(h)(2) of the Act sets forth a methodology for the determination of a hospital-specific base-period per resident amount (PRA) that is calculated by dividing a hospital's allowable direct costs of GME in a base period by its number of full-time equivalent (FTE) residents in the base period. The base period is, for most hospitals, the hospital's cost reporting period beginning in FY 1984 (that is, October 1, 1983 through September 30, 1984). The base year PRA is updated annually for inflation. In general, Medicare direct GME payments are calculated by multiplying the hospital's updated PRA by the weighted number of FTE residents working in all areas of the hospital complex (and at nonprovider sites, when applicable), and the hospital's Medicare share of total inpatient days. The provisions of section 1886(h) of the Act are implemented in regulations at 42 CFR 413.75 through 413.83.
Section 1886(d)(5)(B) of the Act provides for a payment adjustment known as the indirect medical education (IME) adjustment under the IPPS for hospitals that have residents in an approved GME program, in order to account for the higher indirect patient care costs of teaching hospitals relative to nonteaching hospitals. The regulation regarding the calculation of this additional payment is located at 42 CFR 412.105. The hospital's IME adjustment applied to the MS-DRG payments is calculated based on the ratio of the hospital's number of FTE residents training in either the inpatient or outpatient departments of the IPPS hospital to the number of inpatient hospital beds.
The calculation of both direct GME and IME payments is affected by the number of FTE residents that a hospital is allowed to count. Generally, the greater the number of FTE residents a hospital counts, the greater the amount of Medicare direct GME and IME payments the hospital will receive. Congress, through the Balanced Budget Act of 1997 (Pub. L. 105-33), established a limit (that is, a cap) on the number of allopathic and osteopathic residents that a hospital may include in its FTE resident count for direct GME and IME payment purposes. Under section 1886(h)(4)(F) of the Act, for cost reporting periods beginning on or after October 1, 1997, a hospital's unweighted FTE count of residents for purposes of direct GME may not exceed the hospital's unweighted FTE count for direct GME in its most recent cost reporting period ending on or before December 31, 1996. Under section 1886(d)(5)(B)(v) of the Act, a similar limit based on the FTE count for IME during that cost reporting period is applied effective for discharges occurring on or after October 1, 1997. Dental and podiatric residents are not included in this statutorily mandated cap.
Section 5504 of the Affordable Care Act (Pub. L. 111-148) made a number of statutory changes relating to the determination of a hospital's FTE resident count for direct GME and IME payment purposes and the manner in which FTE resident limits are calculated and applied to hospitals under certain circumstances. Regulations implementing these changes are discussed in the November 24, 2010 final rule (75 FR 72133) and the FY 2013 IPPS/LTCH PPS final rule (77 FR 53416).
2. Policy Changes Related to Critical Access Hospitals (CAHs) as NonProviders for Direct GME and IME Payment Purposes
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19447 through 19448), under the regulation governing direct GME payments to nonprovider sites at 42 CFR 413.78(g) (and the corresponding IME regulation at 42 CFR 412.105(f)(1)(ii)(E)), a hospital can include residents training in a nonprovider setting in its FTE count if the hospital incurs the residents' salaries and fringe benefits while the residents are training at that site, in addition to other requirements. Under current policy, critical access hospitals (CAHs) that train residents in approved residency training programs are paid 101 percent of the reasonable costs for any costs they incur associated with training residents in approved programs, consistent with the CAH payment regulations at 42 CFR 413.70. We have heard concerns related to CMS' current policy that CAHs are not considered nonprovider sites for purposes of direct GME and IME payments, including the concern that CMS' current policy is creating barriers to training residents in rural areas, thereby also hindering efforts to increase the practice of physicians in rural areas. We previously heard concerns that not considering CAHs to be nonprovider sites would reduce training in rural and underserved areas and affect primary care and community-based residency training programs, such as family medicine, which train in those areas (78 FR 50737). Stakeholders also raised concerns that not considering CAHs to be nonprovider sites would hinder collaborative efforts between hospitals and CAHs to recruit and retain physicians in rural areas (78 FR 50737) and that some CAHs may be too small to support residency training programs or may not be in a financial position to incur the costs associated with residency training programs (78 FR 50738). In light of these concerns, we reexamined the statutory language associated with this policy, issues raised in prior rulemaking related to this policy, and the intent of the changes made by section 5504 of the Affordable Care Act. As a result, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19447), we proposed to modify our policy, such that a hospital could include residents training in a CAH in its FTE count as long as the nonprovider setting requirements at 42 CFR 413.78(g) are met. In this section of this final rule, we discuss our proposal, respond to public comments received, and provide our final policy.
We adopted our current GME payment policy regarding nonprovider settings and CAHs in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50734 through 50739). Prior to this time, we allowed a CAH the option to either function as a nonhospital site or to incur costs for training residents in an approved program and be paid 101 percent of the reasonable costs for any costs associated with training residents in an approved program. In part, our policy was driven by how we have regarded nonhospital settings and the unique nature of CAHs. Although we generally had used the term “nonhospital” to describe the training sites in which time spent by residents training outside of the hospital setting may be counted for both direct GME and IME payment purposes, we acknowledged in the FY 2014 IPPS/LTCH PPS final rule that we sometimes used the terms “nonhospital” and “nonprovider” interchangeably (78 FR 50735). We considered that a CAH is a unique facility that, by definition, is not always a hospital and noted that, because a CAH is generally not considered a “hospital” under section 1861(e) of the Act, a CAH could be treated as a nonhospital site for GME purposes (78 FR 50735).
Section 5504(a) of the Affordable Care Act amended sections 1886(d)(5)(B)(iv)(II) and 1886(h)(4)(E) of the Act, on a prospective basis, to further address the setting in which time spent by residents training outside of the hospital setting may be counted for both direct GME and IME payment purposes. In particular, the statute was amended to reference a “nonprovider.” As a result of this legislative change and because a CAH is defined as a “provider of services” under section 1861(u) of the Act, we finalized our current policy, effective for portions of cost reporting periods occurring on or after October 1, 2013.
Section 5504 of the Affordable Care Act made several changes to the requirements a hospital must meet in order to include residents training in a nonprovider setting in its FTE count. As we noted in prior rulemaking, these changes include the requirement that a hospital need only incur residents' salaries and fringe benefits in order to count the residents as opposed to incurring “all or substantially all” of the costs of the training at the nonprovider site and the ability for more than one hospital to count FTE residents training at a single nonprovider site (75 FR 72136 through 72139). We believe these changes were intended to promote the training of residents at sites outside of the IPPS hospital setting, many of which provide access to care for patients in rural and underserved areas. Furthermore, as noted in the proposed rule, we reassessed and agreed with prior comments we have received stating that the intent of section 5504 of the Affordable Care Act was to reduce the administrative burden associated with counting residency training time in settings engaged in patient care outside of the IPPS hospital setting (78 FR 50736). Therefore, we believe that, to the extent possible, in accordance with current statutory language, it is important to support residency training in rural and underserved areas, including residency training at CAHs.
As discussed in the proposed rule, while a CAH is considered a “provider of services” under section 1861(u) of the Act, we acknowledge that the term “nonprovider” is not explicitly defined in the statute. Furthermore, section 1861(e) of the Act, which states in part that the term “hospital” does not include, unless the context otherwise requires, a critical access hospital (as defined in section 1861(mm)(1) of the Act), underscores the sometimes ambiguous status of CAHs. We believe that the lack of both an explicit statutory definition of “nonprovider” and a definitive determination as to whether a CAH is considered a hospital along with the fact that a CAH is a facility primarily engaged in patient care (we refer readers to section 1886(h)(5)(K) of the Act which states that the term “nonprovider setting that is primarily engaged in furnishing patient care” means a nonprovider setting in which the primary activity is the care and treatment of patients, as defined by the Secretary), provides flexibility within the current statutory language to consider a CAH as a “nonprovider” setting for direct GME and IME payment purposes.
Therefore, in order to support the training of residents in rural and underserved areas, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed that, effective with portions of cost reporting periods beginning October 1, 2019, a hospital may include FTE residents training at a CAH in its FTE count as long as it meets the nonprovider setting requirements currently included at 42 CFR 412.105(f)(1)(ii)(E) and 413.78(g). We did not propose to change our policy with respect to CAHs incurring the costs of training residents. That is, a CAH may continue to incur the costs of training residents in an approved residency training program(s) and receive payment based on 101 percent of the reasonable costs for these training costs. We stated in the proposed rule that if this proposal is finalized, CMS will work closely with HRSA and the Federal Office of Rural Health Policy to communicate the increased regulatory flexibility to CAHs as well as existing residency programs and the options it affords for increasing rural residency training. We sought public comments on this proposed policy change.
Comment: Most commenters supported the proposed policy to consider CAHs as nonproviders for direct GME and IME payment purposes. A commenter stated it concurred with CMS's assessment that the terms “nonprovider” and “nonhospital” have been used interchangeably, such that the statute leaves some ambiguity as to whether a CAH may be considered a nonprovider site. Commenters stated that although more policies are needed to fully address workforce gaps in rural America, the proposed policy would help to recruit and retain physicians in rural underserved areas. Some commenters described the rural primary care residency training programs in their specific states and noted that these training programs emphasize rotations at CAHs. A commenter stated they have a long history of supporting CAH rotations wherein residents receive a deeper understanding of the community that they practice in, as well as the challenges and opportunities that can be found in remote settings versus those in more urban settings. Another commenter stated that 40 percent of the hospitals in its state are CAHs and therefore, the proposed policy is vitally important to increasing recruitment efforts by CAHs and provider access for patients in rural areas of its state.
Commenters noted the challenges faced by rural facilities as well as flexibilities that could result from the proposed policy. A commenter stated that workforce shortages are a persistent challenge for rural providers as only 10 percent of U.S. physicians practice in rural areas despite nearly 20 percent of Americans residing in these communities. Another commenter stated that in addition to having a positive impact on both the residents and physicians practicing in rural areas, the proposed policy would ease the paperwork burden on cash strapped CAHs. Another commenter stated rural hospitals represent more than half of all hospitals in the U.S., yet they struggle to recruit and retain a health care workforce sufficient to meet the needs of the communities they serve due to financial distress. The commenter stated training facilities in rural hospitals operate on very narrow margins and are cautious to commit to ongoing residency training costs without a stable, predicable source of funding. Modifying the definition of non-provider setting will reduce financial vulnerability and promote greater training of physicians in rural hospitals. Another commenter stated they believe the proposal would expand clinical rotation opportunities to sites of care that cannot alone bear the costs associated with starting and maintaining approved residency programs. The commenter stated the proposal would also allow hospitals that are under their residency caps greater flexibility in offering residents a broad array of clinical rotations in approved residency training programs, including in rural areas. A commenter stated that if the proposal is finalized, it encourages CMS to work with the Health Resources and Services Administration (HRSA) and Federal Office of Rural Health Policy to communicate such information to CAHs and residency programs, as well as to explore additional opportunities for regulatory flexibility that could further increase rural residency training.
Response: We appreciate the commenters' support of the proposed policy to consider CAHs as nonprovider sites for purposes of direct GME and IME payments. As stated in the proposed rule, if the proposal is finalized, CMS will work closely with HRSA and the Federal Office of Rural Health Policy to communicate the increased regulatory flexibility to CAHs as well as existing residency programs and the options it affords for increasing rural residency training. Any additional opportunities for regulatory flexibility would likely need to be a part of the proposed and final rulemaking process.
Comment: A commenter disagreed with the proposed policy. The commenter disagreed with CMS' assessment that there is flexibility within the current statutory language to consider a CAH a nonprovider for direct GME and IME payment purposes. The commenter disagreed with the statement in the proposed rule that the lack of both an explicit statutory definition of nonprovider and a definitive determination as to whether a CAH is considered a hospital allows CMS to consider a CAH a nonprovider for direct GME and IME payment purposes. The commenter stated that the fact that a CAH is explicitly considered to be a “provider of services” under section 1861(u) of the Act, firmly establishes a CAH to be a “provider” and would, therefore, also firmly preclude a CAH from being considered a “nonprovider”.
The commenter stated that regardless of the propagated intent of the changes made by section 5504 of the Affordable Care Act, it does not appear that the existing statutory language will allow for CMS to modify its current policy in order to allow a hospital to include FTE residents training at a CAH in its FTE count. The commenter strongly cautioned CMS in moving forward with the proposal, as it seems as though the proposal could just as easily be reversed back to the current policy upon some future reexamination (falling more in line with the original examination as noted in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50734 through 50739)).
The commenter stated there may also be an increased potential that Medicare funding of residency training time will be incorrectly duplicated if hospitals are allowed to include FTE residents training at CAHs in their FTE counts. The commenter stated that since CAHs may continue to incur the costs of training residents in an approved residency training program(s) and receive payment based on 101 percent of the reasonable costs for these training costs, hospitals that sponsor residency training programs may simply be invoicing CAHs for the cost of the residents' salaries and fringe benefits while the residents are training at the CAHs or may otherwise be generally invoicing the CAHs for portions of the costs of the residency training programs. Those same hospitals, which sponsor the residency training programs, may then incorrectly represent themselves as having incurred the residents' salaries and fringe benefits while the residents were training at the CAHs and include the residents training at the CAHs in their FTE resident counts for direct GME and IME payment purposes. The commenter stated that this potential situation would be a difficult one to uncover under normal auditing procedures and the proposed change in policy opens up a great risk of Medicare double funding residency training time. The commenter stated that another instance of duplication of payment would occur in the instance where the indirect costs incurred by the CAHs for the residency training time are paid to the CAHs at 101 percent of the reasonable costs and also be (conceptually) paid to the hospitals through the IME payments. The commenter stated that in addition, any direct costs incurred by the CAHs such as teaching physician time would be paid to the CAHs at 101 percent of the reasonable costs and would also then be (conceptually) paid to the hospitals through the direct GME payments.
The commenter questioned why the current policy with respect to CAHs and nonproviders would be a concern for the large community of teaching hospitals presently in existence, many of which are already training at levels which are limited by their caps. The commenter stated they assume the current policy with respect to CAHs and nonproviders may be more of a concern for hospitals that either are or plan to train residents in new programs and may therefore be eligible to receive adjustments to the statutorily mandated caps. The commenter stated these hospitals' FTE resident counts would be uncapped for direct GME and IME payment purposes during an allotted cap-building period in the initial years of the new medical residency training programs and would then be used to establish permanent cap adjustments for these hospitals. These hospitals, if allowed to include residents training at a CAHs in their FTE counts, could potentially utilize CAHs as participating sites for the new medical residency training programs and claim the residents training at the CAHs in their FTE counts until such time that these hospitals have established permanent cap adjustments. The commenter stated these hospitals would then be able to proprietarily and immediately use their caps to fund FTE residents training at sites other than those CAHs that had originally helped them to attain the very same permanent cap adjustments, or even to fund FTE residents training at their hospital sites in other established residency training programs. The commenter stated that once the hospitals' potential for additional Medicare reimbursement has been limited by the statutorily mandated caps, these hospitals might then no longer be incentivized to provide resident training rotations at the CAHs. The training of residents in rural and underserved areas would again be reduced, contrary to the propagated intent of the changes made by section 5504 of the Affordable Care Act.
Response: We appreciate hearing the commenter's concerns with respect to the proposed policy. While the commenter is correct that CAHs are included in the definition of “provider of services” under section 1861(u) of the Act, we continue to believe, upon reexamination of the current statutory language, that the lack of a statutory definition of “nonprovider” as well as the consideration that a CAH is a facility primarily engaged in patient care consistent with the term “nonprovider setting that is primarily engaged in furnishing patient care” included at section 1886(h)(5)(K) of the Act, provides enough flexibility within the current statutory language to consider CAHs as nonproviders for purposes of direct GME and IME payments.
Regarding the concern that hospitals may simply invoice CAHs for the cost of the residents' salaries and fringe benefits or for portions of the costs of the residency training program, we note that just as with any FTEs training in a nonprovider setting, the hospital must show its MAC the location of the residents and that it actually paid the residents' salaries and fringe benefits. That is, the hospital must clearly show it had the residents training at a CAH on its payroll or that it made payments to the CAH to cover the residents' salaries and fringe benefits.
In response to the concern of duplicative payments with respect to direct GME costs, if a CAH is including direct costs in the GME cost centers on its cost report, the MAC can ask which entity is claiming the FTE residents and which entity is incurring the salaries and fringe benefits. If the applicable nonprovider site requirements are not being met, the MAC would be able to disallow the FTE residents from the hospital. Regarding the concern of duplicative payments with respect to indirect costs, we understand that as a natural consequence of receiving payment based on reasonable costs under section 1861(v)(1)(A) of the Act, CAHs would be permitted to claim the indirect costs of residency training, regardless of whether or not another hospital claims the FTE residents for IME payment purposes. Nevertheless, in the event a hospital pays the salaries and fringe benefits of the FTE residents training in a nonprovider setting and meets all other applicable requirements, section 1886(d)(5)(B)(iv)(II) of the Act permits that hospital to receive IME payments for those FTE residents.
In response to the concern that hospitals may use CAHs as training sites to establish their caps and then move the training from the CAH to their hospital or other hospitals, while in general cap slots are fungible such that FTE cap slots could be moved from a CAH to a hospital(s), the purpose of the policy finalized in this rule is to address stakeholders' concerns that the previous policy regarding CAHs and nonprovider sites was negatively affecting residency training in rural areas. We would expect then, that the policy finalized in this rule would promote residency training at CAHs rather than promote scenarios where the CAH is acting as a temporary training site for cap-building purposes.
Comment: While many commenters supported our proposed policy, the majority asked that CMS finalize a policy which expands upon our proposed policy in a number of ways. Commenters requested that CMS reconsider the effective date of the proposed policy, specifically that CMS finalize the proposed policy with an effective date retroactive to FY 2014. The commenters stated that those hospitals that partnered with CAHs in rural residency programs, which completed their cap-building period during the six intervening years since implementation of the 2014 IPPS final rule, are permanently and continually harmed by an effective date of October 1, 2019. The commenters stated some hospitals have been harmed by CMS' previous position since the hospitals could not claim FTEs for reimbursement (under the IPPS system) and the participating CAHs did not claim any direct educational costs. One commenter requested that CMS reconsider the effective date of its proposed policy because hospital residency programs, such as its internal medicine program, that were in their cap-building period during the six intervening years since implementation of the FY 2014 IPPS/LTCH PPS final rule are permanently affected by the historical exclusion of CAH rotations. The commenter stated that since these rotations were not allowed to be included in its initial counts in its cap-building period, adding the CAH rotations in later years without some sort of cap adjustment, will merely push the hospital over its cap. The commenter stated they hope CMS will provide this additional consideration for underserved rural areas which will enhance institutions' ability to produce physicians who will practice in rural areas and serve underserved rural populations.
Commenters expressed significant concerns over the permanent impact the current policy with respect to CAHs will have on hospitals that had or will have their caps set based on training residents in new programs during the period of October 1, 2013 through September 30, 2019. Many commenters requested that CMS allow a cap recalculation for those hospitals that partnered with CAHs and set their caps during this period and have cost reports that are still within the 3-year reopening period. The commenters stated this approach would not require any changes or resubmissions of cost reports. Rather, Medicare MACs would recalculate the cap to include time spent by residents in CAHs and help remedy harm caused by CMS' previous policy. A commenter stated there are many teaching hospitals that are several years into, or at the end of, their cap-building period that have struggled to accommodate rotations to CAHs as a result of this restriction. Permitting these hospitals to count FTEs that would have otherwise been counted toward their cap under the proposed policy would allow for additional training in rural and underserved areas each year. Another commenter stated they were concerned that the CAH policy in effect for Medicare GME payment purposes during the period October 1, 2013, through October 1, 2019, may have inappropriately set certain new teaching hospitals' direct GME and IME caps too low. The commenter stated that CMS' current methodology for the calculation of a new teaching hospital's caps utilizes a 5-year cap-building window as a representative time period during which a proper determination of the future steady state can be made. The regulatory text makes clear that the purpose is to ensure that the new teaching hospital does not receive credit for training occurring at another hospital. The commenter believes that CMS has ample authority to separate specific Medicare reimbursement determinations made during the period October 1, 2013, to September 30, 2019, from FTE resident cap determinations made applicable (and permanent) for portions of cost reporting periods beginning on or after July 1, 2020. The commenter recommended CMS permit MACs to consider rotations to a CAH during the period October 1, 2013, to October 1, 2019, as training at a nonprovider setting solely for purpose of calculating a new teaching hospital's permanent direct GME and IME caps. Such clarification would not result in any retroactive payment implications. The commenter stated as CMS' preamble discussion makes clear, the status of CAHs as a hospital/provider/nonprovider in the context of Medicare GME payment policy has been ambiguous at best. CMS has ample authority to address this issue for the betterment of those hospitals seeking to promote the practice of physicians in rural areas. A commenter gave the example of how it first started training residents in a new internal medicine program and therefore is currently in its 5-year cap building period. The commenter stated it strives to teach residents in community settings, to expose trainees to diverse settings of care, which includes a CAH within the commenter's health system. The commenter stated it has struggled to permit residents to spend significant amounts of time at this CAH given the financial incentives created by CMS' current policies. The commenter stated the proposed policy change is particularly helpful in the final year of its cap-building period allowing the hospital to establish resident rotations to the CAH that can be continued long after the Medicare GME cap-building period has closed. The commenter strongly encouraged CMS to provide additional flexibilities by allowing hospitals to count residency training time at CAHs during the entire 5-year cap building window, even for FTE time prior to October 1, 2019. Such an approach would recognize the hospitals need for space within its GME caps to accommodate resident training time and would support new teaching hospitals in continuing to send residents to CAHs in increasing numbers, all the while not requiring the reopening of prior year cost reports.
Some commenters stated that while training time in CAHs during October 1, 2013 through October 1, 2019 could not be counted by hospitals, in many cases CAHs did not claim any direct education costs during this time period either. The commenters requested CMS allow hospitals to claim CAH rotation time for unsettled cost reports (in the 2013 to 2019 window) should they wish to and if the CAH agrees. This claiming of resident training time by the hospital, would be with the understanding that the CAH where the resident was training may also have its cost report(s) opened for the affected year(s), but solely for the purpose of assuring that the CAH did not claim allowable costs for these resident rotations.
Response: We appreciate hearing the commenters' concerns with respect to the proposed policy. As we noted in the proposed rule, in light of concerns expressed by stakeholders, we reexamined the statutory language associated with this policy, issues raised in prior rulemaking related to this policy, and the intent of the changes made by section 5504 of the Affordable Care Act. We determined there is enough flexibility within the current statutory language to consider a CAH a nonprovider setting for direct GME and IME payment purposes. However, the interpretation of CAHs as nonproviders presented in the proposed rule, does not invalidate our previous policy of not considering CAHs to be nonproviders for purposes of direct GME and IME payments established in the FY 2014 IPPS/LTCH PPS final rule, applicable through September 30, 2019. We continue to believe that this policy and interpretation of the applicable law was and is a legally viable alternative reading of the statute. In considering the comments received, we note that none of the commenters' recommendations provide policy alternatives which are purely prospective; but rather, all contain elements which are retroactive in nature. As we do not believe engaging in retroactive rulemaking is appropriate with respect to this policy, we are finalizing our policy as proposed. Specifically, effective with portions of cost reporting periods beginning October 1, 2019, a hospital may include FTE residents training at a CAH in its FTE count as long as it meets the nonprovider setting requirements currently included at 42 CFR 412.105(f)(1)(ii)(E) and 413.78(g). Therefore, if a hospital is at some point in its 5-year cap-building period as of October 1, 2019, and as of that date is sending residents in a new program to train at a CAH, assuming the regulations governing nonprovider site training are met, the time spent by FTE residents training at the CAH on or after October 1, 2019 will be included in the hospital's FTE cap calculation. Alternatively, as we noted in the proposed rule, a CAH may decide to continue to incur the costs of training residents in an approved residency training program(s) and receive payment based on 101 percent of the reasonable costs for these training costs. In that situation no hospital can include the residents training at the CAH in its direct GME and IME FTE counts.
Comment: We received public comments regarding GME issues that were outside of the scope of the proposals included in the FY 2020 IPPS/LTCH PPS proposed rule. These comments requested that—
- While the commenter appreciated the proposed change, the commenter stated it will not help the many teaching hospitals that have resident counts above their 1996 resident counts and still choose to rotate residents to CAHs and other sites. The commenter urged CMS to support bipartisan legislation, the Resident Physician Shortage Reduction Act of 2019 (S. 348/H.R. 1763), which will provide moderate increases to these caps.
- CMS support and advocate for other programs that address health care workforce shortages. The commenter stated the Conrad 30 J-1 Waiver Program was created to address physician shortages across the country and allows each state's department of health to sponsor up to 30 international medical graduates each year for waiver of the 2-year home residency requirement if they serve in federally designated shortages areas. The commenter stated that although each state is eligible to sponsor up to 30 medical graduates, some states do not fill their slots, which results in unused physician slots in some areas when there is a need for more slots in other areas. The commenter urged CMS to work with Congress and other applicable departments to seek ways to increase the number of slots for states that consistently fill their slots, or allow slots that are not used by some states to be distributed to other states that have greater need.
- CMS release its findings with respect to section 5503 of the Affordable Care Act. The commenter referenced the requirement under section 5503 of the Affordable Care Act that a hospital, which is awarded slots, must use 75 percent of the awarded slots for residency training in primary care and/or general surgery. The commenter stated that while they believe that the 75 percent threshold was intended to bolster the primary care and general surgery workforce as part of healthcare delivery for current and future Medicare beneficiaries, CMS has not provided information on the effects of this program, such as: The specialties of the training programs that lost unused slots; how many of the redistributed slots were filled; how many of the redistributed slots were awarded to primary care programs compared to how many were awarded to general surgery programs; whether general surgery experienced a net loss or net gain of residency slots; and how CMS monitored hospitals' adoption of the 75 percent threshold. The commenter stated that now that the 5-year redistribution period has ended, they strongly urge CMS to release its findings regarding awardee hospitals' use of their section 5503 slots and the hospitals' compliance with the terms and conditions of the program. The commenter stated they remain concerned with the lack of consistent, unbiased statistics on physician supply and demand and believe that CMS can provide more accurate and actionable workforce data based on the initial round of unused residency slot redistribution. The commenter requested that in the interest of transparency and accountability, CMS make public a comprehensive description of the specialties from which the unused slots were drawn and subsequently redistributed; the number of slots designated as primary care versus general surgery under the 75 percent threshold; how the Agency and its contractors tracked hospitals' participation and enforced the program's statutory and regulatory requirements; and, in the event that it was determined a hospital did not satisfy these requirements, how its awarded slots were redistributed to another hospital(s) in accordance with section 5503 of the Affordable Care Act.
Response: Because we consider these public comments to be outside of the scope of the proposed rule, we are not addressing them in this final rule.
3. Notice of Closure of Teaching Hospital and Opportunity To Apply for Available Slots
a. Background
Section 5506 of the Affordable Care Act (Pub. L. 111-148), as amended by the Health Care and Education Reconciliation Act of 2010 (Pub. L. 111-152) (collectively, the “Affordable Care Act”), authorizes the Secretary to redistribute residency slots after a hospital that trained residents in an approved medical residency program closes. Specifically, section 5506 of the Affordable Care Act amended the Act by adding subsection (vi) to section 1886(h)(4)(H) of the Act and modifying language at section 1886(d)(5)(B)(v) of the Act, to instruct the Secretary to establish a process to increase the FTE resident caps for other hospitals based upon the FTE resident caps in teaching hospitals that closed “on or after a date that is 2 years before the date of enactment” (that is, March 23, 2008). In the CY 2011 Outpatient Prospective Payment System (OPPS) final rule with comment period (75 FR 72212), we established regulations at 42 CFR 413.79(o) and an application process for qualifying hospitals to apply to CMS to receive direct GME and IME FTE resident cap slots from the hospital that closed. We made certain modifications to those regulations in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53434), and we made changes to the section 5506 application process in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50122 through 50134). The procedures we established apply both to teaching hospitals that closed on or after March 23, 2008, and on or before August 3, 2010, and to teaching hospitals that close after August 3, 2010.
b. Notice of Closure of Providence Hospital Located in Washington, DC and the Application Process—Round 15
CMS has learned of the closure of Providence Hospital, located in Washington, DC (CCN 090006). Accordingly, this notice serves to notify the public of the closure of this teaching hospital and initiate another round of the section 5506 application and selection process. This round will be the 15th round (“Round 15”) of the application and selection process. The table below contains the identifying information and IME and direct GME FTE resident caps for the closed teaching hospital, which are part of the Round 15 application process under section 5506 of the Affordable Care Act.

c. Application Process for Available Resident Slots
The application period for hospitals to apply for slots under section 5506 of the Affordable Care Act is 90 days following notice to the public of a hospital closure (77 FR 53436). Therefore, hospitals that wish to apply for and receive slots from the FTE resident caps of closed Providence Hospital, located in Washington, DC, must submit applications (Section 5506 Application Form posted on Direct Graduate Medical Education (DGME) website as noted at the end of this section) directly to the CMS Central Office no later than October 31, 2019. The mailing address for the CMS Central Office is included on the application form. Applications must be received by the CMS Central Office by the October 31, 2019 deadline date. It is not sufficient for applications to be postmarked by this date.
After an applying hospital sends a hard copy of a section 5506 slot application to the CMS Central Office mailing address, the hospital is encouraged to notify the CMS Central Office of the mailed application by sending an email to: ACA5506application@cms.hhs.gov. In the email, the hospital should state: “On behalf of [insert hospital name and Medicare CCN#], I, [insert your name], am sending this email to notify CMS that I have mailed to CMS a hard copy of a section 5506 application under Round 15 due to the closure of Providence Hospital. If you have any questions, please contact me at [insert phone number] or [insert your email address].” An applying hospital should not attach an electronic copy of the application to the email. The email will only serve to notify the CMS Central Office to expect a hard copy application that is being mailed to the CMS Central Office.
We have not established a deadline by when CMS will issue the final determinations to hospitals that receive slots under section 5506 of the Affordable Care Act. However, we review all applications received by the deadline and notify applicants of our determinations as soon as possible.
We refer readers to the CMS Direct Graduate Medical Education (DGME) website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/DGME.html to download a copy of the section 5506 application form (Section 5506 Application Form) that hospitals must use to apply for slots under section 5506 of the Affordable Care Act. Hospitals should also access this same website for a list of additional section 5506 guidelines for the policy and procedures for applying for slots, and the redistribution of the slots under sections 1886(h)(4)(H)(vi) and 1886(d)(5)(B)(v) of the Act.
K. Rural Community Hospital Demonstration Program
1. Introduction
The Rural Community Hospital Demonstration was originally authorized for a 5-year period by section 410A of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) (Pub. L. 108-173), and extended for another 5-year period by sections 3123 and 10313 of the Affordable Care Act (Pub. L. 111-148). Subsequently, section 15003 of the 21st Century Cures Act (Pub. L. 114-255), enacted December 13, 2016, amended section 410A of Public Law 108-173 to require a 10-year extension period (in place of the 5-year extension required by the Affordable Care Act, as further discussed in this final rule). Section 15003 also required that, no later than 120 days after enactment of Public Law 114-255, the Secretary had to issue a solicitation for applications to select additional hospitals to participate in the demonstration program for the second 5 years of the 10-year extension period, so long as the maximum number of 30 hospitals stipulated by Public Law 114-148 was not exceeded. In this final rule, we are providing a description of the provisions of section 15003 of Public Law 114-255, our final policies for implementation, and the finalized budget neutrality methodology for the extension period authorized by section 15003 of Public Law 114-255. We are including a discussion of the budget neutrality methodology used in previous final rules for periods prior to the extension period, as well as for this upcoming fiscal year. In addition, we will provide an update on the reconciliation of actual and estimated costs of the demonstration for FYs 2014 and 2015.
2. Background
Section 410A(a) of Public Law 108-173 required the Secretary to establish a demonstration program to test the feasibility and advisability of establishing rural community hospitals to furnish covered inpatient hospital services to Medicare beneficiaries. The demonstration pays rural community hospitals under a reasonable cost-based methodology for Medicare payment purposes for covered inpatient hospital services furnished to Medicare beneficiaries. A rural community hospital, as defined in section 410A(f)(1) of Public Law 108-173, is a hospital that—
- Is located in a rural area (as defined in section 1886(d)(2)(D) of the Act) or is treated as being located in a rural area under section 1886(d)(8)(E) of the Act;
- Has fewer than 51 beds (excluding beds in a distinct part psychiatric or rehabilitation unit) as reported in its most recent cost report;
- Provides 24-hour emergency care services; and
- Is not designated or eligible for designation as a CAH under section 1820 of the Act.
Section 410A of Public Law 108-173 required a 5-year period of performance. Subsequently, sections 3123 and 10313 of Public Law 111-148 required the Secretary to conduct the demonstration program for an additional 5-year period, to begin on the date immediately following the last day of the initial 5-year period. Public Law 111-148 required the Secretary to provide for the continued participation of rural community hospitals in the demonstration program during the 5-year extension period, in the case of a rural community hospital participating in the demonstration program as of the last day of the initial 5-year period, unless the hospital made an election to discontinue participation. In addition, Public Law 111-148 limited the number of hospitals participating to no more than 30. We refer readers to previous final rules for a summary of the selection and participation of these hospitals. Starting from December 2014 and extending through December 2016, the 21 hospitals that were still participating in the demonstration ended their scheduled periods of performance on a rolling basis, respectively, according to the end dates of the hospitals' cost report periods.
3. Provisions of the 21st Century Cures Act (Pub. L. 114-255) and Finalized Policies for Implementation
a. Statutory Provisions
As stated earlier, section 15003 of Public Law 114-255 further amended section 410A of Public Law 108-173 to require the Secretary to conduct the Rural Community Hospital Demonstration for a 10-year extension period (in place of the 5-year extension period required by Pub. L. 111-148), beginning on the date immediately following the last day of the initial 5-year period under section 410A(a)(5) of Public Law 108-173. Thus, the Secretary is required to conduct the demonstration for an additional 5-year period. Specifically, section 15003 of Public Law 114-255 amended section 410A(g)(4) of Public Law 108-173 to require that, for hospitals participating in the demonstration as of the last day of the initial 5-year period, the Secretary shall provide for continued participation of such rural community hospitals in the demonstration during the 10-year extension period, unless the hospital makes an election, in such form and manner as the Secretary may specify, to discontinue participation. Furthermore, section 15003 of Public Law 114-255 added subsection (g)(5) to section 410A of Public Law 108-173 to require that, during the second 5 years of the 10-year extension period, the Secretary shall apply the provisions of section 410A(g)(4) of Public Law 108-173 to rural community hospitals that are not described in subsection (g)(4) but that were participating in the demonstration as of December 30, 2014, in a similar manner as such provisions apply to hospitals described in subsection (g)(4).
In addition, section 15003 of Public Law 114-255 amended section 410A of Public Law 108-173 to add paragraph (g)(6)(A) which requires that the Secretary issue a solicitation for applications no later than 120 days after enactment of paragraph (g)(6) to select additional rural community hospitals located in any State to participate in the demonstration program for the second 5 years of the 10-year extension period, without exceeding the maximum number of hospitals (that is, 30) permitted under section 410A(g)(3) of Public Law 108-173 (as amended by Pub. L. 111-148). Section 410A(g)(6)(B) provides that, in determining which hospitals submitting an application pursuant to this solicitation are to be selected for participation in the demonstration, the Secretary must give priority to rural community hospitals located in one of the 20 States with the lowest population densities, as determined using the 2015 Statistical Abstract of the United States. The Secretary may also consider closures of hospitals located in rural areas in the State in which an applicant hospital is located during the 5-year period immediately preceding the date of enactment of Public Law 114-255 (December 13, 2016), as well as the population density of the State in which the rural community hospital is located.
(b) Terms of Participation for the Extension Period Authorized by Public Law 114-255
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38280), we finalized our policy with regard to the effective date for the application of the reasonable cost-based payment methodology under the demonstration for those previously participating hospitals choosing to participate in the second 5-year extension period. According to our finalized policy, each previously participating hospital began the second 5 years of the 10-year extension period and payment for services provided under the cost-based payment methodology under section 410A of Public Law 108-173 (as amended by section 15003 of Pub. L. 114-255) on the date immediately after the period of performance ended under the first 5-year extension period.
Seventeen of the 21 hospitals that completed their periods of participation under the extension period authorized by Public Law 111-148 elected to continue in the second 5-year extension period for the full second 5-year extension period. (Of the four hospitals that did not elect to continue participating, three hospitals converted to CAH status during the time period of the second 5-year extension period). Therefore, the 5-year period of performance for each of these hospitals started on dates beginning May 1, 2015 and extending through January 1, 2017. On November 20, 2017, we announced that, as a result of the solicitation issued earlier in the year responding to the requirement in Public Law 114-255, 13 additional hospitals were selected to participate in the demonstration in addition to these 17 hospitals continuing participation from the first 5-year extension period. (Hereafter, these two groups are referred to as “newly participating” and “previously participating” hospitals, respectively.) We announced that each of these newly participating hospitals would begin its 5-year period of participation effective with the start of the first cost reporting period on or after October 1, 2017. One of the hospitals selected from the solicitation in 2017 withdrew from the demonstration program prior to beginning participation in the demonstration on July 1, 2018. In addition, one of the previously participating hospitals closed effective January 2019. Therefore, 28 hospitals are scheduled to participate in the demonstration in FY 2020.
4. Budget Neutrality
a. Statutory Budget Neutrality Requirement
Section 410A(c)(2) of Public Law 108-173 requires that, in conducting the demonstration program under this section, the Secretary shall ensure that the aggregate payments made by the Secretary do not exceed the amount which the Secretary would have paid if the demonstration program under this section was not implemented. This requirement is commonly referred to as “budget neutrality.” Generally, when we implement a demonstration program on a budget neutral basis, the demonstration program is budget neutral on its own terms; in other words, the aggregate payments to the participating hospitals do not exceed the amount that would be paid to those same hospitals in the absence of the demonstration program. Typically, this form of budget neutrality is viable when, by changing payments or aligning incentives to improve overall efficiency, or both, a demonstration program may reduce the use of some services or eliminate the need for others, resulting in reduced expenditures for the demonstration program's participants. These reduced expenditures offset increased payments elsewhere under the demonstration program, thus ensuring that the demonstration program as a whole is budget neutral or yields savings. However, the small scale of this demonstration program, in conjunction with the payment methodology, made it extremely unlikely that this demonstration program could be held to budget neutrality under the methodology normally used to calculate it—that is, cost-based payments to participating small rural hospitals were likely to increase Medicare outlays without producing any offsetting reduction in Medicare expenditures elsewhere. In addition, a rural community hospital's participation in this demonstration program would be unlikely to yield benefits to the participants if budget neutrality were to be implemented by reducing other payments for these same hospitals. Therefore, in the 12 IPPS final rules spanning the period from FY 2005 through FY 2016, we adjusted the national inpatient PPS rates by an amount sufficient to account for the added costs of this demonstration program, thus applying budget neutrality across the payment system as a whole rather than merely across the participants in the demonstration program. (A different methodology was applied for FY 2017.) As we discussed in the FYs 2005 through 2017 IPPS/LTCH PPS final rules (69 FR 49183; 70 FR 47462; 71 FR 48100; 72 FR 47392; 73 FR 48670; 74 FR 43922, 75 FR 50343, 76 FR 51698, 77 FR 53449, 78 FR 50740, 77 FR 50145; 80 FR 49585; and 81 FR 57034, respectively), we believe that the language of the statutory budget neutrality requirements permits the agency to implement the budget neutrality provision in this manner.
b. Methodology Used In Previous Final Rules for Periods Prior to the Extension Period Authorized by the 21st Century Cures Act (Pub. L. 114-255)
We have generally incorporated two components into the budget neutrality offset amounts identified in the final IPPS rules in previous years. First, we have estimated the costs of the demonstration for the upcoming fiscal year, generally determined from historical, “as submitted” cost reports for the hospitals participating in that year. Update factors representing nationwide trends in cost and volume increases have been incorporated into these estimates, as specified in the methodology described in the final rule for each fiscal year. Second, as finalized cost reports became available, we determined the amount by which the actual costs of the demonstration for an earlier, given year, differed from the estimated costs for the demonstration set forth in the final IPPS rule for the corresponding fiscal year, and incorporated that amount into the budget neutrality offset amount for the upcoming fiscal year. If the actual costs for the demonstration for the earlier fiscal year exceeded the estimated costs of the demonstration identified in the final rule for that year, this difference was added to the estimated costs of the demonstration for the upcoming fiscal year when determining the budget neutrality adjustment for the upcoming fiscal year. Conversely, if the estimated costs of the demonstration set forth in the final rule for a prior fiscal year exceeded the actual costs of the demonstration for that year, this difference was subtracted from the estimated cost of the demonstration for the upcoming fiscal year when determining the budget neutrality adjustment for the upcoming fiscal year. (We note that we have calculated this difference for FYs 2005 through 2013 between the actual costs of the demonstration as determined from finalized cost reports once available, and estimated costs of the demonstration as identified in the applicable IPPS final rules for these years).
c. Budget Neutrality Methodology for the Extension Period Authorized by the 21st Century Cures Act (Pub. L. 114-255)
(1) General Approach
We finalized our budget neutrality methodology for periods of participation under the second 5 years of the 10-year extension period in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38285 through 38287). Similar to previous years, we stated in this rule, as well as in the FY 2019 IPPS/LTCH PPS proposed and final rules (83 FR 20444 and 41503, respectively) that we would incorporate an estimate of the costs of the demonstration, generally determined from historical, “as submitted” cost reports for the participating hospitals and appropriate update factors, into a budget neutrality offset amount to be applied to the national IPPS rates for the upcoming fiscal year. In addition, we stated that we would continue to apply our general policy from previous years of including, as a second component to the budget neutrality offset amount, the amount by which the actual costs of the demonstration for an earlier, given year (as determined from finalized cost reports when available) differed from the estimated costs for the demonstration set forth in the final IPPS rule for the corresponding fiscal year.
In the FY 2018 IPPS/LTCH PPS final rule and FY 2019 IPPS/LTCH PPS proposed and final rules, we described several distinct components to the budget neutrality offset amount for the specific fiscal years of the extension period authorized by Public Law 114-255.
- We include a component to our overall methodology similar to previous years, according to which an estimate of the costs of the demonstration for both previously and newly participating hospitals for the upcoming fiscal year is incorporated into a budget neutrality offset amount to be applied to the national IPPS rates for the upcoming fiscal year. In the FY 2019 IPPS final rule (83 FR 41506), we included such an estimate of the costs of the demonstration for each of FYs 2018 and 2019 into the budget neutrality offset amount for FY 2019. In the FY 2020 IPPS proposed rule, we included an estimate of the costs of the demonstration for FY 2020 for 29 hospitals.
- Similar to previous years, we continue to implement the policy of determining the difference between the actual costs of the demonstration as determined from finalized cost reports for a given fiscal year and the estimated costs indicated in the corresponding year's final rule, and including that difference as a positive or negative adjustment in the upcoming year's final rule. (For each previously participating hospital that has decided to participate in the second 5 years of the 10-year extension period, the cost-based payment methodology under the demonstration began on the date immediately following the end date of its period of performance for the first 5-year extension period. In addition, for previously participating hospitals that converted to CAH status during the time period of the second 5-year extension period, the demonstration payment methodology was applied to the date following the end date of its period of performance for the first extension period to the date of conversion). Therefore, for cost reporting periods starting in FYs 2015, 2016, and 2017, we will use available finalized cost reports that detail the actual costs of the demonstration for each of these fiscal years and incorporate these amounts into the budget neutrality calculation.
In the proposed rule, we identified the amount of the difference between actual and estimated costs based on finalized cost reports for FY 2014; and, in addition, we proposed that if finalized cost reports were available we would include the amount for FY 2015 in the budget neutrality offset adjustment to be applied to the national IPPS rates for FY 2020. In future IPPS rules, we will continue this reconciliation, calculating the difference between actual and estimated costs for the remaining years of the first extension period and, as previously described, the additional years of the demonstration under the second extension period, applying this difference to the budget neutrality offset adjustments identified in future years' final rules.
(2) Methodology for Estimating Demonstration Costs for FY 2020
We are using a methodology similar to previous years, according to which an estimate of the costs of the demonstration for the upcoming fiscal year is incorporated into a budget neutrality offset amount to be applied to the national IPPS rates for the upcoming fiscal year, that is, FY 2020. (In the proposed rule, we conducted this estimate on the basis of 29 participating hospitals; with one closing earlier this year, in this final rule we are limiting this estimate to the 28 currently participating hospitals.) The methodology for calculating this amount for FY 2020 proceeds according to the following steps:
Step 1: For each of the 28 participating hospitals, we identify the reasonable cost amount calculated under the reasonable cost-based methodology for covered inpatient hospital services, including swing beds, as indicated on the “as submitted” cost report for the most recent cost reporting period available. For each of these hospitals, these “as submitted” cost reports are those with cost report period end dates in CY 2017. We note that, for 3 of these hospitals, the 5-year participation authorized by Public Law 114-255 will end prior to the end of FY 2020. Therefore, consistent with previous practice, we prorate the cost amounts for these hospitals by the fraction of total months in the demonstration period of participation that fall within FY 2020 out of the total of 12 months in the fiscal year. For example, for a hospital whose period of performance ends June 30, 2020, this prorating factor is 0.75. We sum these hospital-specific amounts to arrive at a total general amount representing the costs for covered inpatient hospital services, including swing beds, across the 28 participating hospitals.
Then, we multiply this amount by the FYs 2018, 2019, and 2020 IPPS market basket percentage increases, which are formulated by the CMS Office of the Actuary. (We are using the finalized market basket percentage increase for FY 2020, which can be found at section IV.B of the preamble to this final rule). The result for the 28 participating hospitals is the general estimated reasonable cost amount for covered inpatient hospital services for FY 2020.
Consistent with our methods in previous years for formulating this estimate, we are applying the IPPS market basket percentage increases for FYs 2018 through 2020 to the applicable estimated reasonable cost amount (previously described) in order to model the estimated FY 2020 reasonable cost amount under the demonstration. We believe that the IPPS market basket percentage increases appropriately indicate the trend of increase in inpatient hospital operating costs under the reasonable cost methodology for the years involved.
Step 2: For each of the participating hospitals, we identify the estimated amount that would otherwise be paid in FY 2020 under applicable Medicare payment methodologies for covered inpatient hospital services, including swing beds (as indicated on the same set of “as submitted” cost reports as in Step 1), if the demonstration were not implemented. (Also, similar to step 1, we are prorating the amounts for hospitals whose period of participation ends prior to the end of FY 2020 by the fraction of total months in the demonstration period of participation for the hospital that fall within FY 2020 out of the total of 12 months in the fiscal year). We sum these hospital-specific amounts, and, in turn, multiply this sum by the FYs 2018, 2019 and 2020 IPPS applicable percentage increases. (Again, for FY 2020, we are using the finalized applicable percentage increase, per section IV.B of this final rule). This methodology differs from Step 1, in which we apply the market basket percentage increases to the hospitals' applicable estimated reasonable cost amount for covered inpatient hospital services. We believe that the IPPS applicable percentage increases are appropriate factors to update the estimated amounts that generally would otherwise be paid without the demonstration. This is because IPPS payments constitute the majority of payments that would otherwise be made without the demonstration and the applicable percentage increase is the factor used under the IPPS to update the inpatient hospital payment rates.
Step 3: We subtract the amount derived in Step 2 from the amount derived in Step 1. According to our methodology, the resulting amount indicates the total difference for the 28 hospitals (for covered inpatient hospital services, including swing beds), which will be the general estimated amount of the costs of the demonstration for FY 2020.
For this final rule, the resulting amount is $60,972,359, which we are incorporating into the budget neutrality offset adjustment for FY 2020. This estimated amount is based on the specific assumptions regarding the data sources used, that is, recently available “as submitted” cost reports and historical update factors for cost and payment. (This estimated amount differs from the corresponding figure identified in the proposed rule for 2 reasons: (1) Taking into account the hospital closure earlier this year, we are conducting the estimate on the basis of 28 participating hospitals, instead of 29; and (2) we are using the finalized market basket and applicable percentage increase updated for FY 2020. In the proposed rule, we said that if updated data become available prior to the final rule, we would use them as appropriate to estimate the costs for the demonstration program for FY 2020 in accordance with our methodology for determining the budget neutrality estimate).
(3) Reconciling Actual and Estimated Costs of the Demonstration for Previous Years (2014 and 2015)
As described earlier, we have calculated the difference for FYs 2005 through 2013 between the actual costs of the demonstration, as determined from finalized cost reports once available, and estimated costs of the demonstration as identified in the applicable IPPS final rules for these years. In the FY 2020 IPPS/LTCH proposed rule, we identified the difference between the total cost of the demonstration as indicated on finalized FY 2014 cost reports and the estimates for the costs of the demonstration for that year's final rule, and we proposed to adjust the current year's budget neutrality amount by the amount identified. We stated that if any information relevant to the determination of these amounts (for example, a cost report reopening) would necessitate a revision of these amounts, we would make the appropriate change and include the determination in the FY 2020 IPPS/LTCH PPS final rule. Furthermore, we stated, furthermore, that if the needed costs reports were available in time for the FY 2020 IPPS/LTCH PPS final rule, we also would identify the difference between the total cost of the demonstration based on finalized FY 2015 cost reports and the estimates for the costs of the demonstration for that year, and incorporate that amount into the budget neutrality offset amount for FY 2020.
For the proposed rule, we found that the actual costs of the demonstration for FY 2014 (that is, the amount from finalized cost reports for the 22 hospitals that were paid under the demonstration reasonable cost-based payment methodology for cost reporting periods with start dates during FY 2014) fell short of the estimated amount that was finalized in the FY 2014 IPPS/LTCH final rule for FY 2014 by $14,932,060. We have since then found no circumstance relevant to the determination of this amount that would require any change, and are incorporating this amount into the budget neutrality offset for the FY 2020 IPPS final rule.
Currently, finalized cost reports are available for the 21 hospitals that completed cost reports for periods of participation under the demonstration beginning in FY 2015. Accordingly, the actual costs of the demonstration for FY 2015 (that is, the amount from finalized cost reports for these hospitals), fell short of the estimated amount that was finalized in the FY 2015 IPPS/LTCH final rule for FY 2015 by $20,297,477. We note that for both of these fiscal years the amounts identified for the actual cost of the demonstration, determined from finalized cost reports, is less than the amount that was identified in the final rule for the respective year. Therefore, in keeping with previous policy finalized in situations when the costs of the demonstration fell short of the amount estimated in the corresponding year's final rule, we will be including this component as a negative adjustment to the budget neutrality offset amount for the current fiscal year.
(4) Total Proposed Budget Neutrality Offset Amount for FY 2020
Therefore, for this FY 2020 IPPS/LTCH PPS final rule, we are incorporating the following components into the calculation of the total budget neutrality offset for FY 2020:
- The amount determined under section IV.K. of the preamble of this proposed rule, representing the difference applicable to FY 2020 between the sum of the estimated reasonable cost amounts that would be paid under the demonstration to the 28 participating hospitals for covered inpatient hospital services and the sum of the estimated amounts that would generally be paid if the demonstration had not been implemented. This estimated amount is $60,972,359.
- The amount determined under section IV.K. of the preamble of this final rule according to which the actual costs of the demonstration for FY 2014 for the 22 hospitals that completed a cost reporting period beginning in FY 2014 differ from the estimated amount that was incorporated into the budget neutrality offset amount for FY 2014 in the FY 2014 IPPS/LTCH PPS final rule. Analysis of this set of cost reports shows that the actual costs of the demonstration fell short of the estimated amount finalized in the FY 2014 IPPS/LTCH PPS final rule by $14,932,060.
- The amount determined under section IV.K. of the preamble of this final rule according to which the actual costs of the demonstration for FY 2015 for the 21 hospitals that completed a cost reporting period beginning in FY 2015 differ from the estimated amount that was incorporated into the budget neutrality offset amount for FY 2015 in the FY 2015 IPPS/LTCH PPS final rule. Analysis of this set of cost reports shows that the actual costs of the demonstration fell short of the estimated amount finalized in the FY 2015 IPPS/LTCH PPS final rule by $20,297,477.
- In keeping with previously finalized policy, we are proposing to apply these differences, for FYs 2014 and 2015, according to which the actual costs of the demonstration fell short of the estimated amount determined in the final rule for the respective fiscal year by reducing the budget neutrality offset amount for FY 2020 by these amounts.
Therefore, in this FY 2020 IPPS/LTCH final rule, the total budget neutrality offset amount that we are applying to the national IPPS rates for FY 2020 is the estimated amount for FY 2020 ($60,972,359) minus the amount by which the actual costs of the demonstration fell short of the estimated amount for FY 2014 ($14,932,060) minus the amount by which the actual costs of the demonstration fell short of the estimated amount for FY 2015 ($20,297,477). This total is $25,742,822.
V. Changes to the IPPS for Capital-Related Costs
A. Overview
Section 1886(g) of the Act requires the Secretary to pay for the capital-related costs of inpatient acute hospital services in accordance with a prospective payment system established by the Secretary. Under the statute, the Secretary has broad authority in establishing and implementing the IPPS for acute care hospital inpatient capital-related costs. We initially implemented the IPPS for capital-related costs in the FY 1992 IPPS final rule (56 FR 43358). In that final rule, we established a 10-year transition period to change the payment methodology for Medicare hospital inpatient capital-related costs from a reasonable cost-based payment methodology to a prospective payment methodology (based fully on the Federal rate).
FY 2001 was the last year of the 10-year transition period that was established to phase in the IPPS for hospital inpatient capital-related costs. For cost reporting periods beginning in FY 2002, capital IPPS payments are based solely on the Federal rate for almost all acute care hospitals (other than hospitals receiving certain exception payments and certain new hospitals). (We refer readers to the FY 2002 IPPS final rule (66 FR 39910 through 39914) for additional information on the methodology used to determine capital IPPS payments to hospitals both during and after the transition period.)
The basic methodology for determining capital prospective payments using the Federal rate is set forth in the regulations at 42 CFR 412.312. For the purpose of calculating capital payments for each discharge, the standard Federal rate is adjusted as follows:
(Standard Federal Rate) × (DRG Weight) × (Geographic Adjustment Factor (GAF)) × (COLA for hospitals located in Alaska and Hawaii) × (1 + Capital DSH Adjustment Factor + Capital IME Adjustment Factor, if applicable).
In addition, under § 412.312(c), hospitals also may receive outlier payments under the capital IPPS for extraordinarily high-cost cases that qualify under the thresholds established for each fiscal year.
B. Additional Provisions
1. Exception Payments
The regulations at 42 CFR 412.348 provide for certain exception payments under the capital IPPS. The regular exception payments provided under §§ 412.348(b) through (e) were available only during the 10-year transition period. For a certain period after the transition period, eligible hospitals may have received additional payments under the special exceptions provisions at § 412.348(g). However, FY 2012 was the final year hospitals could receive special exceptions payments. For additional details regarding these exceptions policies, we refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51725).
Under § 412.348(f), a hospital may request an additional payment if the hospital incurs unanticipated capital expenditures in excess of $5 million due to extraordinary circumstances beyond the hospital's control. Additional information on the exception payment for extraordinary circumstances in § 412.348(f) can be found in the FY 2005 IPPS final rule (69 FR 49185 and 49186).
2. New Hospitals
Under the capital IPPS, the regulations at 42 CFR 412.300(b) define a new hospital as a hospital that has operated (under previous or current ownership) for less than 2 years and lists examples of hospitals that are not considered new hospitals. In accordance with § 412.304(c)(2), under the capital IPPS, a new hospital is paid 85 percent of its allowable Medicare inpatient hospital capital-related costs through its first 2 years of operation, unless the new hospital elects to receive full prospective payment based on 100 percent of the Federal rate. We refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51725) for additional information on payments to new hospitals under the capital IPPS.
3. Payments for Hospitals Located in Puerto Rico
In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57061), we revised the regulations at 42 CFR 412.374 relating to the calculation of capital IPPS payments to hospitals located in Puerto Rico beginning in FY 2017 to parallel the change in the statutory calculation of operating IPPS payments to hospitals located in Puerto Rico, for discharges occurring on or after January 1, 2016, made by section 601 of the Consolidated Appropriations Act, 2016 (Pub. L. 114-113). Section 601 of Public Law 114-113 increased the applicable Federal percentage of the operating IPPS payment for hospitals located in Puerto Rico from 75 percent to 100 percent and decreased the applicable Puerto Rico percentage of the operating IPPS payments for hospitals located in Puerto Rico from 25 percent to zero percent, applicable to discharges occurring on or after January 1, 2016. As such, under revised § 412.374, for discharges occurring on or after October 1, 2016, capital IPPS payments to hospitals located in Puerto Rico are based on 100 percent of the capital Federal rate.
C. Annual Update for FY 2020
The annual update to the national capital Federal rate, as provided for in 42 CFR 412.308(c), for FY 2020 is discussed in section III. of the Addendum to this FY 2020 IPPS/LTCH PPS final rule.
In section II.D. of the preamble of this FY 2020 IPPS/LTCH PPS final rule, we present a discussion of the MS-DRG documentation and coding adjustment, including previously finalized policies and historical adjustments, as well as the adjustment to the standardized amount under section 1886(d) of the Act that we are making for FY 2020, in accordance with the amendments made to section 7(b)(1)(B) of Public Law 110-90 by section 414 of the MACRA. Because these provisions require us to make an adjustment only to the operating IPPS standardized amount, we are not making a similar adjustment to the national capital Federal rate (or to the hospital-specific rates).
VI. Changes for Hospitals Excluded from the IPPS
A. Rate-of-Increase in Payments to Excluded Hospitals for FY 2020
Certain hospitals excluded from a prospective payment system, including children's hospitals, 11 cancer hospitals, and hospitals located outside the 50 States, the District of Columbia, and Puerto Rico (that is, hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa) receive payment for inpatient hospital services they furnish on the basis of reasonable costs, subject to a rate-of-increase ceiling. A per discharge limit (the target amount, as defined in § 413.40(a) of the regulations) is set for each hospital based on the hospital's own cost experience in its base year, and updated annually by a rate-of-increase percentage. For each cost reporting period, the updated target amount is multiplied by total Medicare discharges during that period and applied as an aggregate upper limit (the ceiling as defined in § 413.40(a)) of Medicare reimbursement for total inpatient operating costs for a hospital's cost reporting period. In accordance with § 403.752(a) of the regulations, religious nonmedical health care institutions (RNHCIs) also are subject to the rate-of-increase limits established under § 413.40 of the regulations discussed previously. Furthermore, in accordance with § 412.526(c)(3) of the regulations, extended neoplastic disease care hospitals also are subject to the rate-of-increase limits established under § 413.40 of the regulations discussed previously.
As explained in the FY 2006 IPPS final rule (70 FR 47396 through 47398), beginning with FY 2006, we have used the percentage increase in the IPPS operating market basket to update the target amounts for children's hospitals, the 11 cancer hospitals, and RNHCIs. Consistent with the regulations at §§ 412.23(g), 413.40(a)(2)(ii)(A), and 413.40(c)(3)(viii), we also have used the percentage increase in the IPPS operating market basket to update target amounts for short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa. In the FYs 2014 and 2015 IPPS/LTCH PPS final rules (78 FR 50747 through 50748 and 79 FR 50156 through 50157, respectively), we adopted a policy of using the percentage increase in the FY 2010-based IPPS operating market basket to update the target amounts for FY 2014 and subsequent fiscal years for children's hospitals, the 11 cancer hospitals, RNHCIs, and short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa. However, in the FY 2018 IPPS/LTCH PPS final rule, we rebased and revised the IPPS operating basket to a 2014 base year, effective for FY 2018 and subsequent years (82 FR 38158 through 38175), and finalized the use of the percentage increase in the 2014-based IPPS operating market basket to update the target amounts for children's hospitals, the 11 cancer hospitals, RNHCIs, and short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa for FY 2018 and subsequent years. Accordingly, for FY 2020, the rate-of-increase percentage to be applied to the target amount for these hospitals is the FY 2020 percentage increase in the 2014-based IPPS operating market basket.
For the FY 2020 IPPS/LTCH PPS proposed rule, based on IGI's fourth quarter 2018 forecast, we estimated that the 2014-based IPPS operating market basket update for FY 2020 would be 3.2 percent (that is, the estimate of the market basket rate-of-increase). Based on this estimate, we stated in the proposed rule (84 FR 19454) that the FY 2020 rate-of-increase percentage that would be applied to the FY 2019 target amounts in order to calculate the FY 2020 target amounts for children's hospitals, the 11 cancer hospitals, RNCHIs, and short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa would be 3.2 percent, in accordance with the applicable regulations at 42 CFR 413.40. However, we proposed that if more recent data became available for the final rule, we would use them to calculate the final IPPS operating market basket update for FY 2020. For this FY 2020 IPPS/LTCH PPS final rule, based on IGI's second quarter 2019 forecast (which is the most recent data available), we calculated the 2014-based IPPS operating market basket update for FY 2020 to be 3.0 percent. Therefore, the FY 2020 rate-of-increase percentage that is applied to the FY 2019 target amounts in order to calculate the FY 2020 target amounts for children's hospitals, the 11 cancer hospitals, RNCHIs, and short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa is 3.0 percent, in accordance with the applicable regulations at 42 CFR 413.40.
In addition, payment for inpatient operating costs for hospitals classified under section 1886(d)(1)(B)(vi) of the Act (which we refer to as “extended neoplastic disease care hospitals”) for cost reporting periods beginning on or after January 1, 2015, is to be made as described in 42 CFR 412.526(c)(3), and payment for capital costs for these hospitals is to be made as described in 42 CFR 412.526(c)(4). (For additional information on these payment regulations, we refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38321 through 38322).) Section 412.526(c)(3) provides that the hospital's Medicare allowable net inpatient operating costs for that period are paid on a reasonable cost basis, subject to that hospital's ceiling, as determined under § 412.526(c)(1), for that period. Under section 412.526(c)(1), for each cost reporting period, the ceiling was determined by multiplying the updated target amount, as defined in § 412.526(c)(2), for that period by the number of Medicare discharges paid during that period. Section 412.526(c)(2)(i) describes the method for determining the target amount for cost reporting periods beginning during FY 2015. Section 412.526(c)(2)(ii) specifies that, for cost reporting periods beginning during fiscal years after FY 2015, the target amount will equal the hospital's target amount for the previous cost reporting period updated by the applicable annual rate-of-increase percentage specified in § 413.40(c)(3) for the subject cost reporting period (79 FR 50197).
For FY 2020, in accordance with § 412.22(i) and § 412.526(c)(2)(ii) of the regulations, for cost reporting periods beginning during FY 2020, the update to the target amount for extended neoplastic disease care hospitals (that is, hospitals described under § 412.22(i)) is the applicable annual rate-of-increase percentage specified in § 413.40(c)(3) for FY 2020, which would be equal to the percentage increase in the hospital market basket index, which, in the proposed rule, was estimated to be the percentage increase in the 2014-based IPPS operating market basket (that is, the estimate of the market basket rate-of-increase). Accordingly, for the FY 2019 IPPS/LTCH PPS proposed rule, the update to an extended neoplastic disease care hospital's target amount for FY 2020 was 3.2 percent, which was based on IGI's fourth quarter 2018 forecast. Furthermore, we proposed that if more recent data became available for the final rule, we would use that updated data to calculate the IPPS operating market basket update for FY 2020. For this final rule, based on IGI's second quarter 2019 forecast (which is the most recent data available), the update to an extended neoplastic disease care hospital's target amount for FY 2020 is 3.0 percent.
We received no comments in response to the proposals discussed above. Thus, for the reasons discussed above and in the proposed rule, we are finalizing these policies as proposed without modification.
We received several public comments related to excluded hospitals that addressed issues that were outside the scope of the FY 2020 proposed rule. We will keep these comments in mind and may consider them for future rulemaking.
B. Request for Public Comments on Methodologies and Requirements for TEFRA Adjustments to the Rate-of-Increase Ceiling
1. General Background
Section 1886(b) of the Act, as amended by the Tax Equity and Fiscal Responsibility Act (TEFRA) of 1982, establishes a ceiling on the allowable rate of increase in hospital inpatient operating costs per discharge applicable to cost reporting periods beginning on or after October 1, 1982. However, effective with cost reporting periods beginning on or after October 1, 1983, most hospitals are paid under the prospective payment system (PPS) as described in section 1886(d) of the Act, 42 CFR part 412, and Chapter 28 of the Provider Reimbursement Manual (PRM) (CMS Pub. 15-1). Currently, hospitals that are paid under TEFRA include cancer hospitals (11 qualified by statute under section 1886(d)(1)(B)(v) of the Act), children's hospitals, and hospitals outside the 50 States, the District of Columbia, and Puerto Rico (that is, acute care hospitals located in the U.S. Virgin Islands, Guam, American Samoa, and the Northern Mariana Islands). Under certain circumstances, we may provide for an adjustment to the rate-of-increase ceiling or may assign a new base period.
Medicare payment for inpatient hospital services under the TEFRA system is made on a reasonable cost basis, as previously noted, subject to a limit or ceiling. The ceiling is determined from a hospital's target amount per discharge updated from its base year. Specifically, a hospital's TEFRA target amount per discharge is determined from its total Medicare inpatient operating costs per Medicare discharge in its base year. This target amount per discharge is updated each year for inflation based on the IPPS operating market basket increase. Multiplying the TEFRA target amount per discharge by the Medicare discharges in a particular cost reporting period produces the maximum amount (the ceiling) Medicare will pay the hospital for inpatient hospital services. In other words, under the TEFRA system, Medicare payment is the lesser of the reasonable costs incurred or the ceiling amount. If a hospital's inpatient operating costs exceed the ceiling in a cost reporting period, section 1886(b)(4)(A)(i) of the Act and implementing regulations at § 413.40 allow hospitals paid under the TEFRA system to request adjustments to increase their Medicare payment limits (that is, their ceiling) or to request a new base year (a permanent revised TEFRA target amount per discharge for determining the ceiling) to account for certain factors such as a significant change in services or patient population.
2. TEFRA Adjustment Requests
Under the regulations at 42 CFR 413.40(g), if a hospital's inpatient operating costs exceed the ceiling in a cost reporting period, hospitals may request an increase to their Medicare payment limits (that is, their ceiling) to account for cost distortions between the base year and current year. Section 3004.1 of the PRM states that distortions in inpatient operating costs resulting in noncomparability of the cost reporting periods are generally the result of extraordinary circumstances, an increase in the average length of stay of Medicare patients, or changes in the volume or intensity of direct patient care services. Section 3004 of the PRM provides extensive examples of noncomparability of cost reporting periods due to direct patient care changes with calculations for increases of average length of stay, changes in the intensity of care, as well as for additions/deletions of services. These examples were developed many years ago to assist providers in filing an adjustment request and to provide guidance to MACs when reviewing and evaluating a provider's adjustment request. The examples emphasize that the methodologies used to determine the amount of the adjustment are based on comparisons between the base year costs and current year costs. To receive an adjustment to its ceiling, the provider must demonstrate that the increased Medicare costs are reasonable, related to direct patient care services, attributable to the circumstances specified, separately identified by the hospital, verified by the contractor, and tie to costs quantified in its cost report. In some cases, an adjustment may be adopted permanently and reflected in the hospital's ceiling in subsequent cost reporting periods.
The delivery of direct patient care services, as well as the cost report form and instructions, have evolved since the guidance and examples currently in section 3004 of the PRM (Pub. 15-1) were originally developed. In the FY 2020 IPPS/LTCH proposed rule (84 FR 19454-19455), we solicited public comments, suggestions, and recommendations regarding the methodologies and examples provided in section 3004 of the PRM to determine an appropriate adjustment amount, considering the current environment facing providers paid by Medicare under the TEFRA system.
As previously noted, under 42 CFR 413.40(i), hospitals can request a permanent change to their ceiling by requesting a new base year for determining their target amount per discharge. In accordance with 42 CFR 413.40(i)(1)(i)(B), this process is meant to account for substantial and permanent changes in furnishing patient care services since the base period, and, as such, the requirements are stringent. Historically, we have rarely authorized assignment of a new base year period because the adjustment mechanism as previously discussed is meant to address most situations where there is distortion in costs between the base year and the current period and providers seldom meet the criteria for a new base period. We requested public comments, suggestions, and recommendations on the possible criteria and circumstances needed to warrant a new base period, and, importantly, the documentation that would be required to qualify, particularly relative to and differentiating it from an adjustment.
As stated earlier, we invited comments, suggestions, and recommendations for regulatory and other policy changes to the TEFRA adjustment process. We also requested feedback on whether or not there should be standardization in the supporting documentation (such as electronic workbooks) as part of TEFRA adjustment requests and, if so, we invited commenters to provide specific examples.
Comment: Several commenters stated their appreciation for CMS's consideration of improvements to the TEFRA adjustment process currently afforded to providers exempted from the IPPS and reimbursed under TEFRA.
Response: We thank commenters for responding and we will take these comments into consideration for future rulemaking.
C. Report on Adjustment (Exception) Payments
Section 4419(b) of Pub. L. 105-33 requires the Secretary to publish annually in the Federal Register a report describing the total amount of adjustment payments made to excluded hospitals and hospital units by reason of section 1886(b)(4) of the Act during the previous fiscal year.
The process of requesting, adjusting, and awarding an adjustment payment is likely to occur over a 2-year period or longer. First, generally, an excluded hospital must file its cost report for the fiscal year in accordance with § 413.24(f)(2) of the regulations. The MAC reviews the cost report and issues a notice of provider reimbursement (NPR). Once the hospital receives the NPR, if its operating costs are in excess of the ceiling, the hospital may file a request for an adjustment payment. After the MAC receives the hospital's request in accordance with applicable regulations, the MAC or CMS, depending on the type of adjustment requested, reviews the request and determines if an adjustment payment is warranted. This determination is sometimes not made until more than 180 days after the date the request is filed because there are times when the request applications are incomplete and additional information must be requested in order to have a completed request application. However, in an attempt to provide interested parties with data on the most recent adjustment payments for which we have data, we are publishing data on adjustment payments that were processed by the MAC or CMS during FY 2018.
This table includes the most recent data available from the MACs and CMS on adjustment payments that were adjudicated during FY 2018. As previously indicated, the adjustments made during FY 2018 only pertain to cost reporting periods ending in years prior to FY 2018. Total adjustment payments made to IPPS-excluded hospitals during FY 2018 are $20,095,056. The table depicts for each class of hospitals, in the aggregate, the number of adjustment requests adjudicated, the excess operating costs over the ceiling, and the amount of the adjustment payments.

D. Critical Access Hospitals (CAHs)
1. Background
Section 1820 of the Act provides for the establishment of Medicare Rural Hospital Flexibility Programs (MRHFPs), under which individual States may designate certain facilities as critical access hospitals (CAHs). Facilities that are so designated and meet the CAH conditions of participation under 42 CFR part 485, subpart F, will be certified as CAHs by CMS. Regulations governing payments to CAHs for services to Medicare beneficiaries are located in 42 CFR part 413.
2. Change Related to CAH Payment for Ambulance Services
a. Background
Section 1834(l) of the Act sets forth the payment rules for ambulance services. Generally, payment to ambulance providers and suppliers for ambulance services are made under the Ambulance Fee Schedule. Section 205 of BIPA (Pub. L. 106-554) amended section 1834(l) of the Act by adding a paragraph (8), which, effective for services furnished on or after December 21, 2000, provided that the Secretary would pay the reasonable costs incurred in furnishing ambulance services if such services are furnished by a CAH (as defined in section 1861(mm)(1) of the Act), or by an entity that is owned and operated by a CAH, but only if the CAH or entity is the only provider or supplier of ambulance services that is located within a 35-mile drive of the CAH. Regulations implementing section 1834(l)(8) of the Act are set forth at 42 CFR 413.70(b)(5). For purposes of this discussion, the term “provider” of ambulance services means all Medicare-participating providers that submit claims under Medicare for ambulance services (for example, hospitals, CAHs, skilled nursing facilities (SNFs), and home health agencies (HHAs)), and the term “supplier” of ambulance services means an entity that provides ambulance services and that is independent of any Medicare-participating or non-Medicare-participating provider. The terms “supplier” and “provider of services” are defined in sections 1861(d) and (u) of the Act, respectively, and the term “provider or supplier of ambulance services” appears in section 1834(l)(8) of the Act.
Section 3128(a) of the Affordable Care Act (Pub. L. 111-148) amended section 1834(l)(8) of the Act by specifying that payment for the reasonable costs incurred by a CAH or by an entity that is owned and operated by a CAH in furnishing ambulance services would be at “101 percent” of the reasonable costs incurred in furnishing such services. As such, section 3128(a) of the Affordable Care Act increased payment for ambulance services furnished by CAHs or entities owned and operated by CAHs to 101 percent of the reasonable costs, subject to the requirements outlined in section 1834(l)(8) of the Act, effective for cost reporting periods beginning on or after January 1, 2004. We amended § 413.70(b)(5)(i) in the FY 2011 IPPS/LTCH PPS final rule (75 FR 50361) to conform to the statute, as amended.
More recently, in the FY 2012 IPPS/LTCH PPS final rule (76 FR 51729), to ensure consistency between the regulations and statute, we revised § 413.70(b)(5)(i) by adding a new paragraph (C) to state that, effective for cost reporting periods beginning on or after October 1, 2011, payment for ambulance services furnished by a CAH or by a CAH-owned and operated entity is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the entity is the only provider or supplier of ambulance services located within a 35-mile drive of the CAH. If there is no provider or supplier of ambulance services located within a 35-mile drive of the CAH and there is an entity that is owned and operated by a CAH that is more than a 35-mile drive from the CAH, payment for ambulance services furnished by that entity is 101 percent of the reasonable costs of the entity in furnishing those services, but only if the entity is the closest provider or supplier of ambulance services to the CAH. Therefore, a CAH is paid 101 percent of the reasonable costs for its ambulance services only if there is no other provider or supplier of ambulance services within a 35-mile drive of the CAH. If there is another provider or supplier of ambulance services located within a 35-mile drive of the CAH, the CAH is paid for its ambulance services using the Ambulance Fee Schedule.
b. Proposed Change and Final Policy
As previously indicated, consistent with the statutory provision at section 1834(l)(8) of the Act, § 413.70(b)(5)(i)(C) currently states in relevant part that payment for ambulance services furnished by a CAH or an entity that is owned and operated by a CAH is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the entity is the only provider or supplier of ambulance services located within a 35-mile drive of the CAH. It has been brought to our attention that there may be instances where a provider or supplier of ambulance services that is not owned or operated by the CAH is located within a 35-mile drive of the CAH, but that provider or supplier of ambulance services is not legally authorized to furnish ambulance services to transport individuals either to or from the CAH. For example, consider the scenario where an ambulance supplier is located within a 35-mile drive of a CAH, but in a different State, and the ambulance supplier is not legally authorized (for example, the supplier of ambulance services does not have the appropriate State licensure) to furnish ambulance services in the State in which the CAH is located. Under this scenario, § 413.70(b)(5)(i)(C) requires that the CAH be paid for its ambulance services using the Ambulance Fee Schedule, even though the out-of-state ambulance supplier cannot actually furnish ambulance services to transport individuals either to or from the CAH. We believe this outcome is not consistent with the intent of the Medicare Rural Hospital Flexibility Program, which is to provide access to care to individuals living in remote and rural areas. A CAH may provide crucial health care services to individuals living in a remote and rural area. However, if transport services to that CAH are limited due to lack of ambulance services, health care services available to individuals living in the CAH's service area may also be limited. A lack of ambulance services within the CAH's service area could limit access to care for individuals living in these remote and rural areas, particularly in emergency situations and when individuals have no other mode of transportation due to hazardous traveling conditions. In general, payment for ambulance services based on 101 percent of the reasonable costs is higher than payment made under the Ambulance Fee Schedule. This higher payment is intended to provide CAHs with sufficient payment to sustain their own ambulance services when no other ambulance services are available in their service area. If a CAH does not receive reasonable cost-based payments for its ambulance services because there is another provider or supplier of ambulance services within a 35-mile drive of the CAH, even if that provider or supplier is not legally authorized to transport individuals either to or from the CAH, the CAH may be unable to support the costs of providing ambulance services in its service area.
Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19455 through 19456), we proposed to address this “gap” in the current regulation at § 413.70(b)(5)(i)(C) by revising our interpretation of the requirement in section 1834(l)(8)(B) of the Act that the CAH or the entity owned and operated by the CAH be the only provider or supplier of ambulance services that is located within a 35-mile drive of such a CAH, to exclude consideration of ambulance providers or suppliers that are not legally authorized to furnish ambulance services to transport individuals either to or from the CAH. Specifically, we proposed to interpret section 1834(l)(8)(B) of the Act to mean that the CAH or the CAH-owned and operated entity must be the only provider or supplier of ambulance services within a 35-mile drive of the CAH that is legally authorized to furnish ambulance services to individuals transported to or from the CAH. We stated that we believe this is a reasonable reading of the statutory language because it retains the requirement that the CAH or the CAH-owned and operated entity be the only provider or supplier of ambulance services within a 35-mile drive of the CAH that is available to transport individuals either to or from the CAH. We proposed to revise § 413.70(b)(5)(i) of the regulations to reflect this revised interpretation by adding a new paragraph (D) to state that, effective for cost reporting periods beginning on or after October 1, 2019, payment for ambulance services furnished by a CAH or by an entity that is owned and operated by a CAH is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the entity is the only provider or supplier of ambulance services located within a 35-mile drive of the CAH, excluding ambulance providers or suppliers that are not legally authorized to furnish ambulance services to transport individuals either to or from the CAH. Consistent with the existing policy under § 413.70(b)(5)(i)(C), if there is no provider or supplier of ambulance services located within a 35-mile drive of the CAH and there is an entity that is owned and operated by a CAH that is more than a 35-mile drive from the CAH, payment for ambulance services furnished by that entity is 101 percent of the reasonable costs of the entity in furnishing those services, but only if the entity is the closest provider or supplier of ambulance services to the CAH. We also proposed a conforming change to § 413.70(b)(5)(i)(C) to make that existing provision effective only through September 30, 2019.
As stated earlier in this discussion, if a CAH does not receive reasonable cost-based payments for its ambulance services, which in general provide higher payment compared to the Ambulance Fee Schedule, the CAH may be unable to support the costs of providing ambulance services in its service area. As such, we stated that we believe that our proposed change to allow for payment based on 101 percent of the reasonable costs of the CAH or the CAH-owned and operated entity in furnishing ambulance services, in a situation where there is another provider or supplier of ambulance services located within a 35-mile drive of the CAH that is not legally authorized to transport individuals either to or from the CAH, would improve access to care in remote and rural areas, particularly in situations where an individual is experiencing an emergency and can only receive the necessary services through ambulance transport to or from the CAH or in situations where no other mode of transportation is advisable. Furthermore, we stated that we believe our proposal is consistent with the original purpose of section 1834(l)(8) of the Act, which was to help ensure that areas served by CAHs would have adequate access to ambulance services.
Comment: Commenters supported CMS' proposal to interpret section 1834(l)(8)(B) of the Act to mean that payment for ambulance services furnished by a CAH or by an entity that is owned and operated by a CAH is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the CAH-owned and operated entity is the only provider or supplier of ambulance services within a 35-mile drive of the CAH that is legally authorized to furnish ambulance services to transport individuals to or from the CAH.
Commenters stated that this proposal supports rural health care, removes artificial reimbursement barriers to regional health care delivery, and will improve access to care for individuals living in remote and rural areas, particularly in emergency situations and when individuals have no other mode of transportation due to hazardous traveling conditions.
Response: We appreciate the commenters' support for the proposed change to the regulation governing payment for ambulance services furnished by a CAH or by a CAH-owned and operated entity.
Comment: Several commenters urged CMS to expand the availability of cost-based reimbursement to ambulance services where patient transfer is required based on the CAH conditions of participation (CoPs). The commenters stated that CAHs are uniquely required to transfer certain patients to receive care at other facilities. However, in many rural areas, even those that are otherwise served by an ambulance service, CAHs often struggle to find medical transport for facility to facility transfers. The commenters stated that rural ambulance services are often staffed by a limited number of volunteers and are unable to provide urgently needed facility to facility transfers because of limited equipment and staffing. The commenters stated that expansion of cost-based reimbursement to transportation that is required under the CoPs is consistent with the statute and CMS' commitment to ensuring rural Americans have access to care.
A commenter stated that within a 35-mile radius of its CAH there are two Emergency Medical Services (EMS) agencies, both of which have a mutual aid agreement with the CAH allowing either agency or the CAH to respond to a 911 call in the rare occurrence when another member of the agreement is unavailable or unable to respond. However, neither EMS agency would be able to absorb the needs of the community should the CAH no longer be able to provide ambulance services.
This commenter also stated that its CAH ambulance service operates significantly in the red, primarily due to its payer mix, the majority of patients being Medicare beneficiaries. The commenter indicated that due to the way the proposed rule is written, its CAH ambulance service does not qualify for cost-based reimbursement due to the EMS exclusion. The commenter stated they are concerned they will not be able to sustain the CAH's EMS service due to significant financial loses and there is not another service that is willing or able to take over their work should they have to discontinue or reduce EMS services. The commenter requested that CMS consider language that may allow their ambulance service and similarly situated organizations to participate in cost-based reimbursement.
Another commenter stated they believe the proposal only benefits a small number of CAHs across the country and urged CMS to either make exceptions to allow all CAHs providing paramedic-level ambulance services to receive reimbursement at 101 percent of reasonable costs or consider making changes to the distance requirements in the IPPS to address reimbursement struggles CAHs are experiencing with respect to EMS. The commenter specified that many of the CAHs in their state are closer than 35 miles and many are the sole provider of ambulance services and the only paramedic-level provider serving their community. The commenter stated that in order for the people of their state to have guaranteed access to EMS, the services would need to be provided by the CAH and to do so, CAHs need cost-based reimbursement as the fee schedule payments do not come close to covering the costs of these services.
Another commenter suggested that CMS consider an additional change that the commenter believed would be consistent with the intent of the proposal and would provide sustainable payments for CAH-operated ambulance services that are functionally the only ambulance services available to a CAH and its community The commenter stated that there are many cases where there is another ambulance service within 35 miles of a CAH, but the ambulance does not serve the CAH or the CAH's community due to geographic and/or economic factors, rather than legal constraints. For example, there are many cases in which the other ambulance service does not serve the CAH or its adjacent community, other than for inter-facility transport or in the event of a regional emergency that exceeds the capacity of the local service. The commenter recommended that CMS consider amending the proposal to allow reimbursement at 101 percent of reasonable costs for CAH ambulance services where the CAH or the CAH-owned and operated entity can demonstrate it is the single source of ambulance services for its community, other than during unusual circumstances.
Response: We are not certain of the specific CoPs that are being referenced by the commenters. We note that the regulation at § 485.603 specifies that a rural health network is an organization that includes the provision of emergency and nonemergency transportation among members. The regulation at § 485.616 includes a requirement that if a CAH is a member of a rural health network as defined in § 485.603, the CAH must have in effect an agreement with at least one hospital that is a member of the network for the provision of emergency and nonemergency transportation between the facility and the hospital. Separately, section 1867 of the Act and the implementing regulations at § 489.24 outline the requirements CAHs and hospitals must meet to ensure compliance with the Emergency Medical Treatment and Labor Act (EMTALA), including the provision of appropriate transfers between participating hospitals.
We also commend the commenters for their efforts to ensure that individuals living in rural areas have access to sufficient ambulance and EMS services, including transportation to other facilities to receive specialty care. We acknowledge the point made by commenters that because CAHs have a legal obligation to transfer patients, the reimbursement they receive for ambulance services should reflect that requirement. However, we note that most of the scenarios described by the commenters, including those regarding transfer of patients, appear to involve situations where there is another provider or supplier of ambulance services within a 35-mile drive of the CAH, and that ambulance provider or supplier is not legally precluded from providing ambulance services to individuals living within the CAH's service area. Section 1834(l)(8) of the Act specifies that payment to a CAH or CAH owned and operated entity is 101 percent of the reasonable costs incurred in furnishing ambulance services “only if the critical access hospital or entity is the only provider or supplier of ambulance services that is located within a 35-mile drive of such critical access hospital.” As we explained in the FY 2020 IPPS proposed rule (84 FR 19456), we believe an interpretation of this statutory language that excludes providers and suppliers of ambulance services that are not legally authorized to transport individuals either to or from the CAH is reasonable because it retains the requirement that the CAH or the CAH-owned or operated entity be the only provider or supplier of ambulance services within a 35-mile drive of the CAH that is available to transport individuals either to or from the CAH. In contrast, we do not believe section 1834(l)(8) of the Act can be interpreted to allow CMS to provide payment to CAHs at 101 percent of the reasonable costs incurred in furnishing ambulance services in situations where there is another provider or supplier of ambulance services within a 35-mile drive of the CAH that is legally authorized, and thus available, to provide ambulance services to transport individuals to or from the CAH.
After consideration of the public comments we received, we are finalizing our proposal to interpret the requirement in section 1834(l)(8)(B) of the Act that the CAH or the CAH-owned and operated entity be the only provider or supplier of ambulance services within a 35-mile drive of the CAH, to exclude consideration of ambulance providers or suppliers that are not legally authorized to furnish ambulance services to transport individuals to or from the CAH. As indicated earlier in this section, the term “provider” of ambulance services means all Medicare-participating providers that submit claims under Medicare for ambulance services (for example, hospitals, CAHs, skilled nursing facilities (SNFs), and home health agencies (HHAs)), and the term “supplier” of ambulance services means an entity that provides ambulance services and that is independent of any Medicare-participating or non-Medicare-participating provider. We are also finalizing our proposal to revise § 413.70(b)(5)(i) of the regulations to reflect our revised interpretation of section 1834(l)(8) of the Act by adding a new paragraph (D) to state that, effective for cost reporting periods beginning on or after October 1, 2019, payment for ambulance services furnished by a CAH or by an entity that is owned and operated by a CAH is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the entity is the only provider or supplier of ambulance services located within a 35-mile drive of the CAH, excluding ambulance providers or suppliers that are not legally authorized to furnish ambulance services to transport individuals either to or from the CAH. Consistent with the existing policy under § 413.70(b)(5)(i)(C), paragraph (D) will also state that if there is no provider or supplier of ambulance services located within a 35-mile drive of the CAH and there is an entity that is owned and operated by a CAH that is more than a 35-mile drive from the CAH, payment for ambulance services furnished by that entity is 101 percent of the reasonable costs of the entity in furnishing those services, but only if the entity is the closest provider or supplier of ambulance services to the CAH. We are also finalizing the proposed conforming change to § 413.70(b)(5)(i)(C), which will make that provision effective only for cost reporting periods starting on or before September 30, 2019.
3. Frontier Community Health Integration Project (FCHIP) Demonstration
As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41516 through 41517) and in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19456 through 19458), section 123 of the Medicare Improvements for Patients and Providers Act of 2008 (Pub. L. 110-275), as amended by section 3126 of the Affordable Care Act, authorizes a demonstration project to allow eligible entities to develop and test new models for the delivery of health care services in eligible counties in order to improve access to and better integrate the delivery of acute care, extended care and other health care services to Medicare beneficiaries. The demonstration is titled “Demonstration Project on Community Health Integration Models in Certain Rural Counties,” and is commonly known as the Frontier Community Health Integration Project (FCHIP) demonstration.
The authorizing statute states the eligibility criteria for entities to be able to participate in the demonstration. An eligible entity, as defined in section 123(d)(1)(B) of Public Law 110-275, as amended, is an MRHFP grantee under section 1820(g) of the Act (that is, a CAH); and is located in a State in which at least 65 percent of the counties in the State are counties that have 6 or less residents per square mile.
The authorizing statute stipulates several other requirements for the demonstration. Section 123(d)(2)(B) of Public Law 110-275, as amended, limits participation in the demonstration to eligible entities in not more than 4 States. Section 123(f)(1) of Public Law 110-275 requires the demonstration project to be conducted for a 3-year period. In addition, section 123(g)(1)(B) of Public Law 110-275 requires that the demonstration be budget neutral. Specifically, this provision states that, in conducting the demonstration project, the Secretary shall ensure that the aggregate payments made by the Secretary do not exceed the amount which the Secretary estimates would have been paid if the demonstration project under the section were not implemented. Furthermore, section 123(i) of Public Law 110-275 states that the Secretary may waive such requirements of titles XVIII and XIX of the Act as may be necessary and appropriate for the purpose of carrying out the demonstration project, thus allowing the waiver of Medicare payment rules encompassed in the demonstration.
In January 2014, CMS released a request for applications (RFA) for the FCHIP demonstration. Using 2013 data from the U.S. Census Bureau, CMS identified Alaska, Montana, Nevada, North Dakota, and Wyoming as meeting the statutory eligibility requirement for participation in the demonstration. The RFA solicited CAHs in these five States to participate in the demonstration, stating that participation would be limited to CAHs in four of the States. To apply, CAHs were required to meet the eligibility requirements in the authorizing legislation, and, in addition, to describe a proposal to enhance health-related services that would complement those currently provided by the CAH and better serve the community's needs. In addition, in the RFA, CMS interpreted the eligible entity definition in the statute as meaning a CAH that receives funding through the MHRFP. The RFA identified four interventions, under which specific waivers of Medicare payment rules would allow for enhanced payment for telehealth, skilled nursing facility/nursing facility beds, ambulance services, and home health services, respectively. These waivers were formulated with the goal of increasing access to care with no net increase in costs.
Ten CAHs were selected for participation in the demonstration, which started on August 1, 2016. These CAHs are located in Montana, Nevada, and North Dakota, and they are participating in three of the four interventions identified in the FY 2017 IPPS/LTCH PPS final rule (81 FR 57064 through 57065), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38294 through 38296), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41516 through 41517). Eight CAHs are participating in the telehealth intervention, three CAHs are participating in the skilled nursing facility/nursing facility bed intervention, and two CAHs are participating in the ambulance services intervention. Each CAH is allowed to participate in more than one of the interventions. None of the selected CAHs are participants in the home health intervention, which was the fourth intervention included in the RFA.
In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57064 through 57065), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38294 through 38296), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41516 through 41517), we finalized a policy to address the budget neutrality requirement for the demonstration. As explained in the FY 2019 IPPS/LTCH PPS final rule, we based our selection of CAHs for participation with the goal of maintaining the budget neutrality of the demonstration on its own terms (that is, the demonstration will produce savings from reduced transfers and admissions to other health care providers, thus offsetting any increase in payments resulting from the demonstration). However, because of the small size of this demonstration and uncertainty associated with projected Medicare utilization and costs, we adopted a contingency plan to ensure that the budget neutrality requirement in section 123 of Public Law110-275 is met. If analysis of claims data for Medicare beneficiaries receiving services at each of the participating CAHs, as well as from other data sources, including cost reports for these CAHs, shows that increases in Medicare payments under the demonstration during the 3-year period are not sufficiently offset by reductions elsewhere, we will recoup the additional expenditures attributable to the demonstration through a reduction in payments to all CAHs nationwide. Because of the small scale of the demonstration, we indicated that we did not believe it would be feasible to implement budget neutrality by reducing payments to only the participating CAHs. Therefore, in the event that this demonstration is found to result in aggregate payments in excess of the amount that would have been paid if this demonstration were not implemented, we will comply with the budget neutrality requirement by reducing payments to all CAHs, not just those participating in the demonstration. We stated that we believe it is appropriate to make any payment reductions across all CAHs because the FCHIP demonstration is specifically designed to test innovations that affect delivery of services by the CAH provider category. We explained our belief that the language of the statutory budget neutrality requirement at section 123(g)(1)(B) of Public Law 110-275 permits the agency to implement the budget neutrality provision in this manner. The statutory language merely refers to ensuring that aggregate payments made by the Secretary do not exceed the amount which the Secretary estimates would have been paid if the demonstration project was not implemented, and does not identify the range across which aggregate payments must be held equal.
Based on actuarial analysis using cost report settlements for FYs 2013 and 2014, the demonstration is projected to satisfy the budget neutrality requirement and likely yield a total net savings. As we estimated for the FY 2019 IPPS/LTCH PPS final rule, for this FY 2020 IPPS/LTCH PPS final rule, we estimate that the total impact of the payment recoupment will be no greater than 0.03 percent of CAHs' total Medicare payments within 1 fiscal year (that is, Medicare Part A and Part B). The final budget neutrality estimates for the FCHIP demonstration will be based on the demonstration period, which is August 1, 2016 through July 31, 2019.
The demonstration is projected to impact payments to participating CAHs under both Medicare Part A and Part B. As stated in the FY 2019 IPPS/LTCH PPS final rule, in the event the demonstration is found not to have been budget neutral, any excess costs will be recouped over a period of 3 cost reporting years, beginning in CY 2020. The 3-year period for recoupment will allow for a reasonable timeframe for the payment reduction and to minimize any impact on CAHs' operations. Based on the currently available data and because any reduction to CAH payments in order to recoup excess costs under the demonstration will not begin until CY 2020, this policy will likely have no impact for any national payment system for FY 2020.
We did not receive any public comments on our discussion of the FCHIP demonstration in the FY 2020 IPPS/LTCH PPS proposed rule.
VII. Changes to the Long-Term Care Hospital Prospective Payment System (LTCH PPS) for FY 2020
A. Background of the LTCH PPS
1. Legislative and Regulatory Authority
Section 123 of the Medicare, Medicaid, and SCHIP (State Children's Health Insurance Program) Balanced Budget Refinement Act of 1999 (BBRA) (Pub. L. 106-113), as amended by section 307(b) of the Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 (BIPA) (Pub. L. 106-554), provides for payment for both the operating and capital-related costs of hospital inpatient stays in long-term care hospitals (LTCHs) under Medicare Part A based on prospectively set rates. The Medicare prospective payment system (PPS) for LTCHs applies to hospitals that are described in section 1886(d)(1)(B)(iv) of the Act, effective for cost reporting periods beginning on or after October 1, 2002.
Section 1886(d)(1)(B)(iv)(I) of the Act originally defined an LTCH as a hospital which has an average inpatient length of stay (as determined by the Secretary) of greater than 25 days. Section 1886(d)(1)(B)(iv)(II) of the Act (“subclause II” LTCHs) also provided an alternative definition of LTCHs. However, section 15008 of the 21st Century Cures Act (Pub. L. 114-255) amended section 1886 of the Act to exclude former “subclause II” LTCHs from being paid under the LTCH PPS and created a new category of IPPS-excluded hospitals, which we refer to as “extended neoplastic disease care hospitals”), to be paid as hospitals that were formally classified as “subclause (II)” LTCHs (82 FR 38298).
Section 123 of the BBRA requires the PPS for LTCHs to be a “per discharge” system with a diagnosis-related group (DRG) based patient classification system that reflects the differences in patient resources and costs in LTCHs.
Section 307(b)(1) of the BIPA, among other things, mandates that the Secretary shall examine, and may provide for, adjustments to payments under the LTCH PPS, including adjustments to DRG weights, area wage adjustments, geographic reclassification, outliers, updates, and a disproportionate share adjustment.
In the August 30, 2002 Federal Register, we issued a final rule that implemented the LTCH PPS authorized under the BBRA and BIPA (67 FR 55954). For the initial implementation of the LTCH PPS (FYs 2003 through FY 2007), the system used information from LTCH patient records to classify patients into distinct long-term care diagnosis-related groups (LTC-DRGs) based on clinical characteristics and expected resource needs. Beginning in FY 2008, we adopted the Medicare severity long-term care diagnosis-related groups (MS-LTC-DRGs) as the patient classification system used under the LTCH PPS. Payments are calculated for each MS-LTC-DRG and provisions are made for appropriate payment adjustments. Payment rates under the LTCH PPS are updated annually and published in the Federal Register.
The LTCH PPS replaced the reasonable cost-based payment system under the Tax Equity and Fiscal Responsibility Act of 1982 (TEFRA) (Pub. L. 97-248) for payments for inpatient services provided by an LTCH with a cost reporting period beginning on or after October 1, 2002. (The regulations implementing the TEFRA reasonable cost-based payment provisions are located at 42 CFR part 413.) With the implementation of the PPS for acute care hospitals authorized by the Social Security Amendments of 1983 (Pub. L. 98-21), which added section 1886(d) to the Act, certain hospitals, including LTCHs, were excluded from the PPS for acute care hospitals and were paid their reasonable costs for inpatient services subject to a per discharge limitation or target amount under the TEFRA system. For each cost reporting period, a hospital-specific ceiling on payments was determined by multiplying the hospital's updated target amount by the number of total current year Medicare discharges. (Generally, in this section of the preamble of this proposed rule, when we refer to discharges, we describe Medicare discharges.) The August 30, 2002 final rule further details the payment policy under the TEFRA system (67 FR 55954).
In the August 30, 2002 final rule, we provided for a 5-year transition period from payments under the TEFRA system to payments under the LTCH PPS. During this 5-year transition period, an LTCH's total payment under the PPS was based on an increasing percentage of the Federal rate with a corresponding decrease in the percentage of the LTCH PPS payment that is based on reasonable cost concepts, unless an LTCH made a one-time election to be paid based on 100 percent of the Federal rate. Beginning with LTCHs' cost reporting periods beginning on or after October 1, 2006, total LTCH PPS payments are based on 100 percent of the Federal rate.
In addition, in the August 30, 2002 final rule, we presented an in-depth discussion of the LTCH PPS, including the patient classification system, relative weights, payment rates, additional payments, and the budget neutrality requirements mandated by section 123 of the BBRA. The same final rule that established regulations for the LTCH PPS under 42 CFR part 412, subpart O, also contained LTCH provisions related to covered inpatient services, limitation on charges to beneficiaries, medical review requirements, furnishing of inpatient hospital services directly or under arrangement, and reporting and recordkeeping requirements. We refer readers to the August 30, 2002 final rule for a comprehensive discussion of the research and data that supported the establishment of the LTCH PPS (67 FR 55954).
In the FY 2016 IPPS/LTCH PPS final rule (80 FR 49601 through 49623), we implemented the provisions of the Pathway for Sustainable Growth Rate (SGR) Reform Act of 2013 (Pub. L. 113-67), which mandated the application of the “site neutral” payment rate under the LTCH PPS for discharges that do not meet the statutory criteria for exclusion beginning in FY 2016. For cost reporting periods beginning on or after October 1, 2015, discharges that do not meet certain statutory criteria for exclusion are paid based on the site neutral payment rate. Discharges that do meet the statutory criteria continue to receive payment based on the LTCH PPS standard Federal payment rate. For more information on the statutory requirements of the Pathway for SGR Reform Act of 2013, we refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49601 through 49623) and the FY 2017 IPPS/LTCH PPS final rule (81 FR 57068 through 57075).
In the FY 2018 IPPS/LTCH PPS final rule, we implemented several provisions of the 21st Century Cures Act (“the Cures Act”) (Pub. L. 114-255) that affected the LTCH PPS. (For more information on these provisions, we refer readers to 82 FR 38299.)
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41529), we made conforming changes to our regulations to implement the provisions of section 51005 of the Bipartisan Budget Act of 2018, Public Law 115-123, which extends the transitional blended payment rate for site neutral payment rate cases for an additional 2 years. We refer readers to section VII.C. of the preamble of the FY 2019 IPPS/LTCH PPS final rule for a discussion of our final policy. In addition, in the FY 2019 IPPS/LTCH PPS final rule, we removed the 25-percent threshold policy under 42 CFR 412.538.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19469), we proposed revisions to our regulations to implement the provisions of the Pathway for SGR Reform Act of 2013 (Pub. L. 113-67) that relate to the payment adjustment for discharges from LTCHs that do not maintain the requisite discharge payment percentage and the process by which such LTCHs may have the payment adjustment discontinued. In section VII.C. of the preamble of this final rule, we discuss in detail the proposed revisions to our regulations, provide summations of the public comments we received in response to our proposals, including the Agency's responses, and present the finalized policy to implement the provisions of Public Law 113-67 that relate to the payment adjustment for discharges from LTCHs that do not maintain the requisite discharge payment percentage and the process by which such LTCHs may have the payment adjustment discontinued.
We received several public comments that addressed issues that were outside the scope of the FY 2020 IPPS/LTCH PPS proposed rule. We will keep these comments in mind and may consider them for future rulemaking.
2. Criteria for Classification as an LTCH
a. Classification as an LTCH
Under the regulations at § 412.23(e)(1), to qualify to be paid under the LTCH PPS, a hospital must have a provider agreement with Medicare. Furthermore, § 412.23(e)(2)(i), which implements section 1886(d)(1)(B)(iv) of the Act, requires that a hospital have an average Medicare inpatient length of stay of greater than 25 days to be paid under the LTCH PPS. In accordance with section 1206(a)(3) of the Pathway for SGR Reform Act of 2013 (Pub. L. 113-67), as amended by section 15007 of Public Law 114-255, we amended our regulations to specify that Medicare Advantage plans' and site neutral payment rate discharges are excluded from the calculation of the average length of stay for all LTCHs, for discharges occurring in cost reporting period beginning on or after October 1, 2015.
b. Hospitals Excluded From the LTCH PPS
The following hospitals are paid under special payment provisions, as described in § 412.22(c) and, therefore, are not subject to the LTCH PPS rules:
- Veterans Administration hospitals.
- Hospitals that are reimbursed under State cost control systems approved under 42 CFR part 403.
- Hospitals that are reimbursed in accordance with demonstration projects authorized under section 402(a) of the Social Security Amendments of 1967 (Pub. L. 90-248) (42 U.S.C. 1395b-1), section 222(a) of the Social Security Amendments of 1972 (Pub. L. 92-603) (42 U.S.C. 1395b-1 (note)) (Statewide all-payer systems, subject to the rate-of-increase test at section 1814(b) of the Act), or section 3201 of the Patient Protection and Affordable Care Act (Pub. L. 111-148 (42 U.S.C. 1315a).
- Nonparticipating hospitals furnishing emergency services to Medicare beneficiaries.
3. Limitation on Charges to Beneficiaries
In the August 30, 2002 final rule, we presented an in-depth discussion of beneficiary liability under the LTCH PPS (67 FR 55974 through 55975). This discussion was further clarified in the RY 2005 LTCH PPS final rule (69 FR 25676). In keeping with those discussions, if the Medicare payment to the LTCH is the full LTC-DRG payment amount, consistent with other established hospital prospective payment systems, § 412.507 currently provides that an LTCH may not bill a Medicare beneficiary for more than the deductible and coinsurance amounts as specified under §§ 409.82, 409.83, and 409.87, and for items and services specified under § 489.30(a). However, under the LTCH PPS, Medicare will only pay for services furnished during the days for which the beneficiary has coverage until the short-stay outlier (SSO) threshold is exceeded. If the Medicare payment was for a SSO case (in accordance with § 412.529), and that payment was less than the full LTC-DRG payment amount because the beneficiary had insufficient coverage as a result of the remaining Medicare days, the LTCH also is currently permitted to charge the beneficiary for services delivered on those uncovered days (in accordance with § 412.507). In the FY 2016 IPPS/LTCH PPS final rule (80 FR 49623), we amended our regulations to expressly limit the charges that may be imposed upon beneficiaries whose LTCHs' discharges are paid at the site neutral payment rate under the LTCH PPS. In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57102), we amended the regulations under § 412.507 to clarify our existing policy that blended payments made to an LTCH during its transitional period (that is, an LTCH's payment for discharges occurring in cost reporting periods beginning in FYs 2016 through 2019) are considered to be site neutral payment rate payments.
B. Medicare Severity Long-Term Care Diagnosis-Related Group (MS-LTC-DRG) Classifications and Relative Weights for FY 2020
1. Background
Section 123 of the BBRA required that the Secretary implement a PPS for LTCHs to replace the cost-based payment system under TEFRA. Section 307(b)(1) of the BIPA modified the requirements of section 123 of the BBRA by requiring that the Secretary examine the feasibility and the impact of basing payment under the LTCH PPS on the use of existing (or refined) hospital DRGs that have been modified to account for different resource use of LTCH patients.
When the LTCH PPS was implemented for cost reporting periods beginning on or after October 1, 2002, we adopted the same DRG patient classification system utilized at that time under the IPPS. As a component of the LTCH PPS, we refer to this patient classification system as the “long-term care diagnosis-related groups (LTC-DRGs).” Although the patient classification system used under both the LTCH PPS and the IPPS are the same, the relative weights are different. The established relative weight methodology and data used under the LTCH PPS result in relative weights under the LTCH PPS that reflect the differences in patient resource use of LTCH patients, consistent with section 123(a)(1) of the BBRA (Pub. L. 106-113).
As part of our efforts to better recognize severity of illness among patients, in the FY 2008 IPPS final rule with comment period (72 FR 47130), the MS-DRGs and the Medicare severity long-term care diagnosis-related groups (MS-LTC-DRGs) were adopted under the IPPS and the LTCH PPS, respectively, effective beginning October 1, 2007 (FY 2008). For a full description of the development, implementation, and rationale for the use of the MS-DRGs and MS-LTC-DRGs, we refer readers to the FY 2008 IPPS final rule with comment period (72 FR 47141 through 47175 and 47277 through 47299). (We note that, in that same final rule, we revised the regulations at § 412.503 to specify that for LTCH discharges occurring on or after October 1, 2007, when applying the provisions of 42 CFR part 412, subpart O applicable to LTCHs for policy descriptions and payment calculations, all references to LTC-DRGs would be considered a reference to MS-LTC-DRGs. For the remainder of this section, we present the discussion in terms of the current MS-LTC-DRG patient classification system unless specifically referring to the previous LTC-DRG patient classification system that was in effect before October 1, 2007.)
The MS-DRGs adopted in FY 2008 represent an increase in the number of DRGs by 207 (that is, from 538 to 745) (72 FR 47171). The MS-DRG classifications are updated annually. There are currently 761 MS-DRG groupings. For FY 2020, there will be 761 MS-DRG groupings based on the changes, as discussed in section II.F. of the preamble of this FY 2020 IPPS/LTCH PPS final rule. Consistent with section 123 of the BBRA, as amended by section 307(b)(1) of the BIPA, and § 412.515 of the regulations, we use information derived from LTCH PPS patient records to classify LTCH discharges into distinct MS-LTC-DRGs based on clinical characteristics and estimated resource needs. Then,we assign an appropriate weight to the MS-LTC-DRGs to account for the difference in resource use by patients exhibiting the case complexity and multiple medical problems characteristic of LTCHs.
In this section of the final rule, we provide a general summary of our existing methodology for determining the FY 2020 MS-LTC-DRG relative weights under the LTCH PPS.
As we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19460), in general, for FY 2020, we are continuing to use our existing methodology to determine the MS-LTC-DRG relative weights (as discussed in greater detail in section VII.B.3. of the of this final rule). As we established when we implemented the dual rate LTCH PPS payment structure codified under § 412.522, which began in FY 2016, as we proposed, the annual recalibration of the MS-LTC-DRG relative weights are determined: (1) Using only data from available LTCH PPS claims that would have qualified for payment under the new LTCH PPS standard Federal payment rate if that rate had been in effect at the time of discharge when claims data from time periods before the dual rate LTCH PPS payment structure applies are used to calculate the relative weights; and (2) using only data from available LTCH PPS claims that qualify for payment under the new LTCH PPS standard Federal payment rate when claims data from time periods after the dual rate LTCH PPS payment structure applies are used to calculate the relative weights (80 FR 49624). That is, under our current methodology, our MS-LTC-DRG relative weight calculations do not use data from cases paid at the site neutral payment rate under § 412.522(c)(1) or data from cases that would have been paid at the site neutral payment rate if the dual rate LTCH PPS payment structure had been in effect at the time of that discharge. For the remainder of this discussion, we use the phrase “applicable LTCH cases” or “applicable LTCH data” when referring to the resulting claims data set used to calculate the relative weights (as described later in greater detail in section VII.B.3.c. of the preamble of this final rule). In addition, in this FY 2020 IPPS/LTCH PPS final rule, for FY 2020, as we proposed, we are continuing to exclude the data from all-inclusive rate providers and LTCHs paid in accordance with demonstration projects, as well as any Medicare Advantage claims from the MS-LTC-DRG relative weight calculations for the reasons discussed in section VII.B.3.c. of the preamble of this final rule.
Furthermore, for FY 2020, in using data from applicable LTCH cases to establish MS-LTC-DRG relative weights, as we proposed, we are continuing to establish low-volume MS-LTC-DRGs (that is, MS-LTC-DRGs with less than 25 cases) using our quintile methodology in determining the MS-LTC-DRG relative weights because LTCHs do not typically treat the full range of diagnoses as do acute care hospitals. Therefore, for purposes of determining the relative weights for the large number of low-volume MS-LTC-DRGs, we grouped all of the low-volume MS-LTC-DRGs into five quintiles based on average charges per discharge. Then, under our existing methodology, we accounted for adjustments made to LTCH PPS standard Federal payments for short-stay outlier (SSO) cases (that is, cases where the covered length of stay at the LTCH is less than or equal to five-sixths of the geometric average length of stay for the MS-LTC-DRG), and we made adjustments to account for nonmonotonically increasing weights, when necessary. The methodology is premised on more severe cases under the MS-LTC-DRG system requiring greater expenditure of medical care resources and higher average charges such that, in the severity levels within a base MS-LTC-DRG, the relative weights should increase monotonically with severity from the lowest to highest severity level. (We discuss each of these components of our MS-LTC-DRG relative weight methodology in greater detail in section VII.B.3.g. of the preamble of this final rule.)
2. Patient Classifications into MS-LTC-DRGs
a. Background
The MS-DRGs (used under the IPPS) and the MS-LTC-DRGs (used under the LTCH PPS) are based on the CMS DRG structure. As noted previously in this section, we refer to the DRGs under the LTCH PPS as MS-LTC-DRGs although they are structurally identical to the MS-DRGs used under the IPPS.
The MS-DRGs are organized into 25 major diagnostic categories (MDCs), most of which are based on a particular organ system of the body; the remainder involve multiple organ systems (such as MDC 22, Burns). Within most MDCs, cases are then divided into surgical DRGs and medical DRGs. Surgical DRGs are assigned based on a surgical hierarchy that orders operating room (O.R.) procedures or groups of O.R. procedures by resource intensity. The GROUPER software program does not recognize all ICD-10-PCS procedure codes as procedures affecting DRG assignment. That is, procedures that are not surgical (for example, EKGs), or minor surgical procedures (for example, a biopsy of skin and subcutaneous tissue (procedure code 0JBH3ZX)) do not affect the MS-LTC-DRG assignment based on their presence on the claim.
Generally, under the LTCH PPS, a Medicare payment is made at a predetermined specific rate for each discharge that varies based on the MS-LTC-DRG to which a beneficiary's discharge is assigned. Cases are classified into MS-LTC-DRGs for payment based on the following six data elements:
- Principal diagnosis.
- Additional or secondary diagnoses.
- Surgical procedures.
- Age.
- Sex.
- Discharge status of the patient.
Currently, for claims submitted using version ASC X12 5010 format, up to 25 diagnosis codes and 25 procedure codes are considered for an MS-DRG assignment. This includes one principal diagnosis and up to 24 secondary diagnoses for severity of illness determinations. (For additional information on the processing of up to 25 diagnosis codes and 25 procedure codes on hospital inpatient claims, we refer readers to section II.G.11.c. of the preamble of the FY 2011 IPPS/LTCH PPS final rule (75 FR 50127).)
Under the HIPAA transactions and code sets regulations at 45 CFR parts 160 and 162, covered entities must comply with the adopted transaction standards and operating rules specified in Subparts I through S of Part 162. Among other requirements, on or after January 1, 2012, covered entities were required to use the ASC X12 Standards for Electronic Data Interchange Technical Report Type 3—Health Care Claim: Institutional (837), May 2006, ASC X12N/005010X223, and Type 1 Errata to Health Care Claim: Institutional (837) ASC X12 Standards for Electronic Data Interchange Technical Report Type 3, October 2007, ASC X12N/005010X233A1 for the health care claims or equivalent encounter information transaction (45 CFR 162.1102(c)).
HIPAA requires covered entities to use the applicable medical data code set requirements when conducting HIPAA transactions (45 CFR 162.1000). Currently, upon the discharge of the patient, the LTCH must assign appropriate diagnosis and procedure codes from the most current version of the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) for diagnosis coding and the International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS) for inpatient hospital procedure coding, both of which were required to be implemented October 1, 2015 (45 CFR 162.1002(c)(2) and (3)). For additional information on the implementation of the ICD-10 coding system, we refer readers to section II.F.1. of the FY 2017 IPPS/LTCH PPS final rule (81 FR 56787 through 56790) and section II.F.1. of the preamble of this final rule. Additional coding instructions and examples are published in the AHA's Coding Clinic for ICD-10-CM/PCS.
To create the MS-DRGs (and by extension, the MS-LTC-DRGs), base DRGs were subdivided according to the presence of specific secondary diagnoses designated as complications or comorbidities (CCs) into one, two, or three levels of severity, depending on the impact of the CCs on resources used for those cases. Specifically, there are sets of MS-DRGs that are split into 2 or 3 subgroups based on the presence or absence of a CC or a major complication or comorbidity (MCC). We refer readers to section II.D. of the FY 2008 IPPS final rule with comment period for a detailed discussion about the creation of MS-DRGs based on severity of illness levels (72 FR 47141 through 47175).
MACs enter the clinical and demographic information submitted by LTCHs into their claims processing systems and subject this information to a series of automated screening processes called the Medicare Code Editor (MCE). These screens are designed to identify cases that require further review before assignment into a MS-LTC-DRG can be made. During this process, certain cases are selected for further explanation (74 FR 43949).
After screening through the MCE, each claim is classified into the appropriate MS-LTC-DRG by the Medicare LTCH GROUPER software on the basis of diagnosis and procedure codes and other demographic information (age, sex, and discharge status). The GROUPER software used under the LTCH PPS is the same GROUPER software program used under the IPPS. Following the MS-LTC-DRG assignment, the MAC determines the prospective payment amount by using the Medicare PRICER program, which accounts for hospital-specific adjustments. Under the LTCH PPS, we provide an opportunity for LTCHs to review the MS-LTC-DRG assignments made by the MAC and to submit additional information within a specified timeframe as provided in § 412.513(c).
The GROUPER software is used both to classify past cases to measure relative hospital resource consumption to establish the MS-LTC-DRG relative weights and to classify current cases for purposes of determining payment. The records for all Medicare hospital inpatient discharges are maintained in the MedPAR file. The data in this file are used to evaluate possible MS-DRG and MS-LTC-DRG classification changes and to recalibrate the MS-DRG and MS-LTC-DRG relative weights during our annual update under both the IPPS (§ 412.60(e)) and the LTCH PPS (§ 412.517), respectively.
b. Changes to the MS-LTC-DRGs for FY 2020
As specified by our regulations at § 412.517(a), which require that the MS-LTC-DRG classifications and relative weights be updated annually, and consistent with our historical practice of using the same patient classification system under the LTCH PPS as is used under the IPPS, in this FY 2020 IPPS/LTCH PPS final rule, as we proposed, we updated the MS-LTC-DRG classifications effective October 1, 2019 through September 30, 2020 (FY 2020), consistent with the changes to specific MS-DRG classifications presented in section II.F. of the preamble of this final rule. Accordingly, the MS-LTC-DRGs for FY 2020 presented in this final rule are the same as the MS-DRGs that are being used under the IPPS for FY 2020. In addition, because the MS-LTC-DRGs for FY 2020 are the same as the MS-DRGs for FY 2020, the other changes that affect MS-DRG (and by extension MS-LTC-DRG) assignments under GROUPER Version 37 as discussed in section II.F. of the preamble of this final rule, including the changes to the MCE software and the ICD-10-CM/PCS coding system, also are applicable under the LTCH PPS for FY 2020.
3. Development of the FY 2020 MS-LTC-DRG Relative Weights
a. General Overview of the Development of the MS-LTC-DRG Relative Weights
One of the primary goals for the implementation of the LTCH PPS is to pay each LTCH an appropriate amount for the efficient delivery of medical care to Medicare patients. The system must be able to account adequately for each LTCH's case-mix in order to ensure both fair distribution of Medicare payments and access to adequate care for those Medicare patients whose care is more costly (67 FR 55984). To accomplish these goals, we have annually adjusted the LTCH PPS standard Federal prospective payment rate by the applicable relative weight in determining payment to LTCHs for each case. In order to make these annual adjustments under the dual rate LTCH PPS payment structure, beginning with FY 2016, we recalibrate the MS-LTC-DRG relative weighting factors annually using data from applicable LTCH cases (80 FR 49614 through 49617). Under this policy, the resulting MS-LTC-DRG relative weights would continue to be used to adjust the LTCH PPS standard Federal payment rate when calculating the payment for LTCH PPS standard Federal payment rate cases.
The established methodology to develop the MS-LTC-DRG relative weights is generally consistent with the methodology established when the LTCH PPS was implemented in the August 30, 2002 LTCH PPS final rule (67 FR 55989 through 55991). However, there have been some modifications of our historical procedures for assigning relative weights in cases of zero volume and/or nonmonotonicity resulting from the adoption of the MS-LTC-DRGs, along with the change made in conjunction with the implementation of the dual rate LTCH PPS payment structure beginning in FY 2016 to use LTCH claims data from only LTCH PPS standard Federal payment rate cases (or LTCH PPS cases that would have qualified for payment under the LTCH PPS standard Federal payment rate if the dual rate LTCH PPS payment structure had been in effect at the time of the discharge). (For details on the modifications to our historical procedures for assigning relative weights in cases of zero volume and/or nonmonotonicity, we refer readers to the FY 2008 IPPS final rule with comment period (72 FR 47289 through 47295) and the FY 2009 IPPS final rule (73 FR 48542 through 48550).) For details on the change in our historical methodology to use LTCH claims data only from LTCH PPS standard Federal payment rate cases (or cases that would have qualified for such payment had the LTCH PPS dual payment rate structure been in effect at the time) to determine the MS-LTC-DRG relative weights, we refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49614 through 49617). Under the LTCH PPS, relative weights for each MS-LTC-DRG are a primary element used to account for the variations in cost per discharge and resource utilization among the payment groups (§ 412.515). To ensure that Medicare patients classified to each MS-LTC-DRG have access to an appropriate level of services and to encourage efficiency, we calculate a relative weight for each MS-LTC-DRG that represents the resources needed by an average inpatient LTCH case in that MS-LTC-DRG. For example, cases in an MS-LTC-DRG with a relative weight of 2 would, on average, cost twice as much to treat as cases in an MS-LTC-DRG with a relative weight of 1.
b. Development of the MS-LTC-DRG Relative Weights for FY 2020
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41521 through 41529), we presented our policies for the development of the MS-LTC-DRG relative weights for FY 2019.
In this FY 2020 IPPS/LTCH PPS final rule, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19462), we are continuing to use our current methodology to determine the MS-LTC-DRG relative weights for FY 2020, including the continued application of established policies related to: The hospital-specific relative value methodology, the treatment of severity levels in the MS-LTC-DRGs, low-volume and no-volume MS-LTC-DRGs, adjustments for nonmonotonicity, the steps for calculating the MS-LTC-DRG relative weights with a budget neutrality factor, and only using data from applicable LTCH cases (which includes our policy of only using cases that would meet the criteria for exclusion from the site neutral payment rate (or, for discharges occurring prior to the implementation of the dual rate LTCH PPS payment structure, would have met the criteria for exclusion had those criteria been in effect at the time of the discharge)).
In this section, we present our application of our existing methodology for determining the MS-LTC-DRG relative weights for FY 2020, and we discuss the effects of our policies concerning the data used to determine the FY 2020 MS-LTC-DRG relative weights on the various components of our existing methodology in the discussion that follows.
As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41522), we now generally provide the low-volume quintiles and no-volume crosswalk data previously published in Tables 13A and 13B for each annual proposed and final rule as one of our supplemental IPPS/LTCH PPS related data files that are made available for public use via the internet on the CMS website for the respective rule and fiscal year (that is, FY 2019 and subsequent fiscal years) at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html to streamline the information made available to the public that is used in the annual development of IPPS Table 11 and to make it easier for the public to navigate and find the relevant data and information used for the development of proposed and final payment rates or factors for the applicable payment year while continuing to furnish the same information the tables provided in previous fiscal years. We refer readers to the CMS website for the low-volume quintiles and no-volume crosswalk data previously furnished via Tables 13A and 13B.
c. Data
For the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19462), consistent with our proposals regarding the calculation of the proposed MS-LTC-DRG relative weights for FY 2020, we obtained total charges from FY 2018 Medicare LTCH claims data from the December 2018 update of the FY 2018 MedPAR file, which was the best available data at that time, and we proposed to use Version 37 of the GROUPER to classify LTCH cases. Consistent with our historical practice, we proposed that if more recent data become available, we would use those data and the finalized Version 37 of the GROUPER in establishing the FY 2020 MS-LTC-DRG relative weights in the final rule. Accordingly, for this final rule, we are establishing the FY 2020 MS-LTC-DRG relative weights based on updated FY 2018 Medicare LTCH claims data from the March 2019 update of the FY 2018 MedPAR file, which is the best available data at the time of development of this final rule, and used the finalized Version 37 of the GROUPER to classify LTCH cases.
To calculate the FY 2020 MS-LTC-DRG relative weights under the dual rate LTCH PPS payment structure, as we proposed, we continued to use applicable LTCH data, which includes our policy of only using cases that meet the criteria for exclusion from the site neutral payment rate (or would have met the criteria had they been in effect at the time of the discharge) (80 FR 49624). Specifically, we began by first evaluating the LTCH claims data in the March 2019 update of the FY 2018 MedPAR file to determine which LTCH cases would meet the criteria for exclusion from the site neutral payment rate under § 412.522(b) had the dual rate LTCH PPS payment structure applied to those cases at the time of discharge. We identified the FY 2018 LTCH cases that were not assigned to MS-LTC-DRGs 876, 880, 881, 882, 883, 884, 885, 886, 887, 894, 895, 896, 897, 945 and 946, which identify LTCH cases that do not have a principal diagnosis relating to a psychiatric diagnosis or to rehabilitation; and that either—
- The admission to the LTCH was “immediately preceded” by discharge from a subsection (d) hospital and the immediately preceding stay in that subsection (d) hospital included at least 3 days in an ICU, as we define under the ICU criterion; or
- The admission to the LTCH was “immediately preceded” by discharge from a subsection (d) hospital and the claim for the LTCH discharge includes the applicable procedure code that indicates at least 96 hours of ventilator services were provided during the LTCH stay, as we define under the ventilator criterion. Claims data from the FY 2018 MedPAR file that reported ICD-10-PCS procedure code 5A1955Z were used to identify cases involving at least 96 hours of ventilator services in accordance with the ventilator criterion. We note that, for purposes of developing the FY 2020 MS-LTC-DRG relative weights using our current methodology, we did not make any exceptions regarding the identification of cases that would have been excluded from the site neutral payment rate under the statutory provisions that provided for temporary exception from the site neutral payment rate under the LTCH PPS for certain severe wound care discharges from certain LTCHs or for certain spinal cord specialty hospitals provided by sections 15009 and 15010 of Public Law 114-255, respectively, had our implementation of that law and the dual rate LTCH PPS payment structure been in effect at the time of the discharge. At this time, it is uncertain how many LTCHs and how many cases in the claims data we are using for this final rule meet the criteria to be excluded from the site neutral payment rate under those exceptions (or would have met the criteria for exclusion had the dual rate LTCH PPS payment structure been in effect at the time of the discharge). Therefore, for the remainder of this section, when we refer to LTCH claims only from cases that meet the criteria for exclusion from the site neutral payment rate (or would have met the criteria had the applicable statutes been in effect at the time of the discharge), such data do not include any discharges that would have been paid based on the LTCH PPS standard Federal payment rate under the provisions of sections 15009 and 15010 of Public Law 114-255, had the exception been in effect at the time of the discharge.
Furthermore, consistent with our historical methodology, we excluded any claims in the resulting data set that were submitted by LTCHs that were all-inclusive rate providers and LTCHs that are paid in accordance with demonstration projects authorized under section 402(a) of Public Law 90-248 or section 222(a) of Public Law 92-603. In addition, consistent with our historical practice and our policies, we excluded any Medicare Advantage (Part C) claims in the resulting data. Such claims were identified based on the presence of a GHO Paid indicator value of “1” in the MedPAR files. The claims that remained after these three trims (that is, the applicable LTCH data) were then used to calculate the MS-LTC-DRG relative weights for FY 2020.
In summary, in general, we identified the claims data used in the development of the FY 2020 MS-LTC-DRG relative weights in this final rule, as we proposed, by trimming claims data that were paid the site neutral payment rate or would have been paid the site neutral payment rate had the dual payment rate structure been in effect. As described in the proposed rule, due to data limitations, we did not except from that trimmed data any discharges which were or would have been excluded from the site neutral payment rate under the temporary exception for certain severe wound care discharges from certain LTCHs and under the temporary exception for certain spinal cord specialty hospitals). Finally, we trimmed the claims data of all-inclusive rate providers reported in the March 2019 update of the FY 2018 MedPAR file and any Medicare Advantage claims data. There were no data from any LTCHs that are paid in accordance with a demonstration project reported in the March 2019 update of the FY 2018 MedPAR file, but, had there been any, we would have trimmed the claims data from those LTCHs as well, in accordance with our established policy. As we proposed, we used the remaining data (that is, the applicable LTCH data) to calculate the relative weights for FY 2020.
d. Hospital-Specific Relative Value (HSRV) Methodology
By nature, LTCHs often specialize in certain areas, such as ventilator-dependent patients. Some case types (MS-LTC-DRGs) may be treated, to a large extent, in hospitals that have, from a perspective of charges, relatively high (or low) charges. This nonrandom distribution of cases with relatively high (or low) charges in specific MS-LTC-DRGs has the potential to inappropriately distort the measure of average charges. To account for the fact that cases may not be randomly distributed across LTCHs, consistent with the methodology we have used since the implementation of the LTCH PPS, in this FY 2020 IPPS/LTCH PPS final rule, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19463), we continued to use a hospital-specific relative value (HSRV) methodology to calculate the MS-LTC-DRG relative weights for FY 2020. We believe that this method removes this hospital-specific source of bias in measuring LTCH average charges (67 FR 55985). Specifically, under this methodology, we reduced the impact of the variation in charges across providers on any particular MS-LTC-DRG relative weight by converting each LTCH's charge for an applicable LTCH case to a relative value based on that LTCH's average charge for such cases.
Under the HSRV methodology, we standardize charges for each LTCH by converting its charges for each applicable LTCH case to hospital-specific relative charge values and then adjusting those values for the LTCH's case-mix. The adjustment for case-mix is needed to rescale the hospital-specific relative charge values (which, by definition, average 1.0 for each LTCH). The average relative weight for an LTCH is its case-mix; therefore, it is reasonable to scale each LTCH's average relative charge value by its case-mix. In this way, each LTCH's relative charge value is adjusted by its case-mix to an average that reflects the complexity of the applicable LTCH cases it treats relative to the complexity of the applicable LTCH cases treated by all other LTCHs (the average LTCH PPS case-mix of all applicable LTCH cases across all LTCHs).
In accordance with our established methodology, for FY 2020, as we proposed, we continued to standardize charges for each applicable LTCH case by first dividing the adjusted charge for the case (adjusted for SSOs under § 412.529 as described in section VII.B.3.g. (Step 3) of the preamble of this final rule) by the average adjusted charge for all applicable LTCH cases at the LTCH in which the case was treated. SSO cases are cases with a length of stay that is less than or equal to five-sixths the average length of stay of the MS-LTC-DRG (§ 412.529 and § 412.503). The average adjusted charge reflects the average intensity of the health care services delivered by a particular LTCH and the average cost level of that LTCH. The resulting ratio was multiplied by that LTCH's case-mix index to determine the standardized charge for the case.
Multiplying the resulting ratio by the LTCH's case-mix index accounts for the fact that the same relative charges are given greater weight at an LTCH with higher average costs than they would at an LTCH with low average costs, which is needed to adjust each LTCH's relative charge value to reflect its case-mix relative to the average case-mix for all LTCHs. By standardizing charges in this manner, we count charges for a Medicare patient at an LTCH with high average charges as less resource intensive than they would be at an LTCH with low average charges. For example, a $10,000 charge for a case at an LTCH with an average adjusted charge of $17,500 reflects a higher level of relative resource use than a $10,000 charge for a case at an LTCH with the same case-mix, but an average adjusted charge of $35,000. We believe that the adjusted charge of an individual case more accurately reflects actual resource use for an individual LTCH because the variation in charges due to systematic differences in the markup of charges among LTCHs is taken into account.
e. Treatment of Severity Levels in Developing the MS-LTC-DRG Relative Weights
For purposes of determining the MS-LTC-DRG relative weights, under our historical methodology, there are three different categories of MS-DRGs based on volume of cases within specific MS-LTC-DRGs: (1) MS-LTC-DRGs with at least 25 applicable LTCH cases in the data used to calculate the relative weight, which are each assigned a unique relative weight; (2) low-volume MS-LTC-DRGs (that is, MS-LTC-DRGs that contain between 1 and 24 applicable LTCH cases that are grouped into quintiles (as described later in this section of the final rule) and assigned the relative weight of the quintile); and (3) no-volume MS-LTC-DRGs that are cross-walked to other MS-LTC-DRGs based on the clinical similarities and assigned the relative weight of the cross-walked MS-LTC-DRG (as described in greater detail in this final rule). For FY 2020, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19463), we are continuing to use applicable LTCH cases to establish the same volume-based categories to calculate the FY 2020 MS-LTC-DRG relative weights.
In determining the FY 2020 MS-LTC-DRG relative weights, when necessary, as is our longstanding practice, as we proposed, we made adjustments to account for nonmonotonicity, as discussed in greater detail later in Step 6 of section VII.B.3.g. of the preamble of this final rule. We refer readers to the discussion in the FY 2010 IPPS/RY 2010 LTCH PPS final rule for our rationale for including an adjustment for nonmonotonicity (74 FR 43953 through 43954).
Comment: Some commenters objected to some of the proposed changes in the severity level designations for certain ICD-10-CM diagnosis codes based on our comprehensive CC/MCC analysis.
Response: As discussed more fully in section II.F. of the preamble of this final rule, in general we are not finalizing the proposed changes to the severity levels for certain ICD-10-CM diagnosis codes based on our comprehensive CC/MCC analysis in order to allow additional opportunity for the public to provide further feedback given the broad scope and impact of those proposed changes. These comments are included in the summary of comments presented in section II.F. of the preamble of this final rule for more information.
f. Low-Volume MS-LTC-DRGs
In order to account for MS-LTC-DRGs with low-volume (that is, with fewer than 25 applicable LTCH cases), consistent with our existing methodology, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19464), we are continuing to employ the quintile methodology for low-volume MS-LTC-DRGs, such that we grouped the “low-volume MS-LTC-DRGs” (that is, MS-LTC-DRGs that contain between 1 and 24 applicable LTCH cases into one of five categories (quintiles) based on average charges (67 FR 55984 through 55995; 72 FR 47283 through 47288; and 81 FR 25148).) In cases where the initial assignment of a low-volume MS-LTC-DRG to a quintile results in nonmonotonicity within a base-DRG, as we proposed, we made adjustments to the resulting low-volume MS-LTC-DRGs to preserve monotonicity, as discussed in detail in section VII.B.3.g. (Step 6) of the preamble of this final rule.
In this final rule, based on the best available data (that is, the March 2019 update of the FY 2018 MedPAR files), we identified 259 MS-LTC-DRGs that contained between 1 and 24 applicable LTCH cases. This list of MS-LTC-DRGs was then divided into 1 of the 5 low-volume quintiles, each containing at least 51 MS-LTC-DRGs (259/5 = 51 with a remainder of 4). We assigned the low-volume MS-LTC-DRGs to specific low-volume quintiles by sorting the low-volume MS-LTC-DRGs in ascending order by average charge in accordance with our established methodology. Based on the data available for this final rule, the number of MS-LTC-DRGs with less than 25 applicable LTCH cases was not evenly divisible by 5 and, therefore, as we proposed, we employed our historical methodology for determining which of the low-volume quintiles would contain the additional low-volume MS-LTC-DRG. Specifically for this final rule, after organizing the MS-LTC-DRGs by ascending order by average charge, we assigned the first 51 (1st through 51st) of low-volume MS-LTC-DRGs (with the lowest average charge) into Quintile 1. Because the average charge of the 52nd low-volume MS-LTC-DRG in the sorted list was closer to the average charge of the 53rd low-volume MS-LTC-DRG (assigned to Quintile 1) than to the average charge of the 51st low-volume MS-LTC-DRG (assigned to Quintile 2), we assigned it to Quintile 2 (such that Quintile 1 contains 51 low-volume MS-LTC-DRGs before any adjustments for nonmonotonicity, as discussed in this final rule). The 52 MS-LTC-DRGs with the highest average charge were assigned into Quintile 5. This resulted in 4 of the 5 low-volume quintiles containing 52 MS-LTC-DRGs (Quintiles 2 through 5) and 1 low-volume quintile containing 51 MS-LTC-DRGs (Quintile 1). As discussed earlier, for this final rule, we are providing the list of the composition of the low-volume quintiles for low-volume MS-LTC-DRGs for FY 2020 in a supplemental data file for public use posted via the internet on the CMS website for this final rule at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html in order to streamline the information made available to the public that is used in the annual development of Table 11.
In order to determine the FY 2020 relative weights for the low-volume MS-LTC-DRGs, consistent with our historical practice, as we proposed, we used the five low-volume quintiles described previously. We determined a relative weight and (geometric) average length of stay for each of the five low-volume quintiles using the methodology described in section VII.B.3.g. of the preamble of this final rule. We assigned the same relative weight and average length of stay to each of the low-volume MS-LTC-DRGs that make up an individual low-volume quintile. We note that, as this system is dynamic, it is possible that the number and specific type of MS-LTC-DRGs with a low-volume of applicable LTCH cases will vary in the future. Furthermore, we note that we continue to monitor the volume (that is, the number of applicable LTCH cases) in the low-volume quintiles to ensure that our quintile assignments used in determining the MS-LTC-DRG relative weights result in appropriate payment for LTCH cases grouped to low-volume MS-LTC-DRGs and do not result in an unintended financial incentive for LTCHs to inappropriately admit these types of cases.
Comment: A commenter objected to the number of low-volume MS-LTC-DRGs. The commenter expressed concern that these low-volume MS-LTC-DRGs may not have relative weights which accurately reflect the resource use for the cases.
Response: While we appreciate the commenter's concern about the number of low-volume MS-LTC-DRGs, we believe our existing methodology for assigning relative weights to low-volume DRGs is appropriate. The commenter provided no alternative to the existing methodology nor any argument which would suggest that our current methodology, which was adopted beginning with the initial implementation of the LTCH PPS for FY 2003, is somehow inappropriate. Additionally, the use of quintiles in assigning weights to low-volume DRGs does account for differences in resource use among these DRGs, at least in so far as the resource use is reflected in the data. As such, we are finalizing the methodology for establishing relative weights for low-volume MS-LTC-DRGs as proposed.
g. Steps for Determining the FY 2020 MS-LTC-DRG Relative Weights
In this final rule, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19464), we are continuing to use our current methodology to determine the FY 2020 MS-LTC-DRG relative weights.
In summary, to determine the FY 2020 MS-LTC-DRG relative weights, as we proposed, we grouped applicable LTCH cases to the appropriate MS-LTC-DRG, while taking into account the low-volume quintiles (as previously described) and cross-walked no-volume MS-LTC-DRGs (as described later in this section). After establishing the appropriate MS-LTC-DRG (or low-volume quintile), as we proposed, we calculated the FY 2020 relative weights by first removing cases with a length of stay of 7 days or less and statistical outliers (Steps 1 and 2 in this section). Next, as we proposed, we adjusted the number of applicable LTCH cases in each MS-LTC-DRG (or low-volume quintile) for the effect of SSO cases (Step 3 in this section). After removing applicable LTCH cases with a length of stay of 7 days or less (Step 1 in this section) and statistical outliers (Step 2 in this section), which are the SSO-adjusted applicable LTCH cases and corresponding charges (Step 3 in this section), as we proposed, we calculated “relative adjusted weights” for each MS-LTC-DRG (or low-volume quintile) using the HSRV method.
Step 1—Remove cases with a length of stay of 7 days or less.
The first step in our calculation of the FY 2020 MS-LTC-DRG relative weights is to remove cases with a length of stay of 7 days or less. The MS-LTC-DRG relative weights reflect the average of resources used on representative cases of a specific type. Generally, cases with a length of stay of 7 days or less do not belong in an LTCH because these stays do not fully receive or benefit from treatment that is typical in an LTCH stay, and full resources are often not used in the earlier stages of admission to an LTCH. If we were to include stays of 7 days or less in the computation of the FY 2020 MS-LTC-DRG relative weights, the value of many relative weights would decrease and, therefore, payments would decrease to a level that may no longer be appropriate. We do not believe that it would be appropriate to compromise the integrity of the payment determination for those LTCH cases that actually benefit from and receive a full course of treatment at an LTCH by including data from these very short stays. Therefore, consistent with our existing relative weight methodology, in determining the FY 2020 MS-LTC-DRG relative weights, as we proposed, we removed LTCH cases with a length of stay of 7 days or less from applicable LTCH cases. (For additional information on what is removed in this step of the relative weight methodology, we refer readers to 67 FR 55989 and 74 FR 43959.)
Step 2—Remove statistical outliers.
The next step in our calculation of the FY 2020 MS-LTC-DRG relative weights is to remove statistical outlier cases from the LTCH cases with a length of stay of at least 8 days. Consistent with our existing relative weight methodology, as we proposed, we continued to define statistical outliers as cases that are outside of 3.0 standard deviations from the mean of the log distribution of both charges per case and the charges per day for each MS-LTC-DRG. These statistical outliers were removed prior to calculating the relative weights because we believe that they may represent aberrations in the data that distort the measure of average resource use. Including those LTCH cases in the calculation of the relative weights could result in an inaccurate relative weight that does not truly reflect relative resource use among those MS-LTC-DRGs. (For additional information on what is removed in this step of the relative weight methodology, we refer readers to 67 FR 55989 and 74 FR 43959.) After removing cases with a length of stay of 7 days or less and statistical outliers, we were left with applicable LTCH cases that have a length of stay greater than or equal to 8 days. In this final rule, we refer to these cases as “trimmed applicable LTCH cases.”
Step 3—Adjust charges for the effects of SSOs.
As the next step in the final calculation of the FY 2020 MS-LTC-DRG relative weights, consistent with our historical approach, as we proposed, we adjusted each LTCH's charges per discharge for those remaining cases (that is, trimmed applicable LTCH cases) for the effects of SSOs (as defined in § 412.529(a) in conjunction with § 412.503). Specifically, as we proposed, we made this adjustment by counting an SSO case as a fraction of a discharge based on the ratio of the length of stay of the case to the average length of stay for the MS-LTC-DRG for non-SSO cases. This had the effect of proportionately reducing the impact of the lower charges for the SSO cases in calculating the average charge for the MS-LTC-DRG. This process produced the same result as if the actual charges per discharge of an SSO case were adjusted to what they would have been had the patient's length of stay been equal to the average length of stay of the MS-LTC-DRG.
Counting SSO cases as full LTCH cases with no adjustment in determining the FY 2020 MS-LTC-DRG relative weights would lower the FY 2020 MS-LTC-DRG relative weight for affected MS-LTC-DRGs because the relatively lower charges of the SSO cases would bring down the average charge for all cases within a MS-LTC-DRG. This would result in an “underpayment” for non-SSO cases and an “overpayment” for SSO cases. Therefore, as we proposed, we continued to adjust for SSO cases under § 412.529 in this manner because it would result in more appropriate payments for all LTCH PPS standard Federal payment rate cases. (For additional information on this step of the relative weight methodology, we refer readers to 67 FR 55989 and 74 FR 43959.)
Step 4—Calculate the FY 2020 MS-LTC-DRG relative weights on an iterative basis.
Consistent with our historical relative weight methodology, as we proposed, we calculated the FY 2020 MS-LTC-DRG relative weights using the HSRV methodology, which is an iterative process. First, for each SSO-adjusted trimmed applicable LTCH case, we calculated a hospital-specific relative charge value by dividing the charge per discharge after adjusting for SSOs of the LTCH case (from Step 3) by the average charge per SSO-adjusted discharge for the LTCH in which the case occurred. The resulting ratio was then multiplied by the LTCH's case-mix index to produce an adjusted hospital-specific relative charge value for the case. We used an initial case-mix index value of 1.0 for each LTCH.
For each MS-LTC-DRG, we calculated the FY 2020 relative weight by dividing the SSO-adjusted average of the hospital-specific relative charge values for applicable LTCH cases for the MS-LTC-DRG (that is, the sum of the hospital-specific relative charge value from above divided by the sum of equivalent cases from Step 3 for each MS-LTC-DRG) by the overall SSO-adjusted average hospital-specific relative charge value across all applicable LTCH cases for all LTCHs (that is, the sum of the hospital-specific relative charge value from above divided by the sum of equivalent applicable LTCH cases from Step 3 for each MS-LTC-DRG). Using these recalculated MS-LTC-DRG relative weights, each LTCH's average relative weight for all of its SSO-adjusted trimmed applicable LTCH cases (that is, its case-mix) was calculated by dividing the sum of all the LTCH's MS-LTC-DRG relative weights by its total number of SSO-adjusted trimmed applicable LTCH cases. The LTCHs' hospital-specific relative charge values (from previous) were then multiplied by the hospital-specific case-mix indexes. The hospital-specific case-mix adjusted relative charge values were then used to calculate a new set of MS-LTC-DRG relative weights across all LTCHs. This iterative process continued until there was convergence between the relative weights produced at adjacent steps, for example, when the maximum difference was less than 0.0001.
Step 5—Determine a FY 2020 relative weight for MS-LTC-DRGs with no applicable LTCH cases.
Using the trimmed applicable LTCH cases, consistent with our historical methodology, we identified the MS-LTC-DRGs for which there were no claims in the March 2019 update of the FY 2018 MedPAR file and, therefore, for which no charge data was available for these MS-LTC-DRGs. Because patients with a number of the diagnoses under these MS-LTC-DRGs may be treated at LTCHs, consistent with our historical methodology, we generally assign a relative weight to each of the no-volume MS-LTC-DRGs based on clinical similarity and relative costliness (with the exception of “transplant” MS-LTC-DRGs, “error” MS-LTC-DRGs, and MS-LTC-DRGs that indicate a principal diagnosis related to a psychiatric diagnosis or rehabilitation (referred to as the “psychiatric or rehabilitation” MS-LTC-DRGs), as discussed later in this section of this final rule). (For additional information on this step of the relative weight methodology, we refer readers to 67 FR 55991 and 74 FR 43959 through 43960.)
As we proposed, we cross-walked each no-volume MS-LTC-DRG to another MS-LTC-DRG for which we calculated a relative weight (determined in accordance with the methodology as previously described). Then, the “no-volume” MS-LTC-DRG was assigned the same relative weight (and average length of stay) of the MS-LTC-DRG to which it was cross-walked (as described in greater detail in this section of this final rule).
Of the 761 MS-LTC-DRGs for FY 2020, we identified 361 MS-LTC-DRGs for which there were no trimmed applicable LTCH cases (the number identified includes the 8 “transplant” MS-LTC-DRGs, the 2 “error” MS-LTC-DRGs, and the 15 “psychiatric or rehabilitation” MS-LTC-DRGs, which are discussed in this final rule). As we proposed, we assigned relative weights to each of the 361 no-volume MS-LTC-DRGs that contained trimmed applicable LTCH cases based on clinical similarity and relative costliness to one of the remaining 400 (761 − 361 = 400) MS-LTC-DRGs for which we calculated relative weights based on the trimmed applicable LTCH cases in the FY 2018 MedPAR file data using the steps described previously. (For the remainder of this discussion, we refer to the “cross-walked” MS-LTC-DRGs as the MS-LTC-DRGs to which we cross-walked one of the 361 “no-volume” MS-LTC-DRGs.) Then, as we generally proposed, we assigned the 361 no-volume MS-LTC-DRGs the relative weight of the cross-walked MS-LTC-DRG. (As explained in Step 6 of this section, when necessary, we made adjustments to account for nonmonotonicity.)
We cross-walked the no-volume MS-LTC-DRG to a MS-LTC-DRG for which we calculated relative weights based on the March 2019 update of the FY 2018 MedPAR file, and to which it is similar clinically in intensity of use of resources and relative costliness as determined by criteria such as care provided during the period of time surrounding surgery, surgical approach (if applicable), length of time of surgical procedure, postoperative care, and length of stay. (For more details on our process for evaluating relative costliness, we refer readers to the FY 2010 IPPS/RY 2010 LTCH PPS final rule (73 FR 48543).) We believe in the rare event that there would be a few LTCH cases grouped to one of the no-volume MS-LTC-DRGs in FY 2020, the relative weights assigned based on the cross-walked MS-LTC-DRGs would result in an appropriate LTCH PPS payment because the crosswalks, which are based on clinical similarity and relative costliness, would be expected to generally require equivalent relative resource use.
We then assigned the relative weight of the cross-walked MS-LTC-DRG as the relative weight for the no-volume MS-LTC-DRG such that both of these MS-LTC-DRGs (that is, the no-volume MS-LTC-DRG and the cross-walked MS-LTC-DRG) have the same relative weight (and average length of stay) for FY 2020. We note that, if the cross-walked MS-LTC-DRG had 25 applicable LTCH cases or more, its relative weight (calculated using the methodology described in Steps 1 through 4 above) is assigned to the no-volume MS-LTC-DRG as well. Similarly, if the MS-LTC-DRG to which the no-volume MS-LTC-DRG was cross-walked had 24 or less cases and, therefore, was designated to 1 of the low-volume quintiles for purposes of determining the relative weights, we assigned the relative weight of the applicable low-volume quintile to the no-volume MS-LTC-DRG such that both of these MS-LTC-DRGs (that is, the no-volume MS-LTC-DRG and the cross-walked MS-LTC-DRG) have the same relative weight for FY 2020. (As we noted previously, in the infrequent case where nonmonotonicity involving a no-volume MS-LTC-DRG resulted, additional adjustments as described in Step 6 were required in order to maintain monotonically increasing relative weights.)
As discussed earlier, for this final rule, we are providing the list of the no-volume MS-LTC-DRGs and the MS-LTC-DRGs to which each was cross-walked (that is, the cross-walked MS-LTC-DRGs) for FY 2020 in a supplemental data file for public use posted via the internet on the CMS website for this final rule at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html in order to streamline the information made available to the public that is used in the annual development of Table 11.
To illustrate this methodology for determining the relative weights for the FY 2020 MS-LTC-DRGs with no applicable LTCH cases, we are providing the following example, which refers to the no-volume MS-LTC-DRGs crosswalk information for FY 2020 (which, as previously stated, we are providing in a supplemental data file posted via the internet on the CMS website for this final rule).
Example: There were no trimmed applicable LTCH cases in the FY 2018 MedPAR file that we used for this final rule for MS-LTC-DRG 061 (Acute Ischemic Stroke with Use of Thrombolytic Agent with MCC). We determined that MS-LTC-DRG 070 (Nonspecific Cerebrovascular Disorders with MCC) is similar clinically and based on resource use to MS-LTC-DRG 061. Therefore, we assigned the same relative weight (and average length of stay) of MS-LTC-DRG 70 of 0.8629 for FY 2020 to MS-LTC-DRG 061 (we refer readers to Table 11, which is listed in section VI. of the Addendum to this final rule and is available via the internet on the CMS website).
Again, we note that, as this system is dynamic, it is entirely possible that the number of MS-LTC-DRGs with no volume will vary in the future. Consistent with our historical practice, as we proposed, we used the most recent available claims data to identify the trimmed applicable LTCH cases from which we determined the relative weights in this final rule.
For FY 2020, consistent with our historical relative weight methodology, as we proposed, we established a relative weight of 0.0000 for the following transplant MS-LTC-DRGs: Heart Transplant or Implant of Heart Assist System with MCC (MS-LTC-DRG 001); Heart Transplant or Implant of Heart Assist System without MCC (MS-LTC-DRG 002); Liver Transplant with MCC or Intestinal Transplant (MS-LTC-DRG 005); Liver Transplant without MCC (MS-LTC-DRG 006); Lung Transplant (MS-LTC-DRG 007); Simultaneous Pancreas/Kidney Transplant (MS-LTC-DRG 008); Pancreas Transplant (MS-LTC-DRG 010); and Kidney Transplant (MS-LTC-DRG 652). This is because Medicare only covers these procedures if they are performed at a hospital that has been certified for the specific procedures by Medicare and presently no LTCH has been so certified. At the present time, we include these eight transplant MS-LTC-DRGs in the GROUPER program for administrative purposes only. Because we use the same GROUPER program for LTCHs as is used under the IPPS, removing these MS-LTC-DRGs would be administratively burdensome. (For additional information regarding our treatment of transplant MS-LTC-DRGs, we refer readers to the RY 2010 LTCH PPS final rule (74 FR 43964).) In addition, consistent with our historical policy, as we proposed, we established a relative weight of 0.0000 for the 2 “error” MS-LTC-DRGs (that is, MS-LTC-DRG 998 (Principal Diagnosis Invalid as Discharge Diagnosis) and MS-LTC-DRG 999 (Ungroupable)) because applicable LTCH cases grouped to these MS-LTC-DRGs cannot be properly assigned to an MS-LTC-DRG according to the grouping logic.
Section 51005 of the Bipartisan Budget Act of 2018 (Pub. L. 115-123) extended the transitional blended payment rate for site neutral payment rate cases for an additional 2 years (that is, discharges occurring in cost reporting periods beginning in FYs 2018 and 2019 continued to be paid under the blended payment rate). Therefore, in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41529), consistent with our practice in FYs 2016 through 2018, we established a relative weight for FY 2019 equal to the respective FY 2015 relative weight of the MS-LTC-DRGs for the following “psychiatric or rehabilitation” MS-LTC-DRGs: MS-LTC-DRG 876 (O.R. Procedure with Principal Diagnoses of Mental Illness); MS-LTC-DRG 880 (Acute Adjustment Reaction & Psychosocial Dysfunction); MS-LTC-DRG 881 (Depressive Neuroses); MS-LTC-DRG 882 (Neuroses Except Depressive); MS-LTC-DRG 883 (Disorders of Personality & Impulse Control); MS-LTC-DRG 884 (Organic Disturbances & Mental Retardation); MS-LTC-DRG 885 (Psychoses); MS-LTC-DRG 886 (Behavioral & Developmental Disorders); MS-LTC-DRG 887 (Other Mental Disorder Diagnoses); MS-LTC-DRG 894 (Alcohol/Drug Abuse or Dependence, Left Ama); MS-LTC-DRG 895 (Alcohol/Drug Abuse or Dependence, with Rehabilitation Therapy); MS-LTC-DRG 896 (Alcohol/Drug Abuse or Dependence, without Rehabilitation Therapy with MCC); MS-LTC-DRG 897 (Alcohol/Drug Abuse or Dependence, without Rehabilitation Therapy without MCC); MS-LTC-DRG 945 (Rehabilitation with CC/MCC); and MS-LTC-DRG 946 (Rehabilitation without CC/MCC). As we discussed when we implemented the dual rate LTCH PPS payment structure, LTCH discharges that are grouped to these 15 “psychiatric and rehabilitation” MS-LTC-DRGs do not meet the criteria for exclusion from the site neutral payment rate. As such, under the criterion for a principal diagnosis relating to a psychiatric diagnosis or to rehabilitation, there are no applicable LTCH cases to use in calculating a relative weight for the “psychiatric and rehabilitation” MS-LTC-DRGs. In other words, any LTCH PPS discharges grouped to any of the 15 “psychiatric and rehabilitation” MS-LTC-DRGs would always be paid at the site neutral payment rate, and, therefore, those MS-LTC-DRGs would never include any LTCH cases that meet the criteria for exclusion from the site neutral payment rate. However, section 1886(m)(6)(B) of the Act establishes a transitional payment method for cases that would be paid at the site neutral payment rate for LTCH discharges occurring in cost reporting periods beginning during FY 2016 or FY 2017, which was extended to include FYs 2018 and 2019 under Public Law 115-123. (We refer readers to section VII.C. of the preamble of the FY 2019 IPPS/LTCH PPS final rule for a detailed discussion of the extension of the transitional blended payment method provisions under Pub. L. 115-123 and our policies for FY 2019). Under the transitional blended payment method for site neutral payment rate cases, for LTCH discharges occurring in cost reporting periods beginning on or after October 1, 2018, and on or before September 30, 2019, site neutral payment rate cases are paid a blended payment rate, calculated as 50 percent of the applicable site neutral payment rate amount for the discharge and 50 percent of the applicable LTCH PPS standard Federal payment rate. Because this transitional blended payment method for site neutral payment rate cases is applicable for LTCH discharges occurring in cost reporting periods beginning on or after October 1, 2018, and on or before September 30, 2019, some LTCHs' site neutral payment rate cases that are discharged during FY 2020 will be paid a blended payment rate.
Because the LTCH PPS standard Federal payment rate is based on the relative weight of the MS-LTC-DRG, in order to determine the transitional blended payment for site neutral payment rate cases grouped to one of the “psychiatric or rehabilitation” MS-LTC-DRGs in FY 2020, consistent with past practice, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19467), in this final rule we assigned a relative weight to these MS-LTC-DRGs for FY 2020 that is the same as the FY 2019 relative weight (which is also the same as the FYs 2016 through 2019 relative weight). We believed that using the respective FY 2015 relative weight for each of the “psychiatric or rehabilitation” MS-LTC-DRGs results in appropriate payments for LTCH cases that are paid at the site neutral payment rate under the transition policy provided by the statute because there are no clinically similar MS-LTC-DRGs for which we were able to determine relative weights based on applicable LTCH cases in the March 2019 update of the FY 2018 MedPAR file data using the steps previously described. Furthermore, we believe that it would be administratively burdensome and introduce unnecessary complexity to the MS-LTC-DRG relative weight calculation to use the LTCH discharges in the MedPAR file data to calculate a relative weight for those 15 “psychiatric and rehabilitation” MS-LTC-DRGs to be used for the sole purposes of determining half of the transitional blended payment for site neutral payment rate cases during the transition period (80 FR 49631 through 49632) or payment for discharges from spinal cord specialty hospitals under § 412.522(b)(4).
In summary, for FY 2020, as we proposed, we established a relative weight (and average length of stay thresholds) equal to the respective FY 2015 relative weight of the MS-LTC-DRGs for the 15 “psychiatric or rehabilitation” MS-LTC-DRGs listed previously (that is, MS-LTC-DRGs 876, 880, 881, 882, 883, 884, 885, 886, 887, 894, 895, 896, 897, 945, and 946). Table 11, which is listed in section VI. of the Addendum to this proposed rule and is available via the internet on the CMS website, reflects this policy.
Step 6—Adjust the FY 2020 MS-LTC-DRG relative weights to account for nonmonotonically increasing relative weights.
The MS-DRGs contain base DRGs that have been subdivided into one, two, or three severity of illness levels. Where there are three severity levels, the most severe level has at least one secondary diagnosis code that is referred to as an MCC (that is, major complication or comorbidity). The next lower severity level contains cases with at least one secondary diagnosis code that is a CC (that is, complication or comorbidity). Those cases without an MCC or a CC are referred to as “without CC/MCC.” When data do not support the creation of three severity levels, the base MS-DRG is subdivided into either two levels or the base MS-DRG is not subdivided. The two-level subdivisions may consist of the MS-DRG with CC/MCC and the MS-DRG without CC/MCC. Alternatively, the other type of two-level subdivision may consist of the MS-DRG with MCC and the MS-DRG without MCC.
In those base MS-LTC-DRGs that are split into either two or three severity levels, cases classified into the “without CC/MCC” MS-LTC-DRG are expected to have a lower resource use (and lower costs) than the “with CC/MCC” MS-LTC-DRG (in the case of a two-level split) or both the “with CC” and the “with MCC” MS-LTC-DRGs (in the case of a three-level split). That is, theoretically, cases that are more severe typically require greater expenditure of medical care resources and would result in higher average charges. Therefore, in the three severity levels, relative weights should increase by severity, from lowest to highest. If the relative weights decrease as severity increases (that is, if within a base MS-LTC-DRG, an MS-LTC-DRG with CC has a higher relative weight than one with MCC, or the MS-LTC-DRG “without CC/MCC” has a higher relative weight than either of the others), they are nonmonotonic. We continue to believe that utilizing nonmonotonic relative weights to adjust Medicare payments would result in inappropriate payments because the payment for the cases in the higher severity level in a base MS-LTC-DRG (which are generally expected to have higher resource use and costs) would be lower than the payment for cases in a lower severity level within the same base MS-LTC-DRG (which are generally expected to have lower resource use and costs). Therefore, in determining the FY 2020 MS-LTC-DRG relative weights, consistent with our historical methodology, as we proposed, we continued to combine MS-LTC-DRG severity levels within a base MS-LTC-DRG for the purpose of computing a relative weight when necessary to ensure that monotonicity is maintained. For a comprehensive description of our existing methodology to adjust for nonmonotonicity, we refer readers to the FY 2010 IPPS/RY 2010 LTCH PPS final rule (74 FR 43964 through 43966). Any adjustments for nonmonotonicity that were made in determining the FY 2020 MS-LTC-DRG relative weights in this final rule by applying this methodology are denoted in Table 11, which is listed in section VI. of the Addendum to this final rule and is available via the internet on the CMS website.
Step 7— Calculate the FY 2020 MS-LTC-DRG reclassification and recalibration budget neutrality factor.
In accordance with the regulations at § 412.517(b) (in conjunction with § 412.503), the annual update to the MS-LTC-DRG classifications and relative weights is done in a budget neutral manner such that estimated aggregate LTCH PPS payments would be unaffected, that is, would be neither greater than nor less than the estimated aggregate LTCH PPS payments that would have been made without the MS-LTC-DRG classification and relative weight changes. (For a detailed discussion on the establishment of the budget neutrality requirement for the annual update of the MS-LTC-DRG classifications and relative weights, we refer readers to the RY 2008 LTCH PPS final rule (72 FR 26881 and 26882).)
The MS-LTC-DRG classifications and relative weights are updated annually based on the most recent available LTCH claims data to reflect changes in relative LTCH resource use (§ 412.517(a) in conjunction with § 412.503). To achieve the budget neutrality requirement at § 412.517(b), under our established methodology, for each annual update, the MS-LTC-DRG relative weights are uniformly adjusted to ensure that estimated aggregate payments under the LTCH PPS would not be affected (that is, decreased or increased). Consistent with that provision, as we proposed, we updated the MS-LTC-DRG classifications and relative weights for FY 2020 based on the most recent available LTCH data for applicable LTCH cases, and continued to apply a budget neutrality adjustment in determining the FY 2020 MS-LTC-DRG relative weights.
In this FY 2020 IPPS/LTCH PPS final rule, to ensure budget neutrality in the update to the MS-LTC-DRG classifications and relative weights under § 412.517(b), as we proposed, we continued to use our established two-step budget neutrality methodology.
To calculate the normalization factor for FY 2020, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19468), we grouped applicable LTCH cases using the FY 2020 Version 37 GROUPER, and the recalibrated FY 2020 MS-LTC-DRG relative weights to calculate the average case-mix index (CMI); we grouped the same applicable LTCH cases using the FY 2019 GROUPER Version 36 and MS-LTC-DRG relative weights and calculated the average CMI; and computed the ratio by dividing the average CMI for FY 2019 by the average CMI for FY 2020. That ratio is the normalization factor. Because the calculation of the normalization factor involves the relative weights for the MS-LTC-DRGs that contained applicable LTCH cases to calculate the average CMIs, any low-volume MS-LTC-DRGs are included in the calculation (and the MS-LTC-DRGs with no applicable LTCH cases are not included in the calculation).
To calculate the budget neutrality adjustment factor, we simulated estimated total FY 2020 LTCH PPS standard Federal payment rate payments for applicable LTCH cases using the FY 2020 normalized relative weights and GROUPER Version 37; simulated estimated total FY 2020 LTCH PPS standard Federal payment rate payments for applicable LTCH cases using the FY 2019 MS-LTC-DRG relative weights and the FY 2019 GROUPER Version 36; and calculated the ratio of these estimated total payments by dividing the simulated estimated total LTCH PPS standard Federal payment rate payments using the FY 2019 MS-LTC-DRG relative weights and the GROUPER Version 36 by the simulated estimated total LTCH PPS standard Federal payment rate payments using the FY 2020 MS-LTC-DRG relative weights and the GROUPER Version 37. The resulting ratio is the budget neutrality adjustment factor. The calculation of the budget neutrality factor involves the relative weights for the LTCH cases used in the payment simulation, which includes any cases grouped to low-volume MS-LTC-DRGs or to MS-LTC-DRGs with no applicable LTCH cases, and generally does not include payments for cases grouped to a MS-LTC-DRG with no applicable LTCH cases. (Occasionally, a few LTCH cases (that is, those with a covered length of stay of 7 days or less, which are removed from the relative weight calculation in step (2) that are grouped to a MS-LTC-DRG with no applicable LTCH cases) are included in the payment simulations used to calculate the budget neutrality factor. However, the number and payment amount of such cases have a negligible impact on the budget neutrality factor calculation).
In this final rule, to ensure budget neutrality in the update to the MS-LTC-DRG classifications and relative weights under § 412.517(b), as we proposed, we continued to use our established two-step budget neutrality methodology. Therefore, in this final rule, in the first step of our MS-LTC-DRG budget neutrality methodology, for FY 2020, as we proposed, we calculated and applied a normalization factor to the recalibrated relative weights (the result of Steps 1 through 6 discussed previously) to ensure that estimated payments are not affected by changes in the composition of case types or the changes to the classification system. That is, the normalization adjustment is intended to ensure that the recalibration of the MS-LTC-DRG relative weights (that is, the process itself) neither increases nor decreases the average case-mix index.
To calculate the normalization factor for FY 2020 (the first step of our budget neutrality methodology), we used the following three steps: (1.a.) Used the most recent available applicable LTCH cases from the most recent available data (that is, LTCH discharges from the FY 2018 MedPAR file) and grouped them using the FY 2020 GROUPER (that is, Version 37 for FY 2020) and the recalibrated FY 2020 MS-LTC-DRG relative weights (as previously determined in Steps 1 through 6) to calculate the average case-mix index; (1.b.) grouped the same applicable LTCH cases (as are used in Step 1.a.) using the FY 2019 GROUPER (Version 36) and FY 2019 MS-LTC-DRG relative weights and calculated the average case-mix index; and (1.c.) computed the ratio of these average case-mix indexes by dividing the average CMI for FY 2020 (determined in Step 1.a.) by the average case-mix index for FY 2019 (determined in Step 1.b.). As a result, in determining the MS-LTC-DRG relative weights for FY 2020, each recalibrated MS-LTC-DRG relative weight was multiplied by the normalization factor of 1.27367 (determined in Step 1.c.) in the first step of the budget neutrality methodology, which produced “normalized relative weights.”
In the second step of our MS-LTC-DRG budget neutrality methodology, we calculated a second budget neutrality factor consisting of the ratio of estimated aggregate FY 2020 LTCH PPS standard Federal payment rate payments for applicable LTCH cases (the sum of all calculations under Step 1.a. mentioned previously) after reclassification and recalibration to estimated aggregate payments for FY 2020 LTCH PPS standard Federal payment rate payments for applicable LTCH cases before reclassification and recalibration (that is, the sum of all calculations under Step 1.b. mentioned previously).
That is, for this final rule, for FY 2020, under the second step of the budget neutrality methodology, as we proposed, we determined the budget neutrality adjustment factor using the following three steps: (2.a.) Simulated estimated total FY 2020 LTCH PPS standard Federal payment rate payments for applicable LTCH cases using the normalized relative weights for FY 2020 and GROUPER Version 37 (as previously described); (2.b.) simulated estimated total FY 2020 LTCH PPS standard Federal payment rate payments for applicable LTCH cases using the FY 2019 GROUPER (Version 36) and the FY 2019 MS-LTC-DRG relative weights in Table 11 of the FY 2019 IPPS/LTCH PPS final rule available on the internet, as described in section VI. of the Addendum of that final rule; and (2.c.) calculated the ratio of these estimated total payments by dividing the value determined in Step 2.b. by the value determined in Step 2.a. In determining the FY 2020 MS-LTC-DRG relative weights, each normalized relative weight was then multiplied by a budget neutrality factor of 0.9959342 (the value determined in Step 2.c.) in the second step of the budget neutrality methodology to achieve the budget neutrality requirement at § 412.517(b).
Accordingly, in determining the FY 2020 MS-LTC-DRG relative weights in this final rule, consistent with our existing methodology, as we proposed, we applied a normalization factor of 1.27367 and a budget neutrality factor of 0.9959342. Table 11, which is listed in section VI. of the Addendum to this final rule and is available via the internet on the CMS website, lists the MS-LTC-DRGs and their respective relative weights, geometric mean length of stay, and five-sixths of the geometric mean length of stay (used to identify SSO cases under § 412.529(a)) for FY 2020.
C. Payment Adjustment for LTCH Discharges That Do Not Meet the Applicable Discharge Payment Percentage
Section 1886(m)(6)(C) of the Act, as added by section 1206 of the Pathway for SGR Reform Act of 2013 (Pub. L. 113-67), imposes several requirements related to an LTCH's discharge payment percentage. As defined by section 1886(m)(6)(C)(iv) of the Act, the term “LTCH discharge payment percentage” is a ratio, expressed as a percentage, of Medicare fee-for-service (FFS) discharges not paid the site neutral payment rate to total number of Medicare FFS discharges occurring during the cost reporting period. In other words, an LTCH's discharge payment percentage is the ratio of an LTCH's Medicare discharges that meet the criteria for exclusion from the site neutral payment rate (as described under § 412.522(a)), that is, discharges paid the LTCH PPS standard Federal payment rate, to an LTCH's total number of Medicare FFS discharges paid under the LTCH PPS during the cost reporting period. Section 1886(m)(6)(C)(ii)(I) of the Act, requires that, for cost reporting periods beginning on or after October 1, 2019, any LTCH with a discharge payment percentage for the cost reporting period that is not at least 50 percent be informed of such a fact; and section 1886(m)(6)(C)(ii)(II) of the Act requires that all of the LTCH's discharges in each successive cost reporting period be paid the payment amount that would apply under subsection (d) for the discharge if the hospital were a subsection (d) hospital, subject to the LTCH's compliance with the process for reinstatement provided for by section 1886(m)(6)(C)(iii) of the Act.
Section 1886(m)(6)(C)(i) of the Act requires that we provide notice to each LTCH of the LTCH's discharge payment percentage for LTCH cost reporting periods beginning during or after FY 2016. We first implemented this requirement in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49613), and established subregulatory policies and timeframes by which we then calculated and informed LTCHs of their discharge payment percentage. Such policies included the form letter to be used in the notification. As we noted in our proposed rule, because the discharge payment percentage for a cost reporting period cannot be calculated until after the cost reporting period has ended, in order to ensure claims for the entire period are reflected, an LTCH has typically been informed of the results of the calculation of the discharge payment percentage between 5 and 6 months after the end of the cost reporting period. (For more information on these policies and timelines, we refer readers to the FY 2016 IPPS/LTCH PPS final rule at 80 FR 49601 through 49614.)
To implement the provisions of section 1886(m)(6)(C)(ii)(I) of the Act, as established by the amendments made by Public Law 113-67, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19469), we proposed to continue to use our established policies and timelines to calculate the discharge payment percentage and to continue to inform LTCHs as we have in the past when their discharge payment percentage for the cost reporting period is not at least 50 percent.
Comment: Some commenters requested that we require MACs use additional data, for example matching the related inpatient PPS and LTCH claims data, when determining whether a discharge qualifies for exclusion from the site neutral payment rate for the purpose of calculating the discharge payment percentage. These commenters believe such a requirement would mitigate LTCH disputes when there is a delay in the availability of the information on the prior hospital stay, such as, data confirming the patient's ICU days during the prior hospital stay. Similarly, some commenters further requested that we revise our existing policy on the requirements for providing supplementary information to exclude a discharge from the site neutral payment rate by requiring MACs to obtain certain information from IPPS hospitals. Other commenters asked that we exclude the use of updated claims data from IPPS hospitals in our calculation of the discharge payment percentage if the original claims data supported exclusion, but the updated claims data does not. In support of this request, some commenters cited concerns about having relied on the initial information they receive from referring hospitals, and that it is unfair to retroactively penalize them in-so-far as the calculation of their discharge payment percentage when their belief that they were admitting a case that would be excluded from the site neutral payment rate was reasonable.
Response: We believe our existing policies, which require MACs to accept supplementary information from LTCHs in circumstances when the data in the Medicare claims system does not contain the applicable information demonstrating the discharge meets the criteria for exclusion from the site neutral payment rate provides a reasonable opportunity for an LTCH to provide additional information to supplement the CMS claims data. (For example, if the subsection (d) hospital from which the patient was immediately discharged was a Veterans Administration hospital, the Medicare claims processing systems would not have data from that discharge.) Furthermore, those policies appropriately balance the interests of ensuring claims are only excluded from the site neutral payment rate when the statutory criteria are met while allowing sufficient flexibility for unusual instances when information that would support exclusion is not contained in the Medicare claims processing system. We believe that in determining whether a discharge is excluded from the site neutral payment rate we should use the best data reasonably available in accordance with the current policy that we proposed continuing to use for purposes of the calculation of the discharge payment percentage (which is based on the actual determination used for making Medicare payment to the LTCH for that discharge). We note our policies for determining whether a discharge is excluded from the site neutral payment rate for purposes of making Medicare payments, which we proposed to continue to use for calculating the discharge payment percentage, were adopted through notice and comment rulemaking in the FY 2016 final rule (for more information on these policies we refer readers to the FY 2016 IPPS/LTCH PPS final rule 80 FR 49601). Finally, in response to specific concerns regarding the accuracy of the information received by the LTCH from the referring hospital at the time an LTCH makes an admission decision, we again encourage LTCHs to work closely with their referring hospitals and vice versa to ensure the accuracy of the information to be used in admission decisions as well as in discharge planning and case management. For these reasons, we believe it is appropriate to finalize our proposal to continue to use the current policies and timelines for determining when a discharge meets the criteria for exclusion from the site neutral payment rate (including those which allow hospitals to submit information to supplement information in the Medicare claims processing system).
In addition to our proposed policies regarding notification of their calculated discharge payment percentage, to implement the provisions of section 1886(m)(6)(C)(ii)(II) of the Act, as established by the amendments made by Public Law 113-67, in the FY 2020 IPPS/LTCH PPS proposed rule we also proposed to establish the policies and timing for when an LTCH that does not meet the required discharge payment percentage would become subject to a payment adjustment for cost reporting periods beginning on or after October 1, 2019. Under our proposal, the LTCH would first be notified of the failure to meet that requirement (we note that, as discussed above, we proposed to use our existing policies regarding notifying an LTCH of its discharge payment percentage). Then, if the LTCH is found not to have met the requisite discharge payment percentage, the LTCH would be subject to the payment adjustment for the first cost reporting period after it has been notified that its discharge payment percentage for a cost reporting period had been calculated to not have been at least 50 percent. For example, if an LTCH has a calendar year cost reporting period, its first cost reporting period beginning on or after October 1, 2019 would be its January 1, 2020 through December 31, 2020 cost reporting period (that is, its FY 2020 cost reporting period). Because a cost reporting period must have ended and claims from the reporting period must be processed prior to the calculation of the discharge payment percentage, generally a hospital's discharge payment percentage for its FY 2020 cost reporting period cannot be calculated for approximately 5-6 months; that is, it would not be completed until sometime during its FY 2021 cost reporting period. If the discharge payment percentage for its FY 2020 cost reporting period is not at least 50 percent (when calculated during its FY 2021 cost reporting period), under our proposal, the LTCH would be notified of that failure during its FY 2021 cost reporting period, and it would become subject to a payment adjustment, which would be applied to all of the LTCH's discharges that occur during its FY 2022 cost reporting period (that is, the first cost reporting period after receiving notification that its discharge payment percentage for a cost reporting period had been calculated to not have been at least 50 percent). In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19470), we proposed to codify the proposed implementation of these regulations establishing this policy under proposed new § 412.522(d)(3).
Comment: Most commenters supported our proposal to apply the payment adjustment for failure to maintain the required discharge payment percentage prospectively, which is to discharges in the cost reporting period after the calculation is performed and the facility is notified of its percentage. A few commenters objected in general to the application of the payment adjustment to facilities that failed to meet the required discharge payment percentage, or requested that its application be delayed.
Response: While we sympathize with commenters requesting an implementation delay, the payment adjustment for LTCHs which do not maintain the requisite discharge payment percentage, we do not have an option to forgo implementation or delay application of this statutory payment adjustment.
Comment: Some commenters requested confirmation that the discharge payment percentage would be calculated based on the LTCH as a whole (for example, for all campuses of a multi-campus LTCH).
Response: As we stated in the proposed rule, the discharge payment percentage is calculated for the hospital, not individual locations of the hospital. Therefore, consistent with our proposal, the discharge payment percentage will be calculated based on the LTCH as a whole using the CMS Certification Number (CCN) on hospital claims submitted to Medicare.
Comment: Some commenters requested confirmation that the LTCH would maintain its IPPS-excluded hospital status when subject to the payment adjustment.
Response: A hospital subject to the payment adjustment will remain an LTCH as long as it maintains an average length of stay of 25 or more days as required under the existing regulations.
After considering the comments received, we are finalizing our proposed payment adjustment policy at § 412.522(d)(3) which will be applied to discharges occurring in cost reporting periods beginning on or after October 1, 2019, with the initial penalties applied to the cost reporting period after the percentage is calculated and the LTCH is notified as to the failure to meet the discharge payment percentage requirement.
As previously noted, section 1886(m)(6)(C)(iii) of the Act, as established by the amendments made by Public Law 113-67, provides for the establishment of a reinstatement process whereby an LTCH can have the payment adjustment discontinued. To do so, in the FY 2020 IPPS/LTCH PPS proposed rule we proposed to discontinue the payment adjustment beginning with the discharges occurring in the cost reporting period after the LTCH has been notified that its discharge payment percentage was calculated to be at least 50 percent. For example, an LTCH with a calendar year cost reporting period that did not have a discharge payment percentage of at least 50 percent during its FY 2020 cost reporting period would be subject to the payment adjustment for its FY 2022 cost reporting period, as previously described. However, if the discharge payment percentage for its FY 2021 cost reporting period equaled at least 50 percent, the calculation of such percentage (and notification thereof) would be made during FY 2022, and the payment adjustment would be discontinued beginning with discharges occurring at the start of its FY 2023 cost reporting period. We noted that this proposed policy is based on cost reporting periods, is cyclical in nature, and, as such, an LTCH that has been reinstated would be subject to the payment adjustment again (in the same manner as described previously) if its discharge payment percentage is again calculated not to meet the required threshold. For instance, if the LTCH in the example above were to once again fail to meet the requisite percentage in FY 2022, it would be subject to a new payment penalty in FY 2024. We proposed to codify this reinstatement process policy at § 412.522(d)(5).
Comment: Several commenters supported our reinstatement process proposals regarding the discontinuation of penalties. In addition, some commenters requested discontinuation of the penalty as soon as an LTCH can demonstrate it has met the required discharge payment percentage using real-time monitoring, as delaying the removal of the penalty until the following cost reporting period would be unduly burdensome for hospitals subject to the adjustment for an entire cost reporting period.
Response: We appreciate the commenters' support of the proposed discontinuation of penalties under our proposed reinstatement process. We do not believe allowing discontinuation of the penalty at any point an LTCH demonstrates it has attained the requisite discharge payment percentage is appropriate. The calculation of the discharge payment percentage is a ratio of discharges paid at the standard Federal payment rate to total discharges. Therefore, by definition, every discharge from the LTCH will change that percentage. We believe that adopting a policy without clear timeframes designated for when the calculation of the discharge payment percentage would apply introduces instability and unpredictability into the LTCH PPS. Additionally, the statute specifically references a hospital's cost reporting period when describing when an LTCH should be subject to the adjustment. Therefore, we believe that applying the payment adjustment by cost reporting period for the entire cost reporting period is most consistent with the statute is. As such we are not adopting the commenters' suggestions.
As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19470), while we believe the proposed reinstatement process policy would satisfy the statutory requirement without further modification, because there could be unusual circumstances that result in a discharge payment percentage for a cost reporting period that may not be fully reflective of an LTCH's typical mix of site neutral and LTCH PPS standard Federal payment rate discharges (for example, patients require a shorter period of ventilation than was expected on admission), we also proposed a special probationary reinstatement process, which is consistent with public comments we received during the FY 2016 rulemaking when the dual-rate payment system was implemented. While the public comments from the FY 2016 rulemaking cycle did not request that the special reinstatement process be probationary, we are concerned that, while there are unusual circumstances that may result in the discharge payment percentage for a cost reporting period not being fully reflective of an LTCH's typical mix of site neutral and LTCH PPS standard Federal payment rate discharges, if the special reinstatement process were not probationary, hospitals may be able to manipulate discharges or delay billing in such a way as to artificially inflate their discharge payment percentage for purposes of qualifying for the special reinstatement process. To alleviate these concerns, in the FY 2020 IPPS/LTCH PPS proposed rule we proposed that the special reinstatement process be probationary. Under this proposed special probationary reinstatement process, a probationary-cure period would allow an LTCH the opportunity to have the payment adjustment delayed during the applicable cost reporting period if, for the period of at least 5 consecutive months of the 6-month period immediately preceding the beginning of the cost reporting period during which the adjustment would apply (we note this time period is consistent with our current policy for the average length-of-stay determination), the discharge payment percentage is calculated to be at least 50 percent. Under such circumstances, the LTCH would not ultimately be subject to the payment adjustment for the cost reporting period during which the adjustment would apply—provided that the discharge payment percentage for that cost reporting period is at least 50 percent. If the discharge payment percentage for that cost reporting period is not at least 50 percent, the adjustment will be applied to the cost reporting period at settlement. For example, an LTCH with a calendar year cost reporting period that does not have a discharge payment percentage of at least 50 percent during its FY 2020 cost reporting period would be informed of this during its FY 2021 cost reporting period. The payment adjustment would then apply during its FY 2022 cost reporting period. However, if in the 6-month period immediately preceding the cost reporting period for which the payment adjustment would apply (in this example, July 1, 2021 through December 31, 2021), the LTCH achieved at least 5 consecutive months with a discharge payment percentage that is calculated to be at least 50 percent, application of the payment adjustment would be delayed during the FY 2022 cost reporting period (that is, the payment adjustment would not be applied to any discharges that occur during the FY 2022 cost reporting period). (We note that the period of time which is used for the cure period calculation must allow sufficient time for the MAC to complete the calculation and notify the LTCH of the results of the calculation prior to the beginning of the cost reporting period during which the payment adjustment otherwise would apply if the hospital fails to cure.) However, if the discharge payment percentage that is ultimately calculated for that LTCH's FY 2022 cost reporting period (the period for which the payment adjustment would have applied if the LTCH had not met the requirements during the probationary cure period) is not at least 50 percent, the payment adjustment delay would be lifted, and the penalty would be applied to payments made for all of the discharges that occurred during the FY 2022 cost reporting period at settlement.
We proposed to codify the policy for a special probationary reinstatement process at § 412.522(d)(6). In the FY 2020 IPPS/LTCH PPS proposed rule, we noted that we expect to issue subregulatory guidance to describe the specific procedures for implementing this proposed probationary-cure period, if the policy is finalized. We also invited public comments on suggestions regarding the specific process to be used, including whether the process should mirror the existing process used by LTCHs for the greater than 25-day average length-of-stay requirements.
Comment: Many commenters supported our proposal to adopt a special probationary cure period, while some commenters opposed it. The commenters that opposed the proposed special probationary cure period stated that such a policy is not required by statute and as such creates unnecessary work for MACs and hospitals.
Response: We appreciate the commenters' support for our proposal to adopt a special probationary cure period as part of the reinstatement process. While we agree that a probationary reinstatement process is not required under the statute, as we stated in the proposed rule, at this time we believe that the use of a probationary cure period is the best way to balance concern for administrative simplicity while allowing for unusual circumstances where the discharge payment percentage calculated for a cost reporting period is not fully representative of the general mix of standard and site neutral discharges for a hospital.
Comment: Some commenters requested that we align the timing of the special probationary reinstatement process with the existing timing for the calculation of the average length of stay cure period.
Response: As we described in the proposed rule and in more detail in this final rule, the timing of the calculations for both the special probationary reinstatement process and the average length of stay cure period are the same, namely at least 5 consecutive months of the 6 months immediately preceding the cost reporting period for which, in the case of the special probationary reinstatement process, the payment adjustment would apply or, in the case of the average length of stay cure period, the hospital would lose its IPPS-excluded status. Therefore, we believe that these comments are generally supportive of our proposal and thank commenters for their support. To the extent that any of these comments were referring to the lack of a provisional determination under the existing timing for the calculation of the average length of stay cure period, we refer reader to our response to the comments opposing the probationary nature of the proposed cure period discussed below.
Comment: Some commenters opposed the probationary nature of the proposed special reinstatement process (that is, probationary cure period). Some commenters objected to the period of time between when the discharges in a cost reporting period may be subject to a payment adjustment and the final determination of whether such an adjustment would be applied, indicating it would be unduly burdensome for hospitals. Other commenters pointed out that because the cure period for the calculation of an LTCH's average length of stay is not probationary, it should not be in this context either. Some commenters argued that our policy concerns underlying the probationary nature of the special reinstatement process are unfounded, some of which cited timely filing requirements that allow for up to a year to bill the Medicare program.
Other commenters argued that the special probationary reinstatement process would result in an LTCH being penalized twice for not maintaining the requisite discharge payment percentage during the same cost reporting period because, in the commenters' view, the payment adjustment would be applied twice based on a single cost reporting period's calculation. Some commenters stated that using a probationary cure period as part of the reinstatement would result in increased unpredictably to payments and is contrary to the principles of prospective payment. Some commenters requested that we also adopt a policy which would allow for application of the payment adjustment to be reversed if, after having been applied it is determined that the hospital met the requisite discharge payment percentage during the cost reporting period in which the penalty is applied (we note that under our proposed policy, the only situation in which this would occur would be if the LTCH did not meet the requisite threshold during its cure period). Lastly, a few commenters stated that our proposal on the mechanics of the special probationary reinstatement process was unclear and did not allow for meaningful comment.
Response: As we previously stated, we believe a probationary reinstatement process balances the ability to provide for an opportunity to allow for unusual circumstances where the discharge payment percentage may not be fully representative of the general mix of an LTCH's discharges and the desire for administrative simplicity, as well as the concerns stated in the proposed rule (and discussed further in this final rule) related to maintaining the integrity of the statutory payment adjustment for LTCHs that do not maintain the required discharge patient percentage. We recognize the special probationary cure period inherently requires additional time between when the discharges in a cost reporting period may be subject to the payment adjustment and when a final determination is made as to whether the adjustment is applied. However, we believe the special probationary cure period appropriately balances the competing goals previously outlined. We also note that under our proposed policy, the timing of final settlement of the cost report will be unaffected. If, as we gain experience under this policy, it appears that the probationary nature of the cure period feature of the reinstatement process results in excessive burden to LTCHs we could re-examine the need for the special probationary reinstatement process entirely as it is not required under the statute (as noted previously). A final prospective determination based on the entirety of a cost reporting period as described in the general reinstatement process would eliminate the concerns regarding the probationary reinstatement process while fulfilling statutory obligations.
In response to the argument that our policy concerns, such as potential manipulation of billing during the cure period, is unfounded, we disagree. As pointed out by commenters, timely filing rules allow for up to a year to bill the Medicare program, and, as such, an LTCH could engineer its discharge payment percentage for the 5 to 6 month cure period, to be greater than 50 percent. For example, within the 1-year timely filing period, an LTCH could purposely chose to hold its claims for site neutral discharges during the cure period (or submit claims for standard Federal payment rate discharges which had been held prior to the start of the cure period) for no reason other than to ensure that its discharge payment percentage for the cure period meets the requisite percentage. While such billing practices may be permissible under the timely filing requirements, it could encourage artificially inflated discharge payment percentages during the cure period in an effort to game the discharge payment percentage to avoid the payment adjustment required by the statute. In such a case, when those held claims are finally submitted and processed, we would expect the discharge payment percentage for discharges occurring during the cure period to be lower than it was calculated to have been based on claims data available at the time it was calculated. As such, the LTCH compliance with the discharge payment percentage requirement could fluctuate solely based on its billing practices. For these reasons, we believe it is appropriate that the cure period component of the reinstatement process be probationary in order to effectively preclude such behavior.
In response to the commenters' observation that the average length of stay cure period is not probationary, we note the loss of IPPS-excluded status as a result of failure to maintain the requisite average length of stay, may only happen at the beginning of a cost reporting period. As we stated in response to previous comments, failure to maintain the requisite discharge payment percentage does not in itself result in a change in the classification of the hospital (that is, a hospital which does not maintain its average length of stay will cease to be an LTCH, while a hospital which does not maintain its discharge payment percentage, but remains in compliance with other requirements will remain an LTCH). The regulations at 42 CFR 412.22(d) require that a change in a hospital's status from IPPS-excluded to non-excluded may only occur at the beginning of a cost reporting period, therefore it is impractical for the average length of stay cure period to be probationary. Because being subject to the payment adjustment is not a change in the hospital's IPPS-excluded status (provided the LTCH remains in compliance with other requirements), this same concern does not exist here, and given the possibility for selective billing practices that could result in manipulation of the calculation of the discharge payment percentage during the cure period discussed previously, we believe the best way to maintain the integrity of the program is to use a special probationary reinstatement process.
As for the assertion that under the probationary cure period an LTCH would be penalized twice for failing to make its discharge payment percent, we note that there is only one penalty for any given cost reporting period in which an LTCH fails to meet the required discharge payment percentage. For example, if an LTCH has an cost reporting period beginning on January 1, and it is found in 2021 to have failed have met the requisite discharge payment percentage for its 2020 cost reporting period, the payment adjustment would be applied in its 2022 cost reporting period. However, if during the cure period (that is, at least 5 consecutive months between July and December 2021) the discharge payment percentage is at least 50 percent, the payment adjustment in 2022 is suspended. If the LTCH failed to cure and its discharge payment percentage for the hospital's FY 2022 cost reporting period did not meet the requisite discharge payment percentage, the suspended adjustment (which is a result of its failure to maintain the requisite discharge payment percentage during the FY 2020 cost reporting period) will be applied to that period. Failure to meet the requisite percentage during the FY 2022 cost reporting period would also mean the LTCH would be notified of that failure in FY 2023, and subject to a separate adjustment (as a result of its failure to maintain the requisite discharge payment percentage) during its FY 2024 period. Prior to the application of the adjustment during its FY 2024 cost reporting period, the LTCH would (again) be allowed to take advantage of the probationary cure period. Thus, while the penalty operates on a 2- year delay, and the granting or denying of the cure is based on a later year's performance, there is only ever one penalty imposed per cost reporting period.
In response to concerns about introducing increased unpredictability, as previously discussed, we believe a probationary cure period appropriately balances providing an opportunity to recognize unusual circumstances when the discharge payment percentage does not fully reflect the general mix of an LTCH's discharges while affording protections to the Medicare program from potential manipulation of discharges or billing practices in an effort to qualify for the special reinstatement process. As previously discussed, if the special reinstatement process is found to be overly burdensome, we will re-examine these policies in a future rulemaking.
In response to concerns that suspending the payment adjustment during interim claims payment but the applying the payment adjustment at final settlement of the cost report is contrary to the principles of prospective payment, we note that there are several other instances where LTCH PPS payments made during a cost reporting period are “trued up” at cost report settlement (for example, periodic interim payments or outlier reconciliation). Therefore we do not believe the special probationary reinstatement policy would be contrary to the principles of prospective payment.
In response to requests to add a second cure period in which adjusted payments may be unadjusted if, during the cost reporting period in which the adjustment was applied, the discharge payment percentage is determined to have exceeded 50 percent, as we noted previously, the only way this is possible is if an LTCH does not maintain the requisite discharge payment percentage during its cure period. Under our proposal, for the LTCH with a January—December cost reporting period, if it fails to meet the requisite discharge payment percentage during its FY 2020 cost reporting period the LTCH would be subject to the payment adjustment during its FY 2022 cost reporting only if the discharge payment percentage threshold for the probationary cure period were not met. As explained above, such an LTCH's cure period would be at least 5 consecutive months between July and December 2021. As such prior to the application of the adjustment, the LTCH will have already had (and failed) two opportunities to demonstrate that it met requisite discharge payment percentage (that is, its 2020 cost reporting period and the cure period (which occurs prior to the start of its FY 2022 cost reporting period). Taking the commenter's suggestion would allow the LTCH a third chance (the FY 2022 cost reporting period) to meet the statutorily required discharge payment percentage.). We note that this would further complicate a cure process that other commenters are already concerned about being overly complex. In addition, our proposed probationary cure period already gives LTCHs an opportunity to earn suspension of the payment adjustment. Such opportunity is not required by statute, but serves to address what we find to be valid concerns about unusual circumstances that could result in fluctuations in patient populations that would lead to an aberrant discharge payment percentage that is not reflective of an LTCH's general admissions practices—we do not believe a second opportunity to cure 2 years' distant from the initial nonconforming cost reporting period is necessary to address such unusual circumstances. That is, we would not anticipate any such unusual circumstances resulting in 2 years-worth of non-compliance. Furthermore, any such reopening process would introduce additional unpredictability and administrative expense that we do not find justified in light of the issue we intended to address with the cure period.
Finally, we disagree with commenters' allegations that our proposal did not provide sufficient details on the mechanics of the special probationary reinstatement process to allow for meaningful comment. As we have previously summarized, we received many comments on various facets of the proposal which would not have been possible had our proposal been as unclear as these commenters allege. For these reasons we believe that the proposed rule provided ample opportunity for meaningful notice and comment rulemaking.
After considering the comments received, for the reasons previously discussed, we are finalizing our policy as proposed.
Section 1886(m)(6)(C)(ii) of the Act specifies that, subject to the process for reinstatement, when the requisite discharge patient percentage threshold is not met, all of the LTCH's discharges in each successive cost reporting period will be paid the payment amount that would apply under subsection (d) for the discharge if the hospital were a subsection (d) hospital. In the FY 2020 IPPS/LTCH PPS proposed rule, we noted that “subsection (d)” as it is referred to under section 1886(d) of the Act refers to IPPS hospitals. For purposes of implementing the payment adjustment provisions of section 1886(m)(6)(C)(ii) of the Act, as established by the amendments of Pub. L. 113-67, we proposed to establish the policy at proposed new § 412.522(d)(4) that, for cost reporting periods beginning on or after October 1, 2019, under this payment adjustment, the LTCH would receive payment for all discharges in the cost reporting periods beginning after the LTCH is informed that its calculated discharge payment percent is not at least 50 percent at the amount determined under §§ 412.529(d)(4)(i)(A) and (ii), with an additional payment for high-cost outlier cases that would be based on the IPPS fixed-loss amount in effect at the time of the LTCH discharge. We noted that the amount determined under §§ 412.529(d)(4)(i)(A) and (ii) is the basis of the IPPS comparable per diem amount (for which the per diem is calculated in accordance with the provisions of §§ 412.529(d)(4)(i)(B) and (C)) that are also used to calculate payments under the SSO policy at § 412.529(c)(4) and site neutral payment rate payments at § 412.522(c).
Comment: Several commenters supported our proposed methodology for calculating the adjusted payment amount. Some commenters requested clarification that the payment adjustment would be the full amount calculated under § 412.529(d)(4)(i)(A), not the per diem amount.
Response: The commenters are correct that the adjusted payment would be the full amount, not the per diem. As noted in the proposed rule and in this final rule stated, the IPPS comparable per diem amount is calculated in accordance with the provisions of §§ 412.529(d)(4)(i)(B) and (C), and our proposed codification of our proposed policy at new § 412.522(d)(4) does not incorporate the provisions of §§ 412.529(d)(4)(i)(B) and (C). In the interests of providing clarity, we are revising our proposed regulation text in response to these comments. In order to distinguish the amount paid under this adjustment from the IPPS comparable per diem amount (used for site neutral payment rate payments and SSO payments), rather than referring to payments under the adjustment as made at “an amount comparable” to the IPPS amount we are finalizing regulations which will refer to the amount paid under this adjustment to “an amount equivalent” to the IPPS amount. We believe this change will prevent any possible confusion of the regulations or any incorrect application of a per diem payment under this adjustment.
Additionally, in light of this comment, we carefully reviewed the proposed regulations text to ensure clarity. It stated that the payment amount for discharges subject to this adjustment is determined under §§ 412.529(d)(4)(i)(A) and (ii). The calculation defined at § 412.529(d)(4)(i)(A) is the calculation of the full IPPS comparable amount, not the per diem (the calculation of the per diem is calculated in § 412.529(d)(4)(i)(B)). As stated in § 412.529(d)(4)(i)(A), the calculation is based on the sum of the applicable operating IPPS standardized amount and the capital IPPS Federal rate in effect at the time of the LTCH discharge. Subclause (ii) of § 412.529(d)(4) sets forth the IPPS operating standardized amount component of the calculation at § 412.529(d)(4)(i)(A), and the IPPS capital Federal rate component of the calculation referenced at § 412.529(d)(4)(i)(A) is set forth at subclause (iii) of § 412.529(d)(4). Having provided a citation to one portion of the cited variables found in § 412.529(d)(4)(i)(A), that is, § 412.529(d)(4)(i)(A)(ii), we should have provided the other, § 412.529(d)(4)(i)(A)(iii), or omitted both and simply relied upon § 412.529(d)(4)(i)(A). As we believe it is clearer to cite to both (ii) and (iii) as well as § 412.529(d)(4)(i)(A), we are adding the citation to the IPPS capital Federal rate component at § 412.529(d)(4)(iii). Therefore, in the interest of clarity, we are including the specific citation to § 412.529(d)(4)(iii) in addition to the proposed citations to § 412.529(d)(4)(i)(A) and (ii). Accordingly, under this payment adjustment at new § 412.522(d)(4), an LTCH will receive payment at the amount equivalent to the IPPS amount determined under §§ 412.529(d)(4)(i)(A), (ii) and (iii), with an additional payment for high cost outlier cases based on the IPPS fixed-loss amount in effect at the time of the LTCH discharge.
While we did not receive any comments specifically related to our proposal to include a payment for high cost outlier cases based on the IPPS fixed-loss amount in the payment adjustment set forth at new § 412.522(d)(4), we are taking this opportunity to clarify that the outlier payment included as part of the calculation under this adjustment differs from our policy for making LTCH PPS outlier payments for site neutral discharges. This is due to the difference in the applicable statutory language. Section 1886(m)(6)(c)(ii)(II) of the Act states the adjusted payment for failing to maintain the requisite discharge payment percentage shall be the amount that “would apply under subsection (d) for the discharge if the hospital were a subsection (d) hospital.” To effectuate this statutory direction, we proposed to use the unadjusted IPPS comparable amount including an amount that would account for any high cost outliers payment which would have been paid to an IPPS hospital for the discharge (that is the amount of outlier payment would be determined based on the IPPS HCO threshold and fixed-loss amount) since high cost outlier payments are provided for under subparagraph (5)(A)(ii) of “subsection (d)”.
Furthermore, while this amount is the same as fixed-loss amount used to determine LTCH PPS outlier payments for the site neutral payment rate for FY 2020 (as discussed in section V.D.4. of the Addendum of this final rule), this may not be the case in the future. As we discussed in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49617), we have stated that when we have sufficiently stable data for site neutral payment rate cases, we intend to calculate an HCO threshold and fixed-loss amount specifically for site neutral discharges rather than continue to use the IPPS HCO threshold and fixed loss amount. At that time, the outlier payment included as part of the calculation under the payment adjustment applied to discharges under this section will continue to use the IPPS HCO threshold and fixed loss amounts because those would determine the payment for a discharge from a subsection (d) hospital. The provisions for payment for site neutral discharges at section 1886(m)(6)(b) of the Act instruct CMS to use the IPPS comparable per diem amount and outliers. CMS' longstanding policy (of which Congress was aware when the site neutral payment rate was enacted) is that high cost outlier payments under a particular prospective payment system are made in a budget neutral manner within that system. This is done through the application of a budget neutrality adjustment to payments in the system. The statutory language that directs adjustment of the payments to hospitals which do not maintain the requisite discharge payment percentage instructs payment equivalent to the amount that would be paid to a subsection (d) hospital.
Comment: Some commenters requested confirmation that the adjustment would be appealable to the PRRB.
Response: These payment adjustments would constitute final agency action which is appealable to the PRRB, assuming all other applicable appeal requirements are met.
After consideration of the comments we received, for the reasons previously discussed, we are finalizing our proposed codification at new § 412.522(d)(4)(i)(A) and (ii) with a modification to add a citation to § 412.529(d)(4)(iii) for the reasons described above, and the substitution of the word “equivalent” for the word “comparable” in the interests of providing clarity in response to commenter's concerns regarding the possibility of the creation of confusion with the IPPS comparable per diem amount.
D. Changes to the LTCH PPS Payment Rates and Other Changes to the LTCH PPS for FY 2020
1. Overview of Development of the LTCH PPS Standard Federal Payment Rates
The basic methodology for determining LTCH PPS standard Federal payment rates is currently set forth at 42 CFR 412.515 through 412.533 and 412.535. In this section, we discuss the factors that we proposed to use to update the LTCH PPS standard Federal payment rate for FY 2020, that is, effective for LTCH discharges occurring on or after October 1, 2019 through September 30, 2020. Under the dual rate LTCH PPS payment structure required by statute, beginning with discharges in cost reporting periods beginning in FY 2016, only LTCH discharges that meet the criteria for exclusion from the site neutral payment rate are paid based on the LTCH PPS standard Federal payment rate specified at § 412.523. (For additional details on our finalized policies related to the dual rate LTCH PPS payment structure required by statute, we refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49601 through 49623).)
Prior to the implementation of the dual payment rate system in FY 2016, all LTCH discharges were paid similarly to those now exempt from the site neutral payment rate. That legacy payment rate was called the standard Federal rate. For details on the development of the initial standard Federal rate for FY 2003, we refer readers to the August 30, 2002 LTCH PPS final rule (67 FR 56027 through 56037). For subsequent updates to the standard Federal rate (FYs 2003 through 2015)/LTCH PPS standard Federal payment rate (FY 2016 through present) as implemented under § 412.523(c)(3), we refer readers to the following final rules: RY 2004 LTCH PPS final rule (68 FR 34134 through 34140); RY 2005 LTCH PPS final rule (69 FR 25682 through 25684); RY 2006 LTCH PPS final rule (70 FR 24179 through 24180); RY 2007 LTCH PPS final rule (71 FR 27819 through 27827); RY 2008 LTCH PPS final rule (72 FR 26870 through 27029); RY 2009 LTCH PPS final rule (73 FR 26800 through 26804); FY 2010 IPPS/RY 2010 LTCH PPS final rule (74 FR 44021 through 44030); FY 2011 IPPS/LTCH PPS final rule (75 FR 50443 through 50444); FY 2012 IPPS/LTCH PPS final rule (76 FR 51769 through 51773); FY 2013 IPPS/LTCH PPS final rule (77 FR 53479 through 53481); FY 2014 IPPS/LTCH PPS final rule (78 FR 50760 through 50765); FY 2015 IPPS/LTCH PPS final rule (79 FR 50176 through 50180); FY 2016 IPPS/LTCH PPS final rule (80 FR 49634 through 49637); FY 2017 IPPS/LTCH PPS final rule (81 FR 57296 through 57310); the FY 2018 IPPS/LTCH PPS final rule (82 FR 58536 through 58547); and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41530 through 41537).
In this FY 2020 IPPS/LTCH PPS final rule, we present our policies related to the annual update to the LTCH PPS standard Federal payment rate for FY 2020.
The update to the LTCH PPS standard Federal payment rate for FY 2020 is presented in section V.A. of the Addendum to this final rule. The components of the annual update to the LTCH PPS standard Federal payment rate for FY 2020 are discussed in this rule, including the statutory reduction to the annual update for LTCHs that fail to submit quality reporting data for FY 2020 as required by the statute (as discussed in section VII.D.2.c. of the preamble of this final rule). As we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19471), we also made an adjustment to the LTCH PPS standard Federal payment rate to account for the estimated effect of the changes to the area wage level for FY 2020 on estimated aggregate LTCH PPS payments, in accordance with § 412.523(d)(4) (as discussed in section V.B. of the Addendum to this final rule).
In addition, as discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41532 through 41537), we eliminated the 25-percent threshold policy in a budget neutral manner. The budget neutrality requirements are codified in the regulations at § 412.523(d)(6). Under these regulations, a temporary, one-time factor is applied to the standard Federal payment rate in FY 2019 and FY 2020, and a permanent, one-time factor in FY 2021. These factors as established in the correction to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41536) are—
- For FY 2019, a temporary, one-time factor of 0.990878;
- For FY 2020, a temporary, one-time factor of 0.990737; and
- For FY 2021 and subsequent years, a permanent, one-time factor of 0.991249.
Therefore, in determining the FY 2020 LTCH PPS standard Federal payment rate, as we proposed, we—
- Removed the temporary, one-time factor of 0.990878 for the estimated cost of the elimination of the 25-percent threshold policy in FY 2019 by applying a factor of (1/0.990878); and
- Applied a temporary, one-time factor of 0.990737 for the estimated cost of the elimination of the 25-percent threshold policy in FY 2020.
Equivalently, in determining the FY 2020 LTCH PPS standard Federal payment rate, as we proposed, we applied a temporary, one-time factor of 0.999858 (1/0.990878 × 0.990737) to the FY 2019 LTCH PPS standard Federal payment rate. The FY 2020 LTCH PPS standard Federal payment rate shown in Table 1E in section VI. of the Addendum to this final rule reflects this adjustment.
2. FY 2020 LTCH PPS Standard Federal Payment Rate Annual Market Basket Update
a. Overview
Historically, the Medicare program has used a market basket to account for input price increases in the services furnished by providers. The market basket used for the LTCH PPS includes both operating and capital related costs of LTCHs because the LTCH PPS uses a single payment rate for both operating and capital-related costs. We adopted the 2013-based LTCH market basket for use under the LTCH PPS beginning in FY 2017 (81 FR 57100 through 57102). For additional details on the historical development of the market basket used under the LTCH PPS, we refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53467 through 53476), and for a complete discussion of the LTCH market basket and a description of the methodologies used to determine the operating and capital-related portions of the 2013-based LTCH market basket, we refer readers to section VII.D. of the preamble of the FY 2017 IPPS/LTCH PPS proposed and final rules (81 FR 25153 through 25167 and 81 FR 57086 through 57099, respectively).
Section 3401(c) of the Affordable Care Act provides for certain adjustments to any annual update to the LTCH PPS standard Federal payment rate and refers to the timeframes associated with such adjustments as a “rate year.” We note that, because the annual update to the LTCH PPS policies, rates, and factors now occurs on October 1, we adopted the term “fiscal year” (FY) rather than “rate year” (RY) under the LTCH PPS beginning October 1, 2010, to conform with the standard definition of the Federal fiscal year (October 1 through September 30) used by other PPSs, such as the IPPS (75 FR 50396 through 50397). Although the language of sections 3004(a), 3401(c), 10319, and 1105(b) of the Affordable Care Act refers to years 2010 and thereafter under the LTCH PPS as “rate year,” consistent with our change in the terminology used under the LTCH PPS from “rate year” to “fiscal year,” for purposes of clarity, when discussing the annual update for the LTCH PPS standard Federal payment rate, including the provisions of the Affordable Care Act, we use “fiscal year” rather than “rate year” for 2011 and subsequent years.
b. Annual Update to the LTCH PPS Standard Federal Payment Rate for FY 2020
CMS has used an estimated market basket increase to update the LTCH PPS. As previously noted, we adopted the 2013-based LTCH market basket for use under the LTCH PPS beginning in FY 2017. The 2013-based LTCH market basket is based solely on the Medicare cost report data submitted by LTCHs and, therefore, specifically reflects the cost structures of only LTCHs. (For additional details on the development of the 2013-based LTCH market basket, we refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 57085 through 57099).) We continue to believe that the 2013-based LTCH market basket appropriately reflects the cost structure of LTCHs for the reasons discussed when we adopted its use in the FY 2017 IPPS/LTCH PPS final rule (81 FR 57100). Therefore, in this final rule, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19472-19473), we used the 2013-based LTCH market basket to update the LTCH PPS standard Federal payment rate for FY 2020.
Section 1886(m)(3)(A) of the Act provides that, beginning in FY 2010, any annual update to the LTCH PPS standard Federal payment rate is reduced by the adjustments specified in clauses (i) and (ii) of subparagraph (A). Clause (i) of section 1886(m)(3)(A) of the Act provides for a reduction, for FY 2012 and each subsequent rate year, by the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act (that is, “the multifactor productivity (MFP) adjustment”). Clause (ii) of section 1886(m)(3)(A) of the Act provided for a reduction, for each of FYs 2010 through 2019, by the “other adjustment” described in section 1886(m)(4)(F) of the Act; therefore, it is not applicable for FY 2020.
Section 1886(m)(3)(B) of the Act provides that the application of paragraph (3) of section 1886(m) of the Act may result in the annual update being less than zero for a rate year, and may result in payment rates for a rate year being less than such payment rates for the preceding rate year.
c. Adjustment to the LTCH PPS Standard Federal Payment Rate Under the Long-Term Care Hospital Quality Reporting Program (LTCH QRP)
In accordance with section 1886(m)(5) of the Act, the Secretary established the Long-Term Care Hospital Quality Reporting Program (LTCH QRP). The reduction in the annual update to the LTCH PPS standard Federal payment rate for failure to report quality data under the LTCH QRP for FY 2014 and subsequent fiscal years is codified under 42 CFR 412.523(c)(4). The LTCH QRP, as required for FY 2014 and subsequent fiscal years by section 1886(m)(5)(A)(i) of the Act, applies a 2.0 percentage point reduction to any update under § 412.523(c)(3) for an LTCH that does not submit quality reporting data to the Secretary in accordance with section 1886(m)(5)(C) of the Act with respect to such a year (that is, in the form and manner and at the time specified by the Secretary under the LTCH QRP) (§ 412.523(c)(4)(i)). Section 1886(m)(5)(A)(ii) of the Act provides that the application of the 2.0 percentage points reduction may result in an annual update that is less than 0.0 for a year, and may result in LTCH PPS payment rates for a year being less than such LTCH PPS payment rates for the preceding year. Furthermore, section 1886(m)(5)(B) of the Act specifies that the 2.0 percentage points reduction is applied in a noncumulative manner, such that any reduction made under section 1886(m)(5)(A) of the Act shall apply only with respect to the year involved, and shall not be taken into account in computing the LTCH PPS payment amount for a subsequent year. These requirements are codified in the regulations at § 412.523(c)(4). (For additional information on the history of the LTCH QRP, including the statutory authority and the selected measures, we refer readers to section VIII.C. of the preamble of this final rule.)
d. Annual Market Basket Update Under the LTCH PPS for FY 2020
Consistent with our historical practice and our proposal, we estimate the market basket increase and the MFP adjustment based on IGI's forecast using the most recent available data. Based on IGI's second quarter 2019 forecast, the FY 2020 full market basket estimate for the LTCH PPS using the 2013-based LTCH market basket is 2.9 percent. The current estimate of the MFP adjustment for FY 2020 based on IGI's second quarter 2019 forecast is 0.4 percent.
For FY 2020, section 1886(m)(3)(A)(i) of the Act requires that any annual update to the LTCH PPS standard Federal payment rate be reduced by the productivity adjustment (“the MFP adjustment”) described in section 1886(b)(3)(B)(xi)(II) of the Act. Consistent with the statute, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule, we are reducing the full estimated FY 2020 market basket increase by the FY 2020 MFP adjustment. To determine the market basket increase for LTCHs for FY 2020, as reduced by the MFP adjustment, consistent with our established methodology, we subtracted the FY 2020 MFP adjustment from the estimated FY 2020 market basket increase. (We note that sections 1886(m)(3)(A)(ii) and 1886(m)(4)(F) of the Act required an additional reduction each year only for FYs 2010 through 2019.) (For additional details on our established methodology for adjusting the market basket increase by the MFP adjustment, we refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51771).)
For FY 2020, section 1886(m)(5) of the Act requires that, for LTCHs that do not submit quality reporting data as required under the LTCH QRP, any annual update to an LTCH PPS standard Federal payment rate, after application of the adjustments required by section 1886(m)(3) of the Act, shall be further reduced by 2.0 percentage points. Therefore, for LTCHs that fail to submit quality reporting data under the LTCH QRP, the 2.9 percent update to the LTCH PPS standard Federal payment rate for FY 2020 is reduced by the 0.4 percentage point MFP adjustment as required under section 1886(m)(3)(A)(i) of the Act and the additional 2.0 percentage points reduction required by section 1886(m)(5) of the Act.
In this FY 2020 IPPS/LTCH PPS final rule, in accordance with the statute, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule, we reduced the FY 2020 full market basket estimate of 2.9 percent (based on IGI's second quarter 2019 forecast of the 2013-based LTCH market basket) by the FY 2020 MFP adjustment of 0.4 percentage point (based on IGI's second quarter 2019 forecast). Therefore, under the authority of section 123 of the BBRA as amended by section 307(b) of the BIPA, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule, we are establishing an annual market basket update to the LTCH PPS standard Federal payment rate for FY 2020 of 2.5 percent (that is, the most recent estimate of the LTCH PPS market basket increase of 2.9 percent less the MFP adjustment of 0.4 percentage point). Accordingly, as we proposed, we are revising § 412.523(c)(3) by adding a new paragraph (xvi), which will specify that the LTCH PPS standard Federal payment rate for FY 2020 is the LTCH PPS standard Federal payment rate for the previous LTCH PPS payment year updated by 2.5 percent, and as further adjusted, as appropriate, as described in § 412.523(d) (including the application of the adjustment factor for the cost of the elimination of the 25-percent threshold policy under § 412.523(d)(6) as previously discussed). For LTCHs that fail to submit quality reporting data under the LTCH QRP, under § 412.523(c)(3)(xvi) in conjunction with § 412.523(c)(4), as we proposed, we further reduced the annual update to the LTCH PPS standard Federal payment rate by 2.0 percentage points, in accordance with section 1886(m)(5) of the Act. Accordingly, as we proposed, we are establishing an annual update to the LTCH PPS standard Federal payment rate of 0.5 percent (that is, 2.5 percent minus 2.0 percentage points) for FY 2020 for LTCHs that fail to submit quality reporting data as required under the LTCH QRP. Consistent with our historical practice, as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19473), we used a more recent estimate of the market basket and the MFP adjustment in this final rule to establish an annual update to the LTCH PPS standard Federal payment rate for FY 2020 under § 412.523(c)(3)(xvi). (We note that, consistent with historical practice, as we also proposed, we adjusted the FY 2020 LTCH PPS standard Federal payment rate by an area wage level budget neutrality factor in accordance with § 412.523(d)(4) (as discussed in section V.B.5. of the Addendum to this final rule).)
VIII. Quality Data Reporting Requirements for Specific Providers and Suppliers
In section VIII. of the preamble of the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19473 through 19554), we proposed changes to the following Medicare quality reporting systems:
- In section VIII.A., the Hospital IQR Program;
- In section VIII.B., the PCHQR Program; and
- In section VIII.C., the LTCH QRP.
In addition, in section VIII.D. of the preamble of that proposed rule (84 FR 19554 through 19569), we proposed changes to the Medicare and Medicaid Promoting Interoperability Programs (previously known as the Medicare and Medicaid EHR Incentive Programs) for eligible hospitals and critical access hospitals (CAHs).
A. Hospital Inpatient Quality Reporting (IQR) Program
1. Background
a. History of the Hospital IQR Program
The Hospital IQR Program strives to put patients first by ensuring they are empowered to make decisions about their own healthcare along with their clinicians using information from data-driven insights that are increasingly aligned with meaningful quality measures. We support technology that reduces burden and allows clinicians to focus on providing high quality health care for their patients. We also support innovative approaches to improve quality, accessibility, and affordability of care, while paying particular attention to improving clinicians' and beneficiaries' experiences when interacting with CMS programs. In combination with other efforts across the Department of Health and Human Services, we believe the Hospital IQR Program incentivizes hospitals to improve health care quality and value, while giving patients the tools and information needed to make the best decisions for them.
We seek to promote higher quality and more efficient health care for Medicare beneficiaries. This effort is supported by the adoption of widely-agreed upon quality and cost measures. We have worked with relevant stakeholders to define measures in almost every care setting and currently measure some aspect of care for almost all Medicare beneficiaries. These measures assess clinical processes, patient safety and adverse events, patient experiences with care, care coordination, and clinical outcomes, as well as cost of care. We have implemented quality measure reporting programs for multiple settings of care. To measure the quality of hospital inpatient services, we implemented the Hospital IQR Program, previously referred to as the Reporting Hospital Quality Data for Annual Payment Update (RHQDAPU) Program.
We refer readers to the FY 2010 IPPS/LTCH PPS final rule (74 FR 43860 through 43861) and the FY 2011 IPPS/LTCH PPS final rule (75 FR 50180 through 50181) for detailed discussions of the history of the Hospital IQR Program, including the statutory history, and to the FY 2015 IPPS/LTCH PPS final rule (79 FR 50217 through 50249), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49660 through 49692), the FY 2017 IPPS/LTCH PPS final rule (81 FR 57148 through 57150), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38326 through 38328 and 82 FR 38348), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41538 through 41609) for the measures we have previously adopted for the Hospital IQR Program measure set for the FY 2022 payment determination and subsequent years.
b. Maintenance of Technical Specifications for Quality Measures
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41538) in which we summarized how the Hospital IQR Program maintains the technical measure specifications for quality measures and the subregulatory process for incorporation of nonsubstantive updates to the measure specifications to ensure that measures remain up-to-date. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19473), we did not propose any changes to these policies.
c. Public Display of Quality Measures
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41538 through 41539) in which we stated the Hospital IQR Program's policy for public display of quality measures. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19473), we did not propose any changes to these policies.
2. Retention of Previously Adopted Hospital IQR Program Measures for Subsequent Payment Determinations
We refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53512 through 53513) for our finalized measure retention policy. Pursuant to this policy, when we adopt measures for the Hospital IQR Program beginning with a particular payment determination, we automatically readopt these measures for all subsequent payment determinations unless we propose to remove, suspend, or replace the measures. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19473), we did not propose any changes to this policy.
3. Removal Factors for Hospital IQR Program Measures
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41540 through 41544) for a summary of the Hospital IQR Program's removal factors. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19473 through 19474), we did not propose any changes to our policies regarding measure removal.
4. Considerations in Expanding and Updating Quality Measures
We refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53510 through 53512) for a discussion of the previous considerations we have used to expand and update quality measures under the Hospital IQR Program. We also refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41147 through 41148), in which we describe the Meaningful Measures Initiative,[335] our objectives under this new framework for quality measurement, and the quality topics that we have identified as high impact measurement areas that are relevant and meaningful to both patients and providers. Furthermore, in selecting measures for the Hospital IQR Program, we are mindful that measures adopted for the Hospital VBP Program must first have been adopted under the Hospital IQR Program and publicly reported on the Hospital Compare website for at least 1 year. We view the value-based purchasing programs, including the Hospital VBP Program, as the next step in promoting higher quality care for Medicare beneficiaries by transforming Medicare from a passive payer of claims into an active purchaser of quality health care for its beneficiaries. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19474), we did not propose any changes to these policies.
5. New Measures for the Hospital IQR Program Measure Set
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19474 through 19485), we proposed to: (1) Adopt two new quality measures beginning with the FY 2023 payment determination; and (2) expand the voluntary reporting status of the Hybrid Hospital-Wide Readmission Measure with Claims and Electronic Health Record Data (Hybrid HWR measure), and then require mandatory reporting of this measure beginning with the FY 2026 payment determination, as discussed in detail in this rule.
a. Adoption of Two Opioid-Related eCQMs
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19474 through 19480), we proposed to add the following two opioid-related electronic clinical quality measures (eCQMs) to the Hospital IQR Program eCQM measure set, beginning with the CY 2021 reporting period/FY 2023 payment determination: (1) Safe Use of Opioids—Concurrent Prescribing eCQM; and (2) Hospital Harm—Opioid-Related Adverse Events eCQM.
We believe these opioid-related measures are valuable patient safety measures and are responsive to stakeholder feedback expressing support for eCQMs that focus on higher priority measurement areas and patient outcomes. While both measures are designed to reduce adverse events or harms associated with opioid use, the main focus of each measure's intent is different.
The Safe Use of Opioids—Concurrent Prescribing eCQM focuses on concurrent prescriptions of opioids and benzodiazepines at discharge, an area of high-risk prescribing. Implementation of the measure has the potential to reduce preventable mortality and costs of adverse events associated with prescription opioid use and could contribute to efforts to combat the current opioid epidemic, which is a high-priority focus area for measurement.
The Hospital Harm—Opioid-Related Adverse Events eCQM is designed to reduce adverse events associated with the administration of opioids in the hospital setting by assessing the administration of naloxone as an indicator of harm. Implementation of the measure can lead to safer patient care by incentivizing hospitals to track and improve their monitoring of patients who receive opioids during hospitalization.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19474), we stated that adopting these two opioid-related eCQMs would further diversify the eCQM measure set by addressing two additional Meaningful Measures quality priorities that are not currently addressed by the eCQM measure set: “Promoting Effective Prevention and Treatment of Chronic Disease” and “Making Care Safer by Reducing Harm Caused in the Delivery of Care” through the Meaningful Measures Areas of “Prevention and Treatment of Opioid and Substance Use Disorders” and “Preventable Healthcare Harm,” respectively.
Additional details on each of the opioid-related eCQMs are presented in this final rule. We also refer readers to two related proposals discussed in this final rule: (1) Section VIII.A.10.d.(1) through (4) of the preamble of this final rule where we discuss our proposed reporting and submission requirements for eCQMs through the CY 2022 reporting period/FY 2024 payment determination, including a discussion of our proposal to require hospitals to report on the Safe Use of Opioids—Concurrent Prescribing eCQM as one of the four required eCQMs beginning with the CY 2022 reporting period/FY 2024 payment determination; and (2) section VIII.D.6.a. and b. of the preamble of this final rule for a discussion of similar proposals to adopt these two opioid-related eCQMs in the Medicare and Medicaid Promoting Interoperability Programs (previously known as the Medicare and Medicaid EHR Incentive Programs).
(1) Safe Use of Opioids—Concurrent Prescribing eCQM
(a) Background
Fatalities from unintentional opioid overdose have become an epidemic in the last 20 years, representing a major public health concern in the United States.[336] According to the Centers for Disease Control and Prevention (CDC), opioid overdose resulted in more than 42,000 deaths in 2016, and 40 percent of those deaths involved prescription opioids.[337] In addition, a recent retrospective study of claims data found that concurrent benzodiazepine and opioid use increased by 80 percent between 2001 and 2013 in a large sample of privately insured patients, and significantly contributed to the overall population risk of opioid overdose in the United States.[338]
Concurrent prescriptions of opioids or opioids and benzodiazepines place patients at a greater risk of unintentional overdose due to the increased risk of respiratory depression.[339] According to the National Institute on Drug Abuse, concurrent use of benzodiazepines with opioids was present in more than 30 percent of fatal overdoses, but many people continue to be prescribed both drugs simultaneously.[340 341] Rates of fatal overdose are 10 times higher in patients who are co-dispensed opioid analgesics and benzodiazepines versus opioids alone.[342] Studies of multiple claims and prescription databases show that 5 to 15 percent of patients receive concurrent opioid prescriptions, and 5 to 20 percent of patients receive concurrent opioid and benzodiazepine prescriptions across various settings.[343 344 345] On average, the number of opioid overdose deaths involving benzodiazepines increased 14 percent each year from 2006 to 2011, whereas the number of opioid analgesic overdose deaths not involving benzodiazepines did not change significantly.[346] One study showed that reducing concurrent use of opioids and benzodiazepines could reduce the risk of opioid overdose-related emergency department (ED) and inpatient visits by 15 percent, and could have prevented an estimated 2,630 deaths related to opioid painkiller overdoses in 2015.[347] In the FY 2018 IPPS/LTCH PPS rulemaking (82 FR 20059 through 20060; 82 FR 38377 through 38378), we sought public comment on the potential future adoption of this measure.
(b) Overview of Measure
We believe that a measure that calculates the proportion of patients who were concurrently prescribed two or more opioids or opioids and benzodiazepines has the potential to reduce preventable mortality and the costs of adverse events associated with opioid use. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19474 through 19477), we proposed to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination.
The Safe Use of Opioids—Concurrent Prescribing eCQM seeks to reduce preventable mortality and the costs of adverse events associated with opioid use by encouraging providers to identify patients who have concurrent prescriptions for opioids or opioids and benzodiazepines, and discouraging providers from prescribing these drugs concurrently whenever possible. The goal of the measure is to provide a patient-centric measure to help systems identify and monitor patients at risk, and ultimately reduce the risk of harm to patients across the continuum of care. This measure also seeks to help combat the opioid crisis, which has been declared a public health emergency,[348] and is recognized as a priority focus area for measurement by CMS and HHS. Specifically, by collecting and reporting concurrent prescribing rates with minimal lag time, this measure advances one of the key strategies prioritized by HHS in its five-point Opioid Strategy, which is to improve our understanding of the crisis through more timely, specific public health data collection and reporting.[349] In addition, under CMS' Meaningful Measures framework, the Safe Use of Opioids—Concurrent Prescribing eCQM addresses the quality priority of “Promoting Effective Prevention and Treatment of Chronic Disease” through the Meaningful Measures Area of “Prevention and Treatment of Opioid and Substance Use Disorders.” [350]
The measure's concept is based on the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain, which recommends that clinicians should avoid prescribing opioids and benzodiazepines concurrently whenever possible.[351] It is also in line with many state-issued and professional society guidelines on concurrent prescribing, which recommend that providers should avoid prescribing multiple opioids and opioids and benzodiazepines concurrently because it puts patients at high risk for respiratory depression, overdose, and death.[352]
In addition, stakeholders involved during development, including the project TEP and public commenters, stated that the measure was useful not only because it could promote adherence to recommended clinical guidelines, but also because capturing data on hospital-level prescribing practices could assist in identifying strategies to address the issue of concurrent prescriptions of opioids and benzodiazepines. Stakeholders also stated that the measure could reduce opioid-related mortality resulting from concurrent opioid prescriptions or opioid-benzodiazepine prescriptions, with minimal implementation costs.[353] Measure testing demonstrated that almost all of the data elements required to calculate and report the measure are collected as part of required clinical workflow protocols in structured fields within the EHR. We note that the NQF Patient Safety Standing Committee did not raise any concerns on the feasibility of the measure during endorsement review. In this final rule, we are clarifying that the Safe Use of Opioids—Concurrent Prescribing eCQM was developed with broader specifications and flexibility in mind. Specifically, the measure, as initially developed, captured both encounters from the hospital outpatient and inpatient settings so that it could be implemented in either setting, with program implementation in either the Hospital Outpatient Quality Reporting (OQR) Program and/or the Hospital IQR Program to be determined at a later date.
We are also clarifying here in the final rule that the measure was included in the publicly available “List of Measures Under Consideration for December 1, 2016” for both the Hospital OQR and Hospital IQR Programs,[354] and considered by the MAP for potential inclusion in both programs in December 2016 and January 2017, which recommended that the measure be refined and resubmitted prior to rulemaking due to the importance of the opioid epidemic.[355] The MAP noted that there are instances where concurrent prescribing may be clinically appropriate, and that the measure could potentially cause unintentional consequences associated with withdrawal of medications if previously prescribed opioids and/or benzodiazepines are reduced or stopped prior to discharge. For more information on the concerns and considerations raised by the MAP related to this measure, we refer readers to the January 2017 NQF MAP Coordinating Committee Meeting Transcript.[356]
In response to the MAP's recommendation, and as suggested by the project's TEP and expert work group, we explored instances where concurrent prescribing may be clinically appropriate and assessed the impact of adding single-condition exclusions, specifically for patients with sickle cell disease and those receiving pharmacotherapy for an opioid use disorder. We found that these instances comprised a very small portion of eligible cases captured by the numerator during testing. After reviewing these testing results, clinicians from our expert work group recommended continuing to include patients for whom concurrent prescribing may be clinically necessary because these populations are at highest risk of adverse drug events due to concurrent prescriptions and should continue to be monitored by clinicians throughout the continuum of care. In addition, there are currently no guidelines supporting exclusion of patients who may require concurrent prescriptions from the measure, other than cancer and palliative care; a broader set of evidence-based exclusions may increase the face validity of the measure, but there are currently no strong evidence-based indicators to support other exclusions beyond what is currently included in the measure that would continue to maintain the strength of the measure's evidence base.
In addition, to address the MAP's feedback regarding the measure's feasibility and usability, in May 2017 we refined the measure to: (1) Include only encounters for inpatient, ED, and hospital observation stays (rather than including encounters spanning inpatient and hospital outpatient settings); and (2) include only medications prescribed at discharge (rather than those spanning the duration of the encounter) (84 FR 19476). In this final rule, we are elaborating on those refinements to provide additional clarity as there seemed to be some confusion from commenters. These refinements were made to address feedback from the MAP concerning the evidence for measuring concurrent prescribing across other hospital settings, such as outpatient departments, as the available evidence primarily focused on the ED and inpatient settings, as well as feasibility and usability concerns around capturing medications active on admission and during the care encounter which may be modified at discharge. For the MAP review that occurred in December 2016 and January 2017, the measure denominator included: (a) Encounters for inpatient stays less than or equal to 120 days, ED, or outpatient stays, and (b) medications prescribed spanning the duration of the encounter. After the MAP's review, we refined the measure to limit: (a) non-ED hospital outpatient encounters to observation stays, and (b) the medications prescribed to only those prescribed at discharge.
The refined measure was submitted to the NQF in late 2017. In this final rule, we are clarifying that when the measure was submitted for endorsement consideration, the testing and analysis data (for example, performance rates, reliability assessment) were separately presented by the hospital inpatient and hospital outpatient (ED and observation) settings.[357] The Patient Safety Standing Committee specifically reviewed the measure testing results for both the inpatient and outpatient settings separately.[358] As a result, the Patient Safety Standing Committee evaluated the measure with data presented for both settings and recommended the measure for endorsement in April 2018, acknowledging that there is strong evidence for an association between increased use of multiple opioids, or opioids and benzodiazepines together, as well as increased risk of unintentional and fatal overdoses.[359] The committee agreed that this measure will likely reduce concurrent prescribing of opioid-opioid and opioid-benzodiazepine medications at discharge in inpatient and ED settings.[360] This measure was endorsed by the NQF in May 2018.[361] On November 8, 2018, we shared with the MAP an update on the progress of the Safe Use of Opioids—Concurrent Prescribing measure since their review in December 2016 and January 2017, as the measure had been refined and became endorsed.[362]
Concurrent opioid or opioid-benzodiazepine prescription use contributes significantly to the overall population's risk of opioid overdose. Currently, however, no measure exists to assess nationwide rates of the concurrent prescribing of opioids and benzodiazepines at the hospital-level.[363] Adopting the Safe Use of Opioids—Concurrent Prescribing eCQM would thus enhance the information available to providers in this area of high-risk prescribing. In addition, we believe the measure is a valuable patient safety measure that has the potential to reduce preventable mortality and other adverse events associated with prescription opioid use, with minimal implementation costs.
The measure is intended to facilitate safer patient care not only by promoting adherence to recommended clinical guidelines on concurrent prescribing practices, but also by incentivizing hospitals to develop strategies to identify and monitor patients on concurrent opioids and opioid-benzodiazepine prescriptions who might be at higher risk of adverse drug events. For instance, the measure could encourage hospital prescribers to use data from prescription drug-monitoring programs when assessing whether to prescribe concurrent substances. The measure could also encourage more effective communication among providers to coordinate care across hospital and ambulatory care settings. The measure could also help establish a national benchmark of opioid prescribing in hospital inpatient settings.
(c) Data Sources
The proposed measure is an eCQM that uses data collected through EHRs to determine hospital performance. Between July 2016 and July 2017, the Safe Use of Opioids—Concurrent Prescribing measure was tested at three health systems (eight hospitals in total) with two different EHR systems for reliability, validity, and feasibility based on the endorsement criteria outlined by NQF.[364] The testing showed that the measure is feasible, valid, and reliable. The measure is feasible as 96 percent of the data elements required to calculate the performance rate are: (1) Collected during routine care; (2) extractable from structured fields in the electronic health systems of test sites; and (3) likely to be accurate. The measure is valid as all data elements needed to calculate the measure had levels of agreement of 84 to 99 percent between electronically extracted and manually abstracted data elements. The measure also has a reliability coefficient of 0.99 across the three health systems' sites with two different EHR systems. This finding indicates that differences in hospital performance reflect true differences in quality, rather than measurement error or noise. For encounters where the patient had at least one active opioid or benzodiazepine prescription at discharge, measure testing also showed concurrent prescribing rates of 18.2 percent in the inpatient setting and 6.1 percent in ED settings. This aligned with the rates found in the literature. We note that NQF reviewed these data as part of their measure endorsement process and endorsed the measure in 2018.[365]
(d) Measure Calculation
While we stated in the FY 2020 IPPS/PPS LTCH proposed rule (84 FR 19475) that the Safe Use of Opioids—Concurrent Prescribing eCQM is a process measure that calculates the proportion of patients age 18 years and older prescribed two or more opioids or an opioid and benzodiazepine concurrently at discharge from a hospital-based encounter (inpatient or emergency department [ED], including observation stays), as further discussed below, in this final rule, we are clarifying that there may be occasions for which patients admitted to the emergency department or for observation stays are not ultimately admitted as inpatients; those patients would be excluded from the measure. As such, we are clarifying that the measure description to reflect that the Safe Use of Opioids—Concurrent Prescribing eCQM is a process measure that calculates the proportion of inpatient hospitalizations for patients 18 years of age and older prescribed, or continued on, two or more opioids or an opioid and benzodiazepine concurrently at discharge. An improvement in quality of care is indicated by a decrease in the measure score. We recognize that there may be some clinically appropriate situations for concurrent prescriptions of two unique opioids or an opioid and benzodiazepine. Thus, we do not expect the measure rate to be zero; rather, the goal of the measure is to help systems identify and monitor patients at risk, and ultimately, to reduce the risk of harm to patients across the continuum of care.
In the FY 2020 IPPS/PPS LTCH proposed rule (84 FR 19475), we stated that the measure's cohort includes all patients aged 18 years and older who were prescribed a new or continued opioid or a benzodiazepine at discharge from a hospital-based encounter (inpatient stay less than or equal to 120 days or ED encounters, including observation stays) that ended during the measurement period. We also stated that to reduce hospital burden, the definition of “hospital-based encounter” is aligned with that of other eCQMs in the Hospital IQR Program (84 FR 19477). In this final rule, we are elaborating on the description of the measure cohort to provide additional clarity as there seemed to be some confusion from commenters. Specifically, we would like to clarify that ED encounters, including observation stays, are only included in the measure if such encounters lead to an inpatient hospitalization for purposes of the Hospital IQR Program. We further discuss this clarification of the measure cohort in response to comments as described below.
Patients are included in the numerator if their discharge medications include two or more active opioids or an active opioid and benzodiazepine resulting in concurrent therapy at discharge from the hospital-based encounter.
As discussed above, while we stated in the FY 2020 IPPS/PPS LTCH proposed rule (84 FR 19475) that patients are included in the denominator if they were discharged from a hospital-based encounter (inpatient stay less than or equal to 120 days or ED encounters, including observation stays) during the measurement period, and their medications at discharge included a new or continued Schedule II or III opioid, or a new or continued Schedule IV benzodiazepine prescription, we would like to clarify that ED encounters, including observation stays, are only included in the measure if such encounters lead to an inpatient hospitalization for purposes of the Hospital IQR Program. Patients are excluded from the denominator if they have an active diagnosis of cancer or order for palliative care (including comfort measures, terminal care, dying care, and hospice care) during the encounter. These exclusions align with the populations excluded from the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain.
We note risk adjustment is not applicable to the Safe Use of Opioids—Concurrent Prescribing eCQM because it is a process measure. The measure addresses any difference in risk levels for patients via the current denominator exclusions as supported by the available evidence, that is, the measure excludes patients with cancer or patients receiving palliative care.
As mentioned earlier in this discussion, in the FY 2020 IPPS/PPS LTCH proposed rule (84 FR 19477), we referred readers to the measure specifications located on the NQF website for more information about the Safe Use of Opioids—Concurrent Prescribing eCQM.[366] We wish to clarify that given this measure was proposed and is being finalized under the Hospital IQR Program, we believe it is appropriate to focus on inpatient stays. As such, and as further discussed in response to comments below, in this final rule, we are providing an updated version of the measure specifications, which can be found at the eCQI Resource Center's Pre-Rulemaking Eligible Hospital/Critical Access Hospital eCQMs website, available at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
We also refer readers to section VIII.A.10.d.(1) through (4) of the preamble of this final rule where we discuss our proposed eCQM reporting and submission requirements through the CY 2022 reporting period/FY 2024 payment determination, including a discussion of our proposal that all participating hospitals report the Safe Use of Opioids—Concurrent Prescribing eCQM as one of the four required eCQMs beginning with the CY 2022 reporting period/FY 2024 payment determination. In addition, we refer readers to section VIII.D.6.a. and b. of the preamble of this final rule for a discussion of a similar proposal to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM (NQF #3316e) for the Promoting Interoperability Program beginning with the reporting period in CY 2021.
Comment: Many commenters supported adopting the Safe Use of Opioids—Concurrent Prescribing eCQM. Noting that concurrent prescribing presents a significant public health risk, many commenters supported the measure because it would promote safer prescribing practices and help focus efforts to address the opioid crisis. Some commenters supported the measure based on their belief that it would reduce the usage of unnecessary opioid prescriptions, provide valuable data about hospital prescribing practices, and help provider efforts to monitor opioid prescribing patterns. A commenter noted that the measure may serve to increase provider awareness of the overall rate of opioid use and potentially increase the use of non-opioid alternatives for pain management when appropriate. Another commenter expressed support for the measure and further noted that the measure could be incorporated into decision support tools via flags or drug warnings.
A commenter supported the measure because it aligns with the goals set forth in the National Action Plan for Adverse Drug Event Prevention (ADE Action Plan), which has identified accidental overdose or respiratory depression associated with opioid use as high-priority areas.[367]
Response: We thank commenters for their support. We agree that this measure promotes safer prescribing practices that may help efforts to combat the negative impacts of the opioid crisis.
Comment: Some commenters did not support the measure because the outpatient observation and emergency department (ED) settings are included with the inpatient setting, based on concerns that many concurrent prescriptions originate in outpatient settings. One commenter requested that CMS provide further clarification about how this measure should be appropriately applied for certain patients who are discharged from the ED. A commenter expressed their belief that it is considered poor clinical care for emergency providers to discontinue preexisting medications for patient conditions they are not managing on a day-to-day basis. A few commenters recommended implementation of the measure in the outpatient setting as a separate measure. A commenter noted that a patient's focus in the acute care setting should be on healing from the acute episode, and suggested that implementing the measure in the outpatient setting when the patient is more stable as more appropriate.
Response: We thank commenters for pointing out this discrepancy. We wish to clarify that given that this measure was proposed and is being finalized under the Hospital IQR Program, we believe it is appropriate to focus on inpatient stays. As we stated in the proposed rule, to reduce hospital burden, the definition of “hospital-based encounter” with regard to this measure is aligned with that of other eCQMs in the Hospital IQR Program (84 FR 19477). We are clarifying here that qualifying encounters for the Safe Use of Opioids—Concurrent Prescribing eCQM are consistent with other eCQMs in the Hospital IQR Program by also evaluating discharge data from inpatient hospitalizations only, including inpatient admissions that were initiated in the emergency department or in observation status followed by hospital admission. For example, the cohort for the ED-02 eCQM includes “inpatient encounters ending during the measurement period with length of stay (discharge date minus admission date) less than or equal to 120 days” (78 FR 50807).[368] This is because there may be occasions in which patients admitted to the emergency department or for observation stays are not ultimately admitted as inpatients. We agree that those patients should be excluded from the measure and this was our intent in the proposed rule; however, the technical specifications referenced in the proposed rule were overly broad and not clearly consistent with the proposal. As noted previously, the Safe Use of Opioids—Concurrent Prescribing eCQM was developed with broader specifications with flexibility in mind. Specifically, the measure, as initially developed, captured both encounters from the hospital outpatient and inpatient settings so that it could be implemented in either setting, with program implementation in either the Hospital Outpatient Quality Reporting (OQR) Program and/or the Hospital IQR Program to be determined at a later date.
To correct this inconsistency, we have adjusted the technical specifications to remove discharges from the emergency department and observation stays such that the measure unambiguously reflects discharges from inpatient hospitalizations only. We have made this minor refinement to the technical specifications to address confusion about which emergency department or observation stay encounters are included in the measure for implementation in the Hospital IQR Program, which are available here at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms. We believe this minor refinement aligns with the scope of the Hospital IQR Program and more accurately reflects the original intent of the measure as proposed—the measure will only capture data at discharge for those ED or observation stay encounters for which the patients are admitted to and ultimately discharged from the inpatient setting for purposes of the Hospital IQR Program. Moreover, we note that the definition of “hospital-based encounter” of the corrected measure specifications is now aligned with that of other eCQMs in the Hospital IQR Program by evaluating discharge data from inpatient hospitalizations only, in keeping with our stated intention when we proposed this measure (84 FR 19477). In addition, the update has simplified the measure specifications by removing a value set and a piece of logic from the original measure specifications. In this final rule, we are providing an updated version of the measure specifications narrowly tailored to the inpatient setting, which can be found at the eCQI Resource Center's Pre-Rulemaking Eligible Hospital/Critical Access Hospital eCQMs website, available at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms. Thus, we are finalizing this measure with a clarification and update to the technical specifications so that the measure is clearly applicable only to the inpatient setting for implementation into the Hospital IQR Program.
As to the commenter's concern that the emergency department is not the appropriate setting to discontinue preexisting medications for patient conditions they are not managing on a day-to-day basis—we reiterate that the goal of this measure is not to discontinue concurrent prescriptions of opioids and/or benzodiazepines that are clinically appropriate. Rather, the goal of this measure is to promote accountability and awareness of medication combinations that potentiate adverse events, help hospitals identify and monitor patients at risk, and provide valuable data about a high-risk prescribing area at discharge from inpatient hospitalizations, including care that originates in the emergency department.
Comment: A commenter recommended that the measure be implemented in other programs that encompass outpatient care, such as Accountable Care Organization (ACO) and Bundled Payments for Care Improvement (BPCI) participants.
Response: We thank commenter for their recommendation, which we will share with these programs.
Comment: Many commenters appreciated that the measure excludes patients with an active diagnosis of cancer or order for palliative care (including hospice care) during the encounter.
Response: We thank commenters for their support. The measure excludes patients with an active diagnosis of cancer or order for palliative care (including comfort measures, terminal care, dying care, and hospital care) during the encounter. These exclusions align with the populations excluded from the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain.
Comment: A commenter supported the measure and also recommended that CMS measure the degree to which orders for opioids involve the use of a Computerized Physician Order Entry (CPOE) system, noting that the checks and balances of CPOE results in safer prescriptions and that this would help measure the measurement gap area of medication errors.
Response: We thank commenter for their support. We note that providers are required to submit eCQMs using certified EHR technology (CEHRT), and that CPOE functionality is part of the 2015 Edition Base EHR definition.[369]
Comment: Some commenters welcomed the addition of the measure to the eCQM measure set and supported the measure from an implementation perspective. A commenter that was involved in feasibility testing of the measure noted that the data elements were reasonable to collect, not disruptive to clinical workflow, and did not cause undue burden. A few commenters noted that the measure used straightforward logic and would be relatively easy to implement within the EHR with discrete data sources. Many commenters noted that the data sources that the measure draws upon are the same ones that hospitals use to evaluate prescribing patterns.
Response: We thank commenters for their support. The measure was developed with implementation feasibility and ease in mind. We note that testing showed that 96 percent of the data elements required to calculate the performance rate are: (1) Collected during routine care; (2) extractable from structured fields in the electronic health systems of test sites; and (3) likely to be accurate.
Comment: A commenter who supported the measure noted that care decisions ultimately rest on the provider-patient relationship in coordination with the clinical best practices based on diagnosis.
Response: We agree with the commenter and note that the Safe Use of Opioids—Concurrent Prescribing eCQM is intended to reduce preventable mortality and adverse outcomes related to opioid use by encouraging providers to identify and be aware of patients with documentation of concurrent prescriptions and discouraging providers from concurrent prescribing whenever appropriate.
Comment: A few commenters who supported the measure recommended that CMS continue to monitor the measure to identify and address any potential unintended consequences.
Response: As with all measures, we monitor and evaluate quality measures after they are adopted and implemented into the Hospital IQR Program. We will continue engaging with stakeholders through education and outreach opportunities, which include webinars and submitted help desk questions through the ONC JIRA's eCQM issue tracker for eCQM implementation and maintenance,[370] for any feedback about potential unintended consequences.
Comment: A few commenters recommended that the measure should be limited to new prescriptions only and not renewals, or to medications initiated during and related to that encounter. A commenter noted that measuring new concurrent prescriptions would provide valuable data about hospital prescribing practices and may be a more relevant and useful indicator of hospital care than assessing continued opioid concurrent prescriptions given at discharge. A number of commenters recommended refinements to exclude patients who are already on two opioids or an opioid and a benzodiazepine prior to hospital admission. A commenter noted that such exclusions could be identified through present on admission codes.
Response: We believe it is important to monitor concurrent prescribing of opioids and/or benzodiazepines regardless of whether the prescriptions are new or existing. As previously discussed, the goal of this measure is to help hospitals identify and monitor patients at risk of an adverse event from opioid use and provide valuable data about a high-risk prescribing area. Patients at risk of an adverse event from opioid use include not only patients prescribed new concurrent prescriptions of opioids and/or benzodiazepines, but also patients on existing concurrent regimens of opioids and/or benzodiazepines identified as medications present on admission. The focus of the measure is to encourage providers to identify patients on medications combinations that could lead to adverse drug events at discharge and inform decision-making about whether reevaluation of the current medications regimen is warranted. We reiterate that the goal of this measure is not to discontinue concurrent prescriptions of opioids and/or benzodiazepines that are clinically appropriate.
Comment: Several commenters expressed concern that the measures do not evaluate the process used by hospital-based providers in reaching the decision to initially prescribe opioids, and therefore may not improve the quality of care or drive the types of changes that would impact the opioid crisis.
Response: We acknowledge commenters' concerns, but note that the Safe Use of Opioids—Concurrent Prescribing eCQM is a measure that seeks to encourage compliance with guidance from several national, state-level, and professional society guidelines and safer prescribing practices by identifying high-risk patients with concurrent regimens by measuring the proportion of patients aged 18 years and older prescribed two or more opioids or an opioid and benzodiazepine concurrently at discharge from a hospital-based encounter. By capturing denominator patients whose discharge medications included a new or continued Schedule II or III opioid, or a new or continued Schedule IV benzodiazepine prescription, and identifying numerator patients who have concurrent medication regimens at discharge from hospitalization, this measure provides a way for hospitals to identify and target interventions to patients in order to reduce risk of adverse drug events and, ultimately, the risk of harm to patients across the continuum of care. By enhancing availability of the measure's information to hospital providers, experts consulted during measure development suggested that the measure would be useful in offering organization insights into the scope of the problem and could result in process improvements such as care coordination with other providers who care for the patient, additional patient education and counselling, or consideration of alternative pain treatment, which is another important strategy in preventing adverse drug events.
Comment: Several commenters expressed concern with the measure exclusions, with a commenter stating their belief that CMS has not provided sufficient data to demonstrate that the measure will capture only those patients for whom concurrent prescribing is not appropriate. A few commenters recommended that the measure's exclusion for cancer and palliative care be expanded, with a commenter expressing concern that the measure's exclusion for palliative care does not fully capture terminally ill patients.
Several commenters recommended that the measure exclude patients with sickle cell disease. A commenter noted that the CDC recently clarified in a letter to three specialty societies that the CDC Guideline for Prescribing Opioids for Chronic Pain do not apply to patients with a diagnosis of sickle cell disease.[371]
Some commenters recommended excluding patients receiving medication for the treatment of opioid use disorder (OUD). A few commenters specifically recommended that the measure exclude patients being treated with buprenorphine or methadone for OUD, with a commenter citing guidance from the U.S. Food & Drug Administration regarding buprenorphine.[372]
Response: We recognize that there may be some clinically necessary situations for concurrent prescriptions of opioids and benzodiazepines, and we agree with the need to properly treat these patients. Regarding the commenter's concern that the measure's exclusion for palliative care does not fully capture terminally ill patients, we note that patients with an order for palliative care during the encounter are excluded from the denominator, which includes comfort measures, terminal care, dying care, and hospice care, and that these exclusions align with the populations excluded from the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain. As recommended by our expert panels, we looked into single-condition exclusions—specifically sickle cell disease and opioid use disorder, and found that a very small portion of cases eligible for the numerator (0 to 3.4 percent) fell into this category. Furthermore, after reviewing the testing results, clinicians from our expert panel recommended continuing to include patients for whom concurrent prescribing is medically necessary, because experts stated these populations: (1) Have the highest risk of receiving concurrent prescriptions; and (2) can experience a lag in adverse events. However, we will consider these comments and other suggested exclusions, such as patients on medication assisted therapy for opioid use disorder (OUD) and patients being treated with buprenorphine or methadone for OUD, when evaluating opportunities to refine the measure in the future.
Comment: A number of commenters recommended expanding the denominator exclusions to include patients with chronic pain and patients who are receiving opioids for the treatment of addiction. A commenter recommended excluding patients with advanced stages of diseases including cancer, AIDS, dementia and other incurable neurodegenerative diseases, chronic lung disease, end stage renal disease, cirrhosis, heart failure, hemophilia, or sickle cell disease. Another commenter recommended excluding patients suffering from complex poly trauma, spinal cord injury with spasticity and extensive burns. A few commenters also suggested excluding patients discharged to other healthcare facilities, such as skilled nursing facilities or hospices, as those patients have more serious disease(s) and require closer monitoring and supervision.
Response: We note that the measure currently excludes patients with an active diagnosis of cancer. Also, as previously discussed, we considered excluding patients with sickle cell disease but found that a very small portion of cases eligible for the numerator fell into this category. We recognize that there are many types of cases in which concurrent prescribing may be clinically appropriate and thus appreciate commenters' recommended exclusions. However, we wish to reiterate that we do not expect the measure rate to be zero; rather, the goal of this measure is to help hospital systems identify and monitor patients at risk, and ultimately, to reduce the risk of harm to patients across the continuum of care.
Comment: A few commenters expressed concern that the measure may show high rates of non-compliance or unfair poor performance for hospitals which disproportionately treat patients for whom concurrent prescribing is appropriate, such as patients with sickle cell disease, or practices that are highly focused on surgical interventions requiring concurrent prescriptions (such as orthopedic/neurosurgery cases). A commenter suggested that an appropriate risk adjustment methodology would incorporate factors such as cognition, functional status, and socioeconomic status, as well as standard demographic and claims-based health factors. A commenter expressed concern with the measure because it does not have clear benchmarks or target levels of performance. Another commenter recommended excluding orthopedic/neurosurgery cases entirely, or grading cases based on surgical intervention performed.
Response: The Safe Use of Opioids—Concurrent Prescribing eCQM is a process measure and therefore is not risk adjusted; rather, the target population of the measure is defined to include all patients for whom the measure is appropriate. The goal of this measure is to help hospital systems identify and monitor patients at risk, and ultimately, to reduce the risk of harm to patients across the continuum of care by providing valuable data about a high-risk prescribing area. Surgical patients and other types of patients that commenters have suggested be excluded from the measure have a high risk of receiving concurrent prescriptions, as well as an increased risk of unintentional and fatal overdose, and thus are included in the measure population. Regarding commenters' concern about high rates of non-compliance or poor performance for hospitals which disproportionately treat patients for whom concurrent prescribing is appropriate, we note that as the Hospital IQR Program is a pay-for-reporting, not a pay-for-performance, quality program, there are no financial penalties based on performance. Payment determinations are based on hospitals meeting all of the reporting requirements, not performance on the measures. As such, the Hospital IQR Program does not implement benchmarks or target levels of performance for its measures. Nor do we expect the measure rate to be zero; rather, the goal of this measure is to help hospital systems identify and monitor patients at risk, and ultimately, to reduce the risk of harm to patients across the continuum of care.
Comment: Some commenters recommended that instead of focusing on the number of concurrent prescriptions, CMS conduct further studies to evaluate different quality indicators, such as the total opioid dose prescribed quantified in morphine milligram equivalents (MME) per day.
Response: The opioid prescribing guidance developed by professional organizations, states, and federal agencies share some common elements for evaluating patient care related to opioids, including dosing thresholds, cautious titration, and risk mitigation strategies such as using risk assessment tools, treatment contracts, and urine drug testing.[373] However, there is considerable variability in the specific recommendations for the range of dosing thresholds (for example, 90 MME/day to 200 MME/day), audience (for example, primary care clinicians versus specialists) and use of evidence (for example, systematic review, grading of evidence and recommendations, and role of expert opinion).[374] CMS will take commenters' suggestions into consideration to evaluate different quality indicators, as well as continue to explore the strength of the evidence to determine whether there is a dose range that is valid and not overly burdensome to compute for potential future inclusion in an eCQM.
Comment: Many commenters did not support the measure because of potential unintended consequences, including that the measure could change clinically appropriate management practices by incentivizing providers to discontinue opioids and/or benzodiazepine in an unsafe and potentially life-threatening manner. In particular, some commenters expressed concern that such changes to a patient's established medication regimen would be conducted by physicians who do not primarily manage the patient's care, or by clinicians not familiar with dose reductions, which could endanger patient safety and lead to patient harm. A few commenters also expressed concern that the measure would incentivize such changes in an abrupt manner given the current average length of stay in the acute care setting. A commenter also noted that dedicating resources to change medication regimens might prove futile if the outpatient receiving team re-instituted the previous regimen. A few commenters noted that disincentivizing appropriate therapies to those for whom medications have been warranted may result in not only undertreatment or mistreatment of pain, but other potential adverse outcomes such as seizures, development of withdrawal syndrome, depression, and loss of function. A commenter expressed concern that patients could turn to other drugs for relief or hesitate to seek medical care due to decreased likelihood that their pain would be effectively managed as hospitals seek to reduce opioid use.
Response: We acknowledge commenters' concerns about implementation of the measure. While we recognize commenters' concerns about potential adverse outcomes—such as seizures, development of withdrawal syndrome, depression, and loss of function, as well as patients turning to other drugs for relief or hesitating to seek medical care due to decreased likelihood that their pain would be effectively managed—we note that pain management is an appropriate part of routine patient care upon which hospitals should focus, and an important concern for patients, their families, and their caregivers. Clinicians on our expert panel noted that if the prescriber believes the patient should continue concurrent opioids and benzodiazepines until further follow-up, that decision should arise in the best interest of the patient to avoid unintended consequences such as adverse outcomes. We remain confident that hospitals will continue to focus on appropriate pain management as part of their commitment to quality of care and ongoing quality improvement efforts, and it is our belief that providers will avoid inappropriate discontinuation of necessary treatment. The focus of the measure is to encourage providers to identify patients on medications combinations that could lead to adverse drug events at discharge and inform decision-making about whether reevaluation of the current medications regimen is warranted. As such, we do not believe implementation of the measure would change clinically appropriate pain management practices by incentivizing providers to discontinue opioids and/or benzodiazepine in an unsafe or abrupt and potentially life-threatening manner. However, we will monitor and evaluate the measure following implementation for any potential unintended consequences, such as the ones noted by commenters. We will also continue engaging with stakeholders through education and outreach opportunities, which include webinars and submitted help desk questions through the ONC JIRA's eCQM issue tracker for eCQM implementation and maintenance,[375] for any feedback about potential unintended consequences.
We reiterate that the Safe Use of Opioids—Concurrent Prescribing eCQM is intended to reduce preventable mortality and adverse outcomes related to opioid use by encouraging providers to identify and be aware of patients with documentation of concurrent prescriptions and discouraging providers from concurrent prescribing whenever clinically appropriate. We also recognize that there may be some clinically necessary situations for concurrent prescriptions of opioids and benzodiazepines, and we agree with the need to properly treat these patients.
Comment: Many commenters expressed concern with the measure and noted that there are valid clinical reasons for prescribing concurrent prescriptions and that concurrent prescribing is not necessarily a sign of poor management. A few commenters noted that there are situations in which the prescribing of long-term and short-term opioids are clinically appropriate.
Response: We recognize that there are many types of cases in which concurrent prescribing may be clinically appropriate and thus appreciate commenters' concerns. However, we reiterate that the measure is not expected to have a zero rate, as clinician judgment, clinical appropriateness, or both might result in concurrent prescribing of two unique opioids or an opioid and benzodiazepine that is medically necessary. Clinicians on our expert panel noted that if the prescriber believes the patient should continue concurrent opioids and benzodiazepines until further follow-up, that decision should arise in the best interest of the patient to avoid unintended consequences such as adverse outcomes. As stated above, we remain confident that hospitals will continue to focus on appropriate pain management as part of their commitment to quality of care and ongoing quality improvement efforts, and it is our belief that providers will avoid inappropriate discontinuation of clinically necessary treatment.
Regarding commenters' concerns about situations in which the prescribing of long-term and short-term opioids are clinically appropriate, we note that experts we engaged during testing agreed and recommended continuing to include patients for whom concurrent prescribing is medically necessary because experts stated that these populations (1) have the highest risk of receiving concurrent prescriptions; and (2) can experience a lag in adverse events, which is why they should be captured by the measure as the measure is intended to promote accountability and awareness for concurrent prescribing, especially in these high-risk populations. This aligns with the intent of the measure, which is to reduce preventable mortality and adverse outcomes related to opioid use by encouraging providers to identify and be aware of patients with documentation of concurrent prescriptions, as well as by discouraging providers from concurrent prescribing whenever possible.
Comment: Some commenters expressed concern with the measure due to its reliance on recommendations from the CDC's Guideline for Prescribing Opioids for Chronic Pain, noting that that the Guideline was developed to provide recommendations for primary care clinicians who prescribe opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care, and that some of the recommendations are not strongly supported by the available evidence when applied to the inpatient setting. A few commenters cited a recently published article in the New England Journal of Medicine clarifying the intent of the CDC Guideline and noted that measures that lead to patient harms through abrupt tapering or discontinuation of opioids for patients already receiving these medications are not consistent with the Guideline's recommendations.[376]
Response: The intent of this measure is to address post-discharge medication use. Thus we considered both primary care and inpatient opioid prescribing guidelines for the evidence base for this measure. The CDC guideline states that, “Although the focus [of the guideline] is on primary care clinicians, because clinicians work within team-based care, the recommendations refer to and promote integrated pain management and collaborative working relationships with other providers (for example, behavioral health providers, pharmacists, and pain management specialists)” [377] The guideline further refers readers to other sources for prescribing recommendations within acute care settings and in dental practice, including the American College of Emergency Physicians' guideline for prescribing opioids in the emergency department;[378] the American Society of Anesthesiologists' guideline for acute pain management in the perioperative setting;[379] and the Washington Agency Medical Directors' Group Interagency Guideline on Prescribing Opioids for Pain, Part II: Prescribing Opioids in the Acute and Subacute Phase.[380] The additional guidelines referenced within the CDC guideline also emphasize that the pain management regimen selected by the prescriber should reflect the individual safe application of the modality in each practice setting, which includes the ability to recognize and treat adverse effects that emerge after initiation of therapy, such as use of multiple opioids or opioids and benzodiazepines.[381 382 383] Clinicians should avoid new prescriptions of benzodiazepines and sedative-hypnotics and consider tapering or discontinuing benzodiazepines and/or sedative-hypnotics when appropriate.[384 385 386]
Comment: A few commenters did not support the measure because of their belief that there is a lack of evidence and literature on when the risks of concurrent prescribing outweigh the benefits. A commenter noted that CMS has not provided adequate evidence to demonstrate that the use of the measure would drive improvements in patient care without also potentially creating negative unintended consequences.
Response: As previously noted, opioid prescribing guidelines issued by various state agencies and professional societies for various settings (including hospital inpatient and emergency department settings) agree with the recommendation to avoid concurrently prescribing opioids and opioids and benzodiazepines whenever possible as the combination of these medications may increase the likelihood of opioid-induced respiratory depression.[387] Emerging data continue to show that concurrent prescribing of the medication in scope of the measure is a problem; specifically, that opioids and benzodiazepines are frequently used in hospitals, and measures assessing prescribing patterns and follow up interventions such as educating providers and patients about risks and alternatives can impact care,[388] and no nationwide measure of the problem at the hospital and inpatient setting currently exists. Data also show that concurrent benzodiazepine and opioid use increased by 80 percent between 2001 and 2013 in the United States and significantly contributes to the overall population risk of opioid overdose.[389] Initial measure testing demonstrated that there was no one point in the care continuum that this scenario was isolated to.[390] Providers and experts engaged during field testing considered the potential for unintended consequences and found that the benefits of the measure outweighed the risks. These providers and experts supported the patient-centric focus of the measure, advocating for the measure's potential to promote individualized care and collaboration between providers across settings. Also, during the endorsement process, the NQF Patient Safety Standing Committee agreed that this measure will likely reduce concurrent prescribing of opioid-opioid and opioid-benzodiazepine medications at discharge in inpatient and ED settings.[391]
Comment: Some commenters did not support adoption of the two opioid eCQMs until eCQMs are proven to be at least as valid and reliable as their traditional claims-based or administrative counterparts. A few commenters urged CMS to balance the usefulness of the information reported through EHRs with the challenges of extracting such data and the accuracy of the data captured before adopting the two eCQMs.
Response: We acknowledge commenters' concerns, but note that eCQMs, like all other types of quality measures in the Hospital IQR Program, including claims-based measures, undergo rigorous testing during the measure development process for feasibility, validity, and reliability. We note that there are no claims-based or chart-abstracted versions of the two opioid-related eCQMs. We further note that reporting eCQMs has been an existing requirement for the Hospital IQR Program for several years, and is part of our ongoing commitment to promote innovation and efficiency through the use of health information technology to improve the quality of care for patients while ultimately decreasing reporting burden for providers by increasingly automating the collection of quality data. Over the past several years, hospitals have continued to build and refine their EHR systems and gain experience with reporting eCQM data, resulting in more complete data submissions with fewer errors. We also began validation of eCQM data submissions, beginning with CY 2017 reported data, to incentivize increased accuracy of data submissions. We are finalizing more lead time for hospitals to implement the new eCQM by waiting until the CY 2021 reporting period, with a submission deadline of Monday, February 28, 2022 (84 FR 19475). Further, as discussed in section VIII.A.10.(d)(4) of the preamble of this final rule, hospitals are not required to report on the Safe Use of Opioids—Concurrent Prescribing eCQM until the CY 2022 reporting period, with a submission deadline of Tuesday, February 28, 2023. We acknowledge that there are some initial implementation activities and costs associated with using new eCQMs, but we believe the long-term benefits of electronic data capture for quality improvement outweigh the burden of using eCQMs. eCQM data enable hospitals to efficiently capture and calculate quality data that can be used to address quality at the point of care and track improvements over time. We further note that based on internal monitoring of eCQM submissions, approximately 97 percent of eligible hospitals successfully submitted eCQMs for CY 2018.
Comment: A few commenters recommended that CMS delay implementation of the Safe Use of Opioids—Concurrent Prescribing eCQM by a year, until the CY 2022 reporting period/FY 2024 payment determination instead of the CY 2021 reporting period/FY 2023 payment determination, in order to allow time for vendors to properly assess the measure specifications, complete development work, and allow hospitals to adopt the measures in a safe and effective way.
Response: We believe our proposal to add the Safe Use of Opioids—Concurrent Prescribing eCQM to the eCQM measure set beginning with the CY 2021 reporting period/FY 2023 payment determination strikes an appropriate balance between CMS' goal of incrementally increasing the use of EHR data for quality measurement as well as the feedback of some stakeholders urging a faster transition to full electronic reporting.[392] We believe adding the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination allows for a reasonable amount of time for vendors to properly assess the new measure specifications, complete development work, and allow hospitals to adopt the measure in a safe and effective way. We note that testing demonstrated the measure is feasible as 96 percent of the data elements required to calculate the performance rate are: (1) Collected during routine care; (2) extractable from structured fields in the electronic health systems of test sites; and (3) likely to be accurate. Furthermore, hospitals have had several years to report data electronically for both the Hospital IQR and Promoting Interoperability Programs, and we have maintained the same eCQM reporting and submission requirements for several years in order to enable hospitals enough time to update systems and workflows to facilitate EHR-based reporting in the least burdensome manner possible. We note that several commenters appreciated and supported the consistency of the eCQM reporting and submission requirements that we are finalizing for the CYs 2020 and 2021 reporting periods, as further discussed in sections VIII.A.10(d)(2) and (3) of the preamble of this final rule, because they believe it will allow vendors and hospitals more time to acclimate to electronic reporting, adopt technology, implement and test measures, and prepare for new measures. We will continue engaging with stakeholders through education and outreach opportunities, including webinars and submitted help desk questions such as through the ONC JIRA's eCQM issue tracker for eCQM implementation and maintenance,[393] during the implementation process.
Comment: A commenter requested that value sets be developed and published on the Value Set Authority Center for opioid medications, which would streamline implementation and ensure that all hospitals are using the same values for reporting. The commenter noted that this could be done by providing a value set and standard drug codes to identify opioids.
Response: The Safe Use of Opioids—Concurrent Prescribing eCQM uses value sets published on the Value Set Authority Center (VSAC) for opioid medications. Value sets define clinical concepts to support effective and interoperable health information exchange.[394] We note that the value sets for eCQMs that have been finalized and adopted through rulemaking (along with eCQMs that are developed but not finalized for reporting in a CMS program) can be found at the Value Set Authority Center's website at: https://vsac.nlm.nih.gov/welcome.[395] Value sets are referenced in eCQMs by their unique numeric identifier, the value set object identifier (OID), which can be found within the measure specification. The measure's published value sets contain RxNorm codes—standard drug codes—to identify the opioid medication name, type, and dose combination, and are located on the VSAC.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination with a clarification and update to the technical specifications so that the measure is clearly applicable only to the inpatient setting for implementation under the Hospital IQR Program as discussed above. The updated measure specifications can be found at the eCQI Resource Center's Pre-rulemaking Eligible Hospital/Critical Access Hospital eCQMs website, available at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
(2) Hospital Harm—Opioid-Related Adverse Events eCQM
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19477 through 19480), we proposed to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination.
(a) Background
Opioids are among the most frequently implicated medications in adverse drug events among hospitalized patients. The most serious opioid-related adverse events include those with respiratory depression, which can lead to brain damage and death. Opioid-related adverse events have both negative impact on patients and financial implications. Patients who experience adverse events due to opioid administration have been noted to have 55 percent longer lengths of stay, 47 percent higher costs, 36 percent higher risk of 30-day readmission, and 3.4 times higher payments than patients without these adverse events.[396] While noting that data are limited, The Joint Commission suggested that opioid-induced respiratory arrest may contribute substantially to the 350,000 to 750,000 in-hospital cardiac arrests annually.[397]
Most opioid-related adverse events are preventable. Of the opioid-related adverse drug events reported to The Joint Commission's Sentinel Event database, 47 percent were due to a wrong medication dose, 29 percent due to improper monitoring, and 11 percent due to other causes (for example, medication interactions and/or drug reactions).[398] In addition, in a review of cases from a malpractice claims database in which there was opioid-induced respiratory depression among post-operative surgical patients, 97 percent of these adverse events were judged preventable with better monitoring and response.[399] While hospital quality interventions such as proper dosing, adequate monitoring, and attention to potential drug interactions that can lead to overdose are key to prevention of opioid-related adverse events, the use of these practices can vary substantially across hospitals.
Administration of opioids also varies widely by hospital, ranging from 5 percent in the lowest-use hospital to 72 percent in the highest-use hospital.[400] Notably, hospitals that use opioids most frequently have increased adjusted risk of severe opioid-related adverse events.[401] We have developed the Hospital Harm—Opioid-Related Adverse Events eCQM to assess the rates of adverse events as well as the variation in rates among hospitals. In the FY 2019 IPPS/LTCH PPS rulemaking (83 FR 20493 through 20494; 83 FR 41588 through 41592), we solicited public comment on the potential future adoption of this measure.
(b) Overview of Measure
The Hospital Harm—Opioid-Related Adverse Events eCQM is an outcome measure focusing specifically on opioid-related adverse events during an admission to an acute care hospital by assessing the administration of naloxone. Naloxone is a lifesaving emergent therapy with clear and unambiguous applications in the setting of opioid overdose.[402 403 404 405] Naloxone administration has also been used in a number of studies as an indicator of opioid-related adverse events to indicate a harm to a patient during inpatient admission to a hospital.[406 407] The intent of this measure is for hospitals to track and improve their monitoring and response to patients administered opioids during hospitalization, and to avoid harm, such as respiratory depression, which can lead to brain damage and death. This measure focuses specifically on in-hospital opioid-related adverse events, rather than opioid overdose events that happen in the community and may bring a patient into the emergency department.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19477 through 19480), we proposed to add this measure to the eCQM measure set from which hospitals could choose to report. For hospitals that select this measure, the measure would provide them with measurement of opioid-related adverse event rates and incentivize improved clinical workflows and monitoring when administering opioids.
The goal of this measure is to incentivize hospitals to closely monitor patients who receive opioids during their hospitalization to prevent respiratory depression. The measure requires evidence of hospital opioid administration prior to the naloxone administration during the first 24 hours after hospital arrival to ensure that the harm was hospital acquired and not due to an overdose that happened outside of the hospital. In addition, the aim of this measure is not to identify preventability of an individual harm instance or whether each instance of harm was an error, but rather to assess the overall rate of harm within a hospital by incorporating a definition of harm that is likely to be reduced as a result of hospital best practice.
The Hospital Harm—Opioid-Related Adverse Events measure (MUC17-210) was included in the publicly available “List of Measures Under Consideration for December 1, 2017.” [408] The measure was reviewed by the NQF MAP Hospital Workgroup in December 2017, and received the recommendation to refine and resubmit prior to rulemaking, as referenced in the “2017-2018 Spreadsheet of Final Recommendations to HHS and CMS.” [409] The MAP acknowledged the significant health risks associated with opioid-related adverse events but recommended adjusting the numerator to consider the impact on chronic opioid users.[410] Patients on chronic opioids remain at risk of preventable over- or mis-administration of opioids in the hospital and ideally would remain in the measure cohort. This decision was supported by the TEP during measure development. In addition, although chronic opioid users may require higher doses of opioids to achieve adequate pain control, providers have the ability to apply appropriate monitoring to prevent severe adverse events requiring naloxone administration.
In response to the MAP's concerns that the measure needed to be tested in more facilities to demonstrate reliability and validity, we have completed testing the Measure Authoring Tool (MAT) [411] output for this measure in multiple hospitals that use a variety of EHR systems,[412] and the measure was shown to be feasible to implement, reliable, and valid. For more information on the concerns and considerations raised by the MAP related to this measure, we refer readers to the December 2017 NQF MAP Hospital Workgroup Meeting Transcript.[413] In response to the MAP's recommendation, the measure was refined and presented to the MAP on November 8, 2018 for any additional feedback; however, there was no additional MAP feedback at that time.
This measure was submitted for endorsement by NQF's Patient Safety Standing Committee for the Spring 2019 cycle, with a complete review of measure validity and reliability (held on June 17, 2019), as further discussed in our responses to public comments received below.
As we stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19478), we believe this measure will provide hospitals with reliable and timely measurement of their opioid-related adverse event rates, which are a high-priority measurement area. We believe implementation of this measure can lead to safer patient care by incentivizing hospitals to implement or refine clinical workflows that facilitate evidence-based use and monitoring when administering opioids. We also believe implementation of this measure may result in fewer patients experiencing adverse events associated with the administration of opioids, such as respiratory depression, which can lead to brain damage and death. This measure addresses the quality priority of “Making Care Safer by Reducing Harm Caused in the Delivery of Care” through the Meaningful Measures Area of “Preventable Harm.” [414] We also stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19479) that adoption of this measure would introduce the first outcome measure to the eCQM measure set under the Hospital IQR Program, which currently is comprised entirely of process measures.
(c) Data Sources
The data source for this measure is entirely EHR data. The measure is designed to be calculated by the hospitals' EHRs, as well as by CMS using the patient level data submitted by hospitals to CMS. As with all quality measures we develop, testing was performed to confirm the feasibility of the measure, data elements, and validity of the numerator, using clinical adjudicators who validated the EHR data compared with medical chart-abstracted data. Based on testing, results showed that rates of missing data elements required for measure calculation were very low (range 0 percent to 0.8 percent). Testing also showed that the positive predictive value (PPV),[415] which describes the probability that a patient with a positive result (numerator case) identified by the EHR data was also a positive result verified by review of the patient's medical record done by a clinical adjudicator, was high at all hospital testing sites (94 percent to 98 percent). For more information on the measure testing and data, we refer readers to the measure's methodology report on the CMS measure methodology page at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Testing was completed using output from the MAT in five hospitals, using two different EHR systems.
(d) Measure Calculation
The Hospital Harm—Opioid-Related Adverse Events eCQM is an outcome measure that assesses, by hospital, the proportion of patients who had an opioid-related adverse event during an admission to an acute care hospital by assessing the administration of naloxone. The measure includes inpatient admissions that were initiated in the emergency department or in observational status followed by a hospital admission. The measure denominator includes all patients 18 years or older discharged from an inpatient hospital admission during the measurement period.
The numerator is the number of patients who received naloxone outside of the operating room either: (1) After 24 hours from hospital arrival; or (2) during the first 24 hours after hospital arrival with evidence of hospital opioid administration prior to the naloxone administration. We do not include naloxone use in the operating room where it could be part of the sedation plan as administered by an anesthesiologist or nurse anesthetist. Uses of naloxone for procedures outside of the operating room (such as bone marrow biopsy) are counted in the numerator as its use would indicate the patient was over sedated. These criteria exist to ensure patients are not considered to have experienced harm if they receive naloxone in the first 24 hours due to an opioid overdose that occurred in the community prior to hospital arrival. We do not require the administration of an opioid prior to naloxone after 24 hours from hospital arrival because an event occurring 24 hours after admission is most likely due to hospitals' administration of opioids. By limiting the requirement of documented opioid administration to the first 24 hours of the encounter, we are reducing the complexity of the measure logic, and therefore, the burden of implementation for hospitals. The measure numerator identifies a harm using the administration of naloxone, and purposely does not include any medications that combine naloxone with other agents.
The measure is intended to capture a type of rare event, such that a full year of data would most reliably capture the quality of care that is associated with low rates. While reliability of this measure was established using 1 year of data, we proposed eCQM reporting and submission requirements, which we discuss in section VIII.A.10.d.(1) through (4) of the preamble of this final rule, with initial reporting that would only require hospitals to submit one self-selected calendar quarter of data. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19479), we stated that hospitals may submit more than one quarter of data for this measure should they so desire, and that were considering a 1-year measurement period for the future public reporting of this measure.
(e) Outcome
This eCQM assesses the proportion of encounters where naloxone is administered as a proxy for administration of excessive amounts of opioid medications, not including naloxone given while in the operating room. In the first 24 hours of the hospitalization, an opioid must have been administered prior to receiving naloxone to be considered part of the outcome.
We note this measure is not risk adjusted for chronic opioid use, as most instances of opioid-related adverse events should be preventable for all patients regardless of prior exposure to opioids or chronic opioid use. In addition, there are several risk factors that affect sensitivity to opioids that physicians should consider when dosing opioids. Risk adjustment would only be needed if certain hospitals have patients with distinctly different risk profiles that cannot be mitigated by providing high-quality care. Similarly, the current measure specification does not include stratification of patients for chronic opioid use for three reasons: (1) This is a challenging data element to capture consistently in the EHR; (2) chronic opioid use should be taken into consideration by clinicians in determining dosing in the hospital and theoretically should not be considered a different risk level for patients; and (3) stratification can reduce the effective sample size of a measure and make the measure less useable. During measure development, TEP members gave feedback on whether the measure required risk adjustment. The majority of TEP members voted against risk adjustment of this measure with the rationale that it would be difficult to capture chronic opioid use within the EHR and that the increased risk of harm associated with these patients can be mitigated by hospital monitoring. For more information on the Hospital Harm—Opioid-Related Adverse Events eCQM, we refer readers to the measure specifications available on the CMS Measure Methodology website, at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html.
We also refer readers to section VIII.A.10.d.(1) through (4) of the preamble of this final rule where we discuss our proposed eCQM reporting and submission requirements through the CY 2022 reporting period/FY 2024 payment determination. In addition, we refer readers to section VIII.D.6.a. and b. of the preamble of this final rule where we discuss a similar proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM for the Promoting Interoperability Program beginning with the reporting period in CY 2021.
We acknowledged that some stakeholders have expressed concern that some providers could withhold the use of naloxone for patients who are in respiratory depression, believing that may help those providers avoid poor performance on the proposed Hospital Harm—Opioid-Related Adverse Events eCQM (83 FR 41591). Therefore, out of an overabundance of caution, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19480), we solicited public comment on the potential for this measure to disincentivize the appropriate use of naloxone in the hospital setting or withholding opioids when they are medically necessary in patients requiring palliative care or who are at end of life.
Comment: Many commenters supported the proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM. They noted the importance of monitoring inpatient medication administration practices and the ready availability of the necessary data from existing EHRs. Commenters appreciated that CMS has developed metrics aimed at reducing opioid-related adverse events and believed that the measure would lead to safer patient care by incentivizing tracking and improvements to the monitoring of patients who receive opioids during hospitalization. Some commenters noted that the measure would be a welcome addition to the Hospital IQR Program eCQM measure set.
Response: We thank commenters for their support of this measure. We agree with commenters that it is important to reduce adverse drug events (ADEs). We note that ADEs present the single greatest source of harm to patients in hospitals.[416] Traditional efforts to detect ADEs have focused on voluntary reporting and tracking of errors. However, studies show that only 10 to 20 percent of errors are ever reported.[417] We believe a more effective way is needed to assist hospitals in identifying the events that are causing harm to patients. While this measure addresses a high priority measurement area, as discussed further in this section of the final rule, we are not finalizing the adoption of the Hospital Harm—Opioid-Related Adverse Events eCQM in this final rule so that we can further assess stakeholder recommendations about the measure and determine what changes, if any, should be incorporated into this important measure for the future. Additional detail is discussed below in this rule.
Comment: Many commenters expressed that they would prefer that CMS secure NQF endorsement before adoption of this measure.
Response: We acknowledge the importance of NQF endorsement and reiterate our strong preference to use endorsed measures when available. Following publication of the proposed rule, the NQF Scientific Methods Panel reviewed and passed the measure for scientific acceptability.[418] The NQF Patient Safety Standing Committee then reviewed the measure for endorsement at its June 2019 meeting. The NQF Patient Safety Standing Committee expressed concerns about using naloxone as a proxy for harm in the numerator because of the potential circumstances where it may trigger numerator cases not as intended, such as for diagnostic purposes, opioid side effects, or to reverse overdoses caused by the administration of opioids that were not hospital-prescribed.[419 420] The NQF Patient Safety Standing Committee also expressed concern with the denominator including all patients admitted to the hospital rather than being limited to patients administered opioids by the hospital.[421] The NQF Patient Safety Standing Committee voted not to move forward with endorsement of this measure.[422] We note that section 1886(b)(3)(B)(viii)(IX)(bb) of the Act provides an exception: In the case of a specified area or medical topic determined appropriate by the Secretary for which a feasible and practical measure has not been endorsed by the entity with a contract under section 1890(a) of the Act, the Secretary may specify a measure that is not so endorsed as long as due consideration is given to measures that have been endorsed or adopted by a consensus organization identified by the Secretary. We attempted to find available measures for this clinical topic that have been endorsed or adopted by a consensus organization and found no other feasible and practical measures on the topic for the inpatient setting. While endorsement is not always required, we give serious consideration to the NQF's assessments. We also take into consideration stakeholder input. After considering stakeholder concerns—primarily, concerns about the requirement of evidence of prior opioid administration only during the initial 24 hours after arrival and the broad nature of the denominator that may result in the calculation of very low rates of adverse events, as discussed further in this section—as well as the concerns expressed by NQF, we plan to reevaluate the measure in response to this feedback and are thus, not finalizing the measure in this final rule. We intend to take NQF's concerns into account when considering what changes, if any, should be incorporated into this important measure for future use.
Comment: Many commenters expressed concern with the measure because of the potential unintended consequence of disincentivizing clinically appropriate treatment. Specifically, commenters expressed concern that implementation of the measure could result in deterring or delaying clinically appropriate administration of naloxone or underprescribing of opioids for pain control when clinically necessary. A commenter expressed particular caution about the measure in the absence of balancing measures related to the appropriate use of naloxone and ensuring that patients receive adequate pain control during their hospitalization. Some commenters expressed concern that the measure could cause hospitals to turn to more invasive alternatives to naloxone, such as BiPAP [423] or intubation.
Response: We acknowledge commenters' concerns about potential unintended consequences, but reiterate that naloxone is a life-saving emergent therapy with clear and unambiguous applications in the setting of opioid overdose.[424 425 426 427] We also note that it would be unethical to withhold life-saving medication. Moreover, opioid-related adverse events are avoidable by following clinical practice guidelines such as proper dosing and monitoring of patients on opioids for signs of overdose such as pinpoint pupils, unconsciousness, and respiratory depression.[428] The goal of this measure is to incentivize hospitals to avoid over-sedation and to closely monitor patients on opioids.
Regarding commenters' concerns about disincentivizing the administration of opioids, we remain confident that hospitals will continue to focus on appropriate pain management as part of their commitment to quality of care and ongoing quality improvement efforts, and use the least invasive means necessary to treat their patients. We appreciate the commenter's recommendation that this measure could benefit from being paired with a balancing measure capturing pain management and will take this into consideration as we consider new measures for future inclusion in the program.
Comment: Some commenters expressed concern with the measure because naloxone may be used to treat conditions other than opioid-related overdose such as side effects from narcotics like itching or nausea/vomiting, or change in mental status where opioids are not the cause of the change in status. Some commenters also expressed concern with the measure as currently specified because naloxone may be administered in situations in which the hospital did not administer opioids, such as patient self-administration of prescribed or illicit drugs during the encounter.
Response: We thank commenters for their suggestions, and will assess these recommendations when considering what changes, if any, should be incorporated into this important measure for future use. While we agree with some commenters that naloxone administration does not in and of itself indicate that an overdose occurred in every instance, we believe that the administration of naloxone is most commonly used for reversing opioid overdoses.[429] As such, we continue to believe that using naloxone as an indicator of overdose is appropriate. While we are not finalizing the measure as currently specified, we will further assess the various stakeholder recommendations about the measure and determine what changes, if any, should be incorporated into this important measure for the future.
Comment: A few commenters recommended modifying the measure specifications to only include opioid administration prior to naloxone use by extending the requirement of prior opioid administration to the entire hospital stay, rather than just the initial 24 hours after admission.
Response: We thank commenters for their recommendation, and will assess this concern in concert with other recommendations when considering what changes, if any, should be incorporated into this important measure for future use.
Comment: Some commenters noted that the measure as proposed includes a very broad denominator that may result in the calculation of very low rates of adverse events.
Response: We thank commenters for their observation and will assess this concern in concert with other recommendations when considering what changes, if any, should be incorporated into this important measure for future use.
Comment: Many commenters requested exclusions or risk adjustment for special cases (for example, chronic opioid users, patients with opioid sensitivity, patients with sickle cell anemia, patients receiving palliative care, clinical indications not related to opioid overdose, code blues, and manual reviews that confirm appropriate use). Some commenters also recommended exclusions for smaller doses of naloxone for opioid related side effects such as itching or nausea and vomiting.
Response: We thank commenters for their suggestions for potential refinements specific to risk adjustment and/or exclusions. As stated above, we are not finalizing the measure at this time and will consider what changes, if any, should be incorporated into this important measure for future use. We note, however, that while we understand that some hospitals may serve patients with different risk profiles, we believe avoidance of hospital-administered opioid overdoses should apply to all patients.
We also note that this measure is constructed to identify naloxone administration regardless of brand name, dosage, or route of administration. The intention of this measure is to look at hospital-administered opioid overdoses by tracking naloxone administration based on Food and Drug Administration (FDA)-approved indication of opioid depression (including respiratory depression).[430] CMS continues to monitor FDA guidance regarding indications for the use of naloxone [431 432] as well as standardization of alternate-use guidelines that support eCQM feasibility.[433]
Comment: A few commenters recommended clarification that the appropriate measure rate is not zero.
Response: The intent of this measure is not to reduce clinically appropriate use of naloxone, nor to bring the measure rate to zero, but to identify if hospitals have particularly high rates of naloxone use as an indicator of high rates of over-administration of opioids in the inpatient setting, and thereby incentivize improved clinical practices when administering opioids. Proper dosing of opioids and monitoring of patients on opioids can reduce the need for naloxone use in patient care. We recognize that naloxone is indicated for the complete or partial reversal of opioid overdose and is also indicated for diagnosis of suspected or known acute opioid over-dosage.[434] We note that of the adverse drug events reported to The Joint Commission's Sentinel Event database, 47 percent were due to a wrong medication dose, 29 percent to improper monitoring, and 11 percent to other causes (for example, medication interactions and drug reactions).[435]
Comment: Some commenters did not support the measure concept and expressed their belief that naloxone administration is not the most appropriate outcome to measure in the context of excessive dosing of opioids in the hospital setting. A commenter instead recommended measuring the reverse of the proposed measure—the proportion of patients after 24 hours who die from opioid administration because naloxone was not administered. Other commenters stated that the administration of naloxone does not necessarily imply unsafe opioid prescribing practices. A commenter noted that respiratory depression may be caused by non-opioid factors. Another commenter noted that this measure could penalize hospitals that order rescue naloxone but do not ultimately administer it.
Response: The Hospital Harm—Opioid-Related Adverse Events eCQM focuses on monitoring hospital-administered opioid overdoses through the administration of naloxone. While we agree that naloxone administration does not in and of itself indicate that an overdose occurred in every instance, we continue to believe that the administration of naloxone is most commonly used for reversing opioid overdoses, and developed a measure based on this concept accordingly. We note that the alternative measure recommended by a commenter to focus on assessing mortality resulting from failure to reverse opioid overdoses by administration of naloxone—the proportion of patients after 24 hours who die from opioid administration because naloxone was not administered—would be addressing a different patient safety issue than that intended by this measure. Regarding commenters' concerns that respiratory depression may be caused by other non-opioid factors and that this measure could penalize hospitals that order rescue naloxone but ultimately do not administer it, we note that as specified, the administration rather than the ordering of naloxone is required to trigger a numerator case.[436] Respiratory depression alone does not trigger a numerator case, nor do cases in which naloxone was only ordered but not administered.
Comment: Several commenters expressed concern that the measure does not evaluate the process used by hospital-based providers in reaching the decision to initially prescribe the opioids, and therefore may not improve the quality of care or drive the types of changes that would impact the opioid crisis.
Response: We acknowledge commenters' concerns, but note that the Hospital Harm—Opioid-Related Adverse Events eCQM is a not a process measure, and therefore would not evaluate the process used by hospital-based providers in reaching the decision to initially prescribe opioids as commenters suggest. Rather, the Hospital Harm—Opioid-Related Adverse Events eCQM is an outcome measure that seeks to promote greater awareness of in-hospital administration of opioids and incentivize providers to identify and improve appropriate opioid prescribing and administration workflows and monitoring of high-risk patients. The measure addresses this intent by measuring the proportion of patients who had an opioid-related adverse event during a hospital stay by assessing the administration of naloxone. We believe the Hospital Harm—Opioid-Related Adverse Events eCQM is a valuable patient safety measure that, by shedding light on opioid use in hospitals, driving improvements in quality of care, and incentivizing the monitoring of patients who receive opioids during hospitalization, can contribute to the multipronged effort to addressing the opioid crisis. We also note that these strategies address the Meaningful Measures quality priority of “Making Care Safer by Reducing Harm Caused in the Delivery of Care” through the Meaningful Measures Area of “Preventable Healthcare Harm.”
Comment: A commenter noted that the eCQM may be nearly topped-out. A few commenters expressed their beliefs that since testing results showed little variation in hospital performance, the measure would not provide useful information to providers or consumers. A commenter stated its belief that since the use of naloxone in inpatient care remains extremely rare, there is little reliable evidence to support using the administration of naloxone as a quality indicator. Another commenter expressed concern with this measure because it does not have clear benchmarks or target levels of performance.
Response: In the FY 2015 IPPS/LTCH PPS final rule (79 FR 50203), we finalized in the Hospital IQR Program that a measure is “topped-out” when measure performance among hospitals is so high and unvarying that meaningful distinctions and improvements in performance can no longer be made. While testing results showed low average rates for opioid-related adverse events between the sites tested (as expected for this important patient safety area), there was statistically significant variation in performance across the hospitals tested. We further noted in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50203) that quality measures, once “topped-out,” represent care standards that have been widely adopted by hospitals. As we noted in the proposed rule, while hospital quality interventions such as proper dosing, adequate monitoring, and attention to potential drug interactions that can lead to overdose are key to prevention of opioid-related adverse events, the use of these practices can vary substantially across hospitals. Administration of opioids also varies widely by hospital, ranging from 5 percent in the lowest-use hospital to 72 percent in the highest-use hospital.[437] The number of harms potentially prevented and lives potentially saved is significant, as thousands of Americans experience severe adverse events related to hospital administered opioids each year, representing significant opportunities for improvement.[438] We intend for this measure to incentivize hospitals to avoid over-sedation, to reduce concomitant opioid and benzodiazepine administration, and to closely monitor patients on opioids by measuring the proportion of encounters of patients who had an opioid-related adverse event during an an inpatient stay at an acute care hospital by assessing the administration of naloxone.[439]
Regarding the commenter's concern that there is little reliable evidence to support using the administration of naloxone as a quality indicator, we note that naloxone administration has been used in a number of studies as an indicator of opioid-related adverse events to indicate a harm to a patient during inpatient admission to a hospital.[440 441]
Regarding the commenter's concern about the measure's lack of benchmarks or target levels of performance, we note that the Hospital IQR Program is a pay for reporting, not a pay for performance, quality program. This means that its payment determinations are based on hospitals meeting all of the reporting requirements, not performance on the measures. As such, the Hospital IQR Program does not implement benchmarks or target levels of performance for its measures. Moreover, we note that the intent of this measure is not to reduce clinically appropriate use of naloxone, nor to bring the measure rate to zero, but to identify if hospitals have particularly high rates of naloxone use as an indicator of high rates of over-administration of opioids in the inpatient setting, and thereby incentivize improved clinical practices when administering opioids.
Comment: Some commenters did not support adoption of the two opioids eCQMs until eCQMs are proven to be at least as valid and reliable as their traditional claims-based or administrative counterparts. A few commenters urged CMS to balance the usefulness of the information reported through EHRs with the challenges of extracting such data and the accuracy of the data captured before adopting the two eCQMs.
Response: We acknowledge commenters' concerns, but note that eCQMs, like all other types of quality measures in the Hospital IQR Program, including claims-based measures, undergo rigorous testing during the measure development process for feasibility, validity, and reliability. We note that there are no claims-based or chart-abstracted versions of the two opioid-related eCQMs. We further note that reporting eCQMs has been an existing requirement for the Hospital IQR Program for several years, and is part of our ongoing commitment to promote innovation and efficiency through the use of health information technology and improve the quality of care for patients while ultimately decreasing reporting burden for providers by increasingly automating the collection of quality data. Over the past several years, hospitals have continued to build and refine their EHR systems and gain experience with reporting eCQM data, resulting in more complete data submissions with fewer errors. We also began validation of eCQM data submissions, beginning with CY 2017 reported data, to incentivize increased accuracy of data submissions. As discussed section VIII.A.5.a.(1) of the preamble of this final rule, we are finalizing more lead time for hospitals to implement the new Safe Use of Opioids—Concurrent Prescribing eCQM by waiting until the CY 2021 reporting period, with a submission deadline of Monday, February 28, 2022 (84 FR 19475). Further, as discussed in section VIII.A.10.(d)(4) of the preamble of this final rule, hospitals are not required to report on the Safe Use of Opioids—Concurrent Prescribing eCQM until the CY 2022 reporting period, with a submission deadline of Tuesday, February 28, 2023. We acknowledge that there are some initial implementation activities and costs associated with using new eCQMs, but we believe the long-term benefits of electronic data capture for quality improvement outweigh the burden of using eCQMs. eCQM data enable hospitals to efficiently capture and calculate quality data that can be used to address quality at the point of care and track improvements over time. We further note that based on internal monitoring of eCQM submissions, approximately 97 percent of eligible hospitals successfully submitted eCQMs for CY 2018.
Comment: A number of commenters provided additional measure suggestions or potential refinements to the measure. These suggestions include considering multiple doses of naloxone or multiple opioid-related adverse events for the same patient; specific thresholds for the administration of naloxone; restricting the measure to documented respiratory failure tied to opioid administration and/or then transfer to a higher level of care with IV use; and recommending that surgical and emergency department patients be considered for future inclusion in the measure.
Response: We thank commenters for their suggestions, and will take them into consideration as we consider potential refinements to the measure and new measures for future inclusion in the program. We note that emergency department patients who are ultimately admitted are captured in the measure, as currently specified.[442]
Comment: A commenter suggested that CMS instead consider alternative measures to address the opioid epidemic, such as the rate of prescribing opioids over 90 morphine milligram equivalent (MME) per day at discharge for patients who did not have opioid prescriptions present at admissions. The commenter recommended that CMS look beyond opioid prescribing measures to measures that assess opioid use disorder treatment, such as percentage of patients initiated on treatment at discharge.
Response: As further discussed in section VIII.A.5.a.(1), where we discuss our adoption of the Safe Use of Opioids—Concurrent Prescribing eCQM, the opioid prescribing recommendations developed by professional organizations, states, and federal agencies share some common elements for evaluating patient care related to opioids, including dosing thresholds, cautious titration, and risk mitigation strategies such as using risk assessment tools, treatment contracts, and urine drug testing.[443] However, there is considerable variability in the specific recommendations for the range of dosing thresholds (for example, 90 MME/day to 200 MME/day), audience (for example, primary care clinicians versus specialists) and use of evidence (for example, systematic review, grading of evidence and recommendations, and role of expert opinion).[444] We will continue to consider additional opioid-related measures and evaluate evidence to determine dose ranges that are valid and not overly burdensome to compute for potential future inclusion in an eCQM. We will also take into consideration the commenter's suggestion about measures that evaluate opioid use disorder treatment as we consider new measures for future inclusion in the program.
After consideration of the public comments we received, we are not finalizing our proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM. We thank the commenters for their comments and suggestions, which we will take into consideration when assessing what changes, if any, should be incorporated into this important measure for the future.
b. Adoption of Hybrid Hospital-Wide Readmission Measure With Claims and Electronic Health Record Data (NQF #2879)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19480 through 19485), we proposed to adopt the Hybrid Hospital-Wide Readmission Measure with Claims and Electronic Health Record Data (NQF #2879) (Hybrid HWR measure) into the Hospital IQR Program in a stepwise fashion. First, we would accept data submissions for the Hybrid HWR measure during two voluntary reporting periods. In those periods, we would collect data on the Hybrid HWR measure in accordance with, and to the extent permitted by, the HIPAA Privacy and Security Rules (45 CFR parts 160 and 164, subparts A, C, and E), and other applicable law. The first voluntary reporting period would run from July 1, 2021 through June 30, 2022, and the second would run from July 1, 2022 through June 30, 2023. Each voluntary reporting period would be for four quarters (or one year), which is an expansion upon the 2018 Voluntary Reporting Period for the Hybrid HWR measure, which only collected two quarters of data. Immediately thereafter, we proposed to require reporting of the Hybrid HWR measure for the reporting period which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination, and for subsequent years. This proposal to adopt the Hybrid HWR measure with a stepwise implementation timeline was made in conjunction with our proposal to remove the Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure (NQF #1789) (HWR claims-only measure) (discussed in section VIII.A.6. of the preamble of this final rule, in this section). These proposals are discussed in detail in this section of this final rule.
(1) Background
Hospital readmission rates are affected by complex and critical aspects of care such as communication between providers or between providers and patients; prevention of, and response to, complications; patient safety; and coordinated transitions to the outpatient environment (82 FR 38350 through 38355). Some readmissions are unavoidable, for example, those that result from inevitable progression of disease or worsening of chronic conditions. However, readmissions may also result from poor quality of care or inadequate transitional care (77 FR 53521). From a patient perspective, an unplanned readmission for any cause is an adverse event. For the July 1, 2016 through June 30, 2017 measurement period (the most recent data available), the readmission rate from the hospital-wide population ranged from 10.6 percent to 20.3 percent, showing a performance gap across hospitals with wide variation and an opportunity to improve quality.[445]
Consistent with our goal of increasing the use of EHR data in quality measurement and in response to stakeholder feedback encouraging the use of clinical data in outcome measures, we developed the Hybrid HWR measure (NQF #2879). The Hybrid HWR measure is designed to capture all unplanned readmissions that arise from acute clinical events requiring urgent rehospitalization within 30 days of discharge. Planned readmissions, which are generally not a signal of quality of care, are not considered readmissions in the measure outcome and all unplanned readmissions are considered an outcome, regardless of cause. The Hybrid HWR measure provides a facility-wide picture of this aspect of care quality in hospitals and was designed to promote hospital quality improvement. The Hybrid HWR measure aligns with the Meaningful Measures Initiative quality priority of “Promoting Effective Communication and Coordination of Care.”
The Hybrid HWR measure was first included in a publicly available document entitled “List of Measures Under Consideration for December 1, 2014.” [446] Upon review, the MAP supported further development of the Hybrid HWR measure, which was an expression of their conditional support pending endorsement for the National Quality Forum (NQF).[447] Thereafter, the Hybrid HWR measure was endorsed by the NQF on December 9, 2016.[448] The Hybrid HWR measure was first discussed in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49698 through 49704).
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38350 through 38355), we finalized a 6-month, limited, voluntary reporting period for the EHR-derived data elements used in the Hybrid HWR measure (hereinafter referred to as the 2018 Voluntary Reporting Period). Specifically, for the 2018 Voluntary Reporting Period, we invited participating hospitals and their health IT vendors to report data on discharges over a 6-month period in the first two quarters of CY 2018 (January 1, 2018 through June 30, 2018). We finalized that a hospital's annual payment determination would not be affected by the 2018 Voluntary Reporting Period. We stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19480) that hospitals that participated in the 2018 Voluntary Reporting Period will receive confidential hospital-specific reports in early summer of 2019 that detail submission results from the reporting period, as well as the Hybrid HWR measure results assessed from merged files created by our merging of the EHR data elements submitted by each participating hospital with claims data from the same set of index admissions.
Hospitals that volunteered to submit data increased their familiarity with submitting data for hybrid quality measures from their EHR systems. Participating hospitals received information and instruction on the use of the electronic specifications for this measure, had an opportunity to test extraction and submission of data to CMS, and received submission feedback reports from CMS, available via the QualityNet Secure Portal, with details on the success of their submissions. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38354), we stated that we were considering proposing the Hybrid HWR measure (NQF #2879) as a required measure as early as the FY 2023 payment determination. We also stated that any requirement for mandatory reporting on this measure would be proposed through future rulemaking.
During the 2018 Voluntary Reporting Period, approximately 150 hospitals submitted data for the Hybrid HWR measure.[449] We stated in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19480 through 19481) that we were merging the EHR data with the claims data and will provide hospitals with confidential hospital-specific reports which will reflect submission results from the reporting period. The assessment will be based on the merged files containing both submitted EHR data elements as well as claims data from the same set of index admissions.
We note that the Hybrid HWR measure cohort and outcome are identical to those in the HWR claims-only measure, which was adopted into the Hospital IQR Program beginning with the FY 2015 payment determination (77 FR 53521 through 53528). Therefore, we intend for the Hybrid HWR measure to replace the previously finalized HWR claims-only measure, as further discussed in section VIII.A.6. of the preamble of this final rule, where we discuss our proposal to remove the HWR claims-only measure beginning with the July 1, 2023 through June 30, 2024 reporting period, for the FY 2026 payment determination, the same year the Hybrid HWR measure would be required if this proposal is finalized.
(2) Measure Overview
Both the previously finalized HWR claims-only measure and proposed Hybrid HWR measure capture the hospital-level, risk-standardized readmission rate (RSRR) of unplanned, all-cause readmissions within 30 days of hospital discharge for any eligible condition. The measure reports a single summary RSRR, derived from the volume-weighted results of five different models, one for each of the following specialty cohorts based on groups of discharge condition categories or procedure categories: (1) Surgery/gynecology; (2) general medicine; (3) cardiorespiratory; (4) cardiovascular; and (5) neurology. The measure also indicates the hospital-level standardized readmission ratios (SRR) for each of these five specialty cohorts. The outcome is defined as unplanned readmission for any cause within 30 days of the discharge date for the index admission (the admission included in the measure cohort). A specified set of readmissions are planned and do not count in the readmission outcome. The target population is Medicare fee-for-service (FFS) beneficiaries who are 65 years or older and hospitalized in non-federal hospitals.
(3) Data Sources
The Hybrid HWR measure uses a combination of administrative data and a set of core clinical data elements extracted from hospital EHRs for each hospitalized Medicare FFS beneficiary over the age of 65 years, which is why it is referred to as a “hybrid” measure. The measure also requires a set of linking variables which are present in both the EHR and claims data, so each patient's core clinical data elements can be matched to the claim for the relevant admission (examples of linking variables are patient unique identifier and patient date of birth).
The administrative data consist of Medicare Part A and Part B claims data and Medicare beneficiary enrollment data, and are used to identify index admissions included in the measure cohort, to create a risk-adjustment model, and to assess the 30-day unplanned readmission outcome. The claims data are merged with EHR-based core clinical data elements, which are routinely collected on hospitalized adults, and are used in this hybrid measure for risk-adjustment of patients' severity of illness. The specific set of core clinical data elements that are used in the Hybrid HWR measure are listed in this section of this final rule.

As we stated in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49703), the core clinical data elements use existing value sets where possible. Because core clinical data elements are data that are routinely collected on hospitalized adults, they are widely available in hospital EHR systems. We have confirmed through testing that extraction of core clinical data elements from hospital EHRs is feasible and can be utilized as part of specific quality outcome measures.[450] The core clinical data elements utilize EHR data, therefore, we developed and tested a MAT output and identified value sets for extraction of the core clinical data elements, which are available at the eCQI Resource Center.[451]
We tested the electronic specifications in four separate health systems that used three different EHR systems. During development and testing of the Hybrid HWR measure, we demonstrated that the core clinical data elements were feasibly extracted from hospital EHRs for nearly all adult patients admitted. We also demonstrated that the use of the core clinical data elements to risk-adjust the Hybrid HWR measure improves the discrimination of the measure, or the ability to distinguish patients with a low risk of readmission from those at high risk of readmission, as assessed by the c-statistic.[452] In addition, inclusion of patients' clinical information from EHRs is responsive to stakeholders who prefer to use clinical information that is available to the clinical care team at the time treatment is rendered to account for patients' severity of illness rather than relying solely on data from claims (80 FR 49702). The Hybrid HWR measure is now fully developed, tested, and NQF-endorsed (NQF #2879).
We note the Hybrid HWR measure was initially developed using claims coded in ICD-9. However, we have identified and tested ICD-10 specifications for all information used in the measure derived from Medicare claims for both the HWR claims-only measure, which is currently in use under the Hospital IQR Program, and for the proposed Hybrid HWR measure. The ICD-10 specifications are identical for both the Hybrid and claims-only HWR measures. Only the Hybrid HWR measure's use of the core clinical data elements in the risk-adjustment model differs between the two measures. Those data elements are not affected by ICD-10 implementation. We update the measure specifications annually for both measures to incorporate new and revised ICD-10 codes effective October 1 of each year after clinical review.
We also clinically and empirically review updates to the Agency for Healthcare Research and Quality (AHRQ) Clinical Classifications Software (CCS) map that incorporate new codes and shifts in CCS categories of existing codes.[453] These updates may impact assignment to HWR sub-cohorts or modify the planned readmission algorithm. For additional details regarding the measure specifications that accommodate ICD-10-coded claims, we refer readers to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report, which is posted on the QualityNet website.[454] We will update and publicly release the MAT output annually to include any updates to the electronic quality measure standards and all included value sets for the measure-specific data elements. We note that the data sources are the same as those used for the 2018 Voluntary Reporting Period.
(4) Measure Calculation
The methods used to calculate the Hybrid HWR measure align with the methods used to calculate the currently adopted HWR claims-only measure. Index admissions are assigned to one of five mutually exclusive specialty cohort groups consisting of related conditions or procedures. An index admission is the hospitalization to which the readmission outcome is attributed and includes admissions for patients:
- Enrolled in Medicare FFS Part A for the 12 months prior to the date of admission and during the index admission;
- Aged 65 or over;
- Discharged alive from a non-federal short-term acute care hospital; and
- Not transferred to another acute care facility.
This measure excludes index admissions for patients:
- Admitted to Prospective Payment System (PPS)-exempt cancer hospitals;
- Without at least 30 days of post-discharge enrollment in Medicare FFS;
- Discharged against medical advice;
- Admitted for primary psychiatric diagnoses;
- Admitted for rehabilitation; or
- Admitted for medical treatment of cancer.
The five specialty cohort groups are: (1) Surgery/gynecology; (2) general medicine; (3) cardiorespiratory; (4) cardiovascular; and (5) neurology. For each specialty cohort group, the standardized readmission ratio (SRR) is calculated as the ratio of the number of “predicted” readmissions to the number of “expected” readmissions at a given hospital. For each hospital, the numerator of the ratio is the number of readmissions predicted within 30 days based on the hospital's performance with its observed case mix and service mix. The denominator for each hospital is the number of readmissions expected based on the nation's performance with each particular hospital's case mix and service mix. This approach is analogous to a ratio of “observed” to “expected” used in other types of statistical analyses. The specialty cohort SRRs are then pooled for each hospital using a volume-weighted geometric mean to create a hospital-wide composite SRR. The composite SRR is multiplied by the national observed readmission rate to produce the Risk-Standardized Readmission Rate (RSRR). For additional details regarding the measure specifications to calculate the RSRR, we refer readers to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report, which is posted on the QualityNet website.[455]
We also note an important distinguishing factor about hybrid measures: Hybrid measure results must be calculated by CMS to determine hospitals' risk-adjusted rates relative to national rates using data from all reporting hospitals. With a hybrid measure, hospitals submit data extracted from the EHR, and CMS performs the measure calculations and disseminates results.
(5) Outcome
As previously stated, the proposed Hybrid HWR measure outcome is aligned with the currently adopted HWR claims-only measure. The Hybrid HWR measure outcome assesses unplanned readmissions for any cause within 30 days of discharge from the index admission. It does not consider planned readmissions as part of the readmission outcome and identifies them by using the CMS Planned Readmission Algorithm, which is a set of criteria for classifying readmissions as planned using Medicare claims. The algorithm for the Hybrid HWR measure [456] is the same algorithm used in the HWR claims-only measure (77 FR 53521).[457] The algorithm and outcomes are also the same as those used for the 2018 Voluntary Reporting Period, although the algorithm is updated annually to reflect changes in the ICD-10 coding system and the CCS map. The algorithm identifies admissions that are typically planned and may occur within 30 days of discharge from the hospital.[458] The most recent version (v 4.0) was described in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50211 through 50216) for the HWR claims-only measure, and the code specifications are updated annually. A complete description of the CMS Planned Readmission Algorithm, which includes lists of planned procedures and acute diagnoses, can be found in the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report.[459]
(6) Risk Adjustment
The proposed Hybrid HWR measure adjusts both for case-mix differences (how severely ill patients are when they are admitted) as well as differences in hospitals' service-mix (the types of conditions that cause patients' admissions). The case-mix variables include patients' ages and comorbidities as well as laboratory test results and vital signs. As previously listed in detail, the Hybrid HWR measure specifically uses 13 core clinical data elements from EHRs—seven laboratory test results (hematocrit, white blood cell count, sodium, potassium, bicarbonate, creatinine, glucose) and six vital signs (heart rate, respiratory rate, temperature, systolic blood pressure, oxygen saturation, weight). The use of the core clinical data elements to risk-adjust the Hybrid HWR measure improves the discrimination of the measure, and inclusion of patients' clinical information from EHRs is responsive to stakeholders who prefer to use clinical information that is available to the clinical care team at the time treatment is rendered to account for patients' severity of illness rather than relying solely on data from claims (80 FR 49702).
The service-mix variables include principal discharge diagnoses grouped into AHRQ Clinical Classification Software. Patient comorbidities are based on the index admission, the admission included in the measure cohort, and a full year of prior history. The risk-adjustment variables included in the development and testing of the proposed Hybrid HWR measure are derived from both claims and clinical EHR data. As identified in the measure specifications, the variables are: (1) 13 core clinical data elements derived from hospital EHRs; [460] (2) the Clinical Classification Software (CCS) categories [461] for the principal discharge diagnosis associated with each index admission derived from ICD-10 codes in administrative claims data; and (3) comorbid conditions of each patient identified from inpatient claims in the 12 months prior to and including the index admission derived from ICD-10 codes and grouped into the CMS condition categories (CC).[462] The condition categories used in the risk-adjustment model and the ICD-10 codes grouped into each condition category can be found in the Annual Updates and Specification Report on the QualityNet website.[463]
All 13 core clinical data elements were shown to be statistically significant predictors of readmission in one or more risk-adjustment models of the five specialty cohort groups used to calculate the proposed Hybrid HWR measure.[464] The testing results demonstrate that the core clinical data elements enhanced the discrimination (assessed using the c-statistic) when used in combination with administrative claims data.[465] For additional details regarding the risk-adjustment model, we refer readers to the Hybrid Hospital-Wide Readmission Measure with Electronic Health Record Extracted Risk Factors (Version 1.1).[466] We note that the risk adjustment methods are the same as those used for the 2018 Voluntary Reporting Period.
(7) Data Submission
As with the 2018 Voluntary Reporting Period (82 FR 38350 through 38355), we proposed that hospitals would use Quality Reporting Data Architecture (QRDA) Category I files for each Medicare FFS beneficiary who is 65 years and older. Submission of data to CMS using QRDA I files is the current EHR data and measure reporting standard adopted for eCQMs implemented in the Hospital IQR Program. This same standard would be used for reporting the core clinical data elements to the CMS data receiving system via the QualityNet Secure Portal.
To successfully submit the Hybrid HWR measure, hospitals would need to submit the core clinical data elements included in the Hybrid HWR measure, as described in the measure specifications, for all Medicare FFS beneficiaries 65 and older discharged from an acute care hospitalization in the 1-year measurement period (July 1 to June 30 of each year). We note this is the same measurement period as the HWR claims-only measure (77 FR 53521 through 53528). Voluntary submission reporting periods would run from July 1, 2021 through June 30, 2022, and from July 1, 2022 through June 30, 2023. Required submission would begin with the reporting period which runs July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination.
Hospitals would also be required to successfully submit the following six linking variables that are necessary in order to merge the core clinical data elements with the CMS claims data to calculate the measure:
- CMS Certification Number;
- Health Insurance Claims Number or Medicare Beneficiary Identifier;
- Date of birth;
- Sex;
- Admission date, and
- Discharge date.
In order for us to be able to calculate the Hybrid HWR measure results, each hospital would need to report vital signs for 90 percent or more of the hospital discharges for Medicare FFS patients, 65 years or older in the measurement period (as determined from the claims submitted to CMS for admissions that ended during the same reporting period). Vital signs are measured on nearly every adult patient admitted to an acute care hospital and should be present for nearly 100 percent of discharges (identified in Medicare FFS claims submitted during the same period). In addition, calculating the measure with more than 10 percent of hospital discharges missing these data elements could cause poor reliability of the measure score and instability of hospitals' results from measurement period to measurement period.
Hospitals would also be required to submit the laboratory test results for 90 percent or more of discharges for non-surgical patients,[467] meaning those not included in the surgical specialty cohort of the HWR measure. For many patients admitted following elective surgery, there are no laboratory values available in the appropriate time window. Therefore, laboratory test results are not used in the risk adjustment of the surgical cohort.
The six variables required for linking EHR and claims data should be submitted for 100 percent of discharges in the measurement period. Because these linking variables are required for billing,[468] they should be available on all Medicare FFS patients and are ideally suited to support merging claims and EHR data. However, hospitals would meet Hospital IQR Program requirements if they submit linking variables on 95 percent or more of discharges with a Medicare FFS claim for the same hospitalization during the measurement period. Beginning with the reporting period which runs from July 1, 2023 through June 30, 2024, a hospital that does not submit any EHR data for the Hybrid HWR measure, or that submits data for less than the specified percentage of applicable patients, would be considered as not having met this Hospital IQR Program requirement and would receive a one-fourth reduction of its Annual Payment Update (APU) for the applicable fiscal year.
Under our stepwise approach, for the voluntary reporting periods which run from July 1, 2021 through June 30, 2022, and July 1, 2022 through June 30, 2023, if a hospital submits data for this proposed measure, it should do so according to the requirements previously described in order for CMS to calculate the measure. However, a hospital's annual payment determination would not be affected during this timeframe. The benefits to hospitals that submit the data in the initial 2-year voluntary reporting period include the opportunity to provide feedback on the measure specifications, to confirm mapping and extraction of data elements, to hone and improve quality assurance practices, and to troubleshoot any problems populating QRDA templates for successful submission to CMS. As previously described, hospitals would receive detailed patient discharge information which would help them perfect these processes before hospitals' payment determinations would be impacted beginning with the FY 2026 payment determination. We refer readers to section VIII.A.10.e. of the preamble of this final rule for a discussion about the form and manner of hybrid measure data submission.
(8) Confidential Feedback Reports
Hospitals that submit data for this measure during the voluntary reporting periods, which run from July 1, 2021 through June 30, 2022, and July 1, 2022 through June 30, 2023, would receive confidential hospital-specific reports that detail submission results from the applicable reporting period, as well as the Hybrid HWR measure results assessed from merged files created by our merging of the EHR data elements submitted by each participating hospital with claims data from the same set of index admissions. Participating hospitals would receive information and instructions on the use of the electronic specifications for this measure, have an opportunity to test extraction and submission of data to CMS, and receive feedback reports from CMS, available via the QualityNet Secure Portal, with details on the success of their submissions.
We proposed to take an incremental approach to implementing this proposed measure in an effort to be responsive to provider and vendor feedback (82 FR 38355), which requested sufficient time to undertake the data mapping, validation, adjustments to clinician workflow (specifically, changes to documentation practices to ensure accurate and complete mapping of the required data elements), and training needed to effectively implement EHR-based quality reporting to CMS. We believe that two additional years of voluntary reporting of the Hybrid HWR measure, in addition to the 2018 Voluntary Reporting Period, would allow hospitals more time to update and validate their systems, to ensure data mapping is accurate and complete, and to implement workflow changes and clinician training as necessary to better prepare for submitting data when the Hybrid HWR measure becomes required beginning with the reporting period which runs from July 1, 2023 through June 30, 2024 (impacting the FY 2026 payment determination) if our proposal is finalized. We believe those hospitals that can implement the Hybrid HWR measure more quickly can have the opportunity to submit their data to CMS and refine their data collection and submission processes. Starting with voluntary and confidential reporting for the Hybrid HWR measure would enable hospitals and their vendors to gain further experience collecting and reporting the core clinical data elements and linking variables so they would be ready for public reporting of the Hybrid HWR measure data on the Hospital Compare website starting with the FY 2026 payment determination.
Under our proposal, the first year of voluntary data collection for confidential reporting would be for the July 1, 2021 through June 30, 2022 reporting period. The 12-month measurement period that runs from July 1 through June 30 would be consistent with the calculation of the HWR claims-only measure. To support hospital reporting, we intend to publish the electronic specifications for this reporting period in the 2021 Annual Update [469] in the spring of 2020, providing hospitals and vendors with the electronic specifications approximately 15 months before the beginning of the reporting period on July 1, 2021. We intend to deliver the first set of confidential hospital-specific feedback reports in the spring of 2023, after we merge the EHR data with the associated claims data for the same reporting period, which is historically pulled from CMS' claims data system at the end of September following the end of the reporting period. During the first year of voluntary data collection, which runs from July 1, 2021 through June 30, 2022, we would not publicly report Hybrid HWR measure data, nor would incomplete or non-submission of the EHR data impact hospitals' APU determinations for the FY 2024 payment determination.
The second year of voluntary data collection for confidential reporting would be for the July 1, 2022 through June 30, 2023 reporting period. Similar to the first year of voluntary reporting, hospitals would use the electronic specifications for this reporting period as published in the 2022 Annual Update planned for the spring of 2021. We plan to deliver confidential hospital-specific feedback reports in the spring of 2024, after we merge the EHR data with the associated claims data. As with the first year of voluntary data collection, there would not be any associated public reporting, nor impact on hospitals' APU determinations for the FY 2025 payment determination. As previously discussed, hospitals' payment determinations could be affected beginning with the FY 2026 payment determination.
(9) Public Reporting
Under our stepwise approach, data collected specifically during the voluntary reporting periods, which would run from July 1, 2021 through June 30, 2022, and July 1, 2022 through June 30, 2023, would not be publicly reported, as previously mentioned. However, we proposed that after the end of the proposed voluntary reporting periods, we would begin public reporting of the Hybrid HWR measure results, beginning with data collected from the July 1, 2023 through June 30, 2024 reporting period, impacting the FY 2026 payment determination. This would be the first set of Hybrid HWR measure data to be publicly reported on the Hospital Compare website, which we anticipate would be included in the July 2025 refresh of Hospital Compare. The EHR data would be merged with the associated claims data, and then Hybrid HWR measure results would be shared with hospitals in the confidential hospital-specific feedback reports planned for the spring of 2025, providing hospitals a 30-day review period prior to public reporting. Thereafter, in subsequent reporting years, we would follow a similar operational timeline for EHR data submissions, availability of hospital-specific reports, and public reporting on the Hospital Compare website.
We note that this proposal was made in conjunction with our proposal to remove the Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure (NQF #1789) beginning with the FY 2026 payment determination as discussed in this final rule. We also refer readers to section VIII.D.6.c. of preamble of this final rule, which includes a discussion of our request for feedback on whether to consider adopting the Hybrid HWR measure for the Promoting Interoperability Program.
Comment: Several commenters supported our proposal to adopt the Hybrid HWR measure. Many commenters noted that the introduction of the Hybrid HWR measure will prove to be more precise in amassing clinical information relative to the claims-based measure. Many commenters stated that they agree with the introduction of clinical data elements in risk adjustment, noting that it is a step forward in improving both reliability and validity of hospitals' all-cause readmission rates. Many commenters supported the measure being included in the Hospital IQR Program. A number of commenters expressed appreciation for the voluntary reporting periods.
Response: We agree and thank the commenters for their support.
Comment: Many commenters noted conditional support for the Hybrid HWR measure. These commenters stated that integrating EHR data with claims data is a positive move towards improving risk adjustment and being able to capture meaningful data; however, they believed that reporting of the measure should remain voluntary at this time to allow any potential data collection issues to be timely addressed.
Response: We thank the commenters for their support and appreciate their perspectives. We are finalizing our proposal to allow for two more years of voluntary reporting, in addition to the 2018 Voluntary Reporting Period, before requiring mandatory reporting of the Hybrid HWR measure, beginning with the reporting period, which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination. We believe that providing this additional opportunity for hospitals to voluntarily report on the Hybrid HWR measure gives hospitals sufficient time to address potential data collection issues before mandatory reporting is required.
Comment: A number of commenters suggested that we delay the implementation of this measure. Many commenters urged us to allow for additional time before the measure becomes mandatory for the Hospital IQR Program, citing concerns about implementation challenges. A commenter stated that low participation in the 2018 Voluntary Reporting Period might result in a failure to fully detect implementation challenges. A commenter stated that based on varying levels of sophistication related to connectivity in hospitals, a hybrid measure may be premature at this time.
Response: We acknowledge the commenters' concerns. As stated above, 150 hospitals successfully participated in the voluntary reporting of 2018 data for the Hybrid HWR measure, either individually or through a vendor, and we respectfully disagree with the commenter that participation was low. We successfully merged 76 percent of the EHR submissions with matching claims data and calculated results on 149 hospitals whose discharges met all inclusion and exclusion criteria. Based on the review of the 2018 Voluntary Reporting Period, we are not concerned that implementation issues went undetected, especially because hospitals will be given an additional two years of voluntary reporting to implement this measure and identify and resolve any implementation challenges.
We acknowledge that hospitals have varying levels of resources to support implementation activities, including varying levels of experience among hospital staff related to EHR implementation and use, but we reiterate that this measure is comprised of claims data, which requires no additional submissions by hospitals, and core clinical data elements, which we believe are readily accessible in EHRs. In the development of the Hybrid HWR measure, we conducted extensive testing to ensure that all EHR data elements used in the measure specifications were readily available for the patient population and feasibly extracted from most commercial EHR systems. The information on patients' vital signs and laboratory test values should be available in all certified EHR systems. Additionally, the 2018 Voluntary Reporting Period provided useful information about the measure's electronic specifications that may lead to non-substantive refinements to clarify value sets in addition to routine annual updates of the measure specifications to ease burden of data extraction on providers.
We proposed two additional years of confidential reporting without impact on hospitals' Hospital IQR Program payment determination to ensure that all hospitals have an opportunity to gain even more experience with the measure specifications and compare their results to those obtained from the claims-only HWR measure prior to mandatory reporting and public reporting. Given that we are finalizing our proposal to adopt the Hybrid HWR measure in a stepwise fashion, first accepting voluntary data submissions during two reporting periods, followed by mandatory reporting, which begins with the reporting period that runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination, we believe that there will be sufficient time to allow hospitals and their health IT vendors to familiarize themselves with the measure reporting process. We strongly encourage hospitals to participate in the voluntary reporting periods.
Comment: Several commenters noted that a slower implementation schedule would allow the measure to be implemented with: (a) The Fast Healthcare Interoperability Resources (FHIR) standard,[470] (b) additional feedback from voluntary reporters regarding implementation challenges, (c) better awareness of the impact on performance the hybrid measure might have, and (d) a longer overlap between the claims-only and Hybrid versions of the measure to account for any unplanned implementation delays and to ensure continuity of hospital-wide readmissions data.
Response: We appreciate the various comments related to the implementation of this measure. We are currently investigating and testing the potential uses of the FHIR standard for EHR-based quality measure data reporting, however, it is not required at this time. We will inform stakeholders of any updates related to the FHIR standard for quality measure reporting as they become available. In the development of the Hybrid HWR measure, we conducted extensive testing to ensure that all EHR data elements used in the measure specifications were readily available for the patient population and feasibly extracted from most commercial EHR systems. The information on patients' vital signs and laboratory test values should be available in all certified EHR systems. Additionally, the 2018 Voluntary Reporting Period provided useful information about the measure's electronic specifications that may lead to non-substantive refinements to clarify value sets in addition to routine annual updates of the measure specifications to ease burden of data extraction on providers. We have already begun to solicit feedback from hospitals and vendors who participated to better understand stakeholders' experiences, challenges they faced, and recommendations for improvement. We will consider applying feedback received from these stakeholders to future confidential and mandatory reporting of this measure.
Hospitals that submit Hybrid HWR measure data will receive confidential hospital-specific reports that detail results in each of the confidential reporting years. This will provide hospitals with opportunities to preview their results on the Hybrid HWR measure and compare it with their performance on the claims-only HWR measure. We do not anticipate that the replacement of the claims-only HWR measure with the Hybrid HWR measure will negatively impact data reporting. We intend to monitor the transition.
Comment: Some commenters expressed concerns regarding the capabilities of the QualityNet Secure Portal and the management of the EHR data submissions given the large volume of data that would be submitted to CMS for the Hybrid HWR measure. Commenters suggested that we consider enhancing our data infrastructure in order to collect data and ensure timely upload and receipt of data. A commenter stated that previous CMS requirements involving submission of large amounts of eCQM data did not perform well, stating that previous CMS platforms were unable to handle the volume.
Response: We recognize stakeholders' concerns about CMS' data receiving infrastructure. The 2018 Voluntary Reporting Period served, in part, to test the capacity of our data receiving and processing systems to accommodate the EHR data and create files with EHR and claims data for measure calculation—150 hospitals successfully participated in the voluntary reporting of 2018 data for the Hybrid HWR measure, either individually or through a vendor. We successfully merged 76 percent of the EHR submissions with matching claims data and calculated results on 149 hospitals whose discharges met all inclusion and exclusion criteria. This demonstrates the feasibility of receiving, processing, and reporting data for the Hybrid HWR measure. We encourage all hospitals to participate in the voluntary reporting period as an opportunity to obtain detailed feedback on their performance on the measure, to provide us with additional feedback on the measure specifications and their implementation experience, to confirm mapping and extraction of data elements, to perform quality assurance, and to troubleshoot any problems during QRDA file submissions. We continue to pursue efficiencies in our data receiving systems to accommodate large QRDA I files.
Comment: A commenter suggested that we partner with EHR vendors to ensure that their products are built to accommodate the technical demands a hybrid measure will require. A commenter expressed concerns that this measure will create a dependency on EHR vendors' ability to build or map the proposed metrics with their respective costs and timeframes.
Response: We appreciate the commenters' position and acknowledge that a degree of reliance on EHR vendors is inherent in quality reporting using EHR-based data. However, as previously discussed, we conducted extensive testing to ensure that all EHR data elements used in the measure specifications were readily available for the patient population and feasibly extracted from most commercial EHR systems. The information on patients' vital signs and laboratory test values should be available in all certified EHR systems. We will continue to engage with vendors and encourage them to support reporting of the Hybrid HWR measure. We note that there are a number of channels for vendors and other stakeholders to provide feedback earlier in the measure development process, including the eCQI Resource Center, which provides numerous current resources to support electronic clinical quality improvement. We anticipate that finalizing future mandatory reporting of the Hybrid HWR measure will incentivize greater vendor participation.
Comment: A few commenters were unsure of the value of adding core clinical data elements to the measure. A commenter noted that they would be interested in further information regarding the added value of capturing other data elements that should be captured in the ICD-CM codes included in the claims, such as weight, glucose, or temperature.
Response: The Hybrid HWR measure uses a combination of administrative data and a set of core clinical data elements extracted from EHRs for each hospitalized Medicare FFS beneficiary over the age 65 years (84 FR 19481). Administrative data consist of Medicare Part A and Part B claims data and Medicare beneficiary enrollment data used to both identify index admissions included in the measure cohort, as well as to create a risk adjustment model. The elements of the clinical data improve the discrimination of hospital outcome measures as assessed by c-statistic and enhances the face validity of measures for the clinical community.[471 472]
There are 13 specific core clinical data elements used in the Hybrid HWR measure. Claims data are merged with the EHR-based core clinical data elements to calculate the risk-adjustment for patients' severity of illness. During measure development, we addressed stakeholder concerns that clinical data garnered from patients, and used by clinicians to guide diagnostic decisions and treatment, are preferable to administrative claims data when profiling hospitals' case mix.[473] To reduce the reporting burden on hospitals, the core clinical data elements were developed as a minimum dataset that could be feasibly collected and used across a variety of condition cohorts and measures.
Comment: A few commenters questioned whether using the core clinical data elements has presented any significant differences in risk adjustment relative to the claims data, and a commenter questioned whether the EHR variables required were related to readmissions outcomes. Commenters stated that additional testing should be completed prior to hospitals having to participate to ensure the addition of the proposed thirteen core clinical data elements makes a significant impact on risk adjustment.
Response: The Hybrid HWR measure uses data from patients' EHRs as well as claims data in the risk adjustment model. When added to claims data, the core clinical data elements enhanced the ability of the risk model to distinguish higher and lower risk patients. Results of testing conducted during original measure development showed that the core clinical data elements combined with the original claims-only HWR measure approach to risk adjustment yielded the best predictive model of readmission. During testing of the 30-day readmission model, the core clinical data elements were statistically significant predictors of readmission in the risk-adjusted hospital-wide cohort. The testing results demonstrate that the core clinical data elements enhanced the discrimination (assessed using the c-statistic) when used either in combination with or in place of administrative claims data for risk adjustment of currently reported CMS 30-day mortality and readmission outcome measures.[474] In addition, inclusion of clinical information from patient EHRs is responsive to stakeholders who find it preferable to use clinical information that is available to the clinical care team at the time treatment is rendered to account for patients' severity of illness in addition to data from claims.
As described in the proposed rule (84 FR 19482 through 19483), the methods used to calculate the Hybrid HWR measure align with the methods used to calculate the claims-only HWR measure. In the Hybrid HWR measure, index admissions are assigned to one of five mutually exclusive specialty cohort groups consisting of related conditions or procedures. For each specialty cohort group, we calculate a standardized readmission ratio (SRR), the ratio of the number of “predicted” readmissions to the number of “expected” readmissions. For each hospital, the numerator of the SRR is the number of readmissions within 30 days predicted based on the hospital's performance with its observed case mix and service mix. The denominator is the number of readmissions expected based on the performance of an average hospital with similar case mix and service mix. This approach is analogous to a ratio of “observed” to “expected” used in other types of statistical analyses. The specialty cohort SRRs are then pooled for each hospital using a volume-weighted geometric mean to create a hospital-wide composite SRR. The composite SRR is multiplied by the national observed readmission rate to produce the hospital's risk-standardized readmission rate (RSRR).
Comment: A few commenters believed that the approach to Hybrid HWR measure scoring lacks transparency.
Response: We refer commenters to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report for more calculation details for Hybrid HWR scores.[475] Hybrid measure results must be calculated by CMS to determine hospitals' risk-adjustment rates relative to other hospitals participating in the voluntary reporting.
Comment: A commenter questioned the impact this measure will have on readmission rates if patients' claims data do not match their EHR data.
Response: In relation to linking variables, we expect that the claims data submitted by hospitals match the information hospitals submit in their QRDA files. We clarify that mismatched data cases would not be included in the measure calculation. For the 2018 Voluntary Reporting Period, we excluded EHR-based admissions that could not be linked to claims data obtained from the measure calculation. We provided feedback to hospitals on all EHR-based admissions they submitted core clinical data elements for, regardless of whether or not it was linked to claims data. Hospitals are encouraged to participate in future voluntary reporting periods if they are interested in monitoring their performance on the Hybrid HWR measure. For the 2018 Voluntary Reporting Period, we have posted the methodology we used to match EHR-based data to claims-based data in the Hybrid HWR Hospital-Specific Report User Guide, available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1228778821616.
Comment: Several commenters expressed concern about the impact that adopting the Hybrid HWR measure could have on hospital resources. Several commenters noted that prior eCQMs have been difficult to collect and costly for hospitals, resulting in greater administrative burden. A commenter expressed doubt as to whether the increased administrative burden of the Hybrid HWR measure outweighed the benefit of the improvements. A commenter stated that reporting data using the Quality Reporting Document Architecture (QRDA) file format for hybrid measures is innately burdensome for eligible hospitals.
Response: We understand the commenters' perspective that eCQMs have been difficult to collect and that they are concerned about the impact that adopting a hybrid measure could have on hospital resources. We acknowledge that there may be costs beyond information collection burden associated with EHR-based quality measures, such as related to data mapping and validation. However, we do not believe that hospitals will need a great deal of time to evaluate and re-design their EHRs because the EHR data used in the Hybrid HWR measure are standard core clinical data elements. The EHR data was selected in part because they are consistently obtained on adult inpatients based on current clinical practice; are captured with a standard definition and recorded in a standard format across providers; and are entered in structured fields that are feasibly retrieved from current EHR systems.[476] The purpose of the core clinical data elements is to extract clinical data that are already routinely captured in EHRs among hospitalized adult patients. We sought to include data available on all patients and to avoid selecting data elements that might require clinical staff to perform additional measurements or tests that are not needed for diagnostic assessment or treatment of patients.
For the Hybrid HWR measure, we anticipate that hospitals will experience a slight information collection burden increase for reporting the core clinical data elements and linking variables used in the measure population, but we believe the burden is outweighed by the improved discrimination of the measure, or the ability to distinguish between patients of high risk of the outcome and low risk of the outcome. There is no additional burden on hospitals to report the claims-based portion of this measure because these data are already reported to the Medicare program for payment purposes. Hospitals are also not responsible for combining the claims data with the EHR data, which ultimately results in the measure score. Therefore, we anticipate hospitals will experience modest costs related to the initial mapping and extraction. We refer readers to sections X.B.3 and I.K. of Appendix A of this final rule for a more detailed discussion of information collection burden and effects, respectively, related to the Hybrid HWR measure.
We acknowledge that submission of EHR data using QRDA I files may be an added burden to hospitals. However, we believe that many stakeholders maintain a strong preference for the use of more timely clinical data in performance measures, which is most readily available in EHRs. Currently, QRDA I is the EHR data and measure reporting standard adopted for eCQMs implemented in the Hospital IQR Program. We continue to pursue efficiencies in our data receiving systems to accommodate large QRDA I files.
Comment: A commenter stated that rural hospitals would be at a disadvantage since they may not have the ability to accurately capture the required EHR data, claiming it could be expensive. A commenter did not support adoption of this measure because it is not specifically recommended by the MAP Rural Health Workgroup.
Response: With respect to rural hospitals, the EHR-derived core clinical data elements used in this measure were selected because they are already routinely captured in EHRs among hospitalized adult patients and readily available in standard formats within structured fields in certified EHR systems. This measure does not require that clinical staff perform additional measurements or tests. It also does not require hospitals to calculate measure results. It only requires hospitals to submit the patients' vital signs and laboratory test results that are already captured in routine care. We believe that rural hospitals have these data available in standard EHR data fields for most adult hospitalized patients. Additionally, twelve rural hospitals successfully participated in the 2018 Voluntary Reporting Period. Finally, because the MAP's Rural Health Workgroup noted that the majority of Critical Access Hospitals meet the threshold number of cases for the claims-only HWR measure, we believe that many small hospitals will have enough data to report on the Hybrid HWR measure.[477] The MAP supported further development of the Hybrid HWR measure, which was an expression of their conditional support pending endorsement from the National Quality Forum (NQF).[478] Thereafter, the Hybrid HWR measure was endorsed by the NQF on December 9, 2016.[479] Therefore, we believe this measure will be feasible for all hospitals. We will continue to monitor the participation of rural hospitals during the confidential reporting periods.
Comment: Some commenters expressed concerns that the hybrid measure requires a measurement period of a full year, as opposed to eCQMs which only require a hospital-selected quarter. Several commenters noted that the measurement years for the Hybrid HWR measure do not align with the eCQMs because the eCQMs are based on a calendar year reporting cycle and the Hybrid HWR measure is based on a measurement year of July through June. Commenters expressed concern that the misalignment in submission timelines will result in confusion and data reporting burden.
Response: We acknowledge the different measurement periods and reporting timelines between eCQMs and the Hybrid HWR measure as well as potential confusion among some caused by the July 1 to June 30 measurement and reporting period for the Hybrid HWR measure. The measurement period of the Hybrid HWR measure aligns with the claims-only HWR measurement period.[480] This aligned measurement period is intended to facilitate a smooth transition from the claims-only measure, which currently uses a 12-month measurement period from July 1 to June 30 of the following year, to the hybrid measure in the Hospital IQR Program and for uninterrupted public reporting of the HWR measure on the Hospital Compare website without a gap or overlap in reporting periods.
We note that we are finalizing the Hybrid HWR measure reporting requirements as proposed, including the hybrid measure submission deadlines. Hospitals must submit the core clinical data elements and linking variables within 3 months following the end of the applicable reporting period (submissions would be required no later than the first business day 3 months following the end of the reporting period). This allows hospitals and their health IT vendors to stagger their efforts during the year with eCQM submissions due in the spring and hybrid measure data submissions due in the fall, rather than being required to submit all of the data at once. We refer readers to section VIII.A.10.e. of the preamble of this final rule for more detail on the submission deadlines for hybrid measures. The current claims-only HWR measure is publicly reported on our Hospital Compare website each July based on claims data pulled during the fall of the previous year. In order to continue this schedule and allow for more rapid reporting of measure results, we proposed to use EHR data from the same July 1 to June 30 measurement period that is used for the currently implemented claims-only HWR measure. We will continue to evaluate the ease and feasibility of this schedule through the confidential reporting periods.
Comment: A commenter recommended that data field definitions be included to ensure consistency in data submission across hospitals. Two commenters noted that CMS' push for interoperability may ease the data collection process over time. A few commenters requested that we clarify how frequently hospitals will be required to submit data, and some commenters suggested we consider requiring more frequent reporting of EHR data.
Response: We interpret the commenter's reference to data field definitions as a reference to the data element descriptions. In response to the comment, we refer readers to the Value Set Authority Center (VSAC), which provides the available value set information, including the data element descriptions and codes used.[481]
We also refer readers to section VIII.A.10.e. of the preamble of this final rule for more detail on the annual submission deadlines for hybrid measures. As the Hybrid HWR measure uses a 12-month measurement period from July 1 to June 30 of the following year, we believe that annual submission of the core clinical data elements and linking variables is an appropriate frequency of reporting.
Comment: Several commenters expressed concern about the claims data extraction process, stating that this measure's reliance on claims data will limit its clinical applicability considering the limitations of claims data.
Response: The scientific acceptability of assessing hospital performance using claims data has been well established over many years.[482] The issue of the validity and reliability of claims data in the readmission measures given its limitations has been carefully considered by CMS and NQF over many cycles of review the conclusion of which has been continued support of the validity of the measure by experts by empiric testing of the measure score and continued endorsement of the measure by NQF.[483 484] We acknowledge that many stakeholders express a preference for the use of clinical information that is collected directly from the patient and used to diagnose and determine treatment.[485] For this reason, we have augmented the risk adjustment models in the Hybrid HWR measure to include data from EHRs indicating patients' severity of illness when they present to the hospital for care.[486] We believe that this enhancement addresses an important stakeholder concern and also enhances the performance of the measure.
Comment: A few commenters noted that it is possible for patient lab values to not be captured in the inpatient encounter if the lab tests were performed prior to an admission. A commenter questioned how lab values would be used if they are not attached to an encounter. Several commenters noted that hospitals will need time to reevaluate and design their EHRs to collect and validate the data.
Response: With respect to concerns about laboratory data that are not available in the EHR, the Hybrid HWR measure methodology allows hospitals to report the first captured core clinical data element values even if they occur within the facility's outpatient setting.[487] If no core clinical data element values were captured within an outpatient setting owned by the facility in the 24 hours prior to the inpatient admission, the hospitals are asked to report the first core clinical data elements captured within the 2 hours (for vital signs) or 24 hours (for laboratory test values) after admission.[488] We performed extensive testing which demonstrated that most patients in the non-surgical specialty cohorts of the Hybrid HWR measure have laboratory data captured within this timeframe.
We do not believe that hospitals will need a great deal of time to evaluate and design their EHRs because the EHR data used in the Hybrid HWR measure are standard core clinical data elements. The EHR data was selected in part because they are consistently obtained on adult inpatients based on current clinical practice; are captured with a standard definition and recorded in a standard format across providers; and are entered in structured fields that are feasibly retrieved from current EHR systems.[489] The purpose of the core clinical data elements is to extract clinical data that are already routinely captured in EHRs among hospitalized adult patients. We sought to include data available on all patients and to avoid selecting data elements that might require clinical staff to perform additional measurements or tests that are not needed for diagnostic assessment or treatment of patients.
However, we do recognize that hospitals that did not elect to participate in the 2018 Voluntary Reporting Period will require time to map, extract, conduct quality assurance, and develop QRDA templates in collaboration with health IT vendors. To support time needed for this implementation work, we are finalizing two more years of voluntary reporting during which the success of data submission will not impact hospitals' Hospital IQR Program payment determinations. Participating hospitals and their vendors will be able to review the confidential hospital-specific reports provided during the voluntary reporting periods to support learning and improvement in their procedures for extracting data and completing QRDA templates.
Comment: A commenter stated that since this is the first-time clinical data on vital signs and lab data are being used to risk-adjust, they recommend alignment and consistency across CMS programs that use risk-adjusted data.
Response: In an effort to ensure harmonization across CMS programs, the core clinical data elements use existing value sets that are already used in other program measures. We agree with the importance of aligning these required core clinical data elements in measures used across CMS programs to reduce burden on hospitals and improve interoperability, and we will take this feedback into consideration as we maintain and refine the core clinical data elements for potential future hybrid measures.
Comment: A commenter encouraged the integration of elements from the Certified Electronic Health Record Technology (CEHRT) to improve the original HWR measure by including core clinical data elements for risk adjustment.
Response: We thank the commenter for their recommendation to consider integrating elements from the Certified Electronic Health Record Technology (CEHRT) when working to improve the HWR measure. The 2015 Edition of CEHRT successfully passed testing on specific standards and criteria by CMS for use in specific programs.[490] CEHRT requirements include laboratory test results, as well as all elements required for reporting on the Hospital IQR Program's eCQMs. This includes vital signs identical to those included in the Hybrid HWR measure, such as heart rate, systolic blood pressure, respiratory rate, temperature, and weight.491Therefore, given the overlap in requirements, we believe the current electronic specifications for this measure are aligned with CEHRT requirements.
Comment: A commenter expressed concerns with the clinical data elements selected, stating that the measure may not accurately reflect the level of acuity for patients.
Response: We agree that the data elements used in this measure cannot fully account for acuity for all patients, for example, some indicators of acuity such as mental status might not be captured in these elements. The EHR data used in the Hybrid HWR measure do capture important aspects of patient acuity and are also standard core clinical data elements, selected because they: (1) Reflect patients' clinical status when they first present to the hospital; (2) are clinically and statistically relevant to patient outcomes; (3) are consistently obtained on adult inpatients based on current clinical practice; (4) are captured with a standard definition and recorded in a standard format across providers; and (5) are entered in structured fields that are feasibly retrieved from current EHR systems. The purpose of the core clinical data elements is to extract clinical data that are already routinely captured in EHRs among hospitalized adult patients.
Comment: A commenter suggested that we include emergency department (ED) data for patients admitted to the hospital from the ED.
Response: This measure does include vital signs and laboratory test values for patients directly admitted to the hospital from the ED.[492 493] If the patient has values captured prior to admission, for example from the emergency department or pre-operative or other outpatient area within the hospital, the logic supports extraction of the first captured vital signs and laboratory test results within 24 hours prior to the start of the inpatient admission.[494 495] All clinical systems used in inpatient and outpatient locations within the hospital facility should be queried when looking for core clinical data element values related to a patient who is subsequently admitted. The purpose of reporting the first core clinical data elements collected after the patient presented to the hospital is to better assess and risk-adjust for the health status of the patient prior to coming to the hospital and receiving care.
Comment: A commenter suggested including medication data in risk-adjustment.
Response: We thank the commenter for their suggestion regarding medication data to risk adjustment. We are not aware of a reliable way to capture upon admission medications that patients take at home, meaning that hospitals would only be able to extract and report those medications on patients for whom they also had reliable outpatient records. Additionally, requiring extraction and submission of medications prescribed at discharge from previous hospitalizations (before the index admission captured in the measure cohort) would add significant burden to hospitals and might not provide more predictive information compared with the conditions encoded in the Medicare claims. As data capture in EHRs is dynamic and evolving, we will continue to consider the feasibility of adding important data in measure reevaluation.
Comment: Many commenters provided feedback regarding measure validity, reliability, and additional testing. Several commenters suggested that we conduct thorough testing on accuracy and usability of the core clinical data elements before mandatory reporting on the Hybrid HWR measure and before the data are publicly reported. A commenter expressed concerns around the accuracy and reliability of eCQMs, encouraged us to postpone implementation of new eCQMs until improvements in the technology occur, and suggested that reporting of the Hybrid HWR measure remain voluntary until eCQM performance improves.
Response: We appreciate the comments about measure testing. We believe that the accuracy and usability of the Hybrid HWR measure has been clearly established. We conducted extensive testing of the validity of the EHR data elements used in this measure in multiple hospitals, health systems, and EHR vendors. During the development of this measure, we tested the validity of the data elements, and assessed how often data were missing in 8 different health systems. We also tested the validity and reliability of the hospital-level measure score. Details about this testing can be found in the materials submitted to the NQF when this measure was endorsed in 2016.[496] In summary, we have established adequate reliability and validity according to NQF experts' standards.
In addition, we have also demonstrated that the addition of the EHR data elements enhance the risk adjustment model, as assessed by improvement in the c-statistic with HWR;HWR+CCDE showing; Surgery/Gynecology 0.800; 0.802, Cardiorespiratory 0.653; 0.668, Cardiovascular 0.713; 0.731, Neurology 0.670;0.708, Medicine 0.646;0.651which demonstrates improved ability to identify patients at high and low risk of the outcome.[497] The measure was reviewed and endorsed by the NQF in 2016, meaning it meets their standards for reliability and validity.[498]
Furthermore, 150 hospitals successfully submitted the EHR data elements required for measure calculation in the 2018 Voluntary Reporting Period. Those QRDA files were successfully merged with claims data and the measure was calculated among the participating hospitals. The Voluntary Reporting Period confirmed the validity of the electronic specifications and data elements, the capacity of data receiving and processing systems, and the success of measure score calculation. As a result, we are confident in the scientific acceptability as well as feasibility of the measure. Additionally, we note that based on internal monitoring of eCQM submissions, approximately 97 percent of eligible hospitals successfully submitted eCQMs for CY 2018; thus, we believe hospitals will be ready for mandatory reporting of the Hybrid HWR measure that we are finalizing to begin with the July 1, 2023 through June 30, 2024 measurement period. Nonetheless and as necessary, we will continue to test and modify the measure through the process of routine measure maintenance and reevaluation during the two additional voluntary reporting periods and during mandatory reporting.
Comment: A few commenters stated that not all EHR vendors supported the voluntary submission process. They expressed a belief that the 80 hospitals that voluntarily submitted the QRDA I files are biased towards the few vendors that supported voluntary submission. Four commenters stated that only one major EHR vendor has a module that supports the Hybrid HWR measure data submission requirements. Many commenters urged us to ensure that the reporting specifications of the Hybrid HWR measure remain stable throughout the reporting period.
Response: We clarify that more than one major vendor and 150 hospitals participated in and successfully submitted core clinical data elements during the 2018 Voluntary Reporting Period for the Hybrid HWR measure. We anticipate that finalizing two additional years of confidential reporting and finalizing a clear timeline for the future mandatory reporting for the measure will incentivize additional vendors to participate in reporting for this measure. We will continue to monitor vendor participation during confidential reporting periods and encourage all hospitals to submit data for both years. We also appreciate the suggestion that the specification remain stable through confidential reporting. We will continue to engage stakeholders in the annual reevaluation and updates of measure specifications to ensure stability.
We realize that hospitals which did not elect to participate in the 2018 Voluntary Reporting Period did not receive results that they could compare to their performance on the claims-only measure. However, all hospitals that submit data during the confidential reporting period will receive data regarding their performance on the Hybrid HWR measure. We are finalizing that hospitals will receive this feedback for two consecutive years before this reporting could affect their Hospital IQR Program payment determination as proposed.
Comment: Several commenters expressed a desire for the measure to be adjusted for social risk factors (SRF). They noted that experts have weighed in on the inclusion of SRFs and have demonstrated the feasibility and significance of SRF inclusions. Another commenter noted that we should not include outcome measures that are sensitive to sociodemographic factors in the Hospital IQR Program.
Response: We understand the important role that sociodemographic factors play in the care of patients. However, we believe the Hybrid HWR measure's risk adjustment is appropriate and reliable. The measure already incorporates a risk adjustment methodology that accounts for age and comorbidities, as well as vital signs and laboratory values at the start of the inpatient encounter.[499] Furthermore, we note that the HWR claims only measure was re-endorsed by the National Quality Forum (NQF) without adjustment for patient-level social risk factors. Although this was not directly tested for the Hybrid HWR measure (because of the smaller, limited sample for measure development), the two measures have identical specifications except for the EHR data elements added to the risk adjustment of the hybrid version. Therefore, the results of the claims measure are directly relevant and demonstrate that social risk factors exert the majority of their effect at the hospital level rather than the patient level. We interpret this to mean that the worst outcome observed in patients with social risk factors is due more to their increased likelihood of receiving care at a lower quality hospital. More information about this decision can be found on the NQF website.[500] We continue to believe that the empiric evidence shows that the measures as currently specified provide accurate and reliable information about hospital performance on readmission without inclusion of social risk factors.[501] We also refer readers to section VIII.A.9. of the preamble of this final rule for a general discussion of accounting for social risk factors.
Comment: Several commenters urged us to continue to test and identify new social risk factors that are known to affect rates of readmission that are beyond hospitals' control. A commenter believed that risk adjustment is needed to prevent disproportionally penalizing safety-net providers and academic medical centers.
Response: We have become aware of recent studies that have demonstrated the feasibility and significance of social/demographic data that can be obtained from CMS claims data,[502] and we continue to pursue analyses examining whether inclusion of data on social risk factors can enhance assessment of hospital performance without obscuring important signals of the quality of care they deliver. We agree with the important role that sociodemographic factors play in the care of patients as well as maintaining access to care as provided by safety-net providers, however, this measure is only being finalized for the Hospital IQR Program, which does not assess financial penalties based on hospital performance on measures. We also note that in most of the publicly reported claims-based readmission measures, there are some safety net providers observed to be better than average performers, demonstrating that they are able to achieve high performance despite caring for a larger proportion of socially vulnerable patients.
Comment: A few commenters expressed concern about the potential unintended consequences of the measure. A commenter encouraged CMS to monitor this measure for potential unintended consequences that could stem from the extraction of EHR data during the voluntary reporting period.
Response: We thank the commenters for their concerns regarding unintended consequences. The EHR data used in the Hybrid HWR measure are standard core clinical data elements that were selected because they: (1) Reflect patients' clinical status when they first present to the hospital; (2) are clinically and statistically relevant to patient outcomes; (3) are consistently obtained on adult inpatients based on current clinical practice; (4) are captured with a standard definition and recorded in a standard format across providers; and (5) are entered in structured fields that are feasibly retrieved from current EHR systems. The purpose of the core clinical data elements is to extract clinical data that are already routinely captured in EHRs among hospitalized adult patients. It is not intended to require that clinical staff perform additional measurements or tests that are not needed for diagnostic assessment or treatment of patients. Therefore, we do not anticipate any unintended consequences or additional burden to providers. The EHR data submission process would align as much as possible with existing electronic clinical quality measure (eCQM) standards and data reporting procedures for hospitals. Submission of data using QRDA I files is the current EHR data and measure reporting standard adopted for eCQMs implemented in the Hospital IQR Program.
Comment: A commenter stated that an unintended consequence could be that reductions in readmissions will create increasing mortality costs.
Response: We believe that requiring quality reporting on readmissions measures has successfully reduced readmissions which are both harmful to patients and costly for the health care system. Keeping patients healthy is one of our highest priorities, and we welcome any research reports pertaining to the unintended consequences of including readmissions measures in the Hospital IQR Program. In conjunction with the Hospital Readmissions Reduction Program, we are committed to monitoring any unintended consequences over time, such as the inappropriate shifting of care or increased patient morbidity and mortality, to ensure that our quality reporting initiatives improves the lives of patients and reduces cost.
Comment: A few commenters suggested retaining the HWR claims-only measure as opposed to replacing it with the Hybrid HWR measure.
Response: We thank the commenters for their feedback. We disagree that we should retain the HWR claims-only measure and not replace it with the Hybrid HWR measure, because the addition of the clinical information from the EHR improves the ability to distinguish patients with higher and lower risk of the outcome as demonstrated by the improved c-statistic. We refer readers to section VIII.A.6. of the preamble of this final rule where we finalize the removal of the HWR claims-only measure. We will continue to engage with stakeholders during the voluntary reporting period when those hospitals that choose to report on the Hybrid HWR measure will receive performance results for the Hybrid and claims-only versions of the HWR measure.
Comment: A commenter stated that they have concerns with the measure because they believed it could be incorrectly applied at the clinician level, rather than the hospital level.
Response: We would like to emphasize that the Hybrid HWR measure, like all Hospital IQR Program measures, is only applied at the hospital level and not the clinician level. We are finalizing its use to assess hospital performance only.
Comment: A commenter expressed concern that the Hybrid HWR measure may not be entirely accurate in determining healthcare-associated infections (HAIs) and shared their belief that administrative coded data could be useful as supplemental to traditional HAI surveillance, but only after validation.
Response: We would like to clarify that HAI data are not a part of the Hybrid HWR measure. The measure uses a combination of administrative data and a set of 13 core clinical data elements extracted from the hospital's EHR to assess readmission occurring within 30 days of discharge from a qualifying index hospital admission.[503] The measure uses an algorithm in the risk adjustment step to exclude diagnoses coded only in the index admission claim that might be related to the quality of care provided in the hospital from the risk model.[504]
Comment: A few commenters believed that CMS will need to collaborate with stakeholders to identify the methods for determining whether a readmission is related or not to a previous diagnosis to ensure fair adjustment of hospital payments and better align with the enacting statute of the Hospital Readmissions Reduction Program. A few commenters recommended that hospital readmissions not be accounted for if they are planned due to treatment staging, reoccurring blood transfusions, other treatments or incidents unrelated to the previous admission or diagnosis. A few commenters noted that the Hybrid HWR measure should only account for unplanned admission that are related to previous admission diagnosis. A few commenters recommended that we focus our efforts on adjusting condition-specific measures that are currently being used in the Hospital Readmissions Reduction Program.
Response: We appreciate the commenters' concerns and suggestions. We clarify that the readmission need not be connected to the original diagnosis for purposes of the Hybrid HWR measure. We emphasize that we sought feedback during the development of the claims-only HWR measure from a Technical Expert Panel regarding the planned readmission algorithm that is used to determine if admissions are likely to be planned and therefore should not count in the measure outcome. We also conducted a validation study across seven hospitals to confirm the accuracy of the planned readmission algorithm through medical record review. We refer readers to the 2018 All Cause Hospital Wide Measure Updates and Specifications Report for more information.[505] Further, we received feedback from experts and the public through the initial NQF measure endorsement processes as well as endorsement maintenance. We refer readers to 84 FR 19480 through 19485 for a detailed discussion of the development, history (including NQF endorsement), and details of this measure. Finally, because the measure is implemented in the Hospital IQR Program, we regularly correspond with the public and experts through our inbox for questions and technical assistance about the readmission measure specifications at CMSreadmissionmeasures@yale.edu.
We believe a number of these commenters are addressing the Hospital Readmissions Reduction Program, and not the Hospital IQR Program. We appreciate the suggestion to focus on the measures that are already included in the Hospital Readmissions Reduction Program, but we note that the Hospital IQR Program is also an important area of focus. We refer readers to section IV.G. of the preamble of this final rule for more information on the Hospital Readmissions Reduction Program.
We reiterate that the Hybrid HWR measure assesses all-cause unplanned readmissions within 30 days of discharge; that is, unplanned readmissions are considered for any reason, not only those that are due to the same or a “related” condition. There are several reasons for measuring all-cause readmissions. First, from the patient perspective, an unplanned readmission is disruptive and costly regardless of cause. Second, restricting the measure outcomes to those readmissions that seem to be directly related to the initial hospitalization may make the measures susceptible to changes in coding practices. Although most hospitals would not engage in such practices, we want to eliminate any incentive for hospitals to change coding practices in an effort to prevent readmissions from being captured in their readmission measure results. Third, an apparently unrelated readmission may represent a complication related to the underlying condition. Finally, hospitals can act to reduce readmissions from all causes. While we do not presume that every readmission is preventable, measuring all-cause readmission incentivizes hospitals to evaluate the full range of factors that increase patients' risk for unplanned readmissions. For example, unclear discharge instructions, poor communication with post-acute care providers, and inadequate follow-up are factors that typically increase the risk for an unplanned readmission. Although measuring all-cause readmissions will include some patients whose readmission may be unrelated to their care (for example, a casualty in a motor vehicle accident), such events should occur randomly across hospitals and therefore will not affect results on measures that assess relative performance.
Comment: Several commenters did not believe there is sufficient evidence to attribute responsibility of readmission rates to hospitals. A commenter believed that a hospital-wide readmission measure is too imprecise to be an accurate indicator of quality. A commenter expressed their belief that the readmissions methodology holds hospitals accountable for admissions that happen outside their facility. A commenter requested for further clarification on how the hospital-wide approach would generate further quality improvement relative to existing condition-specific readmission measures.
Response: The goal of the Hybrid HWR measure is to improve patient outcomes by providing patients, clinicians, and hospitals with information about hospital level, risk-standardized readmission rates of unplanned, all-cause readmission after admission for any eligible condition within 30 days of hospital discharge. Measurement of patient outcomes allows for a broad view of quality of care that encompasses more than what can be captured by individual process-of-care measures. Complex and critical aspects of care, such as communication between providers, prevention of, and response to, complications, patient safety and coordinated transitions to the outpatient environment, all contribute to patient outcomes but are difficult to measure by individual process measures.
In general, randomized controlled trials have shown that improvement in the following areas can directly reduce readmission rates: Quality of care during the initial admission; improvement in communication with patients, their caregivers, and their clinicians; patient education; pre-discharge assessment; and coordination of care after discharge. Evidence that hospitals have been able to reduce readmission rates through these quality-of-care initiatives illustrates the degree to which hospital practices can affect readmission rates.[506] The HWR measure provides an overall signal of quality for hospitals in contrast to condition-specific measures which provide more narrowly focused quality information. We believe that both types of readmission measures provide beneficiaries and providers with useful information that allows them to improve patient outcomes.
Comment: A commenter expressed concern regarding the possibility of the Hybrid HWR measure being included in the Medicare Beneficiary Quality Improvement Project (MBQIP).
Response: We thank the commenter for their comment and clarify that MBQIP is administered by HHS' Health Resources & Services Administration (HRSA).[507] The Hybrid HWR measure was proposed for adoption in the Hospital IQR Program. We will share this comment with HRSA.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Hybrid HWR measure into the Hospital IQR Program in a stepwise fashion as proposed. We will first accept data submissions for the Hybrid HWR measure during two voluntary reporting periods. The first voluntary reporting period will run from July 1, 2021 through June 30, 2022, and the second will run from July 1, 2022 through June 30, 2023. Hospitals will be required to report the Hybrid HWR measure, beginning with the reporting period which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination, and for subsequent years.
6. Removal of Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure (NQF #1789) (HWR Claims-Only Measure)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19485), we proposed to remove the Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure (NQF #1789) in conjunction with our proposal to replace the measure by making the Hybrid HWR measure mandatory beginning with the reporting period which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination. This is discussed in detail in this final rule.
The HWR claims-only measure was adopted in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53521 through 53528) for the FY 2015 payment determination and subsequent years, to allow us to provide a broader assessment of the quality of care at hospitals, especially for hospitals with too few disease specific readmissions to count separately.
In the proposed rule, we proposed to remove the HWR claims-only measure, beginning with the July 1, 2023 through June 30, 2024 reporting period, for the FY 2026 payment determination. As previously discussed in section VIII.A.5.b. of the preamble of this final rule, the Hybrid HWR measure is an enhanced version of the HWR claims-only measure, in that it provides substantive improvement to the current claims-based measure, which is why we proposed to replace it. The Hybrid HWR measure includes clinical variables in the risk adjustment, which improves face validity of the measure. Furthermore, we have heard from stakeholders that they strongly favor electronic measures over claims-based versions due to the incorporation of clinical data (80 FR 49694).
We proposed to remove the HWR claims-only measure under removal Factor 3, “the availability of a more broadly applicable measure (across settings, populations, or the availability of a measure that is more proximal in time to desired patient outcomes for the particular topic).” We took into particular consideration the aspect of removal Factor 3 which emphasizes when there is a different measure that is more proximal in time to desired patient outcomes. Aspects of the Hybrid HWR measure are more proximal in time to desired patient outcomes for this measure because the measurement of the core clinical data elements for each patient in the measure cohort is taken from the beginning of the applicable inpatient stay, in comparison to the claims data used for risk adjustment, which accounts for 1-year preceding admission. In other words, the patient data used for risk adjustment of the Hybrid HWR measure are data that come from the very start of the inpatient stay that is evaluated for a readmission. In addition, as previously noted and discussed in detail in section VIII.A.5.b. of the preamble of this final rule, the Hybrid HWR measure includes clinical variables in the risk adjustment, which improves face validity of the measure, and is responsive to provider stakeholder feedback strongly in favor of electronic measures over claims-based versions due to the incorporation of clinical data. For these reasons, we proposed to remove the HWR claims-only measure and replace it with the Hybrid HWR measure.
We refer readers to sections VIII.A.5.b. and VIII.A.10.e. of the preamble of this final rule for more detail on our proposals to adopt the Hybrid HWR measure with a stepwise implementation timeline starting with 2 years of voluntary confidential reporting, followed by mandatory data submission and public reporting of the Hybrid HWR measure results beginning with data collected from the July 1, 2023 through June 30, 2024 reporting period, impacting the FY 2026 payment determination. To ensure continuity of public reporting on Hospital-Wide All-Cause Unplanned Readmission measure data, we proposed to align the removal of the HWR claims-only measure such that its removal aligns with the end of the 2-year confidential reporting period and beginning of the mandatory data submission and public reporting of the Hybrid HWR measure. In short, the Hybrid HWR measure is intended to replace the HWR claims-only measure. Our proposal to remove the HWR claims-only measure was contingent upon our proposals for the Hybrid HWR measure being finalized.
Comment: Many commenters supported our proposal to remove the HWR claims-only measure. A few commenters appreciated that the Hybrid HWR measure is an improved approach to measuring hospital-wide readmissions, as integrating EHR data and claims data is a step toward improving risk adjustment. A few commenters' support was contingent upon the adoption of the Hybrid HWR measure. A commenter encouraged that we time the removal of the HWR claims-only measure to ensure continuity of available data. A commenter recommended we work with hospitals during the voluntary reporting period to ensure that any issues are identified and addressed before the HWR claims-only measure is removed and the Hybrid HWR measure is adopted as a mandatory measure.
Response: We thank the commenters for their support, and we agree that the Hybrid HWR measure is an improved approach toward measuring hospital-wide readmissions. We reiterate that our proposal to remove the HWR claims-only measure was contingent upon the adoption of the Hybrid HWR measure, which is being finalized in section VIII.A.5.b. of the preamble of this final rule. In this final rule, we are finalizing the removal of the claims-based HWR measure starting with the July 1, 2023 through June 30, 2024 reporting period, for the FY 2026 payment determination, which directly coincides with the mandatory reporting for the Hybrid HWR measure. Hospitals will be required to report the Hybrid HWR measure, beginning with the reporting period which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination, and for subsequent years. The first voluntary reporting period will run from July 1, 2021 through June 30, 2022, and the second will run from July 1, 2022 through June 30, 2023. Therefore, we do not anticipate a gap in data. We appreciate the commenter's suggestion and will continue to monitor reporting issues during the voluntary reporting periods for the Hybrid HWR measure through our standard channels of education and outreach, including webinars and help desk questions.
Comment: Several commenters expressed support for the removal of the HWR claims-only measure because they believed it to be an inaccurate representation of quality. Those commenters stated that claims data are not clinically validated and, therefore, believed that the data do not accurately represent quality of care.
Response: We thank the commenters for this feedback. We disagree with commenters regarding the value of claims-based measures and continue to believe that claims-based measures are an appropriate and relatively low-burden approach to quality measurement. We proposed to remove this measure to replace it with the hybrid version, which also relies on claims data. In constructing claims-based measures, we aim to utilize only those data elements from the claims that have both face validity and reliability. We avoid the use of fields that are believed to be coded inconsistently across hospitals. Specifically, we use fields that are consequential for payment and which are audited. We therefore believe these data have low enough reporting error for the data elements we collect for our claims-based measures to be an accurate representation of quality. For more information about CMS' Medicare fee for service recovery audit program, we refer readers to: https://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/Recovery-Audit-Program/.
In addition, during measure development of the HWR claims-only measure, CMS validated the claims-based risk adjustment for the readmission measures against a medical record data-based model with the same cohort of patients.[508] The medical record data included chart-based risk adjusters, such as blood pressure, not available in the claims data. We then compared the output of the two measures, in the same group of patients. The performance of the administrative and medical record models was similar. The areas under the receiver operating characteristic (ROC) curve were 0.61 and 0.58, respectively; the correlation coefficient of the hospital-level risk-standardized rates from the administrative and medical record models was 0.97. We will continue to explore multiple options to account for the effect of social risk factors on quality measures and in quality programs.
Comment: A number of commenters believed that the claims-based data used in claims-only measures cannot be adequately adjusted to account for clinical and social risk factors and that hospitals that care for vulnerable patient populations may be disadvantaged by the claims-based version of this measure. Most of those commenters also believed that adopting the Hybrid HWR measure is a positive step towards improvements to risk adjustment.
Response: We agree that adopting the Hybrid HWR measure is an important improvement to the risk adjustment methodology by not only accounting for age and comorbidities, but also vital signs and laboratory values at the start of the inpatient encounter, which is why we are finalizing replacing the HWR claims-only measure with the Hybrid HWR measure. We note that neither version of the HWR measure includes social risk factors in the risk adjustment. The HWR claims-only measure underwent extensive testing with social risk factors, which included an assessment of the potential impact on hospital-level performance of including social risk factors in the risk model, as well an estimation of the relative contribution of hospital quality or patient-level risk on the statistical association of social risk variables and the readmission outcome.[509 510] These data were successfully presented to the National Quality Forum (NQF) during endorsement maintenance. The data showed that the hospital-level effects of social risk were significantly greater than the patient-effects in the risk models, suggesting that the greater risk of readmission was attributable to the greater likelihood of patients with social risk to receive care and lower quality hospitals. Therefore, if we were to adjust for patient-level differences in social risk, then some of the differences between hospitals would also be adjusted for, potentially obscuring a signal of hospital quality. Therefore, we determined that it is not appropriate to include these variables in the risk adjustment model.
Comment: A few commenters supported the proposal to remove this measure and also recommended that we remove it earlier than proposed.
Response: We appreciate the commenters' support for removing the claims-only version earlier than proposed; however, as previously discussed, we have coordinated the removal timing to ensure continuity of public reporting on Hospital-Wide All-Cause Unplanned Readmission measure data.
Comment: A few commenters opposed our proposal to remove the HWR claims-only measure. Some commenters opposed the removal of the claims-only version because of concerns about the reliability of the hybrid version that would replace it. A commenter suggested that we retain the HWR claims-only measure until the Hybrid HWR measure is proven to be a reliable measure. Another commenter recommended that we retain the measure while allowing additional time for the Hybrid HWR measure to be reported on a voluntary basis.
Response: We appreciate the commenters' concerns regarding the reliability of the Hybrid HWR measure. We refer readers to section VIII.A.5.b. of this final rule in which we provide a more detailed discussion of the reliability of the hybrid version of this measure. We believe that the accuracy and usability of the Hybrid HWR measure has been clearly established. Nonetheless, we will continue to assess and modify the measure through the process of measure reevaluation during the two additional voluntary reporting periods and in mandatory reporting.
We reiterate that the claims-only version of the measure will remain in the Hospital IQR Program for 2 more years during voluntary reporting of the Hybrid HWR measure, which we believe provides hospitals and vendors with sufficient time to implement the Hybrid HWR measure. As previously noted, we are finalizing our proposal as proposed to adopt the Hybrid HWR measure in a stepwise fashion, with mandatory reporting beginning with the reporting period which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination.
After consideration of the public comments we received, we are finalizing our proposal as proposed to remove the Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure in conjunction with finalizing our proposal to replace the measure by making the Hybrid HWR measure mandatory beginning with the reporting period which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination.
7. Summary of Previously Finalized and Newly Finalized Hospital IQR Program Measures
a. Summary of Previously Finalized Hospital IQR Program Measures for the FY 2022 Payment Determination
This table summarizes the previously finalized Hospital IQR Program measure set for the FY 2022 payment determination:


b. Summary of Previously Finalized and Newly Finalized Hospital IQR Program Measures for the FY 2023 Payment Determination
This table summarizes the previously finalized and newly finalized Hospital IQR Program measure set for the FY 2023 payment determination:


8. Potential Future Quality Measures
In the FY 2013 IPPS/LTCH PPS final rule (77 FR 53510 through 53512), we outlined considerations to guide us in selecting new quality measures to adopt into the Hospital IQR Program. We also refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41147 through 41148), where we describe the Meaningful Measures Initiative and the quality priorities and high impact measurement areas under the Meaningful Measures framework that we have identified as relevant and meaningful to both patients and providers. In keeping with these considerations, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19487 through 19494), we invited public comment on the possible future inclusion of the following three measures in the Hospital IQR Program. We note that these measures are also being considered for potential future inclusion in the Promoting Interoperability Program.
a. Hospital Harm—Severe Hypoglycemia eCQM
(1) Background
Hypoglycemic events in the hospital are among the most common adverse drug events.[511] Hypoglycemia can cause a wide range of symptoms, including mild symptoms of dizziness, sweating, and confusion to more severe symptoms such as seizure, tachycardia or loss of consciousness. Most individuals with hypoglycemia recover fully, but in rare instances, hypoglycemia can progress to coma and death.[512] Hypoglycemia (defined as a blood glucose level of less than 70 mg/dl in this study) is associated with higher in-hospital mortality, increased length of stay, and consequently, increased resource use.[513] In a 2003-2004 study examining clinical outcomes associated with hypoglycemia in hospitalized people with diabetes, patients who had at least one hypoglycemic episode (a blood glucose level of less than 50 mg/dL) were hospitalized 2.8 days longer than patients who did not experience hypoglycemia.[514] Another retrospective cohort study showed hospitalized patients with diabetes who experienced hypoglycemia (a blood glucose level of less than 70 mg/dL) had higher medical costs (by 38.9 percent), longer length of stay (by 3.0 days), and higher odds of being discharged to a skilled nursing facility (odds ratio 1.58; 95 percent Confidence Interval 1.48-1.69) than patients with diabetes without hypoglycemia (p<0.01 for all).[515]
The rate of severe hypoglycemia (a blood glucose level of less than 40 mg/dL) varies across hospitals indicating an opportunity for improvement in care. Severe hypoglycemia rates have been reported to range from 2.3 percent to 5 percent of hospitalized patients with diabetes, and from 0.4 percent of non-ICU patient days to 1.9 percent of ICU patient days.[516 517 518] Severe hypoglycemic events are largely avoidable by careful use of anti-diabetic medication and close monitoring of blood glucose values.
Although there are many occurrences of hypoglycemia in hospital settings, many of which are preventable, there is currently no measure in a CMS quality program that quantifies how often hypoglycemic events happen to patients while in inpatient acute care. AHRQ identified insulin and other hypoglycemic agents as high-alert medications and associated adverse drug events to be included as a measure in the Medicare Patient Safety Monitoring System (MPSMS),[519] signifying the importance of measuring this hospital harm. Unlike the MPSMS which relies on chart abstracted data, the Hospital Harm—Severe Hypoglycemia eCQM identifies hypoglycemic events using direct extraction of structured data from the EHR. In addition, the National Action Plan for Adverse Drug Event Prevention notes the opportunity for health care quality reporting measures and meaningful utilization of EHR data to advance hypoglycemic adverse drug event prevention.[520] To address these gaps in measurement, we developed the Hospital Harm—Severe Hypoglycemia eCQM to identify the rates of severe hypoglycemic events using direct extraction of structured data from the EHR. We believe this measure will provide reliable and timely measurement of the rate at which severe hypoglycemia events occur in the setting of hospital administration of medication during hospitalization, which will create transparency for providers and patients with respect to variation in rates of these events among hospitals.
(2) Overview of Measure
The Hospital Harm—Severe Hypoglycemia eCQM is an outcome measure focusing specifically on in-hospital severe hypoglycemic events in the setting of hospital administered antihyperglycemic medications. The measure identifies the proportion of patients who experienced a severe hypoglycemic event using a low glucose test result of less than 40 mg/dL, within 24 hours of the administration of an antihyperglycemic agent, which indicates harm to a patient. The intent of this measure is for hospitals to track and improve their practices of appropriate dosing and adequate monitoring of patients receiving glycemic control agents, and to avoid patient harm leading to increased risk of mortality and disability. This measure addresses the quality priority of “Making Care Safer by Reducing Harm Caused in the Delivery of Care” through the Meaningful Measure Area of “Preventable Healthcare Harm.” [521]
This measure is a respecification of a hypoglycemia measure originally endorsed by the NQF, Glycemic Control—Severe Hypoglycemia (NQF #2363).[522] The original measure was not implementable because the MAT could not support the measure as specified when it was originally developed due to limitations in the Quality Data Model (QDM) to express the measure logic or syntax as specified. The measure was respecified using the updates to the MAT including expression of the logic with CQL to create a measure that can now be implemented.
The Hospital Harm—Severe Hypoglycemia (MUC18-109) measure was included in the publicly available “List of Measures Under Consideration for December 1, 2018.” [523] This measure was reviewed by the NQF MAP Hospital Workgroup in December 2018 and received conditional support pending NQF review and reendorsement once the revised measure is fully tested.[524 525] MAP stakeholders agreed that severe hypoglycemia events are largely avoidable by careful use of antihyperglycemic medication and blood glucose monitoring. The MAP recommended continuously assessing the low blood glucose threshold of <40 mg/dL for defining harm events to assess unintended consequences. Other recommendations from the MAP included defining the numerator as the total number of hypoglycemia events per hospitalization instead of the current numerator definition as a count of hospitalizations with at least one hypoglycemia event. The numerator definition was discussed at length with the measure TEP during development. The TEP members agreed with the current numerator definition of a count of hospitalizations with at least one hypoglycemic event because this adequately captures differences in quality among hospitals while simultaneously minimizing measure burden by not requiring hospitals to extract every single hypoglycemic event during a hospitalization. We agree with the importance of continually monitoring for unintended consequences once this measure is implemented. We recognize the importance of measuring hyperglycemia in conjunction with hypoglycemia and are currently developing a severe hyperglycemia eCQM. For additional information and discussion of concerns and considerations raised by the MAP related to this measure, we refer readers to the December 2018 NQF MAP Hospital Workgroup meeting transcript.[526] In the proposed rule, we noted that this measure was submitted for endorsement by NQF's Patient Safety Standing Committee for the Spring 2019 cycle, with a complete review of measure validity and reliability scheduled for June 2019. In this final rule, we add that the Scientific Methods Panel reviewed the scientific acceptability (reliability and validity of data elements and the measure as a whole) in March 2019 and the Patient Safety Standing Committee reviewed the measure for all NQF criteria in June 2019. For additional information and discussion of concerns and considerations raised during these reviews, we refer readers to the March 2019 Scientific Methods Panel meeting transcript and the Spring 2019 Patient Safety Standing Committee meeting transcript.[527 528]
(3) Data Sources
The data source for this measure is entirely EHR data. The measure is designed to be calculated by the hospitals' EHRs as well as by CMS using the patient level data submitted by hospitals to CMS.
As with all quality measures we develop, testing was performed to establish the feasibility of the measure, data elements, and validity of the numerator, using clinical adjudicators who validated the EHR data compared with medical chart-abstracted data. Testing was completed using output from the MAT in multiple hospitals, using multiple EHR systems, with the measure shown to be both reliable and valid.
(4) Measure Calculation
This measure assesses the rate at which severe hypoglycemia events caused by hospital administration of medications occur in the acute care hospital setting. It assesses the proportion of patients who had an antihyperglycemic medication given within the 24 hours prior to the harm event; and a laboratory test for glucose with a result of low glucose (less than 40 mg/dL); and no subsequent laboratory test for glucose with a result greater than 80 mg/dL within 5 minutes of the low glucose result. This measure only counts one severe hypoglycemia event per patient admission.
The measure denominator includes all patients 18 years or older discharged from an inpatient hospital encounter during the measurement period, who were administered at least one antihyperglycemic medication during their hospital stay. The measure includes inpatient admissions for patients initially seen in the emergency department or in observation status and subsequently became an inpatient. There are no denominator exclusions for this measure.
The numerator for this measure is the number of hospitalized patients with a blood glucose test result of less than 40 mg/dL (indicating severe hypoglycemia) with no repeat glucose test result greater than 80 mg/dL within 5 minutes of the low glucose test, and where an antihyperglycemic medication was administered within 24 hours prior to the low glucose result. We counted instances of low glucose of less than 40 mg/dL to identify only severe cases of hypoglycemia. Not including severe hypoglycemic events with a repeat test over 80 mg/dL within 5 minutes is to avoid counting false positives (mostly from point-of-care tests that might have returned an initial erroneous result). There are no numerator exclusions for this measure.
For more information on the Hospital Harm—Severe Hypoglycemia eCQM, we refer readers to the measure specifications available on the CMS Measure Methodology website, at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html. In this final rule, we also refer readers to the new space on the eCQI Resource Center for eCQMs that have been developed but are not finalized for reporting in a CMS program by clicking on the “Pre-Rulemaking eCQMs” tab on the right-hand side of the screen. We have posted draft specifications for this eCQM as well as several other eCQMs being finalized, as well as those we sought comment on, in this years' rule on the eCQI Resource Center at the following location: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
(5) Outcome
The outcome of interest is to reduce the rate of severe hypoglycemia events caused by hospital administration of medications that occur in the acute care hospital setting.
In evaluating our measures, we generally consider the following criteria in determining whether risk adjustment is warranted: (1) If many patients are at risk of the harm regardless of their age, clinical status, comorbidities, or reason for admission; (2) if the majority of incidents of the harm are linkable to care provision under the control of providers (for example, harms caused by excessive or inappropriate medication dosing); and (3) if there is evidence that the risk of a harm can be largely ameliorated by best care practices regardless of a patient's inherent risk profile. For example, there may be evidence that even complex patients with multiple risk factors can avoid harm events when providers closely adhere to care guidelines.
In the case of the Hospital Harm—Severe Hypoglycemia eCQM, there is evidence indicating that most hypoglycemic events of this severity (<40 mg/DL) are avoidable.[529 530 531 532] Although specific patients may be particularly vulnerable to hypoglycemia in certain settings (for example, due to organ failure and not related to administration of diabetic agents), the most common causes are lack of caloric intake, overuse of anti-diabetic agents, or both. As these causes are controllable in hospital environments, and risk can easily be reduced by following best practices, we do not believe risk adjustment is warranted for this measure. We will continue to evaluate the appropriateness of risk adjustment in measure reevaluation.
In the proposed rule, we invited public comment on potential future inclusion of the Hospital Harm—Severe Hypoglycemia eCQM in the Hospital IQR Program, including any potential unintended consequences that might result from future adoption of this measure, as well as ways to address those potential unintended consequences. We note that we are also considering this measure for potential future inclusion in the Promoting Interoperability Program.
Comment: Many commenters expressed support for the potential future inclusion of the Hospital Harm—Severe Hypoglycemia eCQM in the Hospital IQR Program. A few commenters noted that the information required to report this measure is easily available in current workflows and EHRs, and that the results accurately reflect true hypoglycemic events. Commenters believed that glycemic control in the hospital setting is very important, and that implementation of the measure reduces patient harm, length of stay, and reduces costs. A few commenters conditioned their support on the feasibility of the specifications and a reasonable implementation timeline.
Response: We thank commenters for their support and input. We agree that this measure captures important quality information that is critical to patient safety. We understand the importance of feasibility for implementing new measures, and we note that this measure was submitted to NQF for the 2019 Spring cycle and received a favorable feasibility rating from the NQF Patient Standing Committee based on an evaluation of the required eCQM feasibility scorecard.[533] We will consider implementation timelines as we continue to assess this measure for potential future adoption into the Hospital IQR Program.
Comment: A commenter supported our proposal because the inclusion of the Severe Hypoglycemia eCQM would expand the options of eCQMs available to hospitals.
Response: We appreciate the commenter's support.
Comment: A commenter supported the intent of the measure and agreed with the 40mg/dL blood glucose threshold, but also encouraged CMS to consider exclusions to the measure.
Response: We thank this commenter for their feedback. We note that this measure aims to capture a broad population and achieve measure feasibility while reducing burden in data collection and measure calculation. We believe that the measure logic accurately identifies patients who received antihyperglycemic medications in the previous 24 hours, thereby filtering out cases in which patients present with severe hypoglycemia due to sepsis, severe liver disease, insulinoma, and other conditions.
Comment: Some commenters supported the intent of the measure but urged CMS to consider clinical evidence for defining the low glucose value for the Hospital Harm—Severe Hypoglycemia eCQM. A few commenters strongly recommended increasing the target blood glucose threshold from 40 mg/dL to 54 mg/dL to align with clinical standards defined by the American Association of Clinical Endocrinologists (AACE), ADA, Advanced Technologies & Treatments for Diabetes (ATTD), European Association for the Study of Diabetes (EASD), the Endocrine Society (ES), and Juvenile Diabetes Research Foundation (JDRF).
Response: We appreciate the commenters' concerns, and we understand the importance of aligning with clinical standards. The American Diabetes Association (ADA) classifies hypoglycemia using three levels: <70 (hypoglycemia alert), <54 (clinically significant hypoglycemia), and no specific glucose threshold (severe hypoglycemia).[534] A threshold of 40 mg/dL aligns with a prior NQF-endorsed measure, has received confirmation from the TEP, and helps to reduce false positives.[535] This threshold is also in line with the empiric literature regarding severe hypoglycemia.[536 537 538]
Comment: A commenter noted that they were ambivalent toward the Hospital Harm—Severe Hypoglycemia eCQM, but expressed concern that the logic seemed convoluted in order to prevent false positives in the numerator.
Response: We thank this commenter for their input, and we will consider their perspective as we continue to evaluate the Hospital Harm—Severe Hypoglycemia eCQM for inclusion in the Hospital IQR Program. We note that, as the standards and tools to support eCQM development evolve, we will continue to explore opportunities to simplify eCQM logic to support implementation.
Comment: A number of commenters urged CMS not to include the Hospital Harm—Severe Hypoglycemia eCQM in the Hospital IQR Program until it is fully tested and has received NQF endorsement. Several commenters expressed concern about the need for additional testing for reliability and validity. A few commenters did not support future inclusion of the measure and expressed concern that testing in only two vendor systems does not provide an adequate understanding of the validity of data elements and does not ensure the measure is feasible to implement in the Hospital IQR Program. Commenters also noted that performance scores observed from testing across six hospitals ranged from 1.05 to 3.56 percent and expressed concern that these scores lacked sufficient variation to yield meaningful information about the quality of care provided.
Response: We thank commenters for providing their perspective. Please note that signal-to-noise reliability, which describes how well the measure can distinguish the performance of one hospital from another, was assessed in testing. The signal is the proportion of the variability in measured performance that can be explained by real differences in performance. Beta testing of 13,636 eligible encounters across 6 hospitals for the signal-to-noise ratio yielded a median reliability score of 0.889 (range: 0.815-0.924), which indicates excellent or near perfect agreement that all the variability is attributable to real differences in performance between hospitals.[539] The intent of this outcome measure is to reduce the frequency of hypoglycemic adverse events and to improve hospitals' practices for appropriate dosing of medication and adequate monitoring of patients receiving glycemic control agents. We also note that the Medicare Patient Safety Monitoring System (MPSMS), a national surveillance system designed to identify and track adverse drug events within the hospitalized fee-for-service Medicare population, found that out of 25,145 hospital visits that the adverse event rate for antihyperglycemic agents to be as high as 10.7 percent.[540 541 542] Although, severe hypoglycemic events are largely avoidable by careful use of anti-diabetic medication and proper glucose monitoring, studies have shown that up to 84 percent of patients with an episode of severe hypoglycemia (<40 mg/dL) had a prior episode of hypoglycemia (<70 mg/dL) during the same admission, and that despite recognition of hypoglycemia, up to 75 percent of patients did not have their dose of basal insulin changed before the next insulin administration.[543 544] Other studies have shown that hypoglycemic events can be reduced by 56 to 80 percent by careful use of antihyperglycemic medication, monitoring of patient blood glucose levels, enhanced use of technology, and implementation of evidence-based best practices.[545 546 547] We also note that this measure has also been submitted to the NQF for the 2019 Spring Cycle and received a favorable recommendation by the Scientific Methods Panel and the Patient Safety Standing Committee for all endorsement criteria including importance, performance gap, scientific acceptability of measurement properties (reliability and validity), feasibility, usability, and use.[548]
Additionally, we understand the value of sample size in measure testing, and note that measure testing was done in compliance with the NQF requirements for eCQM development.[549] The Hospital Harm—Severe Hypoglycemia eCQM was tested in two EHR systems that had good representation of hospitals across the country. This aligns with NQF's recommendation to conduct eCQM testing in more than one EHR system.[550] Empirical results also showed that the measure exhibited high reliability and data element validity. We understand the concern about the usability of this measure given the range of performance rates. We note that such a wide variation indicates ample room for improvement with this serious harm event.
Comment: A number of commenters referenced inclusion of a potential future hyperglycemia measure. Several commenters agreed with the MAP's recommendation to pair the Hospital Harm—Severe Hypoglycemia eCQM with a balancing measure on hyperglycemia to mitigate potential unintended consequences. A few commenters recommended that CMS not move forward with the Hospital Harm—Severe Hypoglycemia until a balancing hyperglycemia measure could be included in the Hospital IQR Program as well. These commenters expressed concerns about potential unintended consequences of only addressing hypoglycemia.
Several commenters expressed concern that providers may be discouraged from administering anti-hyperglycemic agents to lower glucose for patients who are hyperglycemic as a potential unintended consequence of the Hospital Harm—Severe Hypoglycemia eCQM. A commenter suggested that adopting a measure addressing hospital-acquired diabetic ketoacidosis (DKA) could mitigate potential unintended consequences as well.
Response: We recognize the importance of measuring hyperglycemia in conjunction with hypoglycemia and are currently developing a severe hyperglycemia eCQM. We agree with the importance of continually monitoring for unintended consequences, and we intend to consider these comments when assessing which measures to propose for inclusion in the Hospital IQR Program in future rulemaking.
Comment: A commenter expressed concern that the current Hospital Harm—Severe Hypoglycemia eCQM does not include risk adjustment for sociodemographic factors or stratification, which could result in disproportionately penalizing facilities like teaching hospitals and safety hospitals that treat more complex patients.
Response: We thank commenters for their feedback. We note that this measure has been submitted to the NQF and received a favorable recommendation by the Scientific Methods Panel and the Patient Safety Standing Committee for all endorsement criteria including importance, scientific acceptability of measurement properties (reliability and validity), feasibility, usability and use.[551 552] The remaining steps during endorsement consideration are generally a review of public comments and review by the Consensus Standards Approval Committee (CSAC). However, there is also potential for review by the NQF Disparities Standing Committee (DSC) if NQF determines that to be appropriate.
In the case of the Hospital Harm—Severe Hypoglycemia eCQM, there is evidence indicating that hypoglycemic events of this severity (<40 mg/DL) are avoidable. While specific patients may be more vulnerable to hypoglycemia in certain settings, the most common causes are lack of sufficient caloric intake, overuse of anti-diabetic agents, or both.[553] These causes are largely controllable in hospital environments, and risk can be reduced by following best practices, we believe risk adjustment is not warranted in this case.
Comment: Many commenters recommended that CMS consider the feedback it received in discussing the measure with the MAP earlier this year, specifically the MAP's recommendation to continuously assess and monitor potential unintended consequences, including whether the time interval included in this measure (5 minutes between tests) leads to unintended consequences. A commenter noted that the timeframe specified to repeat a blood glucose test for the Hospital Harm—Severe Hypoglycemia eCQM may not be sufficient to properly document measure values, potentially resulting in false positives or erroneous results.
Response: We appreciate commenters' response, and we will take their perspective under consideration, as well as the MAP's, as we continue to assess the appropriateness of including the Hospital Harm—Severe Hypoglycemia eCQM in the Hospital IQR Program. To clarify, the measure logic does not require a repeat blood glucose test to be performed. The expectation is that, in most cases of severe hypoglycemia, the clinical team will treat the patient and will not immediately repeat the test.[554] However, if the severe hypoglycemic event is suspected to be spurious, for example if the patient is clinically asymptomatic, and the staff repeat the point-of-care test to confirm that suspicion, this step will remove false positive results.[555] We use the 5-minute threshold to maintain consistency with a previously endorsed NQF measure for glycemic control.[556]
Comment: A few commenters, including a commenter who did not support future inclusion of the Hospital Harm—Severe Hypoglycemia measure, expressed concern on the lack of clear guidance regarding the medications to be monitored for this measure. Commenters also requested clarification on where this measure would be abstracted from the EHR. A commenter requested that CMS clarify whether point-of-care testing (POCT) lab values would be included in the definition of “laboratory values” for purposes of documenting the measure. The commenter noted that POCT values may not always be in discrete fields and expressed concern for how CMS will receive and process lab values that are not numeric.
Response: We thank commenters for their perspective. We refer readers to the CMS Pre-rulemaking eCQM Value Set available on the Value Set Authority Center (https://vsac.nlm.nih.gov/valueset/expansions?pr=CMS-Pre-rulemaking) for the clinical terminologies and associated values that indicate which proposed anti-hyperglycemic medications will be monitored and the types of glucose tests applicable to the measure. Both lab test results and point of care results are included in the measure. During measure testing, we did not note feasibility issues with capturing results from point of care testing. In addition, this measure was submitted to NQF for the 2019 Spring cycle and received a favorable feasibility rating from the NQF Patient Standing Committee based on an evaluation of the required eCQM feasibility scorecard.[557]
Comment: A commenter recommended that CMS should clearly define the Hospital Harm—Severe Hypoglycemia eCQM's measure terms, utilize data elements that are already captured in the EHR to avoid additional collection burden, and publish measurement specifications at least 18 months prior to the measure's inclusion in the Hospital IQR Program.
Response: We thank commenters for their input, and we refer readers to the new space on the eCQI Resource Center for “Pre-Rulemaking eCQMs”. We have posted draft specifications for this eCQM as well as several other eCQMs being finalized, as well as those we sought comment on, in this year's rule on the eCQI Resource Center at the following location: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
Comment: A commenter expressed concern that the measure is too broad and does not consider enough factors to accurately capture issues with insulin administration and/or hypoglycemia. A few commenters questioned whether severe hypoglycemia was an issue of sufficient scale to include in a national reporting program.
Response: We thank the commenter for their input. We believe that this measure captures important quality information that is critical to patient safety. We note that this measure has been submitted to the NQF and received a favorable recommendation by the Patient Safety Standing Committee for all endorsement criteria including importance to measure. We will consider the commenters' views as we develop future policy regarding potential inclusion of the Hospital Harm—Severe Hypoglycemia eCQM in the Hospital IQR Program.
We thank the commenters and we will consider their views as we develop future policy regarding the potential inclusion of the Hospital Harm—Severe Hypoglycemia eCQM in the Hospital IQR Program.
b. Hospital Harm—Pressure Injury eCQM
(1) Background
Pressure injuries are a common patient hospital harm and can be serious health events. An estimated 1.19 million hospital-acquired pressure injuries occurred in the year 2015.[558] Pressure injuries commonly can lead to local infection, osteomyelitis, anemia, and sepsis,[559] in addition to causing significant depression, pain, and discomfort to patients.[560] The presence or development of a pressure injury can increase the length of a patient's hospital stay by an average of 4 days, which can increase the spending ranging from $20,900 to $151,700 per pressure injury.[561 562]
The rate of pressure injuries varies across hospitals suggesting that there may be opportunity for further improvement. One study of 51,842 patients found that 4.5 percent of patients developed at least one new pressure injury during their hospitalization, with a 3.2 percent between-state variance.[563] Another study revealed pressure injury prevalence rates in U.S. hospitals participating in a registry was 2.0 percent for hospital-acquired pressure injuries,[564] while a third national study found 1.8 percent of inpatients had at least one pressure injury based on ICD-9 codes.[565] Pressure injury is considered a serious reportable event by the NQF,[566] CMS established non-payment for pressure injury,[567] and it is an indicator of the quality of nursing care a hospital provides.[568] It is well-accepted that pressure injury can be reduced through best practices [569] such as frequent repositioning, proper skin care, and specialized cushions or beds.[570] AHRQ published data that showed 3.1 million fewer incidents of hospital-acquired harm in 2011-2015 compared with 2010; 23 percent of this reduction was from a reduction in hospital-acquired pressure injuries.[571] Research has also suggested a link between a hospital's processes of care and the outcome of hospital-acquired pressure injury.[572] We therefore believe that pressure injuries are an important issue to address in the Hospital IQR Program.
(2) Overview of Measure
The intent of the Hospital Harm—Pressure Injury eCQM is to reduce pressure injury prevalence by creating transparency in the rate of these harms which should encourage hospitals to promote best practices such as frequent monitoring of patients at high risk, documenting skin assessments, frequent repositioning, proper skin care, and use of specialized cushions or beds. This measure identifies pressure injuries using direct extraction of structured data from the EHR and will provide hospitals with reliable and timely measurement of their pressure injury rates as well as creating transparency for providers and patients about the variation in rates of these events among hospitals. Pressure injuries staged 3 and staged 4 (or unstageable) are currently measured and publicly reported in the HAC Reduction Program as a component of the CMS Patient Safety and Adverse Events Composite (CMS PSI 90) measure, but this potential Hospital Harm—Pressure Injury measure improves measurement of pressure injuries by using EHR data rather than administrative claims.
The Hospital Harm—Pressure Injury eCQM was included in the publicly available document entitled “List of Measures Under Consideration for December 1, 2018.” [573] This measure was reviewed by the NQF MAP Hospital Workgroup in December 2018 and received conditional support pending NQF review and endorsement once the measure is fully tested.[574] The MAP expressed its broad support for the measure and agreed this measure can reduce patient harm due to pressure injury. Recommendations from the MAP included, excluding patients undergoing certain types of treatment that may not be appropriate to receive evidence-based pressure injury reducing interventions, such as patients at the end-of-life, as well as considering clinical data such as albumin if the measure were to be risk adjusted in the future. The MAP also recommended that the developer consider how multiple pressure injuries are identified and assessed in the same encounter. Based on the evidence gathered during testing and expert input, the measure is currently not risk adjusted and it does not exclude patients with certain conditions from the denominator as evidence shows that most newly acquired pressure injuries can be mitigated through best care and the most common causes of pressure injuries (limited mobility during acute illness, friction against skin) put all hospitalized patients at similar risk.[575 576] This measure only includes one event per hospitalization, which was supported by the TEP during measure development, to provide a quality signal without imposing undue burden on hospitals to have to enumerate every instance of a pressure injury. For additional information and discussion of concerns and considerations raised by the MAP related to this measure, we refer readers to the December 2018 NQF MAP Hospital Workgroup meeting transcript.[577] In this final rule, we add that the Hospital Harm—Pressure Injury eCQM was submitted to NQF for endorsement consideration during the Spring 2019 cycle and received a favorable recommendation by the Patient Safety Standing Committee for all endorsement criteria including importance, scientific acceptability of measurement properties (reliability and validity), feasibility, usability, and use.[578]
(3) Data Sources
The data source for this measure is entirely EHR data. The measure is designed to be calculated by the hospitals' EHRs, as well as by CMS using the patient level data submitted by hospitals to CMS.
As with all quality measures we develop, testing was performed to confirm the feasibility of the measure, data elements, and validity of the numerator, using clinical adjudicators who validated the EHR data by comparison to medical chart abstracted data. Testing was completed using output from the MAT in multiple hospitals, using multiple EHR systems, and the measure was shown to be both reliable and valid. In addition, testing showed data element feasibility is higher at hospitals with a designated “pressure injury” field in the EHR, as opposed to a generic “wound” field.
(4) Measure Calculation
This measure assesses the rate at which new hospital-acquired pressure injuries occur during acute care hospitalizations. It assesses the proportion of encounters with a newly developed stage 2, stage 3, stage 4, deep tissue pressure injury, or unstageable pressure injury during hospitalization.
The measure denominator includes all patients 18 years or older discharged from an inpatient hospital encounter during the measurement period. The measure includes inpatient admissions for patients initially seen in the emergency department or in observation status. There are no exclusions for this measure.
The numerator for this electronic outcome measure is defined as the number of admissions where a patient has a newly-developed pressure injury stage 2, stage 3, stage 4, deep tissue pressure injury, or unstageable pressure injury that was not documented as present in the first 24 hours of hospital arrival. Measure developers and guideline organizations recommend skin assessment within 24 hours of hospital arrival.[579 580 581 582] This measure assumes that any pressure injury not documented within 24 hours of arrival is hospital-acquired. For more information on the Hospital Harm—Pressure Injury eCQM, we refer readers to the measure specifications available on the CMS Measure Methodology website, at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html. In this final rule, we also refer readers to the new space on the eCQI Resource Center for eCQMs that have been developed but are not finalized for reporting in a CMS program by clicking on the “Pre-Rulemaking eCQMs” tab on the right-hand side of the screen. We have posted draft specifications for this eCQM as well as several other eCQMs being finalized, as well as those we sought comment on, in this years' rule on the eCQI Resource Center at the following location: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
(5) Outcome
The outcome of interest is to reduce the rate at which new hospital-acquired pressure injuries occur during acute care hospitalization.
In evaluating our measures, we generally consider the following criteria in determining whether risk adjustment is warranted: (1) If many patients are at risk of the harm regardless of their age, clinical status, comorbidities, or reason for admission; (2) if the majority of incidents of the harm are linkable to care provision under the control of providers (for example, harms caused by inappropriate skin care or lack of frequent repositioning); and (3) if there is evidence that the risk of a harm can be largely ameliorated by best care practices regardless of a patient's inherent risk profile. For example, there may be evidence that even complex patients with multiple risk factors can avoid harm events when providers closely adhere to care guidelines.
In the case of the Hospital Harm—Pressure Injury eCQM, there is evidence indicating that most newly acquired pressure injuries are avoidable with best practice.[583 584] Although specific patients may be particularly vulnerable to pressure injuries in certain settings (for example, permanent or prolonged immobility), the most common causes are limited mobility during an acute illness and friction or shear against sensitive skin. Many hospitalized patients are at risk of these injuries. There are many actions hospitals can take to reduce patient harm risk, such as conducting a structured risk assessment to identify individuals at risk for pressure injury as soon as possible upon arrival and repeating at regular intervals, as well as proper skin care, nutrition, and careful repositioning of patients. As many of the causes can be mitigated through best care in hospital environments, we do not believe risk adjustment is warranted for this measure. We will continue to evaluate the appropriateness of risk adjustment in measure reevaluation.
In the proposed rule, we invited public comment on potential future inclusion of the Hospital Harm—Pressure Injury eCQM in the Hospital IQR Program. We specifically sought public comment on any unintended consequences that might result from future adoption of this measure, as well as ways to address those potential unintended consequences. We note that we are also considering this measure for potential future inclusion in the Promoting Interoperability Program.
Comment: Many commenters support future adoption of the Hospital Harm—Pressure Injury eCQM in the Hospital IQR Program because they believe that pressure injury rate transparency will lead hospitals to identify and implement best practice improvements, which will reduce hospital-acquired pressure injuries. A few commenters noted that the data elements are accessible and that the measure would not require changes to clinician workflows. A commenter urged CMS to expedite the measure development process for this measure. A few commenters conditioned their support on the feasibility of the specifications and a reasonable implementation timeline.
Response: We thank the commenters for their support. As we continue to assess this measure, we will also consider timelines for potential future proposal.
Comment: Several commenters did not support future adoption of the Hospital Harm—Pressure Injury eCQM. Commenters expressed concern about potential confusion and redundancy because they believe that the measure concept is already being captured by other quality improvement measures and efforts. A commenter recommended removing other measures that assess similar cohorts.
Response: We thank the commenters for their feedback. We understand that some commenters are concerned with measuring similar harm events in both chart abstracted and eCQM measures. We remind stakeholders that the PSI-90 composite component, PSI-03, is included in the HAC Reduction Program and not the Hospital IQR Program at this time. Although we acknowledge that similar measures exist in more than one program, these measures are used and calculated from different data sources (Medicare FFS claims vs. all payer EHR data) and we believe that the universal significance of pressure injuries may warrant potential future inclusion of the Hospital Harm—Pressure Injury eCQM.
Comment: A number of commenters recommended that CMS modify the Hospital Harm—Pressure Injury eCQM to exclude certain patient populations, including but not limited to: Those receiving end-of-life care, hospice services and/or patients on extracorporeal membrane oxygenation (ECMO). A few commenters suggested excluding stage 2 pressure injuries while another suggested limiting the measure to only include ICU patients with stage 2 pressure injuries.
Response: We will take these recommendations into consideration as we continue to assess the suitability of this measure for the Hospital IQR Program. We note that this measure aims to be as inclusive as possible so that it ensures the measure will have the most impact on important subgroups of patients. We emphasize that we considered if patients are at risk regardless of age or clinical factors and whether there is evidence that the risk of a harm can be largely ameliorated by best care practices regardless of patients' inherent risk profile. All patients require risk assessment and those at higher risk require individualized care plans specifically tailored to ameliorate those risks. Hence, adjusting away this variation may create an incentive for hospitals to defer implementation of best practices (For example, more frequent assessment, specialty beds and cushions) in higher risk patients.
We clarify that all pressure injuries stage 2-4, unstageable pressure injuries, and deep tissue injuries, which are not present on arrival, are included as harms in this measure because all of these injuries represent patient harm such as pain and/or distress, and that such harms are avoidable by adherence to clinical practice guidelines and best practices such as preventive skin care and frequent repositioning.[585] The measure does not assume a linear progression through the stages of pressure injury.
Comment: Several commenters did not support the future inclusion of the Hospital Harm—Pressure Injury eCQM and expressed concern that the requirement for patients to be assessed for pressure injury within 24 hours of arrival provides too narrow a window for an appropriate skin assessment and wound evaluation. A few commenters expressed concern that the measure specifications provide insufficient time for inpatient staff to document injury if patients transition from the emergency department. Commenters also noted that the EHR may not accurately capture pressure injury documentation upon admission. Some commenters believe that it would be too easy for patients to be included in the measure calculation even though their pressure injuries were present on admission. A few commenters expressed concern that the Hospital Harm—Pressure Injury eCQM will reflect documentation variation rather than pressure injury performance and noted that documentation of pressure injuries may be in free text, not structured EHR fields. A few commenters also noted that, in order to ensure proper documentation of measure data elements, new workflows may have to be implemented in facilities.
Response: We appreciate the commenters' feedback. We note that clinical guidelines, the TEP, and previous public commenters supported the requirement for patients to be assessed for pressure injuries within 24 hours of hospital arrival.[586] The information required for this eCQM is collected during routine patient assessment in accordance with national clinical guidelines. During measure development and testing, we noted that the eCQM requirement for documentation in discrete fields resulted in a need to adjust clinical workflow in some hospitals, but this was offset by the benefit of capturing accurate information from which to drive quality improvement efforts. Documentation is an important component of the quality signal as hospitals cannot measure what is not documented. In addition, this measure was submitted to NQF for the 2019 Spring cycle and received a favorable feasibility rating from the NQF Patient Standing Committee based on an evaluation of the required eCQM feasibility scorecard.[587]
Comment: Many commenters, including a few commenters who did not support future inclusion of the measure, expressed concern that the Hospital Harm-Pressure Injury eCQM does not adequately adjust for various risk factors that affect clinical risk associated with pressure injuries. Commenters recommended that CMS continue to evaluate the appropriateness of risk adjustment during measure reevaluation. A few commenters recommended including clinical factors such as proportion of ICU patients, frailty, nutrition, ECMO patients, and multiple injuries. Several commenters also noted that teaching hospitals and safety net hospitals care for patients that are more complex and more susceptible to pressure injuries, such that a lack of risk adjustment may disproportionately affect performance scores for those facilities. A commenter recommended CMS consider using site stratification to establish separate performance benchmarks across different hospitals settings to account for different patient populations. A commenter also recommend that CMS should account for factors beyond clinical factors, such as socioeconomic and sociodemographic complexities of vulnerable populations.
Response: We appreciate the commenters' concerns. We note that in evaluating measures for adoption into the Hospital IQR Program, we consider if patients are at risk regardless of age or clinical factors and whether there is evidence that the risk of a harm can be largely ameliorated by best care practices regardless of patients' inherent risk profile. In this case, published clinical practice guidelines recommend preventive skin care, frequent repositioning, and nutritional supplementation, which all can ameliorate these risks.[588 589] All patients require risk assessment and those at higher risk require individualized care plans specifically tailored to ameliorate those risks. Hence, adjusting away this variation may create an incentive for hospitals to defer implementation of best practices (for example, more frequent assessment, specialty beds and cushions) in higher risk patients. We will continue to assess commenters' concerns and whether risk adjustment should be implemented for the Hospital Harm—Pressure Injury eCQM.
Comment: Several commenters recommended that CMS only include the Hospital Harm—Pressure Injury eCQM once it has been fully tested and received NQF endorsement. A commenter strongly encouraged CMS to assess the feasibility and validity of collecting the required data elements because testing occurred in only three EHRs. A few commenters suggested that the measure be reviewed by the NQF Disparities Committee.
Response: We clarify that this measure was submitted to NQF for endorsement consideration during the Spring 2019 cycle and received a favorable recommendation by the Scientific Methods Panel and the Patient Safety Standing Committee for all endorsement criteria including importance, scientific acceptability of measurement properties (reliability and validity), feasibility, usability, and use. The remaining steps during endorsement consideration are generally a review of public comments and review by the Consensus Standards Approval Committee (CSAC). However, there is also potential for review by the NQF Disparities Standing Committee (DSC) if NQF determines that to be appropriate.
Comment: Many commenters expressed concern about variability in determining and documenting pressure injuries for the Hospital Harm—Pressure Injury eCQM. Several commenters noted that it is unclear how this measure would affect clinician workflow and expressed concern about the subjective nature of determining stages of pressure injuries. Some commenters did not support the future inclusion of this measure and also noted that physician documentation of pressure injuries may differ from documentation by nursing staff and may vary between individual practitioners. Several commenters urged CMS to ensure consistent reporting by hospitals. A commenter expressed concern that because experts are continuously updating documentation requirements to meet prevention needs, adapting an inherently more static eCQM would not result in quality improvements. A few commenters also expressed concern that data elements for this measure are complex and may be burdensome to document consistently across providers and entities and requested adequate time to develop proper workflow before implementation.
Response: We thank the commenters for their perspective. We agree that clinician variability in documenting stages of pressure injuries does present certain challenges, hence all new hospital-acquired pressure injuries stage 2-4, unstageable pressure injuries, and deep tissue pressure injury are included as a harm in the measure numerator. The measure, as specified, does not penalize hospitals based on variability in clinician staging of pressure injuries.[590] For example, if a bedside nurse documents a stage 2 pressure injury and a wound care certified nurse practitioner later stages the pressure injury as a stage 3, this is counted as one numerator event. The information required for this eCQM is collected during routine patient assessment in accordance with national clinical guidelines. During measure development and testing, we noted that the eCQM requirement for documentation in discrete fields resulted in a need to adjust to clinical workflow in some hospitals, but this was offset by the benefit of capturing accurate information from which to drive quality improvement efforts. Documentation is an important component of the quality signal as hospitals cannot measure what is not documented.
Comment: A number of commenters sought clarification and guidance on elements of this measure. A few commenters requested standardization in the reporting of what is present on admission and the duration of time for the discovery of an injury before it is deemed hospital-acquired. A commenter encouraged CMS to clearly define measure terms and publish measure specifications for this measure at least 18 months prior to including the measure in the program. A commenter requested clarification on how to document: (1) Multiple pressure injuries, and (2) pressure injuries that are charted at different stages during hospitalization.
Response: We thank the commenters for their perspective. We note that clinical guidelines, TEP panelists, and previous public commenters supported the requirement for patients to be assessed for pressure injuries within 24 hours of hospital arrival.[591] This measure assumes that any pressure injury not documented within 24 hours of arrival is hospital-acquired. We intend to provide implementation guidance to address the documentation of multiple pressure injuries for consistent implementation in the future if this measure is proposed and implemented.
Comment: A few commenters expressed concern that the difference in Hospital Harm—Pressure Injury eCQM performance scores across hospitals during testing may not vary enough to ensure comparisons that are useful for distinguishing higher quality of care between hospitals..
Response: We appreciate commenters' concerns. We understand the concern about the usability of this measure given the range of performance rates during testing. We note that the variation in hospital performance during testing is sufficiently wide and indicates ample room for improvement with this serious harm event. We believe that measuring the occurrence of a new pressure injury among patients who were hospitalized is a signal of quality of care provided in the hospital, and. that this measure will incentivize hospitals to support resources needed and to follow best practices to ameliorate the risk of new pressure injury. We will take commenters' concern under consideration as we continue to assess this measure's suitability for the Hospital IQR Program.
We thank the commenters and we will consider their views as we develop future policy regarding the potential inclusion of the Hospital Harm—Pressure Injury eCQM in the Hospital IQR Program.
c. Cesarean Birth (PC-02) eCQM (NQF #0471e)
(1) Background
A Cesarean section (C-section) is the use of surgery to deliver a baby (or babies) in lieu of vaginal delivery. The procedure therefore entails surgical and anesthesia risks and requires mothers to undergo several days of inpatient, postoperative recovery. A C-section may occur on an emergency basis or elective basis.[592] Elective C-sections may be necessary due to preexisting medical conditions, such as high blood pressure (preeclampsia), other medical indications, or may be preferred for non-medical reasons. Non-medical reasons for elective C-section can relate to maternal preference, local practice patterns, fear of malpractice litigation, reimbursement anomalies, or other factors.[593 594 595]
The total rate of (emergency and elective) C-sections has risen since the 1990s in the United States.[596] C-sections accounted for about one-third of U.S. deliveries in 2016,[597] and there is a considerable amount of variation in the rates based on U.S. region, State, and healthcare institution.[598] U.S. practice guidelines have not indicated an optimal rate of C-section or an appropriate variance rate, but international studies suggest a preference for a lower range than current U.S. rates.[599 600 601] When medically justified, a C-section can effectively prevent maternal and perinatal mortality and morbidities. However, clinicians and consensus groups agree that increased C-section rates have not improved overall maternal-fetal outcomes and that C-sections are overused.[602 603] In this final rule, we include literature outlining maternal and neonatal C-section outcomes.
For maternal outcomes, C-sections have significantly higher prenatal and postpartum morbidity and mortality (9.2 percent) than vaginal births (8.6 percent).[604] Existing literature largely does not distinguish whether inferior outcomes derive from cause (higher risk patients undergo C-section) or effect (surgery carries inherent risks due to anesthesia, bleeding, infection, postoperative recovery, etc.). However, taking an aggregate view of multiple studies over time, it appears that C-sections carry a higher risk of subsequent miscarriage, placental abnormalities, and repeat C-section.[605] Conversely, urinary incontinence and pelvic organ prolapse occur less frequently after C-section than after vaginal delivery.[606]
In terms of neonatal outcomes, C-sections have higher respiratory morbidity (1 percent to 4 percent) than vaginal births (<1 percent).[607] Children delivered by C-section also have a higher risk of asthma and obesity.[608] However, C-sections have better outcomes for shoulder dystocia (0 percent versus 1—2 percent).[609] Again, cause (high risk fetuses more likely to be delivered by C-section) versus effect (surgery increases risk to the fetus) remains epidemiologically obscure. The medical indications for C-section necessarily entail broad obstetrician discretion because of the need to: (1) Balance any conflicting medical conditions of mother versus fetus; and (2) balance C-section against any other competing clinical considerations or external constraints (for example, availability of operating room, personnel, and/or blood).
Furthermore, C-sections receive higher reimbursement than vaginal deliveries (typically about 50 percent more). Patient cost sharing may differ, depending upon insurance coverage. Insurance experiments suggest that higher cost sharing causes patients to consume less health care,[610] but that patients distinguish poorly between necessary and unnecessary services. The pervasive use of cesarean births carries economic impacts because C-sections are more expensive than vaginal deliveries and may be accompanied by adverse outcomes and complications which similarly have substantial cost implications.[611]
For these reasons, we are considering including the electronic version of PC-02 (NQF #0471e) in the eCQM measure set to enable hospitals to track C-sections and reduce unnecessary instances of C-sections.
(2) Overview of Measure
The Joint Commission is the steward of the PC-02 measure, which assesses the rate of nulliparous women with a normal-term, singleton fetus in the vertex position (NTSV) undergoing C-section.[612] Nulliparous women are those who have never given birth. They have a lower risk during vaginal birth than do women who have undergone a previous C-section.[613 614] Full-term births have better outcomes than preterm births. Vertex presentations carry less risk than breach or transverse presentations.[615] However, this population still includes some patients with medical indications for elective C-section (for example, dystocia, chorioamnionitis, pelvic deformity, preeclampsia, fetal distress, prolapsed cord, placenta previa, abnormal lie, uterine rupture, macrosomia).[616] While the chart-abstracted and eCQM versions of PC-02 do not exclude those medical indications, extensive testing of the chart-abstracted version of the measure has shown that excluding them does not significantly increase a hospital's adjusted C-section rate, partially because the majority of these indications are rare in the NTSV population.[617]
Determining the NTSV C-section rate permits a hospital to compare its outcomes to other hospitals while focusing only on a lower-risk population. NQF has endorsed the chart-based form of this measure as a voluntary consensus standard since 2008.[618] NQF stated that decreasing the rate of unnecessary C-sections “will result in increased patient safety, a substantial decrease in maternal and neonatal morbidity and substantial savings in health care costs.” [619] Reducing the number of NSTV deliveries by C-section would also reduce the rate of repeat cesarean births.[620] We acknowledge that there are instances where C-sections are medically indicated, and we emphasize that this measure is not intended to discourage practitioners from performing C-sections when they are medically indicated. We believe that assessing the rate of NTSV C-sections may ultimately reduce the occurrence of non-medically indicated C-sections. We have encouraged hospitals whose measure rates are higher than rates at other hospitals to explore and evaluate differences in the medical and nursing management of women in labor.[621] Further, including this measure could help ensure that the Hospital IQR Program includes measures which are applicable to rural hospitals. The Rural Health Workgroup of the NQF's Measure Applications Partnership also identified the chart-abstracted version of PC-02 as a measure that holds particular relevance for rural hospitals, noting how important it is to focus on best practices in obstetric care in rural areas.[622]
The PC-02 eCQM was included in a publicly available document entitled “List of Measures Under Consideration for December 1, 2018.” [623] The MAP Coordinating Committee voted to conditionally support the PC-02 eCQM, citing the failure of the eCQM version of the measure to attain endorsement by the NQF as an area of concern.[624] The Coordinating Committee encouraged The Joint Commission to resubmit the eCQM version of PC-02 to the NQF for endorsement with additional clarifying data that has been collected since the previous attempt to attain endorsement. The MAP's Final Report of February 15, 2019, conditionally supports the PC-02 eCQM for rulemaking pending NQF evaluation and endorsement.[625] The MAP suggested feasibility testing, consultation with multiple stakeholders, and examination of unintended consequences.
(3) Data Sources
Hospitals would provide data for this measure from their EHRs. Incorporating this eCQM would align with our goal to encourage greater use of EHR data for quality measurement.
(4) Measure Calculation
This measure assesses the rate of nulliparous women with a term, singleton baby in a vertex position delivered by cesarean birth. As the measure steward for both the chart-abstracted version of PC-02 (NQF #0471) and the eCQM version (NQF #0471e), The Joint Commission publishes a detailed methodology for its calculation.[626]
The measure's denominator consists of the number of nulliparous women with a singleton, vertex fetus at ≥37 weeks of gestation who deliver a liveborn infant. Its numerator consists of the subset delivering by C-section. The numerator includes women delivering by planned C-section due to obstetric indications and for other reasons.[627] This measure excludes patients with abnormal presentations or single stillbirth during the encounter, or patients with multiple gestations recorded less than or equal to 42 weeks prior to the end of the encounter.
The cohort consists of all patients in the denominator: Nulliparous women with a singleton, vertex fetus at ≥37 weeks of gestation who deliver a liveborn infant. The cohort includes all pertinent patients regardless of payer (for example, Medicare, Medicaid, other public programs, private insurance, self-pay, charity care) or admission source (for example, home, emergency department, nursing home, hospice, another hospital, law enforcement).[628] The cohort for a region, hospital, and practitioner may differ from the national rate because of higher medical indications for C-section.
(5) Outcome
The outcome of interest is the number of C-sections to nulliparous women with a term, singleton baby in a vertex position divided by all deliveries to nulliparous women with a term, singleton baby in a vertex position.[629]
This measure is not risk adjusted. The Joint Commission decided to exclude risk-adjustment from this measure based on careful consideration of a Technical Advisory Panel's recommendations and data that indicated the results adjusted by age were sensitive to low sample sizes and applying age as a risk factor only marginally impacted the outcome.[630] The Joint Commission removed all risk adjustments from this measure, effective with discharges beginning July 1, 2016.[631]
In the proposed rule, we invited public comment on potential future inclusion of the Cesarean Birth (PC-02) eCQM (NQF #0471e) in the Hospital IQR Program. We specifically sought public comment on any unintended consequences that might result from future adoption of this measure, as well as ways to address those potential unintended consequences. We note that we are also considering this measure for potential future inclusion in the Promoting Interoperability Program.
Comment: Many commenters supported the adoption of the PC-02 measure. Their reasons included decreased maternal and perinatal morbidity and mortality, reduced costs, personal use of the resulting information, minimal data collection burden, and increased pool of eCQMs from which hospitals can select for reporting.
Response: We thank the commenters for their feedback.
Comment: A few commenters supported the adoption of PC-02 and recommended that CMS accelerate the implementation date.
Response: We thank the commenters for these suggestions and clarify that the PC-02 has not yet been proposed for adoption into the Hospital IQR Program. There is currently no planned implementation date. Any proposal to add PC-02 to the Hospital IQR Program would be made through future rulemaking
Comment: A few commenters supported the adoption of PC-02 and recommended that CMS adopt additional birth-related quality measures because they believed such additional measures would help decrease maternal and perinatal morbidity and mortality.
Response: We thank the commenters for these suggestions. We continue to monitor for measures that may be beneficial to adopt in the Hospital IQR Program.
Comment: A few commenters recommended emulating The Joint Commission practice of disclosing data only for hospitals with C-section rates that exceed a threshold (For example, 30 percent).
Response: We appreciate the commenters' position. Dissemination of C-section rates permits hospitals to compare their performance to other institutions, not just to high-rate institutions. We intend to take the commenters' recommendations into consideration as we continue to evaluate PC-02 for adoption into the Hospital IQR Program.
Comment: Several commenters did not support the measure because of their belief that the lack of risk adjustment would disadvantage referral centers for high risk deliveries and because it does not exclude eclampsia and pre-eclampsia patients.
Response: We appreciate the commenters' concern. As previously noted, The Joint Commission removed the risk adjustments from this measure in 2016, after considering the recommendations of the Technical Advisory Panel.[632] We will continue to monitor this issue and The Joint Commission's ongoing attention to it.
Comment: A number of commenters addressed the data elements necessary to calculate this measure. A few commenters stated that the necessary data elements are generally already captured by their EHRs, and a commenter noted they could calculate this measure. Meanwhile, other commenters questioned the availability of data elements for this measure from current EHRs. A few commenters supported feasibility testing before implementation of this measure.
Response: We thank the commenters for their perspective. Any future adoption of this measure would be made through notice and comment rulemaking. Hospitals and EHRs would receive advance notice for application development and testing. We appreciate the recommendation for additional feasibility testing and will take it into consideration.
Comment: A commenter could not find specifications for this measure.
Response: This measure is stewarded by The Joint Commission and the NQF has published a detailed specification for calculating this measure.[633 634]
Comment: A few commenters noted the limited number of Medicare-funded C-sections and expressed concern that the measure rate would be calculated using only Medicare-funded deliveries.
Response: As previously discussed in more detail, the measure includes all births regardless of payer.
Comment: A few commenters did not support the measure because it lacks current NQF endorsement.
Response: As previously discussed further in the proposed rule and in this section, the chart-based version of this measure has NQF endorsement.[635] The MAP Coordinating Committee encouraged The Joint Commission to resubmit the eCQM version of PC-02 to the NQF for endorsement with additional clarifying data.[636] The MAP's Final Report of February 15, 2019, conditionally supports the PC-02 eCQM for rulemaking pending NQF evaluation and endorsement.[637] We will continue to monitor the NQF endorsement process.
We thank the commenters and we will consider their views as we develop future policy regarding the potential inclusion of the PC-02 eCQM in the Hospital IQR Program.
9. Accounting for Social Risk Factors: Update on Confidential Reporting of Stratified Data for Hospital Quality Measures
a. Background
We first sought public comment on potentially publicly reporting Hospital IQR Program measure data stratified by social risk factors in the FY 2017 IPPS/LTCH PPS proposed rule (81 FR 57167 through 57168). In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38404), we explained that due to the complexity of interpreting stratified measure data, we would first consider confidentially reporting such data prior to any future public display on the Hospital Compare website. We also noted that providing confidential hospital-specific reports (HSRs) would enable us to obtain hospital feedback on reporting options and ensure the information is valid, reliable, and understandable prior to any future public display (82 FR 38404).
In the FY 2018 IPPS/LTCH PPS rulemaking (82 FR 20070 through 20074; 38403 through 38409), we presented and responded to comments on whether to provide hospitals with confidential results of the Hospital 30-Day, All-Cause, Risk-Standardized Readmission Rate (RSRR) Following Pneumonia Hospitalization (NQF #0506) (Pneumonia Readmission measure) and the Hospital 30-Day, All-Cause, Risk-Standardized Mortality Rate Following Pneumonia Hospitalization (NQF #0468) (Pneumonia Mortality measure) stratified by patient dual eligible status as early as summer of 2018, and described two potential methodologies designed to illuminate potential disparities by calculating outcome measure results stratified by patient dual eligible status (a within-hospital method and an across-hospital method).[638] We selected the two pneumonia measures as the first measures to potentially stratify because pneumonia is a condition that is common in the elderly population and because the results of both measures are publicly reported for a large cohort of hospitals (83 FR 41598).[639] We also explained that the additional information provided by the two disparity methods supplements the overall readmission and mortality measure rates publicly reported on the Hospital Compare website by highlighting disparities based on patient dual eligible status (82 FR 38405).
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41598), we explained that as a first step, in the interest of simplicity and minimizing confusion for hospitals, we planned to provide hospitals with confidential HSRs containing stratified results of the Pneumonia Readmission measure only, using both disparity methods, during a month-long confidential reporting period in late summer of 2018. We also noted that for the future, we were considering: (1) Expanding our efforts to provide stratified data in confidential HSRs for other measures; (2) including other social risk factors beyond dual eligible status in confidential HSRs; and (3) eventually, making stratified data publicly available on the Hospital Compare website (83 FR 41598).
Confidential HSRs containing the results of Pneumonia Readmission measure data using the two disparity methods (disparity results) were made available for hospitals and their QIN-QIOs to download through the QualityNet Secure Portal from August 24 to September 24, 2018. The confidential HSRs also contained additional information to enable a more meaningful comparison and comprehensive assessment of the quality of care for dual eligible patients, including a hospital's overall Pneumonia Readmission measure rate and State and national results for each disparity method. To ensure hospitals and stakeholders would have sufficient information to understand and interpret their disparity results during the confidential reporting period, background materials and educational resources were posted on the QualityNet website, including detailed instructions for interpreting a hospital's HSR and a technical report describing the two disparity methods in detail.[640] We also hosted a National Provider Call and established a monitored email inbox to receive and address questions and comments from hospitals and other stakeholders during the confidential reporting period.641
b. Additional Confidential Reporting of Measures Stratified Using Two Disparity Methods
As previously noted, we have been considering, among other things, expanding our efforts to provide stratified data using the two disparity methods in confidential HSRs for additional measures. Although our preliminary efforts have focused on the Pneumonia Readmission measure, the two disparity methods previously used can be applied to other outcome measures. We believe that it is important to expand our efforts to provide disparity results for additional outcome measures because we believe that providing the results of both disparity methods alongside a hospital's measure data, as a point of reference, allows for a more meaningful comparison. As mentioned, the disparity results could supplement the overall measure data already publicly reported on the Hospital Compare website by providing additional information regarding disparities measured within individual hospitals and across hospitals nationally. The disparity results thus enable a more comprehensive assessment of quality of care for patients with social risk factors and identifies where disparities in health care may exist. This approach also furthers Recommendation 2 of NQF's Disparities Project final report to use and prioritize stratified health equity outcome measures, wherein the two disparity methods were highlighted as exemplary of health equity performance measure alignment such that data collection burden is minimized, measure impact is maximized, and peer group comparisons are enabled.[642] We believe hospitals can use their results from the disparity methods to identify and develop strategies to reduce disparities in the quality of care for patients with social risk factors, including targeted improvement efforts to improve health outcomes for all of their patients, those with and without social risk factors (83 FR 41598). As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41599), the two disparity methods do not place any additional collection or reporting burden on hospitals because dual eligible data are readily available in claims data. For additional information on the two disparity methods, we refer readers to the technical report describing the methods in detail,[643] as well as the FY 2018 IPPS/LTCH PPS final rule (82 FR 38405 through 38407).
In April 2019, we continued to provide confidential reporting of disparity results for the Pneumonia Readmission measure in the confidential HSRs for claims-based measures that were made available for hospitals to download through the QualityNet Secure Portal as was done in 2018. We are also planning to expand our efforts to apply the two disparity methods to additional outcome measures for confidential reporting in a phased manner. As a next step, in the spring of 2020, we plan to add to the confidential HSRs for claims-based measures the confidential reporting of disparity results for five additional claims-based condition- and procedure-specific readmission measures as follows: (1) Hospital 30-Day, All-Cause, Risk-Standardized Readmission Rate (RSRR) Following Acute Myocardial Infarction (AMI) Hospitalization (NQF #0505) (AMI Readmission measure); (2) Hospital 30-Day, All-Cause, Risk-Standardized Readmission Rate (RSRR) Following Coronary Artery Bypass Graft (CABG) Surgery (NQF #2515) (CABG Readmission measure); (3) Hospital 30-Day, All-Cause, Risk-Standardized Readmission Rate (RSRR) Following Chronic Obstructive Pulmonary Disease (COPD) Hospitalization (NQF #1891) (COPD Readmission measure); (4) Hospital 30-Day, All-Cause, Risk-Standardized Readmission Rate (RSRR) Following Heart Failure (HF) Hospitalization (NQF #0330) (HF Readmission measure); and (5) Hospital-Level 30-Day, All-Cause, Risk-Standardized Readmission Rate (RSRR) Following Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA) (NQF #1551) (THA/TKA Readmission measure). To simplify and minimize the number of confidential HSRs that hospitals receive, going forward we plan to include hospitals' disparity results in the regular annual confidential HSRs for claims-based measure results that are made available for hospitals to download through the QualityNet Secure Portal each spring, as opposed to a separate confidential HSR for only the confidential reporting of disparity results as was done for the first confidential reporting of disparity results for the Pneumonia Readmission measure in late summer of 2018.
We believe that expanding our efforts by providing disparity results for the six condition- and procedure-specific readmission measures as previously discussed, while a different set of calculations than those used in the Hospital Readmissions Reduction Program, can complement the stratified methodology used to assess a hospital's performance on these measures for payment penalty scoring purposes under the Hospital Readmissions Reduction Program. To implement the requirements of the 21st Century Cures Act, the Hospital Readmissions Reduction Program developed a stratification methodology to account for social risk factors by which it assigns hospitals into five peer groups based on proportion of dual eligible stays, and assesses hospital performance relative to the performance of hospitals within the same peer group.[644] While this approach is used by the Hospital Readmissions Reduction Program for purposes of payment calculations, the two disparity methods are intended to account for social risk factors by providing additional information that identifies potential disparities in care provided to dual eligible patients within individual hospitals and across hospitals nationally. We believe that providing data from the two disparity methods for the readmission measures complements the payment stratification approach using these measures under the Hospital Readmissions Reduction Program by increasing transparency around, and contributing to an improved understanding of, differences in care on the basis of patient dual eligible status. The two disparity methods and the stratified methodology used by the Hospital Readmissions Reduction Program are all part of CMS' broader efforts to account for social risk factors in quality measurement and value-based purchasing programs. We note that the confidential reporting of disparity results discussed in this section is not driven by a specific quality program, but rather, is intended to supplement already publicly reported measure performance data and is only one part of CMS' overall strategy for accounting for social risk factors. We refer readers to section IV.G.11. of the preamble of this final rule for a similar discussion under the Hospital Readmissions Reduction Program. In the future, we also plan to provide confidential reporting of disparity results for additional outcome measures included in other quality programs.
We plan to continue soliciting feedback from hospitals based on their experiences with the confidential disparity methods reporting process, which will allow hospitals to understand their disparity results prior to any potential future public reporting. As discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41600), we have not yet determined future plans with respect to publicly reporting stratified data, and intend to continue to engage with hospitals and relevant stakeholders about their experiences with and recommendations for the stratification of measure data, and to ensure the reliability of such data before proposing to publicly display stratified measure data in the future. Any proposal to display stratified quality measure data on the Hospital Compare website would be made through future rulemaking.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19495), we invited public comment on our plans to expand our efforts to apply the disparity methods to additional outcome measures for confidential reporting in a phased manner, specifically for five additional measures (AMI Readmission measure; CABG Readmission measure; COPD Readmission measure; HF Readmission measure; and THA/TKA Readmission measure) starting in spring of 2020, and additional outcome measures after spring of 2020, as previously discussed. We refer readers to section IV.G.11. of the preamble of this final rule for a similar discussion under the Hospital Readmissions Reduction Program.
Comment: Many commenters supported our plan to continue to provide hospitals with confidential hospital-specific reports on the Pneumonia Readmission measure using the two disparity methods and to expand that effort to include five additional readmission measures. Several of these commenters specifically believed that the effort would be useful to hospitals. Some commenters noted that it would help hospitals identify potential disparities in care, implement targeted improvement efforts, and reduce disparities in the quality of care for this vulnerable population. A commenter believed the information in the confidential HSRs will help hospitals and CMS make appropriate decisions as they consider disparities and risk-adjustment. A few commenters noted that dual eligible status is a reasonable social risk factor to begin using when assessing for disparities in care for quality measurement and value-based purchasing programs.
Response: We thank commenters for their support for our efforts to provide data on disparities to hospitals. At present, dual eligible status is the only social risk factor used for assessing disparities in hospital outcomes. We continue to explore the use of additional social risk factors for the hospital disparity methods.
Comment: Several commenters requested that CMS provide sufficient opportunity to review and understand the stratified performance and methodology used to develop these reports. They appreciated CMS' intention to remain engaged with stakeholders and to solicit feedback on hospital experiences and recommendations, including the format and usefulness of the reports. A commenter requested that CMS provide educational materials to help stakeholders interpret the information.
Response: We intend to continue to provide educational resources for stakeholders as they continue to become familiar with the data provided from the two disparity methods provided in the confidential reports, including the measure methodology overview, fact sheet, and frequently asked questions resources.[645]
Comment: A few commenters encouraged CMS to make the disparity methods' results in the confidential HSRs available to the public to foster transparency. A few commenters believed that any consideration of publicly reporting these data in the future should be proposed as part of notice and comment rulemaking. A commenter believed that stratified data should not be publicly reported but should be used by hospital staff for internal purposes only in identifying disparities in their patient populations. A commenter encouraged CMS to make the data public once hospitals are able to review and correct their data. A commenter opposed CMS privately sharing reports containing social risk factor data with hospitals because of a belief that the Hospital Compare website should inform the public on how hospitals differentiate in quality and safety and should be fully transparent to the public. Another commenter suggested that CMS be cautious in making these reports public as hospitals are just beginning to gain familiarity with them. A few commenters encouraged CMS to engage with stakeholders before any future public reporting. A few commenters believed it is important to ensure the reliability of the measure data using the two disparity methods before proposing to publicly display it and encouraged CMS to continue to engage with stakeholders to ensure that the data is accurate, fairly assesses hospitals, and is understandable to patients before it is made public. A commenter encouraged CMS to seek input from stakeholders on the usefulness of confidential HSRs before publicly reporting such data, specifically, whether these reports support continuous quality improvement efforts.
Response: The measure data used in the disparity methods are, except for dual eligibility status, the same as the data used in validated and NQF endorsed publicly reported measures. Dual eligibility data have been assessed separately for reliability and consistency of coding across states. In addition, we believe confidential reporting of the measure data using the two disparity methods will enable us to obtain hospital feedback on reporting options and provide additional certainty that the information is valid, reliable, and understandable prior to any future public display. It will also allow hospitals to better understand the complex data from the two disparity methods prior to any potential future public reporting.
We have not yet determined future plans with respect to publicly reporting data using the two disparity methods.
We intend to continue to engage with hospitals and relevant stakeholders about their experiences with and recommendations for the results from the two disparity methods and to ensure the accuracy and reliability of the results from the two disparity methods before proposing to publicly display them in the future. Any proposal to display measure data based on the two disparity methods on the Hospital Compare website would be made through future notice and comment rulemaking.
Comment: A commenter believed that the differences in the results between the two disparity methods used in the confidential reports as compared to the stratified methodology used by the Hospital Readmissions Reduction Program could lead to confusion and may yield conflicting information that may not contribute to informing patients and the public. The commenter recommended that CMS study these differences, the potential impact on decision-making each may have, and what efforts should be made to harmonize these approaches before publicly reporting the data.
Response: We appreciate commenter's feedback regarding the importance of harmonization with existing quality programs, such as the Hospital Readmissions Reduction Program. We believe these two disparity methods complement each other in that they use the same social risk factor and serve two complementary purposes. The Hospital Readmissions Reduction Program stratifies hospitals based on dual-eligible proportion and compares a hospital's excess readmissions to other hospitals in its peer group to assess a hospital's performance, as mandated by the 21st Century Cures Act,[646] whereas the disparity methods discussed in this section highlight opportunities to close the gap in performance among different patient groups. We will continue to examine alignment, wherever appropriate, and intend to continue to engage with hospitals and relevant stakeholders about their experiences with the two disparity methods.
Comment: A commenter suggested that attribution model details for each measure be included within the respective programs' measures' technical specifications guides before publicly reporting data using the two disparity methods because they believed it is important to be clear about who is responsible for the reported outcomes and performance rates.
Response: To minimize the possibility of confusion, the attribution used when applying the disparity methods mirror those used by the corresponding measure in the Hospital Readmissions Reduction Program. Attribution details and other technical specifications for the readmission measures are publicly available in Measure Methodology Reports on our QualityNet website.[647]
Comment: A few commenters expressed concern with stratifying measure data based only on dual eligible status. A commenter noted that dual eligibility may be sensitive to differences in state coverage and benefit policies, and may not fully reflect the level of poverty in communities. A commenter believed that more information may be needed to specify the factors that result in higher spending and/or poorer health care outcomes. A few commenters recommended that CMS continue to consider and refine the social risk factors for stratification in confidential HSRs and consider additional factors that might affect outcomes or result in higher spending, including race, ethnicity, geographic area, sex, disability, education, and access to health care. A commenter expressed concern about the reliability of race and ethnicity data if CMS should consider stratifying hospital quality data by such factors and recommended that CMS develop a proposal to improve the collection of race and ethnicity data, or propose how to promote public transparency using data that are of mixed quality, before reporting such data publicly.
Response: At present, dual eligibility is the only social risk factor used in the disparity methods. We have focused our initial efforts on providing disparity results based on dual eligible status because of strong evidence demonstrating worse health outcomes among dual eligible Medicare beneficiaries, and because reliable information is readily available in CMS administrative claims data. Because dual eligible status is available in CMS administrative data, it also does not require any additional reporting by hospitals for the purposes of applying the disparity methods. With respect to commenter's concern about the differences in state policies, the disparity methods evaluate differences in hospital quality only for adults 65 years and above. Federal minimum standards for allowable income and assets exist for older adults, contributing to more uniformity in Medicaid eligibility status across states relative to other groups, although state-level differences in eligibility standards for optional coverage pathways and benefits are noted. Our internal analyses accounting for state Medicaid eligibility policies reveal no substantive differences in the disparity method results. We continue to examine the impact of state Medicaid policies on the disparity methods. We also continue to explore opportunities to account for additional social risk factors in the future, including evaluating new sources of social risk factor data and how to capture such data, engaging with stakeholders, and examining the availability and feasibly of accounting for social risk factors which might influence quality outcome measures.
Comment: A commenter recommended that CMS consider data concerns related to the use of hospital quality data stratified by sociodemographic factors for hospital-acquired infection measures due to the concern that limited sample sizes at the individual hospital level could limit the statistical reliability of reporting quality measures by race or other sociodemographic characteristics.
Response: We do not currently have plans to provide stratified data for hospital-acquired infection measures, but will take commenter's concerns into account as we continue to consider expanding our efforts to provide stratified data in confidential HSRs for other measures.
Comment: Several commenters recommended that CMS adjust for social risk factors at the measure level for quality reporting and value-based programs, with some commenters expressing concern that hospitals that disproportionately care for vulnerable patient populations are disadvantaged or that customers could be misled with regard to the quality of care provided. However, another commenter expressed concern about incorporating social risk factors at the measure level because of a concern that it could mask the quality of care provided to people of different backgrounds. A commenter suggested providing both risk-adjusted and unadjusted results to providers.
Response: The primary objectives of the disparity methods are to assess and report disparities of care as reflected by differences in outcomes for patients with social risk factors, both within and across hospitals. It is important to note that adjusting for social risk factors within the quality measures would not serve this objective.
Risk adjustment is one strategy which can be used to account for patient-level risk associated with social risk factors in the statistical model to incorporate such factors into calculating expected outcome rates for providers. Extensive previous work from ASPE, National Academies of Science, Engineering and, Medicine (NAM), and NQF have provided guiding recommendations towards the incorporation of risk adjustment for social risk factors at the patient level.[648 649 650]
The disparity methods we have presented here serves a complementary purpose and is intended to allow examination of outcome differences between subgroups of patients. Providing information to providers on disparity results aims to support transparency around disparate health outcomes and incentivize improvements in care for patients with social risk factors. The goals of the methods presented are to demonstrate whether a gap in outcomes exists between patients with and without a given social risk factor (such as dual eligibility) within a single hospital, and to provide comparative information on hospital performance for patients with social risks across all hospitals.
We also note, that applying the two disparity methods furthers Recommendation 2 of NQF's Disparities Project final report to use and prioritize stratified health equity outcome measures, wherein the two disparity methods were highlighted as an exemplary of health equity performance measure alignment such that data collection burden is minimized, measure impact is maximized, and peer group comparisons are enabled.[651] We will continue to explore multiple options to account for the effect of social risk factors on quality measures and in quality programs.
Comment: A few commenters recommended that CMS improve data capture to better allow for risk adjustment related to social determinants of health, including collection of such data, including non-clinical data, via EHRs.
Response: We continue to explore opportunities to account for additional social risk factors in the future, including evaluating new sources of social risk factor data and how to capture such data, engaging with stakeholders, and examining the availability and feasibly of accounting for social risk factors which might influence quality outcome measures.
We thank the commenters for their feedback and suggestions. We will take them into account and consider commenters' views as we develop future policies regarding the accounting for social risk factors and reporting of disparity data.
10. Form, Manner, and Timing of Quality Data Submission
a. Background
Sections 1886(b)(3)(B)(viii)(I) and (b)(3)(B)(viii)(II) of the Act state that the applicable percentage increase for FY 2015 and each subsequent year shall be reduced by one-quarter of such applicable percentage increase (determined without regard to sections 1886(b)(3)(B)(ix), (xi), or (xii) of the Act) for any subsection (d) hospital that does not submit data required to be submitted on measures specified by the Secretary in a form and manner, and at a time, specified by the Secretary. Previously, the applicable percentage increase for FY 2007 and each subsequent fiscal year until FY 2015 was reduced by 2.0 percentage points for subsection (d) hospitals failing to submit data in accordance with the previous description. In accordance with the statute, the FY 2020 payment determination will begin the sixth year that the Hospital IQR Program will reduce the applicable percentage increase by one-quarter of such applicable percentage increase.
In order to participate in the Hospital IQR Program, hospitals must meet specific procedural, data collection, submission, and validation requirements. For each Hospital IQR Program payment determination, we require that hospitals submit data on each specified measure in accordance with the measure's specifications for a particular period of time. The data submission requirements, Specifications Manual, and submission deadlines are posted on the QualityNet website at: http://www.QualityNet.org/. The technical specifications used for electronic clinical quality measures (eCQMs) are contained in the CMS Annual Update for the Hospital Quality Reporting Programs (Annual Update). We generally update the measure specifications on an annual basis through the Annual Update, which includes code updates, logic corrections, alignment with current clinical guidelines, and additional guidance for hospitals and electronic health record (EHR) vendors to use in order to collect and submit data on eCQMs from hospital EHRs. The Annual Update and implementation guidance documents are available on the Electronic Clinical Quality Improvement (eCQI) Resource Center website at: https://ecqi.healthit.gov/. For example, for the CY 2019 reporting period/FY 2021 payment determination, hospitals would need to submit eCQM data using the May 2018 Annual Update and any applicable addenda. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41602 through 41603), in which we discuss the transition to Clinical Quality Language (CQL) for all eCQM specifications published in CY 2018 for the CY 2019 reporting period/FY 2021 payment determination and subsequent years (beginning with the Annual Update that was published in May 2018 for implementation in CY 2019).
Hospitals must register and submit quality data through the secure portion of the QualityNet website. There are safeguards in place in accordance with the HIPAA Privacy and Security Rules to protect patient information submitted through this website. See 45 CFR parts 160 and 164, subparts A, C, and E.
b. Procedural Requirements
The Hospital IQR Program's procedural requirements are codified in regulation at 42 CFR 412.140. We refer readers to these codified regulations for participation requirements, as further explained by the FY 2014 IPPS/LTCH PPS final rule (78 FR 50810 through 50811) and the FY 2017 IPPS/LTCH PPS final rule (81 FR 57168). In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19496), we did not propose any changes to these procedural requirements.
c. Data Submission Requirements for Chart-Abstracted Measures
We refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51640 through 51641), the FY 2013 IPPS/LTCH PPS final rule (77 FR 53536 through 53537), and the FY 2014 IPPS/LTCH PPS final rule (78 FR 50811) for details on the Hospital IQR Program data submission requirements for chart-abstracted measures. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19496), we did not propose any changes to the data submission requirements for chart-abstracted measures.
d. Reporting and Submission Requirements for eCQMs
(1) Background
For a discussion of our previously finalized eCQMs and policies, we refer readers to the FY 2014 IPPS/LTCH PPS final rule (78 FR 50807 through 50810; 50811 through 50819), the FY 2015 IPPS/LTCH PPS final rule (79 FR 50241 through 50253; 50256 through 50259; and 50273 through 50276), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49692 through 49698; and 49704 through 49709), the FY 2017 IPPS/LTCH PPS final rule (81 FR 57150 through 57161; and 57169 through 57172), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38355 through 38361; 38386 through 38394; 38474 through 38485; and 38487 through 38493), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41567 through 41575; 83 FR 41602 through 41607).
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38361), we finalized eCQM reporting and submission requirements such that hospitals are required to report only one, self-selected calendar quarter of data for four self-selected eCQMs for the CY 2018 reporting period/FY 2020 payment determination. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41603 through 41604), we extended the same eCQM reporting and submission requirements, such that hospitals are required to report one, self-selected calendar quarter of data for four self-selected eCQMs for the CY 2019 reporting period/FY 2021 payment determination.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19496 through 19497), we proposed to establish eCQM reporting and submission requirements for the CY 2020 reporting period/FY 2022 payment determination through the CY 2022 reporting period/FY 2024 payment determination, as detailed in this final rule.
(2) Reporting and Submission Requirements for eCQMs for the CY 2020 Reporting Period/FY 2022 Payment Determination
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19496), for the CY 2020 reporting period/FY 2022 payment determination, we proposed to extend the current eCQM reporting and submission requirements, such that hospitals would be required to report one, self-selected calendar quarter of data for four self-selected eCQMs. We believe continuing the same eCQM reporting and submission requirements is appropriate because it offers hospitals reporting flexibility and does not increase the information collection burden on data submitters, allowing them to shift resources to support system upgrades, data mapping, and staff training related to eCQM documentation and reporting.
We refer readers to section VIII.D.6.d.(1). of the preamble of this final rule where we discuss a similar proposal in the Promoting Interoperability Programs for the CY 2020 reporting period.
We note that the commenters who commented on the proposal for the CY 2020 reporting period uniformly also provided similar comments for the CY 2021 reporting period. We therefore refer readers to section VIII.A.10.D.(3). of the preamble of this final rule, where we provide a summary of the comments and responses that apply to the proposals for both the CY 2020 and CY 2021 reporting periods.
(3) Reporting and Submission Requirements for eCQMs for the CY 2021 Reporting Period/FY 2023 Payment Determination
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19496 through 19497), for the CY 2021 reporting period/FY 2023 payment determination, we proposed to extend the same eCQM reporting and submission requirements, such that hospitals would continue to be required to report one, self-selected calendar quarter of data for four self-selected eCQMs for the same reasons as previously discussed. We refer readers to section VIII.D.6.d.(1). of the preamble of this final rule where we discuss a similar proposal in the Medicare Promoting Interoperability Program.
We note that the following comment and response summaries reflect the comments received on proposals for both the CY 2020 reporting period and the CY 2021 reporting period.
Comment: Many commenters supported our proposals to extend the current eCQM reporting and submission requirements, such that hospitals would be required to report one, self-selected calendar quarter of data for four self-selected eCQMs for the CY 2020 and CY 2021 reporting periods. Several commenters appreciated and supported the consistency of the proposals because they believe it will allow vendors and hospitals more time to acclimate to electronic reporting, adopt technology, implement and test measures, and prepare for new measures. One commenter supported the proposal because of their belief that it reduces regulatory burden and gives hospitals the flexibility to focus on measures that are most meaningful to their quality improvement priorities. One commenter specifically noted their support for the proposed CY 2021 eCQM reporting and submission requirements, but was silent as to the proposal for CY 2020.
Response: We appreciate the commenters' support.
Comment: A few commenters recommended that we also continue these same reporting and submission requirements for future years. A few commenters suggested that the requirement to report only one quarter of data be made permanent to allow vendors and hospitals to plan into the future.
Response: We thank the commenters for their recommendations. However, we reiterate our previously stated goal of incrementally increasing the use of EHR data for quality measurement. We believe taking an incremental approach to increasing electronic reporting will allow hospitals and vendors to acclimate to electronic reporting. In keeping with that goal, we are finalizing requirements for the CY 2022 reporting period in this final rule such that hospitals will be required to submit one, self-selected calendar quarter of data for: (1) Three self-selected eCQMs; and (2) the finalized Safe Use of Opioids—Concurrent Prescribing eCQM with a clarification and update, for a total of four eCQMs. We refer readers to section XIII.A.10.d.(4). of the preamble of this final rule, for a discussion of eCQM reporting and submission requirements for the CY 2022 reporting period/FY 2024 payment determination. Any eCQM reporting and submission requirements beyond that time will be addressed in future notice and comment rulemaking.
Comment: A few commenters urged us to consider other approaches to support the advancement of eCQM reporting. A commenter encouraged us to allow hospitals to voluntarily substitute eCQM versions for the chart-abstracted versions of the same measures and suggested that we could establish a bonus structure for hospitals that were willing to progress beyond the standard reporting requirements. Another commenter recommended that we require thresholds be met for the eCQMs on which hospitals chose to report, that we allow for comparisons in performance, and that we penalize facilities for poor performance.
Response: We appreciate the commenters' feedback and recommendations, and will take these recommendations into consideration as we assess how to advance eCQM reporting in the Hospital IQR Program. Increasing the use of EHR data is a goal of the Hospital IQR Program. We remind readers, however, that the Hospital IQR Program is a pay-for-reporting program rather than a pay-for-performance program, meaning the impact on payment is based on whether a hospital complies with the reporting requirements of the program, rather than how well a hospital performs on individual measures. At this time, the Hospital IQR Program does not publicly report eCQM data and any future public reporting of eCQM data would be established through notice and comment rulemaking.
Regarding the commenter's recommendation to allow voluntary substitution of eCQM versions for the chart-abstracted versions of the same measures, we note that following the removal of several chart-abstracted clinical process of care measures in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41562 through 41567), the only chart-abstracted measures that remain in the Hospital IQR Program are the PC-01 and Sepsis measures. The eCQM version of the PC-01 measure was removed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41569) because the measure data are already collected and publicly reported in the chart-abstracted form of this measure in the Hospital IQR Program. We also note that it would not be feasible for hospitals to submit eCQM data for the Sepsis measure as that measure is not currently electronically specified and remains a chart-abstracted measure in the Hospital IQR Program at this time.
Comment: A commenter expressed concerns about our self-selection policies and recommended that we mandate the specific eCQMs for hospitals to report and that we require hospitals to submit a year's worth of data. The commenter noted that when the reporting period is limited to one quarter of data, hospitals can select the quarter in which their rates are the best and expressed concern that rural hospitals have trouble meeting the minimum reporting threshold when the measurement period is one quarter. Another commenter suggested that if we begin to require a full year of reporting for eCQMs, that we should align the reporting period with the calendar year.
Response: We appreciate the commenters' feedback and recommendations, and will take these recommendations into consideration as we assess how to advance eCQM reporting in the Hospital IQR Program. Regarding the commenter's concerns about allowing self-selection of eCQMs and recommendation to mandate specific eCQMs, as further discussed in this final rule, we are finalizing requirements for the CY 2022 reporting period such that hospitals will be required to submit one, self-selected calendar quarter of data for: (1) The finalized Safe Use of Opioids—Concurrent Prescribing eCQM with a clarification and update; and (2) three self-selected eCQMs, for a total of four eCQMs, as part of our goal to incrementally increase eCQM reporting requirements as hospitals continue to gain experience with eCQMs. Any additional changes to our eCQM reporting requirements would be done through notice and comment rulemaking. We will take under consideration for future reporting policies the commenter's concerns about the ability of rural hospitals to meet the minimum reporting threshold based on one quarter of data, and in the meantime, note our zero denominator declaration and case threshold exemption policies in place for eCQM reporting.[652] Finally, while we are not yet requiring the reporting of a full year of data for eCQMs, we will take the commenter's suggestion to align with the calendar year into consideration for the future.
Comment: A few commenters urged us not to publicly report eCQM data for some time. One commenter recommended that CMS develop a feedback loop to monitor for unintended consequences for all quality measures before publicly reporting eCQM data.
Response: At this time, the Hospital IQR Program does not publicly report eCQM data and any future public reporting of eCQM data would be established through notice and comment rulemaking. There are a number of channels for stakeholders to provide feedback on an eCQM throughout the eCQM lifecycle.[653] The eCQI Resource Center provides numerous current resources to support electronic clinical quality improvement.[654] Within the eCQI Resource Center, the Collaborative Measure Development (CMD) Workspace [655] brings together a set of interconnected resources, tools, and processes to promote clarity, transparency, and better interaction across stakeholder communities that develop, implement, and report eCQMs. During the measure development process, stakeholders may also provide feedback through public comment periods,[656] and ONC JIRA's issue tracker for measures under development.[657] We further note that the value sets for both proposed eCQMs and eCQMs that have been finalized and adopted through rulemaking can be found at the Value Set Authority Center's website.[658]
After consideration of the public comments we received, we are finalizing our proposals as proposed for both the CY 2020 reporting period/FY 2022 payment determination and the CY 2021 reporting period/FY 2023 payment determination: To extend the same eCQM reporting and submission requirements, such that hospitals would continue to be required to report one, self-selected calendar quarter of data for four self-selected eCQMs.
(4) Reporting and Submission Requirements for eCQMs for the CY 2022 Reporting Period/FY 2024 Payment Determination
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19497), for the CY 2022 reporting period/FY 2024 payment determination, we proposed to modify the eCQM reporting and submission requirements, such that hospitals would be required to report one, self-selected calendar quarter of data for: (1) Three self-selected eCQMs; and (2) the proposed Safe Use of Opioids—Concurrent Prescribing eCQM, for a total of four eCQMs. We note that the number of calendar quarters of data and total number of eCQMs required would remain the same.
This proposal was made in conjunction with our proposal discussed in section VIII.A.5.a.(1). of the preamble of this final rule, in which we proposed to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination. We believe this measure has the potential to reduce preventable mortality and costs associated with other adverse events related to opioid use. As discussed in section VIII.A.5.a.(1). of the preamble of this final rule, concurrent opioid or opioid-benzodiazepine prescription use contributes significantly to the overall population's risk of opioid overdose. Currently, however, no measure exists to assess nationwide rates of concurrent prescribing of opioids and benzodiazepines at the hospital-level.
In developing this proposal, we also considered an alternative whereby hospitals would have the option to select one of the two proposed opioids-related eCQMs, the Safe Use of Opioids—Concurrent Prescribing eCQM or the Hospital Harm—Opioid-Related Adverse Events eCQM, as their fourth required eCQM. However, such an approach would add complexity to the eCQM reporting requirements, and we believe that the Safe Use of Opioids—Concurrent Prescribing eCQM is more closely related to combating the current opioid epidemic, as previously discussed and in section VIII.A.5.a. of the preamble of this final rule, than the Hospital Harm—Opioid-Related Adverse Events eCQM, which is focused on improved monitoring of patients who receive opioids during hospitalization.
In the proposed rule, we proposed that if our proposal to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination were finalized, while this measure would be available for hospitals to select as one of their four self-selected eCQMs for the CY 2021 reporting period, all hospitals would be required to report this eCQM beginning with the CY 2022 reporting period/FY 2024 payment determination. We believe this measure would provide valuable information on this area of high-risk prescribing to providers, and further our efforts to combat the negative impacts of the opioid crisis. We also believe this proposal is consistent with CMS' goal of incrementally increasing the use of EHR data for quality measurement and is responsive to the feedback of some stakeholders urging a faster transition to full electronic reporting.[659]
In the proposed rule, we noted that this proposal was contingent on finalization of our proposal discussed in section VIII.A.5.a.(1). of the preamble of this final rule to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM. We also refer readers to section VIII.D.6.d.(2). of the preamble of this final rule for a discussion of a similar proposal by the Medicare Promoting Interoperability Program.
Comment: Many commenters supported CMS' proposal for CY 2022 reporting period/FY 2024 payment determination to modify the eCQM reporting and submission requirements, such that hospitals would be required to report one, self-selected calendar quarter of data for: (1) Three self- selected eCQMs; and (2) the proposed Safe Use of Opioids—Concurrent Prescribing eCQM, for a total of four eCQMs. Most of these commenters focused their comments on the proposal to require reporting of the Safe Use of Opioids—Concurrent Prescribing measure. One commenter specifically expressed appreciation for the continued flexibility of the eCQM reporting requirements. Another commenter appreciated that our proposal would standardize the measures required for reporting. One commenter expressed their belief that the significance of the opioid crisis justifies requiring reporting on the Safe Use of Opioids—Concurrent Prescribing eCQM. Another commenter requested that we consider approaches to require the reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM earlier than the CY 2022 reporting period to capture a greater volume of data.
Response: We note that the proposal to require reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM for the CY 2022 reporting period was timed to prevent increasing the complexity of the eCQM reporting requirements too quickly, while also taking into consideration that this measure seeks to combat the negative impacts of the opioid crisis and has the potential to reduce preventable mortality and costs associated with other adverse events related to opioid use. Regarding the commenter recommending to require reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM earlier than CY 2022, we believe that adopting the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period is appropriate to give hospitals time to implement the measure and submit data on the measure as one of four eCQMs for the CY 2021 reporting period/FY 2023 payment determination should they wish to before it is required as one of the four eCQMs for the CY 2022 reporting period/FY 2024 payment determination. We strongly encourage hospitals to report the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period as one of their eCQMs.
Comment: A few commenters supported required reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM, but suggested that a few exclusions be added to the measure and potentially delay required reporting by 1 year.
Response: We refer readers to section XIII.A.5.a.(1). of the preamble of this final rule where we discuss finalizing the adoption of the Safe Use of Opioids—Concurrent Prescribing eCQM with a clarification and update, including a discussion of the measure exclusions as well as exclusions that were considered during the measure development process but not incorporated into the specifications. As discussed in that section, we are finalizing our proposal to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM with a clarification and update beginning with the CY 2021 reporting period/FY 2023 payment determination. We believe requiring reporting on the measure beginning with the CY 2022 reporting period is an appropriate timeframe, as it will enable hospitals sufficient time to work through implementation, testing, and reporting challenges. In addition, hospitals may submit data on the measure as one of four eCQMs for the CY 2021 reporting period/FY 2023 payment determination should they wish to before the measure is required as one of four eCQMs for the CY 2022 reporting period/FY 2024 payment determination.
Comment: A commenter supported required reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM, but suggested that we not publicly report data until further testing has demonstrated the measure's validity and reliability.
Response: We disagree that the Safe Use of Opioids—Concurrent Prescribing eCQM has not been demonstrated to be valid and reliable. We refer readers to section XIII.A.5.a.(1). of the preamble of this final rule for a discussion of how this measure was tested for feasibility, reliability, and validity and received NQF endorsement. We further note that eCQM measure data are currently not publicly reported. We will provide confidential feedback reports to hospitals reporting this measure in advance of any public reporting. We believe that these advance reports will provide hospitals with additional time and information to ask CMS questions and learn more about the measure before public reporting. Any future plans for publicly reporting eCQM data would be conducted through rulemaking.
Comment: A commenter stated their belief that it would be premature to require electronic reporting before all measures are fully electronically specified and field tested and also expressed concern about the extensive impact that eCQM adoption has on hospital resources.
Response: Regarding commenters' concerns about the level of testing that eCQMs have undertaken, we note that eCQMs, like all other types of quality measures in the Hospital IQR Program, undergo rigorous testing during the measure development process for feasibility, validity, and reliability. We refer readers to the eCQI Resource Center for the full measure specifications of the eCQMs used in the Hospital IQR Program.[660] We further note that reporting eCQMs has been an existing requirement for the Hospital IQR Program for several years,[661] and is part of our ongoing commitment to promote efficiency through health information technology while also promoting high quality costs and ultimately decreasing reporting burden to providers. Over the past few years, hospitals have continued to build and refine their EHR systems and gain familiarity with reporting eCQM data, resulting in more accurate data submissions with fewer errors. We recognize that adopting new eCQMs can impact a hospital's resource use, but we believe the long-term benefits associated with electronic data capture outweigh these costs and further advances our goal of incrementally increasing the use of EHR data for quality measurement and improvement.
Comment: A few commenters addressed the availability of measure specifications, with one noting that the proposal allowed for sufficient time for clarifying the measure specifications, and a few commenters requesting that the specifications be made available as soon as possible or at least 18 months in advance of the CY 2022 reporting period. A few commenters noted that accurate eCQM reporting depends on using the correct version of the specifications, which they believe is in control of vendors and not hospitals. A commenter conditioned their support on their vendor's ability to build out new eCQMs.
Response: We note that measure specifications for eCQMs can be found on the eCQI Resource Center,[662] which provides a centralized location for news, information, tools, and standards related to eCQMs.[663] We understand that many hospitals work with vendors to implement measure specifications in their EHRs, and we believe that the proposed timeline for required reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM—the CY 2022 reporting period—will allow hospitals and vendors time to work through implementation, testing, and reporting challenges before reporting on the measure to CMS is required.
Comment: A number of commenters did not support our proposal for the eCQM reporting and submission requirements for the CY 2022 reporting period/FY 2024 payment determination, such that hospitals would be required to report one, self-selected calendar quarter of data for: (1) Three self- selected eCQMs; and (2) the proposed Safe Use of Opioids—Concurrent Prescribing eCQM, for a total of four eCQMs. Many commenters urged us not to finalize the proposed required reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM, and suggested that we retain the current reporting requirements into the future. Some commenters suggested a delay in required reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM for a year or two, while others suggested that we give hospitals and vendors more time, including a period of voluntary reporting, before requiring reporting on this measure. These commenters generally expressed concern about ensuring hospitals and vendors have more time to implement and refine reporting on the measure. Some commenters encouraged us to engage in outreach activities with affected stakeholders.
Response: We acknowledge the commenters' concerns. However, we believe it is important to our goal of incrementally increasing the use of EHR data for quality measurement to require the reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM with a clarification and update beginning with the CY 2022 reporting period/FY 2024 payment determination. While we understand that implementing a new eCQM demands hospital and vendor resources, we also believe that the Safe Use of Opioids—Concurrent Prescribing eCQM could play an important role in improving awareness of the risk of concurrent prescribing and could help address the negative impacts of the opioid epidemic. Regarding commenters' requests for a voluntary reporting period, we note that hospitals may submit data on the measure as one of four eCQMs for the CY 2021 reporting period/FY 2023 payment determination should they wish to before the measure is required as one of four eCQMs for the CY 2022 reporting period/FY 2024 payment determination.
As discussed in section XIII.A.5.a.(1). of the preamble of this final rule, currently no measure exists to assess nationwide rates of the concurrent prescribing of opioids and benzodiazepines at the hospital level. We believe that requiring reporting on this measure beginning with the CY 2022 reporting period will advance our efforts to combat the opioid crisis by enhancing the information available to providers in this area of high-risk prescribing.
We will continue engaging with stakeholders through education and outreach opportunities, including webinars, listserves, and help desk questions, as they implement this new eCQM. In addition, we note that there are other resources available to hospitals and vendors during the implementation process, including: (1) eCQI Resource Center's Collaborative Measure Development (CMD) Workspace, which assists clinicians, eCQM developers, implementers, and submitters during the entire eCQM lifecycle, from initial measure concept through development, implementation, and reporting to CMS; [664] and (2) ONC JIRA's eCQM issue tracker for eCQM implementation and maintenance.[665]
Comment: A commenter opposed the proposal to require the Safe Use of Opioids—Concurrent Prescribing eCQM because they believe that hospitals should retain the flexibility to choose to report on those eCQMs most applicable to their quality improvement priorities.
Response: We appreciate the commenter's feedback, however, we believe that allowing hospitals to still self-select three eCQMs for the CY 2022 reporting period provides enough flexibility to report on eCQMs applicable to their quality improvement priorities, while also reporting on a measure that may help address the opioid epidemic. As discussed in section XIII.A.5.a.(1). of the preamble of this final rule, currently no measure exists to assess nationwide rates of the concurrent prescribing of opioids and benzodiazepines at the hospital level. We believe that requiring reporting on this measure beginning with the CY 2022 reporting period will advance our efforts to combat the opioid crisis by enhancing the information available to providers in this area of high-risk prescribing.
Furthermore, we believe this proposal is consistent with CMS' goal of incrementally increasing the use of EHR data for quality measurement and is responsive to the feedback of some stakeholders urging a faster transition to full electronic reporting. Hospitals have had several years to report data electronically for both the Hospital IQR Program and the Promoting Interoperability Programs, and we have maintained the same eCQM reporting and submission requirements for several years in order to enable hospitals enough time to update systems and workflows in the least burdensome manner possible. Based on internal monitoring of eCQM submissions, approximately 97 percent of eligible hospitals successfully submitted eCQMs for CY 2018. Therefore, we believe that hospitals will be ready for the required reporting of the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2022 reporting period/FY 2024 payment determination.
After consideration of the public comments we received, we are finalizing our proposal as proposed to require hospitals to report one, self-selected calendar quarter of data for: (1) Three self-selected eCQMs; and (2) the finalized Safe Use of Opioids—Concurrent Prescribing eCQM with a clarification and update, for a total of four eCQMs, for the CY 2022 reporting period/FY 2024 payment determination.
(5) Continuation of Certification Requirements for eCQM Reporting
(A) Requiring Use of 2015 Edition Certification Criteria
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41604 through 41607), to align the Hospital IQR Program with the Promoting Interoperability Program, we finalized a policy to require hospitals to use the 2015 Edition certification criteria for certified EHR technology (CEHRT) for the CY 2019 reporting period/FY 2021 payment determination and subsequent years. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19497), we did not propose any changes to this policy.
(B) Requiring EHR Technology To Be Certified to All Available eCQMs
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38391 through 38393), for the CY 2017 reporting period/FY 2019 payment determination and the CY 2018 reporting period/FY 2020 payment determination, we finalized a requirement that EHR technology used for eCQM reporting be certified to all eCQMs, but noted that such certified EHR technology does not need to be recertified each time it is updated to a more recent version of the eCQM electronic specifications.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19497 through 19498), we proposed to continue the requirement that EHRs be certified to all available eCQMs used in the Hospital IQR Program for the CY 2020 reporting period/FY 2022 payment determination and subsequent years. The 2015 Edition Base EHR definition (as defined by HHS' Office of the National Coordinator for Health Information Technology (ONC) 2015 Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications Final Rule (80 FR 62649 through 62655)) requires certified health IT to have the capability to capture and query information relevant to health care quality,[666] which can be ensured by meeting the clinical quality measure certification criteria to record and export (45 CFR 170.315(c)(1)). The 2015 Edition Base EHR definition does not require certified health IT to meet additional clinical quality measure certification criteria such as to import and calculate (45 CFR 170.315(c)(2)), report (45 CFR 170.315(c)(3)), or filter (45 CFR 170.315(c)(4)).
ONC's Health IT Certification Program is “agnostic” to settings and programs, but can support many different use cases and needs.[667] Because the ONC Health IT Certification Program supports multiple program and setting needs, ONC does not include requirements that are specific to CMS programs. CMS may impose more stringent requirements for EHR-based reporting under its programs.
The Hospital IQR and Promoting Interoperability Programs have previously required EHRs to be certified to all available eCQMs used in the programs (that is, individual testing of each eCQM) in order to support flexibility for hospitals when they select the eCQMs on which to report.[668] When EHRs are certified to all available eCQMs in the eCQM measure set, hospitals are able to select and report on those measures that best reflect their patient populations and reporting capabilities. In addition to supporting hospital flexibility, we believe the continuation of this requirement promotes more accurate electronic quality reporting by incentivizing EHR and other health IT vendors to test all available eCQMs and to offer reporting modules with certified eCQMs. This requirement would produce greater certainty for hospitals that their EHR systems would be capable of accurately calculating the particular eCQMs they select to report to CMS. We believe this would help reduce burden for hospitals by potentially reducing the frequency of needing to consult with their EHR and other health IT vendors to troubleshoot implementation or reporting issues.
We have continued to hear from hospital stakeholders during a series of provider listening sessions in 2018 that they believe certification is an important part of ensuring successful reporting to CMS. In addition, because this has been the current policy for the Hospital IQR and Promoting Interoperability Programs (82 FR 38391 through 38393; 83 FR 41672), vendors and providers should be familiar with this requirement, and we expect that most providers' EHR systems are already certified to all currently available eCQMs. Since certified EHR technology does not need to be recertified each time it is updated to a more recent version of the eCQM electronic specifications under the Hospital IQR Program (82 FR 38393), there should be no added burden with regard to the currently adopted eCQMs in the eCQM measure set.
We also refer readers to section VIII.D.6.e.(1). of the preamble of this final rule for discussion of a similar proposal for the Promoting Interoperability Program.
Comment: Several commenters supported our proposal to require that EHR technology used for eCQM reporting be certified to all eCQMs. A number of those commenters expressed appreciation for this policy and noted that it helps preserve hospitals' ability to choose eCQMs which reflect their patient populations and quality improvement goals.
Response: We thank the commenters for their support of our proposal.
Comment: A few commenters requested clarification as to whether we are also requiring health IT developers/vendors to certify their EHR products to the Hybrid HWR measure, such as for eCQMs.
Response: The Hybrid HWR measure only uses core clinical data elements and linking variables from EHRs. The 13 core clinical data elements consist of data captured during a patient evaluation or laboratory test and are included in a structured manner in the 2015 Edition Base EHR, such as Heart Rate, Systolic Blood Pressure and Weight. The six linking variables consist of data included in a structured manner in the 2015 Edition Base EHR, such as Date of Birth; Sex; Admission Date. The 2015 Edition Base EHR definition includes the clinical quality measure certification criteria to record and export EHR data (45 CFR 170.315(c)(1)). It requires that the EHRs be able to record all of the data necessary to calculate each clinical quality measure, enabling users to export a data file that is formatted in accordance with the QRDA-I standard and including all of the data captured for each and every clinical quality measure to which technology was certified. Under the 2015 Edition Base EHR definition, a user must be able to export the data file at any time the user chooses and without subsequent developer assistance to operate. We therefore believe that the technological requirements associated with reporting the Hybrid HWR measure are sufficiently addressed. This approach balances the benefits of certification without increasing burden of additional certification requirements that are not as necessary for this measure, such as the criteria to import and calculate (45 CFR 170.315(c)(2)).
After consideration of the public comments we received, we are finalizing our proposal as proposed to require that EHRs be certified to all available eCQMs used in the Hospital IQR Program for the CY 2020 reporting period/FY 2022 payment determination and subsequent years.
(6) File Format for EHR Data, Zero Denominator Declarations, and Case Threshold Exemptions
We refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49705 through 49708) and the FY 2017 IPPS/LTCH PPS final rule (81 FR 57170) for our previously adopted eCQM file format requirements. Under these requirements, hospitals: (1) Must submit eCQM data via the Quality Reporting Document Architecture Category I (QRDA I) file format as was previously required; (2) may use third parties to submit QRDA I files on their behalf; and (3) may either use abstraction or pull the data from non-certified sources in order to then input these data into CEHRT for capture and reporting QRDA I. Hospitals can continue to meet the reporting requirements by submitting data via QRDA I files, zero denominator declaration, or case threshold exemption (82 FR 38387). In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19498), we did not propose any changes to these requirements for eCQMs.
(7) Submission Deadlines for eCQM Data
We refer readers to the FY 2015 IPPS/LTCH PPS final rule (79 FR 50256 through 50259), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49705 through 49709), and the FY 2017 IPPS/LTCH PPS final rule (81 FR 57169 through 57172) for our previously adopted policies to align eCQM data reporting periods and submission deadlines for both the Hospital IQR and Medicare Promoting Interoperability Programs. In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57172), we finalized the alignment of the Hospital IQR Program eCQM submission deadline with that of the Medicare Promoting Interoperability Program—the end of two months following the close of the calendar year—for the CY 2017 reporting period/FY 2019 payment determination and subsequent years. We note the submission deadline may be moved to the next business day if it falls on a weekend or federal holiday. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19498), we did not propose any changes to the eCQM submission deadlines.
e. Data Submission and Reporting Requirements for Hybrid Measures
(1) Background
In section VIII.A.5.b. of the preamble of this final rule, we discuss our proposal to adopt the Hybrid HWR measure in the Hospital IQR Program beginning with the FY 2026 payment determination, with 2 years of voluntary reporting prior to that time. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38350 through 38355), we finalized voluntary reporting of the Hybrid HWR measure for the CY 2018 reporting period. For data submission and reporting requirements under the 2018 Voluntary Reporting Period, we finalized that the 13 core clinical data elements and six linking variables for the Hybrid HWR measure be submitted using the QRDA I file format, and that hospitals voluntarily reporting data for the Hybrid HWR measure could use EHR technology certified to the 2014 Edition, the 2015 Edition, or a combination thereof (82 FR 38394 through 38397). During the 2018 Voluntary Reporting Period, participating hospitals and their health IT vendors reported data on discharges for the January 1, 2018 through June 30, 2018 reporting period by the submission deadline of January 4, 2019, and approximately 150 [669] hospitals submitted data. In the proposed rule, we stated that we expected that hospitals that voluntarily submitted data for this measure would receive confidential hospital-specific reports detailing submission results from the reporting period in early summer of 2019. In July 2019, we provided confidential hospital-specific reports to those hospitals that participated in the 2018 Voluntary Reporting Period via the QualityNet Secure Portal.
(2) Certification and File Format Requirements
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19498 through 19499), we proposed to require that hospitals use EHR technology certified to the 2015 Edition to submit data on the Hybrid HWR measure. This is consistent with our policy finalized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41604 through 41607), which requires use of the 2015 Edition CEHRT when reporting eCQMs beginning with the CY 2019 reporting period/FY 2021 payment determination.
In addition, we proposed that the core clinical data elements and linking variables identified in hybrid measure specifications, for example as discussed in section VIII.A.5.b. of the preamble of this final rule, be submitted using the QRDA I file format. In order to ensure that the data have been appropriately connected to the encounter, the core clinical data elements specified for risk adjustment need to be captured in relation to the start of an inpatient encounter. The QRDA I standard enables the creation of an individual patient-level quality report that contains quality data for one patient for one or more quality measures. Based on the experience of the 2018 Voluntary Reporting Period, the use of the QRDA I file format is feasible. In addition, hospitals and health IT vendors have been using the QRDA I file format for eCQM reporting for several years.
For details on the implementation guidance provided for the Hybrid HWR measure 2018 Voluntary Reporting Period, we refer readers to the 2018 CMS QRDA I Implementation Guide for Hospital Quality Reporting (HQR) and the 2018 CMS QRDA I Schematrons and Sample Files for HQR, available on the eCQI Resource Center website.[670] In the proposed rule, we stated that if our proposal to adopt the Hybrid HWR measure is finalized, updated implementation guidance, schematrons, and sample files would become available on the eCQI Resource Center website.
As with eCQM reporting, we also encourage all hospitals and their health IT vendors to submit QRDA I files early, and to use one of the pre-submission testing tools for electronic reporting, such as the CMS Pre-Submission Validation Application (PSVA) tool (81 FR 57113), to allow additional time for testing and to make sure all required data files are successfully submitted by the deadline. The PSVA tool can be downloaded from the Secure File Transfer (SFT) section of the QualityNet Secure Portal.
Comment: A commenter supported the proposal to require that hospitals use EHR technology certified to the 2015 Edition to submit data on the Hybrid HWR measure and expressed appreciation for our efforts to align reporting standards.
Response: We thank the commenter for their support.
Comment: A commenter supported the proposal that core clinical data elements and linking variables identified in hybrid measure specifications be submitted using the QRDA I file format.
Response: We thank the commenter for their support.
After consideration of the public comments we received, we are finalizing our proposals as proposed to require that hospitals use EHR technology certified to the 2015 Edition to submit data on the Hybrid HWR measure, and that the core clinical data elements and linking variables identified in the hybrid measure specifications be submitted using the QRDA I file format.
(3) Additional Submission Requirements
In the proposed rule (84 FR 19499), we proposed to allow hospitals to meet the hybrid measure reporting and submission requirements by submitting any combination of data via QRDA I files, zero denominator declarations, and/or case threshold exemptions. We recognize the challenges associated with electronic reporting and encourage hospitals of all sizes to work with their vendors to achieve electronic capture and reporting of data necessary for hybrid measure reporting. We also acknowledge that there are situations in which a hospital may be prepared for electronic reporting, but may not have data to report on a particular measure. For example, hospitals with small patient populations may not have sufficient patient population to report on specific measures, such that those hospitals may find it necessary to utilize a zero denominator declaration and/or case threshold exemption. In addition, there may be situations in which case number thresholds are appropriate, given the burden on hospitals that very seldom have the types of cases addressed by certain measures.
In the proposed rule, we proposed to apply similar zero denominator declaration and case threshold exemption policies to hybrid measure reporting as we allow for eCQM reporting. In other words, for a zero denominator declaration, if a hospital's EHR is otherwise capable of reporting hybrid measure data, but the hospital does not have patients that meet the denominator criteria of that hybrid measure, the hospital may submit a zero in the denominator for that measure. Submission of a zero in the denominator for a hybrid measure would count as a successful submission for that hybrid measure for the Hospital IQR Program. In addition, for the case threshold exemption, hospitals that have five or fewer inpatient discharges per quarter or twenty or fewer inpatient discharges per year as defined by a hybrid measure's denominator population, would be exempted from reporting on that hybrid measure. Hospitals can submit zero denominator declarations or case threshold exemptions by logging into the QualityNet Secure Portal and completing the Denominator Declaration screen.
Comment: A few commenters supported our proposal to allow hospitals to meet the hybrid measure reporting and submission requirements by submitting any combination of data via QRDA I files, zero denominator declarations, and/or case threshold exemptions and expressed appreciation for the consistency across requirements. One commenter sought clarification about the submission process for zero denominator declarations and case threshold exemptions.
Response: As stated in the proposed rule (84 FR 19499) and previously in this final rule, hospitals will be able to submit zero denominator declarations and case threshold exemptions through the QualityNet Secure Portal. Use of the zero denominator declarations and case threshold exemptions will not be needed until reporting on the Hybrid HWR measure is mandatory, which begins with the reporting period which runs from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination. We anticipate that the process for submitting zero denominator declarations and case threshold exemptions for hybrid measures would be very similar to the process for eCQMs (82 FR 38387).
After consideration of the public comments we received, we are finalizing our proposals as proposed to: Allow hospitals to meet the hybrid measure reporting and submission requirements by submitting any combination of data via QRDA I files, zero denominator declarations, and/or case threshold exemptions; and apply similar zero denominator declaration and case threshold exemption policies to hybrid measure reporting as we allow for eCQM reporting.
(4) Submission Deadlines for Hybrid Measures
In the proposed rule, we proposed that hospitals must submit the core clinical data elements and linking variables within 3 months following the end of the applicable reporting period (submissions would be required no later than the first business day 3 months following the end of the reporting period) for hybrid measures in the Hospital IQR Program.
As discussed earlier in this final rule, we proposed that the first voluntary reporting period would run from July 1, 2021 through June 30, 2022. Under this proposal, for example, hospitals would be required to submit the core clinical data elements and linking variable data no later than Friday, September 30, 2022, which is the first business day 3 months following the end of the reporting period. Similarly, for the July 1, 2022 through June 30, 2023 voluntary reporting period, for example, the submission deadline would be Monday, October 2, 2023. In the proposed rule, we stated that if our proposal to adopt the Hybrid HWR measure is finalized, this submission deadline would apply to all reporting periods for which data are submitted.
Comment: A commenter supported our proposal to require that hospitals submit core clinical data elements and linking variables within 3 months following the end of the applicable reporting period.
Response: We thank the commenter for their support.
Comment: A few commenters suggested that submission of the Hybrid HWR measure should be counted as reporting on one of the four eCQMs required for the Hospital IQR Program.
Response: Since the Hybrid HWR measure is being adopted to replace the HWR claims-only measure, the Hybrid HWR measure will necessarily require different reporting and submission requirements compared to the current eCQM reporting policy. We refer readers to section VIII.A.5.b. of the preamble of this final rule for a detailed discussion in which we finalize our proposal to adopt the Hybrid HWR measure in the Hospital IQR Program beginning with the FY 2026 payment determination, with 2 years of voluntary reporting prior to that time.
Comment: A few commenters recommended that a single submission of the Hybrid HWR measure should count toward both the Hospital IQR Program and the Promoting Interoperability Program, in keeping with the single submission of eCQM data for both programs.
Response: The Promoting Interoperability Program for eligible hospitals and critical access hospitals has not yet adopted the Hybrid HWR measure but sought comment on potential future adoption in the proposed rule. We refer readers to section VIII.D.6.c. of the preamble of this final rule for a discussion of the Hybrid HWR measure and the Promoting Interoperability Program. We will take commenters' suggestions into consideration for future rulemaking.
After consideration of the public comments we received, we are finalizing our proposal as proposed to require that hospitals submit core clinical data elements and linking variables within 3 months following the end of the applicable reporting period (submissions would be required no later than the first business day 3 months following the end of the reporting period) for hybrid measures in the Hospital IQR Program.
f. Sampling and Case Thresholds for Chart-Abstracted Measures
We refer readers to the FY 2011 IPPS/LTCH PPS final rule (75 FR 50221), the FY 2012 IPPS/LTCH PPS final rule (76 FR 51641), the FY 2013 IPPS/LTCH PPS final rule (77 FR 53537), the FY 2014 IPPS/LTCH PPS final rule (78 FR 50819), and the FY 2016 IPPS/LTCH PPS final rule (80 FR 49709) for details on our sampling and case thresholds for the FY 2016 payment determination and subsequent years. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19499), we did not propose any changes to our sampling and case threshold policies.
g. HCAHPS Administration and Submission Requirements
We refer readers to the FY 2011 IPPS/LTCH PPS final rule (75 FR 50220), the FY 2012 IPPS/LTCH PPS final rule (76 FR 51641 through 51643), the FY 2013 IPPS/LTCH PPS final rule (77 FR 53537 through 53538), and the FY 2014 IPPS/LTCH PPS final rule (78 FR 50819 through 50820) for details on previously-adopted HCAHPS submission requirements. We also refer hospitals and HCAHPS Survey vendors to the official HCAHPS website at: http://www.hcahpsonline.org for new information and program updates regarding the HCAHPS Survey, its administration, oversight, and data adjustments.
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59140 through 59149), we updated the HCAHPS Survey by removing the Communication About Pain questions effective with October 2019 discharges, for the FY 2021 payment determination and subsequent years, and finalizing a policy of not publicly reporting data regarding these questions. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19499), we did not propose any changes to the HCAHPS Survey or its administration and submission requirements.
h. Data Submission Requirements for Structural Measures
There are no remaining structural measures in the Hospital IQR Program.
i. Data Submission and Reporting Requirements for CDC NHSN HAI Measures
For details on the data submission and reporting requirements for Healthcare-Associated Infection (HAI) measures reported via the CDC's National Healthcare Safety Network (NHSN), we refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51629 through 51633; 51644 through 51645), the FY 2013 IPPS/LTCH PPS final rule (77 FR 53539), the FY 2014 IPPS/LTCH PPS final rule (78 FR 50821 through 50822), and the FY 2015 IPPS/LTCH PPS final rule (79 FR 50259 through 50262). The data submission deadlines are posted on the QualityNet website at: http://www.QualityNet.org/. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19499), we did not propose any changes to those requirements.
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41547 through 41553), in which we finalized the removal of five of these measures (CLABSI, CAUTI, Colon and Abdominal Hysterectomy SSI, MRSA Bacteremia, and CDI) from the Hospital IQR Program. As a result, hospitals will not be required to submit any data for those measures under the Hospital IQR Program following their removal beginning with the CY 2020 reporting period/FY 2022 payment determination. However, the five CDC NHSN HAI measures will be included in the HAC Reduction and Hospital VBP Programs and reported via the CDC NHSN portal (83 FR 41474 through 41477; 83 FR 41449 through 41452). Lastly, we refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41472 through 41492) as well as sections IV.I.6. and 7. and IV.H.5.e. of the preamble of this final rule for more information and proposals regarding NHSN HAI measure data collection and validation under the HAC Reduction Program and use in the HAC Reduction and Hospital VBP Programs. We further note that the HCP measure remains in the Hospital IQR Program and will continue to be reported via NHSN.
11. Validation of Hospital IQR Program Data
We refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53539 through 53553), the FY 2014 IPPS/LTCH PPS final rule (78 FR 50822 through 50835), the FY 2015 IPPS/LTCH PPS final rule (79 FR 50262 through 50273), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49710 through 49712), the FY 2017 IPPS/LTCH PPS final rule (81 FR 57173 through 57181), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38398 through 38403), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41607 through 41608) for detailed information on chart-abstracted and eCQM validation processes and previous updates to these processes for the Hospital IQR Program.[671]
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19500), we did not propose any changes to the existing processes for validation of chart-abstracted and eCQM measure data. In the proposed rule, we noted that if our proposal to adopt the Hybrid HWR measure is finalized, we intend to propose a validation process for core clinical data elements in future rulemaking.
12. Data Accuracy and Completeness Acknowledgement (DACA) Requirements
We refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53554) for previously adopted details on DACA requirements. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19500), we did not propose any changes to the DACA requirements.
13. Public Display Requirements
We refer readers to the FY 2008 IPPS/LTCH PPS final rule (72 FR 47364), the FY 2011 IPPS/LTCH PPS final rule (75 FR 50230), the FY 2012 IPPS/LTCH PPS final rule (76 FR 51650), the FY 2013 IPPS/LTCH PPS final rule (77 FR 53554), the FY 2014 IPPS/LTCH PPS final rule (78 FR 50836), the FY 2015 IPPS/LTCH PPS final rule (79 FR 50277), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49712 through 49713), and the FY 2018 IPPS/LTCH PPS final rule (82 FR 38403 through 38409) for details on public display requirements. The Hospital IQR Program quality measures are typically reported on the Hospital Compare website at: http://www.medicare.gov/hospitalcompare, but on occasion are reported on other CMS websites such as: https://data.medicare.gov. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19500), we did not propose any changes to the public display requirements.
14. Reconsideration and Appeal Procedures
We refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51650 through 51651), the FY 2014 IPPS/LTCH PPS final rule (78 FR 50836), and 42 CFR 412.140(e) for details on reconsideration and appeal procedures for the FY 2017 payment determination and subsequent years. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19500), we did not propose any changes to the reconsideration and appeals procedures.
15. Hospital IQR Program Extraordinary Circumstances Exceptions (ECE) Policy
We refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51651 through 51652), the FY 2014 IPPS/LTCH PPS final rule (78 FR 50836 through 50837), the FY 2015 IPPS/LTCH PPS final rule (79 FR 50277), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49713), the FY 2017 IPPS/LTCH PPS final rule (81 FR 57181 through 57182), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38409 through 38411), and 42 CFR 412.140(c)(2) for details on the current Hospital IQR Program ECE policy. We also refer readers to the QualityNet website at: http://www.QualityNet.org/ for our current requirements for submission of a request for an exception. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19500), we did not propose any changes to the ECE policy.
B. PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program
1. Background
Section 1866(k) of the Act establishes a quality reporting program for hospitals described in section 1886(d)(1)(B)(v) of the Act (referred to as “PPS-Exempt Cancer Hospitals” or “PCHs”) that specifically applies to PCHs that meet the requirements under 42 CFR 412.23(f). Section 1866(k)(1) of the Act states that, for FY 2014 and each subsequent fiscal year, a PCH must submit data to the Secretary in accordance with section 1866(k)(2) of the Act with respect to such fiscal year.
The PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program strives to put patients first by ensuring they, along with their clinicians, are empowered to make decisions about their own health care using data-driven insights that are increasingly aligned with meaningful quality measures. To this end, we support technology that reduces burden and allows clinicians to focus on providing high quality health care to their patients. We also support innovative approaches to improve quality, accessibility, and affordability of care, while paying particular attention to improving clinicians' and beneficiaries' experiences when participating in CMS programs. In combination with other efforts across the Department of Health and Human Services (HHS), we believe the PCHQR Program incentivizes PCHs to improve their health care quality and value, while giving patients the tools and information needed to make the best decisions.
For additional background information, including previously finalized measures and other policies for the PCHQR Program, we refer readers to the following final rules: The FY 2013 IPPS/LTCH PPS final rule (77 FR 53556 through 53561); the FY 2014 IPPS/LTCH PPS final rule (78 FR 50838 through 50846); the FY 2015 IPPS/LTCH PPS final rule (79 FR 50277 through 50288); the FY 2016 IPPS/LTCH PPS final rule (80 FR 49713 through 49723); the FY 2017 IPPS/LTCH PPS final rule (81 FR 57182 through 57193); the FY 2018 IPPS/LTCH PPS final rule (82 FR 38411 through 38425); the FY 2019 IPPS/LTCH PPS final rule (83 FR 41609 through 41624); and the CY 2019 OPPS/ASC final rule with comment period (83 FR 59149 through 59154).
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19500 through 19510), we proposed several new policies for the PCHQR Program. As we noted in that proposed rule, we developed these proposals after conducting an overall review of the program under our new Meaningful Measures Initiative, which is discussed in more detail in I.A.2. of the preamble of the FY 2019 IPPS/LTCH PPS final rule (83 FR 41147 through 41148). We stated that the proposals reflected our efforts to ensure that the PCHQR Program measure set continues to promote improved health outcomes for our beneficiaries. We further stated that the proposals also reflect our efforts to improve the usefulness of the data that we publicly report in the PCHQR Program.
2. Refinement of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Survey (NQF #0166): Removal of the Pain Management Questions
a. Background
The HCAHPS Survey (NQF #0166) (OMB Control Number 0938-0981) is the first national, standardized, publicly reported survey of patients' experience of hospital care and asks discharged patients 32 questions about their recent hospital stay. In May 2005, the HCAHPS Survey was endorsed for the first time by the National Quality Forum (NQF). The HCAHPS Survey is available in English, Spanish, Chinese, Russian, Vietnamese, and Portuguese versions. The HCAHPS Survey, along with its protocols for sampling, data collection and coding, and file submission, can be found in the current HCAHPS Quality Assurance Guidelines, which is available on the official HCAHPS website at: http://www.hcahpsonline.org/en/quality-assurance/.
We adopted the HCAHPS Survey into the PCHQR Program beginning with the FY 2016 program year in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50844 through 50845); we refer readers to that final rule for a detailed discussion of the survey. Further, we finalized in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49722) that we would begin publicly reporting this measure in the PCHQR Program in CY 2016. For HCAHPS Survey data reported in years prior to CY 2018, we refer readers to: http://hcahpsonline.org/en/summary-analyses/.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19500 through 19502), we proposed to adopt a substantive change to the HCAHPS Survey by removing the three Pain Management questions beginning with October 1, 2019 discharges.
The patients treated by the 11 PPS-exempt cancer hospitals eligible to participate in the PCHQR Program have been diagnosed with cancer, which frequently causes substantial pain. Cancer treatment also frequently involves surgery, chemotherapy, and/or radiation therapy, all of which can also cause substantial pain beyond that experienced by the general Medicare population.[672] Pain management is therefore an important safeguard against the unintended consequences of appropriate clinical care in these patients.[673]
The version of the HCAHPS Survey currently implemented in the PCHQR Program includes three Pain Management questions, Q12, Q13, and Q14. The questions are as follows:
12. During this hospital stay, did you need medicine for pain?
1□ Yes
2□ No → If No, Go to Question 15
13. During this hospital stay, how often was your pain well controlled?
1□ Never
2□ Sometimes
3□ Usually
4□ Always
14. During this hospital stay, how often did the hospital staff do everything they could to help you with your pain?
1□ Never
2□ Sometimes
3□ Usually
4□ Always
The pain management questions that the PCHQR Program currently uses were previously also adopted as part of the HCAHPS survey used by the Hospital IQR Program (71 FR 68202 through 68204) and the Hospital VBP Program (76 FR 26510), but the questions have been removed from the survey in both of those programs.
Specifically, in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79862), we noted that that we had received feedback that some stakeholders were concerned about the Pain Management dimension questions being used in a program, including the Hospital VBP Program, where there was any link between scoring well on the questions and higher hospital payments (81 FR 79856). Some stakeholders also stated that they believed that the linkage of the pain management questions to the Hospital VBP Program payment incentives created pressure on hospital staff to prescribe more opioids in order to achieve higher scores on the pain management dimension. We also noted that many factors outside of CMS control could contribute to a perception of a link between the questions and opioid prescribing practices, including misuse of the survey (such as using it for outpatient emergency room care instead of inpatient care, or using it for determining physician performance) and failure to recognize that the HCAHPS survey excludes certain populations from the sampling frame (such as those with a primary substance use disorder diagnosis).
We stated that we had heard that some hospitals have identified patient experience as a potential source of competitive advantage, and that some hospitals may be disaggregating their raw HCAHPS data to compare, assess, and incentivize individual physicians, nurses and other hospital staff. We further stated that some hospitals may be using the HCAHPS survey to assess their emergency and outpatient departments. We stated that the HCAHPS survey was never intended to be used in any of these ways.
In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79859 through 79860), we further noted that numerous commenters had offered support for the development of modified questions regarding pain management for the HCAHPS Survey and that some commenters expressed support for modified pain management questions that focused on effective communication with patients about pain management-related issues. In response, we stated we would follow our standard survey development processes, which include drafting alternative questions, cognitive interviews and focus group evaluation, field testing, statistical analysis, stakeholder input, the Paperwork Reduction Act, and NQF endorsement (81 FR 79856).
We continue to believe that pain control is an appropriate part of routine patient care that hospitals should manage and is an important concern for patients, their families, and their caregivers. It is important to note that the HCAHPS Survey does not specify any particular type of pain control method. In addition, appropriate pain management includes communication with patients about pain-related issues, setting expectations about pain, shared decision-making, and proper prescription practices. However, due to some potential confusion about the appropriate use of the Pain Management dimension questions in the Hospital VBP Program and the public health concern about the ongoing prescription opioid overdose epidemic, in an abundance of caution, we finalized removal of the Pain Management dimension of the HCAHPS Survey in the Patient- and Caregiver-Centered Experience of Care/Care Coordination domain of the Hospital VBP Program beginning with the FY 2018 program year (81 FR 79862).
Subsequently, out of an abundance of caution and in the face of a nationwide epidemic of opioid over-prescription, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38328 through 38342), we finalized a refinement to the HCAHPS Survey measure as used in the Hospital IQR Program by removing the same pain management questions.
b. Removal of the Existing Pain Management Questions From the HCAHPS Survey
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19501 through 19502), we proposed to refine the HCAHPS Survey used in the PCHQR Program by removing the three Pain Management questions beginning with October 1, 2019 discharges. As discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59141), some hospitals have identified patient experience of care as a potential source of competitive advantage, and stakeholders have also informed CMS that some hospitals may be disaggregating their raw HCAHPS Survey data to compare, assess, and incentivize individual physicians, nurses, and other hospital staff. While this issue was raised regarding acute care facilities, we are concerned that similar activity might be occurring in PCHs because the incentives to improve patient experience exist across care settings.
We also stated in the proposed rule that we were concerned about potential confusion about the appropriate use of the pain management questions in the PCHQR Program, given the public health concern about the ongoing prescription opioid overdose epidemic, and that we believed removing the pain management questions would eliminate any such potential misuse. We noted that the HCAHPS Quality Assurance Guidelines,[674] which set forth current survey administration protocols, strongly discourage the unofficial use of HCAHPS scores for comparisons within hospitals, such as for comparisons of particular wards, floors, and individual staff hospital members.
While we recognized the importance of being able to provide performance results within the context of pain management for cancer patients, we also stated in the proposed rule that pain items in generic patient experience surveys (for example, HCAHPS) have limitations when implemented. As previously noted, many factors outside the control of CMS quality program requirements may contribute to the perception of a link between the pain management questions and opioid prescribing practices, including misuse of the HCAHPS Survey (for example, using it for outpatient emergency room care instead of inpatient care, or using it for determining individual physician performance), and failure to recognize that the HCAHPS Survey excludes certain populations from the sampling frame (such as those with a primary substance use disorder diagnosis). Further, in its final report, the President's Commission on Combatting Drug Addiction and the Opioid Crisis recommended removal of the HCAHPS Pain Management questions in order to ensure providers are not incentivized to offer opioids to raise their HCAHPS Survey score.[675] We believe that all of these issues support the removal of the pain management questions in the HCAHPS survey used by PCHs.
We also stated our belief that the removal of the questions will promote programmatic alignment with both the Hospital IQR Program and the Hospital VBP Program. Accordingly, we proposed to remove the Pain Management questions from the version of the HCAHPS Survey currently implemented in the PCHQR Program, beginning with the October 1, 2019 discharges. If finalized as proposed, this would result in the reduction of the number of HCAHPS Survey questions from 32 to 29. We noted that this proposed change would not impact how scores are calculated for the remainder of the survey and would not have a significant effect on the reliability of the HCAHPS Survey instrument as a whole.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19501 through 19502), we also proposed to not publicly report the data collected on the Pain Management questions beginning with October 2018 discharges in order to address the potential misunderstanding associated with these questions as soon as possible. We stated that while the data would not be publicly reported, we would still plan to provide performance results to PCHs in confidential preview reports upon the availability of four quarters of CY 2018 data, as early as July 2019.
Comment: Several commenters supported the proposed refinement of the HCAHPS survey to remove the existing “pain management” questions. Commenters agreed that considering the current opioid epidemic, unintended consequences may result from these questions remaining in the survey. Commenters noted that the removal of these questions is prudent until we can better understand the relationship between these questions and opioid prescribing, and that the best course of action is for CMS to remove them from the HCAHPS survey. Further, commenters indicated that removal of the questions is a positive step toward improving patient safety and changing staff, patient and family perception about appropriate pain management and patient outcomes. Commenters also stated that the removal of the “pain management” questions allows for alignment with the other CMS programs (Hospital IQR and Hospital VBP) and agreed that in order to not create confusion for consumers, CMS should not publicly report performance data on pain assessment.
Commenters acknowledged that pain assessment and management are critical components of cancer care and that under-treatment of pain is still a real concern. Commenters encouraged CMS to explore a range of approaches to assess how well hospitals are addressing pain management in the hospital setting. Commenters also encouraged CMS to continue to work with stakeholders to identify measures that encourage the adoption of appropriate pain assessment and management practices. Lastly, commenters recommended that CMS seek alternative ways to evaluate how cancer patients view their pain management and consult with specialty societies involved in the treatment of cancer patients.
Response: We thank the commenters for their support. We acknowledge the importance of working with stakeholders to identify measures that encourage the adoption of appropriate pain assessment and management practices, and alternative approaches to assess cancer patient pain management. We intend to conduct further education and outreach with stakeholders based on the discussion of these alternative approaches and potential future measures. We also note that in section IX.B.6.b. of the preamble of this final rule, we discuss the responses we received on our request for comments on measures and measurement concepts that would assess pain management in the cancer patient population, as well as measures that would assess post-treatment addiction prevention.
Comment: Some commenters did not support the proposal to remove the “pain management” questions from the HCAHPS survey. The commenters indicated that no evidence is provided that the pain management questions promote opioid overuse and expressed concern that CMS' rationale is therefore anecdotal. Further, rather than removing these questions, commenters recommended that CMS should pursue measures that adequately capture a hospital's performance on pain management and determine whether any such questions do indeed encourage opioid overuse. Until such evidence is confirmed, however, the commenters stated that the current questions should remain. Commenters encouraged CMS to ensure a balanced approach to pain management that reduces the potential for misuse and abuse. Commenters urged CMS to ensure that removing these questions does not inappropriately impact patient quality of care. Additionally, commenters urged CMS to consider alternate questions that seek to ensure adequate patient awareness of the range of treatment options available to manage pain—including non-opioid analgesics and other non-pharmacological modalities of care.
Response: Our belief that the retention of the pain management questions in the HCAHPS survey could lead to unintended consequences is based on known examples of current misuse of the HCAHPS survey (such as using it for outpatient emergency room care instead of inpatient care or using it for determining physician performance). We have also heard from stakeholders that the misuse of the HCAHPS Survey may contribute to the perception of a link between the pain management questions and opioid prescribing practices. We believe that retaining these questions would inadvertently continue to contribute to that perception and we want to avoid any potential for an adverse impact by virtue of retaining those questions in the survey.
We acknowledge the commenters' concern regarding the importance of implementing measures that adequately capture a hospital's performance on pain management. We also appreciate their recommendation to consider alternate questions that seek to ensure adequate patient awareness of the range of treatment options available to manage pain—including non-opioid analgesics and other non-pharmacological modalities of care. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19507 through 19508), we sought public comment on existing and/or newly developed cancer patient, pain-related measures. We refer readers to section IX.B.6.b. of the preamble of this final rule for a more detailed discussion of the comments that we received on this issue.
After consideration of the public comments we received, we are finalizing our proposal to refine the HCAHPS Survey used in the PCHQR Program by removing the three Pain Management questions beginning with October 1, 2019 discharges. With respect to our proposal to discontinue publicly reporting the data collected on these questions beginning with October 1 discharges, due to planned website improvements we are currently targeting January 2020 for removal of those data from Hospital Compare. We note that we are working to provide performance results to PCHs in confidential preview reports that reflect four quarters of CY 2018 data, and we do not intend to make those data public on Hospital Compare.
3. Measure Retention and Removal Factors for the PCHQR Program
a. Measure Retention Factors
We generally retain measures from the previous year's PCHQR Program measure set for subsequent years' measure sets, except when we specifically propose to remove or replace a measure. We have also recognized that there are times when measures may meet one or more of the outlined criteria for removal from the program but continue to bring value to the program. Therefore, we adopted the following factors for consideration in determining whether to retain a measure in the PCHQR Program, which also are based on factors established in the Hospital IQR Program (81 FR 57182 through 57183):
- Measure aligns with other CMS and HHS policy goals.
- Measure aligns with other CMS programs, including other quality reporting programs.
- Measure supports efforts to move PCHs towards reporting electronic measures.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19502), we did not propose any changes to these measure retention factors.
b. Measure Removal Factors
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41609 through 41611), we discussed our existing measure removal factors for the PCHQR Program.[676] We note that these factors are based on factors adopted for the Hospital IQR Program (81 FR 57182 through 57183; 83 FR 41540 through 41544). We also adopted a new measure removal factor, for a total of eight measure removal factors as follows:
- Factor 1. Measure performance among PCHs is so high and unvarying that meaningful distinctions and improvements in performance can no longer be made (that is, “topped-out” measures): statistically indistinguishable performance at the 75th and 90th percentiles; and truncated coefficient of variation ≤ 0.10.
- Factor 2. A measure does not align with current clinical guidelines or practice.
- Factor 3. The availability of a more broadly applicable measure (across settings or populations) or the availability of a measure that is more proximal in time to desired patient outcomes for the particular topic.
- Factor 4. Performance or improvement on a measure does not result in better patient outcomes.
- Factor 5. The availability of a measure that is more strongly associated with desired patient outcomes for the particular topic.
- Factor 6. Collection or public reporting of a measure leads to negative unintended consequences other than patient harm.
- Factor 7. It is not feasible to implement the measure specifications.
- Factor 8. The costs associated with a measure outweigh the benefit of its continued use in the program.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19502), we did not propose any changes to these measure removal factors.
4. Removal of the Web-Based Structural Measure: External Beam Radiotherapy (EBRT) for Bone Metastases From the PCHQR Program Beginning With the FY 2022 Program Year
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19502 through 19503), we proposed to remove the External Beam Radiotherapy (EBRT) for Bone Metastases (formerly NQF #1822) [677] measure from the PCHQR Program beginning with the FY 2022 program year, based on removal Factor 8: the costs associated with a measure outweigh the benefit of its continued use in the program.
a. Background
We adopted the EBRT measure beginning with the FY 2017 program year in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50278 through 50279). The EBRT measure reports the percentage of patients, regardless of age, with a diagnosis of painful bone metastases and no history of previous radiation who receive EBRT with an acceptable fractionation scheme as defined by the guideline.
When the EBRT measure was adopted into the PCHQR Program, it initially used “radiation planning” current procedural terminology (CPT) codes that were billable at the physician level. After finalizing the measure, we learned that at least one of the 11 PCHs did not have access to physician billing data, making reporting complete data on this measure unduly burdensome and difficult. To address this issue, beginning in March 2016, the measure was updated in the PCHQR Program to enable the use of “radiation delivery” CPT codes, which are billable at the hospital level.[678] We note that the timing of this update was at the end of a quarter of the established reporting period for this measure; we finalized in the FY 2015 IPPS/LTCH PPS final rule that PCHs would report this measure on a quarterly basis, beginning with January 1, 2015 discharges for the FY 2017 program year (79 FR 50282). We refer readers to a summary table in the FY 2015 IPPS/LTCH PPS final rule for a summary of the measure reporting periods for CY 2016 (79 FR 50283).
b. Analysis of Measure Use
After implementation of the updated EBRT measure in the PCHQR Program, the measure steward conducted testing of data collection of the updated measure in the outpatient setting and discovered that there are new and significant concerns regarding the revised “radiation delivery” CPT coding used to report the EBRT measure. Although this testing was done in the outpatient setting, we stated in the proposed rule that we believed the issues with the measure that were identified in the outpatient setting similarly affect the inpatient cancer hospital community, as PCHs need to take the same steps as hospital outpatient departments (HOPDs) to report the measure using “radiation delivery” CPT codes. In particular, we noted that the measure steward has observed that implementing the updated measure in the outpatient setting has proven to be very burdensome on hospitals. The use of “radiation delivery” CPT codes requires more complicated measure exclusions to be used because the change to “radiation delivery” CPT codes caused the administration of EBRT to different anatomic sites to be considered separate cases for this measure. Because there is no way to determine the different anatomic sites until detailed review of the patient's record is complete, sampling has become a significant concern, and it has confounded the task of determining which sites should be included or excluded from the measure denominator. In addition, hospitals have had difficulty determining if sample size requirements for the measure are being met. As a result, we stated in the proposed rule that we believed the complexity of reporting this measure places substantial administrative burden on hospitals.
We also noted in the proposed rule that the measure lost NQF endorsement in 2018 and that the measure steward is no longer maintaining the measure or seeking NQF re-endorsement. As a result, especially because the steward is no longer maintaining the measure, we stated that we no longer believed we could ensure that the measure is in line with clinical guidelines and standards, which further diminishes the value of the measure.
c. Summary
We stated in the proposed rule that we believed the burden associated with the measure outweighs the value of its inclusion in the PCHQR Program. Accordingly, we proposed, under removal Factor 8, to remove the EBRT measure from the PCHQR Program beginning with the FY 2022 program year.
Comment: Several commenters supported the proposed removal of the External Beam Radiotherapy (EBRT) for Bone Metastases (formerly NQF #1822) measure. The commenters stated that while this measure addresses a key treatment modality in cancer (radiation therapy), the burden associated with data abstraction and the challenges associated with maintaining updated specifications in the absence of a measure steward warrant removal of the measure from the PCHQR Program. Commenters commended CMS for recognizing the concerns that the radiation treatment delivery CPT codes used for the measure, which were part of a re-specification after the measure was finalized, now require additional exclusions, and that implementation of these additional exclusions has proved burdensome for PCHs. Lastly, commenters indicated that the difficulty in identifying accurate and reliable specifications that would allow for reporting of the measure via claims is another factor that adequately qualifies this measure for removal from the program due to a poor cost/benefit ratio.
Response: We thank the commenters for their support.
After consideration of the public comments we received, we are finalizing our proposal to remove the External Beam Radiotherapy (EBRT) for Bone Metastases (formerly NQF #1822) measure from the PCHQR measure set beginning with the FY 2022 program year.
5. New Quality Measure Beginning With the FY 2022 Program Year
a. Considerations in the Selection of Quality Measures
Under current policy, we take many principles into consideration when developing and selecting measures for the PCHQR Program, and many of these principles are modeled on those we use for measure development and selection under the Hospital IQR Program. In section I.A.2. of the preamble of the FY 2019 IPPS/LTCH PPS final rule (83 FR 41147 through 41148), we also discuss our Meaningful Measures Initiative and its relationship to how we will assess and select quality measures for the PCHQR Program.
Section 1866(k)(3)(A) of the Act requires that any measure specified by the Secretary must have been endorsed by the entity with a contract under section 1890(a) of the Act (the NQF is the entity that currently holds this contract). Section 1866(k)(3)(B) of the Act provides an exception under which, in the case of a specified area or medical topic determined appropriate by the Secretary for which a feasible and practical measure has not been endorsed by the entity with a contract under section 1890(a) of the Act, the Secretary may specify a measure that is not so endorsed as long as due consideration is given to measures that have been endorsed or adopted by a consensus organization.
After considering these principles for measure selection in the PCHQR Program, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19503 through 19507), we proposed to adopt one new measure beginning with the FY 2022 program year, as described below.
b. New Quality Measure Beginning With the FY 2022 Program Year: Surgical Treatment Complications for Localized Prostate Cancer
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19503 through 19507), we proposed to adopt the Surgical Treatment Complications for Localized Prostate Cancer measure for the FY 2022 program year and subsequent years.
(1) Background
Prostate cancer is the most common non-dermatologic malignancy among men in the United States, with an estimated 180,000 new cases/year.[679] Approximately 80 percent of patients are diagnosed with localized disease and therefore may be eligible for prostate directed therapy.[680] This could involve surgical removal of the prostate, radiation therapy, or both. The majority of patients who undergo prostate-directed therapy survive, but these treatments can have serious and potentially longstanding adverse effects, including incontinence, urinary tract obstruction, hydronephrosis, erectile dysfunction, urinary fistula formation, hematuria, cystitis, bowel fistula, proctitis/colitis, bowel bleeding, diarrhea, rectal/anal fissure, abscess, stricture, incision hernia, infection, or others.[681 682] Patients consistently report that these adverse effects, which are patient-centered outcomes, can have a significant detrimental impact on their quality of life.[683 684]
Clinical trials and population-based data have been used to determine whether different prostate-directed treatments result in different patient-centered outcomes. These studies have evaluated a range of prostate-directed treatments, including open radical prostatectomy, robot-assisted radical prostatectomy, minimally invasive radical prostatectomy, brachytherapy, external beam radiation therapy, conformal radiation therapy, intensity modulated radiation therapy (IMRT), and proton therapy, and have demonstrated that some treatments are associated with inferior patient-centered outcomes when compared to others. A number of these studies used Medicare claims after therapy for prostate cancer to identify specific outcomes.[685 686 687] Very few studies have explored whether the patient-centered outcomes experienced after prostate-directed therapy vary by treating facility. However, studies of other cancers have demonstrated that outcomes can vary by treating facility. For example, operative mortality after major cancer surgery varies inversely with hospital volume.[688]
In recognition of the potential impact of this variation, the Surgical Treatment Complications for Localized Prostate Cancer measure was developed. This measure is based on the Localized Prostate Cancer Standard Set (the Standard Set) developed by the International Consortium for Health Outcome Measurement (ICHOM).[689] The Standard Set is a conceptual framework that is supported by a rigorous, evidence-based consensus approach to identify the outcomes that matter most to prostate cancer patients. The Localized Prostate Cancer Standard Set recommends key outcomes that should be measured to improve the lives of patients with localized prostate cancer. We believe that this measure is in line with the Standard Set framework, which recommends measuring complications of prostate-directed surgical treatments. We stated in the proposed rule that we believe the Surgical Treatment Complications for Localized Prostate Cancer measure would add value to the PCHQR Program measure set.
(2) Overview of Measure
The Surgical Treatment Complications for Localized Prostate Cancer measure addresses complications of a prostatectomy. The outcomes selected for this measure are urinary incontinence (UI) and erectile dysfunction (ED). Specifically, the measure uses claims to identify urinary incontinence and erectile dysfunction among patients undergoing localized prostate cancer surgery and uses this information to derive hospital-specific rates. A strong body of literature, including numerous recent systematic reviews, have demonstrated the burden of UI and ED for men following localized prostate surgery and ED.[690 691 692 693 694] By identifying facilities where adverse outcomes associated with prostatectomy are more common, this measure will help to highlight opportunities for quality improvement activities that will address and hopefully mitigate unwarranted variation in prostatectomy procedures.
The proposed measure would be calculated using information from Medicare fee-for-service (FFS) claims, resulting in no new data reporting for PCHs. We would publicly report the measure results to enable patients to make informed decisions about accessing localized prostate surgery and about the rates of potential complications. We would identify a specified timeframe for public reporting of this measure in future rulemaking. In addition, we noted that there are currently no measures assessing complications of prostate surgery in the PCHQR Program measure set.
(3) Data Sources
We proposed that we would calculate this measure on a yearly basis using Medicare administrative claims data. Specifically, we proposed that the data collection period for each program year would span from July 1 of the year 2 years prior to the start of the program year to June 30 of the year 1 year prior to the start of the program year. Therefore, for the FY 2022 program year, we would begin calculating measure rates using PCH claims data from July 1, 2019 through June 30, 2020.
During the development of the measure, the measure steward convened a technical expert panel (TEP), comprising diverse clinical and quality measurement experts from the 11 PPS-exempt cancer hospitals, in 2016. We noted that the TEP endorsed the ICHOM's recommendation to measure prostate-directed surgical treatment complications. Because the measure methodology assesses complications pre-surgery and post-surgery directed to the prostate, this necessitated the availability of claims data. In order to examine data collection burden and data reliability, the TEP requested an analysis of using Medicare claims to assess treatment complications in the ICHOM standard set. For this purpose, a SEER-Medicare dataset [695] was used to validate Medicare claims data. SEER datasets are commonly considered “gold standard” data for cancer stage and other clinical characteristics, and are often used to validate Medicare claims data, which are lacking in these details. The results of this analysis showed that the claims-based algorithm used by the measure could successfully identify patients with prostate cancer, thereby substantiating the use of Medicare claims as the data source for this measure.
(4) Measure Calculation
This outcome measure analyzes hospital/facility-level variation in patient-relevant outcomes during the year after prostate-directed surgery. Specifically, the measure uses claims to identify urinary incontinence and erectile dysfunction among patients undergoing localized prostate cancer surgery and uses this information to derive hospital-specific rates. Those outcomes are rescaled to a 0-100 scale, with 0=worst and 100=best. The numerator includes patients with diagnosis claims that could indicate adverse outcomes following prostate-directed surgery. The numerator is determined by: (1) Calculating the difference in the number of days with claims for incontinence or erectile dysfunction in the year after versus the year before prostate surgery for each patient; (2) truncating (by Winsorizing) to reduce the impact of outliers; (3) rescaling the difference from 0 (worst) to 100 (best); and (4) calculating the mean score for each hospital based on all of the difference values for all of the patients treated at that hospital. The denominator is determined by the following: Men age 66 or older at the time of prostate cancer diagnosis with at least two ICD diagnosis codes for prostate cancer separated by at least 30 days; men who survived at least one year after prostate directed therapy; codes for prostate cancer surgery (either open or minimally invasive/robotic prostatectomy) at any time after the first prostate cancer diagnosis; and continuous enrollment in Medicare Parts A and B (and no Medicare Part C (Medicare Advantage) enrollment)) from 1 year before through 1 year after prostate directed therapy. The measure code lists include all codes required for the numerator and denominator calculation.[696]
The proposed measure excludes patients with metastatic disease, patients with more than one nondermatologic malignancy, patients receiving chemotherapy, patients receiving radiation, and/or patients who die within 1 year after prostatectomy. We noted in the proposed rule that the validity of this measure would be threatened by inclusion of patients who did not meet the denominator criteria. Specifically, patients with more than one nondermatologic malignancy are excluded because a second cancer diagnosis during the measurement period could influence the outcomes. Further, patients receiving chemotherapy are excluded because guidelines for localized prostate cancers do not recommend chemotherapy for routine care; therefore, chemotherapy can indicate advanced disease or other unique clinical characteristics. Patients receiving radiation therapy are excluded because radiation therapy to the prostate can impact the occurrence of complications in these patients. Therefore, the impact of the surgery versus the radiation therapy in these patients cannot be determined. Lastly, patients who die within 1 year after prostatectomy are excluded because death is highly unlikely to be related to localized prostate cancer and unlikely to be related to the surgical complications. Thus, patients who die within the year following surgery likely die from an unrelated reason. As such, we stated that the measure would be calculated as the numerator divided by the denominator (in accordance with the denominator exclusions as previously described). Complete measure specifications for the proposed measure are available in the “2018 Measures Under Consideration List” Excel file, which can be accessed at: http://www.qualityforum.org/map/.
(5) Cohort
This measure includes adult male Medicare FFS beneficiaries, age 66 years and older, who have received prostate cancer directed surgery within the defined measurement period. We note that this measure cohort was determined in accordance with the defined measure denominator and its specified exclusions (as previously discussed) and based on testing conducted on the minimum number of patients attributed to the hospital associated with the claims for the procedure code for prostatectomy. The age of 66 at the time of prostate cancer diagnosis was chosen because per the denominator, a patient must have had Medicare claims data for 1 year prior to and 1 year after surgery. Additional methodology and measure development details are available in the “2018 Measures Under Consideration List,” which can be accessed at: http://www.qualityforum.org/map/.
(6) Risk Adjustment
The measure steward developed a mock risk-adjustment testing protocol based on the case-mix variables identified in the ICHOM data dictionary,[697] and TEP guidance. Specifically, the measure steward identified covariates that could be incorporated for potential risk-adjustment modeling. The covariates were not limited to those available in claims data; clinical covariates were also identified for analysis from SEER to determine adequacy of claims alone for valid measurement. Specifically, the following patient factors were controlled for when deriving the patient-level complication score: Age; year of surgery; other/unknown prostate cancer grade; and prostatectomy type. Hierarchical linear modeling was used to identify which patient, tumor, and hospital factors are associated with a higher IED score. After review of the results of the mock risk-adjustment testing efforts, it was determined that risk adjusting the measure did not yield results that demonstrate any statistically significant differences from the non-risk-adjusted results. The measure steward analyzed the correlation between the unadjusted performance scores and risk-adjusted performance scores and observed that the correlation coefficients were above 95 percent in both analyses. Consequently, the measure steward elected to finalize the development of the measure without the implementation of a risk-adjustment model.
(7) Measure Application Partnership (MAP) Assessment of the Proposed Measure
In compliance with section 1890A(a)(2) of the Act, the proposed measure was included on a publicly available document entitled “2018 Measures under Consideration Spreadsheet,” [698] a list of quality and efficiency measures under consideration for use in various Medicare programs, and was reviewed by the MAP Hospital Workgroup. The MAP noted the importance of patient-relevant outcomes for patients who have undergone surgical treatment for prostate care, but encouraged CMS to resubmit the measure once the measure developer has better streamlined the reliability and validity testing methodologies.[699] Specifically, the MAP discussed the differences between surgical procedures (for example, open, closed, minimally invasive, robotic, among others) and recommended that non-open procedures be grouped separately.[700] The MAP also suggested the measure be risk-adjusted because of the concern of different rates of complications related to how the surgery is performed.[701]
In response to the concern raised by the MAP regarding the grouping of surgical procedures, we noted that the measure is intended to calculate one overall facility rate for accountability purposes. However, given the guidance from the MAP, the steward has recommended to CMS that each hospital's publicly displayed performance on the Hospital Compare website would be stratified by prostatectomy procedure type (open versus not open) to add meaning for consumers and hospital quality improvement. Further, in response to the MAP's question of risk-adjustment, we noted that risk-adjustment is limited for cancer patients when using claims data (for example, cancer stage not captured in claims data). Despite this, we reiterated that the steward conducted a mock risk-adjustment testing protocol and observed that risk-adjusting the measure did not demonstrate any statistically significant differences. As such, the steward chose not to include the risk-adjustment methodology for the measure.
In the proposed rule, we stated that we currently are unaware of an alternative quality measure assessing this measurement topic that is appropriate for the PCHQR Program. This measure is not endorsed by the NQF, and in our environmental scan of the NQF measures portfolio, we noted that we have not been able to identify a feasible and practical endorsed measure that addresses surgical procedures for localized prostate cancer. We also stated that we believe this measure meets the requirement under section 1866(k)(3)(B) of the Act, which provides that in the case of a specified area or medical topic determined appropriate by the Secretary for which a feasible and practical measure has not been endorsed by the entity with a contract under section 1890(a) of the Act, the Secretary may specify a measure that is not so endorsed as long as due consideration is given to measures that have been endorsed or adopted by a consensus organization identified by the Secretary. In addition, we noted this measure aligns with recent initiatives to increase the number of outcome measures in quality reporting programs. Lastly, we stated that this measure aligns with the “Make Care Safer by Reducing Harm Caused in the Delivery of Care” domain of our Meaningful Measures Initiative,[702] and would fill an existing gap area of patient-focused episode of care in the PCHQR Program.
(8) Adoption of the Surgical Treatment Complications for Localized Prostate Cancer Measure
We stated in the proposed rule that we believe this measure would be a valuable addition to the PCHQR Program because it is a high impact (as prostate cancer is a prevalent disease) outcome measure and it addresses reduction in harm. This is a hospital/facility-level, claims-based measure that analyzes variation in the occurrence of incontinence and/or erectile dysfunction during the year after prostate-directed surgery, which is one of the standard treatments for localized prostate cancer. Further, this measure has the potential to improve patient outcomes and decrease costs associated with managing adverse events. By identifying facilities where adverse outcomes associated with prostatectomy are more common, this measure would help to highlight opportunities for quality improvement that address unwarranted variation. This will facilitate improved compliance with guidelines from the American Urology Association (AUA) and other professional societies that call for minimizing the potential for therapy-related adverse outcomes.[703]
Lastly, this measure could be utilized as a tool to foster quality improvement and optimize outcomes for patients with localized prostate cancer. For the reasons previously outlined, we proposed to adopt the Surgical Treatment Complications for Localized Prostate Cancer measure for the FY 2022 program year and subsequent years.
Comment: Many commenters supported the proposed adoption of the Surgical Treatment Complications for Localized Prostate Cancer measure, however, these same commenters recommended that CMS consider conducting confidential national reporting prior to public display of this measure's data. The commenters stated that prostate cancer is a highly prevalent cancer diagnosis, making it particularly important to capture and report on differences in patient outcomes and variations between facilities. Further, analysis of claims data to report rates of urinary incontinence and erectile dysfunction among patients undergoing localized prostate cancer surgery will enable this evaluation and create an important opportunity for quality improvement activities. Commenters indicated that a confidential dry-run on the measure is necessary to ensure the claims codes have been thoroughly vetted and that the measure's specifications are returning valid results. Commenters also noted that the measure was designed and tested for accountability purposes as an overall facility rate. Commenters also noted it would not be feasible or statistically valid to report this stratified data publicly. As such, the commenters recommended that CMS provide stratified results to hospitals in their confidential facility-specific reports for internal hospital quality improvement purposes only. Lastly, commenters expressed that since the measure calculates the risk adjusted rate of the occurrence of urinary and erectile dysfunction following surgical treatment for prostate cancer using Medicare claims data, outcomes data in this area would be useful.
Response: We thank the commenters for their support and their recommendations regarding confidential national reporting of this measure prior to publicly reporting the data. We agree that confidential national reporting would be essential to ensure the reliability and validity of the measure's performance results and we commit to conducting confidential national reporting for this measure prior to publicly reporting the data. We believe that the best course of action is to conduct confidential reporting to ensure the feasibility of providing statistically robust, and valid stratified measure results.
Additionally, we noted in the proposed rule that this measure will be stratified by prostatectomy procedure type (open versus not open) (84 FR 19606). We wish to clarify that the measure is not currently stratified by procedure type, and that we did not propose that the measure would be publicly reported on the Hospital Compare website as stratified by prostatectomy procedure type. CMS will consider this recommendation for future rulemaking on the public reporting of this measure. Further, we wish to clarify that our consideration of stratified measure results does not require a change to the measure's calculation and only has implications for how we would publicly report this measure's data in the future.
Comment: A few commenters did not support the proposed adoption of the Surgical Treatment Complications for Localized Prostate Cancer measure. The commenters expressed concern that adopting such a measure would create financial incentives for hospitals to encourage patients to defer treatment or use other forms of prostate cancer treatments over localized surgical treatments, without regard to the patient's and physician's judgment of the best options for that patient. Further, the commenters indicated that this measure should not be included in the PCHQR Program until it has been refined and adequately tested. The commenters recommended adopting an additional exclusion for patients who have been diagnosed or treated for erectile dysfunction and/or urinary incontinence prior to undergoing surgery for prostate cancer to ensure accurate measurement.
Response: We do not believe that the adoption of this measure into the PCHQR Program would incentivize hospitals to encourage patients to defer treatment or elect alternative treatments over localized surgical treatments. We reiterate that by identifying facilities where adverse outcomes associated with prostatectomy are more common, this measure will help address and hopefully mitigate unwarranted variation in prostatectomy procedures. Further, this measure is not intended nor designed to address whether a patient should undergo a prostatectomy; instead, it provides information on hospital/facility-level variation in adverse outcomes for patients presumably identified as appropriate candidates for this procedure. In this way, the measure may help hospitals/facilities identify potential opportunities for improvement based on their patient outcomes. As such, we believe that the inclusion of this measure in the PCHQR Program will set a precedent for the efficiency of localized treatments, and via positive performance results, help patients better understand that localized surgical treatments are viable care options for urinary incontinence and erectile dysfunction.
Regarding the concerns about the measure's testing, we note that given the limitations of the prostatectomy codes available during the development and testing of this measure, as well as the number of cases required to assess reliability and validity of the stratified data, it was not feasible to provide statistically robust stratified results. The measure was designed and tested for accountability purposes as an overall facility rate; therefore, it would not be feasible or statistically valid to report this stratified data publicly, however, in recognition of the importance of confidential reporting prior to publicly reporting data, we intend to provide stratified results to hospitals in their confidential facility-specific reports for internal hospital quality improvement purposes only. To address the commenters' suggestion about additional exclusions, we note that this measure is calculated by subtracting the number of days with claims for ED and/or UI in the year before the prostatectomy from the number of days with claims in the year after surgery; therefore, patients serve as their own control given that any history of ED and/or UI prior to the surgical intervention is accounted for. Excluding those patients with a prior history of ED and/or UI is not necessary, and in fact, may reduce the number of appropriately eligible patients in the denominator.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Surgical Treatment Complications for Localized Prostate Cancer measure for the FY 2022 program year and subsequent years. We note that to be responsive to stakeholder feedback, we will include confidential national reporting for this measure prior to publicly reporting its performance data. Lastly, we note that we will address the timing of publicly reporting this measure's data in future rulemaking.
c. Summary of Previously Finalized and Newly Finalized PCHQR Program Measures for the FY 2022 Program Year and Subsequent Years
This table summarizes the PCHQR Program measure set for the FY 2022 program year.


6. Possible New Quality Measure Topics for Future Years
a. Background
As discussed in section I.A.2. of the preamble of the FY 2019 IPPS/LTCH PPS final rule (83 FR 41147 through 41148), we have begun analyzing our quality reporting and quality payment programs' measures using the framework we developed for the Meaningful Measures Initiative. We have also discussed future quality measure topics and quality measure domain areas in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50280), the FY 2016 IPPS/LTCH PPS final rule (80 FR4979), the FY 2017 IPPS/LTCH PPS final rule (81 FR 25211), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38421 through 38423), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41618 through 41621).
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19507 through 19508), we again sought public comment on the topics we should consider for quality measurement in the PCHQR Program. In the proposed rule, we stated that we were particularly interested in public comments on measures that could balance the need to assess pain management against efforts to ensure that providers are not incentivized to overprescribe opioids to patients in the PCH setting. We also sought public comment on potential future measures that could assess alternative pain management methodologies for cancer patients.
b. Overview of Pain Management Issues and Request for Comments on Pain Management Measures and Measurement Concepts for the Cancer Patient Population
As discussed earlier, we are finalizing our proposal to remove the current pain management questions from the version of the HCAHPS Survey implemented in the PCHQR Program beginning with October 1, 2019 discharges in order to avoid any potential unintended consequences related to the perception that providers may be incentivized to overprescribe opioids to cancer patients. In the proposed rule, we also discussed how the opioid epidemic is a national crisis, and that we are interested in the feasibility of adopting quality measures that examine a PCH's utilization of pain management strategies other than opioid prescriptions when furnishing care to its patients. We recognize that unintended opioid overdose fatalities have reached epidemic proportions in the last 20 years and are a major public health concern in the United States.[704] As such, reducing the number of unintended opioid overdoses is a priority for HHS. Concurrent prescriptions of opioids or opioids and benzodiazepines put patients at greater risk of unintended opioid overdose due to increased risk of respiratory depression.[705 706] In addition, an analysis of more than 1 million hospital admissions in the United States found that over 43 percent of all patients with nonsurgical admissions were exposed to multiple opioids during their hospitalization.[707] As such, we believe that it is imperative to not inadvertently support the over-prescription of opioids by promoting opioids as a primary pain management remedy for cancer patients. In conjunction with that, we also recognize the need to be responsive to the unique needs of the cancer patient cohort by continually examining the quality measurement landscape for quality measures that balance pain management with efforts to address the opioid epidemic.
We recognize the importance of including quality measures that adequately assess cancer patient pain and quality measures that assess a PCH's use of alternative pain management methodologies. We believe that these types of measures can assess critical components of cancer care. Studies examining the frequency and quality of cancer pain management show room for improvement in these areas—for example, a systematic review revealed that, despite a 25-percent decrease in under-treatment of cancer pain between 2007 and 2013, approximately one-third of patients living with cancer still have pain that is inadequately treated.[708] Further, postsurgical complications related to inadequate pain management negatively affect patient welfare and hospital performance because of extended lengths of stay and readmissions, both of which increase the cost of care.[709] This raises concern in the context of the patient safety issues related to pain management (that is, a patient's physical safety during the administration of sedatives and complications associated with catheter administration).[710] In addition, patients who have not been treated adequately for pain management may be reluctant to seek medical care for other health problems.[711]
On August 7, 2018, the Alliance of Dedicated Cancer Centers,[712] which is a consortium of cancer hospitals that includes among its members 10 of the 11 participating PCHs for the PCHQR Program, convened a group of expert stakeholders to discuss and provide recommendations regarding best practices for the future of pain measurement among cancer patients, within the context of the opioid crisis in the United States. Participants included cancer patient advocates, clinicians, researchers, and health care quality professionals. The participants discussed the pros and cons of various methods to collect and report performance measures related to cancer pain and cancer pain management. The participants acknowledged the importance of addressing the national opioid crisis. However, for cancer patients specifically, the participants unanimously supported ongoing pain-related quality measurement. Further, the participants indicated that the relatively high prevalence of pain symptoms in the cancer patient population,[713] particularly in patients with advanced disease or metastatic cancer, underscores the need for feasible, valid, and reliable pain measures. They also added that pain assessment offers clinicians the greatest utility when the information collected can be used to identify personalized pain management goals for patients.
Further, we are aware of the existence of other cancer-specific, non-survey, patient experience assessment tools that evaluate cancer patient pain and may be more appropriate than the HCAHPS Survey pain questions which, after consideration of public comments, we are removing from the survey. As such, we believe there should be consideration given to the use of pain-related patient experience items for cancer patients, with a shifting focus toward Patient-Reported Outcome (PRO)-Performance Measures (PRO-PMs) in the mid and longer term (for example, 3 years, 5 years). Specifically, a growing body of research demonstrates the benefits of integration of PROs into oncology practice, including improved patient outcomes and survival.[714 715]
Accordingly, in the proposed rule we sought public comment on measures and measurement concepts that can be further developed that would assess appropriate pain management in the cancer patient population. Specific topics could include measures that assess cancer patient safety, patient and family education, and patient experience and engagement (specifically PRO-PMs) in the context of cancer pain management. We also invited public comment on the potential future adoption of measures that assess post-treatment addiction prevention for cancer patients. Lastly, we invited public comment on existing measures or measurement concepts that evaluate pain management for cancer patients, and do not involve opioid use.
Comment: Commenters supported CMS' focus on developing additional pain management PRO measures. The commenters indicated that these newly developed measures should be designed to avoid inadvertently incentivizing the over-prescribing of opioid medication, while also recognizing that opioid medications are an important tool for controlling cancer-related pain. Further, in the years ahead, the tools available to treat acute and chronic pain will continue to expand and patient engagement on these treatment options will remain of critical importance. Commenters encouraged CMS to continue to facilitate research and development of patient-reported outcome performance measures (PROPMs) for health-related quality of life and pain in breast, colon, and non-small lung cancer patients receiving chemotherapy with curative intent, as well as pain and communication measures for patients receiving palliative care. Commenters also noted that while PRO measures are relatively complex to develop and time-consuming to implement, there is compelling data to suggest that collection of PRO data can make a significant difference in patient outcomes when results are actively monitored and paired with timely intervention. Lastly, commenters advised CMS to consider the standards of undue burden to cancer centers and physician practices in its' evaluation of appropriate PRO-PM measures for the PCHQR Program, especially as it relates to Electronic Medical Record (EMR) interoperability and patient survey fatigue.
Response: We appreciate the commenters' feedback regarding PRO-PM measures in the context of cancer patient pain management. We will further explore the options and suggestions provided as we continue look to identify appropriate PRO-PM measures for the PCHQR measure set.
Comment: A few commenters were supportive of CMS' efforts to identify existing measures or measurement concepts that evaluate pain management for cancer patients, and do not involve opioid use. Commenters noted that as CMS considers new measures to curb opioid misuse, it is critical that these measures contain appropriate exclusions to ensure that people living with serious illness have access to necessary medications. At a minimum, exclusions should specify patients who have elected or are discharged to hospice, as well as those who are receiving palliative care. Additionally, other patients with serious illness, such as patients with cancer, AIDS, end-stage chronic lung disease, end stage renal disease, heart failure, hemophilia, or sickle cell disease, should be excluded. Commenters advised CMS to consider the following topical areas when looking to expand the pain management domain of the PCHQR measure set: causes of pain (for example, recurrent disease, second malignancy or late onset treatment effects); pain effect on sleep; pain interference with therapy activities; and pain interference with day-to-day activities.
Lastly, one commenter indicated that there are existing stakeholders that manufacture a range of technologies that can markedly reduce the need to prescribe opioids to patients experiencing chronic and acute pain. Several of these devices may be suitable for use in addressing the acute and chronic pain needs of cancer patients. As such, the commenter recommended that CMS work with these stakeholders to structure those measures in a way that accommodates the evaluation and use of device-based alternatives as an option to prescribe systemic opioids.
Response: We thank the commenters for their opinions and recommendations, and will take them into consideration as we continue to consider possible new quality measure topics for future years.
7. Maintenance of Technical Specifications for Quality Measures
We maintain technical specifications for the PCHQR Program measures, and we periodically update those specifications. The specifications may be found on the QualityNet website at: https://qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1228774479863.
We also use a subregulatory process to make nonsubstantive updates to measures used for the PCHQR Program (79 FR 50281).
8. Public Display Requirements
a. Background
Under section 1866(k)(4) of the Act, we are required to establish procedures for making the data submitted under the PCHQR Program available to the public. Such procedures must ensure that a PCH has the opportunity to review the data that are to be made public with respect to the PCH prior to such data being made public. Section 1866(k)(4) of the Act also provides that the Secretary must report quality measures of process, structure, outcome, patients' perspective on care, efficiency, and costs of care that relate to services furnished in such hospitals on the CMS website.
In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57191 through 57192), we finalized that although we would continue to use rulemaking to establish what year we first publicly report data on each measure, we would publish the data as soon as feasible during that year. We also stated that our intent is to make the data available on at least a yearly basis, and that the time period for PCHs to review their data before the data are made public would be approximately 30 days in length. We announce the exact data review and public reporting timeframes on a CMS website and/or on our applicable Listservs.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41623) and the CY 2019 OPPS/ASC final rule with comment period (83 FR 59149 through 59153), we finalized our public display requirements for the FY 2021 program year.
We recognize the importance of being transparent with stakeholders and keeping them abreast of any changes that arise with the PCHQR Program measure set. As such, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19508 through 19510), we made two proposals regarding the timetable for the public display of data for specific PCHQR Program measures.
b. Public Display of the Admissions and Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy Measure Beginning With CY 2020
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19508 through 19509), we proposed to begin public reporting of the Admissions and Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy measure in CY 2020. In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57187), we stated that we would publicly report the risk-standardized admission rate (RSAR) and risk-standardized ED visit rate (RSEDR) for the Admissions and Emergency Department (ED) Visits for the Patients Receiving Outpatient Chemotherapy measure for all participating PCHs with 25 or more eligible patients per measurement period. We stated that this threshold allowed us to maintain a reliability of at least 0.4 for publicly reported data (as measured by the interclass correlation coefficient (ICC). We also noted that if a PCH did not meet the 25-eligible patient threshold, we would include a footnote on the Hospital Compare website indicating that the number of cases is too small to reliably measure that PCH's rate, but that these patients and PCHs would still be included when calculating the national rates for both the RSAR and RSEDR (81 FR 57187). To prepare PCHs for the public reporting of this measure, we also indicated that we would conduct a confidential national reporting (dry run) of measure results. The objectives of the confidential national reporting were to: (1) Educate PCHs and other stakeholders about the measure; (2) allow PCHs to review their measure results and data prior to public reporting; (3) answer questions from PCHs and other stakeholders; (4) test the production and reporting process; and (5) identify potential technical changes to the measure specifications that might be needed.
We recently completed the confidential national reporting for this measure and have assessed the preliminary results to ensure data accuracy and completeness. Further, we confidentially reported results for the measure to the participating PCHs in October 2018, based on Medicare claims data that were collected on chemotherapy treatments performed from July 1, 2016-June 30, 2017. To execute this confidential reporting, we utilized facility-specific reports (FSRs), which allow facilities to preview measure results and patient data prior to public reporting. The FSRs included the following elements: Measure performance results; national results; detailed patient-level data used to calculate measure results; and a summary of each facility's patient-mix. To ensure continuity in the observed measure performance results, we intend to complete a subsequent round of confidential national reporting in the spring of 2019, using Medicare claims data from July 1, 2017 through June 30, 2018.
Given the success of our first round of confidential reporting and the associated timeline of our subsequent round of confidential reporting, we proposed to begin publicly reporting performance data on the Admissions and Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy measure in CY 2020. We stated our belief that this proposed timeline allows for more accurate assessment of measure results and allows both CMS and the participating PCHs adequate time to review all the confidential reporting results.
Comment: Several commenters supported the proposal to begin public reporting of the Admissions and Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy measure in CY 2020. A few commenters noted support for public display of the measure but recommended that CMS delay reporting for at least 1 year to allow for the provision of additional dry-run data and to ensure that measure data is returning valid results.
Response: In response to recommendations that we delay public reporting by 1 year, we note that we have completed the confidential national reporting for this measure and have assessed the preliminary results to ensure data accuracy and completeness; and therefore, have confirmed that the measure data is returning valid results. As such, we believe it is appropriate to publicly report the Admissions and Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy measure in CY 2020.
Comment: A few commenters noted that they are looking forward to CMS' announcement of the data period that will be included when the measure is publicly displayed in CY 2020.
Response: We thank commenters for their input. We are not able to specify the data reporting period that will be included in the publicly displayed data for this measure at this time. We will announce additional information on the public display to affected providers as soon as is practicable.
Despite our belief that public reporting of this measures is both important and appropriate, we note that planned website improvements may result in a delay in our ability to begin public reporting of this measure. Accordingly, after consideration of the public comments we received, we are finalizing our proposal with a modification to clarify that we will publicly report data for the Admissions and Emergency Department (ED) Visits for Patients Receiving Outpatient Chemotherapy measure as soon as is practicable, rather than beginning in CY 2020, as proposed.
c. Public Display of Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) Measures
(1) Public Display of the Colon and Abdominal Hysterectomy SSI, MRSA, CDI and HCP Measures in CY 2019
At present, all PCHs are reporting the CDC NHSN Healthcare-Associated Infection (HAI) Colon and Abdominal Hysterectomy SSI, MRSA, CDI, and HCP data to the National Healthcare Safety Network (NHSN) for purposes of the PCHQR Program. We finalized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41622) that we would provide stakeholders with performance data for these measures as soon as practicable (that is, we will publicly report it on the Hospital Compare website via the next available Hospital Compare release). In addition, we noted that the CDC announced that HAI data reported to the NHSN for 2015 will be used as the new baseline, serving as a new “reference point” for comparing progress.[716] Currently, these rebaselining efforts—specifically, generation and implementation of new predictive models used to calculate SIRs—are complete. As such, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19509), we proposed to publicly report data for the Colon and Abdominal Hysterectomy SSI, MRSA, CDI, and HCP measures beginning with the October 2019 Hospital Compare release.
Comment: Several commenters supported the proposal to publicly display the CDC National Health Safety Network (NHSN) measures beginning with the October 2019 release of Hospital Compare. A few specifically supported the proposed public display of the HCP measure, noting that cancer patients are at higher risk for influenza related complications.
Response: We thank the commenters for their support.
Comment: A few commenters opposed the proposal to publicly display the MRSA, CDI, and SSI measures beginning with the October 2019 release of Hospital Compare due to concerns that the cancer patient population is at increased risk for HAIs because treatment leaves patients immunocompromised. Commenters noted that comparing PCHs to other hospitals could lead to unfair performance comparisons and recommended that CMS work with NHSN to identify an appropriate strategy for displaying data for these measures. A few commenters specifically expressed concern that testing for CDI occurs at a higher frequency in the cancer population and is not accurate enough to distinguish between CDI infection and CDI colonization. Commenters expressed concern that displaying CDI measure data would not provide useful information to the public.
Response: We noted in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41622) that we would provide stakeholders with performance data for these measures as soon as practicable and that we would publicly report it on the Hospital Compare website via the next available Hospital Compare release. We recognize commenters' concerns that HAIs, and CDI in particular, may occur at a higher frequency than the general patient population due to clinical and treatment variations and believe that it is especially important to track and share this information on Hospital Compare so that this vulnerable patient population can make informed decisions. We do not believe that increased rates of HAIs warrant limiting patient access to measure information. The predictive models used to calculate these summarized measures take into account the hospital's status as a cancer hospital, thereby accounting for the increased risk of HAI in this patient population.
With respect to concerns that unfair performance comparisons will be made between PCHs and other hospitals, we note that PCH measure data are calculated taking cancer hospital status into account, specifically the increased HAI risk among their patients, and the measure data displayed for the 11 participating PPS-Exempt Cancer Hospitals as a separate and discrete group on Hospital Compare. Further, we note that cancer patients are recognized as a unique cohort, thus comparisons of measure data between participating PCHs takes precedence over data comparisons across other hospitals with broader patient populations. Moreover, we believe publicly displaying HAI measure data will provide meaningful data to participating PCHs, cancer patients, and their families when choosing care options.
Despite our belief that public reporting of the Colon and Abdominal Hysterectomy SSI, MRSA, CDI, and HCP measures is both important and appropriate, we note that planned website improvements may result in a delay in our ability to begin public reporting of these measures. Accordingly, after consideration of the public comments we received, we are finalizing our proposal with a modification to clarify that we will publicly report data for the Colon and Abdominal Hysterectomy SSI, MRSA, CDI, and HCP measures as soon as is practicable, rather than beginning with the October 2019 Hospital Compare release, as proposed. We are currently targeting a January 2020 Hospital Compare initial public reporting release date for these measures.
(2) Continued Deferral of Public Display of the CAUTI and CLABSI Measures
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59149 through 59153), we finalized that we would not remove the Catheter-Associated Urinary Tract Infection (CAUTI) Outcome Measure (PCH-5/NQF #0138) and the Central Line-Associated Bloodstream Infection (CLABSI) Outcome Measure (PCH-4/NQF #0139) from the PCHQR measure set. We also noted that we will continue to defer public reporting for the CAUTI and CLABSI measures (83 FR 59153).
We are continuing to work alongside the CDC to evaluate the performance data for the updated, risk-adjusted versions of the CAUTI and CLABSI measures so that we can draw conclusions about their statistical significance in accordance with current risk adjustment methods defined by CDC. In order to allow adequate time for data collection by the CDC, submission of those data to CMS, and our review of the data for accuracy and completeness, we believe that the earliest we will be able to publicly display information on the revised versions of the CAUTI and CLABSI measures will be CY 2022. Therefore, we will continue to defer public reporting of the CAUTI and CLABSI measures and intend to provide stakeholders with performance data on the measures as soon as practicable.
Comment: A few commenters supported the delay of public display of the CLABSI and CAUTI measures, noting that the definitions and organism lists have been changing and comparisons across hospitals may be difficult to make.
Response: We thank commenters for their support. We will continue to defer public reporting of the CAUTI and CLABSI measures.
d. Summary of Finalized Public Display Requirements for the PCHQR Program
Our finalized public display requirements for the PCHQR Program are shown in the following table.

9. Form, Manner, and Timing of Data Submission
a. Background
Data submission requirements and deadlines for the PCHQR Program are posted on the QualityNet website at: http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228772864228.
b. Confidential National Reporting for Certain Existing PCHQR Measures
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19510), we proposed to conduct a confidential national reporting for data collection of the following measures in the PCHQR measure set:
- Proportion of patients who died from cancer receiving chemotherapy in the last 14 days of life (NQF #0210).
- Proportion of patients who died from cancer admitted to the ICU in the last 30 days of life (NQF #0213).
- Proportion of patients who died from cancer not admitted to hospice (NQF #0215).
- Proportion of patients who died from cancer admitted to hospice for less than 3 days (NQF #0216).
- 30-Day Unplanned Readmissions for Cancer Patients measure (NQF #3188).
(1) Background
We initially adopted the four end-of-life care measures in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38414 through 38420) for inclusion in the PCHQR Program beginning with the FY 2020 program year. We also finalized that the initial data collection period would be from July 1, 2017 through June 30, 2018 (82 FR 38424). After we adopted the measures, the American Society of Clinical Oncology (ASCO), which is the measure steward, updated their technical specifications. We believe that these updates are not substantive and that we do not need to use the rulemaking process to incorporate them. We also note that there has been no change in the measures' data source. Specifically, the measures will continue to be calculated using Medicare claims data.
We initially adopted the 30-Day Unplanned Readmissions for Cancer Patients measure (NQF #3188) in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41614 through 41616). This is also a claims-based measure; adopted for implementation beginning with the FY 2021 program year and with an initial data collection period of October 1, 2018 through September 30, 2019 (83 FR 41616).
(2) Confidential National Reporting for Data Collection
To prepare PCHs for public reporting, in the proposed rule, we proposed to conduct two confidential reporting periods of measure results prior to public reporting. Consistent with previous confidential national reporting efforts for measures in the PCHQR Program, we stated that the objectives of the confidential national reporting are to: (1) Educate PCHs and other stakeholders about the measures; (2) allow PCHs to review their measure results and data prior to public reporting; (3) answer questions from PCHs and other stakeholders; (4) test the production and reporting process; and (5) identify potential additional technical changes to the measure specifications that might be needed. We also stated that we believe these confidential national reporting activities will enable hospitals to gain data collection and reporting experience familiarity with these refined measures for their efforts to improve quality and better understand the measure specifications and associated data. We stated that confidential national reporting is important because it affords CMS an opportunity to examine a measure's performance prior to publicly sharing data with stakeholders and is a method of ensuring that the publicly reported measure performance results are as accurate as possible. Confidential national reporting will also allow both CMS and participating PCHs adequate time to review all the performance results for the respective measures. This will mitigate the possibility of CMS having to suppress inaccurate and/or inadequate measure data, because we will have had an opportunity to preview it over a broader span of time than the standard 30-day preview period associated with public reporting.
For the group end-of-life care measures, we proposed to conduct confidential national reporting using Medicare claims data collected from July 1, 2019 through June 30, 2020. For the 30-Day Unplanned Readmissions for Cancer Patients measure, we proposed to conduct confidential national reporting using Medicare claims data collected from October 1, 2019 through September 30, 2020. We stated that we plan to include measure results from the confidential national reporting in the facility-specific feedback reports (FSRs) that we provide to PCHs. The FSRs will include the following elements: Measure performance results, national results (based on the performance of the 11 PCHs), detailed patient-level data used to calculate measure results and a summary of each PCH's patient-mix.
Comment: Several commenters supported the proposal to conduct confidential national reporting of the four end-of-life measures using Medicare claims data collected from July 1, 2019 through June 30, 2020. A commenter noted its agreement that these confidential reports will allow the PCHs to review results, understand the technical specifications, and review any potential concerns regarding attribution and risk adjustment.
Response: We thank the commenters for their support.
Comment: Several commenters supported the proposal to conduct confidential national reporting for the 30-Day Unplanned Readmissions for Cancer Patients measure using Medicare claims data collected from October 1, 2019 through September 30, 2020. A few commenters noted that these reports are especially important for claims-based measures to ensure that the technical measure specifications capture the measures accurately.
Response: We thank the commenters for their support.
After consideration of public comments, we are finalizing our proposals to: (1) Conduct confidential national reporting of the four end-of-life measures using Medicare claims data collected from July 1, 2019 through June 30, 2020; and (2) conduct confidential national reporting for the 30-Day Unplanned Readmissions for Cancer Patients measure using Medicare claims data collected from October 1, 2019 through September 30, 2020 as proposed.
10. Extraordinary Circumstances Exceptions (ECE) Policy Under the PCHQR Program
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41623 through 41624), for a discussion of the Extraordinary Circumstances Exceptions (ECE) policy under the PCHQR Program. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19510), we did not propose any changes to this policy.
C. Long-Term Care Hospital Quality Reporting Program (LTCH QRP)
1. Background
The Long-Term Care Hospital Quality Reporting Program (LTCH QRP) is authorized by section 1886(m)(5) of the Act, and it applies to all hospitals certified by Medicare as long-term care hospitals (LTCHs). Under the LTCH QRP, the Secretary must reduce by 2 percentage points the annual update to the LTCH PPS standard Federal rate for discharges for an LTCH during a fiscal year if the LTCH has not complied with the LTCH QRP requirements specified for that fiscal year. For more information on the requirements we have adopted for the LTCH QRP, we refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51743 through 51744), the FY 2013 IPPS/LTCH PPS final rule (77 FR 53614), the FY 2014 IPPS/LTCH PPS final rule (78 FR 50853), the FY 2015 IPPS/LTCH PPS final rule (79 FR 50286), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49723 through 49725), the FY 2017 IPPS/LTCH PPS final rule (81 FR 57193), the FY 2018 IPPS/LTCH PPS final rule (82 FR 38425 through 38426), and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41624 through 41634).
While we did not solicit comments on previously finalized LTCH QRP policies, we received some comments, which are summarized in this final rule.
Comment: A few commenters supported the proposed changes to the LTCH QRP, recognizing that these changes are part of a multiyear process to reform patient assessment and quality reporting across multiple levels of care. A commenter supported CMS' effort to align areas of best practices with other quality reporting programs, specifically when accounting for social risk factors, applying the Meaningful Measures Framework in support of the Patients Over Paperwork Initiative, and removing, adopting, and retaining quality measures according to standardized decision criteria.
Response: We appreciate the commenters' support and feedback.
Comment: A commenter supported CMS' effort to show the implications and potential methods for addressing health disparities regarding social risk factors in quality measurement and supported the concept of using measures already included in quality reporting programs as tools for hospitals to identify gaps in their respective patients' outcomes. The commenter also requested that attribution details for each measure be addressed in technical specifications.
Response: We appreciate the commenter's support and feedback and will take these comments into consideration.
Comment: A few commenters requested that CMS lower the LTCH QRP compliance threshold of 80 percent for assessment-based items given the number of data elements that have been added to the LTCH CARE Data Set.
Response: We appreciate the commenters' feedback. We did not propose any changes to the compliance threshold, which has been codified in the LTCH QRP regulations at § 412.560(f).
2. General Considerations Used for the Selection of Measures for the LTCH QRP
For a detailed discussion of the considerations we use for the selection of LTCH QRP quality, resource use, and other measures, we refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49728).
3. Quality Measures Currently Adopted for the FY 2021 LTCH QRP
The LTCH QRP currently has 15 measures for the FY 2021 LTCH QRP, which are set out in the following table:

While we did not solicit comments on previously adopted measures (with the exception of the Discharge to Community-PAC LTCH QRP measure discussed in VIII.C.4.c. and the policies regarding public display of the Drug Regimen Review Conducted With Follow-Up for Identified Issues-PAC LTCH QRP measure discussed in section VIII.C.10. of this rule), we received a comment.
Comment: A commenter supported maintaining the Influenza Vaccination Coverage Among Healthcare Personnel (NQF #0431) quality measure in the LTCH QRP, citing the importance of publicly reporting measure data as an important tool for patients and families seeking to evaluate an LTCH setting and an essential component in the identification and management of influenza outbreaks.
Response: We appreciate the commenter's support. We would like to clarify that we did not propose any changes to the previously finalized Influenza Vaccination Coverage Among Healthcare Personnel (NQF #0431) measure.
4. LTCH QRP Quality Measure Proposals Beginning With the FY 2022 LTCH QRP
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19511 through 19517), we proposed to adopt two process measures for the LTCH QRP that would satisfy section 1899B(c)(1)(E)(ii) of the Act, which requires that the quality measures specified by the Secretary include measures with respect to the quality measure domain titled “Accurately communicating the existence of and providing for the transfer of health information and care preferences of an individual to the individual, family caregiver of the individual, and providers of services furnishing items and services to the individual when the individual transitions from a post-acute care (PAC) provider to another applicable setting, including a different PAC provider, a hospital, a critical access hospital, or the home of the individual.” Given the length of this domain title, hereafter, we will refer to this quality measure domain as “Transfer of Health Information.”
The two measures we proposed to adopt are: (1) Transfer of Health Information to the Provider—Post-Acute Care (PAC); and (2) Transfer of Health Information to the Patient—Post-Acute Care (PAC). Both of these proposed measures support our Meaningful Measures priority of promoting effective communication and coordination of care, specifically the Meaningful Measure area of the transfer of health information and interoperability.
In addition to the two measure proposals, in the proposed rule (84 FR 19517), we proposed to update the specifications for the Discharge to Community—Post Acute Care (PAC) LTCH QRP measure to exclude baseline nursing facility (NF) residents from the measure.
a. Transfer of Health Information to the Provider—Post-Acute Care (PAC) Measure
The proposed Transfer of Health Information to the Provider—Post-Acute Care (PAC) Measure is a process-based measure that assesses whether or not a current reconciled medication list is given to the subsequent provider when a patient is discharged or transferred from his or her current PAC setting.
(1) Background
In 2013, 22.3 percent of all acute hospital discharges were discharged to PAC settings, including 11 percent who were discharged to home under the care of a home health agency, and 9 percent who were discharged to SNFs.[717] The proportion of patients being discharged from an acute care hospital to a PAC setting was greater among beneficiaries enrolled in Medicare fee-for-service (FFS). Among Medicare FFS patients discharged from an acute hospital, 42 percent went directly to PAC settings. Of that 42 percent, 20 percent were discharged to a SNF, 18 percent were discharged to a home health agency (HHA), 3 percent were discharged to an IRF, and 1 percent were discharged to an LTCH.[718] Of the Medicare FFS beneficiaries with an LTCH stay in FYs 2016 and 2017, an estimated 9 percent were discharged or transferred to an acute care hospital, 18 percent discharged home with home health services, 38 percent discharged or transferred to a SNF, and 10 percent discharged or transferred to another PAC setting (for example, an IRF, a hospice, or another LTCH).[719]
The transfer and/or exchange of health information from one provider to another can be done verbally (for example, clinician-to-clinician communication in-person or by telephone), paper-based (for example, faxed or printed copies of records), and via electronic communication (for example, through a health information exchange (HIE) network using an electronic health/medical record (EHR/EMR), and/or secure messaging). Health information, such as medication information, that is incomplete or missing increases the likelihood of a patient or resident safety risk, and is often life-threatening.[720 721 722 723 724 725] Poor communication and coordination across health care settings contributes to patient complications, hospital readmissions, emergency department visits, and medication errors.[726 727 728 729 730 731 732 733 734 735] Communication has been cited as the third most frequent root cause in sentinel events, which The Joint Commission defines [736] as a patient safety event that results in death, permanent harm, or severe temporary harm. Failed or ineffective patient handoffs are estimated to play a role in 20 percent of serious preventable adverse events.[737] When care transitions are enhanced through care coordination activities, such as expedited patient information flow, these activities can reduce duplication of care services and costs of care, resolve conflicting care plans, and prevent medical errors.[738 739 740 741 742]
Care transitions across health care settings have been characterized as complex, costly, and potentially hazardous, and may increase the risk for multiple adverse outcomes.[743 744] The rising incidence of preventable adverse events, complications, and hospital readmissions have drawn attention to the importance of the timely transfer of health information and care preferences at the time of transition. Failures of care coordination, including poor communication of information, were estimated to cost the U.S. health care system between $25 billion and $45 billion in wasteful spending in 2011.[745] The communication of health information and patient care preferences is critical to ensuring safe and effective transitions from one health care setting to another.[746 747]
Patients in PAC settings often have complicated medication regimens and require efficient and effective communication and coordination of care between settings, including detailed transfer of medication information.[748 749 750] Individuals in PAC settings may be vulnerable to adverse health outcomes due to insufficient medication information on the part of their health care providers, and the higher likelihood for multiple comorbid chronic conditions, polypharmacy, and complicated transitions between care settings.[751 752] Preventable adverse drug events (ADEs) may occur after hospital discharge in a variety of settings including PAC.[753] A 2014 Office of Inspector General report found that 21 percent of Medicare patients in LTCHs experienced adverse events, with 31 percent of those events being medication related. Over half of the adverse events and temporary harm events were clearly or likely preventable.[754] Patient stays in LTCHs present more opportunities for harm events than other settings because the stays are longer. Medication errors and one-fifth of ADEs occur during transitions between settings, including admission to or discharge from a hospital to home or a PAC setting, or transfer between hospitals.[755 756]
Patients in PAC settings are often taking multiple medications. Consequently, PAC providers regularly are in the position of starting complex new medication regimens with little knowledge of the patients or their medication history upon admission. Furthermore, inter-facility communication barriers delay resolving medication discrepancies during transitions of care.[757] Medication discrepancies are common,[758] and found to occur in 86 percent of all transitions, increasing the likelihood of ADEs.[759 760 761] Up to 90 percent of patients experience at least one medication discrepancy in the transition from hospital to home care, and discrepancies occur within all therapeutic classes of medications.[762 763]
Transfer of a medication list between providers is necessary for medication reconciliation interventions, which have been shown to be a cost-effective way to avoid ADEs by reducing errors,764 765 766 especially when medications are reviewed by a pharmacist using electronic medical records.[767]
(2) Stakeholder and Technical Expert Panel (TEP) Input
The proposed measure was developed after consideration of feedback we received from stakeholders and four TEPs convened by our contractors. Further, the proposed measure was developed after evaluation of data collected during two pilot tests we conducted in accordance with the CMS Measures Management System Blueprint.
Our measure development contractors constituted a TEP which met on September 27, 2016,[768] January 27, 2017,[769] and August 3, 2017 [770] to provide input on a prior version of this measure. Based on this input, we updated the measure concept in late 2017 to include the transfer of a specific component of health information—medication information. Our measure development contractors reconvened this TEP on April 20, 2018 for the purpose of obtaining expert input on the proposed measure, including the measure's reliability, components of face validity, and feasibility of being implemented across PAC settings. Overall, the TEP was supportive of the proposed measure, affirming that the measure provides an opportunity to improve the transfer of medication information. A summary of the April 20, 2018 TEP proceedings titled “Transfer of Health Information TEP Meeting 4—June 2018” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Our measure development contractors solicited stakeholder feedback on the proposed measure by requesting comment on the CMS Measures Management System Blueprint website, and accepted comments that were submitted from March 19, 2018 to May 3, 2018. The comments received expressed overall support for the measure. Several commenters suggested ways to improve the measure, primarily related to what types of information should be included at transfer. We incorporated this input into development of the proposed measure. The summary report for the March 19 to May 3, 2018 public comment period titled “IMPACT—Medication Profile Transferred Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
(3) Pilot Testing
The proposed measure was tested between June and August 2018 in a pilot test that involved 24 PAC facilities/agencies, including five IRFs, six SNFs, six LTCHs, and seven HHAs. The 24 pilot sites submitted a total of 801 records. Analysis of agreement between coders within each participating facility (266 qualifying pairs) indicated a 93-percent agreement for this measure. Overall, pilot testing enabled us to verify its reliability, components of face validity, and feasibility of being implemented across PAC settings. Further, more than half of the sites that participated in the pilot test stated during the debriefing interviews that the measure could distinguish facilities or agencies with higher quality medication information transfer from those with lower quality medication information transfer at discharge. The pilot test summary report titled “Transfer of Health Information 2018 Pilot Test Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
(4) Measure Applications Partnership (MAP) Review and Related Measures
We included the proposed measure in the LTCH QRP section of the 2018 Measures Under Consideration (MUC) list. The MAP conditionally supported this measure pending NQF endorsement, noting that the measure can promote the transfer of important medication information. The MAP also suggested that CMS consider a measure that can be adapted to capture bi-directional information exchange, and recommended that the medication information transferred include important information about supplements and opioids. More information about the MAP's recommendations for this measure is available at: http://www.qualityforum.org/Publications/2019/02/MAP_2019_Considerations_for_Implementing_Measures_Final_Report_-_PAC-LTC.aspx.
As part of the measure development and selection process, we also identified one NQF-endorsed quality measure similar to the proposed measure, titled Documentation of Current Medications in the Medical Record (NQF #0419, CMS eCQM ID: CMS68v8). This measure was adopted as one of the recommended adult core clinical quality measures for eligible professionals for the EHR Incentive Program beginning in 2014 and was also adopted under the Merit-based Incentive Payment System (MIPS) quality performance category beginning in 2017. The measure is calculated based on the percentage of visits for patients aged 18 years and older for which the eligible professional or eligible clinician attests to documenting a list of current medications using all resources immediately available on the date of the encounter.
The proposed Transfer of Health Information to the Provider—Post-Acute Care (PAC) measure addresses the transfer of information whereas the NQF-endorsed measure #0419 assesses the documentation of medications, but not the transfer of such information. This is important as the proposed measure assesses for the transfer of medication information for the proposed measure calculation. Further, the proposed measure utilizes standardized patient assessment data elements (SPADEs), which is a requirement for measures specified under the Transfer of Health Information measure domain under section 1899B(c)(1)(E) of the Act, whereas NQF #0419 does not.
After review of the NQF-endorsed measure, we determined that the proposed Transfer of Health Information to the Provider—Post-Acute Care (PAC) measure better addresses the Transfer of Health Information measure domain, which requires that at least some of the data used to calculate the measure be collected as standardized patient assessment data through the post-acute care assessment instruments. Section 1886(m)(5)(D)(i) of the Act requires that any measure specified by the Secretary be endorsed by the entity with a contract under section 1890(a) of the Act, which is currently the National Quality Form (NQF). However, when a feasible and practical measure has not been NQF endorsed for a specified area or medical topic determined appropriate by the Secretary, section 1886(m)(5)(D)(ii) of the Act allows the Secretary to specify a measure that is not NQF endorsed as long as due consideration is given to the measures that have been endorsed or adopted by a consensus organization identified by the Secretary. For the reasons previously discussed, we believe that there is currently no feasible NQF-endorsed measure that we could adopt under section 1886(m)(5)(D)(ii) of the Act. However, we note that we intend to submit the proposed measure to the NQF for consideration of endorsement when feasible.
(5) Quality Measure Calculation
The proposed Transfer of Health Information to the Provider—Post-Acute Care (PAC) quality measure is calculated as the proportion of patient stays with a discharge assessment indicating that a current reconciled medication list was provided to the subsequent provider at the time of discharge. The proposed measure denominator is the total number of LTCH patient stays, regardless of payer, ending in discharge to a “subsequent provider,” which is defined as a short-term general acute-care hospital, intermediate care (intellectual and developmental disabilities providers), home under care of an organized home health service organization or hospice, hospice in an institutional facility, a SNF, another LTCH, an IRF, an inpatient psychiatric facility, or a CAH. These health care providers were selected for inclusion in the denominator because they are identified as subsequent providers on the discharge destination item that is currently included on the LTCH Continuity Assessment Record and Evaluation Data Set (LTCH CARE Data Set or LCDS). The proposed measure numerator is the number of LTCH patient stays with an LCDS discharge assessment indicating a current reconciled medication list was provided to the subsequent provider at the time of discharge. For additional technical information about this proposed measure, we refer readers to the document titled, “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html. The data source for the proposed quality measure is the LCDS assessment instrument for LTCH patients.
For more information about the data submission requirements we proposed for this measure, we refer readers to the discussion in section VIII.C.8.d. of the preamble of this final rule.
Commenters submitted the following comments related to the proposed rule's discussion of the LTCH QRP quality measure proposals beginning with the FY 2022 LTCH QRP. A discussion of these comments, along with our responses, appears below. We also address comments on the proposed Transfer of Health Information to the Patient—Post-Acute Care measure (discussed further in a subsequent section of this final rule) in this section because commenters frequently addressed both proposed Transfer of Health Information measures together.
Comment: Several commenters supported the Transfer of Health Information measures, stating that they will help improve care coordination, patient safety, and care transitions.
Response: We thank the commenters for their support of the Transfer of Health Information measures.
Comment: A few commenters did not support finalizing the Transfer of Health Information measures. A few commenters suggested that instead of the proposed measures, which focus on whether medication information was transferred, CMS consider measures and approaches to collect information on the accuracy, timeliness, and clarity of critical medication information received by downstream providers, patients, and their families. A commenter described challenges in obtaining important information from acute care hospitals such as a current medication list and dosages, just prior to transition and stated that the downstream PAC provider has no control over the information received. The commenter added that the completeness and clarity of critical information transmitted from the LTCH or any other PAC provider to a patient and/or next care setting upon discharge is important.
Response: We appreciate the suggestions that CMS develop and adopt measures that assess for the accuracy, timeliness, and clarity of critical medication information received by downstream providers, patients, and their families. We agree that measure concepts of this type are important and would complement these measures that focus on whether information was transferred. We would like to note that the measures address the timeliness of the transfer of a medication list by requiring that the information is shared with the subsequent provider and/or the patient as close to the time of discharge as this is actionable. With support from a TEP, public comment, the MAP, and other stakeholders, we have determined that these measures will provide important data and greater understanding of how information is transferred, reinforcing and supporting efforts toward health information exchange. Finally, we agree with the comments that critical information transmitted from the LTCH or any other PAC provider to a patient and/or next care setting upon discharge is important. We will explore the feasibility of expanding this measure set and will use the Transfer of Health Information measures to inform future efforts.
Comment: Several commenters raised concerns about the Transfer of Health Information measures not being endorsed by NQF. Some of the commenters that raised these concerns stated that they generally supported or were not opposed to the Transfer of Health Information measures. Other commenters encouraged CMS to pursue the NQF endorsement process and a few commenters requested that we consider delaying rollout of these two new measures until endorsed by NQF. Commenters also recommended that we only adopt or implement measures that have NQF approval. A commenter elaborated on this recommendation, noting that the MAP was clear that it only “conditionally supported both measures pending NQF endorsement” and believes that CMS should not adopt the measures, or any other LTCH QRP measures, until NQF and MAP unconditionally endorse the new measures. Another commenter was opposed to the measures because they have not been endorsed by NQF.
Response: This measure is not currently NQF-endorsed, and we recognize that the NQF endorsement process is an important part of measure development. As discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19512 through 19517), we believe that the measures better address the Transfer of Health Information measure domain, which requires that at least some of the data used to calculate the measure be collected as standardized patient assessment data through the post-acute care assessment instruments, than any currently endorsed measures. While section 1886(m)(5)(D)(i) of the Act requires that any measure specified by the Secretary be endorsed by the entity with a contract under section 1890(a) of the Act, which is currently the NQF, when a feasible and practical measure has not been NQF endorsed for a specified area or medical topic determined appropriate by the Secretary, section 1886(m)(5)(D)(ii) of the Act allows the Secretary to specify a measure that is not NQF endorsed as long as due consideration is given to the measures that have been endorsed or adopted by a consensus organization identified by the Secretary. We plan to submit the measure to for NQF for endorsement consideration as soon as feasible.
Comment: A commenter suggested that other providers, such as outpatient physical therapists, should be included in the definition of a subsequent provider for the Transfer of Health Information to the Provider—Post-Acute Care measure.
Response: We appreciate the suggestion to expand the Transfer of Health Information to the Provider—Post-Acute Care measure outcome to assess the transfer of health information to other providers such as outpatient physical therapists. We recognize that sharing medication information with outpatient providers is important, and will take into consideration additional providers in future measure modifications. Through our measure development and pilot testing we learned that outpatient providers cannot always be readily identified by the PAC provider, including LTCHs. For this process measure, which serves as a building block for improving the transfer of medication information, we specified providers who will be involved in the care of the patient and medication management after discharge and can be readily identified through the discharge location item on the LCDS. The clear delineation of the recipient of the medication list in the measure specifications will improve measure reliability and validity.
Comment: A few commenters expressed concern over burden. A commenter believed that the measures have no value and so the burden for data collection is not worth the benefit. Another commenter stated that while there will be additional burden on LTCHs to collect and report data for these new measures, the benefit to patients and the CMS program outweighs the additional burden on providers.
Response: We agree that the benefit to patients outweighs any additional burden on providers. We are also very mindful of burden that may occur from the collection and reporting of our measures, as supported by the Meaningful Measures and Patients over Paperwork initiatives. We would like to emphasize that both measures are comprised of one item, and further, the activities associated with the measures align with existing requirements related to transferring information at the time of discharge in order to safeguard patients. Additionally, TEP feedback and pilot testing found that burden of reporting will not be significant. CMS believes that these measures will drive improvements in the transfer of medication information between providers and with patients, families, and caregivers.
Comment: A commenter stated that because providing medication information as part of discharge planning is a Condition of Participation (CoP) requirement for Medicaid and Medicare and the medication list can be generated from the electronic medical record, there should be no added burden to LTCHs.
Response: We believe that these measures will not substantially increase burden because we understand that many hospitals already generate medication lists as a best practice, in accordance with our interpretive guidance regarding our discharge planning CoP at § 482.43(c). While we recognize that not all LTCHs have electronic medical records, providing a medication list to the subsequent provider is standard practice and, therefore, this measure should not substantially increase burden.
Comment: A commenter provided additional data to provide context around data from an OIG report in our background section. The commenter stated that when adjusted for variations in lengths of stay, per 1,000 patient stays, LTCH patients experienced 38 adverse and temporary harm events as compared to 29, 24, and 69 adverse and temporary harm events in IRFs, SNFs, and STACHs, respectively. The commenter stated that OIG also reported that over half of these events (54 percent) were clearly or likely preventable; however, this was not out of the ordinary in comparison to the rate of preventable harm reported in SNFs (59 percent).
Response: We thank the commenter for providing this additional data and note that these data support our contention that there is room for improvement across PAC settings when it comes to adverse and temporary harm events.
Comment: A few commenters expressed concerns that the Transfer of Health Information to the Provider and Transfer of Health Information to the Patient measures are not indicative of provider quality and questioned the ability of the measures to improve patient outcomes or reduce adverse events.
Response: The Transfer of Health Information to the Provider—Post-Acute Care and Transfer of Health Information to the Patient—Post-Acute Care measures are process measures designed to address and improve an important aspect of care quality. Lack of timely transfer of medication information at transitions has been demonstrated to lead to increased risk of adverse events, medication errors and hospitalizations. In addition, public commenters and our TEP members identified many problems and gaps in the timely transfer of medication information at transitions. Process measures, such as these, are building blocks toward improved coordinated care and discharge planning, providing information that will improve shared decision making and coordination. Further, process measures provide value as they delineate negative and/or positive aspects of the health care process. These measures will capture the quality of the process of medication information transfer and, we believe, help to improve those processes.
Comment: A commenter recommended that the Transfer of Health Information to the Provider—Post-Acute Care measure be expanded to include information that would help prevent infections and facilitate appropriate infection prevention and control interventions during care transitions in addition to the medication information in the finalized measure.
Response: The Transfer of Health Information to the Provider—Post-Acute Care measure focuses on the transfer of a reconciled medication list. The measure was designed after input from TEPs, public comment, and other stakeholders that suggested the quality measures focus on the transfer of the most critical pieces of information to support patient safety and care coordination. However, we acknowledge that the transfer of many other forms of health information is important, and while the focus of this measure is on a reconciled medication list, we hope to expand our measures in the future.
Comment: Some commenters recommended ways in which the Transfer of Health Information measures specifications could be updated or changed. A commenter suggested that the “not applicable” (N/A) answer choice available in the home health version of the measure be made available in all settings, including LTCHs. A few commenters also requested clarification about why patients discharged home under the care of an organized home health service or hospice would be captured in the denominators of both Transfer of Health information measures.
Response: We are appreciative of the measure modification suggestions and would like to clarify why the response option of N/A was considered only for the Home Health version of this measure. The coding response, “N/A” or “not applicable” is used when the home health agency (HHA) was not made aware of the transfer in a timely manner, and therefore, the HHA is not able to provide the medication list at the time of transfer to the subsequent provider. For example, a HHA may not be immediately aware when a patient is taken to the emergency room. For facility settings such as the LTCH setting, where 24-hour care is being provided, the facility should always be aware and actively involved in the discharge of the patient, and therefore, able to provide the current reconciled medication list at the time of discharge. Therefore, we believe that the coding option of “N/A” would not be useful in the facility-based measure as the facility is aware and involved in the discharge. We wish to note that while the “N/A” option is considered for the HHA version of the measure, the measure specifications indicate that these patients are not removed from the denominator. In addition, discharge to home under the care of an organized HHA or hospice is captured in the denominator of both the Transfer of Health Information to Provider and Transfer of Health Information to Patient measures because this type of discharge represents two opportunities to transfer the medication list. These measures aim to assure that each of these transfers is taking place. We refer readers to the measure specifications, available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html .
Comment: A commenter urged CMS to enhance its efforts to develop standards and measures for data exchange and sharing across all care settings, including PAC, and that existing clinical and interoperability standards should be considered in the development of these and future measures. The commenter believes that ensuring interoperability across EHR systems and settings of care can unlock barriers to data sharing and care coordination between health systems, physicians and physician group practices, and PAC settings. The commenter further suggested that CMS leverage ongoing efforts to adopt data standards and implementation guides for certified EHRs, such as the USCDI and to build on efforts to base measures and calculations on data within certified EHRs. The commenter also suggested that CMS needs to consider ways to incentivize PAC providers to more readily adopt health IT.
Response: We agree with the comments on the importance of interoperability solutions to support health information transfer. First, we would like to clarify that data collection for the Transfer of Health Information measures does not require adoption of certified EHRs, nor are they calculated from EHRs. CMS and ONC are focused on improving interoperability and the timely sharing of information between providers, patients, families and caregivers. We believe that PAC provider health information exchange supports the goals of high quality, personalized, efficient healthcare, care coordination, person-centered care, and supports real-time, data driven, clinical decision making.
To further support interoperability, we recently released the Data Element Library (DEL), a new public resource aimed at advancing interoperable health information exchange by enabling users to view assessment questions and response options about demographics, medical problems, and other types of health evaluations and their associated health IT standards. The DEL includes a multitude of data elements, including all data elements adopted for use in the quality reporting programs, and not limited to data collected under the IMPACT Act. In the initial version of the DEL (https://del.cms.gov/), assessment questions and response options are mapped to LOINC and SNOMED codes where feasible. We also recognize the importance of leveraging existing standards, obtaining input from standards setting organizations, and alignment across federal interoperability efforts.
We acknowledge that meaningful use incentives have not been extended to LTCHs and other PAC providers. We will share these comments with the appropriate CMS staff and other governmental agencies to ensure they are taken into account as we continue to encourage adoption of health information technology. The Transfer of Health Information measures may encourage the electronic transfer of medication information at transitions. These measures and related efforts may help accelerate interoperability solutions.
Comment: A commenter suggested that future measures could focus on the accuracy of the medication list and the result of medication reconciliation on patient care.
Response: As supported by the CMS Meaningful Measures and Patients over Paperwork initiatives, we will take recommendations for future measures into consideration. We plan to use the data from the Transfer of Health Information measures to inform future efforts.
Comment: In comments related to both the Transfer of Health Information to the Provider and Transfer of Health Information to the Patient measures, a commenter requested the definition of a reconciled medication list and made reference to an older version of measure specifications where a medication profile had been defined.
Response: Reference to a medication profile in this comment appears to have come from measure specifications for a previous version of these measures that were posted for Blueprint public comment in March 2018. We sought input on the types of information included in a medication list from our TEP and other stakeholders. Defining the completeness of that medication list is left to the discretion of the providers and patients who are coordinating this care.
Comment: A commenter encouraged CMS to finalize revisions to “Requirements for Discharge Planning for Hospitals, Critical Access Hospitals, and Home Health Agencies” (CMS-3317-P), which would require hospitals to transfer patient information, including diagnosis and other clinical information, to the patient's next setting in a timely manner and stated that this timely information can improve continuity of care.
Response: We agree that PAC providers' receipt of timely medication information from hospitals at discharge would improve the accuracy and completeness of medication information in the patient's medical record and improve continuity of care. The Revisions to Requirements for Discharge Planning for Hospitals, Critical Access Hospitals, and Home Health Agencies proposed rule (CMS-3317-P) has not been finalized. CMS has issued an extension notice for the publication of the final rule, which extends the timeline for publication of the final rule until November 3, 2019 (please see https://www.federalregister.gov/documents/2018/11/02/2018-23922/medicare-and-medicaid-programs-revisions-to-requirements-for-discharge-planning-for-hospitals).
Comment: A commenter expressed concerns related to the validity and accuracy of the Transfer of Health Information measures and suggested that CMS should ensure accuracy of these measures.
Response: We appreciate the comments about measure accuracy and validity. Elements of validity and reliability were analyzed during pilot testing of these measures, with results showing an inter rater reliability of at least 87 percent for all tested items. As we monitor the outcomes of this measure, we will ensure that the reliability and validity of the measure will meet acceptable standards.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Transfer of Health Information to the Provider—Post-Acute Care (PAC) measure, pursuant to section 1899B(c)(1)(E) of the Act, beginning with October 1, 2020 discharges.
b. Transfer of Health Information to the Patient—Post-Acute Care (PAC) Measure
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19515 through 19517), beginning with the FY 2022 LTCH QRP, we proposed to adopt the Transfer of Health Information to the Patient—Post-Acute Care (PAC) measure, a measure that satisfies the IMPACT Act domain of Transfer of Health Information, with data collection for discharges beginning October 1, 2020. This process-based measure assesses whether or not a current reconciled medication list was provided to the patient, family, or caregiver when the patient was discharged from a PAC setting to a private home/apartment, a board and care home, assisted living, a group home, transitional living or home under care of an organized home health service organization, or a hospice.
(1) Background
In 2013, 22.3 percent of all acute hospital discharges were discharged to PAC settings, including 11 percent who were discharged to home under the care of a home health agency.[771] Of the Medicare FFS beneficiaries with an LTCH stay in fiscal years 2016 and 2017, an estimated 18 percent were discharged home with home health services, nine percent were discharged home with self-care, and two percent were discharged with home hospice services.[772]
The communication of health information, such as a reconciled medication list, is critical to ensuring safe and effective patient transitions from health care settings to home and/or other community settings. Incomplete or missing health information, such as medication information, increases the likelihood of a patient safety risk, often life-threatening.[773 774 775 776 777] Individuals who use PAC care services are particularly vulnerable to adverse health outcomes due to their higher likelihood of having multiple comorbid chronic conditions, polypharmacy, and complicated transitions between care settings.[778 779] Upon discharge to home, individuals in PAC settings may be faced with numerous medication changes, new medication regimes, and follow-up details.[780 781 782] The efficient and effective communication and coordination of medication information may be critical to prevent potentially deadly adverse effects. When care coordination activities enhance care transitions, these activities can reduce duplication of care services and costs of care, resolve conflicting care plans, and prevent medical errors.[783 784]
Finally, the transfer of a patient's discharge medication information to the patient, family, or caregiver is common practice and supported by discharge planning requirements for participation in Medicare and Medicaid programs.[785 786] Most PAC EHR systems generate a discharge medication list to promote patient participation in medication management, which has been shown to be potentially useful for improving patient outcomes and transitional care.[787]
(2) Stakeholder and TEP Input
The proposed measure was developed after consideration of feedback we received from stakeholders and four TEPs convened by our contractors. Further, the proposed measure was developed after evaluation of data collected during two pilot tests we conducted in accordance with the CMS Measures Management System Blueprint.
Our measure development contractors constituted a TEP which met on September 27, 2016,[788] January 27, 2017,[789] and August 3, 2017 [790] to provide input on a prior version of this measure. Based on this input, we updated the measure concept in late 2017 to include the transfer of a specific component of health information—medication information. Our measure development contractors reconvened this TEP on April 20, 2018 to seek expert input on the measure. Overall, the TEP members supported the proposed measure, affirming that the measure provides an opportunity to improve the transfer of medication information. Most of the TEP members believed that the measure could improve the transfer of medication information to patients, families, and caregivers. Several TEP members emphasized the importance of transferring information to patients and their caregivers in a clear manner using plain language. A summary of the April 20, 2018 TEP proceedings titled “Transfer of Health Information TEP Meeting 4—June 2018” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Our measure development contractors solicited stakeholder feedback on the proposed measure by requesting comment on the CMS Measures Management System Blueprint website, and accepted comments that were submitted from March 19, 2018 to May 3, 2018. Several commenters noted the importance of ensuring that the instruction provided to patients and caregivers is clear and understandable to promote transparent access to medical record information and meet the goals of the IMPACT Act. The summary report for the March 19 to May 3, 2018 public comment period titled “IMPACT—Medication Profile Transferred Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
(3) Pilot Testing
Between June and August 2018, we held a pilot test involving 24 PAC facilities/agencies, including five IRFs, six SNFs, six LTCHs, and seven HHAs. The 24 pilot sites submitted a total of 801 assessments. Analysis of agreement between coders within each participating facility (241 qualifying pairs) indicated an 87-percent agreement for this measure. Overall, pilot testing enabled us to verify its reliability, components of face validity, and feasibility of being implemented across PAC settings. Further, more than half of the sites that participated in the pilot test stated, during debriefing interviews, that the measure could distinguish facilities or agencies with higher quality medication information transfer from those with lower quality medication information transfer at discharge. The pilot test summary report titled “Transfer of Health Information 2018 Pilot Test Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
(4) Measure Applications Partnership (MAP) Review and Related Measures
We included the proposed measure in the LTCH QRP section of the 2018 MUC list. The MAP conditionally supported this measure pending NQF endorsement, noting that the measure can promote the transfer of important medication information to the patient. The MAP recommended that providers transmit medication information to patients that is easy to understand because health literacy can impact a person's ability to take medication as directed. More information about the MAP's recommendations for this measure is available at: http://www.qualityforum.org/Publications/2019/02/MAP_2019_Considerations_for_Implementing_Measures_Final_Report_-_PAC-LTC.aspx.
Section 1886 (m)(5)(D)(i) of the Act, requires that any measure specified by the Secretary be endorsed by the entity with a contract under section 1890(a) of the Act, which is currently the NQF. However, when a feasible and practical measure has not been NQF endorsed for a specified area or medical topic determined appropriate by the Secretary, section 1886 (m)(5)(D)(ii) of the Act allows the Secretary to specify a measure that is not NQF endorsed as long as due consideration is given to the measures that have been endorsed or adopted by a consensus organization identified by the Secretary. Therefore, in the absence of any NQF-endorsed measures that address the proposed Transfer of Health Information to the Patient—Post-Acute Care (PAC), which requires that at least some of the data used to calculate the measure be collected as standardized patient assessment data through the post-acute care assessment instruments, we believe that there is currently no feasible NQF-endorsed measure that we could adopt under section 1886(m)(5)(D)(ii) of the Act. However, we note that we intend to submit the proposed measure to the NQF for consideration of endorsement when feasible.
(5) Quality Measure Calculation
The calculation of the proposed Transfer of Health Information to the Patient—Post-Acute Care (PAC) measure would be based on the proportion of patient stays with a discharge assessment indicating that a current reconciled medication list was provided to the patient, family, or caregiver at the time of discharge.
The proposed measure denominator is the total number of LTCH patient stays, regardless of payer, ending in discharge to a private home/apartment, a board and care home, assisted living, a group home, transitional living or home under care of an organized home health service organization, or a hospice. These locations were selected for inclusion in the denominator because they are identified as home locations on the discharge destination item that is currently included on the LCDS. The proposed measure numerator is the number of LTCH patient stays with an LCDS discharge assessment indicating a current reconciled medication list was provided to the patient, family, or caregiver at the time of discharge. For technical information about this proposed measure, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html. Data for the proposed quality measure would be calculated using data from the LCDS assessment instrument for LTCH patients.
For more information about the data submission requirements we proposed for this measure, we refer readers to the discussion in section VIII.C.8.d. of the preamble of this final rule.
Commenters submitted the following comments related to the proposed rule's discussion of the LTCH QRP quality measure proposals beginning with the FY 2022 LTCH QRP. A discussion of these comments, along with our responses, appears below. We received many comments that addressed both of the Transfer of Health Information measures. Comments that applied to both measures are discussed above in section VIII.C.4.a. of this rule.
Comment: A few commenters urged CMS to use the field's experience with transferring information to patients and reporting on this measure to disseminate best practices about how to best convey the medication list. A commenter suggested this include formats and informational elements helpful to patients and families.
Response: We have interpreted “the field” to mean PAC providers. Facilities and clinicians should use clinical judgement to guide their practices around transferring information to patients and how to best convey the medication list, including identifying the best formats and informational elements. This may be determined by the patient's individualized needs in response to their medical condition. We do not determine clinical best practices standards and facilities are advised to refer to other sources, such as professional guidelines.
Comment: A commenter suggested that the Transfer of Health Information to the Patient measure should assess if the medication list was provided to both the patient and family member, when appropriate.
Response: We agree there are times when it is appropriate for the LTCH to provide the medication list to the patient and family and this decision should be based on clinical judgement. However, because it is not always necessary or appropriate to provide the medication list to both the patient and family, we are not requiring this for the measure.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Transfer of Health Information to the Patient—Post-Acute Care (PAC) measure, pursuant to section 1899B(c)(1)(E) of the Act, beginning with October 1, 2020 discharges.
c. Update to the Discharge to Community—Post Acute Care (PAC) Long-Term Care Hospital (LTCH) Quality Reporting Program (QRP) Measure
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19517), we proposed to update the specifications for the Discharge to Community—PAC LTCH QRP measure to exclude baseline nursing facility (NF) residents from the measure. This measure reports an LTCH's risk-standardized rate of Medicare FFS patients who are discharged to the community following an LTCH stay, do not have an unplanned readmission to an acute care hospital or LTCH in the 31 days following discharge to community, and who remain alive during the 31 days following discharge to community. We adopted this measure in the FY 2017 IPPS/LTCH PPS final rule (81 FR 57207 through 57215).
In the FY 2017 IPPS/LTCH PPS final rule (81 FR 57211), we addressed public comments recommending exclusion of LTCH patients who were baseline NF residents, as these patients lived in a NF prior to their LTCH stay and may not be expected to return to the community following their LTCH stay. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38449), we addressed public comments expressing support for a potential future modification of the measure that would exclude baseline NF residents; commenters stated that the exclusion would result in the measure more accurately portraying quality of care provided by LTCHs, while controlling for factors outside of LTCH control.
We assessed the impact of excluding baseline NF residents from the measure using CY 2015 and CY 2016 data and found that this exclusion impacted both patient- and facility-level discharge to community rates. We defined baseline NF residents as LTCH patients who had a long-term NF stay in the 180 days preceding their hospitalization and LTCH stay, with no intervening community discharge between the NF stay and qualifying hospitalization for measure inclusion. Baseline NF residents represented 9.2 percent of the measure population after all measure exclusions were applied. Observed patient-level discharge to community rates were significantly lower for baseline NF residents (1.44 percent) compared with non-NF residents (23.89 percent). The national observed patient-level discharge to community rate was 21.82 percent when baseline NF residents were included in the measure, increasing to 23.89 percent when they were excluded from the measure. After excluding baseline NF residents, 39.2 percent of LTCHs had an increase in their risk-standardized discharge to community rate that exceeded the increase in the national observed patient-level discharge to community rate.
Based on public comments received and our impact analysis, we proposed to exclude baseline NF residents from the Discharge to Community-PAC LTCH QRP measure beginning with the FY 2020 LTCH QRP, with baseline NF residents defined as LTCH patients who had a long-term NF stay in the 180 days preceding their hospitalization and LTCH stay, with no intervening community discharge between the NF stay and hospitalization.
For additional technical information regarding the Discharge to Community-PAC LTCH QRP measure, including technical information about the proposed exclusion, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We invited public comment on this proposal and received several comments. A discussion of these comments, along with our responses, appears in this final rule.
Comment: All commenters, except MedPAC, supported the proposed exclusion of baseline NF residents from the Discharge to Community—PAC LTCH QRP measure. Supportive commenters referred to their recommendation of this exclusion in prior years and appreciated CMS' willingness to consider and implement stakeholder feedback. A commenter suggested that CMS instead consider other quality measures for NF residents, such as functional status measures, to determine whether residents receive the appropriate standard of care they need in a long-term NF stay. Two commenters requested that claims data be modified to indicate whether a patient is a NF resident so that the measure can be replicated with existing CMS claims data.
Response: We thank the commenters for their support of the proposed exclusion of baseline NF residents from this measure and for their recommendations for future consideration.
Comment: MedPAC did not support the proposed exclusion of baseline NF residents from the Discharge to Community—PAC LTCH QRP measure. They suggested that CMS instead expand their definition of “return to the community” to include baseline nursing home residents returning to the nursing home where they live, as this represents their home or community. MedPAC also stated that providers should be held accountable for the quality of care they provide for as much of their Medicare patient population as feasible.
Response: We agree that providers should be accountable for quality of care for as much of their Medicare population as feasible; we endeavor to do this as much as possible, only specifying exclusions we believe are necessary for measure validity. We also believe that monitoring quality of care and outcomes is important for all PAC patients, including baseline NF residents who return to a NF after their PAC stay. We publicly report several long-stay resident quality measures on Nursing Home Compare including measures of hospitalization and emergency department visits.
Community is traditionally understood as representing non-institutional settings by policy makers, providers, and other stakeholders. Including long-term care NF in the definition of community would confuse this long-standing concept of community and would misalign with CMS' definition of community in patient assessment instruments. CMS conceptualized this measure using the traditional definition of “community” and specified the measure as a discharge to community measure, rather than a discharge to baseline residence measure.
Baseline NF residents represent an inherently different patient population with not only a significantly lower likelihood of discharge to community settings, but also a higher likelihood of post-discharge readmissions and death compared with PAC patients who did not live in a NF at baseline. The inherent differences in patient characteristics and PAC processes and goals of care for baseline NF residents and non-NF residents are significant enough that we do not believe risk adjustment using a NF flag would provide adequate control. While we acknowledge that a return to nursing home for baseline NF residents represents a return to their home, this outcome does not align with our measure concept. Thus, we have chosen to exclude baseline NF residents from the measure.
Comment: A commenter requested that CMS provide the definition of “long-term” NF stay in the proposed measure exclusion.
Response: We have further clarified the definition of long-term NF stay in the final measure specifications, “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html. A long-term NF stay is identified by the presence of a non-SNF PPS MDS assessment in the 180 days preceding the qualifying prior acute care admission and index SNF stay.
After consideration of the public comments we received, we are finalizing our proposal to exclude baseline NF residents from the Discharge to Community—PAC LTCH QRP measure.
5. LTCH QRP Quality Measures, Measure Concepts, and Standardized Patient Assessment Data Elements Under Consideration for Future Years: Request for Information
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19517 through 19518), we sought input on the importance, relevance, appropriateness, and applicability of each of the measures, standardized patient assessment data elements (SPADEs), and concepts under consideration listed in this table for future years in the LTCH QRP.
| Quality Measures and Measure Concepts |
| Functional mobility outcomes. |
| Sepsis. |
| Opioid use and frequency. |
| Exchange of electronic health information and interoperability. |
| Nutritional status. |
| Standardized Patient Assessment Data Elements (SPADEs) |
| Cognitive complexity, such as executive function and memory. |
| Dementia. |
| Bladder and bowel continence including appliance use and episodes of incontinence. |
| Care preferences, advance care directives, and goals of care. |
| Caregiver Status. |
| Veteran Status. |
| Health disparities and risk factors, including education, sex and gender identity, and sexual orientation. |
In the proposed rule (84 FR 19518) we noted that, while we will not be responding to specific comments submitted in response to this Request for Information in this FY 2020 IPPS/LTCH PPS final rule, we intend to use this input to inform our future measure and SPADE development efforts.
We received several comments on this Request for Information, which are summarized below. We appreciate the input provided by commenters.
Comment: Several commenters supported the measures under consideration for future years in the LTCH QRP. A commenter supported the functional mobility outcomes future measure, as it could help to further align quality measurement across post-acute care. Another commenter supported a future sepsis measure. Regarding the proposed opioid use measure concept, a few commenters were concerned with how to best balance the growing risks and consequences of Opioid Use Disorder with the need for ready access to appropriate pain medication. The commenters stated that these measure concepts should not result in unintended consequences that leave patients without access to critical treatments for pain management. For the exchange of electronic health information and interoperability future measure, a few commenters acknowledged the need to share patient information with other health care providers, however, they were concerned that challenges may impede this strategy to reduce burden, such as cost, uneven and slow development, limitations, varying technological proficiency, and difference in standards for meeting interoperability. Several commenters supported the inclusion of a nutritional status measure in the LTCH QRP and recommended that existing inpatient hospital malnutrition focused measures be used in the LTCH setting to identify poor nutritional status and subsequent treatment to improve outcomes for patients. A commenter also requested the addition of a standardized patient experience survey to the LTCH QRP. In addition, a commenter recommended the inclusion of quality measures to ensure high quality care for those with mental and/or substance use disorders.
Regarding the SPADEs under consideration for future years in the LTCH QRP, a commenter supported cognitive complexity, dementia, health disparities and risk factors and suggested these are also relevant data elements for ambulatory and acute care settings. Some commenters requested more information on the future SPADEs. A commenter supported the dementia SPADE, as cognitive impairment can affect a beneficiary's ability to participate in his or her care in PAC settings, in addition to managing co-occurring chronic conditions and medications after discharge. A commenter supported the collection of the bowel and bladder incontinence SPADE and another commenter agreed with the future inclusion of the care preference SPADE, because advance directives and caregivers are important in effective discharge planning and facilitates transfers between levels of care. However, a few commenters believed that given their severity and conditions, many LTCH patients are unable to plan their future care with health professionals and must rely on a surrogate decision maker. A commenter supported the caregiver status SPADE because these individuals are more likely to communicate with health professionals, coordinate care, and help manage emotional and behavioral health issues. A commenter described a future desired list of social risk variables in response to the health disparities and risk factors SPADE, including literacy, marital status, live-in home support, family support structure, and home health resources.
6. Standardized Patient Assessment Data Reporting Beginning With the FY 2022 LTCH QRP
Section 1886(m)(5)(F)(ii) of the Act requires that, for fiscal year 2019 and each subsequent year, LTCHs must report standardized patient assessment data, required under section 1899B(b)(1) of the Act. Section 1899B(a)(1)(C) of the Act requires, in part, the Secretary to modify the PAC assessment instruments in order for PAC providers, including LTCHs, to submit SPADEs under the Medicare program. Section 1899B(b)(1)(A) of the Act requires PAC providers to submit SPADEs under applicable reporting provisions (which, for LTCHs, is the LTCH QRP) with respect to the admission and discharge of an individual (and more frequently as the Secretary deems appropriate), and section 1899B(b)(1)(B) of the Act defines standardized patient assessment data as data required for at least the quality measures described in section 1899B(c)(1) of the Act and that is with respect to the following categories: (1) Functional status, such as mobility and self-care at admission to a PAC provider and before discharge from a PAC provider; (2) cognitive function, such as ability to express ideas and to understand, and mental status, such as depression and dementia; (3) special services, treatments, and interventions, such as need for ventilator use, dialysis, chemotherapy, central line placement, and total parenteral nutrition; (4) medical conditions and comorbidities, such as diabetes, congestive heart failure, and pressure ulcers; (5) impairments, such as incontinence and an impaired ability to hear, see, or swallow; and (6) other categories deemed necessary and appropriate by the Secretary.
In the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20100 through 20116), we proposed to adopt SPADEs that would satisfy the first five categories. In the FY 2018 IPPS/LTCH PPS final rule, commenters expressed support for our adoption of SPADEs in general, including support for our broader standardization goal and support for the clinical usefulness of specific proposed SPADEs. However, we did not finalize the majority of our SPADE proposals in recognition of the concern raised by many commenters that we were moving too fast to adopt the SPADEs and modify our assessment instruments in light of all of the other requirements we were also adopting under the IMPACT Act at that time (82 FR 38457 through 38458). In addition, we noted our intention to conduct extensive testing to ensure that the standardized patient assessment data elements we select are reliable, valid, and appropriate for their intended use (82 FR 38451 through 38452).
We did, however, finalize the adoption of SPADEs for two of the categories described in section 1899B(b)(1)(B) of the Act: (1) Functional status: Data elements currently reported by LTCHs to calculate the measure Application of Percent of Long-Term Care Hospital Patients with an Admission and Discharge Functional Assessment and a Care Plan That Addresses Function (NQF #2631); and (2) Medical conditions and comorbidities: the data elements used to calculate the pressure ulcer measures, Percent of Residents or Patients with Pressure Ulcers That Are New or Worsened (Short Stay) (NQF #0678) and the replacement measure, Changes in Skin Integrity Post-Acute Care: Pressure Ulcer/Injury. We stated that these data elements were important for care planning, known to be valid and reliable, and already being reported by LTCHs for the calculation of quality measures (82 FR 38453 through 38454).
Since we issued the FY 2018 IPPS/LTCH PPS final rule, LTCHs have had an opportunity to familiarize themselves with other new reporting requirements that we have adopted under the IMPACT Act. We have also conducted further testing of the SPADEs, as described more fully in this final rule, and believe this testing supports the use of the SPADEs in our PAC assessment instruments. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19518 through 19552), we proposed to adopt many of the same SPADEs that we previously proposed to adopt, along with other SPADEs.
In that proposed rule, we proposed that LTCHs would be required to report these SPADEs beginning with the FY 2022 LTCH QRP. If finalized as proposed, LTCHs would be required to report these data with respect to LTCH admissions and discharges that occur between October 1, 2020 and December 31, 2020 for the FY 2022 LTCH QRP. Beginning with the FY 2023 LTCH QRP, we proposed that LTCHs must report data with respect to admissions and discharges that occur during the subsequent calendar year (for example, CY 2021 for the FY 2023 LTCH QRP, CY 2022 for the FY 2024 LTCH QRP).
We also proposed that LTCHs that submit the Hearing, Vision, Race, and Ethnicity SPADEs with respect to admission will be deemed to have submitted those SPADEs with respect to both admission and discharge, because it is unlikely that the assessment of those SPADEs at admission will differ from the assessment of the same SPADEs at discharge.
In selecting the SPADEs in this final rule, we considered the burden of assessment-based data collection and aimed to minimize additional burden by evaluating whether any data that is currently collected through one or more PAC assessment instruments could be collected as SPADEs. In selecting the SPADEs in this final rule, we also took into consideration the following factors with respect to each data element:
(1) Overall clinical relevance;
(2) Interoperable exchange to facilitate care coordination during transitions in care;
(3) Ability to capture medical complexity and risk factors that can inform both payment and quality; and
(4) Scientific reliability and validity, general consensus agreement for its usability.
In identifying the SPADEs proposed in this final rule, we also drew on input from several sources, including TEPs held by our data element contractor, public input, and the results of a recent National Beta Test of candidate data elements conducted by our data element contractor (hereafter “National Beta Test”).
The National Beta Test collected data from 3,121 patients and residents across 143 PAC facilities (26 LTCHs, 60 SNFs, 22 IRFs, and 35 HHAs) from November 2017 to August 2018 to evaluate the feasibility, reliability, and validity of the candidate data elements across PAC settings. The 3,121 patients and residents with an admission assessment included 507 in LTCHs, 1,167 in SNFs, 794 in IRFs, and 653 in HHAs. The National Beta Test also gathered feedback on the candidate data elements from staff who administered the test protocol in order to understand usability and workflow of the candidate data elements. More information on the methods, analysis plan, and results for the National Beta Test are available in the document titled, “Development and Evaluation of Candidate Standardized Patient Assessment Data Elements: Findings from the National Beta Test (Volume 2),” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Further, to inform the proposed SPADEs, we took into account feedback from stakeholders, as well as from technical and clinical experts, including feedback on whether the candidate data elements would support the factors previously described. Where relevant, we also took into account the results of the Post-Acute Care Payment Reform Demonstration (PAC PRD) that took place from 2006 to 2012.
Comment: Some commenters supported the goals of standardization as well as the SPADEs proposed in this rule. A commenter recognized that data standardization will help facilitate appropriate payment reforms and appropriate quality measures.
Response: We thank the commenters for their support of the goals of standardization and of the proposed SPADEs. We selected the proposed SPADEs in part because of the attributes that the commenters noted.
Comment: A commenter noted strong support for the goals of the IMPACT Act and for CMS' goals of ensuring that patient assessment practices support effective care plans and transitions, but expressed concern about the scope and timing of proposed changes, including the SPADEs.
Response: We thank the commenter for the support for the goals of the IMPACT Act and appreciate the concern about the proposed changes. Since we issued the FY 2018 IPPS/LTCH PPS final rule (82 FR 37990 through 38589), LTCHs have had an opportunity to familiarize themselves with other new reporting requirements that we have adopted under the IMPACT Act and prepare for additional changes. We have provided regular updates to stakeholders and gathered feedback through Special Open Door Forums and other events as described in our proposal. We intend to monitor and evaluate SPADEs as they are submitted, and to continue to engage stakeholders around ways the SPADEs could be best used in the PAC quality programs. We will continue to communicate and collaborate with stakeholders by soliciting input on use of the SPADEs in the LTCH QRP through future rulemaking.
Comment: Some commenters stated support but noted reservations. A commenter described the SPADEs as an appropriate start, but noted that the SPADEs cannot stand alone, and must be built upon to be useful for risk adjustment and quality measurement. Similarly, another commenter suggested CMS continue working with clinicians and researchers to ensure that the SPADEs are collecting valid, reliable, and useful data, and to continue to refine and explore new data elements for standardization.
Response: We agree with the commenter's statement that the SPADEs are an appropriate start for standardization, but we disagree that they cannot stand alone. While we intend to evaluate the SPADEs as they are submitted and explore additional opportunities for standardization, we also believe that the SPADEs as proposed represent an important core set of information about clinical status and patient characteristics and they will be useful for quality measurement. We welcome continued input, recommendations, and feedback from stakeholders about ways to improve assessment and quality measurement for PAC providers including ways that the SPADEs could be used in the LTCH QRP. Input can be shared with CMS through our PAC Quality Initiatives email address: PACQualityInitiative@cms.hhs.gov.
Comment: A commenter suggested CMS consider ways to incentivize PAC providers to adopt health information technology to support these efforts to standardize patient data. This commenter noted that the transfer of data to and from PAC settings often occurs via cumbersome, resource-intensive manual processes and that common data reporting processes alone will not achieve interoperability goals.
Response: We appreciate the commenter's recommendation. It is our intention to use the SPADE data to inform the common standards and definitions to facilitate interoperable exchange of data. We believe that a core, standardized set of data elements that could be shared across PAC and other provider types is an important first step to foster this interoperability between providers. We are hopeful that by requiring the collection of standardized data, the SPADEs may spur providers to adopt health information technology that eases the burden associated with data collection and data exchange. Further, we believe that the collection of these SPADEs reflect common clinical practice and will improve discharge planning and errors that occur during transition from one setting to the next. While the collection of the SPADEs is one of many tasks to supporting interoperability, and will take into consideration how best to decrease burden from data collection including our manual processes. CMS will take into consideration ways to help incentivize providers to adopt health information technology.
Comment: A commenter questioned which clinical specialties (for example, RN, PT, OT, Psychologist) would be responsible for collecting the proposed SPADEs, and recommended that CMS clarify the member of the healthcare team they anticipate collecting the information, if CMS has specific expectations.
Response: We do not require that a certain type of clinician complete assessments; the SPADEs have been developed so that any clinician who is trained in the administration of the assessment will be able to administer it correctly.
Comment: A commenter expressed concerns about the level of evidence to support the SPADEs shared by CMS from the National Beta Test. These include the lack of representativeness of LTCHs included in the sample, the reported exclusion of patients with communication and cognitive impairments, as well as the exclusion of non-English speaking patients. The commenter described how these concerns compromise their confidence in the findings of the National Beta Test.
Response: In a supplementary document to the proposed rule (the document titled “Proposed Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html), we described key findings from the National Beta Test related to the proposed SPADEs. We also referred readers to an initial volume of the National Beta Test report that details the methodology of the field test (“Development and Evaluation of Candidate Standardized Patient Assessment Data Elements: Findings from the National Beta Test (Volume 2),” available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html). Additional volumes of the National Beta Test report will be available in late 2019. These volumes contain supplementary analyses of the SPADEs that may be of interest to stakeholders.
To address the commenter's specific concerns about the lack of representativeness of LTCHs included in the National Beta Test, we note that the National Beta Test was designed to generate valid and robust national SPADE performance estimates for each of the four PAC provider types. This required acceptable geographic diversity, sufficient sample size, and reasonable coverage of the range of clinical characteristics. To meet these requirements, the National Beta Test was carefully designed so that data could be collected from a wide range of environments (such as geographic regions, and PAC providers of different types, sizes, and ownership), allowing for thorough evaluation of candidate SPADE performance in all PAC settings. The approach included a stratified random sample, to maximize generalizability, and subsequent analyses included extensive checks on the sampling design. We contend that performance of the SPADEs in LTCHs in the National Beta Test is generalizable, given the study design and range of LTCHs that were included. LTCH assessments in the National Beta Test were collected from 25 LTCHs in the 14 geographic markets in which the field test was conducted, and included for profit and non-profit facilities in metropolitan and micropolitan areas, ranging in size from 31 to 675 beds.
The National Beta Test did not exclude non-communicative patients/residents; rather, it had two distinct samples, one of which focused on patients/residents who were able to communicate, and one of which focused on patient/residents who were not able to communicate. The assessment of non-communicative patients/residents differed primarily in that observational assessments were substituted for some interview assessments. Non-English-speaking patients were excluded from the National Beta Test due to feasibility constraints during the field test. Including limited English proficiency patients/residents in the sample would have required the Beta test facilities to engage or involve translators during the test assessments. We anticipated that this would have added undue complexity to what facilities/agencies were being asked to do, and would have undermined the ability of facility/agency staff to complete the requested number of assessments during the study period. Moreover, there is strong existing evidence for the feasibility of all clinical patient/resident interview SPADEs included in this proposed rule (BIMS [section VIII.C.7.b in this final rule], Pain Interference [section VIII.C.7.d in this final rule], PHQ [section VIII.C.7.b in this final rule]) when administered in other languages, either through standard PAC workflow as tested and currently collected in the MDS 3.0 or through rigorous translation and testing such as the PHQ. For all these reasons, we determined that the performance of translated versions of these patient/resident interview SPADEs did not need to be further evaluated. In addition, because their exclusion did not threaten our ability to achieve acceptable geographic diversity, sufficient sample size, and reasonable coverage of the range of PAC patient/resident clinical characteristics, the exclusion of limited English proficiency patients/residents was not considered a limitation to interpretation of the National Beta Test results.
Comment: A commenter also remarked on the lack of information about clinical characteristics that has been shared with stakeholders, limiting their ability to draw conclusions about the data, and requested that CMS release the data from the National Beta Test to be analyzed by third parties.
Response: We shared both quantitative and qualitative findings from the National Beta Test with stakeholders at a public meeting on November 27, 2018. For each SPADE proposed in this rule within the clinical categories in the IMPACT Act, we provided information in the supplementary documents to the proposed rule (the document titled “Proposed Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html) on the feasibility and reliability based on findings from the National Beta Test.
We are in the process of writing the final report for the National Beta Test, which includes the clinical SPADEs in this rule as well as additional data elements. Volume 2 of that report (“Development and Evaluation of Candidate Standardized Patient Assessment Data Elements. Findings from the National Beta Test (Volume 2)”) was posted on CMS' website in March 2019 (available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html). The other volumes will be available in late 2019. In addition, we are committed to making data available for researchers and the public to analyze in a way that protects the privacy of patients and providers who participated in the National Beta Test. We are in the process of creating research identifiable files that we anticipate will be available through a data use agreement sometime in 2019.
Comment: Several commenters expressed concerns with respect to the scope of the standardized patient assessment data proposals. These commenters were concerned that the proposed standardized patient assessment data reporting requirements will impose significant burden on providers, given the volume of new standardized patient assessment data elements that were proposed to be simultaneously added to the LCDS within a short timeframe. Commenters calculated the addition of the proposed SPADEs to increase the time spent completing the LCDS by 37 percent and called on CMS to offset the expansion of the LCDS with removal of other data elements or requirements. A commenter remarked on the significant additional staff time that collecting and reporting the SPADEs would entail, and noted that even with electronic medical records in place, significant time and resources are spent on developing linkages and reporting systems between the EMR and CMS' systems.
Response: We acknowledge the additional burden that the SPADEs will impose on providers and patients. Our development and selection process for the SPADEs prioritized data elements essential to comprehensive patient care. We maintain that there will be significant benefit associated with each of the SPADEs to providers and patients, in that they are clinically useful (for example, for care planning), they support patient-centered care, and they will promote interoperability and data exchange between providers. During the SPADE development process, we were cognizant of the changes that providers will need to make to implement these additions to the LCDS. In FY 2018 IPPS/LTCH PPS final rule (82 FR 38451 through 38452), we provided information about goals, scope, and timeline for implementing SPADEs, as well as updated LTCHs about ongoing development and testing of data elements through other public forums. We believe that LTCHs have had an opportunity to familiarize themselves with other new reporting requirements that we have adopted under the IMPACT Act and prepare for additional changes.
Comment: Several commenters expressed concern that this additional burden was not justified because, in their view, there was limited or no evidence for the SPADEs to improve patient care. A commenter noted that there is no minimum number of data elements that must be collected to satisfy the IMPACT Act, and expressed concerns about the relevance of cross-setting assessments and measures, given the differences in the patient populations that they serve (for example, highest-complexity patients in LTCHs). Other commenters stated that proposal of the SPADEs was inconsistent with the Meaningful Measures initiative and the principle to consider whether the costs of a measure outweigh its benefit.
Response: The clinical SPADEs proposed in this rule are the result of an extensive consensus vetting process in which experts and stakeholders were engaged through TEPs, Special Open Door Forums, and posting of interim reports and other documents on the CMS website. Results of these activities provide evidence that experts and providers believe the proposed SPADEs have the potential for measuring quality, describing case mix, and improving care. We refer the commenter to the most recent TEP report: A summary of the most recent TEP meeting (September 17, 2018) titled “SPADE Technical Expert Panel Summary (Third Convening)”, which is available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html. Therefore, we have provided evidence that the SPADEs have the potential for improving quality and utility for describing case mix.
With regard to the consistency of our proposal with the larger Meaningful Measures framework, the proposed SPADEs correspond to several Meaningful Measures Areas. Specifically, the SPADEs will enable transfer of health information and interoperability; support prevention, treatment, and management of mental health; collect data that will support measurement of patient reported functional outcomes; as well as contribute to other Meaningful Measures Areas. We also note Meaningful Measures' priority of focusing health care quality efforts on what matters most to patients, including quality of care, care preferences, and overall experience. Developing appropriate and useful measures of quality of care that empower patients to make choices about their healthcare are only possible with a robust and valid set of data elements, such as the SPADEs.
Comment: Some commenters noted that many of the proposed SPADEs occur too infrequently among LTCH patients to be useful, and that many of the proposed SPADEs will not be applicable or not able to be completed for LTCH patients.
Response: We appreciate the commenters' concern that clinical treatments or response categories documented by some SPADEs are uncommon overall, and/or unlikely in the LTCH setting. We understand that not all SPADEs will be equally relevant to all patients and/or PAC providers. However, we assert that even relatively rare treatments or clinical situations, such as patient undergoing chemotherapy while receiving PAC services, or a having a feeding tube, are important to document, both for care planning within the setting and for transfer of information to the next setting of care. We note that the assessment of many of the less frequently occurring treatments and conditions is formatted as a “check all that apply” list, which minimizes burden. When treatments do not apply the assessor need only check one row for “None of the Above.” Additionally, skip patterns in the assessment tool exempt patients who are unable to communicate from patient interview items (for example, BIMS, PHQ-2 to 9).
Comment: Some commenters stated that the time burden (as in, “time-to-complete”) associated with the clinical SPADEs was underestimated. A commenter stated that because testing conditions focused on cognitively intact, English-speaking patients with no speech or language deficits, the estimates of impact to providers' time and resources is inadequate. Another commenter noted that based on experience of their own LTCHs who participated in the National Beta Test, it took approximately 30 minutes to complete the assessment for patients who were alert and oriented but took over an hour to complete for others who required constant re-directing. Other commenters believe that CMS overlooked the additional staff time necessary for reviewing, auditing, and transmitting the SPADEs to CMS; training clinical staff; or working with EHR vendors, and therefore, underestimated burden. This commenter suggested CMS revise the estimated burden for the proposed SPADEs.
Response: We wish to clarify that time-to-complete estimates from the National Beta Test included the time spent both to collect data, including the review of the medical record, if needed, and to enter the data elements into a tablet. We note that time-to-complete estimates were calculated using the data from Facility/Agency Staff only, and not Research Nurses, who completed more training and conducted more assessments overall than the Facility/Agency staff.
We also wish to clarify that National Beta Test did exclude patients/residents who were not able to communicate in English, but did not categorically exclude patients with cognitive impairment or patients with speech or language deficits. Therefore, we believe that our estimates of time-to-complete capture the general population of LTCH patients, including those with communication impairments.
Comment: To reduce administrative burden, several commenters recommended changes to when and how SPADEs would be collected. These recommendations included collecting data only at admission when answers are unlikely to change between admission and discharge, reducing the speed and scope of SPADE implementation, adopting a staged implementation or only a subset of the proposed data elements that demonstrate high utility and reliability in the LTCH setting, and that CMS explore options for obtaining these data via claims or voluntary reporting only.
Response: We appreciate the commenters' recommendations. To support data exchange between settings, and to support quality measurement, section 1899B(b)(1)(A) of the Act requires that the SPADEs be collected with respect to both admission and discharge. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19518), we proposed that LTCHs that submit four SPADEs with respect to admission will be deemed to have submitted those SPADEs with respect to both admission and discharge because we asserted that it is unlikely that the assessment of those SPADEs at admission would differ from the assessment of the same SPADEs at discharge. We note that a patient's ability to hear or ability to see is more likely to change between admission and discharge than, for example, a patient's self-report of his or her race, ethnicity, preferred language, or need for interpreter services. The Hearing and Vision SPADEs are also different from the other SPADEs (that is, Race, Ethnicity, Preferred Language, and Interpreter Services) because evaluation of sensory status is a fundamental part of the ongoing nursing assessment conducted for LTCH patients. Therefore, clinically significant changes that occur in a patient's hearing or vision status during the LTCH stay would be captured as part of the clinical record and communicated to the next setting of care, as well as taken into account during discharge planning as a part of standard best practice. As discussed in section VIII.C.7.e., section VIII.C.7.f.(2)(a) and section VIII.C.7.f.(2)(b), we are finalizing our policy to deem LTCHs that submit the Hearing, Vision, Race, Ethnicity, Preferred Language, and Interpreter Services SPADEs with respect to admission to have submitted with respect to both admission and discharge.
Regarding the speed and scope of SPADE implementation, and the commenter's recommendation to adopt a staged approach to implementation, we note that since we issued the FY 2018 IPPS/LTCH PPS final rule (82 FR 38451 through 38452), LTCHs have had an opportunity to familiarize themselves with other new reporting requirements that we have adopted under the IMPACT Act and prepare for additional changes. We have provided regular updates to stakeholders and gathered feedback through Special Open Door Forums and other events as described in our proposal. We note that these items span many substantive clinical areas and patient characteristics, and are comprised of a mix of patient interview and non-interview assessments. We contend that we have been highly selective when identifying SPADEs, and that our selections reflect a balanced approach to assessor and patient burden versus the need for assessment data to support care planning, foster interoperability, and inform future quality measures.
Regarding the commenter's recommendation to adopt only a subset of the proposed data elements that demonstrate high utility and reliability in the LTCH setting, we note that part of our process in evaluating candidate SPADEs was clinical relevance to all PAC provider types. We recognize that not all SPADEs will be equally salient to all PAC providers, but we selected clinical topics and a level of detail for the SPADEs that is important to patient care regardless of their care setting. We will take into consideration the recommendation to obtain patient data from claims data in future work.
Comment: Some commenters encouraged CMS to create and make transparent a data use strategy and analysis plan for the SPADEs so PAC providers, including LTCHs, better understand how the agency will further assess the adequacy and usability of the SPADEs to support changes to payment and quality programs. A commenter stated that additional evaluation of SPADEs and their intended uses is needed prior to nationwide implementation and adoption. Another commenter noted appreciation for CMS' efforts to provide opportunities for stakeholder communication and input, but also recommended CMS develop additional lines of communication with stakeholders, such as a multi-disciplinary stakeholder workgroup representing all PAC settings to advise on strategic and operational implications of implementation and a data analytics advisory group to assist CMS in establishing a framework for SPADE analysis and ongoing assessment.
Response: We appreciate the commenter's recommendations. It is our intention, as delineated by the IMPACT Act, to use the SPADE data to inform care planning, the common standards and definitions to facilitate interoperability, and to allow for comparing assessment data for standardized measures. In order to maintain open lines of communication with our stakeholders, we have used the public comment periods, TEPs, Subject Matter Expert working groups, stakeholder meetings, data forums, Medicare Learning Network (MLN) events, open door forums, help desks, in-person trainings, webinars with communication with the public, “We Want to Hear From You” sessions, and have had stakeholders serve as consultants on our measure work. If there are any other opportunities for communication and comment, we will publish those opportunities. We will continue to communicate with stakeholders about how the SPADEs will be used in quality programs, as those plans are established, by soliciting input during the development process and establishing use of the SPADEs in quality programs through future rulemaking.
Comment: A commenter noted complexity and coding nuance related to the proposed SPADEs, stating that the SPADEs introduce a variety of different look-back periods (that is, 2 days, 3 days, 5 days, 7 days, and 2 weeks). The commenter implied that this could harm the quality of the data. The commenter went on to emphasize the importance of valid and reliable data collection, which they stated relies on CMS developing and making available all the necessary education and training for providers.
Response: We agree that correct and consistent data collection practices are essential to accurate data. We wish to clarify that although multiple time frames were associated with individual data elements in the National Beta Test, this was for testing purposes only; a component of the National Beta Test was designed to investigate the stability of patients' responses and patterns of initiation and discontinuation of treatments at admission and discharge, respectively. Each proposed SPADE for the LCDS had only one time frame associated with it, although we acknowledge that several SPADEs have different reference time periods. For example, the PHQ-2 to 9 asks about depressive symptoms in the last 2 weeks, because that time frame is consistent with the diagnostic criteria for depression. The pain interference interview asks about the last 5 days. The 5-day reference period was chosen to conform with similar data elements currently in use in the MDS 3.0 for SNFs, and because, when compared to a 3-day reference period in the National Beta Test, we found minimal differences. With regard to educational materials for assessors, we intend to provide comprehensive training materials for providers and ongoing support through our in-person and web-based trainings, guidance manuals, and website.
7. Standardized Patient Assessment Data by Category
a. Functional Status Data
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19519), we proposed to adopt six functional status data elements as SPADEs under the category of functional status under section 1899B(b)(1)(B)(i) of the Act. These six data elements are: Car transfer; Walking 10 feet on uneven surfaces; 1-step (curb); 4 steps; 12 steps; and Picking up object. We proposed to add these to the LCDS as SPADEs under section 1899B(b)(1)(B)(i) of the Act. We adopted these six mobility data elements into the SNF, IRF, and HH QRPs as SPADEs under their respective patient/resident assessment instruments.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38429 through 38430), we finalized our definition of “standardized patient assessment data” as patient assessment questions and response options that are identical in all four PAC assessment instruments, and to which identical standards and definitions apply. In order for these six mobility data elements to be in all four PAC assessment instruments, we proposed that they also meet the definition of standardized patient assessment data for functional status under section 1899B(b)(1)(B)(i) of the Act, and that the successful reporting of such data under section 1886(m)(5)(F)(i) of the Act will also satisfy the requirement to report standardized patient assessment data under section 1886(m)(5)(F)(ii) of the Act.
The data elements previously listed were implemented in the IRF QRP and SNF QRP when we adopted the quality measures, Change in Mobility Score (NQF #2634) and Discharge Mobility Score (NQF #2636), into the IRF QRP in the FY 2016 IRF PPS final rule (80 FR 47111 through 47120) and the SNF QRP in the FY 2018 SNF PPS final rule (82 FR 36577 through 36593). In addition, we implemented these six mobility data elements in the HH setting. The CY 2018 HH PPS final rule (82 FR 51733 through 51734) finalized that these six mobility data elements meet the definition of standardized patient assessment data for functional status under section 1899B(b)(1)(B)(i) of the Act.
The six mobility data elements are currently collected in Section GG: Functional Abilities and Goals located in the current versions of the MDS, OASIS, and the IRF-PAI assessment instruments. For more information on the six functional mobility data elements, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We proposed to adopt the functional mobility data elements as SPADEs for use in the LTCH QRP.
Comment: A commenter supported the adoption of the six proposed functional mobility data elements to the LTCH CARE Data Set as SPADEs for use in the LTCH QRP.
Response: We appreciate the commenter's support.
Comment: Several commenters were concerned about the addition of the six functional mobility data elements. The commenters stated that LTCHs admit high-acuity patients, and that these data elements are relevant for only a small proportion of LTCH patients. They also stated that CMS has not demonstrated the value of adding these data elements. Therefore, they do not believe the addition of these six data elements will provide useful information and the addition of these data elements would be burdensome.
Response: We appreciate commenters' concerns about the burden associated with the six mobility data elements being added to the LTCH CARE Data Set. We recognize that any new data collection is associated with burden and take such concerns under consideration when selecting new data elements. To reduce the burden associated with collecting the functional mobility data, we have included skip patterns in Section GG to reduce the number of data elements that may need to be completed for any one LTCH patient. For example, if a patient cannot perform the activity of going up one step (or a curb) there is a skip pattern that allows the clinician to skip the 4 steps and 12 steps data elements. The inclusion of skip patterns means that only a subset of mobility data are needed for most LTCH patients. We also recognize that LTCH patients are critically ill and understand that “activity not attempted” codes may be used for higher-ability mobility data elements on admission for many patients. We note that for patients discharged to home (26 percent of LTCH patients in calendar year 2018) these mobility activities are relevant and useful for discharge planning.
After consideration of the public comments we received, we are finalizing the six functional mobility data elements as SPADEs for use in the LTCH QRP as proposed.
b. Cognitive Function and Mental Status Data
A number of underlying conditions, including dementia, stroke, traumatic brain injury, side effects of medication, metabolic and/or endocrine imbalances, delirium, and depression, can affect cognitive function and mental status in PAC patient and resident populations.[791] The assessment of cognitive function and mental status by PAC providers is important because of the high percentage of patients and residents with these conditions,[792] and because these assessments provide opportunity for improving quality of care.
Symptoms of dementia may improve with pharmacotherapy, occupational therapy, or physical activity,[793 794 795] and promising treatments for severe traumatic brain injury are currently being tested.[796] For older patients and residents diagnosed with depression, treatment options to reduce symptoms and improve quality of life include antidepressant medication and psychotherapy,[797 798 799 800] and targeted services, such as therapeutic recreation, exercise, and restorative nursing, to increase opportunities for psychosocial interaction.[801]
In alignment with our Meaningful Measures Initiative, accurate assessment of cognitive function and mental status of patients and residents in PAC is expected to make care safer by reducing harm caused in the delivery of care; promote effective prevention and treatment of chronic disease; strengthen person and family engagement as partners in their care; and promote effective communication and coordination of care. For example, standardized assessment of cognitive function and mental status of patients and residents in PAC will support establishing a baseline for identifying changes in cognitive function and mental status (for example, delirium), anticipating the patient's or resident's ability to understand and participate in treatments during a PAC stay, ensuring patient and resident safety (for example, risk of falls), and identifying appropriate support needs at the time of discharge or transfer. SPADEs will enable or support clinical decision-making and early clinical intervention; person-centered, high quality care through facilitating better care continuity and coordination; better data exchange and interoperability between settings; and longitudinal outcome analysis. Therefore, reliable SPADEs assessing cognitive function and mental status are needed in order to initiate a management program that can optimize a patient's or resident's prognosis and reduce the possibility of adverse events. We describe each of the proposed cognitive function and mental status data SPADEs in this final rule.
Comment: A few commenters were supportive of the proposal to adopt the BIMS, CAM, and PHQ-2 to 9 as SPADEs on the topic of cognitive function and mental status. A commenter agreed that standardizing cognitive assessments will allow providers to identify changes in status, support clinical decision-making, and improve care continuity and interventions.
Response: We thank the commenters for the support and feedback. We selected the Cognitive Function and Mental Status data elements for proposal as standardized data in part because of the attributes that the commenters noted.
Comment: A few commenters noted limitations of these SPADEs to fully assess all areas of cognition and mental status, particularly mild to moderate cognitive impairment, and performance deficits that may be related to cognitive impairment. A few commenters recommended CMS continue exploring assessment tools on the topic of cognition and to include a more comprehensive assessment of cognitive function for use in PAC settings, noting that highly vulnerable patients with a mild cognitive impairment cannot be readily identified through the current SPADEs.
Response: We have strived to balance the scope and level of detail of the data elements against the potential burden placed on patients and providers. In our past work, we evaluated the potential of several different cognition assessments for use as standardized data elements in PAC settings. We ultimately decided on the BIMS, CAM, and PHQ-2 to 9 data elements as a starting point. We would welcome continued input, recommendations, and feedback from stakeholders about additional data elements for standardization. Input can be shared with CMS through our PAC Quality Initiatives email address: PACQualityInitiative@cms.hhs.gov.
Comment: Regarding future use of these data elements, a commenter recommended that CMS monitor the use of the cognition and mental status SPADEs as risk adjustors and make appropriate adjustments to methodology as needed.
Response: We appreciate the commenter's recommendations. It is our intention, as delineated by the IMPACT Act, to use the cognition and mental status SPADEs to inform care planning, the common standards and definitions to facilitate interoperability, and to allow for comparing assessment data for standardized measures. We will continue to communicate with stakeholders about how the SPADEs will be used in quality programs, as those plans are established, by soliciting input during the development process and establishing use of the SPADEs through future rulemaking.
Comment: A commenter recommended that CMS be cautious in their interpretation of SPADEs related to cognitive function and mood, out of consideration of the recent past experience of critically ill patients (for example, ICU stay, sedation, mechanical ventilation). The commenter described how cognitive impairment is nearly universal in LTCH patients who have been discharged from the ICU, and that depression screening may function differently in this population, given the level of somatic complaints related to patients' physical illness.
Response: We appreciate the commenter's recommendation. We intend to monitor and conduct further analyses on the data submitted via the SPADEs to better understand the performance of the data elements among different populations and to determine the suitability of the data elements for other uses (for example, risk adjustment, payment). Notwithstanding the differences in how some patient types may respond to individual data elements, we believe that the SPADEs have immediate value for providers as they inform care planning and care transitions.
• Brief Interview for Mental Status (BIMS)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19520 through 19521), we proposed that the data elements that comprise the BIMS meet the definition of standardized patient assessment data with respect to cognitive function and mental status under section 1899B(b)(1)(B)(ii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20100 through 20101), dementia and cognitive impairment are associated with long-term functional dependence and, consequently, poor quality of life and increased health care costs and mortality.[802] This makes assessment of mental status and early detection of cognitive decline or impairment critical in the PAC setting. The intensity of routine nursing care is higher for patients and residents with cognitive impairment than those without, and dementia is a significant variable in predicting readmission after discharge to the community from PAC providers.[803]
The BIMS is a performance-based cognitive assessment screening tool that assesses repetition, recall with and without prompting, and temporal orientation. The data elements that make up the BIMS are seven questions on the repetition of three words, temporal orientation, and recall that result in a cognitive function score. The BIMS was developed to be a brief, objective screening tool, with a focus on learning and memory. As a brief screener, the BIMS was not designed to diagnose dementia or cognitive impairment, but rather to be a relatively quick and easy to score assessment that could identify cognitively impaired patients as well as those who may be at risk for cognitive decline and require further assessment. It is currently in use in two of the PAC assessments: The MDS used by SNFs and the IRF-PAI used by IRFs. For more information on the BIMS, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The data elements that comprise the BIMS were first proposed as SPADEs in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20100 through 20101). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 expressed support for use of the BIMS, noting that it is reliable, feasible to use across settings, and will provide useful information about patients and residents. We also stated that those commenters had noted that the data collected through the BIMS will provide a clearer picture of patient or resident complexity, help with the care planning process, and be useful during care transitions and when coordinating across providers. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the BIMS, with several commenters noting the importance of routine assessment of cognitive status and supporting the use of the BIMS to identify individuals with cognitive impairment. However, commenters expressed concerns about not having recent, comprehensive field testing of the proposed data elements. In addition, some commenters were critical of the BIMS, citing burden of administering the items and its limitation in assessing mild cognitive impairment and “functional” cognition related to executive function and everyday decision-making.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the BIMS was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the BIMS to be feasible and reliable for use with PAC patients and residents. More information about the performance of the BIMS in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In, addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the proposed standardized patient assessment data elements, and the TEP supported the assessment of patient or resident cognitive status at both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our on-going SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. Some commenters expressed concern that the BIMS, if used alone, may not be sensitive enough to capture the range of cognitive impairments, including mild cognitive impairment. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We understand the concerns raised by stakeholders that BIMS, if used alone, may not be sensitive enough to capture the range of cognitive impairments, including functional cognition and MCI, but note that the purpose of the BIMS data elements as SPADEs is to screen for cognitive impairment in a broad population. We also acknowledge that further cognitive tests may be required based on a patient's condition and will take this feedback into consideration in the development of future standardized patient assessment data elements. However, taking together the importance of assessing for cognitive status, stakeholder input, and strong test results, we proposed that the BIMS data elements meet the definition of standardized patient assessment data with respect to cognitive function and mental status under section 1899B(b)(1)(B)(ii) of the Act, and to adopt the BIMS as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters support the use of the BIMS to assess cognitive function and mental status. A commenter was specifically supportive of the collection of BIMS at both admission and discharge and believes it will result in more complete data and better care. Another commenter appreciated that the BIMS results in a score, which improves the usability of the assessment.
Response: We thank the commenters for their support of the BIMS data element.
Comment: Several commenters stated that the BIMS fails to detect mild cognitive impairment or functional cognition, differentiate cognitive impairment from a language impairment, link impairment to functional limitation, or identify issues with problem solving and executive function. A commenter recommended use of the Development of Outpatient Therapy Payment Alternatives (DOTPA) items for PAC as well as a screener targeting functional cognition.
Response: We recognize that the BIMS assesses components of cognition and does not, alone, provide a comprehensive assessment of potential cognitive impairment. We would like to clarify that any SPADE or set of data elements is intended as a minimum assessment and would not limit the ability of providers to conduct a more comprehensive assessment of cognition to identify the complexities or potential impacts of cognitive impairment that the commenter describes.
We evaluated the suitability of the DOTPA, as well as other screening tools that targeted functional cognition, by engaging our TEP, through “alpha” feasibility testing, and through soliciting input from stakeholders. At the second TEP meeting in March 2017, members questioned the use of data elements that rely on assessor observation and judgment, such as DOTPA CARE tool items, and favored other assessments of cognition that required patient interview or patient actions. The TEP also discussed performance-based assessment of functional cognition. These are assessments that require patients to respond by completing a simulated task, such as ordering from a menu, or reading medication instructions and simulating the taking of medications, as required by the Performance Assessment of Self-Care Skills (PASS) items.
In Alpha 2 feasibility testing, which was conducted between April and July 2017, we included a subset of items from the DOTPA as well as the PASS. Findings of that test identified several limitations of the DOTPA items for use as SPADEs, such as relatively long to administer (5 to 7 minutes), especially in the LTCH setting. Assessors also indicated that these items had low relevance for SNF and LTCH patients. In addition, interrater reliability was highly variable among the DOTPA items, both overall and across settings, with some items showing very low agreement (as low as 0.34) and others showing excellent agreement (as high as 0.81). Similarly, findings of the Alpha 2 feasibility test identified several limitations of the PASS for use as SPADEs. The PASS was relatively time-intensive to administer (also 5 to 7 minutes), many patients in HHAs and IRFs needed assistance completing the PASS tasks, and missing data were prevalent. Unlike the DOTPA items, interrater reliability was consistently high overall for PASS (ranging from 0.78 to 0.92), but the high reliability was not deemed to outweigh fundamental feasibility concerns related to administration challenges. A summary report for the Alpha 2 feasibility testing titled “Development and Maintenance of Standardized Cross Setting Patient Assessment Data for Post-Acute Care: Summary Report of Findings from Alpha 2 Pilot Testing” is available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/Downloads/Alpha-2-SPADE-Pilot-Summary-Document.pdf.
Feedback was obtained on the DOTPA and other assessments of functional cognition through a call for input that was open from April 26, 2017 to June 26, 2017. While we received support for the DOTPA, PASS, and other assessments of functional cognition, commenters also raised concerns about the reliability of the DOTPA, given that it is based on staff evaluation, and the feasibility of the PASS, given that the simulated medication task requires props, such as a medication bottle with printed label and pill box, which may not be accessible in all settings. A summary report for the April 26 to June 26, 2017 public comment period titled “Public Comment Summary Report 2” is available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/Downloads/Public-Comment-Summary-Report_Standardized-Patient-Assessment-Data-Element-Work_PC2_Jan-2018.pdf.
Based on the input from our TEP, results of alpha feasibility testing, and input from stakeholders, we decided to propose the BIMS for standardization at this time due to the body of research literature supporting its feasibility and validity, its relative brevity, and its existing use in the MDS and IRF-PAI.
Comment: Some commenters noted that the BIMS would likely not be completed for many LTCH patients upon admission, as many patients may be on a ventilator and/or may be unresponsive or unable to make him or herself understood. A commenter stated that they do not believe that CMS has adequately demonstrated the value of adding the BIMS data elements to the LCDS, and both commenters requested that the BIMS not be required for LTCHs.
Response: We appreciate the commenters' concern. There are coding responses available in the BIMS to denote patients who are unable to complete the assessment (for example, patients who are rarely or never understood, patients who give nonsensical responses to the interview questions). The BIMS will be considered to have been completed for the purposes of the SPADE if an assessor uses these coding responses. Although a substantial share of LTCH patients may not be able to complete the BIMS at admission, we contend that the BIMS assessment should be attempted for all patients who are able to communicate by any means. We believe it will be feasible for many patients and that the care provided to these patients will benefit from having a standardized assessment of cognition that can be exchanged across settings. After consideration of the public comments we received, we are finalizing our proposal to adopt the BIMS as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Confusion Assessment Method (CAM)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19521 through 19522), we proposed that the data elements that comprise the Confusion Assessment Method (CAM) meet the definition of standardized patient assessment data with respect to cognitive function and mental status under section 1899B(b)(1)(B)(ii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20101 through 20102), the CAM was developed to identify the signs and symptoms of delirium. It results in a score that suggests whether a patient or resident should be assigned a diagnosis of delirium. Because patients and residents with multiple comorbidities receive services from PAC providers, it is important to assess delirium, which is associated with a high mortality rate and prolonged duration of stay in hospitalized older adults.[804] Assessing these signs and symptoms of delirium is clinically relevant for care planning by PAC providers.
The CAM is a patient assessment that screens for overall cognitive impairment, as well as distinguishes delirium or reversible confusion from other types of cognitive impairment. The CAM is currently in use in two of the PAC assessments: A four-item version of the CAM is used in the MDS in SNFs, and a six-item version of the CAM is used in the LCDS in LTCHs. We proposed to replace the version of the CAM currently used in the LCDS with the four-item version of the CAM currently used in the MDS. The proposed four-item version assesses acute change in mental status, inattention, disorganized thinking, and altered level of consciousness. For more information on the CAM, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The data elements that comprise the CAM were first proposed as SPADEs in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20101 through 20102). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 expressed support for use of the CAM, noting that it would provide important information for care planning and care coordination and, therefore, contribute to quality improvement. We also stated that those commenters noted it is particularly helpful in distinguishing delirium and reversible confusion from other types of cognitive impairment. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments (82 FR 20101 through 20102) in support of the CAM. Commenters supported the continued use of the CAM in the LCDS. However, commenters expressed concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the CAM was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the CAM to be feasible and reliable for use with PAC patients and residents. More information about the performance of the CAM in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018, for the purpose of soliciting input on the proposed standardized patient assessment data elements. Although they did not specifically discuss the CAM data elements, the TEP supported the assessment of patient or resident cognitive status with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for delirium, stakeholder input, and strong test results, we proposed that the CAM data elements meet the definition of standardized patient assessment data with respect to cognitive function and mental status under section 1899B(b)(1)(B)(ii) of the Act, and to adopt the CAM as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters support the use of the CAM to assess cognitive function and mental status, but noted that it lacks sensitivity to fully capture cognitive deficits. These commenters support CMS continuing to evaluate ways to assess cognitive function.
Response: We thank the commenters for their support of the CAM data element and also recognize that the CAM assesses components of cognition and does not, alone, provide a comprehensive assessment of potential cognitive impairment.
Comment: Some commenters had concerns with the use of the CAM in the LTCH setting. A commenter stated that the CAM is not sensitive enough to detect improvements in cognitive function within LTCH patients. This commenter did not support adoption of the CAM and recommended that CMS instead study alternative methods that would accurately assess cognitive function in the LTCH setting. Another commenter noted that the CAM is specifically designed to identify delirium only and may be too narrow in scope to prove useful.
Response: We appreciate the commenters' concerns. We recognize that the CAM assesses components of cognition and does not, alone, provide a comprehensive assessment of potential cognitive impairment. As with any brief screening tool, we believe that the CAM has value as a universal assessment to identify patients in need of further clinical evaluation. We note that delirium occurs in up to half of patients/residents receiving PAC services,[805] and signs and symptoms of delirium are associated with poor functional recovery,[806] re-hospitalization, and mortality.[807] Hyperactive delirium—the type of delirium that manifests with agitation—makes up only a quarter of delirium cases.[808 809] Delirium more commonly manifests as hypoactive, or “quiet” delirium,[810] suggesting that brief, universal screening is appropriate. Moreover, because there are treatments for delirium that can be developed based on medication review, physical examination, laboratory tests, and evaluation of environmental factors,[811] we believe that screening for delirium would support care planning and care transitions for these patients.
Comment: A commenter encouraged CMS to make a CAM “score” part of the CAM SPADE. The commenter believes that LTCHs could make better and more immediate use of the results of the CAM assessment if it resulted in an easily interpretable score.
Response: The LCDS guidance manual does not currently include instructions for scoring the CAM. When the CAM is implemented across the four PAC provider types as SPADE, we will standardize the guidance to be consistent with the current guidance for the CAM in the MDS 3.0 for SNFs, which includes instructions for calculating a score. The calculation of the score and how the score is used is at the discretion of the provider. We chose not to include the score for the CAM as part of the SPADE to ensure that a diagnosis of delirium is ultimately conferred by a physician or other qualified provider. In its role as a SPADE, we do not intend the CAM to confer a diagnosis of delirium, only to indicate that delirium is likely present and that the patient requires further evaluation. However, we appreciate the commenter's recommendation and will take it into consideration as we evaluate and refine the SPADEs.
Comment: A commenter believes the CAM would be difficult to administer and raised concerns about the training that staff would receive to ensure that administration is consistent and valid.
Response: We appreciate the commenter's recommendation to provide clear training for administering the CAM and will take it into consideration as we revise the current training for the LTCHs. We intend to reinforce assessment tips and item rationale through training, open door forums, and future rulemaking efforts.
After consideration of the public comments we received, we are finalizing our proposal to adopt the CAM as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Patient Health Questionnaire-2 to 9 (PHQ-2 to 9)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19522 through 19523), we proposed that the Patient Health Questionnaire-2 to 9 (PHQ-2 to 9) data elements meet the definition of standardized patient assessment data with respect to cognitive function and mental status under section 1899B(b)(1)(B)(ii) of the Act. The proposed data elements are based on the PHQ-2 mood interview, which focuses on only the two cardinal symptoms of depression, and the longer PHQ-9 mood interview, which assesses presence and frequency of nine signs and symptoms of depression. The name of the data element, the PHQ-2 to 9, refers to an embedded a skip pattern that transitions patients with a threshold level of symptoms in the PHQ-2 to the longer assessment of the PHQ-9. The skip pattern is described further in this final rule.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20102 through 20103), depression is a common and under-recognized mental health condition. Assessments of depression help PAC providers better understand the needs of their patients and residents by: Prompting further evaluation after establishing a diagnosis of depression; elucidating the patient's or resident's ability to participate in therapies for conditions other than depression during their stay; and identifying appropriate ongoing treatment and support needs at the time of discharge.
The proposed PHQ-2 to 9 is based on the PHQ-9 mood interview. The PHQ-2 consists of questions about only the first two symptoms addressed in the PHQ-9: Depressed mood and anhedonia (inability to feel pleasure), which are the cardinal symptoms of depression. The PHQ-2 has performed well as both a screening tool for identifying depression, to assess depression severity, and to monitor patient mood over time.[812 813] If a patient demonstrates signs of depressed mood and anhedonia under the PHQ-2, then the patient is administered the lengthier PHQ-9. This skip pattern (also referred to as a gateway) is designed to reduce the length of the interview assessment for patients who fail to report the cardinal symptoms of depression. The design of the PHQ-2 to 9 reduces the burden that would be associated with the full PHQ-9, while ensuring that patients with indications of depressive symptoms based on the PHQ-2 receive the longer assessment.
Components of the proposed data elements are currently used in the OASIS for HHAs (PHQ-2) and the MDS for SNFs (PHQ-9). For more information on the PHQ-2 to 9, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We proposed the PHQ-2 data elements as SPADEs in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20102 through 20103). In that proposed rule we stated that the proposal was informed by input we received from the TEP convened by our data element contractor on April 6 and 7, 2016. The TEP members particularly noted that the brevity of the PHQ-2 made it feasible to administer with low burden for both assessors and PAC patients or residents. A summary of the April 6 and 7, 2016 TEP meeting titled “SPADE Technical Expert Panel Summary (First Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
That rule proposal was also informed by public input that we received through a call for input published on the CMS Measures Management System Blueprint website. Input was submitted from August 12 to September 12, 2016 on three versions of the PHQ depression screener: The PHQ-2; the PHQ-9; and the PHQ-2 to 9 with the skip pattern design. Many commenters were supportive of the standardized assessment of mood in PAC settings, given the role that depression plays in well-being. Several commenters expressed support for an approach that would use PHQ-2 as a gateway to the longer PHQ-9 while still potentially reducing burden on most patients and residents, as well as test administrators, and ensuring the administration of the PHQ-9, which exhibits higher specificity,[814] for patients and residents who showed signs and symptoms of depression on the PHQ-2. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal to use the PHQ-2 in the FY 2018 IPPS/LTCH PPS proposed rule, we received comments agreeing that it was important to standardize the assessment of depression in patients receiving PAC services. Many commenters also raised concerns about the ability of the PHQ-2 to correctly identify all patients with signs and symptoms of depression and noted that the proposed PHQ-2 was not included in recent, comprehensive field testing. In response to these comments, we carried out additional testing, and we provide our findings in this final rule.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the PHQ-2 to 9 data elements were included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the PHQ-2 to 9 to be feasible and reliable for use with PAC patients and residents. More information about the performance of the PHQ-2 to 9 in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the PHQ-2 to 9. The TEP was supportive of the PHQ-2 to 9 data element set as a screener for signs and symptoms of depression. The TEP's discussion noted that symptoms evaluated by the full PHQ-9 (for example, concentration, sleep, appetite) had relevance to care planning and the overall well-being of the patient or resident, but that the gateway approach of the PHQ-2 to 9 would be appropriate as a depression screening assessment, as it depends on the well-validated PHQ-2 and focuses on the cardinal symptoms of depression. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our on-going SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for depression, stakeholder input, and strong test results, in the proposed rule, we proposed that the PHQ-2 to 9 data elements meet the definition of standardized patient assessment data with respect to cognitive function and mental status under section 1899B(b)(1)(B)(ii) of the Act, and to adopt the PHQ-2 to 9 as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter supported the use of the PHQ-2 to 9 to assess cognitive function and mental status.
Response: We thank the commenter for the support of the PHQ-2 to 9.
Comment: A commenter noted confusion about how depression relates to cognitive function and the subsequent need for additional evaluation and treatment.
Response: Section 1899(b)(1)(B)(ii) of the Act specifies the category of “cognitive function, such as ability to express ideas and to understand, and mental status, such as depression and dementia.” This category includes both cognitive function and mental status. The PHQ-2 to 9 data elements do not pertain to cognitive function, but do pertain to mental status.
Comment: Several commenters expressed concern about the PHQ-2 to 9. Some commenters did not support adoption either because it was burdensome for staff and patients or because many LTCH patients do not have the cognitive function to comprehend the interview questions. Some commenters stated that asking a patient to consider a prior timeframe of 2 weeks was problematic because the typical LTCH patients are admitted after several days in the ICU, making them both unlikely to be able to respond accurately and likely to endorse depressive symptoms, given what they have recently experienced. A commenter shared results of the past internal study at their facility that identified 65 percent of admitted patients as clinically depressed. The commenter went on to inquire about what CMS hopes that additional PHQ-2 to 9 data will tell LTCHs.
Response: We recognize the challenges faced by patients receiving care from LTCH providers. Patients in LTCH settings may not be able to communicate and many patients are admitted subsequent to acute care and intensive care. This item contains a response option that allows coding for when a patient is unable to communicate or otherwise unable to complete the interview. For example, patients who cannot recall the last 2 weeks would not be required to complete the interview. However, if a patient is able to comprehend the instructions and respond to the questions, those responses should never be considered inaccurate. This is a patient interview that asks a patient about his or her symptoms; the self-report of those symptoms is the gold standard and should not be questioned because of a patient's recent experiences.
Regarding the commenter's concern that patients would be more likely to endorse depressive symptoms based on the prior acute care experiences, we acknowledge that may be the case, however, we believe these patients are perhaps some of the most likely to be experiencing the symptoms of depression and should be identified for further evaluation and treatment. In the National Beta Test, 38 percent of LTCH patients who were assessed with the PHQ-2 to 9 passed the threshold number of symptoms on the first two questions and went on to complete the additional seven questions, as compared to 28 percent of patients across all PAC provider types. This is evidence that LTCH patients in fact report higher rates of depressive symptoms than patients in other PAC settings. We believe the PHQ-2 to 9 is the most accurate and appropriate depression screening for the PAC population, including patients in LTCHs, and that assessing for depression is necessary for high-quality clinical care. We note that screening positive for depressive symptoms on the PHQ-2 to 9 does not confer a diagnosis of depression. Rather, it indicates that the patient requires further assessment by a clinician.
Regardless of the length of stay of patients, the timeframe over which they may have been experiencing signs and symptoms of depression, and the types of circumstances that have led to their LTCH stay, it is the responsibility of the LTCH to deliver high quality care for all the symptoms or conditions a patient may have. Our proposal of the PHQ-2 to 9 as SPADE is intended to improve patient care in LTCHs and across PAC provider types by ensuring that depression is assessed in every patient at admission and discharge. We believe the high prevalence of clinical depression in patients, as noted by a commenter, only highlights the need for universal screening.
Comment: Some commenters questioned the validity of the PHQ-2 to 9 because it is a based on a patient interview, rather than on a clinical assessment by a psychiatrist or psychologist.
Response: The PHQ-2 to 9 is based on the PHQ-2 mood interview, which focuses on only the two cardinal symptoms of depression, and the longer PHQ-9 mood interview, which assesses presence and frequency of nine signs and symptoms of depression. Both the PHQ-9 [815] and PHQ-2 [816] are reliable and valid measures of depression. Screening positive for depression with the PHQ-2 or PHQ-9 does not convey a diagnosis of depression, which requires a clinician's evaluation to consider the contribution of physical illness, situational conditions (for example, bereavement), the presence of additional symptoms (for example, mania) that may suggest other mental illness, and other factors to conclude that the patient has depression. Rather, positive screening for the signs and symptoms of depression with the PHQ-2 to 9 SPADE would identify patients who are in need of further evaluation and treatment.
Comment: Some commenters did not support the PHQ-2 to 9 because they stated it is unclear how it will be used to meaningfully improve care.
Response: As we described in the supporting document to the proposed rule,[817] depression is common in patients/residents receiving PAC services and associated with poor outcomes. A universal depression screening is therefore expected to improve patient outcomes by increasing the likelihood that depression will be identified and treated in LTCH patients. Regardless of the complexity of patients' medical condition, it is the responsibility of the PAC setting to deliver high quality care for all the symptoms or conditions a patient may have, including depression.
After consideration of the public comments we received, we are finalizing our proposal to adopt the PHQ-2 to 9 data elements as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
c. Special Services, Treatments, and Interventions Data
Special services, treatments, and interventions performed in PAC can have a major effect on an individual's health status, self-image, and quality of life. The assessment of these special services, treatments, and interventions in PAC is important to ensure the continuing appropriateness of care for the patients and residents receiving them, and to support care transitions from one PAC provider to another, an acute care hospital, or discharge. In alignment with our Meaningful Measures Initiative, accurate assessment of special services, treatments, and interventions of patients and residents served by PAC providers is expected to make care safer by reducing harm caused in the delivery of care; promote effective prevention and treatment of chronic disease; strengthen person and family engagement as partners in their care; and promote effective communication and coordination of care.
For example, standardized assessment of special services, treatments, and interventions used in PAC can promote patient and resident safety through appropriate care planning (for example, mitigating risks such as infection or pulmonary embolism associated with central intravenous access), and identifying life-sustaining treatments that must be continued, such as mechanical ventilation, dialysis, suctioning, and chemotherapy, at the time of discharge or transfer. Standardized assessment of these data elements will enable or support: Clinical decision-making and early clinical intervention; person-centered, high quality care through, for example, facilitating better care continuity and coordination; better data exchange and interoperability between settings; and longitudinal outcome analysis. Therefore, reliable data elements assessing special services, treatments, and interventions are needed to initiate a management program that can optimize a patient's or resident's prognosis and reduce the possibility of adverse events.
A TEP convened by our data element contractor provided input on the proposed data elements for special services, treatments, and interventions. In a meeting held on January 5 and 6, 2017, this TEP found that these data elements are appropriate for standardization because they would provide useful clinical information to inform care planning and care coordination. The TEP affirmed that assessment of these services and interventions is standard clinical practice, and that the collection of these data by means of a list and checkbox format would conform with common workflow for PAC providers. A summary of the January 5 and 6, 2017 TEP meeting titled “SPADE Technical Expert Panel Summary (Second Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Comments on the category of special services, treatments, and interventions were also submitted by stakeholders during the FY 2018 IPPS/LTCH PPS proposed rule public comment period. Although a few commenters noted the burden that the data elements for special services, treatments, and interventions will place on assessors and providers, we also received support for these data elements, noting their ability to inform care planning and care coordination.
Information on data element performance in the National Beta Test, which collected data between November 2017 and August 2018, is reported within each data element proposal in this final rule. Clinical staff who participated in the National Beta Test supported these data elements because of their importance in conveying patient or resident significant health care needs, complexity, and progress. However, clinical staff also noted that, despite the simple “check box” format of these data element, they sometimes needed to consult multiple information sources to determine a patient's or resident's treatments.
Comment: A commenter was supportive of collecting these data elements, noting that collection will help to better inform CMS and LTCH providers on the severity and needs of patients in this setting.
Response: We thank the commenter for their support.
Comment: Some commenters expressed concern about the relevance of the Special Services, Treatments, and Interventions data elements to patients in LTCHs, given the low prevalence of some of these treatments in the National Beta Test. These and another commenter also noted concern around burden of completion related to these data elements.
Response: We assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We believe that assessment of various special services, treatments, and interventions received by patients in the LTCH setting would provide important information for care planning and resource use in LTCHs. We appreciate the commenter's concern for burden related to completion of these data elements. We note that the assessment of many of the less frequently occurring treatments and conditions is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option. The assessment of the special services, treatments and interventions with multiple responses are formatted as a “check all that apply” format. Therefore, when treatments do not apply the assessor need only check one row for “None of the Above.”
Comment: Some commenters were concerned about the reliability of some Special Services, Treatments, and Interventions data elements, noting that the results of the National Beta Test indicated that some data elements demonstrated fair or even poor reliability.
Response: In the category of Special Services, Treatments, and Interventions, for SPADEs where kappas could be calculated, 1 data element and 2 sub-elements demonstrated overall reliabilities in the moderate range (0.41-0.60) and only 1 sub-element demonstrated an overall reliability in the slight/poor range (0.00-0.20). These overall reliabilities were as follows: 0.60 for the Therapeutic Diet data element, 0.55 for the “Continuous” sub-element of Oxygen Therapy, 0.46 for the “Other” sub-element of IV Medications, and 0.13 for the “Anticoagulant” sub-element of IV Medications. However, the overall reliabilities for all other Special Services, Treatments, and Interventions data elements and sub-elements where kappas could be calculated were substantial/good or excellent/almost perfect. When looking at percent agreement—an alternative measure of interrater agreement—values of overall percent agreement for all Special Services, Treatments, and Interventions SPADEs and sub-elements ranged from 80 to 100 percent.
Comment: A commenter expressed concern that the Special Services, Treatments, and Interventions data elements assess the presence or absence of the service, treatment, or intervention rather than the clinical rationale or patient outcomes. This commenter stressed the importance of bringing this assessment to “the next level” to determine impact on outcomes.
Response: We appreciate the commenter's concern that recording the presence or absence of certain treatments is only a first step in characterizing the complexity that is often the cause of a patient's receipt of special services, treatments, and interventions. We would like to clarify that any SPADE or set of data elements we proposed is intended as a minimum assessment and does not limit the ability of providers to conduct a more comprehensive evaluation of a patient's situation to identify the potential impacts on outcomes that the commenter describes.
Comment: A commenter requested clarification of the phrase, “. . . that apply at discharge.” This phrase would be used in the collection of the SPADEs in the category of Special Services, Treatments, and Interventions.
Response: The commenter is referring to an instruction in the mock-up of the SPADEs that was posted to CMS' website at the same time as the proposed rule. The mock-up is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html. The instruction appears at the top of a column within the group of items in O0110, Special Treatments, Procedures, and Programs. SPADEs on the topics of cancer treatments, respiratory therapies, and other treatments are included in this list. At discharge, the assessor is instructed to, “Check all of the following treatments, procedures, and programs that apply at discharge.”
This column is intended to capture the patient's status when he or she is discharged. Similar to other assessment data elements in current use, guidance related to these data elements will state that they should be assessed as close to the time of discharge as possible.
Final decisions on the SPADEs are given below, following more detailed comments on each SPADE proposal.
• Cancer Treatment: Chemotherapy (IV, Oral, Other)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19523 through 19524), we proposed that the Chemotherapy (IV, Oral, Other) data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20103 through 20104), chemotherapy is a type of cancer treatment that uses drugs to destroy cancer cells. It is sometimes used when a patient has a malignancy (cancer), which is a serious, often life-threatening or life-limiting condition. Both intravenous (IV) and oral chemotherapy have serious side effects, including nausea/vomiting, extreme fatigue, risk of infection due to a suppressed immune system, anemia, and an increased risk of bleeding due to low platelet counts. Oral chemotherapy can be as potent as chemotherapy given by IV, and can be significantly more convenient and less resource-intensive to administer. Because of the toxicity of these agents, special care must be exercised in handling and transporting chemotherapy drugs. IV chemotherapy is administered either peripherally or more commonly given via an indwelling central line, which raises the risk of bloodstream infections. Given the significant burden of malignancy, the resource intensity of administering chemotherapy, and the side effects and potential complications of these highly-toxic medications, assessing the receipt of chemotherapy is important in the PAC setting for care planning and determining resource use. The need for chemotherapy predicts resource intensity, both because of the complexity of administering these potent, toxic drug combinations under specific protocols, and because of what the need for chemotherapy signals about the patient's underlying medical condition. Furthermore, the resource intensity of IV chemotherapy is higher than for oral chemotherapy, as the protocols for administration and the care of the central line (if present) for IV chemotherapy require significant resources.
The Chemotherapy (IV, Oral, Other) data element consists of a principal data element (Chemotherapy) and three response option sub-elements: IV chemotherapy, which is generally resource-intensive; Oral chemotherapy, which is less invasive and generally requires less intensive administration protocols; and a third category, Other, provided to enable the capture of other less common chemotherapeutic approaches. This third category is potentially associated with higher risks and is more resource intensive due to chemotherapy delivery by other routes (for example, intraventricular or intrathecal). If the assessor indicates that the patient is receiving chemotherapy on the principal Chemotherapy data element, the assessor would then indicate by which route or routes (for example, IV, Oral, Other) the chemotherapy is administered.
A single Chemotherapy data element that does not include the proposed three sub-elements is currently in use in the MDS in SNFs. For more information on the Chemotherapy (IV, Oral, Other) data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Chemotherapy data element was proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20103 through 20104). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 expressed support for the IV Chemotherapy data element and suggested it be included as standardized patient assessment data. Commenters stated that assessing the use of chemotherapy services is relevant to share across the care continuum to facilitate care coordination and care transitions and noted the validity of the data element. Commenters also noted the importance of capturing all types of chemotherapy, regardless of route, and stated that collecting data only on patients and residents who received chemotherapy by IV would limit the usefulness of this standardized data element. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the special services, treatments, and interventions data elements in general; no additional comments were received that were specific to the Chemotherapy data element other than concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Chemotherapy data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Chemotherapy data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Chemotherapy data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions. Although the TEP members did not specifically discuss the Chemotherapy data elements, the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for chemotherapy, stakeholder input, and strong test results, we proposed that the Chemotherapy (IV, Oral, Other) data element with a principal data element and three sub-elements meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Chemotherapy (IV, Oral, Other) data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter stated it was important to know if a patient is receiving chemotherapy for cancer and the method of administration but also expressed concern about the lack of an association with a patient outcome. This commenter noted that implications of chemotherapy for patients needing speech-language pathology services include chemotherapy-related cognitive impairment, dysphagia, and speech and voice-related deficits.
Response: We thank the commenter for the support and appreciate the concern. We agree with the commenter that chemotherapy can create related treatment needs for patients, such as the examples noted by the commenter. However, we believe that it is not feasible for SPADEs to capture all of a patient's needs related to any given treatment, and we maintain that the Special Services, Treatments, and Interventions SPADEs provide a common foundation of clinical assessment, which can be built on by the individual provider or a patient's care team.
Comment: Several commenters noted concern about the low frequency of Chemotherapy in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of chemotherapy in the LTCH setting is very low. However, tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including Chemotherapy, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Chemotherapy (IV, Oral, Other) data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Cancer Treatment: Radiation
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19524 through 19525), we proposed that the Radiation data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20104 through 20105), radiation is a type of cancer treatment that uses high-energy radioactivity to stop cancer by damaging cancer cell DNA, but it can also damage normal cells. Radiation is an important therapy for particular types of cancer, and the resource utilization is high, with frequent radiation sessions required, often daily for a period of several weeks. Assessing whether a patient or resident is receiving radiation therapy is important to determine resource utilization because PAC patients and residents will need to be transported to and from radiation treatments, and monitored and treated for side effects after receiving this intervention. Therefore, assessing the receipt of radiation therapy, which would compete with other care processes given the time burden, would be important for care planning and care coordination by PAC providers.
The proposed data element consists of the single Radiation data element. The Radiation data element is currently in use in the MDS in SNFs. For more information on the Radiation data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Radiation data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20104 through 20105). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 expressed support for the Radiation data element, noting its importance and clinical usefulness for patients in PAC settings, due to the side effects and consequences of radiation treatment on patients that need to be considered in care planning and care transitions, the feasibility of the item, and the potential for it to improve quality. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the special services, treatments, and interventions data elements in general; no additional comments were received that were specific to the Radiation data element other than concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Radiation data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Radiation data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Radiation data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for radiation, stakeholder input, and strong test results, we proposed that the Radiation data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Radiation data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter expressed concern that the Radiation data element assesses whether a patient is receiving radiation for cancer treatment, but does not identify the rationale for and outcomes associated with radiation. The commenter noted that implications of radiation for patients needing speech-language pathology services include reduced head and neck range of motion due to radiation or severe fibrosis, scar bands, and reconstructive surgery complications and that these can impact both communication and swallowing abilities.
Response: We appreciate the commenter's concern. We agree with the commenter that radiation can create related treatment needs for patients, such as the examples noted by the commenter. However, we believe that it is not feasible for SPADEs to capture all of a patient's needs related to any given treatment, and we maintain that the Special Services, Treatments, and Interventions SPADEs provide a common foundation of clinical assessment, which can be built on by the individual provider or a patient's care team.
Comment: Several commenters noted concern about the low frequency of Radiation in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of radiation in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including Radiation, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Radiation data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Respiratory Treatment: Oxygen Therapy (Intermittent, Continuous, High-Concentration Oxygen Delivery System)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19525 through 19526), we proposed that the Oxygen Therapy (Intermittent, Continuous, High-Concentration Oxygen Delivery System) data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
In the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20105), we proposed a similar set of data elements related to oxygen therapy. Oxygen therapy provides a patient or resident with extra oxygen when medical conditions such as chronic obstructive pulmonary disease, pneumonia, or severe asthma prevent the patient or resident from getting enough oxygen from breathing. Oxygen administration is a resource-intensive intervention, as it requires specialized equipment such as a source of oxygen, delivery systems (for example, oxygen concentrator, liquid oxygen containers, and high-pressure systems), the patient interface (for example, nasal cannula or mask), and other accessories (for example, regulators, filters, tubing). The data element proposed here captures patient or resident use of three types of oxygen therapy (intermittent, continuous, and high-concentration oxygen delivery system), which reflects the intensity of care needed, including the level of monitoring and bedside care required. Assessing the receipt of this service is important for care planning and resource use for PAC providers.
The proposed data element, Oxygen Therapy, consists of the principal Oxygen Therapy data element and three response option sub-elements: Continuous (whether the oxygen was delivered continuously, typically defined as > =14 hours per day); Intermittent; or High-concentration oxygen delivery system. Based on public comments and input from expert advisors about the importance and clinical usefulness of documenting the extent of oxygen use, we added a third sub-element, high-concentration oxygen delivery system, to the sub-elements, which previously included only intermittent and continuous. If the assessor indicates that the patient is receiving oxygen therapy on the principal oxygen therapy data element, the assessor then would indicate the type of oxygen the patient receives (for example, Continuous, Intermittent, High-concentration oxygen delivery system).
These three proposed sub-elements were developed based on similar data elements that assess oxygen therapy, currently in use in the MDS in SNFs (“Oxygen Therapy”), previously used in the OASIS-C2 (“Oxygen (intermittent or continuous)”), and a data element tested in the PAC PRD that focused on intensive oxygen therapy (“High O2 Concentration Delivery System with FiO2 > 40 percent”). For more information on the proposed Oxygen Therapy (Continuous, Intermittent, High-concentration oxygen delivery system) data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Oxygen Therapy (Continuous, Intermittent) data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20105). In that proposed rule, we stated that the proposal was informed by input we received on the single data element, Oxygen (inclusive of intermittent and continuous oxygen use), through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 expressed the importance of the Oxygen data element, noting feasibility of this item in PAC, and the relevance of it to facilitating care coordination and supporting care transitions, but suggesting that the extent of oxygen use be documented. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the special services, treatments, and interventions data elements in general, which are previously summarized. In response to our proposal, we received comments in support of the Oxygen Therapy (Continuous, Intermittent) data element. A commenter also requested the addition of a third sub-element to differentiate between receipt of high-flow oxygen (6 or more liters per minute) and regular oxygen, noting that it is a form of respiratory support commonly used on patients with acute respiratory failure and, therefore, could be used as an indicator of patient severity in future analysis. We also received public comments related to concerns about not having recent, comprehensive field testing of proposed data elements. In response to public comments, we added a third sub-element to the Oxygen Therapy data element and carried out additional testing, which we provide our findings in this final rule.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Oxygen Therapy data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Oxygen Therapy data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Oxygen Therapy data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for oxygen therapy, stakeholder input, and strong test results, we proposed that the Oxygen Therapy (Intermittent, Continuous, High-concentration oxygen delivery system) data element with a principal data element and three sub-elements meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Oxygen Therapy (Intermittent, Continuous, High-concentration oxygen delivery system) data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter noted concern that CMS is proposing to adopt new SPADEs despite the fact that they believe that the reliability of these SPADEs was not confirmed during the National Beta Test. As an example, they stated that the Continuous sub-element within the Oxygen Therapy SPADE had only a “fair” reliability score for the LTCH setting. However, the description by CMS in the proposed rule only stated that the National Beta Test found that these SPADEs to be feasible and reliable.
Response: We appreciate the commenter's concerns. We note that we have been transparent as to the results of the National Beta Test by sharing early findings with stakeholders at a public meeting on November 27, 2018, and including results from the National Beta Test in supplementary materials to the proposed rule.
The kappa for the overarching Oxygen Therapy data element was good (0.82) when looking at all settings together, and in fact slightly higher in the LTCH setting (0.86). The commenter highlighted that the kappa for the Continuous Therapy sub-element was 0.55 overall and 0.35 in the LTCH setting. Another measure of reliability, percent agreement between assessors, was excellent/almost perfect for the three Oxygen Therapy sub-elements: Percent agreement ranged from 94 to 99 percent across settings, and 92 to 97 percent in the LTCH setting.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Oxygen Therapy (Intermittent, Continuous, High-Concentration Oxygen Delivery System) data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Respiratory Treatment: Suctioning (Scheduled, As needed)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19526 through 19528), we proposed that the Suctioning (Scheduled, As needed) data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20105 through 20106), suctioning is a process used to clear secretions from the airway when a person cannot clear those secretions on his or her own. It is done by aspirating secretions through a catheter connected to a suction source. Types of suctioning include oropharyngeal and nasopharyngeal suctioning, nasotracheal suctioning, and suctioning through an artificial airway such as a tracheostomy tube. Oropharyngeal and nasopharyngeal suctioning are a key part of many patients' care plans, both to prevent the accumulation of secretions than can lead to aspiration pneumonias (a common condition in patients with inadequate gag reflexes), and to relieve obstructions from mucus plugging during an acute or chronic respiratory infection, which often lead to desaturations and increased respiratory effort. Suctioning can be done on a scheduled basis if the patient is judged to clinically benefit from regular interventions, or can be done as needed when secretions become so prominent that gurgling or choking is noted, or a sudden desaturation occurs from a mucus plug. As suctioning is generally performed by a care provider rather than independently, this intervention can be quite resource intensive if it occurs every hour, for example, rather than once a shift. It also signifies an underlying medical condition that prevents the patient from clearing his/her secretions effectively (such as after a stroke, or during an acute respiratory infection). Generally, suctioning is necessary to ensure that the airway is clear of secretions which can inhibit successful oxygenation of the individual. The intent of suctioning is to maintain a patent airway, the loss of which can lead to death, or complications associated with hypoxia.
The Suctioning (Scheduled, As needed) data element consists of a principal data element, and two sub-elements: Scheduled; and As needed. These sub-elements capture two types of suctioning. Scheduled indicates suctioning based on a specific frequency, such as every hour. As needed means suctioning only when indicated. If the assessor indicates that the patient is receiving suctioning on the principal Suctioning data element, the assessor would then indicate the frequency (for example, Scheduled, As needed). The proposed data element is based on an item currently in use in the MDS in SNFs which does not include our proposed two sub-elements, as well as data elements tested in the PAC PRD that focused on the frequency of suctioning required for patients with tracheostomies (“Trach Tube with Suctioning: Specify most intensive frequency of suctioning during stay [Every __ hours]”). For more information on the Suctioning data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Suctioning data elements were first proposed as SPADEs in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20105 through 20106). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12, to September 12, 2016 expressed support of the Suctioning data element currently used in the MDS in SNFs. The input noted the feasibility of this item in PAC, and the relevance of this data element to facilitating care coordination and supporting care transitions. We also received public comments suggesting that we examine the frequency of suctioning in order to better understand the use of staff time, the impact on a patient or resident's capacity to speak and swallow, and intensity of care required. Based on these comments, we decided to add two sub-elements (Scheduled and As needed) to the suctioning element. The proposed Suctioning data element includes both the principal Suctioning data element that is included on the MDS in SNFs and two sub-elements, Scheduled and As needed. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the special services, treatments, and interventions data elements in general; no additional comments were received that were specific to the Suctioning data element other than concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Suctioning data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Suctioning data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Suctioning data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicited additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for suctioning, stakeholder input, and strong test results, we proposed that the Suctioning (Scheduled, As needed) data element with a principal data element and two sub-elements meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Suctioning (Scheduled, As needed) data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter requested that this data element also assess the frequency of suctioning, as it can impact resource utilization and potential medication changes in the plan of care.
Response: We appreciate the commenter's concern that the response options for this data element may not fully capture impacts to resource utilization and care plans. The Suctioning data element includes sub-elements to identify if suctioning is performed on a “Scheduled” or “As Needed” basis, but it does not directly assess the frequency of suctioning by, for example, asking an assessor to specify how often suctioning is scheduled. As finalized, this data element differentiates between patients who only occasionally need suctioning, and patients for whom assessment of suctioning needs is a frequent and routine part of the care they receive, and one that is monitored on a schedule according to physician instructions. In our work to identify standardized data elements, we have strived to balance the scope and level of detail of the data elements against the potential burden placed on patients and providers. However, we would like to clarify that any standardized patient assessment data element is intended as a minimum assessment and does not limit the ability of providers to conduct a more comprehensive evaluation of a patient's situation to identify the potential impacts on outcomes that the commenter describes.
Comment: Several commenters noted concern about the low frequency of Suctioning in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of suctioning in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including the Suctioning data element, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Suctioning (Scheduled, As needed) data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Respiratory Treatment: Tracheostomy Care
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19528), we proposed that the Tracheostomy Care data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20106 through 20107), a tracheostomy provides an air passage to help a patient or resident breathe when the usual route for breathing is obstructed or impaired. Generally, in all of these cases, suctioning is necessary to ensure that the tracheostomy is clear of secretions, which can inhibit successful oxygenation of the individual. Often, individuals with tracheostomies are also receiving supplemental oxygenation. The presence of a tracheostomy, albeit permanent or temporary, warrants careful monitoring and immediate intervention if the tracheostomy becomes occluded or if the device used becomes dislodged. While in rare cases the presence of a tracheostomy is not associated with increased care demands (and in some of those instances, the care of the ostomy is performed by the patient) in general the presence of such as device is associated with increased patient risk, and clinical care services will necessarily include close monitoring to ensure that no life-threatening events occur as a result of the tracheostomy. In addition, tracheostomy care, which primarily consists of cleansing, dressing changes, and replacement of the tracheostomy cannula (tube), is a critical part of the care plan. Regular cleansing is important to prevent infection such as pneumonia and to prevent any occlusions with which there are risks for inadequate oxygenation.
The proposed data element consists of the single Tracheostomy Care data element. The proposed data element is currently in use in the MDS in SNFs (“Tracheostomy care”). For more information on the Tracheostomy Care data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Tracheostomy Care data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20106 through 20107). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 expressed support of the Tracheostomy Care data element, noting the feasibility of this item in PAC, and the relevance of this data element to facilitating care coordination and supporting care transitions. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
During the FY 2018 IPPS/LTCH PPS proposed rule comment period, we received public comments in support of the special services, treatments, and interventions data elements in general; no additional comments were received that were specific to the Tracheostomy Care data element other than concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Tracheostomy Care data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Tracheostomy Care data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Tracheostomy Care data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for tracheostomy care, stakeholder input, and strong test results, we proposed that the Tracheostomy Care data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Tracheostomy Care data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter noted the importance of determining whether a patient is receiving tracheostomy care, as it helps with risk adjustment and identifying increased resource utilization, and recommended that the SPADE be expanded to ask about the size of the tracheostomy and whether the tracheostomy has a cuff or is fenestrated.
Response: Risk adjustment determinations is an issue that we continue to evaluate in all of our QRP programs. We will note this issue for further analysis in our future work to determine how the SPADEs will be used. With regard to the commenter's request to expand the Tracheostomy Care SPADE to include more detail about the type of tracheostomy, we do not believe that this level of clinical detail is necessary to fulfill the purposes of the SPADEs, which are to support care coordination, care planning, and future quality measures. We believe the broad indication that a patient is receiving Tracheostomy Care will be sufficient for the purposes of standardization and quality measurement.
Comment: Several commenters noted concern about the low frequency of Tracheostomy Care in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of tracheostomy care in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including Tracheostomy Care, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
Comment: A commenter stated a concern that emphasizing tracheostomy care may lead to unnecessary testing for bacteria (“cultures”) and thus unnecessary antibiotics.
Response: We appreciate the commenter's concern. We would like to clarify that the Tracheostomy Care SPADE assesses whether or not a patient is receiving care for a tracheostomy, and does not speak to the clinical care that patients with tracheostomies may require. We intend to monitor data and outcomes related to implementation of the SPADEs, especially any adverse events (such as infections) as a result of tracheostomy care.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Tracheostomy Care data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Respiratory Treatment: Non-invasive Mechanical Ventilator (BiPAP, CPAP)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19529 through 19530), we proposed that the Non-invasive Mechanical Ventilator (Bilevel Positive Airway Pressure [BiPAP], Continuous Positive Airway Pressure [CPAP]) data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20107), BiPAP and CPAP are respiratory support devices that prevent the airways from closing by delivering slightly pressurized air via electronic cycling throughout the breathing cycle (BiPAP) or through a mask continuously (CPAP). Assessment of non-invasive mechanical ventilation is important in care planning, as both CPAP and BiPAP are resource-intensive (although less so than invasive mechanical ventilation) and signify underlying medical conditions about the patient or resident who requires the use of this intervention. Particularly when used in settings of acute illness or progressive respiratory decline, additional staff (for example, respiratory therapists) are required to monitor and adjust the CPAP and BiPAP settings and the patient or resident may require more nursing resources.
The proposed data element, Non-invasive Mechanical Ventilator (BIPAP, CPAP), consists of the principal Non-invasive Mechanical Ventilator data element and two sub-elements: BiPAP and CPAP. If the assessor indicates that the patient is receiving non-invasive mechanical ventilation on the principal Non-invasive Mechanical Ventilator data element, the assessor would then indicate which type (that is, BIPAP, CPAP). Data elements that assess non-invasive mechanical ventilation are currently included on LCDS for the LTCH setting (“Non-invasive Ventilator (BIPAP, CPAP)”), and the MDS for the SNF setting (“Non-invasive Mechanical Ventilator (BiPAP/CPAP)”). We proposed to expand the existing “Non-invasive Ventilator (BiPAP, CPAP)” data element on the LCDS, by retaining and renaming the main data element to be Non-invasive Mechanical Ventilator and adding two sub-elements for BiPAP and CPAP. For more information on the Non-invasive Mechanical Ventilator (BIPAP, CPAP) data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Non-invasive Mechanical Ventilator data element was first proposed as SPADEs in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20107). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website on a single data element, BiPAP/CPAP, that captures equivalent clinical information but uses a different label, to what is currently in use on the MDS in SNFs and LCDS in LTCHs. Input submitted from August 12 to September 12, 2016 expressed support of the data element, noting the feasibility in PAC, and the relevance to facilitating care coordination and supporting care transitions. In addition, there was support in the public comment responses for separating out BiPAP and CPAP as distinct sub-elements, as they are therapies used for different types of patients and residents. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the special services, treatments, and interventions data elements in general; no additional comments were received that were specific to the Non-invasive Mechanical Ventilator data element other than concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Non-invasive Mechanical Ventilator data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Non-invasive Mechanical Ventilator data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Non-invasive Mechanical Ventilator data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for non-invasive mechanical ventilation, stakeholder input, and strong test results, we proposed that the Non-invasive Mechanical Ventilator (BiPAP, CPAP) data element, with a principal data element and two sub-elements, meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Non-invasive Mechanical Ventilator (BiPAP, CPAP) data element as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters noted concern about the low frequency of Non-Invasive Mechanical Ventilators in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of non-invasive mechanical ventilators in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many less frequently occurring treatments and conditions, including Non-invasive Mechanical Ventilator, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Non-invasive Mechanical Ventilator (BiPAP, CPAP) data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Respiratory Treatment: Invasive Mechanical Ventilator
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19530 through 19531), we proposed that the Invasive Mechanical Ventilator data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20107 through 20108), invasive mechanical ventilation includes ventilators and respirators that ventilate the patient through a tube that extends via the oral airway into the pulmonary region or through a surgical opening directly into the trachea. Thus, assessment of invasive mechanical ventilation is important in care planning and risk mitigation. Ventilation in this manner is a resource-intensive therapy associated with life-threatening conditions without which the patient or resident would not survive. However, ventilator use has inherent risks requiring close monitoring. Failure to adequately care for the patient or resident who is ventilator dependent can lead to iatrogenic events such as death, pneumonia and sepsis. Mechanical ventilation further signifies the complexity of the patient's underlying medical or surgical condition. Of note, invasive mechanical ventilation is associated with high daily and aggregate costs.[818]
The proposed data element, Invasive Mechanical Ventilator, consists of a single data element. Data elements that capture invasive mechanical ventilation are currently in use in the MDS in SNFs and LCDS in LTCHs. We proposed that this data element will be collected at admission from the “Invasive Mechanical Ventilation Support upon Admission to the LTCH” data element that is already included on the LCDS, and through a new, added data element at discharge. For more information on the Invasive Mechanical Ventilator data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Invasive Mechanical Ventilator data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20107 through 20108). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website on data elements that assess invasive ventilator use and weaning status that were tested in the PAC PRD (“Ventilator—Weaning” and “Ventilator—Non-Weaning”). Input submitted from August 12 to September 12, 2016 expressed support for this data element, highlighting the importance of this information in supporting care coordination and care transitions. Some commenters expressed concern about the appropriateness for standardization, given the prevalence of ventilator weaning across PAC providers; the timing of administration; how weaning is defined; and how weaning status relates to quality of care. These public comments guided our decision to propose a single data element focused on current use of invasive mechanical ventilation only, which does not attempt to capture weaning status. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Special Services, Treatments, and Interventions data elements in general, and support from a commenter on the Invasive Mechanical Ventilator data element. However, concerns were expressed about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Invasive Mechanical Ventilator data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Invasive Mechanical Ventilator data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Invasive Mechanical Ventilator data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for invasive mechanical ventilation, stakeholder input, and strong test results, we proposed that the Invasive Mechanical Ventilator data element that assesses the use of an invasive mechanical ventilator meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Invasive Mechanical Ventilator data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter was disappointed to see that this data element only assesses whether or not a patient is on a mechanical ventilator. The commenter suggested CMS consider collecting data to track functional outcomes related to progress towards independence in communication and swallowing.
Response: In our evaluation of the suitability of data elements for SPADEs, we examined the clinical usefulness of candidate SPADEs across the full range of PAC providers. We intend to use the SPADEs to inform care planning and comparing of assessment data for standardized measures. We believe that assessing the use of an invasive mechanical ventilator is a useful point of information to inform care planning and further assessment, such as related to functional outcomes. We will take into consideration functional outcomes, overall, that are related to progress towards independence in communication and swallowing in future measure modifications.
Comment: Several commenters noted concern about the low frequency of Invasive Mechanical Ventilators in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of invasive mechanical ventilators in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including Invasive Mechanical Ventilator, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Invasive Mechanical Ventilator data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Intravenous (IV) Medications (Antibiotics, Anticoagulants, Vasoactive Medications, Other)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19531 through 19532), we proposed that the IV Medications (Antibiotics, Anticoagulants, Vasoactive Medications, Other) data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
We proposed a similar set of data elements related to IV medications in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20108 through 20109). IV medications are solutions of a specific medication (for example, antibiotics, anticoagulants) administered directly into the venous circulation via a syringe or intravenous catheter (tube). IV medications are administered via intravenous push, single, intermittent, or continuous infusion through a tube placed into the vein. Further, IV medications are more resource intensive to administer than oral medications, and signify a higher patient complexity (and often higher severity of illness).
The clinical indications for each of the sub-elements of the IV Medications data element (Antibiotics, Anticoagulants, Vasoactive Medications, and Other) are very different. IV antibiotics are used for severe infections when: The bioavailability of the oral form of the medication would be inadequate to kill the pathogen; an oral form of the medication does not exist; or the patient is unable to take the medication by mouth. IV anticoagulants refer to anti-clotting medications (that is, “blood thinners”). IV anticoagulants are commonly used for hospitalized patients who have deep venous thrombosis, pulmonary embolism, or myocardial infarction, as well as those undergoing interventional cardiac procedures. Vasoactive medications refer to the IV administration of vasoactive drugs, including vasopressors, vasodilators, and continuous medication for pulmonary edema, which increase or decrease blood pressure or heart rate. The indications, risks, and benefits of each of these classes of IV medications are distinct, making it important to assess each separately in PAC. Knowing whether or not patients are receiving IV medication and the type of medication provided by each PAC provider will improve quality of care.
The IV Medications (Antibiotics, Anticoagulants, Vasoactive Medications, and Other) data element we proposed consists of a principal data element (IV Medications) and four response option sub-elements: Antibiotics; Anticoagulants; Vasoactive Medications; and Other. The Vasoactive Medications sub-element was not proposed in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20108 through 20109). We added the Vasoactive Medications sub-element to our proposal in order to harmonize the proposed IV Mediciations element with the data currently collected in the LCDS.
If the assessor indicates that the patient is receiving IV medications on the principal IV Medications data element, the assessor would then indicate which types of medications (for example, Antibiotics, Anticoagulants, Vasoactive Medications, Other). An IV Medications data element is currently in use on the MDS in SNFs and there is a related data element in OASIS that collects information on Intravenous and Infusion Therapies. The LCDS in LTCHs currently collects data on IV Vasoactive Medications. We proposed to modify the existing IV Vasoactive Medications data element in the LCDS to include additional sub-elements included in the standardized form of the IV Medications (Antibiotics, Anticoagulation, Vasoactive Medications, Other) data element and a principal data element for IV Medications. For more information on the IV Medications (Antibiotics, Anticoagulants, Vasoactive Medications, Other) data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
An IV Medications data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20108 through 20109). In that proposed rule, we stated that the proposal was informed by input we received on Vasoactive Medications through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 supported this data element, with one noting the importance of this data element in supporting care transitions. We also stated that these commenters had criticized the need for collecting specifically Vasoactive Medications, giving feedback that the data element was too narrowly focused. In addition, public comment received indicated that the clinical significance of vasoactive medications administration alone was not high enough in PAC to merit mandated assessment, noting that related and more useful information could be captured in an item that assessed all IV medication use. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Special Services, Treatments, and Interventions data elements in general; no additional comments were received that were specific to the IV Medications data element. However, general concerns were expressed about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the IV Medications data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the IV Medications data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the IV Medications data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for IV medications, stakeholder input, and strong test results, we proposed that the IV Medications (Antibiotics, Anticoagulation, Vasoactive Medications, Other) data element with a principal data element and four sub-elements meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the IV Medications (Antibiotics, Anticoagulation, Vasoactive Medications, Other) data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter was supportive of the IV Medications data element, noting that the data could be leveraged to encourage providers to transition away from the use of IV antibiotics to oral antibiotics, which would support best practices in antimicrobial stewardship.
Response: We thank the commenter for the support.
Comment: Several commenters stated concern about the low reliability of the sub-elements of the Intravenous Medications data element in the National Beta Test.
Response: For the IV Medications data element in the LTCH setting, when looking at the kappa statistic as a measures of reliability, 1 sub-element demonstrated reliability in the moderate range (0.41—0.60) and 1 sub-element demonstrated an overall reliability in the slight/poor range (0.00—0.20). These reliabilities were as follows: 0.46 for the “Other” sub-element of IV Medications, and 0.13 for the “Anticoagulation” sub-element of IV Medications. However, the reliability for the IV Medications data element was substantial/good (0.68) and for the “Antibiotics” sub-element was excellent/almost perfect (0.84). Consultation with assessors suggested that the low kappa for the IV Anticoagulants sub-element was likely due to inconsistent interpretation of the coding instructions. Having identified the likely source of the relatively lower interrater reliability, we are confident that with proper training of LTCHs on how to report the data elements, the reliability of these sub-elements will be improved. We additionally note that, when looking at percent agreement—an alternative measure of interrater agreement—values of overall percent agreement for the IV Medications data element and sub-elements were all strong, ranging from 79 to 93 percent, which provides additional support for the reliability of the IV Medications SPADE.
After consideration of the public comments we received, we are finalizing our proposal to adopt the IV Medications (Antibiotics, Anticoagulants, Vasoactive Medications, Other) data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Transfusions
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19532), we proposed that the Transfusions data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20109 through 20110), transfusion refers to introducing blood or blood products into the circulatory system of a person. Blood transfusions are based on specific protocols, with multiple safety checks and monitoring required during and after the infusion in case of adverse events. Coordination with the provider's blood bank is necessary, as well as documentation by clinical staff to ensure compliance with regulatory requirements. In addition, the need for transfusions signifies underlying patient complexity that is likely to require care coordination and patient monitoring, and impacts planning for transitions of care, as transfusions are not performed by all PAC providers.
The proposed data element consists of the single Transfusions data element. A data element on transfusion is currently in use in the MDS in SNFs (“Transfusions”) and a data element tested in the PAC PRD (“Blood Transfusions”) was found feasible for use in each of the four PAC settings. For more information on the Transfusions data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Transfusions data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20109 through 20110).
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Special Services, Treatments, and Interventions data elements in general. In response to our proposal, we received comments in support of the Transfusions data element. A commenter supported the inclusion of the Transfusions data element because transfusions are increasingly being performed outside of the hospital setting and reporting transfusions as a SPADE will contribute to higher quality, coordinated care for patients who rely on these life-saving treatments. However, concerns were expressed about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Transfusions data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Transfusions data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Transfusions data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions. Although the TEP did not specifically discuss the Transfusions data element, the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for transfusions, stakeholder input, and strong test results, we proposed that the Transfusions data element that is currently in use in the MDS in SNFs meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Transfusions data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter applauded CMS for including the Transfusions data element, noting that it will provide information on care planning, clinical decision making, patient safety, care transitions, and resource use in LTCHs and will contribute to higher quality and coordinated care for patients who rely on these life-saving treatments.
Response: We thank the commenter for the support. We selected the Transfusions data element for proposal as standardized data in part because of the attributes that the commenter noted.
Comment: A commenter was concerned that LTCHs will not have the resources needed to provide patients with access to blood transfusions and requested that CMS consider whether payments to LTCHs are adequate to cover the cost of this resource intensive, specialized service.
Response: We wish to clarify that the Transfusions SPADE collects information on the complexity of the patient and resources the patient requires. At this time, this item will not be used for any payment purposes, and thus we are not able to comment on the cost of this service. This SPADE is not intended to measure the ability of an LTCH to provide in-house transfusions, only to capture the services a given patient may be receiving. Further, for patients who require services related to blood transfusions, information collected by this data element is a part of common clinical workflow, and thus, we believe that burden on resource intensity would not be affected by the standardization of this data element.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Transfusions data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Dialysis (Hemodialysis, Peritoneal dialysis)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19533 through 19534), we proposed that the Dialysis (Hemodialysis, Peritoneal dialysis) data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20110), dialysis is a treatment primarily used to provide replacement for lost kidney function. Both forms of dialysis (hemodialysis and peritoneal dialysis) are resource intensive, not only during the actual dialysis process but before, during and following. Patients and residents who need and undergo dialysis procedures are at high risk for physiologic and hemodynamic instability from fluid shifts and electrolyte disturbances as well as infections that can lead to sepsis. Further, patients or residents receiving hemodialysis are often transported to a different facility, or at a minimum, to a different location in the same facility for treatment. Close monitoring for fluid shifts, blood pressure abnormalities, and other adverse effects is required prior to, during and following each dialysis session. Nursing staff typically perform peritoneal dialysis at the bedside, and as with hemodialysis, close monitoring is required.
The proposed data element, Dialysis (Hemodialysis, Peritoneal dialysis) consists of the principal Dialysis data element and two response option sub-elements: Hemodialysis; and Peritoneal dialysis. If the assessor indicates that the patient is receiving dialysis on the principal Dialysis data element, the assessor would then indicate which type (Hemodialysis or Peritoneal dialysis). Dialysis data elements are currently included on the MDS in SNFs and the LCDS in LTCHs and assess the overall use of dialysis. We proposed to expand the existing Dialysis data element currently in the LCDS to include sub-elements for Hemodialysis and Peritoneal dialysis.
As the result of public feedback described in this final rule, in the proposed rule, we proposed data elements that include the principal Dialysis data element and two sub-elements (Hemodialysis and Peritoneal dialysis). For more information on the Dialysis data elements, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Dialysis data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20110). In that proposed rule, we stated that the proposal was informed by input we received on a singular Hemodialysis data element through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 supported the assessment of hemodialysis and recommended that the data element be expanded to include peritoneal dialysis. We also noted that several commenters had supported the singular Hemodialysis data element, noting the relevance of this information for sharing across the care continuum to facilitate care coordination and care transitions, the potential for this data element to be used to improve quality, and the feasibility for use in PAC. In addition, we received comment that the item would be useful in improving patient and resident transitions of care. We also noted that several commenters had also stated that peritoneal dialysis should be included in a standardized data element on dialysis and recommended collecting information on peritoneal dialysis in addition to hemodialysis. The rationale for including peritoneal dialysis from commenters included the fact that patients and residents receiving peritoneal dialysis will have different needs at post-acute discharge compared to those receiving hemodialysis or not having any dialysis. Based on these comments, the Hemodialysis data element was expanded to include a principal Dialysis data element and two sub-elements, Hemodialysis and Peritoneal dialysis. We proposed the version of the Dialysis element that includes two types of dialysis. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received comments in support of the Special Services, Treatments, and Interventions data elements in general. No additional comments were received that were specific to the Dialysis data element. However, concerns were expressed about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Dialysis data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Dialysis data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Dialysis data elements in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for dialysis, stakeholder input, and strong test results, we proposed that the Dialysis (Hemodialysis, Peritoneal dialysis) data element with a principal data element and two sub-elements meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Dialysis (Hemodialysis, Peritoneal dialysis) data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter was supportive of collecting information on dialysis for LTCH patients and stated it will be an important variable in the analysis of admissions to the hospital for infections.
Response: We thank the commenter for the support of the Dialysis data element.
Comment: Several commenters noted concern about the low frequency of dialysis in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of dialysis in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including Dialysis, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
Comment: A commenter raised a concern about the possible use of the Dialysis SPADE in a future unified PAC payment system, noting that facilities like theirs provide dialysis services to patients without additional reimbursement while many SNFs, for example, send dialysis patients to a dialysis center, and therefore do not incur this cost for the patients under their care. The commenter recommended that future use of the Dialysis SPADE should require additional information on the site of services to properly attribute those services to a provider.
Response: We appreciate the commenter's concern and will take this recommendation into consideration as we consider uses of the Dialysis SPADE in the future.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Dialysis (Hemodialysis, Peritoneal dialysis) data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Intravenous (IV) Access (Peripheral IV, Midline, Central line)
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19534 through 19535), we proposed that the IV Access (Peripheral IV, Midline, Central line) data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20110 through 20111), patients or residents with central lines, including those peripherally inserted or who have subcutaneous central line “port” access, always require vigilant nursing care to keep patency of the lines and ensure that such invasive lines remain free from any potentially life-threatening events such as infection, air embolism, or bleeding from an open lumen. Clinically complex patients and residents are likely to be receiving medications or nutrition intravenously. The sub-elements included in the IV Access data element distinguish between peripheral access and different types of central access. The rationale for distinguishing between a peripheral IV and central IV access is that central lines confer higher risks associated with life-threatening events such as pulmonary embolism, infection, and bleeding.
The proposed data element, IV Access (Peripheral IV, Midline, Central line), consists of the principal IV Access data element and three response option sub-elements: Peripheral IV, Midline, and Central line. The proposed IV Access data element is not currently included on any of the PAC assessment instruments. For more information on the IV Access (Peripheral IV, Midline, Central line) data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
An IV Access data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20110 through 20111). In that proposed rule, we stated that the proposal was informed by input we received on one of the PAC PRD data elements, Central Line Management, a type of IV access, through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 expressed support for the assessment of central line management and recommended that the data element be broadened to also include other types of IV access in addition to central lines. Several commenters supported the data element, noting feasibility and importance for facilitating care coordination and care transitions. However, a few commenters recommended that this data element be broadened to include peripherally inserted central catheters (“PICC lines”) and midline IVs. Based on public comment feedback and in consultation with expert input, we expanded the Central Line Management data element to include more types of IV access (that is, peripheral IV and midline). This expanded version of IV Access is the data element being proposed. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Special Services, Treatments, and Interventions data elements in general. No additional comments were received that were specific to the IV Access data element. However, concerns were expressed about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the IV Access data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the IV Access data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the IV Access data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for IV access, stakeholder input, and strong test results, we proposed that the IV access (Peripheral IV, Midline, Central line) data element with a principal data element and three sub-elements meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the IV access (Peripheral IV, Midline, Central line) data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter was supportive of collecting information on IV Access that includes peripheral IV, midline, and peripherally inserted central catheters (PICCs)—a type of central line—for LTCH patients and stated knowing about the presence of these devices will be helpful when tracking admissions for infections.
Response: We thank the commenter for the support of the IV Access data element.
After consideration of the public comments we received, we are finalizing our proposal to adopt the IV Access (Peripheral IV, Midline, Central line) data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Nutritional Approach: Parenteral/IV Feeding
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19535), we proposed that the Parenteral/IV Feeding data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20111 through 20112), parenteral nutrition/IV feeding refers to a patient or resident being fed intravenously using an infusion pump, bypassing the usual process of eating and digestion. The need for IV/parenteral feeding indicates a clinical complexity that prevents the patient or resident from meeting his or her nutritional needs enterally, and is more resource intensive than other forms of nutrition, as it often requires monitoring of blood chemistries and maintenance of a central line. Therefore, assessing a patient's or resident's need for parenteral feeding is important for care planning and resource use. In addition to the risks associated with central and peripheral intravenous access, total parenteral nutrition is associated with significant risks such as embolism and sepsis.
The proposed data element consists of the single Parenteral/IV Feeding data element. The proposed Parenteral/IV Feeding data element is currently in use in the MDS in SNFs, and equivalent or related data elements are in use in the LCDS, IRF-PAI, and OASIS. We proposed to replace the existing Total Parenteral Nutrition data element in the LCDS with the proposed Parenteral/IV Feeding data element. For more information on the Parenteral/IV Feeding data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Parenteral/IV Feeding data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20111 through 20112). In that proposed rule, we stated that the proposal was informed by input we received on Total Parenteral Nutrition (an item with nearly the same meaning as the proposed data element, but with the label used in the PAC PRD), through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016, supported this data element, noting its relevance to facilitating care coordination and supporting care transitions. After the public input period, the Total Parenteral Nutrition data element was renamed Parenteral/IV Feeding, to be consistent with how this data element is referred to in the MDS in SNFs. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received comments in support of the Special Services, Treatments, and Interventions data elements in general. In response to our proposal, we received public comments in support of the Parenteral/IV Feeding data element. Several commenters supported the inclusion of nutrition data elements and noted their importance in capturing information on additional resources necessary to treat patients with altered dietary needs. However, a commenter noted limitations of the proposed data elements, such as not recording clinical rationale for nutritional or diet needs. We also received public comments expressing concern about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Parenteral/IV Feeding data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Parenteral/IV Feeding data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Parenteral/IV Feeding data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for parenteral/IV feeding, stakeholder input, and strong test results, we proposed that the Parenteral/IV Feeding data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Parenteral/IV Feeding data element as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters were supportive of collection of the Parenteral/IV Feeding data element. A commenter stated it is critical to document information on Parenteral/IV Feeding to ensure the appropriate nutritional management of at-risk patients. Another commenter described how the SPADEs ensure that nutritional status and diet orders are included in discharge planning and transfer of health information documents, which will in turn alert the receiving providers to incorporate this information in the patient's treatment plan. Another commenter was supportive, but noted that the Parenteral/IV Feeding SPADE should not be a substitute for capturing information related to swallowing which reflects additional patient complexity and resource use.
Response: We thank the commenters for their support of the Parenteral/IV Feeding data element. We agree that documenting Parenteral/IV Feeding via this SPADE supports nutritional management and will help ensure that this information is transferred to the next provider at discharge.
We also appreciate the concern raised related to swallow assessment. We agree that the Parenteral/IV Feeding SPADE should not be used as a substitute for an assessment of a patient's swallowing. The SPADEs are not intended to replace comprehensive clinical evaluation and in no way preclude providers from conducting further patient evaluation or assessments in their settings as they believe are necessary and useful. We agree that information related to swallowing can capture patient complexity. However, we also note that Parenteral/IV Feeding data element captures a different construct than an evaluation of swallowing. That is, the Parenteral/IV Feeding data element captures a patient's need to receive calories and nutrients intravenously, while an assessment of swallowing would capture a patient's functional ability to safely consume food orally for digestion in their gastrointestinal tract.
Comment: Several commenters noted concern about the low frequency of Parenteral/IV Feeding in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of parenteral/IV feeding in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including Parenteral/IV Feeding, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Parenteral/IV Feeding data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Nutritional Approach: Feeding Tube
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19535 through 19536), we proposed that the Feeding Tube data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20112), the majority of patients admitted to acute care hospitals experience deterioration of their nutritional status during their hospital stay, making assessment of nutritional status and method of feeding if unable to eat orally very important in PAC. A feeding tube can be inserted through the nose or the skin on the abdomen to deliver liquid nutrition into the stomach or small intestine. Feeding tubes are resource intensive and, therefore, are important to assess for care planning and resource use. Patients with severe malnutrition are at higher risk for a variety of complications.[819] In PAC settings, there are a variety of reasons that patients and residents may not be able to eat orally (including clinical or cognitive status).
The proposed data element consists of the single Feeding Tube data element. The Feeding Tube data element is currently included in the MDS for SNFs, and in the OASIS for HHAs, where it is labeled Enteral Nutrition. A related data element, collected in the IRF-PAI for IRFs (Tube/Parenteral Feeding), assesses use of both feeding tubes and parenteral nutrition. For more information on the Feeding Tube data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Feeding Tube data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20112). In that proposed rule, we stated that the proposal was informed by input we received through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 on an Enteral Nutrition data element (which is the same as the data element we proposed in the proposed rule, but is used in the OASIS under a different name) supported the data element, noting the importance of assessing enteral nutrition status for facilitating care coordination and care transitions. After the public comment period, the Enteral Nutrition data element used in public comment was renamed “Feeding Tube”, indicating the presence of an assistive device. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Special Services, Treatments, and Interventions data elements in general. In response to our proposal, we received public comments in support of the Feeding Tube data element. Several commenters supported the inclusion of nutrition data elements, noting their importance when capturing dietary needs. However, we also received recommendations to increase the specificity of the data element by using more clinical terminology and assessing clinical rationale for nutritional or dietary needs as well as concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Feeding Tube data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Feeding Tube data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Feeding Tube data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for feeding tubes, stakeholder input, and strong test results, we proposed that the Feeding Tube data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Feeding Tube data element as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters were supportive of collection of the Feeding Tube data element, with one stating it is critical to document information on Feeding Tube to ensure the appropriate nutritional management of at-risk patients. A commenter described how the SPADEs ensure that nutritional status and diet orders are included in discharge planning and transfer of health information documents, which will in turn alert the receiving providers to incorporate this information in the patient's treatment plan.
Response: We thank the commenters for their support of the Feeding Tube data element.
Comment: A commenter noted that in addition to identifying if the patient is on a feeding tube, it would be important to assess the patient's progression towards oral feeding within this data element, as this impacts the tube feeding regimen.
Response: We agree that progression to oral feeding is important for care planning and transfer. At this time, we are finalizing a singular Feeding Tube SPADE, which assesses the nutritional approach only and does not capture the patient's prognosis with regard to oral feeding. We wish to clarify that the SPADEs are not intended to replace comprehensive clinical evaluation and in no way preclude providers from conducting further patient evaluation or assessments in their settings as they believe are necessary and useful. We will take this recommendation into consideration in future work on standardized data elements.
Comment: Several commenters noted concern about the low frequency of a Feeding Tube in all PAC patients, which would limit the utility of the data collected.
Response: We appreciate the commenters' concern and we agree that the frequency of a feeding tube in the LTCH setting is very low. However, we assert that tracking important clinical information is important to care planning and transfer of information across settings of care, even if events are rare. We note that the assessment of many of the less frequently occurring treatments and conditions, including Feeding Tube, is formatted as a “check all that apply” list. We believe this approach minimizes burden because a data element only needs to be checked if a patient is receiving that treatment. If a patient is receiving no treatments in the list, the assessor need only check the “none of the above” option.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Feeding Tube data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Nutritional Approach: Mechanically Altered Diet
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19536 through 19537), we proposed that the Mechanically Altered Diet data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20112 through 20113), the Mechanically Altered Diet data element refers to food that has been altered to make it easier for the patient or resident to chew and swallow, and this type of diet is used for patients and residents who have difficulty performing these functions. Patients with severe malnutrition are at higher risk for a variety of complications.[820]
In PAC settings, there are a variety of reasons that patients and residents may have impairments related to oral feedings, including clinical or cognitive status. The provision of a mechanically altered diet may be resource intensive, and can signal difficulties associated with swallowing/eating safety, including dysphagia. In other cases, it signifies the type of altered food source, such as ground or puree, that will enable the safe and thorough ingestion of nutritional substances and ensure safe and adequate delivery of nourishment to the patient. Often, patients on mechanically altered diets also require additional nursing supports such as individual feeding, or direct observation, to ensure the safe consumption of the food product. Assessing whether a patient or resident requires a mechanically altered diet is therefore important for care planning and resource identification.
The proposed data element consists of the single Mechanically Altered Diet data element. The proposed data element for a mechanically altered diet is currently included on the MDS for SNFs. A related data element for modified food consistency/supervision is currently included on the IRF-PAI for IRFs. Another related data element is included in the OASIS for HHAs that collects information about independent eating that requires “a liquid, pureed or ground meat diet.” For more information on the Mechanically Altered Diet data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Mechanically Altered Diet data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20112 through 20113).
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Special Services, Treatments, and Interventions data elements in general. In response to our proposal, we received comments in support of the Mechanically Altered Diet data element. Several commenters supported the inclusion of nutrition data elements noting their importance in capturing information on additional resources necessary to treat patients with altered dietary needs. However, a commenter noted limitations of the proposed data elements, such as not recording clinical rationale for nutritional or diet needs. We received further concerns regarding not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Mechanically Altered Diet data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Mechanically Altered Diet data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Mechanically Altered Diet data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for mechanically altered diet, stakeholder input, and strong test results, we proposed that the Mechanically Altered Diet data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Mechanically Altered Diet data element as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters were supportive of collection of the Mechanically Altered Diet data element, with a commenter stating that it is critical to document information on Mechanically Altered Diet to ensure the appropriate nutritional management of at-risk patients. Another commenter described how the SPADEs ensure that nutritional status and diet orders are included in discharge planning and transfer of health information documents, which will in turn alert the receiving providers to incorporate this information in the patient's treatment plan.
Response: We thank the commenters for their support of the Mechanically Altered Diet data element.
Comment: A commenter was concerned that the Mechanically Altered Diet data element does not capture clinical complexity and does not provide any insight into resource allocation because it only measures whether the patient needs a mechanically altered diet and not, for example, the extent of help a patient needs in consuming a meal.
Response: We believe that assessing patients' needs for mechanically altered diets captures one piece of information about clinical complexity and resource allocation. A patient with this special nutritional requirement may require additional nutritional planning services, special meals, and staff to ensure that meals are prepared and served in the way the patient needs. Additional factors that would affect resource allocation, such as those noted by the commenter, are not captured by this data element. We have decided not to alter the SPADE as proposed in order to balance the scope and level of detail of the data elements against the potential burden placed on providers who must complete the assessment. We will take this suggestion into consideration in future refinement of the clinical SPADEs.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Mechanically Altered Diet data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Nutritional Approach: Therapeutic Diet
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19537 through 19538), we proposed that the Therapeutic Diet data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20113), a therapeutic diet refers to meals planned to increase, decrease, or eliminate specific foods or nutrients in a patient or resident's diet, such as a low-salt diet, for the purpose of treating a medical condition. The use of therapeutic diets among patients in PAC provides insight on the clinical complexity of these patients and their multiple comorbidities. Therapeutic diets are less resource intensive from the bedside nursing perspective, but do signify one or more underlying clinical conditions that preclude the patient from eating a regular diet. The communication among PAC providers about whether a patient is receiving a particular therapeutic diet is critical to ensure safe transitions of care.
The proposed data element consists of the single Therapeutic Diet data element. The Therapeutic Diet data element is currently in use in the MDS in SNFs. For more information on the Therapeutic Diet data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Therapeutic Diet data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20113).
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Special Services, Treatments, and Interventions data elements in general. Several commenters supported the inclusion of nutrition data elements noting their importance in capturing information on additional resources necessary to treat patients with altered dietary needs. However, a commenter noted limitations of the proposed data elements, such as not recording clinical rationale for nutritional or diet needs. Other commenters recommended the addition of specific terminology to these data elements, as well as aligning the definition of Therapeutic Diet with the Academy of Nutrition and Dietetics' definition. A commenter suggested use of the term “medically altered diet” instead of “therapeutic diet.” We also received comments related to concerns about not having recent, comprehensive field testing of proposed data elements.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Therapeutic Diet data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Therapeutic Diet data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Therapeutic Diet data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the special services, treatments, and interventions and the TEP supported the assessment of the special services, treatments, and interventions included in the National Beta Test with respect to both admission and discharge. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for therapeutic diet, stakeholder input, and strong test results, we proposed that the Therapeutic Diet data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the Therapeutic Diet data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A few commenters were supportive of collection of the Therapeutic Diet data element, with one stating that it is critical to document information on Therapeutic Diet to ensure the appropriate nutritional management of at-risk patients. Another commenter described how the SPADEs ensure that nutritional status and diet orders are included in discharge planning and transfer of health information documents, which will in turn alert the receiving providers to incorporate this information in the patient's treatment plan.
Response: We thank the commenters for their support of the Therapeutic Diet data element.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Therapeutic Diet data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• High-Risk Drug Classes: Use and Indication
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19538 through 19540), we proposed that the High-Risk Drug Classes: Use and Indication data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act.
Most patients receiving PAC services depend on short- and long-term medications to manage their medical conditions. However, as a treatment, medications are not without risk; medications are in fact a leading cause of adverse events. A study by the U.S. Department of Health and Human Services found that 31 percent of adverse events that occurred in 2008 among hospitalized Medicare beneficiaries were related to medication.[821] Moreover, changes in a patient's condition, medications, and transitions between care settings put patients at risk of medication errors and adverse drug events (ADEs). ADEs may be caused by medication errors such as drug omissions, errors in dosage, and errors in dosing frequency.[822]
ADEs are known to occur across different types of healthcare settings. For example, the incidence of ADEs in the outpatient setting has been estimated at 1.15 ADEs per 100 person-months,[823] while the rate of ADEs in the long-term care setting is approximately 9.80 ADEs per 100 resident-months.[824] In the hospital setting, the incidence has been estimated at 15 ADEs per 100 admissions.[825] In addition, approximately half of all hospital-related medication errors and 20 percent of ADEs occur during transitions within, admission to, transfer to, or discharge from a hospital.[826 827 828] ADEs are more common among older adults, who make up most patients receiving PAC services. The rate of emergency department visits for ADEs is three times higher among adults 65 years of age and older compared to that among those younger than age 65.[829]
Understanding the types of medication a patient is taking and the reason for its use are key facets of a patient's treatment with respect to medication. Some classes of drugs are associated with more risk than others.[830] We proposed one High-Risk Drug Class data element with six medication classes as sub-elements. The six medication classes we proposed as response options for the High-Risk Drug Classes: Use and Indication data element are: Anticoagulants; antiplatelets; hypoglycemics (including insulin); opioids; antipsychotics; and antibiotics. These drug classes are high-risk due to the adverse effects that may result from use. In particular, bleeding risk is associated with anticoagulants and antiplatelets; [831 832] fluid retention, heart failure, and lactic acidosis are associated with hypoglycemics; [833] misuse is associated with opioids; [834] fractures and strokes are associated with antipsychotics; [835 836] and various adverse events such as central nervous systems effects and gastrointestinal intolerance are associated with antimicrobials,[837] the larger category of medications that include antibiotics. Moreover, some medications in five of the six drug classes included in this data element are included in the 2019 Updated Beers Criteria® list as potentially inappropriate medications for use in older adults.[838] Finally, although a complete medication list should record several important attributes of each medication (for example, dosage, route, stop date), recording an indication for the drug is of crucial importance.[839]
The High-Risk Drug Classes: Use and Indication data element requires an assessor to record whether or not a patient is taking any medications within six drug classes. The six response options for this data element are high-risk drug classes with particular relevance to PAC patients and residents, as identified by our data element contractor. The six data response options are Anticoagulants, Antiplatelets, Hypoglycemics, Opioids, Antipsychotics, and Antibiotics. For each drug class, the assessor is asked to indicate if the patient is taking any medications within the class, and, for drug classes in which medications were being taken, whether indications for all drugs in the class are noted in the medical record. For example, for the response option Anticoagulants, if the assessor indicates that the patient is taking anticoagulant medication, the assessor would then indicate if an indication is recorded in the medication record for the anticoagulant(s).
The High-Risk Drug Classes: Use and Indication data element that is being proposed as a SPADE was developed as part of a larger set of data elements to assess medication reconciliation, the process of obtaining a patient's multiple medication lists and reconciling any discrepancies. For more information on the High-Risk Drug Classes: Use and Indication data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We sought public input on the relevance of conducting assessments on medication reconciliation and specifically on the proposed High-Risk Drug Classes: Use and Indication data element. Our data element contractor presented data elements related to medication reconciliation to the TEP convened on April 6 and 7, 2016. The TEP supported a focus on high-risk drugs, because of higher potential for harm to patients and residents, and were in favor of a data element to capture whether or not indications for medications were recorded in the medical record. A summary of the April 6 and 7, 2016 TEP meeting titled “SPADE Technical Expert Panel Summary (First Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html. Medication reconciliation data elements were also discussed at a second TEP meeting on January 5 and 6, 2017, convened by our data element contractor. At this meeting, the TEP agreed about the importance of evaluating the medication reconciliation process, but disagreed about how this could be accomplished through standardized assessment. The TEP also disagreed about the usability and appropriateness of using the Beers Criteria to identify high-risk medications.[840] A summary of the January 5 and 6, 2017 TEP meeting titled “SPADE Technical Expert Panel Summary (Second Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also solicited public input on data elements related to medication reconciliation during a public input period from April 26 to June 26, 2017. Several commenters expressed support for the medication reconciliation data elements that were put on display, noting the importance of medication reconciliation in preventing medication errors and stated that the items seemed feasible and clinically useful. A few commenters were critical of the choice of 10 drug classes posted during that comment period, arguing that ADEs are not limited to high-risk drugs, and raised issues related to training assessors to correctly complete a valid assessment of medication reconciliation. A summary report for the April 26 to June 26, 2017 public comment period titled “SPADE May-June 2017 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The High-Risk Drug Classes: Use and Indication data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the High-Risk Drug Classes: Use and Indication data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the High-Risk Drug Classes: Use and Indication data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our contractor convened a TEP on September 17, 2018 for the purpose of soliciting input on the standardized patient assessment data elements. The TEP acknowledged the challenges of assessing medication safety, but was supportive of some of the data elements focused on medication reconciliation that were tested in the National Beta Test. The TEP was especially supportive of the focus on the six high-risk drug classes and using these classes to assess whether the indication for a drug is recorded. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. These activities provided updates on the field-testing work and solicited feedback on data elements considered for standardization, including the High-Risk Drug Classes: Use and Indication data element. A stakeholder group was critical of the six drug classes included as response options in the High-Risk Drug Classes: Use and Indication data element, noting that potentially risky medications (for example, muscle relaxants) are not included in this list; that there may be important differences between drugs within classes (for example, more recent versus older style antidepressants); and that drug allergy information is not captured. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. In addition, a commenter questioned whether the time to complete the High-Risk Drug Classes: Use and Indication data element would differ across settings. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for the use and having indications recorded for high-risk drugs, stakeholder input, and strong test results, we proposed that the High-Risk Drug Classes: Use and Indication data element meets the definition of standardized patient assessment data with respect to special services, treatments, and interventions under section 1899B(b)(1)(B)(iii) of the Act, and to adopt the High-Risk Drug Classes: Use and Indication data element as standardized patient assessment data for use in the LTCH QRP.
Comment: A commenter supported the High-Risk Drug Class data element and the efforts of CMS to ensure LTCH patients are protected from unintended consequences that may occur with the use of high-risk medications. The commenter stated that including a documented indication for use may be helpful in assessing quality of care. The commenter also supported the six drug classes but encouraged CMS to consider the addition of the classes of high-risk medications captured in measures currently used in the Medicare Advantage program and the Merit-based Incentive Payment System (MIPS), which are also based on the Beers criteria, and to continue to refine the measures to ensure that providers are conducting high quality medication reconciliation for all patients.
Response: We thank the commenter for the support of the High-Risk Drug Class data element and the six drug classes. We believe the commenter was referring to the Use of High-Risk Medications in the Elderly (NQF #0022) quality measure which is used by MIPS and is not in the LTCH QRP at this time. We will consider their recommendation to expand and further align the drug classes in the SPADE with the drug classes used in the Use of High-Risk Medications in the Elderly quality measure, as well as the recommendation to include a documented indication for use.
Comment: Some commenters stated that the High-Risk Drugs: Use and Indication data element is not appropriate for use in patient assessments and has limited utility, because ADEs are not limited to high-risk drugs and finding the indications for drugs in a class is highly burdensome.
Response: We understand that not all ADEs are associated with “high-risk” drugs, and we also note that medications in the named drug classes are mostly used in a safe manner. Prescribed high-risk medications are defined as a “proximate factor” to preventable ADEs by the Joint Commission. However, the Joint Commission's conceptual model of preventable ADEs also includes provider, patient, health care system, organization, and technical factors, all of which present many opportunities for disrupting preventable ADEs. We have decided to focus on a selection of drug classes that are commonly used by older adults and are related to ADEs which are clinically significant, preventable, and measurable. Anticoagulants, antibiotics, and diabetic agents have been implicated in an estimated 46.9 percent (95 percent CI, 44.2 percent-49.7 percent) of emergency department visits for adverse drug events.[841] Among older adults (aged ≥65 years), three drug classes (anticoagulants, diabetic agents, and opioid analgesics) have been implicated in an estimated 59.9 percent (95 percent CI, 56.8 percent-62.9 percent) of emergency department visits for adverse drug events.[842] Further, antipsychotic medications have been identified as a drug class for which there is a need for increased outreach and educational efforts to reduce use among older adults.
After consideration of the public comments we received, we are finalizing our proposal to adopt the High-Risk Drug Classes: Use and Indication data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
d. Medical Condition and Comorbidity Data
Assessing medical conditions and comorbidities is critically important for care planning and safety for patients and residents receiving PAC services, and the standardized assessment of selected medical conditions and comorbidities across PAC providers is important for managing care transitions and understanding medical complexity.
We discuss our proposals for data elements related to the medical condition of pain as standardized patient assessment data. Appropriate pain management begins with a standardized assessment, and thereafter establishing and implementing an overall plan of care that is person-centered, multi-modal, and includes the treatment team and the patient. Assessing and documenting the effect of pain on sleep, participation in therapy, and other activities may provide information on undiagnosed conditions and comorbidities and the level of care required, and do so more objectively than subjective numerical scores. With that, we assess that taken separately and together, these proposed data elements are essential for care planning, consistency across transitions of care, and identifying medical complexities including undiagnosed conditions. We also conclude that it is the standard of care to always consider the risks and benefits associated with a personalized care plan, including the risks of any pharmacological therapy, especially opioids.[843] We also conclude that in addition to assessing and appropriately treating pain through the optimum mix of pharmacologic, non-pharmacologic, and alternative therapies, while being cognizant of current prescribing guidelines, clinicians in partnership with patients are best able to mitigate factors that contribute to the current opioid crisis.[844 845 846]
In alignment with our Meaningful Measures Initiative, accurate assessment of medical conditions and comorbidities of patients and residents in PAC is expected to make care safer by reducing harm caused in the delivery of care; promote effective prevention and treatment of chronic disease; strengthen person and family engagement as partners in their care; and promote effective communication and coordination of care. The SPADEs will enable or support clinical decision-making and early clinical intervention; person-centered, high quality care through: Facilitating better care continuity and coordination; better data exchange and interoperability between settings; and longitudinal outcome analysis. Therefore, reliable data elements assessing medical conditions and comorbidities are needed in order to initiate a management program that can optimize a patient or resident's prognosis and reduce the possibility of adverse events.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19540 through 19542), we invited comment that apply specifically to the standardized patient assessment data for the category of medical conditions and comorbidities, specifically on:
- Pain Interference (Pain Effect on Sleep, Pain Interference With Therapy Activities, and Pain Interference With Day-to-Day Activities)
In acknowledgement of the opioid crisis, we specifically sought comment on whether or not we should add these pain items in light of those concerns. Commenters were asked to address to what extent the collection of the SPADES described in this final rule through patient queries might encourage providers to prescribe opioids.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19541 through 19542), we proposed that a set of three data elements on the topic of Pain Interference (Pain Effect on Sleep, Pain Interference With Therapy Activities, and Pain Interference With Day-to-Day Activities) meet the definition of standardized patient assessment data with respect to medical condition and comorbidity data under section 1899B(b)(1)(B)(iv) of the Act.
The practice of pain management began to undergo significant changes in the 1990s because the inadequate, non-standardized, non-evidence-based assessment and treatment of pain became a public health issue.[847] In pain management, a critical part of providing comprehensive care is performance of a thorough initial evaluation, including assessment of both the medical and any biopsychosocial factors causing or contributing to the pain, with a treatment plan to address the causes of pain and to manage pain that persists over time.[848] Quality pain management, based on current guidelines and evidence-based practices, can minimize unnecessary opioid prescribing both by offering alternatives or supplemental treatment to opioids and by clearly stating when they may be appropriate, and how to utilize risk-benefit analysis for opioid and non-opioid treatment modalities.[849]
Pain is a common symptom in PAC patients and residents, where healing, recovery, and rehabilitation often require regaining mobility and other functions after an acute event. Standardized assessment of pain that interferes with function is an important first step towards appropriate pain management in PAC settings. The National Pain Strategy called for refined assessment items on the topic of pain, and describes the need for these improved measures to be implemented in PAC assessments.[850] Further, the focus on pain interference, as opposed to pain intensity or pain frequency, was supported by the TEP convened by our data element contractor as an appropriate and actionable metric for assessing pain. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We appreciate the important concerns related to the misuse and overuse of opioids in the treatment of pain and to that end, we note that in the proposed rule we also proposed a SPADE that assesses for the use of, as well as importantly the indication for the use of, high-risk drugs, including opioids. Further, in the FY 2017 IPPS/LTCH PPS final rule (81 FR 57193), we adopted the Drug Regimen Review Conducted With Follow-Up for Identified Issues-Post Acute Care (PAC) Long-Term Care Hospital (LTCH) Quality Reporting Program (QRP) measure which assesses whether PAC providers were responsive to potential or actual clinically significant medication issue(s), which includes issues associated with use and misuse of opioids for pain management, when such issues were identified.
We also note that the SPADEs related to pain assessment are not associated with any particular approach to management. Since the use of opioids is associated with serious complications, particularly in the elderly,[851 852 853] an array of successful non-pharmacologic and non-opioid approaches to pain management may be considered. PAC providers have historically used a range of pain management strategies, including non-steroidal anti-inflammatory drugs, ice, transcutaneous electrical nerve stimulation (TENS) therapy, supportive devices, acupuncture, and the like. In addition, non-pharmacological interventions for pain management include, but are not limited to, biofeedback, application of heat/cold, massage, physical therapy, nerve block, stretching and strengthening exercises, chiropractic, electrical stimulation, radiotherapy, and ultrasound.[854 855 856]
We believe that standardized assessment of pain interference will support PAC clinicians in applying best-practices in pain management for chronic and acute pain, consistent with current clinical guidelines. For example, the standardized assessment of both opioids and pain interference would support providers in successfully tapering patients/residents who arrive in the PAC setting with long-term opioid use off of opioids onto non-pharmacologic treatments and non-opioid medications, as recommended by the Society for Post-Acute and Long-Term Care Medicine,[857] and consistent with HHS' 5-Point Strategy To Combat the Opioid Crisis [858] which includes “Better Pain Management.”
The Pain Interference data element set consists of three data elements: Pain Effect on Sleep, Pain Interference with Therapy Activities, and Pain Interference with Day-to-Day Activities. Pain Effect on Sleep assesses the frequency with which pain effects a patient's sleep. Pain Interference with Therapy Activities assesses the frequency with which pain interferes with a patient's ability to participate in therapies. Pain Interference with Day-to-Day Activities assesses the extent to which pain interferes with a patient's ability to participate in day-to-day activities excluding therapy.
A similar data element on the effect of pain on activities is currently included in the OASIS. A similar data element on the effect on sleep is currently included in the MDS instrument. For more information on the Pain Interference data elements, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We sought public input on the relevance of conducting assessments on pain and specifically on the larger set of Pain Interview data elements included in the National Beta Test. The proposed data elements were supported by comments from the TEP meeting held by our data element contractor on April 7 to 8, 2016. The TEP affirmed the feasibility and clinical utility of pain as a concept in a standardized assessment. The TEP agreed that data elements on pain interference with ability to participate in therapies versus other activities should be addressed. Further, during a more recent convening of the same TEP on September 17, 2018, the TEP supported the interview-based pain data elements included in the National Beta Test. The TEP members were particularly supportive of the items that focused on how pain interferes with activities (that is, Pain Interference data elements), because understanding the extent to which pain interferes with function would enable clinicians to determine the need for appropriate pain treatment. A summary of the September 17, 2018 TEP meeting titled “SPADE Technical Expert Panel Summary (Third Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We held a public input period in 2016 to solicit feedback on the standardization of pain and several other items that were under development in prior efforts. From the prior public comment period, we included several pain data elements (Pain Effect on Sleep; Pain Interference—Therapy Activities; Pain Interference—Other Activities) in a second call for public input, open from April 26 to June 26, 2017. The items we sought comment on were modified from all stakeholder and test efforts. Commenters provided general comments about pain assessment in general in addition to feedback on the specific pain items. A few commenters shared their support for assessing pain, the potential for pain assessment to improve the quality of care, and for the validity and reliability of the data elements. Commenters affirmed that the item of pain and the effect on sleep would be suitable for PAC settings. Commenters' main concerns included redundancy with existing data elements, feasibility and utility for cross-setting use, and the applicability of interview-based items to patients and residents with cognitive or communication impairments, and deficits. A summary report for the April 26 to June 26, 2017 public comment period titled “SPADE May-June 2017 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Pain Interference data elements were included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Pain Interference data elements to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Pain Interference data elements in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. In addition, a commenter expressed strong support for the Pain data elements and was encouraged by the fact that this portion of the assessment goes beyond merely measuring the presence of pain. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for the effect of pain on function, stakeholder input, and strong test results, we proposed that the three data elements (Pain Effect on Sleep, Pain Interference with Therapy Activities, and Pain Interference with Day-to-Day Activities) that comprise the set of Pain Interference data elements meet the definition of standardized patient assessment data with respect to medical conditions and comorbidities under section 1899B(b)(1)(B)(iv) of the Act, and to adopt the Pain Interference data elements as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters noted support for the Pain Interference SPADEs, noting that these SPADEs will provide a useful and more accurate assessment of a patient's ability to function, and that understanding the impact of pain on therapy and other activities, including sleep, can improve the quality of care, which in turn will support providers in their ability to provide effective pain management services.
Response: We thank the commenters for their support of the Pain Interference SPADEs.
Comment: A commenter noted that the proposed Pain Interference SPADEs document pain frequency but stated that it is important to identify both pain frequency and pain intensity.
Response: We wish to clarify that the Pain Interference SPADEs are interview data elements that ask the patient the frequency with which pain interferes with sleep, therapy, or non-therapy activities. These data elements therefore combine the concepts of frequency and intensity, with the measure of intensity being interference with the named activities. Self-reported measures of pain intensity are often criticized for being infeasible to standardize. In these data elements, interference with activities is an alternative to asking about intensity.
Comment: A commenter expressed concern about the suitability of the Pain Interference SPADEs for use in patients with cognitive and communication deficits and suggested CMS consider the use of non-verbal means to allow patients to respond to SPADEs related to pain.
Response: We appreciate the commenter's concern surrounding pain assessment with patients with cognitive and communication deficits. The Pain Interference SPADEs require that a patient be able to communicate, whether verbally, in writing, or using another method. Assessors may use non-verbal means to administer the questions (for example, providing the questions and response in writing for a patient with severe hearing impairment). Patients who are unable to communicate by any means would not be required to complete the Pain Interference SPADEs. However, evidence suggests that pain presence can be reliably assessed through structural observational protocols. To that end, we tested observational pain presence elements in the National Beta Test, but have chosen not to propose those data elements as SPADEs at this time, out of consideration of the scale of additions and changes that would be required of PAC providers. We will take the commenters' concern into consideration as the SPADEs are monitored and refined in the future.
Comment: A commenter expressed concerns about how CMS might use these data elements, noting particular concern that collection of these SPADEs may inappropriately translate into an assessment of quality, and that data collection on this topic could create incentives that directly or indirectly interfere with treatment decisions.
Response: We appreciate the commenter's concern related to wanting to understand how we will use the SPADEs. It is our intention, as delineated by the IMPACT Act, to use the SPADE data to inform care planning, the common standards and definitions to facilitate interoperability, and to allow for comparing assessment data for standardized measures. We will continue to communicate and collaborate with stakeholders about how the SPADEs will be used in the LTCH QRP, as those plans are established, by soliciting input during the development process and establishing use of the SPADEs in quality programs through future rulemaking.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Pain Interference data elements (Pain Effect on Sleep, Pain Interference with Therapy Activities, and Pain Interference with Day-to-Day Activities) as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
e. Impairment Data
Hearing and vision impairments are conditions that, if unaddressed, affect activities of daily living, communication, physical functioning, rehabilitation outcomes, and overall quality of life. Sensory limitations can lead to confusion in new settings, increase isolation, contribute to mood disorders, and impede accurate assessment of other medical conditions. Failure to appropriately assess, accommodate, and treat these conditions increases the likelihood that patients will require more intensive and prolonged treatment. Onset of these conditions can be gradual, so individualized assessment with accurate screening tools and follow-up evaluations are essential to determining which patients need hearing- or vision-specific medical attention or assistive devices and accommodations, including auxiliary aids and/or services, and to ensure that person-directed care plans are developed to accommodate a patient's or resident's needs. Accurate diagnosis and management of hearing or vision impairment would likely improve rehabilitation outcomes and care transitions, including transition from institutional-based care to the community. Accurate assessment of hearing and vision impairment would be expected to lead to appropriate treatment, accommodations, including the provision of auxiliary aids and services during the stay, and ensure that patients continue to have their vision and hearing needs met when they leave the facility.
In alignment with our Meaningful Measures Initiative, we expect accurate individualized assessment, treatment, and accommodation of hearing and vision impairments of patients and residents in PAC to make care safer by reducing harm caused in the delivery of care; promote effective prevention and treatment of chronic disease; strengthen person and family engagement as partners in their care; and promote effective communication and coordination of care. For example, standardized assessment of hearing and vision impairments used in PAC will support ensuring patient safety (for example, risk of falls), identifying accommodations needed during the stay, and appropriate support needs at the time of discharge or transfer. Standardized assessment of these data elements will enable or support clinical decision-making and early clinical intervention; person-centered, high quality care (for example, facilitating better care continuity and coordination); better data exchange and interoperability between settings; and longitudinal outcome analysis. Therefore, reliable data elements assessing hearing and vision impairments are needed to initiate a management program that can optimize a patient or resident's prognosis and reduce the possibility of adverse events.
• Hearing
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19543 through 19544), we proposed that the Hearing data element meets the definition of standardized patient assessment data with respect to impairments data under section 1899B(b)(1)(B)(v) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20114 through 20115), accurate assessment of hearing impairment is important in the PAC setting for care planning and resource use. Hearing impairment has been associated with lower quality of life, including poorer physical, mental, and social functioning, and emotional health.[859 860] Treatment and accommodation of hearing impairment led to improved health outcomes, including but not limited to quality of life.[861] For example, hearing loss in elderly individuals has been associated with depression and cognitive impairment,[862 863 864] higher rates of incident cognitive impairment and cognitive decline,[865] and less time in occupational therapy.[866] Accurate assessment of hearing impairment is important in the PAC setting for care planning and defining resource use.
The proposed data element consists of the single Hearing data element. This data consists of one question that assesses level of hearing impairment. This data element is currently in use in the MDS in SNFs. For more information on the Hearing data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Hearing data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20114 through 20115). In that proposed rule, we stated that the proposal was informed by input we received on the PAC PRD form of the data element (“Ability to Hear”) through a call for input published on the CMS Measures Management System Blueprint website. Input submitted from August 12 to September 12, 2016 recommended that hearing, vision, and communication assessments be administered at the beginning of patient assessment process. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received public comments in support of the Hearing data element as well as concerns about not having recent, comprehensive field testing of proposed data elements. Commenters were supportive of adopting the Hearing data element for standardized cross-setting use, noting that it would help address the needs of patient and residents with disabilities and that failing to identify impairments during the initial assessment can result in inaccurate diagnoses of impaired language or cognition and can invalidate other information obtained from patient assessment.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Hearing data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Hearing data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Hearing data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on January 5 and 6, 2017 for the purpose of soliciting input on all the SPADEs, including the Hearing data element. The TEP affirmed the importance of standardized assessment of hearing impairment in PAC patients and residents. A summary of the January 5 and 6, 2017 TEP meeting titled “SPADE Technical Expert Panel Summary (Second Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. In addition, a commenter expressed support for the Hearing data element and suggested administration at the beginning of the patient assessment to maximize utility. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for hearing, stakeholder input, and strong test results, we proposed that the Hearing data element meets the definition of standardized patient assessment data with respect to impairments under section 1899B(b)(1)(B)(v) of the Act, and to adopt the Hearing data element as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters supported the collection of information on hearing impairment, with some noting that LTCHs are already collecting similar information. One of these commenters also suggested that CMS consider how hearing impairment impacts a patient's ability to respond to the assessment tool in general. Another of these commenters noted that collecting this data at admission only is a logical approach since a patient's hearing impairment status is unlikely to change during an LTCH admission.
Response: We thank the commenters for their support of the Hearing data element and support for the collection of hearing at admission. Concerning how hearing impairment affects a patient's ability to respond to the assessment overall, we offer guidance and recommendations through our CMS LTCH QRP Manual. Coding tips and steps for assessment direct assessors to take appropriate steps to accommodate sensory and communication impairments when conducting the assessment, so as to minimize the impact of a patient's impairment on their responses or ability to participate in the full assessment. For example, in the coding tips for BB0700, Expression of Ideas and Wants, the CMS LTCH QRP Manual states: “Assess using the patient's preferred language.” And “Interact with the patient. Be sure he or she can hear you or has access to his or her preferred method for communication, such as an electronic device or paper and pencil. If appropriate, be sure he or she has access to his or her hearing aid or hearing appliance and glasses or other visual appliances. If appropriate, offer alternative means of communication such as an electronic device (smart phone, tablet, laptop, etc.), writing, pointing, nodding, or using cue cards.”
Comment: A commenter stated that the rate of hearing impairment as measured by the Hearing SPADE occurs too infrequently to provide information that would benefit LTCH patients.
Response: Based on findings from the National Beta Test, although the level of PAC patients/residents who were assessed as “Highly Impaired” was 1 percent, an additional 8 percent were assessed to have “Moderate difficulty” and 17 percent were assessed to have “Minimal difficulty” with Hearing. These results are provided in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html. The Hearing SPADE consists of one data element completed by the assessor based primarily on interacting with the patient and reviewing the medical record. Given the low burden of reporting the Hearing data element, and despite severe hearing impairment occurring in a small proportion of LTCH patients, we believe it is important to systematically assess for hearing impairment to improve clinical care and care transitions.
Comment: A commenter recommended adding “unable to assess” as a response option, which the commenter believes would be the appropriate choice if the patient is comatose or is unable to effectively answer questions related to an assessment of their hearing.
Response: We appreciate the commenter's recommendation. The assessment of hearing is completed based on observing the patient during assessment, patient interactions with others, reviewing medical record documentation, and consulting with patient's family and other staff, in addition to interviewing the patient. Therefore, the assessment can be completed when the patient is unable to effectively answer questions related to an assessment of their hearing.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Hearing data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
• Vision
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19544 through 19545), we proposed that the Vision data element meets the definition of standardized patient assessment data with respect to impairments under section 1899B(b)(1)(B)(v) of the Act.
As described in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20115 through 20116), evaluation of an individual's ability to see is important for assessing for risks such as falls and provides opportunities for improvement through treatment and the provision of accommodations, including auxiliary aids and services, which can safeguard patients and improve their overall quality of life. Further, vision impairment is often a treatable risk factor associated with adverse events and poor quality of life. For example, individuals with visual impairment are more likely to experience falls and hip fracture, have less mobility, and report depressive symptoms.[867 868 869 870 871 872 873] Individualized initial screening can lead to life-improving interventions such as accommodations, including the provision of auxiliary aids and services, during the stay and/or treatments that can improve vision and prevent or slow further vision loss. In addition, vision impairment is often a treatable risk factor associated with adverse events which can be prevented and accommodated during the stay. Accurate assessment of vision impairment is important in the LTCH setting for care planning and defining resource use.
The proposed data element consists of the single Vision data element (Ability To See in Adequate Light) that consists of one question with five response categories. The Vision data element that we proposed for standardization was tested as part of the development of the MDS and is currently in use in that assessment in SNFs. Similar data elements, but with different wording and fewer response option categories, are in use in the OASIS. For more information on the Vision data element, we refer readers to the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
The Vision data element was first proposed as a SPADE in the FY 2018 IPPS/LTCH PPS proposed rule (82 FR 20115 through 20116). In that proposed rule, we stated that the proposal was informed by input we received on the Ability to See in Adequate Light data element (version tested in the PAC PRD with three response categories) through a call for input published on the CMS Measures Management System Blueprint website. Although the data element on which we solicited input differed from the proposed data element, input submitted from August 12 to September 12, 2016 supported the assessment of vision in PAC settings and the useful information such a vision data element would provide. The commenters stated that the Ability to See item would provide important information that would facilitate care coordination and care planning, and consequently improve the quality of care. Other commenters suggested it would be helpful as an indicator of resource use and noted that the item would provide useful information about the abilities of patients and residents to care for themselves. Additional commenters noted that the item could feasibly be implemented across PAC providers and that its kappa scores from the PAC PRD support its validity. Some commenters noted a preference for MDS version of the Vision data element over the form put forward in public comment, citing the widespread use of this data element. A summary report for the August 12 to September 12, 2016 public comment period titled “SPADE August 2016 Public Comment Summary Report” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In response to our proposal in the FY 2018 IPPS/LTCH PPS proposed rule, we received comments in support of the Vision data element as well as concerns about not having recent, comprehensive field testing of proposed data elements. Commenters supported addressing the needs of persons with disabilities and noted the importance of the Vision data element because unaddressed impairments during the initial assessment can result in inaccurate diagnoses of impaired language or cognition and can invalidate other information obtained from the patient assessment. Commenters recommended that hearing, vision, and communication assessments be administered at the beginning of the patient assessment process. A commenter expressed concern that the Ability to See data element would not capture all aspects of functional vision—that is, the person's ability to use vision to complete daily activities and participate in environments—because it fails to assess visual field and low contract visual acuity.
Subsequent to receiving comments on the FY 2018 IPPS/LTCH PPS proposed rule, the Vision data element was included in the National Beta Test of candidate data elements conducted by our data element contractor from November 2017 to August 2018. Results of this test found the Vision data element to be feasible and reliable for use with PAC patients and residents. More information about the performance of the Vision data element in the National Beta Test can be found in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In addition, our data element contractor convened a TEP on January 5 and 6, 2017 for the purpose of soliciting input on all the SPADEs, including the Vision data element. The TEP affirmed the importance of standardized assessment of vision impairment in PAC patients and residents. A summary of the January 5 and 6, 2017 TEP meeting titled “SPADE Technical Expert Panel Summary (Second Convening)” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We also held Special Open Door Forums and small-group discussions with PAC providers and other stakeholders in 2018 for the purpose of updating the public about our ongoing SPADE development efforts. Finally, on November 27, 2018, our data element contractor hosted a public meeting of stakeholders to present the results of the National Beta Test and solicit additional comments. General input on the testing and item development process and concerns about burden were received from stakeholders during this meeting and via email through February 1, 2019. In addition, a commenter expressed support for the Vision data element and suggested administration at the beginning of the patient assessment to maximize utility. A summary of the public input received from the November 27, 2018 stakeholder meeting titled “Input on Standardized Patient Assessment Data Elements (SPADEs) Received After November 27, 2018 Stakeholder Meeting” is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Taking together the importance of assessing for vision, stakeholder input, and strong test results, we proposed that the Vision data element meets the definition of standardized patient assessment data with respect to impairments under section 1899B(b)(1)(B)(v) of the Act, and to adopt the Vision data element as standardized patient assessment data for use in the LTCH QRP.
Comment: Several commenters supported the collection of information on vision impairment. Some commenters noted that LTCHs are already collecting similar information.
Response: We thank the commenters for their support of the Vision data element. To the extent that LTCHs are already collecting similar information, we hope that it will be possible to integrate the Vision SPADE into the existing workflow.
Comment: A commenter recommended that a doctor of optometry should play a lead role in conducting vision assessments, and that vision assessments done by other clinicians should also obtain the patient's own assessment of his or her vision, such as used by the Centers for Disease Control and Prevention (CDC) Behavioral Risk Factors Surveillance System survey, which asks patients “Do you have serious difficulty seeing, even when wearing glasses?” This commenter expressed concerns about the proposed SPADE being subjective and risks of mis-categorizing patients.
Response: We appreciate the commenter's recommendation about how to assess for vision impairment. We do not require that a certain type of clinician complete assessments; the SPADEs have been developed so that any clinician who is trained in the administration of the assessment will be able to administer it correctly. This data element relies on the assessor's evaluation of the patient's vision, which has the advantage of reducing burden placed on the patient. We will take the recommendation to use patient-reported vision impairment assessment into consideration in the development of future assessments.
Comment: A commenter also recommended that CMS require vision assessment at discharge, noting that vision impairment could be related to challenges in medication management and compliance with written follow-up instructions for care.
Response: We appreciate the commenter's recommendation. We agree that adequate vision—or the accommodations and assistive technology needed to compensate for vision impairment—is important to patient safety in the community, in part for the reasons the commenter mentions. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19544 through 19545), we proposed that LTCHs that submitted the Vision SPADE with respect to admission will be deemed to have submitted with respect to both admission and discharge, as there is a low likelihood that the assessment of this SPADE at admission would differ from the assessment at discharge. Vision assessment, collected via the Vision SPADE, will provide information that will support the patient's care while in the LTCH. We also contend that significant clinical changes to a patient's vision will be documented in the medical record as part of routine clinical practice. We note that during the discharge planning process, it is incumbent on LTCH providers to make reasonable assurances that the patient's needs will be met in the next care setting, including in the home.
Comment: A commenter recommended adding “unable to assess” as a response option, which the commenter believes would be the appropriate choice if a patient is comatose or is unable to effectively answer questions related to an assessment of their vision.
Response: We appreciate the commenter's recommendation. However, the assessment of vision is completed based on consulting with patient's family and other staff, observing the patient including asking the patient to read text or examine pictures or numbers in addition to interviewing the patient about their vision abilities. These other sources/methods can be used to complete the assessment of vision when the patient is unable to effectively answer questions related to an assessment of their vision.
Comment: A commenter stated that the rate of vision impairment as measured by the Vision SPADE occurs too infrequently to provide information that would benefit LTCH patients.
Response: Based on findings from the National Beta Test. Although the level of PAC patients/residents who were assessed as “Severely Impaired” and “Highly Impaired” was 1 percent, respectively, an additional four percent were assessed to “Moderately impaired” and 16 percent were assessed to be “Impaired”. These results are provided in the document titled “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html . The Vision SPADE consists of one data element completed by the assessor based primarily on interacting with the patient and reviewing the medical record. Given the low burden of the Vision data element, and despite severe vision impairment occurring in a small proportion of LTCH patients, we believe it is important to systematically assess for vision impairment to improve clinical care and care transitions.
Comment: A commenter noted that assessment through the vision data element is just an initial step towards a care coordination system that recognizes the impact that eye health has on overall health outcomes. This commenter noted that a critical next step would be to ensure that patients get to the physician who can address their eye health needs.
Response: We appreciate the commenter's recommendation and we agree that screening for vision impairment is an initial step towards ensuring patients receive the care they need. We expect LTCH providers to provide a standard of care to patients, and we defer to the clinical judgement of the patient's care team to determine when further assessment of vision or eye-related issues is warranted.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Vision data element as standardized patient assessment data beginning with the FY 2022 LTCH QRP as proposed.
f. New Category: Social Determinants of Health
(1) Social Determinants of Health Data Collection To Inform Measures and Other Purposes
Subparagraph (A) of section 2(d)(2) of the IMPACT Act requires CMS to assess appropriate adjustments to quality measures, resource measures, and other measures, and to assess and implement appropriate adjustments to payment under Medicare, based on those measures, after taking into account studies conducted by ASPE on social risk factors (described in this final rule) and other information, and based on an individual's health status and other factors. Subparagraph (C) of section 2(d)(2) of the IMPACT Act further requires the Secretary to carry out periodic analyses, at least every 3 years, based on the factors referred to subparagraph (A) so as to monitor changes in possible relationships. Subparagraph (B) of section 2(d)(2) of the IMPACT Act requires CMS to collect or otherwise obtain access to data necessary to carry out the requirement of the paragraph (both assessing adjustments previously described in such subparagraph (A) and for periodic analyses in such subparagraph (C)). Accordingly, we proposed to use our authority under subparagraph (B) of section 2(d)(2) of the IMPACT Act to establish a new data source for information to meet the requirements of subparagraphs (A) and (C) of section 2(d)(2) of the IMPACT Act. In the proposed rule, we proposed to collect and access data about social determinants of health (SDOH) to perform CMS' responsibilities under subparagraphs (A) and (C) of section 2(d)(2) of the IMPACT Act, as explained in more detail in this final rule. Social determinants of health, also known as social risk factors, or health-related social needs, are the socioeconomic, cultural and environmental circumstances in which individuals live that impact their health. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19545 through 19552), we proposed to collect information on seven proposed SDOH SPADEs relating to race, ethnicity, preferred language, interpreter services, health literacy, transportation, and social isolation; a detailed discussion of each of the proposed SDOH data elements is found in section VIII.C.7.f.(2) of the preamble of this final rule.
We also proposed to use the assessment instrument for the LTCH QRP, the LCDS, described as a PAC assessment instrument under section 1899B(a)(2)(B) of the Act, to collect these data via an existing data collection mechanism. We believe this approach will provide CMS with access to data with respect to the requirements of section 2(d)(2) of the IMPACT Act, while minimizing the reporting burden on PAC health care providers by relying on a data reporting mechanism already used and an existing system to which PAC health care providers are already accustomed.
The IMPACT Act includes several requirements applicable to the Secretary, in addition to those imposing new data reporting obligations on certain PAC providers as discussed in section VIII.C.7.f.(2) of the preamble of this final rule. Subparagraphs (A) and (B) of section 2(d)(1) of the IMPACT Act require the Secretary, acting through the Office of the Assistant Secretary for Planning and Evaluation (ASPE), to conduct two studies that examine the effect of risk factors, including individuals' socioeconomic status, on quality, resource use and other measures under the Medicare program. The first ASPE study was completed in December 2016 and is discussed in this final rule, and the second study is to be completed in the fall of 2019. We recognize that ASPE, in its studies, is considering a broader range of social risk factors than the SDOH data elements in this proposal, and address both PAC and non-PAC settings. We acknowledge that other data elements may be useful to understand, and that some of those elements may be of particular interest in non-PAC settings. For example, for beneficiaries receiving care in the community, as opposed to an in-patient facility, housing stability and food insecurity may be more relevant. We will continue to take into account the findings from both of ASPE's reports in future policy making. We also intend to review SDOH data elements across our programs and the industry to harmonize and align in instances where it is appropriate.
One of the ASPE's first actions under the IMPACT Act was to commission the National Academies of Sciences, Engineering, and Medicine (NASEM) to define and conceptualize socioeconomic status for the purposes of ASPE's two studies under section 2(d)(1) of the IMPACT Act. The NASEM convened a panel of experts in the field and conducted an extensive literature review. Based on the information collected, the 2016 NASEM panel report titled, “Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors,” concluded that the best way to assess how social processes and social relationships influence key health-related outcomes in Medicare beneficiaries is through a framework of social risk factors instead of socioeconomic status. Social risk factors discussed in the NASEM report include socioeconomic position, race, ethnicity, gender, social context, and community context. These factors are discussed at length in chapter 2 of the NASEM report, titled “Social Risk Factors.” [874] Consequently NASEM framed the results of its report in terms of “social risk factors” rather than “socioeconomic status” or “sociodemographic status.” The full text of the “Social Risk Factors” NASEM report is available for reading on the website at: https://www.nap.edu/read/21858/chapter/1.
Each of the data elements we proposed to collect and access under our authority under section 2(d)(2)(B) of the IMPACT Act is identified in the 2016 NASEM report as a social risk factor that has been shown to impact care use, cost and outcomes for Medicare beneficiaries. CMS uses the term social determinants of health (SDOH) to denote social risk factors, which is consistent with the objectives of Healthy People 2020.[875]
ASPE issued its first Report to Congress, titled “Social Risk Factors and Performance Under Medicare's Value-Based Purchasing Programs,” under section 2(d)(1)(A) of the IMPACT Act on December 21, 2016.[876] Using NASEM's social risk factors framework, ASPE focused on the following social risk factors, in addition to disability: (1) Dual enrollment in Medicare and Medicaid as a marker for low income, (2) residence in a low-income area, (3) Black race, (4) Hispanic ethnicity, and; (5) residence in a rural area. ASPE acknowledged that the social risk factors examined in its report were limited due to data availability. The report also noted that the data necessary to meaningfully attempt to reduce disparities and identify and reward improved outcomes for beneficiaries with social risk factors have not been collected consistently on a national level in post-acute care settings. Where these data have been collected, the collection frequently involves lengthy questionnaires. More information on the Report to Congress on Social Risk Factors and Performance under Medicare's Value-Based Purchasing Programs, including the full report, is available on the website at: https://aspe.hhs.gov/social-risk-factors-and-medicares-value-based-purchasing-programs-reports.
Section 2(d)(2) of the IMPACT Act relates to CMS activities and imposes several responsibilities on the Secretary relating to quality, resource use, and other measures under Medicare. As mentioned previously, under subparagraph (A) of section 2(d)(2) of the IMPACT Act, the Secretary is required, on an ongoing basis, taking into account the ASPE studies and other information, and based on an individual's health status and other factors, to assess appropriate adjustments to quality, resource use, and other measures, and to assess and implement appropriate adjustments to Medicare payments based on those measures. Section 2(d)(2)(A)(i) of the IMPACT Act applies to measures adopted under subsections (c) and (d) of section 1899B of the Act and to other measures under Medicare. However, CMS' ability to perform these analyses, and assess and make appropriate adjustments is hindered by limits of existing data collections on SDOH data elements for Medicare beneficiaries. In its first study in 2016, in discussing the second study, ASPE noted that information relating to many of the specific factors listed in the IMPACT Act, such as health literacy, limited English proficiency, and Medicare beneficiary activation, are not available in Medicare data.
Subparagraph 2(d)(2)(A) of the IMPACT Act specifically requires the Secretary to take the studies and considerations from ASPE's reports to Congress, as well as other information as appropriate, into account in assessing and implementing adjustments to measures and related payments based on measures in Medicare. The results of the ASPE's first study demonstrated that Medicare beneficiaries with social risk factors tended to have worse outcomes on many quality measures, and providers who treated a disproportionate share of beneficiaries with social risk factors tended to have worse performance on quality measures. As a result of these findings, ASPE suggested a three-pronged strategy to guide the development of value-based payment programs under which all Medicare beneficiaries receive the highest quality healthcare services possible. The three components of this strategy are to: (1) Measure and report quality of care for beneficiaries with social risk factors; (2) set high, fair quality standards for care provided to all beneficiaries; and (3) reward and support better outcomes for beneficiaries with social risk factors. In discussing how measuring and reporting quality for beneficiaries with social risk factors can be applied to Medicare quality payment programs, the report offered nine considerations across the three-pronged strategy, including enhancing data collection and developing statistical techniques to allow measurement and reporting of performance for beneficiaries with social risk factors on key quality and resource use measures.
Congress, in section 2(d)(2)(B) of the IMPACT Act, required the Secretary to collect or otherwise obtain access to the data necessary to carry out the provisions of paragraph (2) of section 2(d) of the IMPACT Act through both new and existing data sources. Taking into consideration NASEM's conceptual framework for social risk factors previously discussed, ASPE's study, and considerations under section 2(d)(1)(A) of the IMPACT Act, as well as the current data constraints of ASPE's first study and its suggested considerations, we proposed to collect and access data about SDOH under section 2(d)(2) of the IMPACT Act. Our collection and use of the SDOH data described in section VIII.C.7.f.(1) of the preamble of this final rule, under section 2(d)(2) of the IMPACT Act, would be independent of our proposal discussed in this final rule (in section VIII.C.7.f.(2) of the preamble of this final rule) and our authority to require submission of that data for use as SPADE under section 1899B(a)(1)(B) of the Act.
Accessing standardized data relating to the SDOH data elements on a national level is necessary to permit CMS to conduct periodic analyses, to assess appropriate adjustments to quality measures, resource use measures, and other measures, and to assess and implement appropriate adjustments to Medicare payments based on those measures. We agree with ASPE's observations, in the value-based purchasing context, that the ability to measure and track quality, outcomes, and costs for beneficiaries with social risk factors over time is critical as policymakers and providers seek to reduce disparities and improve care for these groups. Collecting the data as proposed will provide the basis for our periodic analyses of the relationship between an individual's health status and other factors and quality, resource use, and other measures, as required by section 2(d)(2) of the IMPACT Act, and to assess appropriate adjustments. These data will also permit us to develop the statistical tools necessary to maximize the value of Medicare data, reduce costs and improve the quality of care for all beneficiaries. Collecting and accessing SDOH data in this way also supports the three-part strategy put forth in the first ASPE report, specifically ASPE's consideration to enhance data collection and develop statistical techniques to allow measurement and reporting of performance for beneficiaries with social risk factors on key quality and resource use measures.
For the reasons previously discussed, in the proposed rule we proposed under section 2(d)(2) of the IMPACT Act, to collect the data on the following SDOH: (1) Race, as discussed in section VIII.C.7.f.(2)(a) of the preamble of this final rule; (2) Ethnicity, as discussed in section VIII.C.7.f.(2)(a) of the preamble of this final rule; (3) Preferred Language, as discussed in section VIII.C.7.f.(2)(b) of the preamble of this final rule; (4) Interpreter Services as discussed in section VIII.C.7.f.(2)(b) of the preamble of this final rule; (5) Health Literacy, as discussed in section VIII.C.7.f.(2)(c) of the preamble of this final rule; (6) Transportation, as discussed in section VIII.C.7.f.(2)(d) of the preamble of this final rule; and (7) Social Isolation, as discussed in section VIII.C.7.f.(2)(e) of the preamble of this final rule. These data elements are discussed in more detail in this section VIII.C.7.f.(2) of the preamble of this final rule. A discussion of the comments we received, along with our responses, is included in each section.
(2) Standardized Patient Assessment Data
Section 1899B(b)(1)(B)(vi) of the Act authorizes the Secretary to collect SPADEs with respect to other categories deemed necessary and appropriate. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19547 through 19552), we proposed to create a Social Determinants of Health SPADE category under section 1899B(b)(1)(B)(vi) of the Act. In addition to collecting SDOH data for the purposes previously outlined under section 2(d)(2)(B) of the IMPACT Act, in the proposed rule we also proposed to collect as SPADE these same data elements (race, ethnicity, preferred language, interpreter services, health literacy, transportation, and social isolation) under section 1899B(b)(1)(B)(vi) of the Act. We believe that this proposed new category of Social Determinants of Health will inform provider understanding of individual patient risk factors and treatment preferences, facilitate coordinated care and care planning, and improve patient outcomes. We proposed to deem this category necessary and appropriate, for the purposes of SPADE, because using common standards and definitions for PAC data elements is important in ensuring interoperable exchange of longitudinal information between PAC providers and other providers to facilitate coordinated care, continuity in care planning, and the discharge planning process from post-acute care settings.
All of the Social Determinants of Health data elements we proposed under section 1899B(b)(1)(B)(vi) of the Act have the capacity to take into account treatment preferences and care goals of patients and to inform our understanding of patient complexity and risk factors that may affect care outcomes. While acknowledging the existence and importance of additional SDOH, we proposed to assess some of the factors relevant for patients receiving post-acute care that PAC settings are in a position to impact through the provision of services and supports, such as connecting patients with identified needs with transportation programs, certified interpreters, or social support programs.
We proposed to adopt the following seven data elements as SPADE under the proposed Social Determinants of Health category: Race, ethnicity, preferred language, interpreter services, health literacy, transportation, and social isolation. To select these data elements, we reviewed the research literature, a number of validated assessment tools and frameworks for addressing SDOH currently in use (for example, Health Leads,[877] NASEM, Protocol for Responding to and Assessing Patients' Assets, Risks, and Experiences (PRAPARE), and ICD-10), and we engaged in discussions with stakeholders. We also prioritized balancing the reporting burden for PAC providers with our policy objective to collect SPADEs that will inform care planning and coordination and quality improvement across care settings. Furthermore, incorporating SDOH data elements into care planning has the potential to reduce readmissions and help beneficiaries achieve and maintain their health goals.
We also considered feedback received during a listening session that we held on December 13, 2018. The purpose of the listening session was to solicit feedback from health systems, research organizations, advocacy organizations and state agencies, and other members of the public on collecting patient-level data on SDOH across care settings, including consideration of race, ethnicity, spoken language, health literacy, social isolation, transportation, sex, gender identity, and sexual orientation. We also gave participants an option to submit written comments. A full summary of the listening session, titled “Listening Session on Social Determinants of Health Data Elements: Summary of Findings,” includes a list of participating stakeholders and their affiliations, and is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
We solicited comment on these proposals.
Commenters submitted the following comments related to the proposed rule's discussion of SDOH SPADEs. A discussion of these comments, along with our responses, appears below.
Comment: A commenter supported the incorporation of SDOH in the LTCH QRP, in the interest of promoting access and assure high-quality care for all beneficiaries. The commenter also encouraged CMS to be mindful of meaningful data collection and the potential impact for data overload. Since SDOH have impacts far beyond the post-acute care setting, the commenter cautioned the collection of data that cannot be readily gathered, shared or replicated beyond the PAC setting.
The commenter also encouraged CMS to consider leveraging data points collected during primary care visits by using social risk factor data captured during those encounters. They pointed out that the ability to have a hospital's or physician's EHR also collect, capture, and exchange segments of this information is powerful. The commenter recommended CMS to take a holistic view of SDOH across the care continuum so that all care settings may gather, collect or leverage this data efficiently and in a way that maximizes its impact.
Response: We thank the commenter for the comment, and we agree that collecting SDOH data elements can be useful in identifying and address health disparities. We also agree that we should be mindful that data elements selected are useful. The proposed SDOH SPADEs are aligned with the SDOH identified in the 2016 NASEM report, which was commissioned by Office of the Assistant Secretary for Planning and Evaluation (ASPE). Regarding the commenter's suggestion that we consider how it can align existing and future SDOH data collection to minimize burden on providers, we agree that it is important to minimize duplication of effort and will take this under advisement for future policy development.
Comment: Many commenters support the inclusion of the seven proposed SDOH data elements on the LTCH CARE Data Set, as they serve populations affected by social determinants. However, they also recommend including additional factors within the SDOH SPADE category to ensure that the full spectrum of social needs is examined. These factors included: Disability status, dual eligibility of beneficiaries, health insurance status, food insecurity, housing insecurity, independent living status, and ability to return to work. Another commenter suggested BMI, smoking status, age, sex, back pain, pain in non-operative lower extremity joint, health risk status, depression/mental health status, chronic narcotic or pre-operative narcotic use, and socioeconomic status as they stated they are relevant to musculoskeletal care. A commenter also suggested that CMS explore family caregiver assessment as a future social risk factor because the health and capability of the family caregiver can have an impact on their health and medical interventions.
The commenters noted that the inclusion of the additional SDOH would provide greater breadth and depth of data and would offer additional support to the Agency when developing policies to address social factors related to health. A commenter noted that disability status is already included in some Medicare risk adjustment. Furthermore, disability is included in risk adjustment across many aspects of the Medicare program. The commenters stated that the ASPE's report to Congress on Social Risk Factors and Medicare's Value-Based Purchasing Programs reported that disability is an independent predictor of poor mental and physical health outcomes, and that individuals with disabilities may receive lower-quality preventive care.
Response: We thank the commenters for the comments and we will take the comments under advisement as we continue to improve and refine the SPADEs. We agree that it is important to understand the needs of patients with disabilities. However, we also want to note that disability status does not need to be added as a SDOH SPADE since disability/functionality is comprehensively assessed as part of the existing patient assessments in order to establish care plans and set health goals to allow the patient to return to the setting in which they are most comfortable. However, as we continue to evaluate SDOH SPADEs, we will keep commenters' feedback in mind and may consider these suggestions in future rulemaking.
Comment: A few commenters recognize the importance of collecting SDOH information, as it is important to ensure that quality of care is assessed fairly for providers. However, they do not support using the information to penalize PAC settings for patient issues. They stated that it is unclear how CMS will utilize the information collected. The commenters request that CMS provide detailed information about how the collected information will be used in assessing PAC settings.
Response: We appreciate the commenters for recognizing that collecting SDOH data elements can be useful in identifying and address health disparities. It is our intention, as delineated by the IMPACT Act, to use the SPADE data to inform care planning, the common standards and definitions to facilitate interoperability, and to allow for comparing assessment data for standardized measures. We will continue to work with stakeholders to promote transparency and support providers who serve vulnerable populations, promote high quality care, and refine and further implement SDOH SPADE. We appreciate the comment on collecting stakeholder feedback before implementing any adjustments to measures based on the SDOH SPADE. Collection of this data will help us in identifying potential disparities, conducting analyses, and assessing whether any adjustments are needed. Any future use of this data would be done transparently, through solicitation of stakeholder feedback, and through future proposals. With regard to the commenter's concerns about penalizing PAC settings for patient issues, we interpret the commenter to be referring to the 2 percent reduction in their annual payment update (APU) for failure to meet the minimum data completion threshold for the LTCH QRP. We do not penalize providers for patient issues. LTCHs must meet the APU minimum data completion threshold of no less than 80 percent of the LCDS assessments having 100 percent completion of the required data elements. Successful completion means that the assessment does not contain non-informative responses, that is, a “dash” for required data elements. Failure to meet the minimum threshold may result in a 2 percent reduction in the LTCH's APU.
Comment: A commenter was encouraged to see CMS propose a new category of SDOH. However, they noted that the proposal is a first step because collection of the information is reliant on paper questionnaires and ICD-10 codes. They encouraged CMS to move to electronic capture of this information to allow for more robust and granular data and recommended CMS move towards harmonization of assessment tools across settings (including LCDS PAC), and define explicit linkages between data capture/representation and terminology standards to allow data aggregation and analysis across populations and systems. They also suggested that CMS consider piloting of SDOH programs through the CMS Innovation Center. They cautioned that CMS must ensure data derived from assessment surveys, and the algorithms used to analyze those data, should be free of bias that exacerbate health disparities. The commenter welcomes the opportunity to work with CMS on piloting innovative solutions for capturing SDOH data and explain our ongoing efforts on improving SDOH data.
Response: We appreciate the comment about electronic capture of data and note that at we offer free software to our providers (LASER for LTCHs) that allows LTCHs to record and transmit required assessment data; this data is submitted to CMS electronically. However, at this time we do not require that providers use EMRs to populate assessment data but note our support of this platform to facilitate interoperability. We further note that through the intent of the IMPACT Act, we have been working to align the assessment instruments. In order to align data capture and terminology standards, we have built the CMS DEL as a public resource aimed at advancing interoperable health information exchange by enabling users to view assessment questions and response options about demographics, medical problems, and other types of health evaluations and their associated health IT standards. The DEL includes a multitude of data elements, including all data elements adopted for use in the quality reporting programs, and not limited to data collected under the IMPACT Act. In the initial version of the DEL (https://del.cms.gov/), assessment questions and response options are mapped to LOINC and SNOMED codes, where feasible. We also recognize the importance of leveraging existing standards, obtaining input from standards setting organizations, and alignment across federal interoperability efforts. We appreciate the comments and we will take them under advisement for future consideration.
(a) Race and Ethnicity
The persistence of racial and ethnic disparities in health and health care is widely documented, including in PAC settings.[878 879 880 881 882] Despite the trend toward overall improvements in quality of care and health outcomes, the Agency for Healthcare Research and Quality, in its National Healthcare Quality and Disparities Reports, consistently indicates that racial and ethnic disparities persist, even after controlling for factors such as income, geography, and insurance.[883] For example, racial and ethnic minorities tend to have higher rates of infant mortality, diabetes and other chronic conditions, and visits to the emergency department, and lower rates of having a usual source of care and receiving immunizations such as the flu vaccine.[884] Studies have also shown that African Americans are significantly more likely than white Americans to die prematurely from heart disease and stroke.[885] However, our ability to identify and address racial and ethnic health disparities has historically been constrained by data limitations, particularly for smaller populations groups such as Asians, American Indians and Alaska Natives, and Native Hawaiians and other Pacific Islanders.[886]
The ability to improve understanding of and address racial and ethnic disparities in PAC outcomes requires the availability of better data. There is currently a Race and Ethnicity data element, collected in the MDS, LCDS, IRF-PAI, and OASIS, that consists of a single question, which aligns with the 1997 Office of Management and Budget (OMB) minimum data standards for federal data collection efforts.[887] The 1997 OMB Standard lists five minimum categories of race: (1) American Indian or Alaska Native; (2) Asian; (3) Black or African American; (4) Native Hawaiian or Other Pacific Islander; (5) and White. The 1997 OMB Standard also lists two minimum categories of ethnicity: (1) Hispanic or Latino; and (2) Not Hispanic or Latino. The 2011 HHS Data Standards requires a two-question format when self-identification is used to collect data on race and ethnicity. Large federal surveys such as the National Health Interview Survey, Behavioral Risk Factor Surveillance System, and the National Survey on Drug Use and Health, have implemented the 2011 HHS race and ethnicity data standards. CMS has similarly updated the Medicare Current Beneficiary Survey, Medicare Health Outcomes Survey, and the Health Insurance Marketplace Application for Health Coverage with the 2011 HHS data standards. More information about the HHS Race and Ethnicity Data Standards are available on the website at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=54.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19547 through 19549), we proposed to revise the current Race and Ethnicity data element for purposes of this proposal to conform to the 2011 HHS Data Standards for person-level data collection, while also meeting the 1997 OMB minimum data standards for race and ethnicity. Rather than one data element that assesses both race and ethnicity, we proposed two separate data elements: One for Race and one for Ethnicity, that would conform with the 2011 HHS Data Standards and the 1997 OMB Standard. In accordance with the 2011 HHS Data Standards, a two-question format would be used for the proposed race and ethnicity data elements.
The proposed Race data element asks, “What is your race?” In the proposed rule, we proposed to include fourteen response options under the race data element: (1) White; (2) Black or African American; (3) American Indian or Alaska Native; (4) Asian Indian; (5) Chinese; (6) Filipino; (7) Japanese; (8) Korean; (9) Vietnamese; (10) Other Asian; (11) Native Hawaiian; (12) Guamanian or Chamorro; (13) Samoan; and, (14) Other Pacific Islander.
The proposed Ethnicity data element asks, “Are you Hispanic, Latino/a, or Spanish origin?” In the proposed rule, we proposed to include five response options under the ethnicity data element: (1) Not of Hispanic, Latino/a, or Spanish origin; (2) Mexican, Mexican American, Chicano/a; (3) Puerto Rican; (4) Cuban; and, (5) Another Hispanic, Latino, or Spanish Origin. We are including the addition of “of” to the Ethnicity data element to read, “Are you of Hispanic, Latino/a, or Spanish origin?”
We believe that the two proposed data elements for race and ethnicity conform to the 2011 HHS Data Standards for person-level data collection, while also meeting the 1997 OMB minimum data standards for race and ethnicity, because under those standards, more detailed information on population groups can be collected if those additional categories can be aggregated into the OMB minimum standard set of categories.
In addition, we received stakeholder feedback during the December 13, 2018 SDOH listening session on the importance of improving response options for race and ethnicity as a component of health care assessments and for monitoring disparities. Some stakeholders emphasized the importance of allowing for self-identification of race and ethnicity for more categories than are included in the 2011 HHS Standard to better reflect state and local diversity, while acknowledging the burden of coding an open-ended health care assessment question across different settings.
We believe that the proposed modified race and ethnicity data elements more accurately reflect the diversity of the U.S. population than the current race/ethnicity data element included in MDS, LCDS, IRF-PAI, and OASIS.[888 889 890 891] We believe, and research consistently shows, that improving how race and ethnicity data are collected is an important first step in improving quality of care and health outcomes. Addressing disparities in access to care, quality of care, and health outcomes for Medicare beneficiaries begins with identifying and analyzing how SDOH, such as race and ethnicity, align with disparities in these areas.[892] Standardizing self-reported data collection for race and ethnicity allows for the equal comparison of data across multiple healthcare entities.[893] By collecting and analyzing these data, CMS and other healthcare entities will be able to identify challenges and monitor progress. The growing diversity of the U.S. population and knowledge of racial and ethnic disparities within and across population groups supports the collection of more granular data beyond the 1997 OMB minimum standard for reporting categories. The 2011 HHS race and ethnicity data standard includes additional detail that may be used by PAC providers to target quality improvement efforts for racial and ethnic groups experiencing disparate outcomes. For more information on the Race and Ethnicity data elements, we refer readers to the document titled “Final Specifications for LTCH QRP Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In an effort to standardize the submission of race and ethnicity data among IRFs, HHAs, SNFs and LTCHs, for the purposes outlined in section 1899B(a)(1)(B) of the Act, while minimizing the reporting burden, we proposed to adopt the Race and Ethnicity data elements previously described as SPADEs with respect to the proposed Social Determinants of Health category.
Specifically, we proposed to replace the current Race/Ethnicity data element with the proposed Race and Ethnicity data elements on the LCDS. We also proposed that LTCHs that submit the Race and Ethnicity data elements with respect to admission will be considered to have submitted with respect to discharge as well, because it is unlikely that the results of these assessment findings will change between the start and end of the LTCH stay, making the information submitted with respect to a patient's admission the same with respect to a patient's discharge.
Comment: Some commenters noted that the response options for race do not align with those used in other government data, such as the U.S. Census or the Office of Management and Budget (OMB). The commenters also stated these responses are not consistent with the recommendations made in the 2009 Institute of Medicine report. The commenters pointed out that Institute of Medicine (IOM) report recommended using broader OMB race categories and granular ethnicities chosen from a national standard set that can be “rolled up” into the broader categories. The commenters stated that it is unclear how CMS chose the 14 response options under the race data element and the five options under the ethnicity element and worried that these response options would add to the confusion that already may exist for patients about what terms like “race” and “ethnicity” mean for the purposes of health care data collection. A few commenters questioned why race response categories include additional granularity for Asian and Pacific Islander, but not for other races. They noted concern that the proposed question may interfere with successful efforts to collect data in culturally appropriate and standardized ways. They encouraged CMS to seek stakeholder feedback and consensus on the response categories for race and ethnicity data. Another commenter provided that the proposed list of response options for Race may not include all races that should be reflected, for example, Native African, Middle Eastern. In addition, the item should include “check all that apply” to ensure accurate and complete data collection. The commenter encouraged CMS to refine the list of response options for Race and provide a rational for the final list of response options. The commenters also noted that CMS should confer directly with experts on the issue to ensure patient assessments are collecting the right data in the right way before these SDOH SPADEs are finalized.
Response: The proposed race and ethnicity categories align with and are rolled up into the 1997 OMB minimum data standards and conforming with the 2011 HHS Data Standards as described in the implementation guidance titled “U.S. Department of Health and Human Services Implementation Guidance on Data Collection Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status” at https://aspe.hhs.gov/basic-report/hhs-implementation-guidance-data-collection-standards-race-ethnicity-sex-primary-language-and-disability-status. For example, the 1997 OMB minimum data standard for Hispanic is the roll up category for the following response options on the 2011 HHS Data Standards: Mexican, Mexican American, Chicano/a; Puerto Rican; Cuban; another Hispanic, Latino, or Spanish origin. The race and ethnicity data element that we proposed also includes “check all that apply” language. As stated in the proposed rule (84 FR 19548), the 14 race categories and the 5 ethnicity categories conform with the 2011 HHS Data Standards for person-level data collection, which were developed in fulfillment of section 4302 of the Affordable Care Act that required the Secretary of HHS to establish data collection standards for race, ethnicity, sex, primary language, and disability status. Through the HHS Data Council, which is the principal, senior internal Departmental forum and advisory body to the Secretary on health and human services data policy and coordinates HHS data collection and analysis activities, the Section 4302 Standards Workgroup was formed. The Workgroup included representatives from HHS, the OMB, and the Census Bureau. The Workgroup examined current federal data collection standards, adequacy of prior testing, and quality of the data produced in prior surveys; consulted with statistical agencies and programs; reviewed OMB data collection standards and the IOM Report Race, Ethnicity, and Language Data Collection: Standardization for Health Care Quality Improvement; sought input from national experts; and built on its members' experience with collecting and analyzing demographic data. As a result of this Workgroup, a set of data collection standards were developed, and then published for public comment. This set of data collection standards is referred to as the 2011 HHS Data Standards.[894] As described in the implementation guidance provided above, the categories of race and ethnicity under the 2011 HHS Data Standards allow for more detailed information to be collected and the additional categories under the 2011 HHS Data Standards can be aggregated into the OMB minimum standards set of categories.
As noted in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19547 through 19549), we conferred with experts by conducting a listening session regarding the proposed SDOH data elements regarding the importance of improving response options for race and ethnicity as a component of health care assessments and for monitoring disparities. Some stakeholders emphasized the importance of allowing for self-identification of race and ethnicity for more categories than are included in the 2011 HHS Data Standards to better reflect state and local diversity. We thank the commenter for the comment on including Middle Eastern and North African (MENA), and Native African. The 2011 HHS Data Standards does not include MENA or Native African but we will be aligning with the 2011 HHS Data Standards to ensure data is consistently being collected and will take it under consideration.
After consideration of the public comments we received, we are finalizing our proposal to adopt the Race and Ethnicity data elements as SPADEs beginning with the FY 2022 LTCH QRP.
(b) Preferred Language and Interpreter Services
More than 64 million Americans speak a language other than English at home, and nearly 40 million of those individuals have limited English proficiency (LEP).[895] Individuals with LEP have been shown to receive worse care and have poorer health outcomes, including higher readmission rates.[896 897 898] Communication with individuals with LEP is an important component of high quality health care, which starts by understanding the population in need of language services. Unaddressed language barriers between a patient and provider care team negatively affects the ability to identify and address individual medical and non-medical care needs, to convey and understand clinical information, as well as discharge and follow up instructions, all of which are necessary for providing high quality care. Understanding the communication assistance needs of patients with LEP, including individuals who are Deaf or hard of hearing, is critical for ensuring good outcomes.
Presently, the preferred language of patients and need for interpreter services are assessed in two PAC assessment tools. The LCDS and the MDS use the same two data elements to assess preferred language and whether a patient or resident needs or wants an interpreter to communicate with health care staff. The MDS initially implemented preferred language and interpreter services data elements to assess the needs of SNF residents and patients and inform care planning. For alignment purposes, the LCDS later adopted the same data elements for LTCHs. The 2009 NASEM (formerly Institute of Medicine) report on standardizing data for health care quality improvement emphasizes that language and communication needs should be assessed as a standard part of health care delivery and quality improvement strategies.[899]
In developing our proposal for a standardized language data element across PAC settings, we considered the current preferred language and interpreter services data elements that are in LCDS and MDS. We also considered the 2011 HHS Primary Language Data Standard and peer-reviewed research. The current preferred language data element in LCDS and MDS asks, “What is your preferred language?” Because the preferred language data element is open-ended, the patient or resident is able to identify their preferred language, including American Sign Language (ASL). Finally, we considered the recommendations from the 2009 NASEM (formerly Institute of Medicine) report, “Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement.” In it, the committee recommended that organizations evaluating a patient's language and communication needs for health care purposes, should collect data on the preferred spoken language and on an individual's assessment of his/her level of English proficiency.
A second language data element in LCDS and MDS asks, “Do you want or need an interpreter to communicate with a doctor or health care staff?” and includes yes or no response options. In contrast, the 2011 HHS Primary Language Data Standard recommends either a single question to assess how well someone speaks English or, if more granular information is needed, a two-part question to assess whether a language other than English is spoken at home and if so, identify that language. However, neither option allows for a direct assessment of a patient's or resident's preferred spoken or written language nor whether they want or need interpreter services for communication with a doctor or care team, both of which are an important part of assessing patient and resident needs and the care planning process. More information about the HHS Data Standard for Primary Language is available on the website at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=54.
Research consistently recommends collecting information about an individual's preferred spoken language and evaluating those responses for purposes of determining language access needs in health care.[900] However, using “preferred spoken language” as the metric does not adequately account for people whose preferred language is ASL, which would necessitate adopting an additional data element to identify visual language. The need to improve the assessment of language preferences and communication needs across PAC settings should be balanced with the burden associated with data collection on the provider and patient. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19549 through 19550), we proposed to retain the Preferred Language and Interpreter Services data elements currently in use on the LCDS.
In addition, we received feedback during the December 13, 2018 listening session on the importance of evaluating and acting on language preferences early to facilitate communication and allowing for patient self-identification of preferred language. Although the discussion about language was focused on preferred spoken language, there was general consensus among participants that stated language preferences may or may not accurately indicate the need for interpreter services, which supports collecting and evaluating data to determine language preference, as well as the need for interpreter services. An alternate suggestion was made to inquire about preferred language specifically for discussing health or health care needs. While this suggestion does allow for ASL as a response option, we do not have data indicating how useful this question might be for assessing the desired information and thus we did not include this question in our proposal.
Improving how preferred language and need for interpreter services data are collected is an important component of improving quality by helping PAC providers and other providers understand patient needs and develop plans to address them. For more information on the Preferred Language and Interpreter Services data elements, we refer readers to the document titled “Final Specifications for LTCH QRP Measures and Standardized Patient Assessment Data Elements,” available on the website at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In an effort to standardize the submission of language data among IRFs, HHAs, SNFs and LTCHs, for the purposes outlined in section 1899B(a)(1)(B) of the Act, while minimizing the reporting burden, we proposed to adopt the Preferred Language and Interpreter Services data elements currently used on the LCDS, and previously described, as SPADEs with respect to the Social Determinants of Health category.
Comment: A commenter noted that, if finalized, LTCHs should only need to submit data on the Race and Ethnicity SPADEs with respect to admission and would not need to collect and report again at discharge, as it is unlikely that patient status for these elements will change. They believe that a patient's preferred language and need for an interpreter also are unlikely to change between admission and discharge; thus, the commenter recommended CMS to require collection of these SDOH SPADEs with respect to admission only.
Response: With regard to the submission of the Preferred Language and Interpreter Services SPADEs, we agree with the commenters that it is unlikely that the assessment of Preferred Language and Interpreter Services at admission would differ from assessment at discharge. As discussed in the previous response for Hearing and Vision, we believe that the submission of preferred language and the need for an interpreter is similar to the submission of the Race, Ethnicity, Hearing, and Vision SPADEs.
We account for this change to the Collection of Information Requirements for the LTCH QRP in section X.B.6. of the preamble of this final rule.
Based on the comments received, and for the reasons discussed, we are finalizing that the Preferred Language and Interpreter Services SPADEs be collected as proposed with the modification that we will deem LTCHs that submit these two SPADEs with respect to admission to have submitted with respect to both admission and discharge.
(c) Health Literacy
The Department of Health and Human Services defines health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” [901] Similar to language barriers, low health literacy can interfere with communication between the provider and patient and the ability for patients or their caregivers to understand and follow treatment plans, including medication management. Poor health literacy is linked to lower levels of knowledge about health, worse health outcomes, and the receipt of fewer preventive services, but higher medical costs and rates of emergency department use.[902]
Health literacy is prioritized by Healthy People 2020 as an SDOH.[903] Healthy People 2020 is a long-term, evidence-based effort led by the Department of Health and Human Services that aims to identify nationwide health improvement priorities and improve the health of all Americans. Although not designated as a social risk factor in NASEM's 2016 report on accounting for social risk factors in Medicare payment, the NASEM noted that health literacy is impacted by other social risk factors and can affect access to care as well as quality of care and health outcomes.[904] Assessing for health literacy across PAC settings would facilitate better care coordination and discharge planning. A significant challenge in assessing the health literacy of individuals is avoiding excessive burden on patients and health care providers. The majority of existing, validated health literacy assessment tools use multiple screening items, generally with no fewer than four, which would make them burdensome if adopted in MDS, LCDS, IRF-PAI, and OASIS.
The Single Item Literacy Screener (SILS) question asks, “How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?” Possible response options are: (1) Never; (2) Rarely; (3) Sometimes; (4) Often; and (5) Always. The SILS question, which assesses reading ability, (a primary component of health literacy), tested reasonably well against the 36 item Short Test of Functional Health Literacy in Adults (S-TOFHLA), a thoroughly vetted and widely adopted health literacy test, in assessing the likelihood of low health literacy in an adult sample from primary care practices participating in the Vermont Diabetes Information System.[905 906] The S-TOFHLA is a more complex assessment instrument developed using actual hospital related materials such as prescription bottle labels and appointment slips, and often considered the instrument of choice for a detailed evaluation of health literacy.[907] Furthermore, the S-TOFHLA instrument is proprietary and subject to purchase for individual entities or users.[908] Given that SILS is publicly available, shorter and easier to administer than the full health literacy screen, and research found that a positive result on the SILS demonstrates an increased likelihood that an individual has low health literacy, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19550 through 19551), we proposed to use the single-item reading question for health literacy in the standardized data collection across PAC settings. We believe that use of this data element will provide sufficient information about the health literacy of LTCH patients to facilitate appropriate care planning, care coordination, and interoperable data exchange across PAC settings.
In addition, we received feedback during the December 13, 2018 SDOH listening session on the importance of recognizing health literacy as more than understanding written materials and filling out forms, as it is also important to evaluate whether patients understand their conditions. However, the NASEM recently recommended that health care providers implement health literacy universal precautions instead of taking steps to ensure care is provided at an appropriate literacy level based on individualized assessment of health literacy.[909] Given the dearth of Medicare data on health literacy and gaps in addressing health literacy in practice, we recommend the addition of a health literacy data element.
The proposed Health Literacy data element is consistent with considerations raised by NASEM and other stakeholders and research on health literacy, which demonstrates an impact on health care use, cost, and outcomes.[910] For more information on the proposed Health Literacy data element, we refer readers to the document titled “Final Specifications for LTCH QRP Measures and Standardized Patient Assessment Data Elements,” available on the website at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In an effort to standardize the submission of health literacy data among IRFs, HHAs, SNFs and LTCHs, for the purposes outlined in section 1899B(a)(1)(B) of the Act, while minimizing the reporting burden, we proposed to adopt the SILS question, previously described for the Health Literacy data element, as SPADE under the Social Determinants of Health category. We proposed to add the Health Literacy data element to the LCDS.
Comment: A commenter noted that, if finalized, LTCHs should only need to submit data on the Race and Ethnicity SPADEs with respect to admission and would not need to collect and report again at discharge, as it is unlikely that patient status for these elements will change. They believe that a patient's health literacy also is unlikely to change between admission and discharge; thus, the commenter recommended CMS to require collection of this SDOH SPADE with respect to admission only.
Response: We disagree with the commenter who stated that health literacy responses will always be the same from admission to discharge. Unlike Vision, Hearing, Race, Ethnicity, Preferred Language, and Interpreter Services, we believe that the response to this question will change from admission to discharge; therefore, the SPADE is required to be collected at both admission and discharge. For example, some patients may develop health issues, such as cognitive decline during their stay that could impact their response to health literacy thus changing their status at discharged. While not directly evaluating health literacy, clinical conditions that impact a patient's health literacy status would be captured in the clinical record, even if they are not assessed by a SPADE. Therefore, we proposed to collect this SPADE with respect to both admission and discharge.
Comment: A commenter stated that the health literacy question could be improved to capture whether the patient can read, understand, and implement/respond to the information. In addition, the commenter stated that the proposed question does not take into account whether a patient's need for help is due to limited vision, which is different from the purpose of the separate Vision data element. Another possible question the commenter suggested was “How often do you have difficulty?”. The commenter suggested that a single construct may not be sufficient for this area, depending on the aspect of health literacy that CMS intends to identify. Another commenter requested that CMS provide more clarity regarding the timeframe of reference for this question.
Response: We thank the commenter for the comment on the Health Literacy data element. We agree that knowing whether a patient has a reading or comprehension challenge, or limited vision would be helpful. However, we specifically proposed data elements that have been tested. We were also mindful to try and limit the potential burden of asking additional questions related to health literacy. The SILS Health Literacy data element that we proposed performed well when tested, and it minimizes concerns related to burden by requiring one instead of multiple questions on health literacy. If commenters have examples of SDOH questions that have been cognitively tested, we would welcome that feedback as we seek to refine SDOH SPADEs in future rulemaking.
(d) Transportation
Transportation barriers commonly affect access to necessary health care, causing missed appointments, delayed care, and unfilled prescriptions, all of which can have a negative impact on health outcomes.[911] Access to transportation for ongoing health care and medication access needs, particularly for those with chronic diseases, is essential to successful chronic disease management. Adopting a data element to collect and analyze information regarding transportation needs across PAC settings would facilitate the connection to programs that can address identified needs. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19551), we therefore proposed to adopt as SPADE a single transportation data element that is from the Protocol for Responding to and Assessing Patients' Assets, Risks, and Experiences (PRAPARE) assessment tool and currently part of the Accountable Health Communities (AHC) Screening Tool.
The proposed Transportation data element from the PRAPARE tool asks, “Has lack of transportation kept you from medical appointments, meetings, work, or from getting things needed for daily living?” The three response options are: (1) Yes, it has kept me from medical appointments or from getting my medications; (2) Yes, it has kept me from non-medical meetings, appointments, work, or from getting things that I need; and (3) No. The patient would be given the option to select all responses that apply. We proposed to use the transportation data element from the PRAPARE Tool, with permission from National Association of Community Health Centers (NACHC), after considering research on the importance of addressing transportation needs as a critical SDOH.[912]
The proposed data element is responsive to research on the importance of addressing transportation needs as a critical SDOH and would adopt the Transportation item from the PRAPARE tool.[913] This data element comes from the national PRAPARE social determinants of health assessment protocol, developed and owned by NACHC, in partnership with the Association of Asian Pacific Community Health Organization, the Oregon Primary Care Association, and the Institute for Alternative Futures. Similarly, the Transportation data element used in the AHC Screening Tool was adapted from the PRAPARE tool. The AHC screening tool was implemented by the Center for Medicare and Medicaid Innovation's AHC Model and developed by a panel of interdisciplinary experts that looked at evidence-based ways to measure SDOH, including transportation. While the transportation access data element in the AHC screening tool serves the same purposes as our proposed SPADE collection about transportation barriers, the AHC tool has binary yes or no response options that do not differentiate between challenges for medical versus non-medical appointments and activities. We believe that this is an important nuance for informing PAC discharge planning to a community setting, as transportation needs for non-medical activities may differ than for medical activities and should be taken into account.[914] We believe that use of this data element will provide sufficient information about transportation barriers to medical and non-medical care for LTCH patients to facilitate appropriate discharge planning and care coordination across PAC settings. As such, we proposed to adopt the Transportation data element from PRAPARE. More information about development of the PRAPARE tool is available on the website at: https://protect2.fireeye.com/url?k=7cb6eb44-20e2f238-7cb6da7b-0cc47adc5fa2-1751cb986c8c2f8c&u=http://www.nachc.org/prapare.
In addition, we received stakeholder feedback during the December 13, 2018 SDOH listening session on the impact of transportation barriers on unmet care needs. While recognizing that there is no consensus in the field about whether providers should have responsibility for resolving patient transportation needs, discussion focused on the importance of assessing transportation barriers to facilitate connections with available community resources.
Adding a Transportation data element to the collection of SPADE would be an important step to identifying and addressing SDOH that impact health outcomes and patient experience for Medicare beneficiaries. For more information on the Transportation data element, we refer readers to the document titled “Final Specifications for LTCH QRP Measures and Standardized Patient Assessment Data Elements,” available on the website at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In an effort to standardize the submission of transportation data among IRFs, HHAs, SNFs and LTCHs, for the purposes outlined in section 1899B(a)(1)(B) of the Act, while minimizing the reporting burden, we proposed to adopt the Transportation data element previously described as SPADE with respect to the proposed Social Determinants of Health category. If finalized as proposed, we would add the Transportation data element to the LCDS.
Comment: A commenter supported the collection of data to capture the reason(s) transportation affects a patient's access to health care. The commenter appreciated the inclusion of these items on the LCDS and encouraged exploration of quality measures in this area as transportation is an extremely important instrumental activity of daily living to effectively transition to the community.
Response: We thank the commenter for the comment and we will consider this feedback as we continue to improve and refine the SPADEs.
Comment: A commenter noted that, if finalized, LTCHs should only need to submit data on the Race and Ethnicity SPADEs with respect to admission and would not need to collect and report again at discharge, as it is unlikely that patient status for these elements will change. They believe that a patient's response to the Transportation SPADE also is unlikely to change between admission and discharge; thus, the commenter recommended CMS to require collection of this SDOH SPADE with respect to admission only.
Response: We disagree with the commenter who stated that Transportation responses will always be the same from admission to discharge. Unlike Vision, Hearing, Race, Ethnicity, Preferred Language, and Interpreter Services, we believe that the response to this question will change from admission to discharge; therefore, the SPADE is required to be collected at both admission and discharge. For example, losing a family member or caregiver between admission and discharge could change how the patient responds to the Transportation SPADE. Therefore, we are finalizing to collect this SPADE with respect to both admission and discharge as proposed.
After consideration of the public comments we received, and for the reasons discussed, we are finalizing our proposal with regard to Transportation as proposed.
(e) Social Isolation
Distinct from loneliness, social isolation refers to an actual or perceived lack of contact with other people, such as living alone or residing in a remote area.[915 916] Social isolation tends to increase with age, is a risk factor for physical and mental illness, and a predictor of mortality.[917 918 919] Post-acute care providers are well-suited to design and implement programs to increase social engagement of patients, while also taking into account individual needs and preferences. Adopting a data element to collect and analyze information about social isolation in LTCHs and across PAC settings would facilitate the identification of patients who are socially isolated and who may benefit from engagement efforts.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19551 through 19552), we proposed to adopt as SPADE a single social isolation data element that is currently part of the AHC Screening Tool. The AHC item was selected from the Patient-Reported Outcomes Measurement Information System (PROMIS®) Item Bank on Emotional Distress and asks, “How often do you feel lonely or isolated from those around you?” The five response options are: (1) Never; (2) Rarely; (3) Sometimes; (4) Often; and (5) Always.[920] The AHC Screening Tool was developed by a panel of interdisciplinary experts that looked at evidence-based ways to measure SDOH, including social isolation. More information about the AHC Screening Tool is available on the website at: https://innovation.cms.gov/Files/worksheets/ahcm-screeningtool.pdf.
In addition, we received stakeholder feedback during the December 13, 2018 SDOH listening session on the value of receiving information on social isolation for purposes of care planning. Some stakeholders also recommended assessing social isolation as an SDOH as opposed to social support.
The proposed Social Isolation data element is consistent with NASEM considerations about social isolation as a function of social relationships that impacts health outcomes and increases mortality risk, as well as the current work of a NASEM committee examining how social isolation and loneliness impact health outcomes in adults 50 years and older. We believe that adding a Social Isolation data element would be an important component of better understanding patient complexity and the care goals of patients, thereby facilitating care coordination and continuity in care planning across PAC settings. For more information on the Social Isolation data element, we refer readers to the document titled “Final Specifications for LTCH QRP Measures and Standardized Patient Assessment Data Elements,” available on the website at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
In an effort to standardize the submission of social isolation data among IRFs, HHAs, SNFs and LTCHs, for the purposes outlined in section 1899B(a)(1)(B) of the Act, while minimizing the reporting burden, we proposed to adopt the Social Isolation data element previously described as SPADE with respect to the proposed Social Determinants of Health category. We proposed to add the Social Isolation data element to the LCDS.
Commen t: A commenter noted that, if finalized, LTCHs should only need to submit data on the Race and Ethnicity SPADEs with respect to admission and would not need to collect and report again at discharge, as it is unlikely that patient status for these elements will change. They believe that a patient's response to the Social Isolation SPADE also is unlikely to change between admission and discharge; thus, the commenter recommended CMS to require collection of this SDOH SPADE with respect to admission only.
Response: We disagree with the commenter who stated that social isolation responses will always be the same from admission to discharge. Unlike Vision, Hearing, Race, Ethnicity, Preferred Language, and Interpreter Services, we believe that the response to this question will change from admission to discharge; therefore, the SPADE is required to be collected at both admission and discharge. For example, losing a family member or caregiver between admission and discharge could change how the patient responds to the Social Isolation SPADE. Therefore, we proposed to collect this SPADE with respect to both admission and discharge.
Comment: A commenter stated that the proposed question on social isolation may have a very different answer based on the time horizon considered by the beneficiary as beneficiaries who are newly admitted to an LTCH may have experienced differing levels of social isolation over the preceding week due to interactions with health care providers, emergency providers, and friends or family visiting due to hospitalization. The commenter believes this question could be improved by adding timeframe to the question. For example, “How often have you felt lonely or isolated from those around you in the past 6 months?”
Response: We thank the commenter for this comment. The Social Isolation data element is assessing if a patient has experienced social isolation in the past six months to a year. The proposed Social Isolation data element is currently part of the Accountable Health Communities (AHC) Screening Tool. The AHC item was selected from the Patient-Reported Outcomes Measurement Information System (PROMIS®) Item Bank on Emotional Distress. The Social Isolation SPADE is asking about the last 6 months to 1 year.
After consideration of the public comments we received, and for the reasons discussed, we are finalizing our proposal with regard to the Social Isolation SPADE as proposed.
After consideration of the public comments, we are finalizing our proposals to collect SDOH data for the purposes under section 2(d)(2)(B) of the IMPACT Act and section 1899B(b)(1)(B)(vi) of the Act as follows. We are finalizing our proposals for Race, Ethnicity, Health Literacy, Transportation, and Social Isolation as proposed. In response to stakeholder comments, we are revising our proposed policies and finalizing that LTCHs that submit the Preferred Language and Interpreter Services SPADEs with respect to admission will be deemed to have submitted with respect to both admission and discharge.
8. Form, Manner, and Timing of Data Submission Under the LTCH QRP
a. Background
We refer readers to the regulations at § 412.560(b) for information regarding the current policies for reporting LTCH QRP data.
We received some comments regarding the LTCH CARE Data Set, which we summarize and respond to in this final rule.
Comment: A commenter was appreciative that CMS provided extensive supporting materials describing the proposed new and modified LTCH CARE Data Set items along with a change table as it helps foresee necessary software updates and system changes from a very early date. However, the commenter stated that it would be extremely useful to have early drafts of the new and modified data elements within the context of the entire assessment instrument.
Response: We appreciate the commenters' support and suggestions and will take them into consideration for future proposed new and modified LTCH CARE Data Set data elements.
Comment: A commenter provided feedback on the proposed set of LTCH CARE Data Set changes and the effect, if finalized, it would have on existing software user interfaces. The proposed changes to ethnicity, race, admitted from, and discharge location were cited as items which would require many LTCHs to reopen existing and long-running interfaces; this would likely result in many LTCHs no longer being able to take race and ethnicity information electronically. The commenter also cited that these data set changes would require reworking of existing interoperability as both sides of the interface (sending hospitals and receiving systems) would need to rewrite whole sections of that functionality to accommodate the modifications to CAM and Spontaneous Breathing Trial (SBT) items and that the cost of making these changes will act as a deterrent to hospitals to invest the time and money in building out interoperability. The commenter further specified that very small item set changes would require disproportionate amounts of work that impact all activities associated with data collection, submission, and reporting.
Response: We acknowledge the complexities and level of effort required to modify an existing software user interface to collect the revised ethnicity, race, admitted from, discharge location, CAM, and SBT data elements. As mentioned previously, the Race and Ethnicity data elements were modified to standardize the submission of race and ethnicity data among IRFs, HHAs, SNFs and LTCHs. In addition, we agree on the importance of improving response options for these items as a component of improving health care assessments and for monitoring disparities and as a first step in improving quality of care and health outcomes. The Admission From and Discharge Location data elements were also modified to standardize among IRFs, HHAs, SNFs, and LTCHs for the Transfer of Health Information quality measures. Modifications to the CAM and SBT items were made to support alignment with the SNF and IRF settings and for clarity, respectively.
b. Update to the CMS System for Reporting Quality Measures and Standardized Patient Assessment Data and Associated Procedural Proposals
LTCHs are currently required to submit LCDS data to CMS using the Quality Improvement and Evaluation System (QIES) Assessment and Submission Processing (ASAP) system. We have recently migrated to a new internet Quality Improvement and Evaluation System (iQIES) that will enable real-time upgrades, and, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19552), we proposed to designate that system as the data submission system for the LTCH QRP beginning October 1, 2019. We also proposed to revise our regulations at § 412.560(d)(1) by replacing the reference to “Quality Improvement and Evaluation System (QIES) Assessment Submission and Processing (ASAP) system” with “CMS designated data submission system”, and to revise § 412.560(d)(3) and § 412.560(f)(1) by replacing the references to “QIES ASAP system” with “CMS designated data submission system” effective October 1, 2019. In addition, we proposed to notify the public of any future changes to the CMS designated system using subregulatory mechanisms such as website postings, listserv messaging, and webinars.
We did not receive any comments on this proposal. Therefore, we are finalizing our proposal to revise our regulations at § 412.560(d)(1), (d)(3), and (f)(1) as proposed. We are also finalizing our proposal to notify the public of any future changes to the CMS designated system using subregulatory mechanisms such as website postings, listserv messaging, and webinars.
c. Reporting Requirement Updates Beginning With the FY 2022 LTCH QRP
In the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20515), we sought public comment on moving the implementation date of any new version of the LCDS from April to October of the same year. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41633), we summarized the comments we received on this topic. After considering those comments, and to align with the MDS and IRF-PAI implementation dates, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19552 through 19553), we proposed to move the implementation date of any new version of the LCDS from April to October, beginning October 1, 2020. This would provide LTCHs an additional 6 months to prepare for any changes to the reporting requirements.
We also proposed that, for the first program year in which measures or standardized patient assessment data are adopted, LTCHs would only be required to report data on patients who are admitted and discharged during the last quarter (October 1 to December 31) of the calendar year that applies to the program year. For subsequent program years, LTCHs would be required to report data on patients who are admitted and discharged during the 12-month calendar year that applies to the program year.
The tables in this section illustrate the proposed quarterly data collection reporting periods and data submission deadlines using the FY 2022 LTCH QRP and FY 2023 LTCH QRP. The data submission deadline applies to all measures and standardized patient assessment data except the Influenza Vaccination Coverage Among Healthcare Personnel (NQF #0431) measure data, which is submitted annually.

Comment: Commenters supported moving the implementation date of the LTCH CARE Data Set from April to October. A commenter appreciated that this change will provide LTCHs with an additional 6 months to prepare for any changes made to the LTCH CARE Data Set and will provide more time to adequately train staff on any changes to the LTCH CARE Data Set. The commenter also supported CMS' related proposal that for the first program year in which a new measure or SPADE is adopted, LTCHs would only need to report data on patients admitted or discharged in the last calendar quarter of the year (October 1 to December 31).
Response: We appreciate the commenters' support. We would like to clarify that for the first program year in which a new measure or SPADE is adopted, LTCHs would only need to report data on patients admitted or discharged in the last calendar quarter of the year (October 1 to December 31). For subsequent program years, LTCHs would be required to report data on patients who are admitted and discharged during the 12-month calendar year that applies to the program year.
After consideration of the public comments we received, we are finalizing our proposal to move the implementation date of any new version of the LCDS from April to October, beginning October 1, 2020. We are also finalizing our proposal that, for the first program year in which measures or standardized patient assessment data are adopted, LTCHs will only be required to report data on patients who are admitted and discharged during the last quarter (October 1 to December 31) of the calendar year that applies to the program year. For subsequent program years, LTCHs will be required to report data on patients who are admitted and discharged during the 12-month calendar year that applies to the program year.
d. Schedule for Reporting the Transfer of Health Information Quality Measures Beginning With the FY 2022 LTCH QRP
As discussed in section VIII.C.4. of the preamble of this final rule, we are adopting the Transfer of Health Information to the Provider-Post-Acute Care (PAC) and Transfer of Health Information to the Patient-Post-Acute Care (PAC) quality measures beginning with the FY 2022 LTCH QRP. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19553), we also proposed that LTCHs would report the data on those measures using the LCDS. LTCHs would be required to collect data on both measures for all patients beginning with October 1, 2020 discharges. We refer readers to the tables in section VIII.C.8.c. of the preamble of this final rule for an illustration of the initial and calendar year reporting cycles.
We did not receive any comments on this proposal.
We are finalizing our proposal that LTCHs report the data on the Transfer of Health Information to the Provider-Post-Acute Care (PAC) and Transfer of Health Information to the Patient-Post-Acute Care (PAC) quality measures using the LTCH CARE Data Set as proposed. LTCHs will be required to collect data on both measures for all patients beginning with October 1, 2020 discharges.
e. Schedule for Reporting Standardized Patient Assessment Data Elements Beginning With the FY 2022 LTCH QRP
As discussed in section VIII.C.7. of the preamble of this final rule, we are adopting SPADEs beginning with the FY 2022 LTCH QRP. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19553), we proposed that LTCHs would report the data using the LCDS. Similar to the proposed schedule for reporting the Transfer of Health Information to the Provider-Post-Acute Care (PAC) and Transfer of Health Information to the Patient-Post-Acute Care (PAC) quality measures, LTCHs would be required to collect the SPADEs for all patients beginning with October 1, 2020 admissions and discharges. LTCHs that submit data with respect to admission for the Hearing, Vision, Race, and Ethnicity SPADEs would be considered to have submitted data with respect to discharge. We refer readers to the tables in section VIII.C.8.c. of the preamble of this final rule for an illustration of the initial and calendar year reporting cycles.
We did not receive any comments on this proposal.
We are finalizing our proposal that LTCHs must submit the SPADEs for all patients beginning October 1, 2020 with respect to admissions and discharges using the LTCH CARE Data Set. LTCHs that submit data with respect to admission for the Hearing, Vision, Preferred Language, Interpreter Services, Race, and Ethnicity SPADEs will be considered to have submitted data with respect to discharges.
9. Removal of the List of Compliant LTCHs
In the FY 2016 IPPS/LTCH PPS final rule (80 FR 49754 through 49755), we finalized that we would publish a list of LTCHs that successfully met the reporting requirements for the applicable payment determination on the LTCH QRP website and update the list on an annual basis.
We have received feedback from stakeholders that this list offers minimal benefit. Although the posting of successful providers was the final step in the applicable payment determination process, it does not provide new information or clarification to the providers regarding their annual payment update status. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19553), we proposed that we will no longer publish a list of compliant LTCHs on the LTCH QRP website effective beginning with the FY 2020 payment determination.
We did not receive any comments on this proposal.
We are finalizing our proposal that we will no longer publish a list of compliant LTCHs on the LTCH QRP website beginning with the FY 2020 payment determination.
10. Policies Regarding Public Display of Measure Data for the LTCH QRP
Section 1886(m)(5)(E) of the Act requires the Secretary to establish procedures for making the LTCH QRP data available to the public after ensuring that LTCHs have the opportunity to review their data prior to public display. Measure data are currently displayed on the LTCH Compare website, an interactive web tool that assists individuals by providing information on LTCH quality of care. For more information on LTCH Compare, we refer readers to our website at: https://www.medicare.gov/longtermcarehospitalcompare/. For a more detailed discussion about our policies regarding public display of LTCH QRP measure data and procedures for the opportunity to review and correct data and information, we refer readers to the FY 2017 IPPS/LTCH PPS final rule (81 FR 57231 through 57236).
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19553 through 19554), we proposed to begin publicly displaying data for the Drug Regimen Review Conducted With Follow-Up for Identified Issues—Post Acute Care (PAC) Long-Term Care Hospital (LTCH) Quality Reporting Program (QRP) measure beginning CY 2020 or as soon as technically feasible. We finalized the Drug Regimen Review Conducted With Follow-Up for Identified Issues—Post Acute Care (PAC) Long-Term Care Hospital (LTCH) Quality Reporting Program (QRP) measure in the FY 2017 IPPS/LTCH PPS final rule (81 FR 57219 through 57223).
Data collection for this assessment-based measure began with patients admitted and discharged on or after July 1, 2018. We proposed to display data based on four rolling quarters, initially using discharges from January 1, 2019 through December 31, 2019 (Quarter 1 2019 through Quarter 4 2019). To ensure the statistical reliability of the data, we proposed that we would not publicly report an LTCH's performance on the measure if the LTCH had fewer than 20 eligible cases in any four consecutive rolling quarters. LTCHs that have fewer than 20 eligible cases would be distinguished with a footnote that states: “The number of cases/patient stays is too small to publicly report.”
Comment: Several commenters supported the proposal to begin publicly displaying data for the Drug Regimen Review Conducted With Follow-Up for Identified Issues—Post Acute Care (PAC) Long Term Care Hospital (LTCH) Quality Reporting Program (QRP) measure in CY 2020 or as soon as technically feasible, including the exception for LTCHs with fewer than 20 eligible cases.
Response: We appreciate the commenters support.
After consideration of the public comments we received, we are finalizing our proposal to begin publicly displaying data for the Drug Regimen Review Conducted With Follow-Up for Identified Issues—PAC LTCH QRP measure beginning CY 2020 or as soon as technically feasible.
D. Changes to the Medicare and Medicaid Promoting Interoperability Programs
1. Background
a. Statutory Authority for the Medicare and Medicaid Promoting Interoperability Programs
The HITECH Act (Title IV of Division B of the ARRA, together with Title XIII of Division A of the ARRA) authorizes incentive payments under Medicare and Medicaid for the adoption and meaningful use of certified electronic health record technology (CEHRT). Incentive payments under Medicare were available to eligible hospitals and CAHs for certain payment years (as authorized under sections 1886(n) and 1814(l) of the Act, respectively) if they successfully demonstrated meaningful use of CEHRT, which included reporting on clinical quality measures (CQMs) using CEHRT. Incentive payments were available to Medicare Advantage (MA) organizations under section 1853(m)(3) of the Act for certain affiliated hospitals that meaningfully used CEHRT. In accordance with the timeframe set forth in the statute, these incentive payments under Medicare generally are no longer available, except for Puerto Rico eligible hospitals (for more information on the Medicare incentive payments available to Puerto Rico eligible hospitals, we refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41672 through 41675).
Sections 1886(b)(3)(B)(ix) and 1814(l)(4) of the Act also establish downward payment adjustments under Medicare, beginning with FY 2015, for eligible hospitals and CAHs that do not successfully demonstrate meaningful use of CEHRT for certain associated EHR reporting periods. Section 1853(m)(4) of the Act establishes a negative payment adjustment to the monthly prospective payments of a qualifying MA organization if its affiliated eligible hospitals are not meaningful users of CEHRT, beginning in 2015.
Section 1903(a)(3)(F)(i) of the Act establishes 100 percent Federal financial participation (FFP) to States for providing incentive payments to eligible Medicaid providers (described in section 1903(t)(2) of the Act) to adopt, implement, upgrade, and meaningfully use CEHRT.
2. EHR Reporting Period
a. Change to the EHR Reporting Period in CY 2019 for Eligible Hospitals
Under § 495.4, in the definition of “EHR reporting period for a payment adjustment year,” for 2019, if an eligible hospital has not successfully demonstrated it is a meaningful EHR user in a prior year, the EHR reporting period is any continuous 90-day period within CY 2019 and applies for the FY 2020 and 2021 payment adjustment years. For the FY 2020 payment adjustment year, the EHR reporting period must end before and the eligible hospital must successfully register for and attest to meaningful use no later than October 1, 2019.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19554 through 19555), we proposed that, if we finalize our proposal to modify the Query of PDMP measure to require a “yes/no” attestation response instead of a numerator/denominator, as discussed in greater detail in section VIII.D.3.b. of the preamble of this final rule, we would eliminate the October 1, 2019 deadline for an eligible hospital that has not successfully demonstrated it is a meaningful EHR user in a prior year. This proposal will provide such eligible hospitals all of CY 2019 to complete their respective minimum 90-day EHR reporting period for the FY 2020 payment adjustment year. We also proposed to revise the definition of “EHR reporting period for a payment adjustment year” at 42 CFR 495.4 to reflect this proposal.
Comment: Many commenters supported the modification of the Query of PDMP measure to a “yes/no” attestation. Those same commenters were strongly in favor of CMS eliminating the October 1, 2019 deadline for an eligible hospital that has not successfully demonstrated it is a meaningful EHR user in a prior year and for CMS allowing flexibility to attest on data from any continuous 90-day period from January 1, 2019 through December 31, 2019. Commenters stated that this continuation will allow hospitals to focus on improving interoperability and patient access to health information.
Response: We appreciate the commenters' support, and we believe that both of these changes will help to reduce burden for eligible hospitals.
As described in this section of the final rule, we are finalizing the conversion of the Query of PDMP measure to a yes/no attestation. Because we are finalizing this change, and after consideration of the public comments, we are, also, finalizing our proposal to eliminate the October 1, 2019 deadline for an eligible hospital that has not successfully demonstrated it is a meaningful EHR user in a prior year. Those eligible hospitals that have not demonstrated themselves as being meaningful EHR users in a prior year will have all of CY 2019 to complete their respective minimum 90-day EHR reporting period for the FY 2020 payment adjustment year. We are, also, finalizing the revised definition of “EHR reporting period for a payment adjustment year” at 42 CFR 495.4 as proposed.
b. EHR Reporting Period in CY 2021
As finalized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41636), and codified in the definitions of “EHR reporting period” and “EHR reporting period for a payment adjustment year” at § 495.4, the EHR reporting period in CY 2020 is a minimum of any continuous 90-day period in CY 2020 for new and returning participants in the Promoting Interoperability Programs attesting to CMS or their State Medicaid agency. Eligible professionals, eligible hospitals, and CAHs may select an EHR reporting period of a minimum of any continuous 90-day period in CY 2020 from January 1, 2020 through December 31, 2020.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19554 through 19555), for CY 2021, we proposed an EHR reporting period of a minimum of any continuous 90-day period in CY 2021 for new and returning participants (eligible hospitals and CAHs) in the Medicare Promoting Interoperability Program attesting to CMS. We also proposed corresponding changes to the definitions of “EHR reporting period” and “EHR reporting period for a payment adjustment year” at § 495.4.
In the July 28, 2010 final rule titled “Medicare and Medicaid Programs; Electronic Health Record Incentive Program” (75 FR 44319), we established that, in accordance with section 1903(t)(5)(D) of the Act, in no case may any Medicaid eligible hospital receive an incentive after 2021 (see § 495.310(f)). Therefore, December 31, 2021 is the last date that States could make Medicaid Promoting Interoperability Program payments to Medicaid eligible hospitals (other than pursuant to a successful appeal related to 2021 or a prior year). For additional discussion of this issue, we refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41676 through 41677) and the CY 2019 PFS/QPP final rule (83 FR 59704 through 59706). As discussed in those rules, the same deadline applies to Medicaid Promoting Interoperability Program incentive payments to Medicaid eligible professionals, under section 1903(t)(4)(A)(iii) of the Act and 42 CFR 495.310(a)(2)(v). To help States meet this deadline, in the CY 2019 PFS/QPP final rule (83 FR 59704 through 59706), we changed the CY 2021 EHR and CQM reporting periods for Medicaid eligible professionals. However, we did not change the 2021 EHR and CQM reporting periods for Medicaid eligible hospitals in that rule, and did not propose to do so in the FY 2020 IPPS/LTCH PPS proposed rule.
That is because, based on attestation data and information from State Medicaid Health Information Technology Plans regarding the number of years States disburse Medicaid Promoting Interoperability Program payments to hospitals, we believe that there will be no hospitals eligible to receive Medicaid Promoting Interoperability Program payments in 2021 due to the requirement that, after 2016, eligible hospitals cannot receive a Medicaid Promoting Interoperability Program payment unless they have received such a payment for the prior fiscal year. At this time, we believe that there are no Medicaid-only eligible hospitals or “dually-eligible” hospitals (those that are eligible for an incentive payment under Medicare for meaningful use of CEHRT and/or subject to the Medicare payment reduction for failing to demonstrate meaningful use of CEHRT, and are also eligible to earn a Medicaid incentive payment for meaningful use of CEHRT) that will be able to receive Medicaid Promoting Interoperability Program payments in 2021. We invited comments on whether this belief was accurate in the CY 2019 PFS/QPP rulemaking (83 FR 35873) and received a comment agreeing with us, but we also stated that we will solicit additional comments on this issue in a proposed rule that is more specifically related to hospital payment (83 FR 59705 through 59706). Accordingly, in the proposed rule we again invited comments on whether we are correct in believing that there are no hospitals that would be able to receive Medicaid Promoting Interoperability Program payments in 2021. If this is not true, we sought comment on how we should adjust 2021 EHR reporting periods for Medicaid eligible hospitals in a manner that limits the burden on hospitals and States.
Comment: Many commenters strongly supported the minimum of a continuous 90-day EHR reporting period. Commenters stated that the proposed EHR reporting period allows eligible hospitals and CAHs to adequately plan for any system updates and that it reduces administrative and regulatory burden. Several commenters, also, expressed their appreciation toward CMS for its efforts, including the proposed 90-day EHR reporting period, to help stabilize the Promoting Interoperability Programs.
Response: We appreciate the support for our EHR reporting period proposal. We agree that keeping the EHR reporting period to a minimum of 90 days affords eligible hospitals and CAHs the flexibility they may need to develop and update their evolving EHRs.
Comment: A commenter suggested that CMS should make the minimum 90-day EHR reporting period permanent, as opposed to what CMS has done over the past several years, which is propose the minimum 90-day EHR reporting period each year.
Response: We thank the commenter for the suggestion, and we will take this into consideration for future rulemaking.
Comment: A commenter agreed with the 90-day EHR reporting period, but suggested that CMS not put an end date on the EHR reporting period.
Response: We understand the concern over the limitations an end date could have, but the EHR reporting period is not required to end on the 90th day. The minimum EHR reporting period is a continuous 90 days, but an eligible hospital or CAH may choose to extend the period to be as long as the full calendar year, as long as the EHR reporting period ends no later than December 31.
Comment: A commenter responded to CMS' invitation of comments on its understanding that there are no hospitals that will be able to receive Medicaid Promoting Interoperability Program payments in 2021, and the commenter was in agreement with CMS.
Response: We thank the commenter for his or her input. In addition, we did not receive any comments indicating that there are hospitals that would be able to receive Medicaid Promoting Interoperability Program payments in 2021.
After consideration of the public comments received, we are finalizing our proposal of an EHR reporting period of a minimum of any continuous 90-day period in CY 2021 for new and returning participants (eligible hospitals and CAHs) in the Medicare Promoting Interoperability Program attesting to CMS. We are, also, finalizing the corresponding changes to the definitions of “EHR reporting period” and “EHR reporting period for a payment adjustment year” at 42 CFR 495.4 as proposed.
b. Promoting Interoperability Measures: Actions Must Occur Within the EHR Reporting Period
Stakeholders have questioned whether the actions in the numerator for the Medicare Promoting Interoperability Program are limited to the EHR reporting period or if we allow the numerator to continue to increment outside of the EHR reporting period but within the calendar year. We note that we had issued a frequently asked question (FAQ number 8231 [921] ) applicable to the Medicare and Medicaid EHR Incentive Programs. The FAQ stated that, regarding the reporting of numerators, “the . . . numerator is not constrained to the EHR reporting period unless expressly stated in the numerator statement.” The FAQ went further to state that, for some measures, “the actions may reasonably fall outside of the EHR reporting period timeframe but must take place no earlier than the start of the reporting year and no later than the date of attestation, in order for patients to be counted in the numerator.” When we adopted a new scoring methodology and revised objectives and measures for eligible hospitals and CAHs under the Medicare Promoting Interoperability Program last year in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41634 through 41677), we neglected to state whether the policy in the FAQ will still be applicable in light of the changes to the objectives and measures. As we have established an EHR reporting period that is a minimum of 90 consecutive days, eligible hospitals and CAHs may select an EHR reporting period that ranges from 90 days to the entire CY so that the numerators will increment over a longer period of time. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19555 through 19556), we proposed that, beginning with the EHR reporting period in CY 2020, for eligible hospitals and CAHs that submit an attestation to CMS under the Medicare Promoting Interoperability Program, both the numerators and denominators of measures in the Medicare Promoting Interoperability Program will only increment based on actions that have occurred during the EHR reporting period that was selected by the eligible hospital or CAH. We also proposed to codify this proposed policy at § 495.24(e)(1)(ii).
We noted that there is one exception to this proposed policy, and that is the Security Risk Analysis measure. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41644), we finalized that the actions included in the Security Risk Analysis measure may occur any time during the calendar year in which the EHR reporting period occurs. We proposed to revise § 495.24(e)(4)(iii) to reflect this existing policy for the Security Risk Analysis measure.
In addition, we stated that these proposals will not apply to the Medicaid Promoting Interoperability Program.
Comment: Several commenters supported CMS' proposal that the numerators and denominators of measures in the Medicare Promoting Interoperability Program will only increment based on actions that have occurred during the EHR reporting period that was selected by the eligible hospital or CAH.
Response: We believe that incrementing the numerator and denominator should be limited to actions that have occurred in the EHR reporting period chosen by the eligible hospital or CAH, as opposed to requiring some measures to be incremented outside of the EHR reporting period as this will help to eliminate the confusion surrounding when measures may be incremented.
Comment: Several commenters recommended that CMS maintain its current policy, with the belief that changes to EHR systems and reporting processes will be challenging. Additionally, commenters expressed confusion about the length of time the numerators of measures could accrue, as long as the action occurred within the calendar year, versus actions only being counted that have occurred during the selected EHR reporting period.
Response: We disagree that any changes to EHR systems and reporting processes will be challenging, and we believe that this policy change will help to eliminate the confusion for both, vendors and eligible hospitals/CAHs, surrounding when the numerators and denominators of measures will increment. The EHR reporting period is not limited to the minimum 90 consecutive days. Eligible hospitals and CAHs have the flexibility to choose an EHR reporting period that is as long as the entire calendar year, so that the numerators and denominators will increment over a longer period of time. Doing this will allow for all actions that occurred in the calendar year to be counted in the numerators and denominators. However, if an eligible hospital or CAH elects to have their EHR reporting period be, for example, 200 consecutive days, then only the actions that occurred over the course of those 200 consecutive days will be counted in the numerators and denominators.
Comment: A commenter sought clarification on whether an eligible hospital or CAH may achieve “active engagement” for purposes of the Public Health and Clinical Data Exchange objective by engaging in one of the three types of active engagement outside its selected EHR reporting period.
Response: Our proposal that the numerators and denominators of measures will only increment based on actions that have occurred during the EHR reporting period that was selected by the eligible hospital or CAH was limited to measures with numerators and denominators. Our proposal did not include measures that require a “yes/no” response, such as the measures associated with the Public Health and Clinical Data Exchange objective.
After consideration of the public comments we received, we are finalizing our proposal so that, beginning with the EHR reporting period in CY 2020, eligible hospitals and CAHs that submit an attestation to CMS under the Medicare Promoting Interoperability Program will have the numerators and denominators of measures increment based on actions that have occurred during the EHR reporting period that was selected by the eligible hospital or CAH. We are, also, codifying this policy at § 495.24(e)(1)(ii) as proposed. As previously noted, the actions included in the Security Risk Analysis measure may still occur any time during the calendar year in which the EHR reporting period occurs, and we are finalizing our proposal to revise § 495.24(e)(4)(iii) to reflect this existing policy for the Security Risk Analysis measure.
3. Changes to Measures Under the Electronic Prescribing Objective
a. Background
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41648 through 41656), we adopted two opioid measures for the Electronic Prescribing objective: (1) Query of Prescription Drug Monitoring Program (PDMP), which is optional in CY 2019 and required beginning in CY 2020; and (2) Verify Opioid Treatment Agreement, which is optional in CY 2019 and 2020.
As explained in further detail in this final rule and in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19556 through 19559), we proposed to make certain changes to the Query of PDMP and Verify Opioid Treatment Agreement measures. In section VIII.D.6.b. of the preamble of the proposed rule (84 FR 19560 through 19561), we proposed to adopt two opioid-related clinical quality measures beginning with the EHR reporting period in CY 2021.
c. Query of PDMP Measure
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41637 through 41645), we finalized that the Query of PDMP measure is optional and available for bonus points for CY 2019, and required in CY 2020. We stated that we will be moving towards requiring EHR-PDMP integration in CY 2020 (83 FR 41652). We gave eligible hospitals and CAHs flexibility in implementing this measure, including the flexibility to query the PDMP in any manner allowed under their State law (83 FR 41649). We believe incorporating a requirement for integration, in the context of future changes to the measure, between PDMPs and CEHRT utilized by eligible hospitals and CAHs, will advance the access to and usability of PDMP data by health care providers, and it will reduce health care provider burden associated with the actions of this measure. Integration could reflect a variety of different approaches for interaction between EHRs and PDMPs that are currently being pursued in different locations and settings.
We understand that there is wide variation across the country in how health care providers are implementing and integrating PDMP queries into health IT and clinical workflows, and that it could be burdensome for health care providers if we were to narrow the measure to allow for only one single workflow. At the same time, we have heard extensive feedback from EHR developers that incorporating the ability to count the number of PDMP queries in CEHRT will require more robust certification specifications and standards. Stakeholders stated that health IT developers may face significant cost burdens under the current flexibility allowed for health care providers if they fully develop numerator and denominator calculations for all the potential use cases, and are required to change the specification at a later date. Developers expressed their view that the costs of additional development will likely be passed on to health care providers without additional benefit as they believe this development will be solely for the purpose of calculating the measure rather than furthering the clinical end goal of the measure.
For the reasons discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19557 through 19558), we proposed to make the Query of PDMP measure optional in CY 2020 and eligible for 5 bonus points, and we proposed corresponding changes to the regulations at §§ 495.24(e)(5)(ii)(B) and 495.24(e)(5)(iii)(B). We stated that making the measure optional in CY 2020 will allow time for further integration of PDMPs and EHRs to minimize the burden on eligible hospitals and CAHs when reporting on this measure. We proposed that, in the event we finalize the proposed changes to the Query of PDMP measure, the e-Prescribing measure will be worth up to 10 points in CY 2020 and subsequent years, and we proposed corresponding changes to the regulations at § 495.24(e)(5)(iii)(A).
In addition, beginning with the EHR reporting period in CY 2019, we proposed to remove the numerator and denominator that we established for the Query of PDMP measure in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41649 through 41653) and instead require a “yes/no” response. Under this proposal, the measure description at § 495.24(e)(5)(iii)(B) and 83 FR 41653 will remain the same, but instead of submitting numerator and denominator information for the measure, eligible hospitals and CAHs will submit a “yes/no” response during attestation. A “yes” response would indicate that for at least one Schedule II opioid electronically prescribed using CEHRT during the EHR reporting period, the eligible hospital or CAH used data from CEHRT to conduct a query of a PDMP for prescription drug history, except where prohibited and in accordance with applicable law.
We also proposed to remove the exclusions associated with the Query of PDMP measure beginning in CY 2020, and we proposed corresponding changes to the regulations at §§ 495.24(e)(5)(iv) and 495.24(e)(5)(v)(B) through (D). For CY 2019, we did not provide exclusions for the Query of PDMP and Verify Opioid Treatment Agreement measures because they were optional and eligible for bonus points, and similarly, we do not believe exclusions will be necessary for the Query of PDMP measure if we finalize our proposal to make the measure optional and eligible for bonus points in CY 2020.
Finally, we proposed to address the scoring of the Query of PDMP measure. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41644), we stated that the measure is optional in CY 2019 and worth “up to 5 bonus points.” Our intent, however, was to refer to a full 5 bonus points; we did not intend for the optional measure to be scored based on performance in CY 2019. We proposed to revise § 495.24(e)(5)(iii)(B) to better reflect our intended policy that the Query of PDMP measure is worth a full 5 bonus points (not “up to 5 bonus points”) in CY 2019, and in the event we finalize the proposed changes to the Query of PDMP measure as previously discussed, in CY 2020 as well. We stated that in the event we finalize those proposed changes, if an eligible hospital or CAH submits a “yes” for this measure, it will earn 5 bonus points in CY 2019 and 2020.
Comment: A few commenters agreed with changing the maximum points for e-Prescribing measure from 5 points to 10 points.
Response: We thank commenters for their support.
Comment: A majority of commenters are supportive of the proposed changes to the Query of PDMP measure. Many commenters agree with retaining the measure as optional in CY 2020, further recommending that in order to make it mandatory, the Office of the National Coordinator for Health Information Technology (ONC) should consider adopting new certification criteria requiring EHRs to integrate with PDMPs. These commenters also agree with changing the measure to a yes/no attestation response rather than the current performance-based numerator-denominator calculation. Commenters agree that these changes will reduce unnecessary burden, as developing custom reports are often time-consuming and inaccurate.
Response: We appreciate commenters' support of our proposal to make the Query of PDMP measure optional in CY 2020, and to require a yes/no measure instead of a numerator-denominator calculation. We believe this proposal will reduce overall provider burden by requiring a yes/no measure instead of a numerator and denominator calculations that have various potential use cases calculations varying by states which will require changes to the specifications at a later date and eliminate providers performing manual calculations of the numerator and denominator outside of certified EHR functionality.
We also wish to note that ONC has proposed in the 21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program Notice of Proposed Rulemaking (84 FR 7444) to update the electronic prescribing (e-Rx) SCRIPT standard used for “electronic prescribing” in the 2015 Edition to NCPDP SCRIPT 2017071, which will result in a new e-Rx standard becoming the baseline for certification . As summarized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41650), stakeholders have stated that they believe adoption of the NCPDP SCRIPT 2017071 standard for EHRs can more effectively support medication history transactions for PDMP queries and responses.
Comment: A commenter suggested removing the e-prescribing component of the measure altogether due to time and cost burdens associated with its implementation.
Response: We appreciate the concern surrounding provider and data collection burden, and we continue to make burden reduction a priority in the decision making process. The electronic prescribing component of the Query of PDMP measure is a central aspect in interoperability and alignment between the Query of PDMP measures with the e-Prescribing measure. This may reduce burden for eligible hospitals and CAHs that may have prescribed differently without those standards in place.
Comment: A commenter expressed doubt in the ability of a “yes/no” measure to capture any clinically useful information, and suggested that CMS not use “yes/no” measures moving forward. Other commenters shared similar concerns that a yes/no measure would not capture enough clinically useful information, and that changing the scoring system in the middle of CY 2019 might be challenging for reporting.
Response: We understand the concern and appreciate the feedback. However, regarding the Query of PDMP measure specifically, we believe that it is premature for this measure to be a numerator/denominator measure at this time and the numerator and denominator measure would not capture any clinically useful information.
We also disagree that changing the scoring in the middle of CY 2019 would be challenging for reporting as this would reduce provider burden when manually calculated numerator/denominators. Currently, there is limited use of consistent standards-based approaches to support integration between CEHRT and PDMPs, which contributes to eligible hospitals and CAHs having to manually track each PDMP query. Considering the added burden that doing this creates, we believe a “yes/no” measure is more appropriate.
Comment: Some commenters expressed concerns with the PDMP measure, primarily due to the lack of uniformity in the implementation and functionality of PDMPs across state lines. Because there are no standard criteria for PDMP functionality, commenters told CMS that, in their view, the measure is not ready for mandatory inclusion in the performance-based scoring methodology. Several commenters stated that eligible hospitals and CAHs will have wasted effort if the measure were removed completely.
Response: We understand that PDMP systems comprise various processes and components that vary significantly across state lines, and that in any given state the PDMP system may include varying state-developed and vendor-based solutions along with the core PDMP database. State laws and policies also differ on data storage and use, access roles and disclosures, and key definitions. The degree of PDMP and health IT (EHR, HIE, PDS) access integration (how the provider can access the PMDP) varies significantly across states, but also within states by product and/or health system. Today, most PDMP systems allow a provider “view only” access to PDMP data rather than allowing for the integration of discrete data from the PDMP system into the patient's record.
The Substance Use—Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT for Patients and Communities Act) (Pub. L. 115-271) includes new requirements and federal funding for PDMP enhancement, integration, and interoperability, and establishes mandatory use of PDMPs by certain Medicaid providers. CMS is continuously working with various stakeholders and the ONC to evaluate the implementation of the SUPPORT for Patients and Communities Act and progress around PDMP-EHR integration.
We proposed to change the measure to optional in CY 2020 in order to account for readiness concerns such as those raised by stakeholders. CMS is dedicated to alleviating the concerns of the commenters as we work to further develop the measure.
Comment: Several commenters requested clarification on whether CMS' intention is that the query activity must be facilitated by the use of CEHRT or if it can be performed outside of CEHRT and still be counted toward the numerator of the measure. Others stated that it is also unclear whether providers are to count queries of the PDMP for inpatients only.
Response: As stated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41653), the measure description is as follows: for at least one Schedule II opioid electronically prescribed using CEHRT during the EHR reporting period, the eligible hospital or CAH uses data from CEHRT to conduct a query of a Prescription Drug Monitoring Program (PDMP) for prescription drug history, except where prohibited and in accordance with applicable law. In regards to commenters' assertion that it is unclear whether providers are to count queries of the PDMP for inpatients only, we have not addressed this issue in previous rulemaking and will consider doing so in future rulemaking.
After consideration of the public comments we received, we are finalizing that the Query of PDMP measure is optional and eligible for 5 bonus points in CY 2020 and finalizing corresponding changes to the regulations at §§ 495.24(e)(5)(ii)(B) and 495.24(e)(5)(iii)(B) as proposed. We are also finalizing that the e-Prescribing measure will be worth up to 10 points beginning in CY 2020 and finalizing corresponding changes to the regulations at § 495.24(e)(5)(iii)(A) as proposed.
In addition, beginning with the EHR reporting period in CY 2019, we are finalizing our proposal to remove the numerator and denominator that we established for the Query of PDMP measure in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41649 through 41653) and instead require a “yes/no” response. The measure description at § 495.24(e)(5)(iii)(B) and 83 FR 41653 will remain the same, but instead of submitting numerator and denominator information for the measure, eligible hospitals and CAHs would submit a “yes/no” response during attestation. A “yes” response indicates that for at least one Schedule II opioid electronically prescribed using CEHRT during the EHR reporting period, the eligible hospital or CAH used data from CEHRT to conduct a query of a PDMP for prescription drug history, except where prohibited and in accordance with applicable law. We are also finalizing the proposal to remove the exclusions associated with the Query of PDMP measure beginning in CY 2020, and finalizing the corresponding changes to the regulations at §§ 495.24(e)(5)(iv) and 495.24(e)(5)(v)(B) through (D) as proposed.
Finally, we are finalizing our proposal to revise § 495.24(e)(5)(iii)(B) as proposed to better reflect our intended policy that the Query of PDMP measure is worth a full 5 bonus points (not up to 5 bonus points) in CY 2019 and CY 2020.
d. Verify Opioid Treatment Agreement Measure
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41653 through 41656), we finalized the Verify Opioid Treatment Agreement measure as optional in both CYs 2019 and 2020. Since we proposed this measure (83 FR 20528 through 20530), we have received feedback from stakeholders that this measure presents significant implementation challenges, leads to an increase in burden, and does not promote interoperability. Stakeholders cited the lack of definition around a treatment agreement, the lack of certification standards and criteria, confusion with how to calculate the 30 cumulative day look-back period, and the burden caused by the lack of definition and standards. For the reasons discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19558 through 19559), we proposed to remove the Verify Opioid Treatment Agreement measure from the Promoting Interoperability Program beginning with the EHR reporting period in CY 2020, and we proposed corresponding changes to the regulations at §§ 495.24(e)(5)(ii)(B) and 495.24(e)(5)(iii)(C).
We also proposed to address the scoring of the Verify Opioid Treatment Agreement measure. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41644) we stated that the measure is optional in CYs 2019 and 2020 and worth “up to five bonus points.” As with the previously discussed Query of PDMP measure, in section VIII.D.3.b. of the preamble of this final rule, our intent was to refer to a full 5 bonus points; we did not intend for the optional Verify Opioid Treatment Agreement measure to be scored based on performance in CY 2019 or CY 2020. Accordingly, we proposed in (84 FR 19559) to revise § 495.24(e)(5)(iii)(C) to better reflect our intended policy that the Verify Opioid Treatment Agreement measure is worth a full 5 bonus points (not up to 5 bonus points) in CY 2019, and, in the event we do not finalize our proposal to remove the measure beginning with CY 2020, it will be worth a full 5 bonus points in CY 2020, as well.
Comment: A vast majority of commenters were in general agreement with removing the Verify Opioid Treatment Agreement measure. Several commenters stated that if the measure were to remain, it would result in increased provider burden and decreased interoperability. A few commenters supported removing the measure until treatment agreement standards themselves are addressed, defined, and further clarified. A number of commenters were strongly supportive, further stating their belief that this measure is not appropriate for inpatient hospitals, and lacks standards defining the specific data points and structure to be included in such an agreement. Commenters expressed that this measure is therefore burdensome, vague and insurmountable, presenting significant implementation challenges as it is subject to misinterpretation until and unless such certification requirements are made clear.
Response: We thank all commenters for their overwhelming support for removing the Verify Opioid Treatment Agreement measure beginning with CY 2020. We agree that while addressing OUD prevention and treatment is vital, the Verify Opioid Treatment Agreement measure presents significant implementation challenges, leads to an increase in burden, and as-is, does not promote interoperability. We thank all commenters for their suggestions on how to enhance and improve such a measure as we continue to combat the opioid crisis.
Comment: A few commenters suggested that instead of removing the measure entirely, CMS should change it to a yes/no measure starting from CY 2019 rather than CY 2020. One commenter requested making the measure an optional, yes/no measure for three EHR reporting periods before retiring the measure entirely in CY 2022. The commenter further stated that based on the FY 2019 IPPS/LTCH PPS final rule, this measure would be required in 2021, and as some hospitals have already put significant work toward implementing functionality to meet the measure, retaining the optional bonus points for an additional two years would respect the good faith effort that has already been made. A commenter suggested removing the measure in CY 2019, or, changing it to a yes/no measure as both options would significantly reduce reporting burden until a more appropriate measure set could be developed. Many commenters agreed that an opioid specific measure is important in addressing the opioid epidemic, but requested that the Verify Opioid Treatment Agreement measure be removed while encouraging innovation around future collaborative measure development.
Response: We understand and appreciate the concerns and suggestions addressed by the commenters who do not agree with the removal of the Verify Opioid Treatment Agreement measure starting in CY 2020. We considered the suggestions to change the measure to a yes/no measure or to delay its retirement until 2022. However, we agree with the vast majority of commenters who cited the lack of definition around the treatment agreements, and the lack of certification criteria and standards as reasons for the removal of the measure at this time. In addition, many stakeholders have stated that this measure presents significant implementation challenges that leads to an increase in burden, and does not promote interoperability which we do not believe would be beneficial by requested keeping the measure as an optional, yes/no measure for three EHR reporting periods before retiring the measure entirely in CY 2022. While several commenters requested changing the measure to a yes/no attestation for CY 2019, we have decided that the measure will remain an optional, numerator/denominator-based measure in CY 2019 only.
Comment: A few commenters have requested additional clarification on the CY 2019 EHR reporting period, specifically, on how the measure will be scored. A commenter further suggested conducting pilot testing to assess the feasibility of exchanging information before reintroducing the measure in the future.
Response: We thank commenters for the suggestions. For the CY 2019 EHR reporting period, the Verify Opioid Treatment Agreement measure will remain an optional, numerator/denominator-based measure. Additionally, the measure will be worth a full 5 bonus points. We would like to thank the commenter for their suggestion of conducting pilot/feasibility testing for future measures, and if we decide to pursue this measure in the future, we will consider how to best operationalize the requirements while minimizing the burden on providers.
After consideration of the public comments we received, we are finalizing the proposal to remove the Verify Opioid Treatment Agreement measure from the Promoting Interoperability Program beginning with the EHR reporting period in CY 2020 and the corresponding changes to the regulations at §§ 495.24(e)(5)(ii)(B) and 495.24(e)(5)(iii)(C) as proposed. In addition, we are finalizing the proposal to revise § 495.24(e)(5)(iii)(C) as proposed to better reflect our intended policy that the Verify Opioid Treatment Agreement measure is worth a full 5 bonus points (not up to 5 bonus points) in CY 2019.
4. Health Information Exchange Objective: Support Electronic Referral Loops by Receiving and Incorporating Health Information
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41661), we finalized the Support Electronic Referral Loops by Receiving and Incorporating Health Information measure. Although the numerator and denominator of the measure state that CEHRT must be used (83 FR 41661), we inadvertently omitted a reference to the use of CEHRT from the measure description in the regulations at § 495.24(e)(6)(ii)(B). In addition, we stated at 83 FR 41660 that an eligible hospital or CAH must use the capabilities and standards for CEHRT at 45 CFR 170.315(b)(1) and (b)(2).
In an effort to more clearly capture the previously established policy, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19559), we proposed to revise the regulations for the Support Electronic Referral Loops by Receiving and Incorporate Health Information measure. We proposed to revise § 495.24(e)(6)(ii)(B) to provide that the electronic summary of care record must be received using CEHRT and that clinical information reconciliation for medication, medication allergy, and current problem list must be conducted using CEHRT.
Comment: Commenters supported our proposal and appreciated the effort CMS puts forth to keep language clear and expectations precise. They shared that the proposal reflects how eligible hospitals and CAHs have interpreted and implemented the measure requirements.
Response: We thank commenters for their support.
Comment: Several commenters raised issues not related to the proposal for this measure, including separating the two elements of the measure and creating two separate measures, requesting that the measure be a yes/no measure, and removing the requirements to reconcile medication, medication allergy, and current problem list.
Response: We appreciate this input and may take it under consideration in future rulemaking.
Comment: A commenter requested clarification as to whether the requirement that clinical information reconciliation must be conducted using CEHRT under the Support Electronic Referral Loops by Receiving and Incorporating Health Information measure is applicable only to the HIE objective within the Medicare Promoting Interoperability Program.
Response: Our proposal was only applicable to the Support Electronic Referral Loops by Receiving and Incorporating Health Information measure under § 495.24(e)(6)(ii)(B) for the Medicare Promoting Interoperability Program.
After consideration of the public comments we received, we are finalizing the proposed revisions to § 495.24(e)(6)(ii)(B) as proposed.
5. Changes to the Scoring Methodology for Eligible Hospitals and CAHs Attesting to CMS Under the Medicare Promoting Interoperability Program for an EHR Reporting Period in CY 2020
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41636 through 41668), we finalized under § 495.24(e) a new performance-based scoring methodology and changes to the objectives and measures for eligible hospitals and CAHs that submit an attestation to CMS under the Medicare Promoting Interoperability Program beginning with the EHR reporting period in CY 2019. For more information, we refer readers to that final rule (83 FR 41636 through 41668) and § 495.24(e). As previously discussed in sections VIII.D.3. and 4. of the preamble of this final rule, we are finalizing our proposals for CY 2020 to: (1) Remove the Verify Opioid Treatment Agreement Measure; (2) continue the Query of PDMP measure as optional with 5 bonus points; and (3) make the maximum points available for the e-Prescribing measure 10 points.
This table reflects the policies that we are finalizing for the objectives, measures, and maximum points available for the EHR reporting period in CY 2020. The maximum points available per measure do not include points that would be redistributed in the event that an exclusion is claimed.

6. Clinical Quality Measurement for Eligible Hospitals and Critical Access Hospitals (CAHs) Participating in the Medicare and Medicaid Promoting Interoperability Programs
a. Background and Current CQMs
Under sections 1814(l)(3)(A), 1886(n)(3)(A), and 1903(t)(6)(C)(i)(II) of the Act and the definition of “meaningful EHR user” under 42 CFR 495.4, eligible hospitals and CAHs must report on clinical quality measures (referred to as CQMs) selected by CMS using CEHRT, as part of being a meaningful EHR user under the Medicare and Medicaid Promoting Interoperability Programs.
This table lists the CQMs available for eligible hospitals and CAHs to report under the Medicare and Medicaid Promoting Interoperability Programs beginning with the reporting period in CY 2020 (83 FR 41670 through 41671).

b. Additional CQMs for Reporting Periods Beginning With CY 2021
As we have stated previously in rulemaking (82 FR 38479), we plan to continue to align the CQM reporting requirements for the Promoting Interoperability Programs with similar requirements under the Hospital IQR Program. To do this in a way that would minimize burden, while maintaining a set of meaningful clinical quality measures and continuing to incentivize improvement in the quality of care provided to patients, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19560 through 19561), we proposed to adopt two new opioid-related clinical quality measures and sought comments on whether we should consider proposing to adopt the Hybrid Hospital-Wide Readmission (HWR) Measure with Claims and EHR Data in future rulemaking for the Promoting Interoperability Program.
In the proposed rule, we proposed to add the following two opioid-related CQMs to the Promoting Interoperability Program measure set, beginning with the reporting period in CY 2021: (1) Safe Use of Opioids—Concurrent Prescribing CQM (NQF #3316e) and (2) Hospital Harm—Opioid-Related Adverse Events eCQM. We also proposed to adopt these measures under the Hospital IQR Program, and we refer readers to the discussion of the Hospital IQR Program in sections VIII.A.5.a. of the preamble of this final rule.
In the proposed rule, we acknowledged that some stakeholders have expressed concern that some providers could withhold the use of naloxone for patients who are in respiratory depression, believing it may help providers to avoid poor performance on the proposed Hospital Harm—Opioid-Related Adverse Events CQM (84 FR 19479 through 19480). Therefore, we solicited public comment on the potential of this measure to disincentivize the appropriate use of naloxone in the hospital setting, or, for the withholding of opioids where they are clinically necessary, such as with patients requiring palliative care or those who are considered end of life, out of an overabundance of caution.
Comment: Several commenters applauded the proposed alignment between the Hospital IQR Program and the Promoting Interoperability Program on the two opioid-related CQM policies; (1) Safe Use of Opioids—Concurrent Prescribing and (2) Hospital Harm—Opioid-Related Adverse Events eCQM.
Response: We appreciate commenters' support for the proposed alignment between the Hospital IQR Program and the Promoting Interoperability Program on the two opioid-related CQM policies. Together, we want to ensure that we continue to minimize burden while maintaining a set of meaningful CQMs that will ultimately improve the quality of care provided to patients.
Comment: Many commenters are supportive of the proposal to include the two new opioid CQMs. Of the reasons given, several state that these CQMs will aid in reducing opioid related adverse events, it will provide a richer picture into clinical care, and they will aid in assessing the high priority opioid epidemic.
Response: We thank commenters for their overwhelming support as we continue to align the Hospital IQR Program and the Promoting Interoperability Program on the opioid related policies CQM policies. We agree with commenters that the Safe Use of Opioids—Concurrent Prescribing CQM will aid in reducing opioid related adverse events, it will provide a richer picture into clinical care, and they will aid in assessing the high priority opioid epidemic. Together, we want to ensure that we continue to minimize burden for the Hospital IQR Program and the Promoting Interoperability Program while maintaining a set of meaningful CQMs that will ultimately improve the quality of care provided to patients.
Comment: A commenter suggested that CMS define and implement a long-term plan for PDMP and EHR integration before adding new CQMs.
Response: We thank the commenter for their feedback. PDMP systems comprise various processes and components that vary significantly across state lines, and in any given state, the PDMP system may include varying levels of state-developed and/or vendor-based solutions along with the core PDMP database. State laws and policies also differ on data storage and usage, access roles and disclosures, and key definitions. The degree of PDMP and health IT (EHR, HIE, PDS) access integration (how the provider can access the PMDP) varies significantly both across and within state lines, by product and/or health system. CMS is continuously working with various stakeholders and the ONC to evaluate the implementation of the Support for Patients and Communities Act and the readiness of a standardized, integrated PDMP into EHRs.
Additionally, The Safe Use of Opioids—Concurrent Prescribing CQM does not require the use of PDMP and EHR integration. The goal of The Safe Use of Opioids—Concurrent Prescribing CQM is to is intended to facilitate safer patient care not only by promoting adherence to recommended clinical guidelines on concurrent prescribing practices, but also in incentivizing hospitals to develop strategies to identify and monitor patients on concurrent opioid and opioid-benzodiazepine prescriptions, who might be at higher risk of adverse drug events. We do not believe that adding The Safe Use of Opioids—Concurrent Prescribing CQM should wait until PDMPs and EHRs are universally integrated, as this measure seeks to promote safer prescribing practices and incentivize providers to recognize and identify high-risk patients with concurrent regimens; these strategies may help combat the negative effects of the opioid crisis.
Comment: Several commenters requested that CMS extend timeframes for mandating the proposed CQMs until each is fully endorsed by the NQF, to avoid any unforeseen consequences from implementation. Further, the general consensus is that until measure specifications have been clearly defined, the CQMs should not be made mandatory.
Response: We refer readers to section XIII.A.5.a.(1). of the preamble of this final rule where we discuss the adoption of the Safe Use of Opioids—Concurrent Prescribing CQM and how this measure was tested for feasibility, reliability, and validity and received NQF endorsement. We believe adding the Safe Use of Opioids—Concurrent Prescribing CQM to the CQM measure set beginning in CY 2021 for reporting and requiring eligible hospitals and CAHs to report on the Safe Use of Opioids—Concurrent Prescribing CQM beginning with the CY 2022 reporting period is an appropriate timeframe because it will afford hospitals and vendors sufficient time to work through implementation, testing, and reporting challenges.
With regard to the Hospital Harm—Opioid-Related Adverse Events CQM, the NQF Patient Safety Standing Committee was concerned about using naloxone as a proxy for harm in the numerator and including all patients admitted to the hospital in the denominator, rather than limiting the denominator to only patients that have been administered opioids by the hospital. With respect to commenters' concerns, and with the NQF Patient Safety Standing Committee voting to not endorse this measure, we are not finalizing our proposal to adopt the Hospital Harm—Opioid-Related Adverse Events CQM for the Promoting Interoperability Program. For a complete discussion of the reasons why we are not adopting the Hospital Harm—Opioid-Related Adverse Events CQM, we refer readers to section XIII.A.5.a.(1). of the preamble of this final rule.
Comment: Several commenters requested clarification on the Safe Use of Opioids—Concurrent Prescribing CQM's definition.
Response: In the proposed rule, we provided readers with a link to NQF's Patient Safety, Fall 2017 Cycle: CDP Report (84 FR 19477), where the measure specifications for the Safe Use of Opioids—Concurrent Prescribing CQM can be found. We further note that measure specifications can be found on the eCQI Resource Center,[2] which provides a centralized location for news, information, tools, and standards related to CQMs. For a more complete discussion of this measure, we refer readers to section XIII.A.5.a. (1). of the preamble of this final rule.
Comment: One commenter expressed concerns with including the Emergency department setting in the Safe Use of Opioids—Concurrent Prescribing CQM. Specifically, it was mentioned that in Emergency medicine, the goal is to provide short-term, life-saving care to patients, with the intention of those patients following-up with primary care. Given this unique environment, the commenter stated that there are instances where concurrent prescription of multiple opioids, or an opioid and benzodiazepine, would be clinically appropriate. Further, the commenter expressed a larger concern that providers may withhold clinically appropriate treatment based on misinterpretations of the measure.
Response: Because this measure was proposed and is being finalized under the Hospital IQR Program, we believe it is appropriate to focus on inpatient stays. Specifically, there may be occasions in which patients admitted to the emergency department or for observation stays are not ultimately admitted as inpatients. We agree that those patients should be excluded from the measure and this was our intent in the proposed rule; however, the technical specifications referenced in the proposed rule were overbroad and not clearly consistent with the proposal. The Safe Use of Opioids—Concurrent Prescribing CQM was developed with broader specifications with flexibility in mind. Specifically, the measure, as initially developed, captured both encounters from the hospital outpatient and inpatient settings so that it could be implemented in either setting, with program implementation in either the Hospital Outpatient Quality Reporting (OQR) Program and/or the Hospital IQR Program/Promoting Interoperability Program to be determined at a later date.
We have made this minor refinement to the technical specifications to address confusion about which emergency department or observation stay encounters are included in the measure for implementation in the Promoting Interoperability Program and Hospital IQR Program, which are available here at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms. For a more detailed discussion of the Safe Use of Opioids—Concurrent Prescribing CQM clarification to emergency department or observation stay encounters, we refer readers to section XIII.A.5.a. (1). of the preamble of this final rule.
After consideration of the public comments, we are finalizing our proposal to add the Safe Use of Opioids—Concurrent Prescribing CQM to the Promoting Interoperability Program measure set, beginning with the reporting period in CY 2021. We are not finalizing the proposed addition of the Hospital Harm—Opioid-Related Adverse Events CQM.
c. Request for Information (RFI) Regarding Potential Adoption of the Hybrid Hospital-Wide Readmission (HWR) Measure With Claims and EHR Data (Hybrid HWR Measure) for Reporting Periods Beginning With CY 2023
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19561), we made a Request for Information regarding whether we should consider proposing to adopt the Hybrid Hospital-Wide Readmission (HWR) measure with claims and EHR data (also known as the Hybrid HWR measure) in future rulemaking for the Promoting Interoperability Program starting with the reporting period in CY 2023. While we are not summarizing and responding to the comments we received in this final rule, we thank the commenters for their responses and we will take them it account as we develop future policies for the Promoting Interoperability Program.
d. CQM Reporting Periods and Criteria for the Medicare and Medicaid Promoting Interoperability Programs in CY 2020, 2021, and 2022
(1) CQM Reporting Periods and Criteria in CY 2020 and 2021
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19561 through 19562), for CY 2020 and 2021, we proposed generally the same CQM reporting periods and criteria as established in the FY 2019 IPPS/LTCH PPS final rule for the Medicare and Medicaid Promoting Interoperability Programs in CY 2019 (83 FR 41671). We proposed that the CQM reporting period and criteria under the Medicare and Medicaid Promoting Interoperability Programs for eligible hospitals and CAHs reporting CQMs electronically would be as follows: For eligible hospitals and CAHs participating only in the Promoting Interoperability Program, or participating in the both Promoting Interoperability Program and the Hospital IQR Program, report one, self-selected calendar quarter of data for four self-selected CQMs from the set of available CQMs. We proposed the following reporting criteria for eligible hospitals and CAHs that report CQMs by attestation under the Medicare Promoting Interoperability Program as a result of electronic reporting not being feasible—report on all CQMs from the set of available CQMs. For eligible hospitals and CAHs that report CQMs by attestation, we previously established a CQM reporting period of the full CY (consisting of 4 quarterly data reporting periods) (80 FR 62893).
We proposed a submission period for the Medicare Promoting Interoperability Program that would be the 2 months following the close of the calendar year, ending February 28, 2021 (for the CQM reporting period in CY 2020) and February 28, 2022 (for the CQM reporting period in CY 2021). With regard to the Medicaid Promoting Interoperability Program, we provided States with the flexibility to determine the method of reporting CQMs (attestation or electronic reporting) and the submission periods for reporting CQMs, subject to prior approval by CMS.
We stated that we believe that continuing the same CQM reporting and submission requirements is appropriate because it continues to offer hospitals reporting flexibility and does not increase the information collection burden on data submitters. In addition, we stated that alignment with the requirements of the Hospital IQR Program reduces burden for hospitals as they may report once and fulfill the requirements of both programs.
Comment: Many commenters expressed overwhelming support for the proposals including reporting one self-selected calendar quarter of data for four self-selected CQMs; aligning with the requirements of the Hospital IQR Program; and submitting data during the 2 months following the close of the calendar year. We note that several commenters appreciated and supported the consistency of the proposed CQM reporting and submission requirements. A commenter was appreciative of CMS extending the requirement of 4 self-selected CQMs for 1 calendar quarter through CY2021, as it has been challenging for EMR vendors and hospitals to respond in an efficient manner due to ongoing CMS maintenance and updates. Another commenter was grateful for CMS' sensitivity to provider burden, by focusing on measures and efforts that support CQMs. Commenters have expressed sincere gratitude that CMS has provided advanced notification and program consistency. Lastly, a commenter supported the continuation of these reporting requirements, as this will aid hospitals in the data extraction processes while providing flexibility and supporting the ultimate goal of creating a more efficient and seamless electronic collection and submission process for quality measures.
Response: We thank all the commenters for their overwhelming support of our proposals. As we align with the Hospital IQR Program CQMs, we want to continue to offer eligible hospitals and CAHs reporting flexibility and decreased data collection burden.
After consideration of public comments, we are finalizing all of the proposals for the CQM reporting periods, reporting criteria, and submission periods for CY 2020 and 2021 as proposed.
(2) CQM Reporting Periods and Criteria in CY 2022
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19562), for CY 2022, we proposed that the CQM reporting period and criteria under the Medicare Promoting Interoperability Program for eligible hospitals and CAHs reporting CQMs electronically would be as follows—for eligible hospitals and CAHs participating only in the Promoting Interoperability Program or participating in both the Promoting Interoperability Program and in the Hospital IQR Program, report one, self-selected calendar quarter of data for: (1) Three self-selected CQMs from the set of available CQMs; and (2) the proposed Safe Use of Opioids—Concurrent Prescribing CQM (NQF #3316e), for a total of four CQMs. Under this proposal, we would not change the number of CQMs that hospitals must report while ensuring that health care providers still have meaningful choice among the set of available CQMs. We proposed the following reporting criteria for eligible hospitals and CAHs that report CQMs by attestation under the Medicare Promoting Interoperability Program as a result of electronic reporting not being feasible—report on all CQMs from the set of available CQMs. For eligible hospitals and CAHs that report CQMs by attestation, we previously established a CQM reporting period of the full CY (consisting of 4 quarterly data reporting periods) (80 FR 62893).
We proposed that the submission period for the Medicare Promoting Interoperability Program would be the 2 months following the close of the calendar year 2022, ending February 28, 2023.
We also refer readers to section VIII.A.10.d. of the preamble of this final rule for the reporting and submission requirements associated with the proposal to add the Safe Use of Opioids—Concurrent Prescribing CQM (NQF #3316e) to the measure set for the Hospital IQR Program.
Comment: A few commenters have expressed support for the proposal that the submission period would be the 2 months following the close of the calendar year 2022, ending February 28, 2023.
Response: Thank you to all commenters for the valuable input. In an effort to decrease data collection and hospital burden, and so that we continue to align with the Hospital IQR Program, we are pleased to have such support from the public.
Comment: Many commenters, while fully supportive of the intent and introduction of the Safe Use of Opioids—Concurrent Prescribing CQM, have expressed concern with making this a required measure in CY 2022. Of the concerns, a few commenters have stated that as a new measure, adequate time is necessary to allow for vendors and eligible hospitals and CAHs to prepare and test its use, as well as make any necessary adjustments, and two years is not enough time for this to be done. One commenter had a concern that CMS needs to ensure that hospitals and CAHs are allowed an adequate amount of time in order to develop and execute validity testing. A couple commenters shared concern that additional time would be needed to develop the technology necessary to support reporting on such a measure, as implementation challenges often arise with new measures and the lag between data collection and reporting.
Alongside these concerns, the overarching suggestion is to include the Safe Use of Opioids—Concurrent Prescribing CQM in the measure set, but not require it until CY 2023. This would allow for one additional year to ensure that the technology has been fully developed, and successful validation testing has been completed. Lastly, a commenter suggested that as an alternative to requiring all hospitals to report on the new CQM in CY 2022, CMS should instead consider incentivizing organizations to report the measure by offering bonus points.
Response: We thank all commenters for sharing and expressing their concerns, and offering suggestions. We further note that the measure specifications for the measure can also be found on the eCQI Resource Center,[922] which provides a centralized location for news, information, tools, and standards related to CQMs.[923] We believe requiring the reporting of the Safe Use of Opioids—Concurrent Prescribing CQM beginning with the reporting period in CY 2022 will provide sufficient time to work through implementation, testing, and reporting challenges. We refer readers to section XIII.A.5.a.(1). of the preamble of this final rule for a discussion of how this measure was tested for feasibility, reliability, and validity and received NQF endorsement. We understand that many hospitals work with vendors to implement measure specifications in their EHRs, and we believe that the proposed timeline for required reporting of the Safe Use of Opioids—Concurrent Prescribing CQM—the CY 2022 reporting period—will allow hospitals and vendors time to work through implementation, testing, and reporting challenges before reporting on the measure to CMS is required.
After consideration of public comments, we are finalizing all of the proposals for the CQM reporting periods, reporting criteria, and submission periods for CY 2022 as proposed.
e. CQM Reporting Form and Method Requirements for the Medicare Promoting Interoperability Program in CY 2020
(1) Requiring EHR Technology to be Certified to All Available CQMs
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19562), we proposed to continue requiring that EHRs be certified to all available CQMs adopted for the Medicare Promoting Interoperability Program for CY 2020 and subsequent years. This policy was previously finalized in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38483 through 38485) for CY 2018 and in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41671 through 41672) for CY 2019. Because this is the current policy for the Hospital IQR and Medicare Promoting Interoperability Programs, vendors and health care providers should be familiar with this requirement, and their EHR systems should already be certified to all currently available CQMs.
Comment: Several commenters supported our proposal to require that EHR technology used for CQM reporting be certified to all CQMs. A number of those commenters expressed appreciation for this policy and shared that it helps preserve hospitals' ability to choose CQMs which reflect their patient populations and quality improvement goals.
Response: We thank the commenters for their support of our proposal and believe that it gives eligible hospitals and CAHs flexibility to report on any of the CQMs available instead of being limited to those that their vendor chooses to have certified.
After consideration of public comments, we are finalizing our proposal to continue requiring that EHRs be certified to all available CQMs adopted for the Medicare Promoting Interoperability Program for CY 2020 and subsequent years.
(2) Other CQM Form and Method Requirements
As we stated in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49759 through 49760), for the reporting periods in 2016 and future years, we are requiring QRDA-I for CQM electronic submissions for the Medicare EHR Incentive (now the Promoting Interoperability) Program. As noted in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49760), States would continue to have the option, subject to our prior approval, to allow or require QRDA-III for CQM reporting.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19562 through 19563), for the reporting period in CY 2020, we proposed the following for CQM submission under the Medicare Promoting Interoperability Program:
- Eligible hospitals and CAHs participating in the Medicare Promoting Interoperability Program (single program participation)—electronically report CQMs through QualityNet Portal.
- Eligible hospital and CAH options for electronic reporting for multiple programs (that is, Promoting Interoperability Program and Hospital IQR Program participation)—electronically report through QualityNet Portal.
As noted in the 2015 EHR Incentive Programs final rule (80 FR 62894), starting in 2018, eligible hospitals and CAHs participating in the Medicare EHR Incentive Program must electronically report CQMs where feasible; and attestation to CQMs will no longer be an option except in certain circumstances where electronic reporting is not feasible. For the Medicaid Promoting Interoperability Program, States continue to be responsible for determining whether and how electronic reporting of CQMs would occur, or if they wish to allow reporting through attestation. Any changes that States make to their CQM reporting methods must be submitted through the State Medicaid Health IT Plan (SMHP) process for CMS review and approval prior to being implemented.
For CY 2020, we proposed to continue our policy regarding the electronic submission of CQMs, which requires the use of the most recent version of the CQM electronic specification for each CQM to which the EHR is certified. For the CY 2020 electronic reporting of CQMs, we stated that this means eligible hospitals and CAHs are required to use the 2018 CQM specifications update (published in May 2018) and any applicable addenda available on the eCQI Resource Center web page at: https://ecqi.healthit.gov/. For the CY 2020 electronic reporting of CQMs, we have published an updated version and requiring eligible hospitals and CAHs to use the 2019 CQM specifications update (published in May 2019 and any applicable addenda available on the eCQI Resource Center web page at: https://ecqi.healthit.gov/. As noted in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41635 through 41636), participants are required to use 2015 Edition CEHRT for the Medicare and Medicaid Promoting Interoperability Programs, beginning with the EHR reporting period in CY 2019. We reiterated that an EHR certified for CQMs under the 2015 Edition certification criteria does not have to be recertified each time it is updated to a more recent version of the CQMs (82 FR 38485).
Comment: A commenter appreciated the ability to report CQMs once and have the submission fulfill both the Hospital IQR requirement and the Promoting Interoperability Program requirements.
Response: We thank the commenter for their support and believe that the alignment between the Hospital IQR requirement and the Promoting Interoperability Program alleviates burden for eligible hospitals and CAHs.
Comment: A commenter shared support for the proposal that requires the use of the most recent version of the CQM electronic specification for each CQM to which the EHR is certified and appreciated that we were specifying in rulemaking.
Response: We appreciate commenter support for using the most recent version of the CQM electronic specifications and believe that not requiring recertification of CEHRT every time that the specifications are updated with alleviate burden for eligible hospitals and CAHs.
Comment: A commenter appreciated CMS' recognition and response to the challenges regarding feasibility of electronically submitted measures. They believe that maintaining the reduced reporting burden through CY 2021 would provide consistency and predictability while allowing hospitals additional time and bandwidth needed to address present challenges.
Response: We thank the commenters for their support of our proposal and agree that establishing the requirements for through 2021 gives eligible hospitals and CAHs the ability to plan for the future.
After consideration of the public comments we received, we are finalizing the following for CQM submission under the Medicare Promoting Interoperability Program for the reporting period in CY 2020:
- Eligible hospitals and CAHs participating in the Medicare Promoting Interoperability Program (single program participation)—electronically report CQMs through QualityNet Portal.
- Eligible hospital and CAH options for electronic reporting for multiple programs (that is, Promoting Interoperability Program and Hospital IQR Program participation)—electronically report through QualityNet Portal.
Additionally, we are finalizing the proposal to continue our policy for CY 2020 regarding the electronic submission of CQMs, which requires the use of the most recent version of the CQM electronic specification for each CQM to which the EHR is certified.
(3) Modification to Reporting Methods for CQMs Beginning With the Reporting Period in CY 2023
We currently allow eligible hospitals and CAHs to report CQMs by attestation for the Medicare Promoting Interoperability Program only in certain circumstances where electronic reporting is not feasible (80 FR 62893 through 62894). In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19563), beginning with the CQM reporting period in CY 2023, we proposed to eliminate attestation as a method for reporting CQMs for the Medicare Promoting Interoperability Program and instead require all eligible hospitals and CAHs to submit their CQM data electronically through the reporting methods available for the Hospital IQR Program. We stated that we believe that data submitted electronically is preferable so that we can use the data to analyze trends across hospitals and further refine quality data in the future. We stated that limiting the available reporting methods to electronic submission would enable us to have a more robust data set so that we can ensure that hospitals are delivering effective, safe, efficient, patient-centered, equitable, and timely care. Also, we stated that we are allowing an adequate transition period for eligible hospitals and CAHs to migrate to electronic submission.
Comment: A commenter supported the proposed modification to reporting methods for CQMs beginning with the reporting period in CY 2023.
Response: We thank the commenter for their supportive feedback and believe that by CY 2023 all eligible hospitals and CAHs should be able to submit their data electronically.
Comment: A commenter agrees that while most hospitals and CAHs have the capacity for electronic reporting of CQMs, they believe CMS should retain a hardship exception process for unanticipated situations where they are unable to submit or report CQMs electronically.
Response: For the Medicare Promoting Interoperability Program we do offer hardship exceptions for extreme and uncontrollable circumstances.
After consideration of the public comments we received, we are finalizing our proposal to eliminate attestation as a method for reporting CQMs for the Medicare Promoting Interoperability Program and instead require all eligible hospitals and CAHs to submit their CQM data electronically through the reporting methods available for the Hospital IQR Program beginning with the CQM reporting period in CY 2023.
7. Future Direction of the Promoting Interoperability Program
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19563 through 19569), we made Requests for Information regarding several issues involving the Promoting Interoperability Program. While we are not summarizing and responding to the comments we received in this final rule, we thank the commenters for their responses and we will take them it account as we develop future policies for the Promoting Interoperability Program.
IX. MedPAC Recommendations
Under section 1886(e)(4)(B) of the Act, the Secretary must consider MedPAC's recommendations regarding hospital inpatient payments. Under section 1886(e)(5) of the Act, the Secretary must publish in the annual proposed and final IPPS rules the Secretary's recommendations regarding MedPAC's recommendations. We have reviewed MedPAC's March 2019 “Report to the Congress: Medicare Payment Policy” and have given the recommendations in the report consideration in conjunction with the policies set forth in this final rule. MedPAC recommendations for the IPPS for FY 2020 are addressed in Appendix B to this final rule.
For further information relating specifically to the MedPAC reports or to obtain a copy of the reports, contact MedPAC at (202) 653-7226, or visit MedPAC's website at: http://www.medpac.gov.
X. Other Required Information
A. Publicly Available Files
IPPS-related data are available on the internet for public use. The data can be found on the CMS website at: http://www.cms.hhs.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. We listed the data files available in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19570 through 19571).
Commenters interested in discussing any data files used in construction of this final rule should contact Michael Treitel at (410) 786-4552.
B. Collection of Information Requirements
1. Statutory Requirement for Solicitation of Comments
Under the Paperwork Reduction Act (PRA) of 1995, we are required to provide 60-day notice in the Federal Register and solicit public comment before a collection of information requirement is submitted to the Office of Management and Budget (OMB) for review and approval. In order to fairly evaluate whether an information collection should be approved by OMB, section 3506(c)(2)(A) of the PRA of 1995 requires that we solicit comment on the following issues:
- The need for the information collection and its usefulness in carrying out the proper functions of our agency.
- The accuracy of our estimate of the information collection burden.
- The quality, utility, and clarity of the information to be collected.
- Recommendations to minimize the information collection burden on the affected public, including automated collection techniques.
In the FY 2020 IPPS/LTCH PPS proposed rule, we solicited public comment on each of these issues for the following sections of this document that contain information collection requirements (ICRs).
2. ICRs for Application for GME Resident Slots
The information collection requirements associated with the preservation of resident cap positions from closed hospitals, addressed in section IV.J.3. of the preamble of the proposed rule and this final rule are not subject to the Paperwork Reduction Act, as stated in section 5506 of the Affordable Care Act, included at section 1886(h)(4)(H)(vi)(V) of the Act.
3. ICRs for the Hospital Inpatient Quality Reporting (IQR) Program
a. Background
The Hospital IQR Program (formerly referred to as the Reporting Hospital Quality Data for Annual Payment Update (RHQDAPU) Program) was originally established to implement section 501(b) of the MMA, Public Law 108-173. OMB has currently approved 2,520,100 hours of burden and approximately $92.2 million under OMB Control Number 0938-1022, accounting for information collection burden experienced by 3,300 IPPS hospitals and 1,100 non-IPPS hospitals for the FY 2021 payment determination. In this final rule, we describe the burden changes with regard to collection of information under OMB Control Number 0938-1022 (expiration date February 28, 2022) for IPPS hospitals due to the policies in the proposed rule and this final rule.
In section VIII.A.5.b. of the preamble of this final rule, we are adopting the Hybrid Hospital-Wide Readmission Measure with Claims and Electronic Health Record Data (Hybrid HWR measure) (NQF #2879) as we proposed, in a stepwise approach, beginning with 2 years of voluntary reporting which will run from July 1, 2021 through June 30, 2022, and from July 1, 2022 through June 30, 2023, before requiring reporting of the measure for the reporting period that will run from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination and subsequent years. We are also adopting reporting and submission requirements for the Hybrid HWR measure. We expect these policies will affect our collection of information burden estimates. Details on these policies, as well as the expected burden changes, are discussed further in this final rule.
In section VIII.A. of the preamble of this final rule, we are: (1) Adopting the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination with a clarification and update; (2) removing the claims-only version of the Hospital-Wide All-Cause Readmission measure beginning with the FY 2026 payment determination; (3) extending the current eCQM reporting and submission requirements for the CY 2020 reporting period/FY 2022 payment determination and CY 2021 reporting period/FY 2023 payment determination; (4) changing the eCQM reporting and submission requirements for the CY 2022 reporting period/FY 2024 payment determination, such that hospitals will be required to report one, self-selected calendar quarter of data for: (a) Three self-selected eCQMs, and (b) the finalized Safe Use of Opioids—Concurrent Prescribing eCQM, for a total of four eCQMs; and (5) continuing the requirement that EHRs be certified to all available eCQMs used in the Hospital IQR Program for the CY 2020 reporting period/FY 2022 payment determination and subsequent years. We are not finalizing our proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM. As discussed further in this final rule, we do not expect these policies to affect our information collection burden estimates.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38501 through 38504) and FY 2019 IPPS/LTCH PPS final rule (83 FR 41689 through 41694), we estimated that reporting measures for the Hospital IQR Program could be accomplished by staff with a median hourly wage of $18.29 per hour. We note that since then, more recent wage data have become available, and we are updating the wage rate used in these calculations in this final rule. The most recent data from the Bureau of Labor Statistics reflects a median hourly wage of $18.83 per hour for a Medical Records and Health Information Technician professional.[924] We calculated the cost of overhead, including fringe benefits, at 100 percent of the median hourly wage, consistent with previous years. This is necessarily a rough adjustment, both because fringe benefits and overhead costs vary significantly by employer and methods of estimating these costs vary widely in the literature. Nonetheless, we believe that doubling the hourly wage rate ($18.83 × 2 = $37.66) to estimate total cost is a reasonably accurate estimation method. Accordingly, we will calculate cost burden to hospitals using a wage plus benefits estimate of $37.66 per hour throughout the discussion in this final rule for the Hospital IQR Program.
b. Information Collection Burden Estimate for the Adoption of One eCQM Beginning With the CY 2021 Reporting Period/FY 2023 Payment Determination
In section VIII.A.5.a. of the preamble of this final rule, we are adopting the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination with a clarification and update. We are not finalizing our proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM.
We do not believe that adding one new eCQM to the measure set will affect the information collection burden of submitting information to CMS under the Hospital IQR Program. As discussed in section VIII.A.10.d.(2) and (3) of the preamble of this final rule, we are extending, for the CYs 2020 and 2021 reporting periods/FYs 2022 and 2023 payment determinations, our current eCQM reporting requirements, which require hospitals to submit one self-selected calendar quarter of data for four self-selected eCQMs each year. The Safe Use of Opioids—Concurrent Prescribing eCQM will be added to the eight available eCQMs in the eCQM measure set from which hospitals may choose to report in order to satisfy these requirements.[925] In other words, while this new measure will be added to the eCQM measure set, hospitals will not be required to report more than a total of four eCQMs as currently required. Therefore, we do not expect the adoption of this measure to impact our collection of information estimates. However, we refer readers to section I.K. of Appendix A of this final rule for a discussion of the potential costs associated with the implementation of a new eCQM that are not strictly related to information collection burden.
c. Information Collection Burden Estimate for the Voluntary Reporting Periods and Subsequent Required Submission of the Hybrid Hospital-Wide Readmission Measure With Claims and Electronic Health Record Data (Hybrid HWR Measure)
In section VIII.A.5.b. of the preamble of this final rule, as we proposed, we are establishing two additional voluntary reporting periods for the Hybrid Hospital-Wide Readmission Measure with Claims and Electronic Health Record Data (NQF #2879) (Hybrid HWR measure). The first voluntary reporting period will run from July 1, 2021 through June 30, 2022, and the second will run from July 1, 2022 through June 30, 2023. We also are requiring reporting of the Hybrid HWR measure immediately thereafter and for subsequent years, beginning with the reporting period which runs from July 1, 2023 through June 30, 2024 and which will affect the FY 2026 payment determination.
As a hybrid measure, this measure uses both claims-based data and EHR data, specifically, a set of core clinical data elements consisting of vital signs and laboratory test information and patient linking variables collected from hospitals' EHR systems. We do not expect any additional burden to hospitals to report the claims-based portion of this measure because these data are already reported to the Medicare program for payment purposes.
However, we do expect that hospitals will experience burden in reporting the EHR data. To report the EHR data, as discussed earlier in this final rule, we are providing that hospitals will use the same submission process required for eCQM reporting; specifically, these data will be required to be reported using QRDA I files submitted to the CMS data receiving system, and using EHR technology certified to the 2015 Edition of CEHRT. Accordingly, we expect the burden associated with the reporting of this measure to be similar to our estimates for eCQM reporting; that is, 10 minutes per measure, per quarter. Therefore, using the estimate of 10 minutes per measure per quarter (10 minutes × 1 measure × 4 quarters = 40 minutes), we estimate that this policy will result in a burden increase of 0.67 hours (40 minutes) per hospital per year. Beginning with the first voluntary reporting period, which runs from July 1, 2021 through June 30, 2022, we estimate an annual burden increase of 2,211 hours across participating hospitals (0.67 hours × 3,300 IPPS hospitals). Using the updated wage estimate as previously described, we estimate this to represent a cost increase of $83,266 ($37.66 hourly wage × 2,211 annual hours) across hospitals. We acknowledge that reporting during the first two years of this policy is voluntary, but we encourage all hospitals to submit data for the Hybrid HWR measure during these voluntary reporting periods. For that reason, our burden estimates are based on the assumption that all hospitals will participate across the two voluntary reporting periods (July 1, 2021 through June 30, 2022, and July 1, 2022 through June 30, 2023), the reporting period in which public reporting begins (July 1, 2023 through June 30, 2024), and subsequent reporting periods.
d. Information Collection Burden Estimate for Removal of Claims-Only Hospital-Wide All-Cause Readmission Measure (HWR Claims-Only Measure) Beginning with the FY 2026 Payment Determination
In section VIII.A.6. of the preamble of this final rule, as we proposed, we are removing the HWR claims-only measure, beginning with the FY 2026 payment determination when the Hybrid HWR measure begins to be publicly reported. Because the HWR claims-only measure is calculated using data that are already reported to the Medicare program for payment purposes, we do not anticipate that removing this measure will decrease our previously finalized burden estimates.
e. Information Collection Burden Estimates for Policies Related to eCQM Reporting and Submission Requirements
(1) Information Collection Burden Estimates for eCQM Reporting and Submission Requirements for the CYs 2020 and 2021 Reporting Periods/FYs 2022 and 2023 Payment Determinations
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41602 through 41607), we finalized eCQM reporting and submission requirements such that hospitals submit one, self-selected calendar quarter of data for four eCQMs in the Hospital IQR Program measure set for the CY 2019 reporting period/FY 2021 payment determination. Our related information collection estimates were discussed at 83 FR 41689 through 41694. In sections VIII.A.10.(d)(2) and (3) of the preamble of this final rule, we are extending the current requirements for 2 additional years, the CY 2020 reporting period/FY 2022 payment determination and the CY 2021 reporting period/FY 2023 payment determination. We believe there will be no change to the burden estimate due to these policies because the previous burden estimate of 40 minutes per hospital per year (10 minutes per record × 4 eCQMs × 1 quarter) associated with the eCQM reporting and submission requirements finalized for the CY 2019 reporting period/FY 2021 payment determination will also apply to the CY 2020 reporting period/FY 2022 payment determination and the CY 2021 reporting period/FY 2023 payment determination.
(2) Information Collection Burden Estimate for eCQM Reporting and Submission Requirements for the CY 2022 Reporting Period/FY 2024 Payment Determination
In section VIII.A.10.d.(4) of the preamble of this final rule, for the CY 2022 reporting period/FY 2024 payment determination, as we proposed, we are finalizing changing the eCQM reporting and submission requirements, such that hospitals will be required to report one, self-selected calendar quarter of data for: (1) Three self-selected eCQMs, and (2) the finalized Safe Use of Opioids—Concurrent Prescribing eCQM, for a total of four eCQMs. We note that the number of calendar quarters of data and total number of eCQMs required will remain the same. We believe there will be no change to the burden estimate because hospitals will still be required to submit one, self-selected calendar quarter of data for a total of four eCQMs in the Hospital IQR Program measure set.
(3) Information Collection Burden Estimate for Requirement That EHRs Be Certified to All Available eCQMs
In section VIII.A.10.d.(5)(B) of the preamble of this final rule, as we proposed, we are continuing to require that EHRs be certified to all available eCQMs in the Hospital IQR Program measure set for the CY 2020 reporting period/FY 2022 payment determination and subsequent years. We do not believe that hospitals will experience an increase in information collection burden associated with this policy because the use of EHR technology that is certified to all available eCQMs has been required for the Promoting Interoperability Program (83 FR 41672). However, we refer readers to section I.K. of Appendix A of this final rule for a discussion of the potential costs associated with this policy that are not strictly related to information collection burden.
f. Summary of Information Collection Burden Estimates for the Hospital IQR Program
In summary, under OMB Control Number 0938-1022, we estimate a total information collection burden increase of 2,211 hours associated with our policy to adopt the Hybrid Hospital-Wide All-Cause Readmission (Hybrid HWR) measure and a total cost increase related to this information collection of approximately $83,266 (which also reflects use of an updated hourly wage rate as previously discussed), beginning with the first voluntary reporting period which runs July 1, 2021 through June 30, 2022. These are the total changes to the information collection burden estimates. We will submit the revised information collection estimates to OMB for approval under OMB Control Number 0938-1022.

4. ICRs for PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program
a. Background
As discussed in sections VIII.B. of the preamble of the proposed rule and this final rule, section 1866(k)(1) of the Act requires, for purposes of FY 2014 and each subsequent fiscal year, that a hospital described in section 1886(d)(1)(B)(v) of the Act (a PPS-exempt cancer hospital, or a PCH) submit data in accordance with section 1866(k)(2) of the Act with respect to such fiscal year. There is no financial impact to PCH Medicare payment if a PCH does not participate.
We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41694 through 41696), the CY 2019 OPPS/ASC final rule with comment period ((83 FR 59149 through 59153), and OMB Control Number 0938-1175 for a detailed discussion of the most recently finalized burden estimates for the program requirements that we have previously adopted. In this final rule, we discuss only changes in burden that will result from the policies that we are finalizing in this final rule.
In the FY 2018 IPPS/LTCH PPS final rule, we finalized a proposal to utilize the median hourly wage rate, in accordance with the Bureau of Labor Statistics (BLS), to calculate our burden estimates going forward (82 FR 38505). The BLS describes Medical Records and Health Information Technicians as those responsible for organizing and managing health information data; therefore, we believe it is reasonable to assume that these individuals will be tasked with abstracting clinical data for submission for the PCHQR Program. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41695), we utilized a median hourly wage of $18.29 per hour.[926]
We note that, since then, more recent wage data have become available, and we are updating the wage rate used in these calculations. The most recent data from the Bureau of Labor Statistics reflects a median hourly wage of $18.83 [927] per hour for a Medical Records and Health Information Technician professional. We have finalized a policy to calculate the cost of overhead, including fringe benefits, at 100 percent of the mean hourly wage (82 FR 38505). This is necessarily a rough adjustment, both because fringe benefits and overhead costs vary significantly from employer-to-employer and because methods of estimating these costs vary widely from study-to-study. Nonetheless, we believe that doubling the hourly wage rate ($18.83 × 2 = $37.66) to estimate total cost is a reasonably accurate estimation method and allows for a conservative estimate of hourly costs. This approach is consistent with our previously finalized burden calculation methodology (82 FR 38505). Accordingly, we calculate cost burden to PCHs using a wage plus benefits estimate of $37.66 per hour throughout the discussion in this final rule.
b. Estimated Burden of New PCHQR Program Policies Beginning With the FY 2022 Program Year
(1) Removal of One Web-Based Structural Measure
As discussed in section VIII.B.4. of the preamble of this final rule, we are finalizing the removal of one web-based, structural measure beginning with the FY 2022 program year: External Beam Radiotherapy (EBRT) for Bone Metastases (formerly NQF #1822). As finalized in the FY 2019 IPPS/LTCH PPS final rule, we utilize a time estimate of 15-minutes per measure when assessing web-based and/or structural measures (83 FR 41694). As such, we estimate a reduction of 15 minutes per PCH, and a total annual reduction of approximately 3 hours for all 11 PCHs (.25 hour × 11 PCHs), due to the removal of this measure.
(2) New Quality Measure Beginning With the FY 2022 Program Year
In section VIII.B.5. of the preamble of this final rule, we are finalizing the adoption of the Surgical Treatment Complications for Localized Prostate Cancer claims-based measure beginning with the FY 2022 program year. Because this measure is claims based, we do not anticipate any increase in burden on PCHs related to our adoption of this measure, as it does not require facilities to submit any additional data.
c. Summary of Burden Estimates Related to the PCHQR Program for the FY 2022 Program Year
In summary, for our finalized policies to remove the External Beam Radiotherapy (EBRT) for Bone Metastases (formerly NQF #1822) measure and to adopt the Surgical Treatment Complications for Localized Prostate Cancer claims-based measure, we estimate an overall burden decrease of approximately 3 hours across all 11 PCHs. Coupled with our estimated salary costs, we estimate that these changes will result in a reduction in annual labor costs of approximately $113 (3 hours × $37.66 hourly labor cost) across the 11 PCHs beginning with the FY 2022 PCHQR Program. Further, the PCHQR Program measure set consists of 15 measures for the FY 2022 program year. The burden associated with these reporting requirements is currently approved under OMB control number 0938-1175. The information collection will be revised and submitted to OMB.
5. ICRs for the Hospital Value-Based Purchasing (VBP) Program
In section IV.H. of the preamble of this final rule, we discuss our proposed and finalized requirements for the Hospital VBP Program. Specifically, in this final rule, with respect to quality measures, we are calculating scores for the five NHSN HAI measures used in the Hospital VBP Program using the same data that the HAC Reduction Program uses for purposes of calculating NHSN HAI measure scores under that program, beginning on January 1, 2020 for CY 2020 measure data, which will apply to the Hospital VBP Program starting with data for the FY 2022 program year performance period. Because scores for these measures will be calculated using the same data that we use to calculate scores for the same measures in the HAC Reduction Program, there will be no new data collection burden associated with these measures under the Hospital VBP Program.
Comment: A few commenters noted a general belief that using the same administrative requirements that are used in the HAC Reduction Program will help reduce administrative burden associated with the programs.
Response: We thank commenters for their feedback.
6. ICRs for the Long-Term Care Hospital Quality Reporting Program (LTCH QRP)
In section VIII.C. of the preamble of this final rule, we are adopting two Transfer of Health Information quality measures as well as standardized patient assessment data elements (SPADEs) beginning with the FY 2022 LTCH QRP.
We estimate the data elements for the two Transfer of Health Information quality measures will take 1.5 minutes of clinical staff time to report data on discharge. We believe that the additional LTCH CARE Data Set data elements will be completed by registered nurses and licensed vocational nurses. Individual LTCHs determine the staffing resources necessary. We estimate 102,468 discharges from 415 LTCHs annually. This equates to an increase of 2,562 hours in burden for all LTCHs (0.025 hours × 102,468 discharges). Given 0.8 minutes of registered nurse time at $72.60 per hour and 0.7 minutes of licensed vocational nurse time at $45.24 per hour to complete an average of 247 sets of LTCH CARE Data Set assessments per provider per year, we estimated the total cost will be increased by $367.08 per LTCH annually, or $152,337 for all LTCHs annually. This increase in burden will be accounted for in the information collection under OMB control number 0938-1163 (Expiration Date: December 31, 2021).
We estimate the SPADEs will take 11.3 minutes of clinical staff time to report data on admission and 10.4 minutes of clinical staff time to report data on discharge, for a total of 21.7 minutes. We note that this is a decrease from the proposed 10.5 minutes on discharge because of the final decision in section VIII.C.7.f.(2)(b) of the preamble of this final rule. We believe that the additional LTCH CARE Data Set data elements will be completed by registered nurses and licensed vocational nurses. Individual LTCHs determine the staffing resources necessary. We estimate 102,468 discharges from 415 LTCHs annually. This equates to an increase of 37,093 hours in burden for all LTCHs (0.362 hours × 102,468 discharges). Given 11.4 minutes of registered nurse time at $72.60 per hour and 10.2 minutes of licensed vocational nurse time at $45.24 per hour to complete an average of 247 sets of LTCH CARE Data Set assessments per provider per year, we estimated the total cost will be increased by $5,308.21 per LTCH annually, or $2,202,906 for all LTCHs annually. This increase in burden will be accounted for in the information collection under OMB control number 0938-1163 (Expiration Date: December 31, 2021).
Overall, the changes added 11.3 minutes of clinical staff time to report data on admission and 11.9 minutes of clinical staff time to report data on discharge, for a total of 23.2 minutes. As a result, the cost associated with the changes to the LTCH QRP is estimated at $5,675.29 per LTCH annually or $2,355,243 for all LTCHs annually.
7. ICRs Relating to the Hospital-Acquired Condition (HAC) Reduction Program
In section IV.I. of the preamble of this final rule, we discuss proposed and finalized requirements for the HAC Reduction Program. In this final rule, we are not removing any measures or adopting any new measures into the HAC Reduction Program. The HAC Reduction Program has adopted six measures. We do not believe that the claims-based CMS PSI 90 measure in the HAC Reduction Program creates or reduces any burden for hospitals because it is collected using Medicare FFS claims hospitals are already submitting to the Medicare program for payment purposes. We note the burden associated with collecting and submitting data for the HAI measures (CDI, CAUTI, CLABSI, MRSA, and Colon and Abdominal Hysterectomy SSI) via the NHSN system is captured under a separate OMB control number, 0920-0666 (expiration November 30, 2021), and therefore will not impact our burden estimates.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41478 through 41484), we finalized our policy to validate NHSN HAI measures under the HAC Reduction Program, which will require hospitals to submit validation templates for the NHSN HAI measures beginning with Q3 CY 2020 discharges. We previously estimated that this policy will result in a net neutral shift of 43,200 hours and approximately $1,580,256.00 with no overall net increase in burden to the HAC Reduction Program (83 FR 41151). OMB has currently approved these 43,200 hours of burden and approximately $1.6 million under OMB control number 0938-1352 (expiration date January 31, 2021), accounting for information collection requirements experienced by 3,300 IPPS hospitals for FY 2021 program year.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41697), we used an hourly wage estimate of $18.29 per hour to estimate information collection costs.[928] We note that, since then, more recent wage data have become available, and we are finalizing our proposal to update the wage rate used in these calculation. The most recent data from the Bureau of Labor Statistics reflects a median hourly wage of $18.83 [929] per hour for a Medical Records and Health Information Technician professional. We calculate the cost of overhead, including fringe benefits, at 100 percent of the hourly wage estimate, as has been done under the Hospital IQR Program in the previous years (82 FR 38504 through 38505; 83 FR 41689 through 41690). This is necessarily a rough adjustment, both because fringe benefits and overhead costs vary significantly from employer-to-employer and because methods of estimating these costs vary widely from study-to-study. Nonetheless, we believe that doubling the hourly wage rate ($18.83 × 2 = $37.66) to estimate total cost is a reasonably accurate estimation method. Accordingly, we calculate cost burden to hospitals using a wage plus benefits estimate of $37.66 per hour.
We estimate a reporting burden of 80 hours (20 hours per record × 1 record per hospital per quarter × 4 quarters) per hospital selected for validation per year to submit the CLABSI and CAUTI templates, and 64 hours (16 hours per record × 1 record per hospital per quarter × 4 quarters) per hospital selected for validation per year to submit the MRSA and CDI templates. We estimate a total burden shift of 43,200 hours ([80 hours per hospital to submit CLABSI and CAUTI templates + 64 hours per hospital to submit MRSA and CDI templates] × 300 hospitals selected for validation) and approximately $1,626,912.00 (43,200 hours × $37.66 per hour [930] ) as a result of our policy to validate NHSN HAI data under the HAC Reduction Program. A nonsubstantive information collection request will be submitted to OMB under control number 0938-1352 to account for the updated costs.
We received a comment on our proposal to update the wage rate used in our calculation.
Comment: A commenter supported updating the BLS wage rate used in the burden calculation.
Response: We thank the commenter for the support.
8. ICRs Relating to the Hospital Readmissions Reduction Program
In section IV.G. of the preamble of this final rule, we discuss proposed and finalized requirements for the Hospital Readmissions Reduction Program. In this final rule, we are not removing or adopting any new measures into the Hospital Readmissions Reduction Program. All six of the Hospital Readmissions Reduction Program's measures are claims-based measures. We do not believe that continuing to use these claims-based measures creates or reduces any burden for hospitals because they will continue to be collected using Medicare FFS claims that hospitals are already submitting to the Medicare program for payment purposes.
We did not receive any comments regarding the ICRs for the Hospital Readmissions Reduction Program.
9. ICRs for the Promoting Interoperability Programs
a. Background
In section VIII.D. of the preamble of this final rule, we discuss proposed and finalized requirements for the Promoting Interoperability Programs. OMB has currently approved 623,562 total burden hours and approximately $61 million under OMB control number 0938-1278, accounting for information collection burden experienced by approximately 3,300 eligible hospitals and CAHs (Medicare-only and dual-eligible) that attest to CMS under the Medicare Promoting Interoperability Program. The collection of information burden analysis in this final rule focuses on eligible hospitals and CAHs that attest to the objectives and measures, and report CQMs, under the Medicare Promoting Interoperability Program for the reporting period in CY 2020.
b. Summary of Policies for Eligible Hospitals and CAHs That Attest to CMS Under the Medicare Promoting Interoperability Program for CY 2020
In section VIII.D.3.b. of the preamble of this final rule, as we proposed, we are changing the reporting requirement for the Query of Prescription Drug Monitoring Program (PDMP) measure from numerator and denominator to a “yes/no” response beginning with CY 2019 for eligible hospitals and CAHs that attest to CMS under the Medicare Promoting Interoperability Program. We expect this policy to affect our collection of information burden estimates for CY 2019 and CY 2020.
This final rule also includes the following finalized proposals for eligible hospitals and CAHs that attest to CMS under the Medicare Promoting Interoperability Program, which we do not expect to affect our collection of information burden estimates for CY 2020: (1) Elimination of the requirement that, for the FY 2020 payment adjustment year, for an eligible hospital that has not successfully demonstrated it is a meaningful EHR user in a prior year, the EHR reporting period in CY 2019 must end before and the eligible hospital must successfully register for and attest to meaningful use no later than October 1, 2019 deadline; (2) establishment of an EHR reporting period of a minimum of any continuous 90-day period in CY 2021 for new and returning participants (eligible hospitals and CAHs) in the Medicare Promoting Interoperability Program attesting to CMS; (3) requirement that the Medicare Promoting Interoperability Program measure actions must occur within the EHR reporting period beginning with the EHR reporting period in CY 2020; (4) revision of the Query of PDMP measure to make it an optional measure worth five bonus points in CY 2020, removal of the exclusions associated with this measure in CY 2020, and a clear statement of our intended policy that the measure is worth a full 5 bonus points in CY 2019 and CY 2020; (5) change of the maximum points available for the e-Prescribing measure to 10 points beginning in CY 2020, because we are finalizing the proposed changes to the Query of PDMP measure; (6) removal of the Verify Opioid Treatment Agreement measure beginning in CY 2020 and a clear statement of our intended policy that the measure is worth a full 5 bonus points in CY 2019; and (7) revision of the Support Electronic Referral Loops by Receiving and Incorporating Health Information measure to more clearly capture the previously established policy regarding CHERT use. We also are amending our regulations to incorporate several of these policies.
Although we are removing the Verify Opioid Treatment Agreement measure, we do not anticipate a change of burden for the Electronic Prescribing objective that this measure is associated with. In the Medicare and Medicaid Programs, Electronic Health Record Incentive Program—Stage 3 and Modifications to Meaningful Use in 2015 Through 2017 final rule (80 FR 62917), we estimated it would take an individual provider or designee approximately 10 minutes to attest to each objective and associated measure that requires a numerator and denominator to be generated. For objectives and associated measures requiring a numerator and denominator, we limit our estimates to actions taken in the presence of certified EHR technology. We do not anticipate a provider will maintain two recordkeeping systems when certified EHR technology is present. Therefore, we assume that all patient records that will be counted in the denominator will be kept using certified EHR technology. In addition, our estimates, provided in Table 21—Burden Estimates Stage 3—495.24 of the Medicare and Medicaid Programs; Electronic Health Record Incentive Program—Stage 3 and Modifications to Meaningful Use in 2015 Through 2017 final rule (80 FR 62918 through 62922), are calculated at the objective level, not for each individual measure being reported. We relied on this approach to create our burden estimates and determined that removing the Verify Opioid Treatment Agreement measure will not change burden since eligible hospitals and CAHs will still have to calculate a numerator and denominator for the e-Prescribing measure, which is associated with the Electronic Prescribing objective.
We anticipate that the burden will decrease for the Electronic Prescribing objective due to the policy to require a “yes/no” response instead of a numerator/denominator manual calculation for the Query of PDMP measure. The current numerator/denominator response for the Query of PDMP measure may require an eligible hospital or CAH to manually calculate the numerators and denominators outside of the certified EHR technology. The burden that was calculated for the Electronic Prescribing objective included the numerator/denominator calculated by the certified EHR technology, which is 10 minutes per respondent, plus the calculations performed manually outside of the certified EHR technology for the Query of PDMP measure, which we estimated at 40 minutes per respondent. We estimated that all eligible hospitals and CAHs will take 40 minutes per respondent to complete this measure by using the data found in certified EHR technology and manually tracking the number of times that they query the PDMP outside of certified EHR technology. This is a reduction in total burden of 40 minutes per respondent from FY 2019 IPPS/LTCH PPS final rule (83 FR 41698) reporting estimates which we estimate a total burden estimate of 7 hours and 10.8 minutes per respondent. With the reporting requirement change for the Query of PDMP measure from a numerator and denominator to a “yes/no” response beginning CY 2019, the certified EHR technology will be able to capture all of the actions required for the measures associated with the Electronic Prescribing objective; as a result, we estimate 10 minutes per respondent for this objective.
In section VIII.D.6. of the preamble of this final rule, as we proposed, we are making a number of changes with respect to the reporting of CQM data, including the addition of one opioid-related measure beginning with the reporting period in CY 2021 and the reporting period, reporting criteria, submission period, and form and method requirements for CQM reporting in CY 2020. However, for the reporting period in CY 2020, these policies are continuations of current policies and therefore we do not believe that there will be a change in burden for CY 2020.
c. Information Collection Burden Estimates for the Update to the Query of PDMP Measure
In section VIII.D.3.b. of the preamble of this final rule, as we proposed, we are changing the Query of PDMP measure's reporting requirement from a numerator and denominator to a “yes/no” response beginning in CY 2019. We stated in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41652) that we acknowledge that due to the varying integration of PDMPs into EHR systems, additional time, workflow changes and manual data capture and calculation would be needed to complete the query. This will result in some eligible hospitals and CAHs having to manually calculate the numerator and denominator for the Query of PDMP measure. We estimated that the action for eligible hospitals and CAHs to manually capture this measure will be a total of 40 minutes respectively for CY 2019 and CY 2020. By reducing the Query of PDMP measure reporting requirement from a numerator and denominator to a “yes/no” response, manual calculation will not be required by eligible hospitals and CAHs. We estimate that the change in reporting requirement for the Query of PDMP measure will result in a reduction of collection of information burden of 2,200 hours (40 minutes * 3300 respondents = 2,200 hours) for eligible hospitals and CAHs that attest to CMS under the Medicare Promoting Interoperability Program for CY 2020. The total saving for CY 2019 and CY 2020 is 4,400 collection of information burden hours.

d. Summary of Collection of Information Burden Estimates
1. Summary of Estimates Used To Calculate the Collection of Information Burden
In the Medicare and Medicaid Programs; Electronic Health Record Incentive Program—Stage 3 and Modifications to Meaningful Use in 2015 Through 2017 final rule (80 FR 62917), we estimated it will take an individual provider or designee approximately 10 minutes to attest to each objective and associated measure that requires a numerator and denominator to be generated. The measures that require a “yes/no” response will take approximately one minute to complete. We estimated that the Security Risk Analysis measure will take approximately 6 hours for an individual provider or designee to complete (we note this measure is still part of the program, but is not subject to performance-based scoring). We continue to believe these are appropriate burden estimates for reporting and have used this methodology in our collection of information burden estimates for this final rule.
Given the finalized proposals in this final rule, we estimate a total burden estimate of 6 hours 31 minutes per respondent. This is a reduction in total burden of 40 minutes per respondent from FY 2019 IPPS/LTCH PPS final rule (83 FR 41698) reporting estimates which we estimate a total burden estimate of 7 hours and 10.8 minutes per respondent. This represents a reduction of 2,200 total burden hours (0.66 hours × 3,300 respondents) for the Medicare Promoting Interoperability Program.

2. Hourly Labor Costs
In the Medicare and Medicaid Programs; Electronic Health Record Incentive Program—Stage 3 and Modifications to Meaningful Use in 2015 Through 2017 final rule (80 FR 62917), we estimated a mean hourly rate of $63.46 for the staff involved in attesting to EHR technology, meaningful use objectives and associated measures, and electronically submitting the clinical quality measures. We also used the mean hourly rate of $67.25 for the staff involved in attesting the objectives and measures under § 495.24(e) in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41698). Based on more recent 2017 data from the Bureau of Labor Statistics (BLS), we are updating this rate to $68.22 per hour for CY 2020.[931]
Based on the number of respondents for the Medicare Promoting Interoperability Program, the estimated burden response per respondent and the hourly labor cost of reporting, we estimate a total cost of $1,445,471.50 for CY 2019 and $1,466,320.68 for CY 2020. Due to a manual computation error in the proposed rule (84 FR 19578), the total costs for CY 2019 and CY 2020 are slightly different in this final rule. However, as seen in the below tables, and explained in greater detail in the next paragraph, the end result is a cost reduction for CY 2019 and for CY 2020.


This estimate takes into account the reduction of 2,200 total reporting burden hours per CY and the finalized hourly labor cost for CY 2019 and the updated hourly labor cost for CY 2020. This estimate represents a cost reduction of $147,950 ($1,593,421.50−$1,445,471.50) for CY 2019 and $127,100.82 ($1,593,421.50−$1,466,320.68) for CY 2020 when comparing to the total cost from the FY 2019 IPPS/LTCH PPS final rule (83 FR 41698) estimates.
10. ICRs for New Technology Add-On Payments
Section II.H. of the preamble of this final rule discusses new technology add-on payments. Applicants for these add-on payments must submit a formal request that includes information used to demonstrate that the medical service or technology meets the new technology add-on payment criteria. The burden associated with this application process is the time and effort necessary for an applicant to complete and submit the application and associated supporting information. The burden associated with this requirement is subject to the PRA, and is currently approved under OMB control number 0938-1347.
Section II.H.8. of the preamble of the proposed rule and this final rule discusses the alternative inpatient new technology add-on payment pathway for certain transformative new devices and for certain antimicrobial products. The burden associated with the finalized changes that will be needed for the new technology add-on payment application process will be discussed in a forthcoming revision of the information collection request (ICR) currently approved under OMB control number 0938-1347. The revised ICR is currently under development. However, upon completion of the revised ICR, we will publish the required 60-day and 30-day notices to solicit public comments in accordance with the requirements of the PRA.
11. Summary of All Burden in This Final Rule
Below is a chart reflecting the total burden and associated costs for the provisions included in this final rule.

XI. Provider Reimbursement Review Board Appeals
As we discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19579), the Provider Reimbursement Review Board (PRRB) was established in 1972 to handle Medicare Part A provider cost reimbursement appeals. Congress' intent with the creation of the PRRB was to provide an administrative appeals forum for Medicare payment disputes, and an opportunity for providers who are dissatisfied with the reimbursement determination made by their Medicare contractor or CMS to request and be afforded a hearing to adjudicate the issues involved.
Between 2015 and 2017, Medicare Part A providers filed cost report appeals at a higher rate than were resolved. On average, 3,000 appeals were filed per year and approximately 2,200 were resolved. The appeals inventory is now over 10,000 (including approximately 5,000 group appeals). The resolution process can take an average of 4 years, excluding cases in district court. CMS, providers, and MACs must expend considerable time and resources preparing and processing appeals.
As part of CMS' ongoing efforts to reduce provider burden, we are examining the growing inventory of PRRB appeals. To date, we have identified certain action initiatives that could be implemented with the goal to: Decrease the number of appeals submitted; decrease the number of appeals in inventory; reduce the time to resolution; and increase customer satisfaction. Some examples of these initiatives are as follows:
- Develop standard formats and more structured data for submitting cost reports and supplemental and supporting documentation.
- Create more clear standards for documentation to be used in auditing of cost reports.
- Enhance the Medicare Cost Report Electronic Filing (MCReF) portal by creating more automation for letter notifications, increasing provider transparency during the cost report reconciliation process, and improving the ability for providers to see where they are in the process.
- Explore opportunities to improve the process for claiming DSH Medicaid eligible days as part of the annual Medicare cost report submission and settlement process.
- Utilize artificial intelligence (AI) design risk protocols based on historical audit outcomes and empirical data to drive the audit and desk review processes.
- Triage the current appeals inventory and expand the provider's utilization of PRRB rules 46 and 47.2.3 (that is, resolve appeal issues through the cost report reopening process).
As part of this effort, in section IV.F.5. of the preamble of the proposed rule, we requested public comments on PRRB appeals related to a hospital's Medicaid fraction in the DSH payment adjustment calculation. We refer readers to that section for a discussion of the public comments we received and our response.
List of Subjects
42 CFR Part 412
- Administrative practice and procedure
- Health facilities
- Medicare
- Puerto Rico
- Reporting and recordkeeping requirements
42 CFR Part 413
- Health facilities
- Kidney diseases
- Medicare
- Puerto Rico
- Reporting and recordkeeping requirements
42 CFR Part 495
- Administrative practice and procedure
- Electronic health records
- Health facilities
- Health professions
- Health maintenance organizations (HMO)
- Medicaid
- Medicare
- Penalties
- Privacy
- Reporting and recordkeeping requirements
For the reasons set forth in the preamble, the Centers for Medicare and Medicaid Services is amending 42 CFR chapter IV as set forth below:
PART 412—PROSPECTIVE PAYMENT SYSTEMS FOR INPATIENT HOSPITAL SERVICES
1. The authority citation for part 412 is revised to read as follows:
2. Section 412.64 is amended by adding paragraph (d)(1)(viii) to read as follows:
(d) * * *
(1) * * *
(viii) For fiscal year 2020 and subsequent fiscal years, the percentage increase in the market basket index (as defined in § 413.40(a)(3) of this chapter) for prospective payment hospitals, subject to the provisions of paragraphs (d)(2) and (3) of this section, less a multifactor productivity adjustment (as determined by CMS).
3. Section 412.87 is amended by—
a. Adding paragraphs (b)(1)(i) through (v);
b. Redesignating paragraph (c) as paragraph (e);
c. Adding a new paragraph (c) and paragraph (d); and
d. Revising newly redesignated paragraph (e).
The additions and revision read as follows:
(b) * * *
(1) * * *
(i) The totality of the circumstances is considered when making a determination that a new medical service or technology represents an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
(ii) A determination that a new medical service or technology represents an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of Medicare beneficiaries means one of the following:
(A) The new medical service or technology offers a treatment option for a patient population unresponsive to, or ineligible for, currently available treatments.
(B) The new medical service or technology offers the ability to diagnose a medical condition in a patient population where that medical condition is currently undetectable, or offers the ability to diagnose a medical condition earlier in a patient population than allowed by currently available methods and there must also be evidence that use of the new medical service or technology to make a diagnosis affects the management of the patient.
(C) The use of the new medical service or technology significantly improves clinical outcomes relative to services or technologies previously available as demonstrated by one or more of the outcomes described in paragraphs (b)(1)(ii)(C(1) through (7) of this section.
(1) A reduction in at least one clinically significant adverse event, including a reduction in mortality or a clinically significant complication.
(2) A decreased rate of at least one subsequent diagnostic or therapeutic intervention.
(3) A decreased number of future hospitalizations or physician visits.
(4) A more rapid beneficial resolution of the disease process treatment including, but not limited to, a reduced length of stay or recovery time
(5) An improvement in one or more activities of daily living
(6) An improved quality of life
(7) A demonstrated greater medication adherence or compliance.
(D) The totality of the information otherwise demonstrates that the new medical service or technology substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
(iii) Evidence from published or unpublished information sources from within the United States or elsewhere may be sufficient to establish that a new medical service or technology represents an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of Medicare beneficiaries. Information source may include the following:
(A) Clinical trials;
(B) Peer reviewed journal articles;
(C) Study results;
(D) Meta-analyses;
(E) Consensus statements;
(F) White papers;
(G) Patient surveys;
(H) Case studies;
(I) Reports;
(J) Systematic literature reviews;
(K) Letters from major healthcare associations;
(L) Editorials and letters to the editor; and,
(M) Public comments.
(N) Other appropriate information sources may be considered.
(iv) The medical condition diagnosed or treated by the new medical service or technology may have a low prevalence among Medicare beneficiaries.
(v) The new medical service or technology may represent an advance that substantially improves, relative to services or technologies previously available, the diagnosis or treatment of a subpopulation of patients with the medical condition diagnosed or treated by the new medical service or technology.
(c) Eligibility criteria for alternative pathway for certain transformative new devices. For discharges occurring on or after October 1, 2020, CMS provides for additional payments (as specified in § 412.88) beyond the standard DRG payments and outlier payments to a hospital for discharges involving covered inpatient hospital services that are new medical devices, if the following conditions are met:
(1) A new medical device has received Food and Drug Administration (FDA) marketing authorization and is part of the FDA's Breakthrough Devices Program.
(2) A medical device that meets the condition in paragraph (c)(1) of this section will be considered new for not less than 2 years and not more than 3 years after the point at which data begin to become available reflecting the inpatient hospital code (as defined in section 1886(d)(5)(K)(iii) of the Social Security Act) assigned to the new technology (depending on when a new code is assigned and data on the new technology become available for DRG recalibration). After CMS has recalibrated the DRGs, based on available data, to reflect the costs of an otherwise new medical technology, the medical technology will no longer be considered “new” under the criterion of this section.
(3) The new medical device meets the conditions described in paragraph (b)(3) of this section.
(d) Eligibility criteria for alternative pathway for Qualified Infectious Disease Products. For discharges occurring on or after October 1, 2020, CMS provides for additional payments (as specified in § 412.88) beyond the standard DRG payments and outlier payments to a hospital for discharges involving covered inpatient hospital services that are new medical products, if the following conditions are met:
(1) A new medical product has received Food and Drug Administration (FDA) marketing authorization and is designated as a Qualified Infectious Disease Product by the FDA.
(2) A medical product that meets the condition in paragraph (d)(1) of this section will be considered new for not less than 2 years and not more than 3 years after the point at which data begin to become available reflecting the inpatient hospital code (as defined in section 1886(d)(5)(K)(iii) of the Social Security Act) assigned to the new technology (depending on when a new code is assigned and data on the new technology become available for DRG recalibration). After CMS has recalibrated the DRGs, based on available data, to reflect the costs of an otherwise new medical technology, the medical technology will no longer be considered “new” under the criterion of this section.
(3) The new medical product meets the conditions described in paragraph (b)(3) of this section.
(e) Announcement of determinations and deadline for consideration of new medical service or technology applications. (1) CMS will consider whether a new medical service or technology meets the eligibility criteria specified in paragraph (b), (c), or (d) of this section and announce the results in the Federal Register as part of its annual updates and changes to the IPPS. CMS will only consider any particular new medical service or technology for add-on payments under paragraph (b), (c), or (d) of this section.
(2) CMS will only consider, for add-on payments for a particular fiscal year, an application for which the new medical service or technology has received FDA approval or clearance by July 1 prior to the particular fiscal year.
4. Section 412.88 is amended by revising paragraphs (a)(2) and (b) to read as follows:
(a) * * *
(2)(i) For discharges occurring before October 1, 2019. If the costs of the discharge (determined by applying the operating cost-to-charge ratios as described in § 412.84(h)) exceed the full DRG payment, an additional amount equal to the lesser of—
(A) 50 percent of the costs of the new medical service or technology; or
(B) 50 percent of the amount by which the costs of the case exceed the standard DRG payment.
(ii) For discharges occurring on or after October 1, 2019. (A) Except as provided under paragraph (a)(2)(ii)(2) of this section, if the costs of the discharge (determined by applying the operating cost-to-charge ratios as described in § 412.84(h)) exceed the full DRG payment, an additional amount equal to the lesser of—
(1) 65 percent of the costs of the new medical service or technology; or
(2) 65 percent of the amount by which the costs of the case exceed the standard DRG payment.
(B) For a medical product designated by the Food and Drug Administration (FDA) as a Qualified Infectious Disease Product, if the costs of the discharge (determined by applying the operating cost-to-charge ratios as described in § 412.84(h)) exceed the full DRG payment, an additional amount equal to the lesser of—
(1) 75 percent of the costs of the new medical service or technology; or
(2) 75 percent of the amount by which the costs of the case exceed the standard DRG payment.
(b)(1) For discharges occurring before October 1, 2019. Unless a discharge case qualifies for outlier payment under § 412.84, Medicare will not pay any additional amount beyond the DRG payment plus 50 percent of the estimated costs of the new medical service or technology.
(2) For discharges occurring on or after October 1, 2019. Unless a discharge case qualifies for outlier payment under § 412.84, Medicare will not pay any additional amount beyond the DRG payment plus 65 percent, or the DRG payment plus 75 percent for a medical product designated by the FDA as a Qualified Infectious Disease Product, of the estimated costs of the new medical service or technology.
5. Section 412.101 is amended by revising paragraph (e) to read as follows:
(e) Special treatment regarding hospitals operated by the Indian Health Service (IHS) or a Tribe. (1) For discharges occurring in FY 2018 and subsequent fiscal years—
(i) A hospital operated by the IHS or a Tribe will be considered to meet the applicable mileage criterion specified under paragraph (b)(2) of this section if it is located more than the specified number of road miles from the nearest subsection (d) hospital operated by the IHS or a Tribe.
(ii) A hospital, other than a hospital operated by the IHS or a Tribe, will be considered to meet the applicable mileage criterion specified under paragraph (b)(2) of this section if it is located more than the specified number of road miles from the nearest subsection (d) hospital other than a subsection (d) hospital operated by the IHS or a Tribe.
(2) Subject to the requirements set forth in § 405.1885 of this chapter, a hospital may request the application of the policy described in paragraph (e)(1) of this section for discharges occurring in FY 2011 through FY 2017.
6. Section 412.103 is amended by—
a. Revising paragraph (b)(3);
b. Adding paragraph (g)(1)(iii);
c. Revising paragraph (g)(2)(iii); and
d. Adding paragraphs (g)(3) and (4).
The revisions and additions read as follows:
(b) * * *
(3) Submission of application. An application may be submitted to the CMS Regional Office by the requesting hospital by mail or by facsimile or other electronic means.
(g) * * *
(1) * * *
(iii) The provisions of paragraphs (g)(1)(i) and (ii) of this section are effective for all written requests submitted by hospitals before October 1, 2019 to cancel rural reclassifications.
(2) * * *
(iii) The provisions of paragraphs (g)(2)(i) and (ii) of this section are effective for all written requests submitted by hospitals on or after October 1, 2007 and before October 1, 2019, to cancel rural reclassifications.
(3) Cancellation of rural reclassification on or after October 1, 2019. For all written requests submitted by hospitals on or after October, 1, 2019 to cancel rural reclassifications, a hospital may cancel its rural reclassification by submitting a written request to the CMS Regional Office not less than 120 days prior to the end of a Federal fiscal year. The hospital's cancellation of the classification is effective beginning with the next Federal fiscal year.
(4) Special rule for hospitals that opt to receive county out-migration adjustment. A rural reclassification will be considered canceled effective for the next Federal fiscal year when a hospital, by submitting a request to CMS within 45 days of the date of public display of the proposed rule for the next Federal fiscal year at the Office of the Federal Register, opts to accept and receives its county out-migration wage index adjustment determined under section 1886(d)(13) of the Act in lieu of its geographic reclassification described under section 1886(d)(8)(B) of the Act.
7. Section 412.106 is amended by adding paragraph (g)(1)(iii)(C)( 6) to read as follows:
(g) * * *
(1) * * *
(iii) * * *
(C) * * *
(6) For fiscal year 2020, CMS will base its estimates of the amount of hospital uncompensated care on data on uncompensated care costs, defined as charity care costs plus non-Medicare and non-reimbursable Medicare bad debt costs from 2015 cost reports from the most recent HCRIS database extract, except that, for Puerto Rico hospitals and Indian Health Service or Tribal hospitals, CMS will base its estimates on utilization data for Medicaid and Medicare SSI patients, as determined by CMS in accordance with paragraphs (b)(2)(i) and (b)(4) of this section, using data on Medicaid utilization from 2013 cost reports from the most recent HCRIS database extract and the most recent available year of data on Medicare SSI utilization (or, for Puerto Rico hospitals, a proxy for Medicare SSI utilization data);
8. Section 412.152 is amended by revising the definitions of “Aggregate payments for excess readmissions”, “Applicable condition”, “Base operating DRG payment amount”, and “Dual-eligible” to read as follows:
Aggregate payments for excess readmissions is, for a hospital for the applicable period, the sum, for the applicable conditions, of the product for each applicable condition of:
(1) The base operating DRG payment amount for the hospital for the applicable period for such condition or procedure;
(2) The number of admissions for such condition or procedure for the hospital for the applicable period;
(3) The excess readmission ratio for the hospital for the applicable period minus the peer-group median excess readmission ratio (ERR); and
(4) The neutrality modifier, a multiplicative factor that equates total Medicare savings under the current stratified methodology to the previous non-stratified methodology.
Applicable condition is a condition or procedure selected by the Secretary—
(1) Among the conditions and procedures for which—
(i) Readmissions represent conditions or procedures that are high volume or high expenditures; and
(ii) Measures of such readmissions have been endorsed by the entity with a contract under section 1890(a) of the Act and such endorsed measures have exclusions for readmissions that are unrelated to the prior discharge (such as a planned readmission or transfer to another applicable hospital); or
(2) Among other conditions and procedures as determined appropriate by the Secretary. In expanding the applicable conditions, the Secretary will seek endorsement of the entity with a contract under section 1890(a) of the Act, but may apply such measures without such an endorsement in the case of a specified area or medical topic determined appropriate by the Secretary for which a feasible and practical measure has not been endorsed by the entity with a contract under section 1890(a) of the Act as long as due consideration is given to measures that have been endorsed or adopted by a consensus organization identified by the Secretary.
Base operating DRG payment amount is the wage-adjusted DRG operating payment plus any applicable new technology add-on payments under subpart F of this part. This amount is determined without regard to any payment adjustments under the Hospital Value-Based Purchasing Program, as specified under § 412.162. This amount does not include any additional payments for indirect medical education under § 412.105, the treatment of a disproportionate share of low-income patients under § 412.106, outliers under subpart F of this part, and a low volume of discharges under § 412.101. With respect to a sole community hospital that receives payments under § 412.92(d) this amount also does not include the difference between the hospital-specific payment rate and the Federal payment rate determined under subpart D of this part. With respect to a Medicare-dependent, small rural hospital that receives payments under § 412.108(c), this amount includes the difference between the hospital-specific payment rate and the Federal payment rate determined under subpart D of this part. With respect to a hospital that is paid under section 1814(b)(3) of the Act, this amount is an amount equal to the wage-adjusted DRG payment amount plus new technology payments that would be paid to such hospitals, absent the provisions of section 1814(b)(3) of the Act.
Dual-eligible—(1) For payment adjustment factor calculations prior to the FY 2021 program year, is a patient beneficiary who has been identified as having full benefit status in both the Medicare and Medicaid programs in the State Medicare Authorization Act (MMA) files for the month the beneficiary was discharged from the hospital; and
(2) For payment adjustment factor calculations beginning in the FY 2021 program year, is a patient beneficiary who has been identified as having full benefit status in both the Medicare and Medicaid programs in data sourced from the State MMA files for the month the beneficiary was discharged from the hospital, except for those patient beneficiaries who die in the month of discharge, which will be identified using the previous month's data as sourced from the State MMA files.
9. Section 412.154 is amended by redesignating paragraph (e)(4) as paragraph (e)(6) and adding new paragraph (e)(4) and paragraph (e)(5) to read as follows:
(e) * * *
(4) The neutrality modifier.
(5) The proportion of dual-eligibles.
10. Section 412.172 is amended by revising paragraphs (f)(2) and (4) to read as follows:
(f) * * *
(2) Hospitals will have a period of 30 days after the receipt of the information provided under paragraph (f)(1) of this section to review and submit corrections for the hospital-acquired condition program score s for each condition that is used to calculate the total hospital-acquired condition score for the fiscal year.
(4) CMS will post the total hospital-acquired condition score and the score on each measure for each hospital on the Hospital Compare website.
11. Section 412.230 is amended by revising paragraph (a)(4) to read as follows:
(a) * * *
(4) Application of criteria. In applying the numeric criteria contained in paragraphs (b)(1) and (2) and (d)(1)(iii) and (iv) of this section, rounding of numbers to meet the mileage or qualifying percentage standards is not permitted.
12. Section 412.256 is amended by revising paragraph (a)(1) to read as follows:
(a) * * *
(1) An application must be submitted to the MGCRB according to the method prescribed by the MGCRB.
13. Section 412.522 is amended by adding paragraphs (d)(3) through (6) to read as follows:
(d) * * *
(3) For cost reporting periods beginning on or after October 1, 2019, if a long-term care hospital's discharge payment percentage for the cost reporting period is not at least 50 percent, discharges in all cost reporting periods beginning after the notification described under paragraph (d)(2) of this section will be paid under the payment adjustment described in paragraph (d)(4) of this section until reinstated under paragraph (d)(5) or (6) of this section.
(4) For cost reporting periods subject to the payment adjustment under paragraph (d)(3) of this section, the payment for all discharges consists of—
(i) An amount equivalent to the hospital inpatient prospective payment system amount as determined under § 412.529(d)(4)(i)(A) and (d)(4)(ii) and (iii); and
(ii) If applicable, an additional payment for high cost outlier cases based on the fixed-loss amount established for the hospital inpatient prospective payment system in effect at the time of the LTCH discharge.
(5) For full reinstatement—
(i) When the discharge payment percentage for a cost reporting period is calculated to be at least 50 percent, any payment adjustment described in paragraph (d)(4) of this section will be discontinued for cost reporting periods beginning on or after the notification described under paragraph (d)(2) of this section.
(ii) A long-term care hospital reinstated under paragraph (d)(5)(i) of this section will be subject to the payment adjustment under paragraph (d)(4) of this section if, after being reinstated, it again meets the criteria in paragraph (d)(3) of this section.
(6) For special probationary reinstatement—
(i) A hospital that would be subject to the payment adjustment under paragraph (d)(4) of this section for a cost reporting period will have application of the payment adjustment delayed for that period if, for the period of at least 5 consecutive months of the 6 months immediately preceding the cost reporting period, the discharge payment percentage is calculated to be at least 50 percent.
(ii) For any cost reporting period to which the payment adjustment under paragraph (d)(4) of this section would have applied but for a delay under paragraph (d)(6)(i) of this section, the payment adjustment under paragraph (d)(4) of this section will be applied to all discharges in the cost reporting period if the discharge payment percentage for the cost reporting period is not calculated to be at least 50 percent.
14. Section 412.523 is amended by adding paragraph (c)(3)(xvi) to read as follows:
(c) * * *
(3) * * *
(xvi) For long-term care prospective payment system fiscal year beginning October 1, 2019, and ending September 30, 2020. The long-term care hospital prospective payment system standard Federal payment rate for the long-term care hospital prospective payment system beginning October 1, 2019 and ending September 30, 2020 is the standard Federal payment rate for the previous long-term care prospective payment system fiscal year updated by 2.5 percent and further adjusted, as appropriate, as described in paragraph (d) of this section.
15. Section 412.560 is amended by revising paragraphs (d)(1) and (3) and (f)(1) to read as follows:
(d) * * *
(1) Written letter of non-compliance decision. Long-term care hospitals that do not meet the requirement in paragraph (b) of this section for a program year will receive a notification of non-compliance sent through at least one of the following methods: The CMS designated data submission system, the United States Postal Service, or via an email from the MAC.
(3) CMS decision on reconsideration request. CMS will notify long-term care hospitals, in writing, of its final decision regarding any reconsideration request through at least one of the following methods: The CMS designated data submission system, the United States Postal Service, or via an email from the MAC.
(f) * * *
(1) Long-term care hospitals must meet or exceed two separate data completeness thresholds: One threshold set at 80 percent for completion of measures data and standardized patient assessment data collected using the LTCH CARE Data Set submitted through the CMS designated data submission system; and a second threshold set at 100 percent for measures data collected and submitted using the CDC NHSN.
PART 413—PRINCIPLES OF REASONABLE COST REIMBURSEMENT; PAYMENT FOR END-STAGE RENAL DISEASE SERVICES; OPTIONAL PROSPECTIVELY DETERMINED PAYMENT RATES FOR SKILLED NURSING FACILITIES
16. The authority for part 413 is revised to read as follows:
17. Section 413.70 is amended by revising paragraph (b)(5)(i)(C) and adding paragraph (b)(5)(i)(D) to read as follows:
(b) * * *
(5) * * *
(i) * * *
(C) Effective for cost reporting periods beginning on or after October 1, 2011 and on or before September 30, 2019, payment for ambulance services furnished by a CAH or an entity that is owned and operated by a CAH is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the entity is the only provider or supplier of ambulance services located within a 35-mile drive of the CAH. If there is no provider or supplier of ambulance services located within a 35-mile drive of the CAH and there is an entity that is owned and operated by a CAH that is more than a 35-mile drive from the CAH, payment for ambulance services furnished by that entity is 101 percent of the reasonable costs of the entity in furnishing those services, but only if the entity is the closest provider or supplier of ambulance services to the CAH.
(D) Effective for cost reporting periods beginning on or after October 1, 2019, payment for ambulance services furnished by a CAH or by a CAH-owned and operated entity is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the entity is the only provider or supplier of ambulance services located within a 35-mile drive of the CAH, excluding ambulance providers or suppliers that are not legally authorized to furnish ambulance services to transport individuals to or from the CAH. If there is no provider or supplier of ambulance services located within a 35-mile drive of the CAH and there is an entity that is owned and operated by a CAH that is more than a 35-mile drive from the CAH, payment for ambulance services furnished by that entity is 101 percent of the reasonable costs of the entity in furnishing those services, but only if the entity is the closest provider or supplier of ambulance services to the CAH.
PART 495—STANDARDS FOR THE ELECTRONIC HEALTH RECORD TECHNOLOGY INCENTIVE PROGRAM
18. The authority citation for part 495 continues to read as follows:
19. Section 495.4 is amended—
a. In the definition of “EHR reporting period”, by adding paragraph (2)(v); and
b. In the definition of “EHR reporting period for a payment adjustment year”, by revising paragraph (2)(iii)(A) and adding paragraphs (2)(v) and (3)(v).
The additions and revision read as follows:
EHR reporting period. * * *
(2) * * *
(v) For the FY 2021 payment year as follows: Under the Medicare Promoting Interoperability Program, for a Puerto Rico eligible hospital, any continuous 90-day period within CY 2021.
EHR reporting period for a payment adjustment year. * * *
(2) * * *
(iii) * * *
(A) If an eligible hospital has not successfully demonstrated it is a meaningful EHR user in a prior year, the EHR reporting period is any continuous 90-day period within CY 2019 and applies for the FY 2020 and FY 2021 payment adjustment years.
(v) The following are applicable for 2021:
(A) If an eligible hospital has not successfully demonstrated it is a meaningful EHR user in a prior year, the EHR reporting period is any continuous 90-day period within CY 2021 and applies for the FY 2022 and 2023 payment adjustment years. For the FY 2022 payment adjustment year, the EHR reporting period must end before and the eligible hospital must successfully register for and attest to meaningful use no later than October 1, 2021.
(B) If in a prior year an eligible hospital has successfully demonstrated it is a meaningful EHR user, the EHR reporting period is any continuous 90-day period within CY 2021 and applies for the FY 2023 payment adjustment year.
(3) * * *
(v) The following are applicable for 2021:
(A) If a CAH has not successfully demonstrated it is a meaningful EHR user in a prior year, the EHR reporting period is any continuous 90-day period within CY 2021 and applies for the FY 2021 payment adjustment year.
(B) If in a prior year a CAH has successfully demonstrated it is a meaningful EHR user, the EHR reporting period is any continuous 90-day period within CY 2021 and applies for the FY 2021 payment adjustment year.
20. Section 495.24 is amended by revising paragraphs (e)(1), (e)(4)(iii), (e)(5)(ii)(B), (e)(5)(iii), (iv), and (v), and (e)(6)(ii)(B) to read as follows:
(e) * * *
(1) General rule. (i) Except as specified in paragraph (e)(2) of this section, eligible hospitals and CAHs must meet all objectives and associated measures of the Stage 3 criteria specified in this paragraph (e) and earn a total score of at least 50 points to meet the definition of a meaningful EHR user.
(ii) Beginning in CY 2020, the numerator and denominator of measures increment based on actions occurring during the EHR reporting period selected by the eligible hospital or CAH, unless otherwise indicated.
(4) * * *
(iii) Security risk analysis measure. Conduct or review a security risk analysis in accordance with the requirements under 45 CFR 164.308(a)(1), including addressing the security (including encryption) of data created or maintained by CEHRT in accordance with requirements under 45 CFR 164.312(a)(2)(iv) and 45 CFR 164.306(d)(3), implement security updates as necessary, and correct identified security deficiencies as part of the provider's risk management process. Actions included in the security risk analysis measure may occur any time during the calendar year in which the EHR reporting period occurs.
(5) * * *
(ii) * * *
(B) In 2020 and subsequent years, eligible hospitals and CAHs must meet the e-Prescribing measure in paragraph (e)(5)(iii)(A) of this section and have the option to report on the query of PDMP measure in paragraph (e)(5)(iii)(B) of this section. In 2020 and subsequent years, the electronic prescribing objective in paragraph (e)(5)(i) of this section is worth up to 15 points.
(iii) Measures—(A) e-Prescribing measure. Subject to paragraph (e)(3) of this section, at least one hospital discharge medication order for permissible prescriptions (for new and changed prescriptions) is queried for a drug formulary and transmitted electronically using CEHRT. This measure is worth up to 10 points in CY 2019 and subsequent years.
(B) Query of prescription drug monitoring program (PDMP) measure. Subject to paragraph (e)(3) of this section, for at least one Schedule II opioid electronically prescribed using CEHRT during the EHR reporting period, the eligible hospital or CAH uses data from CEHRT to conduct a query of a Prescription Drug Monitoring Program (PDMP) for prescription drug history, except where prohibited and in accordance with applicable law. This measure is worth 5 bonus points in CY 2019 and CY 2020.
(C) Verify opioid treatment agreement measure. Subject to paragraph (e)(3) of this section, for at least one unique patient for whom a Schedule II opioid was electronically prescribed by the eligible hospital or CAH using CEHRT during the EHR reporting period, if the total duration of the patient's Schedule II opioid prescriptions is at least 30 cumulative days within a 6-month look-back period, the eligible hospital or CAH seeks to identify the existence of a signed opioid treatment agreement and incorporates it into the patient's electronic health record using CEHRT. This measure is worth 5 bonus points in CY 2019.
(iv) Exclusions in accordance with paragraph (e)(2) of this section and redistribution of points. An exclusion claimed under paragraph (e)(5)(v) of this section will redistribute 10 points in CY 2019 and CY 2020 equally among the measures associated with the health information exchange objective under paragraph (e)(6) of this section.
(v) Exclusion in accordance with paragraph (e)(2) of this section. Beginning with the EHR reporting period in CY 2019, any eligible hospital or CAH that does not have an internal pharmacy that can accept electronic prescriptions and there are no pharmacies that accept electronic prescriptions within 10 miles at the start of the eligible hospital or CAH's EHR reporting period may be excluded from the measure specified in paragraph (e)(5)(iii)(A) of this section.
(6) * * *
(ii) * * *
(B) Support electronic referral loops by receiving and incorporating health information measure. Subject to paragraph (e)(3) of this section, for at least one electronic summary of care record received using CEHRT for patient encounters during the EHR reporting period for which an eligible hospital or CAH was the receiving party of a transition of care or referral, or for patient encounters during the EHR reporting period in which the eligible hospital or CAH has never before encountered the patient, the eligible hospital or CAH conducts clinical information reconciliation for medication, medication allergy, and current problem list using CEHRT.
Dated: July 26, 2019.
Seema Verma,
Administrator, Centers for Medicare and Medicaid Services.
Dated: July 26, 2019.
Alex M. Azar II,
Secretary, Department of Health and Human Services.
Note:
The following Addendum and Appendices will not appear in the Code of Federal Regulations.
Addendum—Schedule of Standardized Amounts, Update Factors, Rate-of-Increase Percentages Effective With Cost Reporting Periods Beginning on or After October 1, 2019, and Payment Rates for LTCHs Effective for Discharges Occurring on or After October 1, 2019
I. Summary and Background
In this Addendum, we are setting forth a description of the methods and data we used to determine the prospective payment rates for Medicare hospital inpatient operating costs and Medicare hospital inpatient capital-related costs for FY 2020 for acute care hospitals. We also are setting forth the rate-of-increase percentage for updating the target amounts for certain hospitals excluded from the IPPS for FY 2020. We note that, because certain hospitals excluded from the IPPS are paid on a reasonable cost basis subject to a rate-of-increase ceiling (and not by the IPPS), these hospitals are not affected by the figures for the standardized amounts, offsets, and budget neutrality factors. Therefore, in this final rule, we are setting forth the rate-of-increase percentage for updating the target amounts for certain hospitals excluded from the IPPS that will be effective for cost reporting periods beginning on or after October 1, 2019.
In addition, we are setting forth a description of the methods and data we used to determine the LTCH PPS standard Federal payment rate that will be applicable to Medicare LTCHs for FY 2020.
In general, except for SCHs and MDHs, for FY 2020, each hospital's payment per discharge under the IPPS is based on 100 percent of the Federal national rate, also known as the national adjusted standardized amount. This amount reflects the national average hospital cost per case from a base year, updated for inflation.
SCHs are paid based on whichever of the following rates yields the greatest aggregate payment: The Federal national rate (including, as discussed in section IV.G. of the preamble of this final rule, uncompensated care payments under section 1886(r)(2) of the Act); the updated hospital-specific rate based on FY 1982 costs per discharge; the updated hospital-specific rate based on FY 1987 costs per discharge; the updated hospital-specific rate based on FY 1996 costs per discharge; or the updated hospital-specific rate based on FY 2006 costs per discharge.
Under section 1886(d)(5)(G) of the Act, MDHs historically were paid based on the Federal national rate or, if higher, the Federal national rate plus 50 percent of the difference between the Federal national rate and the updated hospital-specific rate based on FY 1982 or FY 1987 costs per discharge, whichever was higher. However, section 5003(a)(1) of Public Law 109-171 extended and modified the MDH special payment provision that was previously set to expire on October 1, 2006, to include discharges occurring on or after October 1, 2006, but before October 1, 2011. Under section 5003(b) of Public Law 109-171, if the change results in an increase to an MDH's target amount, we must rebase an MDH's hospital specific rates based on its FY 2002 cost report. Section 5003(c) of Public Law 109-171 further required that MDHs be paid based on the Federal national rate or, if higher, the Federal national rate plus 75 percent of the difference between the Federal national rate and the updated hospital specific rate. Further, based on the provisions of section 5003(d) of Public Law 109-171, MDHs are no longer subject to the 12-percent cap on their DSH payment adjustment factor. Section 50205 of the Bipartisan Budget Act of 2018 extended the MDH program for discharges on or after October 1, 2017 through September 30, 2022.
As discussed in section IV.B. of the preamble of this final rule, in accordance with section 1886(d)(9)(E) of the Act as amended by section 601 of the Consolidated Appropriations Act, 2016 (Pub. L. 114-113), for FY 2020, subsection (d) Puerto Rico hospitals will continue to be paid based on 100 percent of the national standardized amount. Because Puerto Rico hospitals are paid 100 percent of the national standardized amount and are subject to the same national standardized amount as subsection (d) hospitals that receive the full update, our discussion below does not include references to the Puerto Rico standardized amount or the Puerto Rico-specific wage index.
As discussed in section II. of this Addendum, as we proposed, we are making changes in the determination of the prospective payment rates for Medicare inpatient operating costs for acute care hospitals for FY 2020. In section III. of this Addendum, we discuss our policy changes for determining the prospective payment rates for Medicare inpatient capital-related costs for FY 2020. In section IV. of this Addendum, we are setting forth the rate-of-increase percentage for determining the rate-of-increase limits for certain hospitals excluded from the IPPS for FY 2020. In section V. of this Addendum, we discuss policy changes for determining the LTCH PPS standard Federal rate for LTCHs paid under the LTCH PPS for FY 2020. The tables to which we refer to in the preamble of this final rule are listed in section VI. of this Addendum and are available via the internet on the CMS website.
II. Changes to Prospective Payment Rates for Hospital Inpatient Operating Costs for Acute Care Hospitals for FY 2020
The basic methodology for determining prospective payment rates for hospital inpatient operating costs for acute care hospitals for FY 2005 and subsequent fiscal years is set forth under § 412.64. The basic methodology for determining the prospective payment rates for hospital inpatient operating costs for hospitals located in Puerto Rico for FY 2005 and subsequent fiscal years is set forth under §§ 412.211 and 412.212. Below we discuss the factors we used for determining the prospective payment rates for FY 2020.
In summary, the standardized amounts set forth in Tables 1A, 1B, and 1C that are listed and published in section VI. of this Addendum (and available via the internet on the CMS website) reflect—
- Equalization of the standardized amounts for urban and other areas at the level computed for large urban hospitals during FY 2004 and onward, as provided for under section 1886(d)(3)(A)(iv)(II) of the Act.
- The labor-related share that is applied to the standardized amounts to give the hospital the highest payment, as provided for under sections 1886(d)(3)(E) and 1886(d)(9)(C)(iv) of the Act. For FY 2020, depending on whether a hospital submits quality data under the rules established in accordance with section 1886(b)(3)(B)(viii) of the Act (hereafter referred to as a hospital that submits quality data) and is a meaningful EHR user under section 1886(b)(3)(B)(ix) of the Act (hereafter referred to as a hospital that is a meaningful EHR user), there are four possible applicable percentage increases that can be applied to the national standardized amount. We refer readers to section IV.B. of the preamble of this final rule for a complete discussion on the FY 2020 inpatient hospital update. Below is a table with these four scenarios:

We note that section 1886(b)(3)(B)(viii) of the Act, which specifies the adjustment to the applicable percentage increase for “subsection (d)” hospitals that do not submit quality data under the rules established by the Secretary, is not applicable to hospitals located in Puerto Rico.
In addition, section 602 of Public Law 114-113 amended section 1886(n)(6)(B) of the Act to specify that Puerto Rico hospitals are eligible for incentive payments for the meaningful use of certified EHR technology, effective beginning FY 2016, and also to apply the adjustments to the applicable percentage increase under section 1886(b)(3)(B)(ix) of the Act to Puerto Rico hospitals that are not meaningful EHR users, effective FY 2022. Accordingly, because the provisions of section 1886(b)(3)(B)(ix) of the Act are not applicable to hospitals located in Puerto Rico until FY 2022, the adjustments under this provision are not applicable for FY 2020.
- An adjustment to the standardized amount to ensure budget neutrality for DRG recalibration and reclassification, as provided for under section 1886(d)(4)(C)(iii) of the Act.
- An adjustment to ensure the wage index and labor-related share changes (depending on the fiscal year) are budget neutral, as provided for under section 1886(d)(3)(E)(i) of the Act (as discussed in the FY 2006 IPPS final rule (70 FR 47395) and the FY 2010 IPPS final rule (74 FR 44005). We note that section 1886(d)(3)(E)(i) of the Act requires that when we compute such budget neutrality, we assume that the provisions of section 1886(d)(3)(E)(ii) of the Act (requiring a 62-percent labor-related share in certain circumstances) had not been enacted.
- An adjustment to ensure the effects of geographic reclassification are budget neutral, as provided for under section 1886(d)(8)(D) of the Act, by removing the FY 2019 budget neutrality factor and applying a revised factor.
- A positive adjustment of 0.5 percent in FYs 2019 through 2023 as required under section 414 of the MACRA.
- An adjustment to ensure the effects of the Rural Community Hospital Demonstration program are budget neutral as required under section 410A(c)(2) of Public Law 108-173. This demonstration program is required under section 410A of Public Law 108-173, as amended by sections 3123 and 10313 of Public Law 111-148, which extended the demonstration program for an additional 5 years, as amended by section 15003 of Public Law 114-255 which amended section 410A of Public Law 108-173 to provide for a 10-year extension of the demonstration program (in place of the 5-year extension required by the Affordable Care Act) beginning on the date immediately following the last day of the initial 5-year period under section 410A(a)(5) of Public Law 108-173.
- An adjustment to the standardized amount to implement in a budget neutral manner the increase in the wage index values for hospitals with a wage index value below the 25th percentile wage index value across all hospitals (as described in section III.N. of the preamble of this final rule).
- An adjustment to the standardized amount (using our exceptions and adjustments authority under section 1886(d)(5)(I)(i) of the Act) to implement in a budget neutral manner our transition (described in section III.N.2.d. of the preamble of this final rule) for hospitals negatively impacted due to changes to the wage index. We refer readers to section III.N. of the preamble of this final rule for a detailed discussion.
- An adjustment to remove the FY 2019 outlier offset and apply an offset for FY 2020, as provided for in section 1886(d)(3)(B) of the Act.
For FY 2020, consistent with current law, as we proposed, we applied the rural floor budget neutrality adjustment to hospital wage indexes. Also, consistent with section 3141 of the Affordable Care Act, instead of applying a State-level rural floor budget neutrality adjustment to the wage index, as we proposed, we applied a uniform, national budget neutrality adjustment to the FY 2020 wage index for the rural floor.
A. Calculation of the Adjusted Standardized Amount
1. Standardization of Base-Year Costs or Target Amounts
In general, the national standardized amount is based on per discharge averages of adjusted hospital costs from a base period (section 1886(d)(2)(A) of the Act), updated and otherwise adjusted in accordance with the provisions of section 1886(d) of the Act. The September 1, 1983 interim final rule (48 FR 39763) contained a detailed explanation of how base-year cost data (from cost reporting periods ending during FY 1981) were established for urban and rural hospitals in the initial development of standardized amounts for the IPPS.
Sections 1886(d)(2)(B) and 1886(d)(2)(C) of the Act require us to update base-year per discharge costs for FY 1984 and then standardize the cost data in order to remove the effects of certain sources of cost variations among hospitals. These effects include case-mix, differences in area wage levels, cost-of-living adjustments for Alaska and Hawaii, IME costs, and costs to hospitals serving a disproportionate share of low-income patients.
For FY 2020, as we proposed, we are continuing to use the national labor-related and nonlabor-related shares (which are based on the 2014-based hospital market basket) that were used in FY 2019. Specifically, under section 1886(d)(3)(E) of the Act, the Secretary estimates, from time to time, the proportion of payments that are labor-related and adjusts the proportion (as estimated by the Secretary from time to time) of hospitals' costs which are attributable to wages and wage-related costs of the DRG prospective payment rates. We refer to the proportion of hospitals' costs that are attributable to wages and wage-related costs as the “labor-related share.” For FY 2020, as discussed in section III. of the preamble of this final rule, as we proposed, we are continuing to use a labor-related share of 68.3 percent for the national standardized amounts for all IPPS hospitals (including hospitals in Puerto Rico) that have a wage index value that is greater than 1.0000. Consistent with section 1886(d)(3)(E) of the Act, as we proposed, we applied the wage index to a labor-related share of 62 percent of the national standardized amount for all IPPS hospitals (including hospitals in Puerto Rico) whose wage index values are less than or equal to 1.0000.
The standardized amounts for operating costs appear in Tables 1A, 1B, and 1C that are listed and published in section VI. of the Addendum to this final rule and are available via the internet on the CMS website.
2. Computing the National Average Standardized Amount
Section 1886(d)(3)(A)(iv)(II) of the Act requires that, beginning with FY 2004 and thereafter, an equal standardized amount be computed for all hospitals at the level computed for large urban hospitals during FY 2003, updated by the applicable percentage update. Accordingly, as we proposed, we calculated the FY 2020 national average standardized amount irrespective of whether a hospital is located in an urban or rural location.
3. Updating the National Average Standardized Amount
Section 1886(b)(3)(B) of the Act specifies the applicable percentage increase used to update the standardized amount for payment for inpatient hospital operating costs. We note that, in compliance with section 404 of the MMA, in this final rule, as we proposed, we used the 2014-based IPPS operating and capital market baskets for FY 2020. As discussed in section IV.B. of the preamble of this final rule, in accordance with section 1886(b)(3)(B) of the Act, as amended by section 3401(a) of the Affordable Care Act, as we proposed, we reduced the FY 2020 applicable percentage increase (which for this final rule is based on IGI's second quarter 2019 forecast of the 2014-based IPPS market basket) by the MFP adjustment (the 10-year moving average of MFP for the period ending FY 2020) of 0.4 percentage point, which for this final rule is also calculated based on IGI's second quarter 2019 forecast.
Based on IGI's 2019 second quarter forecast of the hospital market basket increase (as discussed in Appendix B of this final rule), the forecast of the hospital market basket increase for FY 2020 for this final rule is 3.0 percent. As discussed earlier, for FY 2020, depending on whether a hospital submits quality data under the rules established in accordance with section 1886(b)(3)(B)(viii) of the Act and is a meaningful EHR user under section 1886(b)(3)(B)(ix) of the Act, there are four possible applicable percentage increases that can be applied to the standardized amount. We refer readers to section IV.B. of the preamble of this final rule for a complete discussion on the FY 2020 inpatient hospital update to the standardized amount. We also refer readers to the table above for the four possible applicable percentage increases that will be applied to update the national standardized amount. The standardized amounts shown in Tables 1A through 1C that are published in section VI. of this Addendum and that are available via the internet on the CMS website reflect these differential amounts.
Although the update factors for FY 2020 are set by law, we are required by section 1886(e)(4) of the Act to recommend, taking into account MedPAC's recommendations, appropriate update factors for FY 2020 for both IPPS hospitals and hospitals and hospital units excluded from the IPPS. Section 1886(e)(5)(A) of the Act requires that we publish our recommendations in the Federal Register for public comment. Our recommendation on the update factors is set forth in Appendix B of this final rule.
4. Methodology for Calculation of the Average Standardized Amount
The methodology we used to calculate the FY 2020 standardized amount is as follows:
- To ensure we are only including hospitals paid under the IPPS in the calculation of the standardized amount, we applied the following inclusion and exclusion criteria: Include hospitals whose last four digits fall between 0001 and 0879 (section 2779A1 of Chapter 2 of the State Operations Manual on the CMS website at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/som107c02.pdf); exclude CAHs at the time of this final rule; exclude hospitals in Maryland (because these hospitals are paid under an all payer model under section 1115A of the Act); and remove PPS-excluded cancer hospitals that have a “V” in the fifth position of their provider number or a “E” or “F” in the sixth position.
- As in the past, we adjusted the FY 2020 standardized amount to remove the effects of the FY 2019 geographic reclassifications and outlier payments before applying the FY 2020 updates. We then applied budget neutrality offsets for outliers and geographic reclassifications to the standardized amount based on FY 2020 payment policies.
- We do not remove the prior year's budget neutrality adjustments for reclassification and recalibration of the DRG relative weights and for updated wage data because, in accordance with sections 1886(d)(4)(C)(iii) and 1886(d)(3)(E) of the Act, estimated aggregate payments after updates in the DRG relative weights and wage index should equal estimated aggregate payments prior to the changes. If we removed the prior year's adjustment, we would not satisfy these conditions.
Budget neutrality is determined by comparing aggregate IPPS payments before and after making changes that are required to be budget neutral (for example, changes to MS-DRG classifications, recalibration of the MS-DRG relative weights, updates to the wage index, and different geographic reclassifications). We include outlier payments in the simulations because they may be affected by changes in these parameters.
- Consistent with our methodology established in the FY 2011 IPPS/LTCH PPS final rule (75 FR 50422 through 50433), because IME Medicare Advantage payments are made to IPPS hospitals under section 1886(d) of the Act, we believe these payments must be part of these budget neutrality calculations. However, we note that it is not necessary to include Medicare Advantage IME payments in the outlier threshold calculation or the outlier offset to the standardized amount because the statute requires that outlier payments be not less than 5 percent nor more than 6 percent of total “operating DRG payments,” which does not include IME and DSH payments. We refer readers to the FY 2011 IPPS/LTCH PPS final rule for a complete discussion on our methodology of identifying and adding the total Medicare Advantage IME payment amount to the budget neutrality adjustments.
- Consistent with the methodology in the FY 2012 IPPS/LTCH PPS final rule, in order to ensure that we capture only fee-for-service claims, we are only including claims with a “Claim Type” of 60 (which is a field on the MedPAR file that indicates a claim is an FFS claim).
- Consistent with our methodology established in the FY 2017 IPPS/LTCH PPS final rule (81 FR 57277), in order to further ensure that we capture only FFS claims, we are excluding claims with a “GHOPAID” indicator of 1 (which is a field on the MedPAR file that indicates a claim is not an FFS claim and is paid by a Group Health Organization).
- Consistent with our methodology established in the FY 2011 IPPS/LTCH PPS final rule (75 FR 50422 through 50423), we examine the MedPAR file and remove pharmacy charges for anti-hemophilic blood factor (which are paid separately under the IPPS) with an indicator of “3” for blood clotting with a revenue code of “0636” from the covered charge field for the budget neutrality adjustments. We also remove organ acquisition charges from the covered charge field for the budget neutrality adjustments because organ acquisition is a pass-through payment not paid under the IPPS.
- The participation of hospitals under the BPCI (Bundled Payments for Care Improvement) Advanced Model started on October 1, 2018. The BPCI Advanced Model, tested under the authority of section 3021 of the Affordable Care Act (codified at section 1115A of the Act), is comprised of a single payment and risk track, which bundles payments for multiple services beneficiaries receive during a Clinical Episode. Acute care hospitals may participate in the BPCI Advanced Model in one of two capacities: As a model Participant or as a downstream Episode Initiator. Regardless of the capacity in which they participate in the BPCI Advanced Model, participating acute care hospitals will continue to receive IPPS payments under section 1886(d) of the Act. Acute care hospitals that are Participants also assume financial and quality performance accountability for Clinical Episodes in the form of a reconciliation payment. For additional information on the BPCI Advanced Model, we refer readers to the BPCI Advanced web page on the CMS Center for Medicare and Medicaid Innovation's website at: https://innovation.cms.gov/initiatives/bpci-advanced/.
For FY 2020, consistent with how we treated hospitals that participated in the BPCI Advanced Model in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41259), as we proposed, we are including all applicable data from subsection (d) hospitals participating in the BPCI Advanced Model in our IPPS payment modeling and ratesetting calculations. We believe it is appropriate to include all applicable data from the subsection (d) hospitals participating in the BPCI Advanced Model in our IPPS payment modeling and ratesetting calculations because these hospitals are still receiving regular IPPS fee-for-service payments under section 1886(d) of the Act. For the same reasons, as we also proposed, we included all applicable data from subsection (d) hospitals participating in the Comprehensive Care for Joint Replacement (CJR) Model in our IPPS payment modeling and ratesetting calculations.
- Consistent with our methodology established in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53687 through 53688), we believe that it is appropriate to include adjustments for the Hospital Readmissions Reduction Program and the Hospital VBP Program (established under the Affordable Care Act) within our budget neutrality calculations.
Both the hospital readmissions payment adjustment (reduction) and the hospital VBP payment adjustment (redistribution) are applied on a claim-by-claim basis by adjusting, as applicable, the base-operating DRG payment amount for individual subsection (d) hospitals, which affects the overall sum of aggregate payments on each side of the comparison within the budget neutrality calculations.
In order to properly determine aggregate payments on each side of the comparison, consistent with the approach we have taken in prior years, for FY 2020 and subsequent years, as we proposed, we are continuing to apply a proxy based on the prior fiscal year hospital readmissions payment adjustment (for FY 2020, this will be FY 2019 final adjustment factors) and a proxy based on the prior fiscal year hospital VBP payment adjustment (for FY 2020, this will be FY 2019 final adjustment factors) on each side of the comparison, consistent with the methodology that we adopted in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53687 through 53688). That is, we applied a proxy readmissions payment adjustment factor and a proxy hospital VBP payment adjustment factor from the prior final rule on both sides of our comparison of aggregate payments when determining all budget neutrality factors described in section II.A.4. of this Addendum.
For the purpose of calculating the proxy FY 2020 readmissions payment adjustment factors, for both the proposed rule and this final rule, as discussed in section IV.H. of the preamble of this final rule, we used the proportion of dually-eligible Medicare beneficiaries, excess readmission ratios, and aggregate payments for excess readmissions from the prior fiscal year's applicable period because, at the time of the development of the proposed rule and this final rule, hospitals will not yet have had the opportunity to review and correct the data (program calculations based on the FY 2020 applicable period of July 1, 2015 to June 30, 2018) before the data are made public under our policy regarding the reporting of hospital-specific readmission rates, consistent with section 1886(q)(6) of the Act. (For additional information on our general policy for the reporting of hospital-specific readmission rates, consistent with section 1886(q)(6) of the Act, we refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53399 through 53400) and section IV.G. of the preamble of this final rule.)
In addition, for FY 2020, for the purpose of modeling aggregate payments when determining all budget neutrality factors, as we proposed, we used proxy hospital VBP payment adjustment factors for FY 2020 that are based on data from the prior fiscal year's applicable period because hospitals have not yet had an opportunity to review and submit corrections for their data from the FY 2020 performance period. (For additional information on our policy regarding the review and correction of hospital-specific measure rates under the Hospital VBP Program, consistent with section 1886(o)(10)(A)(ii) of the Act, we refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53578 through 53581), the CY 2012 OPPS/ASC final rule with comment period (76 FR 74544 through 74547), and the Hospital Inpatient VBP final rule (76 FR 26534 through 26536).)
- The Affordable Care Act also established section 1886(r) of the Act, which modifies the methodology for computing the Medicare DSH payment adjustment beginning in FY 2014. Beginning in FY 2014, IPPS hospitals receiving Medicare DSH payment adjustments receive an empirically justified Medicare DSH payment equal to 25 percent of the amount that would previously have been received under the statutory formula set forth under section 1886(d)(5)(F) of the Act governing the Medicare DSH payment adjustment. In accordance with section 1886(r)(2) of the Act, the remaining amount, equal to an estimate of 75 percent of what otherwise would have been paid as Medicare DSH payments, reduced to reflect changes in the percentage of individuals who are uninsured and any additional statutory adjustment, will be available to make additional payments to Medicare DSH hospitals based on their share of the total amount of uncompensated care reported by Medicare DSH hospitals for a given time period. In order to properly determine aggregate payments on each side of the comparison for budget neutrality, prior to FY 2014, we included estimated Medicare DSH payments on both sides of our comparison of aggregate payments when determining all budget neutrality factors described in section II.A.4. of this Addendum.
To do this for FY 2020 (as we did for the last 6 fiscal years), as we proposed, we included estimated empirically justified Medicare DSH payments that will be paid in accordance with section 1886(r)(1) of the Act and estimates of the additional uncompensated care payments made to hospitals receiving Medicare DSH payment adjustments as described by section 1886(r)(2) of the Act. That is, we considered estimated empirically justified Medicare DSH payments at 25 percent of what would otherwise have been paid, and also the estimated additional uncompensated care payments for hospitals receiving Medicare DSH payment adjustments on both sides of our comparison of aggregate payments when determining all budget neutrality factors described in section II.A.4. of this Addendum.
- When calculating total payments for budget neutrality, to determine total payments for SCHs, we model total hospital-specific rate payments and total Federal rate payments and then include whichever one of the total payments is greater. As discussed in section IV.F. of the preamble of this final rule and below, we are continuing to use the FY 2014 finalized methodology under which we take into consideration uncompensated care payments in the comparison of payments under the Federal rate and the hospital-specific rate for SCHs. Therefore, we included estimated uncompensated care payments in this comparison.
Similarly, for MDHs, as discussed in section IV.F. of the preamble of this final rule, when computing payments under the Federal national rate plus 75 percent of the difference between the payments under the Federal national rate and the payments under the updated hospital-specific rate, as we proposed, we continued to take into consideration uncompensated care payments in the computation of payments under the Federal rate and the hospital-specific rate for MDHs.
- As we proposed, we include an adjustment to the standardized amount for those hospitals that are not meaningful EHR users in our modeling of aggregate payments for budget neutrality for FY 2020. Similar to FY 2019, we are including this adjustment based on data on the prior year's performance. Payments for hospitals will be estimated based on the applicable standardized amount in Tables 1A and 1B for discharges occurring in FY 2020.
- In our determination of all budget neutrality factors described in section II.A.4. of this Addendum, we used transfer-adjusted discharges. Specifically, we calculated the transfer-adjusted discharges using the statutory expansion of the postacute care transfer policy to include discharges to hospice care by a hospice program as discussed in section IV.A.2.b. of the preamble of this final rule.
a. Recalibration of MS-DRG Relative Weights
Section 1886(d)(4)(C)(iii) of the Act specifies that, beginning in FY 1991, the annual DRG reclassification and recalibration of the relative weights must be made in a manner that ensures that aggregate payments to hospitals are not affected. As discussed in section II.H. of the preamble of this final rule, we normalized the recalibrated MS-DRG relative weights by an adjustment factor so that the average case relative weight after recalibration is equal to the average case relative weight prior to recalibration. However, equating the average case relative weight after recalibration to the average case relative weight before recalibration does not necessarily achieve budget neutrality with respect to aggregate payments to hospitals because payments to hospitals are affected by factors other than average case relative weight. Therefore, as we have done in past years, we are making a budget neutrality adjustment to ensure that the requirement of section 1886(d)(4)(C)(iii) of the Act is met.
For FY 2020, to comply with the requirement that MS-DRG reclassification and recalibration of the relative weights be budget neutral for the standardized amount and the hospital-specific rates, we used FY 2018 discharge data to simulate payments and compared the following:
- Aggregate payments using the FY 2019 labor-related share percentages, the FY 2019 relative weights, and the FY 2019 pre-reclassified wage data, and applied the FY 2020 hospital readmissions payment adjustments and estimated FY 2020 hospital VBP payment adjustments; and
- Aggregate payments using the FY 2019 labor-related share percentages, the FY 2020 relative weights, and the FY 2019 pre-reclassified wage data, and applied the FY 2020 hospital readmissions payment adjustments and estimated FY 2020 hospital VBP payment adjustments applied above. (We note that these FY 2020 relative weights reflect our temporary measure for FY 2020, as discussed in section II.G. of the preamble of this final rule, to set the FY 2020 relative weight for the MS-DRG equal to the FY 2019 relative weight, which was in turn set equal to the FY 2018 relative weight). Based on this comparison, we computed a budget neutrality adjustment factor equal to 0.997649 and applied this factor to the standardized amount. As discussed in section IV. of this Addendum, as we also proposed, we also applied the MS-DRG reclassification and recalibration budget neutrality factor of 0.997649 to the hospital-specific rates that are effective for cost reporting periods beginning on or after October 1, 2019.
b. Updated Wage Index—Budget Neutrality Adjustment
Section 1886(d)(3)(E)(i) of the Act requires us to update the hospital wage index on an annual basis beginning October 1, 1993. This provision also requires us to make any updates or adjustments to the wage index in a manner that ensures that aggregate payments to hospitals are not affected by the change in the wage index. Section 1886(d)(3)(E)(i) of the Act requires that we implement the wage index adjustment in a budget neutral manner. However, section 1886(d)(3)(E)(ii) of the Act sets the labor-related share at 62 percent for hospitals with a wage index less than or equal to 1.0000, and section 1886(d)(3)(E)(i) of the Act provides that the Secretary shall calculate the budget neutrality adjustment for the adjustments or updates made under that provision as if section 1886(d)(3)(E)(ii) of the Act had not been enacted. In other words, this section of the statute requires that we implement the updates to the wage index in a budget neutral manner, but that our budget neutrality adjustment should not take into account the requirement that we set the labor-related share for hospitals with wage indexes less than or equal to 1.0000 at the more advantageous level of 62 percent. Therefore, for purposes of this budget neutrality adjustment, section 1886(d)(3)(E)(i) of the Act prohibits us from taking into account the fact that hospitals with a wage index less than or equal to 1.0000 are paid using a labor-related share of 62 percent. Consistent with current policy, for FY 2020, as we proposed, we are adjusting 100 percent of the wage index factor for occupational mix. We describe the occupational mix adjustment in section III.E. of the preamble of this final rule.
To compute a budget neutrality adjustment factor for wage index and labor-related share percentage changes, we used FY 2018 discharge data to simulate payments and compared the following:
- Aggregate payments using the FY 2020 relative weights and the FY 2019 pre-reclassified wage indexes, applied the FY 2019 labor-related share of 68.3 percent to all hospitals (regardless of whether the hospital's wage index was above or below 1.0000), and applied the FY 2020 hospital readmissions payment adjustment and the estimated FY 2020 hospital VBP payment adjustment; and
- Aggregate payments using the FY 2020 relative weights and the FY 2020 pre-reclassified wage indexes, applied the labor-related share for FY 2020 of 68.3 percent to all hospitals (regardless of whether the hospital's wage index was above or below 1.0000), and applied the same FY 2020 hospital readmissions payment adjustments and estimated FY 2020 hospital VBP payment adjustments applied above.
In addition, we applied the MS-DRG reclassification and recalibration budget neutrality adjustment factor (derived in the first step) to the payment rates that were used to simulate payments for this comparison of aggregate payments from FY 2019 to FY 2020. By applying this methodology, we determined a budget neutrality adjustment factor of 1.001573 for changes to the wage index.
c. Reclassified Hospitals—Budget Neutrality Adjustment
Section 1886(d)(8)(B) of the Act provides that certain rural hospitals are deemed urban. In addition, section 1886(d)(10) of the Act provides for the reclassification of hospitals based on determinations by the MGCRB. Under section 1886(d)(10) of the Act, a hospital may be reclassified for purposes of the wage index.
Under section 1886(d)(8)(D) of the Act, the Secretary is required to adjust the standardized amount to ensure that aggregate payments under the IPPS after implementation of the provisions of sections 1886(d)(8)(B) and (C) and 1886(d)(10) of the Act are equal to the aggregate prospective payments that would have been made absent these provisions. We note that, with regard to the requirement under section 1886(d)(8)(C)(iii) of the Act, in our calculation of a budget neutrality adjustment factor, we applied the provisions of our policy proposal discussed in section III.N. of the preamble of this final rule to exclude the wage data of urban hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented in § 412.103) from the calculation of “the wage index for rural areas in the State in which the county is located.” We refer readers to the FY 2015 IPPS final rule (79 FR 50371 through 50372) for a complete discussion regarding the requirement of section 1886(d)(8)(C)(iii) of the Act. We further note that the wage index adjustments provided for under section 1886(d)(13) of the Act are not budget neutral. Section 1886(d)(13)(H) of the Act provides that any increase in a wage index under section 1886(d)(13) shall not be taken into account in applying any budget neutrality adjustment with respect to such index under section 1886(d)(8)(D) of the Act. To calculate the budget neutrality adjustment factor for FY 2020, we used FY 2018 discharge data to simulate payments and compared the following:
- Aggregate payments using the FY 2020 labor-related share percentages, the FY 2020 relative weights, and the FY 2020 wage data prior to any reclassifications under sections 1886(d)(8)(B) and (C) and 1886(d)(10) of the Act, and applied the FY 2020 hospital readmissions payment adjustments and the estimated FY 2020 hospital VBP payment adjustments; and
- Aggregate payments using the FY 2020 labor-related share percentages, the FY 2020 relative weights, and the FY 2020 wage data after such reclassifications, and applied the same FY 2020 hospital readmissions payment adjustments and the estimated FY 2020 hospital VBP payment adjustments applied above.
We note that the reclassifications applied under the second simulation and comparison are those listed in Table 2 associated with this final rule, which is available via the internet on the CMS website. This table reflects reclassification crosswalks for FY 2020, and applies the policies explained in section III. of the preamble of this final rule. Based on these simulations, we calculated a budget neutrality adjustment factor of 0.985425 to ensure that the effects of these provisions are budget neutral, consistent with the statute.
The FY 2020 budget neutrality adjustment factor was applied to the standardized amount after removing the effects of the FY 2019 budget neutrality adjustment factor. We note that the FY 2020 budget neutrality adjustment reflects FY 2020 wage index reclassifications approved by the MGCRB or the Administrator at the time of development of this final rule.
d. Rural Floor Budget Neutrality Adjustment
Under § 412.64(e)(4), we make an adjustment to the wage index to ensure that aggregate payments after implementation of the rural floor under section 4410 of the BBA (Pub. L. 105-33) are equal to the aggregate prospective payments that would have been made in the absence of this provision. Consistent with section 3141 of the Affordable Care Act and as discussed in section III.G. of the preamble of this final rule and codified at § 412.64(e)(4)(ii), the budget neutrality adjustment for the rural floor is a national adjustment to the wage index. We note, as discussed in section III.N. of the preamble of this final rule, we are calculating the rural floor without including the wage data of urban hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented in § 412.103).
Similar to our calculation in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50369 through 50370), for FY 2020, as we proposed, we are calculating a national rural Puerto Rico wage index. Because there are no rural Puerto Rico hospitals with established wage data, our calculation of the FY 2020 rural Puerto Rico wage index is based on the policy adopted in the FY 2008 IPPS final rule with comment period (72 FR 47323). That is, we used the unweighted average of the wage indexes from all CBSAs (urban areas) that are contiguous (share a border with) to the rural counties to compute the rural floor (72 FR 47323; 76 FR 51594). Under the OMB labor market area delineations, except for Arecibo, Puerto Rico (CBSA 11640), all other Puerto Rico urban areas are contiguous to a rural area. Therefore, based on our existing policy, the FY 2020 rural Puerto Rico wage index is calculated based on the average of the FY 2020 wage indexes for the following urban areas: Aguadilla-Isabela, PR (CBSA 10380); Guayama, PR (CBSA 25020); Mayaguez, PR (CBSA 32420); Ponce, PR (CBSA 38660); San German, PR (CBSA 41900); and San Juan-Carolina-Caguas, PR (CBSA 41980).
To calculate the national rural floor budget neutrality adjustment factor, we used FY 2018 discharge data to simulate payments and the post-reclassified national wage indexes and compared the following:
- National simulated payments without the national rural floor; and
- National simulated payments with the national rural floor.
Based on this comparison, we determined a national rural floor budget neutrality adjustment factor of 0.997081. The national adjustment was applied to the national wage indexes to produce a national rural floor budget neutral wage index.
e. Rural Community Hospital Demonstration Program Adjustment
In section IV.K. of the preamble of this final rule, we discuss the Rural Community Hospital Demonstration program, which was originally authorized for a 5-year period by section 410A of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) (Pub. L. 108-173), and extended for another 5-year period by sections 3123 and 10313 of the Affordable Care Act (Pub. L. 111-148). Subsequently, section 15003 of the 21st Century Cures Act (Pub. L. 114-255), enacted December 13, 2016, amended section 410A of Public Law 108-173 to require a 10-year extension period (in place of the 5-year extension required by the Affordable Care Act, as further discussed below). We make an adjustment to the standardized amount to ensure the effects of the Rural Community Hospital Demonstration program are budget neutral as required under section 410A(c)(2) of Public Law 108-173. We refer readers to section IV.K. of the preamble of this final rule for complete details regarding the Rural Community Hospital Demonstration.
With regard to budget neutrality, as mentioned earlier, we make an adjustment to the standardized amount to ensure the effects of the Rural Community Hospital Demonstration are budget neutral, as required under section 410A(c)(2) of Pub. L. 108-173. For FY 2020, based on the latest data for this final rule, the total amount that we are applying to make an adjustment to the standardized amounts to ensure the effects of the Rural Community Hospital Demonstration program are budget neutral is $25,742,822. Accordingly, using the most recent data available to account for the estimated costs of the demonstration program, for FY 2020, we computed a factor of 0.999771 for the Rural Community Hospital Demonstration budget neutrality adjustment that will be applied to the IPPS standard Federal payment rate. We refer readers to section IV.K. of the preamble of this final rule for complete details regarding the calculation of the amount we are applying to make an adjustment to the standardized amount.
f. Budget Neutrality Adjustment for Lowest Quartile Wage Index Hospital Policy
As discussed in section III.N. of the preamble of this final rule, to address wage index disparities, we are establishing a policy to increase the wage index values for hospitals with a wage index value below the 25th percentile wage index value across all hospitals. In addition, under our finalized policy, in order to offset the estimated increase in IPPS payments to hospitals with wage index values below the 25th percentile, we are adjusting the standardized amount. We refer readers to section III.N. of the preamble of this final rule for a complete discussion regarding this finalized policy.
To calculate this budget neutrality adjustment factor for FY 2020, we used FY 2018 discharge data to simulate payments and compared the following:
- Aggregate payments using the FY 2020 labor-related share percentages, the FY 2020 relative weights, and the FY 2020 wage index for each hospital before adjusting the wage indexes under the finalized policy for the lowest quartile wage index hospitals but without the 5 percent cap, and applied the FY 2020 hospital readmissions payment adjustments and the estimated FY 2020 hospital VBP payment adjustments, and the operating outlier reconciliation adjusted outlier percentage discussed below; and
- Aggregate payments using the FY 2020 labor-related share percentages, the FY 2020 relative weights, and the FY 2020 wage index for each hospital after adjusting the wage indexes under the finalized policy for the lowest quartile wage index hospitals but without the 5 percent cap, and applied the same FY 2020 hospital readmissions payment adjustments and the estimated FY 2020 hospital VBP payment adjustments applied above, and the operating outlier reconciliation adjusted outlier percentage discussed below. This FY 2020 budget neutrality adjustment factor was applied to the standardized amount. Based on this comparison, we determined the lowest quartile wage index budget neutrality adjustment factor of 0.997987.
g. Transition Budget Neutrality Adjustment Reflecting the FY 2020 Wage Index Changes
In section III.N. of the preamble of this final rule, we state that we recognize that, absent further adjustments, the combined effect of the changes to the FY 2020 wage index could lead to significant decreases in the wage index values for some hospitals depending on the data for the final rule. Therefore, for FY 2020, as we proposed, we established a transition wage index to help mitigate any significant decreases in the wage index values of hospitals compared to their final wage indexes for FY 2019. Specifically, we are placing a 5-percent cap on any decrease in a hospital's wage index from the hospital's final wage index in FY 2019. In other words, we are establishing a policy that a hospital's final wage index for FY 2020 will not be less than 95 percent of its final wage index for FY 2019. For FY 2020, we are using our exceptions and adjustments authority under section 1886(d)(5)(I)(i) of the Act to apply a budget neutrality adjustment to the standardized amount so that our transition for hospitals negatively impacted (described in section III.N.2.d. of the preamble of this final rule) is implemented in a budget neutral manner. We refer readers to section III.N. of the preamble of this final rule for a complete discussion regarding this finalized policy.
To calculate a transition budget neutrality adjustment factor for FY 2020, we used FY 2018 discharge data to simulate payments and compared the following:
- Aggregate payments without the 5-percent cap using the FY 2020 labor-related share percentages, the FY 2020 relative weights, the FY 2020 wage index for each hospital after adjusting the wage indexes under the finalized policy for the lowest quartile wage index hospitals with the associated budget neutrality adjustment to the standardized amount, and applied the FY 2020 hospital readmissions payment adjustments and the estimated FY 2020 hospital VBP payment adjustments, and the operating outlier reconciliation adjusted outlier percentage discussed below; and
- Aggregate payments with the 5-percent cap using the FY 2020 labor-related share percentages, the FY 2020 relative weights, the FY 2020 wage index for each hospital after adjusting the wage indexes under the finalized policy for the lowest quartile wage index hospitals with the associated budget neutrality adjustment to the standardized amount, and applied the FY 2020 hospital readmissions payment adjustments and the estimated FY 2020 hospital VBP payment adjustments, and the operating outlier reconciliation adjusted outlier percentage discussed below.
This FY 2020 budget neutrality adjustment factor was applied to the standardized amount. Based on this comparison, we determined a transition budget neutrality adjustment factor of 0.998838. We note that Table 2 associated with this final rule (which is available via the internet on the CMS website) contains the wage index by provider before adjusting the wage indexes under the finalized policy for lowest quartile wage index hospitals and the 5-percent cap and the wage index by provider after the application of these policies.
h. Adjustment for FY 2020 Required Under Section 414 of Public Law 114-10 (MACRA)
As stated in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56785), once the recoupment required under section 631 of the ATRA was complete, we had anticipated making a single positive adjustment in FY 2018 to offset the reductions required to recoup the $11 billion under section 631 of the ATRA. However, section 414 of the MACRA (which was enacted on April 16, 2015) replaced the single positive adjustment we intended to make in FY 2018 with a 0.5 percent positive adjustment for each of FYs 2018 through 2023. (As noted in the FY 2018 IPPS/LTCH PPS proposed and final rules, section 15005 of the 21st Century Cures Act (Pub. L. 114-255), which was enacted December 13, 2016, reduced the adjustment for FY 2018 from 0.5 percentage points to 0.4588 percentage points.) Therefore, for FY 2020, as we proposed, we are implementing the required +0.5 percent adjustment to the standardized amount. This is a permanent adjustment to the payment rates.
i. Outlier Payments
Section 1886(d)(5)(A) of the Act provides for payments in addition to the basic prospective payments for “outlier” cases involving extraordinarily high costs. To qualify for outlier payments, a case must have costs greater than the sum of the prospective payment rate for the MS-DRG, any IME and DSH payments, uncompensated care payments, any new technology add-on payments, and the “outlier threshold” or “fixed-loss” amount (a dollar amount by which the costs of a case must exceed payments in order to qualify for an outlier payment). We refer to the sum of the prospective payment rate for the MS-DRG, any IME and DSH payments, uncompensated care payments, any new technology add-on payments, and the outlier threshold as the outlier “fixed-loss cost threshold.” To determine whether the costs of a case exceed the fixed-loss cost threshold, a hospital's CCR is applied to the total covered charges for the case to convert the charges to estimated costs. Payments for eligible cases are then made based on a marginal cost factor, which is a percentage of the estimated costs above the fixed-loss cost threshold. The marginal cost factor for FY 2020 is 80 percent, or 90 percent for burn MS-DRGs 927, 928, 929, 933, 934 and 935. We have used a marginal cost factor of 90 percent since FY 1989 (54 FR 36479 through 36480) for designated burn DRGs as well as a marginal cost factor of 80 percent for all other DRGs since FY 1995 (59 FR 45367).
In accordance with section 1886(d)(5)(A)(iv) of the Act, outlier payments for any year are projected to be not less than 5 percent nor more than 6 percent of total operating DRG payments (which does not include IME and DSH payments) plus outlier payments. Similar to prior years, when setting the outlier threshold, we compute the percent target by dividing the total operating outlier payments by the total operating DRG payments plus outlier payments. As discussed in the next section, for FY 2020, as we proposed, we incorporated an estimate of outlier reconciliation when setting the outlier threshold. We do not include any other payments such as IME and DSH within the outlier target amount. Therefore, it is not necessary to include Medicare Advantage IME payments in the outlier threshold calculation. Section 1886(d)(3)(B) of the Act requires the Secretary to reduce the average standardized amount by a factor to account for the estimated proportion of total DRG payments made to outlier cases. More information on outlier payments may be found on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/outlier.htm.
(1) Methodology To Incorporate an Estimate of Outlier Reconciliation in the FY 2020 Outlier Fixed-Loss Cost Threshold
The regulations in 42 CFR 412.84(i)(4) state that any outlier reconciliation at cost report settlement will be based on operating and capital cost-to-charge ratios (CCRs) calculated based on a ratio of costs to charges computed from the relevant cost report and charge data determined at the time the cost report coinciding with the discharge is settled. We have instructed MACs to identify for CMS any instances where: (1) A hospital's actual CCR for the cost reporting period fluctuates plus or minus 10 percentage points compared to the interim CCR used to calculate outlier payments when a bill is processed; and (2) the total outlier payments for the hospital exceeded $500,000.00 for that cost reporting period. If we determine that a hospital's outlier payments should be reconciled, we reconcile both operating and capital outlier payments. We refer readers to section 20.1.2.5 of Chapter 3 of the Medicare Claims Processing Manual (available on the CMS website at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c03.pdf) for complete details regarding outlier reconciliation. The regulation at § 412.84(m) further states that at the time of any outlier reconciliation under § 412.84(i)(4), outlier payments may be adjusted to account for the time value of any underpayments or overpayments. Section 20.1.2.6 of Chapter 3 of the Medicare Claims Processing Manual contains instructions on how to assess the time value of money for reconciled outlier amounts.
If the operating CCR of a hospital subject to outlier reconciliation is lower at cost report settlement compared to the operating CCR used for payment, the hospital will owe CMS money because it received an outlier overpayment at the time of claim payment. Conversely, if the operating CCR increases at cost report settlement compared to the operating CCR used for payment, CMS will owe the hospital money because the hospital outlier payments were underpaid. In prior fiscal years, commenters have requested that CMS incorporate outlier reconciliation in the development of the outlier threshold.
As we have stated in prior rulemaking, outlier reconciliation is a function of the cost report, and MACs record the outlier reconciliation amount on each provider's cost report. Therefore, as the MACs continue to perform these outlier reconciliations, they record these amounts on the cost report, which are then publicly available through the HCRIS database. Therefore, the outlier reconciliation data used in the following process is publicly available through the cost report.
In the FY 2004 IPPS final rule (68 FR 45476 through 45477), we included an estimate for outlier reconciliation that identified and adjusted the CCRs of hospitals in our calculation of the outlier fixed loss threshold. However, outlier cases are difficult to predict with regard to their occurrence for any individual hospital. Generally, an outlier payment is made if the estimated costs of the case exceed the sum of the outlier threshold plus the relevant payment amounts. There are many different variables that determine whether a case will be eligible for an outlier payment, including the CCR, the estimated costs of the case, the payment amounts, and the outlier threshold itself. We refer readers to section II.C.1. of this Addendum for additional detail regarding how the outlier payment is computed. In addition, predicting both the specific hospitals that will have outlier payments reconciled and the dollar amount of any such outlier reconciliation is difficult, which makes incorporating reconciliation into the modeling of the outlier threshold challenging.
In the FY 2019 IPPS/LTCH PPS final rule and other prior rulemaking, we have stated that we continue to believe that, due to the policy implemented in the June 9, 2003 Outlier Final Rule (68 FR 34494), CCRs will no longer fluctuate as significantly and, therefore, few hospitals will actually have their outlier payments reconciled upon cost report settlement. In addition, we stated that it is difficult to predict the specific hospitals that will have fluctuating CCRs and outlier payments reconciled in any given year. In the FY 2020 IPPS/LTCH PPS proposed rule, we noted that in the FY 2019 IPPS/LTCH PPS final rule, in response to comments expressing concern with CMS' decision not to consider outlier reconciliation in developing the outlier threshold, we stated that we intended to revisit this issue in next year's proposed rule (that is, the FY 2020 proposed rule) as we continued to consider the feasibility of including outlier reconciliation in the modeling of the outlier threshold.
Since the issuance of the FY 2019 IPPS/LTCH PPS final rule, we have continued to consider how outlier reconciliation could be included in the modeling of the outlier threshold. Rather than trying to predict which claims and/or hospitals may be subject to outlier reconciliation for FY 2020, we stated in the proposed rule that we believe a methodology that incorporates an estimate of outlier reconciliation dollars based on actual outlier reconciliation amounts reported in historical cost reports would be a more feasible approach and provide a better estimate and predictor of outlier reconciliation for the upcoming fiscal year. We stated that we believe this methodology would address concerns on the impact of outlier reconciliation on the modeling of the outlier threshold.
We stated that we also believe the cost report data available in the HCRIS may be sufficiently complete for certain historical fiscal years to allow for calculating an estimate of outlier reconciliation for FY 2020. We issued Change Request 7192 on December 3, 2010 (available via the internet on the CMS website at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R2111CP.pdf) which updated a utility to reprice outlier claims for purposes of outlier reconciliation. Prior to this update, cost reports subject to outlier reconciliation were being held open until there was a mechanism to perform the outlier reconciliation. The outlier reconciliation amounts on the cost report are reflected in HCRIS once the cost report is final settled. As MACs began performing the outlier reconciliations, they were able to final settle many of these cost reports and the data for outlier reconciliation began to become available in HCRIS. However, even with a utility available beginning in 2010, not all cost reports were final settled for reasons other than outlier reconciliation. Therefore, HCRIS may not have reflected all of the hospitals subject to outlier reconciliation. We believe that many of these other reasons for the delay in cost reports being final settled have now been resolved. In contrast to prior years, HCRIS now contains more final settled cost reports that include outlier reconciliation, in particular for FY 2014, as we discuss below, which can be used to develop an annual estimate of total dollars related to outlier reconciliation payments based on this historical cost report data. Therefore, for FY 2020, we proposed to incorporate into the outlier model the total outlier reconciliation dollars based on historical data. We are providing below a step-by-step explanation of how we proposed, and after consideration of public comments, are finalizing, to incorporate these dollars into the model.
Currently, outlier reconciliation is among the last steps before the cost report is final settled. In order to determine if a hospital meets the outlier reconciliation criteria, all cost report adjustments must be finalized in order to compare the final settled operating CCR from the cost report to the operating CCR used for the original claim payment. Generally, MACs attempt to have a cost report final settled 12 months after the cost report is submitted by the provider to CMS. However, there are sometimes issues or adjustments that are unique to the cost report that extend the final settlement beyond 12 months. This will delay the MAC from recording the outlier reconciliation amounts on the cost report, which will also delay the availability of these amounts in HCRIS. Because of these potential delays, in the proposed rule we proposed to use the historical outlier reconciliation amounts from the FY 2014 cost reports (cost reports with a begin date on or after October 1, 2013, and on or before September 30, 2014), which we stated in the proposed rule were currently the most recent and complete set of outlier reconciliation data, which were finalized and/or approved by the MAC as of the time of development of the FY 2020 proposed rule. In the proposed rule we noted that approximately 90 percent of the FY 2014 cost reports were final settled, as compared to approximately 60 percent of the FY 2015 cost reports that were final settled. As of the December 2018 HCRIS, 16 of the FY 2014 cost reports and 8 of the FY 2015 cost reports had completed outlier reconciliation amounts. Therefore, we stated that we believed that the FY 2014 cost reports provide the most recent and complete available data to estimate the effect of outlier reconciliation dollars on the outlier cost threshold. We also stated that we considered using FY 2015 cost report data. However, because, as previously noted, the FY 2015 and later years cost reports have a larger percent of not final settled cost reports, outlier reconciliation dollars for these years may not be sufficiently available in the HCRIS. Therefore, we stated that we believed that it may not be appropriate to use those more recent cost reports to estimate outlier reconciliation for the FY 2020 proposed and final rules.
In order to prospectively determine the outlier threshold, we proposed to use the FY 2014 cost reports from the most recent publically available HCRIS extract at the time of development of the proposed and final rules. For the FY 2020 proposed rule, we used the December 2018 HCRIS extract to calculate the proposed percentage adjustment for outlier reconciliation. In the proposed rule we stated that for the FY 2020 final rule, we would use the HCRIS extract that is publically available at the time of the development of that rule which, for FY 2020, would be the March 2019 extract. We stated that we believe hospitals that have a FY 2014 cost report approved for outlier reconciliation will have had their cost reports final settled by the issuance of the proposed rule and, therefore, would have outlier reconciliation estimates available for use in the FY 2020 final rule.
(a) Incorporating a Projection of Outlier Payment Reconciliations for the FY 2020 Outlier Threshold Calculation
We proposed the following methodology to incorporate a projection of outlier payment reconciliations for the FY 2020 outlier threshold calculation.
Step 1.—Use the Federal FY 2014 cost reports for hospitals paid under the IPPS from the most recent publicly available quarterly HCRIS extract available at the time of development of the proposed and final rules, and exclude SCHs that were paid under their hospital-specific rate (that is, if Worksheet E, Part A, Line 48 is greater than Line 47 in the applicable columns). In the proposed rule, we stated that we used the December 2018 HCRIS extract for the proposed rule and that we expected to use the March 2019 HCRIS extract for the FY 2020 final rule.
Step 2.—Calculate the aggregate amount of the historical total of capital outlier reconciliation dollars (Worksheet E, Part A, Line 93, Column 1) using the Federal FY 2014 cost reports from Step 1.
Step 3.—Calculate the aggregate amount of total capital Federal payments using the Federal FY 2014 cost reports from Step 1. The total capital Federal payments consist of the capital DRG payments, including capital indirect medical education (IME) and capital disproportionate share hospital (DSH) payments (Worksheet E, Part A, Line 50, Column 1) and the capital outlier reconciliation payments (Worksheet E, Part A, Line 93, Column 1). We note that a negative amount on Worksheet E, Part A, Line 93 for capital outlier reconciliation indicates an amount that was owed by the hospital, and a positive amount indicates this amount was paid to the hospital.
Step 4.—Divide the amount from Step 2 by the amount from Step 3 and multiply the resulting amount by 100 to produce the percentage of total capital outlier reconciliation dollars to total capital Federal payments for FY 2014. This percentage amount would be used to adjust the estimate of capital outlier payments for FY 2020 as described in Step 5.
Step 5.—Because the outlier reconciliation dollars are only available on the cost reports, and not in the specific Medicare claims data in the MedPAR file used to estimate outlier payments, we proposed that the estimate of capital outlier payments for FY 2020 would be determined by adding the percentage in Step 4 to the estimated percentage of capital outlier payments otherwise determined using the shared outlier threshold that is applicable to both hospital inpatient operating costs and hospital inpatient capital-related costs. (We noted that this percentage is added for capital outlier payments but subtracted in the analogous step for operating outlier payments. We have a unified outlier payment methodology that uses a shared threshold to identify outlier cases for both operating and capital payments. The difference stems from the fact that operating outlier payments are determined by first setting a “target” percentage of operating outlier payments relative to aggregate operating payments which produces the outlier threshold. Once the shared threshold is set, it is used to estimate the percentage of capital outlier payments to total capital payments based on that threshold. Because the threshold is already set based on the operating target, rather than adjusting the threshold (or operating target), we adjusted the percentage of capital outlier to total capital payments to account for the estimated effect of capital outlier reconciliation payments. This percentage is adjusted by adding the capital outlier reconciliation percentage from Step 4 to the estimate of the percentage of capital outlier payments to total capital payments based on the shared threshold.) We stated in the proposed rule that because the aggregate capital outlier reconciliation dollars from Step 2 are negative, the estimate of capital outlier payments for FY 2020 under our proposed methodology would be lower than the percentage of capital outlier payments otherwise determined using the shared outlier threshold.
For the FY 2020 proposed rule, the estimated percentage of FY 2020 capital outlier payments otherwise determined using the shared outlier threshold was 5.39 percent (estimated capital outlier payments of $433,416,367 divided by (estimated capital outlier payments of $433,416,367 plus the estimated total capital Federal payment of $7,603,919,535)). Based on the December 2018 HCRIS, 16 hospitals had an outlier reconciliation amount recorded on Worksheet E, Part A, Line 93 for total capital outlier reconciliation dollars of negative $3,860,075 (Step 2). The total Federal capital payments based on the December 2018 HCRIS was $7,506,907,042 (Step 3) which results in a ratio (Step 4) of −0.05 percent. We stated that therefore, for FY 2020, taking into account projected capital outlier reconciliation payments under our proposed methodology would decrease the estimated percentage of FY 2020 aggregate capital outlier payments by 0.05 percent.
As explained in our discussion of the outlier threshold methodology above, we stated that we believe this is an appropriate method to include capital outlier reconciliation dollars in the estimated percentage of capital outlier payments because it uses the total outlier reconciliation dollars based on historic data rather than predicting which specific hospitals will have outlier payments reconciled for FY 2020. As discussed in section III.A.2. of the Addendum to the proposed rule and this final rule, we proposed to incorporate the capital outlier reconciliation dollars from Step 5 when applying the outlier adjustment factor in determining the capital Federal rate based on the estimated percentage of capital outlier payments to total capital Federal rate payments for FY 2020.
We invited public comment on our proposed methodology for projecting the estimate of capital outlier reconciliation and incorporating that estimate into the modeling of the estimate of FY 2020 capital outlier payments for purposes of determining the capital outlier adjustment factor.
Comment: Commenters provided similar feedback regarding the proposed methodology for projecting the estimate of capital outlier reconciliation as they did with respect to the proposed methodology for projecting the estimate of operating outlier reconciliation, as previously summarized. Commenters requested the same clarifications as with respect to the operating outlier methodology, and noted the same concern regarding completeness of FY 2014 reports compared to other earlier reporting years (FY 2012 or FY 2013).
Response: We refer readers to the response in the previous section regarding the methodology for projecting the estimate of operating outlier reconciliation and why we believe the FY 2014 cost reports are the best available data for use in calculating the estimated operating outlier reconciliation adjustments for FY 2020, as we believe these same reasons support the use of this FY 2014 data for calculating the estimated capital outlier reconciliation adjustments for FY 2020. In addition, with respect to comments regarding the proposed methodology for projecting the estimate of capital outlier reconciliation (for example, when there are multiple columns relevant to IPPS payments), we refer readers to our discussion in the previous section in response to similar comments on the estimated operating outlier reconciliation adjustment methodology. We note we use the same general methodology to project the estimate of outlier reconciliation for both operating payments and capital payments (aside from the different cost report worksheets from which the data is collected). We also note, similar to the estimated operating outlier reconciliation adjustment methodology, the proposed rule capital outlier reconciliation adjustment methodology calculation inadvertently did not incorporate the multiple columns, however these multiple columns have been used in projecting the estimated outlier reconciliation for this final rule.
Additionally, for projecting the estimate of capital outlier reconciliation, similar to our projection of the estimate of operating outlier reconciliation, we are using cost report data of 17 hospitals from the March 2019 HCRIS supplemented for two hospitals for a total of 19 hospitals. As noted above, for this final rule, 22 cost reports were used for projecting the estimate of operating outlier reconciliation; however 19 cost reports were used for projecting the estimate of capital outlier reconciliation. This difference in the number of cost reports for the operating and capital outlier reconciliation projections may be due to new hospitals defined in the regulations at 42 CFR 412.300(b) that may receive capital cost-based payments (in lieu of Federal rate payments), and therefore would not receive capital outlier payments. As a result, capital outlier reconciliation is not applicable to such hospitals since there is no capital outlier payment.
The following table shows the March 2019 HCRIS with the addition of the two hospitals' outlier reconciliation reports for this final rule:

After consideration of the comments received and for the reasons discussed in the proposed rule and this final rule, we are finalizing the methodology for projecting an estimate of capital outlier reconciliation. Therefore, for this final rule we used the same steps as described in the proposed rule and this final rule to reduce the FY 2020 capital standard Federal rate by an adjustment factor to account for the projected proportion of capital IPPS payments paid as outliers.
Specifically, for this FY 2020 final rule, as stated above, we used the March HCRIS extract of FY 2014 cost reports supplemented by the data for two additional providers. The estimated percentage of FY 2020 capital outlier payments otherwise determined using the shared outlier threshold is 5.47 percent (estimated capital outlier payments of $441,745,478 divided by (estimated capital outlier payments of $441,745,478 plus the estimated total capital Federal payment of $8,077,508,094)). Based on the March 2019 HCRIS supplemented by the data for two additional providers, 19 hospitals had an outlier reconciliation amount recorded on Worksheet E, Part A, Line 93 for total capital outlier reconciliation dollars of negative $6,196,382 (Step 2). The total Federal capital payments based on the March 2019 HCRIS is $7,570,974,974 (Step 3). The ratio (Step 4) is a negative 0.081844 percent, which, when rounded to the second digit, is negative 0.08 percent (Step 4). Therefore, for FY 2020, taking into account projected capital outlier reconciliation payments under our methodology would decrease the estimated percentage of FY 2020 aggregate capital outlier payments by 0.08 percent.
(2) FY 2020 Outlier Fixed-Loss Cost Threshold
In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50977 through 50983), in response to public comments on the FY 2013 IPPS/LTCH PPS proposed rule, we made changes to our methodology for projecting the outlier fixed-loss cost threshold for FY 2014. We refer readers to the FY 2014 IPPS/LTCH PPS final rule for a detailed discussion of the changes.
As we have done in the past, to calculate the FY 2020 outlier threshold, we simulated payments by applying FY 2020 payment rates and policies using cases from the FY 2018 MedPAR file. As noted in section II.C. of this Addendum, we specify the formula used for actual claim payment which is also used by CMS to project the outlier threshold for the upcoming fiscal year. The difference is the source of some of the variables in the formula. For example, operating and capital CCRs for actual claim payment are from the PSF while CMS uses an adjusted CCR (as described below) to project the threshold for the upcoming fiscal year. In addition, charges for a claim payment are from the bill while charges to project the threshold are from the MedPAR data with an inflation factor applied to the charges (as described earlier).
In order to determine the FY 2020 outlier threshold, we inflated the charges on the MedPAR claims by 2 years, from FY 2018 to FY 2020. To produce the most stable measure of charge inflation, we applied the following inclusion and exclusion criteria of hospitals claims in our measure of charge inflation:
- Include hospitals whose last four digits fall between 0001 and 0899 (section 2779A1 of Chapter 2 of the State Operations Manual on the CMS website at https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/som107c02.pdf); include CAHs that were IPPS hospitals for the time period of the MedPAR data being used to calculate the charge inflation factor; include hospitals in Maryland; and remove PPS-excluded cancer hospitals who have a “V” in the fifth position of their provider number or a “E” or “F” in the sixth position.
- Include providers that are in both periods of charge data that are used to calculate the 1-year average annual rate-of-change in charges per case. We note this is consistent with the methodology used since FY 2014 and are providing this as a technical clarification.
- We excluded Medicare Advantage IME claims for the reasons described in section I.A.4. of this Addendum. We refer readers to the FY 2011 IPPS/LTCH PPS final rule for a complete discussion on our methodology of identifying and adding the total Medicare Advantage IME payment amount to the budget neutrality adjustments.
- In order to ensure that we capture only FFS claims, we included claims with a “Claim Type” of 60 (which is a field on the MedPAR file that indicates a claim is an FFS claim).
- In order to further ensure that we capture only FFS claims, we excluded claims with a “GHOPAID” indicator of 1 (which is a field on the MedPAR file that indicates a claim is not an FFS claim and is paid by a Group Health Organization).
- We examined the MedPAR file and removed pharmacy charges for anti-hemophilic blood factor (which are paid separately under the IPPS) with an indicator of “3” for blood clotting with a revenue code of “0636” from the covered charge field. We also removed organ acquisition charges from the covered charge field because organ acquisition is a pass-through payment not paid under the IPPS.
Our general methodology to inflate the charges computes the 1-year average annual rate-of-change in charges per case which is then applied twice to inflate the charges on the MedPAR claims by 2 years (for example, FY 2018 to FY 2020). Specifically, under the methodology we have used since FY 2014, we compare the average charge per case from the latest 12-month period of MedPAR claims data available at the time of the proposed rule and the final rule to the average charge per case for the 12 month period from the prior year. For example, for the FY 2019 IPPS/LTCH PPS proposed rule (83 FR 20581), we used the December 2017 update of MedPAR claims data to calculate the average charges per case for the periods of January through December for CYs 2016 and 2017. Because the publicly released MedPAR claims do not contain claims beyond the end of the Federal fiscal year, the data for the last quarter of CY 2017 were not included in the publicly available December 2017 release. As we have in prior rulemaking, we included in the FY 2019 proposed rule a table grouping the claims data used in the calculation by quarter, and also made available on the CMS website more detailed summary tables by provider with the monthly charges that were used to compute the charge inflation factor.
As summarized in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41718), we have continued to receive comments expressing concern with what commenters stated was a lack of transparency with respect to the charge inflation component of the fixed-loss threshold calculation. The commenters concluded that, in the absence of access to the data or more specific data and information about how CMS arrived at the totals used in the charge inflation calculation, their ability to comment or to review the calculation of the charge inflation factor was limited.
Another commenter stated that CMS has not made the necessary data available or any guidance that describes whether and how CMS edited such data to arrive at the total of quarterly charges and charges per case used to measure charge inflation. Consequently, the commenter stated that the table of quarterly charges provided in the proposed rule was not useful in assessing the accuracy of the charge inflation figure that CMS used in the proposed rule to calculate the outlier threshold.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41718), we noted that we responded to similar comments in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50375), the FY 2016 IPPS/LTCH PPS final rule (80 FR 49779 through 49780), the FY 2017 IPPS/LTCH PPS final rule (81 FR 57283), and the FY 2018 IPPS/LTCH PPS final rule (82 FR 38524). We also explained that we have not yet been able to restructure the files (such as ensuring that personal identification information is compliant with privacy regulations) for release with the publication of the proposed rule and the final rule, and we continue to be confronted with the dilemma of either using older data that commenters can access earlier or using the most up-to-date data which will be more accurate, but will not be available to the public until after publication of the proposed and final rules. We stated that we continue to prefer using the latest data available at the time of the development of the proposed and final rules to compute the charge inflation factor because we believe it leads to greater accuracy in the calculation of the fixed-loss cost outlier threshold. We also noted that commenters did not recommend using charge data from a different period to compute the charge inflation factor. However, we stated that, for the FY 2020 IPPS/LTCH PPS proposed rule, we were continuing to consider using data that commenters can access earlier.
For the FY 2020 IPPS/LTCH PPS proposed rule, after further consideration, we stated that we believe balancing our preference to use the latest available data from the MedPAR files and stakeholders' concerns about being able to use publicly available MedPAR files to review the charge inflation factor can be achieved by modifying our methodology to use the publicly available Federal fiscal year period (that is, for FY 2020, we would use the charge data from Federal fiscal years 2017 and 2018), rather than the most recent data available to CMS. That is, for FY 2020, we proposed to use the charge data from Federal fiscal years 2017 and 2018 to calculate the 1-year average annual rate-of-change in charges per case for purposes of calculating both the proposed and final charge inflation factors, rather than the charge data from CYs 2017 and 2018 for purposes of calculating the proposed charge inflation factor and charge data from the periods April 1, 2017 through March 31, 2018 and April 1, 2018 through March 31, 2019 for purposes of calculating the final charge inflation factor as we would under our prior methodology. We stated that we believe there are benefits to using comparable Federal fiscal year periods rather than the most recent available data to calculate charge inflation, such as seasonality effects and the completeness of claims (that is, run-out). Specifically, under the methodology used for FYs 2014 through 2019, there is no run-out time between some of the claims and the MedPAR release. We stated that for example, under our current methodology, the most recent data available for purposes of the proposed rule was the December 2018 MedPAR release, with the final month of charge data being December 2018, and for this FY 2020 IPPS/LTCH PPS final rule, the most recent data available would be the March 2019 MedPAR release, with the final month of charge data being March 2019. With no run-out time between the end of the claims data period and the MedPAR release, some claims are not included from the last month of the applicable MedPAR release due to factors such as when the claim is submitted and claims processing time. In comparison, there is a 3-month run-out between the end of Federal fiscal year 2018 (September 30, 2018) and the December 2018 MedPAR release (cut-off as of December 31, 2018) for the proposed rule and a 6-month run-out between the end of Federal fiscal year 2018 (September 30, 2018) and the March 2019 MedPAR release (cut off as of March 31, 2019) for the final rule, which allows for more completeness in those FY 2018 claims. In addition to the completeness of the data, we stated that we believe this would also address commenters' concerns regarding transparency with respect to the data used to calculate the charge inflation factor. Adopting a methodology that uses charge data based on Federal fiscal years would allow for the MedPAR data to be readily available after publication of the proposed and final rules.
After further consideration of the issue and for the reasons discussed above, we proposed to use the publicly available MedPAR files for the two most recent Federal fiscal year time periods to calculate the charge inflation factor beginning in FY 2020. Specifically, for the proposed rule, we used the December 2017 MedPAR file of FY 2017 (October 1, 2016 through September 30, 2017) charge data (released in conjunction with the FY 2019 IPPS/LTCH PPS proposed rule) and the December 2018 MedPAR file of FY 2018 (October 1, 2017 through September 30, 2018) charge data (released in conjunction with the FY 2020 IPPS/LTCH PPS proposed rule) to compute the proposed charge inflation factor. In addition, we proposed that, for the FY 2020 final rule, we would use the most recent available data; that is, the MedPAR files from March 2018 for the FY 2017 charge data and the MedPAR files from March 2019 for the FY 2018 charge data. Because these data are publicly available at the time of the issuance of the proposed and final rules, we proposed that, beginning with the FY 2020 final rule, we would no longer provide the table of quarterly charges that we have included in prior rulemaking, if this proposed change to our methodology is finalized. (We note that in the proposed rule we provided a table for comparison purposes and refer the reader to the FY 2020 IPPS/LTCH proposed rule to view the table (84 FR 19597.) We invited public comments on this proposed change to our methodology to use in the proposed rule the December 2017 and December 2018 MedPAR releases for the respective FY 2017 and FY 2018 October to September applicable periods rather than the respective CY 2017 and CY 2018 January to December applicable periods for purposes of calculating the proposed charge inflation factor for the FY 2020 outlier threshold calculation.
For FY 2020, in the proposed rule, under this proposed methodology, to compute the 1-year average annual rate-of-change in charges per case, we compared the average covered charge per case of $58,355.91 ($562,621,348,420/9,641,206) from October 1, 2016 through September 31, 2017, to the average covered charge per case of $61,533.91 ($583,577,793,654/9,483,841) from October 1, 2017 through September 31, 2018. This rate-of-change was 5.4 percent (1.05446) or 11.2 percent (1.11189) over 2 years. The billed charges are obtained from the claims from the MedPAR file and inflated by the inflation factor specified above.
Comment: Some commenters were concerned with what they stated was a lack of transparency with respect to the charge inflation component of the fixed-loss threshold calculation. One commenter stated that they were unable to match the figures in the table from the proposed rule with publicly available data sources and CMS did not disclose the source of the data. The commenter's estimate was 5.38%, in comparison to the proposed rule's estimate of 5.45%. The commenter further stated that CMS has not made the necessary data available, or any guidance that describes whether and how CMS edited such data to arrive at the total of quarterly charges and charges per case used to measure charge inflation. Consequently, the commenter stated that the table provided in the proposed rule was not useful in assessing the accuracy of the charge inflation figure that CMS used in the proposed rule to calculate the outlier threshold.
Commenters supported the decision to move to publically available data for the proposed rule, however they believed that the final rule should use more current data and that CMS should disclose all aspects of its edits to the most current data. Commenters also requested that CMS should commit to disclose the charge inflation data files used in the final rule, including edits and calculations, when it publishes the final rule.
Response: We appreciate the commenter's input on the proposed methodology. As discussed in the FY 2020 proposed rule, under our proposed methodology, for this FY 2020 final rule, we proposed to use the MedPAR files from March 2019 for the FY 2018 charge data. These data are publically available, including for use by commenters that wish to reproduce charge inflation results. As discussed in the proposed rule, we provided the table of quarterly charges in the proposed rule for comparison with the methodology we used for FYs 2014 through FY 2019, but for FY 2020, under our proposed methodology, we calculated the 1-year average annual rate-of-change in charges per case using the publicly available MedPAR data. The edits and calculation were described in the proposed rule (84 FR 19595) and are also discussed in this final rule. Since the MedPAR files are publically available, we do not believe it is necessary to publish a separate PUF of the monthly charge data, which was done in the proposed rule and previous rules under our prior methodology for calculating charge inflation. In response to the commenter who believes more current data should be used in the final rule, we note that the FY 2018 claims used in this final rule are updated through March 2019, which we consider more current data than the proposed rule. In addition, as discussed in the proposed rule and in this final rule, since the MedPAR files are publically available, we believe this provides additional transparency.
After consideration of the comments received and for the reasons discussed in the proposed rule and this final rule, we are finalizing as proposed the methodology to calculate charge inflation using the publically available FY 2017 and FY 2018 claims data. Below we provide the charge inflation information based on the finalized methodology.
As we have done in the past, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to establish the FY 2020 outlier threshold using hospital CCRs from the December 2018 update to the Provider-Specific File (PSF)—the most recent available data at the time of the development of the proposed rule. We proposed to apply the following edits to providers' CCRs in the PSF. We believe these edits are appropriate in order to accurately model the outlier threshold. We first search for Indian Health Service providers and those providers assigned the statewide average CCR from the current fiscal year. We then replace these CCRs with the statewide average CCR for the upcoming fiscal year. We also assign the statewide average CCR (for the upcoming fiscal year) to those providers that have no value in the CCR field in the PSF or whose CCRs exceed the ceilings described later in this section (3.0 standard deviations from the mean of the log distribution of CCRs for all hospitals). We do not apply the adjustment factors described below to hospitals assigned the statewide average CCR. For FY 2020, we also proposed to continue to apply an adjustment factor to the CCRs to account for cost and charge inflation (as explained below). We also proposed that, if more recent data become available, we would use that data to calculate the final FY 2020 outlier threshold.
In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50979), we adopted a new methodology to adjust the CCRs. Specifically, we finalized a policy to compare the national average case-weighted operating and capital CCR from the most recent update of the PSF to the national average case-weighted operating and capital CCR from the same period of the prior year.
Therefore, as we have done since FY 2014, we proposed to adjust the CCRs from the December 2018 update of the PSF by comparing the percentage change in the national average case-weighted operating CCR and capital CCR from the December 2017 update of the PSF to the national average case-weighted operating CCR and capital CCR from the December 2018 update of the PSF. We note that, in the proposed rule, we used total transfer-adjusted cases from FY 2018 to determine the national average case-weighted CCRs for both sides of the comparison. As stated in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50979), we believe that it is appropriate to use the same case count on both sides of the comparison because this will produce the true percentage change in the average case-weighted operating and capital CCR from one year to the next without any effect from a change in case count on different sides of the comparison.
Using the proposed methodology above, for the proposed rule, we calculated a proposed December 2017 operating national average case-weighted CCR of 0.263267 and a proposed December 2018 operating national average case-weighted CCR of 0.256730. We then calculated the percentage change between the two national operating case-weighted CCRs by subtracting the proposed December 2017 operating national average case-weighted CCR from the proposed December 2018 operating national average case-weighted CCR and then dividing the result by the proposed December 2017 national operating average case-weighted CCR. This resulted in a proposed national operating CCR adjustment factor of 0.975167.
We used the same methodology proposed above to adjust the capital CCRs. Specifically, we calculated a proposed December 2017 capital national average case-weighted CCR of 0.022094 and a proposed December 2018 capital national average case-weighted CCR of 0.021121. We then calculated the percentage change between the two national capital case-weighted CCRs by subtracting the proposed December 2017 capital national average case-weighted CCR from the proposed December 2018 capital national average case-weighted CCR and then dividing the result by the proposed December 2017 capital national average case-weighted CCR. This resulted in a proposed national capital CCR adjustment factor of 0.955983.
For purposes of estimating the proposed outlier threshold for FY 2020, we used a wage index based on the proposed FY 2020 wage index that hospitals would be paid. This included our proposal to remove urban to rural reclassifications from the calculation of the rural floor, the frontier State floor adjustment in accordance with section 10324(a) of the Affordable Care Act, and the out-migration adjustment as added by section 505 of Public Law 108-173, and incorporated our FY 2020 wage index proposals to: (1) Increase the wage index values for hospitals with a wage index value below the 25th percentile wage index value across all hospitals and offset the estimated increase in IPPS payments to hospitals with wage index values below the 25th percentile by decreasing the wage index values for hospitals with a wage index value above the 75th percentile wage index value across all hospitals; and (2) apply a 5-percent cap for FY 2020 on any decrease in a hospital's final wage index from the hospital's final wage index in FY 2019. We stated that if we did not take the above into account, our estimate of total FY 2020 payments would be too low, and, as a result, our proposed outlier threshold would be too high, such that estimated outlier payments would be less than our projected 5.13 percent of total payments (which reflected the estimate of outlier reconciliation as calculated for the proposed rule).
As described in sections IV.G. and IV.H. of the Addendum, respectively, of the preamble of this final rule, sections 1886(q) and 1886(o) of the Act establish the Hospital Readmissions Reduction Program and the Hospital VBP Program, respectively. We do not believe that it is appropriate to include the proposed hospital VBP payment adjustments and the hospital readmissions payment adjustments in the proposed outlier threshold calculation or the proposed outlier offset to the standardized amount. Specifically, consistent with our definition of the base operating DRG payment amount for the Hospital Readmissions Reduction Program under § 412.152 and the Hospital VBP Program under § 412.160, outlier payments under section 1886(d)(5)(A) of the Act are not affected by these payment adjustments. Therefore, outlier payments would continue to be calculated based on the unadjusted base DRG payment amount (as opposed to using the base-operating DRG payment amount adjusted by the hospital readmissions payment adjustment and the hospital VBP payment adjustment). Consequently, we proposed to exclude the hospital VBP payment adjustments and the estimated hospital readmissions payment adjustments from the calculation of the proposed outlier fixed-loss cost threshold.
We note that, to the extent section 1886(r) of the Act modifies the DSH payment methodology under section 1886(d)(5)(F) of the Act, the uncompensated care payment under section 1886(r)(2) of the Act, like the empirically justified Medicare DSH payment under section 1886(r)(1) of the Act, may be considered an amount payable under section 1886(d)(5)(F) of the Act such that it would be reasonable to include the payment in the outlier determination under section 1886(d)(5)(A) of the Act. As we have done since the implementation of uncompensated care payments in FY 2014, for FY 2020, we proposed to allocate an estimated per-discharge uncompensated care payment amount to all cases for the hospitals eligible to receive the uncompensated care payment amount in the calculation of the outlier fixed-loss cost threshold methodology. We continue to believe that allocating an eligible hospital's estimated uncompensated care payment to all cases equally in the calculation of the outlier fixed-loss cost threshold would best approximate the amount we would pay in uncompensated care payments during the year because, when we make claim payments to a hospital eligible for such payments, we would be making estimated per-discharge uncompensated care payments to all cases equally. Furthermore, we continue to believe that using the estimated per-claim uncompensated care payment amount to determine outlier estimates provides predictability as to the amount of uncompensated care payments included in the calculation of outlier payments. Therefore, consistent with the methodology used since FY 2014 to calculate the outlier fixed-loss cost threshold, for FY 2020, we proposed to include estimated FY 2020 uncompensated care payments in the computation of the proposed outlier fixed-loss cost threshold. Specifically, we proposed to use the estimated per-discharge uncompensated care payments to hospitals eligible for the uncompensated care payment for all cases in the calculation of the proposed outlier fixed-loss cost threshold methodology.
Using this methodology, we used the formula described in section I.C.1. of the Addendum to the proposed and final rules to simulate and calculate the Federal payment rate and outlier payments for all claims. In addition, as described in the earlier section to this Addendum, we proposed to incorporate an estimate of FY 2020 outlier reconciliation in the methodology for determining the outlier threshold. Under this proposed approach, we determined a threshold of $26,994 and calculated total operating Federal payments of $90,721,309,065 and total outlier payments of $4,905,819,657. We then divided total outlier payments by total operating Federal payments plus total outlier payments and determined that this threshold matched with the 5.13 percent target, which reflected our proposal to incorporate an estimate of outlier reconciliation in the determination of the outlier threshold (as discussed in more detail in the previous section of this Addendum). We noted that, if calculated without applying our proposed methodology for incorporating an estimate of outlier reconciliation in the determination of the outlier threshold, the proposed threshold would be $27,154. We proposed an outlier fixed-loss cost threshold for FY 2020 equal to the prospective payment rate for the MS-DRG, plus any IME, empirically justified Medicare DSH payments, estimated uncompensated care payment, and any add-on payments for new technology, plus $26,994.
Comment: Commenters expressed concerns with the increase of the outlier threshold from $25,769 in FY 2019 to $ 26,994 in the FY 2020 proposed rule. They asserted that the increase will reduce the number of Medicare inpatient cases that qualify for an outlier payment. The commenters recommended that CMS maintain the current threshold of $ 25,769. Another commenter recommended that CMS develop a reconciliation process model that indicates at its conclusion, should it be determined the outlier threshold was set too high resulting in fewer outlier payments, a funding mechanism to allow hospitals access to additional outlier payments.
Response: As noted above, section 1886(d)(5)(A)(iv) of the Act states that outlier payments may not be not less than 5 percent nor more than 6 percent of the total payments projected or estimated to be made based on DRG prospective payment rates for discharges in that year. We believe that maintaining the FY 2019 outlier fixed-loss cost threshold for FY 2020 would be inconsistent with the statute because we would be setting a threshold based on the prior fiscal year. Also, when we calculate the threshold, we use the updated data that is available at the time of the development of the proposed and final rule. As the outlier threshold is set based on a prospective estimate of future payments, we do not believe adjusting payments after the fact, whether because of reconciled amounts or otherwise, is appropriate.
Comment: Some commenters requested that CMS consider whether it is appropriate to include extreme cases when calculating the threshold. One commenter explained that high charge cases have a significant impact on the threshold. The commenter observed that the amount of cases with over $1.5 million in covered charges has increased significantly from FY 2011 (926 cases) to FY 2018 (2,606 cases). The commenter believed that the impact of these cases will cause the threshold to rise and recommended that CMS carefully consider what is causing the trend, whether the inclusion of these cases in the calculation of the threshold is appropriate, and whether a separate outlier mechanism should apply to these cases that more closely hews outlier payments to marginal costs.
Response: As we explained when responding to a similar comment in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38526), the methodology used to calculate the outlier threshold includes all claims in order to account for all different types of cases, including high charge cases, to ensure that CMS meets the 5.1 percent target. As the commenter pointed out, the volume of these cases continues to rise, making their impact on the threshold significant. We believe excluding these cases would artificially lower the threshold. We believe it is important to include all cases in the calculation of the threshold no matter how high or low the charges. Including these cases with high charges lends more accuracy to the threshold, as these cases have an impact on the threshold and continue to rise in volume. Therefore, we believe the inclusion of the high-cost outlier cases in the calculation of the outlier threshold is appropriate.
Comment: One commenter stated that it could not confirm from the data CMS provided for the proposed outlier threshold whether CMS modeled and included the new technology payments that would apply in FY 2019 and in FY 2020, when it included claims for the MS-DRG that would include CAR-T payments. The commenter stated that if the claims used in the calculation predated FY 2019, and they do in fact relate to FY 2018, they would not have included such payments and that would otherwise significantly reduce or eliminate outlier payments for these cases. The commenter concluded that as a general matter, new technology add-on payments should be modeled and included in the outlier threshold calculation for claims that pre-date the first fiscal year in which the payments are available. Another commenter requested that CMS examine the reasons for the continuing rise in the outlier threshold and whether there are any interventions it can take to ensure that outlier payments remain equitable and continue to protect hospitals from high cost cases where Medicare's IPPS payments are insufficient to adequately compensate the hospital.
Response: We appreciate the input from the commenters. We did not include new technology add-on payments in the calculation of the FY 2020 outlier threshold. We welcome comments from the public how to incorporate new technology add-on payments into the outlier calculation. Because the commenters did not provide specifics how to incorporate these payments into the threshold, we will consider these comments for future rulemaking. Additionally, we believe the comment with regard to protecting hospitals from high cost cases is referring to new technology add on payments and cases such as CAR T-cell therapy. We refer the reader to section II.F.2.c. of the preamble of this final rule for comments regarding CAR T-cell therapy. With regard to including new technology add-on payments in the calculation of the outlier threshold, as stated above, we will consider this for future rulemaking.
Comment: A commenter noted that, for a given year, typically the final outlier threshold established by CMS in the final rule is lower than the threshold set forth in the proposed rule. The commenter emphasized that CMS should use the most recent data available when the Agency calculates the outlier threshold.
Response: We responded to similar comments in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50378 through 50379) and refer readers to that rule for our response.
After consideration of the public comments we received, we are using the same methodology we proposed to calculate the final outlier threshold. As discussed above, we are adopting for this final rule to calculate charge inflation using the publically available FY 2017 and FY 2018 claims data and to incorporate a projection of outlier payment reconciliations for the FY 2020 outlier threshold calculation.
For the FY 2020 final outlier threshold, we used the used the March 2018 MedPAR file of FY 2017 (October 1, 2016 through September 30, 2017) charge data (released in conjunction with the FY 2019 IPPS/LTCH PPS final rule) and the March 2019 MedPAR file of FY 2018 (October 1, 2017 through September 30, 2018) charge data (released in conjunction with this FY 2020 IPPS/LTCH PPS final rule) to determine the charge inflation factor. To compute the 1-year average annual rate-of-change in charges per case, we compared the average covered charge per case of $58,422.22 ($565,500,080,304/9,679,538 cases) from October 1, 2016 through September 31, 2017, to the average covered charge per case of $61,579.19 ($586,179,656,482/9,519,120 cases) from October 1, 2017 through September 31, 2018. This rate-of-change was 5.4 percent (1.05404) or 11.1 percent (1.11100) over 2 years. The billed charges are obtained from the claims from the MedPAR file and inflated by the inflation factor specified above.
As we have done in the past, we are establishing the FY 2020 outlier threshold using hospital CCRs from the March 2019 update to the Provider-Specific File (PSF)— the most recent available data at the time of the development of the final rule. We applied the following edits to providers' CCRs in the PSF. We believe these edits are appropriate in order to accurately model the outlier threshold. We first search for Indian Health Service providers and those providers assigned the statewide average CCR from the current fiscal year. We then replaced these CCRs with the statewide average CCR for the upcoming fiscal year. We also assigned the statewide average CCR (for the upcoming fiscal year) to those providers that have no value in the CCR field in the PSF or whose CCRs exceed the ceilings described later in this section (3.0 standard deviations from the mean of the log distribution of CCRs for all hospitals). We did not apply the adjustment factors described below to hospitals assigned the statewide average CCR. For FY 2020, we also are continuing to apply an adjustment factor to the CCRs to account for cost and charge inflation (as explained below).
For this final rule, as we have done since FY 2014, we are adjusting the CCRs from the March 2019 update of the PSF by comparing the percentage change in the national average case-weighted operating CCR and capital CCR from the March 2018 update of the PSF to the national average case-weighted operating CCR and capital CCR from the March 2019 update of the PSF. We note that we used total transfer-adjusted cases from FY 2018 to determine the national average case weighted CCRs for both sides of the comparison. As stated in the FY 2014 IPPS/LTCH PPS final rule (78 FR 50979), we believe that it is appropriate to use the same case count on both sides of the comparison because this will produce the true percentage change in the average case-weighted operating and capital CCR from one year to the next without any effect from a change in case count on different sides of the comparison.
Using the methodology above, for this final rule, we calculated a March 2018 operating national average case-weighted CCR of 0.260798 and a March 2019 operating national average case-weighted CCR of 0.254578. We then calculated the percentage change between the two national operating case-weighted CCRs by subtracting the March 2018 operating national average case-weighted CCR from the March 2019 operating national average case-weighted CCR and then dividing the result by the March 2018 national operating average case-weighted CCR. This resulted in a national operating CCR adjustment factor of 0.976150.
We used the same methodology above to adjust the capital CCRs. Specifically, for this final rule, we calculated a March 2018 capital national average case-weighted CCR of 0.021618 and a March 2019 capital national average case-weighted CCR of 0.020794. We then calculated the percentage change between the two national capital case weighted CCRs by subtracting the March 2018 capital national average case-weighted CCR from the March 2019 capital national average case-weighted CCR and then dividing the result by the March 2018 capital national average case-weighted CCR. This resulted in a national capital CCR adjustment factor of 0.961884.
As discussed previously, similar to the proposed rule, for FY 2020, we applied the following policies (as discussed in more detail earlier):
- We used a wage index based on the FY 2020 wage index that hospitals would be paid. This included our final policy to remove urban to rural reclassifications from the calculation of the rural floor, the frontier State floor adjustment in accordance with section 10324(a) of the Affordable Care Act, and the out migration adjustment as added by section 505 of Public Law 108-173, and incorporates our final FY 2020 wage index policies to (1) increase the wage index values for hospitals with a wage index value below the 25th percentile wage index value across all hospitals, and (2) apply a 5 percent cap for FY 2020 on any decrease in a hospital's final wage index from the hospital's final wage index in FY 2019. (We note that, as discussed in section III.N. of the preamble of this final rule, we are not finalizing our proposal to decrease the wage index for hospitals with wage index values above the 75th percentile wage index value). As stated above, if we did not take the above into account, our estimate of total FY 2020 payments would be too low, and, as a result, our outlier threshold would be too high, such that estimated outlier payments would be less than our projected 5.14 percent of total payments (which reflects the estimate of outlier reconciliation calculated for this final rule).
- We excluded the hospital VBP payment adjustments and the hospital readmissions payment adjustments from the calculation of the outlier fixed-loss cost threshold.
- We used the estimated per-discharge uncompensated care payments to hospitals eligible for the uncompensated care payment for all cases in the calculation of the outlier fixed-loss cost threshold methodology.
Using this methodology, we used the formula described in section I.C.1. of this Addendum to simulate and calculate the Federal payment rate and outlier payments for all claims. In addition, as described in the earlier section to this Addendum, we are finalizing to incorporate an estimate of FY 2020 outlier reconciliation in the methodology for determining the outlier threshold. Under this approach, we determined a threshold of $26,473 and calculated total operating Federal payments of $ 91,413,886,336 and total outlier payments of $4,943,282,951. We then divided total outlier payments by total operating Federal payments plus total outlier payments and determined that this threshold matched with the 5.14 percent target, which reflects our finalized methodology to incorporate an estimate of outlier reconciliation in the determination of the outlier threshold (as discussed in more detail in the previous section of this Addendum). We note that, if calculated without applying our finalized methodology for incorporating an estimate of outlier reconciliation in the determination of the outlier threshold, the threshold would have been $26,662. We are finalizing an outlier fixed-loss cost threshold for FY 2020 equal to the prospective payment rate for the MS-DRG, plus any IME, empirically justified Medicare DSH payments, estimated uncompensated care payment, and any add-on payments for new technology, plus $26,473.
(2) Other Changes Concerning Outliers
As stated in the FY 1994 IPPS final rule (58 FR 46348), we establish an outlier threshold that is applicable to both hospital inpatient operating costs and hospital inpatient capital-related costs. When we modeled the combined operating and capital outlier payments, we found that using a common threshold resulted in a lower percentage of outlier payments for capital-related costs than for operating costs. We project that the threshold for FY 2020 of $26,473 (which reflects our methodology to incorporate an estimate of outlier reconciliations) will result in outlier payments that will equal 5.1 percent of operating DRG payments and 5.42 percent of capital payments based on the Federal rate.
In accordance with section 1886(d)(3)(B) of the Act and as discussed above, we reduced the FY 2020 standardized amount by 5.1 percent to account for the projected proportion of payments paid as outliers.
The outlier adjustment factors applied to the operating standardized amount and capital Federal rate based on the FY 2020 outlier threshold are as follows:

We are applying the outlier adjustment factors to the FY 2020 payment rates after removing the effects of the FY 2019 outlier adjustment factors on the standardized amount.
To determine whether a case qualifies for outlier payments, we currently apply hospital-specific CCRs to the total covered charges for the case. Estimated operating and capital costs for the case are calculated separately by applying separate operating and capital CCRs. These costs are then combined and compared with the outlier fixed-loss cost threshold.
Under our current policy at § 412.84, we calculate operating and capital CCR ceilings and assign a statewide average CCR for hospitals whose CCRs exceed 3.0 standard deviations from the mean of the log distribution of CCRs for all hospitals. Based on this calculation, for hospitals for which the MAC computes operating CCRs greater than 1.155 or capital CCRs greater than 0.144, or hospitals for which the MAC is unable to calculate a CCR (as described under § 412.84(i)(3) of our regulations), statewide average CCRs are used to determine whether a hospital qualifies for outlier payments. Table 8A listed in section VI. of this Addendum (and available only via the internet on the CMS website) contains the statewide average operating CCRs for urban hospitals and for rural hospitals for which the MAC is unable to compute a hospital-specific CCR within the above range. These statewide average ratios are effective for discharges occurring on or after October 1, 2019 and replace the statewide average ratios from the prior fiscal year. Table 8B listed in section VI. of this Addendum (and available via the internet on the CMS website) contains the comparable statewide average capital CCRs. As previously stated, the CCRs in Tables 8A and 8B will be used during FY 2020 when hospital-specific CCRs based on the latest settled cost report either are not available or are outside the range noted above. Table 8C listed in section VI. of this Addendum (and available via the internet on the CMS website) contains the statewide average total CCRs used under the LTCH PPS as discussed in section V. of this Addendum.
We finally note that we published a manual update (Change Request 3966) to our outlier policy on October 12, 2005, which updated Chapter 3, Section 20.1.2 of the Medicare Claims Processing Manual. The manual update covered an array of topics, including CCRs, reconciliation, and the time value of money. We encourage hospitals that are assigned the statewide average operating and/or capital CCRs to work with their MAC on a possible alternative operating and/or capital CCR as explained in Change Request 3966. Use of an alternative CCR developed by the hospital in conjunction with the MAC can avoid possible overpayments or underpayments at cost report settlement, thereby ensuring better accuracy when making outlier payments and negating the need for outlier reconciliation. We also note that a hospital may request an alternative operating or capital CCR at any time as long as the guidelines of Change Request 3966 are followed. In addition, as mentioned above, we published an additional manual update (Change Request 7192) to our outlier policy on December 3, 2010, which also updated Chapter 3, Section 20.1.2 of the Medicare Claims Processing Manual. The manual update outlines the outlier reconciliation process for hospitals and Medicare contractors. To download and view the manual instructions on outlier reconciliation, we refer readers to the CMS website: http://www.cms.hhs.gov/manuals/downloads/clm104c03.pdf.
(3) FY 2018 Outlier Payments
Our current estimate, using available FY 2018 claims data, is that actual outlier payments for FY 2018 were approximately 4.98 percent of actual total MS-DRG payments. Therefore, the data indicate that, for FY 2018, the percentage of actual outlier payments relative to actual total payments is lower than we projected for FY 2018. Consistent with the policy and statutory interpretation we have maintained since the inception of the IPPS, we do not make retroactive adjustments to outlier payments to ensure that total outlier payments for FY 2018 are equal to 5.1 percent of total MS-DRG payments. As explained in the FY 2003 Outlier Final Rule (68 FR 34502), if we were to make retroactive adjustments to all outlier payments to ensure total payments are 5.1 percent of MS-DRG payments (by retroactively adjusting outlier payments), we would be removing the important aspect of the prospective nature of the IPPS. Because such an across-the-board adjustment would either lead to more or less outlier payments for all hospitals, hospitals would no longer be able to reliably approximate their payment for a patient while the patient is still hospitalized. We believe it would be neither necessary nor appropriate to make such an aggregate retroactive adjustment. Furthermore, we believe it is consistent with the statutory language at section 1886(d)(5)(A)(iv) of the Act not to make retroactive adjustments to outlier payments. This section states that outlier payments be equal to or greater than 5 percent and less than or equal to 6 percent of projected or estimated (not actual) MS-DRG payments. We believe that an important goal of a PPS is predictability. Therefore, we believe that the fixed-loss outlier threshold should be projected based on the best available historical data and should not be adjusted retroactively. A retroactive change to the fixed-loss outlier threshold would affect all hospitals subject to the IPPS, thereby undercutting the predictability of the system as a whole.
We note that, because the MedPAR claims data for the entire FY 2019 will not be available until after September 30, 2019, we are unable to provide an estimate of actual outlier payments for FY 2019 based on FY 2019 claims data in this final rule. We will provide an estimate of actual FY 2019 outlier payments in the FY 2021 IPPS/LTCH PPS proposed rule.
Comment: A commenter noted that, in the proposed rule, CMS stated that actual outlier payments for FY 2018 were approximately 4.94 percent of total MS-DRG payments. The commenter performed its own analysis and concluded that outlier payments for FY 2018 are approximately 4.89 percent of total MS-DRG payments. The commenter was concerned that CMS' estimate was overstated.
Response: We reviewed our data to ensure the estimate provided is accurate. Therefore, we believe we have provided a reliable estimate of the outlier percentage for FY 2018. In addition, the commenter did not provide specifics as to why CMS's estimate differed from the commenter's estimate. We welcome additional suggestions from the public, including the commenter, to improve the accuracy of our estimate of actual outlier payments.
5. FY 2020 Standardized Amount
The adjusted standardized amount is divided into labor-related and nonlabor-related portions. Tables 1A and 1B listed and published in section VI. of this Addendum (and available via the internet on the CMS website) contain the national standardized amounts that we are applying to all hospitals, except hospitals located in Puerto Rico, for FY 2020. The standardized amount for hospitals in Puerto Rico is shown in Table 1C listed and published in section VI. of this Addendum (and available via the internet on the CMS website). The amounts shown in Tables 1A and 1B differ only in that the labor-related share applied to the standardized amounts in Table 1A is 68.3 percent, and the labor-related share applied to the standardized amounts in Table 1B is 62 percent. In accordance with sections 1886(d)(3)(E) and 1886(d)(9)(C)(iv) of the Act, we are applying a labor-related share of 62 percent, unless application of that percentage would result in lower payments to a hospital than would otherwise be made. In effect, the statutory provision means that we will apply a labor-related share of 62 percent for all hospitals whose wage indexes are less than or equal to 1.0000.
In addition, Tables 1A and 1B include the standardized amounts reflecting the applicable percentage increases for FY 2020.
The labor-related and nonlabor-related portions of the national average standardized amounts for Puerto Rico hospitals for FY 2020 are set forth in Table 1C listed and published in section VI. of this Addendum (and available via the internet on the CMS website). Similar to above, section 1886(d)(9)(C)(iv) of the Act, as amended by section 403(b) of Pub. L. 108-173, provides that the labor-related share for hospitals located in Puerto Rico be 62 percent, unless the application of that percentage would result in lower payments to the hospital.
The following table illustrates the changes from the FY 2019 national standardized amounts to the FY 2020 national standardized amounts. The second through fifth columns display the changes from the FY 2019 standardized amounts for each applicable FY 2020 standardized amount. The first row of the table shows the updated (through FY 2019) average standardized amount after restoring the FY 2019 offsets for outlier payments and the geographic reclassification budget neutrality. The MS-DRG reclassification and recalibration and wage index budget neutrality adjustment factors are cumulative. Therefore, those FY 2019 adjustment factors are not removed from this table. Additionally, for FY 2020, we have applied the budget neutrality factor for the finalized policy for lowest quartile wage index hospitals and transition, described above.



B. Adjustments for Area Wage Levels and Cost-of-Living
Tables 1A through 1C, as published in section VI. of this Addendum (and available via the internet on the CMS website), contain the labor-related and nonlabor-related shares that we used to calculate the prospective payment rates for hospitals located in the 50 States, the District of Columbia, and Puerto Rico for FY 2020. This section addresses two types of adjustments to the standardized amounts that are made in determining the prospective payment rates as described in this Addendum.
1. Adjustment for Area Wage Levels
Sections 1886(d)(3)(E) and 1886(d)(9)(C)(iv) of the Act require that we make an adjustment to the labor-related portion of the national prospective payment rate to account for area differences in hospital wage levels. This adjustment is made by multiplying the labor-related portion of the adjusted standardized amounts by the appropriate wage index for the area in which the hospital is located. For FY 2020, as discussed in section IV.B.3. of the preamble of this final rule, as we proposed, we are applying a labor-related share of 68.3 percent for the national standardized amounts for all IPPS hospitals (including hospitals in Puerto Rico) that have a wage index value that is greater than 1.0000. Consistent with section 1886(d)(3)(E) of the Act, as we proposed, we are applying the wage index to a labor-related share of 62 percent of the national standardized amount for all IPPS hospitals (including hospitals in Puerto Rico) whose wage index values are less than or equal to 1.0000. In section III. of the preamble of this final rule, we discuss the data and methodology for the FY 2020 wage index.
2. Adjustment for Cost-of-Living in Alaska and Hawaii
Section 1886(d)(5)(H) of the Act provides discretionary authority to the Secretary to make adjustments as the Secretary deems appropriate to take into account the unique circumstances of hospitals located in Alaska and Hawaii. Higher labor-related costs for these two States are taken into account in the adjustment for area wages described above. To account for higher nonlabor-related costs for these two States, we multiply the nonlabor-related portion of the standardized amount for hospitals located in Alaska and Hawaii by an adjustment factor.
In the FY 2013 IPPS/LTCH PPS final rule, we established a methodology to update the COLA factors for Alaska and Hawaii that were published by the U.S. Office of Personnel Management (OPM) every 4 years (at the same time as the update to the labor-related share of the IPPS market basket), beginning in FY 2014. We refer readers to the FY 2013 IPPS/LTCH PPS proposed and final rules for additional background and a detailed description of this methodology (77 FR 28145 through 28146 and 77 FR 53700 through 53701, respectively).
For FY 2018, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38530 through 38531), we updated the COLA factors published by OPM for 2009 (as these are the last COLA factors OPM published prior to transitioning from COLAs to locality pay) using the methodology that we finalized in the FY 2013 IPPS/LTCH PPS final rule.
Based on the policy finalized in the FY 2013 IPPS/LTCH PPS final rule, as we proposed, we are continuing to use the same COLA factors in FY 2020 that were used in FY 2019 to adjust the nonlabor-related portion of the standardized amount for hospitals located in Alaska and Hawaii. Below is a table listing the COLA factors for FY 2020.

Based on the policy finalized in the FY 2013 IPPS/LTCH PPS final rule, the next update to the COLA factors for Alaska and Hawaii would occur at the same time as the update to the labor-related share of the IPPS market basket (no later than FY 2022).
C. Calculation of the Prospective Payment Rates
1. General Formula for Calculation of the Prospective Payment Rates for FY 2020
In general, the operating prospective payment rate for all hospitals (including hospitals in Puerto Rico) paid under the IPPS, except SCHs and MDHs, for FY 2020 equals the Federal rate (which includes uncompensated care payments).
Under current law, the MDH program has been extended for discharges through September 30, 2022.
SCHs are paid based on whichever of the following rates yields the greatest aggregate payment: The Federal national rate (which, as discussed in section IV.F. of the preamble of this final rule, includes uncompensated care payments); the updated hospital-specific rate based on FY 1982 costs per discharge; the updated hospital-specific rate based on FY 1987 costs per discharge; the updated hospital-specific rate based on FY 1996 costs per discharge; or the updated hospital-specific rate based on FY 2006 costs per discharge to determine the rate that yields the greatest aggregate payment.
The prospective payment rate for SCHs for FY 2020 equals the higher of the applicable Federal rate, or the hospital-specific rate as described below. The prospective payment rate for MDHs for FY 2020 equals the higher of the Federal rate, or the Federal rate plus 75 percent of the difference between the Federal rate and the hospital-specific rate as described below. For MDHs, the updated hospital-specific rate is based on FY 1982, FY 1987, or FY 2002 costs per discharge, whichever yields the greatest aggregate payment.
2. Operating and Capital Federal Payment Rate and Outlier Payment Calculation
Note:
The formula below is used for actual claim payment and is also used by CMS to project the outlier threshold for the upcoming fiscal year. The difference is the source of some of the variables in the formula. For example, operating and capital CCRs for actual claim payment are from the PSF while CMS uses an adjusted CCR (as described above) to project the threshold for the upcoming fiscal year. In addition, charges for a claim payment are from the bill, while charges to project the threshold are from the MedPAR data with an inflation factor applied to the charges (as described earlier).
Step 1—Determine the MS-DRG and MS-DRG relative weight for each claim based on the ICD-10-CM procedure and diagnosis codes on the claim.
Step 2—Select the applicable average standardized amount depending on whether the hospital submitted qualifying quality data and is a meaningful EHR user, as described above.
Step 3—Compute the operating and capital Federal payment rate:
- Federal Payment Rate for Operating Costs = MS-DRG Relative Weight × [(Labor-Related Applicable Standardized Amount × Applicable CBSA Wage Index) + (Nonlabor-Related Applicable Standardized Amount × Cost-of-Living Adjustment)] × (1 + IME + (DSH * 0.25))
- Federal Payment for Capital Costs = MS-DRG Relative Weight × Federal Capital Rate × Geographic Adjustment Fact × (l + IME + DSH)
Step 4—Determine operating and capital costs:
- Operating Costs = (Billed Charges × Operating CCR)
- Capital Costs = (Billed Charges × Capital CCR).
Step 5—Compute operating and capital outlier threshold (CMS applies a geographic adjustment to the operating and capital outlier threshold to account for local cost variation):
- Operating CCR to Total CCR = (Operating CCR)/(Operating CCR + Capital CCR)
- Operating Outlier Threshold = [Fixed Loss Threshold × ((Labor-Related Portion × CBSA Wage Index) + Nonlabor-Related portion)] × Operating CCR to Total CCR + Federal Payment with IME, DSH + Uncompensated Care Payment + New Technology Add-On Payment Amount
- Capital CCR to Total CCR = (Capital CCR)/(Operating CCR + Capital CCR)
- Capital Outlier Threshold = (Fixed Loss Threshold × Geographic Adjustment Factor × Capital CCR to Total CCR) + Federal Payment with IME and DSH
Step 6—Compute operating and capital outlier payments:
- Marginal Cost Factor = 0.80 or 0.90 (depending on the MS-DRG)
- Operating Outlier Payment = (Operating Costs − Operating Outlier Threshold) × Marginal Cost Factor
- Capital Outlier Payment = (Capital Costs − Capital Outlier Threshold) × Marginal Cost Factor
The payment rate may then be further adjusted for hospitals that qualify for a low-volume payment adjustment under section 1886(d)(12) of the Act and 42 CFR 412.101(b). The base-operating DRG payment amount may be further adjusted by the hospital readmissions payment adjustment and the hospital VBP payment adjustment as described under sections 1886(q) and 1886(o) of the Act, respectively. Payments also may be reduced by the 1-percent adjustment under the HAC Reduction Program as described in section 1886(p) of the Act. We also make new technology add-on payments in accordance with section 1886(d)(5)(K) and (L) of the Act. Finally, we add the uncompensated care payment to the total claim payment amount. As noted in the formula above, we take uncompensated care payments and new technology add-on payments into consideration when calculating outlier payments.
2. Hospital-Specific Rate (Applicable Only to SCHs and MDHs)
a. Calculation of Hospital-Specific Rate
Section 1886(b)(3)(C) of the Act provides that SCHs are paid based on whichever of the following rates yields the greatest aggregate payment: The Federal rate; the updated hospital-specific rate based on FY 1982 costs per discharge; the updated hospital-specific rate based on FY 1987 costs per discharge; the updated hospital-specific rate based on FY 1996 costs per discharge; or the updated hospital-specific rate based on FY 2006 costs per discharge to determine the rate that yields the greatest aggregate payment.
As noted previously, the MDH program has been extended under current law for discharges occurring through September 30, 2022. For MDHs, the updated hospital-specific rate is based on FY 1982, FY 1987, or FY 2002 costs per discharge, whichever yields the greatest aggregate payment.
For a more detailed discussion of the calculation of the hospital-specific rates, we refer readers to the FY 1984 IPPS interim final rule (48 FR 39772); the April 20, 1990 final rule with comment period (55 FR 15150); the FY 1991 IPPS final rule (55 FR 35994); and the FY 2001 IPPS final rule (65 FR 47082).
b. Updating the FY 1982, FY 1987, FY 1996, FY 2002 and FY 2006 Hospital-Specific Rate for FY 2020
Section 1886(b)(3)(B)(iv) of the Act provides that the applicable percentage increase applicable to the hospital-specific rates for SCHs and MDHs equals the applicable percentage increase set forth in section 1886(b)(3)(B)(i) of the Act (that is, the same update factor as for all other hospitals subject to the IPPS). Because the Act sets the update factor for SCHs and MDHs equal to the update factor for all other IPPS hospitals, the update to the hospital-specific rates for SCHs and MDHs is subject to the amendments to section 1886(b)(3)(B) of the Act made by sections 3401(a) and 10319(a) of the Affordable Care Act. Accordingly, the applicable percentage increases to the hospital-specific rates applicable to SCHs and MDHs are the following:

For a complete discussion of the applicable percentage increase applied to the hospital-specific rates for SCHs and MDHs, we refer readers to section IV.B. of the preamble of this final rule.
In addition, because SCHs and MDHs use the same MS-DRGs as other hospitals when they are paid based in whole or in part on the hospital-specific rate, the hospital-specific rate is adjusted by a budget neutrality factor to ensure that changes to the MS-DRG classifications and the recalibration of the MS-DRG relative weights are made in a manner so that aggregate IPPS payments are unaffected. Therefore, the hospital-specific rate for an SCH or an MDH is adjusted by the MS-DRG reclassification and recalibration budget neutrality factor of 0.997649, as discussed in section III. of this Addendum. The resulting rate is used in determining the payment rate that an SCH or MDH would receive for its discharges beginning on or after October 1, 2019. We note that, in this final rule, for FY 2020, we are not making a documentation and coding adjustment to the hospital-specific rate. We refer readers to section II.D. of the preamble of this final rule for a complete discussion regarding our policies and previously finalized policies (including our historical adjustments to the payment rates) relating to the effect of changes in documentation and coding that do not reflect real changes in case-mix.
III. Changes to Payment Rates for Acute Care Hospital Inpatient Capital-Related Costs for FY 2020
The PPS for acute care hospital inpatient capital-related costs was implemented for cost reporting periods beginning on or after October 1, 1991. The basic methodology for determining Federal capital prospective rates is set forth in the regulations at 42 CFR 412.308 through 412.352. Below we discuss the factors that we used to determine the capital Federal rate for FY 2020, which are effective for discharges, occurring on or after October 1, 2019.
All hospitals (except “new” hospitals under § 412.304(c)(2)) are paid based on the capital Federal rate. We annually update the capital standard Federal rate, as provided in § 412.308(c)(1), to account for capital input price increases and other factors. The regulations at § 412.308(c)(2) also provide that the capital Federal rate be adjusted annually by a factor equal to the estimated proportion of outlier payments under the capital Federal rate to total capital payments under the capital Federal rate. In addition, § 412.308(c)(3) requires that the capital Federal rate be reduced by an adjustment factor equal to the estimated proportion of payments for exceptions under § 412.348. (We note that, as discussed in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53705), there is generally no longer a need for an exceptions payment adjustment factor.) However, in limited circumstances, an additional payment exception for extraordinary circumstances is provided for under § 412.348(f) for qualifying hospitals. Therefore, in accordance with § 412.308(c)(3), an exceptions payment adjustment factor may need to be applied if such payments are made. Section 412.308(c)(4)(ii) requires that the capital standard Federal rate be adjusted so that the effects of the annual DRG reclassification and the recalibration of DRG weights and changes in the geographic adjustment factor (GAF) are budget neutral.
Section 412.374 provides for payments to hospitals located in Puerto Rico under the IPPS for acute care hospital inpatient capital-related costs, which currently specifies capital IPPS payments to hospitals located in Puerto Rico are based on 100 percent of the Federal rate.
A. Determination of the Federal Hospital Inpatient Capital-Related Prospective Payment Rate Update for FY 2020
In the discussion that follows, we explain the factors that we used to determine the capital Federal rate for FY 2020. In particular, we explain why the FY 2020 capital Federal rate increased approximately 0.70 percent, compared to the FY 2019 capital Federal rate. As discussed in the impact analysis in Appendix A to this FY 2020 IPPS/LTCH PPS final rule, we estimate that capital payments per discharge will increase approximately 1.4 percent during that same period. Because capital payments constitute approximately 10 percent of hospital payments, a 1-percent change in the capital Federal rate yields only approximately a 0.1 percent change in actual payments to hospitals.
1. Projected Capital Standard Federal Rate Update
Under § 412.308(c)(1), the capital standard Federal rate is updated on the basis of an analytical framework that takes into account changes in a capital input price index (CIPI) and several other policy adjustment factors. Specifically, we adjust the projected CIPI rate of change, as appropriate, each year for case-mix index-related changes, for intensity, and for errors in previous CIPI forecasts. The update factor for FY 2020 under that framework is 1.5 percent based on a projected 1.5 percent increase in the 2014-based CIPI, a 0.0 percentage point adjustment for intensity, a 0.0 percentage point adjustment for case-mix, a 0.0 percentage point adjustment for the DRG reclassification and recalibration, and a forecast error correction of 0.0 percentage point. As discussed in section III.C. of this Addendum, we continue to believe that the CIPI is the most appropriate input price index for capital costs to measure capital price changes in a given year. We also explain the basis for the FY 2020 CIPI projection in that same section of this Addendum. Below we describe the policy adjustments that we applied in the update framework for FY 2020.
The case-mix index is the measure of the average DRG weight for cases paid under the IPPS. Because the DRG weight determines the prospective payment for each case, any percentage increase in the case-mix index corresponds to an equal percentage increase in hospital payments.
The case-mix index can change for any of the following reasons:
- The average resource use of Medicare patient changes (“real” case-mix change).
- Changes in hospital documentation and coding of patient records result in higher-weighted DRG assignments (“coding effects”).
- The annual DRG reclassification and recalibration changes may not be budget neutral (“reclassification effect”).
We define real case-mix change as actual changes in the mix (and resource requirements) of Medicare patients, as opposed to changes in documentation and coding behavior that result in assignment of cases to higher-weighted DRGs, but do not reflect higher resource requirements. The capital update framework includes the same case-mix index adjustment used in the former operating IPPS update framework (as discussed in the May 18, 2004 IPPS proposed rule for FY 2005 (69 FR 28816)). (We no longer use an update framework to make a recommendation for updating the operating IPPS standardized amounts, as discussed in section II. of Appendix B to the FY 2006 IPPS final rule (70 FR 47707).)
For FY 2020, we project a 0.5 percent total increase in the case-mix index. We estimate that the real case-mix increase will equal 0.5 percent for FY 2020. The net adjustment for change in case-mix is the difference between the projected real increase in case-mix and the projected total increase in case-mix. Therefore, as we proposed, the net adjustment for case-mix change in FY 2020 is 0.0 percentage point.
The capital update framework also contains an adjustment for the effects of DRG reclassification and recalibration. This adjustment is intended to remove the effect on total payments of prior year's changes to the DRG classifications and relative weights, in order to retain budget neutrality for all case-mix index-related changes other than those due to patient severity of illness. Due to the lag time in the availability of data, there is a 2-year lag in data used to determine the adjustment for the effects of DRG reclassification and recalibration. For example, we have data available to evaluate the effects of the FY 2018 DRG reclassification and recalibration as part of our update for FY 2020. We assume, for purposes of this adjustment, that the estimate of FY 2018 DRG reclassification and recalibration will result in no change in the case-mix when compared with the case-mix index that would have resulted if we had not made the reclassification and recalibration changes to the DRGs. Therefore, as we proposed, we are making a 0.0 percentage point adjustment for reclassification and recalibration in the update framework for FY 2020.
The capital update framework also contains an adjustment for forecast error. The input price index forecast is based on historical trends and relationships ascertainable at the time the update factor is established for the upcoming year. In any given year, there may be unanticipated price fluctuations that may result in differences between the actual increase in prices and the forecast used in calculating the update factors. In setting a prospective payment rate under the framework, we make an adjustment for forecast error only if our estimate of the change in the capital input price index for any year is off by 0.25 percentage point or more. There is a 2-year lag between the forecast and the availability of data to develop a measurement of the forecast error. Historically, when a forecast error of the CIPI is greater than 0.25 percentage point in absolute terms, it is reflected in the update recommended under this framework. A forecast error of −0.1 percentage point was calculated for the FY 2018 update, for which there are historical data. That is, current historical data indicated that the forecasted FY 2018 CIPI (1.3 percent) used in calculating the FY 2018 update factor was 0.1 percentage point higher than actual realized price increases (1.2 percent). As this does not exceed the 0.25 percentage point threshold, as we proposed, we are not making an adjustment for forecast error in the update for FY 2020.
Under the capital IPPS update framework, we also make an adjustment for changes in intensity. Historically, we calculate this adjustment using the same methodology and data that were used in the past under the framework for operating IPPS. The intensity factor for the operating update framework reflects how hospital services are utilized to produce the final product, that is, the discharge. This component accounts for changes in the use of quality-enhancing services, for changes within DRG severity, and for expected modification of practice patterns to remove noncost-effective services. Our intensity measure is based on a 5-year average.
We calculate case-mix constant intensity as the change in total cost per discharge, adjusted for price level changes (the CPI for hospital and related services) and changes in real case-mix. Without reliable estimates of the proportions of the overall annual intensity changes that are due, respectively, to ineffective practice patterns and the combination of quality-enhancing new technologies and complexity within the DRG system, we assume that one-half of the annual change is due to each of these factors. The capital update framework thus provides an add-on to the input price index rate of increase of one-half of the estimated annual increase in intensity, to allow for increases within DRG severity and the adoption of quality-enhancing technology.
In this final rule, as we proposed, we are continuing to use a Medicare-specific intensity measure that is based on a 5-year adjusted average of cost per discharge for FY 2020 (we refer readers to the FY 2011 IPPS/LTCH PPS final rule (75 FR 50436) for a full description of our Medicare-specific intensity measure). Specifically, for FY 2020, we used an intensity measure that is based on an average of cost per discharge data from the 5-year period beginning with FY 2013 and extending through FY 2017. Based on these data, we estimated that case-mix constant intensity declined during FYs 2013 through 2017. In the past, when we found intensity to be declining, we believed a zero (rather than a negative) intensity adjustment was appropriate. Consistent with this approach, because we estimated that intensity would decline during that 5-year period, we believe it is appropriate to continue to apply a zero-intensity adjustment for FY 2020. Therefore, as we proposed, we made a 0.0 percentage point adjustment for intensity in the update for FY 2020.
Above we described the basis of the components we used to develop the 1.5 percent capital update factor under the capital update framework for FY 2020, as shown in the following table.

2. Outlier Payment Adjustment Factor
Section 412.312(c) establishes a unified outlier payment methodology for inpatient operating and inpatient capital-related costs. A shared threshold is used to identify outlier cases for both inpatient operating and inpatient capital-related payments. Section 412.308(c)(2) provides that the standard Federal rate for inpatient capital-related costs be reduced by an adjustment factor equal to the estimated proportion of capital-related outlier payments to total inpatient capital-related PPS payments. The outlier threshold is set so that operating outlier payments are projected to be 5.1 percent of total operating IPPS DRG payments. For FY 2020, as we proposed, we are incorporating the estimated outlier reconciliation payment amounts into the outlier threshold model. (For more details on our incorporation of the estimated outlier reconciliation payment amounts into the outlier threshold model, we refer readers to section II.A.4.h. of this Addendum.)
For FY 2019, we estimated that outlier payments for capital-related PPS payments would equal 5.06 percent of inpatient capital-related payments based on the capital Federal rate in FY 2019. In FY 2020, based on the threshold discussed in section II.A. of this Addendum, we estimate that prior to taking into account projected capital outlier reconciliation payments, outlier payments for capital-related costs would equal 5.47 percent for inpatient capital-related payments based on the capital Federal rate. However, as we proposed, using the methodology outlined in section II.A.4.h. of this Addendum, we estimate that taking into account projected capital outlier reconciliation payments will decrease FY 2020 aggregate estimated capital outlier payments by 0.08 percent. Therefore, accounting for estimated capital outlier reconciliation, estimated outlier payments for capital-related PPS payments equal 5.39 percent (5.47 percent −0.08 percent) of inpatient capital-related payments based on the capital Federal rate in FY 2020. Accordingly, we applied an outlier adjustment factor of 0.9461 in determining the capital Federal rate for FY 2020. Thus, we estimate that the percentage of capital outlier payments to total capital Federal rate payments for FY 2020 will be higher than the percentage for FY 2019.
The outlier reduction factors are not built permanently into the capital rates; that is, they are not applied cumulatively in determining the capital Federal rate. The FY 2020 outlier adjustment of 0.9461 is a −0.35 percent change from the FY 2019 outlier adjustment of 0.9494. Therefore, the net change in the outlier adjustment to the capital Federal rate for FY 2020 is 0.9965 (0.9461/0.9494; calculation performed on unrounded numbers) so that the outlier adjustment will decrease the FY 2020 capital Federal rate by approximately −0.35 percent compared to the FY 2019 outlier adjustment.
3. Budget Neutrality Adjustment Factor for Changes in DRG Classifications and Weights and the GAF
Section 412.308(c)(4)(ii) requires that the capital Federal rate be adjusted so that aggregate payments for the fiscal year based on the capital Federal rate, after any changes resulting from the annual DRG reclassification and recalibration and changes in the GAF, are projected to equal aggregate payments that would have been made on the basis of the capital Federal rate without such changes.
In section III.N. of the preamble of this final rule, we discuss our finalized policies to address wage index disparities between high and low wage index value hospitals. Specifically, we are: (1) Increasing the wage index for hospitals with a wage index value below the 25th percentile wage index, where the increase in the wage index value for these hospitals will be equal to half the difference between the otherwise applicable final wage index value for a year for that hospital and the 25th percentile wage index value for that year across all hospitals; (2) calculating the rural floor without including the wage data of urban hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented in § 412.103) and removing urban to rural reclassifications under § 412.103 from the calculation of “the wage index for rural areas in the State in which the county is located” in applying the provisions of section 1886(d)(8)(C)(iii) of the Act; and (3) placing a 5-percent cap in FY 2020 on any decrease in a hospital's wage index from the hospital's final wage index in FY 2019. These finalized policies directly affect the GAF because it is calculated based on the hospital wage index value that is applicable to the hospital under 42 CFR part 412, subpart D (Basic Methodology for Determining Prospective Payment Federal Rates for Inpatient Operating Costs). Given these changes will affect the GAFs, as we proposed, we augmented our historical methodology for computing the budget neutrality factor for changes in the GAFs. Historically, we determine a budget neutrality factor for changes in the GAF that accounts for changes resulting from the update to the wage data, wage index reclassifications and redesignations, and the rural floor in a single step. (We note that this historical GAF budget neutrality factor does not reflect changes in the frontier State adjustment or the out-migration adjustment because these statutory adjustments to the wage index are not budget neutral.)
In light of these changes to the wage index, which directly affect the GAF, as we proposed, we computed a budget neutrality factor for changes in the GAFs in two steps. Under our 2-step methodology, as we proposed, we first calculate a factor to ensure budget neutrality for changes to the FY 2020 GAFs due to the update to the wage data, wage index reclassifications and redesignations, including our removal of urban to rural reclassifications under § 412.103 from the calculation of “the wage index for rural areas in the State in which the county is located” in applying the provisions of section 1886(d)(8)(C)(iii) of the Act, and the rural floor, including our calculation of the rural floor without including the wage data of urban hospitals that have reclassified as rural under § 412.103, consistent with our historical GAF budget neutrality factor methodology. In the second step, as we proposed, we calculate a factor to ensure budget neutrality for the changes to the FY 2020 GAFs due to our increase in the wage index for hospitals with a wage index value below the 25th percentile wage index and placement of a 5-percent cap on any decrease in a hospital's wage index from the hospital's final wage index in FY 2019. In this section, we refer to these two policies as the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases. We discuss our 2-step calculation of the GAF budget neutrality factors below.
To determine the GAF budget neutrality factors for FY 2020, we first compared estimated aggregate capital Federal rate payments based on the FY 2019 MS-DRG classifications and relative weights and the FY 2019 GAFs to estimated aggregate capital Federal rate payments based on the FY 2019 MS-DRG classifications and relative weights and the FY 2020 GAFs without incorporating the effects on the GAFs of the lowest quartile hospital wage index adjustment, and the 5-percent cap on wage index decreases. To achieve budget neutrality for these changes in the GAFs, we calculated an incremental GAF budget neutrality adjustment factor of 1.0005 for FY 2020. Next, we compared estimated aggregate capital Federal rate payments based on the FY 2020 GAFs with and without incorporating the effects on the GAFs of the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases. For this calculation, estimated aggregate capital Federal rate payments were calculated using the FY 2020 MS-DRG classifications and relative weights, and the FY 2020 GAFs (both with and without incorporating the effects on the GAF of the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases). (We note that, for this calculation, the GAFs included the out-migration and frontier State adjustments.) To achieve budget neutrality for the effects of the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases on the FY 2020 GAFs, we calculated an incremental GAF budget neutrality adjustment factor of 0.9964. Therefore, to achieve budget neutrality for the changes in the GAFs, based on the calculations described above, we applied an incremental budget neutrality adjustment factor of 0.9968 (1.0005 × 0.9964; calculation performed on unrounded numbers) for FY 2020 to the previous cumulative FY 2019 adjustment factor.
We also compared estimated aggregate capital Federal rate payments based on the FY 2019 MS-DRG classifications and relative weights and the FY 2020 GAFs to estimated aggregate capital Federal rate payments based on the cumulative effects of the FY 2020 MS-DRG classifications and relative weights and the FY 2020 GAFs without the effects of the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases. The incremental adjustment factor for DRG classifications and changes in relative weights is 0.9987. The incremental adjustment factor for MS-DRG classifications and changes in relative weights (0.9987) and for changes in the GAFs through FY 2020 (0.9968) is 0.9956 (0.9987 × 0.9968). We note that all the values are calculated with unrounded numbers.
The GAF/DRG budget neutrality adjustment factors are built permanently into the capital rates; that is, they are applied cumulatively in determining the capital Federal rate. This follows the requirement under § 412.308(c)(4)(ii) that estimated aggregate payments each year be no more or less than they would have been in the absence of the annual DRG reclassification and recalibration and changes in the GAFs.
The methodology used to determine the recalibration and geographic adjustment factor (GAF/DRG) budget neutrality adjustment is similar to the methodology used in establishing budget neutrality adjustments under the IPPS for operating costs. One difference is that, under the operating IPPS, the budget neutrality adjustments for the effect of geographic reclassifications are determined separately from the effects of other changes in the hospital wage index and the MS-DRG relative weights. Under the capital IPPS, there is a single GAF/DRG budget neutrality adjustment factor for changes in the GAF (including geographic reclassification and the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases described above) and the MS-DRG relative weights. In addition, there is no adjustment for the effects that geographic reclassification or the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases described above have on the other payment parameters, such as the payments for DSH or IME.
The incremental GAF/DRG adjustment factor of 0.9956 (the product of the incremental GAF budget neutrality adjustment factor of 0.9968 and the incremental DRG budget neutrality adjustment factor of 0.9987) accounts for the MS-DRG reclassifications and recalibration and for changes in the GAFs. As noted previously, it also incorporates the effects on the GAFs of FY 2020 geographic reclassification decisions made by the MGCRB compared to FY 2019 decisions and the lowest quartile hospital wage index adjustment and the 5-percent cap on wage index decreases described above. However, it does not account for changes in payments due to changes in the DSH and IME adjustment factors.
4. Capital Federal Rate for FY 2020
For FY 2019, we established a capital Federal rate of $459.41 (83 FR 41729, as corrected at 83 FR 49845). We are establishing an update of 1.5 percent in determining the FY 2020 capital Federal rate for all hospitals. As a result of the update and the budget neutrality factors discussed earlier, we are establishing a national capital Federal rate of $462.61 for FY 2020, which results in a net change of 0.70 percent. The national capital Federal rate for FY 2020 was calculated as follows:
- The FY 2020 update factor is 1.015; that is, the update is 1.5 percent.
- The FY 2020 budget neutrality adjustment factor that is applied to the capital Federal rate for changes in the MS-DRG classifications and relative weights and changes in the GAFs is 0.9956.
- The FY 2020 outlier adjustment factor is 0.9461.
We are providing the following chart that shows how each of the factors and adjustments for FY 2020 affects the computation of the FY 2020 national capital Federal rate in comparison to the FY 2019 national capital Federal rate. The FY 2020 update factor has the effect of increasing the capital Federal rate by 1.5 percent compared to the FY 2019 capital Federal rate. The GAF/DRG budget neutrality adjustment factor has the effect of decreasing the capital Federal rate by 0.44 percent. The FY 2020 outlier adjustment factor has the effect of decreasing the capital Federal rate by 0.35 percent compared to the FY 2019 capital Federal rate. The combined effect of all the changes will increase the national capital Federal rate by approximately 0.70 percent, compared to the FY 2019 national capital Federal rate.

B. Calculation of the Inpatient Capital-Related Prospective Payments for FY 2020
For purposes of calculating payments for each discharge during FY 2020, the capital Federal rate is adjusted as follows: (Standard Federal Rate) × (DRG Weight) × (GAF) × (COLA for hospitals located in Alaska and Hawaii) × (1 + DSH Adjustment Factor + IME Adjustment Factor, if applicable). The result is the adjusted capital Federal rate.
Hospitals also may receive outlier payments for those cases that qualify under the threshold established for each fiscal year. Section 412.312(c) provides for a shared threshold to identify outlier cases for both inpatient operating and inpatient capital-related payments. The outlier threshold for FY 2020 are in section II.A. of this Addendum. For FY 2020, a case will qualify as a cost outlier if the cost for the case plus the (operating) IME and DSH payments (including both the empirically justified Medicare DSH payment and the estimated uncompensated care payment, as discussed in section II.A.4.h.(1). of this Addendum) is greater than the prospective payment rate for the MS-DRG plus the fixed-loss amount of $26,473.
Currently, as provided under § 412.304(c)(2), we pay a new hospital 85 percent of its reasonable costs during the first 2 years of operation, unless it elects to receive payment based on 100 percent of the capital Federal rate. Effective with the third year of operation, we pay the hospital based on 100 percent of the capital Federal rate (that is, the same methodology used to pay all other hospitals subject to the capital PPS).
C. Capital Input Price Index
1. Background
Like the operating input price index, the capital input price index (CIPI) is a fixed-weight price index that measures the price changes associated with capital costs during a given year. The CIPI differs from the operating input price index in one important aspect—the CIPI reflects the vintage nature of capital, which is the acquisition and use of capital over time. Capital expenses in any given year are determined by the stock of capital in that year (that is, capital that remains on hand from all current and prior capital acquisitions). An index measuring capital price changes needs to reflect this vintage nature of capital. Therefore, the CIPI was developed to capture the vintage nature of capital by using a weighted-average of past capital purchase prices up to and including the current year.
We periodically update the base year for the operating and capital input price indexes to reflect the changing composition of inputs for operating and capital expenses. For this FY 2020 IPPS/LTCH PPS final rule, we used the rebased and revised IPPS operating and capital market baskets that reflect a 2014 base year. For a complete discussion of this rebasing, we refer readers to section IV. of the preamble of the FY 2018 IPPS/LTCH PPS final rule (82 FR 38170).
2. Forecast of the CIPI for FY 2020
Based on IHS Global Inc.'s second quarter 2019 forecast, for this FY 2020 IPPS/LTCH/PPS final rule, we forecast the 2014-based CIPI to increase 1.5 percent in FY 2020. This reflects a projected 1.8 percent increase in vintage-weighted depreciation prices (building and fixed equipment, and movable equipment), and a projected 3.3 percent increase in other capital expense prices in FY 2020, partially offset by a projected 1.1 percent decline in vintage-weighted interest expense prices in FY 2020. The weighted average of these three factors produces the forecasted 1.5 percent increase for the 2014-based CIPI in FY 2020.
IV. Changes to Payment Rates for Excluded Hospitals: Rate-of-Increase Percentages for FY 2020
Payments for services furnished in children's hospitals, 11 cancer hospitals, and hospitals located outside the 50 States, the District of Columbia and Puerto Rico (that is, short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa) that are excluded from the IPPS are made on the basis of reasonable costs based on the hospital's own historical cost experience, subject to a rate-of-increase ceiling. A per discharge limit (the target amount, as defined in § 413.40(a) of the regulations) is set for each hospital, based on the hospital's own cost experience in its base year, and updated annually by a rate-of-increase percentage specified in § 413.40(c)(3). In addition, as specified in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38536), effective for cost reporting periods beginning during FY 2018, the annual update to the target amount for extended neoplastic disease care hospitals (hospitals described in § 412.22(i) of the regulations) also is the rate-of-increase percentage specified in § 413.40(c)(3). (We note that, in accordance with § 403.752(a), religious nonmedical health care institutions (RNHCIs) are also subject to the rate-of-increase limits established under § 413.40 of the regulations.)
The FY 2020 rate-of-increase percentage for updating the target amounts for the 11 cancer hospitals, children's hospitals, the short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa, RNHCIs, and extended neoplastic disease care hospitals is the estimated percentage increase in the IPPS operating market basket for FY 2020, in accordance with applicable regulations at § 413.40. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19609), based on IGI's 2018 fourth quarter forecast, we estimated that the 2014-based IPPS operating market basket update for FY 2020 was 3.2 percent (that is, the estimate of the market basket rate-of-increase). However, we proposed that if more recent data became available for the final rule, we would use them to calculate the IPPS operating market basket update for FY 2020. For this final rule, based on IGI's 2019 second quarter forecast, (which is the most recent available data), we estimate that the 2014-based IPPS operating market basket update for FY 2020 is 3.0 percent (that is, the estimate of the market basket rate-of-increase). Therefore, for children's hospitals, the 11 cancer hospitals, hospitals located outside the 50 States, the District of Columbia, and Puerto Rico (that is, short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa), extended neoplastic disease care hospitals, and RNHCIs, the FY 2020 rate-of-increase percentage that will be applied to the FY 2019 target amounts, in order to determine the FY 2020 target amounts is 3.0 percent.
The IRF PPS, the IPF PPS, and the LTCH PPS are updated annually. We refer readers to section VII. of the preamble of this final rule and section V. of the Addendum to this final rule for the updated changes to the Federal payment rates for LTCHs under the LTCH PPS for FY 2020. The annual updates for the IRF PPS and the IPF PPS are issued by the agency in separate Federal Register documents.
V. Changes to the Payment Rates for the LTCH PPS for FY 2020
A. LTCH PPS Standard Federal Payment Rate for FY 2020
1. Overview
In section VII. of the preamble of this final rule, we discuss our annual updates to the payment rates, factors, and specific policies under the LTCH PPS for FY 2020.
Under § 412.523(c)(3) of the regulations, for LTCH PPS FYs 2012 through 2019, we updated the standard Federal payment rate by the most recent estimate of the LTCH PPS market basket at that time, including additional statutory adjustments required by sections 1886(m)(3) (citing sections 1886(b)(3)(B)(xi)(II), and 1886(m)(4) of the Act as set forth in the regulations at §§ 412.523(c)(3)(viii) through (c)(3)(xv)). (For a summary of the payment rate development prior to FY 2012, we refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38310 through 38312) and references therein.)
Section 1886(m)(3)(A) of the Act specifies that, for rate year 2020 and each subsequent rate year, any annual update to the standard Federal payment rate shall be reduced by the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act (which we refer to as “the multifactor productivity (MFP) adjustment”) as discussed in section VII.D.2. of the preamble of this final rule.
This section of the Act further provides that the application of section 1886(m)(3)(B) of the Act may result in the annual update being less than zero for a rate year, and may result in payment rates for a rate year being less than such payment rates for the preceding rate year. (As noted in section VII.D.2.a. of the preamble of this final rule, the annual update to the LTCH PPS occurs on October 1 and we have adopted the term “fiscal year” (FY) rather than “rate year” (RY) under the LTCH PPS beginning October 1, 2010. Therefore, for purposes of clarity, when discussing the annual update for the LTCH PPS, including the provisions of the Affordable Care Act, we use the term “fiscal year” rather than “rate year” for 2011 and subsequent years.)
For LTCHs that fail to submit the required quality reporting data in accordance with the LTCH QRP, the annual update is reduced by 2.0 percentage points as required by section 1886(m)(5) of the Act.
2. Development of the FY 2020 LTCH PPS Standard Federal Payment Rate
Consistent with our historical practice, for FY 2020, as we proposed, we are applying the annual update to the LTCH PPS standard Federal payment rate from the previous year. Furthermore, in determining the LTCH PPS standard Federal payment rate for FY 2020, we also are making certain regulatory adjustments, consistent with past practices. Specifically, in determining the FY 2020 LTCH PPS standard Federal payment rate, as we proposed, we are applying a budget neutrality adjustment factor for the changes related to the area wage level adjustment (that is, changes to the wage data and labor-related share) in accordance with § 412.523(d)(4) and a temporary budget neutrality adjustment factor (applied to LTCH PPS standard Federal payment rate cases only) for the cost of the elimination of the 25-percent threshold policy for FY 2020 (discussed in VII.D. of the preamble of this final rule).
In this FY 2020 IPPS/LTCH PPS final rule, we are establishing an annual update to the LTCH PPS standard Federal payment rate of 2.5 percent. Accordingly, as reflected in § 412.523(c)(3)(xvi), we are applying a factor of 1.025 to the FY 2019 LTCH PPS standard Federal payment rate of $42,558.68 to determine the FY 2020 LTCH PPS standard Federal payment rate. Also, as reflected in § 412.523(c)(3)(xvi), applied in conjunction with the provisions of § 412.523(c)(4), we are establishing an annual update to the LTCH PPS standard Federal payment rate of 0.5 percent (that is, an update factor of 1.005) for FY 2020 for LTCHs that fail to submit the required quality reporting data for FY 2020 as required under the LTCH QRP. Additionally, we are applying a temporary budget neutrality adjustment factor of 0.990737 to the LTCH PPS standard Federal payment rate for the cost of the elimination of the 25-percent threshold policy for FY 2020 after removing the temporary budget neutrality adjustment factor of 0.990878 that was applied to the LTCH PPS standard Federal payment rate for the cost of the elimination of the 25-percent threshold policy for FY 2019 (or a temporary, one-time factor of 0.999858 as discussed in VII.D. of the preamble of this final rule). Consistent with § 412.523(d)(4), we also are applying an area wage level budget neutrality factor to the FY 2020 LTCH PPS standard Federal payment rate of 1.0020203, based on the best available data at this time, to ensure that any changes to the area wage level adjustment (that is, the annual update of the wage index values and labor-related share) would not result in any change (increase or decrease) in estimated aggregate LTCH PPS standard Federal payment rate payments. Accordingly, we are establishing an LTCH PPS standard Federal payment rate of $42,677.63 (calculated as $41,558.68 × 0.999858 × 1.025 × 1.0020203) for FY 2020 (calculations performed on rounded numbers). For LTCHs that fail to submit quality reporting data for FY 2020, in accordance with the requirements of the LTCH QRP under section 1866(m)(5) of the Act, we are establishing an LTCH PPS standard Federal payment rate of $41,844.89 (calculated as $41,558.68 × 0.999858 × 1.005 × 1.0020203) (calculations performed on rounded numbers) for FY 2020.
Comment: Some commenters objected to our application of the budget neutrality adjustment stemming from elimination of the 25-percent threshold policy on the grounds that doing so penalizes LTCHs that have historically maintained compliance with this policy.
Response: We addressed similar comments when we finalized the FY 2020 budget neutrality adjustment stemming from elimination of the 25-percent threshold policy in the FY 2019 IPPS/LTCH Final Rule (83 FR 41532 through 41537). As a result of that rulemaking, this budget neutrality adjustment is required by regulations at § 412.523(d)(6).
After review of public comments on our proposed development of the FY 2020 LTCH PPS standard Federal payment rate, we are finalizing our proposals as previously described, without modification.
B. Adjustment for Area Wage Levels Under the LTCH PPS for FY 2020
1. Background
Under the authority of section 123 of the BBRA, as amended by section 307(b) of the BIPA, we established an adjustment to the LTCH PPS standard Federal payment rate to account for differences in LTCH area wage levels under § 412.525(c). The labor-related share of the LTCH PPS standard Federal payment rate is adjusted to account for geographic differences in area wage levels by applying the applicable LTCH PPS wage index. The applicable LTCH PPS wage index is computed using wage data from inpatient acute care hospitals without regard to reclassification under section 1886(d)(8) or section 1886(d)(10) of the Act.
2. Geographic Classifications (Labor Market Areas) for the LTCH PPS Standard Federal Payment Rate
In adjusting for the differences in area wage levels under the LTCH PPS, the labor-related portion of an LTCH's Federal prospective payment is adjusted by using an appropriate area wage index based on the geographic classification (labor market area) in which the LTCH is located. Specifically, the application of the LTCH PPS area wage level adjustment under existing § 412.525(c) is made based on the location of the LTCH—either in an “urban area,” or a “rural area,” as defined in § 412.503. Under § 412.503, an “urban area” is defined as a Metropolitan Statistical Area (MSA) (which includes a Metropolitan division, where applicable), as defined by the Executive OMB and a “rural area” is defined as any area outside of an urban area (75 FR 37246).
The CBSA-based geographic classifications (labor market area definitions) currently used under the LTCH PPS, effective for discharges occurring on or after October 1, 2014, are based on the OMB labor market area delineations based on the 2010 Decennial Census data. The current statistical areas (which were implemented beginning with FY 2015) are based on revised OMB delineations issued on February 28, 2013, in OMB Bulletin No. 13-01. We adopted these labor market area delineations because they are based on the best available data that reflect the local economies and area wage levels of the hospitals that are currently located in these geographic areas. We also believe that these OMB delineations will ensure that the LTCH PPS area wage level adjustment most appropriately accounts for and reflects the relative hospital wage levels in the geographic area of the hospital as compared to the national average hospital wage level. We noted that this policy was consistent with the IPPS policy adopted in FY 2015 under § 412.64(b)(1)(ii)(D) of the regulations (79 FR 49951 through 49963). (For additional information on the CBSA-based labor market area (geographic classification) delineations currently used under the LTCH PPS and the history of the labor market area definitions used under the LTCH PPS, we refer readers to the FY 2015 IPPS/LTCH PPS final rule (79 FR 50180 through 50185).)
In general, it is our historical practice to update the CBSA-based labor market area delineations annually based on the most recent updates issued by OMB. Generally, OMB issues major revisions to statistical areas every 10 years, based on the results of the decennial census. However, OMB occasionally issues minor updates and revisions to statistical areas in the years between the decennial censuses. OMB Bulletin No. 17-01, issued August 15, 2017, establishes the current delineations for the Nation's statistical areas, and the corresponding changes to the CBSA-based labor market areas were adopted in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41731). A copy of this bulletin may be obtained on the website at: https://www.whitehouse.gov/sites/whitehouse.gov/files/omb/bulletins/2017/b-17-01.pdf.
We believe the current CBSA-based labor market area delineations as established in OMB Bulletin 17-01 and adopted in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41731) will ensure that the LTCH PPS area wage level adjustment most appropriately accounts for and reflects the relative hospital wage levels in the geographic area of the hospital as compared to the national average hospital wage level based on the best available data that reflect the local economies and area wage levels of the hospitals that are currently located in these geographic areas (81 FR 57298). Therefore, as we proposed, we are continuing to use the CSBA-based labor market area delineations adopted under the LTCH PPS, effective October 1, 2019 (as adopted in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41731)). Accordingly, the FY 2020 LTCH PPS wage index values in Tables 12A and 12B listed in section VI. of the Addendum to this final rule (which are available via the internet on the CMS website) reflect the CBSA-based labor market area delineations as previously described. We note that, as discussed in section III.A.2. of the preamble of this final rule, these CBSA-based delineations also are being used under the IPPS.
We did not receive any public comments in response to our proposals. Therefore, we are finalizing our proposals, without modification.
3. Labor-Related Share for the LTCH PPS Standard Federal Payment Rate
Under the payment adjustment for the differences in area wage levels under § 412.525(c), the labor-related share of an LTCH's standard Federal payment rate payment is adjusted by the applicable wage index for the labor market area in which the LTCH is located. The LTCH PPS labor-related share currently represents the sum of the labor-related portion of operating costs and a labor-related portion of capital costs using the applicable LTCH PPS market basket. Additional background information on the historical development of the labor-related share under the LTCH PPS can be found in the RY 2007 LTCH PPS final rule (71 FR 27810 through 27817 and 27829 through 27830) and the FY 2012 IPPS/LTCH PPS final rule (76 FR 51766 through 51769 and 51808).
For FY 2013, we rebased and revised the market basket used under the LTCH PPS by adopting a 2009-based LTCH-specific market basket. In addition, beginning in FY 2013, we determined the labor-related share annually as the sum of the relative importance of each labor-related cost category of the 2009-based LTCH-specific market basket for the respective fiscal year based on the best available data. (For more details, we refer readers to the FY 2013 IPPS/LTCH PPS final rule (77 FR 53477 through 53479).) As noted previously, we rebased and revised the 2009-based LTCH-specific market basket to reflect a 2013 base year. In conjunction with that policy, as discussed in section VII.D. of the preamble of this FY 2020 IPPS/LTCH PPS final rule, as we proposed, we are establishing that the LTCH PPS labor-related share for FY 2020 is the sum of the FY 2020 relative importance of each labor-related cost category in the 2013-based LTCH market basket using the most recent available data.
Specifically, in the proposed rule, we proposed to establish that the labor-related share for FY 2020 includes the sum of the labor-related portion of operating costs from the 2013-based LTCH market basket (that is, the sum of the FY 2020 relative importance share of Wages and Salaries; Employee Benefits; Professional Fees: Labor-Related; Administrative and Facilities Support Services; Installation, Maintenance, and Repair Services; All Other: Labor-related Services) and a portion of the relative importance of the Capital-Related cost weight from the 2013-based LTCH PPS market basket. Based on IGI's fourth quarter 2018 forecast of the 2013-based LTCH market basket, we proposed to establish a labor-related share under the LTCH PPS for FY 2020 of 66.0 percent. (We noted that a proposed labor-related share of 66.0 percent was the same as the labor-related share for FY 2019, and although the relative importance of some components of the market basket have changed, the proposed labor-related share remained at 66.0 percent when aggregating these components and rounding to one decimal.) This proposed labor-related share was determined using the same methodology as employed in calculating all previous LTCH PPS labor-related shares. Consistent with our historical practice, we also proposed that if more recent data became available, we would use that data, if appropriate, to determine the final FY 2020 labor-related share in the final rule. We did not receive any public comments in response to our proposals. Therefore, we are finalizing our proposals, without modification.
In this final rule, we are establishing that the labor-related share for FY 2020 includes the sum of the labor-related portion of operating costs from the 2013-based LTCH market basket (that is, the sum of the FY 2020 relative importance share of Wages and Salaries; Employee Benefits; Professional Fees: Labor-Related; Administrative and Facilities Support Services; Installation, Maintenance, and Repair Services; All Other: Labor-related Services) and a portion of the relative importance of the Capital-Related cost weight from the 2013-based LTCH PPS market basket. Based on IGI's second quarter 2019 forecast of the 2013-based LTCH market basket, consistent with our proposal to use more recent data, if appropriate, we are establishing a labor-related share under the LTCH PPS for FY 2020 of 66.3 percent.
The labor-related share for FY 2020 is the sum of the FY 2020 relative importance of each labor-related cost category, and reflects the different rates of price change for these cost categories between the base year (2013) and FY 2020. The sum of the relative importance for FY 2020 for operating costs (Wages and Salaries; Employee Benefits; Professional Fees: Labor-Related; Administrative and Facilities Support Services; Installation, Maintenance, and Repair Services; All Other: Labor-Related Services) is 62.2 percent. The portion of capital-related costs that is influenced by the local labor market is estimated to be 46 percent (the same percentage applied to the 2009-based LTCH-specific market basket). Because the relative importance for capital-related costs under our policies is 9.0 percent of the 2013-based LTCH market basket in FY 2020, as we proposed, we are taking 46 percent of 9.0 percent to determine the labor-related share of capital-related costs for FY 2020 (0.46 × 9.0). The result is 4.1 percent, which we added to 62.2 percent for the operating cost amount to determine the total labor-related share for FY 2020. Therefore, as we proposed, we are establishing that the labor-related share under the LTCH PPS for FY 2020 is 66.3 percent.
4. Wage Index for FY 2020 for the LTCH PPS Standard Federal Payment Rate
Historically, we have established LTCH PPS area wage index values calculated from acute care IPPS hospital wage data without taking into account geographic reclassification under sections 1886(d)(8) and 1886(d)(10) of the Act (67 FR 56019). The area wage level adjustment established under the LTCH PPS is based on an LTCH's actual location without regard to the “urban” or “rural” designation of any related or affiliated provider.
In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41732), we calculated the FY 2019 LTCH PPS area wage index values using the same data used for the FY 2019 acute care hospital IPPS (that is, data from cost reporting periods beginning during FY 2015), without taking into account geographic reclassification under sections 1886(d)(8) and 1886(d)(10) of the Act, as these were the most recent complete data available at that time. In that same final rule, we indicated that we computed the FY 2019 LTCH PPS area wage index values, consistent with the urban and rural geographic classifications (labor market areas) that were in place at that time and consistent with the pre-reclassified IPPS wage index policy (that is, our historical policy of not taking into account IPPS geographic reclassifications in determining payments under the LTCH PPS). As with the IPPS wage index, wage data for multicampus hospitals with campuses located in different labor market areas (CBSAs) are apportioned to each CBSA where the campus (or campuses) are located. We also continued to use our existing policy for determining area wage index values for areas where there are no IPPS wage data.
Consistent with our historical methodology, as discussed in the FY 2020 IPPS/LTCH PPS proposed rule, to determine the applicable area wage index values for the FY 2020 LTCH PPS standard Federal payment rate, under the broad authority of section 123 of the BBRA, as amended by section 307(b) of the BIPA, we proposed to use wage data collected from cost reports submitted by IPPS hospitals for cost reporting periods beginning during FY 2016, without taking into account geographic reclassification under sections 1886(d)(8) and 1886(d)(10) of the Act because these data are the most recent complete data available. We also note that these are the same data we are using to compute the FY 2020 acute care hospital inpatient wage index, as discussed in section III. of the preamble of this final rule. We proposed to compute the FY 2020 LTCH PPS standard Federal payment rate area wage index values consistent with the “urban” and “rural” geographic classifications (that is, labor market area delineations, including the updates, as previously discussed in section V.B. of this Addendum) and our historical policy of not taking into account IPPS geographic reclassifications under sections 1886(d)(8) and 1886(d)(10) of the Act in determining payments under the LTCH PPS. We also proposed to continue to apportion the wage data for multicampus hospitals with campuses located in different labor market areas to each CBSA where the campus or campuses are located, consistent with the IPPS policy. Lastly, consistent with our existing methodology for determining the LTCH PPS wage index values, for FY 2020, we proposed to continue to use our existing policy for determining area wage index values for areas where there are no IPPS wage data. Under our existing methodology, the LTCH PPS wage index value for urban CBSAs with no IPPS wage data would be determined by using an average of all of the urban areas within the State, and the LTCH PPS wage index value for rural areas with no IPPS wage data would be determined by using the unweighted average of the wage indices from all of the CBSAs that are contiguous to the rural counties of the State.
While our existing methodology remains unchanged, we identified an error in the proposed rule wage index values after the FY 2020 IPPS/LTCH PPS proposed rule was published. A programming error caused the data for all providers in a single county to be included twice, which affected the national average hourly rate, and therefore affected all wage index values. In this final rule, we have changed the programming logic so this error cannot occur again. In addition, in this final rule, we corrected the classification of one county in North Carolina to rural status, as this county was erroneously identified as being in an urban CBSA. Finally, we standardized our procedures for rounding, to ensure consistency.
Comment: A commenter objected to the underlying IPPS average hourly wage data, as released in the public use file, used to determine the FY 2020 LTCH PPS proposed wage index values, calling the exclusion of certain IPPS hospitals' wage index data, as discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19375 through 19376), from the calculation untenable and asserting that the exclusion must be reversed. This commenter is referring to the exclusion of seven hospitals' wage data discussed in section III.C. of the preamble of this final rule.
Response: Consistent with historical our practice (see, for example, the RY 2008 LTCH PPS final rule (72 FR 26891)), the proposed FY 2020 LTCH PPS wage index values were calculated using the same data we use to compute the FY 2020 acute care hospital inpatient wage index. While the commenter did not clarify how the exclusion of those seven hospitals' wage data made the LTCH PPS wage index calculation “untenable”, or why we should deviate from our historical methodology of using IPPS hospital data to compute the FY 2020 LTCH PPS wage index values, we note as discussed in more detail in section III.C. of this rule, the IPPS hospital wage data used to determine both the FY 2020 IPPS wage index and, by extension, the FY 2020 LTCH PPS wage index includes data from those seven IPPS hospitals originally excluded in the proposed FY 2020 wage index values, therefore rendering the commenter's objections moot. For more information on the IPPS hospital wage data, including the data of those seven IPPS hospitals, we refer readers to III.C. of this rule).
After consideration of public comments (and correction of the inadvertent programming errors discussed above), we are finalizing our proposals related to the FY 2020 LTCH PPS wage index values.
Based on the FY 2016 IPPS wage data that we used to determine the FY 2020 LTCH PPS standard Federal payment rate area wage index values in this final rule, there are no IPPS wage data for the urban area of Hinesville, GA (CBSA 25980). Consistent with the methodology as previously discussed, we calculated the FY 2020 wage index value for CBSA 25980 as the average of the wage index values for all of the other urban areas within the State of Georgia (that is, CBSAs 10500, 12020, 12060, 12260, 15260, 16860, 17980, 19140, 23580, 31420, 40660, 42340, 46660 and 47580), as shown in Table 12A, which is listed in section VI. of the Addendum to this final rule and available via the internet on the CMS website. (We note that although we had no IPPS wage data for the urban area of Carson City, NV (CBSA 16810) in the proposed rule, based on the updated data used for this final rule, there is now IPPS wage data for the urban area of Carson City, NV (CBSA 16810) for this final rule.)
Based on the FY 2016 IPPS wage data that we used to determine the FY 2020 LTCH PPS standard Federal payment rate area wage index values in this final rule, there are no rural areas without IPPS hospital wage data. Therefore, it is not necessary to use our established methodology to calculate a LTCH PPS standard Federal payment rate wage index value for rural areas with no IPPS wage data for FY 2020. We note that, as IPPS wage data are dynamic, it is possible that the number of rural areas without IPPS wage data will vary in the future. The FY 2020 LTCH PPS standard Federal payment rate wage index values that will be applicable for LTCH PPS standard Federal payment rate discharges occurring on or after October 1, 2019, through September 30, 2020, are presented in Table 12A (for urban areas) and Table 12B (for rural areas), which are listed in section VI. of the Addendum to this final rule and available via the internet on the CMS website.
Historically, we have calculated the LTCH PPS wage index values using unadjusted wage index values from the IPPS hospitals. Stakeholders have frequently commented on certain aspects of the wage index values and their impact on payments. In the proposed rule, we solicited public comments on concerns that stakeholders may have regarding the wage index used to adjust LTCH PPS payments and suggestions for possible updates and improvements to the geographic adjustment of LTCH PPS payments. We appreciate the responses from commenters and shall consider their suggestions in future rulemaking.
5. Budget Neutrality Adjustment for Changes to the LTCH PPS Standard Federal Payment Rate Area Wage Level Adjustment
Historically, the LTCH PPS wage index and labor-related share are updated annually based on the latest available data. Under § 412.525(c)(2), any changes to the area wage index values or labor-related share are to be made in a budget neutral manner such that estimated aggregate LTCH PPS payments are unaffected; that is, will be neither greater than nor less than estimated aggregate LTCH PPS payments without such changes to the area wage level adjustment. Under this policy, we determine an area wage level adjustment budget neutrality factor that will be applied to the standard Federal payment rate to ensure that any changes to the area wage level adjustments are budget neutral such that any changes to the area wage index values or labor-related share would not result in any change (increase or decrease) in estimated aggregate LTCH PPS payments. Accordingly, under § 412.523(d)(4), we apply an area wage level adjustment budget neutrality factor in determining the standard Federal payment rate, and we also established a methodology for calculating an area wage level adjustment budget neutrality factor. (For additional information on the establishment of our budget neutrality policy for changes to the area wage level adjustment, we refer readers to the FY 2012 IPPS/LTCH PPS final rule (76 FR 51771 through 51773 and 51809).)
In the FY 2020 IPPS/LTCH PPS proposed rule, for FY 2020 LTCH PPS standard Federal payment rate cases, in accordance with § 412.523(d)(4), we proposed to apply an area wage level adjustment budget neutrality factor to adjust the LTCH PPS standard Federal payment rate to account for the estimated effect of the adjustments or updates to the area wage level adjustment under § 412.525(c)(1) on estimated aggregate LTCH PPS payments using a methodology that is consistent with the methodology we established in the FY 2012 IPPS/LTCH PPS final rule (76 FR 51773). We did not receive any public comments in response to our proposals. Therefore, we are finalizing our proposals, without modification.
Specifically, as we proposed, we determined an area wage level adjustment budget neutrality factor that would be applied to the LTCH PPS standard Federal payment rate under § 412.523(d)(4) for FY 2020 using the following methodology:
Step 1—We simulated estimated aggregate LTCH PPS standard Federal payment rate payments using the FY 2019 wage index values and the FY 2019 labor-related share of 66.0 percent (as established in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41732)).
Step 2—We simulated estimated aggregate LTCH PPS standard Federal payment rate payments using the FY 2020 wage index values (as shown in Tables 12A and 12B listed in the Addendum to this final rule and available via the internet on the CMS website) and the FY 2020 labor-related share of 66.3 percent (based on the latest available data as previously discussed in this Addendum).
Step 3—We calculated the ratio of these estimated total LTCH PPS standard Federal payment rate payments by dividing the estimated total LTCH PPS standard Federal payment rate payments using the FY 2019 area wage level adjustments (calculated in Step 1) by the estimated total LTCH PPS standard Federal payment rate payments using the FY 2020 area wage level adjustments (calculated in Step 2) to determine the area wage level adjustment budget neutrality factor for FY 2020 LTCH PPS standard Federal payment rate payments.
Step 4—We then applied the FY 2020 area wage level adjustment budget neutrality factor from Step 3 to determine the FY 2020 LTCH PPS standard Federal payment rate after the application of the FY 2020 annual update (discussed previously in section V.A. of this Addendum).
We note that, with the exception of cases subject to the transitional blended payment rate provisions and certain temporary exemptions for certain spinal cord specialty hospitals and certain severe wound cases, under the dual rate LTCH PPS payment structure, only LTCH PPS cases that meet the statutory criteria to be excluded from the site neutral payment rate (that is, LTCH PPS standard Federal payment rate cases) are paid based on the LTCH PPS standard Federal payment rate. Because the area wage level adjustment under § 412.525(c) is an adjustment to the LTCH PPS standard Federal payment rate, we only used data from claims that would have qualified for payment at the LTCH PPS standard Federal payment rate if such rate had been in effect at the time of discharge to calculate the FY 2020 LTCH PPS standard Federal payment rate area wage level adjustment budget neutrality factor as previously described. Moreover, we note that the estimated LTCH PPS standard Federal payment rate used in the calculations in Steps 1 through 4, as previously discussed, include the one-time budget neutrality adjustment factor for the estimated cost of eliminating the 25-percent threshold policy in FY 2020, as discussed in section VII.D. of the preamble of this final rule.
For this final rule, using the steps in the methodology previously described, we determined a FY 2020 LTCH PPS standard Federal payment rate area wage level adjustment budget neutrality factor of 1.0020203. Accordingly, in section V.A. of the Addendum to this final rule, to determine the FY 2020 LTCH PPS standard Federal payment rate, as we proposed, we are applying an area wage level adjustment budget neutrality factor of 1.0020203, in accordance with § 412.523(d)(4).
C. LTCH PPS Cost-of-Living Adjustment (COLA) for LTCHs Located in Alaska and Hawaii
Under § 412.525(b), a cost-of-living adjustment (COLA) is provided for LTCHs located in Alaska and Hawaii to account for the higher costs incurred in those States. Specifically, we apply a COLA to payments to LTCHs located in Alaska and Hawaii by multiplying the nonlabor-related portion of the standard Federal payment rate by the applicable COLA factors established annually by CMS. Higher labor-related costs for LTCHs located in Alaska and Hawaii are taken into account in the adjustment for area wage levels previously described. The methodology used to determine the COLA factors for Alaska and Hawaii is based on a comparison of the growth in the Consumer Price Indexes (CPIs) for Anchorage, Alaska, and Honolulu, Hawaii, relative to the growth in the CPI for the average U.S. city as published by the Bureau of Labor Statistics (BLS). It also includes a 25-percent cap on the CPI-updated COLA factors. Under our current policy, we update the COLA factors using the methodology as previously described every 4 years (at the same time as the update to the labor-related share of the IPPS market basket), and we last updated the COLA factors for Alaska and Hawaii published by OPM for 2009 in FY 2018 (82 FR 38539 through 38540).
We continue to believe that determining updated COLA factors using this methodology would appropriately adjust the nonlabor-related portion of the LTCH PPS standard Federal payment rate for LTCHs located in Alaska and Hawaii. Therefore, in the FY 2020 IPPS/LTCH PPS proposed rule, for FY 2020, under the broad authority conferred upon the Secretary by section 123 of the BBRA, as amended by section 307(b) of the BIPA, to determine appropriate payment adjustments under the LTCH PPS, we proposed to continue to use the COLA factors based on the 2009 OPM COLA factors updated through 2016 by the comparison of the growth in the CPIs for Anchorage, Alaska, and Honolulu, Hawaii, relative to the growth in the CPI for the average U.S. city as established in the FY 2018 IPPS/LTCH PPS final rule. (For additional details on our current methodology for updating the COLA factors for Alaska and Hawaii and for a discussion on the FY 2018 COLA factors, we refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38539 through 38540).)
We did not receive any public comments on our proposal. Therefore, we are adopting our proposal, without modification. Consistent with our historical practice, we are establishing that the COLA factors shown in the following table will be used to adjust the nonlabor-related portion of the LTCH PPS standard Federal payment rate for LTCHs located in Alaska and Hawaii under § 412.525(b).

D. Adjustment for LTCH PPS High Cost Outlier (HCO) Cases
1. HCO Background
From the beginning of the LTCH PPS, we have included an adjustment to account for cases in which there are extraordinarily high costs relative to the costs of most discharges. Under this policy, additional payments are made based on the degree to which the estimated cost of a case (which is calculated by multiplying the Medicare allowable covered charge by the hospital's overall hospital CCR) exceeds a fixed-loss amount. This policy results in greater payment accuracy under the LTCH PPS and the Medicare program, and the LTCH sharing the financial risk for the treatment of extraordinarily high-cost cases.
We retained the basic tenets of our HCO policy in FY 2016 when we implemented the dual rate LTCH PPS payment structure under section 1206 of Pub. L. 113-67. LTCH discharges that meet the criteria for exclusion from the site neutral payment rate (that is, LTCH PPS standard Federal payment rate cases) are paid at the LTCH PPS standard Federal payment rate, which includes, as applicable, HCO payments under § 412.523(e). LTCH discharges that do not meet the criteria for exclusion are paid at the site neutral payment rate, which includes, as applicable, HCO payments under § 412.522(c)(2)(i). In the FY 2016 IPPS/LTCH PPS final rule, we established separate fixed-loss amounts and targets for the two different LTCH PPS payment rates. Under this bifurcated policy, the historic 8-percent HCO target was retained for LTCH PPS standard Federal payment rate cases, with the fixed-loss amount calculated using only data from LTCH cases that would have been paid at the LTCH PPS standard Federal payment rate if that rate had been in effect at the time of those discharges. For site neutral payment rate cases, we adopted the operating IPPS HCO target (currently 5.1 percent) and set the fixed-loss amount for site neutral payment rate cases at the value of the IPPS fixed-loss amount. Under the HCO policy for both payment rates, an LTCH receives 80 percent of the difference between the estimated cost of the case and the applicable HCO threshold, which is the sum of the LTCH PPS payment for the case and the applicable fixed-loss amount for such case.
In order to maintain budget neutrality, consistent with the budget neutrality requirement for HCO payments to LTCH PPS standard Federal rate payment cases, we also adopted a budget neutrality requirement for HCO payments to site neutral payment rate cases by applying a budget neutrality factor to the LTCH PPS payment for those site neutral payment rate cases. (We refer readers to § 412.522(c)(2)(i) of the regulations for further details.) We note that, during the 2-year transitional period, the site neutral payment rate HCO budget neutrality factor did not apply to the LTCH PPS standard Federal payment rate portion of the blended payment rate at § 412.522(c)(3) payable to site neutral payment rate cases. (For additional details on the HCO policy adopted for site neutral payment rate cases under the dual rate LTCH PPS payment structure, including the budget neutrality adjustment for HCO payments to site neutral payment rate cases, we refer readers to the FY 2016 IPPS/LTCH PPS final rule (80 FR 49617 through 49623).)
2. Determining LTCH CCRs Under the LTCH PPS
a. Background
As noted above, CCRs are used to determine payments for HCO adjustments for both payment rates under the LTCH PPS and also are used to determine payments for site neutral payment rate cases. As noted earlier, in determining HCO and the site neutral payment rate payments (regardless of whether the case is also an HCO), we generally calculate the estimated cost of the case by multiplying the LTCH's overall CCR by the Medicare allowable charges for the case. An overall CCR is used because the LTCH PPS uses a single prospective payment per discharge that covers both inpatient operating and capital-related costs. The LTCH's overall CCR is generally computed based on the sum of LTCH operating and capital costs (as described in Section 150.24, Chapter 3, of the Medicare Claims Processing Manual (Pub. 100-4)) as compared to total Medicare charges (that is, the sum of its operating and capital inpatient routine and ancillary charges), with those values determined from either the most recently settled cost report or the most recent tentatively settled cost report, whichever is from the latest cost reporting period. However, in certain instances, we use an alternative CCR, such as the statewide average CCR, a CCR that is specified by CMS, or one that is requested by the hospital. (We refer readers to § 412.525(a)(4)(iv) of the regulations for further details regarding HCO adjustments for either LTCH PPS payment rate and § 412.522(c)(1)(ii) for the site neutral payment rate.)
The LTCH's calculated CCR is then compared to the LTCH total CCR ceiling. Under our established policy, an LTCH with a calculated CCR in excess of the applicable maximum CCR threshold (that is, the LTCH total CCR ceiling, which is calculated as 3 standard deviations from the national geometric average CCR) is generally assigned the applicable statewide CCR. This policy is premised on a belief that calculated CCRs above the LTCH total CCR ceiling are most likely due to faulty data reporting or entry, and CCRs based on erroneous data should not be used to identify and make payments for outlier cases.
b. LTCH Total CCR Ceiling
Consistent with our historical practice, as we proposed, we used the most recent data available to determine the LTCH total CCR ceiling for FY 2020 in this final rule. Specifically, in this final rule, using our established methodology for determining the LTCH total CCR ceiling based on IPPS total CCR data from the March 2019 update of the Provider Specific File (PSF), which is the most recent data available, we are establishing an LTCH total CCR ceiling of 1.253 under the LTCH PPS for FY 2020 in accordance with § 412.525(a)(4)(iv)(C)(2) for HCO cases under either payment rate and § 412.522(c)(1)(ii) for the site neutral payment rate. (For additional information on our methodology for determining the LTCH total CCR ceiling, we refer readers to the FY 2007 IPPS final rule (71 FR 48118 through 48119).)
We did not receive any public comments on our proposals. Therefore, we are finalizing our proposals as described above, without modification.
c. LTCH Statewide Average CCRs
Our general methodology for determining the statewide average CCRs used under the LTCH PPS is similar to our established methodology for determining the LTCH total CCR ceiling because it is based on “total” IPPS CCR data. (For additional information on our methodology for determining statewide average CCRs under the LTCH PPS, we refer readers to the FY 2007 IPPS final rule (71 FR 48119 through 48120).) Under the LTCH PPS HCO policy for cases paid under either payment rate at § 412.525(a)(4)(iv)(C)(2), the current SSO policy at § 412.529(f)(4)(iii)(B), and the site neutral payment rate at § 412.522(c)(1)(ii), the MAC may use a statewide average CCR, which is established annually by CMS, if it is unable to determine an accurate CCR for an LTCH in one of the following circumstances: (1) New LTCHs that have not yet submitted their first Medicare cost report (a new LTCH is defined as an entity that has not accepted assignment of an existing hospital's provider agreement in accordance with § 489.18); (2) LTCHs whose calculated CCR is in excess of the LTCH total CCR ceiling; and (3) other LTCHs for whom data with which to calculate a CCR are not available (for example, missing or faulty data). (Other sources of data that the MAC may consider in determining an LTCH's CCR include data from a different cost reporting period for the LTCH, data from the cost reporting period preceding the period in which the hospital began to be paid as an LTCH (that is, the period of at least 6 months that it was paid as a short-term, acute care hospital), or data from other comparable LTCHs, such as LTCHs in the same chain or in the same region.)
Consistent with our historical practice of using the best available data, in this final rule, using our established methodology for determining the LTCH statewide average CCRs, based on the most recent complete IPPS “total CCR” data from the March 2019 update of the PSF, as we proposed, we are establishing LTCH PPS statewide average total CCRs for urban and rural hospitals that will be effective for discharges occurring on or after October 1, 2019, through September 30, 2020, in Table 8C listed in section VI. of the Addendum to this final rule (and available via the internet on the CMS website). Consistent with our historical practice, as we also proposed, we used more recent data to determine the LTCH PPS statewide average total CCRs for FY 2020 in this final rule.
Under the current LTCH PPS labor market areas, all areas in Delaware, the District of Columbia, New Jersey, and Rhode Island are classified as urban. Therefore, there are no rural statewide average total CCRs listed for those jurisdictions in Table 8C. This policy is consistent with the policy that we established when we revised our methodology for determining the applicable LTCH statewide average CCRs in the FY 2007 IPPS final rule (71 FR 48119 through 48121) and is the same as the policy applied under the IPPS. In addition, although Connecticut and Nevada have areas that are designated as rural, in our calculation of the LTCH statewide average CCRs, there was no data available from short-term, acute care IPPS hospitals to compute a rural statewide average CCR or there were no short-term, acute care IPPS hospitals or LTCHs located in these areas as of March 2019. Therefore, consistent with our existing methodology, as we proposed, we used the national average total CCR for rural IPPS hospitals for rural Connecticut and Nevada in Table 8C. Furthermore, consistent with our existing methodology, in determining the urban and rural statewide average total CCRs for Maryland LTCHs paid under the LTCH PPS, as we proposed, we are continuing to use, as a proxy, the national average total CCR for urban IPPS hospitals and the national average total CCR for rural IPPS hospitals, respectively. We are using this proxy because we believe that the CCR data in the PSF for Maryland hospitals may not be entirely accurate (as discussed in greater detail in the FY 2007 IPPS final rule (71 FR 48120)).
We did not receive any public comments on our proposals. Therefore, we are finalizing our proposals as described above, without modification.
d. Reconciliation of HCO Payments
Under the HCO policy for cases paid under either payment rate at § 412.525(a)(4)(iv)(D), the payments for HCO cases are subject to reconciliation. Specifically, any such payments are reconciled at settlement based on the CCR that was calculated based on the cost report coinciding with the discharge. For additional information on the reconciliation policy, we refer readers to Sections 150.26 through 150.28 of the Medicare Claims Processing Manual (Pub. 100-4), as added by Change Request 7192 (Transmittal 2111; December 3, 2010), and the RY 2009 LTCH PPS final rule (73 FR 26820 through 26821).
3. High-Cost Outlier Payments for LTCH PPS Standard Federal Payment Rate Cases
a. Changes to High-Cost Outlier Payments for LTCH PPS Standard Federal Payment Rate Cases
Under the regulations at § 412.525(a)(2)(ii) and as required by section 1886(m)(7) of the Act, the fixed-loss amount for HCO payments is set each year so that the estimated aggregate HCO payments for LTCH PPS standard Federal payment rate cases are 99.6875 percent of 8 percent (that is, 7.975 percent) of estimated aggregate LTCH PPS payments for LTCH PPS standard Federal payment rate cases. (For more details on the requirements for high-cost outlier payments in FY 2018 and subsequent years under section 1886(m)(7) of the Act and additional information regarding high-cost outlier payments prior to FY 2018, we refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38542 through 38544).)
b. Fixed-Loss Amount for LTCH PPS Standard Federal Payment Rate Cases for FY 2020
When we implemented the LTCH PPS, we established a fixed-loss amount so that total estimated outlier payments are projected to equal 8 percent of total estimated payments under the LTCH PPS (67 FR 56022 through 56026). When we implemented the dual rate LTCH PPS payment structure beginning in FY 2016, we established that, in general, the historical LTCH PPS HCO policy would continue to apply to LTCH PPS standard Federal payment rate cases. That is, the fixed-loss amount and target for LTCH PPS standard Federal payment rate cases would be determined using the LTCH PPS HCO policy adopted when the LTCH PPS was first implemented, but we limited the data used under that policy to LTCH cases that would have been LTCH PPS standard Federal payment rate cases if the statutory changes had been in effect at the time of those discharges.
To determine the applicable fixed-loss amount for LTCH PPS standard Federal payment rate cases, we estimate outlier payments and total LTCH PPS payments for each LTCH PPS standard Federal payment rate case (or for each case that would have been a LTCH PPS standard Federal payment rate case if the statutory changes had been in effect at the time of the discharge) using claims data from the MedPAR files. In accordance with § 412.525(a)(2)(ii), the applicable fixed-loss amount for LTCH PPS standard Federal payment rate cases results in estimated total outlier payments being projected to be equal to 7.975 percent of projected total LTCH PPS payments for LTCH PPS standard Federal payment rate cases. We use MedPAR claims data and CCRs based on data from the most recent PSF (or from the applicable statewide average CCR if an LTCH's CCR data are faulty or unavailable) to establish an applicable fixed-loss threshold amount for LTCH PPS standard Federal payment rate cases.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19615 through 19616), we proposed to continue to use our current methodology to calculate an applicable fixed-loss amount for LTCH PPS standard Federal payment rate cases for FY 2020 using the best available data that would maintain estimated HCO payments at the projected 7.975 percent of total estimated LTCH PPS payments for LTCH PPS standard Federal payment rate cases (based on the payment rates and policies for these cases presented in the proposed rule).
Specifically, based on the most recent complete LTCH data available at that time (that is, LTCH claims data from the December 2018 update of the FY 2018 MedPAR file and CCRs from the December 2018 update of the PSF), we determined a proposed fixed-loss amount for LTCH PPS standard Federal payment rate cases for FY 2020 of $29,997 that would result in estimated outlier payments projected to be equal to 7.975 percent of estimated FY 2020 payments for such cases. Under this proposal, we proposed to continue to make an additional HCO payment for the cost of an LTCH PPS standard Federal payment rate case that exceeds the HCO threshold amount that is equal to 80 percent of the difference between the estimated cost of the case and the outlier threshold (the sum of the proposed adjusted LTCH PPS standard Federal payment rate payment and the proposed fixed-loss amount for LTCH PPS standard Federal payment rate cases of $29,997).
Consistent with our historical practice of using the best data available, as we proposed, when determining the fixed-loss amount for LTCH PPS standard Federal payment rate cases for FY 2020 in this final rule, we used the most recent available LTCH claims data and CCR data. In this FY 2020 IPPS/LTCH PPS final rule, we are continuing to use our current methodology to calculate an applicable fixed-loss amount for LTCH PPS standard Federal payment rate cases for FY 2020 using the best available data that will maintain estimated HCO payments at the projected 7.975 percent of total estimated LTCH PPS payments for LTCH PPS standard Federal payment rate cases (based on the payment rates and policies for these cases presented in this final rule). Specifically, based on the most recent complete LTCH data available at this time (that is, LTCH claims data from the March 2019 update of the FY 2018 MedPAR file and CCRs from the March 2019 update of the PSF), we determined a fixed-loss amount for LTCH PPS standard Federal payment rate cases for FY 2020 of $26,778 that will result in estimated outlier payments projected to be equal to 7.975 percent of estimated FY 2020 payments for such cases. Under the broad authority of section 123(a)(1) of the BBRA and section 307(b)(1) of the BIPA, we are establishing a fixed-loss amount of $26,778 for LTCH PPS standard Federal payment rate cases for FY 2020. Under this policy, we would continue to make an additional HCO payment for the cost of an LTCH PPS standard Federal payment rate case that exceeds the HCO threshold amount that is equal to 80 percent of the difference between the estimated cost of the case and the outlier threshold (the sum of the adjusted LTCH PPS standard Federal payment rate and the fixed-loss amount for LTCH PPS standard Federal payment rate cases of $26,778).
We note, the fixed-loss amount for FY 2020 for LTCH PPS standard Federal payment rate cases we are establishing in this final rule based on the most recent LTCH claims data from the MedPAR file and the latest CCRs from the PSF, result in a fixed-loss amount for such cases that is lower than the proposed fixed-loss amount. This change is largely attributable to updates to CCRs from the December 2018 update of the PSF to the March 2019 update of the PSF.
4. High-Cost Outlier Payments for Site Neutral Payment Rate Cases
Under § 412.525(a), site neutral payment rate cases receive an additional HCO payment for costs that exceed the HCO threshold that is equal to 80 percent of the difference between the estimated cost of the case and the applicable HCO threshold (80 FR 49618 through 49629). In the following discussion, we note that the statutory transitional payment method for cases that are paid the site neutral payment rate for LTCH discharges occurring in cost reporting periods beginning during FY 2016 through FY 2019 used a blended payment rate, which is determined as 50 percent of the site neutral payment rate amount for the discharge and 50 percent of the LTCH PPS standard Federal payment rate amount for the discharge (§ 412.522(c)(3)). As such, for FY 2020 discharges paid under the transitional payment method, the discussion below pertains only to the site neutral payment rate portion of the blended payment rate under § 412.522(c)(3)(i).
When we implemented the application of the site neutral payment rate in FY 2016, in examining the appropriate fixed-loss amount for site neutral payment rate cases issue, we considered how LTCH discharges based on historical claims data would have been classified under the dual rate LTCH PPS payment structure and the CMS' Office of the Actuary projections regarding how LTCHs will likely respond to our implementation of policies resulting from the statutory payment changes. We again relied on these considerations and actuarial projections in FY 2017 and FY 2018 because the historical claims data available in each of these years were not all subject to the LTCH PPS dual rate payment system. Similarly, for FY 2019, we continued to rely on these considerations and actuarial projections because, due to the transitional blended payment policy for site neutral payment rate cases, FY 2017 claims for these cases were not subject to the full effect of the site neutral payment rate.
For FYs 2016 through 2019, at that time our actuaries projected that the proportion of cases that would qualify as LTCH PPS standard Federal payment rate cases versus site neutral payment rate cases under the statutory provisions would remain consistent with what is reflected in the historical LTCH PPS claims data. Although our actuaries did not project an immediate change in the proportions found in the historical data, they did project cost and resource changes to account for the lower payment rates. Our actuaries also projected that the costs and resource use for cases paid at the site neutral payment rate would likely be lower, on average, than the costs and resource use for cases paid at the LTCH PPS standard Federal payment rate and would likely mirror the costs and resource use for IPPS cases assigned to the same MS-DRG, regardless of whether the proportion of site neutral payment rate cases in the future remains similar to what is found based on the historical data. As discussed in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49619), this actuarial assumption is based on our expectation that site neutral payment rate cases would generally be paid based on an IPPS comparable per diem amount under the statutory LTCH PPS payment changes that began in FY 2016, which, in the majority of cases, is much lower than the payment that would have been paid if these statutory changes were not enacted. In light of these projections and expectations, we discussed that we believed that the use of a single fixed-loss amount and HCO target for all LTCH PPS cases would be problematic. In addition, we discussed that we did not believe that it would be appropriate for comparable LTCH PPS site neutral payment rate cases to receive dramatically different HCO payments from those cases that would be paid under the IPPS (80 FR 49617 through 49619 and 81 FR 57305 through 57307). For those reasons, we stated that we believed that the most appropriate fixed-loss amount for site neutral payment rate cases for FYs 2016 through 2019 would be equal to the IPPS fixed-loss amount for that particular fiscal year. Therefore, we established the fixed-loss amount for site neutral payment rate cases as the corresponding IPPS fixed-loss amounts for FYs 2016 through 2019. In particular, in FY 2019, we established the fixed-loss amount for site neutral payment rate cases as the FY 2019 IPPS fixed-loss amount of $25,743 (as corrected at 83 FR 49845).
As noted earlier, because not all claims in the data used for this FY 2020 IPPS/LTCH PPS final rule were subject to the unblended site neutral payment rate, we continue to rely on the same considerations and actuarial projections used in FYs 2016 through 2019 when developing a fixed-loss amount for site neutral payment rate cases for FY 2020. Our actuaries continue to project that site neutral payment rate cases in FY 2020 will continue to mirror an IPPS case paid under the same MS-DRG. That is, our actuaries continue to project that the costs and resource use for FY 2020 cases paid at the site neutral payment rate would likely be lower, on average, than the costs and resource use for cases paid at the LTCH PPS standard Federal payment rate and will likely mirror the costs and resource use for IPPS cases assigned to the same MS-DRG, regardless of whether the proportion of site neutral payment rate cases in the future remains similar to what was found based on the historical data. (Based on the most recent FY 2018 LTCH claims data used in the development of this FY 2020 IPPS/LTCH PPS final rule, approximately 71 percent of LTCH cases would have been paid the LTCH PPS standard Federal payment rate and approximately 29 percent of LTCH cases would have been paid the site neutral payment rate for discharges occurring in FY 2018.)
For these reasons, we continue to believe that the most appropriate fixed-loss amount for site neutral payment rate cases for FY 2020 is the IPPS fixed-loss amount for FY 2020. Therefore, consistent with past practice, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19617), we proposed that the applicable HCO threshold for site neutral payment rate cases is the sum of the site neutral payment rate for the case and the IPPS fixed-loss amount. That is, we proposed a fixed-loss amount for site neutral payment rate cases of $26,994, which is the same proposed FY 2020 IPPS fixed-loss amount discussed in section II.A.4.j.(1). of the Addendum to the proposed rule. Accordingly, for FY 2020, we proposed to calculate a HCO payment for site neutral payment rate cases with costs that exceed the HCO threshold amount that is equal to 80 percent of the difference between the estimated cost of the case and the outlier threshold (the sum of the site neutral payment rate payment and the proposed fixed-loss amount for site neutral payment rate cases of $26,994).
Comment: Some commenters requested CMS develop an HCO fixed-loss amount and HCO target based on data from site neutral discharges rather than adopting these figures from the IPPS. These commenters allege that the resource use of site neutral payment rate cases are not similar to IPPS cases based on their comparison of factors such as length of stay and average cost. However these commenters did not indicate what the HCO fixed-loss amount and HCO target should be based on data from site neutral discharges. Other commenters generally indicated that their analysis of LTCH claims data since the implementation of the site neutral payment rate shows that site neutral payment rate cases do not mirror similar IPPS cases, but did not specifically comment on the an HCO fixed-loss amount and HCO target for site neutral payment rate cases.
Response: FY 2018 LTCH claims data are currently the best available data, and as noted above, LTCH site neutral payment rate cases discharged during FY 2018 were paid the blended payment rate under the statutory extension of the transitional period. As we explained in the proposed rule (84 FR 19616), since not all of the FY 2018 LTCH claims data were subject to the unblended site neutral payment rate, we continue to rely on the same considerations and actuarial projections used in FYs 2016 through 2019 when developing a fixed-loss amount for site neutral payment rate cases for FY 2020. That is, the expectation that the costs and resource use for FY 2020 cases paid at the site neutral payment rate will likely mirror the costs and resource use for IPPS cases assigned to the same MS-DRG. Moreover, we note that evidence provided by commenters is not inconsistent with our assumptions. Leaving aside the fact that the LTCH site neutral payment rate cases discharged during FY 2018 were paid the blended payment rate under the statutory extension of the transitional period, our actuarial assumptions rests on comparing cases assigned to the same MS-DRG, and the commenters' analysis ignores this distinction by comparing all LTCH site neutral payment rate cases with the subset of IPPS cases having less than 3 days in an ICU.
In addition, the statutory extension of the transitional blended payment rate for site neutral payment rate cases inherently reduces any financial incentives for LTCHs to respond as compared to the full site neutral payment rate. As LTCHs continue to transition to the full site neutral payment rate, it is reasonable to expect that the costs and resource use for cases paid at the site neutral payment rate would likely be lower, on average, than the costs and resource use for cases paid prior to the implementation of the site neutral payment, and would continue to more closely resemble the costs and resource use for IPPS cases assigned to the same MS-DRG. Because of the on-going transition, it is not straightforward to project the costs and resource use for cases paid at the site neutral payment rate based on historical data as we near the end of the transitional period. For these reasons, we continue to believe the most appropriate fixed-loss amount for site neutral payment rate cases would be the IPPS fixed-loss amount.
As we stated when adopted this approach in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49619), to the extent experience under the revised LTCH PPS indicates site neutral payment rate cases differ sufficiently from these expectations, we agree it would be appropriate to revisit in future rulemaking the most appropriate fixed-loss amount used to determine HCO payments for site neutral payment rate cases. We intend to continue to review the most recent available LTCH PPS site neutral claims data. As we approach the end of the statutory transitional period, we will take stakeholders' feedback into consideration and continue to explore in future rulemaking the development of a HCO fixed-loss amount and HCO target for the site neutral payment rate rather than continuing to adopt the IPPS figures, and intend to explore for future rulemaking, perhaps as early as for next year's rule.
After consideration of the public comments received on our proposals to use the FY 2020 IPPS fixed-loss amount and 5.1 percent HCO target for LTCH discharges paid at the site neutral payment rate in FY 2020, we are finalizing these proposals without modification.
Therefore, for FY 2020, as we proposed, we are establishing that the applicable HCO threshold for site neutral payment rate cases is the sum of the site neutral payment rate for the case and the IPPS fixed loss amount. That is, we are establishing a fixed-loss amount for site neutral payment rate cases of $26,473, which is the same FY 2020 IPPS fixed-loss amount discussed in section II.A.4.g.(1). of the Addendum to this final rule. Accordingly, under this policy, for FY 2020, we will calculate a HCO payment for site neutral payment rate cases with costs that exceed the HCO threshold amount, which is equal to 80 percent of the difference between the estimated cost of the case and the outlier threshold (the sum of site neutral payment rate payment and the fixed loss amount for site neutral payment rate cases of $26,473).
In establishing a HCO policy for site neutral payment rate cases, we established a budget neutrality adjustment under § 412.522(c)(2)(i). We established this requirement because we believed, and continue to believe, that the HCO policy for site neutral payment rate cases should be budget neutral, just as the HCO policy for LTCH PPS standard Federal payment rate cases is budget neutral, meaning that estimated site neutral payment rate HCO payments should not result in any change in estimated aggregate LTCH PPS payments.
To ensure that estimated HCO payments payable to site neutral payment rate cases in FY 2020 would not result in any increase in estimated aggregate FY 2020 LTCH PPS payments, under the budget neutrality requirement at § 412.522(c)(2)(i), it is necessary to reduce site neutral payment rate payments (or the portion of the blended payment rate payment for FY 2020 discharges occurring in LTCH cost reporting periods beginning before October 1, 2019) by 5.1 percent to account for the estimated additional HCO payments payable to those cases in FY 2020. In order to achieve this, for FY 2020, in general, we proposed to continue this policy.
As discussed earlier, consistent with the IPPS HCO payment threshold, we estimate our fixed-loss threshold of $26,473 results in HCO payments for site neutral payment rate cases to equal 5.1 percent of the site neutral payment rate payments that are based on the IPPS comparable per diem amount. As such, to ensure estimated HCO payments payable for site neutral payment rate cases in FY 2020 would not result in any increase in estimated aggregate FY 2020 LTCH PPS payments, under the budget neutrality requirement at § 412.522(c)(2)(i), it is necessary to reduce the site neutral payment rate amount paid under § 412.522(c)(1)(i) by 5.1 percent to account for the estimated additional HCO payments payable for site neutral payment rate cases in FY 2020. In order to achieve this, for FY 2020, we proposed to apply a budget neutrality factor of 0.949 (that is, the decimal equivalent of a 5.1 percent reduction, determined as 1.0−5.1/100 = 0.949) to the site neutral payment rate for those site neutral payment rate cases paid under § 412.522(c)(1)(i). We note that, consistent with our current policy, this proposed HCO budget neutrality adjustment would not be applied to the HCO portion of the site neutral payment rate amount (81 FR 57309).
Comment: Some commenters, as they have done since the inception of the site neutral payment rate, objected to the proposed site neutral payment rate HCO budget neutrality adjustment, claiming that it would result in savings to the Medicare program instead of being budget neutral. The commenters' primary objection continued to be based on their belief that, because the IPPS base rates used in the IPPS comparable per diem amount calculation of the site neutral payment rate include a budget neutrality adjustment for IPPS HCO payments (for example, a 5.1 percent adjustment on the operating IPPS standardized amount), an “additional” budget neutrality factor is not necessary and is, in fact, duplicative. Based on their belief that the proposed site neutral payment rate HCO budget neutrality adjustment is duplicative, some commenters recommended that if CMS continues with the application of that budget neutrality adjustment, the calculation of the IPPS comparable per diem amount should be revised to use the IPPS operating standardized amount prior to the application of the IPPS HCO budget neutrality adjustment.
Some commenters indicated that their analysis of LTCH claims data since the implementation of the site neutral payment rate shows that site neutral payment rate cases continue to be “inappropriately underpaid”. These commenters believe the site neutral payment rate HCO budget neutrality adjustment exacerbates the “underpayment”, as well as impacts access to care for Medicare patients that are LTCH site neutral payment rate cases.
Response: We continue to disagree with the commenters that a budget neutrality adjustment for site neutral payment rate HCO payments is unnecessary or duplicative. We have stated such disagreement during each previous rulemaking cycle. We refer readers to 83 FR 41737 through 41738, 82 FR 38545 through 38546, 81 FR 57308 through 57309, and 80 FR 49621 through 49622 for more information on our responses to these comments. As we stated in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49621 through 49622), while the commenters are correct that the IPPS base rates that are used in site neutral payment rate calculation include a budget neutrality adjustment for IPPS HCO payments, that adjustment is merely a part of the calculation of one of the inputs (that is, the IPPS base rates) that are used in the LTCH PPS computation of site neutral payment rate. The purpose of the HCO budget neutrality factor that is applied in determining the IPPS base rates is to ensure that estimated HCO payments made under the IPPS do not increase aggregate IPPS payments in a given year. As such, the HCO budget neutrality factor that is applied to the IPPS base rates does not account for the additional HCO payments under the LTCH PPS that will be made to LTCH site neutral payment rate cases. Without a budget neutrality adjustment when determining payment for a case under the LTCH PPS, any HCO payments to site neutral payment rate cases would increase aggregate LTCH PPS payments above the level of expenditure if there were no HCO payments for site neutral payment rate cases.
The fact that the budget neutrality factor for site neutral payment rate HCO payments and the outlier budget neutrality adjustment factor on the operating IPPS standardized amount are both set at the same outlier target percentage, that is, 5.1 percent, does not demonstrate the commenters' repeated assertions that the budget neutrality factor for site neutral payment rate HCO payments is duplicative. As we have explained since the implementation of the site neutral payment rate and above, we adopted the same percentage as is used under the IPPS due to our projection that costs and resource use of site neutral payment rate cases would likely mirror similar IPPS cases. (We discuss this projection in greater detail earlier in this section.) We also stated that, in the future, we will continue to explore in subsequent rulemaking the most appropriate fixed-loss amount, and thereby the outlier target percentage, used to determine LTCH PPS HCO payments for site neutral payment rate cases. The fact that the two outlier target percentages and the corresponding HCO budget neutrality factors (that is, the one under the operating IPPS and the one under the LTCH PPS for site neutral payment rate cases) do not necessarily have to match underscores that they serve to maintain budget neutrality in two distinct payment systems.
The methodology for calculating the “IPPS comparable per diem amount” under § 412.529(d)(4) had been already established by CMS at the time section 1886(m)(6)(B)(ii) of the Act, which defines the site neutral payment rate, was enacted, as that regulation has been used under the LTCH PPS since 2006 as a component in the calculation of short-stay outlier payments. The regulation at § 412.529(d)(4)(A) specifies that the “IPPS comparable per diem amount” is calculated by summing the applicable operating IPPS standardized amount and the capital IPPS Federal rate in effect at the time of the LTCH discharge. Both the IPPS standardized amount and the capital IPPS Federal rate are calculated by applying, among other adjustments, a budget neutrality factor to adjust for estimated outlier payments under the operating IPPS and capital IPPS, respectively. In other words, the statute requires the calculation of site neutral payment rate payments using defined amounts that already incorporate an IPPS outlier budget neutrality adjustment. Furthermore, since the implementation of the LTCH PPS, CMS has made a budget neutrality adjustment for estimated high cost outlier payments under the LTCH PPS (applied to the standard Federal rate) every year, by applying a reduction factor based on the estimated proportion of outlier payments under the LTCH PPS which are paid that rate. Given CMS's longstanding practice of budget neutralizing outlier payments throughout the various Medicare payment systems, including within the LTCH PPS, it is reasonable to expect when the site neutral payment rate was implemented, high cost outlier payments to cases paid at the site neutral payment rate would also be made in a budget neutral manner in the absence of any directive to the contrary.
For these reasons, we continue to disagree with the commenters that a budget neutrality adjustment for site neutral payment rate HCO payments is unnecessary or duplicative, and we are, again, not adopting the commenters' recommendation to change the calculation of the IPPS comparable amount by adjusting the IPPS operating standardized amount used in that calculation to account for the application of the IPPS HCO budget neutrality adjustment.
While commenters' analysis of LTCH claims data since the implementation of the site neutral payment rate may show that site neutral payment rate cases are typically paid less than the estimated cost, we disagree with the characterization that this results in an “underpayment”. The statute requires that LTCH cases that do not meet the statutory patient criteria be paid the site neutral payment rate, and as discussed previously, the statute specifies the calculation of that site neutral payment rate. CMS's implementation of the site neutral payment rate is consistent with the statutory requirements at section 1886(m)(6) of the Act, and therefore, Medicare's payment for those cases is not inappropriate.
While we understand and share commenters' concerns about access to and quality of care for Medicare beneficiaries, including those that are site neutral payment rate cases, as we have stated in the past, we believe the site neutral payment rate will not negatively impact access to or quality of care. As demonstrated in areas where there is little or no LTCH presence, general short-term acute care hospitals are effectively providing treatment for the same types of patients that are treated in LTCHs in areas where there is one or more LTCH present (82 FR 38754 through 38575). We further note, LTCHs must meet Medicare conditions of participation as general acute care hospitals.
After consideration of public comments, for the reasons discussed above, we disagree with commenters that the site neutral payment rate case HCO budget neutrality factor is not necessary and duplicative or inappropriately reduces payments or Medicare patients' access to care, and we are, adopting our proposed site neutral payment rate HCO budget neutrality adjustment as final without modification.
In order to achieve this, for FY 2020, as we proposed, we are applying a budget neutrality factor of 0.949 (that is, the decimal equivalent of a 5.1 percent reduction, determined as 1.0−5.1/100 = 0.949) to the site neutral payment rate for those site neutral payment rate cases paid under § 412.522(c)(1)(i). We note that, consistent with our current policy, as proposed, this HCO budget neutrality adjustment will not apply to the HCO portion of the site neutral payment rate amount.
E. Update to the IPPS Comparable Amount To Reflect the Statutory Changes to the IPPS DSH Payment Adjustment Methodology
In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50766), we established a policy to reflect the changes to the Medicare IPPS DSH payment adjustment methodology made by section 3133 of the Affordable Care Act in the calculation of the “IPPS comparable amount” under the SSO policy at § 412.529 and the “IPPS equivalent amount” under the site neutral payment rate at § 412.522. Historically, the determination of both the “IPPS comparable amount” and the “IPPS equivalent amount” includes an amount for inpatient operating costs “for the costs of serving a disproportionate share of low-income patients.” Under the statutory changes to the Medicare DSH payment adjustment methodology that began in FY 2014, in general, eligible IPPS hospitals receive an empirically justified Medicare DSH payment equal to 25 percent of the amount they otherwise would have received under the statutory formula for Medicare DSH payments prior to the amendments made by the Affordable Care Act. The remaining amount, equal to an estimate of 75 percent of the amount that otherwise would have been paid as Medicare DSH payments, reduced to reflect changes in the percentage of individuals who are uninsured and any additional statutory adjustment, is made available to make additional payments to each hospital that qualifies for Medicare DSH payments and that has uncompensated care. The additional uncompensated care payments are based on the hospital's amount of uncompensated care for a given time period relative to the total amount of uncompensated care for that same time period reported by all IPPS hospitals that receive Medicare DSH payments.
To reflect the statutory changes to the Medicare DSH payment adjustment methodology in the calculation of the “IPPS comparable amount” and the “IPPS equivalent amount” under the LTCH PPS, we stated that we will include a reduced Medicare DSH payment amount that reflects the projected percentage of the payment amount calculated based on the statutory Medicare DSH payment formula prior to the amendments made by the Affordable Care Act that will be paid to eligible IPPS hospitals as empirically justified Medicare DSH payments and uncompensated care payments in that year (that is, a percentage of the operating Medicare DSH payment amount that has historically been reflected in the LTCH PPS payments that are based on IPPS rates). We also stated that the projected percentage will be updated annually, consistent with the annual determination of the amount of uncompensated care payments that will be made to eligible IPPS hospitals. We believe that this approach results in appropriate payments under the LTCH PPS and is consistent with our intention that the “IPPS comparable amount” and the “IPPS equivalent amount” under the LTCH PPS closely resemble what an IPPS payment would have been for the same episode of care, while recognizing that some features of the IPPS cannot be translated directly into the LTCH PPS (79 FR 50766 through 50767).
For FY 2020, as discussed in greater detail in the FY 2020 IPPS/LTCH PPS proposed rule and in section IV.F.3. of the preamble of this final rule, based on the most recent data available, our estimate of 75 percent of the amount that would otherwise have been paid as Medicare DSH payments (under the methodology outlined in section 1886(r)(2) of the Act) is adjusted to 67.14 percent of that amount to reflect the change in the percentage of individuals who are uninsured. The resulting amount is then used to determine the amount available to make uncompensated care payments to eligible IPPS hospitals in FY 2020. In other words, the amount of the Medicare DSH payments that would have been made prior to the amendments made by the Affordable Care Act is adjusted to 50.36 percent (the product of 75 percent and 67.14 percent) and the resulting amount is used to calculate the uncompensated care payments to eligible hospitals. As a result, for FY 2020, we projected that the reduction in the amount of Medicare DSH payments pursuant to section 1886(r)(1) of the Act, along with the payments for uncompensated care under section 1886(r)(2) of the Act, will result in overall Medicare DSH payments of 75.36 percent of the amount of Medicare DSH payments that would otherwise have been made in the absence of the amendments made by the Affordable Care Act (that is, 25 percent + 50.36 percent = 75.36 percent).
Therefore, for FY 2020, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to establish that the calculation of the “IPPS comparable amount” under § 412.529 would include an applicable operating Medicare DSH payment amount that is equal to 75.36 percent of the operating Medicare DSH payment amount that would have been paid based on the statutory Medicare DSH payment formula absent the amendments made by the Affordable Care Act. Furthermore, consistent with our historical practice, we proposed that, if more recent data became available, we would use that data to determine this factor in this final rule.
We did not receive any public comments in response to our proposal. In addition, there are no more recent data available to use that would affect the calculations determined in the proposed rule. Therefore, we are finalizing our proposal that, for FY 2020, the calculation of the “IPPS comparable amount” under § 412.529 includes an applicable operating Medicare DSH payment amount that is equal to 75.36 percent of the operating Medicare DSH payment amount that would have been paid based on the statutory Medicare DSH payment formula absent the amendments made by the Affordable Care Act.
F. Computing the Adjusted LTCH PPS Federal Prospective Payments for FY 2020
Section 412.525 sets forth the adjustments to the LTCH PPS standard Federal payment rate. Under the dual rate LTCH PPS payment structure, only LTCH PPS cases that meet the statutory criteria to be excluded from the site neutral payment rate are paid based on the LTCH PPS standard Federal payment rate. Under § 412.525(c), the LTCH PPS standard Federal payment rate is adjusted to account for differences in area wages by multiplying the labor-related share of the LTCH PPS standard Federal payment rate for a case by the applicable LTCH PPS wage index (the FY 2020 values are shown in Tables 12A through 12B listed in section VI. of the Addendum to this final rule and are available via the internet on the CMS website). The LTCH PPS standard Federal payment rate is also adjusted to account for the higher costs of LTCHs located in Alaska and Hawaii by the applicable COLA factors (the FY 2020 factors are shown in the chart in section V.C. of this Addendum) in accordance with § 412.525(b). In this final rule, we are establishing an LTCH PPS standard Federal payment rate for FY 2020 of $42,677.64, as discussed in section V.A. of the Addendum to this final rule. We illustrate the methodology to adjust the LTCH PPS standard Federal payment rate for FY 2020 in the following example:
Example:
During FY 2020, a Medicare discharge that meets the criteria to be excluded from the site neutral payment rate, that is, an LTCH PPS standard Federal payment rate case, is from an LTCH that is located in Chicago, Illinois (CBSA 16974). The FY 2020 LTCH PPS wage index value for CBSA 16974 is 1.0405 (obtained from Table 12A listed in section VI. of the Addendum to this final rule and available via the internet on the CMS website). The Medicare patient case is classified into MS-LTC-DRG 189 (Pulmonary Edema & Respiratory Failure), which has a relative weight for FY 2020 of 0.9616 (obtained from Table 11 listed in section VI. of the Addendum to this final rule and available via the internet on the CMS website). The LTCH submitted quality reporting data for FY 2020 in accordance with the LTCH QRP under section 1886(m)(5) of the Act.
To calculate the LTCH's total adjusted Federal prospective payment for this Medicare patient case in FY 2020, we computed the wage-adjusted Federal prospective payment amount by multiplying the unadjusted FY 2020 LTCH PPS standard Federal payment rate ($42,677.64) by the labor-related share (66.3 percent) and the wage index value (1.0405). This wage-adjusted amount was then added to the nonlabor-related portion of the unadjusted LTCH PPS standard Federal payment rate (33.7 percent; adjusted for cost of living, if applicable) to determine the adjusted LTCH PPS standard Federal payment rate, which is then multiplied by the MS-LTC-DRG relative weight (0.9616) to calculate the total adjusted LTCH PPS standard Federal prospective payment for FY 2020 ($42,140.77). The table below illustrates the components of the calculations in this example.

VI. Tables Referenced in This Final Rule Generally Available Through the Internet on the CMS Website
This section lists the tables referred to throughout the preamble of this FY 2020 IPPS/LTCH PPS final rule and in the Addendum. In the past, a majority of these tables were published in the Federal Register as part of the annual proposed and final rules. However, similar to FYs 2012 through 2019, for the FY 2020 rulemaking cycle, the IPPS and LTCH PPS tables will not be published in the Federal Register in the annual IPPS/LTCH PPS proposed and final rules and will be available through the internet. Specifically, all IPPS tables listed below, with the exception of IPPS Tables 1A, 1B, 1C, and 1D, and LTCH PPS Table 1E, will generally be available through the internet. IPPS Tables 1A, 1B, 1C, and 1D, and LTCH PPS Table 1E are displayed at the end of this section and will continue to be published in the Federal Register as part of the annual proposed and final rules. For additional discussion of the information included in the IPPS and LTCH PPS tables associated with the IPPS/LTCH PPS proposed and final rules, as well as prior changes to the information included in these tables, we refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41739 through 41740).
In addition, under the HAC Reduction Program, established by section 3008 of the Affordable Care Act, a hospital's total payment may be reduced by 1 percent if it is in the lowest HAC performance quartile. The hospital-level data for the FY 2020 HAC Reduction Program will be made publicly available once it has undergone the review and corrections process.
As discussed in section IV.G. of the preamble of this final rule, the fiscal year readmissions payment adjustment factors, which are typically included in Table 15 of the rules, are not available at this time because hospitals have not yet had the opportunity to review and correct the data (program calculations based on the FY 2020 applicable period of July 1, 2015 to June 30, 2018) before the data are made public under our policy regarding the reporting of hospital-specific data. After hospitals have been given an opportunity to review and correct their calculations for FY 2020, we will post Table 15 (which will be available via the internet on the CMS website) to display the final FY 2020 readmissions payment adjustment factors that will be applicable to discharges occurring on or after October 1, 2019. We expect Table 15 will be posted on the CMS website in the fall of 2019.
Readers who experience any problems accessing any of the tables that are posted on the CMS websites identified below should contact Michael Treitel at (410) 786-4552.
The following IPPS tables for this final rule are generally available through the internet on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. Click on the link on the left side of the screen titled, “FY 2020 IPPS Final Rule Home Page” or “Acute Inpatient—Files for Download.”
Table 2.—Case-Mix Index and Wage Index Table by CCN—FY 2020
Table 3.—Wage Index Table by CBSA—FY 2020
Table 4.—List of Counties Eligible for the Out-Migration Adjustment under Section 1886(d)(13) of the Act—FY 2020
Table 5.—List of Medicare Severity Diagnosis-Related Groups (MS-DRGs), Relative Weighting Factors, and Geometric and Arithmetic Mean Length of Stay—FY 2020
Table 6A.—New Diagnosis Codes—FY 2020
Table 6B.—New Procedure Codes—FY 2020
Table 6C.—Invalid Diagnosis Codes—FY 2020
Table 6D.—Invalid Procedure Codes—FY 2020
Table 6E.—Revised Diagnosis Code Titles—FY 2020
Table 6F.—Revised Procedure Code Titles—FY 2020
Table 6G.1.—Secondary Diagnosis Order Additions to the CC Exclusions List—FY 2020
Table 6G.2.—Principal Diagnosis Order Additions to the CC Exclusions List—FY 2020
Table 6H.1.—Secondary Diagnosis Order Deletions to the CC Exclusions List—FY 2020
Table 6H.2.—Principal Diagnosis Order Deletions to the CC Exclusions List—FY 2020
Table 6I.—Complete MCC List—FY 2020
Table 6I.1.—Additions to the MCC List—FY 2020
Table 6I.2.—Deletions to the MCC List—FY 2020
Table 6J.—Complete CC List—FY 2020
Table 6J.1.—Additions to the CC List—FY 2020
Table 6J.2.—Deletions to the CC List—FY 2020
Table 6K.—Complete List of CC Exclusions —FY 2020
Table 6P.— ICD-10-PCS Codes for MS-DRG Changes—FY 2020 (Table 6P contains tables, 6P.1a. and 6P.1b., that include the ICD-10-PCS code lists relating to specific MS-DRG changes. These tables are referred to throughout section II.F. of the preamble of this final rule.)
Table 7A.—Medicare Prospective Payment System Selected Percentile Lengths of Stay: FY 2018 MedPAR Update—March 2019 GROUPER Version 36 MS-DRGs
Table 7B.—Medicare Prospective Payment System Selected Percentile Lengths of Stay: FY 2018 MedPAR Update—March 2019 GROUPER Version 37 MS-DRGs
Table 8A.—FY 2020 Statewide Average Operating Cost-to-Charge Ratios (CCRs) for Acute Care Hospitals (Urban and Rural)
Table 8B.—FY 2020 Statewide Average Capital Cost-to-Charge Ratios (CCRs) for Acute Care Hospitals
Table 16A.—Updated Proxy Hospital Value-Based Purchasing (VBP) Program Adjustment Factors for FY 2020
Table 18.—FY 2020 Medicare DSH Uncompensated Care Payment Factor 3
The following LTCH PPS tables for this FY 2020 final rule are available through the internet on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/LongTermCareHospitalPPS/index.html under the list item for Regulation Number CMS-1716-F:
Table 8C.—FY 2020 Statewide Average Total Cost-to-Charge Ratios (CCRs) for LTCHs (Urban and Rural)
Table 11.—MS-LTC-DRGs, Relative Weights, Geometric Average Length of Stay, and Short-Stay Outlier (SSO) Threshold for LTCH PPS Discharges Occurring from October 1, 2019 through September 30, 2020
Table 12A.—LTCH PPS Wage Index for Urban Areas for Discharges Occurring from October 1, 2019 through September 30, 2020
Table 12B.—LTCH PPS Wage Index for Rural Areas for Discharges Occurring from October 1, 2019 through September 30, 2020





Appendix A: Economic Analyses
I. Regulatory Impact Analysis
A. Statement of Need
This final rule is necessary in order to make payment and policy changes under the Medicare IPPS for Medicare acute care hospital inpatient services for operating and capital-related costs as well as for certain hospitals and hospital units excluded from the IPPS. This final rule also is necessary to make payment and policy changes for Medicare hospitals under the LTCH PPS. Also, as we note below, the primary objective of the IPPS and the LTCH PPS is to create incentives for hospitals to operate efficiently and minimize unnecessary costs, while at the same time ensuring that payments are sufficient to adequately compensate hospitals for their legitimate costs in delivering necessary care to Medicare beneficiaries. In addition, we share national goals of preserving the Medicare Hospital Insurance Trust Fund.
We believe that the changes in this final rule, such as the updates to the IPPS and LTCH PPS rates, are needed to further each of these goals while maintaining the financial viability of the hospital industry and ensuring access to high quality health care for Medicare beneficiaries. We expect that these changes will ensure that the outcomes of the prospective payment systems are reasonable and equitable, while avoiding or minimizing unintended adverse consequences.
B. Overall Impact
We have examined the impacts of this final rule as required by Executive Order 12866 on Regulatory Planning and Review (September 30, 1993), Executive Order 13563 on Improving Regulation and Regulatory Review (January 18, 2011), the Regulatory Flexibility Act (RFA) (September 19, 1980, Pub. L. 96-354), section 1102(b) of the Social Security Act, section 202 of the Unfunded Mandates Reform Act of 1995 (March 22, 1995; Pub. L. 104-4), Executive Order 13132 on Federalism (August 4, 1999), the Congressional Review Act (5 U.S.C. 804(2), and Executive Order 13771 on Reducing Regulation and Controlling Regulatory Costs (January 30, 2017).
Executive Orders 12866 and 13563 direct agencies to assess all costs and benefits of available regulatory alternatives and, if regulation is necessary, to select regulatory approaches that maximize net benefits (including potential economic, environmental, public health and safety effects, distributive impacts, and equity). Section 3(f) of Executive Order 12866 defines a “significant regulatory action” as an action that is likely to result in a rule: (1) Having an annual effect on the economy of $100 million or more in any 1 year, or adversely and materially affecting a sector of the economy, productivity, competition, jobs, the environment, public health or safety, or State, local or tribal governments or communities (also referred to as “economically significant”); (2) creating a serious inconsistency or otherwise interfering with an action taken or planned by another agency; (3) materially altering the budgetary impacts of entitlement grants, user fees, or loan programs or the rights and obligations of recipients thereof; or (4) raising novel legal or policy issues arising out of legal mandates, the President's priorities, or the principles set forth in the Executive Order.
We have determined that this final rule is a major rule as defined in 5 U.S.C. 804(2). We estimate that the changes for FY 2020 acute care hospital operating and capital payments will redistribute amounts in excess of $100 million to acute care hospitals. The applicable percentage increase to the IPPS rates required by the statute, in conjunction with other payment changes in this final rule, will result in an estimated $3.9 billion increase in FY 2020 payments, primarily driven by a combined $3.5 billion increase in FY 2020 operating payments and uncompensated care payments, and a net increase of $0.4 billion primarily resulting from estimated changes in FY 2020 capital payments and new technology add-on payments. These changes are relative to payments made in FY 2019. The impact analysis of the capital payments can be found in section I.I. of this Appendix. In addition, as described in section I.J. of this Appendix, LTCHs are expected to experience an increase in payments by $43 million in FY 2020 relative to FY 2019.
Our operating impact estimate includes the 0.5 percentage point adjustment required under section 414 of the MACRA applied to the IPPS standardized amount, as discussed in section II.D. of the preamble of this final rule. In addition, our operating payment impact estimate includes the 2.6 percent hospital update to the standardized amount (which includes the estimated 3.0 percent market basket update less the 0.4 percentage point for the multifactor productivity (MFP) adjustment). The estimates of IPPS operating payments to acute care hospitals do not reflect any changes in hospital admissions or real case-mix intensity, which will also affect overall payment changes.
The analysis in this Appendix, in conjunction with the remainder of this document, demonstrates that this final rule is consistent with the regulatory philosophy and principles identified in Executive Orders 12866 and 13563, the RFA, and section 1102(b) of the Act. This final rule will affect payments to a substantial number of small rural hospitals, as well as other classes of hospitals, and the effects on some hospitals may be significant. Finally, in accordance with the provisions of Executive Order 12866, the Executive Office of Management and Budget has reviewed this final rule.
C. Objectives of the IPPS and the LTCH PPS
The primary objective of the IPPS and the LTCH PPS is to create incentives for hospitals to operate efficiently and minimize unnecessary costs, while at the same time ensuring that payments are sufficient to adequately compensate hospitals for their legitimate costs in delivering necessary care to Medicare beneficiaries. In addition, we share national goals of preserving the Medicare Hospital Insurance Trust Fund.
We believe that the changes in this final rule will further each of these goals while maintaining the financial viability of the hospital industry and ensuring access to high quality health care for Medicare beneficiaries. We expect that these changes will ensure that the outcomes of the prospective payment systems are reasonable and equitable, while avoiding or minimizing unintended adverse consequences.
Because this final rule contains a range of policies, we refer readers to the section of the final rule where each policy is discussed. These sections include the rationale for our decisions, including the need for the policy.
D. Limitations of Our Analysis
The following quantitative analysis presents the projected effects of our policy changes, as well as statutory changes effective for FY 2020, on various hospital groups. We estimate the effects of individual policy changes by estimating payments per case, while holding all other payment policies constant. We use the best data available, but, generally unless specifically indicated, we do not attempt to make adjustments for future changes in such variables as admissions, lengths of stay, case-mix, changes to the Medicare population, or incentives. In addition, we discuss limitations of our analysis for specific policies in the discussion of those policies as needed.
E. Hospitals Included in and Excluded From the IPPS
The prospective payment systems for hospital inpatient operating and capital-related costs of acute care hospitals encompass most general short-term, acute care hospitals that participate in the Medicare program. There were 29 Indian Health Service hospitals in our database, which we excluded from the analysis due to the special characteristics of the prospective payment methodology for these hospitals. Among other short-term, acute care hospitals, hospitals in Maryland are paid in accordance with the Maryland Total Cost of Care Model, and hospitals located outside the 50 States, the District of Columbia, and Puerto Rico (that is, 6 short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa) receive payment for inpatient hospital services they furnish on the basis of reasonable costs, subject to a rate-of-increase ceiling.
As of July 2019, there were 3,239 IPPS acute care hospitals included in our analysis. This represents approximately 54 percent of all Medicare-participating hospitals. The majority of this impact analysis focuses on this set of hospitals. There also are approximately 1,406 CAHs. These small, limited service hospitals are paid on the basis of reasonable costs, rather than under the IPPS. IPPS-excluded hospitals and units, which are paid under separate payment systems, include IPFs, IRFs, LTCHs, RNHCIs, children's hospitals, 11 cancer hospitals, 1 extended neoplastic disease care hospital, and 6 short-term acute care hospitals located in the Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa. Changes in the prospective payment systems for IPFs and IRFs are made through separate rulemaking. Payment impacts of changes to the prospective payment systems for these IPPS-excluded hospitals and units are not included in this final rule. The impact of the update and policy changes to the LTCH PPS for FY 2020 is discussed in section I.J. of this Appendix.
F. Effects on Hospitals and Hospital Units Excluded From the IPPS
As of July 2019, there were 97 children's hospitals, 11 cancer hospitals, 6 short-term acute care hospitals located in the Virgin Islands, Guam, the Northern Mariana Islands and American Samoa, 1 extended neoplastic disease care hospital, and 16 RNHCIs being paid on a reasonable cost basis subject to the rate-of-increase ceiling under § 413.40. (In accordance with § 403.752(a) of the regulation, RNHCIs are paid under § 413.40.) Among the remaining providers, 289 rehabilitation hospitals and 833 rehabilitation units, and approximately 384 LTCHs, are paid the Federal prospective per discharge rate under the IRF PPS and the LTCH PPS, respectively, and 543 psychiatric hospitals and 1,038 psychiatric units are paid the Federal per diem amount under the IPF PPS. As stated previously, IRFs and IPFs are not affected by the rate updates discussed in this final rule. The impacts of the changes on LTCHs are discussed in section I.J. of this Appendix.
For children's hospitals, the 11 cancer hospitals, the 6 short-term acute care hospitals located in the Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa, the 1 extended neoplastic disease care hospital, and RNHCIs, the update of the rate-of-increase limit (or target amount) is the estimated FY 2020 percentage increase in the 2014-based IPPS operating market basket, consistent with section 1886(b)(3)(B)(ii) of the Act, and §§ 403.752(a) and 413.40 of the regulations. Consistent with current law, based on IGI's second quarter 2019 forecast of the 2014-based IPPS market basket increase, we are estimating the FY 2020 update to be 3.0 percent (that is, the estimate of the market basket rate-of-increase). We used the most recent data available for this final rule to calculate the IPPS operating market basket update for FY 2020. However, the Affordable Care Act requires a reduction for the multifactor productivity adjustment (0.4 percentage point for FY 2020), resulting in a 2.6 percent applicable percentage increase for IPPS hospitals that submit quality data and are meaningful EHR users, as discussed in section IV.B. of the preamble of this final rule. Children's hospitals, the 11 cancer hospitals, the 6 short-term acute care hospitals located in the Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa, the 1 extended neoplastic disease care hospital, and RNHCIs that continue to be paid based on reasonable costs subject to rate-of-increase limits under § 413.40 of the regulations are not subject to the reductions in the applicable percentage increase required under the Affordable Care Act. Therefore, for those hospitals paid under § 413.40 of the regulations, the update is the percentage increase in the 2014-based IPPS operating market basket for FY 2020, estimated at 3.0 percent.
The impact of the update in the rate-of-increase limit on those excluded hospitals depends on the cumulative cost increases experienced by each excluded hospital since its applicable base period. For excluded hospitals that have maintained their cost increases at a level below the rate-of-increase limits since their base period, the major effect is on the level of incentive payments these excluded hospitals receive. Conversely, for excluded hospitals with cost increases above the cumulative update in their rate-of-increase limits, the major effect is the amount of excess costs that would not be paid.
We note that, under § 413.40(d)(3), an excluded hospital that continues to be paid under the TEFRA system and whose costs exceed 110 percent of its rate-of-increase limit receives its rate-of-increase limit plus the lesser of: (1) 50 percent of its reasonable costs in excess of 110 percent of the limit; or (2) 10 percent of its limit. In addition, under the various provisions set forth in § 413.40, hospitals can obtain payment adjustments for justifiable increases in operating costs that exceed the limit.
G. Quantitative Effects of the Policy Changes Under the IPPS for Operating Costs
1. Basis and Methodology of Estimates
In this final rule, we are announcing policy changes and payment rate updates for the IPPS for FY 2020 for operating costs of acute care hospitals. The FY 2020 updates to the capital payments to acute care hospitals are discussed in section I.I. of this Appendix.
Based on the overall percentage change in payments per case estimated using our payment simulation model, we estimate that total FY 2020 operating payments will increase by 2.9 percent, compared to FY 2019. In addition to the applicable percentage increase, this amount reflects the +0.5 percentage point permanent adjustment to the standardized amount required under section 414 of MACRA. The impacts do not reflect changes in the number of hospital admissions or real case-mix intensity, which will also affect overall payment changes.
We have prepared separate impact analyses of the changes to each system. This section deals with the changes to the operating inpatient prospective payment system for acute care hospitals. Our payment simulation model relies on the most recent available claims data to enable us to estimate the impacts on payments per case of certain changes in this final rule. However, there are other changes for which we do not have data available that would allow us to estimate the payment impacts using this model. For those changes, we have attempted to predict the payment impacts based upon our experience and other more limited data.
The data used in developing the quantitative analyses of changes in payments per case presented in this section are taken from the FY 2018 MedPAR file and the most current Provider-Specific File (PSF) that are used for payment purposes. Although the analyses of the changes to the operating PPS do not incorporate cost data, data from the most recently available hospital cost reports were used to categorize hospitals. Our analysis has several qualifications. First, in this analysis, we do not make adjustments for future changes in such variables as admissions, lengths of stay, or underlying growth in real case-mix. Second, due to the interdependent nature of the IPPS payment components, it is very difficult to precisely quantify the impact associated with each change. Third, we use various data sources to categorize hospitals in the tables. In some cases, particularly the number of beds, there is a fair degree of variation in the data from the different sources. We have attempted to construct these variables with the best available source overall. However, for individual hospitals, some miscategorizations are possible.
Using cases from the FY 2018 MedPAR file, we simulate payments under the operating IPPS given various combinations of payment parameters. As described previously, Indian Health Service hospitals and hospitals in Maryland were excluded from the simulations. The impact of the payments under the capital IPPS, and the impact of the payments for costs other than inpatient operating costs, are not analyzed in this section. Estimated payment impacts of the capital IPPS for FY 2020 are discussed in section I.I. of this Appendix.
We discuss the following changes:
- The effects of the application of the applicable percentage increase of 2.6 percent (that is, a 3.0 percent market basket update with a reduction of 0.4 percentage point for the multifactor productivity adjustment), and a 0.5 percentage point adjustment required under section 414 of the MACRA to the IPPS standardized amount, and the applicable percentage increase (including the market basket update and the multifactor productivity adjustment) to the hospital-specific rates.
- The effects of the changes to the relative weights and MS-DRG GROUPER.
- The effects of the changes in hospitals' wage index values reflecting updated wage data from hospitals' cost reporting periods beginning during FY 2016, compared to the FY 2015 wage data, to calculate the FY 2020 wage index.
- The effects of the geographic reclassifications by the MGCRB (as of publication of this final rule) that will be effective for FY 2020.
- The effects of the rural floor with the application of the national budget neutrality factor to the wage index and the policy to calculate the FY 2020 rural floor without including the wage data of hospitals that have reclassified as rural under § 412.103.
- The effects of the frontier State wage index adjustment under the statutory provision that requires hospitals located in States that qualify as frontier States to not have a wage index less than 1.0. This provision is not budget neutral.
- The effects of the implementation of section 1886(d)(13) of the Act, as added by section 505 of Public Law 108-173, which provides for an increase in a hospital's wage index if a threshold percentage of residents of the county where the hospital is located commute to work at hospitals in counties with higher wage indexes for FY 2020. This provision is not budget neutral.
- The effects of the policies to increase the wage index for hospitals with wage index values below the 25th percentile wage index value (that is, the lowest quartile wage index adjustment), the transition policy in FY 2020 pursuant to which a 5-percent cap will be placed on any decrease in a hospital's wage index compared to its final FY 2019 wage index value (that is, the 5-percent cap), and the associated budget neutrality adjustments.
- The total estimated change in payments based on the FY 2020 policies relative to payments based on FY 2019 policies, including estimated changes in outlier payments.
To illustrate the impact of the FY 2020 changes, our analysis begins with a FY 2019 baseline simulation model using: The FY 2019 applicable percentage increase of 1.35 percent; the 0.5 percentage point adjustment required under section 414 of the MACRA applied to the IPPS standardized amount; the FY 2019 MS-DRG GROUPER (Version 36); the FY 2019 CBSA designations for hospitals based on the OMB definitions from the 2010 Census; the FY 2019 wage index; and no MGCRB reclassifications. Outlier payments are set at 5.1 percent of total operating MS-DRG and outlier payments for modeling purposes.
Section 1886(b)(3)(B)(viii) of the Act, as added by section 5001(a) of Public Law 109-171, as amended by section 4102(b)(1)(A) of the ARRA (Pub. L. 111-5) and by section 3401(a)(2) of the Affordable Care Act (Pub. L. 111-148), provides that, for FY 2007 and each subsequent year through FY 2014, the update factor will include a reduction of 2.0 percentage points for any subsection (d) hospital that does not submit data on measures in a form and manner, and at a time specified by the Secretary. Beginning in FY 2015, the reduction is one-quarter of such applicable percentage increase determined without regard to section 1886(b)(3)(B)(ix), (xi), or (xii) of the Act, or one-quarter of the market basket update. Therefore, for FY 2020, hospitals that do not submit quality information under rules established by the Secretary and that are meaningful EHR users under section 1886(b)(3)(B)(ix) of the Act will receive an applicable percentage increase of 1.85 percent. At the time this impact was prepared, 41 hospitals are estimated to not receive the full market basket rate-of-increase for FY 2020 because they failed the quality data submission process or did not choose to participate, but are meaningful EHR users. For purposes of the simulations shown later in this section, we modeled the payment changes for FY 2020 using a reduced update for these hospitals.
For FY 2020, in accordance with section 1886(b)(3)(B)(ix) of the Act, a hospital that has been identified as not a meaningful EHR user will be subject to a reduction of three-quarters of such applicable percentage increase determined without regard to section 1886(b)(3)(B)(ix), (xi), or (xii) of the Act. Therefore, for FY 2020, hospitals that are identified as not being meaningful EHR users and do submit quality information under section 1886(b)(3)(B)(viii) of the Act will receive an applicable percentage increase of 0.35 percent. At the time this impact analysis was prepared, 167 hospitals are estimated to not receive the full market basket rate-of-increase for FY 2020 because they are identified as not meaningful EHR users that do submit quality information under section 1886(b)(3)(B)(viii) of the Act. For purposes of the simulations shown in this section, we modeled the payment changes for FY 2020 using a reduced update for these hospitals.
Hospitals that are identified as not meaningful EHR users under section 1886(b)(3)(B)(ix) of the Act and also do not submit quality data under section 1886(b)(3)(B)(viii) of the Act will receive an applicable percentage increase of −0.4 percent, which reflects a one-quarter reduction of the market basket update for failure to submit quality data and a three-quarter reduction of the market basket update for being identified as not a meaningful EHR user. At the time this impact was prepared, 30 hospitals are estimated to not receive the full market basket rate-of-increase for FY 2020 because they are identified as not meaningful EHR users that do not submit quality data under section 1886(b)(3)(B)(viii) of the Act.
Each policy change, statutory or otherwise, is then added incrementally to this baseline, finally arriving at an FY 2020 model incorporating all of the changes. This simulation allows us to isolate the effects of each change.
Our comparison illustrates the percent change in payments per case from FY 2019 to FY 2020. Two factors not discussed separately have significant impacts here. The first factor is the update to the standardized amount. In accordance with section 1886(b)(3)(B)(i) of the Act, we are updating the standardized amounts for FY 2020 using an applicable percentage increase of 2.6 percent. This includes our forecasted IPPS operating hospital market basket increase of 3.0 percent with a 0.4 percentage point reduction for the multifactor productivity adjustment. Hospitals that fail to comply with the quality data submission requirements and are meaningful EHR users will receive an update of 1.85 percent. This update includes a reduction of one-quarter of the market basket update for failure to submit these data. Hospitals that do comply with the quality data submission requirements but are not meaningful EHR users will receive an update of 0.35 percent, which includes a reduction of three-quarters of the market basket update. Furthermore, hospitals that do not comply with the quality data submission requirements and also are not meaningful EHR users will receive an update of −0.4 percent. Under section 1886(b)(3)(B)(iv) of the Act, the update to the hospital-specific amounts for SCHs and MDHs is also equal to the applicable percentage increase, or 2.6 percent, if the hospital submits quality data and is a meaningful EHR user.
A second significant factor that affects the changes in hospitals' payments per case from FY 2019 to FY 2020 is the change in hospitals' geographic reclassification status from one year to the next. That is, payments may be reduced for hospitals reclassified in FY 2019 that are no longer reclassified in FY 2020. Conversely, payments may increase for hospitals not reclassified in FY 2019 that are reclassified in FY 2020.
2. Analysis of Table I
Table I displays the results of our analysis of the changes for FY 2020. The table categorizes hospitals by various geographic and special payment consideration groups to illustrate the varying impacts on different types of hospitals. The top row of the table shows the overall impact on the 3,239 acute care hospitals included in the analysis.
The next four rows of Table I contain hospitals categorized according to their geographic location: All urban, which is further divided into large urban and other urban; and rural. There are 2,476 hospitals located in urban areas included in our analysis. Among these, there are 1,259 hospitals located in large urban areas (populations over 1 million), and 1,217 hospitals in other urban areas (populations of 1 million or fewer). In addition, there are 763 hospitals in rural areas. The next two groupings are by bed-size categories, shown separately for urban and rural hospitals. The last groupings by geographic location are by census divisions, also shown separately for urban and rural hospitals.
The second part of Table I shows hospital groups based on hospitals' FY 2020 payment classifications, including any reclassifications under section 1886(d)(10) of the Act. For example, the rows labeled urban, large urban, other urban, and rural show that the numbers of hospitals paid based on these categorizations after consideration of geographic reclassifications (including reclassifications under sections 1886(d)(8)(B) and 1886(d)(8)(E) of the Act that have implications for capital payments) are 2,183; 1,281; 902; and 1,056, respectively.
The next three groupings examine the impacts of the changes on hospitals grouped by whether or not they have GME residency programs (teaching hospitals that receive an IME adjustment) or receive Medicare DSH payments, or some combination of these two adjustments. There are 2,116 nonteaching hospitals in our analysis, 873 teaching hospitals with fewer than 100 residents, and 250 teaching hospitals with 100 or more residents.
In the DSH categories, hospitals are grouped according to their DSH payment status, and whether they are considered urban or rural for DSH purposes. The next category groups together hospitals considered urban or rural, in terms of whether they receive the IME adjustment, the DSH adjustment, both, or neither.
The next three rows examine the impacts of the changes on rural hospitals by special payment groups (SCHs, MDHs and RRCs). There were 383 RRCs, 306 SCHs, 150 MDHs, 144 hospitals that are both SCHs and RRCs, and 19 hospitals that are both MDHs and RRCs.
The next series of groupings are based on the type of ownership and the hospital's Medicare utilization expressed as a percent of total inpatient days. These data were taken from the FY 2017 or FY 2016 Medicare cost reports.
The next grouping concerns the geographic reclassification status of hospitals. The first subgrouping is based on whether a hospital is reclassified or not. The second and third subgroupings are based on whether urban and rural hospitals were reclassified by the MGCRB for FY 2020 or not, respectively. The fourth subgrouping displays hospitals that reclassified from urban to rural in accordance with section 1886(d)(8)(E) of the Act. The fifth subgrouping displays hospitals deemed urban in accordance with section 1886(d)(8)(B) of the Act.




a. Effects of the Hospital Update and Other Adjustments (Column 1)
As discussed in section IV.B. of the preamble of this final rule, this column includes the hospital update, including the 3.0 percent market basket update and the reduction of 0.4 percentage point for the multifactor productivity adjustment. In addition, as discussed in section II.D. of the preamble of this final rule, this column includes the FY 2020 +0.5 percentage point adjustment required under section 414 of the MACRA. As a result, we are making a 3.1 percent update to the national standardized amount. This column also includes the update to the hospital-specific rates which includes the 3.0 percent market basket update and the reduction of 0.4 percentage point for the multifactor productivity adjustment. As a result, we are making a 2.6 percent update to the hospital-specific rates.
Overall, hospitals will experience a 3.0 percent increase in payments primarily due to the combined effects of the hospital update to the national standardized amount and the hospital update to the hospital-specific rate. Hospitals that are paid under the hospital-specific rate will experience a 2.6 percent increase in payments; therefore, hospital categories containing hospitals paid under the hospital-specific rate will experience a lower than average increase in payments.
b. Effects of the Changes to the MS-DRG Reclassifications and Relative Cost-Based Weights With Recalibration Budget Neutrality (Column 2)
Column 2 shows the effects of the changes to the MS-DRGs and relative weights with the application of the recalibration budget neutrality factor to the standardized amounts. Section 1886(d)(4)(C)(i) of the Act requires us annually to make appropriate classification changes in order to reflect changes in treatment patterns, technology, and any other factors that may change the relative use of hospital resources. Consistent with section 1886(d)(4)(C)(iii) of the Act, we calculated a recalibration budget neutrality factor to account for the changes in MS-DRGs and relative weights to ensure that the overall payment impact is budget neutral.
As discussed in section II.E. of the preamble of this final rule, the FY 2020 MS-DRG relative weights will be 100 percent cost-based and 100 percent MS-DRGs. For FY 2020, the MS-DRGs are calculated using the FY 2018 MedPAR data grouped to the Version 37 (FY 2020) MS-DRGs. The methodology to calculate the relative weights and the reclassification changes to the GROUPER are described in more detail in section II.G. of the preamble of this final rule.
The “All Hospitals” line in Column 2 indicates that changes due to the MS-DRGs and relative weights will result in a 0.0 percent change in payments with the application of the recalibration budget neutrality factor of 0.997649 to the standardized amount. Hospital categories that generally treat cases in higher severity MS-DRGs, such as large urban hospitals, will experience a slight increase in their payments, while hospitals that generally treat fewer of these cases will experience a decrease in their payments under the relative weights. For example, rural hospitals will experience a 0.2 percent decrease in payments in part because rural hospitals tend to treat fewer cases in higher severity MS-DRGs. Conversely, teaching hospitals with more than 100 residents will experience a slight increase in payments of 0.2 percent as those hospitals typically treat more cases in higher severity MS-DRGs.
c. Effects of the Wage Index Changes (Column 3)
Column 3 shows the impact of the updated wage data using FY 2016 cost report data, with the application of the wage budget neutrality factor. The wage index is calculated and assigned to hospitals on the basis of the labor market area in which the hospital is located. Under section 1886(d)(3)(E) of the Act, beginning with FY 2005, we delineate hospital labor market areas based on the Core Based Statistical Areas (CBSAs) established by OMB. The current statistical standards used in FY 2020 are based on OMB standards published on February 28, 2013 (75 FR 37246 and 37252), and 2010 Decennial Census data (OMB Bulletin No. 13-01), as updated in OMB Bulletin Nos. 15-01 and 17-01. (We refer readers to the FY 2015 IPPS/LTCH PPS final rule (79 FR 49951 through 49963) for a full discussion on our adoption of the OMB labor market area delineations, based on the 2010 Decennial Census data, effective beginning with the FY 2015 IPPS wage index, to the FY 2017 IPPS/LTCH PPS final rule (81 FR 56913) for a discussion of our adoption of the CBSA updates in OMB Bulletin No. 15-01, which were effective beginning with the FY 2017 wage index, and to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41362) for a discussion of our adoption of the CBSA update in OMB Bulletin No. 17-01 for the FY 2019 wage index.)
Section 1886(d)(3)(E) of the Act requires that, beginning October 1, 1993, we annually update the wage data used to calculate the wage index. In accordance with this requirement, the wage index for acute care hospitals for FY 2020 is based on data submitted for hospital cost reporting periods, beginning on or after October 1, 2015 and before October 1, 2016. The estimated impact of the updated wage data using the FY 2016 cost report data and the OMB labor market area delineations on hospital payments is isolated in Column 3 by holding the other payment parameters constant in this simulation. That is, Column 3 shows the percentage change in payments when going from a model using the FY 2019 wage index, based on FY 2015 wage data, the labor-related share of 68.3 percent, under the OMB delineations and having a 100-percent occupational mix adjustment applied, to a model using the FY 2020 pre-reclassification wage index based on FY 2016 wage data with the labor-related share of 68.3 percent, under the OMB delineations, also having a 100-percent occupational mix adjustment applied, while holding other payment parameters, such as use of the Version 37 MS-DRG GROUPER constant. The FY 2020 occupational mix adjustment is based on the CY 2016 occupational mix survey.
In addition, the column shows the impact of the application of the wage budget neutrality to the national standardized amount. In FY 2010, we began calculating separate wage budget neutrality and recalibration budget neutrality factors, in accordance with section 1886(d)(3)(E) of the Act, which specifies that budget neutrality to account for wage index changes or updates made under that subparagraph must be made without regard to the 62 percent labor-related share guaranteed under section 1886(d)(3)(E)(ii) of the Act. Therefore, for FY 2020, we calculated the wage budget neutrality factor to ensure that payments under updated wage data and the labor-related share of 68.3 percent are budget neutral, without regard to the lower labor-related share of 62 percent applied to hospitals with a wage index less than or equal to 1.0. In other words, the wage budget neutrality is calculated under the assumption that all hospitals receive the higher labor-related share of the standardized amount. The FY 2020 wage budget neutrality factor is 1.001573 and the overall payment change is 0 percent.
Column 3 shows the impacts of updating the wage data using FY 2016 cost reports. Overall, the new wage data and the labor-related share, combined with the wage budget neutrality adjustment, will lead to no change for all hospitals, as shown in Column 3.
In looking at the wage data itself, the national average hourly wage would increase 1.03 percent compared to FY 2019. Therefore, the only manner in which to maintain or exceed the previous year's wage index was to match or exceed the 1.03 percent increase in the national average hourly wage. Of the 3,220 hospitals with wage data for both FYs 2019 and 2020, 1490 or 46.3 percent would experience an average hourly wage increase of 1.03 percent or more.
The following chart compares the shifts in wage index values for hospitals due to changes in the average hourly wage data for FY 2020 relative to FY 2019. Among urban hospitals, none would experience a decrease of 10 percent or more, and 1 urban hospitals would experience an increase of 10 percent or more. Sixty six urban hospitals would experience an increase or decrease of at least 5 percent or more but less than 10 percent. Among rural hospitals, none would experience an increase of 10 percent or more, and none would experience a decrease of 10 percent or more. Two rural hospitals would experience an increase or decrease of at least 5 percent or more but less than 10 percent. However, 747 rural hospitals would experience increases or decreases of less than 5 percent, while 2,398 urban hospitals would experience increases or decreases of less than 5 percent. Four urban hospitals and 2 rural hospitals would experience no change to their wage index. These figures reflect changes in the “pre-reclassified, occupational mix-adjusted wage index,” that is, the wage index before the application of geographic reclassification, the rural floor, the out-migration adjustment, and other wage index exceptions and adjustments. (We refer readers to sections III.G. through III.L. of the preamble of this final rule for a complete discussion of the exceptions and adjustments to the wage index.) We note that the “post-reclassified wage index” or “payment wage index,” which is the wage index that includes all such exceptions and adjustments (as reflected in Tables 2 and 3 associated with this final rule, which are available via the internet on the CMS website) is used to adjust the labor-related share of a hospital's standardized amount, either 68.3 percent or 62 percent, depending upon whether a hospital's wage index is greater than 1.0 or less than or equal to 1.0. Therefore, the pre-reclassified wage index figures in the following chart may illustrate a somewhat larger or smaller change than would occur in a hospital's payment wage index and total payment.
The following chart shows the projected impact of changes in the area wage index values for urban and rural hospitals.

d. Effects of MGCRB Reclassifications (Column 4)
Our impact analysis to this point has assumed acute care hospitals are paid on the basis of their actual geographic location (with the exception of ongoing policies that provide that certain hospitals receive payments on bases other than where they are geographically located). The changes in Column 4 reflect the per case payment impact of moving from this baseline to a simulation incorporating the MGCRB decisions for FY 2020.
By spring of each year, the MGCRB makes reclassification determinations that will be effective for the next fiscal year, which begins on October 1. The MGCRB may approve a hospital's reclassification request for the purpose of using another area's wage index value. Hospitals may appeal denials of MGCRB decisions to the CMS Administrator. Further, hospitals have 45 days from the date the IPPS proposed rule is issued in the Federal Register to decide whether to withdraw or terminate an approved geographic reclassification for the following year (we refer readers to the discussion of our clarification of this policy in section III.I.2. of the preamble to this final rule).
The overall effect of geographic reclassification is required by section 1886(d)(8)(D) of the Act to be budget neutral. Therefore, for purposes of this impact analysis, we applied an adjustment of 0.985425 to ensure that the effects of the reclassifications under sections 1886(d)(8)(B) and (C) and 1886(d)(10) of the Act are budget neutral (section II.A. of the Addendum to this final rule). We note that, with regard to the requirement under section 1886(d)(8)(C)(iii) of the Act, in our calculation of the budget neutrality adjustment of 0.985425, we applied the provisions of our policy discussed in section III.N. of the preamble of this final rule to exclude the wage data of urban hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act from the calculation of “the wage index for rural areas in the State in which the county is located” (section II.A.4. of the Addendum to this final rule). Geographic reclassification generally benefits hospitals in rural areas. We estimate that the geographic reclassification will increase payments to rural hospitals by an average of 1.1 percent. By region, all the rural hospital categories will experience increases in payments due to MGCRB reclassifications.
Table 2 listed in section VI. of the Addendum to this final rule and available via the internet on the CMS website reflects the reclassifications for FY 2020.
e. Effects of the Rural Floor, Including Application of National Budget Neutrality (Column 5)
As discussed in section III.B. of the preamble of the FY 2009 IPPS final rule, the FY 2010 IPPS/RY 2010 LTCH PPS final rule, the FYs 2011 through 2019 IPPS/LTCH PPS final rules, and this FY 2020 IPPS/LTCH PPS final rule, section 4410 of Public Law 105-33 established the rural floor by requiring that the wage index for a hospital in any urban area cannot be less than the wage index applicable to hospitals located in rural areas in the same State. We applied a uniform budget neutrality adjustment to the wage index. Column 5 shows the effects of the rural floor.
The Affordable Care Act requires that we apply one rural floor budget neutrality factor to the wage index nationally. We have calculated a FY 2020 rural floor budget neutrality factor that was applied to the wage index of 0.997081, which will reduce wage indexes by 0.29 percent.
Column 5 shows the projected impact of the rural floor with the national rural floor budget neutrality factor applied to the wage index based on the OMB labor market area delineations. The column compares the post-reclassification FY 2020 wage index of providers before the rural floor adjustment and the post-reclassification FY 2020 wage index of providers with the rural floor adjustment based on the OMB labor market area delineations. Only urban hospitals can benefit from the rural floor. Because the provision is budget neutral, all other hospitals (that is, all rural hospitals and those urban hospitals to which the adjustment is not made) will experience a decrease in payments due to the budget neutrality adjustment that is applied nationally to their wage index. We note that, as discussed in section III.N of the preamble of this final rule, we calculated the FY 2020 rural floor without including the wage data of hospitals that have reclassified as rural under § 412.103. This column reflects effects of this change to the rural floor calculation methodology.
We estimate that 164 hospitals will receive the rural floor in FY 2020. We note that there are approximately 99 fewer hospitals receiving the rural floor in FY 2020 than in FY 2019. This is due, in part, to our calculation of the rural floor for FY 2020 (and subsequent fiscal years) without including the wage data of hospitals that have reclassified as rural under § 412.103. This policy will impact States whose rural floors were heavily influenced by the wage data of hospitals that reclassified under § 412.103, such as Massachusetts and Arizona. All IPPS hospitals in our model will have their wage index reduced by the rural floor budget neutrality adjustment of 0.997081. We project that, in aggregate, rural hospitals will experience a 0.1 percent decrease in payments as a result of the application of the rural floor budget neutrality because the rural hospitals do not benefit from the rural floor, but have their wage indexes downwardly adjusted to ensure that the application of the rural floor is budget neutral overall. We project that, in the aggregate, hospitals located in urban areas will experience no change in payments because increases in payments to hospitals benefitting from the rural floor offset decreases in payments to non-rural floor urban hospitals whose wage index is downwardly adjusted by the rural floor budget neutrality factor. Urban hospitals in the New England region will experience a 0.4 percent increase in payments primarily due to the application of the rural floor in Massachusetts. Eleven urban providers in Massachusetts are expected to receive the rural floor wage index value, including the rural floor budget neutrality adjustment, which will increase payments overall to hospitals in Massachusetts by an estimated $25 million. We estimate that Massachusetts hospitals will receive approximately a 0.6 percent increase in IPPS payments due to the application of the rural floor in FY 2020.
Urban Puerto Rico hospitals are expected to experience a 0.3 percent increase in payments as a result of the application of the rural floor for FY 2020.
The table below shows a comparison of the payment impact of the rural floor (with budget neutrality) by State based on the FY 2020 rural floor and the payment impact of the rural floor (with budget neutrality) by State based on the FY 2019 rural floor. Columns 1a through 4a in the table below reflect the FY 2019 rural floor calculation. The FY 2019 rural floor, as published in the October 3, 2018 Final Rule Correction Notice (83 FR 49836), was calculated by including the wage data of hospitals that reclassified as rural under § 412.103. As indicated earlier, for FY 2020 and subsequent fiscal years, we are calculating the rural floor without including the wage data of hospitals that have reclassified as rural under § 412.103. Columns 1b through 4b in the table below reflect this FY 2020 rural floor calculation. Columns 1a and 1b of the table display the number of IPPS hospitals located in each State in FY 2019 and FY 2020, respectively. Columns 2a and 2b display the number of hospitals in each State that received the rural floor wage index for FY 2019 (column 2a) and those that will receive the rural floor wage index for FY 2020 (column 2b). Columns 3a and 3b display the percentage change in total payments to hospitals in each State due to the application of the rural floor with national budget neutrality for FY 2019 (column 3a) and FY 2020 (column 3b). To show the percentage change in total payments for FY 2019 and FY 2020, in columns 3a and 3b, respectively, we calculated total payments using the post-reclassification wage index of providers prior to the rural floor adjustment and total payments using the post-reclassification wage index of providers with the rural floor adjustment for FY 2019 and FY 2020, respectively. The differences in those payments are reflected in columns 3a and 3b. Columns 4a and 4b display the payment amount that hospitals in each State will gain or lose due to the application of the FY 2019 rural floor with national budget neutrality (column 4a) and the estimated payment amount that hospitals in each State will gain or lose due to the application of the FY 2020 rural floor with national budget neutrality (column 4b). We note that columns 2b, 3b, and 4b of this table do not include the application of the policy to increase the wage index for hospitals with a wage index value below the 25th percentile wage index, the 5-percent cap, and the associated budget neutrality factors.



f. Effects of the Application of the Frontier State Wage Index and Out-Migration Adjustment (Column 6)
This column shows the combined effects of the application of section 10324(a) of the Affordable Care Act, which requires that we establish a minimum post-reclassified wage index of 1.00 for all hospitals located in “frontier States,” and the effects of section 1886(d)(13) of the Act, as added by section 505 of Public Law 108-173, which provides for an increase in the wage index for hospitals located in certain counties that have a relatively high percentage of hospital employees who reside in the county, but work in a different area with a higher wage index. These two wage index provisions are not budget neutral and will increase payments overall by 0.1 percent compared to the provisions not being in effect.
The term “frontier States” is defined in the statute as States in which at least 50 percent of counties have a population density less than 6 persons per square mile. Based on these criteria, 5 States (Montana, Nevada, North Dakota, South Dakota, and Wyoming) are considered frontier States and 44 hospitals located in those States will receive a frontier wage index of 1.0000. Overall, this provision is not budget neutral and is estimated to increase IPPS operating payments by approximately $64 million. Urban hospitals located in the West North Central region will experience an increase in payments by 0.6 percent, because many of the hospitals located in this region are frontier State hospitals.
In addition, section 1886(d)(13) of the Act, as added by section 505 of Public Law 108-173, provides for an increase in the wage index for hospitals located in certain counties that have a relatively high percentage of hospital employees who reside in the county, but work in a different area with a higher wage index. Hospitals located in counties that qualify for the payment adjustment will receive an increase in the wage index that is equal to a weighted average of the difference between the wage index of the resident county, post-reclassification and the higher wage index work area(s), weighted by the overall percentage of workers who are employed in an area with a higher wage index. There are an estimated 176 providers that will receive the out-migration wage adjustment in FY 2020. Rural hospitals generally will qualify for the adjustment, resulting in a 0.1 percent increase in payments. This provision appears to benefit section 401 hospitals and RRCs in that they will each experience a 0.1 and 0.2 percent increase in payments, respectively. This out-migration wage adjustment also is not budget neutral, and we estimate the impact of these providers receiving the out-migration increase will be approximately $44 million.
g. Effects of the Lowest Quartile Wage Index Adjustment and 5-Percent Transition Policy With Application of Budget Neutrality
Column 7 shows the effects of the wage index adjustment for hospitals with a wage index value below the 25th percentile wage index value, the transition policy placing a 5-percent cap for FY 2020 on any decrease in a hospital's wage index from its final FY 2019 wage index, and the associated budget neutrality policy. As discussed in section III.N. of the preamble to this final rule, hospitals with a wage index value below the 25th percentile wage index value will receive an increase to their wage index value of half the difference between the otherwise applicable final wage index value for a year for that hospital and the 25th percentile wage index value for that year across all hospitals. We are also applying a budget neutrality factor to the standardized rate in order to ensure that our increase to the wage index for hospitals with a wage index value below the 25th percentile is budget neutral. In addition, for FY 2020, we are applying a 5-percent cap on any decrease in a hospital's wage index from the hospital's final wage index in FY 2019 (which will include any decrease resulting from our policy to not include urban to rural reclassifications in the rural floor calculation).
The overall effect of the application of the wage index adjustment for hospitals with a wage index value below the 25th percentile will be budget neutral. In order to ensure that the overall effect of the application of the wage index adjustment for hospitals with a wage index value below the 25th percentile is budget neutral, we are applying a budget neutrality factor of 0.997987 to the FY 2020 standardized amount (as described in section III.N.2.b. of this final rule). In addition, we are implementing the 5-percent cap on any decrease in a hospital's wage index in a budget neutral manner under the authority at section 1886(d)(5)(I) of the Act. Therefore, for purposes of this impact analysis, we are applying a budget neutrality adjustment factor of 0.998838 to the FY 2020 standardized amount to implement the 5-percent cap in a budget neutral manner.
To show the effects of the lowest quartile wage index adjustments, the 5-percent cap, and the associated budget neutrality factors, column 7 compares payments calculated with the FY 2020 wage index prior to the application of: (a) The adjustment for hospitals with a wage index value below the 25th percentile; (b) the 5-percent cap on any decrease in a hospital's wage index; and (c) the budget neutrality factors to the standardized rate associated with (1) the adjustment for hospitals with a wage index value below the 25th percentile and (2) the 5-percent cap to payments calculated using the FY 2020 wage index with the above mentioned adjustments applied (that is, the lowest quartile wage index adjustment, the 5-percent cap, and the associated budget neutrality factors). The net effect of these three policies generally benefits hospitals in rural areas. For example, we estimate that the adjustments for hospitals with a wage index value below the 25th percentile wage index, the 5-percent cap on any decrease in a hospital's wage index, and the application of the associated budget neutrality factors, will increase payments to rural hospitals by an average of 0.3 percent. By region, rural South Atlantic and West South Central hospital categories will experience increases in payments by 0.5 and 0.7 percent, respectively. Puerto Rico providers will experience a 12.5 percent increase in payments due to the application of the lowest quartile wage index adjustment because they generally have the lowest wage index values.
h. Effects of All FY 2020 Changes (Column 8)
Column 8 shows our estimate of the changes in payments per discharge from FY 2019 and FY 2020, resulting from all changes reflected in this final rule for FY 2020. It includes combined effects of the year-to-year change of the previous columns in the table.
The average increase in payments under the IPPS for all hospitals is approximately 2.9 percent for FY 2020 relative to FY 2019 and for this row is primarily driven by the changes reflected in Column 1. Column 8 includes the annual hospital update of 2.6 percent to the national standardized amount. This annual hospital update includes the 3.0 percent market basket update and the 0.4 percentage point reduction for the multifactor productivity adjustment. As discussed in section II.D. of the preamble of this final rule, this column also includes the +0.5 percentage point adjustment required under section 414 of the MACRA. Hospitals paid under the hospital-specific rate will receive a 2.6 percent hospital update. As described in Column 1, the annual hospital update with the +0.5 percent adjustment for hospitals paid under the national standardized amount, combined with the annual hospital update for hospitals paid under the hospital-specific rates, will result in a 2.9 percent increase in payments in FY 2020 relative to FY 2019. This estimated increase also reflects an estimated decrease in outlier payments of 0.13 percent (from our current estimate of FY 2019 outlier payments of approximately 5.23 percent to 5.1 percent projected for FY 2020 based on the FY 2018 MedPAR data used for this final rule calculated for purposes of this impact analysis). There are also interactive effects among the various factors comprising the payment system that we are not able to isolate, which contribute to our estimate of the changes in payments per discharge from FY 2019 and FY 2020 in Column 8.
Overall payments to hospitals paid under the IPPS due to the applicable percentage increase and changes to policies related to MS-DRGs, geographic adjustments, and outliers are estimated to increase by 2.9 percent for FY 2020. Hospitals in urban areas will experience a 2.9 percent increase in payments per discharge in FY 2020 compared to FY 2019. Hospital payments per discharge in rural areas are estimated to increase by 2.8 percent in FY 2020.
3. Impact Analysis of Table II
Table II below presents the projected impact of the changes for FY 2020 for urban and rural hospitals and for the different categories of hospitals shown in Table I. It compares the estimated average payments per discharge for FY 2019 with the estimated average payments per discharge for FY 2020, as calculated under our models. Therefore, this table presents, in terms of the average dollar amounts paid per discharge, the combined effects of the changes presented in Table I. The estimated percentage changes shown in the last column of Table II equal the estimated percentage changes in average payments per discharge from Column 8 of Table I.


H. Effects of Other Policy Changes
In addition to those policy changes discussed previously that we are able to model using our IPPS payment simulation model, we are making various other changes in this final rule. As noted in section I.G. of this regulatory impact analysis, our payment simulation model uses the most recent available claims data to estimate the impacts on payments per case of certain changes in this final rule. Generally, we have limited or no specific data available with which to estimate the impacts of these changes using that payment simulation model. For those changes, we have attempted to predict the payment impacts based upon our experience and other more limited data. Our estimates of the likely impacts associated with these other changes are discussed in this section.
1. Effects of Policies Relating to New Medical Service and Technology Add-On Payments
a. Technologies Approved for FY 2020 New Technology Add-On Payments
In section II.H. of the preamble to this final rule, we discuss 13 technologies for which we received applications for add-on payments for new medical services and technologies for FY 2020. We note that three applicants withdrew their applications prior to the issuance of this final rule, and one applicant did not receive FDA approval for its technology by the July 1 deadline. We also discuss the status of the new technologies that were approved to receive new technology add-on payments in FY 2019. As explained in the preamble to this final rule, add-on payments for new medical services and technologies under section 1886(d)(5)(K) of the Act are not required to be budget neutral.
As discussed in section II.H.5. of the preamble of this final rule, we are approving the following 9 applications for new technology add-on payments for FY 2020: AZEDRA® (Ultratrace® iobenguane Iodine-131) Solution; CABLIVI® (caplacizumab-yhdp); ELZONRISTM (tagraxofusp, SL-401); BalversaTM (Erdafitinib); ERLEADATM (Apalutamide); SPRAVATO (Esketamine); XOSPATA® (gilteritinib); JAKAFITM (Ruxolitinib) and T2 Bacteria Test Panel.
In addition, as we proposed, as discussed in section II.H.4. of the preamble of this final rule, we are continuing to make new technology add-on payments for AndexXaTM, the AQUABEAM System (Aquablation), GIAPREZATM, KYMRIAH® and YESCARTA®, the remedē® System, the Sentinel® Cerebral Protection System, VABOMERETM, VYXEOSTM, and ZEMDRITM in FY 2020 because these technologies are still considered new for purposes of new technology add-on payments. (We note, as proposed, we are discontinuing new technology add-on payments for Defitelio® (Defibrotide), Ustekinumab (Stelara®) and Bezlotoxumab (ZinplavaTM) for FY 2020 because these technologies will have been on the U.S. market for 3 years.)
Under our change to the calculation of the new technology add-on payments, in general the new technology add-on payment for each case will be limited to the lesser of: (1) 65 percent of the costs of the new technology; or (2) 65 percent of the amount by which the costs of the case exceed the standard MS-DRG payment for the case. For antimicrobials designated as a Qualified Infectious Disease Product (QIDP), the new technology add-on payment for each case will be limited to the lesser of (1) 75 percent of the costs of the new technology; or (2) 75 percent of the amount by which the costs of the case exceed the standard MS-DRG payment for the case.
The following are estimates for FY 2020 for the nine technologies for which we are continuing to make new technology add-on payments in FY 2020:
- Based on the applicant's estimate from FY 2019, we currently estimate that new technology add-on payments for AndexXaTM will increase overall FY 2020 payments by $98,755,313 (maximum add-on payment of $18,281.25 * 5,402 patients).
- Based on the applicant's estimate from FY 2019, we currently estimate that new technology add-on payments for the AQUABEAM System (Aquablation) will increase overall FY 2020 payments by $677,625 (maximum add-on payment of $1,625 * 417 patients).
- Based on the applicant's estimate for FY 2019, we currently estimate that new technology add-on payments for GIAPREZATM will increase overall FY 2020 payments by $11,173,500 (maximum add-on payment of $1,950 * 5,730 patients).
- Based on both applicants' estimates of the average cost for an administered dose for FY 2019, we currently estimate that new technology add-on payments for KYMRIAH® and YESCARTA® will increase overall FY 2020 payments by $93,585,700 (maximum add-on payment of $242,450 * 386 patients).
- Based on the applicant's estimate for FY 2019, we currently estimate that new technology add-on payments for Sentinel® Cerebral Protection System will increase overall FY 2020 payments by $11,830,000 (maximum add-on payment of $1,820 * 6,500 patients).
- Based on the applicant's estimate for FY 2019, we currently estimate that new technology add-on payments for the remedē® System will increase overall FY 2020 payments by $1,794,000 (maximum add-on payment of $22,425 * 80 patients).
- Based on the applicant's estimate for FY 2019, we currently estimate that new technology add-on payments for VABOMERETM will increase overall FY 2020 payments by $22,020,768 (maximum add-on payment of $8,316 * 2,648 patients).
- Based on the applicant's estimate for FY 2019, we currently estimate that new technology add-on payments for VYXEOSTM will increase overall FY 2020 payments by $45,458,400 (maximum add-on payment of $47,352.50 * 960 patients).
- Based on the applicant's estimate for FY 2019, we currently estimate that new technology add-on payments for ZEMDRITM will increase overall FY 2020 payments by $10,209,375 (maximum add-on payment of $4,083.75 * 2,500 patients).
The following are estimates for FY 2020 for the nine technologies that we are approving for new technology add-on payments beginning in FY 2020.
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for AZEDRA® (Ultratrace® iobenguane Iodine-131) Solution will increase overall FY 2020 payments by $39,260,000 (maximum add-on payment of $98,150 * 400 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for CABLIVI® (caplacizumab-yhdp) will increase overall FY 2020 payments by $4,351,165 (maximum add-on payment of $33,215 * 131 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for ELZONRISTM (tagraxofusp, SL-401) will increase overall FY 2020 payments by $30,985,668 (maximum add-on payment of $125,448.05 * 247 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for BalversaTM (Erdafitinib) will increase overall FY 2020 payments by $178,162 (maximum add-on payment of $3,563.23 * 50 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for ERLEADATM (Apalutamide) will increase overall FY 2020 payments by $286,171 (maximum add-on payment of $1,858.25 * 154 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for SPRAVATO (Esketamine) will increase overall FY 2020 payments by $6,494,656 (maximum add-on payment of $1,014.79 * 6,400 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for XOSPATA® (gilteritinib) will increase overall FY 2020 payments by $13,710,938 (maximum add-on payment of $7,312.50 * 1,875 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for JAKAFITM (Ruxolitinib) will increase overall FY 2020 payments by $556,788 (maximum add-on payment of $3,977.06 * 140 patients).
- Based on the applicant's estimate for FY 2020, we currently estimate that new technology add-on payments for T2 Bacteria Test Panel will increase overall FY 2020 payments by $3,669,803 (maximum add-on payment of $97.50 * 37,639 patients).
b. Alternative Inpatient New Technology Add-On Payment Pathway for Transformative New Devices and Certain Antimicrobial Resistant Products
In section II.H.8. of the preamble of this final rule, we discuss the alternative inpatient new technology add-on payment pathway for certain new devices and certain antimicrobial resistant products we are establishing for applications received for IPPS new technology add-on payments for FY 2021 and subsequent fiscal years. Specifically, we are providing that, if a medical device is part of the FDA's Breakthrough Devices Program or if medical product is designated by the FDA as a Qualified Infectious Disease Product (QIDP), and received FDA market authorization, such a device or product will be considered new and not substantially similar to an existing technology for purposes of new technology add-on payment under the IPPS. We also are providing that such a medical device or product will not need to meet the requirement under § 412.87(b)(1) that it represent an advance that substantially improves, relative to technologies previously available, the diagnosis or treatment of Medicare beneficiaries.
Given the relatively recent introduction of the Breakthrough Devices Program, there have not been any medical devices that were part of the Breakthrough Devices Program and received FDA market authorization, and that applied for a new technology add-on payment under the IPPS and were not approved.
If all of the future new transformative medical devices or QIDPs that apply for new technology add-on payments would be approved under the existing criteria, this policy has no impact. To the extent that there are future medical devices or QIDPs that are the subject of applications for new technology add-on payments, and those applications would have been denied under the current new technology add-on payment criteria, this policy is a cost, but that cost is not estimable.
The FDA has granted a total of 147 QIDP designations (74 of which were novel). However, designations may be granted at any point in the drug development process (e.g., Phase 1), and the majority of QIDP-designated drugs are not expected to get market authorization. Of all antibiotics to date, the FDA has only approved 12 QIDP drugs. Therefore, we believe there is minimal to no impact on Medicare program expenditures due to the alternative inpatient new technology add-on payment pathway for QIDPs. We also note that as this finalized policy will be effective beginning with new technology add-on payment applications for FY 2021, there is no impact of this policy in FY 2020.
c. Changes to the Calculation of the Inpatient New Technology Add-On Payment
In section II.H.9. of the preamble of this final rule, we discuss our policy to modify the current new technology add-on payment mechanism to increase the amount of the maximum add-on payment amount to 65 percent (and 75 percent for Qualified Infectious Disease Products (QIDPs)). Specifically, for technologies other than QIDPs, if the costs of a discharge (determined by applying CCRs as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 65 percent of the costs of the new medical service or technology; or (2) 75 percent of the amount by which the costs of the case exceed the standard DRG payment. For technologies designated as QIDPs, if the costs of a discharge (determined by applying CCRs as described in § 412.84(h)) exceed the full DRG payment (including payments for IME and DSH, but excluding outlier payments), Medicare will make an add-on payment equal to the lesser of: (1) 75 percent of the costs of the new medical service or technology; or (2) 75 percent of the amount by which the costs of the case exceed the standard DRG payment. Unless the discharge qualifies for an outlier payment, the additional Medicare payment will be limited to the full MS-DRG payment plus 65 percent (or 75 percent for QIDPs) of the estimated costs of the new technology or medical service.
We estimate that for the nine technologies for which we are continuing to make new technology add-on payments in FY 2020 and for the nine FY 2020 new technology add-on payment applications that we are approving for new technology add-on payments for FY 2020, these changes to the calculation of the inpatient new technology add-on payment will increase IPPS spending by approximately $94 million in FY 2020, of which approximately $4 million is due to the differential new technology add-on payment percentage (that is, 75 percent versus 65 percent).
2. Effects of Changes to MS-DRGs Subject to the Postacute Care Transfer Policy and the MS-DRG Special Payment Policy
In section IV.A. of the preamble of this final rule, we discuss our changes to the list of MS-DRGs subject to the postacute care transfer policy and the MS-DRG special payment policy for FY 2020. As reflected in Table 5 listed in section VI. of the Addendum to this final rule (which is available via the internet on the CMS website), using criteria set forth in regulations at 42 CFR 412.4, we evaluated MS-DRG charge, discharge, and transfer data to determine which new or revised MS-DRGs will qualify for the postacute care transfer and MS-DRG special payment policies. As a result of our finalized policies to revise the MS-DRG classifications for FY 2020, which are discussed in section II.F. of the preamble of this final rule, we are removing two MS-DRGs from the list of MS-DRGs that will be subject to the postacute care transfer policy and the MS-DRG special payment policy. Column 2 of Table I in this Appendix A shows the effects of the changes to the MS-DRGs and the relative payment weights and the application of the recalibration budget neutrality factor to the standardized amounts. Section 1886(d)(4)(C)(i) of the Act requires us annually to make appropriate DRG classification changes in order to reflect changes in treatment patterns, technology, and any other factors that may change the relative use of hospital resources. The analysis and methods for determining the changes due to the MS-DRGs and relative payment weights account for and include changes as a result of the changes to the MS-DRGs subject to the MS-DRG postacute care transfer and MS-DRG special payment policies. We refer readers to section I.G. of this Appendix A for a detailed discussion of payment impacts due to the MS-DRG reclassification policies for FY 2020.
3. Effects of Low-Volume Hospital Payment Adjustment Policy
In section IV.D. of the preamble of this final rule, we discuss the low-volume hospital payment policy for FY 2020. Specifically, to qualify for the low-volume hospital payment adjustment, a hospital must be located more than 15 road miles from another subsection (d) hospital and have less than 3,800 total discharges during the fiscal year based on the hospital's most recently submitted cost report. The low-volume hospital payment adjustment is a per-discharge payment adjustment calculated as follows:
- 25 percent for low-volume hospitals with 500 or fewer total discharges;
- (95/330)—(number of total discharges/13,200) for low-volume hospitals with fewer than 3,800 discharges but more than 500 discharges.
Based upon the best available data at this time, we estimate payments made under the low-volume hospital payment adjustment policy will decrease Medicare payments by $7 million in FY 2020 as compared to FY 2019. More specifically, in FY 2020, we estimate that 594 providers will receive approximately $442 million compared to our estimate of 600 providers receiving approximately $449 million in FY 2019. These payment estimates were determined by identifying providers that, based on the best available data, qualify in FY 2019 (that is, are located at least 15 miles from the nearest subsection (d) hospital and have less than 3,800 total discharges).
4. Effects of the Changes to Medicare DSH and Uncompensated Care Payments for FY 2020
As discussed in section IV.F. of the preamble of this final rule, under section 3133 of the Affordable Care Act, hospitals that are eligible to receive Medicare DSH payments will receive 25 percent of the amount they previously would have received under the statutory formula for Medicare DSH payments under section 1886(d)(5)(F) of the Act. The remainder, equal to an estimate of 75 percent of what formerly would have been paid as Medicare DSH payments (Factor 1), reduced to reflect changes in the percentage of uninsured individuals (Factor 2), is available to make additional payments to each hospital that qualifies for Medicare DSH payments and that has uncompensated care. Each hospital eligible for Medicare DSH payments will receive an additional payment based on its estimated share of the total amount of uncompensated care for all hospitals eligible for Medicare DSH payments. The uncompensated care payment methodology has redistributive effects based on the proportion of a hospital's amount of uncompensated care relative to the aggregate amount of uncompensated care of all hospitals eligible for Medicare DSH payments (Factor 3). The change to Medicare DSH payments under section 3133 of the Affordable Care Act is not budget neutral.
In this final rule, we are establishing the amount to be distributed as uncompensated care payments to DSH eligible hospitals, which for FY 2020 is $8,350,599,096.04. This figure represents 75 percent of the amount that otherwise would have been paid for Medicare DSH payment adjustments adjusted by a proposed Factor 2 of 67.14 percent. For FY 2019, the amount available to be distributed for uncompensated care was $8,272,872,447.22, or 75 percent of the amount that otherwise would have been paid for Medicare DSH payment adjustments adjusted by a Factor 2 of 67.51 percent. To calculate Factor 3 for FY 2020, we used hospitals' FY 2015 cost reports from the HCRIS database, as updated through June 30, 2019, Medicaid days from hospitals' FY 2013 cost reports from the same extract of HCRIS, and SSI days from the FY 2017 SSI ratios. For each eligible hospital, with the exception of Puerto Rico hospitals and Indian Health Service and Tribal hospitals, we calculated a Factor 3 using information on uncompensated care costs from cost reports for FY 2015. To calculate Factor 3 for Puerto Rico hospitals and Indian Health Service and Tribal hospitals, we used data regarding Medicaid days for FY 2013 and SSI days for FY 2017. For a complete discussion of the methodology for calculating Factor 3, we refer readers to section IV.F.4. of the preamble of this final rule.
To estimate the impact of the combined effect of changes in Factors 1 and 2, as well as the changes to the data used in determining Factor 3, on the calculation of Medicare uncompensated care payments, we compared total uncompensated care payments estimated in the FY 2019 IPPS/LTCH PPS final rule to total uncompensated care payments estimated in this FY 2020 IPPS/LTCH PPS final rule. For FY 2019, we calculated 75 percent of the estimated amount that would be paid as Medicare DSH payments absent section 3133 of the Affordable Care Act, adjusted by a Factor 2 of 67.51 percent and multiplied by a Factor 3 calculated using the methodology described in the FY 2019 IPPS/LTCH PPS final rule. For FY 2020, we calculated 75 percent of the estimated amount that would be paid as Medicare DSH payments absent section 3133 of the Affordable Care Act, adjusted by a Factor 2 of 67.14 percent and multiplied by a Factor 3 calculated using the methodology described previously.
Our analysis included 2,432 hospitals that are projected to be eligible for DSH in FY 2020. It did not include hospitals that terminated their participation from the Medicare program as of June 18, 2019, Maryland hospitals, new hospitals, MDHs, and SCHs that are expected to be paid based on their hospital-specific rates. The 28 hospitals participating in the Rural Community Hospital Demonstration Program were excluded from this analysis, as participating hospitals are not eligible to receive empirically justified Medicare DSH payments and uncompensated care payments. In addition, the data from merged or acquired hospitals were combined under the surviving hospital's CMS certification number (CCN), and the nonsurviving CCN was excluded from the analysis. The estimated impact of the changes in Factors 1, 2, and 3 on uncompensated care payments across all hospitals projected to be eligible for DSH payments in FY 2020, by hospital characteristic, is presented in the following table.



Changes in projected FY 2020 uncompensated care payments from payments in FY 2019 are driven by an increase in Factor 1 and a decrease in Factor 2, as well as by a decrease in the number of hospitals projected to be eligible to receive DSH in FY 2020 relative to FY 2019. Factor 1 has increased from $12.254 billion to $12.438 billion, and the percent change in the percent of individuals who are uninsured (Factor 2) has decreased from 67.51 percent to 67.14 percent. Based on the changes in these two factors, the impact analysis found that, across all projected DSH eligible hospitals, FY 2020 uncompensated care payments are estimated at approximately $8.351 billion, or an increase of approximately 0.94 percent from FY 2019 uncompensated care payments (approximately $8.273 billion). While these changes will result in a net increase in the amount available to be distributed in uncompensated care payments, the projected payment increases vary by hospital type. This redistribution of uncompensated care payments is caused by changes in Factor 3. As seen in the above table, percent increases smaller than 0.94 percent indicate that hospitals within the specified category are projected to experience a smaller increase in uncompensated care payments, on average, compared to the universe of projected FY 2020 DSH hospitals. Conversely, percent increases that are greater than 0.94 percent indicate a hospital type is projected to have a larger increase than the overall average. The variation in the distribution of payments by hospital characteristic is largely dependent on a given hospital's uncompensated care costs as reported in the Worksheet S-10, or number of Medicaid days and SSI days for Puerto Rico hospitals and Indian Health Service and Tribal hospitals, used in the Factor 3 computation.
Rural hospitals, in general, are projected to experience significantly larger increases in uncompensated care payments than their urban counterparts. In general, rural hospitals, benefit under the FY 2020 final rule's methodology to use one year of Worksheet S-10 data compared to FY 2019 final rule's methodology, which used a three-year average approach with low-income insured days proxy and two-years of uncompensated care cost Worksheet S-10 data. Overall, rural hospitals are projected to receive a 15.44 percent increase in uncompensated care payments, while urban hospitals are projected to receive a 0.07 percent increase in uncompensated care payments.
By bed size, smaller hospitals are projected to receive larger increases in uncompensated care payments than larger hospitals, in both rural and urban settings. Rural hospitals with 0-99 beds are projected to receive a 23.00 percent payment increase, rural hospitals with 100-249 beds are projected to receive a 7.15 percent increase, and larger rural hospitals with 250+ beds are projected to receive a 10.96 percent payment increase. These increases for rural hospitals are all greater than the overall hospital average. This trend is also generally true for urban hospitals, with the smallest urban hospitals (0-99 beds) projected to receive an increase in uncompensated care payments of 14.42 percent, and urban hospitals with 100-249 beds projected to receive an increase of 2.14 percent, both of which are greater than the overall average. Larger urban hospitals with 250+ beds are projected to receive a 1.24 percent decrease in uncompensated care payments.
By region, rural hospitals are expected to receive a larger than average increase in uncompensated care payments in all Regions, except for rural hospitals in the Middle Atlantic Region, which are projected to receive a decrease in uncompensated care payments. Regionally, urban hospitals are projected to receive a more varied range of payment changes. Urban hospitals in the New England, East North Central, West North Central, Mountain and Pacific Regions are projected to receive a decrease in uncompensated care payments. A smaller than average increase in uncompensated care payments is projected in the Middle Atlantic Region, while urban hospitals in the South Atlantic, East South Central, West South Central Regions and in Puerto Rico are projected to receive a larger than average increase in uncompensated care payments.
By payment classification, although urban hospitals overall are expected to receive a 2.32 percent increase in uncompensated care payments, hospitals in large urban areas are expected to see an increase in uncompensated care payments of 4.99 percent, while hospitals in other urban areas are expected to receive a decrease in uncompensated care payments of 3.01 percent. Hospitals in rural areas are also projected to receive a decrease of 4.17 percent.
Nonteaching hospitals are projected to receive a larger than average payment increase of 3.82 percent. Teaching hospitals with fewer than 100 residents are projected to receive a payment decrease of 1.92 percent, while those teaching hospitals with 100+ residents have a projected payment increase of 1.27 percent, slightly higher than the overall average. Government hospitals are projected to receive a larger than average increase of 21.32 percent, while proprietary and voluntary hospitals are projected to receive decreases of 1.97 and 7.06 percent respectively. Hospitals with 0 to 25 percent Medicare utilization, or above 50 percent Medicare utilization, are projected to receive increases in uncompensated care payments. Hospitals with 25-50 percent Medicare utilization are projected to receive a decrease in uncompensated care payments.
5. Effects of Reductions Under the Hospital Readmissions Reduction Program for FY 2020
In section IV.G. of the preamble of this final rule, we discuss our proposed policies for the FY 2020 Hospital Readmissions Reduction Program. This program requires a reduction to a hospital's base operating DRG payment to account for excess readmissions of selected applicable conditions and procedures. The table and analysis in this final rule illustrate the estimated financial impact the Hospital Readmissions Reduction Program payment adjustment methodology by hospital characteristic. As outlined in section IV.G. of the preamble of this final rule, hospitals are stratified into quintiles based on the proportion of dual-eligible stays among Medicare fee-for-service (FFS) and managed care stays between July 1, 2015 and June 30, 2018 (that is, the FY 2020 Hospital Readmissions Reduction Program's performance period). Hospitals' excess readmission ratios (ERRs) are assessed relative to their peer group median and a neutrality modifier is applied in the payment adjustment factor calculation to maintain budget neutrality. To analyze the results by hospital characteristic, we used the FY 2020 Hospital IPPS Proposed Rule Impact File.
These analyses include 3,027 non-Maryland hospitals eligible to receive a penalty during the performance period. Hospitals are eligible to receive a penalty if they have 25 or more eligible discharges for at least one measure between July 1, 2015 and June 30, 2018. The second column in the table indicates the total number of non-Maryland hospitals with available data for each characteristic that have an estimated payment adjustment factor less than 1 (that is penalized hospitals).
The third column in the table indicates the percentage of penalized hospitals among those eligible to receive a penalty by hospital characteristic. For example, 82.80 percent of eligible hospitals characterized as non-teaching hospitals are expected to be penalized. Among teaching hospitals, 88.41 percent of eligible hospitals with fewer than 100 residents and 95.22 percent of eligible hospitals with 100 or more residents are expected to be penalized.
The fourth column in the table estimates the financial impact on hospitals by hospital characteristic. The table shows the share of penalties as a percentage of all base operating DRG payments for hospitals with each characteristic. This is calculated as the sum of penalties for all hospitals with that characteristic over the sum of all base operating DRG payments for those hospitals between October 1, 2017 and September 30, 2018 (FY 2018). For example, the penalty as a share of payments for urban hospitals is 0.69 percent. This means that total penalties for all urban hospitals are 0.69 percent of total payments for urban hospitals. Measuring the financial impact on hospitals as a percentage of total base operating DRG payments accounts for differences in the amount of base operating DRG payments for hospitals within the characteristic when comparing the financial impact of the program on different groups of hospitals.


6. Effects of Changes Under the FY 2020 Hospital Value-Based Purchasing (VBP) Program
In section IV.H. of the preamble of this final rule, we discuss the Hospital VBP Program under which the Secretary makes value-based incentive payments to hospitals based on their performance on measures during the performance period with respect to a fiscal year. These incentive payments will be funded for FY 2020 through a reduction to the FY 2020 base operating DRG payment amount for the discharge for the hospital for such fiscal year, as required by section 1886(o)(7)(B) of the Act. The applicable percentage for FY 2020 and subsequent years is 2 percent. The total amount available for value-based incentive payments must be equal to the total amount of reduced payments for all hospitals for the fiscal year, as estimated by the Secretary.
In section IV.H.1.b. of the preamble of this final rule, we estimate the available pool of funds for value-based incentive payments in the FY 2020 program year, which, in accordance with section 1886(o)(7)(C)(v) of the Act, will be 2.00 percent of base operating DRG payments, or a total of approximately $1.9 billion. This estimated available pool for FY 2020 is based on the historical pool of hospitals that were eligible to participate in the FY 2019 program year and the payment information from the March 2019 update to the FY 2018 MedPAR file.
The estimated impacts of the FY 2020 program year by hospital characteristic, found in the table in this section, are based on historical TPSs. We used the FY 2019 program year's TPSs to calculate the proxy adjustment factors used for this impact analysis. These are the most recently available scores that hospitals were given an opportunity to review and correct. The proxy adjustment factors use estimated annual base operating DRG payment amounts derived from the March 2019 update to the FY 2018 MedPAR file. The proxy adjustment factors can be found in Table 16A associated with this final rule (available via the internet on the CMS website).
The impact analysis shows that, for the FY 2020 program year, the number of hospitals that are expected to receive an increase in their base operating DRG payment amount is higher than the number of hospitals that are expected to receive a decrease. On average, among urban hospitals, hospitals in the West North Central region are expected to have the largest positive percent change in base operating DRG, and among rural hospitals, hospitals in the Mountain region are expected to have the largest positive percent change in base operating DRG. Urban Middle Atlantic, Urban East South Central, and Urban West South Central regions are expected to experience, on average, a decrease in base operating DRG. All other regions, both urban and rural, are expected to experience, on average, an increase in base operating DRG.
As DSH patient percentage increases, the average percent change in base operating DRG is expected to decrease. With respect to hospitals' Medicare utilization as a percent of inpatient days (MCR), as the MCR percent increases, the average percent change in base operating DRG is expected to increase. On average, teaching hospitals are expected to have a decrease in base operating DRG while non-teaching hospitals are expected to have an increase in base operating DRG.


Actual FY 2020 program year's TPSs will not be reviewed and corrected by hospitals until after this FY 2020 IPPS/LTCH PPS final rule has been published. Therefore, the same historical universe of eligible hospitals and corresponding TPSs from the FY 2019 program year were used for the updated impact analysis in this final rule.
7. Effects of Requirements Under the HAC Reduction Program for FY 2020
In section IV.I. of the preamble of this final rule, we discuss the requirements for the HAC Reduction Program for FY 2020. In this final rule, we are not removing measures or adopting any new measures into the HAC Reduction Program.
a. Burden Associated With Validation
We note the burden associated with collecting and submitting data via the NHSN system is captured under a separate OMB control number, 0920-0666 (expiration date November 30, 2021), and therefore will not impact our burden estimates.
We discuss the burden hours associated with NHSN HAI validation (43,200 hours over 600 hospitals) in section X.B.7. of the preamble of this final rule, and note the burden associated with these requirements is captured in an information collection request currently available for review and comment, OMB control number 0938-1352. We are updating our cost burden to hospitals using a wage plus benefit rate of $37.66 per hour to account for an increase in wage rate used in the last year's PRA package from $18.29 to $18.83. We believe that doubling the hourly wage rate ($18.83 × 2 = $37.66) to estimate total cost is a reasonably accurate estimation method. Accordingly, we calculate cost burden to hospitals using a wage plus benefits estimate of $37.66 per hour.
b. The Cumulative Effect of Program Measures and the Scoring Methodology
We are presenting the estimated impact of the FY 2020 Hospital-Acquired Condition (HAC) Reduction Program on hospitals by hospital characteristic. These FY 2020 HAC Reduction Program results were calculated using the Equal Measure Weights approach finalized in the FY 2019 IPPS/LTCH PPS Final Rule (83 FR 41486 through 41489). Each hospital's Total HAC Score was calculated as the equally weighted average of the hospital's measure scores. The table in this section presents the estimated proportion of hospitals in the worst-performing quartile of Total HAC Scores by hospital characteristic.
Hospitals' CMS Patient Safety Indicator (PSI) 90 measure results are based on Medicare fee-for-service (FFS) discharges from July 1, 2016 through June 30, 2018 and version 9.0 of the PSI software. Hospitals' measure results for Centers for Disease Control and Prevention (CDC) Central Line-Associated Bloodstream Infection (CLABSI), Catheter-Associated Urinary Tract Infection (CAUTI), Colon and Abdominal Hysterectomy Surgical Site Infection (SSI), Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia, and Clostridium difficile Infection (CDI) are derived from standardized infection ratios (SIRs) calculated with hospital surveillance data reported to the National Healthcare Safety Network (NHSN) for infections occurring between January 1, 2017 and December 31, 2018.
To analyze the results by hospital characteristic, we used the FY 2020 Proposed Rule Impact File. This table includes 3,169 non-Maryland hospitals with a FY 2020 Total HAC Score. Maryland hospitals and hospitals without a Total HAC Score are excluded from the table. Of these 3,169 hospitals, 3,154 hospitals had information for geographic location with bed size, Safety-net status, Disproportionate Share Hospital (DSH) percent, and teaching status; 3,168 had information on region, 3,126 had information for ownership; and 3,132 had information for Medicare Cost Report (MCR) percent. The first column presents a breakdown of each characteristic.
The second column in the table indicates the total number of non-Maryland hospitals with an FY 2020 Total HAC Score and available data for each characteristic. For example, with regard to teaching status, 2,058 hospitals are characterized as non-teaching hospitals, 845 are characterized as teaching hospitals with fewer than 100 residents, and 251 are characterized as teaching hospitals with at least 100 residents. This only represents a total of 3,154 hospitals because the other 15 hospitals are missing from the FY 2020 Proposed Rule Impact File.
The third column in the table indicates the number of hospitals for each characteristic that would be in the worst-performing quartile of Total HAC Scores. These hospitals would receive a payment reduction under the FY 2020 HAC Reduction Program. For example, with regard to teaching status, 449 hospitals out of 2,058 hospitals characterized as non-teaching hospitals would be subject to a payment reduction. Among teaching hospitals, 211 out of 845 hospitals with fewer than 100 residents and 121 out of 251 hospitals with 100 or more residents would be subject to a payment reduction.
The fourth column in the table indicates the proportion of hospitals for each characteristic that would be in the worst-performing quartile of Total HAC Scores and thus receive a payment reduction under the FY 2020 HAC Reduction Program. For example, 21.9 percent of the 2,058 hospitals characterized as non-teaching hospitals, 25.0 percent of the 845 teaching hospitals with fewer than 100 residents, and 48.2 percent of the 251 teaching hospitals with 100 or more residents would be subject to a payment reduction.


8. Effects of Changes Related to Critical Access Hospitals (CAHs) as Nonproviders for Direct GME and IME Payment Purposes
In section IV.J.2. of the preamble of this final rule, we discuss our finalized policy to consider CAHs as nonprovider settings for purposes of direct GME and IME payments such that, effective with portions of cost reporting periods beginning October 1, 2019, a hospital may include full-time equivalent (FTE) residents training at a CAH in its FTE count as long as it meets the nonprovider setting requirements currently included at 42 CFR 413.78(g) (and the corresponding IME regulation at 42 CFR 412.105(f)(1)(ii)(E)). We note that we are not changing our policy with respect to CAHs incurring the costs of training residents. That is, a CAH may continue to incur the costs of training residents in an approved residency training program(s) and be paid based on 101 percent of the reasonable costs for these training costs.
We anticipate any impact associated with this change to be negligible. Because IPPS teaching hospitals have caps in place for the number of FTE residents they may claim for direct GME and IME payment purposes, these hospitals can only receive direct GME and IME payments for the FTE residents for which they incur the training costs at CAHs within their existing FTE caps. Allowing IPPS hospitals to claim FTE residents training at CAHs will not mean the hospitals will be able to claim additional FTE residents above their FTE caps. Thus, because no additional funded slots will be created for IPPS hospitals by this policy, and because CAHs will no longer be claiming and receiving payment for the salary costs of the residents in situations where the CAHs are being treated as nonprovider sites, we believe there is minimal to no impact.
9. Effects of Implementation of the Rural Community Hospital Demonstration Program in FY 2020
In section IV.K of the preamble of this final rule for FY 2020, we discussed our implementation and budget neutrality methodology for section 410A of Public Law 108-173, as amended by sections 3123 and 10313 of Public Law 111-148, and more recently, by section 15003 of Public Law 114-255, which requires the Secretary to conduct a demonstration that would modify payments for inpatient services for up to 30 rural hospitals.
Section 15003 of Public Law 114-255 requires the Secretary to conduct the Rural Community Hospital Demonstration for a 10-year extension period (in place of the 5-year extension period required by the Affordable Care Act), beginning on the date immediately following the last day of the initial 5-year period under section 410A(a)(5) of Public Law 108-173. Specifically, section 15003 of Public Law 114-255 amended section 410A(g)(4) of Public Law 108-173 to require that, for hospitals participating in the demonstration as of the last day of the initial 5-year period, the Secretary shall provide for continued participation of such rural community hospitals in the demonstration during the 10-year extension period, unless the hospital makes an election to discontinue participation. Furthermore, section 15003 of Public Law 114-255 requires that, during the second 5 years of the 10-year extension period, the Secretary shall provide for participation under the demonstration during the second 5 years of the 10 year extension period for hospitals that are not described in subsection 410A(g)(4).
Section 15003 of Public Law 114-255 also requires that no later than 120 days after enactment of Public Law 114-255 that the Secretary issue a solicitation for applications to select additional hospitals to participate in the demonstration program for the second 5 years of the 10-year extension period so long as the maximum number of 30 hospitals stipulated by Public Law 111-148 is not exceeded. Section 410A(c)(2) requires that in conducting the demonstration program under this section, the Secretary shall ensure that the aggregate payments made by the Secretary do not exceed the amount which the Secretary would have paid if the demonstration program under this section was not implemented (budget neutrality).
In the preamble to this IPPS/LTCH PPS final rule, we described the terms of participation for the extension period authorized by Public Law 114-255. In the FY 2018 IPPS/LTCH PPS final rule, we finalized our policy with regard to the effective date for the application of the reasonable cost-based payment methodology under the demonstration for those among the hospitals that had previously participated and were choosing to participate in the second 5-year extension period. According to our finalized policy, each of these previously participating hospitals began the second 5 years of the 10-year extension period on the date immediately after the date the period of performance under the 5-year extension period ended. Seventeen of the 21 hospitals that completed their periods of participation under the extension period authorized by the Affordable Care Act elected to continue in the second 5-year extension period, while 13 additional hospitals were selected to participate. One of the hospitals selected in 2017 withdrew from the demonstration prior to beginning participation on July 1, 2018, and, in addition, one among the previously participating hospitals closed effective January 2019. Each of the remaining newly participating hospitals began its 5-year period of participation effective the start of the first cost reporting period on or after October 1, 2017. Thus, 28 hospitals are scheduled to participate in FY 2020.
In the FY 2018 IPPS/LTCH PPS final rule, we finalized the budget neutrality methodology in accordance with our policies for implementing the demonstration, adopting the general methodology used in previous years, whereby we estimated the additional payments made by the program for each of the participating hospitals as a result of the demonstration. In order to achieve budget neutrality, we adjusted the national IPPS rates by an amount sufficient to account for the added costs of this demonstration. In other words, we have applied budget neutrality across the payment system as a whole rather than across the participants of this demonstration. The language of the statutory budget neutrality requirement permits the agency to implement the budget neutrality provision in this manner. The statutory language requires that aggregate payments made by the Secretary do not exceed the amount which the Secretary would have paid if the demonstration was not implemented, but does not identify the range across which aggregate payments must be held equal.
For this final rule, the resulting amount applicable to FY 2020 is $60,972,359, which we are including in the budget neutrality offset adjustment for FY 2020. This estimated amount is based on the specific assumptions regarding the data sources used, that is, recently available “as submitted” cost reports and historical and currently finalized update factors for cost and payment.
In previous years, we have incorporated a second component into the budget neutrality offset amounts identified in the final IPPS rules. As finalized cost reports became available, we determined the amount by which the actual costs of the demonstration for an earlier, given year differed from the estimated costs for the demonstration set forth in the final IPPS rule for the corresponding fiscal year, and we incorporated that amount into the budget neutrality offset amount for the upcoming fiscal year. We have calculated this difference for FYs 2005 through 2013 between the actual costs of the demonstration as determined from finalized cost reports once available, and estimated costs of the demonstration as identified in the applicable IPPS final rules for these years.
With the extension of the demonstration for another 5-year period, as authorized by section 15003 of Public Law 114-255, we will continue this general procedure. Finalized cost reports are now available for the 22 and 21 hospitals that completed a cost reporting period according to the demonstration cost-based payment methodology beginning in FYs 2014 and 2015, respectively. The actual costs of the demonstration for FY 2014 as determined from the finalized cost reports fell short of the estimated amount that was finalized in the FY 2014 IPPS/LTCH PPS final rule by $14,932,060; the actual costs of the demonstration for FY 2015 determined from finalized cost reports fell short of the estimated amount finalized in the FY 2015 IPPS/LTCH PPS final rule by $20,297,477.
We note that, for this final rule, the amounts identified for the actual costs of the demonstration for each of FYs 2014 and 2015 (determined from finalized cost reports) is less than the amount that was identified in the final rule for the corresponding fiscal year. Therefore, in keeping with previous policy finalized in similar situations when the costs of the demonstration fell short of the amount estimated in the corresponding year's final rule, we will be including this component, respective to each of FYs 2014 and 2015, as a negative adjustment to the budget neutrality offset amount for the current fiscal year.
Therefore, for FY 2020, the total amount that we are applying to the national IPPS rates is $25,742,822.
10. Effects of Change Related to CAH Payment for Ambulance Services
In section VI.C.2. of the preamble of this final rule, we discuss our decision to finalize the proposed revisions to the regulations at § 413.70(b)(5) by adding a new paragraph (D) to state that, effective for cost reporting periods beginning on or after October 1, 2019, payment for ambulance services furnished by a CAH or by an entity that is owned and operated by a CAH is 101 percent of the reasonable costs of the CAH or the entity in furnishing those services, but only if the CAH or the entity is the only provider or supplier of ambulance services located within a 35-mile drive of the CAH, excluding ambulance providers or suppliers that are not legally authorized to furnish ambulance services to transport individuals either to or from the CAH. Consistent with the existing policy under § 413.70(b)(5)(i)(C), if there is no provider or supplier of ambulance services located within a 35-mile drive of the CAH and there is an entity that is owned and operated by a CAH that is more than a 35-mile drive from the CAH, payment for ambulance services furnished by that entity is 101 percent of the reasonable costs of the entity in furnishing those services, but only if the entity is the closest provider or supplier of ambulance services to the CAH. We are also finalizing the proposed conforming change to § 413.70(b)(5)(i)(C), which will make that provision effective only for cost reporting periods starting on or before September 30, 2019.
Based on the best data available, assuming no significant change in the volume of CAH ambulance trips and that approximately 5 CAHs may be affected by the specific situation addressed by our revised policy under § 413.70(b)(5)(i)(D), we estimate Medicare payments will increase by approximately $2 million in FY 2020 as compared to FY 2019.
11. Effects of Continued Implementation of the Frontier Community Health Integration Project (FCHIP) Demonstration
In section VI.C.3. of the preamble of this final rule, we discuss the implementation of the FCHIP demonstration, which allows eligible entities to develop and test new models for the delivery of health care services in eligible counties in order to improve access to and better integrate the delivery of acute care, extended care, and other health care services to Medicare beneficiaries in no more than four States. Budget neutrality estimates for the demonstration will be based on the demonstration period of August 1, 2016 through July 31, 2019. The demonstration includes three intervention prongs, under which specific waivers of Medicare payment rules will allow for enhanced payment: Telehealth, skilled nursing facility/nursing facility services, and ambulance services. These waivers are being implemented with the goal of increasing access to care with no net increase in costs. (We initially addressed this demonstration in the FY 2017 IPPS/LTCH PPS final rule (81 FR 57064 through 57065), FY 2018 IPPS/LTCH PPS final rule (82 FR 38294 through 38296) and FY 2019 IPPS/LTCH PPS final rule (83 FR 41516 through 41517).)
We specified the payment enhancements for the demonstration and selected CAHs for participation with the goal of maintaining the budget neutrality of the demonstration on its own terms (that is, the demonstration will produce savings from reduced transfers and admissions to other health care providers, thus offsetting any increase in payments resulting from the demonstration). However, because of the small size of this demonstration program and uncertainty associated with projected Medicare utilization and costs, in the FY 2019 IPPS/LTCH PPS final rule we adopted a contingency plan (83 FR 41516 through 41517) to ensure that the budget neutrality requirement in section 123 of Public Law 110-275 is met. Accordingly, if analysis of claims data for the Medicare beneficiaries receiving services at each of the participating CAHs, as well as of other data sources, including cost reports, shows that increases in Medicare payments under the demonstration during the 3-year period are not sufficiently offset by reductions elsewhere, we will recoup the additional expenditures attributable to the demonstration through a reduction in payments to all CAHs nationwide. The demonstration is projected to impact payments to participating CAHs under both Medicare Part A and Part B. Thus, in the event that we determine that aggregate payments under the demonstration exceed the payments that would otherwise have been made, CMS will recoup payments through reductions of Medicare payments to all CAHs under both Medicare Part A and Part B.
Because of the small scale of the demonstration, it would not be feasible to implement budget neutrality by reducing payments only to the participating CAHs. Therefore, we will make the reduction to payments to all CAHs, not just those participating in the demonstration, because the FCHIP demonstration is specifically designed to test innovations that affect delivery of services by this provider category. As we explained in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41516 through 41517), we believe that the language of the statutory budget neutrality requirement at section 123(g)(1)(B) of the Act permits the agency to implement the budget neutrality provision in this manner. The statutory language merely refers to ensuring that aggregate payments made by the Secretary do not exceed the amount which the Secretary estimates would have been paid if the demonstration project was not implemented, and does not identify the range across which aggregate payments must be held equal.
Given the 3-year period of performance of the FCHIP demonstration and the time needed to conduct the budget neutrality analysis, in the event the demonstration is found not to have been budget neutral, we plan to recoup any excess costs over a period of three cost report periods, beginning in FY 2021. Therefore, this policy has no impact for any national payment system for FY 2020.
I. Effects of Changes in the Capital IPPS
1. General Considerations
For the impact analysis presented below, we used data from the March 2019 update of the FY 2018 MedPAR file and the March 2019 update of the Provider-Specific File (PSF) that was used for payment purposes. Although the analyses of the changes to the capital prospective payment system do not incorporate cost data, we used the March 2019 update of the most recently available hospital cost report data (FYs 2016 and 2017) to categorize hospitals. Our analysis has several qualifications. We use the best data available and make assumptions about case-mix and beneficiary enrollment, as described later in this section.
Due to the interdependent nature of the IPPS, it is very difficult to precisely quantify the impact associated with each change. In addition, we draw upon various sources for the data used to categorize hospitals in the tables. In some cases (for instance, the number of beds), there is a fair degree of variation in the data from different sources. We have attempted to construct these variables with the best available sources overall. However, it is possible that some individual hospitals are placed in the wrong category.
Using cases from the March 2019 update of the FY 2018 MedPAR file, we simulated payments under the capital IPPS for FY 2019 and the payments for FY 2020 for a comparison of total payments per case. Short-term, acute care hospitals not paid under the general IPPS (for example, hospitals in Maryland) are excluded from the simulations.
The methodology for determining a capital IPPS payment is set forth at § 412.312. The basic methodology for calculating the capital IPPS payments in FY 2020 is as follows:
(Standard Federal rate) × (DRG weight) × (GAF) × (COLA for hospitals located in Alaska and Hawaii) × (1 + DSH adjustment factor + IME adjustment factor, if applicable).
In addition to the other adjustments, hospitals may receive outlier payments for those cases that qualify under the threshold established for each fiscal year. We modeled payments for each hospital by multiplying the capital Federal rate by the GAF and the hospital's case-mix. Then we added estimated payments for indirect medical education, disproportionate share, and outliers, if applicable. For purposes of this impact analysis, the model includes the following assumptions:
- An estimated increase in the Medicare case-mix index of 0.5 percent in FY 2019 and 0.5 percent in FY 2020 based on preliminary FY 2019 data.
- We estimate that Medicare discharges will be approximately 10.8 million in both FYs 2019 and 2020.
- The capital Federal rate was updated, beginning in FY 1996, by an analytical framework that considers changes in the prices associated with capital-related costs and adjustments to account for forecast error, changes in the case-mix index, allowable changes in intensity, and other factors. As discussed in section III.A.1.a. of the Addendum to this final rule, the update to the capital Federal rate is 1.5 percent for FY 2020.
- In addition to the FY 2020 update factor, the FY 2020 capital Federal rate was calculated based on a GAF/DRG budget neutrality adjustment factor of 0.9956 and a outlier adjustment factor of 0.9461.
2. Results
We used the actuarial model previously described in section I.I. of Appendix A of this final rule to estimate the potential impact of the changes for FY 2020 on total capital payments per case, using a universe of 3,239 hospitals. As previously described, the individual hospital payment parameters are taken from updated data, including the March 2019 update of the FY 2018 MedPAR file, the March 2019 update to the PSF, and the cost report data from the March 2019 update of HCRIS. In Table III, we present a comparison of estimated total payments per case for FY 2019 and estimated total payments per case for FY 2020 based on the FY 2020 payment policies. Column 2 shows estimates of payments per case under our model for FY 2019. Column 3 shows estimates of payments per case under our model for FY 2020. Column 4 shows the total percentage change in payments from FY 2019 to FY 2020. The change represented in Column 4 includes the 1.5 percent update to the capital Federal rate and other changes in the adjustments to the capital Federal rate. The comparisons are provided by: (1) Geographic location; (2) region; and (3) payment classification.
The simulation results show that, on average, capital payments per case in FY 2020 are expected to increase, as compared to capital payments per case in FY 2019. This expected increase, overall, is largely due to the 1.5 percent update to the capital Federal rate for FY 2020. In general, regional variations in estimated capital payments per case in FY 2020 as compared to capital payments per case in FY 2019 are primarily due to changes in the GAFs, and are generally consistent with the projected changes in payments due to changes in the wage index (and policies affecting the wage index), as shown in Table I in section I.G. of this Appendix A.
The net impact of these changes is an estimated 1.4 percent change in capital payments per case from FY 2019 to FY 2020 for all hospitals (as shown in Table III).
The geographic comparison shows that, on average, hospitals in both urban and rural classifications will experience an increase in capital IPPS payments per case in FY 2020 as compared to FY 2019. Capital IPPS payments per case will increase by an estimated 1.4 percent for hospitals in large urban areas and by 1.2 percent for hospitals in other urban areas, while payments to hospitals in rural areas will increase by 2.0 percent in FY 2019 to FY 2020.
The comparisons by region show that the estimated changes in capital payments per case from FY 2019 to FY 2020 in urban areas range from a 1.3 percent decrease for the New England region to a 2.5 percent increase for the East South Central region. Similarly, for rural regions, the East South Central rural region is projected to experience an increase in capital IPPS payments per case of 3.1 percent, while the New England rural region is projected to decrease 0.6 percent. These regional differences are primarily due to the changes in the GAFs resulting from the changes we are adopting to the wage index to address wage index disparities. (As explained in section III.A.3. of the Addendum to this final rule, these finalized policies directly affect the GAF because the GAFs are calculated based on the hospital wage index value that is applicable to the hospital under 42 CFR part 412, subpart D which governs the methodology for determining the operating IPPS payments.) As discussed in section III.N of the preamble of this final rule, hospitals with a wage index value below the 25th percentile wage index value will receive an increase to their wage index value of half the difference between the otherwise applicable final wage index value for a year for that hospital and the 25th percentile wage index value for that year across all hospitals; urban to rural reclassifications are no longer included in the rural floor calculation; and any decrease in a hospital's wage index from the hospital's final wage index in FY 2019 is capped at 5-percent. We note that application of the lowest quartile wage index adjustment results in regions with hospitals that have the lowest wage index values generally projected to experience the largest increases in payment. Hospitals of all types of ownership (that is, voluntary hospitals, government hospitals, and proprietary hospitals) are expected to experience an increase in capital payments per case from FY 2019 to FY 2020. The projected increase in capital payments for voluntary hospitals is estimated to be 1.3 percent compared with an increase of 1.5 percent for proprietary hospitals. Government hospitals are expected to experience an increase in capital IPPS payments of 1.6 percent.
Section 1886(d)(10) of the Act established the MGCRB. Hospitals may apply for reclassification for purposes of the wage index for FY 2020. Reclassification for wage index purposes also affects the GAFs because that factor is constructed from the hospital wage index. To present the effects of the hospitals being reclassified, as of the publication of this final rule for FY 2020, we show the average capital payments per case for reclassified hospitals for FY 2020. Urban reclassified hospitals are expected to experience an increase in capital payments of 1.2 percent; urban nonreclassified hospitals are expected to experience an increase in capital payments of 1.5 percent. The estimated percentage increase for rural reclassified hospitals is 1.7 percent, and for rural nonreclassified hospitals, the estimated percentage increase in capital payments is 2.7 percent. This variation is largely due to the effect of changes in the GAF on capital payments for these hospitals.


J. Effects of Payment Rate Changes and Policy Changes Under the LTCH PPS
1. Introduction and General Considerations
In section VII. of the preamble of this final rule and section V. of the Addendum to this final rule, we set forth the annual update to the payment rates for the LTCH PPS for FY 2020. In the preamble of this final rule, we specify the statutory authority for the provisions that are presented, identify the policies for FY 2020, and present rationales for our decisions as well as alternatives that were considered. In this section of Appendix A to this final rule, we discuss the impact of the changes to the payment rate, factors, and other payment rate policies related to the LTCH PPS that are presented in the preamble of this final rule in terms of their estimated fiscal impact on the Medicare budget and on LTCHs.
There are 384 LTCHs included in this impact analysis. We note that, although there are currently approximately 392 LTCHs, for purposes of this impact analysis, we excluded the data of all-inclusive rate providers consistent with the development of the FY 2020 MS-LTC-DRG relative weights (discussed in section VII.B.3.c. of the preamble of this final rule. Moreover, in the claims data used for this final rule, 2 of these 384 LTCHs only have claims for site neutral payment rate cases and, therefore, do not affect our impact analysis for LTCH PPS standard Federal payment rate cases.) In the impact analysis, we used the payment rate, factors, and policies presented in this final rule, the 2.5 percent annual update to the LTCH PPS standard Federal payment rate, the one-time budget neutrality adjustment factor for the estimated cost of eliminating the 25-percent threshold policy in FY 2020 as discussed in section VII.D. of the preamble of this final rule, the update to the MS-LTC-DRG classifications and relative weights, the update to the wage index values and labor-related share, and the best available claims and CCR data to estimate the change in payments for FY 2020.
Under the dual rate LTCH PPS payment structure, payment for LTCH discharges that meet the criteria for exclusion from the site neutral payment rate (that is, LTCH PPS standard Federal payment rate cases) is based on the LTCH PPS standard Federal payment rate. Consistent with the statute, the site neutral payment rate is the lower of the IPPS comparable per diem amount as determined under § 412.529(d)(4), including any applicable outlier payments as specified in § 412.525(a), reduced by 4.6 percent for FYs 2018 through 2026; or 100 percent of the estimated cost of the case as determined under § 412.529(d)(2). In addition, there are two separate high cost outlier targets—one for LTCH PPS standard Federal payment rate cases and one for site neutral payment rate cases. The statute also establishes a transitional payment method for cases that are paid the site neutral payment rate for LTCH discharges occurring in cost reporting periods beginning during FY 2016 through FY 2019. The transitional payment amount for site neutral payment rate cases is a blended payment rate, which is calculated as 50 percent of the applicable site neutral payment rate amount for the discharge as determined under § 412.522(c)(1) and 50 percent of the applicable LTCH PPS standard Federal payment rate for the discharge determined under § 412.523. For FY 2020, the applicability of this transitional payment method for site neutral payment rate cases is dependent upon both the discharge date of the case and the start date of the LTCH's FY 2019 cost reporting period. Specifically, the transitional payment method only applies to those site neutral payment rate cases whose discharges occur during a LTCH's cost reporting period that begins before October 1, 2019. While the transitional payment amount for site neutral payment rate cases is a blended payment rate determined under § 412.522(c)(3), site neutral payment rate cases whose discharges from an LTCH occur during the LTCH's cost reporting period that begins on or after October 1, 2019 are paid the site neutral payment rate amount determined under § 412.522(c)(1).
Based on the best available data for the 384 LTCHs in our database that were considered in the analyses used for this final rule, we estimate that overall LTCH PPS payments in FY 2020 will increase by approximately 1.0 percent (or approximately $43 million) based on the rates and factors presented in section VII. of the preamble and section V. of the Addendum to this final rule.
The statutory transitional payment method for cases that are paid the site neutral payment rate for LTCH discharges occurring in cost reporting periods beginning during FY 2018 or FY 2019 uses a blended payment rate, which is determined as 50 percent of the site neutral payment rate amount for the discharge and 50 percent of the LTCH PPS standard Federal prospective payment rate amount for the discharge (§ 412.522(c)(3)). Therefore, when estimating FY 2019 LTCH PPS payments for site neutral payment rate cases for this impact analysis, the transitional blended payment rate was applied to all such cases because all discharges in FY 2019 are either in the LTCH's cost reporting period that began during FY 2018 or in the LTCH's cost reporting period that will begin during FY 2019. However, when estimating FY 2020 LTCH PPS payments for site neutral payment rate cases for this impact analysis, because the statute specifies that the site neutral payment rate effective date for a given LTCH is based on the date that the LTCH's cost reporting period begins during FY 2020, we included an adjustment to account for this rolling effective date, consistent with the general approach used for the LTCH PPS impact analysis presented in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49831). This approach accounts for the fact that site neutral payment rate cases in FY 2019 that are in an LTCH's cost reporting period that begins before October 1, 2019 continue to be paid under the transitional payment method until the start of the LTCH's first cost reporting period beginning on or after October 1, 2019. Site neutral payment rate cases whose discharges from LTCHs occurring during an LTCH's cost reporting period that begins on or after October 1, 2019 will no longer be paid under the transitional payment method and will instead be paid the site neutral payment rate amount as determined under § 412.522(c)(1).
For purposes of this impact analysis, to estimate total FY 2020 LTCH PPS payments for site neutral payment rate cases, as we proposed, we used the same general approach as was used in the FY 2016 IPPS/LTCH PPS final rule with modifications to account for the rolling end date to the transitional blended payment rate in FY 2020 instead of the rolling effective date for implementation of the transitional site neutral payment rate in FY 2016. In summary, under this approach, we grouped LTCHs based on the quarter their cost reporting periods will begin during FY 2020. For example, LTCHs with cost reporting periods that begin during October through December 2019 are grouped to site neutral payment rate cases whose discharges will occur during the first quarter of FY 2020. For LTCHs grouped in each quarter of FY 2020, we modeled those LTCHs' estimated FY 2020 site neutral payment rate payments under the transitional blended payment rate based on the quarter in which the LTCHs in each group will continue to be paid the transitional payment method for the site neutral payment rate cases.
For purposes of this estimate, then, we assume the cost reporting period is the same for all LTCHs in each of the quarterly groups and that this cost reporting period begins on the first day of that quarter. (For example, our first group consists of 37 LTCHs whose cost reporting period will begin in the first quarter of FY 2020 so that, for purposes of this estimate, we assume all 37 LTCHs will begin their FY 2020 cost reporting period on October 1, 2019.) Second, we estimated the proportion of FY 2020 site neutral payment rate cases in each of the quarterly groups, and we then assume this proportion is applicable for all four quarters of FY 2020. (For example, as discussed in more detail below, we estimate the first quarter group will discharge 7.0 percent of all FY 2020 site neutral payment rate cases and, therefore, we estimate that group of LTCHs will discharge 7.0 percent of all FY 2018 site neutral payment rate cases in each quarter of FY 2020.) Then, we modeled estimated FY 2020 payments on a quarterly basis under the LTCH PPS standard Federal payment rate based on the assumptions described above. We continue to believe that this approach is a reasonable means of taking the rolling effective date into account when estimating FY 2020 payments.
Based on the fiscal year begin date information in the March 2019 update of the PSF and the LTCH claims from the March 2019 update of the FY 2018 MedPAR files for the 384 LTCHs in our database used for this final rule, we found the following: 7.0 percent of site neutral payment rate cases are from 37 LTCHs whose cost reporting periods will begin during the first quarter of FY 2020; 23.4 percent of site neutral payment rate cases are from 94 LTCHs whose cost reporting periods will begin in the second quarter of FY 2020; 9.2 percent of site neutral payment rate cases are from 52 LTCHs whose cost reporting periods will begin in the third quarter of FY 2020; and 60.3 percent of site neutral payment rate cases are from 201 LTCHs whose cost reporting periods will begin in the fourth quarter of FY 2020. Therefore, the following percentages apply in the approach described above:
- First Quarter FY 2020: 7.0 percent of site neutral payment rate cases (that is, the percentage of discharges from LTCHs whose FY 2020 cost reporting period will begin in the first quarter of FY 2020) are no longer eligible for the transitional blended payment method, while the remaining 93.0 percent of site neutral payment rate discharges are eligible to be paid under the transitional payment method.
- Second Quarter FY 2020: 30.4 percent of site neutral payment rate second quarter discharges (that is, the percentage of discharges from LTCHs whose FY 2020 cost reporting period will begin in the first or second quarter of FY 2020) are no longer eligible for the transitional blended payment method, while the remaining 69.6 percent of site neutral payment rate second quarter discharges are eligible to be paid under the transitional payment method.
- Third Quarter FY 2020: 39.7 percent of site neutral payment rate third quarter discharges (that is, the percentage of discharges from LTCHs whose FY 2020 cost reporting period will begin in the first, second, or third quarter of FY 2020) are no longer eligible for the transitional blended payment method while the remaining 60.3 percent of site neutral payment rate third quarter discharges are eligible to be paid under the transitional payment method.
- Fourth Quarter FY 2020: 100.0 percent of site neutral payment rate fourth quarter discharges (that is, the percentage of discharges from LTCHs whose FY 2020 cost reporting period will begin in the first, second, third, or fourth quarter of FY 2020) are no longer eligible for the transitional blended payment method.
Based on the FY 2018 LTCH cases that were used for the analysis in this final rule, approximately 29 percent of those cases were classified as site neutral payment rate cases (that is, 29 percent of LTCH cases did not meet the patient-level criteria for exclusion from the site neutral payment rate). Our Office of the Actuary currently estimates that the percent of LTCH PPS cases that will be paid at the site neutral payment rate in FY 2020 will not change significantly from the most recent historical data. Taking into account the transitional blended payment rate and other changes that will apply to the site neutral payment rate cases in FY 2020, we estimate that aggregate LTCH PPS payments for these site neutral payment rate cases will decrease by approximately 5.9 percent (or approximately $49 million).
Comment: Some commenters expressed concern that the payment-to-cost differential for site neutral payment rate cases, which they estimate to have decreased from 78 percent in FY 2017 to 46 percent in FY 2020, represents an “inappropriate underpayment of site-neutral cases”. These commenters stated that CMS should address the “chronic and substantial underpayment of site-neutral cases and its impact on patients seeking medically necessary LTCH services at the site-neutral level.” Moreover, as discussed in section V.D.4. of the Addendum of this final rule, these commenters expressed their belief that this payment-to-cost differential, among other reasons, invalidates our assumptions that site neutral payment rate discharges are expected to mirror comparable IPPS discharges.
Response: With respect to commenters' claims that the site neutral payment rate represents a “chronic and substantial underpayment”, we remind readers that the site neutral payment rate is statutory. In explicitly defining the site neutral payment rate, the statute does so without regard to payment-to-cost ratios. For these reasons and as we discuss in greater detail section V.D.4. of the Addendum of this final rule, we believe Medicare's payment for those cases is appropriate. As we also discuss in section V.D.4. of the Addendum of this final rule, we continue to believe the site neutral payment rate will not negatively impact access to or quality of care for Medicare beneficiaries given that general acute care hospitals are effectively providing treatment for the same types of patients. We respond to the comments regarding our assumptions that site neutral discharges will mirror comparable IPPS discharges in our discussion of the establishment of the HCO threshold for site neutral cases while the blended payment rate remains in effect, and we refer readers to section V.D.4. of the Addendum of this final rule for that full discussion.
For this final rule, we expect approximately 71 percent of LTCH cases to meet the patient-level criteria for exclusion from the site neutral payment rate in FY 2020, and will be paid based on the LTCH PPS standard Federal payment rate for the full year. We estimate that total LTCH PPS payments for these LTCH PPS standard Federal payment rate cases in FY 2020 will increase approximately 2.7 percent (or approximately $91 million). This estimated increase in LTCH PPS payments for LTCH PPS standard Federal payment rate cases in FY 2020 is primarily due to the 2.5 percent annual update to the LTCH PPS standard Federal payment rate for FY 2020 and the projected 0.2 percent increase in high cost outlier payments discussed in section V.D.3.b.(3). of the Addendum to this final rule.
Based on the 384 LTCHs that were represented in the FY 2018 LTCH cases that were used for the analyses in this final rule presented in this Appendix, we estimate that aggregate FY 2019 LTCH PPS payments will be approximately $4.271 billion, as compared to estimated aggregate FY 2020 LTCH PPS payments of approximately $4.314 billion, resulting in an estimated overall increase in LTCH PPS payments of approximately $43 million. We note that the estimated $43 million increase in LTCH PPS payments in FY 2020 does not reflect changes in LTCH admissions or case-mix intensity, which will also affect the overall payment effects of the policies in this final rule.
The LTCH PPS standard Federal payment rate for FY 2019 is $41,558.68. For FY 2020, we are establishing an LTCH PPS standard Federal payment rate of $42,677.64 which reflects the 2.5 percent annual update to the LTCH PPS standard Federal payment rate, the incremental change in the one-time budget neutrality adjustment factor of 0.999858 for eliminating the 25-percent threshold policy in FY 2020 as discussed in section VII.D. of the preamble of this final rule, and the area wage budget neutrality factor of 1.0020203 to ensure that the changes in the wage indexes and labor-related share do not influence aggregate payments. For LTCHs that fail to submit data for the LTCH QRP, in accordance with section 1886(m)(5)(C) of the Act, we are establishing an LTCH PPS standard Federal payment rate of $41,844.90. This LTCH PPS standard Federal payment rate reflects the updates and factors previously described, as well as the required 2.0 percentage point reduction to the annual update for failure to submit data under the LTCH QRP. We note that the factors previously described to determine the FY 2020 LTCH PPS standard Federal payment rate are applied to the FY 2019 LTCH PPS standard Federal rate set forth under § 412.523(c)(3)(xiv) (that is, $41,558.68).
Table IV shows the estimated impact for LTCH PPS standard Federal payment rate cases. The estimated change attributable solely to the annual update of 2.5 percent to the LTCH PPS standard Federal payment rate is projected to result in an increase of 2.4 percent in payments per discharge for LTCH PPS standard Federal payment rate cases from FY 2019 to FY 2020, on average, for all LTCHs (Column 6). In addition to the annual update to the LTCH PPS standard Federal payment rate for FY 2020, the estimated increase of 2.4 percent shown in Column 6 of Table IV also includes estimated payments for short-stay outlier (SSO) cases, a portion of which are not affected by the annual update to the LTCH PPS standard Federal payment rate, as well as the reduction that is applied to the annual update for LTCHs that do not submit the required LTCH QRP data. Therefore, for all hospital categories, the projected increase in payments based on the LTCH PPS standard Federal payment rate to LTCH PPS standard Federal payment rate cases is somewhat less than the 2.5 percent annual update for FY 2020.
For FY 2020, we are updating the wage index values based on the most recent available data (data from cost reporting periods beginning during FY 2016 which is the same data used for the FY 2020 acute care hospital IPPS), and we are continuing to use labor market areas based on the CBSA delineations (as discussed in section V.B. of the Addendum to this final rule). In addition, the labor-related share will be 66.3 percent under the LTCH PPS for FY 2020, based on the most recent available data (IGI's second quarter 2019 forecast) on the relative importance of the labor-related share of operating and capital costs of the 2013-based LTCH market basket. We also are applying an area wage level budget neutrality factor of 1.0020203 to ensure that the changes to the wage data and labor-related share do not result in any change in estimated aggregate LTCH PPS payments to LTCH PPS standard Federal payment rate cases.
We currently estimate total high cost outlier payments for LTCH PPS standard Federal payment rate cases will increase from FY 2019 to FY 2020. Based on the FY 2018 LTCH cases that were used for the analyses in this final rule, we estimate that the FY 2019 high cost outlier threshold of $27,121 (as established in the FY 2019 IPPS/LTCH PPS final rule correction notice) will result in estimated high cost outlier payments for LTCH PPS standard Federal payment rate cases in FY 2019 that are projected to fall slightly below the 7.975 percent target. Specifically, we currently estimate that high cost outlier payments for LTCH PPS standard Federal payment rate cases will be approximately 7.74 percent of the estimated total LTCH PPS standard Federal payment rate payments in FY 2019. Combined with our estimate that FY 2020 high cost outlier payments for LTCH PPS standard Federal payment rate cases will be 7.975 percent of estimated total LTCH PPS standard Federal payment rate payments in FY 2020, this will result in an estimated increase in high cost outlier payments of approximately 0.2 percent between FY 2019 and FY 2020. We note that, consistent with past practice, in calculating these estimated high cost outlier payments, we increased estimated costs by an inflation factor of 5.5 percent (determined by the Office of the Actuary) to update the FY 2018 costs of each case to FY 2020.
Table IV shows the estimated impact of the payment rate and policy changes on LTCH PPS payments for LTCH PPS standard Federal payment rate cases for FY 2020 by comparing estimated FY 2019 LTCH PPS payments to estimated FY 2020 LTCH PPS payments. (As noted earlier, our analysis does not reflect changes in LTCH admissions or case-mix intensity.) We note that these impacts do not include LTCH PPS site neutral payment rate cases for the reasons discussed in section I.J.4. of this Appendix.
As we discuss in detail throughout this final rule, based on the most recent available data, we believe that the provisions of this final rule relating to the LTCH PPS, which are projected to result in an overall increase in estimated aggregate LTCH PPS payments, and the resulting LTCH PPS payment amounts will result in appropriate Medicare payments that are consistent with the statute.
2. Impact on Rural Hospitals
For purposes of section 1102(b) of the Act, we define a small rural hospital as a hospital that is located outside of an urban area and has fewer than 100 beds. As shown in Table IV, we are projecting a 2.7 percent increase in estimated payments for LTCH PPS standard Federal payment rate cases for LTCHs located in a rural area. This estimated impact is based on the FY 2018 data for the 19 rural LTCHs (out of 384 LTCHs) that were used for the impact analyses shown in Table IV.
3. Effect of Payment Adjustment for LTCH Discharges That Do Not Meet the Applicable Discharge Payment Percentage
In section VII.C. of the preamble of this final rule, we discuss our implementation of the requirements of section 1886(m)(6)(C)(ii) of the Act, which specifies for cost reporting periods beginning on or after October 1, 2019, any LTCH with a discharge payment percentage for the period that is not at least 50 percent will be informed of such a fact, and all of the LTCH's discharges in each successive cost reporting period will be paid the payment amount that would apply under subsection (d) for the discharge if the hospital were a subsection (d) hospital, subject to the process for reinstatement provided for by section 1886(m)(6)(C)(iii) of the Act. Specifically, we are continuing to use our existing policy to calculate the discharge payment percentage and to inform LTCHs when their discharge payment percentage for the period is not at least 50 percent. We also are providing that an LTCH will become subject to this payment adjustment for each cost reporting period after its calculated discharge payment percentage that is not at least 50 percent.
To establish a reinstatement process as required by the statute, we are providing that the payment adjustment for an LTCH will be discontinued beginning with the discharges occurring in the cost reporting period after the LTCH's discharge payment percentage is calculated to be at least 50 percent. Furthermore, we are establishing a probationary-cure period that will allow an LTCH the opportunity to have the payment adjustment suspended for a cost reporting period if, for the period of at least 5 consecutive months of the immediately preceding 6-month period, the discharge payment percentage is at least 50 percent. Under this probationary-cure period, an LTCH will have an opportunity to delay the application of the payment adjustment until the end of the cost reporting period, and waive the payment adjustment for that cost reporting period if the discharge payment percentage for that cost reporting period is ultimately found to be at least 50 percent.
As noted previously, under our finalized policy, an LTCH will be first subject to a potential payment adjustment based on the hospital's discharge payment percentage for its FY 2020 cost reporting period. Hospitals will be notified of that percentage in FY 2021, with the payment adjustment taking effect in FY 2022. Therefore, we do not estimate any effect on LTCH PPS payments until FY 2022. Based on the most recent information available at the time of development of this final rule, we estimate that, for FY 2022, our finalized policy will reduce Medicare spending under the LTCH PPS by approximately $50 million. While we expect that there will be less than the maximum estimated savings due to the inclusion of a provisional-cure period, at this time we do not have a reliable estimate of the effect of that policy on the estimated savings.
Based on the FY 2018 claims data (the most recent set of full claims available), on average, each discharge from an LTCH that fails to meet the 50-percent patient discharge threshold will result in a payment decrease of approximately $19,700 for LTCH PPS standard Federal payment rate discharges and an estimated payment increase of approximately $1,600 for site neutral payment rate discharges. To estimate the number of discharges, we assumed that LTCHs that fail to meet the 50-percent patient discharge threshold are those whose discharge payment percentage is below 40 percent based on FY 2018 claims data. We expect that an LTCH whose discharge payment percentage is at least 40 percent based on FY 2018 claims data will adjust its admission/discharge practices, such that it would no longer be below the 50-percent patient discharge threshold. Applying our actuary's assumption of a 74-percent to 26-percent split between LTCH PPS standard Federal payment rate discharges and site neutral payment rate discharges in FY 2022, we estimate there will be 2,903 LTCH PPS standard Federal payment rate discharges and 7,275 site neutral payment rate discharges. The FY 2018 estimate is inflated to FY 2022, resulting in estimated savings of $50 million (comprised of approximately $60 million in savings from LTCH PPS standard Federal payment rate discharges and approximately $10 million in costs from site neutral payment rate discharges).
4. Anticipated Effects of LTCH PPS Payment Rate Changes and Policy Changes
a. Budgetary Impact
Section 123(a)(1) of the BBRA requires that the PPS developed for LTCHs “maintain budget neutrality.” We believe that the statute's mandate for budget neutrality applies only to the first year of the implementation of the LTCH PPS (that is, FY 2003). Therefore, in calculating the FY 2003 standard Federal payment rate under § 412.523(d)(2), we set total estimated payments for FY 2003 under the LTCH PPS so that estimated aggregate payments under the LTCH PPS were estimated to equal the amount that would have been paid if the LTCH PPS had not been implemented.
Section 1886(m)(6)(A) of the Act establishes a dual rate LTCH PPS payment structure with two distinct payment rates for LTCH discharges beginning in FY 2016. Under this statutory change, LTCH discharges that meet the patient-level criteria for exclusion from the site neutral payment rate (that is, LTCH PPS standard Federal payment rate cases) are paid based on the LTCH PPS standard Federal payment rate. LTCH discharges paid at the site neutral payment rate are generally paid the lower of the IPPS comparable per diem amount, reduced by 4.6 percent for FYs 2018 through 2026, including any applicable HCO payments, or 100 percent of the estimated cost of the case, reduced by 4.6 percent. The statute also establishes a transitional payment method for cases that are paid at the site neutral payment rate for LTCH discharges occurring in cost reporting periods beginning during FY 2016 through FY 2019, under which the site neutral payment rate cases are paid based on a blended payment rate calculated as 50 percent of the applicable site neutral payment rate amount for the discharge and 50 percent of the applicable LTCH PPS standard Federal payment rate for the discharge.
As discussed in section I.J. of this Appendix, we project an increase in aggregate LTCH PPS payments in FY 2020 of approximately $43 million. This estimated increase in payments reflects the projected increase in payments to LTCH PPS standard Federal payment rate cases of approximately $91 million and the projected decrease in payments to site neutral payment rate cases of approximately $49 million under the dual rate LTCH PPS payment rate structure required by the statute beginning in FY 2016. (We note that these calculations are based on unrounded numbers and thus may not sum as expected.)
As discussed in section V.D. of the Addendum to this final rule, our actuaries project cost and resource changes for site neutral payment rate cases due to the site neutral payment rates required under the statute. Specifically, our actuaries project that the costs and resource use for cases paid at the site neutral payment rate will likely be lower, on average, than the costs and resource use for cases paid at the LTCH PPS standard Federal payment rate, and will likely mirror the costs and resource use for IPPS cases assigned to the same MS-DRG. While we are able to incorporate this projection at an aggregate level into our payment modeling, because the historical claims data that we are using in this final rule to project estimated FY 2020 LTCH PPS payments (that is, FY 2018 LTCH claims data) do not reflect this actuarial projection, we are unable to model the impact of the change in LTCH PPS payments for site neutral payment rate cases at the same level of detail with which we are able to model the impacts of the changes to LTCH PPS payments for LTCH PPS standard Federal payment rate cases. Therefore, Table IV only reflects changes in LTCH PPS payments for LTCH PPS standard Federal payment rate cases and, unless otherwise noted, the remaining discussion in section I.J.4. of this Appendix refers only to the impact on LTCH PPS payments for LTCH PPS standard Federal payment rate cases. In the following section, we present our provider impact analysis for the changes that affect LTCH PPS payments for LTCH PPS standard Federal payment rate cases.
b. Impact on Providers
The basic methodology for determining a per discharge payment for LTCH PPS standard Federal payment rate cases is currently set forth under §§ 412.515 through 412.533 and 412.535. In addition to adjusting the LTCH PPS standard Federal payment rate by the MS-LTC-DRG relative weight, we make adjustments to account for area wage levels and SSOs. LTCHs located in Alaska and Hawaii also have their payments adjusted by a COLA. Under our application of the dual rate LTCH PPS payment structure, the LTCH PPS standard Federal payment rate is generally only used to determine payments for LTCH PPS standard Federal payment rate cases (that is, those LTCH PPS cases that meet the statutory criteria to be excluded from the site neutral payment rate). LTCH discharges that do not meet the patient-level criteria for exclusion are paid the site neutral payment rate, which we are calculating as the lower of the IPPS comparable per diem amount as determined under § 412.529(d)(4), reduced by 4.6 percent for FYs 2018 through 2026, including any applicable outlier payments, or 100 percent of the estimated cost of the case as determined under existing § 412.529(d)(2). In addition, when certain thresholds are met, LTCHs also receive HCO payments for both LTCH PPS standard Federal payment rate cases and site neutral payment rate cases that are paid at the IPPS comparable per diem amount.
To understand the impact of the changes to the LTCH PPS payments for LTCH PPS standard Federal payment rate cases presented in this final rule on different categories of LTCHs for FY 2020, it is necessary to estimate payments per discharge for FY 2019 using the rates, factors, and the policies established in the FY 2019 IPPS/LTCH PPS final rule and estimate payments per discharge for FY 2020 using the rates, factors, and the policies in this FY 2020 IPPS/LTCH PPS final rule (as discussed in section VII. of the preamble of this final rule and section V. of the Addendum to this final rule). As discussed elsewhere in this final rule, these estimates are based on the best available LTCH claims data and other factors, such as the application of inflation factors to estimate costs for HCO cases in each year. The resulting analyses can then be used to compare how our policies applicable to LTCH PPS standard Federal payment rate cases affect different groups of LTCHs.
For the following analysis, we group hospitals based on characteristics provided in the OSCAR data, cost report data in HCRIS, and PSF data. Hospital groups included the following:
- Location: Large urban/other urban/rural.
- Participation date.
- Ownership control.
- Census region.
- Bed size.
c. Calculation of LTCH PPS Payments for LTCH PPS Standard Federal Payment Rate Cases
For purposes of this impact analysis, to estimate the per discharge payment effects of our policies on payments for LTCH PPS standard Federal payment rate cases, we simulated FY 2019 and final FY 2020 payments on a case-by-case basis using historical LTCH claims from the FY 2018 MedPAR files that met or would have met the criteria to be paid at the LTCH PPS standard Federal payment rate if the statutory patient-level criteria had been in effect at the time of discharge for all cases in the FY 2018 MedPAR files. For modeling FY 2019 LTCH PPS payments, we used the FY 2019 standard Federal payment rate of $41,558.68 (or $40,738.57 for LTCHs that failed to submit quality data as required under the requirements of the LTCH QRP). Similarly, for modeling payments based on the FY 2020 LTCH PPS standard Federal payment rate, we used the FY 2020 standard Federal payment rate of $42,677.64 (or $41,844.90 for LTCHs that failed to submit quality data as required under the requirements of the LTCH QRP). In each case, we applied the applicable adjustments for area wage levels and the COLA for LTCHs located in Alaska and Hawaii. Specifically, for modeling FY 2019 LTCH PPS payments, we used the current FY 2019 labor-related share (66.0 percent), the wage index values established in the Tables 12A and 12B listed in the Addendum to the FY 2019 IPPS/LTCH PPS final rule (which are available via the internet on the CMS website), the FY 2019 HCO fixed-loss amount for LTCH PPS standard Federal payment rate cases of $27,121 (as reflected in the FY 2019 IPPS/LTCH PPS correction notice to the final rule), and the FY 2019 COLA factors (shown in the table in section V.C. of the Addendum to that final rule) to adjust the FY 2019 nonlabor-related share (34.0 percent) for LTCHs located in Alaska and Hawaii. Similarly, for modeling FY 2020 LTCH PPS payments, we used the FY 2020 LTCH PPS labor-related share (66.3 percent), the FY 2020 wage index values from Tables 12A and 12B listed in section VI. of the Addendum to this final rule (which are available via the internet on the CMS website), the FY 2020 fixed-loss amount for LTCH PPS standard Federal payment rate cases of $26,778 (as discussed in section V.D.3. of the Addendum to this final rule), and the FY 2020 COLA factors (shown in the table in section V.C. of the Addendum to this final rule) to adjust the FY 2020 nonlabor-related share (33.7 percent) for LTCHs located in Alaska and Hawaii. We note that in modeling payments for HCO cases for LTCH PPS standard Federal payment rate cases, we applied an inflation factor of 2.6 percent (determined by the Office of the Actuary) to update the FY 2018 costs of each case to FY 2019, and an inflation factor of 5.5 percent (determined by the Office of the Actuary) to update the FY 2018 costs of each case to FY 2020.
The impacts that follow reflect the estimated “losses” or “gains” among the various classifications of LTCHs from FY 2019 to FY 2020 based on the payment rates and policy changes applicable to LTCH PPS standard Federal payment rate cases presented in this final rule. Table IV illustrates the estimated aggregate impact of the change in LTCH PPS payments for LTCH PPS standard Federal payment rate cases among various classifications of LTCHs. (As discussed previously, these impacts do not include LTCH PPS site neutral payment rate cases.)
- The first column, LTCH Classification, identifies the type of LTCH.
- The second column lists the number of LTCHs of each classification type.
- The third column identifies the number of LTCH cases expected to meet the LTCH PPS standard Federal payment rate criteria.
- The fourth column shows the estimated FY 2019 payment per discharge for LTCH cases expected to meet the LTCH PPS standard Federal payment rate criteria (as described previously).
- The fifth column shows the estimated FY 2020 payment per discharge for LTCH cases expected to meet the LTCH PPS standard Federal payment rate criteria (as described previously).
- The sixth column shows the percentage change in estimated payments per discharge for LTCH cases expected to meet the LTCH PPS standard Federal payment rate criteria from FY 2019 to FY 2020 due to the annual update to the standard Federal rate (as discussed in section V.A.2. of the Addendum to this final rule).
- The seventh column shows the percentage change in estimated payments per discharge for LTCH PPS standard Federal payment rate cases from FY 2019 to FY 2020 for changes to the area wage level adjustment (that is, the wage indexes and the labor-related share), including the application of the area wage level budget neutrality factor (as discussed in section V.B. of the Addendum to this final rule).
- The eighth column shows the percentage change in estimated payments per discharge for LTCH PPS standard Federal payment rate cases from FY 2019 (Column 4) to FY 2020 (Column 5) for all changes.


d. Results
Based on the FY 2018 LTCH cases (from 384 LTCHs) that were used for the analyses in this final rule, we have prepared the following summary of the impact (as shown in Table IV) of the LTCH PPS payment rate and proposed policy changes for LTCH PPS standard Federal payment rate cases presented in this final rule. The impact analysis in Table IV shows that estimated payments per discharge for LTCH PPS standard Federal payment rate cases are projected to increase 2.7 percent, on average, for all LTCHs from FY 2019 to FY 2020 as a result of the payment rate and policy changes applicable to LTCH PPS standard Federal payment rate cases presented in this final rule. This estimated 2.7 percent increase in LTCH PPS payments per discharge was determined by comparing estimated FY 2020 LTCH PPS payments (using the payment rates and factors discussed in this final rule) to estimated FY 2019 LTCH PPS payments for LTCH discharges which will be LTCH PPS standard Federal payment rate cases if the dual rate LTCH PPS payment structure was or had been in effect at the time of the discharge (as described in section I.J.4. of this Appendix).
As stated previously, we are updating the LTCH PPS standard Federal payment rate for FY 2020 by 2.5 percent. For LTCHs that fail to submit quality data under the requirements of the LTCH QRP, as required by section 1886(m)(5)(C) of the Act, a 2.0 percentage point reduction is applied to the annual update to the LTCH PPS standard Federal payment rate. In addition, we are applying the incremental change in the one-time budget neutrality adjustment factor of 0.999858 for the cost of eliminating the 25-percent threshold policy in FY 2020 as discussed in section VII.D. of the preamble of this final rule. Consistent with § 412.523(d)(4), we also are applying an area wage level budget neutrality factor to the FY 2020 LTCH PPS standard Federal payment rate of 1.0020203, based on the best available data at this time, to ensure that any changes to the area wage level adjustment (that is, the annual update of the wage index values and labor-related share) will not result in any change (increase or decrease) in estimated aggregate LTCH PPS standard Federal payment rate payments. As we also explained earlier in this section, for most categories of LTCHs (as shown in Table IV, Column 6), the estimated payment increase due to the 2.5 percent annual update to the LTCH PPS standard Federal payment rate is projected to result in approximately a 2.4 percent increase in estimated payments per discharge for LTCH PPS standard Federal payment rate cases for all LTCHs from FY 2019 to FY 2020. This is because our estimate of the changes in payments due to the update to the LTCH PPS standard Federal payment rate also reflects estimated payments for SSO cases that are paid using a methodology that is not entirely affected by the update to the LTCH PPS standard Federal payment rate. Consequently, for certain hospital categories, we estimate that payments to LTCH PPS standard Federal payment rate cases may increase by less than 2.5 percent due to the annual update to the LTCH PPS standard Federal payment rate for FY 2020.
(1) Location
Based on the most recent available data, the vast majority of LTCHs are located in urban areas. Only approximately 5 percent of the LTCHs are identified as being located in a rural area, and approximately 4 percent of all LTCH PPS standard Federal payment rate cases are expected to be treated in these rural hospitals. The impact analysis presented in Table IV shows that the overall average percent increase in estimated payments per discharge for LTCH PPS standard Federal payment rate cases from FY 2019 to FY 2020 for all hospitals is 2.7 percent. This 2.7 percent increase is constant across all rural and urban LTCHs (both large urban and other urban), as shown in Table IV.
(2) Participation Date
LTCHs are grouped by participation date into four categories: (1) Before October 1983; (2) between October 1983 and September 1993; (3) between October 1993 and September 2002; and (4) October 2002 and after. Based on the most recent available data, the categories of LTCHs with the largest expected percentage of LTCH PPS standard Federal payment rate cases (approximately 46 percent) are in LTCHs that began participating in the Medicare program between October 1993 and September 2002, and they are projected to experience a 2.7 percent increase in estimated payments per discharge for LTCH PPS standard Federal payment rate cases from FY 2019 to FY 2020, as shown in Table IV.
Approximately 3 percent of LTCHs began participating in the Medicare program before October 1983, and these LTCHs are projected to experience an average percent increase of 2.9 percent in estimated payments per discharge for LTCH PPS standard Federal payment rate cases from FY 2019 to FY 2020. Approximately 11 percent of LTCHs began participating in the Medicare program between October 1983 and September 1993, and these LTCHs are projected to experience an increase of 2.6 percent in estimated payments for LTCH PPS standard Federal payment rate cases from FY 2019 to FY 2020. LTCHs that began participating in the Medicare program after October 1, 2002, which treat approximately 37 percent of all LTCH PPS standard Federal payment rate cases, are projected to experience a 2.6 percent increase in estimated payments from FY 2019 to FY 2020.
(3) Ownership Control
LTCHs are grouped into three categories based on ownership control type: Voluntary, proprietary, and government. Based on the most recent available data, approximately 20 percent of LTCHs are identified as voluntary (Table IV). The majority (approximately 77 percent) of LTCHs are identified as proprietary, while government owned and operated LTCHs represent approximately 4 percent of LTCHs. Based on ownership type, voluntary LTCHs are expected to experience a 2.8 percent increase in payments to LTCH PPS standard Federal payment rate cases, while proprietary LTCHs are expected to experience an average increase of 2.6 percent in payments to LTCH PPS standard Federal payment rate cases. Government owned and operated LTCHs, meanwhile, are expected to experience a 3.2 percent increase in payments to LTCH PPS standard Federal payment rate cases from FY 2019 to FY 2020. These LTCHs are projected to experience a somewhat higher percent increase in payments in LTCH PPS standard Federal payment rate payments from FY 2019 to FY 2020 due to a higher than average increase in payments due to changes in the MS-LTC-DRGs and wage index.
(4) Census Region
Estimated payments per discharge for LTCH PPS standard Federal payment rate cases for FY 2020 are projected to increase across all census regions. LTCHs located in the East South Central and the Pacific region are projected to experience the largest increase at 3.1 percent. The remaining regions are projected to experience an increase in the range of 2.5 to 2.7 percent. These regional variations are largely due to updates in the wage index.
(5) Bed Size
LTCHs are grouped into six categories based on bed size: 0-24 beds; 25-49 beds; 50-74 beds; 75-124 beds; 125-199 beds; and greater than 200 beds. We project that LTCHs with 0-24 beds will experience the largest increase in payments for LTCH PPS standard Federal payment rate cases of 3.1 percent, and LTCHs with 75-124 beds are projected to experience the next largest increase of 2.9 percent. This somewhat higher percent increase in payments for these LTCHs is due mostly to a higher than average increase in payments due to changes in the wage index. LTCHs with 25-49 beds and 50-74 beds are both projected to experience an increase of 2.6 percent, while LTCHs with 125 or more beds are projected to experience an increase in payments of 2.5 percent.
5. Effect on the Medicare Program
As stated previously, we project that the provisions of this final rule will result in an increase in estimated aggregate LTCH PPS payments to LTCH PPS standard Federal payment rate cases in FY 2020 relative to FY 2019 of approximately $91 million (or approximately 2.7 percent) for the 384 LTCHs in our database. Although, as stated previously, the hospital-level impacts do not include LTCH PPS site neutral payment rate cases, we estimate that the provisions of this final rule will result in a decrease in estimated aggregate LTCH PPS payments to site neutral payment rate cases in FY 2020 relative to FY 2019 of approximately $49 million (or approximately −5.9 percent) for the 384 LTCHs in our database. Therefore, we project that the provisions of this final rule will result in an increase in estimated aggregate LTCH PPS payments for all LTCH cases in FY 2020 relative to FY 2019 of approximately $43 million (or approximately 1.0 percent) for the 384 LTCHs in our database.
6. Effect on Medicare Beneficiaries
Under the LTCH PPS, hospitals receive payment based on the average resources consumed by patients for each diagnosis. We do not expect any changes in the quality of care or access to services for Medicare beneficiaries as a result of this final rule, but we continue to expect that paying prospectively for LTCH services will enhance the efficiency of the Medicare program. As discussed above, we do not expect the continued implementation of the site neutral payment system to have a negative impact on access to or quality of care, as demonstrated in areas where there is little or no LTCH presence, general short-term acute care hospitals are effectively providing treatment for the same types of patients that are treated in LTCHs.
K. Effects of Requirements for the Hospital Inpatient Quality Reporting (IQR) Program
In section VIII.A. of the preamble of this final rule, we discuss our current and proposed requirements that are being finalized for hospitals to report quality data under the Hospital IQR Program in order to receive the full annual percentage increase for the FY 2021 payment determination and subsequent years.
In this final rule, we are: (1) Adopting the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination with a clarification and update; (2) adopting the Hybrid Hospital-Wide Readmission Measure with Claims and Electronic Health Record Data (Hybrid HWR measure) (NQF #2879) in a stepwise manner, beginning with 2 years of voluntary reporting periods which will run from July 1, 2021 through June 30, 2022, and from July 1, 2022 through June 30, 2023, before requiring reporting of the measure for the reporting period that will run from July 1, 2023 through June 30, 2024, impacting the FY 2026 payment determination and subsequent years; (3) removing the Claims-Based Hospital-Wide All-Cause Unplanned Readmission Measure (NQF #1789) (HWR claims-only measure) beginning with the FY 2026 payment determination; [932] (4) extending the current eCQM reporting and submission requirements for the CY 2020 reporting period/FY 2022 payment determination and CY 2021 reporting period/FY 2023 payment determination; (5) changing the eCQM reporting and submission requirements for the CY 2022 reporting period/FY 2024 payment determination, such that hospitals will be required to report one, self-selected calendar quarter of data for: (a) Three self-selected eCQMs; and (b) the Safe Use of Opioids—Concurrent Prescribing eCQM, for a total of four eCQMs; (6) continuing to require that EHRs be certified to all available eCQMs used in the Hospital IQR Program for the CY 2020 reporting period/FY 2022 payment determination and subsequent years; and (7) establishing reporting and submission requirements for the Hybrid HWR measure. We are not finalizing our proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM.
Regarding the newly finalized Hybrid HWR measure, we estimate a total information collection burden increase of 2,211 hours and a total cost increase related to information collection of approximately $83,266 (due to this finalized proposal and our updated hourly wage plus benefits estimate), beginning with the first voluntary reporting period, which runs from July 1, 2021 through June 30, 2022. We refer readers to section X.B.3. of the preamble of this final rule (information collection requirements) for a detailed discussion of the calculations estimating the changes to the information collection burden for submitting data to the Hospital IQR Program. We acknowledge that there may be costs beyond information collection burden associated with EHR based quality measures. Due to differences in the build of EHRs deployed in hospitals, the cost involved is not quantifiable as it will vary across hospitals.
With regard to our finalized policy to add a new eCQM to the eCQM measure set, while we expect no change to the information collection burden for the Hospital IQR Program as discussed in section X.B.3.b. of the preamble of this final rule because we are also adopting as final our proposed eCQM reporting requirements such that the total number of eCQMs that will be reported and the total quarters of data will remain unchanged from previously finalized requirements, we expect some investment in EHR system updates. Due to differences in the build of EHRs deployed in hospitals, the cost involved is not quantifiable as it will vary across hospitals.
We are also requiring that hospitals use certified electronic heath record technology (CEHRT) that are certified to report all available eCQMs. We expect no change to the information collection burden for the Hospital IQR Program as discussed in section X.B.3.e.(3). of the preamble of this final rule, because this policy does not require hospitals to submit new data to CMS, and we do not require CEHRT to be recertified each time it is updated to a more recent version of the eCQM electronic specifications. Due to the differences in the build of respective CEHRT deployed in hospitals, the mapping required to capture required data for measure calculation, and the range of hospital participation in the development, implementation, and testing of new CEHRT functionality, however, an estimated cost impact of the policy is not quantifiable as it will vary by CEHRT and hospital. For certifying the new eCQM in the eCQM measure set specifically, we expect some costs for hospitals and EHR vendors in certifying the new eCQM so that hospitals have the option to report it.
Historically, 100 hospitals, on average, that participate in the Hospital IQR Program do not receive the full annual percentage increase in any fiscal year due to the failure to meet all requirements of this Program. We anticipate that the number of hospitals not receiving the full annual percentage increase will be approximately the same as in past years.
L. Effects of Requirements for the PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program
In section VIII.B. of the preamble of this final rule, we discuss our finalized policies for the quality data reporting program for PPS-exempt cancer hospitals (PCHs), which we refer to as the PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program. The PCHQR Program is authorized under section 1866(k) of the Act, which was added by section 3005 of the Affordable Care Act. There is no financial impact to PCH Medicare reimbursement if a PCH does not submit data.
In section VIII.B.3.b. of the preamble of this final rule, we are finalizing the removal of one web-based, structural measure beginning with the FY 2022 program year: External Beam Radiotherapy (EBRT) for Bone Metastases (formerly NQF #1822). In addition, in section VIII.B.4. of the preamble of this final rule, we are finalizing the adoption of a claims-based measure for the FY 2022 program year and subsequent years: Surgical Treatment Complications for Localized Prostate Cancer.
As explained in section X.B.4. of the preamble of this final rule, we anticipate that the removal of the External Beam Radiotherapy (EBRT) for Bone Metastases (formerly NQF #1822) measure will reduce the overall burden on participating PCHs by 15-mins per PCH. We estimate a total annual reduction of approximately 3 hours for all 11 PCHs (15 minutes × 11 PCHs/60 minutes per hour), due to the removal of this measure.
We do not anticipate any change in burden on the PCHs associated with our adoption of the Surgical Treatment Complications for Localized Prostate Cancer measure into the PCHQR Program beginning with the FY 2022 program year. This measure is claims-based and does not require PCHs to report any additional data beyond that already submitted on Medicare administrative claims for payment purposes. Therefore, we do not believe that there will be any associated change in burden resulting from this policy.
M. Effects of Requirements for the Long-Term Care Hospital Quality Reporting Program (LTCH QRP)
Under the LTCH QRP, the Secretary must reduce by 2 percentage points the annual update to the LTCH PPS standard Federal rate for discharges for an LTCH during a fiscal year if the LTCH fails to comply with the LTCH QRP requirements specified for that fiscal year. Information is not available to determine the precise number of LTCHs that will not meet the requirements to receive the full annual update for the FY 2020 payment determination.
We believe that the burden and costs associated with the LTCH QRP is the time and effort associated with complying with the requirements of the LTCH QRP. We intend to closely monitor the effects of this quality reporting program on LTCHs to help facilitate successful reporting outcomes through ongoing stakeholder education, national trainings, and help desk support.
We refer readers to section X.B.6. of the preamble of this final rule (information collection requirements) for a detailed discussion of the burden associated with the new requirements for the LTCH QRP.
N. Effects of Requirements Regarding the Promoting Interoperability Program
In section VIII.D. of the preamble of this final rule, we discuss our current and finalized proposed requirements for eligible hospitals and CAHs participating in the Medicare and Medicaid Promoting Interoperability Programs.
In this final rule, as we proposed, we are making the following changes to the Medicare Promoting Interoperability Program: (1) Eliminating the requirement that, for the FY 2020 payment adjustment year, for an eligible hospital that has not successfully demonstrated it is a meaningful EHR user in a prior year, the EHR reporting period in CY 2019 must end before and the eligible hospital must successfully register for and attest to meaningful use no later than October 1, 2019; (2) establishing an EHR reporting period of a minimum of any continuous 90-day period in CY 2021 for new and returning participants (eligible hospitals and CAHs) in the Medicare Promoting Interoperability Program attesting to CMS; (3) requiring that the Medicare Promoting Interoperability Program measure actions must occur within the EHR reporting period beginning with the EHR reporting period in CY 2020; (4) revising the Query of PDMP measure to change the reporting requirement from numerator and denominator to a “yes/no” response beginning with CY 2019 for eligible hospitals and CAHs that attest to CMS under the Medicare Promoting Interoperability Program, making it an optional measure worth five bonus points in CY 2020, removing the exclusions associated with this measure in CY 2020, and clearly stating our intended policy that the measure is worth a full 5 bonus points in CY 2019 and CY 2020; (5) changing the maximum points available for the e-Prescribing measure to 10 points beginning in CY 2020, to coincide with our finalization of the proposed changes to the Query of PDMP measure; (6) removing the Verify Opioid Treatment Agreement measure beginning in CY 2020 and clearly state our intended policy that the measure is worth a full 5 bonus points in CY 2019; and (7) revising the Support Electronic Referral Loops by Receiving and Incorporating Health Information measure to more clearly capture the previously established policy regarding CHERT use. We are also amending our regulations to incorporate several of these proposals.
For CQM reporting under the Medicare and Medicaid Promoting Interoperability Programs, in section VIII.D.6. of the preamble of this final rule, we are making a number of policy changes with respect to the reporting of CQM data, including adding one opioid-related measures beginning with the reporting period in CY 2021 and establishing the reporting period, reporting criteria, submission period, and form and method requirements for CQM reporting in CY 2020. However, for the reporting period in CY 2020, these finalized proposals are continuations of current policies and therefore we do not believe that there will be a change in burden for CY 2020.
As explained in section X.B.9. of the preamble of this final rule, we estimate for CY 2020 a total information collection burden decrease of 2,200 hours, associated with our revision of the Query of PDMP measure to change the reporting requirement from numerator and denominator to a “yes/no” response beginning with CY 2019 for eligible hospitals and CAHs that attest to CMS under the Medicare Interoperability Program, and a total cost decrease of $130,102.50 related to information collection burden cost estimates due to this finalized proposal and our updated hourly wage plus benefits estimate.
O. Alternatives Considered
This final rule contains a range of policies. It also provides descriptions of the statutory provisions that are addressed, identifies the finalized policies, and presents rationales for our decisions and, where relevant, alternatives that were considered.
1. Wage Index
We considered a number of alternatives to our finalized policies discussed in section III.N.2.b of the preamble of this final rule to address the budget neutrality for the increase in the wage index for hospitals with wage index values below the 25th percentile wage index value (that is, low wage index hospitals).
As described more fully in section III.N.2.b. of the preamble of this final rule, rather than reducing the wage index of hospitals with wage index values above the 75th percentile wage index value (that is, high wage index hospitals) as we proposed in the FY 2020 IPPS/LTCH PPS proposed rule (summarized in section III.N.2.b of this final rule), we are maintaining budget neutrality for the increase in the wage index for low wage index hospitals by reducing the FY 2020 standardized amount, which is one of the alternatives we considered in the proposed rule. We also considered the suggestion by many commenters that the policy should not be implemented in a budget neutral manner at all. However, as discussed in section III.N.2.b of the preamble of this final rule, given that budget neutrality is required under section 1886(d)(3)(E) of the Act, given that even if it were not required we think it would be inappropriate to use the wage index to increase or decrease overall IPPS spending, and given that we wish to consider further the policy arguments raised against our proposed budget neutrality on high wage hospitals, we are finalizing a budget neutrality adjustment for the increase in the wage index values for low wage hospitals that will be applied to the national standardized amount.
As discussed in section III.N.2.f of the preamble of this final rule, we received very few public comments supporting the other two alternatives to our wage index disparities proposals discussed in the proposed rule, namely mirroring our approach of raising the wage index for low wage index hospitals by reducing the wage index values for high wage index hospitals (that is, reducing the wage index for high wage index hospitals by half the difference between the otherwise applicable final wage index value for these hospitals and the 75th percentile wage index value), or creating a national rural wage index area. Refer to section III.N.2.f of the preamble of this final rule for further discussion of the alternatives considered for our wage index disparities proposals.
2. New Technology Add-On Payments
As discussed in section II.H.8. of the preamble of this final rule, in situations where a new medical device is part of the Breakthrough Devices Program and has received FDA marketing authorization, we proposed an alternative inpatient new technology add-on payment pathway to facilitate access to this technology for Medicare beneficiaries. We also considered in the proposed rule whether it would be appropriate to apply this alternative inpatient new technology add-on payment pathway in situations where a new drug is part of an FDA-expedited program for drugs and has received FDA marketing authorization. However, as discussed in the proposed rule, in reviewing this issue, we noted that the current drug-pricing system provides generous incentives for innovation, but too often fails to deliver important medications at an affordable cost. We stated that making this policy applicable to drugs would further incentivize innovation but without decreasing cost, a key priority of this Administration. In May 2018, President Donald Trump and HHS Secretary Alex Azar released the American Patients First blueprint (available at https://www.hhs.gov/sites/default/files/AmericanPatientsFirst.pdf), a comprehensive plan to lower drug prices and out-of-pocket costs. Since the launch of the blueprint, we have been taking action to turn the President's vision into action, and improve the health and well-being of every American. We stated that while we continue to work on these initiatives for drug affordability, we continue to believe that it is appropriate to distinguish between drugs and devices in our consideration of a proposed policy change for transformative new technologies.
In this final rule, are finalizing an alternative inpatient new technology add-on payment pathway for new medical devices that are part of the Breakthrough Devices Program and have received FDA marketing authorization, beginning with FY 2021 new technology applications. As also discussed in section II.H.8. of the preamble of this final rule, after consideration of specific concerns and consistent with the Administration's commitment to address issues related to antimicrobial resistance, we extended the proposed alternative new technology add-on payment pathway to a product that is designated by the FDA as a QIDP in order to secure access to antibiotics, and improve health outcomes for Medicare beneficiaries in a manner that is as expeditious as possible. We further state that we continue to believe that it is appropriate to distinguish between drugs and devices in our consideration of a policy change for transformative new technologies while we continue to work on these initiatives for drug affordability for the reasons stated in the proposed rule.
3. Uncompensated Care Payments
Another policy area where an alternative was considered in the proposed rule was in the calculation of the FY 2020 Medicare uncompensated care payments to hospitals, as discussed in greater detail in section IV.F.4.c. of the preamble of this final rule. We proposed to use Worksheet S-10 data from the FY 2015 cost reports in the calculation of Factor 3 for FY 2020. Although we proposed to use Worksheet S-10 data from the FY 2015 cost reports, we discussed an alternative in the proposed rule under which we would use a single year of uncompensated care data from the FY 2017 cost reports, instead of the FY 2015 cost reports, to calculate Factor 3 for FY 2020. We sought comment on whether, due to the changes in the cost reporting instructions, we should use uncompensated care data from the FY 2017 cost reports instead of the FY 2015 data. As discussed in section IV.F.4.c. of this final rule, after considering the comments received, we agree with the commenters who indicated that our proposed approach of using the FY 2015 data is more appropriate. The FY 2015 data has been through an auditing process, while the FY 2017 data has not.
4. LTCHs
Another policy area where an alternative was considered was in the reinstatement process for LTCHs that do not meet the applicable discharge payment percentage, as discussed in greater detail in section VII.C. of the preamble of this final rule. We proposed to implement a special probationary reinstatement process. Although we proposed to use a special probationary reinstatement process, we believe a reinstatement process that would not use a probationary period (as discussed in more detail in section VII.C. of the preamble of the proposed rule and this final rule) would satisfy the statutory requirement without further modification. But, as discussed in more detail in section VII.C. of the preamble of this final rule, in developing our proposals for the a special probationary reinstatement process, we were concerned that hospitals may be able to manipulate discharges or delay billing in such a way as to artificially inflate their discharge payment percentage for purposes of a special reinstatement process if the special reinstatement process were not probationary. We solicited public comments as to whether we should have a special reinstatement process and, if so, whether it should be probationary. A summary of those comments and our responses, along with our final policy, are discussed in section VII.C. of the preamble of this final rule.
5. eCQM
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19497), in the context of proposing eCQM reporting and submission requirements under the Hospital IQR Program for the CY 2022 reporting period/FY 2024 payment determination, we proposed that hospitals would be required to report one, self-selected calendar quarter of data for three self-selected eCQMs and for all hospitals to report the proposed Safe Use of Opioids—Concurrent Prescribing eCQM as their fourth eCQM. We also considered in the proposed rule an alternative whereby hospitals would have the option to select one of the two proposed opioid-related eCQMs, the Safe Use of Opioids eCQM or Opioid-Related Adverse Events eCQM, as their fourth required eCQM. We stated, however, that such an approach would add additional complexity to the eCQM reporting requirements, and we believe that the Safe Use of Opioids eCQM is more closely related to combating the current opioid epidemic, as discussed in sections VIII.A.5.a. and VIII.A.9.d.(4) of the preamble of the proposed rule and this final rule, than the Opioid-Related Adverse Events eCQM, which is focused on improved monitoring of patients who receive opioids during hospitalization. Because the alternative considered would not impact the collection of information for hospitals, we stated that we did not expect these alternatives to affect the reporting burden on hospitals. We considered this alternative and sought public comment on it.
As discussed in sections VIII.A.5.a.(1) and (2) of the preamble of this final rule, while we are finalizing our proposal to adopt the Safe Use of Opioids—Concurrent Prescribing eCQM beginning with the CY 2021 reporting period/FY 2023 payment determination with a clarification and update, we are not finalizing our proposal to adopt the Hospital Harm—Opioid-Related Adverse Events eCQM. As discussed above in section I.K. of Appendix A of this final rule, we do not expect the adoption of the Safe Use of Opioids—Concurrent Prescribing eCQM or any of the alternatives considered to affect the reporting burden on hospitals.
6. MS-DRG Severity Level Designations
As discussed in section II.F.14.c. of the preamble of this final rule, while we are continuing to examine the implementation of broader comprehensive changes to the CC/MCC designations, we believe it is appropriate to finalize the change in the severity level designations from non-CC to CC for the ICD-10-CM diagnosis codes specifying antimicrobial drug resistance. Commenters expressed significant concerns related to the public health crisis represented by antimicrobial resistance and urged CMS to also apply the change in the severity level designation from non-CC to CC to the other ICD 10-CM diagnosis codes specifying antimicrobial drug resistance, in addition the codes included in our proposal. Addressing the concerns related to the public health crisis that antimicrobial resistance represents is consistent with the Administration's key priorities, and for the reasons discussed in section II.F.14.c. of the preamble of this final rule, we are finalizing a change to the severity level designation for all of the codes in category Z16- (Resistance to antimicrobial drugs) from a non-CC to a CC designation.
In expressing their concerns regarding antimicrobial resistance, we also received several comments urging CMS to consider a separate payment mechanism that removes certain antimicrobials from the MS-DRG, where those antimicrobial resistant drugs would be “carved out” from the MS-DRG and paid separately at 100 percent. Commenters also suggested that CMS develop a “drug resistant modifier” for infection-related MS-DRGs in certain circumstances related to antimicrobial resistance. We believe further information is required before engaging in broader changes to the severity levels of the MS-DRGs. As stated in section II.F.14.c. of the preamble of this final rule, we will be gathering additional public input on these issues more broadly, and welcome feedback specifically on policy reforms aimed at recalibrating severity levels for antimicrobial resistance within the MS-DRGs.
P. Reducing Regulation and Controlling Regulatory Costs
Executive Order 13771, titled Reducing Regulation and Controlling Regulatory Costs, was issued on January 30, 2017. This final rule is considered an E.O. 13771 regulatory action. We estimate that this rule generates approximately $2.4 million in annualized costs, discounted at 7 percent relative to FY 2016, over a perpetual time horizon.
We discuss the estimated burden and costs for the Hospital IQR Program in section X.B.3. of the preamble of this final rule, and estimate that the impact of these changes is an increase in costs of approximately $25 per hospital annually or approximately $83,266 for all hospitals annually.
We discuss the estimated burden and cost reductions for the PCHQR Program in section X.B.4. of the preamble of this final rule, and estimate that the impact of these changes is a reduction in costs of approximately $10 per PCH annually or approximately $113 for all participating PCHs annually.
We discuss the estimated burden for the LTCH QRP in section X.B.6. of the preamble of this final rule, and estimate that the impact of these changes is an increase in costs of approximately $5,675.29 per LTCH annually or approximately $2,355,243 for all LTCHs annually.
We do not anticipate an increase or decrease in burden and costs for the Hospital Readmissions Reduction Program, the HAC Reduction Program, or the Hospital Value-Based Purchasing Program based on the finalized policies in this final rule.
Also, as noted in section I.R. of this Appendix, the regulatory review cost for this final rule is $1,905,475.

Q. Overall Conclusion
1. Acute Care Hospitals
Acute care hospitals are estimated to experience an increase of approximately $3.8 billion in FY 2020, taking into account operating, capital, new technology, and low volume hospital payments as modeled for this final rule. Approximately $3.5 billion of this estimated increase is due to the changes in operating payments, including $0.1 billion in uncompensated care payments (discussed in sections I.G. and I.H. of this Appendix), approximately $0.1 billion is due to the change in capital payments (discussed in section I.I. of this Appendix), approximately $0.2 billion is due to the change in new technology add-on payments (discussed in section I.H. of this Appendix), and approximately $-7 million is due to the change in low-volume hospital payments (discussed in section I.H. of this Appendix). Total differs from the sum of the components due to rounding.
Table I. of section I.G. of this Appendix also demonstrates the estimated redistributional impacts of the IPPS budget neutrality requirements for the MS-DRG and wage index changes, and for the wage index reclassifications under the MGCRB.
We estimate that hospitals will experience a 1.4 percent increase in capital payments per case, as shown in Table III. of section I.I. of this Appendix. We project that there will be a $0.1 billion increase in capital payments in FY 2020 compared to FY 2019.
The discussions presented in the previous pages, in combination with the remainder of this final rule, constitute a regulatory impact analysis.
2. LTCHs
Overall, LTCHs are projected to experience an increase in estimated payments per discharge in FY 2020. In the impact analysis, we are using the rates, factors, and policies presented in this final rule based on the best available claims and CCR data to estimate the change in payments under the LTCH PPS for FY 2020. Accordingly, based on the best available data for the 384 LTCHs in our database, we estimate that overall FY 2020 LTCH PPS payments will increase approximately $43 million relative to FY 2019 as a result of the payment rates and factors presented in this final rule.
R. Regulatory Review Costs
If regulations impose administrative costs on private entities, such as the time needed to read and interpret a rule, we should estimate the cost associated with regulatory review. In the FY 2020 IPPS/LTCH PPS proposed rule, due to the uncertainty involved with accurately quantifying the number of entities that would review the proposed rule, we assumed that the total number of timely pieces of correspondence on last year's proposed rule will be the number of reviewers of this proposed rule. We acknowledge that this assumption may understate or overstate the costs of reviewing the rule. It is possible that not all commenters reviewed last year's rule in detail, and it is also possible that some reviewers chose not to comment on the proposed rule. For those reasons, and consistent with our approach in previous rulemakings (82 FR 38585; 83 FR 41777), we believe that the number of past commenters would be a fair estimate of the number of reviewers of the rule. We welcomed any public comments on the approach in estimating the number of entities that will review this final rule. We did not receive any public comments specific to our solicitation.
We also recognize that different types of entities are in many cases affected by mutually exclusive sections of the rule. Therefore, for the purposes of our estimate, and consistent with our approach in previous rulemaking (82 FR 38585; 83 FR 41777), we assume that each reviewer read approximately 50 percent of the rule. In the proposed rule, we welcomed public comments on this assumption. We did not receive any public comments specific to our solicitation.
We have used the number of timely pieces of correspondence on the FY 2020 proposed rule as our estimate for the number of reviewers of the proposed rule. We continue to acknowledge the uncertainty involved with using this number, but we believe it is a fair estimate due to the variety of entities affected and the likelihood that some of them choose to rely (in full or in part) on press releases, newsletters, fact sheets, or other sources rather than the comprehensive review of preamble and regulatory text. Using the wage information from the BLS for medical and health service managers (Code 11-9111), we estimate that the cost of reviewing the final rule is $107.38 per hour, including overhead and fringe benefits (https://www.bls.gov/oes/current/oes_nat.htm). Assuming an average reading speed, we estimate that it would take approximately 21.40 hours for the staff to review half of this final rule. For each IPPS hospital or LTCH that reviews this final rule, the estimated cost is $2,297 (21.40 hours × $107.38). Therefore, we estimate that the total cost of reviewing this final rule is $8,972,082 ($2,297 × 3,906 reviewers).
II. Accounting Statements and Tables
A. Acute Care Hospitals
As required by OMB Circular A-4 (available at https://obamawhitehouse.archives.gov/omb/circulars_a-004_a-4/ and https://georgewbush-whitehouse.archives.gov/omb/circulars/a004/a-4.html), in the following Table V., we have prepared an accounting statement showing the classification of the expenditures associated with the provisions of this final rule as they relate to acute care hospitals. This table provides our best estimate of the change in Medicare payments to providers as a result of the changes to the IPPS presented in this final rule. All expenditures are classified as transfers to Medicare providers.
As shown below in Table V., the net costs to the Federal Government associated with the policies in this final rule are estimated at $3.8 billion.

B. LTCHs
As discussed in section I.J. of this Appendix, the impact analysis of the payment rates and factors presented in this final rule under the LTCH PPS is projected to result in an increase in estimated aggregate LTCH PPS payments in FY 2020 relative to FY 2019 of approximately $43 million based on the data for 384 LTCHs in our database that are subject to payment under the LTCH PPS. Therefore, as required by OMB Circular A-4 (available at: https://obamawhitehouse.archives.gov/omb/circulars_a004_a-4/ and https://georgewbush-whitehouse.archives.gov/omb/circulars/a004/a-4.html), in Table VI., we have prepared an accounting statement showing the classification of the expenditures associated with the provisions of this final rule as they relate to the changes to the LTCH PPS. Table VI. provides our best estimate of the estimated change in Medicare payments under the LTCH PPS as a result of the payment rates and factors and other provisions presented in this final rule based on the data for the 384 LTCHs in our database. All expenditures are classified as transfers to Medicare providers (that is, LTCHs).
As shown in Table VI., the net cost to the Federal Government associated with the final policies for LTCHs in this final rule are estimated at $43 million.

III. Regulatory Flexibility Act (RFA) Analysis
The RFA requires agencies to analyze options for regulatory relief of small entities. For purposes of the RFA, small entities include small businesses, nonprofit organizations, and small government jurisdictions. We estimate that most hospitals and most other providers and suppliers are small entities as that term is used in the RFA. The great majority of hospitals and most other health care providers and suppliers are small entities, either by being nonprofit organizations or by meeting the SBA definition of a small business (having revenues of less than $7.5 million to $38.5 million in any 1 year). (For details on the latest standards for health care providers, we refer readers to page 36 of the Table of Small Business Size Standards for NAIC 622 found on the SBA website at: http://www.sba.gov/sites/default/files/files/Size_Standards_Table.pdf.)
For purposes of the RFA, all hospitals and other providers and suppliers are considered to be small entities. Individuals and States are not included in the definition of a small entity. We believe that the provisions of this final rule relating to acute care hospitals will have a significant impact on small entities as explained in this Appendix. For example, because all hospitals are considered to be small entities for purposes of the RFA, the hospital impacts described in this final rule are impacts on small entities. For example, we refer readers to “Table I—Impact Analysis of Changes to the IPPS for Operating Costs for FY 2020.” Because we lack data on individual hospital receipts, we cannot determine the number of small proprietary LTCHs. Therefore, we are assuming that all LTCHs are considered small entities for the purpose of the analysis in section I.J. of this Appendix. MACs are not considered to be small entities because they do not meet the SBA definition of a small business. Because we acknowledge that many of the affected entities are small entities, the analysis discussed throughout the preamble of this final rule constitutes our regulatory flexibility analysis. This final rule contains a range of policies. It provides descriptions of the statutory provisions that are addressed, identifies the policies, and presents rationales for our decisions and, where relevant, alternatives that were considered.
For purposes of the RFA, as stated above, all hospitals and other providers and suppliers are considered to be small entities. We estimate the provisions of this final rule will result in an estimated $3.9 billion increase in FY 2020 payments to IPPS hospitals, primarily driven by the applicable percentage increase to the IPPS rates in conjunction with other payment changes including uncompensated care payments, capital payments, and new technology add-on payments, as discussed in section I.B. of this Appendix. As discussed in section I.J. of this Appendix, the impact analysis of the payment rates and factors presented in this final rule under the LTCH PPS is projected to result in an increase in estimated aggregate LTCH PPS payments in FY 2020 relative to FY 2019 of approximately $43 million. We solicited public comments on our estimates and analysis of the impact of our proposals on those small entities. Any public comments that we received and our responses are presented throughout this final rule.
IV. Impact on Small Rural Hospitals
Section 1102(b) of the Act requires us to prepare a regulatory impact analysis for any proposed or final rule that may have a significant impact on the operations of a substantial number of small rural hospitals. This analysis must conform to the provisions of section 604 of the RFA. With the exception of hospitals located in certain New England counties, for purposes of section 1102(b) of the Act, we define a small rural hospital as a hospital that is located outside of an urban area and has fewer than 100 beds. Section 601(g) of the Social Security Amendments of 1983 (Pub. L. 98-21) designated hospitals in certain New England counties as belonging to the adjacent urban area. Thus, for purposes of the IPPS and the LTCH PPS, we continue to classify these hospitals as urban hospitals. (As shown in Table I. in section I.G. of this Appendix, rural IPPS hospitals with 0-49 beds and 50-99 beds are expected to experience an increase in payments from FY 2019 to FY 2020 of 3.4 percent and 2.8 percent, respectively. We refer readers to Table I. in section I.G. of this Appendix for additional information on the quantitative effects of the policy changes under the IPPS for operating costs.)
V. Unfunded Mandates Reform Act Analysis
Section 202 of the Unfunded Mandates Reform Act of 1995 (Pub. L. 104-4) also requires that agencies assess anticipated costs and benefits before issuing any rule whose mandates require spending in any 1 year of $100 million in 1995 dollars, updated annually for inflation. In 2019, that threshold level is approximately $154 million. This final rule will not mandate any requirements for State, local, or tribal governments, nor would it affect private sector costs.
VI. Executive Order 13175
Executive Order 13175 requires that, to the extent practicable and permitted by law, no agency shall promulgate any regulation that has tribal implications, that imposes substantial direct compliance costs on Indian tribal governments, and that is not required by statute, unless: (1) Funds necessary to pay the direct costs incurred by the Indian tribal government or the tribe in complying with the regulation are provided by the Federal Government; or (2) the agency, prior to the formal promulgation of the regulation, (A) consulted with tribal officials early in the process of developing the proposed regulation; (B) in a separately identified portion of the preamble to the regulation as it is to be issued in the Federal Register, provides to the Director of the Office of Management and Budget (OMB) a tribal summary impact statement, which consists of a description of the extent of the agency's prior consultation with tribal officials, a summary of the nature of their concerns and the agency's position supporting the need to issue the regulation, and a statement of the extent to which the concerns of tribal officials have been met; and (C) makes available to the Director of OMB any written communications submitted to the agency by tribal officials.
Section 1880(a) of the Act states that a hospital of the Indian Health Service, whether operated by such Service or by an Indian tribe or tribal organization, is eligible for payments under title XVIII of the Act, so long as it meets all of the conditions and requirements for such payments which are applicable generally to hospitals under title XVIII of the Act.
This final rule will not mandate any requirement for Indian tribal governments, and it will not impose substantial direct compliance costs on Indian tribal governments.
VII. Executive Order 12866
In accordance with the provisions of Executive Order 12866, the Executive Office of Management and Budget reviewed this final rule.
Appendix B: Recommendation of Update Factors for Operating Cost Rates of Payment for Inpatient Hospital Services
I. Background
Section 1886(e)(4)(A) of the Act requires that the Secretary, taking into consideration the recommendations of MedPAC, recommend update factors for inpatient hospital services for each fiscal year that take into account the amounts necessary for the efficient and effective delivery of medically appropriate and necessary care of high quality. Under section 1886(e)(5) of the Act, we are required to publish update factors recommended by the Secretary in the proposed and final IPPS rules. Accordingly, this Appendix provides the recommendations for the update factors for the IPPS national standardized amount, the hospital-specific rate for SCHs and MDHs, and the rate-of-increase limits for certain hospitals excluded from the IPPS, as well as LTCHs. In prior years, we made a recommendation in the IPPS proposed rule and final rule for the update factors for the payment rates for IRFs and IPFs. However, for FY 2020, consistent with our approach for FY 2019, we are including the Secretary's recommendation for the update factors for IRFs and IPFs in separate Federal Register documents at the time that we announce the annual updates for IRFs and IPFs. We also discuss our response to MedPAC's recommended update factors for inpatient hospital services.
II. Inpatient Hospital Update for FY 2020
A. FY 2020 Inpatient Hospital Update
As discussed in section IV.B. of the preamble to this final rule, for FY 2020, consistent with section 1886(b)(3)(B) of the Act, as amended by sections 3401(a) and 10319(a) of the Affordable Care Act, we are setting the applicable percentage increase by applying the following adjustments in the following sequence. Specifically, the applicable percentage increase under the IPPS is equal to the rate-of-increase in the hospital market basket for IPPS hospitals in all areas, subject to a reduction of one-quarter of the applicable percentage increase (prior to the application of other statutory adjustments; also referred to as the market basket update or rate-of-increase (with no adjustments)) for hospitals that fail to submit quality information under rules established by the Secretary in accordance with section 1886(b)(3)(B)(viii) of the Act and a reduction of three-quarters of the applicable percentage increase (prior to the application of other statutory adjustments; also referred to as the market basket update or rate-of-increase (with no adjustments)) for hospitals not considered to be meaningful electronic health record (EHR) users in accordance with section 1886(b)(3)(B)(ix) of the Act, and then subject to an adjustment based on changes in economy-wide productivity (the multifactor productivity (MFP) adjustment). Section 1886(b)(3)(B)(xi) of the Act, as added by section 3401(a) of the Affordable Care Act, states that application of the MFP adjustment may result in the applicable percentage increase being less than zero. (We note that section 1886(b)(3)(B)(xii) of the Act required an additional reduction each year only for FYs 2010 through 2019.)
In compliance with section 404 of the MMA, in the FY 2018 IPPS/LTCH PPS final rule (82 FR 38587), we replaced the FY 2010-based IPPS operating and capital market baskets with the rebased and revised 2014-based IPPS operating and capital market baskets, effective beginning in FY 2018.
In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19401), in accordance with section 1886(b)(3)(B) of the Act, we proposed to base the proposed FY 2020 market basket update used to determine the applicable percentage increase for the IPPS on IGI's fourth quarter 2018 forecast of the 2014-based IPPS market basket rate-of-increase with historical data through third quarter 2018, which was estimated to be 3.2 percent. In accordance with section 1886(b)(3)(B) of the Act, as amended by section 3401(a) of the Affordable Care Act, in section IV.B. of the preamble of the FY 2020 IPPS/LTCH PPS proposed rule, based on IGI's fourth quarter 2018 forecast, we proposed an MFP adjustment of 0.5 percent for FY 2020. We also proposed that if more recent data subsequently became available, we would use such data, if appropriate, to determine the FY 2020 market basket update and MFP adjustment for the final rule. Based on the most recent data available for this FY 2020 IPPS/LTCH PPS final rule, in accordance with section 1886(b)(3)(B) of the Act, we are establishing the FY 2020 market basket update used to determine the applicable percentage increase for the IPPS based on IGI's second quarter 2019 forecast of the 2014-based IPPS market basket rate-of-increase with historical data through first quarter 2019, which is estimated to be 3.0 percent. Based on the most recent data available for this final rule, we are establishing an MFP adjustment of 0.4 percent.
In the FY 2020 IPPS/LTCH PPS proposed rule, based on IGI's fourth quarter 2018 forecast of the 2014-based IPPS market basket and the MFP adjustment, depending on whether a hospital submits quality data under the rules established in accordance with section 1886(b)(3)(B)(viii) of the Act (hereafter referred to as a hospital that submits quality data) and is a meaningful EHR user under section 1886(b)(3)(B)(ix) of the Act (hereafter referred to as a hospital that is a meaningful EHR user), we presented four possible applicable percentage increases that could be applied to the standardized amount.
In accordance with section 1886(b)(3)(B) of the Act, as amended by section 3401(a) of the Affordable Care Act, in section IV.B. of the preamble of this final rule, we are establishing the applicable percentages increase for the FY 2020 updates based on IGI's second quarter 2019 forecast of the 2014-based IPPS market basket and the MFP adjustment, depending on whether a hospital submits quality data under the rules established in accordance with section 1886(b)(3)(B)(viii) of the Act and is a meaningful EHR user under section 1886(b)(3)(B)(ix) of the Act, as shown in the table in this section.

B. Update for SCHs and MDHs for FY 2020
Section 1886(b)(3)(B)(iv) of the Act provides that the FY 2020 applicable percentage increase in the hospital-specific rate for SCHs and MDHs equals the applicable percentage increase set forth in section 1886(b)(3)(B)(i) of the Act (that is, the same update factor as for all other hospitals subject to the IPPS). Under current law, the MDH program is effective for discharges through September 30, 2022, as discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41429 through 41430).
As previously mentioned, the update to the hospital specific rate for SCHs and MDHs is subject to section 1886(b)(3)(B)(i) of the Act, as amended by sections 3401(a) and 10319(a) of the Affordable Care Act. Accordingly, depending on whether a hospital submits quality data and is a meaningful EHR user, we are establishing the same four possible applicable percentage increases in the previous table for the hospital-specific rate applicable to SCHs and MDHs.
C. FY 2020 Puerto Rico Hospital Update
As discussed in the FY 2017 IPPS/LTCH PPS final rule (81 FR 56939), prior to January 1, 2016, Puerto Rico hospitals were paid based on 75 percent of the national standardized amount and 25 percent of the Puerto Rico-specific standardized amount. Section 601 of Pub. L. 114-113 amended section 1886(d)(9)(E) of the Act to specify that the payment calculation with respect to operating costs of inpatient hospital services of a subsection (d) Puerto Rico hospital for inpatient hospital discharges on or after January 1, 2016, shall use 100 percent of the national standardized amount. Because Puerto Rico hospitals are no longer paid with a Puerto Rico-specific standardized amount under the amendments to section 1886(d)(9)(E) of the Act, there is no longer a need for us to make an update to the Puerto Rico standardized amount. Hospitals in Puerto Rico are now paid 100 percent of the national standardized amount and, therefore, are subject to the same update to the national standardized amount discussed under section IV.B.1. of the preamble of this final rule. Accordingly, for FY 2020, we are establishing an applicable percentage increase of 2.6 percent to the standardized amount for hospitals located in Puerto Rico.
D. Update for Hospitals Excluded From the IPPS for FY 2020
Section 1886(b)(3)(B)(ii) of the Act is used for purposes of determining the percentage increase in the rate-of-increase limits for children's hospitals, cancer hospitals, and hospitals located outside the 50 States, the District of Columbia, and Puerto Rico (that is, short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and America Samoa). Section 1886(b)(3)(B)(ii) of the Act sets the percentage increase in the rate-of-increase limits equal to the market basket percentage increase. In accordance with § 403.752(a) of the regulations, RNHCIs are paid under the provisions of § 413.40, which also use section 1886(b)(3)(B)(ii) of the Act to update the percentage increase in the rate-of-increase limits.
Currently, children's hospitals, PPS-excluded cancer hospitals, RNHCIs, and short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa are among the remaining types of hospitals still paid under the reasonable cost methodology, subject to the rate-of-increase limits. In addition, in accordance with § 412.526(c)(3) of the regulations, extended neoplastic disease care hospitals (described in § 412.22(i) of the regulations) also are subject to the rate-of-increase limits. As discussed in section VI. of the preamble of this final rule, in the FY 2018 IPPS/LTCH PPS final rule, we finalized the use of the percentage increase in the 2014-based IPPS operating market basket to update the target amounts for children's hospitals, PPS-excluded cancer hospitals, RNHCIs, and short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa for FY 2018 and subsequent fiscal years. In addition, as discussed in section IV.B. of the preamble of this final rule, the update to the target amount for extended neoplastic disease care hospitals for FY 2020 is the percentage increase in the 2014-based IPPS operating market basket. Accordingly, for FY 2020, the rate-of-increase percentage to be applied to the target amount for these children's hospitals, cancer hospitals, RNHCIs, extended neoplastic disease care hospitals, and short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa is the FY 2020 percentage increase in the 2014-based IPPS operating market basket. For this final rule, the current estimate of the IPPS operating market basket percentage increase for FY 2020 is 3.0 percent.
E. Update for LTCHs for FY 2020
Section 123 of Public Law 106-113, as amended by section 307(b) of Public Law 106-554 (and codified at section 1886(m)(1) of the Act), provides the statutory authority for updating payment rates under the LTCH PPS.
As discussed in section V.A. of the Addendum to this final rule, we are establishing an update to the LTCH PPS standard Federal payment rate for FY 2020 of 2.5 percent, consistent with the amendments to section 1886(m)(3) of the Act which provides that any annual update be reduced by the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act (that is, the MFP adjustment). Furthermore, in accordance with the LTCHQR Program under section 1886(m)(5) of the Act, we are reducing the annual update to the LTCH PPS standard Federal rate by 2.0 percentage points for failure of a LTCH to submit the required quality data. Accordingly, we are establishing an update factor of 1.025 in determining the LTCH PPS standard Federal rate for FY 2020. For LTCHs that fail to submit quality data for FY 2020, we are establishing an annual update to the LTCH PPS standard Federal rate of 0.5 percent (that is, the annual update for FY 2020 of 2.5 percent less 2.0 percentage points for failure to submit the required quality data in accordance with section 1886(m)(5)(C) of the Act and our rules) by applying an update factor of 1.005 in determining the LTCH PPS standard Federal rate for FY 2020. (We note that, as discussed in section VII.D. of the preamble of this final rule, the update to the LTCH PPS standard Federal payment rate of 2.5 percent for FY 2020 does not reflect any budget neutrality factors.)
III. Secretary's Recommendations
MedPAC is recommending an inpatient hospital update in the amount specified in current law for FY 2020. MedPAC's rationale for this update recommendation is described in more detail in this section. As previously mentioned, section 1886(e)(4)(A) of the Act requires that the Secretary, taking into consideration the recommendations of MedPAC, recommend update factors for inpatient hospital services for each fiscal year that take into account the amounts necessary for the efficient and effective delivery of medically appropriate and necessary care of high quality. Consistent with current law, depending on whether a hospital submits quality data and is a meaningful EHR user, we are recommending the four applicable percentage increases to the standardized amount listed in the table under section II. of this Appendix B. We are recommending that the same applicable percentage increases apply to SCHs and MDHs.
In addition to making a recommendation for IPPS hospitals, in accordance with section 1886(e)(4)(A) of the Act, we are recommending update factors for certain other types of hospitals excluded from the IPPS. Consistent with our policies for these facilities, we are recommending an update to the target amounts for children's hospitals, cancer hospitals, RNHCIs, short-term acute care hospitals located in the U.S. Virgin Islands, Guam, the Northern Mariana Islands, and American Samoa and extended neoplastic disease care hospitals of 3.0 percent.
For FY 2020, consistent with policy set forth in section VII. of the preamble of this final rule, for LTCHs that submit quality data, we are recommending an update of 2.5 percent to the LTCH PPS standard Federal rate. For LTCHs that fail to submit quality data for FY 2020, we are recommending an annual update to the LTCH PPS standard Federal rate of 0.5 percent.
IV. MedPAC Recommendation for Assessing Payment Adequacy and Updating Payments in Traditional Medicare
In its March 2019 Report to Congress, MedPAC assessed the adequacy of current payments and costs, and the relationship between payments and an appropriate cost base. MedPAC recommended an update to the hospital inpatient rates by 2 percent with the difference between this and the update amount specified in current law to be used to increase payments in a new suggested Medicare quality program, the “Hospital Value Incentive Program (HVIP).” MedPAC stated that together, these recommendations, paired with the recommendation to eliminate the current hospital quality program incentives, would increase hospital payments by increasing the base payment rate and by increasing the average rewards hospitals receive under MedPAC's proposed Medicare HVIP.
We refer readers to the March 2019 MedPAC report, which is available for download at www.medpac.gov, for a complete discussion on these recommendations.
Response: With regard to MedPAC's recommendation of an update to the hospital inpatient rates equal to 2 percent, with the remainder of the 2.6 percent to be used to fund its recommended Medicare HVIP, section 1886(b)(3)(B) of the Act sets the requirements for the FY 2020 applicable percentage increase. Therefore, consistent with the statute, we are establishing an applicable percentage increase for FY 2020 of 2.6 percent, provided the hospital submits quality data and is a meaningful EHR user consistent with these statutory requirements.
Furthermore, we appreciate MedPAC's recommendation concerning a new HVIP. We agree that continual improvement motivated by quality programs is an important incentive of the IPPS. However, under current law, the inpatient hospital quality programs include the Hospital Readmissions Reduction Program, the Hospital Value-Based Purchasing Program, and the Hospital-Acquired Condition Reduction Program.
We note that, because the operating and capital prospective payment systems remain separate, we are continuing to use separate updates for operating and capital payments. The update to the capital rate is discussed in section III. of the Addendum to this final rule.
Footnotes
1. Internal analysis from the Centers for Disease Control and Prevention.
Back to Citation2. Beard, C.M., Sheps, S.G., Kurland, L.T., Carney, J.A., Lie, J.T., “Occurrence of pheochromocytoma in Rochester, Minnesota”, pp. 1950-1979.
3. Stenström, G., Svärdsudd, K., “Pheochromocytoma in Sweden 1958-1981. An analysis of the National Cancer Registry Data,” Acta Medica Scandinavica, 1986, vol. 220(3), pp. 225-232.
Back to Citation4. Fishbein, Lauren, “Pheochromocytoma and Paraganglioma,” Hematology/Oncology Clinics 30, no. 1, 2016, pp. 135-150.
5. Lloyd, R.V., Osamura, R.Y., Klöppel, G., & Rosai, J. (2017). World Health Organization (WHO) Classification of Tumours of Endocrine Organs. Lyon, France: International Agency for Research on Center (IARC).
Back to Citation6. Kantorovich, Vitaly, and Karel Pacak. “Pheochromocytoma and paraganglioma.” Progress in Brain Research., 2010, vol. 182, pp. 343-373.
Back to Citation7. Carty, S.E., Young, W.F., Elfky, A., “Paraganglioma and pheochromocytoma: Management of malignant disease,” UpToDate. Available at: https://www.uptodate.com/contents/paraganglioma-and-pheochromocytoma-management-of-malignant-disease.
Back to Citation8. Kantorovich, Vitaly, and Karel Pacak. “Pheochromocytoma and paraganglioma.” Progress in Brain Research., 2010, vol. 182, pp. 343-373.
Back to Citation9. Noda, T., Nagano, H., Miyamoto, A., et al., “Successful outcome after resection of liver metastasis arising from an extraadrenal retroperitoneal paraganglioma that appeared 9 years after surgical excision of the primary lesion,” Int J Clin Oncol, 2009, vol. 14, pp. 473.
Back to Citation10. Carty, S.E., Young, W.F., Elfky, A., “Paraganglioma and pheochromocytoma: Management of malignant disease,” UpToDate. Available at: https://www.uptodate.com/contents/paraganglioma-and-pheochromocytoma-management-of-malignant-disease.
Back to Citation11. Ibid.
Back to Citation12. Ibid.
Back to Citation13. Fitzgerald, P.A., Goldsby, R.E., Huberty, J.P., et al., “Malignant pheochromocytomas and paragangliomas: a phase II study of therapy with high-dose 131I-metaiodobenzylguanidine (131I-MIBG),” Ann N Y Acad Sci, 2006, vol. 1073, pp. 465.
Back to Citation14. Loh, K.C., Fitzgerald, P.A., Matthay, K.K., Yeo, P.P., Price, D.C., “The treatment of malignant pheochromocytoma with iodine-131 metaiodobenzylguanidine (131. I-MIBG): a comprehensive review of 116 reported patients,” J Endocrinol Invest, 1997, vol. 20(11), pp. 648-658.
Back to Citation15. Gonias, S, et. al., “Phase II Study of High-Dose [131. I ]Metaiodobenzylguanidine Therapy for Patients With Metastatic Pheochromocytoma and Paraganglioma,” J of Clin Onc, July 27, 2009.
Back to Citation16. Carty, S.E., Young, W.F., Elfky, A., “Paraganglioma and pheochromocytoma: Management of malignant disease,” UpToDate. Available at: https://www.uptodate.com/contents/paraganglioma-and-pheochromocytoma-management-of-malignant-disease.
Back to Citation17. Niemeijer, N.D., Alblas, G., Hulsteijn, L.T., Dekkers, O.M. and Corssmit, E.P.M., “Chemotherapy with cyclophosphamide, vincristine and dacarbazine for malignant paraganglioma and pheochromocytoma: systematic review and meta‐analysis,” Clinical endocrinology, 2014, vol 81(5), pp. 642-651.
18. Ayala-Ramirez, Montserrat, et al., “Clinical Benefits of Systemic Chemotherapy for Patients with Metastatic Pheochromocytomas or Sympathetic Extra-Adrenal Paragangliomas: Insights from the Largest Single Institutional Experience,” Cancer, 2012, vol. 118(11), pp. 2804-2812.
Back to Citation19. Wu, L.T., Dicpinigaitis, P., Bruckner, H., et al., “Hypertensive crises induced by treatment of malignant pheochromocytoma with a combination of cyclophosphamide, vincristine, and dacarbazine,” Med Pediatr Oncol, 1994, vol. 22(6), pp. 389-392.
Back to Citation20. Carty, S.E., Young, W.F., Elfky, A., “Paraganglioma and pheochromocytoma: Management of malignant disease,” UpToDate. Available at: https://www.uptodate.com/contents/paraganglioma-and-pheochromocytoma-management-of-malignant-disease.
Back to Citation21. Noto, Richard B., et al., “Phase 1 Study of High-Specific-Activity I-131 MIBG for Metastatic and/or Recurrent Pheochromocytoma or Paraganglioma (IB12 Phase 1 Study),” J Clin Endocrinol Metab, vol. 103(1), pp. 213-220.
Back to Citation22. Noto, Richard B., et al., “Phase 1 Study of High-Specific-Activity I-131 MIBG for Metastatic and/or Recurrent Pheochromocytoma or Paraganglioma (IB12 Phase 1 Study),” J Clin Endocrinol Metab, vol. 103(1), pp. 213-220.
Back to Citation23. Ibid.
Back to Citation24. Fitzgerald, P.A., Goldsby, R.E., Huberty, J.P., et al., “Malignant pheochromocytomas and paragangliomas: a phase II study of therapy with high-dose 131I-metaiodobenzylguanidine (131I-MIBG).” Ann N Y Acad Sci, 2006, vol. 1073, pp. 465.
Back to Citation25. Therasse, P., Arbuck, S.G., Eisenhauer, J.W., Kaplan, R.S., Rubinsten, L., Verweij, J., Van Blabbeke, M., Van Oosterom, A.T., Christian, M.D., and Gwyther, S.G., “New guidelines to evaluate the response to treatment in solid tumors,” J Natl Cancer Inst, 2000, vol. 92(3), pp. 205-16. Available at: http://www.eortc.be/Services/Doc/RECIST.pdf.
Back to Citation26. Hescot, S., Leboulleux, S., Amar, L., Vezzosi, D., Borget, I., Bournaud-Salinas, C., de la Fouchardiere, C., Libé, R., Do Cao, C., Niccoli, P., Tabarin, A., “One-year progression-free survival of therapy-naive patients with malignant pheochromocytoma and paraganglioma,” The J Clin Endocrinol Metab, 2013, vol. 98(10), pp. 4006-4012.
Back to Citation27. Scully, M., et al., “Regional UK TTP registry: correlation with laboratory ADAMTS 13 analysis and clinical Features,” Br. J. Haematol., 2008, vol. 142(5), pp. 819-26.
28. Reese, J.A., et al., “Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features,” Pediatr. Blood Cancer, 2013, vol. 60(10), pp. 1676-82.
29. Terrell, D.R., et al., “The incidence of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: all patients, idiopathic patients, and patients with severe ADAMTS-13 deficiency,” J. Thromb. Haemost., 2005, vol. 3(7), pp. 1432-6.
Back to Citation30. Scully, M., et al., “Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies,” Br. J. Haematol., 2012, vol. 158(3), pp. 323-35.
31. George, J.N., “Corticosteroids and rituximab as adjunctive treatments for thrombotic thrombocytopenic Purpura,” Am. J. Hematol., 2012, vol. 87 Suppl 1, pp. S88-91.
Back to Citation32. Form for Notification of a Compassionate Use Programme to the Paul-Ehrlich-Institut.
33. Benhamou, Y., et al., “Cardiac troponin-I on diagnosis predicts early death and refractoriness in acquired thrombotic thrombocytopenic purpura. Experience of the French Thrombotic Microangiopathies Reference Center,” J. Thromb. Haemost., 2015, vol. 13(2), pp. 293-302.
34. Han, B., et al., “Depression and cognitive impairment following recovery from thrombotic thrombocytopenic purpura,” Am. J. of Hematol., 2015, vol. 90(8), pp. 709-14.
35. Rajan, S.K., “BMJ Best Practice; Thrombotic thrombocyopenic purpura,” May 27, 2016.
36. Goel, R., et al., “Prognostic risk-stratified score for predicting mortality in hospitalized patients with thrombotic thrombocytopenic purpura: nationally representative data from 2007 to 2012,” Transfusion, 2016, vol. 56(6), pp. 1451-8.
37. Rock, G.A., Shumak, K.H., Buskard, N.A., et al., “Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group,” N Engl J Med, 1991, vol. 325, pp. 393-397.
Back to Citation38. Goel, R., et al., “Prognostic risk-stratified score for predicting mortality in hospitalized patients with thrombotic thrombocytopenic purpura: nationally representative data from 2007 to 2012,” Transfusion, 2016, vol. 56(6), pp. 1451-8.
Back to Citation39. Scully, M., et al., “Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies,” Br. J. Haematol., 2012, vol. 158(3), pp. 323-35.
40. George, J.N., “Corticosteroids and rituximab as adjunctive treatments for thrombotic thrombocytopenic Purpura,” Am. J. Hematol., 2012, vol. 87 Suppl 1, pp. S88-91.
Back to Citation41. Bell, W.R., et al., “Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic Syndrome. Clinical experience in 108 patients,” N. Engl. J. Med., 1991, vol. 325(6), pp. 398-403.
42. Phillips, E.H., et al., “The role of ADAMTS-13 activity and complement mutational analysis in differentiating acute thrombotic microangiopathies,” J. Thromb. Haemost., 2016, vol. 14(1), pp. 175-85.
Back to Citation43. Coppo, P., “Management of thrombotic thrombocytopenic purpura,” Transfus Clin Biol., Sep 2017, vol. 24(3), pp. 148-153.
44. Froissart, A., et al., “Rituximab in autoimmune thrombotic thrombocytopenic purpura: A success story,” Eur. J. Intern. Med., 2015, vol. 26(9), pp. 659-65.
Back to Citation45. Peyvandi, F., Scully, M., Kremer Hovinga, J.A., Cataland, S., Knöbl, P., Wu, H., Artoni, A., Westwood, J.P., Mansouri Taleghani, M., Jilma, B., Callewaert, F., Ulrichts, H., Duby, C., Tersago, D., TITAN Investigators, “Caplacizumab for Acquired Thrombotic Thrombocytopenic Purpura,” N Engl J Med., February 11, 2016, vol. 374(6), pp. 511-22. PMID: 26863353.
Back to Citation46. Scully, M., et al., “Treatment of Acquired Thrombotic Thrombocytopenic Purpura with Caplacizumab,” N. Engl. J. Med., (In Press).
Back to Citation47. Reese, J.A., Muthurajah, D.S., Kremer-Hovinga, J.A., Vesely, S.K., Terrell, D.R., George, J.N., “Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features,” Pediatr Blood Cancer, October 2013, vol. 60(10), pp. 1676-82, Epub June 1, 2013.
Back to Citation48. Rock, G.A., Shumak, K.H., Buskard, N.A., et al., “Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group,” N Engl J Med, 1991, vol. 325, pp. 393-397.
Back to Citation49. Bhadrasain, M.D., Vikram, Shivaji, Ph.D., Deore, Beitler, M.D., Jonathan J., Sood, M.D., Brij, Mullokandov, Ph.D., Eduard, Kapulsky, Ph.D., Alexander, Fontenla, Ph,d, Doracy P, “The relationship between dose heterogeneity (“hot” spots) and complications following high-dose rate brachytherapy,” Int. J. Radiation Oncology Biol. Phys., 1999, vol. 43, no. 5, pp. 983-987.
Back to Citation50. Rivard, Mark J., “Low energy brachytherapy sources for pelvic sidewall treatment,” abstract presented at the ABS 2016 Annual Meeting.
Back to Citation51. Seneviratne, Danushka, et al., “The CivaSheet: The new frontier of intraoperative radiation therapy or a pricer alternative to LDR brachytherapy,” Advances in Radiation Oncology, 2018, vol. 3, pp. 87-91.
Back to Citation52. Castaneda SA, Emrich J, Bowne WB, Kemmerer EJ, Sangani R, Khalili M, Rivard MJ, Poli J. “Clinical outcomes using a novel directional Pd-103 brachytherapy device: 20-month report of a patient with leiomyosarcoma of the pelvic sidewall.” ACRO 2018 Annual Meeting.
Back to Citation53. Seneviratne, D., McLaughlin, C., Todor, D., Kaplan, B., Fields, E., “The CivaSheet: The new frontier of intraoperative radiation therapy or a pricier alternative to LDR brachytherapy?,” Advances in Radiation Oncology, 2018, vol. 3, pp. 87-91.
Back to Citation54. Howell, K.J., Meyer, J.E., Rivard, M.J., et al., “Initial Clinical Experience with Directional LDR Brachytherapy for Retroperitoneal Sarcoma,” submitted Int J of Rad Onc Biol Phys, 2018.
Back to Citation55. Cavanaugh, S.X., Rothley, D.J., Richman, C., “Directional LDR Intraoperative Brachytherapy for Head and Neck Cancer,” Presented at ABS 2017 Annual Meeting.
Back to Citation56. On file at CivaTech.
Back to Citation57. Ibid.
Back to Citation58. Yoo, S.S., Todor, D.A., Myers, J.M., Kaplan, B.J., Fields, E.C., “Widening the therapeutic window using an implantable, uni-directional LDR brachytherapy sheet as a boost in pancreatic cancer,” ASTRO 2018 Annual Meeting San Antonio, TX.
Back to Citation59. Castaneda, S.A., Emrich, J., Bowne, W.B., Kemmerer, E.J., Sangani, R., Khalili, M., Rivard, M.J., Poli, J., “Clinical outcomes using a novel directional Pd-103 brachytherapy device: 20-month report of a patient with leiomyosarcoma of the pelvic sidewall,” ACRO 2018 Annual Meeting.
Back to Citation60. Seneviratne, D., McLaughlin, C., Todor, D., Kaplan, B., Fields, E., “The CivaSheet: The new frontier of intraoperative radiation therapy or a pricier alternative to LDR brachytherapy?,” Advances in Radiation Oncology, 2018, vol. 3, pp. 87-91.
Back to Citation61. Zhen, H., Turian, J.V., Sen, N., et al.,”Initial clinical experience using a novel Pd-103 surface applicator for the treatment of retroperitoneal and abdominal wall malignancies,” Advances in Radiation Oncology, 2018, vol. 3, pp. 216-220.
62. Howell, K.J., Meyer, J.E., Rivard, M.J., et al., “Initial Clinical Experience with Directional LDR Brachytherapy for Retroperitoneal Sarcoma,” submitted Int J of Rad Onc Biol Phys, 2018.
63. Turian, J.V., “Emerging Technologies for IORT: Unidirectional Planar Brachytherapy Sources,” Presented at AAPM 2017 Annual Meeting.
Back to Citation64. Zhen, H., Turian, J.V., Sen, N., et al.,”Initial clinical experience using a novel Pd-103 surface applicator for the treatment of retroperitoneal and abdominal wall malignancies”, Advances in Radiation Oncology, 2018, vol. 3, pp. 216-220.
Back to Citation65. Turian, J.V., “Emerging Technologies for IORT: Unidirectional Planar Brachytherapy Sources,” Presented at AAPM 2017 Annual Meeting.
Back to Citation66. Howell, K.J., Meyer, J.E.,Rivard, M.J. et al., “Initial Clinical Experiences with Directional LDR Brachytherapy for Retroperitoneal Sarcomo, submitted to Int J of Rad Onc Biol Phys, 2018.
Back to Citation67. Taunk, N.K., Cohen, G., Taggar, A.S., et al., “Preliminary Clinical Experience from a Phase I Feasibility Study of a Novel Permanent Unidirectional Intraoperative Brachytherapy Device,” ABS 2017 Annual Meeting.
Back to Citation68. Rivard, M.J., “Low-energy brachytherapy sources for pelvic sidewall treatment,” Presented at ABS 2016 Annual Meeting.
Back to Citation69. Taunk, N.K., Cohen, G., Taggar, A.S., et al., “Preliminary Clinical Experience from a Phase I Feasibility Study of a Novel Permanent Unidirectional Intraoperative Brachytherapy Device,” ABS 2017 Annual Meeting.
Back to Citation70. Rivard, Mark J., “Low energy brachytherapy sources for pelvic sidewall treatment,” abstract presented at the ABS 2016 Annual Meeting.
71. Yoo, S.S., Todor, D.A., Myers, J.M., Kaplan, B.J., Fields, E.C., “Widening the therapeutic window using an implantable, uni-directional LDR brachytherapy sheet as a boost in pancreatic cancer,” ASTRO 2018 Annual Meeting San Antonio, TX.
72. Howell, K.J., Meyer, J.E., Rivard, M.J., et al., “Initial Clinical Experience with Directional LDR Brachytherapy for Retroperitoneal Sarcoma,” submitted Int J of Rad Onc Biol Phys, 2018.
Back to Citation73. Ibid.
74. Rivard, Mark J., “Low energy brachytherapy sources for pelvic sidewall treatment,” abstract presented at the ABS 2016 Annual Meeting.
75. Yoo, S.S., Todor, D.A., Myers, J.M., Kaplan, B.J., Fields, E.C., “Widening the therapeutic window using an implantable, uni-directional LDR brachytherapy sheet as a boost in pancreatic cancer,” ASTRO 2018 Annual Meeting San Antonio, TX.
Back to Citation76. Neschis, David G. & MD, Golden, M., “Clinical features and diagnosis of lower extremity peripheral artery disease.” Available at: https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-lower-extremity-peripheral-artery-disease.
Back to Citation77. Centers for Disease Control and Prevention, “Peripheral Arterial Disease (PAD) Fact Sheet,” 2018, Retrieved from https://www.cdc.gov/DHDSP/data_statistics/fact_sheets/fs_PAD.htm.
Back to Citation78. Berger, J. & Davies, M, “Overview of lower extremity peripheral artery disease,” Retrieved October 29, 2018, from https://www.uptodate.com/contents/overview-of-lower-extremity-peripheral-artery-disease.
Back to Citation79. Müller-Hülsbeck, S., et al., “Long-Term Results from the MAJESTIC Trial of the Eluvia Paclitaxel-Eluting Stent for Femoropopliteal Treatment: 3-Year Follow-up,” Cardiovasc Intervent Radiol, December 2017, vol. 40(12), pp. 1832-1838.
Back to Citation80. Gray, W.A., et al., “A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): A randomised, non-inferiority trial,” Lancet, September 24, 2018.
Back to Citation81. Forrester, J.S., Fishbein, M., Helfant, R., Fagin, J., “A paradigm for restenosis based on cell biology: Clues for the development of new preventive therapies,” J Am Coll Cardiol, March 1, 1991, vol. 17(3), pp. 758-69.
Back to Citation82. Gray, W.A., Keirse, K., Soga, Y., et al., “A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): A randomized, non-inferiority trial,” Lancet, 2018, published online Sept 22, http://dx.doi.org/10.1016/S0140-6736(18)32262-1.
Back to Citation83. Katsanos, K., et al., “Risk of Death Following Application of Paclitaxel-Coated Balloons and Stents in the Femoropopliteal Artery of the Leg: A Systematic Review and Meta-Analysis of Randomized Controlled Trials,” JAHA, vol. 7(24).
Back to Citation84. Gray W.A., Keirse K., Soga Y., Benko A., Babaev A., Yokoi Y., et al. A polymer-coated, paclitaxel-eluting stent (eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): A randomised non-inferiority trial. Lancet. 2018;392:1541-1551.
Back to Citation85. Committee for Proprietary Medicinal Products. Points to consider on switching between superiority and non-inferiority. Br J Clin Pharmacol. 2001 Sep;52(3):223-8.
Back to Citation86. https://www.fda.gov/medical-devices/letters-health-care-providers/update-treatment-peripheral-arterial-disease-paclitaxel-coated-balloons-and-paclitaxel-eluting.
Back to Citation87. https://www.fda.gov/advisory-committees/advisory-committee-calendar/june-19-20-2019-circulatory-system-devices-panel-medical-devices-advisory-committee-meeting#event-materials.
Back to Citation88. Pagano, L., Valentini, C.G., Grammatico, S., Pulsoni, A., “Blastic plasmacytoid dendritic cell neoplasm: Diagnostic criteria and therapeutical approaches,” British Journal of Haematology, 2016, vol. 174(2), pp. 188-202.
Back to Citation89. Falcone, U., Sibai, H., Deotare, U, “A critical review of treatment modalities for blastic plasmacytoid dendritic cell neoplasm,” Critical Reviews in Oncology/Hematology, 2016, vol. 107, pp. 156-162.
Back to Citation90. Pagano, L., Valentini, C.G., Grammatico, S., Pulsoni, A., “Blastic plasmacytoid dendritic cell neoplasm: diagnostic criteria and therapeutical approaches,” British Journal of Haematology, 2016, vol. 174(2), pp. 188-202.
Back to Citation91. Pagano, L., Valentini, C.G., Pulsoni, A., et al for GIMEMA-ALWP (Gruppo Italiano Malattie EMatologiche dell'Adulto, Acute Leukemia Working Party), “Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study,” Haematologica, 2013, vol. 98(2), pp. 239-246.
Back to Citation92. Pemmaraju, N., et al., “Results of Pivotal Phase 2 Trial of SL-401 in Patients with Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN),” Proceedings from the 2018 European Hematology Association Congress, 2018, Abstract 214438.
Back to Citation93. Pagano, L., Valentini, C.G., Pulsoni, A., et al for GIMEMA-ALWP (Gruppo Italiano Malattie EMatologiche dell'Adulto, Acute Leukemia Working Party), “Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study,” Haematologica, 2013, vol. 98(2), pp. 239-246.
Back to Citation94. Pemmaraju, N., et al., “Results of Pivotal Phase 2 Clinical Trial of Tagraxofusp (SL-401) in Patients with Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN),” Proceedings from the 2018 American Society of Hematology (ASH), 2018, Abstract S765.
Back to Citation95. Dietrich, S., et al., “Blastic plasmacytoid dendritic cell neoplasia (BPDC) in elderly patients: results of a treatment algorithm employing allogeneic stem cell transplantation with moderately reduced conditioning intensity, Biology of Blood and Marrow Transplantation, 2011, vol. 17, pp. 1250-1254.
Back to Citation96. Aoki, T., et al., “Long-term survival following autologous and allogenic stem cell transplantation for Blastic plasmacytoid dendritic cell neoplasm,” Blood, 2015, vol. 125(23), pp. 3559-3562.
Back to Citation97. Pagano, L., Valentini, C.G., Pulsoni, A., et al. for GIMEMA-ALWP (Gruppo Italiano Malattie EMatologiche dell'Adulto, Acute Leukemia Working Party), “Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study,” Haematologica, 2013, vol. 98(2), pp. 239-246.
Back to Citation98. Dalle, S., et al., “Blastic plasmacytoid dendritic cell neoplasm: is transplantation the treatment of choice?” The British Journal of Dermatology, 2010, vol. 162, pp. 74-79.
Back to Citation99. Pagano, L., Valentini, C.G., Grammatico, S., Pulsoni, A., “Blastic plasmacytoid dendritic cell neoplasm: diagnostic criteria and therapeutical approaches,” British Journal of Haematology, 2016, vol. 174(2), pp. 188-202.
Back to Citation100. Pemmaraju, N., et al., “Results of Pivotal Phase 2 Trial of SL-401 in Patients with Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN),” Proceedings from the 2018 European Hematology Association Congress, 2018, Abstract 214438.
Back to Citation101. Ibid.
Back to Citation102. Angelot-Delettre, F., Roggy, A., Frankel, A.E., Lamarthee, B., Seilles, E., Biichle, S., et al., “In vivo and in vitro sensitivity of blastic plasmacytoid dendritic cell neoplasm to SL-401, an interleukin-3 receptor targeted biologic agent,” Haematologica, 2015, vol. 100(2), pp. 223-30.
Back to Citation103. Pemmaraju, N., et al., “Results of Pivotal Phase 2 Trial of SL-401 in Patients with Blastic Plasmacytoid Dendritic Cell Neoplasm (BPDCN),” Proceedings from the 2018 European Hematology Association Congress, 2018, Abstract 214438.
Back to Citation104. Pemmaraju, N., et al., “Tagraxofusp in Blastic Plasmacytoid Dendritic-Cell Neoplasm.” N Engl J Med. 2019, doi: 10.1056/NEJMoa1815105.
Back to Citation105. Pagano, L., Valentini, C.G., Pulsoni, A., et al for GIMEMA-ALWP (Gruppo Italiano Malattie EMatologiche dell'Adulto, Acute Leukemia Working Party), “Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study,” Haematologica, 2013, vol. 98(2), pp. 239-246.
Back to Citation106. Pemmaraju, N., et al., “Tagraxofusp in Blastic Plasmacytoid Dendritic-Cell Neoplasm.” N Engl J Med. 2019, doi: 10.1056/NEJMoa1815105.
Back to Citation107. Ibid.
Back to Citation108. American Cancer Society, “Key Statistics for Bladder Cancer,” www.cancer.org/cancer/bladder-cancer/about/key-statistics.html.
Back to Citation109. Nishina, T., Takahashi, S., Iwasawa, R., et al., “Safety, pharmacokinetic, and pharmacodynamics of erdafitinib, a pan-fibroblast growth factor receptor (FGFR) tyrosine kinase inhibitor, in patients with advanced or refractory solid tumors,” Invest New Drugs, 2018, vol. 36, pp. 424-434.
110. Tabernero, J., Bahleda, R., Dienstmann, R., et al., “Phase I Dose-Escalation Study of JNJ-42756493, an Oral Pan-Fibroblast Growth Factor Receptor Inhibitor, in Patients With Advanced Solid Tumors,” J Clin Onc, Vol. 33(30), October 20, 2015, pp. 3001-3008.
Back to Citation111. KEYTRUDA® (pembrolizumab injection) [package insert]. Whitehouse Station, NJ: Merck Sharp & Dohme Corp.; April 2019.
Back to Citation112. McCaffrey JA, Hilton S, Mazumdar M, et al. Phase 2 trial of docetaxel in patients with advanced or metastatic transitional-cell carcinoma. J Clin Oncol. 1997;15(5):1853-1857.
Back to Citation113. KEYTRUDA® (pembrolizumab injection) [package insert]. Whitehouse Station, NJ: Merck Sharp & Dohme Corp.; April 2019.
Back to Citation114. American Cancer Society. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2019.html
Back to Citation115. Dai, C., Heemers, H., Sharifi, N., “Androgen signaling in prostate cancer,” Cold Spring Harb Perspect Med, 2017, vol. 7(9), pp. a030452.
Back to Citation116. Center for Drug Evaluation and Research. NDA/BLA Multi-Disciplinary Review and Evaluation (Summary Review, Office Director, Cross Discipline Team Leader Review, Clinical Review, Non-Clinical Review, Statistical Review and Clinical Pharmacology Review) NDA 210951—ERLEADA (apalutamide)—Reference ID: 4221387. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2018/210951Orig1s000MultidisciplineR.pdf. Published March 19, 2018.
Back to Citation117. Beaver, Julia A., Kluetz, Paul, Pazdur, Richard, “Metastasis-free Survival—A New End Point in Prostate Cancer Trials,” 2018, N Eng J of Med, vol. 378, pp. 2458-2460, 10.1056/NEJMp1805966.
Back to Citation118. Clegg, N.J., Wongvipat, J., Joseph, J.D., et al., “ARN-509: a novel antiandrogen for prostate cancer treatment,” Cancer Res, 2012, vol. 72(6), pp. 1494-503.
Back to Citation119. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Prostate Cancer (Version 4.2018). National Comprehensive Cancer Network. Available at: www.nccn.org. Published August 15, 2018.
120. Lowrance, W.T., Murad, M.H., Oh, W.K., et al., “Castration-Resistant Prostate Cancer: AUA Guideline Amendment 2018,” J Urol, 2018, pii: S0022-5347(18)43671-3.
Back to Citation121. Smith, M.R., et al., “Apalutamide Treatment and Metastasis-free Survival in Prostate Cancer,” N Engl J Med, 2018, vol. 12;378(15), pp. 1408-1418.
Back to Citation122. Ibid.
Back to Citation123. Saad, F., et al., “Effect of apalutamide on health-related quality of life in patients with non-metastatic castration-resistant prostate cancer: an analysis of the SPARTAN randomized, placebo- controlled, phase 3 trial,” Lancet Oncology, 2018 Oct; Epub 2018 Sep 10.
Back to Citation124. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, U.S. Cancer Statistics Working Group, U.S. Cancer Statistics Data Visualizations Tool, based on November 2017 submission data (1999-2015), Available at: www.cdc.gov/cancer/dataviz, June 2018.
Back to Citation125. Smith, M.R., et al., “Apalutamide Treatment and Metastasis-free Survival in Prostate Cancer,” N Engl J Med, 2018, vol. 12;378(15), pp. 1408-1418.
Back to Citation126. ICECaP Working Group, Sweeney, C., Nakabayashi, M., et al., “The development of intermediate clinical endpoints in cancer of the prostate (ICECaP)”, J Natl Cancer Inst, 2015, vol. 107(12), pp. djv261
Back to Citation127. Li S., Ding Z, Lin J.H., et al., “Association of prostate-specific antigen (PSA) trajectories with risk for metastasis and mortality in nonmetastatic castration-resistant prostate cancer (nmCRPC),” Abstract presented at: 2018 Genitorurinary Cancers Symposium, February 8-10, 2018, San Francisco, CA.
Back to Citation128. Center for Drug Evaluation and Research (CDER) & Center for Biologics Evaluation and Research (CBER). Nonmetastatic, Castration-Resistant Prostate Cancer: Considerations for Metastasis-Free Survival Endpoint in Clinical Trials Guidance for Industry DRAFT GUIDANCE; 2018. https://www.fda.gov/regulatory-information/search-fda-guidancedocuments/nonmetastatic-castration-resistant-prostate-cancer-considerations-metastasis-free-survival-endpoint. Accessed June 1, 2019.
Back to Citation129. Xie W., Regan M.M., Buyse M., et al. Metastasis-free survival is a strong surrogate of overall survival in localized prostate cancer. J Clin Oncol. 2017;35(27):3097-3104.
Back to Citation130. Li S., Ding Z., Lin J.H., et al. Association of prostate-specific antigen (PSA) trajectories with risk for metastasis and mortality in non- metastatic castration-resistant prostate cancer (nmCRPC). Abstract presented at: 2018 Genitorurinary Cancers Symposium; February 8-10, 2018; San Francisco, CA.
Back to Citation131. World Health Organization. (2018, March). Depression. Available at: http://www.who.int/mediacentre/factsheets/fs369/en/.
Back to Citation132. National Institute of Mental Health. (2006, January). Questions and Answers about the NIMH Sequenced Treatment Alternatives to Relieve Depression (STAR*D)—Background. Available at: https://www.nimh.nih.gov/funding/clinical-research/practical/stard/backgroundstudy.shtml.
Back to Citation133. Manthorpe, J., & Iliffe, S., “Suicide in later life: Public health and practitioner perspectives,” International Journal of Geriatric Psychiatry, 2010, vol. 25(12), pp. 1230-1238.
134. Lenze, E., Sheffrin, M., Driscoll, H., Mulsant, B., Pollock, B., Dew, M., Reynolds, C., “Incomplete response in late-life depression: Getting to remission,” Dialogues in Clinical Neuroscience, 2008, vol. 10(4), pp. 419-430.
135. Alexopoulos, G., & Kelly, R., “Research advances in geriatric depression,” World Psychiatry, 2009, vol. 8 (3), pp. 140-149.
Back to Citation136. Sanacora, G., et. al., “Targeting the Glutamatergic System to Develop Novel, Improved Therapeutics for Mood Disorders,” Nat Rev Drug Discov., 2008, pp. 426-437.
Back to Citation137. Duman, R. (2018). Ketamine and rapid-acting anti-depressants: A new era in the battle against depression and suicide. F1000Research, 7, 659. doi:10.12688/f1000research.14344.1.
138. Dubovsky, S., “What Is New about New Anti-depressants?,” Psychotherapy and Psychosomatics, 2018, vol. 87(3), pp. 129-139, doi:10.1159/000488945.
Back to Citation139. Sanacora, G., et. al., “Targeting the Glutamatergic System to Develop Novel, Improved Therapeutics for Mood Disorders,” Nat Rev Drug Discov., 2008, pp. 426-437.
Back to Citation140. Duman R.S. Ketamine and rapid-acting antidepressants: A new era in the battle against depression and suicide. F1000Research. 2018;7:F1000 Faculty Rev-659. doi:10.12688/f1000research.14344.1.
141. Dubovsky S.L. What Is New about New Antidepressants? Psychotherapy and Psychosomatics. 2018;87(3):129-139. doi:10.1159/000488945.
Back to Citation142. Duman R.S., Li N., Liu R.J., et al. Signaling pathways underlying the rapid antidepressant actions of ketamine. Neuropharmacology. 2012;62(1):35-41.
143. Duman R.S., Aghajanian G.K., Sanacora G., et al. Synaptic plasticity and depression: New insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(3):238-249.
144. Sanacora G., Zarate C.A., Krystal J.H., et al. Targeting the glutaminergic system to develop novel, improved therapeutics for mood disorders. Nat Rev Drug Discov. 2008;7(5):426-437.
Back to Citation145. Rush A.J., Trivedi M.H., Wisniewski S.R., et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am J Psychiatry. 2006;163(11):1905-1917.
Back to Citation146. AHRQ 2018
Back to Citation147. National Institute of Mental Health. (2006, January). Questions and Answers about the NIMH Sequenced Treatment Alternatives to Relieve Depression (STAR*D)—Background. Available at: https://www.nimh.nih.gov/funding/clinical-research/practical/stard/backgroundstudy.shtml.
148. Rush, A. J., Trivedi, M., Wisniewski, S., Nierenberg, A., Steward, J., Warden, D., Fava, M., “Acute and Longer-term Outcomes in Depressed Outpatients Requiring One or Several Treatment Steps: A STAR*D report,” American Journal of Psychiatry, 2006, vol, 163(11), pp. 1905-1917.
Back to Citation149. Benson, C, Szukis, H. An Evaluation of Increased Clinical and Economic Burden Among Elderly Medicare-covered Beneficiaries With Treatment-Resistant Depression. Poster Presented at the Academy of Managed Care Pharmacy (AMCP) Annual Meeting; April 23-26, 2018; Boston, Massachusetts.
Back to Citation150. Rush, A. J., Trivedi, M., Wisniewski, S., Nierenberg, A., Steward, J., Warden, D., Fava, M., “Acute and Longer-term Outcomes in Depressed Outpatients Requiring One or Several Treatment Steps: A STAR*D report,” American Journal of Psychiatry, 2006, vol. 163(11), pp. 1905-1917.
Back to Citation151. Cristancho, M., & Thase, M, “Drug safety evaluation of olanzapine/fluoxetine combination,” Expert Opinion on Drug Safety, 2014, vol. 13(8), pp. 1133-1141.
Back to Citation152. Daly, E., Singh, J., Fedgchin, M., Cooper, K., Lim, P., Shelton, R., Drevets, W., “Efficacy and Safety of Intranasal Esketamine Adjunctive to Oral Anti-depressant Therapy in Treatment-Resistant Depression,” JAMA Psychiatry, 2018, vol. 75(2), pp. 139-148.
Back to Citation153. Daly, E., Singh, J., Fedgchin, M., Cooper, K., Lim, P., Shelton, R., Drevets, W., “Efficacy and Safety of Intranasal Esketamine Adjunctive to Oral Anti-depressant Therapy in Treatment-Resistant Depression,” JAMA Psychiatry, 2018, vol. 75(2), pp. 139-148.
Back to Citation154. Daly, E., Singh, J., Fedgchin, M., Cooper, K., Lim, P., Shelton, R., Drevets, W., “Efficacy and Safety of Intranasal Esketamine Adjunctive to Oral Anti-depressant Therapy in Treatment-Resistant Depression,” JAMA Psychiatry, 2018, vol. 75(2), pp. 139-148.
Back to Citation155. Fedgchin, M., Trivedi, M., Daly, E., Melkote, R., Lane, R., Lim, P., Singh, J., “Randominzed, Double-blind Study of Fixed-dosed Intranasal Esketamine Plus Oral Anti-depressant vs. Active Control in Treatment-resistant Depression,” 9th Biennial Conference of the International Society for Affective Disorders (ISAD) and the Houston Mood Disorders Conference, September 2018.
Back to Citation156. Popova, V., Daly, E., Trivedi, M., Cooper, K., Lane, R., Lim, P., Singh, J., “Randomized, Double-blind Study of Flexibly-dosed Intranasal Esketamine Pus Oral Anti-depressant vs. Active Control in Treatment-resistant Depression,” Canadian College of Neuropsychopharmacology (CCNP) 41st Annual Meeting, 2018.
Back to Citation157. Fedgchin, M., Trivedi, M., Daly, E., Melkote, R., Lane, R., Lim, P., Singh, J., “Randominzed, Double-blind Study of Fixed-dosed Intranasal Esketamine Plus Oral Anti-depressant vs. Active Control in Treatment-resistant Depression,” 9th Biennial Conference of the International Society for Affective Disorders (ISAD) and the Houston Mood Disorders Conference, September 2018.
Back to Citation158. Alphs, L., Cooper, K., Starr, L., DiBernardo, A., Shawi, M., Jamieson, C., Singh, J., “Clinical Efficacy and Safety of Flexibly Dosed Esketamine Nasal Spray in a US Population of Patients With Treatment-Resistant Depression,” American Psychiatry Association, 2018, Chicago.
Back to Citation159. Ochs-Ross, R., Daly, E., Lane, R., Zhang, Y., Lim, P., Foster, K., Sign, J., “Efficacy and Safety of Esketamine Nasal Spray Plus an Oral Anti-depressant in Elderly Patients with Treatment-resistant Depression,” 2018 Annual Meeting of the American Psychiatric Association (APA), 2018, New York.
Back to Citation160. Starr, L., Ochs-Ross, R., Zhang, Y., Singh, J., Lim, P., Lane, R., Alphs, L., “Clinical Response, Remission, and Safety of Esketamine Nasal Spray in a US Population of Geriatric Patients With Treatment-Resistant Depression,” American Psychiatric Association, 2018, New York.
Back to Citation161. Daly, E., Trivedi, M., Janik, A., Li, H., Zhang, Y., Li, X., Singh, J., “A Randomized Withdrawal, Double-blind, Multicenter Study of Esketamine Nasal Spray Plus an Oral Anti-depressant for Relapse Prevent in Treatment-resistant Depression,” 2018 Annual Meeting of the American Society of Clinical Psychopharmacology (ASCP), 2018, Miami.
Back to Citation162. Wajs, E., Aluisio, L., Morrison, R., Daly, E., Lane, R., Lim, P., Singh, J., “Long-term Safety of Esketamine Nasal Spray Plus Oral Anti-depressant in Patients with Treatment-resistant Depression: Phase III, Open-label, Safety and Efficacy Study (SUSTAIN-2),” 2018 Annual Meeting of the American Society of Clinical Psychopharmacology (ASCP), 2018, Miami.
Back to Citation163. Thorpe, K., Jain, S., & Joski, P., “Prevalence and Spending Associated with Patients Who have a Behavioral Health Disorder and Other Conditions,” Health Affairs, 2017, vol. 36(1), pp. 124-132, doi:10.1377/hlthaff.2016.0875.
164. Druss, B., & Walker, E., 2011, “Mental Disorders and Medical Comorbidity,” Robert Wood Johnson Foundation, 2011. Available at: http://www.policysynthesis.org.
Back to Citation165. Kim, J., & Parish, A., “Polypharmcy and Medication Management in Older Adults,” Nurs Clin N Am, 2017, vol. 52, pp. 457-468, doi: http://dx.doi.org/10.1016/j.cnur.2017.04.007.
166. Kim, L., Koncilja, K., & Nielsen, C., “Medication Management in Older Adults,” Cleveland Clinic Journal of Medicine, 2018, vol. 85(2), pp. 129-135, doi:10.3949/ccjm.85a.16109.
Back to Citation167. Schak, K., Vande Voort, J., Johnson, E., Kung, S., Leung, J., Rasmussen, K., Frye, M., “Potential Risks of Poorly Monitored Ketamine Use in Depression Treatment,” American Journal of Psychiatry, 2016, vol. 173(3), pp. 215-218. Available at: http://www.ajp.psychiatryonline.org.
168. Freedman, R., Brown, A., Cannon, T., Druss, B., Earls, F., Escobar, J., Xin, Y., “Can a Framework be Established for the Safe Use of Ketamine?,” American Journal of Psychiatry, 2018, vol. 7, pp. 587-589. Available at: http://www.ajp.psychiatryonline.org.
169. Sanacora, G., Frye, M., McDonald, W., Mathew, S., Turner, M., Schatzberg, A., Nemeroff, C., “A Consensus Statement on the Use of Ketamine in the Treatment of Mood Disorders,” JAMA Psychiatry, 2017, Special Communication, E1-E6. doi:10.1001/jamapsychiatry.2017.0080.
Back to Citation170. Schak, K., Vande Voort, J., Johnson, E., Kung, S., Leung, J., Rasmussen, K., Frye, M., “Potential Risks of Poorly Monitored Ketamine Use in Depression Treatment,” American Journal of Psychiatry, 2016, vol. 173(3), pp. 215-218. Available at: http://www.ajp.psychiatryonline.org.
Back to Citation171. Sanacora, G., Frye, M., McDonald, W., Mathew, S., Turner, M., Schatzberg, A., Nemeroff, C., “A Consensus Statement on the Use of Ketamine in the Treatment of Mood Disorders,” JAMA Psychiatry, 2017, Special Communication, E1-E6. doi:10.1001/jamapsychiatry.2017.0080.
Back to Citation172. Cristancho MA., Thase ME. Drug safety evaluation of olanzapine/fluoxetine combination. Expert Opin Drug Saf. 2014;13(8):1133-1141.
Back to Citation173. Ochs-Ross R., Daly EJ., Lane R., et al. Efficacy and safety of esketamine nasal spray plus an oral antidepressant in elderly patients with treatment-resistant depression. Poster presented at: Annual Meeting of the American Society of Clinical Psychopharmacology (ASCP); May 29-June 1, 2018; Miami, Florida.
174. Amos T., Tandon N., Lefebvre P., et al. Direct and indirect cost burden and change of employment status in treatment-resistant depression: a matched-cohort study using a U.S. commercial claims database. J. Clin Psychiatry. 2018;79(2).
Back to Citation175. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019a;176(6):428-438.
Back to Citation176. Montgomery SA, Möller HJ. Is the significant superiority of escitalopram compared with other antidepressants clinically relevant? Int Clin Psychopharmacol. 2009;24(3):111-118.
177. Montgomery SA, Nielsen RZ, Poulsen LH, et al. A randomised, double-blind study in adults with major depressive disorder with an inadequate response to a single course of selective serotonin reuptake inhibitor or serotonin-noradrenaline reuptake inhibitor treatment switched to vortioxetine or agomelatine. Hum Psychopharmacol. 2014;29(5):470-482.
Back to Citation178. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of Esketamine Nasal Spray Plus Oral Antidepressant Treatment for Relapse Prevention in Patients with Treatment-Resistant Depression: A Randomized Clinical Trial [Epub ahead of print]. JAMA Psychiatry. 2019a. doi:10.1001/jamapsychiatry.2019.1189
Back to Citation179. Kim J, Farchione T, Potter A, et al. Esketamine for treatment-resistant depression—first FDA-approved antidepressant in a new class [epub ahead of print]. N Engl J Med. 2019 May 22. doi: 10.1056/NEJMp1903305
Back to Citation180. Snaith RP, Harrop FM, Newby DA, Teale C. Grade scores of the Montgomery-Asberg Depression and the Clinical Anxiety Scales. Br J Psychiatry. 1986;148:599-601.
Back to Citation181. Leucht S, Fennema H, Engel RR, et la. What does the MADRS mean? Equipercentile linking with the CGI using a company database of mirtazapine studies. J Affect Disord. 2017; 210:287-293.
182. Turkoz I, Alphs, L, Singh J, et al. Demonstration of the relationship among Clinical Global Impression of Severity of Depression Scale and Montgomery-Åsberg Depression Rating, Patient Health Questionnaire-9, and Sheehan Disability Scales [poster]. Presented at: The International Society for CNS Clinical Trials and Methodology (ISCTM) Annual Scientific Meeting; February 20-22, 2018; Washington, DC.
Back to Citation183. Montgomery SA, Möller HJ. Is the significant superiority of escitalopram compared with other antidepressants clinically relevant? Int Clin Psychopharmacol. 2009;24(3):111-118.
184. Montgomery SA, Nielsen RZ, Poulsen LH, et al. A randomised, double-blind study in adults with major depressive disorder with an inadequate response to a single course of selective serotonin reuptake inhibitor or serotonin-noradrenaline reuptake inhibitor treatment switched to vortioxetine or agomelatine. Hum Psychopharmacol. 2014;29(5):470-482.
Back to Citation185. Daly EJ, Trivedi MH, Janik A, et al. Supplementary Online Content for: Efficacy of Esketamine Nasal Spray Plus Oral Antidepressant Treatment for Relapse Prevention in Patients with Treatment-Resistant Depression: A Randomized Clinical Trial [epub ahead of print]. JAMA Psychiatry. 2019b. doi:10.1001/jamapsychiatry.2019.1189
Back to Citation186. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019a;176(6):428-438.
187. Daly EJ, Trivedi MH, Janik A, et al. Efficacy of Esketamine Nasal Spray Plus Oral Antidepressant Treatment for Relapse Prevention in Patients with Treatment-Resistant Depression: A Randomized Clinical Trial [Epub ahead of print]. JAMA Psychiatry. 2019a. doi:10.1001/jamapsychiatry.2019.1189
Back to Citation188. Kim J, Farchione T, Potter A, et al. Esketamine for treatment-resistant depression—first FDA-approved antidepressant in a new class [epub ahead of print]. N Engl J Med. 2019 May 22. doi: 10.1056/NEJMp1903305.
Back to Citation189. Popova V, Daly EJ, Trivedi M, et al. Data Supplement for: Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019b;176(6):428-438.
Back to Citation190. Atlanta: American Cancer Society; 2017 [cited October 2018]. Available from: https://www.cancer.org/content/dam/cancerorg/research/cancer-facts-and-statistics/cancer-treatment-and-survivorship-facts-and-figures/cancer-treatment-and-survivorshipfacts-and-figures-2016-2017.pdf.
Back to Citation191. Siegel, R.L., Miller, K.D., Jemal, A., “Cancer statistics, 2018,” CA Cancer J Clin, 2018, vol. 68(1), pp. 7-30.
Back to Citation192. Tallman, M.S., “New strategies for the treatment of acute myeloid leukemia including antibodies and other novel agents,” Hematology Am Soc Hematol Educ Program, 2005, pp. 143-50.
Back to Citation193. Rowe, J.M., Tallman, M.S., “How I treat acute myeloid leukemia,” Blood, 2010, vol. 116(17), pp. 3147-56.
194. Breems, D.A., Van Putten, W.L., Huijgens, P.C., Ossenkoppele, G.J., Verhoef, G.E., Verdonck, L.F., et al., “Prognostic index for adult patients with acute myeloid leukemia in first relapse,” J Clin Oncol, 2005, vol. 23(9), pp. 1969-78.
195. Karanes, C., Kopecky, K.J., Head, D.R., Grever, M.R., Hynes, H.E., Kraut, E.H., et al., “A Phase III comparison of high dose ARA-C (HIDAC) versus HIDAC plus mitoxantrone in the treatment of first relapsed of refractory acute myeloid leukemia Southwest Oncology Group Study,” Leuk Res, 1999, vol. 23(9), pp. 787-94.
Back to Citation196. Forman, S.J., Rowe, J.M., “The myth of the second remission of acute leukemia in the adult,” Blood, 2013, vol. 121(7), pp. 1077-82.
Back to Citation197. Rowe, J.M., Tallman, M.S., “How I treat acute myeloid leukemia,” Blood, 2010, vol. 116(17), pp. 3147-56.
Back to Citation198. Itzykson, R., Thepot, S., Berthon, C., et al., “Azacitidine for the treatment of relapsed and refractory AML in older patients,” Leuk Res, 2015, vol. 39, pp. 124-130.
199. Khan, N., Hantel, A., Knoebel, R., et al., “Efficacy of single-agent decitabine in relapsed and refractory acute myeloid leukemia,” Leuk Lymphoma, 2017, vol. 58, pp. 1-7.
Back to Citation200. Giles, F., O'Brien, S., Cortes, J., Verstovsek, S., Bueso-Ramos, C., Shan, J., et al., “Outcome of patients with acute myelogenous leukemia after second salvage therapy,” Cancer, 2005, vol. 104(3), pp. 547-54.
Back to Citation201. Goldstone, A.H., et al., “Attempts to improve treatment outcomes in acute myeloid leukemia (AML) in older patients: the results of the United Kingdom Medical Research Council AML11 trial,” Blood, 2001, vol. 98(5), pp. 1302-1311.
202. Pandya, B.J., et al., “Quality of life of Acute Myeloid Leukemia Patients in a Real-World Setting,” JCO, 2017, vol. 35(15) suppl., e18525.
203. Medeiros, B.C., et al., “Economic Burden of Treatment Episodes in Acute Myeloid Leukemia (AML) Patients in the US: A Retrospective Analysis of a Commercial Payer Database,” ASH, 2017 Poster.
204. Aly, A., et al., “Economic Burden of Relapsed/Refractory AML in the U.S.,” ASH, 2017 Poster.
Back to Citation205. The Cancer Genome Atlas Research Network, “Genomic and Epigenomic Landscapes of Adult De Novo Acute Myeloid Leukemia,” N Engl J Med, 2013, vol. 368(22), pp. 2059-2074.
206. Leukemia and Lymphoma Society Facts 2016-2017. Available at: https://www.lls.org/facts-and-statistics/facts-and-statistics-overview, [Last accessed March 7, 2018].
Back to Citation207. Kindler, T., Lipka, D.B., Fischer, T., “FLT3 as a therapeutic target in AML: still challenging after all these years,” Blood, 2010, vol. 116(24), pp. 5089-102.
Back to Citation208. Yamamoto, Y., Kiyoi, H., Nakano, Y., Suzuki, R., Kodera, Y., Miyawaki, S., et al., “Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies,” Blood,. 2001, vol. 97, pp. 2434-9.En
Back to Citation209. Brunet, S., et al., “Impact of FLT3 Internal Tandem Duplication on the Outcome of Related and Unrelated Hematopoietic Transplantation for Adult Acute Myeloid Leukemia in First Remission: A Retrospective Analysis,” J Clin Oncol, March 1, 2012, vol. 30(7), pp. 735-41.
Back to Citation210. Sotak, M.L., et al., “Burden of Illness of FLT3 Mutated Acute Myeloid Leukemia (AML),” Blood, 2011, vol. 118(21), pp. 4765 4765.
Back to Citation211. Konig, H., Levis, M., “Targeting FLT3 to treat leukemia. Expert Opin Ther Targets,” 2015, vol. 19(1), pp. 37-54.
212. Chevallier, P., Labopin, M., Turlure, P., Prebet, T., Pigneux, A., Hunault, M., et al., “A new Leukemia Prognostic Scoring System for refractory/relapsed adult acute myelogeneous leukaemia patients: a GOELAMS study,” Leukemia, 2011, vol. 25(6), pp. 939-44.
213. Levis, M., Ravandi, F., Wang, E.S., Baer, M.R., Perl, A., Coutre, S., et al., “Results from a randomized trial of salvage chemotherapy followed by lestaurtinib for patients with FLT3 mutant AML in first relapse,” Blood, 2011, vol. 117(12), pp. 3294-301.
Back to Citation214. Astellas, “A Phase 3 Open-label, Multicenter, Randomized Study of ASP2215 versus Salvage Chemotherapy in Patients with Relapsed or Refractory Acute Myeloid Leukemia (AML) with FLT3 Mutation, Clinical Study Report,” March 2018.
Back to Citation215. Ibid.
Back to Citation216. Draft XOSPATA® (package insert) Northbrook, IL, Astellas Pharma US, Inc., 2018.
Back to Citation217. Gale, R.P., Barosi, G., Barbui, T., Cervantes, F., Dohner, K., Dupriez, B., et al., “What are RBC-transfusion-dependence and -independence?,” Leuk. Res, 2011, vol. 35(1).
Back to Citation218. Brachman, D., et al., “Resection and permanent intracranial brachytherpay using modular, biocompatible cesium-131 implants: Results in 20 recurrent previously irradiated meningiomas,” J Neurosurgery, December 21, 2018.
Back to Citation219. Brachman, D., et al., “Surgery and Permanent Intraoperative Brachytherapy Improves Time to Progress of Recurrent Intracranial Neoplasms,” Society for Neuro-Oncology Conference on Meningioma, June 2016.
Back to Citation220. Dardis, C., “Surgery and Permanent Intraoperative Brachytherapy Improves Times to Progression of Recurrent Intracranial Neoplasms,” Society for Neuro-Oncology, November 2014.
Back to Citation221. Brachman, D., et al, “Surgery and Permanent Intraoperative Brachytherapy Improves Time to Progress of Recurrent Intracranial Neoplasms,” Society for Neuro-Oncology Conference on Meningioma, June 2016.
Back to Citation222. Youssef, E., “C-131 Implants for Salvage Therapy of Recurrent High Grade Gliomas,” Society for Neuro-Oncology Annual Meeting, November 2016.
Back to Citation223. Brachman D., Youssef E., Dardis C., et al.: Surgically Targeted Radiation Therapy: Safety Profile of Collagen Tile Brachytherapy in 79 Recurrent, Previously Irradiated Intracranial Neoplasms on a Prospective Clinical Trial. Brachytherapy 18 (2019) S35-36.
Back to Citation224. D'Souza, A., Lee, S., Zhu, X., Pasquini, M., “Current use and trends in hematopoietic cell transplantation in the United States,” Biol Blood Marrow Transplant, 2017, vol. 23(9), pp. 1417-1421.
Back to Citation225. Martin, P.J., Rizzo, J.D., Wingard, J.R., et al., “First and second-line systemic treatment of acute graft-versus-host disease: recommendations of the American Society of Blood and Marrow Transplantation,” Biol Blood Marrow Transplant, 2012, vol. 18(8), pp. 1150-1163.
Back to Citation226. FDA website: https//www.fda.gpv/drugs/resources-information-approved-drugs/fda-approves-ruxolitinib-acute-graft-versus-host-disease.
227. Jakafi Prescribing Information: https://www.acessdata.fda.gov/drugsatfda_docs/label/2019/202192s017lb1.pdf.
Back to Citation228. Martin, P.J., Rizzo, J.D., Wingard, J.R., et al., “First and second-line systemic treatment of acute graft-versus-host disease: recommendations of the American Society of Blood and Marrow Transplantation,” Biol Blood Marrow Transplant, 2012, vol. 18(8), pp. 1150-1163.
Back to Citation229. Martin, P.J., Rizzo, J.D., Wingard, J.R., et al., “First and second-line systemic treatment of acute graft-versus-host disease: recommendations of the American Society of Blood and Marrow Transplantation,” Biol Blood Marrow Transplant, 2012, vol. 18(8), pp. 1150-1163.
Back to Citation230. Martin, P.J., Rizzo, J.D., Wingard, J.R., et al., “First and second-line systemic treatment of acute graft-versus-host disease: recommendations of the American Society of Blood and Marrow Transplantation,” Biol Blood Marrow Transplant, 2012, vol. 18(8), pp. 1150-1163.
Back to Citation231. Martin, P.J., Rizzo, J.D., Wingard, J.R., et al., “First and second-line systemic treatment of acute graft-versus-host disease: Recommendations of the American Society of Blood and Marrow Transplantation,” Biol Blood Marrow Transplant, 2012, vol. 18(8), pp. 1150-1163.
Back to Citation232. Martin, P.J., Rizzo, J.D., Wingard, J.R., et al., “First and second-line systemic treatment of acute graft-versus-host disease: Recommendations of the American Society of Blood and Marrow Transplantation,” Biol Blood Marrow Transplant, 2012, vol. 18(8), pp. 1150-1163.
Back to Citation233. Martin PJ, Rizzo JD, Wingard JR, et al. First and second-line systemic treatment of acute graft-versus-host disease: Recommendations of the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2012;18(8):1150-1163.
Back to Citation234. Burns, R.J., Gibbons, R.J., Yi, Q., et al., “The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis,” J Am Coll Cardiol, 2002, vol. 39, pp. 30-6.
Back to Citation235. Ibid.
Back to Citation236. Stone, G.W., Selker, H.P., Thiele, H., et al., “Relationship between infarct size and outcomes following primary PCI,” J Am Coll Cardiol, 2016, vol. 67(14), pp. 1674-83.
Back to Citation237. Ibid.
Back to Citation238. O'Neill, W.W., Martin, J.L., Dixon, S.R., et al., “Acute Myocardial Infarction with Hyperoxemic Therapy (AMIHOT), J Am Coll Cardiol, 2007, vol. 50(5), pp. 397-405.
Back to Citation239. Ibid.
Back to Citation240. Ibid.
Back to Citation241. Stone, G.W., Martin, J.L., de Boer, M.J., et al., “Effect of Supersaturated Oxygen Delivery on Infarct Size after Percutaneous Coronary Intervention in Acute Myocardial Infarction,” Circ Cardiovasc Intervent, 2009, vol. 2, pp. 366-75.
Back to Citation242. Ibid.
Back to Citation243. Ibid.
Back to Citation244. Warda, H.M., Bax, J.J., Bosch, J.G., et al., “Effect of intracoronary aqueous oxygen on left ventricular remodeling after anterior wall ST-elevation acute myocardial infarction,” Am J Cardiol, 2005, vol. 96(1), pp. 22-4.
Back to Citation245. Ibid.
Back to Citation246. David, SW, Khan, Z.A., Patel, N.C., et al., “Evaluation of intracoronary hyperoxemic oxygen therapy in acute anterior myocardial infarction: The IC-HOT study,” Catheter Cardiovasc Interv, 2018, pp. 1-9.
Back to Citation247. Ibid.
Back to Citation248. Ibid.
Back to Citation249. Ibid.
Back to Citation250. Spears, J.R., Henney, C., Prcevski, P., et al., “Aqueous Oxygen Hyperbaric Reperfusion in a Porcine Model of Myocardial Infarction,” J Invasive Cardiol, 2002, vol. 14(4), pp. 160-6.
251. Spears, J.R., Prcevski, P., Xu, R., et al., “Aqueous Oxygen Attenuation of Reperfusion Microvascular Ischemia in a Canine Model of Myocardial Infarction,” ASAIO J, 2003, vol. 49(6), pp. 716-20.
Back to Citation252. Boucher, H., Talbot, G., Bradley, J., Edwards, J., Gilbert, D., Rice, L., Bartlett, J.,”Bad Bugs, No Drugs: No ESKAPE! An update from the infectious disease society of America,” Clinical Infectious Diseases, 2009, vol. 48, pp. 1-12, doi:10.1086/595011.
253. Rice, L., “Federal Funding for the Study of Antimicrobial Resistance in Nosocomial Pathogens: No ESKAPE,” Journal of Infectious Diseases, 2008, vol. 197, pp. 1079-1081, doi:10.1086/533452.
Back to Citation254. Clancy, C., & Nguyen, H., “T2 magnetic resonance for the diagnosis of bloodstream infections: Charting a path forward,” Journal of Antimicrobial Chemotherapy, 2018, vol. 73(4), pp. iv2-iv5, doi:10.1093/jac/dky050.
Back to Citation255. Clancy, C., & Nguyen, M. H., “Finding the “Missing 50%” of Invasive Candidiasis: How nonculture Diagnostics will improve understanding of disease spectrum and transform patient care,” Clinical Infectious Diseases, 2013, vol. 56(9), pp. 1284-1292, doi:10.1093/cid/cit006.
256. Cockerill, F., Wilson, J., Vetter, E., Goodman, K., Torgerson, C., Harmsen, W., Wilson, W., “Optimal Testing Parameters for Blood Cultures,” Clinical Infectious Diseases, 2004, vol. 38, pp. 1724-1730.
Back to Citation257. Tabak, Y., Vankeepuram, L., Ye, G., Jeffers, K., Gupta, V., & Murray, P., “Blood Culture Turanaround Time in US Acute Care Hospitals and Implications for Laboratory Process Optimization,” Journal of Clinical Microbiology, August 2018, pp. 1-15.
Back to Citation258. T2 Biosystems, Inc., “T2Bacteria® Panel for use on the T2Dx® Instrument, 510(k) summary,” Lexington, 2018.
Back to Citation259. Calderwood, S., “Clinical manifestations, diagnosis and treatment of enterohemorrhagic Escherichia coli (EHEC) infection,” September 2017. Available at: https://www.uptodate.com/contents/clinical-manifestations-diagnosis-and-treatment-of-enterohemorrhagic-escherichia-coli-ehec-infection.
260. Yu, W. L., & Chuang, Y. C., “Clinical features, diagnosis, and treatment of Klebsiella pneumoniae infection,” May 18, 2017. Available at: https://www.uptodate.com/contents/clinical-features-diagnosis-and-treatment-of-klebsiella-pneumoniae-infection?search=Klebsiella%20pneumoniae&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1.
261. Kanj, S., & Sexton, D., “Epidemiology, microbiology, and pathogenesis of Pseudomonas aeruginosa infection,” October 9, 2018. Available at: https://www.uptodate.com/contents/epidemiology-microbiology-and-pathogenesis-of-pseudomonas-aeruginosa;-infection?search=Pseudomonas%20aeruginosa&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2.
262. Holland, T., & Fowler, V., “Clinical manifestations of Staphylococcus aureus infection in adults,” September 22, 2017. Available at: https://www.uptodate.com/contents/clinical-manifestations-of-staphylococcus-aureus-infection-in-adults?search=Staphylococcus%20aureus&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3.
263. Murray, B., “Microbiology of enterococci,” August 31, 2017. Available at: https://www.uptodate.com/contents/microbiology-of-enterococci?search=Enterococcus%20faecium&source=search_result&selectedTitle=2~21&usage_type=default&display_rank=2.
Back to Citation264. Huang, A., Newton, D., Kunapuli, A., Gandhi, T., Washer, L., Isip, J., Nagel, J., “Impact of Rapid Organism Identification via Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Combined with Antimicrobial Stewardship Team Intervention in Adult Patients with Bacteremia and Candidemia,” Clinical Infectious Diseases, 2013, vol. 57(9), pp. 1237-1245.
265. Perez, K., Olsen, R., Musick, W., Cernoch, P., Davis, J., Peterson, L., & Musser, J., “Integrating Rapid Diagnostics and Antimicrobial Stewardship Improves Outcomes in Patients with Antibiotic-Resistant Gram-Negative Bacteremia,” Journal of Infection, 2014, vol. 69(3), pp. 216-225.
Back to Citation266. T2 Biosystems, Inc., “T2Bacteria® Panel for use on the T2Dx® Instrument, 510(k) summary,” Lexington, 2018.
Back to Citation267. Nguyen, M. H., Clancy, C., Pasculle, A. W., Pappas, P., Alangaden, G., Pankey, G., Mylonakis, E. “Clinical performance of the T2Bacteria panel for diagnosis bloodstream infections due to five common bacterial pathogens,” Manuscript for submission.
Back to Citation268. T2 Biosystems, Inc., “T2Bacteria® Panel for use on the T2Dx® Instrument, 510(k) summary,” Lexington, 2018.
Back to Citation269. Voigt, C., Silbert, S., Widen, R., Marturano, J., Lowery, T., Ashcraft, D., & Pankey, G., “The T2Bacteria assay is a sensitive and rapid detector of bacteremia that can be initiated in the emergency department and has potential to favorably influence subsequent therapy,” Journal of Emergency Medical Review, pp. 1-30.
Back to Citation270. Ibid.
Back to Citation271. Voigt, C., Silbert, S., Widen, R., Marturano, J., Lowery, T., Ashcraft, D., & Pankey, G., “The T2Bacteria assay is a sensitive and rapid detector of bacteremia that can be initiated in the emergency department and has potential to favorably influence subsequent therapy,” Journal of Emergency Medical Review, pp. 1-30.
Back to Citation272. De Angelis, G., Posteraro, B., Dr. Carolis, E., Menchinelli, G., Franceschi, F., Tumbarello, M., Sanguinetti, M., “T2Bacteria magnetic resonance assay for the rapid detection of ESKAPEc pathogens directly in whole blood,” Journal of Antimicrobial Chemotherapy, 2018, vol. 73, pp. iv20-iv26, doi:10.1093/jac/dky049.
273. Nguyen, M. H., Clancy, C., Pasculle, A. W., Pappas, P., Alangaden, G., Pankey, G., Mylonakis, E., “Clinical performance of the T2Bacteria panel for diagnosis bloodstream infections due to five common bacterial pathogens,” Manuscript for submission.
Back to Citation274. De Angelis, G., Posteraro, B., Dr. Carolis, E., Menchinelli, G., Franceschi, F., Tumbarello, M., Sanguinetti, M., “T2Bacteria magnetic resonance assay for the rapid detection of ESKAPEc pathogens directly in whole blood,” Journal of Antimicrobial Chemotherapy, 2018, vol. 73, pp. iv20-iv26, doi:10.1093/jac/dky049.
Back to Citation275. Clancy, C., & Nguyen, H., “T2 magnetic resonance for the diagnosis of bloodstream infections: charting a path forward,” Journal of Antimicrobial Chemotherapy, 2018, vol. 73(4), pp. iv2-iv5, doi:10.1093/jac/dky050.
Back to Citation276. Paul, M., Shani, V., Muchtar, E., Kariv, G., Robenshtok, E., & Leibovici, L., “Systematic Review and Meta-Analysis of the Efficacy of Appropriate Empiric Antibiotic Therapy for Sepsis,” Antimicrobial Agents and Chemotherapy, 2010, vol. 54(11), pp. 4851-4863.
Back to Citation277. Castellanos-Ortega, A., Suberviola, B., Garcia-Astudillo, L., Holanda, M., Ortiz, F., Llorca, J., & Delgado-Rodriguez, M., “Impact of the Surviving Sepsis Campaign Protocols on Hospital Length of Stay and Mortality in Septic Shock Patients: Results of a three-year follow-up quasi-experimental study,” Crit Care Med, 2010, vol. 38(4), pp. 1036-1043, doi:10.1097/CCM.0b0bl3e3181d455b6.
278. Karlsson, S., Varpula, M., Pettila, V., & Parvlainen, I., “Incidence, Treatment, and Outcome of Severe Sepsis in ICU-treated Adults in Finland: The Finnsepsis study,” Intensive Care Medicine, 2007, vol. 33, pp. 435-443, doi:10.1007/s00134-006-0504-z.
279. Suberviola, B., Marquez-Lopez, A., Castellanos-Ortega, A., Fernandez-Mazarrasa, C., Santibanez, M., & Martinez, L., “Microbiological Diagnosis of Speis: Polymerase chain reaction system versus blood cultures,” American Journal of Critical Care, 2016, vol. 25(1), pp. 68-75.
Back to Citation280. Voigt, C., Silbert, S., Widen, R., Marturano, J., Lowery, T., Ashcraft, D., & Pankey, G., “The T2Bacteria assay is a sensitive and rapid detector of bacteremia that can be initiated in the emergency department and has potential to favorably influence subsequent therapy,” Journal of Emergency Medical Review, pp. 1-30.
Back to Citation281. Ohji, G., Doi, A., Yamamoto, S., & Iwata, K., “Is De-escalation of Antimicrobials Effective? A systematic review and meta-analysis,” International Journal of Infectious Diseases, 2016, vol. 49, pp. 71-79, Retrieved from http://dx.doi.org/10.1016/j.ijid.2016.06.002.
Back to Citation282. Bhattacharyya, S., Darby, R. R., Raibagkar, P., Gonzalez Castro, L. N., & Berkowitz, A., “Antibiotic-associated Encephalopathy,” American Academy of Neurology, 2016, pp. 963-971.
Back to Citation283. Koch-Weser, J., Sidel, V., Federman, E., Kanarek, P., Finer, D., & Eaton, A., “Adverse Effects of Sodium Colistimethate; Manifestations and specific reaction rates during 317 courses of therapy,” Annals of Internal Medicine, 1970, vol. 72, pp. 857-868.
Back to Citation284. Nguyen, M. H., Clancy, C., Pasculle, A. W., Pappas, P., Alangaden, G., Pankey, G., Mylonakis, E., “Clinical performance of the T2Bacteria panel for diagnosis bloodstream infections due to five common bacterial pathogens,” Manuscript for submission.
Back to Citation285. Weisz, E., Newton, E., Estrada, S., & Saunders, M., “Early Experience with the T2Bacteria Research Use Only (RUO) Panel at a Community Hospital,” Lee Memorial Hospital, Fort Meyers.
Back to Citation286. Paul, M., Shani, V., Muchtar, E., Kariv, G., Robenshtok, E., & Leibovici, L., “Systematic Review and Meta-Analysis of the Efficacy of Appropriate Empiric Antibiotic Therapy for Sepsis,” Antimicrobial Agents and Chemotherapy, 2010, vol. 54(11), pp. 4851-4863.
287. Kumar, A., Roberts, D., Wood, K., Light, B., Parrillo, J., Sharma, S., Cheang, M., “Duration of Hypotension before Initiation of Effective Antimicrobial Therapy is the Critical Determinant of Survival in Human Septic Shock,” Crit Care Med, 2006, vol. 34(6), pp. 1589-1596, doi:10.1097/01.CCM.0000217961.75225.E9.
288. Seymour, C., Gesten, F., Prescott, H., Friedrich, M., Iwashyna, T., Phillips, G., Levy, M., “Time to Treatment and Mortality during Mandated Emergency Care for Sepsis,” The New England Journal of Medicine, 2017, vol. 376(23), pp. 2235-2244, doi:10.1056/NEJMoa1703058.
Back to Citation289. Paul, M., Shani, V., Muchtar, E., Kariv, G., Robenshtok, E., & Leibovici, L., “Systematic Review and Meta-Analysis of the Efficacy of Appropriate Empiric Antibiotic Therapy for Sepsis,” Antimicrobial Agents and Chemotherapy, 2010, vol. 54(11), pp. 4851-4863.
Back to Citation290. Voigt, C., Silbert, S., Widen, R., Marturano, J., Lowery, T., Ashcraft, D., & Pankey, G., “The T2Bacteria assay is a sensitive and rapid detector of bacteremia that can be initiated in the emergency department and has potential to favorably influence subsequent therapy,” Journal of Emergency Medical Review, pp. 1-30.
Back to Citation291. Wilson, M., Mitchell, M., Morris, A., Murray, P., Reimer, L., Reller, L. B., Welch, D., “Prinicples and Procedures for Blood Cultures; Approved Guildeline,” Clinical and Laboratory Standards Institute, 2007.
Back to Citation292. T2 Biosystems, Inc., “T2Bacteria® Panel for use on the T2Dx® Instrument, 510(k) summary,” Lexington, 2018.
Back to Citation293. De Angelis, G., Posteraro, B., Dr Carolis, E., Menchinelli, G., Franceschi, F., Tumbarello, M., Sanguinetti, M., “T2Bacteria magnetic resonance assay for the rapid detection of ESKAPEc pathogens directly in whole blood,” Journal of Antimicrobial Chemotherapy, 2018, vol. 73, pp. iv20-iv26, doi:10.1093/jac/dky049.
Back to Citation294. Nguyen, M. H., Clancy, C., Pasculle, A. W., Pappas, P., Alangaden, G., Pankey, G., Mylonakis, E., “Clinical performance of the T2Bacteria panel for diagnosis bloodstream infections due to five common bacterial pathogens,” Manuscript for submission.
Back to Citation295. Doern GV, Vautour R, Gaudet M, Levy B. Clinical impact of rapid in vitro susceptibility testing and bacterial identification. J Clin Microbiol. 1994;32(7):1757-62.
296. Byl B, Clevenbergh P, Jacobs F, et al. Impact of infectious diseases specialists and microbiological data on the appropriateness of antimicrobial therapy for bacteremia. Clin Infect Dis. 1999;29(1):60-6; discussion 7-8. Epub 1999/08/05.
297. Kerremans JJ, Verbrugh HA, Vos MC. Frequency of microbiologically correct antibiotic therapy increased by infectious disease consultations and microbiological results. J Clin Microbiol. 2012;50(6):2066-8. Epub 2012/03/17.
Back to Citation298. She RC, Alrabaa S, Lee SH, Norvell M, Wilson A, Petti CA. Survey of physicians' perspectives and knowledge about diagnostic tests for bloodstream infections. PLoS One. 2015;10(3):e0121493.
Back to Citation299. Karlowsky JA, Jones ME, Draghi DC, Thornsberry C, Sahm DF, Volturo GA. Prevalence and antimicrobial susceptibilities of bacteria isolated from blood cultures of hospitalized patients in the United States in 2002. Ann Clin Microbiol Antimicrob. 2004;3:7. Epub 2004/05/12.
300. Kumar A, Ellis P, Arabi Y, et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest. 2009;136(5):1237-48.
301. Boucher HW, Talbot GH, Bradley JS, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(1):1-12. Epub 2008/11/28.
302. Karlowsky JA, Jones ME, Draghi DC, Thornsberry C, Sahm DF, Volturo GA. Prevalence and antimicrobial susceptibilities of bacteria isolated from blood cultures of hospitalized patients in the United States in 2002. Ann Clin Microbiol Antimicrob. 2004;3:7. Epub 2004/05/12.
303. Kumar A, Ellis P, Arabi Y, et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest. 2009;136(5):1237-48.
Back to Citation304. Nguyen MH, Clancy CJ, Pasculle AW, et al. Performance of the T2Bacteria Panel for Diagnosing Bloodstream Infections: A Diagnostic Accuracy Study. Ann Intern Med. 2019. Epub 2019/05/15.
Back to Citation305. Zacharioudakis IM, Zervou FN, Shehadeh F, Mylonakis E. Cost-effectiveness of molecular diagnostic assays for the therapy of severe sepsis and septic shock in the emergency department. PLoS One. 2019;14(5):e0217508. Epub 2019/05/28.
Back to Citation306. Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L. Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother. 2010;54(11):4851-63. Epub 2010/08/25.
Back to Citation307. Roustit M, Francois P, Sellier E, et al. Evaluation of glycopeptide prescription and therapeutic drug monitoring at a university hospital. Scand J Infect Dis. 2010;42(3):177-84. Epub 2009/12/17.
Back to Citation308. Logsdon BA, Lee KR, Luedtke G, Barrett FF. Evaluation of vancomycin use in a pediatric teaching hospital based on CDC criteria. Infect Control Hosp Epidemiol. 1997;18(11):780-2. Epub 1997/12/16.
Back to Citation309. Kim NH, Koo HL, Choe PG, et al. Inappropriate continued empirical vancomycin use in a hospital with a high prevalence of methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2015;59(2):811-7. Epub 2014/11/19.
Back to Citation310. Junior MS, Correa L, Marra AR, Camargo LF, Pereira CA. Analysis of vancomycin use and associated risk factors in a university teaching hospital: a prospective cohort study. BMC Infect Dis. 2007;7:88. Epub 2007/08/07.
Back to Citation311. https://ascopubs.org/doi/full/10.1200/jop.0922001.
Back to Citation312. 21 U.S.C. 355f(g)(l)-(2).
Back to Citation313. “Antibiotic/Antimicrobial Resistance (AR/AMR),” Centers for Disease Control and Prevention, (page last updated Sept. 10, 2018), https://www.cdc.gov/drugresistance/index.html.
Back to Citation314. Internal analysis from the Centers for Disease Control and Prevention.
Back to Citation315. Id.
Back to Citation316. Certification of Rates of Uninsured. March 28, 2019. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInPatientPPS/dsh.html.
Back to Citation317. Medicare Payment Advisory Commission (MedPAC), “Chapter 1, The Effects of the Hospital Readmissions Reduction Program,” Report to Congress: Medicare and Health Care Delivery System, June 2018. http://www.medpac.gov/docs/default-source/reports/jun18_ch1_medpacreport_sec.pdf?sfvrsn=0.
Back to Citation318. When there is reason to believe that the continued collection of a measure as it is currently specified raises potential patient safety concerns, CMS will take immediate action to remove a measure from the program and not wait for the annual rulemaking cycle. In such situations, we would promptly retire such measures followed by subsequent confirmation of the retirement in the next IPPS rulemaking. When we do so, we will notify hospitals and the public through the usual hospital and QIO communication channels used for the Hospital Readmissions Reduction Program, which include memo and email notification and QualityNet website articles and postings.
Back to Citation319. We refer readers to the Hospital IQR Program's measure removal factors discussions in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49641 through 49643) and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41540 through 41544) for additional details on the removal factors and the rationale supporting them.
Back to Citation320. In addition, it has come to our attention that the determination of dual eligibility is made from data sourced from the State MMA files, not the original State MMA files. The program also considers this to be a nonsubstantive change as the data are obtained from the previously finalized specified source.
Back to Citation321. QualityNet. Confidential Reporting Overview: Disparity Methods. Available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776708906.
Back to Citation322. https://www.qualitynet.org/dcs/ContentServer?cid=%201219069855841&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page.
Back to Citation323. Please note that this sentence was updated via the Correction Notice (CMS-1716-CN) published on June 18, 2019. We refer readers to the correction notice for more information.
Back to Citation324. We previously adopted the two criteria for determining the “topped-out” status of Hospital VBP Program measures in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50055).
Back to Citation325. The FY 2019 IPPS/LTCH PPS final rule (83 FR 41478 through 41483) includes additional information regarding provider selection, targeting criteria, calculation of the confidence, education review process, and application of validation penalty for the HAC Reduction Program's validation processes compared to the Hospital IQR Program's processes. We also refer readers to section IV.I.7. of the preamble of this final rule for changes to the validation selection methodology and clarifications to the validation filtering methodology for the HAC Reduction Program.
Back to Citation326. The term “Never Event” was first introduced in 2001 by Ken Kizer, MD, former CEO of the National Quality Forum (NQF), in reference to particularly shocking medical errors (such as wrong-site surgery) that should never occur. Over time, the list has been expanded to signify adverse events that are unambiguous (clearly identifiable and measurable), serious (resulting in death or significant disability), and usually preventable. The NQF initially defined 27 such events in 2002. The list has been revised since then, most recently in 2011, and now consists of 29 events grouped into 7 categories: Surgical, product or device, patient protection, care management, environmental, radiologic, and criminal.” Never Events are available at: https://psnet.ahrq.gov/primers/primer/3/neverevents.
Back to Citation327. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41485 through 41489), we finalized the equal weighting of measures to coincide with the removal of Domains for scoring purposes, so these measures are no longer grouped by Domain.
Back to Citation328. When there is reason to believe that the continued collection of a measure as it is currently specified raises potential patient safety concerns, CMS will take immediate action to remove a measure from the program and not wait for the annual rulemaking cycle. In such situations, we would promptly retire such measures followed by subsequent confirmation of the retirement in the next IPPS rulemaking. When we do so, we will initially notify hospitals and the public through the usual hospital and QIO communication channels used for the HAC Reduction Program, which include memo and email notification and QualityNet website articles and postings, and if necessary, will proceed via notice and comment rulemaking.
Back to Citation329. We refer readers to the Hospital IQR Program's removal factors discussions in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49641 through 49643) and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41540 through 41544) for additional details on the removal factors and the rationale supporting them.
Back to Citation330. FY 2011 IPPS/LTCH PPS final rule (75 FR 50223 through 50224); FY 2012 IPPS/LTCH PPS final rule (76 FR 51644 through 51645); FY 2013 IPPS/LTCH PPS final rule (77 FR 53539); FY 2014 IPPS/LTCH PPS final rule (78 FR 50821 through 50822); FY 2015 IPPS/LTCH PPS final rule (79 FR 50259 through 50262); FY 2016 IPPS/LTCH PPS final rule (80 FR 49710); FY 2017 IPPS/LTCH PPS final rule (81 FR 57173); FY 2018 IPPS/LTCH PPS final rule (82 FR 38398); FY 2019 IPPS/LTCH PPS final rule (83 FR 41607).
Back to Citation331. The CMS Clinical Data Abstraction Center (CDAC) performs the validation.
Back to Citation332. We refer readers to the FY 2019 IPPS/LTCH PPS final rule (83 FR 41480), where we detailed the criteria for selecting additional hospitals for targeted validation.
Back to Citation333. We refer readers to CDC guidance on this issue and the “CLABSI Tool Display” on the CDC website and on QualityNet, located at: http://www.cdc.gov/nhsn/PDFs/pscManual/2PSC_IdentifyingHAIs_NHSNcurrent.pdf and https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1140537256076.
Back to Citation334. April 2017 OIG report titled “CMS Validated Hospital Inpatient Quality Reporting Program Data, But Should Use Additional Tools to Identify Gaming.” Available at: https://www.oig.hhs.gov/oei/reports/oei-01-15-00320.asp.
Back to Citation335. Meaningful Measures web page: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/MMF/General-info-Sub-Page.html.
Back to Citation336. Rudd, R., Aleshire, N., Zibbell, J. & Gladden, R.M. (2016). Increases in Drug and Opioid Overdose Deaths—United States, 2000-2014. Morbidity and Mortality Weekly Report, 64(50): 1378-82. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm.
Back to Citation337. Centers for Disease Control and Prevention. Drug Overdose Epidemic: Behind the Numbers. Available at: https://www.cdc.gov/drugoverdose/data/index.html.
Back to Citation338. Sun, E., Dixit, A., Humphreys, K., Darnall, B., Baker, L. & Mackey, S. (2017). Association Between Concurrent Use of Prescription Opioids and Benzodiazepines and Overdose: Retrospective Analysis. BMJ, 356: j760.
Back to Citation339. Dowell, D., Haegerich, T. & Chou, R. (2016). CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. Morbidity and Mortality Weekly Report: Recommendations and Reports, 65. Available at: http://www.cdc.gov/media/dpk/2016/dpk-opioid-prescription-guidelines.html.
Back to Citation340. National Institute on Drug Abuse. Benzodiazepines and Opioids. Available at: https://www.drugabuse.gov/drugs-abuse/opioids/benzodiazepines-opioids.
341. Sun, E., Dixit, A., Humphreys, K., Darnall, B., Baker, L. & Mackey, S. (2017). Association Between Concurrent Use of Prescription Opioids and Benzodiazepines and Overdose: Retrospective Analysis. BMJ, 356: j760.
Back to Citation342. Dasgupta, N., Jonsson Funk, M., Proescholdbell, S., Hirsch, A., Ribisl, K.M. & Marshall, S. (2015). Cohort Study of the Impact of High-Dose Opioid Analgesics on Overdose Mortality. Pain Medicine. Available at: http://onlinelibrary.wiley.com/doi/10.1111/pme.12907/abstract.
Back to Citation343. Liu, Y., Logan, J., Paulozzi, L., Zhang, K., Jones, C. (2013). Potential Misuse and Inappropriate Prescription Practices Involving Opioid Analgesics. American Journal of Managed Care, 19(8): 648-65.
344. Mack, K., Zhang, K., Paulozzi, L. & Jones, C. (2015). Prescription Practices Involving Opioid Analgesics Among Americans with Medicaid, 2010. Journal of Health Care for the Poor and Underserved, 26(1): 182-98.
345. Park, T., Saitz, R., Ganoczy, D., Ilgen, M.A. & Bohnert, A.S.B. (2015). Benzodiazepine Prescribing Patterns and Deaths from Drug Overdose Among U.S. Veterans Receiving Opioid Analgesics: Case-Cohort Study. BMJ, 350: h2698.
Back to Citation346. Jones, C.M. & McAninch, J.K. (2015). Emergency Department Visits and Overdose Deaths from Combined Use of Opioids and Benzodiazepines. American Journal of Preventive Medicine, 49(4): 493-501.
Back to Citation347. Sun, E., Dixit, A., Humphreys, K., Darnall, B., Baker, L. & Mackey, S. (2017). Association Between Concurrent Use of Prescription Opioids and Benzodiazepines and Overdose: Retrospective Analysis. BMJ, 356: j760.
Back to Citation348. Office of the Assistant Secretary for Preparedness and Response (ASPR). Public Health Emergency Declarations. Available at: https://www.phe.gov/emergency/news/healthactions/phe/pages/default.aspx.
Back to Citation349. In April 2017, HHS identified the opioid crisis as a top priority and prioritized five specific strategies to combat the epidemic, including “Better Data” on the epidemic to improve our understanding of the crisis. HHS aims to strengthen public health data collection and reporting to improve the timeliness and specificity of data and to inform a real-time public health response as the epidemic evolves. In its Strategy to Combat Opioid Abuse, Misuse, and Overdose, HHS sets forth a number of activities that can be taken by the Secretary and HHS agencies to advance its “Better Data” strategy, including the collection of data on opioid prescriptions, new drug patterns, and related harms, with minimal lag time. More information on HHS' Opioid Strategy is available at: https://www.hhs.gov/opioids/about-the-epidemic/hhs-response/index.html.
Back to Citation350. The Safe Use of Opioids—Concurrent Prescribing measure also addresses the quality priority of “Promoting Effective Communication and Coordination of Care” through the Meaningful Measure area of “Medication Management.” More information on CMS' Meaningful Measures Initiative is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/MMF/General-info-Sub-Page.html.
Back to Citation351. Dowell, D., Haegerich, T. & Chou, R. (2016). CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. Morbidity and Mortality Weekly Report: Recommendations and Reports, 65. Available at: https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm.
Back to Citation352. See, for example, American Academy of Emergency Medicine, Emergency Department Opioid Prescribing Guidelines for the Treatment of Non-Cancer Related Pain (available at: https://www.deepdyve.com/lp/elsevier/american-academy-of-emergency-medicine-PlQtPNi8J4) (recommending that clinicians should avoid prescribing opioid analgesics to patients currently taking sedative hypnotic medications or concurrent opioid analgesics); Washington State Agency Medical Directors' Group, Interagency Guideline on Prescribing Opioids for Pain (available at: http://agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf) (recommending that clinicians should avoid combining opioids with benzodiazepines, sedative-hypnotics or barbiturates when prescribing opioid for chronic noncancer pain).
Back to Citation353. Gao, A., Bandyopadhyay, J., Barrett, K., Morales, N. & Tu, D. (2017). Beta Testing Report on the Safe Use of Opioids—Concurrent Prescribing Electronic Clinical Quality Measure. Hospital Inpatient and Outpatient Process and Structural Measure Development and Maintenance Project (HHSM-500-2013-13011I, Task Order HHSM-500-T0003).
Back to Citation354. List of Measures Under Consideration for December 1, 2016. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=83923.
Back to Citation355. 2016-2017 Spreadsheet of Final Recommendations to HHS and CMS. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=84452.
Back to Citation356. Measure Applications Partnership, January 2017 NQF MAP Coordinating Committee Meeting Transcript. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75367.
Back to Citation357. Measure Worksheet. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=86521.
Back to Citation358. Ibid.
Back to Citation359. National Quality Forum. (2018). Patient Safety Fall 2017 Final Report. Available at: http://www.qualityforum.org/Publications/2018/07/Patient_Safety_Fall_2017_Final_Report.aspx.
Back to Citation360. Ibid.
Back to Citation361. Ibid.
Back to Citation362. Meeting agenda from November 8, 2018 web meeting are available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=88674. Presentation slides are available at: http://www.qualityforum.org/Projects/i-m/MAP/Hospital_Workgroup/Slides_11082018.aspx.
Back to Citation363. The Veterans Health Administration (VHA), as part of its Opioid Safety Initiative, implemented a measure of concurrent opioid and benzodiazepine prescribing that is similar to the Safe Use of Opioids—Concurrent Prescribing measure. The Opioid Safety Initiative was associated with a decrease in patients receiving benzodiazepine concurrently with an opioid—specifically, a recent study showed a 20.67 percent decrease overall and a 0.86 percent decrease in patients per month (781 patients per month)—among all adult VHA patients who filled outpatient opioid prescriptions from October 2012 to September 2014. See Lin, L.A., Bohnert, A.S., Kerns, R.D., Clay, M.A., Ganoczy, D. & Ilgen, M.A. (2017). Impact of the Opioid Safety Initiative on Opioid-Related Prescribing in Veterans. Pain, 158(5): 833-39.
Back to Citation364. National Quality Forum. What NQF Endorsement Means. Available at: http://www.qualityforum.org/Measuring_Performance/ABCs/What_NQF_Endorsement_Means.aspx.
Back to Citation365. National Quality Forum. (2018). Patient Safety, Fall 2017 Final Report. Available at: http://www.qualityforum.org/Publications/2018/07/Patient_Safety_Fall_2017_Final_Report.aspx.
Back to Citation366. National Quality Forum. (2018). Patient Safety, Fall 2017 Final Report. Available at: http://www.qualityforum.org/Publications/2018/07/Patient_Safety_Fall_2017_Final_Report.aspx.
Back to Citation367. Office of Disease Prevention and Health Promotion (ODPHP). (2014). National Action Plan for Adverse Drug Event Prevention. Available at: https://health.gov/hcq/ade-action-plan.asp.
Back to Citation368. Measure specifications for ED-02 are available at: https://ecqi.healthit.gov/ecqm/measures/cms111v8.
Back to Citation369. https://www.healthit.gov/test-method/computerized-provider-order-entry-cpoe-medications.
Back to Citation370. Available at: https://oncprojectracking.healthit.gov/support/secure/BrowseProjects.jspa?selectedCategory=all&selectedProjectType=all.
Back to Citation371. Clarification letter to NCCN, ASCO, and ASH on the CDC's Guideline for Prescribing Opioids for Chronic Pain. February 2019. Available at: https://www.asco.org/sites/new-www.asco.org/files/content-files/advocacy-and-policy/documents/2019-CDC-Opioid-Guideline-Clarification-Letter-to-ASCO-ASH-NCCN.pdf.
Back to Citation372. U.S. Dep't of Food & Drug Administration. (2019). Opioid Use Disorder: Developing Depot Buprenorphine Products for Treatment Guidance for Industry. Available at: https://www.fda.gov/media/112739/download.
Back to Citation373. See, for example, American Academy of Emergency Medicine, Emergency Department Opioid Prescribing Guidelines for the Treatment of Non-Cancer Related Pain (available at: https://www.deepdyve.com/lp/elsevier/american-academy-of-emergency-medicine-PlQtPNi8J4); Washington State Agency Medical Directors' Group, Interagency Guideline on Prescribing Opioids for Pain (available at: http://agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf); and American Society of Interventional Pain Physicians (ASIPP), Guidelines for Responsible Opioid Prescribing in Chronic Noncancer Pain (available at: https://www.asipp.org/opioidguidelines.htm).
Back to Citation374. Dowell, D., Haegerich, T. & Chou, R. (2016). CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. Morbidity and Mortality Weekly Report: Recommendations and Reports, 65. Available at: http://www.cdc.gov/media/dpk/2016/dpk-opioid-prescription-guidelines.html.
Back to Citation375. Available at: https://oncprojectracking.healthit.gov/support/secure/BrowseProjects.jspa?selectedCategory=all&selectedProjectType=all.
Back to Citation376. Dowell, D., Haegerich, T. & Chou, R. No Shortcuts to Safer Opioid Prescribing. N. Engl. J. Med. 380:24 (June 13, 2019).
Back to Citation377. Dowell, D., Haegerich, T., Chou, R. “CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016”. MMWR Recomm Rep 2016;65. http://www.cdc.gov/media/dpk/2016/dpk-opioid-prescription-guidelines.html.
Back to Citation378. Cantrill SV, Brown MD, Carlisle RJ, et al.; American College of Emergency Physicians Opioid Guideline Writing Panel. Clinical policy: Critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med 2012;60:499-525.
Back to Citation379. American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: An updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012;116:248-73.
Back to Citation380. Washington State Agency Medical Directors' Group. AMDG 2015 interagency guideline on prescribing opioids for pain. Olympia, WA: Washington State Agency Medical Directors' Group; 2015. http://www.agencymeddirectors.wa.gov/guidelines.asp.
Back to Citation381. Cantrill SV, Brown MD, Carlisle RJ, et al.; American College of Emergency Physicians Opioid Guideline Writing Panel. Clinical policy: Critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med 2012;60:499-525.
382. American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: An updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012;116:248-73.
383. Washington State Agency Medical Directors' Group. AMDG 2015 interagency guideline on prescribing opioids for pain. Olympia, WA: Washington State Agency Medical Directors' Group; 2015. http://www.agencymeddirectors.wa.gov/guidelines.asp.
Back to Citation384. Cantrill SV, Brown MD, Carlisle RJ, et al.; American College of Emergency Physicians Opioid Guideline Writing Panel. Clinical policy: Critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med 2012;60:499-525.
385. American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: An updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012;116:248-73.
386. Washington State Agency Medical Directors' Group. AMDG 2015 interagency guideline on prescribing opioids for pain. Olympia, WA: Washington State Agency Medical Directors' Group; 2015. http://www.agencymeddirectors.wa.gov/guidelines.asp.
Back to Citation387. See, for example, American Academy of Emergency Medicine, Emergency Department Opioid Prescribing Guidelines for the Treatment of Non-Cancer Related Pain (available at: https://www.deepdyve.com/lp/elsevier/american-academy-of-emergency-medicine-PlQtPNi8J4); Washington State Agency Medical Directors' Group, Interagency Guideline on Prescribing Opioids for Pain (available at: http://agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf).
Back to Citation388. Meisenberg BR, Grover J, Campbell C, Korpon D. Assessment of Opioid Prescribing Practices Before and After Implementation of a Health System Intervention to Reduce Opioid Overprescribing. JAMA Netw Open. Sept. 28, 2018. 1(5):e182908. doi:10.1001/jamanetworkopen.2018.2908.
Back to Citation389. Sun, E., Dixit, A., Humphreys, K., Darnall, B., Baker, L. & Mackey, S. (2017). Association Between Concurrent Use of Prescription Opioids and Benzodiazepines and Overdose: Retrospective Analysis. BMJ, 356: j760.
Back to Citation390. Gao, A., Bandyopadhyay, J., Barrett, K., Morales, N. & Tu, D. (2017). Beta Testing Report on the Safe Use of Opioids—Concurrent Prescribing Electronic Clinical Quality Measure. Hospital Inpatient and Outpatient Process and Structural Measure Development and Maintenance Project (HHSM-500-2013-13011I, Task Order HHSM-500-T0003).
Back to Citation391. National Quality Forum. (2018). Patient Safety Fall 2017 Final Report. Available at: http://www.qualityforum.org/Publications/2018/07/Patient_Safety_Fall_2017_Final_Report.aspx.
Back to Citation392. The Office of the National Coordinator for Health Information Technology. (2018). Strategy on Reducing Regulatory and Administrative Burden Relating to the Use of Health IT and EHRs (Draft for Public Comment). Available at: https://www.healthit.gov/sites/default/files/page/2018-11/Draft%20Strategy%20on%20Reducing%20Regulatory%20and%20Administrative%20Burden%20Relating.pdf.
Back to Citation393. Available at: https://oncprojectracking.healthit.gov/support/secure/BrowseProjects.jspa?selectedCategory=all&selectedProjectType=all.
Back to Citation394. Value sets are lists of codes and corresponding terms from National Library of Medicine (NLM)-hosted standard clinical vocabularies (such as SNOMED CT, RxNorm, LOINC and others). Value Set Authority Center. Available at: https://vsac.nlm.nih.gov/welcome.
Back to Citation395. While the VSAC does not create value set content, it is a central repository for, and provides downloadable access to, all official versions of value sets that support CMS' eCQMs. The VSAC provides measure developers with tools to search existing value sets, create new value sets, and maintain value set content consistent with current versions of the terminologies they use. The VSAC is provided by the NLM in collaboration with ONC and CMS. More information is available at the VSAC website (available at: https://vsac.nlm.nih.gov/welcome) and the eCQI Resource Center (available at: https://ecqi.healthit.gov/ecqi-tools-key-resources/content/vsac).
Back to Citation396. Kessler, E.R., Shah, M., Gruschkkus, S.K., et al. (2013). Cost and quality implications of opioid-based postsurgical pain control using administrative claims data from a large health system: opioid-related adverse events and their impact on clinical and economic outcomes. Pharmacotherapy, 33(4): 383-91.
Back to Citation397. Overdyk, F.J. (2009). Postoperative Respiratory Depression and Opioids. Initiatives in Safe Patient Care.
Back to Citation398. The Joint Commission. (2012.) Safe Use of Opioids in Hospitals. The Joint Commission Sentinel Event Alert, 49:1-5.
Back to Citation399. Lee, L.A., Caplan, R.A., Stephens, L.S., et al. (2015). Postoperative opioid-induced respiratory depression: a closed claims analysis. Anesthesiology, 122(3): 659-65.
Back to Citation400. Herzig, S.J., Rothberg, M.B., Cheung, M., et al. (2014). Opioid utilization and opioid-related adverse events in nonsurgical patients in US hospitals. Journal of Hospital Medicine, 9(2): 73-81.
Back to Citation401. Ibid.
Back to Citation402. Surgeon General's Advisory on Naloxone and Opioid Overdose. Available at: https://www.surgeongeneral.gov/priorities/opioid-overdose-prevention/naloxone-advisory.html.
403. Agency for Healthcare Research and Quality (AHRQ). (2017). Management of Suspected Opioid Overdose with Naloxone by Emergency Medical Services Personnel. Comparative Effectiveness Review No. 193. Available at: https://effectivehealthcare.ahrq.gov/topics/emt-naloxon/systematic-review.
404. Substance Abuse and Mental Health Services Administration (SAMHSA). (2018). Opioid Overdose Prevention Toolkit: Information for Prescribers. Available at: https://store.samhsa.gov/system/files/information-for-prescribers.pdf.
405. Harm Reduction Coalition. (2012). Guide To Developing and Managing Overdose Prevention and Take-Home Naloxone Projects. Available at: https://harmreduction.org/issues/overdose-prevention/tools-best-practices/manuals-best-practice/od-manual/.
Back to Citation406. Eckstrand, J.A., Habib, A.S., Williamson, A., et al. (2009). Computerized surveillance of opioid-related adverse drug events in perioperative care: A cross-sectional study. Patient Safety Surgery, 3:18.
407. Nwulu, U., Nirantharakumar, K., Odesanya, R., et al. (2013). Improvement in the detections of adverse drug events by the use of electronic health and prescription records: an evaluation of two trigger tools. European Journal of Clinical Pharmacology, 69(2): 255-59.
Back to Citation408. List of Measures Under Consideration for December 1, 2017. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation409. 2017-2018 Spreadsheet of Final Recommendations to HHS and CMS. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation410. National Quality Forum, Measure Applications Partnership, MAP 2018 Considerations for Implementing Measures in Federal Programs: Hospitals. Available at: http://www.qualityforum.org/Publications/2018/02/MAP_2018_Considerations_for_Implementing_Measures_Final_Report_-_Hospitals.aspx.
Back to Citation411. The Measure Authoring Tool (MAT) is a web-based tool used to develop the electronic measure specifications, which expresses complicated measure logic in several formats including a human-readable document. For additional information, we refer readers to: https://www.emeasuretool.cms.gov/.
Back to Citation412. National Quality Forum, Measure Applications Partnership, MAP 2018 Considerations for Implementing Measures in Federal Programs: Hospitals. Available at: http://www.qualityforum.org/Publications/2018/02/MAP_2018_Considerations_for_Implementing_Measures_Final_Report_-_Hospitals.aspx.
Back to Citation413. Measure Applications Partnership, December 2017 NQF MAP Hospital Workgroup Meeting Transcript. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation414. More information on CMS' Meaningful Measures Initiative is available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/MMF/General-info-Sub-Page.html.
Back to Citation415. “Predictive Value.” Farlex Partner Medical Dictionary. Available at: https://medical-dictionary.thefreedictionary.com/predictive+value.
Back to Citation416. Rozich, J., Haraden, C., & Resar, R. (2003). Adverse drug event trigger tool: A practical methodology for measuring medication related harm. Quality and Safety in Health Care, 12(3), 194-200.
Back to Citation417. Institute for Healthcare Improvement (IHI). Measures, Adverse Drug Events Per 1,000 Doses. Available at: http://www.ihi.org/resources/Pages/Measures/ADEsper1000Doses.aspx.
Back to Citation418. NQF. Transcript of March 19, 2019 NQF Scientific Methods Panel Transcript. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=89690.
Back to Citation419. NQF. Transcript of June 17, 2019 NQF Patient Safety Standing Committee Meeting. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90487.
420. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/Work Area/linkit.aspx?LinkIdentifier=id&ItemID=90662.
Back to Citation421. NQF. Transcript of June 17, 2019 NQF Patient Safety Standing Committee Meeting. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90487.
Back to Citation422. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/Work Area/linkit.aspx?LinkIdentifier=id&ItemID=90662.
Back to Citation423. A bilevel positive airway pressure (BiPAP or BPap) is a type of ventilator that helps with breathing.
Back to Citation424. Surgeon General's Advisory on Naloxone and Opioid Overdose. Available at: https://www.surgeongeneral.gov/priorities/opioid-overdose-prevention/naloxone-advisory.html.
425. Agency for Healthcare Research and Quality (AHRQ). (2017). Management of Suspected Opioid Overdose with Naloxone by Emergency Medical Services Personnel. Comparative Effectiveness Review No. 193. Available at: https://effectivehealthcare.ahrq.gov/topics/emt-naloxon/systematic-review.
426. Substance Abuse and Mental Health Services Administration (SAMHSA). (2018). Opioid Overdose Prevention Toolkit: Information for Prescribers. Available at: https://store.samhsa.gov/system/files/information-for-prescribers.pdf.
427. Harm Reduction Coalition. (2012). Guide To Developing and Managing Overdose Prevention and Take-Home Naloxone Projects. Available at: https://harmreduction.org/issues/overdose-prevention/tools-best-practices/manuals-best-practice/od-manual/.
Back to Citation428. Centers for Disease Control and Prevention (CDC) Preventing an Opioid Overdose. Available at: https://www.cdc.gov/drugoverdose/pdf/patients/Preventing-an-Opioid-Overdose-Tip-Card-a.pdf.
Back to Citation429. Louy C. “IV Naloxone Infusion: A Forgotten Gem,” presented at PAINWeek 2018, September 4-8, in Las Vegas, Nevada.
Back to Citation430. Gottlieb, S., Unprecedented new efforts to support development of over-the-counter naloxone to help reduce opioid overdose deaths (2019) Available at: https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-unprecedented-new-efforts-support-development-over
Back to Citation431. December 2018 HHS Press Release (Adm. Brett P. Giroir, MD). Available at: https://www.hhs.gov/about/news/2018/12/19/hhs-recommends-prescribing-or-co-prescribing-naloxone-to-patients-at-high-risk-for-an-opioid-overdose.html.
432. AMA Opioid Task Force, AMA Opioid Task Force Issues Updated Naloxone Guidance. Available at: https://www.aafp.org/news/health-of-the-public/20170828naloxoneresource.html.
Back to Citation433. Doheney, K., More Potential Uses for Low-Dose IV Naloxone (2018) Available at: https://www.practicalpainmanagement.com/meeting-summary/more-potential-uses-low-dose-iv-naloxone
Back to Citation434. Barrie, J. (2006) Diagnosis of drug overdose by rapid reversal with naloxone, Emergency Medicine Journal, 23(11): 874-875. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2464401/.
Back to Citation435. The Joint Commission. (2012). Safe Use of Opioids in Hospitals. The Joint Commission Sentinel Event Alert, 49:1-5.
Back to Citation436. As noted by the Guidance provided in the measure specifications, the numerator includes only encounters in which a patient was administered rather than ordered naloxone during their hospitalization. The measure specifications are on the CMS Measure Methodology website, available at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html.
Back to Citation437. Herzig, S.J., Rothberg, M.B., Cheung, M., et al. (2014). Opioid utilization and opioid-related adverse events in nonsurgical patients in US hospitals. Journal of Hospital Medicine, 9(2): 73-81.
Back to Citation438. Herzig SJ, Rothberg MB, Cheung M, Ngo LH, Marcantonio ER. Opioid utilization and opioid-related adverse events in nonsurgical patients in US hospitals. J Hosp Med. 2014;9(2):73-81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3976956/.
Back to Citation439. The measure specifications are on the CMS Measure Methodology website, available at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html.
Back to Citation440. Eckstrand, J.A., Habib, A.S., Williamson, A., et al. (2009). Computerized surveillance of opioid-related adverse drug events in perioperative care: a cross-sectional study. Patient Safety Surgery, 3:18.
441. Nwulu, U., Nirantharakumar, K., Odesanya, R., et al. (2013). Improvement in the detections of adverse drug events by the use of electronic health and prescription records: an evaluation of two trigger tools. European Journal of Clinical Pharmacology, 69(2): 255-59.
Back to Citation442. For more information about the denominator, we refer readers to the measure specifications on the CMS Measure Methodology website, available at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html.
Back to Citation443. See, for example, American Academy of Emergency Medicine, Emergency Department Opioid Prescribing Guidelines for the Treatment of Non-Cancer Related Pain (available at: https://www.deepdyve.com/lp/elsevier/american-academy-of-emergency-medicine-PlQtPNi8J4); Washington State Agency Medical Directors' Group, Interagency Guideline on Prescribing Opioids for Pain (available at: http://agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf); and American Society of Interventional Pain Physicians (ASIPP), Guidelines for Responsible Opioid Prescribing in Chronic Noncancer Pain (available at: https://www.asipp.org/opioidguidelines.htm).
Back to Citation444. Dowell, D., Haegerich, T. & Chou, R. (2016). CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. Morbidity and Mortality Weekly Report: Recommendations and Reports, 65. Available at: http://www.cdc.gov/media/dpk/2016/dpk-opioid-prescription-guidelines.html.
Back to Citation445. Centers for Medicare & Medicaid Services. (2018). 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report: Hospital-Wide Readmission. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation446. List of Measures Under Consideration for December 1, 2014. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation447. Measure Applications Partnership, 2015 Considerations for Implementing Measures in Federal Programs: Hospitals. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=78711.
Back to Citation448. National Quality Forum. (2017). All-Cause Admissions and Readmissions 2015-2017 Technical Report. Available at: https://www.qualityforum.org/Publications/2017/04/All-Cause_Admissions_and_Readmissions_2015-2017_Technical_Report.aspx.
Back to Citation449. In this final rule, we are updating this figure from 80 to 150, to reflect an update to the total number of hospitals that participated.
Back to Citation450. For more detail about core clinical data elements used in the Hybrid HWR measure, we refer readers to our discussion in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49698 through 49704) and to the QualityNet website at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1228763452133.
Back to Citation451. Electronic Clinical Quality Improvement (eCQI) Resource Center. Hybrid Hospital-Wide Readmission. Available at: https://ecqi.healthit.gov/ecqm/measures/cms529v0.
Back to Citation452. Hybrid 30-day Risk-standardized Acute Myocardial Infarction Mortality Measure with Electronic Health Record Extracted Risk Factors (Version 1.1); Hybrid Hospital-Wide Readmission Measure with Electronic Health Record Extracted Risk Factors (Version 1.1); 164 2013 Core Clinical Data Elements Technical Report (Version 1.1); all available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation453. https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp. Version 2019.1 of CCS for ICD-10-CM and CCS for ICD-10 for PCS.
Back to Citation454. Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation455. Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation456. Centers for Medicare & Medicaid Services. Hybrid Hospital-Wide Readmission Measure with Electronic Health Record Extracted Risk Factors (Version 1.1). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation457. Centers for Medicare & Medicaid Services. Measure Methodology. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation458. Ibid.
Back to Citation459. Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation460. Electronic Clinical Quality Improvement (eCQI) Resource Center. Hybrid Hospital-Wide Readmission. Available at: https://ecqi.healthit.gov/ecqm/measures/cms529v0.
Back to Citation461. Centers for Medicare & Medicaid Services. (2018). 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report: Hospital-Wide Readmission. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation462. Centers for Medicare & Medicaid Services. (2018). 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report: Hospital-Wide Readmission. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation463. Available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841.
Back to Citation464. Centers for Medicare & Medicaid Services. Hybrid Hospital-Wide Readmission Measure with Electronic Health Record Extracted Risk Factors (Version 1.1). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation465. Centers for Medicare & Medicaid Services. Hybrid Hospital-Wide Readmission Measure with Electronic Health Record Extracted Risk Factors (Version 1.1). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation466. Ibid.
Back to Citation467. Centers for Medicare & Medicaid Services. (2018). 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report: Hospital-Wide Readmission. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation468. CMS, Medicare Claims Processing Manual (100-04). Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/internet-Only-Manuals-IOMs.html.
Back to Citation469. Electronic Clinical Quality Improvement (eCQI) Resource Center. 2018 Measure Specifications. Available at: https://ecqi.healthit.gov/ecqm/measures/cms529v0. Note that the measure specifications may be further refined in the 2021 Annual Update.
Back to Citation470. FHIR, developed by Health Level Seven International (HL7), is designed to enable information exchange to support the provision of healthcare in a wide variety of settings. The specification builds on and adapts modern, widely used RESTful practices to enable the provision of integrated healthcare across a wide range of teams and organizations. Additional information is available at: https://www.hl7.org/fhir/overview.html.
Back to Citation471. We refer readers to the 2015 Hybrid HWR Measure with Electronic Health Record Extracted Risk Factors report, available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776337297.
472. 80 FR 49699
Back to Citation473. Centers for Medicare and Medicaid Services (CMS). Hybrid Hospital-Wide Readmission Methodology Report (2013). Available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776337297.
Back to Citation474. 80 FR 49699.
Back to Citation475. Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation476. For additional details regarding the measure specifications, we refer readers to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report. (Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.)
Back to Citation477. MAP Rural Health Workgroup, A Core Set of Rural-Relevant Measures and Measuring and Improving Access to Care: 2018 Recommendations from the MAP Rural Health Workgroup, August 31, 2018, available at: http://www.qualityforum.org/Publications/2018/08/MAP_Rural_Health_Final_Report_-_2018.aspx.
Back to Citation478. Measure Applications Partnership, 2015 Considerations for Implementing Measures in Federal Programs: Hospitals. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=78711.
Back to Citation479. National Quality Forum. (2017). All-Cause Admissions and Readmissions 2015-2017 Technical Report. Available at: https://www.qualityforum.org/Publications/2017/04/All-Cause_Admissions_and_Readmissions_2015-2017_Technical_Report.aspx.
Back to Citation480. 77 FR 53522 through 53528.
Back to Citation481. Value Set Authority Center. Available at: https://vsac.nlm.nih.gov/.
Back to Citation482. We refer readers to the Hospital 30-Day AMI Readmission Measure Methodology Report, available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841.
Back to Citation483. http://www.qualityforum.org/QPS/2879e.
484. We refer readers to the Hospital 30-Day AMI Readmission Measure Methodology Report, available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841.
Back to Citation485. 80 FR 49702 through 49703.
Back to Citation486. For additional details regarding the measure specifications, we refer readers to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report. (Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.)
Back to Citation487. For additional details regarding the measure specifications, we refer readers to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report. (Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.)
Back to Citation488. For additional details regarding the measure specifications, we refer readers to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report. (Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.)
Back to Citation489. For additional details regarding the measure specifications, we refer readers to the 2018 All-Cause Hospital-Wide Measure Updates and Specifications Report. (Centers for Medicare & Medicaid Services. (2018). 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.)
Back to Citation490. For additional details about the updates to the 2015 Edition, we refer readers to ONC's Common Clinical Data Set resource, available at: https://www.healthit.gov/sites/default/files/commonclinicaldataset_ml_11-4-15.pdf.
Back to Citation491. For more detail about core clinical data elements used in the Hybrid HWR measure, we refer readers to our discussion in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49698 through 49704) and to the QualityNet website at: https://www.qualitynet.org/dcs/ContentServer?cid=1228776337082&pagename=QnetPublic%2FPage%2FQnetTier3&%20c=Page.
Back to Citation492. 84 FR 19480 through 19485; Centers for Medicare & Medicaid Services. (2018).
493. 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation494. 84 FR 19480 through 19485; Centers for Medicare & Medicaid Services. (2018).
495. 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation496. National Quality Forum. Hybrid Hospital-Wide Readmission (HWR) Measure with Claims and Electronic Health Record Data (2879e), eHWR Tech Report 01-29-16 v1.0. Available at: http://www.qualityforum.org/QPS/QPSTool.aspx?m=2879&e=1#qpsPageState=%7B%22TabType%22%3A1,%22TabContentType%22%3A2,%22ItemsToCompare%22%3A%5B%5D,%22StandardID%22%3A2879,%22EntityTypeID%22%3A1%7D.
Back to Citation497. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776337297.
Back to Citation498. https://www.qualityforum.org/QPS/2879e.
Back to Citation499. 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation500. https://www.qualityforum.org/home.aspx.
Back to Citation501. National Quality Forum (July 2017). Social Risk Trial Final Report: Evaluation of the NQF Trial Period for Risk Adjustment for Social Risk Factors, available at: https://www.qualityforum.org/Publications/2017/07/Social_Risk_Trial_Final_Report.aspx.
Back to Citation502. Assistant Secretary for Planning and Evaluation (ASPE). 2016 Report to Congress: Social Risk Factors and Performance Under Medicare's Value-Based Purchasing Programs. Available at: https://aspe.hhs.gov/pdf-report/report-congress-social-risk-factors-and-performance-under-medicares-value-based-purchasing-programs.
Back to Citation503. 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation504. 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation505. 2018 All Cause Hospital Wide Measure Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation506. We refer readers to the following sources for more detail on these issues: 1. Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Intern Med 2009;150(3):178-87; 2. Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: The Care Transitions Intervention. J Am Geriatr Soc 2004;52(11):1817-25; 3. Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K. Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: A randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc 2009;57(3):395-402; 4. Garasen H, Windspoll R, Johnsen R. Intermediate care at a community hospital as an alternative to prolonged general hospital care for elderly patients: A randomised controlled trial. BMC Public Health 2007;7:68; 5. Koehler BE, Richter KM, Youngblood L, Cohen BA, Prengler ID, Cheng D, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med 2009;4(4):211-218; 6. Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: A systematic metareview. BMC Health Serv Res 2007;7:47; 7. Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med 1994;120(12):999-1006; 8. Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. Jama 1999;281(7):613-20; 9. van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med 2002;17(3):186-92; 10. Weiss M, Yakusheva O, Bobay K. Nurse and patient perceptions of discharge readiness in relation to postdischarge utilization. Med Care 2010;48(5):482-6; and 11. Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. Jan 2 2002;39(1):8389.
Back to Citation507. https://www.ruralcenter.org/tasc/mbqip.
Back to Citation508. Center for Medicare and Medicaid Services (CMS). 2019 Condition-Specific Readmission Measures Updates and Specifications Report. Available at: https://www.qualitynet.org/dcs/BlobServer?blobkey=id&blobnocache=true&blobwhere=1228890945658&blobheader=multipart%2Foctet-stream&blobheadername1=Content-Disposition&blobheadervalue1=attachment%3Bfilename%3D2019CondSpecific_Readmission_AUS_Report.pdf&blobcol=urldata&blobtable=MungoBlobs.
Back to Citation509. National Quality Forum (NQF). Hospital-Wide All-Cause Unplanned Readmission Measure (HWR) Specifications, 2018. Available at: http://www.qualityforum.org/QPS/QpsMeasureExport.aspx?exportType=pdf&exportFrom=s&measureIDs=1789.
510. http://www.qualityforum.org/QPS/2879e.
Back to Citation511. Office of Disease Prevention and Health Promotion. (2014). National Action Plan for Adverse Drug Event Prevention. Available at: https://health.gov/hcq/pdfs/ADE-Action-Plan-508c.pdf.
Back to Citation512. Diabetes Control and Complications Trial Research Group. (1993). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine, 329(14): 977-86.
Back to Citation513. Krinsley, J.S., Schultz, M.J., Spronk, P.E., van Braam Houckgeest, F., van der Sluijs, J.P., Melot, C. & Preiser, J.C. (2011). Mild hypoglycemia is strongly associated with increased intensive care unit length of stay. Ann Intensive Care, 1, 49.
Back to Citation514. Turchin, A., Matheny, M.E., Shubina, M., Scanlon, J.V., Greenwood, B., & Pendergrass, M.L. (2009). Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care, 32(7): 1153-57.
Back to Citation515. Curkendall, S.M., Natoli, J.L., Alexander, C.M., Nathanson, B.H., Haidar, T., & Dubois, R.W. (2009). Economic and clinical impact of inpatient diabetic hypoglycemia. Endocrine Practice, 15(4): 302-312.
Back to Citation516. Nirantharakumar, K., Marshall, T., Kennedy, A., Narendran, P., Hemming, K., & Coleman, J.J. (2012). Hypoglycemia is associated with increased length of stay and mortality in people with diabetes who are hospitalized. Diabetic Medicine, 29(12): e445-e448.
517. Wexler, D.J., Meigs, J.B., Cagliero, E., Nathan, D.M., & Grant, R.W. (2007). Prevalence of hyper- and hypoglycemia among inpatients with diabetes: A national survey of 44 U.S. hospitals. Diabetes Care, 30(2): 367-369.
518. Cook, C.B., Kongable, G.L., Potter, D.J., Abad, V.J., Leija, D.E., & Anderson, M. (2009). Inpatient glucose control: A glycemic survey of 126 U.S. hospitals. Journal of Hospital Medicine, 4(9): E7-E14.
Back to Citation519. Classen, D.C., Jaser, L., Budnitz, D.S. (2010). Adverse Drug Events among Hospitalized Medicare Patients: Epidemiology and national estimates from a new approach to surveillance. Joint Commission Journal on Quality and Patient Safety, 36(1): 12-21.
Back to Citation520. Office of Disease Prevention and Health Promotion. (2014). National Action Plan for Adverse Drug Event Prevention. Available at: https://health.gov/hcq/pdfs/ADE-Action-Plan-508c.pdf.
Back to Citation521. More information on CMS' Meaningful Measures Initiative can be found at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/MMF/General-info-Sub-Page.html.
Back to Citation522. For more information on the Glycemic Control—Severe Hypoglycemia measure, we refer readers to the measure specifications, available at: http://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=2363&print=1&entityTypeID=1.
Back to Citation523. List of Measures Under Consideration for December 1, 2018. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation524. 2018-2019 Spreadsheet of Final Recommendations to HHS and CMS. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
525. National Quality Forum, Measure Applications Partnership, MAP 2019 Considerations for Implementing Measures in Federal Programs: Hospitals. Available at: http://www.qualityforum.org/Publications/2019/02/MAP_2019_Considerations_for_Implementing_Measures_Final_Report_-_Hospitals.aspx.
Back to Citation526. Measure Applications Partnership, December 2018 NQF MAP Hospital Workgroup Meeting Transcript. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation527. March 2019 Scientific Methods Panel meeting transcript. Available at: https://www.qualityforum.org/Measuring_Performance/Scientific_Methods_Panel/Meetings/2019_Scientific_Methods_Panel_Meetings.aspx.
528. Spring 2019 Patient Safety Standing Committee meeting transcript. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=86057.
Back to Citation529. Cook, C.B., Kongable, G.L., Potter, D.J., Abad, V.J., Leija, D.E., & Anderson, M. (2009). Inpatient glucose control: A glycemic survey of 126 U.S. hospitals. Journal of Hospital Medicine, 4(9), E7-E14.
530. Moghissi, E.S., Korytkowski, M.T., DiNardo, M., et al. (2009). American Association of Clinical Endocrinologists and American Diabetes Association Consensus Statement on Inpatient Glycemic Control. Diabetes Care, 32(6):1119-1131.
531. Office of the Inspector General (OIG). (2010). Adverse Events in Hospitals: National Incidence Among Medicare Beneficiaries.
532. Wexler, D.J., Meigs, J.B., Cagliero, E., Nathan, D.M., & Grant, R.W. (2007). Prevalence of hyper- and hypoglycemia among inpatients with diabetes: A national survey of 44 U.S. hospitals. Diabetes Care, 30(2): 367-69.
Back to Citation533. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90662.
Back to Citation534. American Diabetes Association. 14. Diabetes care in the hospital: Standards of Medical Care in Diabetesd2018. Diabetes Care 2018;41(Suppl. 1):S144-S151.
Back to Citation535. National Quality Forum. Glycemic Control—Hypoglycemia. Available at: http://www.qualityforum.org/Qps/MeasureDetails.aspx?standardID=2363&print=0&entityTypeID=1.
Back to Citation536. Krinsley, J.S., Grover A. (2007). Severe hypoglycemia in critically ill patients: Risk factors and outcomes. Critical Care Medicine, 35(10):2262-7.
537. Cook, C.B., Kongable, G.L., Potter, D.J., Abad, V.J., Leija, D.E., & Anserson, M, (2009). Inpatient glucose control: A glycemic survey of 126 U.S. hospitals. Journal of Hospital Medicine, 4(9):E7-E14.
538. Egi, M., et al. (2010). Hypoglycemia and outcome in critically ill patients. Mayo Clinic Proc, 85(3):217-224.
Back to Citation539. Landis J, Koch G. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-174. PubMedLink: https://www.ncbi.nlm.nih.gov/pubmed/843571.
Back to Citation540. AHRQ Quality and Safety Review System. Content last reviewed September 2018. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/professionals/quality-patient-safety/qsrs/index.html.
541. New System Aims To Improve Patient Safety Monitoring. Content last reviewed October 2016. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/news/blog/ahrqviews/new-system-aims-to-improve-patient-safety-monitoring.html.
542. Classen DC, Jaser L, Budnitz DS. Adverse drug events among hospitalized Medicare patients: epidemiology and national estimates from a new approach to surveillance. Jt Comm J Qual Patient Saf. 2010;36(1):12-21.
Back to Citation543. Dendy JA, Chockalingam, V, Tirumalasetty NN, et al. Identifying risk factors for severe hypoglycemia in hospitalized patients with diabetes. Endocr Pract 2014;20:1051-1056.
544. Ulmer BJ, Kara A, Mariash CN. Temporal occurrences and recurrence patterns of hypoglycemia during hospitalization. Endocr Pract 2015;21:501-507.
Back to Citation545. Maynard G, Kulasa K, Ramos P, et al. Impact of a hypoglycemia reduction bundle and a systems approach to inpatient glycemic management. Endocr Pract 2015;21:355-367.
546. Milligan PE, Bocox MC, Pratt E, Hoehner CM, Krettek JE, Dunagan WC. Multifaceted approach to reducing occurrence of severe hypoglycemia in a large healthcare system. Am J Health Syst Pharm 2015;72:1631-1641.
547. American Diabetes Association. Diabetes Care in the Hospital: Standards of Medical Care in Diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S144.
Back to Citation548. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90662.
Back to Citation549. National Quality Forum. Measure Evaluation Criteria and Guidance for Evaluating Measures for Endorsement. 2016. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=83123.
Back to Citation550. Ibid.
Back to Citation551. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90662.
552. National Quality Forum (NQF) Scientific Methods Panel. Subgroup #4—Evaluation Meeting Transcript. March 19, 2019. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=89690.
Back to Citation553. American Diabetes Association. 14. Diabetes care in the hospital: Standards of Medical Care in Diabetesd2018. Diabetes Care 2018;41(Suppl. 1):S144-S151.
Back to Citation554. eCQI Resource Center. Hospital Harm—Severe Hypoglycemia. Available at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
Back to Citation555. Ibid.
Back to Citation556. National Quality Forum. Glycemic Control—Hypoglycemia. Available at: http://www.qualityforum.org/Qps/MeasureDetails.aspx?standardID=2363&print=0&entityTypeID=1.
Back to Citation557. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90662.
Back to Citation558. Agency for Healthcare Research and Quality. National Scorecard on Rates of Hospital-Acquired Conditions 2010 to 2015: Interim Data From National Efforts to Make Health Care Safer. (2016). Available at: https://www.ahrq.gov/professionals/quality-patient-safety/pfp/2015-interim.html?utm_source=AHRQ&utm_medium=PSLS&utm_term=&utm_content=14&utm_campaign=AHRQ_NSOHAC_2016.
Back to Citation559. Brem, H., Maggi, J., Nierman, D., Rolnitzky, L., Bell, D., Rennert, R., Golinko, M., Yan, A., Lyder, C., Vladeck, B. (2010). High cost of stage IV. The American Journal of Surgery, 200: 473-477.
Back to Citation560. Gunningberg, L., Donaldson, N., Aydin, C. & Idvall, E. (2012). Exploring variation in pressure ulcer prevalence in Sweden and the USA: benchmarking in action. Journal of Evaluation in Clinical Practice, 18: 904-910.
Back to Citation561. Agency for Healthcare Research and Quality. National Scorecard on Rates of Hospital-Acquired Conditions 2010 to 2015: Interim Data From National Efforts to Make Health Care Safer. (2016). Available at: https://www.ahrq.gov/professionals/quality-patient-safety/pfp/2015-interim.html?utm_source=AHRQ&utm_medium=PSLS&utm_term=&utm_content=14&utm_campaign=AHRQ_NSOHAC_2016.
562. Bauer, K., Rock, K., Nazzai, M.J., & Qu, W. (2016). Pressure Ulcers in the United States Inpatient Population from 2008 to 2012: Results of a Retrospective Nationwide Study. Ostomy Wound Management, 62(11): 30-38.
Back to Citation563. Lyder, C.H., Wang, Y., Metersky, M., Curry, M., Kliman, R., Verzier, N.R., Hunt D.R. (2012). Hospital-acquired pressure ulcers: results from the national Medicare Patient Safety Monitoring System study. Journal of American Geriatrics Society, 60(9): 1603-8.
Back to Citation564. Gunningberg, L., Donaldson, N., Aydin, C. & Idvall, E. (2012). Exploring variation in pressure ulcer prevalence in Sweden and the USA: benchmarking in action. Journal of Evaluation in Clinical Practice, 18: 904-910.
Back to Citation565. Bauer, K., Rock, K., Nazzai, M.J., & Qu, W. (2016). Pressure Ulcers in the United States Inpatient Population from 2008 to 2012: Results of a Retrospective Nationwide Study. Ostomy Wound Management, 62(11): 30-38.
Back to Citation566. National Quality Forum, List of SREs. Available at: http://www.qualityforum.org/Topics/SREs/List_of_SREs.aspx.
Back to Citation567. Centers for Medicare & Medicaid Services. Hospital-Acquired Conditions. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/Hospital-Acquired_Conditions.html.
Back to Citation568. National Quality Forum. (2004). National Voluntary Consensus Standards for Nursing-Sensitive Care: An Initial Performance Measure Set 2005. Available at: http://www.qualityforum.org/Publications/2004/10/National_Voluntary_Consensus_Standards_for_Nursing-Sensitive_Care__An_Initial_Performance_Measure_Set.aspx.
Back to Citation569. Agency for Healthcare Research and Quality. (2012). Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care. Available at: https://www.ahrq.gov/sites/default/files/publications/files/putoolkit.pdf.
Back to Citation570. Gunningberg, L., Donaldson, N., Aydin, C. & Idvall, E. (2012). Exploring variation in pressure ulcer prevalence in Sweden and the USA: benchmarking in action. Journal of Evaluation in Clinical Practice, 18: 904-910.
Back to Citation571. Agency for Healthcare Research and Quality. (2016). National Scorecard on Rates of Hospital-Acquired Conditions 2010-2015: Interim Data From Nation Efforts to Male Health Care Safer. Available at: https://www.ahrq.gov/professionals/quality-patient-safety/pfp/2015-interim.html.
Back to Citation572. Gunningberg, L., Donaldson, N., Aydin, C. & Idvall, E. (2012). Exploring variation in pressure ulcer prevalence in Sweden and the USA: benchmarking in action. Journal of Evaluation in Clinical Practice, 18: 904-910.
Back to Citation573. List of Measures Under Consideration for December 1, 2018. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation574. 2018-2019 Spreadsheet of Final Recommendations to HHS and CMS. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation575. Gunningberg, L., Donaldson, N., Aydin, C., Idvall, E. (2011). Exploring variation in pressure ulcer prevalence in Sweden and the USA: Benchmarking in action. 18. 10.1111/j.1365-2753.2011.01702.x. Journal of evaluation in clinical practice, 904-910.
576. Berlowitz, D., VanDeusen Lukas, C., Parker, V., Niederhauser, A., Silver, J., Logan, C., Ayello, E., Zulkowski, K. (2012). Preventing Pressure Ulcers in Hospitals—A Toolkit for Improving Quality of Care.
Back to Citation577. Measure Applications Partnership, December 2018 NQF MAP Hospital Workgroup Meeting Transcript. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation578. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90662.
Back to Citation579. National Pressure Ulcer Advisory Panel. (2016). NPAUAP Pressure Injury Stages. Available at: http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-injury-stages/.
580. Agency for Healthcare Research and Quality. (2012). Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care. Available at: https://www.ahrq.gov/sites/default/files/publications/files/putoolkit.pdf.
581. Catania, K. et al. (2007). PUPPI: The Pressure Ulcer Prevention Protocol Interventions. American Journal of Nursing, 107(4): 44-52.
582. National Quality Forum. (2004). National Voluntary Consensus Standards for Nursing-Sensitive Care: An Initial Performance Measure Set 2005. Available at: http://www.qualityforum.org/Publications/2004/10/National_Voluntary_Consensus_Standards_for_Nursing-Sensitive_Care__An_Initial_Performance_Measure_Set.aspx.
Back to Citation583. Gunningberg, L., Donaldson, N., Aydin, C., Idvall, E. (2011). Exploring variation in pressure ulcer prevalence in Sweden and the USA: Benchmarking in action. 18. 10.1111/j.1365-2753.2011.01702.x. Journal of evaluation in clinical practice, 904-910.
584. Berlowitz, D., VanDeusen Lukas, C., Parker, V., Niederhauser, A., Silver, J., Logan, C., Ayello, E., Zulkowski, K. (2012). Preventing Pressure Ulcers in Hospitals—A Toolkit for Improving Quality of Care.
Back to Citation585. Hospital Harm—Pressure Injury eCQM Measure Specifications. Available at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html.
Back to Citation586. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Emily Haesler (Ed.). Cambridge Media: Osborne Park, Western Australia; 2014. Available at: http://www.internationalguideline.com/static/pdfs/NPUAP-EPUAP-PPPIA-CPG-2017.pdf.
Back to Citation587. National Quality Forum (NQF) Patient Safety Standing Committee. Meeting Summary—Measure Evaluation In-person Meeting—Spring 2019 Cycle. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=90662.
Back to Citation588. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Emily Haesler (Ed.). Cambridge Media: Osborne Park, Western Australia; 2014 Available at: http://www.internationalguideline.com/static/pdfs/NPUAP-EPUAP-PPPIA-CPG-2017.pdf.
589. The Joint Commission. (2016). Preventing Pressure Injuries Quick Safety. Available at: https://www.jointcommission.org/issues/article.aspx?Article=n+OspqDzBBeZ/tRoyTzpsyZ4GrBDhJpdtlQvqSl5hsQ=.
Back to Citation590. eCQI Resource Center. Pre-rulemaking Eligible Hospital/Critical Access Hospital eCQMs. Hospital Harm—Pressure Injury. Available at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms .
Back to Citation591. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Emily Haesler (Ed.). Cambridge Media: Osborne Park, Western Australia; 2014 Available at: http://www.internationalguideline.com/static/pdfs/NPUAP-EPUAP-PPPIA-CPG-2017.pdf.
Back to Citation592. National Quality Forum, Quality Measure PC-02 (Cesarean Birth). Available at: https://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=291&print=1&entityTypeID=1.
Back to Citation593. Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014 Mar;210(3):179-93. doi: 10.1016/j.ajog.2014.01.026.
594. Schifrin BS, Cohen WR. The effect of malpractice claims on the use of caesarean section. Best Pract Res Clin Obstet Gynaecol. 2013 Apr;27(2):269-83. doi: 10.1016/j.bpobgyn.2012.10.004. Epub 2012 Dec 1. Review.
595. Chen CS, Liu TC, Chen B, Lin CL. The failure of financial incentive? The seemingly inexorable rise of cesarean section. Soc Sci Med. 2014 Jan;101:47-51. doi: 10.1016/j.socscimed.2013.11.010. Epub 2013 Nov 15.
Back to Citation596. Osterman, M.J.K., Martin, J.A. (2014). Trends in Low-risk Cesarean Delivery in the United States, 1990-2013. National Vital Statistics Reports, 63(6): 1-16.
Back to Citation597. Martin, J.A., Hamilton, B.E., Osterman, M.J.K., Driscoll, A.K., Drake, P. (2018). Births: Final Data for 2016. National Vital Statistics Reports, 67(1): 1-55.
Back to Citation598. Kozhimannil, K.B., Law, M.R. & Virnig, B.A. (2013). Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Affairs, 32(3): 527-35.
Back to Citation599. National Collaborating Centre for Women's and Children's Health. (2011). Caesarean Section: NICE Clinical Guideline (commissioned by the United Kingdom National Institute for Health and Clinical Excellence).
600. American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology, 210(3): 179-93.
601. Keag, O.E., Norman, J.E. & Stock, S.J. (2018). Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. Plos Med, 15(1): e1002494.
Back to Citation602. American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology, 210(3): 179-93.
603. National Collaborating Centre for Women's and Children's Health. (2011). Caesarean Section: NICE Clinical Guideline (commissioned by the United Kingdom National Institute for Health and Clinical Excellence).
Back to Citation604. American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology, 210(3): 179-93.
Back to Citation605. Keag, O.E., Norman, J.E. & Stock, S.J. (2018). Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. Plos Med, 15(1): e1002494.
Back to Citation606. Keag, O.E., Norman, J.E. & Stock, S.J. (2018). Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. Plos Med, 15(1): e1002494.
Back to Citation607. American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology, 210(3): 179-93.
Back to Citation608. Keag, O.E., Norman, J.E. & Stock, S.J. (2018). Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. Plos Med, 15(1): e1002494.
Back to Citation609. American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology, 210(3): 179-93.
Back to Citation610. Aron-Dine, A., Einav, L. & Finkelstein, A. (2013). The RAND Health Insurance Experiment, Three Decades Later. The Journal of Economic Perspectives, 27(1): 197-222.
Back to Citation611. Kozhimannil, K.B., Law, M.R. & Virnig, B.A. (2013). Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Affairs, 32(3): 527-35.
Back to Citation612. National Quality Forum, Quality Measure PC-02 (Cesarean Birth). Available at: https://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=291&print=1&entityTypeID=1.
Back to Citation613. American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology, 210(3): 179-93.
614. National Quality Forum, Perinatal and Reproductive Health 2015-2016 Final Report. Available at: http://www.qualityforum.org/Publications/2016/12/Perinatal_and_Reproductive_Health_2015-2016_Final_Report.aspx.
Back to Citation615. American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. (2014). Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology, 210(3): 179-93.
Back to Citation616. Mylonas, I. & Friese, K. (2015). Indications for and Risks of Elective Cesarean Section. Deutsches Arzteblatt International, 112(29-30): 489-95.
Back to Citation617. Centers for Medicare & Medicaid Services. (2015). Cesarean Birth (PC-02) Measure Public Comment Summary. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/Downloads/PC-02-Public-Comment-Summary-Memo.pdf. The PC-02 eCQM cannot capture all possible medical indications. Thus, PC-02 does not equate to elective C-section for non-medical reasons.
Back to Citation618. National Quality Forum, Quality Measure PC-02 (Cesarean Birth). Available at: https://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=291&print=1&entityTypeID=1.
Back to Citation619. National Quality Forum (NQF), Perinatal and Reproductive Health Project. NQF #0471 PC-02 Cesarean Section: Measure Submission and Evaluation Worksheet 5.0. October 24, 2008. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=69252.
Back to Citation620. Curtin, S.C., Gregory, K.D., Korst, L.M., & Uddin, S.F. (2015). Maternal Morbidity for Vaginal and Cesarean Deliveries, According to Previous Cesarean History: New Data From the Birth Certificate, 2013. National Vital Statistics Reports, 64(4): 1-13.
Back to Citation621. Centers for Medicare & Medicaid Services. (2015). Cesarean Birth (PC-02) Measure Public Comment Summary. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/Downloads/PC-02-Public-Comment-Summary-Memo.pdf.
Back to Citation622. National Quality Forum, Measure Applications Partnership. (2018). A Core Set of Rural-Relevant Measures and Measuring and Improving Access to Care: 2018 Recommendations from the MAP Rural Health Workgroup. Available at: http://www.qualityforum.org/Publications/2018/08/MAP_Rural_Health_Final_Report_-_2018.aspx.
Back to Citation623. List of Measures Under Consideration for December 1, 2018. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation624. Measure Applications Partnership, December 2018 NQF MAP Hospital Workgroup Meeting Transcript. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation625. National Quality Forum, Measure Applications Partnership, MAP 2019 Considerations for Implementing Measures in Federal Programs: Hospitals. Available at: http://www.qualityforum.org/Publications/2019/02/MAP_2019_Considerations_for_Implementing_Measures_Final_Report_-_Hospitals.aspx.
Back to Citation626. See, for example, The Joint Commission. Specifications Manual for Joint Commission National Quality Measures, Measure Information Form PC-02. Available at: https://manual.jointcommission.org/releases/TJC2018A1/MIF0167.html.
Back to Citation627. List of Measures Under Consideration for December 1, 2018. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation628. Ibid.
Back to Citation629. The Joint Commission, Specifications Manual for Joint Commission National Quality Measures, Measure Information Form PC-02. Available at: https://manual.jointcommission.org/releases/TJC2018A1/MIF0167.html.
Back to Citation630. National Quality Forum, (2016) Perinatal and Reproductive Health 2015-2016 Final Report. Available at: http://www.qualityforum.org/Publications/2016/12/Perinatal_and_Reproductive_Health_2015-2016_Final_Report.aspx.
Back to Citation631. National Quality Forum, Perinatal and Reproductive Health 2015-2016 Final Report. Available at: http://www.qualityforum.org/Publications/2016/12/Perinatal_and_Reproductive_Health_2015-2016_Final_Report.aspx.
Back to Citation632. National Quality Forum, (2016) Perinatal and Reproductive Health 2015-2016 Final Report. Available at: http://www.qualityforum.org/Publications/2016/12/Perinatal_and_Reproductive_Health_2015-2016_Final_Report.aspx.
Back to Citation633. https://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=291&print=1&entityTypeID=1.
634. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=69252.
Back to Citation635. National Quality Forum, Quality Measure PC-02 (Cesarean Birth). Available at: https://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=291&print=1&entityTypeID=1.
Back to Citation636. Measure Applications Partnership, December 2018 NQF MAP Hospital Workgroup Meeting Transcript. Available at: http://www.qualityforum.org/ProjectMaterials.aspx?projectID=75369.
Back to Citation637. National Quality Forum, Measure Applications Partnership, MAP 2019 Considerations for Implementing Measures in Federal Programs: Hospitals. Available at: http://www.qualityforum.org/Publications/2019/02/MAP_2019_Considerations_for_Implementing_Measures_Final_Report_-_Hospitals.aspx.
Back to Citation638. The Within-Hospital Disparity Method (also referred to as the Dual Eligible Disparity Method for Within-Hospital Comparison) highlights differences in outcomes for dual eligible versus non-dual eligible patients within an individual hospital, while the Dual Eligible Outcome Method (also referred to as the Dual Eligible Outcome Method for Across Hospital Comparison) allows for a comparison of performance in care for dual eligible patients across hospitals.
Back to Citation639. Assessing Hospital Disparities for Dual Eligible Patients: Thirty-Day All-Cause Unplanned Readmission Following Pneumonia Hospitalization, Measure Methodology Report for 2018 Confidential Reporting. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=%201228776709103&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page.
Back to Citation640. These materials, as well as other confidential reporting resources such as Frequently Asked Questions (FAQs), Disparity Methods HSR User Guide, and National Provider Call materials, are available on the confidential reporting pages of the QualityNet website, available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776708906.
641. Available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776708906.
Back to Citation642. National Quality Forum. (2017). A Roadmap for Promoting Health Equity and Eliminating Disparities: The Four I's for Health Equity. Available at: http://www.qualityforum.org/Publications/2017/09/A_Roadmap_for_Promoting_Health_Equity_and_Eliminating_Disparities__The_Four_I_s_for_Health_Equity.aspx.
Back to Citation643. Assessing Hospital Disparities for Dual Eligible Patients: Thirty-Day All-Cause Unplanned Readmission Following Pneumonia Hospitalization, Measure Methodology Report for 2018 Confidential Reporting. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=%201228776709103&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page.
Back to Citation644. As required by the 21st Century Cures Act, the Hospital Readmissions Reduction Program implemented a transitional adjustment methodology for dual eligible patients beginning in FY 2019. For additional details on the stratified methodology used in the Hospital Readmissions Reduction Program, we refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38226 through 38237) and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41436 through 41438).
Back to Citation645. QualityNet. Confidential Reporting Overview: Disparity Methods. Available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228776708906.
Back to Citation646. For additional details on the stratified methodology used in the Hospital Readmissions Reduction Program, we refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38226 through 38237) and the FY 2019 IPPS/LTCH PPS final rule (83 FR 41436 through 41438).
Back to Citation647. https://www.qualitynet.org/dcs/ContentServer?cid=%201219069855841&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page.
Back to Citation648. Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation (ASPE), “Accounting for Social Risk Factors in Medicare Payment.” Jan. 2017. Available at: http://nationalacademies.org/hmd/Reports/2017/accounting-for-social-risk-factors-in-medicare-payment-5.aspx.
649. Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation (ASPE), “Report to Congress: Social Risk Factors and Performance Under Medicare's Value-Based Purchasing Programs.” December 2016. Available at: https://aspe.hhs.gov/pdf-report/report-congress-social-risk-factors-and-performance-under-medicares-value-based-purchasing-programs.
650. National Quality Forum (NQF). “Evaluation of the NQF Trial Period for Risk Adjustment for Social Risk Factors.” Available at: https://www.qualityforum.org/Publications/2017/07/Social_Risk_Trial_Final_Report.aspx.
Back to Citation651. National Quality Forum. (2017). A Roadmap for Promoting Health Equity and Eliminating Disparities: The Four I's for Health Equity.
Back to Citation652. FY 2018 IPPS/LTCH PPS final rule (82 FR 38387).
Back to Citation653. CMS, How CMS Engages You. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/How-CMS-Engages-You.html.
Back to Citation654. https://ecqi.healthit.gov/.
Back to Citation655. https://ecqi.healthit.gov/collaborative-measure-development.
Back to Citation656. CMS, Public Comment Page. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/PC-Currently-Accepting-Comments.html.
Back to Citation657. Available at: https://oncprojectracking.healthit.gov/support/secure/BrowseProjects.jspa?selectedCategory=all&selectedProjectType=all.
Back to Citation658. Value Set Authority Center. Available at: https://vsac.nlm.nih.gov/welcome.
Back to Citation659. The Office of the National Coordinator for Health Information Technology. (2018). Strategy on Reducing Regulatory and Administrative Burden Relating to the Use of Health IT and EHRs (Draft for Public Comment). Available at: https://www.healthit.gov/sites/default/files/page/2018-11/Draft%20Strategy%20on%20Reducing%20Regulatory%20and%20Administrative%20Burden%20Relating.pdf.
Back to Citation660. Available at: https://ecqi.healthit.gov/ecqms.
Back to Citation661. FY 2016 IPPS/LTCH PPS final rule (80 FR 49693 through 49698).
Back to Citation662. We refer readers to the eCQI Resource Center's Pre-Rulemaking Eligible Hospital/Critical Access Hospital eCQMs website, available at: https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
Back to Citation663. https://ecqi.healthit.gov/content/about-ecqi.
Back to Citation664. Available at: https://ecqi.healthit.gov/.
Back to Citation665. Available at: https://oncprojectracking.healthit.gov/support/secure/BrowseProjects.jspa?selectedCategory=all&selectedProjectType=all.
Back to Citation666. 45 CFR 170.102.
Back to Citation667. ONC, 2015 Edition Final Rule: Overview of the 2015 Edition Health IT Certification Criteria & ONC Health IT Certification Program Provisions. Available at: https://www.healthit.gov/sites/default/files/onc_2015_edition_final_rule_presentation_10-28-15.pdf.
Back to Citation668. 82 FR 38391 through 38393; 83 FR 41672.
Back to Citation669. We have updated the number of hospitals that submitted Hybrid HWR measure data for the 2018 Voluntary Reporting Period since the publication of the proposed rule (from approximately 80 to 150 hospitals).
Back to Citation670. The Electronic Clinical Quality Improvement (eCQI) Resource Center. Eligible Hospitals/Critical Access Hospital eCQMs. Available at: https://ecqi.healthit.gov/eligible-hospital/critical-access-hospital-ecqms.
Back to Citation671. We note that in the FY 2020 IPPS/LTCH PPS proposed rule, we inadvertently omitted reference to the FY 2019 IPPS/LTCH PPS final rule. We have added the citation to the language above.
Back to Citation672. American Cancer Society. “Cancer Pain.” Available at: https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/pain.html.
Back to Citation673. Mayo Clinic. “Cancer Pain: Relief is Possible.” Available at: https://www.mayoclinic.org/diseases-conditions/cancer/in-depth/cancer-pain/art-20045118.
Back to Citation674. HCAHPS Quality Assurance Guidelines (v.13.0), available at: http://www.hcahpsonline.org/en/quality-assurance/.
Back to Citation675. President's Commission on Combating Drug Addiction and the Opioid Crisis draft report, available at: https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Final_Report_Draft_11-15-2017.pdf.
Back to Citation676. We note that we previously referred to these factors as “criteria” (for example, 81 FR 57182 through 57183); we now use the term “factors” to align the PCHQR Program terminology with the terminology we use in other CMS quality reporting and pay for performance value-based purchasing programs.
Back to Citation677. This measure was initially endorsed by NQF, with corresponding measure number 1822. This measure lost its NQF endorsement in March 2018. National Quality Forum Cancer Project Final Report-Spring 2018. Available at: http://www.qualityforum.org/Publications/2018/08/Cancer_Final_Report_-_Spring_2018_Cycle.aspx.
Back to Citation678. 2018 EBRT Measure Information Form. Retrieved from: https://www.qualitynet.org/dcs/ContentServer?cid=1228774479863&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation679. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA: a cancer journal for clinicians. 2016; 66(1):7-30.
Back to Citation680. Ibid.
Back to Citation681. Bekelman JE, Mitra N, Efstathiou J, et al. Outcomes after intensity-modulated versus conformal radiotherapy in older men with nonmetastatic prostate cancer. International journal of radiation oncology, biology, physics. 2011;81(4):e325-334.
682. Potosky AL, Warren JL, Riedel ER, Klabunde CN, Earle CC, Begg CB. Measuring complications of cancer treatment using the SEER-Medicare data. Medical care. 2002;40(8 Suppl):IV-62-68.
Back to Citation683. Aizer AA, Gu X, Chen MH, et al. Cost implications and complications of overtreatment of low-risk prostate cancer in the United States. Journal of the National Comprehensive Cancer Network. 2015; 13(1):61-68.
684. Hayes JH, Ollendorf DA, Pearson SD, et al. Active surveillance compared with initial treatment for men with low-risk prostate cancer: a decision analysis. JAMA. 2010; 304(21):2373-2380.
Back to Citation685. Schmid M, Meyer CP, Reznor G, et al. Racial Differences in the Surgical Care of Medicare Beneficiaries With Localized Prostate Cancer. JAMA oncology. 2016; 2(1):85-93.
686. Jiang R, Tomaszewski JJ, Ward KC, Uzzo RG, Canter DJ. The burden of overtreatment: comparison of toxicity between single and combined modality radiation therapy among low risk prostate cancer patients. The Canadian journal of urology. 2015; 22(1):7648-7655.
687. Loeb S, Carter HB, Berndt SI, Ricker W, Schaeffer EM. Complications after prostate biopsy: Data from SEER-Medicare. The Journal of urology. 2011; 186(5):1830-1834.
Back to Citation688. Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998; 280(20):1747-1751.
Back to Citation689. Localized Prostate Cancer Standard Set, available at: http://www.ichom.org/medical-conditions/localized-prostate-cancer/.
Back to Citation690. Garcia-Baquero R, Fernandez-Avila CM, Alvarez-Ossorio JL. Functional results in the treatment of localized prostate cancer. An updated literature review. Rev Int Androl. 2018 Nov 22. pii: S1698-031X(18)30085-2.
691. Du Y, Long Q, Guan B, Mu L, Tian J, Jiang Y, Bai X, Wu D. Robot-Assisted Radical Prostatectomy Is More Beneficial for Prostate Cancer Patients: A System Review and Meta-Analysis. Med Sci Monit. 2018 Jan 14;24:272-287.
692. Wang X, Wu Y, Guo J, Chen H, Weng X, Liu X. Intrafascial nerve-sparing radical prostatectomy improves patients' postoperative continence recovery and erectile function: A pooled analysis based on available literatures. Medicine (Baltimore). 2018 Jul; 97(29):e11297.
693. Wallis CJD, Glaser A, Hu JC, Huland H, Lawrentschuk N, Moon D, Murphy DG, Nguyen PL, Resnick MJ, Nam RK. Survival and Complications Following Surgery and Radiation for Localized Prostate Cancer: An International Collaborative Review. Eur Urol. 2018 Jan; 73(1):11-20.
694. Huang X, Wang L, Zheng X, Wang X. Comparison of perioperative, functional, and oncologic outcomes between standard laparoscopic and robotic-assisted radical prostatectomy: A systemic review and meta-analysis. Surg Endosc. 2017 Mar; 31(3):1045-1060.
Back to Citation695. SEER-Medicare Dataset. Available at: https://healthcaredelivery.cancer.gov/seermedicare/overview/.
Back to Citation696. 2018-2019 Measure Applications Partnership Workgroup Final Recommendations Excel spreadsheet. Available at: http://www.qualityforum.org/Project_Pages/MAP_Hospital_Workgroup.aspx.
Back to Citation697. International Consortium for Health Outcomes Measurement (ICHOM) in the Localized Prostate Cancer Standard Set. https://www.ichom.org/medical-conditions/localized-prostate-cancer/.
Back to Citation698. Measures Application Partnership “2018 measures Under Consideration Spreadsheet.” Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=88813.
Back to Citation699. MAP 2019 Considerations for Implementing Measures, Final Report. Available at: http://www.qualityforum.org/Publications/2019/02/MAP_2019_Considerations_for_Implementing_Measures_Final_Report_-_Hospitals.aspx.
Back to Citation700. Ibid.
Back to Citation701. Ibid.
Back to Citation702. Overview of CMS “Meaningful Measures” Initiative. Available at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2017-Press-releases-items/2017-10-30.html.
Back to Citation703. Prostate Cancer Clinical Guidelines. Available at: http://www.auanet.org/guidelines/clinically-localized-prostate-cancer-new-(aua/astro/suo-guideline-2017.
Back to Citation704. Rudd, R., Aleshire, N., Zibbell, J., et al. “Increases in Drug and Opioid Overdose Deaths—United States, 2000-2014.” MMWR, Jan 2016. 64(50): 1378-82. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm.
Back to Citation705. Dowell, D., Haegerich, T., Chou, R. “CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016.” MMWR Recomm Rep 2016;65. Available at: http://www.cdc.gov/media/dpk/2016/dpk-opioid-prescription-guidelines.html.
706. Jena, A., et al. “Opioid prescribing by multiple providers in Medicare: retrospective observational study of insurance claims.” BMJ. 2014; 348:g1393 doi: 10.1136/bmj.g1393. Available at: http://www.bmj.com/content/348/bmj.g1393.
Back to Citation707. Herzig, S., Rothberg, M., Cheung, M., et al. “Opioid utilization and opioid-related adverse events in nonsurgical patients in U.S. hospitals.” Nov 2013. DOI: 10.1002/jhm.2102. Available at: http://onlinelibrary.wiley.com/doi/10.1002/jhm.2102/abstract.
Back to Citation708. Optimal Pain Management for Patients with Cancer in the Modern Era. Available at: https://onlinelibrary.wiley.com/doi/full/10.3322/caac.21453.
Back to Citation709. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Available at: https://www.ncbi.nlm.nih.gov/books/NBK2658/.
Back to Citation710. Ibid.
Back to Citation711. Ibid.
Back to Citation712. Alliance of Dedicate Cancer Centers website: http://www.adcc.org/.
Back to Citation713. National Quality Forum. Patient Reported Outcomes (PROs) in Performance Measurement. Available at: http://www.qualityforum.org/Publications/2012/12/Patient-Reported_Outcomes_in_Performance_Measurement.aspx. Published December 2012.
Back to Citation714. Basch E, Deal AM, Dueck AC, et al. Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment. JAMA. 2017; 318(2):197-198. doi:10.1001/jama.2017.7156.
715. Denis, F et al. Patient-Reported Outcomes, Mobile Technology, and Response Burden. 2018 ASCO Annual Meeting. Abstract No: 6500.
Back to Citation716. Centers for Disease Control and Prevention. “Paving Path Forward: 2015 Rebase line.” Available at: https://www.cdc.gov/nhsn/2015rebaseline/index.html.
Back to Citation717. Tian, W. “An all-payer view of hospital discharge to post-acute care,” May 2016. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.jsp.
Back to Citation718. Ibid.
Back to Citation719. RTI International analysis of Medicare claims data for index stays in LTCH 2016/2017. (RTI program reference: MM150).
Back to Citation720. Kwan, J. L., Lo, L., Sampson, M., & Shojania, K. G., “Medication reconciliation during transitions of care as a patient safety strategy: a systematic review,” Annals of Internal Medicine, 2013, Vol. 158(5), pp. 397-403.
721. Boockvar, K. S., Blum, S., Kugler, A., Livote, E., Mergenhagen, K. A., Nebeker, J. R., & Yeh, J., “Effect of admission medication reconciliation on adverse drug events from admission medication changes,” Archives of Internal Medicine, 2011, Vol. 171(9), pp. 860-861.
722. Bell, C. M., Brener, S. S., Gunraj, N., Huo, C., Bierman, A. S., Scales, D. C., & Urbach, D. R., “Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases,” JAMA, 2011, Vol. 306(8), pp. 840-847.
723. Basey, A. J., Krska, J., Kennedy, T. D., & Mackridge, A. J., “Prescribing errors on admission to hospital and their potential impact: a mixed-methods study,” BMJ Quality & Safety, 2014, Vol. 23(1), pp. 17-25.
724. Desai, R., Williams, C. E., Greene, S. B., Pierson, S., & Hansen, R. A., “Medication errors during patient transitions into nursing homes: characteristics and association with patient harm,” The American Journal of Geriatric Pharmacotherapy, 2011, Vol. 9(6), pp. 413-422.
725. Boling, P. A., “Care transitions and home health care,” Clinical Geriatric Medicine, 2009, Vol. 25(1), pp. 135-48.
Back to Citation726. Barnsteiner, J. H., “Medication Reconciliation: Transfer of medication information across settings—keeping it free from error,” The American Journal of Nursing, 2005, Vol. 105(3), pp. 31-36.
727. Arbaje, A. I., Kansagara, D. L., Salanitro, A. H., Englander, H. L., Kripalani, S., Jencks, S. F., & Lindquist, L. A., “Regardless of age: incorporating principles from geriatric medicine to improve care transitions for patients with complex needs,” Journal of General Internal Medicine, 2014, Vol. 29(6), pp. 932-939.
728. Jencks, S. F., Williams, M. V., & Coleman, E. A., “Rehospitalizations among patients in the Medicare fee-for-service program,” New England Journal of Medicine, 2009, Vol. 360(14), pp. 1418-1428.
729. Institute of Medicine. “Preventing medication errors: quality chasm series,” Washington, DC: The National Academies Press 2007. Available at: https://www.nap.edu/read/11623/chapter/1.
730. Kitson, N. A., Price, M., Lau, F. Y., & Showler, G., “Developing a medication communication framework across continuums of care using the Circle of Care Modeling approach,” BMC Health Services Research, 2013, Vol. 13(1), pp. 1-10.
731. Mor, V., Intrator, O., Feng, Z., & Grabowski, D. C., “The revolving door of rehospitalization from skilled nursing facilities,” Health Affairs, 2010, Vol. 29(1), pp. 57-64.
732. Institute of Medicine. “Preventing medication errors: quality chasm series,” Washington, DC: The National Academies Press 2007. Available at: https://www.nap.edu/read/11623/chapter/1.
733. Kitson, N. A., Price, M., Lau, F. Y., & Showler, G., “Developing a medication communication framework across continuums of care using the Circle of Care Modeling approach,” BMC Health Services Research, 2013, Vol. 13(1), pp. 1-10.
734. Forster, A. J., Murff, H. J., Peterson, J. F., Gandhi, T. K., & Bates, D. W., “The incidence and severity of adverse events affecting patients after discharge from the hospital.” Annals of Internal Medicine, 2003, 138(3), pp. 161-167.
735. King, B. J., Gilmore‐Bykovskyi, A. L., Roiland, R. A., Polnaszek, B. E., Bowers, B. J., & Kind, A. J. “The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study,” Journal of the American Geriatrics Society, 2013, Vol. 61(7), 1095-1102.
Back to Citation736. The Joint Commission, “Sentinel Event Policy” available at: https://www.jointcommission.org/sentinel_event_policy_and_procedures/.
Back to Citation737. The Joint Commission. “Sentinel Event Data Root Causes by Event Type 2004-2015.” 2016. Available at: https://www.jointcommission.org/assets/1/23/jconline_Mar_2_2016.pdf.
Back to Citation738. Mor, V., Intrator, O., Feng, Z., & Grabowski, D. C., “The revolving door of rehospitalization from skilled nursing facilities,” Health Affairs, 2010, Vol. 29(1), pp. 57-64.
739. Institute of Medicine, “Preventing medication errors: quality chasm series,” Washington, DC: The National Academies Press, 2007. Available at: https://www.nap.edu/read/11623/chapter/1.
740. Starmer, A. J., Sectish, T. C., Simon, D. W., Keohane, C., McSweeney, M. E., Chung, E. Y., Yoon, C.S., Lipsitz, S.R., Wassner, A.J., Harper, M. B., & Landrigan, C. P., “Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle,” JAMA, 2013, Vol. 310(21), pp. 2262-2270.
741. Pronovost, P., M. M. E. Johns, S. Palmer, R. C. Bono, D. B. Fridsma, A. Gettinger, J., Goldman, W. Johnson, M. Karney, C. Samitt, R. D. Sriram, A. Zenooz, and Y. C. Wang, Editors. Procuring Interoperability: Achieving High-Quality, Connected, and Person-Centered Care. Washington, DC, 2018.; National Academy of Medicine. Available at: https://nam.edu/wp-content/uploads/2018/10/Procuring-Interoperability_web.pdf.
742. Balaban RB, Weissman JS, Samuel PA, & Woolhandler, S., “Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study,” J Gen Intern Med, 2008, Vol. 23(8), pp. 1228-33.
Back to Citation743. Arbaje, A. I., Kansagara, D. L., Salanitro, A. H., Englander, H. L., Kripalani, S., Jencks, S. F., & Lindquist, L. A., “Regardless of age: incorporating principles from geriatric medicine to improve care transitions for patients with complex needs,” Journal of General Internal Medicine, 2014, Vol 29(6), pp. 932-939.
744. Simmons, S., Schnelle, J., Slagle, J., Sathe, N. A., Stevenson, D., Carlo, M., & McPheeters, M. L., “Resident safety practices in nursing home settings.” Technical Brief No. 24 (Prepared by the Vanderbilt Evidence-based Practice Center under Contract No. 290-2015-00003-I.) AHRQ Publication No. 16-EHC022-EF. Rockville, MD: Agency for Healthcare Research and Quality. May 2016. Available at: https://www.ncbi.nlm.nih.gov/books/NBK384624/.
Back to Citation745. Berwick, D. M. & Hackbarth, A. D. “Eliminating Waste in US Health Care,” JAMA, 2012, Vol. 307(14), pp. 1513-1516.
Back to Citation746. McDonald, K. M., Sundaram, V., Bravata, D. M., Lewis, R., Lin, N., Kraft, S. A. & Owens, D. K. Care Coordination. Vol. 7 of: Shojania K.G., McDonald K.M., Wachter R.M., Owens D.K., editors. “Closing the quality gap: A critical analysis of quality improvement strategies.” Technical Review 9 (Prepared by the Stanford University-UCSF Evidence-based Practice Center under contract 290-02-0017). AHRQ Publication No. 04(07)-0051-7. Rockville, MD: Agency for Healthcare Research and Quality. June 2006. Available at: https://www.ncbi.nlm.nih.gov/books/NBK44015/.
747. Lattimer, C., “When it comes to transitions in patient care, effective communication can make all the difference,” Generations, 2011, Vol. 35(1), pp. 69-72.
Back to Citation748. Starmer A. J, Spector N. D., Srivastava R., West, D. C., Rosenbluth, G., Allen, A. D., Noble, E. L., & Landrigen, C. P., “Changes in medical errors after implementation of a handoff program,” N Engl J Med, 2014, Vol. 37(1), pp. 1803-1812.
749. Kruse, C.S. Marquez, G., Nelson, D., & Polomares, O., “The use of health information exchange to augment patient handoff in long-term care: a systematic review,” Applied Clinical Informatics, 2018, Vol. 9(4), pp. 752-771.
750. Brody, A. A., Gibson, B., Tresner-Kirsch, D., Kramer, H., Thraen, I., Coarr, M. E., & Rupper, R., “High prevalence of medication discrepancies between home health referrals and Centers for Medicare and Medicaid Services home health certification and plan of care and their potential to affect safety of vulnerable elderly adults,” Journal of the American Geriatrics Society, 2016, Vol. 64(11), pp. e166-e170.
Back to Citation751. Chhabra, P. T., Rattinger, G. B., Dutcher, S. K., Hare, M. E., Parsons, K., L., & Zuckerman, I. H., “Medication reconciliation during the transition to and from long-term care settings: a systematic review,” Res Social Adm Pharm, 2012, Vol. 8(1), pp. 60-75.
752. Health and Human Services Office of Inspector General. Adverse Events in Long-Term-Care Hospitals: National Incidence Among Medicare Beneficiaries. (OEI-06-14-00530). 2018. Available at: https://oig.hhs.gov/oei/reports/oei-06-14-00530.asp.
Back to Citation753. Battles J., Azam I., Grady M., & Reback K., “Advances in patient safety and medical liability,” AHRQ Publication No. 17-0017-EF. Rockville, MD: Agency for Healthcare Research and Quality, August 2017. Available at: https://www.ahrq.gov/sites/default/files/publications/files/advances-complete_3.pdf.
Back to Citation754. Health and Human Services Office of Inspector General. Adverse Events in Long-Term-Care Hospitals: National Incidence Among Medicare Beneficiaries. (OEI-06-14-00530). 2018. Available at: https://oig.hhs.gov/oei/reports/oei-06-14-00530.asp.
Back to Citation755. Barnsteiner, J. H., “Medication Reconciliation: Transfer of medication information across settings—keeping it free from error,” The American Journal of Nursing, 2005, Vol. 105(3), pp. 31-36.
756. Gleason, K. M., Groszek, J. M., Sullivan, C., Rooney, D., Barnard, C., Noskin, G. A., “Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients,” American Journal of Health System Pharmacy, 2004, Vol. 61(16), pp. 1689-1694.
Back to Citation757. Patterson M., Foust J. B., Bollinger, S., Coleman, C., Nguyen, D., “Inter-facility communication barriers delay resolving medication discrepancies during transitions of care,” Research in Social & Administrative Pharmacy (2018), doi: 10.1016/j.sapharm.2018.05.124.
Back to Citation758. Manias, E., Annaikis, N., Considine, J., Weerasuriya, R., & Kusljic, S. “Patient-, medication- and environment-related factors affecting medication discrepancies in older patients,” Collegian, 2017, Vol. 24, pp. 571-577.
Back to Citation759. Tjia, J., Bonner, A., Briesacher, B. A., McGee, S., Terrill, E., Miller, K., “Medication discrepancies upon hospital to skilled nursing facility transitions,” J Gen Intern Med, 2009, Vol. 24(5), pp. 630-635.
760. Sinvani, L. D., Beizer, J., Akerman, M., Pekmezaris, R., Nouryan, C., Lutsky, L., Cal, C., Dlugacz, Y., Masick, K., Wolf-Klein, G.,“Medication reconciliation in continuum of care transitions: a moving target,” J Am Med Dir Assoc, 2013, Vol. 14(9), 668-672.
761. Coleman E. A., Parry C., Chalmers S., & Min, S. J., “The Care Transitions Intervention: results of a randomized controlled trial,” Arch Intern Med, 2006, Vol. 166, pp. 1822-28.
Back to Citation762. Corbett C. L., Setter S. M., Neumiller J. J., & Wood, l. D., “Nurse identified hospital to home medication discrepancies: implications for improving transitional care,” Geriatr Nurs, 2011, Vol. 31(3), pp. 188-96.
763. Setter S. M., Corbett C. F., Neumiller J. J., Gates, B. J., Sclar, D. A., & Sonnett, T. E., “Effectiveness of a pharmacist-nurse intervention on resolving medication discrepancies in older patients transitioning from hospital to home care: impact of a pharmacy/nursing intervention,” Am J Health Syst Pharm, 2009, Vol. 66, pp. 2027-31.
Back to Citation764. Boockvar, K.S., Blum, S., Kugler, A., Livote, E., Mergenhagen, K.A., Nebeker, J.R., & Yeh, J., “Effect of admission medication reconciliation on adverse drug events from admission medication changes,” Archives of Internal Medicine, 2011, Vol. 171(9), pp. 860-861.
765. Kwan, J.L., Lo, L., Sampson, M., & Shojania, K.G., “Medication reconciliation during transitions of care as a patient safety strategy: a systematic review,” Annals of Internal Medicine, 2013, Vol. 158(5), pp. 397-403.
766. Chhabra, P.T., Rattinger, G.B., Dutcher, S.K., Hare, M.E., Parsons, K.L., & Zuckerman, I.H., “Medication reconciliation during the transition to and from long-term care settings: a systematic review,” Res Social Adm Pharm, 2012, Vol. 8(1), pp. 60-75.
Back to Citation767. Agrawal A, Wu WY. “Reducing medication errors and improving systems reliability using an electronic medication reconciliation system,” The Joint Commission Journal on Quality and Patient Safety, 2009, Vol. 35(2), pp. 106-114.
Back to Citation768. Technical Expert Panel Summary Report: Development of two quality measures to satisfy the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) Domain of Transfer of Health Information and Care Preferences When an Individual Transitions to Skilled Nursing Facilities (SNFs), Inpatient Rehabilitation Facilities (IRFs), Long Term Care Hospitals (LTCHs) and Home Health Agencies (HHAs). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/Downloads/Transfer-of-Health-Information-TEP_Summary_Report_Final-June-2017.pdf.
Back to Citation769. Technical Expert Panel Summary Report: Development of two quality measures to satisfy the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) Domain of Transfer of Health Information and Care Preferences When an Individual Transitions to Skilled Nursing Facilities (SNFs), Inpatient Rehabilitation Facilities (IRFs), Long Term Care Hospitals (LTCHs) and Home Health Agencies (HHAs). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/Downloads/Transfer-of-Health-Information-TEP-Meetings-2-3-Summary-Report_Final_Feb2018.pdf.
Back to Citation770. Ibid.
Back to Citation771. Tian, W. “An all-payer view of hospital discharge to postacute care,” May 2016. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.jsp.
Back to Citation772. RTI International analysis of Medicare claims data for index stays in LTCH 2016/2017. (RTI program reference: MM150).
Back to Citation773. Kwan, J.L., Lo, L., Sampson, M., & Shojania, K.G., “Medication reconciliation during transitions of care as a patient safety strategy: a systematic review,” Annals of Internal Medicine, 2013, Vol. 158(5), pp. 397-403.
774. Boockvar, K.S., Blum, S., Kugler, A., Livote, E., Mergenhagen, K.A., Nebeker, J.R., & Yeh, J., “Effect of admission medication reconciliation on adverse drug events from admission medication changes,” Archives of Internal Medicine, 2011, Vol. 171(9), pp. 860-861.
775. Bell, C.M., Brener, S.S., Gunraj, N., Huo, C., Bierman, A.S., Scales, D.C., & Urbach, D.R., “Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases,” JAMA, 2011, Vol. 306(8), pp. 840-847.
776. Basey, A.J., Krska, J., Kennedy, T.D., & Mackridge, A.J., “Prescribing errors on admission to hospital and their potential impact: a mixed-methods study,” BMJ Quality & Safety, 2014, Vol. 23(1), pp. 17-25.
777. Desai, R., Williams, C.E., Greene, S.B., Pierson, S., & Hansen, R.A., “Medication errors during patient transitions into nursing homes: characteristics and association with patient harm,” The American Journal of Geriatric Pharmacotherapy, 2011, Vol. 9(6), pp. 413-422.
Back to Citation778. Brody, A.A., Gibson, B., Tresner-Kirsch, D., Kramer, H., Thraen, I., Coarr, M.E., & Rupper, R. “High prevalence of medication discrepancies between home health referrals and Centers for Medicare and Medicaid Services home health certification and plan of care and their potential to affect safety of vulnerable elderly adults,” Journal of the American Geriatrics Society, 2016, Vol. 64(11), pp. e166-e170.
779. Chhabra, P.T., Rattinger, G.B., Dutcher, S.K., Hare, M.E., Parsons, K., L., & Zuckerman, I.H., “Medication reconciliation during the transition to and from long-term care settings: a systematic review,” Res Social Adm Pharm, 2012, Vol. 8(1), pp. 60-75.
Back to Citation780. Brody, A.A., Gibson, B., Tresner-Kirsch, D., Kramer, H., Thraen, I., Coarr, M.E., & Rupper, R. “High prevalence of medication discrepancies between home health referrals and Centers for Medicare and Medicaid Services home health certification and plan of care and their potential to affect safety of vulnerable elderly adults,” Journal of the American Geriatrics Society, 2016, Vol. 64(11), pp. e166-e170.
781. Bell, C.M., Brener, S.S., Gunraj, N., Huo, C., Bierman, A.S., Scales, D.C., & Urbach, D.R., “Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases,” JAMA, 2011, Vol. 306(8), pp. 840-847.
782. Sheehan, O.C., Kharrazi, H., Carl, K.J., Leff, B., Wolff, J.L., Roth, D.L., Gabbard, J., & Boyd, C.M., “Helping older adults improve their medication experience (HOME) by addressing medication regimen complexity in home healthcare,” Home Healthcare Now. 2018, Vol. 36(1) pp. 10-19.
Back to Citation783. Mor, V., Intrator, O., Feng, Z., & Grabowski, D.C., “The revolving door of rehospitalization from skilled nursing facilities,” Health Affairs, 2010, Vol. 29(1), pp. 57-64.
784. Starmer, A.J., Sectish, T.C., Simon, D.W., Keohane, C., McSweeney, M.E., Chung, E.Y., Yoon, C.S., Lipsitz, S.R., Wassner, A.J., Harper, M.B., & Landrigan, C.P., “Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle,” JAMA, 2013, Vol. 310(21), pp. 2262-2270.
Back to Citation785. CMS, “Revision to state operations manual (SOM), Hospital Appendix A—Interpretive Guidelines for 42 CFR 482.43, Discharge Planning” May 17, 2013. Available at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-32.pdf.
786. The State Operations Manual Guidance to Surveyors for Long Term Care Facilities (Guidance § 483.21(c)(1) Rev. 11-22-17) for discharge planning process. Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_pp_guidelines_ltcf.pdf.
Back to Citation787. Toles, M., Colon-Emeric, C., Naylor, M.D., Asafu-Adjei, J., Hanson, L.C., “Connect-home: transitional care of skilled nursing facility patients and their caregivers,” Am Geriatr Soc., 2017, Vol. 65(10), pp. 2322-2328.
Back to Citation788. Technical Expert Panel Summary Report: Development of two quality measures to satisfy the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) Domain of Transfer of health Information and Care Preferences When an Individual Transitions to Skilled Nursing Facilities (SNFs), Inpatient Rehabilitation Facilities (IRFs), Long Term Care Hospitals (LTCHs) and Home Health Agencies (HHAs). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/Downloads/Transfer-of-Health-Information-TEP_Summary_Report_Final-June-2017.pdf.
Back to Citation789. Technical Expert Panel Summary Report: Development of two quality measures to satisfy the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) Domain of Transfer of health Information and Care Preferences When an Individual Transitions to Skilled Nursing Facilities (SNFs), Inpatient Rehabilitation Facilities (IRFs), Long Term Care Hospitals (LTCHs) and Home Health Agencies (HHAs). Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/Downloads/Transfer-of-Health-Information-TEP-Meetings-2-3-Summary-Report_Final_Feb2018.pdf.
Back to Citation790. Ibid.
Back to Citation791. National Institute on Aging. (2014). Assessing Cognitive Impairment in Older Patients. A Quick Guide for Primary Care Physicians. Retrieved from: https://www.nia.nih.gov/alzheimers/publication/assessing-cognitive-impairment-older-patients.
Back to Citation792. Gage B., Morley M., Smith L., et al. (2012). Post-Acute Care Payment Reform Demonstration (Final report, Volume 4 of 4). Research Triangle Park, NC: RTI International.
Back to Citation793. Casey D.A., Antimisiaris D., O'Brien J. (2010). Drugs for Alzheimer's Disease: Are They Effective? Pharmacology & Therapeutics, 35, 208-11.
794. Graff M.J., Vernooij-Dassen M.J., Thijssen M., Dekker J., Hoefnagels W.H., Rikkert M.G.O. (2006). Community Based Occupational Therapy for Patients with Dementia and their Care Givers: Randomised Controlled Trial. BMJ, 333(7580): 1196.
795. Bherer L., Erickson K.I., Liu-Ambrose T. (2013). A Review of the Effects of Physical Activity and Exercise on Cognitive and Brain Functions in Older Adults. Journal of Aging Research, 657508.
Back to Citation796. Giacino J.T., Whyte J., Bagiella E., et al. (2012). Placebo-controlled trial of amantadine for severe traumatic brain injury. New England Journal of Medicine, 366(9), 819-826.
Back to Citation797. Alexopoulos G.S., Katz I.R., Reynolds C.F. 3rd, Carpenter D., Docherty J.P., Ross R.W. (2001). Pharmacotherapy of depression in older patients: a summary of the expert consensus guidelines. Journal of Psychiatric Practice, 7(6), 361-376.
798. Arean P.A., Cook B.L. (2002). Psychotherapy and combined psychotherapy/pharmacotherapy for late life depression. Biological Psychiatry, 52(3), 293-303.
799. Hollon S.D., Jarrett R.B., Nierenberg A.A., Thase M.E., Trivedi M., Rush A.J. (2005). Psychotherapy and medication in the treatment of adult and geriatric depression: which monotherapy or combined treatment? Journal of Clinical Psychiatry, 66(4), 455-468.
800. Wagenaar D., Colenda CC., Kreft M., Sawade J., Gardiner J., Poverejan E. (2003). Treating depression in nursing homes: practice guidelines in the real world. J Am Osteopath Assoc. 103(10), 465-469.
Back to Citation801. Crespy SD., Van Haitsma K., Kleban M., Hann CJ. Reducing Depressive Symptoms in Nursing Home Residents: Evaluation of the Pennsylvania Depression Collaborative Quality Improvement Program. J Healthc Qual. 2016. Vol. 38, No. 6, pp. e76-e88.
Back to Citation802. Agüero-Torres, H., Fratiglioni, L., Guo, Z., Viitanen, M., von Strauss, E., & Winblad, B. (1998). “Dementia is the major cause of functional dependence in the elderly: 3-year follow-up data from a population-based study.” Am J of Public Health 88(10): 1452-1456.
Back to Citation803. RTI International. Proposed Measure Specifications for Measures Proposed in the FY 2017 LTCH QRP NPRM. Research Triangle Park, NC. 2016.
Back to Citation804. Fick, D. M., Steis, M. R., Waller, J. L., & Inouye, S. K. (2013). “Delirium superimposed on dementia is associated with prolonged length of stay and poor outcomes in hospitalized older adults.” J of Hospital Med 8(9): 500-505.
Back to Citation805. Dan K. Kiely et al., “Characteristics Associated with Delirium Persistence Among Newly Admitted Post-Acute Facility Patients,” Journals of Gerontology: Series A (Biological Sciences and Medical Sciences), Vol. 59, No. 4, April 2004; Edward R. Marcantonio et al., “Delirium Symptoms in Post-Acute Care: Prevalent, Persistent, and Associated with Poor Functional Recovery,” Journal of the American Geriatrics Society, Vol. 51, No. 1, January 2003.
Back to Citation806. Marcantonio, Edward R., Samuel E. Simon, Margaret A. Bergmann, Richard N. Jones, Katharine M. Murphy, and John N. Morris, “Delirium Symptoms in Post-Acute Care: Prevalent, Persistent, and Associated with Poor Functional Recovery,” Journal of the American Geriatrics Society, Vol. 51, No. 1, January 2003, pp. 4-9.
Back to Citation807. Edward R. Marcantonio et al., Outcomes of Older People Admitted to Postacute Facilities with Delirium,” Journal of the American Geratrics Society, Vol. 53, No. 6, June 2005.
Back to Citation808. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet 2014;383:911-922.
809. Marcantonio ER. In the clinic: delirium. Ann Intern Med 2011;154:ITC6-1-ITC6-1.
Back to Citation810. Yang FM, Marcantonio ER, Inouye SK, et al. Phenomenological subtypes of delirium in older persons: patterns, prevalence, and prognosis. Psychosomatics2009;50:248-254
Back to Citation811. Marcantonio ER. Delirium in Hospitalized Older Adults. N Engl J Med. 2017 Oct 12;377(15):1456-1466.
Back to Citation812. Li, C., Friedman, B., Conwell, Y., & Fiscella, K. (2007). “Validity of the Patient Health Questionnaire 2 (PHQ-2) in identifying major depression in older people.” J of the A Geriatrics Society, 55(4): 596-602.
813. Löwe, B., Kroenke, K., & Gräfe, K. (2005). “Detecting and monitoring depression with a two-item questionnaire (PHQ-2).” J of Psychosomatic Research, 58(2): 163-171.
Back to Citation814. Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Annals of family medicine. 2010;8(4):348-53. doi: 10.1370/afm.1139 pmid:20644190; PubMed Central PMCID: PMC2906530.
Back to Citation815. Kroenke K, Spitzer RL, Williams JWB. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001 Sep; 16(9): 606-613.
Back to Citation816. Kroenke K, Spitzer RL, Williams JWB. The Patient Health Questionnaire-2: Validity of a Two-Item Depression Screener. Med Care. Vol. 41, No. 11 (Nov., 2003), pp. 1284-1292.
Back to Citation817. “Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements,” available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Post-Acute-Care-Quality-Initiatives/IMPACT-Act-of-2014/IMPACT-Act-Downloads-and-Videos.html.
Back to Citation818. Wunsch, H., Linde-Zwirble, W. T., Angus, D. C., Hartman, M. E., Milbrandt, E. B., & Kahn, J. M. (2010). “The epidemiology of mechanical ventilation use in the United States.” Critical Care Med 38(10): 1947-1953.
Back to Citation819. Dempsey, D.T., Mullen, J.L., & Buzby, G.P. (1988). “The link between nutritional status and clinical outcome: can nutritional intervention modify it?” Am J of Clinical Nutrition, 47(2): 352-356.
Back to Citation820. Dempsey, D.T., Mullen, J.L., & Buzby, G.P. (1988). “The link between nutritional status and clinical outcome: can nutritional intervention modify it?” Am J of Clinical Nutrition, 47(2): 352-356.
Back to Citation821. U.S. Department of Health and Human Services. Office of Inspector General. Daniel R. Levinson Adverse Events in Hospitals: National Incidence Among Medicare Beneficiaries. OEI-06-09-00090. November 2010. Available at: https://www.oig.hhs.gov/oei/reports/oei-06-09-00090.pdf.
Back to Citation822. Boockvar KS, Liu S, Goldstein N, Nebeker J, Siu A, Fried T. Prescribing discrepancies likely to cause adverse drug events after patient transfer. Qual Saf Health Care. 2009;18(1):32-6.
Back to Citation823. Gandhi TK, Seger AC, Overhage JM, et al. Outpatient adverse drug events identified by screening electronic health records. J Patient Saf 2010;6:91-6.doi:10.1097/PTS.0b013e3181dcae06.
Back to Citation824. Gurwitz JH, Field TS, Judge J, Rochon P, Harrold LR, Cadoret C, et al. The incidence of adverse drug events in two large academic long-term care facilities. Am J Med. 2005; 118(3):251±8. Epub 2005/03/05. Available at: https://doi.org/10.1016/j.amjmed.2004.09.018 PMID: 15745723.
Back to Citation825. Hug BL, Witkowski DJ, Sox CM, Keohane CA, Seger DL, Yoon C, Matheny ME, Bates DW. Occurrence of adverse, often preventable, events in community hospitals involving nephrotoxic drugs or those excreted by the kidney. Kidney Int. 2009; 76:1192-1198. [PubMed: 19759525].
Back to Citation826. Barnsteiner JH. Medication reconciliation: transfer of medication information across settings—keeping it free from error. J Infus Nurs. 2005;28(2 Suppl):31-36.
827. Rozich J, Roger, R. Medication safety: one organization's approach to the challenge. Journal of Clinical Outcomes Management. 2001(8):27-34.
828. Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health Syst Pharm. 2004;61(16):1689-1695.
Back to Citation829. Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA. doi: 10.1001/jama.2016.16201.
Back to Citation830. Ibid.
Back to Citation831. Shoeb M, Fang MC. Assessing bleeding risk in patients taking anticoagulants. J Thromb Thrombolysis. 2013;35(3):312-319. doi: 10.1007/s11239-013-0899-7.
832. Melkonian M, Jarzebowski W, Pautas E. Bleeding risk of antiplatelet drugs compared with oral anticoagulants in older patients with atrial fibrillation: a systematic review and meta‐analysis. J Thromb Haemost. 2017;15:1500-1510. DOI: 10.1111/jth.13697.
Back to Citation833. Hamnvik OP, McMahon GT. Balancing Risk and Benefit with Oral Hypoglycemic Drugs. The Mount Sinai journal of medicine, New York. 2009; 76:234-243.
Back to Citation834. Naples JG, Gellad WF, Hanlon JT. The Role of Opioid Analgesics in Geriatric Pain Management. Clin Geriatr Med. 2016;32(4):725-735.
Back to Citation835. Rigler SK, Shireman TI, Cook-Wiens GJ, Ellerbeck EF, Whittle JC, Mehr DR, Mahnken JD. Fracture risk in nursing home residents initiating antipsychotic medications. J Am Geriatr Soc. 2013; 61(5):715-722. [PubMed: 23590366].
836. Wang S, Linkletter C, Dore D et al. Age, antipsychotics, and the risk of ischemic stroke in the Veterans Health Administration. Stroke 2012;43:28-31. doi:10.1161/STROKEAHA.111.617191.
Back to Citation837. Faulkner CM, Cox HL, Williamson JC. Unique aspects of antimicrobial use in older adults. Clin Infect Dis. 2005;40(7):997-1004.
Back to Citation838. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society. Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 2015; 63:2227-2246.
Back to Citation839. Li Y, Salmasian H, Harpaz R, Chase H, Friedman C. Determining the reasons for medication prescriptions in the EHR using knowledge and natural language processing. AMIA Annu Symp Proc. 2011;2011:768-76.
Back to Citation840. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society. Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 2015; 63:2227-2246.
Back to Citation841. Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA 2016;316(2):2115-2125.
Back to Citation842. Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA 2016;316(2):2115-2125.
Back to Citation843. Department of Health and Human Services: Pain Management Best Practices Inter-Agency Task Force. Draft Report on Pain Management Best Practices: Updates, Gaps, Inconsistencies, and Recommendations. Accessed April 1, 2019. https://www.hhs.gov/sites/default/files/final-pmtf-draft-report-on-pain-management%20-best-practices-2018-12-12-html-ready-clean.pdf.
Back to Citation844. Department of Health and Human Services: Pain Management Best Practices Inter-Agency Task Force. Draft Report on Pain Management Best Practices: Updates, Gaps, Inconsistencies, and Recommendations. Accessed April 1, 2019. https://www.hhs.gov/sites/default/files/final-pmtf-draft-report-on-pain-management%20-best-practices-2018-12-12-html-ready-clean.pdf.
845. Fishman SM, Carr DB, Hogans B, et al. Scope and Nature of Pain- and Analgesia-Related Content of the United States Medical Licensing Examination (USMLE). Pain Med Malden Mass. 2018;19(3):449-459. doi:10.1093/pm/pnx336.
846. Fishman SM, Young HM, Lucas Arwood E, et al. Core competencies for pain management: results of an interprofessional consensus summit. Pain Med Malden Mass. 2013;14(7):971-981. doi:10.1111/pme.12107.
Back to Citation847. Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. http://www.ncbi.nlm.nih.gov/books/NBK91497/.
Back to Citation848. Department of Health and Human Services: Pain Management Best Practices Inter-Agency Task Force. Draft Report on Pain Management Best Practices: Updates, Gaps, Inconsistencies, and Recommendations. Accessed April 1, 2019. https://www.hhs.gov/sites/default/files/final-pmtf-draft-report-on-pain-management%20-best-practices-2018-12-12-html-ready-clean.pdf.
Back to Citation849. National Academies. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Washington, DC: National Academies of Sciences, Engineering, and Medicine; 2017.
Back to Citation850. National Pain Strategy: A Comprehensive Population-Health Level Strategy for Pain. Available at: https://iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy_508C.pdf.
Back to Citation851. Chau, D.L., Walker, V., Pai, L., & Cho, L.M. (2008). Opiates and elderly: use and side effects. Clinical interventions in aging, 3 (2), 273-8.
852. Fine, P.G. (2009). Chronic Pain Management in Older Adults: Special Considerations. Journal of Pain and Symptom Management, 38(2): S4-S14.
853. Solomon, D.H., Rassen, J.A., Glynn, R.J., Garneau, K., Levin, R., Lee, J., & Schneeweiss, S. (2010). Archives Internal Medicine, 170(22):1979-1986.
Back to Citation854. Byrd L. Managing chronic pain in older adults: a long-term care perspective. Annals of Long-Term Care: Clinical Care and Aging. 2013;21(12):34-40.
855. Kligler, B., Bair, M.J., Banerjea, R. et al. (2018). Clinical Policy Recommendations from the VHA State-of-the-Art Conference on Non-Pharmacological Approaches to Chronic Musculoskeletal Pain. Journal of General Internal Medicine, 33 (Suppl 1): 16. https://doi.org/10.1007/s11606-018-4323-z.
856. Chou, R., Deyo, R., Friedly, J., et al. (2017). Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Annals of Internal Medicine, 166 (7):493-505.
Back to Citation857. Society for Post-Acute and Long-Term Care Medicine (AMDA). (2018). Opioids in Nursing Homes: Position Statement. Available at: https://paltc.org/opioids%20in%20nursing%20homes.
Back to Citation858. https://www.hhs.gov/opioids/about-the-epidemic/hhs-response/index.html.
Back to Citation859. Dalton DS, Cruickshanks KJ, Klein BE, Klein R, Wiley TL, Nondahl DM. The impact of hearing loss on quality of life in older adults . Gerontologist. 2003;43(5):661-668.
860. Hawkins K, Bottone FG, Jr., Ozminkowski RJ, et al. The prevalence of hearing impairment and its burden on the quality of life among adults with Medicare Supplement Insurance. Qual Life Res. 2012;21(7):1135-1147.
Back to Citation861. Horn KL, McMahon NB, McMahon DC, Lewis JS, Barker M, Gherini S. Functional use of the Nucleus 22-channel cochlear implant in the elderly. The Laryngoscope. 1991;101(3):284-288.
Back to Citation862. Sprinzl GM, Riechelmann H. Current trends in treating hearing loss in elderly people: a review of the technology and treatment options—a mini-review. Gerontology. 2010;56(3):351-358.
863. Lin FR, Thorpe R, Gordon-Salant S, Ferrucci L. Hearing Loss Prevalence and Risk Factors Among Older Adults in the United States. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2011;66A(5):582-590.
864. Hawkins K, Bottone FG, Jr., Ozminkowski RJ, et al. The prevalence of hearing impairment and its burden on the quality of life among adults with Medicare Supplement Insurance. Qual Life Res. 2012;21(7):1135-1147.
Back to Citation865. Lin FR, Metter EJ, O'Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing Loss and Incident Dementia. Arch Neurol. 2011;68(2):214-220.
Back to Citation866. Cimarolli VR, Jung S. Intensity of Occupational Therapy Utilization in Nursing Home Residents: The Role of Sensory Impairments. J Am Med Dir Assoc. 2016;17(10):939-942.
Back to Citation867. Colon-Emeric CS, Biggs DP, Schenck AP, Lyles KW. Risk factors for hip fracture in skilled nursing facilities: who should be evaluated? Osteoporos Int. 2003;14(6):484-489.
868. Freeman EE, Munoz B, Rubin G, West SK. Visual field loss increases the risk of falls in older adults: the Salisbury eye evaluation. Invest Ophthalmol Vis Sci. 2007;48(10):4445-4450.
869. Keepnews D, Capitman JA, Rosati RJ. Measuring patient-level clinical outcomes of home health care. J Nurs Scholarsh. 2004;36(1):79-85.
870. Nguyen HT, Black SA, Ray LA, Espino DV, Markides KS. Predictors of decline in MMSE scores among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2002;57(3):M181-185.
871. Prager AJ, Liebmann JM, Cioffi GA, Blumberg DM. Self-reported Function, Health Resource Use, and Total Health Care Costs Among Medicare Beneficiaries With Glaucoma. JAMA ophthalmology. 2016;134(4):357-365.
872. Rovner BW, Ganguli M. Depression and disability associated with impaired vision: the MoVies Project. J Am Geriatr Soc. 1998;46(5):617-619.
873. Tinetti ME, Ginter SF. The nursing home life-space diameter. A measure of extent and frequency of mobility among nursing home residents. J Am Geriatr Soc. 1990;38(12):1311-1315.
Back to Citation874. National Academies of Sciences, Engineering, and Medicine. 2016. Accounting for social risk factors in Medicare payment: Identifying social risk factors. Chapter 2. Washington, DC: The National Academies Press.
Back to Citation875. Social Determinants of Health. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. (February 2019).
Back to Citation876. U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. 2016. Report to Congress: Social Risk Factors and Performance Under Medicare's Value-Based Payment Programs. Washington, DC.
Back to Citation877. Health Leads. Available at: https://healthleadsusa.org/.
Back to Citation878. 2017 National Healthcare Quality and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; September 2018. AHRQ Pub. No. 18-0033-EF.
879. Fiscella, K. and Sanders, M.R. Racial and Ethnic Disparities in the Quality of Health Care. (2016). Annual Review of Public Health. 37:375-394.
880. 2018 National Impact Assessment of the Centers for Medicare & Medicaid Services (CMS) Quality Measures Reports. Baltimore, MD: U.S. Department of Health and Human Services, Centers for Medicare and Medicaid Services; February 28, 2018.
881. Smedley, B.D., Stith, A.Y., & Nelson, A.R. (2003). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC, National Academy Press.
882. Chase, J., Huang, L. and Russell, D. (2017). Racial/ethnic disparities in disability outcomes among post-acute home care patients. J of Aging and Health. 30(9):1406-1426.
Back to Citation883. National Healthcare Quality and Disparities Reports. (December 2018). Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/research/findings/nhqrdr/index.html.
Back to Citation884. National Center for Health Statistics. Health, United States, 2017: With special feature on mortality. Hyattsville, Maryland. 2018.
Back to Citation885. HHS. Heart disease and African Americans. 2016b. (October 24, 2016). http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=19.
Back to Citation886. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States; Baciu A., Negussie Y., Geller A., et al., editors. Communities in Action: Pathways to Health Equity. Washington (DC): National Academies Press (US); 2017 Jan 11. 2, The State of Health Disparities in the United States. Available from: https://www.ncbi.nlm.nih.gov/books/NBK425844/.
Back to Citation887. “Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity (Notice of Decision)”. Federal Register 62:210 (October 30, 1997) pp. 58782-58790. Available from: https://www.govinfo.gov/content/pkg/FR-1997-10-30/pdf/97-28653.pdf.
Back to Citation888. Penman-Aguilar, A., Talih, M., Huang, D., Moonesinghe, R., Bouye, K., Beckles, G. (2016). Measurement of Health Disparities, Health Inequities, and Social Determinants of Health to Support the Advancement of Health Equity. J Public Health Manag Pract. 22 Suppl 1: S33-42.
889. Ramos, R., Davis, J.L., Ross, T., Grant, C.G., Green, B.L. (2012). Measuring health disparities and health inequities: do you have REGAL data? Qual Manag Health Care. 21(3):176-87.
890. IOM (Institute of Medicine). 2009. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: The National Academies Press.
891. “Revision of Standards for Maintaining, Collecting, and Presenting Federal Data on Race and Ethnicity: Proposals From Federal Interagency Working Group (Notice and Request for Comments).” Federal Register 82: 39 (March 1, 2017) p. 12242.
Back to Citation892. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States; Baciu A., Negussie Y., Geller A., et al., editors. Communities in Action: Pathways to Health Equity. Washington (DC): National Academies Press (US); 2017 Jan 11. 2, The State of Health Disparities in the United States. Available from: https://www.ncbi.nlm.nih.gov/books/NBK425844/.
Back to Citation893. IOM (Institute of Medicine). 2009. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: The National Academies Press.
Back to Citation894. HHS Data Standards. Available at https://aspe.hhs.gov/basic-report/hhs-implementation-guidance-data-collection-standards-race-ethnicity-sex-primary-language-and-disability-status.
Back to Citation895. U.S. Census Bureau, 2013-2017 American Community Survey 5-Year Estimates.
Back to Citation896. Karliner LS, Kim SE, Meltzer DO, Auerbach AD. Influence of language barriers on outcomes of hospital care for general medicine inpatients. J Hosp Med. 2010 May-Jun;5(5):276-82. doi: 10.1002/jhm.658.
897. Kim EJ, Kim T, Paasche-Orlow MK, et al. Disparities in Hypertension Associated with Limited English Proficiency. J Gen Intern Med. 2017 Jun;32(6):632-639. doi: 10.1007/s11606-017-3999-9.
898. National Academies of Sciences, Engineering, and Medicine. 2016. Accounting for social risk factors in Medicare payment: Identifying social risk factors. Washington, DC: The National Academies Press.
Back to Citation899. IOM (Institute of Medicine). 2009. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: The National Academies Press.
Back to Citation900. Guerino, P. and James, C. Race, Ethnicity, and Language Preference in the Health Insurance Marketplaces 2017 Open Enrollment Period. Centers for Medicare & Medicaid Services, Office of Minority Health. Data Highlight: Volume 7—April 2017. Available at: https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Data-Highlight-Race-Ethnicity-and-Language-Preference-Marketplace.pdf.
Back to Citation901. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National action plan to improve health literacy. Washington (DC): Author; 2010.
Back to Citation902. National Academies of Sciences, Engineering, and Medicine. 2016. Accounting for social risk factors in Medicare payment: Identifying social risk factors. Washington, DC: The National Academies Press.
Back to Citation903. Social Determinants of Health. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. (February 2019).
Back to Citation904. U.S. Department of Health & Human Services, Office of the Assistant Secretary for Planning and Evaluation. Report to Congress: Social Risk Factors and Performance Under Medicare's Value-Based Purchasing Programs. Available at: https://aspe.hhs.gov/pdf-report/report-congress-social-risk-factors-and-performance-under-medicares-value-based-purchasing-programs. Washington, DC: 2016.
Back to Citation905. Morris, N.S., MacLean, C.D., Chew, L.D., & Littenberg, B. (2006). The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC family practice, 7, 21. doi:10.1186/1471-2296-7-21.
906. Brice, J.H., Foster, M.B., Principe, S., Moss, C., Shofer, F.S., Falk, R.J., Ferris, M.E., DeWalt, D.A. (2013). Single-item or two-item literacy screener to predict the S-TOFHLA among adult hemodialysis patients. Patient Educ Couns. 94(1):71-5.
Back to Citation907. University of Miami, School of Nursing & Health Studies, Center of Excellence for Health Disparities Research. Test of Functional Health Literacy in Adults (TOFHLA). (March 2019). Available from: https://elcentro.sonhs.miami.edu/research/measures-library/tofhla/index.html.
Back to Citation908. Nurss, J.R., Parker, R.M., Williams, M.V., &Baker, D.W. David W. (2001). TOFHLA. Peppercorn Books & Press. Available from: http://www.peppercornbooks.com/catalog/information.php?info_id=5.
Back to Citation909. Hudson, S., Rikard, R.V., Staiculescu, I. & Edison, K. (2017). Improving health and the bottom line: The case for health literacy. In Building the case for health literacy: Proceedings of a workshop. Washington, DC: The National Academies Press.
Back to Citation910. National Academies of Sciences, Engineering, and Medicine. 2016. Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors. Washington, DC: The National Academies Press.
Back to Citation911. Syed, S.T., Gerber, B.S., and Sharp, L.K. (2013). Traveling Towards Disease: Transportation Barriers to Health Care Access. J Community Health. 38(5): 976-993.
Back to Citation912. Health Research & Educational Trust. (2017, November). Social determinants of health series: Transportation and the role of hospitals. Chicago, IL. Available at: www.aha.org/transportation.www.aha.org/transportation.
Back to Citation913. Health Research & Educational Trust. (2017, November). Social determinants of health series: Transportation and the role of hospitals. Chicago, IL. Available at: www.aha.org/transportation.
Back to Citation914. Northwestern University. (2017). PROMIS Item Bank v. 1.0—Emotional Distress—Anger—Short Form 1.
Back to Citation915. Tomaka, J., Thompson, S., and Palacios, R. (2006). The Relation of Social Isolation, Loneliness, and Social Support to Disease Outcomes Among the Elderly. J of Aging and Health. 18(3): 359-384.
916. Social Connectedness and Engagement Technology for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide. (2019). Leading Age. Available at: https://www.leadingage.org/white-papers/social-connectedness-and-engagement-technology-long-term-and-post-acute-care-primer-and#1.1.
Back to Citation917. Landeiro, F., Barrows, P., Nuttall Musson, E., Gray, A.M., and Leal, J. (2017). Reducing Social Loneliness in Older People: A Systematic Review Protocol. BMJ Open. 7(5): e013778.
918. Ong, A.D., Uchino, B.N., and Wethington, E. (2016). Loneliness and Health in Older Adults: A Mini-Review and Synthesis. Gerontology. 62:443-449.
919. Leigh-Hunt, N., Bagguley, D., Bash, K., Turner, V., Turnbull, S., Valtorta, N., and Caan, W. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 152:157-171.
Back to Citation920. Northwestern University. (2017). PROMIS Item Bank v. 1.0—Emotional Distress—Anger—Short Form 1.
Back to Citation921. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/FAQs.pdf.
Back to Citation2. https://protect2.fireeye.com/url?k=6e2af5a1-327ffcb2-6e2ac49e-0cc47adb5650-387d438bf4672a83&u=https://ecqi.healthit.gov/pre-rulemaking-eh-cah-ecqms.
Back to Citation922. Measure specifications for the Safe Use of Opioids—Concurrent Prescribing eCQM are available at: https://ecqi.healthit.gov/ecqm/measures/cms506v1.
Back to Citation923. https://ecqi.healthit.gov/content/about-ecqi.
Back to Citation924. U.S. Bureau of Labor Statistics. Occupational Outlook Handbook, Medical Records and Health Information Technicians. Available at: https://www.bls.gov/ooh/healthcare/medical-records-and-health-information-technicians.htm.
Back to Citation925. We note that in section VIII.A.9.d.(4). of the preamble of this final rule we are finalizing that, beginning with the CY 2022 reporting period, hospitals must report data on the Safe Use of Opioids—Concurrent Prescribing eCQM as one of the four required eCQMs.
Back to Citation926. In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38505), we finalized an hourly wage estimate of $18.29 per hour, plus 100 percent overhead and fringe benefits, for the PCHQR Program using Bureau of Labor Statistics information.
Back to Citation927. Occupational Employment and Wages. Available at: https://www.bls.gov/ooh/healthcare/medical-records-and-health-information-technicians.htm.
Back to Citation928. In the FY 2019 IPPS/LTCH PPS final rule (83 FR 41697), we finalized an hourly wage estimate of $18.29 per hour, plus 100 percent overhead and fringe benefits, for the HAC Reduction Program using Bureau of Labor Statistics information.
Back to Citation929. Occupational Employment and Wages. Available at: https://www.bls.gov/ooh/healthcare/medical-records-and-health-information-technicians.htm.
Back to Citation930. Occupational Employment and Wages. Available at: https://www.bls.gov/ooh/healthcare/medical-records-and-health-information-technicians.htm.
Back to Citation931. https://www.bls.gov/oes/2017/may/oes231011.htm.
Back to Citation932. As discussed in section X.B.3.d. of the preamble of this final rule, because the HWR claims-only measure is calculated using data that are already reported to the Medicare program for payment purposes, we do not anticipate that removing the HWR claims-only measure will decrease our previously finalized burden estimates. We believe there are no other changes in costs for hospitals associated with removal of this measure.
Back to CitationBILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
[FR Doc. 2019-16762 Filed 8-2-19; 4:15 pm]
BILLING CODE 4120-01-P
