AGENCY:
Centers for Medicare & Medicaid Services (CMS), HHS.
ACTION:
Final rule with comment period.
SUMMARY:
This final rule with comment period revises the Medicare hospital outpatient prospective payment system (OPPS) and the Medicare ambulatory surgical center (ASC) payment system for Calendar Year 2020 based on our continuing experience with these systems. In this final rule with comment period, we describe the changes to the amounts and factors used to determine the payment rates for Medicare services paid under the OPPS and those paid under the ASC payment system. Also, this final rule with comment period updates and refines the requirements for the Hospital Outpatient Quality Reporting (OQR) Program and the ASC Quality Reporting (ASCQR) Program. In addition, this final rule with comment period establishes a process and requirements for prior authorization for certain covered outpatient department services; revise the conditions for coverage of organ procurement organizations; and revise the regulations to allow grandfathered children's hospitals-within-hospitals to increase the number of beds without resulting in the loss of grandfathered status; and provides notice of the closure of two teaching hospitals and the opportunity to apply for available slots for purposes of indirect medical education (IME) and direct graduate medical education (DGME) payments.
DATES:
Effective date: This final rule is effective on January 1, 2020.
Comment period: To be assured consideration, comments on the payment classifications assigned to the interim APC assignments and/or status indicators of new or replacement Level II HCPCS codes in this final rule with comment period must be received at one of the addresses provided in the ADDRESSES section no later than 5 p.m. EST on December 2, 2019.
ADDRESSES:
In commenting, please refer to file code CMS-1717-FC when commenting on the issues in this final rule with comment period. Because of staff and resource limitations, we cannot accept comments by facsimile (FAX) transmission.
Comments, including mass comment submissions, must be submitted in one of the following three ways (please choose only one of the ways listed):
1. Electronically. You may (and we encourage you to) submit electronic comments on this regulation to http://www.regulations.gov. Follow the instructions under the “submit a comment” tab.
2. By regular mail. You may mail written comments to the following address ONLY: Centers for Medicare & Medicaid Services, Department of Health and Human Services, Attention: CMS-1717-FC, P.O. Box 8013, Baltimore, MD 21244-1850.
Please allow sufficient time for mailed comments to be received before the close of the comment period.
3. By express or overnight mail. You may send written comments via express or overnight mail to the following address ONLY: Centers for Medicare & Medicaid Services, Department of Health and Human Services, Attention: CMS-1717-FC, Mail Stop C4-26-05, 7500 Security Boulevard, Baltimore, MD 21244-1850.
b. For delivery in Baltimore, MD—Centers for Medicare & Medicaid Services, Department of Health and Human Services, 7500 Security Boulevard, Baltimore, MD 21244-1850.
For information on viewing public comments, we refer readers to the beginning of the SUPPLEMENTARY INFORMATION section.
FOR FURTHER INFORMATION CONTACT:
2-Midnight Rule (Short Inpatient Hospital Stays), contact Lela Strong-Holloway via email Lela.Strong@cms.hhs.gov or at 410-786-3213.
Advisory Panel on Hospital Outpatient Payment (HOP Panel), contact the HOP Panel mailbox at APCPanel@cms.hhs.gov.
Ambulatory Surgical Center (ASC) Payment System, contact Scott Talaga via email Scott.Talaga@cms.hhs.gov or at 410-786-4142 or Mitali Dayal via email Mitali.Dayal2@cms.hhs.gov or at 410-786-4329.
Ambulatory Surgical Center Quality Reporting (ASCQR) Program Administration, Validation, and Reconsideration Issues, contact Anita Bhatia via email Anita.Bhatia@cms.hhs.gov or at 410-786-7236.
Ambulatory Surgical Center Quality Reporting (ASCQR) Program Measures, contact Nicole Hewitt via email Nicole.Hewitt@cms.hhs.gov or at 410-786-7778.
Blood and Blood Products, contact Josh McFeeters via email Joshua.McFeeters@cms.hhs.gov or at 410-786-9732.
Cancer Hospital Payments, contact Scott Talaga via email Scott.Talaga@cms.hhs.gov or at 410-786-4142.
CMS Web Posting of the OPPS and ASC Payment Files, contact Chuck Braver via email Chuck.Braver@cms.hhs.gov or at 410-786-6719.
Control for Unnecessary Increases in Volume of Outpatient Services, contact Elise Barringer via email Elise.Barringer@cms.hhs.gov or at 410-786-9222.
Composite APCs (Low Dose Brachytherapy and Multiple Imaging), contact Elise Barringer via email Elise.Barringer@cms.hhs.gov or at 410-786-9222.
Comprehensive APCs (C-APCs), contact Lela Strong-Holloway via email Lela.Strong@cms.hhs.gov or at 410-786-3213, or Mitali Dayal via email at Mitali.Dayal2@cms.hhs.gov or at 410-786-4329.
CPT and Level II HCPCS Codes, contact Marjorie Baldo via email Marjorie.Baldo@cms.hhs.gov or at 410-786-4617.
Grandfathered Children's Hospitals-within-Hospitals, contact Michele Hudson via email Michele.Hudson@cms.hhs.gov or 410-786-4487.
Hospital Cost Reporting and Chargemaster Comment Solicitation, contact Dr. Terri Postma at 410-786-4169.
Hospital Outpatient Quality Reporting (OQR) Program Administration, Validation, and Reconsideration Issues, contact Anita Bhatia via email Anita.Bhatia@cms.hhs.gov or at 410-786-7236.
Hospital Outpatient Quality Reporting (OQR) Program Measures, contact Vinitha Meyyur via email Vinitha.Meyyur@cms.hhs.gov or at 410-786-8819.
Hospital Outpatient Visits (Emergency Department Visits and Critical Care Visits), contact Elise Barringer via email Elise.Barringer@cms.hhs.gov or at 410-786-9222.
Inpatient Only (IPO) Procedures List, contact Lela Strong-Holloway via email Lela.Strong@cms.hhs.gov or at 410-786-3213, or Au'Sha Washington via email at Ausha.Washington@cms.hhs.gov or at 410-786-3736.
New Technology Intraocular Lenses (NTIOLs), contact Scott Talaga via email Scott.Talaga@cms.hhs.gov or at 410-786-4142.
No Cost/Full Credit and Partial Credit Devices, contact Scott Talaga via email Scott.Talaga@cms.hhs.gov or at 410-786-4142.
Notice of Closure of Two Teaching Hospitals and Opportunity to Apply for Available Slots, contact Michele Hudson via email Michele.Hudson@cms.hhs.gov or 410-786-4487.
OPPS Brachytherapy, contact Scott Talaga via email Scott.Talaga@cms.hhs.gov or at 410-786-4142.
OPPS Data (APC Weights, Conversion Factor, Copayments, Cost-to-Charge Ratios (CCRs), Data Claims, Geometric Mean Calculation, Outlier Payments, and Wage Index), contact Erick Chuang via email Erick.Chuang@cms.hhs.gov or at 410-786-1816, or Scott Talaga via email Scott.Talaga@cms.hhs.gov or at 410-786-4142, or Josh McFeeters via email at Joshua.McFeeters@cms.hhs.gov or at 410-786-9732.
OPPS Drugs, Radiopharmaceuticals, Biologicals, and Biosimilar Products, contact Josh McFeeters via email Joshua.McFeeters@cms.hhs.gov or at 410-786-9732.
OPPS New Technology Procedures/Services, contact the New Technology APC mailbox at NewTechAPCapplications@cms.hhs.gov.
OPPS Packaged Items/Services, contact Lela Strong-Holloway via email Lela.Strong@cms.hhs.gov or at 410-786-3213, or Mitali Dayal via email at Mitali.Dayal2@cms.hhs.gov or at 410-786-4329.
OPPS Pass-Through Devices, contact the Device Pass-Through mailbox at DevicePTapplications@cms.hhs.gov.
OPPS Status Indicators (SI) and Comment Indicators (CI), contact Marina Kushnirova via email Marina.Kushnirova@cms.hhs.gov or at 410-786-2682.
Organ Procurement Organization (OPO) Conditions for Coverage (CfCs), contact Alpha-Banu Wilson via email at AlphaBanu.Wilson@cms.hhs.gov or at 410-786-8687, or Diane Corning via email at Diane.Corning@cms.hhs.gov or at 410-786-8486.
Partial Hospitalization Program (PHP) and Community Mental Health Center (CMHC) Issues, contact the PHP Payment Policy Mailbox at PHPPaymentPolicy@cms.hhs.gov.
Prior Authorization Process and Requirements for Certain Hospital Outpatient Department Services, contact Thomas Kessler via email at Thomas.Kessler@cms.hhs.gov or at 410-786-1991.
Rural Hospital Payments, contact Josh McFeeters via email at Joshua.McFeeters@cms.hhs.gov or at 410-786-9732.
Skin Substitutes, contact Josh McFeeters via email Joshua.McFeeters@cms.hhs.gov or at 410-786-9732.
Supervision of Outpatient Therapeutic Services in Hospitals and CAHs, contact Josh McFeeters via email Joshua.McFeeters@cms.hhs.gov or at 410-786-9732.
All Other Issues Related to Hospital Outpatient and Ambulatory Surgical Center Payments Not Previously Identified, contact Elise Barringer via email Elise.Barringer@cms.hhs.gov or at 410-786-9222.
SUPPLEMENTARY INFORMATION:
Inspection of Public Comments: All comments received before the close of the comment period are available for viewing by the public, including any personally identifiable or confidential business information that is included in a comment. We post all comments received before the close of the comment period on the following website as soon as possible after they have been received: http://www.regulations.gov/. Follow the search instructions on that website to view public comments.
Addenda Available Only Through the Internet on the CMS Website
In the past, a majority of the Addenda referred to in our OPPS/ASC proposed and final rules were published in the Federal Register as part of the annual rulemakings. However, beginning with the CY 2012 OPPS/ASC proposed rule, all of the Addenda no longer appear in the Federal Register as part of the annual OPPS/ASC proposed and final rules to decrease administrative burden and reduce costs associated with publishing lengthy tables. Instead, these Addenda are published and available only on the CMS website. The Addenda relating to the OPPS are available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html. The Addenda relating to the ASC payment system are available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
Current Procedural Terminology (CPT) Copyright Notice
Throughout this final rule with comment period, we use CPT codes and descriptions to refer to a variety of services. We note that CPT codes and descriptions are copyright 2018 American Medical Association. All Rights Reserved. CPT is a registered trademark of the American Medical Association (AMA). Applicable Federal Acquisition Regulations (FAR and Defense Federal Acquisition Regulations (DFAR) apply.
Table of Contents
I. Summary and Background
A. Executive Summary of This Document
B. Legislative and Regulatory Authority for the Hospital OPPS
C. Excluded OPPS Services and Hospitals
D. Prior Rulemaking
E. Advisory Panel on Hospital Outpatient Payment (the HOP Panel or the Panel)
F. Public Comments Received in Response to the CY 2020 OPPS/ASC Proposed Rule
G. Public Comments Received on the CY 2019 OPPS/ASC Final Rule With Comment Period
II. Updates Affecting OPPS Payments
A. Recalibration of APC Relative Payment Weights
B. Conversion Factor Update
C. Wage Index Changes
D. Statewide Average Default Cost-to-Charge Ratios (CCRs)
E. Adjustment for Rural Sole Community Hospitals (SCHs) and Essential Access Community Hospitals (EACHs) Under Section 1833(t)(13)(B) of the Act for CY 2020
F. Payment Adjustment for Certain Cancer Hospitals for CY 2020
G. Hospital Outpatient Outlier Payments
H. Calculation of an Adjusted Medicare Payment From the National Unadjusted Medicare Payment
I. Beneficiary Copayments
III. OPPS Ambulatory Payment Classification (APC) Group Policies
A. OPPS Treatment of New and Revised HCPCS Codes
B. OPPS Changes—Variations Within APCs
C. New Technology APCs
D. APC-Specific Policies
IV. OPPS Payment for Devices
A. Pass-Through Payments for Devices
B. Device-Intensive Procedures
V. OPPS Payment Changes for Drugs, Biologicals, and Radiopharmaceuticals
A. OPPS Transitional Pass-Through Payment for Additional Costs of Drugs, Biologicals, and Radiopharmaceuticals
B. OPPS Payment for Drugs, Biologicals, and Radiopharmaceuticals Without Pass-Through Payment Status
VI. Estimate of OPPS Transitional Pass-Through Spending for Drugs, Biologicals, Radiopharmaceuticals, and Devices
A. Background
B. Estimate of Pass-Through Spending
VII. OPPS Payment for Hospital Outpatient Visits and Critical Care Services
VIII. Payment for Partial Hospitalization Services
A. Background
B. PHP APC Update for CY 2020
C. Outlier Policy for CMHCs
D. Update to PHP Allowable HCPCS Codes
IX. Procedures That Will Be Paid Only as Inpatient Procedures
A. Background
B. Changes to the Inpatient Only (IPO) List
X. Nonrecurring Policy Changes
A. Changes in the Level of Supervision of Outpatient Therapeutic Services in Hospitals and Critical Access Hospitals (CAHs)
B. Short Inpatient Hospital Stays
C. Method To Control Unnecessary Increases in the Volume of Clinic Visit Services Furnished in Excepted Off-Campus Provider-Based Departments (PBDs)
XI. CY 2020 OPPS Payment Status and Comment Indicators
A. CY 2020 OPPS Payment Status Indicator Definitions
B. CY 2020 Comment Indicator Definitions
XII. MedPAC Recommendations
A. OPPS Payment Rates Update
B. ASC Conversion Factor Update
C. ASC Cost Data
XIII. Updates to the Ambulatory Surgical Center (ASC) Payment System
A. Background
B. ASC Treatment of New and Revised Codes
C. Update to the List of ASC Covered Surgical Procedures and Covered Ancillary Services
D. Update and Payment for ASC Covered Surgical Procedures and Covered Ancillary Services
E. New Technology Intraocular Lenses (NTIOLs)
F. ASC Payment and Comment Indicators
G. Calculation of the ASC Payment Rates and the ASC Conversion Factor
XIV. Requirements for the Hospital Outpatient Quality Reporting (OQR) Program
A. Background
B. Hospital OQR Program Quality Measures
C. Administrative Requirements
D. Form, Manner, and Timing of Data Submitted for the Hospital OQR Program
E. Payment Reduction for Hospitals That Fail To Meet the Hospital OQR Program Requirements for the CY 2020 Payment Determination
XV. Requirements for the Ambulatory Surgical Center Quality Reporting (ASCQR) Program
A. Background
B. ASCQR Program Quality Measures
C. Administrative Requirements
D. Form, Manner, and Timing of Data Submitted for the ASCQR Program
E. Payment Reduction for ASCs That Fail To Meet the ASCQR Program Requirements
XVI. Requirements for Hospitals To Make Public a List of Their Standard Charges and Request for Information (RFI): Quality Measurement Relating to Price Transparency for Improving Beneficiary Access to Provider and Supplier Charge Information
XVII. Organ Procurement Organizations (OPOs) Conditions for Coverage (CfCs): Revision of the Definition of “Expected Donation Rate”
A. Background
B. Revision of the Definition of “Expected Donation Rate”
C. Request for Information Regarding Potential Changes to the Organ Procurement Organization and Transplant Center Regulations
XVIII. Clinical Laboratory Fee Schedule: Potential Revisions to the Laboratory Date of Service Policy
A. Background on the Medicare Part B Laboratory Date of Service Policy
B. Medicare DOS Policy and the “14-Day Rule”
C. Billing and Payment for Laboratory Services Under the OPPS
D. ADLTs Under the New Private Payor Rate-Based CLFS
E. Additional Laboratory DOS Policy Exception for the Hospital Outpatient Setting
F. Potential Revisions to Laboratory DOS Policy and Request for Public Comments
XIX. Prior Authorization Process and Requirements for Certain Hospital Outpatient Department (OPD) Services
A. Background
B. Prior Authorization Process for Certain OPD Services
C. List of Outpatient Department Services Requiring Prior Authorization
XX. Comments Received in Response to Comment Solicitation on Cost Reporting, Maintenance of Hospital Chargemasters, and Related Medicare Payment Issues
XXI. Changes to Requirements for Grandfathered Children's Hospitals-Within-Hospitals (HwHs)
XXII. Notice of Closure of Two Teaching Hospitals and Opportunity To Apply for Available Slots
XXIII. Files Available to the Public via the Internet
XXIV. Collection of Information Requirements
A. Statutory Requirement for Solicitation of Comments
B. ICRs for the Hospital OQR Program
C. ICRs for the ASCQR Program
D. ICRs for Revision of the Definition of “Expected Donation Rate” for Organ Procurement Organizations
E. ICR for Prior Authorization Process and Requirements for Certain Hospital Outpatient Department (OPD) Services
F. Potential Revisions to Laboratory Date of Service (DOS) Policy
G. Total Reduction in Burden Hours and in Costs
XXV. Response to Comments
XXVI. Economic Analyses
A. Statement of Need
B. Overall Impact for the Provisions of This Final Rule
C. Detailed Economic Analyses
D. Effects of Prior Authorization Process and Requirements for Certain Hospital Outpatient Department (OPD) Services
E. Effects of Requirement Relating to Changes in the Definition of Expected Donation Rate for Organ Procurement Organizations
F. Potential Revisions to the Laboratory Date of Service Policy
G. Effect of Changes to Requirements for Grandfathered Children's Hospitals-Within-Hospitals (HwHs)
H. Regulatory Review Costs
I. Regulatory Flexibility Act (RFA) Analysis
J. Unfunded Mandates Reform Act Analysis
K. Reducing Regulation and Controlling Regulatory Costs
L. Conclusion
XXVII. Federalism Analysis
Regulation Text
I. Summary and Background
A. Executive Summary of This Document
1. Purpose
In this final rule with comment period, we are updating the payment policies and payment rates for services furnished to Medicare beneficiaries in hospital outpatient departments (HOPDs) and ambulatory surgical centers (ASCs), beginning January 1, 2020. Section 1833(t) of the Social Security Act (the Act) requires us to annually review and update the payment rates for services payable under the Hospital Outpatient Prospective Payment System (OPPS). Specifically, section 1833(t)(9)(A) of the Act requires the Secretary to review certain components of the OPPS not less often than annually, and to revise the groups, the relative payment weights, and the wage and other adjustments that take into account changes in medical practices, changes in technologies, and the addition of new services, new cost data, and other relevant information and factors. In addition, under section 1833(i) of the Act, we annually review and update the ASC payment rates. This final rule with comment period also includes additional policy changes made in accordance with our experience with the OPPS and the ASC payment system. We describe these and various other statutory authorities in the relevant sections of this final rule with comment period. In addition, this final rule with comment period updates and refines the requirements for the Hospital Outpatient Quality Reporting (OQR) Program and the ASC Quality Reporting (ASCQR) Program.
In this final rule with comment period, we establish a process and requirements for prior authorization for certain covered outpatient department services; revise the conditions for coverage for organ procurement organizations; and revise the regulations to allow grandfathered children's hospitals-within-hospitals to increase the number of beds without resulting in the loss of grandfathered status.
2. Summary of the Major Provisions
- OPPS Update: For CY 2020, we are increasing the payment rates under the OPPS by an Outpatient Department (OPD) fee schedule increase factor of 2.6 percent. This increase factor is based on the final hospital inpatient market basket percentage increase of 3.0 percent for inpatient services paid under the hospital inpatient prospective payment system (IPPS), minus the multifactor productivity (MFP) adjustment required by the Affordable Care Act of 0.4 percentage point. Based on this update, we estimate that total payments to OPPS providers (including beneficiary cost-sharing and estimated changes in enrollment, utilization, and case-mix) for calendar year (CY) 2020 will be approximately $79.0 billion, an increase of approximately $6.3 billion compared to estimated CY 2019 OPPS payments.
We are continuing to implement the statutory 2.0 percentage point reduction in payments for hospitals failing to meet the hospital outpatient quality reporting requirements, by applying a reporting factor of 0.981 to the OPPS payments and copayments for all applicable services.
- 2-Midnight Rule (Short Inpatient Hospital Stays): For CY 2020, we are establishing a 2-year exemption from Beneficiary and Family-Centered Care Quality Improvement Organizations (BFCC-QIOs) referrals to Recovery Audit Contractors (RACs) and RAC reviews for “patient status” (that is, site-of-service) for procedures that are removed from the inpatient only (IPO) list under the OPPS beginning on January 1, 2020.
- Comprehensive APCs: For CY 2020, we are creating two new comprehensive APCs (C-APCs). These new C-APCs include the following: C-APC 5182 (Level 2 Vascular Procedures) and C-APC 5461 (Level 1 Neurostimulator and Related Procedures). This increases the total number of C-APCs to 67.
- Changes to the Inpatient Only (IPO) List: For CY 2020, we are removing Total Hip Arthroplasty, six spinal procedure codes, and five anesthesia codes from the inpatient only list.
- Method to Control Unnecessary Increases in the Volume of Clinic Visit Services Furnished in Excepted Off-Campus Provider-Based Departments (PBDs): For CY 2020, we are completing the phase-in of the reduction in payment for the clinic visit services described by HCPCS code G0463 furnished in expected off-campus provider based departments as a method to control unnecessary increases in the volume of this service. We acknowledge that the district court vacated the volume control policy for CY 2019 and we are working to ensure affected 2019 claims for clinic visits are paid consistent with the court's order. We do not believe it is appropriate at this time to make a change to the second year of the two-year phase-in of the clinic visit policy. The government has appeal rights, and is still evaluating the rulings and considering, at the time of this writing, whether to appeal from the final judgment.
- Device Pass-Through Payment Applications: For CY 2020, we evaluated seven applications for device pass-through payments and based on public comments received, we are approving four of these applications for device pass-through payment status. Additionally, we are approving an additional application that was not discussed in the CY 2020 OPPS/ASC proposed rule, but has received a Breakthrough Devices designation from the Food and Drug Administration (FDA) and qualifies for the alternative pathway to the OPPS device pass-through substantial clinical improvement criterion.
- Changes to Substantial Clinical Improvement Criterion: For CY 2020, we are finalizing an alternative pathway to the substantial clinical improvement criterion for devices approved under the FDA Breakthrough Devices Program to qualify for device pass-through status beginning with determinations effective on or after January 1, 2020.
- Cancer Hospital Payment Adjustment: For CY 2020, we are continuing to provide additional payments to cancer hospitals so that a cancer hospital's payment-to-cost ratio (PCR) after the additional payments is equal to the weighted average PCR for the other OPPS hospitals using the most recently submitted or settled cost report data. However, section 16002(b) of the 21st Century Cures Act requires that this weighted average PCR be reduced by 1.0 percentage point. Based on the data and the required 1.0 percentage point reduction, we are providing that a target PCR of 0.89 will be used to determine the CY 2020 cancer hospital payment adjustment to be paid at cost report settlement. That is, the payment adjustments will be the additional payments needed to result in a PCR equal to 0.89 for each cancer hospital.
- Rural Adjustment: For 2020 and subsequent years, we are continuing the 7.1 percent adjustment to OPPS payments for certain rural SCHs, including essential access community hospitals (EACHs). We intend to continue the 7.1 percent adjustment for future years in the absence of data to suggest a different percentage adjustment should apply.
- 340B-Acquired Drugs: We are continuing to pay ASP-22.5 percent for 340B-acquired drugs including when furnished in nonexcepted off-campus PBDs paid under the PFS. In light of ongoing litigation, we also summarized comments received on a potential remedy for 2018 and 2019. CMS announced in the Federal Register (84 FR 51590) its intent to conduct a 340B hospital survey to collect drug acquisition cost data for CY 2018 and 2019. Such survey data may be used in setting the Medicare payment amount for drugs acquired by 340B hospitals for cost years going forward, and also may be used to devise a remedy for prior years in the event of an adverse decision on appeal. In the event 340B hospital survey data are not used to devise a remedy, we intend to consider the suggestions commenters submitted in response to the comment solicitation in the proposed rule to propose a remedy in the CY 2021 OPPS/ASC proposed rule.
- ASC Payment Update: For CYs 2019 through 2023, we adopted a policy to update the ASC payment system using the hospital market basket update. Using the hospital market basket methodology, for CY 2020, we are increasing payment rates under the ASC payment system by 2.6 percent for ASCs that meet the quality reporting requirements under the ASCQR Program. This increase is based on a hospital market basket percentage increase of 3.0 percent minus a proposed multifactor productivity adjustment required by the Affordable Care Act of 0.4 percentage point. Based on this update, we estimate that total payments to ASCs (including beneficiary cost-sharing and estimated changes in enrollment, utilization, and case-mix) for CY 2020 will be approximately $4.96 billion, an increase of approximately $230 million compared to estimated CY 2019 Medicare payments.
- Changes to the List of ASC Covered Surgical Procedures: For CY 2020, we are adding several procedures to the ASC list of covered surgical procedures. Additions to the list include a total knee arthroplasty procedure, a mosaicplasty procedure, as well as six coronary intervention procedures, as well as 12 surgical procedures with new CPT codes for CY 2020.
- Changes to the Level of Supervision of Outpatient Therapeutic Services in Hospitals and Critical Access Hospitals: For CY 2020, we are changing the minimum required level of supervision from direct supervision to general supervision for all hospital outpatient therapeutic services provided by all hospitals and CAHs. This ensures a standard minimum level of supervision for each hospital outpatient service furnished incident to a physician's service.
- Hospital Outpatient Quality Reporting (OQR) Program: For the Hospital OQR Program, we are removing OP-33: External Beam Radiotherapy for Bone Metastases for the CY 2022 payment determination and subsequent years with modification.
- Ambulatory Surgical Center Quality Reporting (ASCQR) Program: For the ASCQR Program, we are adopting one new measure, ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers, beginning with the CY 2024 payment determination and for subsequent years.
- Prior Authorization Process and Requirements for Certain Hospital Outpatient Department (OPD) Services: We are finalizing a prior authorization process using the authority at section 1833(t)(2)(F) of the Act as a method for controlling unnecessary increases in the volume of the following five categories of services: (1) Blepharoplasty, (2) botulinum toxin injections, (3) panniculectomy, (4) rhinoplasty, and (5) vein ablation.
- Organ Procurement Organizations (OPOs) Conditions for Coverage (CfCs) Revision of the Definition of “Expected Donation Rate.” We are revising the definition of “expected donation rate” that is included in the second outcome measure to match the Scientific Registry of Transplant Recipients (SRTR) definition. In conjunction with this change, we are also temporarily suspending the requirement that OPOs meet two of three outcome measures for the 2022 recertification cycle only.
- Request for Information Regarding Potential Changes to the Organ Procurement Organization and Transplant Center Regulations: We solicited public comments regarding what revisions may be appropriate for the current OPO CfCs and the current transplant center CoPs. In addition, we solicited public comments on two potential outcome measures for OPOs.
3. Summary of Costs and Benefits
In sections XXVI. and XXVII. of this final rule with comment period, we set forth a detailed analysis of the regulatory and federalism impacts that the changes will have on affected entities and beneficiaries. Key estimated impacts are described below.
a. Impacts of All OPPS Changes
Table 70 in section XXV.B of this final rule with comment period displays the distributional impact of all the OPPS changes on various groups of hospitals and CMHCs for CY 2020 compared to all estimated OPPS payments in CY 2019. We estimate that the policies in this final rule with comment period will result in a 1.3 percent overall increase in OPPS payments to providers. We estimate that total OPPS payments for CY 2020, including beneficiary cost-sharing, to the approximately 3,732 facilities paid under the OPPS (including general acute care hospitals, children's hospitals, cancer hospitals, and CMHCs) will increase by approximately $1.21 billion compared to CY 2019 payments, excluding our estimated changes in enrollment, utilization, and case-mix.
We estimated the isolated impact of our OPPS policies on CMHCs because CMHCs are only paid for partial hospitalization services under the OPPS. Continuing the provider-specific structure we adopted beginning in CY 2011, and basing payment fully on the type of provider furnishing the service, we estimate a 3.7 percent increase in CY 2020 payments to CMHCs relative to their CY 2019 payments.
b. Impacts of the Updated Wage Indexes
We estimate that our update of the wage indexes based on the FY 2020 IPPS proposed rule wage indexes will result in no estimated payment change for urban hospitals under the OPPS and an estimated increase of 0.7 percent for rural hospitals. These wage indexes include the continued implementation of the OMB labor market area delineations based on 2010 Decennial Census data, with updates, as discussed in section II.C. of this final rule with comment period.
c. Impacts of the Rural Adjustment and the Cancer Hospital Payment Adjustment
There are no significant impacts of our CY 2020 payment policies for hospitals that are eligible for the rural adjustment or for the cancer hospital payment adjustment. We are not making any change in policies for determining the rural hospital payment adjustments. While we are implementing the required reduction to the cancer hospital payment adjustment required by section 16002 of the 21st Century Cures Act for CY 2020, the target payment-to-cost ratio (PCR) for CY 2020 is 0.89, compared to 0.88 for CY 2019, and therefore has a slight impact on budget neutrality adjustments.
d. Impacts of the OPD Fee Schedule Increase Factor
For the CY 2020 OPPS/ASC, we are establishing an OPD fee schedule increase factor of 2.6 percent and applying that increase factor to the conversion factor for CY 2020. As a result of the OPD fee schedule increase factor and other budget neutrality adjustments, we estimate that urban hospitals will experience an increase of approximately 2.7 percent and that rural hospitals will experience an increase of 2.8 percent. Classifying hospitals by teaching status, we estimate nonteaching hospitals will experience an increase of 2.8 percent, minor teaching hospitals will experience an increase of 2.9 percent, and major teaching hospitals will experience an increase of 2.4 percent. We also classified hospitals by the type of ownership. We estimate that hospitals with voluntary ownership will experience an increase of 2.6 percent in payments, while hospitals with government ownership will experience an increase of 2.8 percent in payments. We estimate that hospitals with proprietary ownership will experience an increase of 3.2 percent in payments.
e. Impacts of the ASC Payment Update
For impact purposes, the surgical procedures on the ASC list of covered procedures are aggregated into surgical specialty groups using CPT and HCPCS code range definitions. The percentage change in estimated total payments by specialty groups under the CY 2020 payment rates, compared to estimated CY 2019 payment rates, generally ranges between an increase of 1 and 5 percent, depending on the service, with some exceptions. We estimate the impact of applying the hospital market basket update to ASC payment rates will increase payments by $230 million under the ASC payment system in CY 2020.
f. Impact of the Changes to the Hospital OQR Program
Across 3,300 hospitals participating in the Hospital OQR Program, we estimate that our requirements will result in the following changes to costs and burdens related to information collection for the Hospital OQR Program compared to previously adopted requirements: There is a net reduction of one measure reported by hospitals, which results in a minimal net reduction in burden of $21,379.
g. Impacts of the Revision of the Definition of “Expected Donation Rate” for Organ Procurement Organizations
We are finalizing our revision to the definition of “expected donation rate” used in the second outcome measure of the OPO CfCs at 42 CFR 486.318(a) and (b) to eliminate the potential for confusion in the OPO community due to different definitions of the same term; however, due to comments received on the CY 2020 OPPS/ASC proposed rule we are finalizing a policy that would not require all OPOs to meet the standards of the second outcome measure for the 2022 recertification cycle only. As a result, OPOs will only have to meet one of the remaining outcome measures, which may provide temporary relief for a small number of OPOs that, absent this waiver, might have faced de-certification and the appeal process due to only meeting one outcome measure.
For subsequent recertification cycles, all 58 OPOs will once again be required to meet two out of three outcome measures detailed in the OPO CfCs. The revised definition of “expected donation rate” used in the second outcome measure will not affect data collection or reporting by the OPTN and SRTR, nor their statistical evaluation of OPO performance; therefore, it will not result in any quantifiable financial impact.
B. Legislative and Regulatory Authority for the Hospital OPPS
When Title XVIII of the Act was enacted, Medicare payment for hospital outpatient services was based on hospital-specific costs. In an effort to ensure that Medicare and its beneficiaries pay appropriately for services and to encourage more efficient delivery of care, the Congress mandated replacement of the reasonable cost-based payment methodology with a prospective payment system (PPS). The Balanced Budget Act of 1997 (BBA) (Pub. L. 105-33) added section 1833(t) to the Act, authorizing implementation of a PPS for hospital outpatient services. The OPPS was first implemented for services furnished on or after August 1, 2000. Implementing regulations for the OPPS are located at 42 CFR parts 410 and 419.
The Medicare, Medicaid, and SCHIP Balanced Budget Refinement Act of 1999 (BBRA) (Pub. L. 106-113) made major changes in the hospital OPPS. The following Acts made additional changes to the OPPS: The Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 (BIPA) (Pub. L. 106-554); the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) (Pub. L. 108-173); the Deficit Reduction Act of 2005 (DRA) (Pub. L. 109-171), enacted on February 8, 2006; the Medicare Improvements and Extension Act under Division B of Title I of the Tax Relief and Health Care Act of 2006 (MIEA-TRHCA) (Pub. L. 109-432), enacted on December 20, 2006; the Medicare, Medicaid, and SCHIP Extension Act of 2007 (MMSEA) (Pub. L. 110-173), enacted on December 29, 2007; the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) (Pub. L. 110-275), enacted on July 15, 2008; the Patient Protection and Affordable Care Act (Pub. L. 111-148), enacted on March 23, 2010, as amended by the Health Care and Education Reconciliation Act of 2010 (Pub. L. 111-152), enacted on March 30, 2010 (these two public laws are collectively known as the Affordable Care Act); the Medicare and Medicaid Extenders Act of 2010 (MMEA, Pub. L. 111-309); the Temporary Payroll Tax Cut Continuation Act of 2011 (TPTCCA, Pub. L. 112-78), enacted on December 23, 2011; the Middle Class Tax Relief and Job Creation Act of 2012 (MCTRJCA, Pub. L. 112-96), enacted on February 22, 2012; the American Taxpayer Relief Act of 2012 (Pub. L. 112-240), enacted January 2, 2013; the Pathway for SGR Reform Act of 2013 (Pub. L. 113-67) enacted on December 26, 2013; the Protecting Access to Medicare Act of 2014 (PAMA, Pub. L. 113-93), enacted on March 27, 2014; the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 (Pub. L. 114-10), enacted April 16, 2015; the Bipartisan Budget Act of 2015 (Pub. L. 114-74), enacted November 2, 2015; the Consolidated Appropriations Act, 2016 (Pub. L. 114-113), enacted on December 18, 2015, the 21st Century Cures Act (Pub. L. 114-255), enacted on December 13, 2016; the Consolidated Appropriations Act, 2018 (Pub. L. 115-141), enacted on March 23, 2018; and the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (Pub. L. 115-271), enacted on October 24, 2018.
Under the OPPS, we generally pay for hospital Part B services on a rate-per-service basis that varies according to the APC group to which the service is assigned. We use the Healthcare Common Procedure Coding System (HCPCS) (which includes certain Current Procedural Terminology (CPT) codes) to identify and group the services within each APC. The OPPS includes payment for most hospital outpatient services, except those identified in section I.C. of this final rule with comment period. Section 1833(t)(1)(B) of the Act provides for payment under the OPPS for hospital outpatient services designated by the Secretary (which includes partial hospitalization services furnished by CMHCs), and certain inpatient hospital services that are paid under Medicare Part B.
The OPPS rate is an unadjusted national payment amount that includes the Medicare payment and the beneficiary copayment. This rate is divided into a labor-related amount and a nonlabor-related amount. The labor-related amount is adjusted for area wage differences using the hospital inpatient wage index value for the locality in which the hospital or CMHC is located.
All services and items within an APC group are comparable clinically and with respect to resource use, as required by section 1833(t)(2)(B) of the Act. In accordance with section 1833(t)(2)(B) of the Act, subject to certain exceptions, items and services within an APC group cannot be considered comparable with respect to the use of resources if the highest median cost (or mean cost, if elected by the Secretary) for an item or service in the APC group is more than 2 times greater than the lowest median cost (or mean cost, if elected by the Secretary) for an item or service within the same APC group (referred to as the “2 times rule”). In implementing this provision, we generally use the cost of the item or service assigned to an APC group.
For new technology items and services, special payments under the OPPS may be made in one of two ways. Section 1833(t)(6) of the Act provides for temporary additional payments, which we refer to as “transitional pass-through payments,” for at least 2 but not more than 3 years for certain drugs, biological agents, brachytherapy devices used for the treatment of cancer, and categories of other medical devices. For new technology services that are not eligible for transitional pass-through payments, and for which we lack sufficient clinical information and cost data to appropriately assign them to a clinical APC group, we have established special APC groups based on costs, which we refer to as New Technology APCs. These New Technology APCs are designated by cost bands which allow us to provide appropriate and consistent payment for designated new procedures that are not yet reflected in our claims data. Similar to pass-through payments, an assignment to a New Technology APC is temporary; that is, we retain a service within a New Technology APC until we acquire sufficient data to assign it to a clinically appropriate APC group.
C. Excluded OPPS Services and Hospitals
Section 1833(t)(1)(B)(i) of the Act authorizes the Secretary to designate the hospital outpatient services that are paid under the OPPS. While most hospital outpatient services are payable under the OPPS, section 1833(t)(1)(B)(iv) of the Act excludes payment for ambulance, physical and occupational therapy, and speech-language pathology services, for which payment is made under a fee schedule. It also excludes screening mammography, diagnostic mammography, and effective January 1, 2011, an annual wellness visit providing personalized prevention plan services. The Secretary exercises the authority granted under the statute to also exclude from the OPPS certain services that are paid under fee schedules or other payment systems. Such excluded services include, for example, the professional services of physicians and nonphysician practitioners paid under the Medicare Physician Fee Schedule (MPFS); certain laboratory services paid under the Clinical Laboratory Fee Schedule (CLFS); services for beneficiaries with end-stage renal disease (ESRD) that are paid under the ESRD prospective payment system; and services and procedures that require an inpatient stay that are paid under the hospital IPPS. In addition, section 1833(t)(1)(B)(v) of the Act does not include applicable items and services (as defined in subparagraph (A) of paragraph (21)) that are furnished on or after January 1, 2017 by an off-campus outpatient department of a provider (as defined in subparagraph (B) of paragraph (21). We set forth the services that are excluded from payment under the OPPS in regulations at 42 CFR 419.22.
Under § 419.20(b) of the regulations, we specify the types of hospitals that are excluded from payment under the OPPS. These excluded hospitals include:
- Critical access hospitals (CAHs);
- Hospitals located in Maryland and paid under Maryland's All-Payer or Total Cost of Care Model;
- Hospitals located outside of the 50 States, the District of Columbia, and Puerto Rico; and
- Indian Health Service (IHS) hospitals.
D. Prior Rulemaking
On April 7, 2000, we published in the Federal Register a final rule with comment period (65 FR 18434) to implement a prospective payment system for hospital outpatient services. The hospital OPPS was first implemented for services furnished on or after August 1, 2000. Section 1833(t)(9)(A) of the Act requires the Secretary to review certain components of the OPPS, not less often than annually, and to revise the groups, relative payment weights, and the wage and other adjustments that take into account changes in medical practices, changes in technologies, and the addition of new services, new cost data, and other relevant information and factors.
Since initially implementing the OPPS, we have published final rules in the Federal Register annually to implement statutory requirements and changes arising from our continuing experience with this system. These rules can be viewed on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices.html.
E. Advisory Panel on Hospital Outpatient Payment (the HOP Panel or the Panel)
1. Authority of the Panel
Section 1833(t)(9)(A) of the Act, as amended by section 201(h) of Public Law 106-113, and redesignated by section 202(a)(2) of Public Law 106-113, requires that we consult with an external advisory panel of experts to annually review the clinical integrity of the payment groups and their weights under the OPPS. In CY 2000, based on section 1833(t)(9)(A) of the Act, the Secretary established the Advisory Panel on Ambulatory Payment Classification Groups (APC Panel) to fulfill this requirement. In CY 2011, based on section 222 of the Public Health Service Act, which gives discretionary authority to the Secretary to convene advisory councils and committees, the Secretary expanded the panel's scope to include the supervision of hospital outpatient therapeutic services in addition to the APC groups and weights. To reflect this new role of the panel, the Secretary changed the panel's name to the Advisory Panel on Hospital Outpatient Payment (the HOP Panel or the Panel). The HOP Panel is not restricted to using data compiled by CMS, and in conducting its review, it may use data collected or developed by organizations outside the Department.
2. Establishment of the Panel
On November 21, 2000, the Secretary signed the initial charter establishing the Panel, and, at that time, named the APC Panel. This expert panel is composed of appropriate representatives of providers (currently employed full-time, not as consultants, in their respective areas of expertise) who review clinical data and advise CMS about the clinical integrity of the APC groups and their payment weights. Since CY 2012, the Panel also is charged with advising the Secretary on the appropriate level of supervision for individual hospital outpatient therapeutic services. The Panel is technical in nature, and it is governed by the provisions of the Federal Advisory Committee Act (FACA). The current charter specifies, among other requirements, that the Panel—
- May advise on the clinical integrity of Ambulatory Payment Classification (APC) groups and their associated weights;
- May advise on the appropriate supervision level for hospital outpatient services;
- Continues to be technical in nature;
- Is governed by the provisions of the FACA;
- Has a Designated Federal Official (DFO); and
- Is chaired by a Federal Official designated by the Secretary.
The Panel's charter was amended on November 15, 2011, renaming the Panel and expanding the Panel's authority to include supervision of hospital outpatient therapeutic services and to add critical access hospital (CAH) representation to its membership. The Panel's charter was also amended on November 6, 2014 (80 FR 23009), and the number of members was revised from up to 19 to up to 15 members. The Panel's current charter was approved on November 19, 2018, for a 2-year period (84 FR 26117).
The current Panel membership and other information pertaining to the Panel, including its charter, Federal Register notices, membership, meeting dates, agenda topics, and meeting reports, can be viewed on the CMS website at: https://www.cms.gov/Regulations-and-Guidance/Guidance/FACA/AdvisoryPanelonAmbulatoryPaymentClassificationGroups.html.
3. Panel Meetings and Organizational Structure
The Panel has held many meetings, with the last meeting taking place on August 19, 2019. Prior to each meeting, we publish a notice in the Federal Register to announce the meeting and, when necessary, to solicit nominations for Panel membership, to announce new members, and to announce any other changes of which the public should be aware. Beginning in CY 2017, we have transitioned to one meeting per year (81 FR 31941). Further information on the 2019 summer meeting can be found in the meeting notice titled “Medicare Program: Announcement of the Advisory Panel on Hospital Outpatient Payment (the Panel) Meeting on August 19 through 20, 2019” (84 FR 26117).
In addition, the Panel has established an operational structure that, in part, currently includes the use of three subcommittees to facilitate its required review process. The three current subcommittees include the following:
- APC Groups and Status Indicator Assignments Subcommittee, which advises the Panel on the appropriate status indicators to be assigned to HCPCS codes, including but not limited to whether a HCPCS code or a category of codes should be packaged or separately paid, as well as the appropriate APC assignment of HCPCS codes regarding services for which separate payment is made;
- Data Subcommittee, which is responsible for studying the data issues confronting the Panel and for recommending options for resolving them; and
- Visits and Observation Subcommittee, which reviews and makes recommendations to the Panel on all technical issues pertaining to observation services and hospital outpatient visits paid under the OPPS.
Each of these subcommittees was established by a majority vote from the full Panel during a scheduled Panel meeting, and the Panel recommended at the August 19, 2019, meeting that the subcommittees continue. We accepted this recommendation.
For discussions of earlier Panel meetings and recommendations, we refer readers to previously published OPPS/ASC proposed and final rules, the CMS website mentioned earlier in this section, and the FACA database at http://facadatabase.gov.
Comment: One commenter supported CMS' extension of the HOP Panel meeting presentation submission deadline when there is a truncated submittal timeframe due to delayed publication of the OPPS/ASC proposed rule. However, to avoid the need to modify the submission deadline in the future, the commenter suggested that CMS revise the submission deadline in the Federal Register notice from a firm date to a fluid 21 days from the proposed rule display date to avoid this deadline issue in the future.
Response: We appreciate the commenter's request to modify the HOP Panel meeting submission deadline format. However, frequency, timing, and presentation deadlines are outside the scope of the proposed rule and are generally announced through either a separate Federal Register notice or subregulatory channel such as the CMS website, or both.
F. Public Comments Received in Response to the CY 2020 OPPS/ASC Proposed Rule
We received over 3400 timely pieces of correspondence on the CY 2020 OPPS/ASC proposed rule that appeared in the Federal Register on August 9, 2019 (84 FR 39398). We note that we received some public comments that were outside the scope of the CY 2020 OPPS/ASC proposed rule. Out-of-scope-public comments are not addressed in this CY 2020 OPPS/ASC final rule with comment period. Summaries of those public comments that are within the scope of the proposed rule and our responses are set forth in the various sections of this final rule with comment period under the appropriate headings.
G. Public Comments Received on the CY 2019 OPPS/ASC Final Rule With Comment Period
We received over 540 timely pieces of correspondence on the CY 2019 OPPS/ASC final rule with comment period that appeared in the Federal Register on November 30, 2018 (83 FR 61567), some of which contained comments on the interim APC assignments and/or status indicators of new or replacement Level II HCPCS codes (identified with comment indicator “NI” in OPPS Addendum B, ASC Addendum AA, and ASC Addendum BB to that final rule). Summaries of the public comments on new or replacement Level II HCPCS codes are set forth in the CY 2020 OPPS/ASC proposed rule and this final rule with comment period under the appropriate subject matter headings.
II. Updates Affecting OPPS Payments
A. Recalibration of APC Relative Payment Weights
1. Database Construction
a. Database Source and Methodology
Section 1833(t)(9)(A) of the Act requires that the Secretary review not less often than annually and revise the relative payment weights for APCs. In the April 7, 2000 OPPS final rule with comment period (65 FR 18482), we explained in detail how we calculated the relative payment weights that were implemented on August 1, 2000 for each APC group.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39406), for CY 2020, we proposed to recalibrate the APC relative payment weights for services furnished on or after January 1, 2020, and before January 1, 2021 (CY 2020), using the same basic methodology that we described in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58827 through 58828), using updated CY 2018 claims data. That is, as we proposed, we recalibrate the relative payment weights for each APC based on claims and cost report data for hospital outpatient department (HOPD) services, using the most recent available data to construct a database for calculating APC group weights.
For the purpose of recalibrating the APC relative payment weights for CY 2020, we began with approximately 164 million final action claims (claims for which all disputes and adjustments have been resolved and payment has been made) for HOPD services furnished on or after January 1, 2018, and before January 1, 2019, before applying our exclusionary criteria and other methodological adjustments. After the application of those data processing changes, we used approximately 88 million final action claims to develop the proposed CY 2020 OPPS payment weights. For exact numbers of claims used and additional details on the claims accounting process, we refer readers to the claims accounting narrative under supporting documentation for the CY 2020 OPPS/ASC proposed rule on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
Addendum N to the proposed rule (which is available via the internet on the CMS website) included the proposed list of bypass codes for CY 2020. The proposed list of bypass codes contained codes that were reported on claims for services in CY 2018 and, therefore, included codes that were in effect in CY 2018 and used for billing, but were deleted for CY 2019. We retained these deleted bypass codes on the proposed CY 2020 bypass list because these codes existed in CY 2018 and were covered OPD services in that period, and CY 2018 claims data were used to calculate CY 2020 payment rates. Keeping these deleted bypass codes on the bypass list potentially allows us to create more “pseudo” single procedure claims for ratesetting purposes. “Overlap bypass codes” that are members of the proposed multiple imaging composite APCs were identified by asterisks (*) in the third column of Addendum N to the proposed rule. HCPCS codes that we proposed to add for CY 2020 were identified by asterisks (*) in the fourth column of Addendum N.
Table 1 contains the list of codes that we proposed to remove from the CY 2020 bypass list.

b. Calculation and Use of Cost-to-Charge Ratios (CCRs)
For CY 2020, in the CY 2020 OPPS/ASC proposed rule (84 FR 39407), we proposed to continue to use the hospital-specific overall ancillary and departmental cost-to-charge ratios (CCRs) to convert charges to estimated costs through application of a revenue code-to-cost center crosswalk. To calculate the APC costs on which the CY 2020 APC payment rates are based, we calculated hospital-specific overall ancillary CCRs and hospital-specific departmental CCRs for each hospital for which we had CY 2018 claims data by comparing these claims data to the most recently available hospital cost reports, which, in most cases, are from CY 2017. For the proposed CY 2020 OPPS payment rates, we used the set of claims processed during CY 2018. We applied the hospital-specific CCR to the hospital's charges at the most detailed level possible, based on a revenue code-to-cost center crosswalk that contains a hierarchy of CCRs used to estimate costs from charges for each revenue code. That crosswalk is available for review and continuous comment on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
To ensure the completeness of the revenue code-to-cost center crosswalk, we reviewed changes to the list of revenue codes for CY 2018 (the year of claims data we used to calculate the proposed CY 2020 OPPS payment rates) and found that the National Uniform Billing Committee (NUBC) did not add any new revenue codes to the NUBC 2018 Data Specifications Manual.
In accordance with our longstanding policy, we calculate CCRs for the standard and nonstandard cost centers accepted by the electronic cost report database. In general, the most detailed level at which we calculate CCRs is the hospital-specific departmental level. For a discussion of the hospital-specific overall ancillary CCR calculation, we refer readers to the CY 2007 OPPS/ASC final rule with comment period (71 FR 67983 through 67985). The calculation of blood costs is a longstanding exception (since the CY 2005 OPPS) to this general methodology for calculation of CCRs used for converting charges to costs on each claim. This exception is discussed in detail in the CY 2007 OPPS/ASC final rule with comment period and discussed further in section II.A.2.a.(1) of the proposed rule and this final rule with comment period.
In the CY 2014 OPPS/ASC final rule with comment period (78 FR 74840 through 74847), we finalized our policy of creating new cost centers and distinct CCRs for implantable devices, magnetic resonance imaging (MRIs), computed tomography (CT) scans, and cardiac catheterization. However, in response to the CY 2014 OPPS/ASC proposed rule, commenters reported that some hospitals used a less precise “square feet” allocation methodology for the costs of large moveable equipment like CT scan and MRI machines. They indicated that while CMS recommended using two alternative allocation methods, “direct assignment” or “dollar value,” as a more accurate methodology for directly assigning equipment costs, industry analysis suggested that approximately only half of the reported cost centers for CT scans and MRIs rely on these preferred methodologies. In response to concerns from commenters, we finalized a policy for the CY 2014 OPPS to remove claims from providers that use a cost allocation method of “square feet” to calculate CCRs used to estimate costs associated with the APCs for CT and MRI (78 FR 74847). Further, we finalized a transitional policy to estimate the imaging APC relative payment weights using only CT and MRI cost data from providers that do not use “square feet” as the cost allocation statistic. We provided that this finalized policy would sunset in 4 years to provide a sufficient time for hospitals to transition to a more accurate cost allocation method and for the related data to be available for ratesetting purposes (78 FR 74847). Therefore, beginning CY 2018, with the sunset of the transition policy, we would estimate the imaging APC relative payment weights using cost data from all providers, regardless of the cost allocation statistic employed. However, in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59228 and 59229) and in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58831), we finalized a policy to extend the transition policy for 1 additional year and we continued to remove claims from providers that use a cost allocation method of “square feet” to calculate CT and MRI CCRs for the CY 2018 OPPS and the CY 2019 OPPS.
As we discussed in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59228), some stakeholders have raised concerns regarding using claims from all providers to calculate CT and MRI CCRs, regardless of the cost allocations statistic employed (78 FR 74840 through 74847). Stakeholders noted that providers continue to use the “square feet” cost allocation method and that including claims from such providers would cause significant reductions in the imaging APC payment rates.
Table 2 demonstrates the relative effect on imaging APC payments after removing cost data for providers that report CT and MRI standard cost centers using “square feet” as the cost allocation method by extracting HCRIS data on Worksheet B-1. Table 3 provides statistical values based on the CT and MRI standard cost center CCRs using the different cost allocation methods.


Our analysis shows that since the CY 2014 OPPS in which we established the transition policy, the number of valid MRI CCRs has increased by 18.8 percent to 2,207 providers and the number of valid CT CCRs has increased by 16.0 percent to 2,291 providers. However, as shown in Table 2, nearly all imaging APCs would see an increase in payment rates for CY 2020 if claims from providers that report using the “square feet” cost allocation method were removed. This can be attributed to the generally lower CCR values from providers that use a “square feet” cost allocation method as shown in Table 2.
We noted in the CY 2020 OPPS/ASC proposed rule that the CT and MRI cost center CCRs have been available for ratesetting since the CY 2014 OPPS in which we established the transition policy. Since the initial 4-year transition, we have extended the transition an additional 2 years to offer provider flexibility in applying cost allocation methodologies for CT and MRI cost centers other than “square feet.” We noted that we believed we had provided sufficient time for providers to adopt an alternative cost allocation methodology for CT and MRI cost centers if they intended to do so. However, many providers continue to use the “square feet” cost allocation methodology, which we believe indicates that these providers believe this methodology is a sufficient method for attributing costs to this cost center. Additionally, we generally believe that increasing the amount of claims data available for use in ratesetting improves our ratesetting process. Therefore, we proposed that for the CY 2020 OPPS we would use all claims with valid CT and MRI cost center CCRs, including those that use a “square feet” cost allocation method, to estimate costs for the APCs for CT and MRI identified in Table 2. We noted that we did not believe another extension was warranted and expected to determine the imaging APC relative payment weights for CY 2020 using cost data from all providers, regardless of the cost allocation method employed.
Comment: One commenter noted that approximately half of all hospitals paid under the OPPS had CT and/or MRI cost centers that were reporting CCRs using the preferred methods (“dollar value” or “direct assignment”). This commenter further suggested that hospitals not using these preferred methods are either unable or unwilling to make the change to using these preferred methods. This commenter stated that some CT and MRI procedures show a significant number of CCRs that are close to zero, and that the commenter believed that these hospitals are likely unable to accurately reallocate these costs across hospital departments to new CT and MRI departmental cost centers. This commenter acknowledged that the number of valid CT and MRI CCRs has increased over time, but noted that incorrect cost allocation has negative effects on payment rates for almost all imaging APCs.
Several commenters recommended that CMS continue to exclude “square feet” cost allocation data and continue to educate hospitals on the importance of reporting direct CT and MRI services. Several commenters requested that CMS not use the CT and MRI-specific cost centers and instead estimate cost using the single diagnostic radiology cost center, believing this will solve the inaccurate reporting of costs for CT and MR services. They further suggested that we should advise hospitals through regulation and cost reporting instructions to no longer report costs separately for CT and MRI cost centers and make sure they review their diagnostic radiology cost center inclusive of CT and MR equipment, space, labor and over factors. This same commenter noted that the benefits of using a single diagnostic radiology cost center include consistency across hospitals, properly accounting for high-cost medical equipment, simplifying and standardizing cost reporting within the diagnostic radiology cost center, eliminating partial allocation of costs to CT and MRI cost centers, and reducing burden. One commenter requested that we work with various hospital organizations to help educate the hospital community on how to report these costs on the CT and MRI CCRs in hopes to transition to this policy over time.
Other commenters requested that we extend the transition to using all claims for one additional year. These same commenters requested that if extending the transition 1 additional year is not possible, that we phase in the payment impacts of this transition over 2 years. One commenter requested that CMS extend the transition for 2 additional years and stated that we should study the effects of this policy even further to better understand its payment impacts. One commenter noted that we should continue the transition policy of removing provider claims using the “square feet” cost allocation method to calculate cost-to-charge ratios (CCRs) associated with CT and MRI procedures into 2020 and require providers to report costs via the direct assignment or dollar value methodologies moving forward. Another commenter noted that the use of separate CT and MRI CCRs creates unintended consequences on the technical component of CT and MRI codes in the Medicare Physician Fee Schedule (MPFS). The commenter noted the resulting reductions in hospital payments would also affect the physician office practice setting. They believed that the OPPS technical payments would fall below the payment rates in the MPFS causing further cuts as mandated by the Deficit Reduction Act of 2005 (DRA), which mandates CMS pay the lesser of MPFS or OPPS rate.
One commenter suggested that, because CMS has various APC groupings for MRI and CT, the individual MRI and CT cost centers are no longer needed. This commenter suggested that, at the time separate cost centers for these services were established, the classification of imaging procedures into APCs was very specific, but that CMS is now “intermingling” the MRI and CT costs with other imaging services.
Response: We appreciate the comments regarding the use of CT and MRI cost center CCRs. As we stated in prior rulemaking, we recognize the concerns with regard to the application of the CT and MRI standard cost center CCRs and their use in the OPPS ratesetting. We understand that there is greater sensitivity to the cost allocation method being used on the cost report forms for these relatively new standard imaging cost centers under the OPPS due to the limited size of the OPPS payment bundles and because the OPPS applies the CCRs at the departmental level for cost estimation purposes. However, it is important to note that since we initially established the transition policy in the OPPS in CY 2014, we have continued to develop the OPPS as a prospective payment system. This includes greater packaging and the development of comprehensive APCs. As we have packaged a greater number of items and services with imaging payment under the OPPS, we believe imaging payments are somewhat less sensitive to the cost allocation method being used than they previously were. We also note that we still find value in obtaining more specific cost data and that the CT and MRI-specific cost centers provide useful cost and charge data for ratesetting purposes.
However, to address concerns in the comments about the amount of the decrease in imaging payment in CY 2020 due to ending of the transition period, we are finalizing a 2-year phased-in approach, as suggested by some commenters, that will apply 50 percent of the payment impact from ending the transition in CY 2020 and 100 percent of the payment impact from ending the transition in CY 2021. For CY 2020, we will calculate the imaging payment rates using both the transition methodology (excluding providers that use a “square feet” cost allocation method) and the standard methodology (including all providers, regardless of cost allocation method) and will assign the imaging APCs a payment rate that includes data representing 50 percent of the transition methodology payment rate and includes data representing 50 percent of the standard methodology payment rate. Beginning in CY 2021, we will set the imaging APC payment rates at 100 percent of the payment rate using the standard payment methodology (including all providers, regardless of cost allocation method). Table 4 below illustrates the estimated impact on geometric mean costs for CT and MRI APCs under our blended approach of utilizing 50 percent of the transitional payment methodology and 50 percent of the standard payment methodology for CY 2020.

As noted earlier, the Deficit Reduction Act (DRA) of 2005 requires Medicare to limit Medicare payment for certain imaging services covered by the physician fee schedule to not exceed what Medicare pays for these services under the OPPS. As required by law, for certain imaging series paid for under the MPFS, we cap the technical component of the PFS payment amount for the applicable year at the OPPS payment amount (71 FR 69659 through 69661). As we stated in the CY 2014 OPPS/ASC final rule with comment period (78 FR 74845), we have noted the potential impact the CT and MRI CCRs may have on other payment systems. We understand that payment reductions for imaging services under the OPPS could have significant payment impacts under the Physician Fee Schedule (PFS) where the technical component payment for many imaging services is capped at the OPPS payment amount. We will continue to monitor OPPS imaging payments in the future and consider the potential impacts of payment changes on the PFS and the ASC payment system.
2. Data Development and Calculation of Costs Used for Ratesetting
In this section of this final rule with comment period, we discuss the use of claims to calculate the OPPS payment rates for CY 2020. The Hospital OPPS page on the CMS website on which this final rule with comment period is posted (http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html) provides an accounting of claims used in the development of the final payment rates. That accounting provides additional detail regarding the number of claims derived at each stage of the process. In addition, below in this section, we discuss the file of claims that comprises the data set that is available upon payment of an administrative fee under a CMS data use
agreement. The CMS website http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html, includes information about obtaining the “OPPS Limited Data Set,” which now includes the additional variables previously available only in the OPPS Identifiable Data Set, including ICD-10-CM diagnosis codes and revenue code payment amounts. This file is derived from the CY 2018 claims that were used to calculate the final payment rates for this CY 2020 OPPS/ASC final rule with comment period.
Previously, the OPPS established the scaled relative weights, on which payments are based using APC median costs, a process described in the CY 2012 OPPS/ASC final rule with comment period (76 FR 74188). However, as discussed in more detail in section II.A.2.f. of the CY 2013 OPPS/ASC final rule with comment period (77 FR 68259 through 68271), we finalized the use of geometric mean costs to calculate the relative weights on which the CY 2013 OPPS payment rates were based. While this policy changed the cost metric on which the relative payments are based, the data process in general remained the same, under the methodologies that we used to obtain appropriate claims data and accurate cost information in determining estimated service cost. For CY 2020, in the CY 2020 OPPS/ASC proposed rule (84 FR 39409), we proposed to continue to use geometric mean costs to calculate the proposed relative weights on which the CY 2020 OPPS payment rates are based.
We used the methodology described in sections II.A.2.a. through II.A.2.c. of this final rule with comment period to calculate the costs we used to establish the relative payment weights used in calculating the OPPS payment rates for CY 2020 shown in Addenda A and B to this final rule with comment period (which are available via the internet on the CMS website). We refer readers to section II.A.4. of this final rule with comment period for a discussion of the conversion of APC costs to scaled payment weights.
We note that under the OPPS, CY 2019 was the first year in which claims data containing lines with the modifier “PN” were available, which indicate nonexcepted items and services furnished and billed by off-campus provider-based departments (PBDs) of hospitals. Because nonexcepted services are not paid under the OPPS, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58832), we finalized a policy to remove those claim lines reported with modifier “PN” from the claims data used in ratesetting for the CY 2019 OPPS and subsequent years. For the CY 2020 OPPS, we will continue to remove these claim lines with modifier “PN” from the ratesetting process.
Comment: Several commenters noted a potential issue with missing lines with the PN modifier. Specifically, these commenters believed that the CY 2020 proposed rule data, based on CY 2018 claims, excluded approximately 400,000 lines with Healthcare Common Procedure Coding System (HCPCS) codes and the PN modifier. They noted that this would mean that there was over an 80 percent decline from the CY 2017 claims data, which had approximately 2.8 million lines with HCPCS and the PN modifier. These commenters reviewed the 2018 Outpatient Standard Analytic File (SAF) and noted that they found approximately 3.5 million lines with HCPCS codes and the PN modifier. These commenters asserted that the ratesetting data included substantially less PN modifiers than in the SAF file for the same time period. These same commenters assert that if the PN lines were not included in the ratesetting process then the OPPS payment weights are accurate. They noted that, conversely, if the PN lines were included in the payment weights then payments would be inaccurate. These commenters wanted CMS to explain what occurred in the proposed rule data files to ensure that the APC payment weights correctly reflect the exclusion of PN modifier claims in the final rule.
Response: We thank the commenters for their input. First, we would like to note that claim lines with the PN modifier are excluded from the ratesetting process. Please note that the difference between the 2019 OPPS Final Rule and the 2020 OPPS Proposed rule is the following: We processed the claim lines with the PN modifier differently between the two rules, which resulted in the decrease in the number of PN lines in the OPPS limited data set as noted above. Specifically, the programs used for the CY 2020 proposed rule were modified to not factor in those lines as being OPPS lines, which resulted in more lines, and potentially, more total claims being categorized as non-OPPS claims. Previously, even though those lines were excluded from OPPS for ratesetting purposes, they were still considered OPPS in categorizing the claims for the limited data set. This change in processing logic had no effect on ratesetting and all of the lines with modifier “PN” are excluded from the OPPS ratesetting process for both CY 2019 and CY 2020. We are including these lines as non-OPPS claims in the CY 2020 OPPS final rule limited data set, but as discussed, are continuing to exclude them for ratesetting purposes.
For details of the claims accounting process used in this final rule with comment period, we refer readers to the claims accounting narrative under supporting documentation for this CY 2020 OPPS/ASC final rule with comment period on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
2. Final Data Development and Calculation of Costs Used for Ratesetting
a. Calculation of Single Procedure APC Criteria-Based Costs
(1) Blood and Blood Products
(a) Methodology
Since the implementation of the OPPS in August 2000, we have made separate payments for blood and blood products through APCs rather than packaging payment for them into payments for the procedures with which they are administered. Hospital payments for the costs of blood and blood products, as well as for the costs of collecting, processing, and storing blood and blood products, are made through the OPPS payments for specific blood product APCs.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39409), we proposed to continue to establish payment rates for blood and blood products using our blood-specific CCR methodology, which utilizes actual or simulated CCRs from the most recently available hospital cost reports to convert hospital charges for blood and blood products to costs. This methodology has been our standard ratesetting methodology for blood and blood products since CY 2005. It was developed in response to data analysis indicating that there was a significant difference in CCRs for those hospitals with and without blood-specific cost centers, and past public comments indicating that the former OPPS policy of defaulting to the overall hospital CCR for hospitals not reporting a blood-specific cost center often resulted in an underestimation of the true hospital costs for blood and blood products. Specifically, in order to address the differences in CCRs and to better reflect hospitals' costs, we proposed to continue to simulate blood CCRs for each hospital that does not report a blood cost center by calculating the ratio of the blood-specific CCRs to hospitals' overall CCRs for those hospitals that do report costs and charges for blood cost centers. We also proposed to apply this mean ratio to the overall CCRs of hospitals not reporting costs and charges for blood cost centers on their cost reports in order to simulate blood-specific CCRs for those hospitals. We proposed to calculate the costs upon which the proposed CY 2020 payment rates for blood and blood products are based using the actual blood-specific CCR for hospitals that reported costs and charges for a blood cost center and a hospital-specific, simulated blood-specific CCR for hospitals that did not report costs and charges for a blood cost center.
We continue to believe that the hospital-specific, simulated blood-specific, CCR methodology better responds to the absence of a blood-specific CCR for a hospital than alternative methodologies, such as defaulting to the overall hospital CCR or applying an average blood-specific CCR across hospitals. Because this methodology takes into account the unique charging and cost accounting structure of each hospital, we believe that it yields more accurate estimated costs for these products. We stated in the proposed rule that we continue to believe that this methodology in CY 2020 would result in costs for blood and blood products that appropriately reflect the relative estimated costs of these products for hospitals without blood cost centers and, therefore, for these blood products in general.
We note that, as discussed in section II.A.2.b.(1). of the CY 2019 OPPS/ASC final rule with comment period (82 FR 58837 through 58843), we defined a comprehensive APC (C-APC) as a classification for the provision of a primary service and all adjunctive services provided to support the delivery of the primary service. Under this policy, we include the costs of blood and blood products when calculating the overall costs of these C-APCs. In the CY 2020 OPPS/ASC proposed rule (84 FR 39410), we proposed to continue to apply the blood-specific CCR methodology described in this section when calculating the costs of the blood and blood products that appear on claims with services assigned to the C-APCs. Because the costs of blood and blood products would be reflected in the overall costs of the C-APCs (and, as a result, in the payment rates of the C-APCs), we proposed to not make separate payments for blood and blood products when they appear on the same claims as services assigned to the C-APCs (we refer readers to the CY 2015 OPPS/ASC final rule with comment period (79 FR 66796)).
We also referred readers to Addendum B to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website) for the proposed CY 2020 payment rates for blood and blood products (which are identified with status indicator “R”). For a more detailed discussion of the blood-specific CCR methodology, we refer readers to the CY 2005 OPPS proposed rule (69 FR 50524 through 50525). For a full history of OPPS payment for blood and blood products, we refer readers to the CY 2008 OPPS/ASC final rule with comment period (72 FR 66807 through 66810).
We did not receive any comments on our proposal to establish payment rates for blood and blood products using our blood-specific CCR methodology and we are finalizing this policy as proposed.
(b) Pathogen-Reduced Platelets Payment Rate
In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70322 through 70323), we reiterated that we calculate payment rates for blood and blood products using our blood-specific CCR methodology, which utilizes actual or simulated CCRs from the most recently available hospital cost reports to convert hospital charges for blood and blood products to costs. Because HCPCS code P9072 (Platelets, pheresis, pathogen reduced or rapid bacterial tested, each unit), the predecessor code to HCPCS code P9073 (Platelets, pheresis, pathogen-reduced, each unit), was new for CY 2016, there were no claims data available on the charges and costs for this blood product upon which to apply our blood-specific CCR methodology. Therefore, we established an interim payment rate for HCPCS code P9072 based on a crosswalk to existing blood product HCPCS code P9037 (Platelets, pheresis, leukocytes reduced, irradiated, each unit), which we believed provided the best proxy for the costs of the new blood product. In addition, we stated that once we had claims data for HCPCS code P9072, we would calculate its payment rate using the claims data that should be available for the code beginning in CY 2018, which is our practice for other blood product HCPCS codes for which claims data have been available for 2 years.
We stated in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59233) that, although our standard practice for new codes involves using claims data to set payment rates once claims data become available, we were concerned that there may have been confusion among the provider community about the services that HCPCS code P9072 described. That is, as early as 2016, there were discussions about changing the descriptor for HCPCS code P9072 to include the phrase “or rapid bacterial tested”, which is a less costly technology than pathogen reduction. In addition, effective January 2017, the code descriptor for HCPCS code P9072 was changed to describe rapid bacterial testing of platelets and, effective July 1, 2017, the descriptor for the temporary successor code (HCPCS code Q9988) for HCPCS code P9072 was changed again back to the original descriptor for HCPCS code P9072 that was in place for 2016.
Based on the ongoing discussions involving changes to the original HCPCS code P9072 established in CY 2016, we believed that claims from CY 2016 for pathogen reduced platelets may have potentially reflected certain claims for rapid bacterial testing of platelets. Therefore, we decided to continue to crosswalk the payment amount for services described by HCPCS code P9073 (the successor code to HCPCS code P9072 established January 1, 2018) to the payment amount for services described by HCPCS code P9037 for CY 2018 (82 FR 59232), to determine the payment rate for services described by HCPCS code P9072. In the CY 2019 OPPS/ASC proposed rule (83 FR 37058), for CY 2019, we discussed that we had reviewed the CY 2017 claims data for the two predecessor codes to HCPCS code P9073 (HCPCS codes P9072 and Q9988), along with the claims data for the CY 2017 temporary code for pathogen test for platelets (HCPCS code Q9987), which describes rapid bacterial testing of platelets. We found that there were over 2,200 claims billed with either HCPCS code P9072 or Q9988 in the CY 2017 claims data available for CY 2019 rulemaking. Accordingly, we believed that there were a sufficient number of claims to calculate a payment rate for HCPCS code P9073 for CY 2019 without using a crosswalk.
We also performed checks to estimate the share of claims that may have been billed for rapid bacterial testing of platelets as compared to the share of claims that may have been billed for pathogen-reduced, pheresis platelets (based on when HCPCS code P9072 was an active procedure code from January 1, 2017 to June 30, 2017). First, we found that the geometric mean cost for pathogen-reduced, pheresis platelets, as reported by HCPCS code Q9988 when billed separately from rapid bacterial testing of platelets, was $453.87, and that over 1,200 claims were billed for services described by HCPCS code Q9988. Next, we found that the geometric mean cost for rapid bacterial testing of platelets, as reported by HCPCS code Q9987 on claims, was $33.44, and there were 59 claims reported for services described by HCPCS code Q9987, of which 3 were separately paid.
These findings implied that almost all of the claims billed for services reported with HCPCS code P9072 were for pathogen-reduced, pheresis platelets. In addition, the geometric mean cost for services described by HCPCS code P9072, which may have contained rapid bacterial testing of platelets claims, was $468.11, which was higher than the geometric mean cost for services described by HCPCS code Q9988 of $453.87, which should not have contained claims for rapid bacterial testing of platelets. Because the geometric mean for services described by HCPCS code Q9987 was only $33.44, it would be expected that if a significant share of claims billed for services described by HCPCS code P9072 were for the rapid bacterial testing of platelets, the geometric mean cost for services described by HCPCS code P9072 would be lower than the geometric mean cost for services described by HCPCS code Q9988. Instead, we found that the geometric mean cost for services described by HCPCS code Q9988 was higher than the geometric mean cost for services described by HCPCS code P9072.
However, we received many comments from providers and other stakeholders including blood product industry stakeholder groups and the company who developed the pathogen-reduced platelets technology requesting that we not implement our proposal for CY 2019, and instead that we should once again establish the payment rate for HCPCS code P9073 by performing a crosswalk from the payment amount for services described by HCPCS code P9073 to the payment amount for services described by HCPCS code P9037. The commenters were concerned that the payment rate for HCPCS code P9073 calculated by using claims data for that service was too low. Several commenters believed the claim costs for pathogen-reduced platelets were lower than actual costs because of coding errors by providers, providers who did not use pathogen-reduced platelets when billing the service, and confusion over whether to use the hospital CCR or the blood center CCR to report charges for pathogen-reduced platelets. We considered the comments we received and decided not to finalize our proposal for CY 2019 to calculate the payment rate for services described by HCPCS code P9073 using claims payment history. Instead, for CY 2019, we established the payment rate for services described by HCPCS code P9073 by crosswalking the payment rate for the services described by HCPCS code P9073 from the payment rate for services described by HCPCS code P9037 (83 FR 58834).
For CY 2020 and subsequent years, we proposed to calculate the payment rate for services described by HCPCS code P9073 by using claims payment history, which is the standard methodology used under the OPPS to calculate payment rates for HCPCS codes with at least 2 years of claims history. Claims for HCPCS code P9073 and its predecessor codes have been billed under the OPPS for over 3 years and we believe providers have had sufficient time to become familiar with the services covered by the procedure code and the appropriate charges and CCRs used to report the service. Also, it has been more than a year and half since the issue in which payment for pathogen-reduced platelets and payment for rapid bacterial testing were combined under the same code was resolved. In our analysis of claims data from CY 2018, we found that approximately 4,700 claims have been billed for services described by HCPCS code P9073 and the estimated payment rate for services described by HCPCS code P9073 based on the claims data was approximately $585. The claims-based payment rate for services described by HCPCS code P9073 was approximately $60 less than the estimated crosswalked payment rate using HCPCS code P9037 of approximately $645. The claims data show that services described by HCPCS code P9073 have been reported regularly by providers during CY 2018 and the payment rate is close to the payment rate of the crosswalked payment rate for services described by HCPCS code P9037. Therefore, we believe that the payment rate for services described by HCPCS code P9073 can be determined using claims data without a crosswalk from the payment rate for services described by HCPCS code P9037.
We refer readers to Addendum B of the proposed rule for the proposed payment rate for services described by HCPCS code P9073 reportable under the OPPS. Addendum B is available via the internet on the CMS website.
Comment: We received comments that opposed the proposal to end the crosswalk between P9073 (Platelets, pheresis, pathogen-reduced, each unit) and P9037 (Platelets, pheresis, leukocytes reduced, irradiated, each unit) and calculate the payment rate for services described by HCPCS code P9073 using claims payment history. The commenters stated that the 2018 claims data used to establish the CY 2020 payment rate for pathogen-reduced platelets continue to include erroneous claims and is therefore inaccurate. The commenters further state, as an example of the inaccuracies of the 2018 claims data, that approximately 30 percent of the 2018 claims data for P9073 contain costs that are at least $100 lower than the costs of P9037, which is a less expensive technology. The commenters requested that we continue the crosswalk between these two codes for both CYs 2020 and 2021 to allow hospitals time to continue to correct errors in their chargemasters and to prevent underpayment to hospitals for pathogen-reduced platelets. The commenters also claim that hospitals may be reluctant to adopt a relatively new technology, such as pathogen-reduced platelets, if the payment is too low.
Response: We continue to believe that, beginning in CY 2020, it is appropriate to calculate the payment rate for services described by HCPCS code P9073 using the standard methodology (which involves using data from CY 2018 claims for the code). We have previously acknowledged (83 FR 58834) that there was confusion among the provider community surrounding the reporting and billing for P9073 and have made exceptions to our standard methodology for calculating payment rates for this service. At this time, we believe providers have had sufficient time to become familiar with the services covered by the procedure code and we believe the issue in which payment for pathogen-reduced platelets and payment for rapid bacterial testing was combined under the same code has been resolved. Additionally, in response to concerns that hospitals may be reluctant to adopt the pathogen-reduced platelet technology based on a payment rate that is too low, in our analysis of claims data from CY 2018, we found that approximately 5,300 claims have been billed for services described by HCPCS code P9073, which is significantly higher that the approximately 2,200 claims billed in 2017 for services described by the predecessor codes for HCPCS code P9073, HCPCS codes Q9988 and P9072. Also, the estimated CY 2020 payment rate for services described by HCPCS code P9073 based on the CY 2018 claims data is approximately $600 which is comparable to the CY 2020 estimated crosswalked payment rate using HCPCS code P9037 of approximately $620. These data suggest that a crosswalk is no longer necessary. Further, we have now used a cross-walk for P9073 and its predecessor codes for 4 years, which is longer than the typical 2-year period for which we normally cross-walk new HCPCS codes. We agreed with past commenters that an extended period of cross-walking payment for P9073 was necessary to address the coding confusion in 2016 that may have led to the claims data reflecting costs for services not described by HCPCS code P9073. However, the above-referenced coding issues were resolved in January 2018, so we have no reason to believe that the data may reflect the costs for services other than those described by P9073.
Accordingly, for CY 2020 and subsequent years, we are finalizing the policy to calculate the payment rate for services described by HCPCS code P9073 by using claims payment history and to end the crosswalk between HCPCS codes P9037 and P9073.
(2) Brachytherapy Sources
Section 1833(t)(2)(H) of the Act mandates the creation of additional groups of covered OPD services that classify devices of brachytherapy consisting of a seed or seeds (or radioactive source) (“brachytherapy sources”) separately from other services or groups of services. The statute provides certain criteria for the additional groups. For the history of OPPS payment for brachytherapy sources, we refer readers to prior OPPS final rules, such as the CY 2012 OPPS/ASC final rule with comment period (77 FR 68240 through 68241). As we have stated in prior OPPS updates, we believe that adopting the general OPPS prospective payment methodology for brachytherapy sources is appropriate for a number of reasons (77 FR 68240). The general OPPS methodology uses costs based on claims data to set the relative payment weights for hospital outpatient services. This payment methodology results in more consistent, predictable, and equitable payment amounts per source across hospitals by averaging the extremely high and low values, in contrast to payment based on hospitals' charges adjusted to costs. We believe that the OPPS methodology, as opposed to payment based on hospitals' charges adjusted to cost, also would provide hospitals with incentives for efficiency in the provision of brachytherapy services to Medicare beneficiaries. Moreover, this approach is consistent with our payment methodology for the vast majority of items and services paid under the OPPS. We refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70323 through 70325) for further discussion of the history of OPPS payment for brachytherapy sources.
In the CY 2020 OPPS/ASC proposed rule, for CY 2020, we proposed to use the costs derived from CY 2018 claims data to set the proposed CY 2020 payment rates for brachytherapy sources because CY 2018 is the year of data we proposed to use to set the proposed payment rates for most other items and services that would be paid under the CY 2020 OPPS. We proposed to base the payment rates for brachytherapy sources on the geometric mean unit costs for each source, consistent with the methodology that we proposed for other items and services paid under the OPPS, as discussed in section II.A.2. of the proposed rule. We also proposed to continue the other payment policies for brachytherapy sources that we finalized and first implemented in the CY 2010 OPPS/ASC final rule with comment period (74 FR 60537). We proposed to pay for the stranded and nonstranded not otherwise specified (NOS) codes, HCPCS codes C2698 (Brachytherapy source, stranded, not otherwise specified, per source) and C2699 (Brachytherapy source, non-stranded, not otherwise specified, per source), at a rate equal to the lowest stranded or nonstranded prospective payment rate for such sources, respectively, on a per source basis (as opposed to, for example, a per mCi), which is based on the policy we established in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66785). We also proposed to continue the policy we first implemented in the CY 2010 OPPS/ASC final rule with comment period (74 FR 60537) regarding payment for new brachytherapy sources for which we have no claims data, based on the same reasons we discussed in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66786; which was delayed until January 1, 2010 by section 142 of Pub. L. 110-275). Specifically, this policy is intended to enable us to assign new HCPCS codes for new brachytherapy sources to their own APCs, with prospective payment rates set based on our consideration of external data and other relevant information regarding the expected costs of the sources to hospitals. The proposed CY 2020 payment rates for brachytherapy sources were included in Addendum B to the proposed rule (which is available via the internet on the CMS website) and were identified with status indicator “U”.
For CY 2018, we assigned status indicator “U” (Brachytherapy Sources, Paid under OPPS; separate APC payment) to HCPCS code C2645 (Brachytherapy planar source, palladium-103, per square millimeter) in the absence of claims data and established a payment rate using external data (invoice price) at $4.69 per mm2. For CY 2019, in the absence of sufficient claims data, we continued to establish a payment rate for C2645 at $4.69 per mm2. For CY 2020, we proposed to continue to assign status indicator “U” to HCPCS code C2645 (Brachytherapy planar source, palladium-103, per square millimeter). Our CY 2018 claims data available for the proposed CY 2020 rule, included two claims with over 9,000 units of HCPCS code C2645. Therefore, we stated our belief that the CY 2018 claims data were adequate to establish an APC payment rate for HCPCS code C2645 and to discontinue our use of external data for this brachytherapy source. Specifically, we proposed to set the proposed CY 2020 payment rate at the geometric mean cost of HCPCS code C2645 based on CY 2018 claims data, which is $1.02 per mm2.
Comment: One commenter stated that the reduction in the payment rate for HCPCS code C2645 (Brachytherapy planar source, palladium-103, per square millimeter) for CY 2020 will preclude outpatient use for an FDA-cleared, predominantly outpatient indication, for C2645. Additionally, the commenter argued that the two claims used to establish the payment rate for C2645 are not a sufficient volume for ratesetting and that the claims are most likely erroneous in that the brachytherapy source was used for procedures on the inpatient-only list.
Response: Claims that include brachytherapy sources along with procedures on the inpatient-only list are sufficient and appropriate to use for our ratesetting process as brachytherapy sources are line-item paid. However, given the limited number of claims for HCPCS C2645 for both CY 2020 and previous calendar years and the new FDA-approved outpatient indication for HCPCS code C2645, we are persuaded that the proposed CY 2020 payment rate, which is significantly lower than that of the rate in effect in prior years, may not adequately represent the costs associated with C2645. Therefore, we are using our equitable adjustment authority under section 1833(t)(2)(E) of the Act, which states that the Secretary shall establish, in a budget neutral manner, other adjustments as determined to be necessary to ensure equitable payments, to maintain the CY 2019 rate for this brachytherapy source, despite the lower geometric mean costs of $1.03 per mm2 available in the claims data used for this final rule with comment period. We believe this situation is unique, given the very limited number of claims for this brachytherapy source for both CY 2020 ratesetting purposes and previous calendar years.
After consideration of the public comment we received, we are not finalizing the proposed rate for C2645 and are instead assigning the brachytherapy source described by HCPCS code C2645 a payment rate of $4.69 mm2 for CY 2020 through use of our equitable adjustment authority.
Comment: Some commenters recommended that we reevaluate our approach to ratesetting HCPCS C2642 (Brachytherapy source, stranded, cesium-131, per source) and stated that our proposed CY 2020 payment rate of $67.29 per source for HCPCS code C2642 would be too low to ensure fair and adequate reimbursement. Additionally, one provider who billed C2642 stated there was a clerical error and that it may have inadvertently underreported the actual costs for C2642 incurred by the provider.
Response: Based on the most current available data for the CY 2020 OPPS/ASC final rule with comment period, the geometric mean for HCPCS code C2642 based on 85 claims from CY 2018 is $75.06 per source. We note that the CY 2019 payment rate for HCPCS Code C2642 was $79.94 per source. We believe that the variation in costs for HCPCS code C2642 does not appear unusual or erroneous and that the CY 2020 geometric mean for HCPCS code C2642 based on CY 2018 claims data is consistent with historical payment rates for this brachytherapy source.
Comment: One commenter stated that the geometric mean cost and payment for brachytherapy sources has fluctuated significantly since 2013. The commenter argued that such fluctuations may put financial pressure on providers and create access barriers for beneficiaries to receive brachytherapy. The commenter requested we review and consider removing outliers to ensure payment stability for low-volume brachytherapy sources in future rulemaking.
Response: We thank the commenter for their recommendation and will take it under consideration in future rulemaking. As discussed in the CY 2013 OPPS/ASC final rule with comment period (77 FR 68259 through 68271), geometric mean costs better encompass the variation in costs that occur when providing a service because, in addition to the individual cost values that are reflected by medians, geometric means reflect the magnitude of the cost measurements, and thus are more sensitive to changes in the data. OPPS relative payment weights based on geometric mean costs would better capture the range of costs associated with providing services. Further, geometric means capture cost changes that are introduced slowly into the system on a case-by-case or hospital-by-hospital basis. For these reasons, we believe it would be inappropriate to remove outliers when determining brachytherapy geometric mean costs and payment rates.
We continue to invite hospitals and other parties to submit recommendations to us for new codes to describe new brachytherapy sources. Such recommendations should be directed to the Division of Outpatient Care, Mail Stop C4-01-26, Centers for Medicare and Medicaid Services, 7500 Security Boulevard, Baltimore, MD 21244. We will continue to add new brachytherapy source codes and descriptors to our systems for payment on a quarterly basis.
b. Comprehensive APCs (C-APCs) for CY 2020
(1) Background
In the CY 2014 OPPS/ASC final rule with comment period (78 FR 74861 through 74910), we finalized a comprehensive payment policy that packages payment for adjunctive and secondary items, services, and procedures into the most costly primary procedure under the OPPS at the claim level. The policy was finalized in CY 2014, but the effective date was delayed until January 1, 2015, to allow additional time for further analysis, opportunity for public comment, and systems preparation. The comprehensive APC (C-APC) policy was implemented effective January 1, 2015, with modifications and clarifications in response to public comments received regarding specific provisions of the C-APC policy (79 FR 66798 through 66810).
A C-APC is defined as a classification for the provision of a primary service and all adjunctive services provided to support the delivery of the primary service. We established C-APCs as a category broadly for OPPS payment and implemented 25 C-APCs beginning in CY 2015 (79 FR 66809 through 66810). In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70332), we finalized 10 additional C-APCs to be paid under the existing C-APC payment policy and added 1 additional level to both the Orthopedic Surgery and Vascular Procedures clinical families, which increased the total number of C-APCs to 37 for CY 2016. In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79584 through 79585), we finalized another 25 C-APCs for a total of 62 C-APCs. In the CY 2018 OPPS/ASC final rule with comment period, we did not change the total number of C-APCs from 62. In the CY 2019 OPPS/ASC final rule with comment period, we created 3 new C-APCs, increasing the total number to 65 (83 FR 58844 through 58846).
Under our C-APC policy, we designate a service described by a HCPCS code assigned to a C-APC as the primary service when the service is identified by OPPS status indicator “J1”. When such a primary service is reported on a hospital outpatient claim, taking into consideration the few exceptions that are discussed below, we make payment for all other items and services reported on the hospital outpatient claim as being integral, ancillary, supportive, dependent, and adjunctive to the primary service (hereinafter collectively referred to as “adjunctive services”) and representing components of a complete comprehensive service (78 FR 74865 and 79 FR 66799). Payments for adjunctive services are packaged into the payments for the primary services. This results in a single prospective payment for each of the primary, comprehensive services based on the costs of all reported services at the claim level.
Services excluded from the C-APC policy under the OPPS include services that are not covered OPD services, services that cannot by statute be paid for under the OPPS, and services that are required by statute to be separately paid. This includes certain mammography and ambulance services that are not covered OPD services in accordance with section 1833(t)(1)(B)(iv) of the Act; brachytherapy seeds, which also are required by statute to receive separate payment under section 1833(t)(2)(H) of the Act; pass-through payment drugs and devices, which also require separate payment under section 1833(t)(6) of the Act; self-administered drugs (SADs) that are not otherwise packaged as supplies because they are not covered under Medicare Part B under section 1861(s)(2)(B) of the Act; and certain preventive services (78 FR 74865 and 79 FR 66800 through 66801). A list of services excluded from the C-APC policy is included in Addendum J to this final rule with comment period (which is available via the internet on the CMS website).
The C-APC policy payment methodology set forth in the CY 2014 OPPS/ASC final rule with comment period for the C-APCs and modified and implemented beginning in CY 2015 is summarized as follows (78 FR 74887 and 79 FR 66800):
Basic Methodology. As stated in the CY 2015 OPPS/ASC final rule with comment period, we define the C-APC payment policy as including all covered OPD services on a hospital outpatient claim reporting a primary service that is assigned to status indicator “J1”, excluding services that are not covered OPD services or that cannot by statute be paid for under the OPPS. Services and procedures described by HCPCS codes assigned to status indicator “J1” are assigned to C-APCs based on our usual APC assignment methodology by evaluating the geometric mean costs of the primary service claims to establish resource similarity and the clinical characteristics of each procedure to establish clinical similarity within each APC.
In the CY 2016 OPPS/ASC final rule with comment period, we expanded the C-APC payment methodology to qualifying extended assessment and management encounters through the “Comprehensive Observation Services” C-APC (C-APC 8011). Services within this APC are assigned status indicator “J2”. Specifically, we make a payment through C-APC 8011 for a claim that:
- Does not contain a procedure described by a HCPCS code to which we have assigned status indicator “T”
- Contains 8 or more units of services described by HCPCS code G0378 (Hospital observation services, per hour);
- Contains services provided on the same date of service or 1 day before the date of service for HCPCS code G0378 that are described by one of the following codes: HCPCS code G0379 (Direct admission of patient for hospital observation care) on the same date of service as HCPCS code G0378; CPT code 99281 (Emergency department visit for the evaluation and management of a patient (Level 1)); CPT code 99282 (Emergency department visit for the evaluation and management of a patient (Level 2)); CPT code 99283 (Emergency department visit for the evaluation and management of a patient (Level 3)); CPT code 99284 (Emergency department visit for the evaluation and management of a patient (Level 4)); CPT code 99285 (Emergency department visit for the evaluation and management of a patient (Level 5)) or HCPCS code G0380 (Type B emergency department visit (Level 1)); HCPCS code G0381 (Type B emergency department visit (Level 2)); HCPCS code G0382 (Type B emergency department visit (Level 3)); HCPCS code G0383 (Type B emergency department visit (Level 4)); HCPCS code G0384 (Type B emergency department visit (Level 5)); CPT code 99291 (Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74 minutes); or HCPCS code G0463 (Hospital outpatient clinic visit for assessment and management of a patient); and
- Does not contain services described by a HCPCS code to which we have assigned status indicator “J1”.
The assignment of status indicator “J2” to a specific combination of services performed in combination with each other allows for all other OPPS payable services and items reported on the claim (excluding services that are not covered OPD services or that cannot by statute be paid for under the OPPS) to be deemed adjunctive services representing components of a comprehensive service and resulting in a single prospective payment for the comprehensive service based on the costs of all reported services on the claim (80 FR 70333 through 70336).
Services included under the C-APC payment packaging policy, that is, services that are typically adjunctive to the primary service and provided during the delivery of the comprehensive service, include diagnostic procedures, laboratory tests, and other diagnostic tests and treatments that assist in the delivery of the primary procedure; visits and evaluations performed in association with the procedure; uncoded services and supplies used during the service; durable medical equipment as well as prosthetic and orthotic items and supplies when provided as part of the outpatient service; and any other components reported by HCPCS codes that represent services that are provided during the complete comprehensive service (78 FR 74865 and 79 FR 66800).
In addition, payment for hospital outpatient department services that are similar to therapy services and delivered either by therapists or nontherapists is included as part of the payment for the packaged complete comprehensive service. These services that are provided during the perioperative period are adjunctive services and are deemed not to be therapy services as described in section 1834(k) of the Act, regardless of whether the services are delivered by therapists or other nontherapist health care workers. We have previously noted that therapy services are those provided by therapists under a plan of care in accordance with section 1835(a)(2)(C) and section 1835(a)(2)(D) of the Act and are paid for under section 1834(k) of the Act, subject to annual therapy caps as applicable (78 FR 74867 and 79 FR 66800). However, certain other services similar to therapy services are considered and paid for as hospital outpatient department services. Payment for these nontherapy outpatient department services that are reported with therapy codes and provided with a comprehensive service is included in the payment for the packaged complete comprehensive service. We note that these services, even though they are reported with therapy codes, are hospital outpatient department services and not therapy services. We refer readers to the July 2016 OPPS Change Request 9658 (Transmittal 3523) for further instructions on reporting these services in the context of a C-APC service.
Items included in the packaged payment provided in conjunction with the primary service also include all drugs, biologicals, and radiopharmaceuticals, regardless of cost, except those drugs with pass-through payment status and SADs, unless they function as packaged supplies (78 FR 74868 through 74869 and 74909 and 79 FR 66800). We refer readers to Section 50.2M, Chapter 15, of the Medicare Benefit Policy Manual for a description of our policy on SADs treated as hospital outpatient supplies, including lists of SADs that function as supplies and those that do not function as supplies.
We define each hospital outpatient claim reporting a single unit of a single primary service assigned to status indicator “J1” as a single “J1” unit procedure claim (78 FR 74871 and 79 FR 66801). Line item charges for services included on the C-APC claim are converted to line item costs, which are then summed to develop the estimated APC costs. These claims are then assigned one unit of the service with status indicator “J1” and later used to develop the geometric mean costs for the C-APC relative payment weights. (We note that we use the term “comprehensive” to describe the geometric mean cost of a claim reporting “J1” service(s) or the geometric mean cost of a C-APC, inclusive of all of the items and services included in the C-APC service payment bundle.) Charges for services that would otherwise be separately payable are added to the charges for the primary service. This process differs from our traditional cost accounting methodology only in that all such services on the claim are packaged (except certain services as described above). We apply our standard data trims, which exclude claims with extremely high primary units or extreme costs.
The comprehensive geometric mean costs are used to establish resource similarity and, along with clinical similarity, dictate the assignment of the primary services to the C-APCs. We establish a ranking of each primary service (single unit only) to be assigned to status indicator “J1” according to its comprehensive geometric mean costs. For the minority of claims reporting more than one primary service assigned to status indicator “J1” or units thereof, we identify one “J1” service as the primary service for the claim based on our cost-based ranking of primary services. We then assign these multiple “J1” procedure claims to the C-APC to which the service designated as the primary service is assigned. If the reported “J1” services on a claim map to different C-APCs, we designate the “J1” service assigned to the C-APC with the highest comprehensive geometric mean cost as the primary service for that claim. If the reported multiple “J1” services on a claim map to the same C-APC, we designate the most costly service (at the HCPCS code level) as the primary service for that claim. This process results in initial assignments of claims for the primary services assigned to status indicator “J1” to the most appropriate C-APCs based on both single and multiple procedure claims reporting these services and clinical and resource homogeneity.
Complexity Adjustments. We use complexity adjustments to provide increased payment for certain comprehensive services. We apply a complexity adjustment by promoting qualifying paired “J1” service code combinations or paired code combinations of “J1” services and certain add-on codes (as described further below) from the originating C-APC (the C-APC to which the designated primary service is first assigned) to the next higher paying C-APC in the same clinical family of C-APCs. We apply this type of complexity adjustment when the paired code combination represents a complex, costly form or version of the primary service according to the following criteria:
- Frequency of 25 or more claims reporting the code combination (frequency threshold); and
- Violation of the 2 times rule, as stated in section 1833(t)(2) of the Act and section III.B.2. of this final rule, in the originating C-APC (cost threshold).
These criteria identify paired code combinations that occur commonly and exhibit materially greater resource requirements than the primary service. The CY 2017 OPPS/ASC final rule with comment period (81 FR 79582) included a revision to the complexity adjustment eligibility criteria. Specifically, we finalized a policy to discontinue the requirement that a code combination (that qualifies for a complexity adjustment by satisfying the frequency and cost criteria thresholds described above) also not create a 2 times rule violation in the higher level or receiving APC.
After designating a single primary service for a claim, we evaluate that service in combination with each of the other procedure codes reported on the claim assigned to status indicator “J1” (or certain add-on codes) to determine if there are paired code combinations that meet the complexity adjustment criteria. For a new HCPCS code, we determine initial C-APC assignment and qualification for a complexity adjustment using the best available information, crosswalking the new HCPCS code to a predecessor code(s) when appropriate.
Once we have determined that a particular code combination of “J1” services (or combinations of “J1” services reported in conjunction with certain add-on codes) represents a complex version of the primary service because it is sufficiently costly, frequent, and a subset of the primary comprehensive service overall according to the criteria described above, we promote the claim including the complex version of the primary service as described by the code combination to the next higher cost C-APC within the clinical family, unless the primary service is already assigned to the highest cost APC within the C-APC clinical family or assigned to the only C-APC in a clinical family. We do not create new APCs with a comprehensive geometric mean cost that is higher than the highest geometric mean cost (or only) C-APC in a clinical family just to accommodate potential complexity adjustments. Therefore, the highest payment for any claim including a code combination for services assigned to a C-APC would be the highest paying C-APC in the clinical family (79 FR 66802).
We package payment for all add-on codes into the payment for the C-APC. However, certain primary service add-on combinations may qualify for a complexity adjustment. As noted in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70331), all add-on codes that can be appropriately reported in combination with a base code that describes a primary “J1” service are evaluated for a complexity adjustment.
To determine which combinations of primary service codes reported in conjunction with an add-on code may qualify for a complexity adjustment for CY 2020, in the CY 2020 OPPS/ASC proposed rule (84 FR 39414), we proposed to apply the frequency and cost criteria thresholds discussed above, testing claims reporting one unit of a single primary service assigned to status indicator “J1” and any number of units of a single add-on code for the primary “J1” service. If the frequency and cost criteria thresholds for a complexity adjustment are met and reassignment to the next higher cost APC in the clinical family is appropriate (based on meeting the criteria outlined above), we make a complexity adjustment for the code combination; that is, we reassign the primary service code reported in conjunction with the add-on code to the next higher cost C-APC within the same clinical family of C-APCs. As previously stated, we package payment for add-on codes into the C-APC payment rate. If any add-on code reported in conjunction with the “J1” primary service code does not qualify for a complexity adjustment, payment for the add-on service continues to be packaged into the payment for the primary service and is not reassigned to the next higher cost C-APC. We listed the complexity adjustments for “J1” and add-on code combinations for CY 2020, along with all of the other proposed complexity adjustments, in Addendum J to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website).
Addendum J to the proposed rule included the cost statistics for each code combination that would qualify for a complexity adjustment (including primary code and add-on code combinations). Addendum J to the proposed rule also contained summary cost statistics for each of the paired code combinations that describe a complex code combination that would qualify for a complexity adjustment and were proposed to be reassigned to the next higher cost C-APC within the clinical family. The combined statistics for all proposed reassigned complex code combinations were represented by an alphanumeric code with the first 4 digits of the designated primary service followed by a letter. For example, the proposed geometric mean cost listed in Addendum J for the code combination described by complexity adjustment assignment 3320R, which is assigned to C-APC 5224 (Level 4 Pacemaker and Similar Procedures), includes all paired code combinations that were proposed to be reassigned to C-APC 5224 when CPT code 33208 is the primary code. Providing the information contained in Addendum J to the proposed rule allowed stakeholders the opportunity to better assess the impact associated with the proposed reassignment of claims with each of the paired code combinations eligible for a complexity adjustment.
Comment: Several commenters requested that CMS alter the established C-APC complexity adjustment eligibility criteria to allow additional code combinations to qualify for complexity adjustments. Some commenters reiterated their request to allow clusters of procedures, consisting of a “J1” code-pair and multiple other associated add-on codes used in combination with that “J1” code-pair to qualify for complexity adjustments. Other commenters requested that CMS allow procedures assigned status indicator “S” or “T” to be eligible for complexity adjustments, to allow a C-APC to receive payment at the C-APC rate two levels higher within the clinical family when there is a violation of the two-times rule in the receiving C-APC and also to account for patient characteristics such as comorbidities and sociodemographic factors in the complexity adjustment policy. One commenter recommended that HCPCS code 0546T—Radiofrequency spectroscopy, real time, intraoperative margin assessment, at the time of partial mastectomy, with report—be assigned to APC 5091—Level 1 Breast/Lymphatic Surgery and Related Procedures and designated for complexity adjustment to APC 5092—Level 2 Breast/Lymphatic Surgery and Related Procedures for CY 2020.
We also received a comment requesting that CMS modify its complexity adjustment criteria and apply the complexity adjustment to all blue light cystoscopy with Cysview procedures in the HOPD, including eliminating the claim frequency requirement to determine eligibility for the complexity adjustment and expanding the eligibility for a complexity adjustment to other APCs besides C-APCs.
Response: We appreciate these comments. However, at this time, we do not believe changes to the C-APC complexity adjustment criteria are necessary or that we should make exceptions to the criteria to allow claims with the code combinations suggested by the commenters to receive complexity adjustments. As stated previously (81 FR 79582), we continue to believe that the complexity adjustment criteria, which require a frequency of 25 or more claims reporting a code combination and a violation of the 2 times rule in the originating C-APC in order to receive payment in the next higher cost C-APC within the clinical family, are adequate to determine if a combination of procedures represents a complex, costly subset of the primary service. If a code combination meets these criteria, the combination receives payment at the next higher cost C-APC. Code combinations that do not meet these criteria receive the C-APC payment rate associated with the primary “J1” service. A minimum of 25 claims is already a very low threshold for a national payment system. Lowering the minimum of 25 claims further could lead to unnecessary complexity adjustments for service combinations that are rarely performed.
We also do not believe that it is necessary to provide payment for claims including qualifying code combinations at two APC levels higher than the originating APC. As stated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58842), we believe that payment at the next higher paying C-APC is adequate for code combinations that exhibit materially greater resource requirements than the primary service and that, in many cases, paying the rate assigned to two levels higher may lead to a significant overpayment. As mentioned previously, we do not create new APCs with a comprehensive geometric mean cost that is higher than the highest geometric mean cost C-APC in a clinical family just to accommodate potential complexity adjustments. The highest payment for any claim including a code combination for services assigned to a C-APC would be the highest paying C- APC in the clinical family (79 FR 66802). Therefore, a policy to pay for claims with qualifying code combinations at two C-APC levels higher than the originating APC is not always feasible.
Lastly, as stated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58843), we do not believe that it is necessary to adjust the complexity adjustment criteria to allow claims that include more than two “J1” procedures, procedures that are not assigned to C-APCs, or procedures performed at certain hospitals with patients with more comorbidities, to qualify for a complexity adjustment. As mentioned earlier, we believe the current criteria are adequate to determine if a combination of procedures represents a complex, costly subset of the primary service.
With regard to the requests for further complexity adjustments for blue light cystoscopy procedures using the drug Cysview, as discussed in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59243-59246), we acknowledged that there are additional equipment, supplies, operating room time, and other resources required to perform blue light cystoscopy in addition to white light cystoscopy. We also acknowledged stakeholder concerns that the payment for blue light cystoscopy procedures involving Cysview® may be creating a barrier to beneficiaries receiving access to reasonable and necessary care for which there may not be a clinically comparable alternative. Based on these issues, in CY 2018, we created a HCPCS C-code (C9738—Adjunctive blue light cystoscopy with fluorescent imaging agent (list separately in addition to code for primary procedure)) to describe blue light cystoscopy with fluorescent imaging agent and allowed this code to be eligible for complexity adjustments when billed with procedure codes used to describe white light cystoscopy of the bladder, although this code is not a “J1” service or an add-on code for the primary “J1” service. For CY 2020, there are three code combinations of six total involving C9738 and procedure codes used to describe white light cystoscopy that will qualify for a complexity adjustment. At this time, we do not believe that further modifications to the C-APC policy are necessary.
After consideration of the public comments we received on the proposed complexity adjustment policy, we are finalizing the C-APC complexity adjustment policy for CY 2020, as proposed, without modification.
(2) Additional C-APCs for CY 2020
For CY 2020 and subsequent years, in the CY 2020 OPPS/ASC proposed rule (84 FR 39414), we proposed to continue to apply the C-APC payment policy methodology. We refer readers to the CY 2017 OPPS/ASC final rule with comment period (81 FR 79583) for a discussion of the C-APC payment policy methodology and revisions.
Each year, in accordance with section 1833(t)(9)(A) of the Act, we review and revise the services within each APC group and the APC assignments under the OPPS. As a result of our annual review of the services and the APC assignments under the OPPS, in the proposed rule (84 FR 39414), we proposed to add two C-APCs under the existing C-APC payment policy in CY 2020: Proposed C-APC 5182 (Level 2 Vascular Procedures); and proposed C-APC 5461 (Level 1 Neurostimulator and Related Procedures). These APCs were selected to be included in this proposal because, similar to other C-APCs, these APCs include primary, comprehensive services, such as major surgical procedures, that are typically reported with other ancillary and adjunctive services. Also, similar to other APCs that have been converted to C-APCs, there are higher APC levels within the clinical family or related clinical family of these APCs that have previously been assigned to a C-APC. Table 4 of the proposed rule listed the proposed C-APCs for CY 2020. All C-APCs were displayed in Addendum J to the proposed rule (which is available via the internet on the CMS website). Addendum J to the proposed rule also contained all of the data related to the C-APC payment policy methodology, including the list of proposed complexity adjustments and other information.
We also are considering developing an episode-of-care for skin substitutes and are interested in comments regarding a future C-APC for procedures using skin substitute products furnished in the hospital outpatient department setting. We note that this comment solicitation is discussed in section V.B.7. of the proposed rule and this final rule with comment period.
Comment: Several commenters supported the creation of the two new proposed C-APCs, encouraging CMS to continue to evaluate outpatient charge and cost data for additions to the list of C-APCs during future rulemaking periods. One commenter requested that CMS closely monitor payments for the proposed C-APC 5461 (Level 1 Neurostimulator and Related Products) relative to costs of the procedure to ensure accurate compensation and availability in the ASC setting.
Response: We appreciate the commenters' support and note that we annually review the most recent data available to determine costs associated with furnishing a service and update payment rates accordingly.
Comment: We received comments requesting that CMS create a C-APC for autologous hematopoietic stem cell transplant similar to the C-APC established for allogeneic hematopoietic stem cell transplant. The commenters stated CMS' APC rate-setting process of using single and pseudo-single procedure claims results in an inadequately low APC payment rate for autologous stem cell transplant and believed that the creation of a C-APC for autologous hematopoietic stem cell transplant would improve payment rates by allowing a greater number of claims to be used in the rate setting process. The Advisory Panel on Hospital Outpatient Payment (HOP Panel) also recommended that CMS consider creating a comprehensive APC for autologous stem cell transplantation and that CMS provide a rationale if it decides not to create such an APC.
Response: We thank the commenter for this comment. In order to determine whether it would be appropriate to create a C-APC for autologous hematopoietic stem cell transplant, we modeled this change with APC 5242—Level 2 Blood Product Exchange and Related Services, which includes CPT code 38241 Hematopoietic progenitor cell (hpc); autologous transplantation as well as APC 5243—Level 3 Blood Product Exchange and Related Services, in keeping with our practice of converting APCs to C-APCs that have higher APC levels within the clinical family that are assigned to a C-APC.
After analyzing the results, we found that creating a C-APC for APC 5242 would increase the number of single claims available for ratesetting for this APC by approximately 8 percent, however creating new C-APCs in the Stem Cell Transplant clinical family would decrease the geometric mean cost of C-APC 5244—Level 4 Blood Product Exchange and Related Services by approximately 75 percent due to complexity adjustments of code combinations within the clinical family, specifically complexity adjustments from C-APC 5243 to C-APC 5244. Therefore, at this time we do not believe it is appropriate to create a C-APC for autologous hematopoietic stem cell transplant.
Comment: Two manufacturers of drugs used in ocular procedures requested that CMS discontinue the C-APC payment policy for existing C-APCs that include procedures involving their drugs and instead provide separate payment for the drugs. The manufacturer commenters believed that the C-APC packaging policy, which packages payment for certain drugs that are adjunctive to the primary service, results in underpayment for the drugs and violates the 2 times rule.
Response: We continue to believe that the procedures assigned to the proposed C-APCs, including the procedures involving the drugs used in ocular procedures mentioned by the commenters, are appropriately paid through a C-APC and the costs of drugs (as well as other items or services furnished with the procedures) are reflected in hospital billing, and therefore the rates that are established for the ocular procedures. As stated in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79584), procedures assigned to C-APCs are primary services (mostly major surgical procedures) that are typically the focus of the hospital outpatient stay. In addition, with regard to the packaging of the drugs based on the C-APC policy, as stated in previous rules (78 FR 74868 through 74869 and 74909 and 79 FR 66800), items included in the packaged payment provided with the primary “J1” service include all drugs, biologicals, and radiopharmaceuticals payable under the OPPS, regardless of cost, except those drugs with pass-through payment status. In accordance with section 1833(t)(2) of the Act and § 419.31 of the regulations, we annually review the items and services within an APC group to determine if there are any APC violations of the 2 times rule and whether there are any revisions to APC assignments that may be necessary or any exceptions that should be made.
Comment: Several commenters, including device manufacturer associations, expressed concern that the C-APC payment rates may not adequately reflect the costs associated with services and requested that CMS not establish any additional C-APCs. These comments questioned the broader C-APC payment methodology, ratesetting accuracy, the impact of C-APCs on broader agency objectives, and recommended methodological changes to better capture costs of providing comprehensive services before further expansion. Some commenters were concerned that hospital are not correctly charging for procedures assigned to C-APCs and urged CMS to invest in policies and education for hospitals regarding correct billing patterns. These commenters also requested that CMS provide an analysis of the impact of the C-APC policy on affected procedures and patient access to services.
Response: We appreciate the comments. We continue to believe that the proposed new C-APCs for CY 2020 are appropriate to be added to the existing C-APC payment policy. We also note that, in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59246), we conducted an analysis of the effects of the C-APC policy. The analysis looked at data from CY 2016 OPPS/ASC final rule with comment period, the CY 2017 OPPS/ASC final rule with comment period, and the CY 2018 OPPS/ASC proposed rule, which involved claims data from CY 2014 (before C-APCs became effective) to CY 2016. We looked at separately payable codes that were then assigned to C-APCs and, overall, we observed an increase in claim line frequency, units billed, and Medicare payment for those procedures, which suggest that the C-APC payment policy did not adversely affect access to care or reduce payments to hospitals.
Comment: One commenter requested that CMS discontinue the C-APC payment policy for single session stereotactic radiosurgery (SRS) procedures, stating concerns that the C-APC methodology does not account for the complexity of delivering radiation therapy and fails to capture appropriately coded claims. The commenters also requested that CMS continue to make separate payments for the 10 planning and preparation codes related to SRS and include the HCPCS code for IMRT planning (77301) on the list of planning and preparation codes, stating that the service has become more common in single fraction radiosurgery treatment planning.
Response: At this time, we do not believe that it is necessary to discontinue the C-APCs that include single session SRS procedures. We continue to believe that the C-APC policy is appropriately applied to these surgical procedures for the reasons cited when this policy was first adopted and note that the commenters did not provide any empirical evidence to support their claims that the existing C-APC policy does not adequately pay for these procedures. Also, we will continue in CY 2020 to pay separately for the 10 planning and preparation services (HCPCS codes 70551, 70552, 70553, 77011, 77014, 77280, 77285, 77290, 77295, and 77336) adjunctive to the delivery of the SRS treatment using either the Cobalt-60-based or LINAC based technology when furnished to a beneficiary within 1 month of the SRS treatment for CY 2020 (82 FR 59242 and 59243).
Comment: Several commenters requested that CMS discontinue the C-APC payment policy for all surgical insertion codes required for brachytherapy treatment. The commenters stated concerns about how the C-APC methodology impacts radiation oncology, particularly the delivery of brachytherapy for the treatment of cervical cancer. They also stated that they oppose C-APC payment for cancer care given the complexity of coding, serial billing for cancer care, and potentially different sites of service for the initial surgical device insertion and subsequent treatment delivery or other supportive services.
Response: While we continue to believe that the C-APC policy is appropriately applied to these surgical procedures, we will continue to examine these concerns and will determine if any modifications to this policy are warranted in future rulemaking.
Comment: We received requests for clarifications related to C-APC 8011 Comprehensive Observation Services (status indicator “J2”). One commenter requested that CMS clarify the distinction between status indicators for “V” and “J2”. Another commenter questioned the rationale for the established criteria for payment through C-APC 8011, specifically the requirement that the claim does not contain a procedure described by a HCPCS code to which we have assigned status indicator “T” that is reported with a date of service on the same day or 1 day earlier than the date of service associated with services described by HCPCS code G0378.
Response: The comprehensive observation services C-APC (C-APC 8011) was established in CY 2016 (80 FR 70333 through 70336) to provide payment for extended assessment and management encounters. C-APC 8011 is paid and status indicator “J2” is assigned when a specific combination of services is performed. This combination of services was described in previous rulemaking (80 FR 70333 through 70336) in detail and is repeated for clarity below. Specifically, we make a payment through C-APC 8011 for a claim that:
- Does not contain a procedure described by a HCPCS code to which we have assigned status indicator “T;”
- Contains 8 or more units of services described by HCPCS code G0378 (Hospital observation services, per hour);
- Contains services provided on the same date of service or 1 day before the date of service for HCPCS code G0378 that are described by one of the following codes: HCPCS code G0379 (Direct admission of patient for hospital observation care) on the same date of service as HCPCS code G0378; CPT code 99281 (Emergency department visit for the evaluation and management of a patient (Level 1)); CPT code 99282 (Emergency department visit for the evaluation and management of a patient (Level 2)); CPT code 99283 (Emergency department visit for the evaluation and management of a patient (Level 3)); CPT code 99284 (Emergency department visit for the evaluation and management of a patient (Level 4)); CPT code 99285 (Emergency department visit for the evaluation and management of a patient (Level 5)) or HCPCS code G0380 (Type B emergency department visit (Level 1)); HCPCS code G0381 (Type B emergency department visit (Level 2)); HCPCS code G0382 (Type B emergency department visit (Level 3)); HCPCS code G0383 (Type B emergency department visit (Level 4)); HCPCS code G0384 (Type B emergency department visit (Level 5)); CPT code 99291 (Critical care, evaluation and management of the critically ill or critically injured patient; first 30-74 minutes); or HCPCS code G0463 (Hospital outpatient clinic visit for assessment and management of a patient); and
- Does not contain services described by a HCPCS code to which we have assigned status indicator “J1'.'
The assignment of status indicator “J2” results in a single prospective payment for the comprehensive observation services based on the costs of all reported services on the claim. We make payment for all other items and services reported on the hospital outpatient claim as being adjunctive to the specific combination of observation services. The assignment of status indicator “V” describes a clinic or emergency department visit. It does not describe services paid through a comprehensive APC and it will not trigger payment through C-APC 8011.
With regard to the comment questioning the rationale for the requirement that the claim does not contain a procedure described by a HCPCS code to which we have assigned status indicator “T” that is reported with a date of service on the same day or 1 day earlier than the date of service associated with services described by HCPCS code G0378 in order to be paid through C-APC 8011, this criterion was incorrectly quoted as the final policy in the CY 2020 OPPS/ASC proposed rule (84 FR 39412). This language has been updated in this final rule with comment period. This criterion was proposed in the CY 2016 OPPS/ASC proposed rule, however a modification of this criterion was finalized. We refer readers to the discussion of the establishment of C-APC 8011 in the CY 2016 OPPS/ASC Final Rule with comment period (80 FR 70335-70336). In this rule, we stated in response to commenters' concerns regarding packaging payment for potentially high-cost surgical procedures into the payment for an observation C-APC, we finalized a policy that claims reporting procedures assigned status indicator “T” should not qualify for payment through C-APC 8011, regardless of whether the procedure assigned status indicator “T” was furnished before or after observation services (described by HCPCS code G0378) were provided. We state the final criteria for assignment for payment through C-APC 8011 in the CY 2016 OPPS/ASC final rule with comment period, including that the claims must not contain a procedure described by a HCPCS code to which we have assigned status indicator “T” (80 FR 70335).
After consideration of the public comments we received, we are finalizing the proposed C-APCs for CY 2020. Table 4 below lists the final C-APCs for CY 2020. All C-APCs are displayed in Addendum J to this final rule with comment period (which is available via the internet on the CMS website). Addendum J to this final rule with comment period also contains all of the data related to the C-APC payment policy methodology, including the list of complexity adjustments and other information for CY 2020.


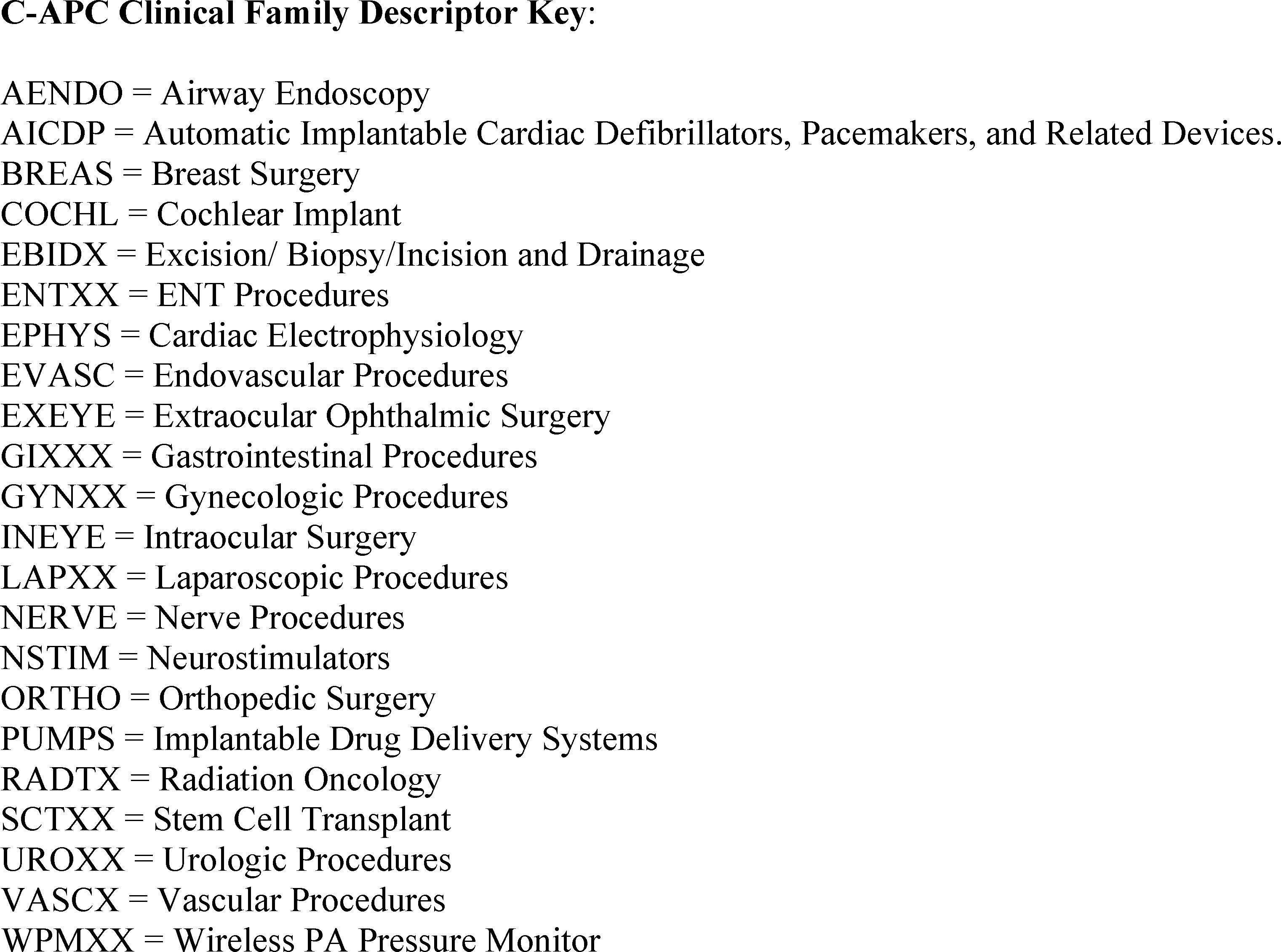
(3) Exclusion of Procedures Assigned to New Technology APCs from the C-APC Policy
Services that are assigned to New Technology APCs are typically new procedures that do not have sufficient claims history to establish an accurate payment for the procedures. Beginning in CY 2002, we retain services within New Technology APC groups until we gather sufficient claims data to enable us to assign the service to an appropriate clinical APC. This policy allows us to move a service from a New Technology APC in less than 2 years if sufficient data are available. It also allows us to retain a service in a New Technology APC for more than 2 years if sufficient data upon which to base a decision for reassignment have not been collected (82 FR 59277).
The C-APC payment policy packages payment for adjunctive and secondary items, services, and procedures into the most costly primary procedure under the OPPS at the claim level. Prior to CY 2019 when a procedure assigned to a New Technology APC was included on the claim with a primary procedure, identified by OPPS status indicator “J1”, payment for the new technology service was typically packaged into the payment for the primary procedure. Because the new technology service was not separately paid in this scenario, the overall number of single claims available to determine an appropriate clinical APC for the new service was reduced. This was contrary to the objective of the New Technology APC payment policy, which is to gather sufficient claims data to enable us to assign the service to an appropriate clinical APC.
For example, for CY 2017, there were seven claims generated for HCPCS code 0100T (Placement of a subconjunctival retinal prosthesis receiver and pulse generator, and implantation of intraocular retinal electrode array, with vitrectomy), which involves the use of the Argus® II Retinal Prosthesis System. However, several of these claims were not available for ratesetting because HCPCS code 0100T was reported with a “J1” procedure and, therefore, payment was packaged into the associated C-APC payment. If these services had been separately paid under the OPPS, there would be at least two additional single claims available for ratesetting. As mentioned previously, the purpose of the new technology APC policy is to ensure that there are sufficient claims data for new services, which is particularly important for services with a low volume such as procedures described by HCPCS code 0100T. Another concern is the costs reported for the claims when payment is not packaged for a new technology procedure may not be representative of all of the services included on a claim that is generated, which may also affect our ability to assign the new service to the most appropriate clinical APC.
To address this issue and help ensure that there is sufficient claims data for services assigned to New Technology APCs, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58847), we proposed excluded payment for any procedure that is assigned to a New Technology APC (APCs 1491 through 1599 and APCs 1901 through 1908) from being packaged when included on a claim with a “J1” service assigned to a C-APC. For CY 2020, we proposed to continue to exclude payment for any procedure that is assigned to a New Technology APC from being packaged when included on a claim with a “J1” service assigned to a C-APC.
Some stakeholders have raised questions about whether the policy established in the CY 2019 OPPS/ASC final rule with comment period would also apply to comprehensive observation services assigned status indicator “J2.” We recognize that the policy described and adopted in the CY 2019 rulemaking may have been ambiguous with respect to this issue. While our intention in the CY 2019 rulemaking was only to exclude payment for services assigned to New Technology APCs from being bundled into the payment for a comprehensive “J1” service, we believe that there may also be some instances in which it would be clinically appropriate to provide a new technology service when providing comprehensive observation services. We would not generally expect that to be the case, because procedures assigned to New Technology APCs typically are new or low-volume surgical procedures, or are specialized tests to diagnosis a specific condition. In addition, it is highly unlikely a general observation procedure would be assigned to a New Technology APC because there are clinical APCs already established under the OPPS to classify general observation procedures. As we stated in the CY 2016 OPPS/ASC final rule with comment period, observation services may not be used for post-operative recovery and, as such, observation services furnished with services assigned to status indicator “T” will always be packaged (80 FR 70334). Therefore, we proposed that payment for services assigned to a New Technology APC when included on a claim for a service assigned status indicator “J2” assigned to a C-APC will be packaged into the payment for the comprehensive service. Nonetheless, we sought public comments on whether it would be clinically appropriate to exclude payment for any New Technology APC procedures from being packaged into the payment for a comprehensive “J2” service starting in CY 2020.
Comment: Several commenters, including device manufacturers, device manufacturer associations and physicians were opposed to our proposal to package payment for procedures assigned to a New Technology APC into the payment for comprehensive observation services assigned status indicator “J2”. The commenters stated that there were instances where beneficiaries receiving observation services may require the types of procedures that are assigned to new technology APCs. Several commenters specifically mentioned the HeartFlow Analysis, and stated that it could be performed appropriately for a patient receiving observation services. The commenters also stated that providing separate payment for this new technology procedure will allow CMS to collect sufficient claims data to enable assignment of the procedure to an appropriate clinical APC.
Response: We appreciate the stakeholders' comments regarding this proposal and agree that, although rare, there are situations in which it is clinically appropriate to provide a new technology service when providing comprehensive observation services. As discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58847), the purpose of the new technology APC policy is to ensure that there are sufficient claims data for new services to assign these procedures to an appropriate clinical APC and therefore, we excluded procedures assigned to New Technology APCs from packaging under the C-APC policy. In the CY 2019 final rule, we specifically stated that the exclusion policy included circumstances when New Technology procedures were billed with comprehensive services assigned to status indicator “J1”, however we believe this rationale is also applicable to comprehensive observation services that are assigned status indicator “J2”. Therefore, we are modifying our policy for excluding procedures assigned to New Technology APCs from the C-APC policy. For CY 2020, we are finalizing our policy to continue to exclude payment for any procedure that is assigned to a New Technology APC from being packaged when included on a claim with a “J1” service assigned to a C-APC. For CY 2020, we are also finalizing a policy to exclude payment for any procedures that are assigned to a New Technology APC from being packaged into the payment for comprehensive observation services assigned to status indicator “J2” when they are included on a claim with “J2” procedures.
c. Calculation of Composite APC Criteria-Based Costs
As discussed in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66613), we believe it is important that the OPPS enhance incentives for hospitals to provide necessary, high quality care as efficiently as possible. For CY 2008, we developed composite APCs to provide a single payment for groups of services that are typically performed together during a single clinical encounter and that result in the provision of a complete service. Combining payment for multiple, independent services into a single OPPS payment in this way enables hospitals to manage their resources with maximum flexibility by monitoring and adjusting the volume and efficiency of services themselves. An additional advantage to the composite APC model is that we can use data from correctly coded multiple procedure claims to calculate payment rates for the specified combinations of services, rather than relying upon single procedure claims which may be low in volume and/or incorrectly coded. Under the OPPS, we currently have composite policies for mental health services and multiple imaging services. (We note that, in the CY 2018 OPPS/ASC final rule with comment period, we finalized a policy to delete the composite APC 8001 (LDR Prostate Brachytherapy Composite) for CY 2018 and subsequent years.) We refer readers to the CY 2008 OPPS/ASC final rule with comment period (72 FR 66611 through 66614 and 66650 through 66652) for a full discussion of the development of the composite APC methodology, and the CY 2012 OPPS/ASC final rule with comment period (76 FR 74163) and the CY 2018 OPPS/ASC final rule with comment period (82 FR 59241 through 59242 and 59246 through 52950) for more recent background.
(1) Mental Health Services Composite APC
In the CY 2020 OPPS/ASC proposed rule (84 FR 39398), we proposed to continue our longstanding policy of limiting the aggregate payment for specified less resource-intensive mental health services furnished on the same date to the payment for a day of partial hospitalization services provided by a hospital, which we consider to be the most resource-intensive of all outpatient mental health services. We refer readers to the April 7, 2000 OPPS final rule with comment period (65 FR 18452 through 18455) for the initial discussion of this longstanding policy and the CY 2012 OPPS/ASC final rule with comment period (76 FR 74168) for more recent background.
In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79588 through 79589), we finalized a policy to combine the existing Level 1 and Level 2 hospital-based PHP APCs into a single hospital-based PHP APC, and thereby discontinue APCs 5861 (Level 1—Partial Hospitalization (3 services) for Hospital-Based PHPs) and 5862 (Level—2 Partial Hospitalization (4 or more services) for Hospital-Based PHPs) and replace them with APC 5863 (Partial Hospitalization (3 or more services per day)).
In the CY 2018 OPPS/ASC proposed rule and final rule with comment period (82 FR 33580 through 33581 and 59246 through 59247, respectively), we proposed and finalized the policy for CY 2018 and subsequent years that, when the aggregate payment for specified mental health services provided by one hospital to a single beneficiary on a single date of service, based on the payment rates associated with the APCs for the individual services, exceeds the maximum per diem payment rate for partial hospitalization services provided by a hospital, those specified mental health services will be paid through composite APC 8010 (Mental Health Services Composite). In addition, we set the payment rate for composite APC 8010 for CY 2018 at the same payment rate that will be paid for APC 5863, which is the maximum partial hospitalization per diem payment rate for a hospital, and finalized a policy that the hospital will continue to be paid the payment rate for composite APC 8010. Under this policy, the I/OCE will continue to determine whether to pay for these specified mental health services individually, or to make a single payment at the same payment rate established for APC 5863 for all of the specified mental health services furnished by the hospital on that single date of service. We continue to believe that the costs associated with administering a partial hospitalization program at a hospital represent the most resource intensive of all outpatient mental health services. Therefore, we do not believe that we should pay more for mental health services under the OPPS than the highest partial hospitalization per diem payment rate for hospitals.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39398), for CY 2020, we proposed that when the aggregate payment for specified mental health services provided by one hospital to a single beneficiary on a single date of service, based on the payment rates associated with the APCs for the individual services, exceeds the maximum per diem payment rate for partial hospitalization services provided by a hospital, those specified mental health services would be paid through composite APC 8010 for CY 2020. In addition, we proposed to set the proposed payment rate for composite APC 8010 at the same payment rate that we proposed for APC 5863, which is the maximum partial hospitalization per diem payment rate for a hospital, and that the hospital continue to be paid the proposed payment rate for composite APC 8010.
We did not receive any public comment on these proposals. Therefore, we are finalizing our proposal, without modification, that when the aggregate payment for specified mental health services provided by one hospital to a single beneficiary on a single date of service, based on the payment rates associated with the APCs for the individual services, exceeds the maximum per diem payment rate for partial hospitalization services provided by a hospital, those specified mental health services would be paid through composite APC 8010 for CY 2020. In addition, we are finalizing our proposal to set the payment rate for composite APC 8010 for CY 2020 at the same payment rate that we set for APC 5863, which is the maximum partial hospitalization per diem payment rate for a hospital.
(2) Multiple Imaging Composite APCs (APCs 8004, 8005, 8006, 8007, and 8008)
Effective January 1, 2009, we provide a single payment each time a hospital submits a claim for more than one imaging procedure within an imaging family on the same date of service, in order to reflect and promote the efficiencies hospitals can achieve when performing multiple imaging procedures during a single session (73 FR 41448 through 41450). We utilize three imaging families based on imaging modality for purposes of this methodology: (1) Ultrasound; (2) computed tomography (CT) and computed tomographic angiography (CTA); and (3) magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA). The HCPCS codes subject to the multiple imaging composite policy and their respective families are listed in Table 12 of the CY 2014 OPPS/ASC final rule with comment period (78 FR 74920 through 74924).
While there are three imaging families, there are five multiple imaging composite APCs due to the statutory requirement under section 1833(t)(2)(G) of the Act that we differentiate payment for OPPS imaging services provided with and without contrast. While the ultrasound procedures included under the policy do not involve contrast, both CT/CTA and MRI/MRA scans can be provided either with or without contrast. The five multiple imaging composite APCs established in CY 2009 are:
- APC 8004 (Ultrasound Composite);
- APC 8005 (CT and CTA without Contrast Composite);
- APC 8006 (CT and CTA with Contrast Composite);
- APC 8007 (MRI and MRA without Contrast Composite); and
- APC 8008 (MRI and MRA with Contrast Composite).
We define the single imaging session for the “with contrast” composite APCs as having at least one or more imaging procedures from the same family performed with contrast on the same date of service. For example, if the hospital performs an MRI without contrast during the same session as at least one other MRI with contrast, the hospital will receive payment based on the payment rate for APC 8008, the “with contrast” composite APC.
We make a single payment for those imaging procedures that qualify for payment based on the composite APC payment rate, which includes any packaged services furnished on the same date of service. The standard (noncomposite) APC assignments continue to apply for single imaging procedures and multiple imaging procedures performed across families. For a full discussion of the development of the multiple imaging composite APC methodology, we refer readers to the CY 2009 OPPS/ASC final rule with comment period (73 FR 68559 through 68569).
In the CY 2020 OPPS/ASC proposed rule (84 FR 39398), we proposed to continue to pay for all multiple imaging procedures within an imaging family performed on the same date of service using the multiple imaging composite APC payment methodology. We stated that we continue to believe that this policy would reflect and promote the efficiencies hospitals can achieve when performing multiple imaging procedures during a single session.
The proposed CY 2020 payment rates for the five multiple imaging composite APCs (APCs 8004, 8005, 8006, 8007, and 8008) were based on proposed geometric mean costs calculated from CY 2018 claims available for the CY 2020 OPPS/ASC proposed rule that qualified for composite payment under the current policy (that is, those claims reporting more than one procedure within the same family on a single date of service). To calculate the proposed geometric mean costs, we used the same methodology that we have used to calculate the geometric mean costs for these composite APCs since CY 2014, as described in the CY 2014 OPPS/ASC final rule with comment period (78 FR 74918). The imaging HCPCS codes referred to as “overlap bypass codes” that we removed from the bypass list for purposes of calculating the proposed multiple imaging composite APC geometric mean costs, in accordance with our established methodology as stated in the CY 2014 OPPS/ASC final rule with comment period (78 FR 74918), were identified by asterisks in Addendum N to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website) and were discussed in more detail in section II.A.1.b. of the CY 2020 OPPS/ASC proposed rule.
For the CY 2020 OPPS/ASC proposed rule, we were able to identify approximately 700,000 “single session” claims out of an estimated 4.9 million potential claims for payment through composite APCs from our ratesetting claims data, which represents approximately 14 percent of all eligible claims, to calculate the proposed CY 2020 geometric mean costs for the multiple imaging composite APCs. Table 5 of the CY 2020 OPPS/ASC proposed rule listed the proposed HCPCS codes that would be subject to the multiple imaging composite APC policy and their respective families and approximate composite APC proposed geometric mean costs for CY 2020.
We did not receive any public comments on these proposals. Therefore, we are finalizing our proposal to continue the use of multiple imaging composite APCs to pay for services providing more than one imaging procedure from the same family on the same date, without modification. Table 6 below lists the HCPCS codes that will be subject to the multiple imaging composite APC policy and their respective families and approximate composite APC final geometric mean costs for CY 2020.





3. Changes to Packaged Items and Services
a. Background and Rationale for Packaging in the OPPS
Like other prospective payment systems, the OPPS relies on the concept of averaging to establish a payment rate for services. The payment may be more or less than the estimated cost of providing a specific service or a bundle of specific services for a particular beneficiary. The OPPS packages payments for multiple interrelated items and services into a single payment to create incentives for hospitals to furnish services most efficiently and to manage their resources with maximum flexibility. Our packaging policies support our strategic goal of using larger payment bundles in the OPPS to maximize hospitals' incentives to provide care in the most efficient manner. For example, where there are a variety of devices, drugs, items, and supplies that could be used to furnish a service, some of which are more costly than others, packaging encourages hospitals to use the most cost-efficient item that meets the patient's needs, rather than to routinely use a more expensive item, which may occur if separate payment is provided for the item.
Packaging also encourages hospitals to effectively negotiate with manufacturers and suppliers to reduce the purchase price of items and services or to explore alternative group purchasing arrangements, thereby encouraging the most economical health care delivery. Similarly, packaging encourages hospitals to establish protocols that ensure that necessary services are furnished, while scrutinizing the services ordered by practitioners to maximize the efficient use of hospital resources. Packaging payments into larger payment bundles promotes the predictability and accuracy of payment for services over time. Finally, packaging may reduce the importance of refining service-specific payment because packaged payments include costs associated with higher cost cases requiring many ancillary items and services and lower cost cases requiring fewer ancillary items and services. Because packaging encourages efficiency and is an essential component of a prospective payment system, packaging payments for items and services that are typically integral, ancillary, supportive, dependent, or adjunctive to a primary service has been a fundamental part of the OPPS since its implementation in August 2000. For an extensive discussion of the history and background of the OPPS packaging policy, we refer readers to the CY 2000 OPPS final rule (65 FR 18434), the CY 2008 OPPS/ASC final rule with comment period (72 FR 66580), the CY 2014 OPPS/ASC final rule with comment period (78 FR 74925), the CY 2015 OPPS/ASC final rule with comment period (79 FR 66817), the CY 2016 OPPS/ASC final rule with comment period (80 FR 70343), the CY 2017 OPPS/ASC final rule with comment period (81 FR 79592), the CY 2018 OPPS/ASC final rule with comment period (82 FR 59250), and the CY 2019 OPPS/ASC final rule with comment period (83 FR 58854). As we continue to develop larger payment groups that more broadly reflect services provided in an encounter or episode of care, we have expanded the OPPS packaging policies. Most, but not necessarily all, categories of items and services currently packaged in the OPPS are listed in 42 CFR 419.2(b). Our overarching goal is to make payments for all services under the OPPS more consistent with those of a prospective payment system and less like those of a per-service fee schedule, which pays separately for each coded item. As a part of this effort, we have continued to examine the payment for items and services provided under the OPPS to determine which OPPS services can be packaged to further achieve the objective of advancing the OPPS toward a more prospective payment system.
For CY 2020, we examined the items and services currently provided under the OPPS, reviewing categories of integral, ancillary, supportive, dependent, or adjunctive items and services for which we believe payment would be appropriately packaged into payment for the primary service that they support. Specifically, we examined the HCPCS code definitions (including CPT code descriptors) and outpatient hospital billing patterns to determine whether there were categories of codes for which packaging would be appropriate according to existing OPPS packaging policies or a logical expansion of those existing OPPS packaging policies. In the CY 2020 OPPS/ASC proposed rule (84 FR 39423 through 39424), beginning in CY 2020, we proposed to conditionally package the costs of selected newly identified ancillary services into payment with a primary service where we believe that the packaged item or service is integral, ancillary, supportive, dependent, or adjunctive to the provision of care that was reported by the primary service HCPCS code. Below we discuss the proposed and finalized changes to the packaging policies beginning in CY 2020.
Comment: We received several comments from patient advocates, physicians, drug manufacturers, and professional medical societies regarding payment for blue light cystoscopy procedures involving Cysview® (hexaminolevulinate HCl) (described by HCPCS code C9275). Cysview® is a drug that functions as a supply in a diagnostic test or procedure and therefore payment for this product is packaged with payment for the primary procedure in the OPPS and ASC settings. Commenters stated that utilization of Cysview® is low in the HOPD and ASC settings, which they attributed to the packaging of Cysview as a drug that functions as a supply in a diagnostic test or procedure. Commenters indicated that packaged payment does not adequately pay for the blue light cystoscopy procedures, particularly in the ASC setting where payment is generally approximately 55 percent of the HOPD payment. Commenters believe that providers have been deterred from the use of this technology, especially in the ASC, and as a result a significant percentage of beneficiaries are not able to access the procedure.
Commenters also stated that there has been literature published showing that Blue Light Cystoscopy with Cysview® is more effective than white light cystoscopy alone at detecting and eliminating nonmuscle invasive bladder cancer tumors, leading to a reduction in bladder cancer recurrence.
Commenters made various recommendations for payment for blue light cystoscopy procedures involving Cysview®, including to pay separately for Cysview® when it is used with blue light cystoscopy in the HOPD and ASC settings, to pay separately for Cysview® when it is used with blue light cystoscopy in the ASC setting, similar to the policy finalized for Exparel® in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58860), or to utilize our equitable adjustment authority at section 1833(t)(2)(E) of the Act to provide an “add-on” or “drug intensive” payment to ASCs when using Cysview® in blue light cystoscopy procedures. Other commenters requested separate payment for all diagnostic imaging drugs (radiopharmaceuticals and contrast agents).
Response: We acknowledge the concerns of the numerous stakeholders who commented on this issue and understand the importance of blue light cystoscopy procedures involving Cysview®. Cysview has been packaged as a drug, biological, or radiopharmaceutical that functions as a supply in a diagnostic test or procedure since CY 2014 (78 FR 74930). As we stated in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59244), we recognize that blue light cystoscopy represents an additional elective but distinguishable service as compared to white light cystoscopy that, in some cases, may allow greater detection of bladder tumors in beneficiaries relative to white light cystoscopy alone. Given the additional equipment, supplies, operating room time, and other resources required to perform blue light cystoscopy in addition to white light cystoscopy, in CY 2018, we created a new HCPCS C-code to describe blue light cystoscopy and since CY 2018 have allowed for complexity adjustments to higher paying C-APCs for qualifying white light and blue light cystoscopy code combinations. At this time, we continue to believe that Cysview® is a drug that functions as a supply in a diagnostic test or procedure and payment for this drug is packaged with payment for the diagnostic procedure. Therefore, we do not believe it is necessary to pay separately for Cysview® when it is used with blue light cystoscopy in either the HOPD or ASC setting. We also do not believe that it would be appropriate to utilize our equitable adjustment authority at section 1833(t)(2)(E) of the Act to provide an “add-on” or “drug intensive” payment to ASCs when using Cysview® in blue light cystoscopy procedures nor do we have any evidence to show that separate payment for all diagnostic imaging drugs (radiopharmaceuticals, contrast agents) is required. However, we will continue to examine payment for blue light cystoscopy procedures involving Cysview to determine if any changes to this policy would be appropriate in future rulemaking.
Comment: Some commenters requested that we eliminate the packaging policy for drugs that function as a supply when used in a diagnostic test or procedure.
Response: In the CY 2014 OPPS/ASC final rule with comment period, we established a policy to package drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure. In particular, we referred to drugs, biologicals, and radiopharmaceuticals that function as supplies as a part of a larger, more encompassing service or procedure, namely, the diagnostic test or procedure in which the drug, biological, or radiopharmaceutical is employed (78 FR 74927). At this time, we do not believe it is necessary to eliminate this policy. As previously noted, the OPPS packages payments for multiple interrelated items and services into a single payment to create incentives for hospitals to furnish services most efficiently and to manage their resources with maximum flexibility. Our packaging policies support our strategic goal of using larger payment bundles in the OPPS to maximize hospitals' incentives to provide care in the most efficient manner.
Comment: One commenter requested separate payment for add-on codes for Fractional Flow Reserve Studies (FFR/iFR) and Intravascular Ultrasound (IVUS). The commenter stated that they believe the packaging of these codes will disincentivize physicians to perform these adjunct procedures because of cost. The codes include:
- 93571—Intravascular doppler velocity and/or pressure derived coronary flow reserve measurement (coronary vessel or graft) during coronary angiography including pharmacologically induced stress; initial vessel (list separately in addition to code for primary procedure);
- 93572—Intravascular doppler velocity and/or pressure derived coronary flow reserve measurement (coronary vessel or graft) during coronary angiography including pharmacologically induced stress; each additional vessel (list separately in addition to code for primary procedure));
- 92978—Endoluminal imaging of coronary vessel or graft using intravascular ultrasound (ivus) or optical coherence tomography (oct) during diagnostic evaluation and/or therapeutic intervention including imaging supervision, interpretation and report; initial vessel (list separately in addition to code for primary procedure); and
- 92979—Endoluminal imaging of coronary vessel or graft using intravascular ultrasound (ivus) or optical coherence tomography (oct) during diagnostic evaluation and/or therapeutic intervention including imaging supervision, interpretation and report; each additional vessel (list separately in addition to code for primary procedure)).
Response: As stated in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66630), we continue to believe that IVUS and FFR are dependent services that are always provided in association with a primary service. Add-on codes represent services that are integral, ancillary, supportive, dependent, or adjunctive items and services for which we believe payment would be appropriately packaged into payment for the primary service that they support. As we have noted in past rules, add-on codes do not represent standalone procedures and are inclusive to other procedures performed at the same time (79 FR 66818). We continue to believe it is unnecessary to provide separate payment for the previously mentioned add-on codes at this time.
b. Packaging Policy for Non-Opioid Pain Management Treatments
(1) Background on OPPS/ASC Non-Opioid Pain Management Packaging Policies
In the CY 2018 OPPS/ASC proposed rule (82 FR 33588), within the framework of existing packaging categories, such as drugs that function as supplies in a surgical procedure or diagnostic test or procedure, we requested stakeholder feedback on common clinical scenarios involving currently packaged items and services described by HCPCS codes that stakeholders believe should not be packaged under the OPPS. We also expressed interest in stakeholder feedback on common clinical scenarios involving separately payable HCPCS codes for which payment would be most appropriately packaged under the OPPS. Commenters who responded to the CY 2018 OPPS/ASC proposed rule expressed a variety of views on packaging under the OPPS. In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59255), we summarized these public comments. The public comments ranged from requests to unpackage most items and services that are either conditionally or unconditionally packaged under the OPPS, including drugs and devices, to specific requests for separate payment for a specific drug or device.
In terms of Exparel® in particular, we received several requests to pay separately for the drug Exparel® rather than packaging payment for it as a surgical supply. We had previously stated that we considered Exparel® to be a drug that functions as a surgical supply because it is indicated for the alleviation of postoperative pain (79 FR 66874 and 66875). We had also stated before that we considered all items related to the surgical outcome and provided during the hospital stay in which the surgery is performed, including postsurgical pain management drugs, to be part of the surgery for purposes of our drug and biological surgical supply packaging policy. (We note that Exparel® is a liposome injection of bupivacaine, an amide local anesthetic, indicated for single-dose infiltration into the surgical site to produce postsurgical analgesia. In 2011, Exparel® was approved by FDA for single-dose infiltration into the surgical site to provide postsurgical analgesia.[1 2] Exparel® had pass-through payment status from CYs 2012 through 2014 and was separately paid under both the OPPS and the ASC payment system during this 3-year period. Beginning in CY 2015, Exparel® was packaged as a surgical supply under both the OPPS and the ASC payment system.)
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 52485, we reiterated our position with regard to payment for Exparel®, stating that we believed that payment for this drug is appropriately packaged with the primary surgical procedure. We also stated in the CY 2018 OPPS/ASC final rule with comment period that CMS would continue to explore and evaluate packaging policies under the OPPS and consider these policies in future rulemaking.
In addition to stakeholder feedback regarding OPPS packaging policies in response to the CY 2019 OPPS/ASC proposed rule, the President's Commission on Combating Drug Addiction and the Opioid Crisis (the Commission) had recommended that CMS examine payment policies for certain drugs that function as a supply, specifically non-opioid pain management treatments (83 FR 37068). The Commission was established in 2017 to study ways to combat and treat drug abuse, addiction, and the opioid crisis. The Commission's report [3] included a recommendation for CMS to “. . . review and modify ratesetting policies that discourage the use of non-opioid treatments for pain, such as certain bundled payments that make alternative treatment options cost prohibitive for hospitals and doctors, particularly those options for treating immediate postsurgical pain . . . .” [4] With respect to the packaging policy, the Commission's report states that “. . . the current CMS payment policy for `supplies' related to surgical procedures creates unintended incentives to prescribe opioid medications to patients for postsurgical pain instead of administering non-opioid pain medications. Under current policies, CMS provides one all-inclusive bundled payment to hospitals for all `surgical supplies,' which includes hospital administered drug products intended to manage patients' postsurgical pain. This policy results in the hospitals receiving the same fixed fee from Medicare whether the surgeon administers a non-opioid medication or not.” [5] HHS also presented an Opioid Strategy in April 2017 [6] that aims in part to support cutting-edge research and advance the practice of pain management. On October 26, 2017, the President declared the opioid crisis a national public health emergency under Federal law [7] and this declaration was most recently renewed on April 19, 2019.[8]
For the CY 2019 rulemaking, we reviewed available literature with respect to Exparel®, including a briefing document [9] submitted for FDA Advisory Committee Meeting held February 14-15, 2018, by the manufacturer of Exparel® that notes that “. . . Bupivacaine, the active pharmaceutical ingredient in Exparel®, is a local anesthetic that has been used for infiltration/field block and peripheral nerve block for decades” and that “since its approval, Exparel® has been used extensively, with an estimated 3.5 million patient exposures in the US.” [10] On April 6, 2018, FDA approved Exparel®'s new indication for use as an interscalene brachial plexus nerve block to produce postsurgical regional analgesia.[11] Therefore, we also stated in the CY 2019 OPPS/ASC proposed rule that, based on our review of currently available OPPS Medicare claims data and public information from the manufacturer of the drug, we did not believe that the OPPS packaging policy had discouraged the use of Exparel® for either of the drug's indications when furnished in the hospital outpatient department setting.
In the CY 2019 OPPS/ASC proposed rule, in response to stakeholder comments on the CY 2018 OPPS/ASC final rule with comment period (82 FR 52485) and in light of the recommendations regarding payment policies for certain drugs, we evaluated the impact of our packaging policy for drugs that function as a supply when used in a surgical procedure on the utilization of these drugs in both the hospital outpatient department and the ASC setting. Our packaging policy is that the costs associated with packaged drugs that function as a supply are included in the ratesetting methodology for the surgical procedures with which they are billed, and the payment rate for the associated procedure reflects the costs of the packaged drugs and other packaged items and services to the extent they are billed with the procedure. In our evaluation, we used currently available data to analyze the utilization patterns associated with specific drugs that function as a supply over a 5-year time period to determine whether this packaging policy reduced the use of these drugs. If the packaging policy discouraged the use of drugs that function as a supply or impeded access to these products, we would expect to see a significant decline in utilization of these drugs over time, although we note that a decline in utilization could also reflect other factors, such as the availability of alternative products, or a combination thereof.
The results of the evaluation of our packaging policies under the OPPS and the ASC payment system showed decreased utilization for certain drugs that function as a supply in the ASC setting, in comparison to the hospital outpatient department setting. In light of these results, as well as the Commission's recommendation to examine payment policies for non-opioid pain management drugs that function as a supply, we stated that we believe it was appropriate to pay separately for evidence-based non-opioid pain management drugs that function as a supply in a surgical procedure in the ASC setting to address the decreased utilization of these drugs and to encourage use of these types of drugs rather than prescription opioids. Therefore, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58855 through 58860), we finalized the proposed policy to unpackage and pay separately at ASP + 6 percent for the cost of non-opioid pain management drugs that function as surgical supplies when they are furnished in the ASC setting for CY 2019. We also stated that we would continue to analyze the issue of access to non-opioid alternatives in the hospital outpatient department setting and in the ASC setting as we implemented section 6082 of the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act (Pub. L. 115-271) enacted on October 24, 2018 (83 FR 58860 through 58861).
(2) Evaluation and CY 2020 Proposal for Payment for Non-Opioid Alternatives
Section 1833(t)(22)(A)(i) of the Act, as added by section 6082(a) of the SUPPORT Act, states that the Secretary must review payments under the OPPS for opioids and evidence-based non-opioid alternatives for pain management (including drugs and devices, nerve blocks, surgical injections, and neuromodulation) with a goal of ensuring that there are not financial incentives to use opioids instead of non-opioid alternatives. As part of this review, under section 1833(t)(22)(A)(iii) of the Act, the Secretary must consider the extent to which revisions to such payments (such as the creation of additional groups of covered OPD services to separately classify those procedures that utilize opioids and non-opioid alternatives for pain management) would reduce the payment incentives for using opioids instead of non-opioid alternatives for pain management. In conducting this review and considering any revisions, the Secretary must focus on covered OPD services (or groups of services) assigned to C-APCs, APCs that include surgical services, or services determined by the Secretary that generally involve treatment for pain management. If the Secretary identifies revisions to payments pursuant to section 1833(t)(22)(A)(iii) of the Act, section 1833(t)(22)(C) of the Act requires the Secretary to, as determined appropriate, begin making revisions for services furnished on or after January 1, 2020. Any revisions under this paragraph are required to be treated as adjustments for purposes of paragraph (9)(B), which requires any adjustments to be made in a budget neutral manner. Pursuant to these requirements, in our evaluation of whether there are payment incentives for using opioids instead of non-opioid alternatives, for the CY 2020 OPPS/ASC proposed rule, we used currently available data to analyze the payment and utilization patterns associated with specific non-opioid alternatives, including drugs that function as a supply, nerve blocks, and neuromodulation products, to determine whether our packaging policies have reduced the use of non-opioid alternatives. We focused on covered OPD services for this review, including services assigned to C-APCs, surgical APCs, and other pain management services. We believed that if the packaging policy discouraged the use of these non-opioid alternatives or impeded access to these products, we would expect to see a decline in the utilization over time, although we note that a decline in utilization could also reflect other factors, such as the availability of alternative products or a combination thereof.
We evaluated continuous peripheral nerve blocks and neuromodulation alternatives to determine if the current packaging policy represented a barrier to access. For each product, we examined the most recently available Medicare claims data. All of the alternatives examined showed consistent or increasing utilization in recent years, with no products showing decreases in utilization.
We also evaluated drugs that function as surgical supplies over a 6-year time period (CYs 2013 through 2018). During our evaluation, we did not observe significant declines in the total number of units used in the hospital outpatient department for a majority of the drugs included in our analysis. In fact, under the OPPS, we observed the opposite effect for several drugs that function as surgical supplies, including Exparel® (HCPCS code C9290). This trend indicates appropriate packaged payments that adequately reflect the cost of the drug and are not prohibiting beneficiary access.
From CYs 2013 through 2018, we found that there was an overall increase in the OPPS Medicare utilization of Exparel® of approximately 491 percent (from 2.3 million units to 13.6 million units) during this 6-year time period. The total number of claims reporting the use of Exparel® increased by 463 percent (from 10,609 claims to 59,724 claims) over this 6-year time period. This increase in utilization continued, even after the expiration of the 3-year period of pass-through payment status for this drug in 2014, resulting in a 109-percent overall increase in the total number of units used between CYs 2015 and 2018, from 6.5 million units to 13.6 million units. The number of claims reporting the use of Exparel® increased by 112 percent during this time period, from 28,166 claims to 59,724 claims.
The results of our review and evaluation of our claims data do not provide evidence to indicate that the OPPS packaging policy has had the unintended consequence of discouraging the use of non-opioid treatments for postsurgical pain management in the hospital outpatient department. Therefore, based on this data evaluation, we stated in the proposed rule that we do not believe that changes are necessary under the OPPS for the packaged drug policy for drugs that function as a surgical supply, nerve blocks, surgical injections, and neuromodulation products when used in a surgical procedure in the OPPS setting at this time.
For Exparel®, we reviewed claims data for development of the CY 2020 OPPS/ASC proposed rule and, based on these data and available literature, we concluded that there is no clear evidence that the OPPS packaging policy discourages the use of Exparel® for either of the drug's indications in the hospital outpatient department setting because the use of Exparel® continues to increase in this setting. Accordingly, we stated in the proposed rule that we continue to believe it is appropriate to package payment for the use of Exparel®, as we do for other postsurgical pain management drugs, when it is furnished in a hospital outpatient department. In addition, our updated review of claims data for the proposed rule showed a continued decline in the utilization of Exparel® in the ASC setting, which we believed supports our proposal to continue paying separately for Exparel® in the ASC setting.
Therefore, for CY 2020, we proposed to continue our policy to pay separately at ASP+6 percent for the cost of non-opioid pain management drugs that function as surgical supplies in the performance of surgical procedures when they are furnished in the ASC setting and to continue to package payment for non-opioid pain management drugs that function as surgical supplies in the performance of surgical procedures in the hospital outpatient department setting for CY 2020. However, we invited public comments on this proposal and asked the public to provide peer-reviewed evidence, if any, to describe existing evidence-based non-opioid pain management therapies used in the outpatient and ASC setting. We also invited the public to provide detailed claims-based evidence to document how specific unfavorable utilization trends are due to the financial incentives of the payment systems rather than other factors.
Multiple stakeholders, largely manufacturers of devices and drugs, requested separate payments for various non-opioid pain management treatments, such as continuous nerve blocks (including a disposable elastomeric pump that delivers non-opioid local anesthetic to a surgical site or nerve), cooled thermal radiofrequency ablation, and local anesthetics designed to reduce postoperative pain for cataract surgery and other procedures. These stakeholders suggested various mechanisms through which separate payment or a higher-paying APC assignment for the primary service could be made. The stakeholders offered surveys, reports, studies, and anecdotal evidence of varying degrees to support why the devices, drugs, or services offer an alternative to or a reduction of the need for opioid prescriptions. The majority of these stakeholder offerings lacked adequate sample size, contained possible conflicts of interest such as studies conducted by employees of device manufacturers, have not been fully published in peer-reviewed literature, or have only provided anecdotal evidence as to how the drug or device could serve as an alternative to, or reduce the need for, opioid prescriptions.
After reviewing the data from stakeholders and Medicare claims data, we did not find compelling evidence to suggest that revisions to our OPPS payment policies for non-opioid pain management alternatives are necessary for CY 2020. Additionally, MedPAC's March 2019 Report to Congress supports our conclusion; specifically, Chapter 16 of MedPAC's report, titled Mandated Report: Opioids and Alternatives in Hospital Settings—Payments, Incentives, and Medicare Data, concludes that there is no clear indication that Medicare's OPPS provides systematic payment incentives that promote the use of opioid analgesics over non-opioid analgesics.[12] However, we invited public comments on whether there were other non-opioid pain management alternatives for which our payment policy should be revised to allow separate payment. We requested public comments that provided evidence-based support, such as published peer-reviewed literature, that we could use to determine whether these products help to deter or avoid prescription opioid use and addiction as well as evidence that the current packaged payment for such non-opioid alternatives presents a barrier to access to care and therefore warrants revised, including possibly separate, payment under the OPPS. We noted that evidence that current payment policy provides a payment incentive for using opioids instead of non-opioid alternatives should align with available Medicare claims data.
We provide a summary of the comments received and our responses to those comments below.
Comment: Multiple commenters, including hospital associations, medical specialty societies, and drug manufacturers, requested that we pay separately for Exparel and other drugs that function as surgical supply in the hospital outpatient setting. Some of these commenters noted that Exparel is more frequently used in this setting and the use of non-opioid pain management treatments should also be encouraged in the hospital outpatient department. The manufacturer of Exparel, Pacira Pharmaceuticals, presented a 5-year OPPS claims data analysis of hospital trends in Exparel use and a 200 hospital survey on purchasing decisions for non-opioid alternatives, concluding that Medicare's packaging policy has led to hospitals reducing or stopping Exparel use.
Response: As we stated in the CY 2019 OPPS/ASC final rule (83 FR 58856), we do not believe that there is sufficient evidence that non-opioid pain management drugs should be paid separately in the hospital outpatient setting at this time. The commenters did not provide evidence that the OPPS packaging policy for Exparel (or other non-opioid drugs) creates a barrier to use of Exparel in the hospital setting. Further, while we received some public comments suggesting that, as a result of using Exparel in the OPPS setting, providers may prescribe fewer opioids for Medicare beneficiaries, we do not believe that the OPPS payment policy presents a barrier to use of Exparel or affects the likelihood that providers will prescribe fewer opioids in the HOPD setting. Several drugs are packaged under the OPPS and payment for such drugs is included in the payment for the associated primary procedure. We were not persuaded by the information supplied by commenters suggesting that some providers avoid use of non-opioid alternatives (including Exparel) solely because of the OPPS packaged payment policy. We observed increasing Exparel utilization in the HOPD setting with the total units increasing from 9.0 million in 2017 to 13.6 million in 2018, despite the bundled payment in the OPPS setting. This upward trend has been consistent since 2015, as the data shows approximately 6.5 million total units in 2015 and 8.1 million total units in 2016. Therefore, we do not believe that the current OPPS payment methodology for Exparel and other non-opioid pain management drugs presents a widespread barrier to their use.
In addition, higher use in the hospital outpatient setting not only supports the notion that the packaged payment for Exparel is not causing an access to care issue, but also that the payment rate for primary procedures in the HOPD using Exparel adequately reflects the cost of the drug. That is, because Exparel is commonly used and billed under the OPPS, the APC rates for the primary procedures reflect such utilization. Therefore, the higher utilization in the OPPS setting should mitigate the need for separate payment. We remind readers that the OPPS is a prospective payment system, not a cost-based system and, by design, is based on a system of averages under which payment for certain cases may exceed the costs incurred, while for others, it may not. As stated earlier in this section, the OPPS packages payments for multiple interrelated items and services into a single payment to create incentives for hospitals to furnish services most efficiently and to manage their resources with maximum flexibility. Our packaging policies support our strategic goal of using larger payment bundles in the OPPS to maximize hospitals' incentives to provide care in the most efficient manner. We continue to invite stakeholders to share evidence, such as published peer-reviewed literature, on these non-opioid alternatives. We also intend to continue to analyze the evidence and monitor utilization of non-opioid alternatives in the OPD and ASC settings for potential future rulemaking.
We also stated in the CY 2020 OPPS/ASC proposed rule that, although we found increases in utilization for Exparel when it is paid under the OPPS, we did notice a continued decline in Exparel utilization in the ASC setting. While several variables may contribute to this difference in utilization and claims reporting between the hospital outpatient department and the ASC setting, one potential explanation is that, in comparison to hospital outpatient departments, ASCs tend to provide specialized care and a more limited range of services. Also, ASCs are paid, in aggregate, approximately 55 percent of the OPPS rate. Therefore, fluctuations in payment rates for specific services may impact these providers more acutely than hospital outpatient departments, and as a result, ASCs may be less likely to choose to furnish non-opioid postsurgical pain management treatments, which are typically more expensive than opioids. Another possible contributing factor is that ASCs do not typically report packaged items and services and, accordingly, our analysis may be undercounting the number of Exparel units utilized in the ASC setting.
Therefore, we are finalizing our proposal to continue to unpackage and pay separately for the cost of non-opioid pain management drugs that function as surgical supplies when they are furnished in the ASC setting without modification. This policy and related comments are addressed in section XIII.D.3. of this final rule with comment period.
As we stated previously in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59250), our packaging policies are designed to support our strategic goal of using larger payment bundles in the OPPS to maximize hospitals' incentives to provide clinically appropriate care in the most efficient manner. The packaging policies established under the OPPS also typically apply when services are provided in the ASC setting, and the policies have the same strategic goals in both settings. While unpackaging and paying separately for drugs that function as surgical supplies is a departure from our overall packaging policy for drugs, we believe that the proposed change will continue to incentivize the use of non-opioid pain management drugs and is responsive to the Commission's recommendation to examine payment policies for non-opioid pain management drugs that function as a supply, with the overall goal of combating the current opioid addiction crisis. As previously noted, a discussion of the CY 2020 proposal for payment of non-opioid pain management drugs in the ASC setting was presented in further detail in section XIII.D.3 of the CY 2020 OPPS/ASC proposed rule, and we refer readers to section XIII.D.3 of this CY 2020 OPPS/ASC final rule with comment period for further discussion of the final policy for CY 2020. As stated above, we also requested public comments in the CY 2020 OPPS/ASC proposed rule that provide peer-reviewed evidence, such as published peer-reviewed literature, that we could use to determine whether these products help to deter or avoid prescription opioid use and addiction as well as evidence that the current packaged payment for such non-opioid alternatives presents a barrier to access to care and therefore warrants revised, including possibly separate, payment under the OPPS. We also stated that evidence that current payment policy provides a payment incentive for using opioids instead of non-opioid alternatives should align with available Medicare claims data.
Comment: Several commenters supported the assignment of status indicator “K” (Nonpass-Through Drugs and Nonimplantable Biologicals, Including Therapeutic Radiopharmaceuticals) and continuing to pay separately for the drug Prialt (HCPCS J2278, injection, ziconitide), a non-narcotic pain reliever administered via intrathecal injection. Commenters provided data indicating that Prialt potentially could lower opioid use, including opioids such as morphine. In addition to continued separate payment, several commenters recommended CMS reduce or eliminate the coinsurance for the drug in order to increase beneficiary access. Commenters stated that due to the drug's significant cost, the 20 percent coinsurance would put the drug out of reach for beneficiaries. Additionally, commenters stated that there is not enough financial incentive for providers to use Prialt in their patients compared to lower cost opioids. Commenters claim that Prialt is only paid at invoice cost, which they believe discourages provider use.
Response: We thank commenters for their feedback and for their support of the continued assignment of status indicator “K” to HCPCS J2278. Prialt is paid at its average sales price plus 6 percent according to the ASP methodology under the OPPS. We note that under section 1833(t)(8) of the Act, the payment is subject to applicable deductible and coinsurance, and we are unaware of statutory authority to alter beneficiary coinsurance for payments made under the OPPS. We note that because the dollar value of beneficiary coinsurance is directly proportionate to the payment rate (which is ASP + 6 percent for HCPCS code J2278), a lower sales price for the drug (which would lead to a lower Medicare payment rate under current policy) would be necessary for beneficiaries to have a lower coinsurance amount.
Comment: Many commenters requested that the drug Omidria (HCPCS code C9447, injection, phenylephrine ketorolac) be excluded from the packaging policy once its pass-through status expires on September 30, 2020. Omidria is indicated for maintaining pupil size by preventing intraoperative miosis and reducing postoperative ocular pain in cataract or intraocular surgeries. The commenters stated that the available data and multiple peer-reviewed articles on Omidria meet the section 6082 criteria for packaging exclusion. Commenters asserted that the use of Omidria decreases patients' need for fentanyl during surgeries and another commenter stated that Omidria reduces opioid use after cataract surgeries. In addition, commenters asserted that the OPPS and ASC payment system do not address the cost of packaged products used by small patient populations. Therefore, the OPPS and ASC payment structures for packaged supplies creates an access barrier and patients are forced to use inferior products that have increased complication risk and require the continued use of opioids to manage pain. One commenter referenced the results of a study that showed that Omidria reduces the need for opioids during cataract surgery by nearly 80 percent while decreasing pain scores by more than 50 percent.
Response: We thank commenters for their feedback on Omidria. Omidria received pass-through status for a 3-year period from 2015 to 2017. After expiration of its pass-through status, it was packaged per OPPS policy. Subsequently, Omidria's pass-through status was reinstated in October 2018 through September 30, 2020 as required by section 1833(t)(6)(G) of the Act, as added by section 1301(a)(1)(C) of the Consolidated Appropriations Act 2018 (Pub. L. 115-141). While our analysis supports the commenter's assertion that there was a decrease in the utilization of Omidria in 2018 following its pass-through expiration, we note that there could be many reasons that utilization declines after the pass-through period ends that are unrelated to the lack of separate payment, including the availability of other alternatives on the market (many of which had been used for several years before Omidria came on the market and are sold for a lower price), or physician preference among others.
Further, our clinical advisors' review of the clinical evidence submitted concluded that the study the commenter submitted was not sufficiently compelling or authoritative to overcome contrary evidence. Moreover, the results of a CMS study of cataract procedures performed on Medicare beneficiaries in the OPPS between January 2015 and July 2019 comparing procedures performed with Omidria to procedures performed without Omidria did not demonstrate a significant decrease in fentanyl utilization during the cataract surgeries in the OPPS when Omidria was used. Our results also did not suggest any decrease in opioid utilization post-surgery for procedures involving Omidria. At this time, we do not have compelling evidence to exclude Omidria from packaging after its current pass-through expires on September 30, 2020. We will continue to analyze the evidence and monitor utilization of this drug.
Comment: One commenter requested that MKO Melt, a non-FDA-approved, compounded drug comprised of midazolam/ketamine/ondansetron be excluded from the packaging policy under section 1833(t)(22)(A)(iii) of the Act. The commenter contended that MKO Melt are drugs functioning as a surgical supply in the ASC setting. The commenter provided a reference to a study titled, “Anesthesia for opioid addict: Challenges for perioperative physician” by Goyal et al., on the need for pain management in the opioid-dependent patient. The commenter also referenced a review article, “Perioperative Management of Acute Pain in the Opioid-dependent Patient,” by Mitra et al., on the special needs of opioid-dependent patients in surgeries and the potential opioid relapse in those patients who are recovering from opioid use disorder. Additionally, the commenter referenced a clinical trial registered in clinicaltrials.gov (NCT03653520) that supports sublingual MKO Melt for use during cataract surgeries to replace opioids. The study looked at 611 patients that were divided into three arms: (1) MKO melt arm, (2) diazepam/tramadol/ondansetron arm, (3) diazepam only arm. The study concluded that the MKO melt arm had the lowest incidence for supplemental injectable anesthesia to control pain.
Response: We thank the commenter for the comment. Based on the information provided, we are not able to validate that MKO Melt reduces the use of opioids. We note that ketamine, one of the components of MKO melt, exhibits some addictive properties. Moreover, we did not identify any compelling evidence that MKO Melt is effective for patients with a prior opioid addiction nor did we receive any data demonstrating that the current OPPS packaging policy incentivized providers to use opioids over MKO Melt. In accordance with our review under section 1833(t)(22)(A)(i) of the Act, as well as the lack of HCPCS code for the drug, and FDA approval, we were not able to establish any compelling evidence that MKO should be excluded from packaged payment.
Comment: Several commenters, including individual physicians, medical associations, and device manufacturers, supported separate payment for continuous peripheral nerve blocks as the commenters believed they significantly reduce opioid use. One commenter suggested that CMS provide separate payment for HCPCS code A4306 (Disposable drug delivery system, flow rate of less than 50 ml per hour) in the hospital outpatient department setting and the ASC setting because packaging represents a cost barrier for providers. The commenter contended that continuous nerve block procedures have been shown in high quality clinical studies to reduce the use of opioids, attaching studies for review. The commenter stated that separate payment for A4306 will remove the financial disincentive for HOPDs and ASCs to use these items, and would encourage continuous nerve blocks as a non-opioid alternative for post-surgical pain management.
Response: We appreciate the commenters' suggestion. We examined the data for A4306 and noted an overall trend of increasing utilization from CY 2014 through CY 2017. There was a slight decrease in utilization in CY 2018. However, we note that this slight decline may be an outlier, given the four year trend of consistently increasing utilization. Additionally, the geometric mean cost for HCPCS code A4306 was approximately $30 each year during that 4-year period. We acknowledge that use of these items may help in the reduction of opioid use. However, we note that packaged payment of such an item does not prevent the use of these items, as we found with the overall increased utilization of this product. We do not believe that the current utilization trends for HCPCS code A4306 suggest that the packaged payment is preventing use and remind readers that payment for packaged items is included in the payment for the primary service. We share the commenter's concern about the need to reduce opioid use and will take the commenter's suggestion regarding the need for separate payment for HCPCS code A4306 into consideration for future rulemaking.
Comment: Multiple commenters identified other non-opioid pain management alternatives that they believe decrease the dose, duration, and/or number of opioid prescriptions beneficiaries receive during and following an outpatient visit or procedure (especially for beneficiaries at high-risk for opioid addiction) and that may warrant separate payment for CY 2020. Commenters representing various stakeholders requested separate payments for various non-opioid pain management treatments, such as continuous nerve blocks, neuromodulation radiofrequency ablation, implants for lumbar stenosis, enhanced recovery after surgery, IV acetaminophen, IV ibuprofen, Polar ice devices for postoperative pain relief, THC oil, acupuncture, and dry needling procedures.
For neuromodulation, several commenters noted that spinal cord stimulators (SCS) may lead to a reduction in the use of opioids for chronic pain patients. One manufacturer commented that SCS provides the opportunity to potentially stabilize or decrease opioid usage and that neuromodulation retains its efficacy over multiple years. Regarding barriers to access, the commenter noted that Medicare beneficiaries often do not have access to SCS until after they have exhausted other treatments, which often includes opioids. The commenter presented evidence from observational studies that use of SCS earlier in a patient's treatment could help reduce opioid use while controlling pain, suggesting CMS look for ways to incorporate SCS earlier in the treatment continuum.
Another commenter asserted that the standard endpoints, such as a greater than 50 percent reduction in pain, that are used to determine if a neuromodulation-based non-opioid pain alternative therapy is effective are well-established and validated in all types of clinical trials and that CMS should establish a general, national coverage determination for neuromodulation-based non-opioid pain therapy based on these endpoints, rather than taking the time to create and process specific national coverage determinations or local coverage determinations. The commenter suggested that this would be a much faster and streamlined process for enhancing Medicare beneficiary access to neuromodulation-based pain management therapies.
One of the manufacturers of a high-frequency SCS device stated that additional payment was warranted for non-opioid pain management treatments because they provide an alternative treatment option to opioids for patients with chronic, leg, or back pain. The commenter provided supporting studies that claimed that patients treated with their high-frequency SCS device reported a statistically significant average decrease in opioid use compared to the control group. This commenter also submitted data that showed a decline in the mean daily dosage of opioid medication taken and that fewer patients were relying on opioids at all to manage their pain when they used the manufacturer's device.
Other commenters wrote regarding their personal experiences with radiofrequency ablation for sacral iliac joints and knees. One commenter referenced several studies, one of which found a decrease in analgesic medications associated with radiofrequency ablation; however, it did not provide evidence regarding a decrease in opioid usage.
One national hospital association commenter recommended that while “certainly not a solution to the opioid epidemic, unpackaging appropriate non-opioid therapies, like Exparel, is a low-cost tactic that could change long-standing practice patterns without major negative consequences.” This same commenter suggested that Medicare consider separate payment for IV acetaminophen, IV ibuprofen, and Polar ice devices for postoperative pain relief after knee procedures. The commenter also noted that therapeutic massage, topically applied THC oil, acupuncture, and dry needling procedures are very effective therapies for relief of both postoperative pain and long-term and chronic pain. Several other commenters expressed support for separate payment for IV acetaminophen.
Response: We appreciate the detailed responses from commenters on this topic. At this time, we have not found compelling evidence for other non-opioid pain management alternatives described above to warrant separate payment under the OPPS or ASC payment systems for CY 2020. We plan to take these comments and suggestions into consideration for future rulemaking. We agree that providing incentives to avoid and/or reduce opioid prescriptions may be one of several strategies for addressing the opioid epidemic. To the extent that the items and services mentioned by the commenters are effective alternatives to opioid prescriptions, we encourage providers to use them when medically necessary. We note that some of the items and services mentioned by commenters are not covered by Medicare, and we do not intend to establish payment for noncovered items and services at this time. We look forward to working with stakeholders as we further consider suggested refinements to the OPPS and the ASC payment system that will encourage use of medically necessary items and services that have demonstrated efficacy in decreasing opioid prescriptions and/or opioid abuse or misuse during or after an outpatient visit or procedure.
After reviewing the non-opioid pain management alternatives suggested by the commenters as well as the studies and other data provided to support the request for separate payment, we have not determined that separate payment is warranted at this time for any of the non-opioid pain management alternatives discussed above.
Comment: Several commenters addressed payment barriers that may inhibit access to non-opioid pain management treatments discussed throughout this section. Several commenters disagreed with CMS's assessment that current payment policies do not represent barriers to access for certain non-opioid pain management alternatives. Commenters encouraged CMS to provide timely insurance coverage for evidence-informed interventional procedures early in the course of treatment when clinically appropriate. Several other commenters encouraged CMS to more broadly evaluate all of its packaging policies to help ensure patient access to appropriate therapies and to evaluate how packaging affects the utilization of a medicine.
Response: We appreciate the various, insightful comments we received from stakeholders regarding barriers that may inhibit access to non-opioid alternatives for pain treatment and management in order to more effectively address the opioid epidemic. We will take these comments into consideration for future rulemaking. Many of these comments have been previously addressed throughout this section. CMS recognizes that medical exposure to opioids entails inherent risks, which may include delayed recovery, diversion, misuse, accidental overdose, development or re-emergence of addiction, and neonatal abstinence syndrome. However, there are challenges in developing a methodology to identify disincentives to use opioid alternatives. In the context of the opioid crisis, and given the central role the federal government plays in addressing it, these issues are of particular concern to CMS. Because of this, CMS intends to work with an interagency task force to review available data and to develop criteria for revisions to payment for opioid alternatives that are effective for pain relief or in reducing opioid use.
After consideration of the public comments we received, we are finalizing the proposed policy, without modification, to unpackage and pay separately at ASP+6 percent for the cost of non-opioid pain management drugs that function as surgical supplies when they are furnished in the ASC setting for CY 2020. Under this policy, the only FDA-approved drug that meets this criteria is Exparel.
We will continue to analyze the issue of access to non-opioid alternatives in the OPPS and the ASC settings for any subsequent reviews we conduct under section 1833(t)(22)(A)(ii). We are continuing to examine whether there are other non-opioid pain management alternatives for which our payment policy should be revised to allow separate payment. We will be reviewing evidence-based support, such as published peer-reviewed literature, that we could use to determine whether these products help to deter or avoid prescription opioid use and addiction as well as evidence that the current packaged payment for such non-opioid alternatives presents a barrier to access to care and therefore warrants revised, including possibly separate, payment under the OPPS. This policy is also discussed in section XII.D.3 of this final rule with comment period.
4. Calculation of OPPS Scaled Payment Weights
We established a policy in the CY 2013 OPPS/ASC final rule with comment period (77 FR 68283) of using geometric mean-based APC costs to calculate relative payment weights under the OPPS. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 58860 through 58861), we applied this policy and calculated the relative payment weights for each APC for CY 2019 that were shown in Addenda A and B to that final rule with comment period (which were made available via the internet on the CMS website) using the APC costs discussed in sections II.A.1. and II.A.2. of that final rule with comment period. For CY 2020, as we did for CY 2019, we proposed to continue to apply the policy established in CY 2013 and calculate relative payment weights for each APC for CY 2020 using geometric mean-based APC costs.
For CY 2012 and CY 2013, outpatient clinic visits were assigned to one of five levels of clinic visit APCs, with APC 0606 representing a mid-level clinic visit. In the CY 2014 OPPS/ASC final rule with comment period (78 FR 75036 through 75043), we finalized a policy that created alphanumeric HCPCS code G0463 (Hospital outpatient clinic visit for assessment and management of a patient), representing any and all clinic visits under the OPPS. HCPCS code G0463 was assigned to APC 0634 (Hospital Clinic Visits). We also finalized a policy to use CY 2012 claims data to develop the CY 2014 OPPS payment rates for HCPCS code G0463 based on the total geometric mean cost of the levels one through five CPT E/M codes for clinic visits previously recognized under the OPPS (CPT codes 99201 through 99205 and 99211 through 99215). In addition, we finalized a policy to no longer recognize a distinction between new and established patient clinic visits.
For CY 2016, we deleted APC 0634 and reassigned the outpatient clinic visit HCPCS code G0463 to APC 5012 (Level 2 Examinations and Related Services) (80 FR 70372). For CY 2020, as we did for CY 2019, we proposed to continue to standardize all of the relative payment weights to APC 5012. We believe that standardizing relative payment weights to the geometric mean of the APC to which HCPCS code G0463 is assigned maintains consistency in calculating unscaled weights that represent the cost of some of the most frequently provided OPPS services. For CY 2020, as we did for CY 2019, we proposed to assign APC 5012 a relative payment weight of 1.00 and to divide the geometric mean cost of each APC by the geometric mean cost for APC 5012 to derive the unscaled relative payment weight for each APC. The choice of the APC on which to standardize the relative payment weights does not affect payments made under the OPPS because we scale the weights for budget neutrality.
We did not receive any public comments on our proposal to continue to use the geometric mean cost of APC 5012 to standardize relative payment weights for CY 2020. Therefore, we are finalizing our proposal and assigning APC 5012 the relative payment weight of 1.00, and using the relative payment weight for APC 5012 to derive the unscaled relative payment weight for each APC for CY 2020.
We note that in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59004 through 59015), we discuss our policy, implemented on January 1, 2019, to control for unnecessary increases in the volume of covered outpatient department services by paying for clinic visits furnished at excepted off-campus provider-based department (PBD) at a reduced rate, and we are continuing the policy with the second year of the two-year transition in CY 2020. While the volume associated with these visits is included in the impact model, and thus used in calculating the weight scalar, the policy has a negligible effect on the scalar. Specifically, under this policy, there is no change to the relativity of the OPPS payment weights because the adjustment is made at the payment level rather than in the cost modeling. Further, under this policy, the savings that will result from the change in payments for these clinic visits will not be budget neutral. Therefore, the impact of this policy will generally not be reflected in the budget neutrality adjustments, whether the adjustment is to the OPPS relative weights or to the OPPS conversion factor. We refer readers to section X.C. of this CY 2020 OPPS/ASC final rule with comment period for further discussion of this final policy.
Section 1833(t)(9)(B) of the Act requires that APC reclassification and recalibration changes, wage index changes, and other adjustments be made in a budget neutral manner. Budget neutrality ensures that the estimated aggregate weight under the OPPS for CY 2020 is neither greater than nor less than the estimated aggregate weight that would have been calculated without the changes. To comply with this requirement concerning the APC changes, we proposed to compare the estimated aggregate weight using the CY 2019 scaled relative payment weights to the estimated aggregate weight using the proposed CY 2020 unscaled relative payment weights.
For CY 2019, we multiplied the CY 2019 scaled APC relative payment weight applicable to a service paid under the OPPS by the volume of that service from CY 2018 claims to calculate the total relative payment weight for each service. We then added together the total relative payment weight for each of these services in order to calculate an estimated aggregate weight for the year. For CY 2020, we proposed to apply the same process using the estimated CY 2020 unscaled relative payment weights rather than scaled relative payment weights. We proposed to calculate the weight scalar by dividing the CY 2019 estimated aggregate weight by the unscaled CY 2020 estimated aggregate weight.
For a detailed discussion of the weight scalar calculation, we refer readers to the OPPS claims accounting document available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html. Click on the CY 2020 OPPS final rule link and open the claims accounting document link at the bottom of the page.
We proposed to compare the estimated unscaled relative payment weights in CY 2020 to the estimated total relative payment weights in CY 2019 using CY 2018 claims data, holding all other components of the payment system constant to isolate changes in total weight. Based on this comparison, we proposed to adjust the calculated CY 2020 unscaled relative payment weights for purposes of budget neutrality. We proposed to adjust the estimated CY 2020 unscaled relative payment weights by multiplying them by a proposed weight scalar of 1.4401 to ensure that the proposed CY 2020 relative payment weights are scaled to be budget neutral. The proposed CY 2020 relative payment weights listed in Addenda A and B to the proposed rule (which are available via the internet on the CMS website) were scaled and incorporated the recalibration adjustments discussed in sections II.A.1. and II.A.2. of the proposed rule.
Section 1833(t)(14) of the Act provides the payment rates for certain SCODs. Section 1833(t)(14)(H) of the Act provides that additional expenditures resulting from this paragraph shall not be taken into account in establishing the conversion factor, weighting, and other adjustment factors for 2004 and 2005 under paragraph (9), but shall be taken into account for subsequent years. Therefore, the cost of those SCODs (as discussed in section V.B.2. of this final rule with comment period) is included in the budget neutrality calculations for the CY 2020 OPPS.
We did not receive any public comments on the proposed weight scalar calculation. Therefore, we are finalizing our proposal to use the calculation process described in the proposed rule, without modification, for CY 2020. Using updated final rule claims data, we are updating the estimated CY 2020 unscaled relative payment weights by multiplying them by a weight scalar of 1.4349 to ensure that the final CY 2020 relative payment weights are scaled to be budget neutral. The final CY 2020 relative payments weights listed in Addenda A and B to this final rule with comment period (which are available via the internet on the CMS website) were scaled and incorporate the recalibration adjustments discussed in sections II.A.1. and II.A.2. of this final rule with comment period.
B. Conversion Factor Update
Section 1833(t)(3)(C)(ii) of the Act requires the Secretary to update the conversion factor used to determine the payment rates under the OPPS on an annual basis by applying the OPD fee schedule increase factor. For purposes of section 1833(t)(3)(C)(iv) of the Act, subject to sections 1833(t)(17) and 1833(t)(3)(F) of the Act, the OPD fee schedule increase factor is equal to the hospital inpatient market basket percentage increase applicable to hospital discharges under section 1886(b)(3)(B)(iii) of the Act. In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19401), consistent with current law, based on IHS Global, Inc.'s fourth quarter 2018 forecast of the FY 2020 market basket increase, the proposed FY 2020 IPPS market basket update was 3.2 percent. However, sections 1833(t)(3)(F) and 1833(t)(3)(G)(v) of the Act, as added by section 3401(i) of the Patient Protection and Affordable Care Act of 2010 (Pub. L. 111-148) and as amended by section 10319(g) of that law and further amended by section 1105(e) of the Health Care and Education Reconciliation Act of 2010 (Pub. L. 111-152), provide adjustments to the OPD fee schedule increase factor for CY 2020.
Specifically, section 1833(t)(3)(F)(i) of the Act requires that, for 2012 and subsequent years, the OPD fee schedule increase factor under subparagraph (C)(iv) be reduced by the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act. Section 1886(b)(3)(B)(xi)(II) of the Act defines the productivity adjustment as equal to the 10-year moving average of changes in annual economy-wide, private nonfarm business multifactor productivity (MFP) (as projected by the Secretary for the 10-year period ending with the applicable fiscal year, year, cost reporting period, or other annual period) (the “MFP adjustment”). In the FY 2012 IPPS/LTCH PPS final rule (76 FR 51689 through 51692), we finalized our methodology for calculating and applying the MFP adjustment, and then revised this methodology, as discussed in the FY 2016 IPPS/LTCH PPS final rule (80 FR 49509). According to the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19402), the proposed MFP adjustment for FY 2020 was 0.5 percentage point.
For CY 2020, we proposed that the MFP adjustment for the CY 2020 OPPS is 0.5 percentage point (84 FR 39428). We proposed that if more recent data become subsequently available after the publication of the proposed rule (for example, a more recent estimate of the market basket increase and the MFP adjustment), we would use such updated data, if appropriate, to determine the CY 2020 market basket update and the MFP adjustment, which are components in calculating the OPD fee schedule increase factor under sections 1833(t)(3)(C)(iv) and 1833(t)(3)(F) of the Act, in this CY 2020 OPPS/ASC final rule with comment period.
We note that section 1833(t)(3)(F) of the Act provides that application of this subparagraph may result in the OPD fee schedule increase factor under section 1833(t)(3)(C)(iv) of the Act being less than 0.0 percent for a year, and may result in OPPS payment rates being less than rates for the preceding year. As described in further detail below, we proposed for CY 2020 an OPD fee schedule increase factor of 2.7 percent for the CY 2020 OPPS (which was 3.2 percent, the final estimate of the hospital inpatient market basket percentage increase, less the final 0.5 percentage point MFP adjustment).
We proposed that hospitals that fail to meet the Hospital OQR Program reporting requirements would be subject to an additional reduction of 2.0 percentage points from the OPD fee schedule increase factor adjustment to the conversion factor that would be used to calculate the OPPS payment rates for their services, as required by section 1833(t)(17) of the Act. For further discussion of the Hospital OQR Program, we refer readers to section XIV. of this final rule with comment period.
In the CY 2020 OPPS/ASC proposed rule, we proposed to amend 42 CFR 419.32(b)(1)(iv)(B) by adding a new paragraph (11) to reflect the requirement in section 1833(t)(3)(F)(i) of the Act that, for CY 2020, we reduce the OPD fee schedule increase factor by the MFP adjustment as determined by CMS.
To set the OPPS conversion factor for CY 2020, we proposed to increase the CY 2019 conversion factor of $79.490 by 2.7 percent. In accordance with section 1833(t)(9)(B) of the Act, we proposed further to adjust the conversion factor for CY 2020 to ensure that any revisions made to the wage index and rural adjustment were made on a budget neutral basis. We proposed to calculate an overall budget neutrality factor of 0.9993 for wage index changes. This adjustment was comprised of a 1.0005 proposed budget neutrality adjustment, using our standard calculation, of comparing proposed total estimated payments from our simulation model using the proposed FY 2020 IPPS wage indexes to those payments using the FY 2019 IPPS wage indexes, as adopted on a calendar year basis for the OPPS as well as a 0.9988 proposed budget neutrality adjustment for the proposed CY 2020 5 percent cap on wage index decreases to ensure that this transition wage index is implemented in a budget neutral manner, consistent with the proposed FY 2020 IPPS wage index policy (84 FR 19398). We stated in the proposed rule that we believed it was appropriate to ensure that this proposed wage index transition policy (that is, the proposed CY 2020 5 percent cap on wage index decreases) did not increase estimated aggregate payments under the OPPS beyond the payments that would be made without this transition policy. We proposed to calculate this budget neutrality adjustment by comparing total estimated OPPS payments using the FY 2020 IPPS wage index, adopted on a calendar year basis for the OPPS, where a 5 percent cap on wage index decreases is not applied to total estimated OPPS payments where the 5 percent cap on wage index decreases is applied. We stated in the proposed rule that these two proposed wage index budget neutrality adjustments would maintain budget neutrality for the proposed CY 2020 OPPS wage index (which, as we discussed in section II.C of the proposed rule, would use the FY 2020 IPPS post-reclassified wage index and any adjustments, including without limitation any adjustments finalized under the IPPS to address wage index disparities).
We did not receive any public comments on our proposed methodology for calculating the wage index budget neutrality adjustments discussed earlier in this section. Therefore, for the reasons discussed above and in the CY 2020 OPPS/ASC proposed rule (84 FR 39428 through 39429), we are finalizing our methodology for calculating the wage index budget neutrality adjustments as proposed, without modification. For CY 2020, we are finalizing an overall budget neutrality factor of 0.9981 for wage index changes. This adjustment is comprised of a 0.9990 budget neutrality adjustment, using our standard calculation of comparing total estimated payments from our simulation model using the final FY 2020 IPPS wage indexes to those payments using the FY 2019 IPPS wage indexes, as adopted on a calendar year basis for the OPPS as well as a 0.9991 budget neutrality adjustment for the CY 2020 5 percent cap on wage index decreases to ensure that this transition wage index is implemented in a budget neutral manner. We note that the final wage index budget neutrality adjustment figures set forth above differ from the figures set forth in the proposed rule due to updated data for the final rule.
For the CY 2020 OPPS, we are maintaining the current rural adjustment policy, as discussed in section II.E. of the proposed rule. Therefore, the proposed budget neutrality factor for the rural adjustment is 1.0000.
For the CY 2020 OPPS/ASC proposed rule, we proposed to continue previously established policies for implementing the cancer hospital payment adjustment described in section 1833(t)(18) of the Act, as discussed in section II.F. of the proposed rule and this final rule with comment period. We proposed to calculate a CY 2020 budget neutrality adjustment factor for the cancer hospital payment adjustment by comparing estimated total CY 2020 payments under section 1833(t) of the Act, including the proposed CY 2020 cancer hospital payment adjustment, to estimated CY 2020 total payments using the CY 2019 final cancer hospital payment adjustment, as required under section 1833(t)(18)(B) of the Act. The proposed CY 2020 estimated payments applying the proposed CY 2020 cancer hospital payment adjustment were the same as estimated payments applying the CY 2019 final cancer hospital payment adjustment. Therefore, we proposed to apply a budget neutrality adjustment factor of 0.9998 to the conversion factor for the cancer hospital payment adjustment. In accordance with section 16002(b) of the 21st Century Cures Act, we stated in the proposed rule that we are applying a budget neutrality factor calculated as if the proposed cancer hospital adjustment target payment-to-cost ratio was 0.90, not the 0.89 target payment-to-cost ratio we applied as stated in section II.F. of the proposed rule.
For the CY 2020 OPPS/ASC proposed rule, we estimated that proposed pass-through spending for drugs, biologicals, and devices for CY 2020 would equal approximately $268.8 million, which represented 0.34 percent of total projected CY 2020 OPPS spending. Therefore, the proposed conversion factor would be adjusted by the difference between the 0.14 percent estimate of pass-through spending for CY 2019 and the 0.34 percent estimate of proposed pass-through spending for CY 2020, resulting in a proposed decrease for CY 2020 of 0.20 percent. Proposed estimated payments for outliers would remain at 1.0 percent of total OPPS payments for CY 2020. We estimated for the proposed rule that outlier payments would be 1.03 percent of total OPPS payments in CY 2019; the 1.00 percent for proposed outlier payments in CY 2020 would constitute a 0.03 percent increase in payment in CY 2020 relative to CY 2019.
For the CY 2020 OPPS/ASC proposed rule, we also proposed that hospitals that fail to meet the reporting requirements of the Hospital OQR Program would continue to be subject to a further reduction of 2.0 percentage points to the OPD fee schedule increase factor. For hospitals that fail to meet the requirements of the Hospital OQR Program, we proposed to make all other adjustments discussed above, but use a reduced OPD fee schedule update factor of 0.7 percent (that is, the proposed OPD fee schedule increase factor of 2.7 percent further reduced by 2.0 percentage points). This would result in a proposed reduced conversion factor for CY 2020 of $79.770 for hospitals that fail to meet the Hospital OQR Program requirements (a difference of −1.628 in the conversion factor relative to hospitals that met the requirements).
In summary, for CY 2020, we proposed to amend § 419.32 by adding a new paragraph (b)(1)(iv)(B)(11) to reflect the reductions to the OPD fee schedule increase factor that are required for CY 2020 to satisfy the statutory requirements of sections 1833(t)(3)(F) and (t)(3)(G)(v) of the Act. We proposed to use a reduced conversion factor of $79.770 in the calculation of payments for hospitals that fail to meet the Hospital OQR Program requirements (a difference of −1.628 in the conversion factor relative to hospitals that met the requirements).
For CY 2020, we proposed to use a conversion factor of $81.398 in the calculation of the national unadjusted payment rates for those items and services for which payment rates are calculated using geometric mean costs; that is, the proposed OPD fee schedule increase factor of 2.7 percent for CY 2020, the required proposed wage index budget neutrality adjustment of approximately 0.9993, the proposed cancer hospital payment adjustment of 0.9998, and the proposed adjustment of −0.20 percentage point of projected OPPS spending for the difference in pass-through spending that resulted in a proposed conversion factor for CY 2020 of $81.398. We referred readers to section XXVI.B. of the proposed rule for a discussion of the estimated effect on the conversion factor of a policy to pay for 340B-acquired drugs at ASP + 3 percent, which is a policy on which we solicited comments for potential future rulemaking in the event of an adverse decision on appeal in the ongoing litigation involving our payment policy for 340B-acquired drugs.
Comment: One commenter, a state hospital association, asserts its member hospitals receive payments from CMS that are substantially lower than the costs their members incur to provide services. The commenter believes underpayments occur because the CMS hospital market basket estimate of inflation of 2.7 percent substantially underestimates overall health care inflation which the commenter claims to be between 5.5 percent and 7 percent. The commenter also states that hospital payments from CMS are reduced because of payment sequestration and the policy to reduce payment rates for clinic visits at off-campus hospital outpatient departments to 40 percent of the standard OPPS payment rate. The commenter suggests that CMS should help hospitals in all states regain this lost revenue by implementing a much larger annual increase in the market basket amount. The commenter advocates a 4.7 percent market basket adjustment in CY 2020, and even larger percentage increases in following years.
Response: The percentage change in the hospital market basket reflects the average change in the price of goods and services purchased by hospitals in order to provide medical care. A general measure of health care inflation (such as the Consumer Price Index for Medical Care Services) would not be appropriate as it is not specific to hospital medical services and is not reflective of the input price changes experienced by hospitals but rather the inflation experienced by the consumer for their medical expenses. In addition, the OPPS conversion factor is not designed to redress payment reductions made in a non-budget neutral manner. The policies cited by the commenter are intended to reduce Medicare expenditures. If the conversion factor was to be increased to offset these payment reductions, it would defeat the intent of these policy initiatives.
Comment: A commenter expressed their support for the proposed market basket increase of 2.7 percent.
Response: We appreciate the support of the commenter.
After reviewing the public comments we received, we are finalizing these proposals without modification. For CY 2020, we proposed to continue previously established policies for implementing the cancer hospital payment adjustment described in section 1833(t)(18) of the Act (discussed in section II.F. of this final rule with comment period). Based on the final rule updated data used in calculating the cancer hospital payment adjustment in section II.F. of this final rule with comment period, the target payment-to-cost ratio for the cancer hospital payment adjustment, which was 0.88 for CY 2019, is 0.89 for CY 2020. As a result, we are applying a budget neutrality adjustment factor of 0.9999 to the conversion factor for the cancer hospital payment adjustment.
As a result of these finalized policies, the OPD fee schedule increase factor for the CY 2020 OPPS is 2.6 percent (which reflects the 3.0 percent final estimate of the hospital inpatient market basket percentage increase, less the final 0.4 percentage point MFP adjustment). For CY 2020, we are using a conversion factor of $80.784 in the calculation of the national unadjusted payment rates for those items and services for which payment rates are calculated using geometric mean costs; that is, the OPD fee schedule increase factor of 2.6 percent for CY 2020, the required wage index budget neutrality adjustment of approximately 0.9981, and the adjustment of 0.88 percentage point of projected OPPS spending for the difference in pass-through spending that results in a conversion factor for CY 2020 of $80.784.
C. Wage Index Changes
Section 1833(t)(2)(D) of the Act requires the Secretary to determine a wage adjustment factor to adjust the portion of payment and coinsurance attributable to labor-related costs for relative differences in labor and labor-related costs across geographic regions in a budget neutral manner (codified at 42 CFR 419.43(a)). This portion of the OPPS payment rate is called the OPPS labor-related share. Budget neutrality is discussed in section II.B. of this final rule with comment period.
The OPPS labor-related share is 60 percent of the national OPPS payment. This labor-related share is based on a regression analysis that determined that, for all hospitals, approximately 60 percent of the costs of services paid under the OPPS were attributable to wage costs. We confirmed that this labor-related share for outpatient services is appropriate during our regression analysis for the payment adjustment for rural hospitals in the CY 2006 OPPS final rule with comment period (70 FR 68553). In the CY 2020 OPPS/ASC proposed rule (84 FR 39429), we proposed to continue this policy for the CY 2020 OPPS. We refer readers to section II.H. of this final rule with comment period for a description and an example of how the wage index for a particular hospital is used to determine payment for the hospital. We did not receive any public comments on this proposal. Therefore, for the reasons discussed above and in the CY 2020 OPPS/ASC proposed rule (84 FR 39429), we are finalizing our proposal, without modification, to continue this policy as discussed above for the CY 2020 OPPS.
As discussed in the claims accounting narrative included with the supporting documentation for this final rule with comment period (which is available via the internet on the CMS website), for estimating APC costs, we standardize 60 percent of estimated claims costs for geographic area wage variation using the same FY 2020 pre-reclassified wage index that that is used under the IPPS to standardize costs. This standardization process removes the effects of differences in area wage levels from the determination of a national unadjusted OPPS payment rate and copayment amount.
Under 42 CFR 419.41(c)(1) and 419.43(c) (published in the OPPS April 7, 2000 final rule with comment period (65 FR 18495 and 18545)), the OPPS adopted the final fiscal year IPPS post-reclassified wage index as the calendar year wage index for adjusting the OPPS standard payment amounts for labor market differences. Therefore, the wage index that applies to a particular acute care, short-stay hospital under the IPPS also applies to that hospital under the OPPS. As initially explained in the September 8, 1998 OPPS proposed rule (63 FR 47576), we believe that using the IPPS wage index as the source of an adjustment factor for the OPPS is reasonable and logical, given the inseparable, subordinate status of the HOPD within the hospital overall. In accordance with section 1886(d)(3)(E) of the Act, the IPPS wage index is updated annually.
The Affordable Care Act contained several provisions affecting the wage index. These provisions were discussed in the CY 2012 OPPS/ASC final rule with comment period (76 FR 74191). Section 10324 of the Affordable Care Act added section 1886(d)(3)(E)(iii)(II) to the Act, which defines a frontier State and amended section 1833(t) of the Act to add paragraph (19), which requires a frontier State wage index floor of 1.00 in certain cases, and states that the frontier State floor shall not be applied in a budget neutral manner. We codified these requirements at § 419.43(c)(2) and (3) of our regulations. For the CY 2020 OPPS, we proposed to implement this provision in the same manner as we have since CY 2011. Under this policy, the frontier State hospitals would receive a wage index of 1.00 if the otherwise applicable wage index (including reclassification, the rural floor, and rural floor budget neutrality) is less than 1.00. Because the HOPD receives a wage index based on the geographic location of the specific inpatient hospital with which it is associated, we stated that the frontier State wage index adjustment applicable for the inpatient hospital also would apply for any associated HOPD. In the CY 2020 OPPS/ASC proposed rule (84 FR 39430), we referred readers to the FY 2011 through FY 2019 IPPS/LTCH PPS final rules for discussions regarding this provision, including our methodology for identifying which areas meet the definition of “frontier States” as provided for in section 1886(d)(3)(E)(iii)(II) of the Act: For FY 2011, 75 FR 50160 through 50161; for FY 2012, 76 FR 51793, 51795, and 51825; for FY 2013, 77 FR 53369 through 53370; for FY 2014, 78 FR 50590 through 50591; for FY 2015, 79 FR 49971; for FY 2016, 80 FR 49498; for FY 2017, 81 FR 56922; for FY 2018, 82 FR 38142; and for FY 2019, 83 FR 41380. We did not receive any public comments on this proposal. Accordingly, for the reasons discussed above and in the CY 2020 OPPS/ASC proposed rule (84 FR 39430), we are finalizing our proposal, without modification, to continue to implement the frontier State floor under the OPPS in the same manner as we have since CY 2011.
In addition to the changes required by the Affordable Care Act, we noted in the CY 2020 OPPS/ASC proposed rule (84 FR 39430) that the FY 2020 IPPS wage indexes continue to reflect a number of adjustments implemented over the past few years, including, but not limited to, reclassification of hospitals to different geographic areas, the rural floor provisions, an adjustment for occupational mix, and an adjustment to the wage index based on commuting patterns of employees (the out-migration adjustment). Also, we noted that, as discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19393 through 19399), we proposed a number of policies under the IPPS to address wage index disparities between high and low wage index value hospitals. In particular, in the FY 2020 IPPS/LTCH PPS proposed rule, we proposed to (1) calculate the rural floor without including the wage data of urban hospitals that have reclassified as rural under section 1886(d)(8)(E) of the Act (as implemented in § 412.103) (84 FR 19396 through 19398); (2) remove the wage data of urban hospitals that have reclassified as rural under § 412.103 from the calculation of “the wage index for rural areas in the State” for purposes of applying section 1886(d)(8)(C)(iii) of the Act (84 FR 19398); (3) increase the wage index values for hospitals with a wage index below the 25th percentile wage index value across all hospitals by half the difference between the otherwise applicable final wage index value for a year for that hospital and the 25th percentile wage index value for that year, and to offset the estimated increase in payments to hospitals with wage index values below the 25th percentile by decreasing the wage index values for hospitals with wage index values above the 75th percentile wage index value across all hospitals (84 FR 19394 through 19396); and (4) apply a 5-percent cap for FY 2020 on any decrease in a hospital's final wage index from the hospital's final wage index in FY 2019, as a proposed transition wage index to help mitigate any significant negative impacts on hospitals (84 FR 19398). In addition, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19398), we proposed to apply a budget neutrality adjustment to the standardized amount so that our proposed transition wage index for hospitals that may be negatively impacted (described in item (4) above) would be implemented in a budget neutral manner. Furthermore, in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19398 through 19399), we noted that our proposed adjustment relating to the rural floor calculation also would be budget neutral. We referred readers to the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19373 through 19399) for a detailed discussion of all proposed changes to the FY 2020 IPPS wage indexes.
Furthermore, as discussed in the FY 2015 IPPS/LTCH PPS final rule (79 FR 49951 through 49963) and in each subsequent IPPS/LTCH PPS final rule, including the FY 2019 IPPS/LTCH PPS final rule (83 FR 41362), the Office of Management and Budget (OMB) issued revisions to the labor market area delineations on February 28, 2013 (based on 2010 Decennial Census data), that included a number of significant changes, such as new Core Based Statistical Areas (CBSAs), urban counties that became rural, rural counties that became urban, and existing CBSAs that were split apart (OMB Bulletin 13-01). This bulletin can be found at: https://obamawhitehouse.archives.gov/sites/default/files/omb/bulletins/2013/b13-01.pdf. In the FY 2015 IPPS/LTCH PPS final rule (79 FR 49950 through 49985), for purposes of the IPPS, we adopted the use of the OMB statistical area delineations contained in OMB Bulletin No. 13-01, effective October 1, 2014. For purposes of the OPPS, in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66826 through 66828), we adopted the use of the OMB statistical area delineations contained in OMB Bulletin No. 13-01, effective January 1, 2015, beginning with the CY 2015 OPPS wage indexes. In the FY 2017 IPPS/LTCH PPS final rule (81 FR 56913), we adopted revisions to statistical areas contained in OMB Bulletin No. 15-01, issued on July 15, 2015, which provided updates to and superseded OMB Bulletin No. 13-01 that was issued on February 28, 2013. For purposes of the OPPS, in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79598), we adopted the revisions to the OMB statistical area delineations contained in OMB Bulletin No. 15-01, effective January 1, 2017, beginning with the CY 2017 OPPS wage indexes.
On August 15, 2017, OMB issued OMB Bulletin No. 17-01, which provided updates to and superseded OMB Bulletin No. 15-01 that was issued on July 15, 2015. The attachments to OMB Bulletin No. 17-01 provide detailed information on the update to the statistical areas since July 15, 2015, and are based on the application of the 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas to Census Bureau population estimates for July 1, 2014 and July 1, 2015. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 58863 through 58865), we adopted the updates set forth in OMB Bulletin No. 17-01, effective January 1, 2019, beginning with the CY 2019 wage index. We continue to believe that it is important for the OPPS to use the latest labor market area delineations available as soon as is reasonably possible in order to maintain a more accurate and up-to-date payment system that reflects the reality of population shifts and labor market conditions. For a complete discussion of the adoption of the updates set forth in OMB Bulletin No. 17-01, we refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 58864 through 58865).
As we stated in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42301), for the FY 2020 IPPS wage indexes, we are using the OMB delineations that were adopted, beginning with FY 2015 (based on the revised delineations issued in OMB Bulletin No. 13-01) to calculate the area wage indexes, with updates as reflected in OMB Bulletin Nos. 15-01 and 17-01. Similarly, in the CY 2020 OPPS/ASC proposed rule (84 FR 39431), for the proposed CY 2020 OPPS wage indexes, we proposed to continue to use the OMB delineations that were adopted under the OPPS, beginning with CY 2015 (based on the revised delineations issued in OMB Bulletin No. 13-01) to calculate the area wage indexes, with updates as reflected in OMB Bulletin Nos. 15-01 and 17-01. We did not receive any public comments on our proposal. Accordingly, for the reasons discussed above and in the CY 2020 OPPS/ASC proposed rule (84 FR 39430 through 39431), we are finalizing our proposal to continue to use the OMB delineations that were adopted beginning with CY 2015 to calculate area wage indexes under the OPPS, with updates as reflected in the OMB Bulletin Nos. 15-01, and 17-01.
CBSAs are made up of one or more constituent counties. Each CBSA and constituent county has its own unique identifying codes. The FY 2018 IPPS/LTCH PPS final rule (82 FR 38130) discussed the two different lists of codes to identify counties: Social Security Administration (SSA) codes and Federal Information Processing Standard (FIPS) codes. Historically, CMS listed and used SSA and FIPS county codes to identify and crosswalk counties to CBSA codes for purposes of the IPPS and OPPS wage indexes. However, the SSA county codes are no longer being maintained and updated, although the FIPS codes continue to be maintained by the U.S. Census Bureau. The Census Bureau's most current statistical area information is derived from ongoing census data received since 2010; the most recent data are from 2015. The Census Bureau maintains a complete list of changes to counties or county equivalent entities on the website at: https://www.census.gov/geo/reference/county-changes.html (which, as of May 6, 2019, migrated to: https://www.census.gov/programs-surveys/geography.html). In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38130), for purposes of crosswalking counties to CBSAs for the IPPS wage index, we finalized our proposal to discontinue the use of the SSA county codes and begin using only the FIPS county codes. Similarly, for the purposes of crosswalking counties to CBSAs for the OPPS wage index, in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59260), we finalized our proposal to discontinue the use of SSA county codes and begin using only the FIPS county codes. For CY 2020, under the OPPS, we are continuing to use only the FIPS county codes for purposes of crosswalking counties to CBSAs.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39431), we proposed to use the FY 2020 hospital IPPS post-reclassified wage index for urban and rural areas as the wage index for the OPPS to determine the wage adjustments for both the OPPS payment rate and the copayment standardized amount for CY 2020. Therefore, we stated in the proposed rule that any adjustments for the FY 2020 IPPS post-reclassified wage index, including, but not limited to, any policies finalized under the IPPS to address wage index disparities between low and high wage index value hospitals, would be reflected in the final CY 2020 OPPS wage index beginning on January 1, 2020. (We referred readers to the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19373 through 19399) and the proposed FY 2020 hospital wage index files posted on the CMS website.) With regard to budget neutrality for the CY 2020 OPPS wage index, we referred readers to section II.B. of the CY 2020 OPPS/ASC proposed rule. We stated that we continue to believe that using the IPPS wage index as the source of an adjustment factor for the OPPS is reasonable and logical, given the inseparable, subordinate status of the HOPD within the hospital overall. Summarized below are the comments we received regarding our proposal to use the final FY 2020 hospital IPPS post-reclassified wage index for urban and rural areas as the wage index for the OPPS, including any adjustments for the final FY 2020 IPPS post-reclassified wage index as discussed above, along with our responses.
Comment: Several commenters supported CMS adopting the finalized post-reclassified wage index from the FY 2020 IPPS/LTCH PPS final rule for use under the OPPS. Many of these commenters noted that the gap in payment between rural and urban hospitals has contributed to disparities in care and noted that increasing the wage index for hospitals with wage index values below the 25th percentile wage index value will help to lessen the gap. Some of these commenters noted that this change will help rural areas have access to quality, affordable health care. One commenter supported the proposal to increase the wage index for hospitals with wage index values below the 25th percentile, but wanted CMS to consider this solution temporary until the wage index is more equitable between hospitals.
Response: We appreciate the commenters' support. In response to the comment that CMS should consider the increase in the wage index for hospitals with wage index values below the 25th percentile wage index value (that it, low wage index hospitals) temporary until the wage index is more equitable between hospitals, as we stated in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42326 through 42327), the increase in the IPPS wage index for low wage index hospitals is not intended to be permanent. As we stated in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42326 through 42327), we expect that this policy will be in place for at least 4 years in order to allow employee compensation increases implemented by low wage index hospitals sufficient time to be reflected in the wage index calculation. We stated in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42327) that, once there has been sufficient time for that increased employee compensation to be reflected in the wage data, there should not be a continuing need for this policy.
Comment: Several commenters supported the proposal to increase the wage index for low wage index hospitals but wanted it implemented in a non-budget neutral manner. They believe this would mitigate disparities for median wage index hospitals. Several commenters opposed the proposal to recalculate the wage index to help the lowest wage hospitals. These commenters believed that applying a budget neutrality adjustment for all hospitals to offset the increase in payments for low wage index hospitals would result in a significant loss of resources for patient care in other hospitals. While these commenters understood and appreciated the goal of the proposed changes to increase the wage index for low wage hospitals, they did not believe that these policies would help rural hospitals. They believed that certain communities would benefit from increasing the wage index for low wage hospitals but believed this policy does not adequately recognize differences in geographic labor markets. They further claimed that the offsetting reductions to the wage index in some areas will hinder hospitals' ability to attract and recruit quality health care practitioners.
Some commenters noted that OPPS payments to hospitals in their respective states would decrease by millions in CY 2020 due to the budget neutral implementation of the increase in the wage index for low wage hospitals. These commenters noted that any reduction in Medicare payments would force hospitals to reduce staff and/or salary and benefits. One commenter noted that, for many years, the disparities among geographic areas have continued to grow and have resulted in challenges recruiting staff. Some commenters recommended CMS convene a meeting to understand all of the challenges and issues in order to develop a comprehensive reform of the wage index. One commenter recommended that, if CMS is going to redistribute the area wage index, CMS offset the increased wage index for very low wage areas with a budget neutrality adjustment to the wage index applied evenly to all hospitals. However, this commenter preferred that CMS not use budget neutrality for the area wage index. They did not believe that the budget neutrality adjustment policy follows statutory requirements for adjusting the area wage index that require CMS to address real differences in labor costs. Several commenters believed CMS went beyond its authority in reallocating funding from hospitals in high wage areas, to provide funding to low wage area hospitals, without any relationship to actual wage-related data for the impacted areas. Another commenter strongly opposed decreasing payments to some or all hospitals to offset an increase in the area wage index for low wage index hospitals and did not believe the rationale in the FY 2020 IPPS final rule supported this change. One commenter opposed CMS making a budget neutrality adjustment across all hospitals as well as the transition wage index adjustment to ensure that no hospital's wage index decreases by more than 5 percent. This commenter believed that these adjustments negatively impact hospitals in the bottom quartile of wage index that would have seen a larger increase in payment without these additional adjustments.
Response: As we stated in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42331), the intent of the wage index increase for hospitals with wage indexes below the 25th percentile wage index value across all hospitals (that is, low wage index hospitals) is to increase the accuracy of the wage index as a technical adjustment, and not to use the wage index as a policy tool to address non-wage issues related to rural hospitals, or the laudable goals of the overall financial health of hospitals in low wage areas or broader wage index reform. As we stated in the FY 2020 IPPS/LTCH PPS final rule, we believe the wage index increase we finalized for low wage index hospitals increases the accuracy of the wage index as a relative measure because it allows low wage index hospitals to increase their employee compensation in ways that we would expect if there were no lag in reflecting compensation adjustments in the wage index. Thus, we stated in the FY 2020 IPPS/LTCH PPS final rule that we believe the IPPS wage index adjustment for low wage index hospitals will appropriately reflect the relative hospital wage level in those areas compared to the national average wage level. We further stated in the FY 2020 IPPS/LTCH PPS final rule that because this policy is based on the actual wages that we expect low wage index hospitals to pay, it falls within the scope of the authority of section 1886(d)(3)(E) of the Act.
However, we note that, in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42331 through 42332), we did not finalize our budget neutrality proposal to decrease the wage index for hospitals with wage index values above the 75th percentile wage index value to offset the estimated increase in payments to low wage index hospitals. Instead, in the FY 2020 IPPS/LTCH PPS final rule, consistent with our current methodology for implementing wage index budget neutrality under the IPPS, we finalized a budget neutrality adjustment to the IPPS national standardized amount for all hospitals so that the increase in the IPPS wage index for low wage index hospitals is implemented in a budget neutral manner. As explained in the FY 2020 IPPS/LTCH PPS final rule (84 FR42331), under section 1886(d)(3)(E) of the Act, the IPPS wage index adjustment is required to be implemented in a budget neutral manner. We further noted in the FY 2020 IPPS/LTCH PPS final rule that, even if the wage index were not required to be budget neutral, we would consider it inappropriate to use the wage index to increase or decrease overall spending. Similarly, under section 1886(t)(2)(D) and (9)(B) of the Act, the OPPS wage index adjustment is required to be implemented in a budget neutral manner. Accordingly, consistent with the policy finalized in the FY 2020 IPPS/LTCH PPS final rule, in this CY 2020 OPPS/ASC final rule with comment period, we are finalizing a budget neutrality adjustment to the conversion factor for all hospitals paid under the OPPS so that the increase in the OPPS wage index for low wage index hospitals is implemented in a budget neutral manner. We refer readers to section II.B. of this final rule with comment period for a discussion of budget neutrality. In addition, we refer readers to the FY 2020 IPPS/LTCH PPS final rule (84 FR 42328 through 42332) for further discussion of the final FY 2020 IPPS wage index policies (including the transition wage index adjustment) and detailed responses to similar comments.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39431), we proposed to use the FY 2020 IPPS post-reclassified wage index for urban and rural areas as the wage index under the OPPS to determine the wage adjustments for both the OPPS payment rate and the copayment standardized amount. Because we continue to believe that using the IPPS post-reclassified wage index as the source of the wage index adjustment factor under the OPPS is reasonable and logical given the inseparable, subordinate status of the HOPD within the hospital overall, as proposed, we are finalizing the use of the FY 2020 hospital IPPS post-reclassified wage index for urban and rural areas as the wage index under the OPPS to determine the wage adjustments for both the OPPS payment rate and the copayment standardized amount for CY 2020. Accordingly, any adjustments for the final FY 2020 IPPS post-reclassified wage index, including, but not limited to, any policies finalized in the FY 2020 IPPS/LTCH PPS final rule to address wage index disparities between low and high wage index value hospitals, will be reflected in the final CY 2020 OPPS wage index beginning on January 1, 2020.
Comment: Several commenters noted support for the revised rural floor policy finalized in the FY 2020 IPPS/LTCH final rule. Many of these commenters supported the proposal to exclude the wage data of urban hospitals that reclassify as rural in calculating the rural floor. These commenters suggested that including the wage data of these hospitals in the rural floor calculation has inflated wage index values in certain states and that excluding the wage data of these hospitals will have positive effects on OPPS payment for rural hospitals.
Response: We thank commenters for their support.
Comment: A few commenters opposed the change to exclude the wage data of urban hospitals that have been reclassified as rural in calculating the IPPS rural floor. One of these commenters believed that CMS lacks the legal authority to remove from the rural floor calculation the wage data of hospitals that have been reclassified from urban to rural as implemented in the FY 2020 IPPS/LTCH final rule. This commenter believed CMS misread the applicable law in Section 1886(d)(8)(E) of the Act. One of the commenter's believed that removing the urban to rural reclassifications from the calculation of the rural floor penalizes hospitals that are allowed to reclassify under HHS authority.
One commenter believed that CMS should put more structure around the rural floor policy and should not apply the rural floor in primarily urban states with only one or two rural facilities. The commenter believed that this would reduce the potential for gaming the system in determining an equitable wage adjustment.
Response: We addressed similar comments in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42334 through 42336). As provided in the FY 2020 IPPS/LTCH final rule (84 FR 42334), in the absence of broader wage index reform from Congress, we believe it is appropriate to revise the rural floor calculation as part of an effort to reduce wage index disparities. Regarding CMS's statutory authority to exclude the wage data of urban hospitals reclassified as rural from the IPPS rural floor calculation, as we stated in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42334), we believe our calculation methodology is permissible under section 1886(d)(8)(E) of the Act (as implemented in § 412.103) and the rural floor statute (section 4410 of Pub. L. 105-33). Further, as we discussed in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42336), we do not believe this policy penalizes or adversely impacts urban hospitals that have reclassified as rural. We refer readers to the FY 2020 IPPS/LTCH PPS final rule (84 FR 42332 through 42336) for further discussion of this policy and detailed responses to similar comments. We note that impact files and supporting data files available on the FY 2020 IPPS Final Rule Home Page provide the data necessary to understand the impact of the finalized policies under the IPPS. Furthermore, we appreciate the comment that CMS should not apply the rural floor in primarily urban states with only one or two rural facilities; however, because we consider this comment to be outside the scope of the CY 2020 OPPS wage index proposals, we are not addressing it in this final rule with comment period.
As we discussed above, we continue to believe that using the IPPS post-reclassified wage index as the source of the wage index adjustment factor under the OPPS is reasonable and logical given the inseparable, subordinate status of the HOPD within the hospital overall. Thus, as proposed, we are using the FY 2020 hospital IPPS post-reclassified wage index for urban and rural areas as the wage index under the OPPS to determine the wage adjustments for both the OPPS payment rate and the copayment standardized amount for CY 2020. Accordingly, as we proposed, any adjustments for the final FY 2020 IPPS post-reclassified wage index, including, but not limited to, the revised rural floor calculation methodology and other IPPS wage index policies finalized in the FY 2020 IPPS/LTCH PPS final rule to address wage index disparities, will be reflected in the final CY 2020 OPPS wage index beginning on January 1, 2020.
After considering the public comments received, for the reasons discussed earlier in this section and in the CY 2020 OPPS/ASC proposed rule, we are finalizing without modification our proposal to use the final FY 2020 IPPS post-reclassified wage index for urban and rural areas as the wage index under the OPPS to determine the wage adjustments for both the OPPS payment rate and the copayment standardized amount for CY 2020. Accordingly, as we proposed, any adjustments for the final FY 2020 IPPS post-reclassified wage index (as set forth in the FY 2020 IPPS/LTCH PPS final rule, 84 FR 42300 through 42339), including, but not limited to, any policies finalized in the FY 2020 IPPS/LTCH PPS final rule to address wage index disparities between low and high wage index value hospitals (as set forth at 84 FR 42300 through 42339), will be reflected in the final CY 2020 OPPS wage index beginning on January 1, 2020. As discussed above, we note that in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42325 through 42332), we did not finalize our budget neutrality proposal to decrease the wage index for hospitals with wage index values above the 75th percentile wage index value to offset the estimated increase in payments to hospitals with wage index values below the 25th percentile wage index value, and thus this budget neutrality policy will not be applied under the OPPS. Instead, in the FY 2020 IPPS/LTCH PPS final rule, consistent with our current methodology for implementing IPPS wage index budget neutrality, we finalized a budget neutrality adjustment to the IPPS national standardized amount for all hospitals so that the increase in the IPPS wage index for low wage index hospitals is implemented in a budget neutral manner. Consistent with this IPPS policy, in this CY 2020 OPPS/ASC final rule with comment period, we are finalizing a budget neutrality adjustment to the conversion factor for all hospitals paid under the OPPS so that the increase in the OPPS wage index for low wage index hospitals is implemented in a budget neutral manner. We refer readers to section II.B. of this final rule with comment period for a discussion of budget neutrality.
Hospitals that are paid under the OPPS, but not under the IPPS, do not have an assigned hospital wage index under the IPPS. Therefore, for non-IPPS hospitals paid under the OPPS, it is our longstanding policy to assign the wage index that would be applicable if the hospital were paid under the IPPS, based on its geographic location and any applicable wage index adjustments. In the CY 2020 OPPS/ASC proposed rule (84 FR 39431), we proposed to continue this policy for CY 2020, and included a brief summary of the major proposed FY 2020 IPPS wage index policies and adjustments that we proposed to apply to these hospitals under the OPPS for CY 2020, which we have summarized below. We refer readers to the FY 2020 IPPS/LTCH PPS final rule (84 FR 42300 through 42339) for a detailed discussion of the final changes to the FY 2020 IPPS wage indexes.
It has been our longstanding policy to allow non-IPPS hospitals paid under the OPPS to qualify for the out-migration adjustment if they are located in a section 505 out-migration county (section 505 of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA)). Applying this adjustment is consistent with our policy of adopting IPPS wage index policies for hospitals paid under the OPPS. We note that, because non-IPPS hospitals cannot reclassify, they are eligible for the out-migration wage index adjustment if they are located in a section 505 out-migration county. This is the same out-migration adjustment policy that applies if the hospital were paid under the IPPS. For CY 2020, we proposed to continue our policy of allowing non-IPPS hospitals paid under the OPPS to qualify for the out-migration adjustment if they are located in a section 505 out-migration county (section 505 of the MMA). In addition, for non-IPPS hospitals paid under the OPPS, we proposed to apply any policies that are finalized under the IPPS relating to wage index disparities. We also proposed that the wage index that would apply to non-IPPS hospitals for CY 2020 would include the rural floor adjustment. We did not receive any public comments on these proposals. Accordingly, for the reasons discussed above and in the CY 2020 OPPS/ASC proposed rule (84 FR 39431), we are finalizing these proposals without modifications.
For CMHCs, for CY 2020, we proposed to continue to calculate the wage index by using the post-reclassification IPPS wage index based on the CBSA where the CMHC is located. We also proposed to apply any policies that are finalized under the IPPS relating to wage index disparities. In addition, we proposed that the wage index that would apply to CMHCs for CY 2020 would include the rural floor adjustment. Also, we proposed that the wage index that would apply to CMHCs would not include the out-migration adjustment because that adjustment only applies to hospitals. We did not receive any public comments on these proposals. Therefore, for the reasons discussed above and in the CY 2020 OPPS/ASC proposed rule (84 FR 39431), we are finalizing these proposals without modifications.
Table 4 associated with the FY 2020 IPPS/LTCH PPS final rule (available via the internet on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html) identifies counties eligible for the out-migration adjustment. Table 2 associated with the FY 2020 IPPS/LTCH PPS final rule (available for download via the website above) identifies IPPS hospitals that will receive the out-migration adjustment for FY 2020. We are including the out-migration adjustment information from Table 2 associated with the FY 2020 IPPS/LTCH PPS final rule as Addendum L to this final rule with comment period with the addition of non-IPPS hospitals that will receive the section 505 out-migration adjustment under this CY 2020 OPPS/ASC final rule with comment period. Addendum L is available via the internet on the CMS website. We refer readers to the CMS website for the OPPS at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html. At this link, readers will find a link to the final FY 2020 IPPS wage index tables and Addendum L.
D. Statewide Average Default Cost-to-Charge Ratios (CCRs)
In addition to using CCRs to estimate costs from charges on claims for ratesetting, CMS uses overall hospital-specific CCRs calculated from the hospital's most recent cost report to determine outlier payments, payments for pass-through devices, and monthly interim transitional corridor payments under the OPPS during the PPS year. For certain hospitals, under the regulations at 42 CFR 419.43(d)(5)(iii), CMS uses the statewide average default CCRs to determine the payments mentioned earlier if it is unable to determine an accurate CCR for a hospital in certain circumstances. This includes hospitals that are new, hospitals that have not accepted assignment of an existing hospital's provider agreement, and hospitals that have not yet submitted a cost report. CMS also uses the statewide average default CCRs to determine payments for hospitals whose CCR falls outside the predetermined ceiling threshold for a valid CCR or for hospitals in which the most recent cost report reflects an all-inclusive rate status (Medicare Claims Processing Manual (Pub. 100-04), Chapter 4, Section 10.11).
We discussed our policy for using default CCRs, including setting the ceiling threshold for a valid CCR, in the CY 2009 OPPS/ASC final rule with comment period (73 FR 68594 through 68599) in the context of our adoption of an outlier reconciliation policy for cost reports beginning on or after January 1, 2009. For details on our process for calculating the statewide average CCRs, we referred readers to the CY 2020 OPPS proposed rule Claims Accounting Narrative that is posted on the CMS website. In the CY 2020 OPPS/ASC proposed rule (84 FR 39432), we proposed to update the default ratios for CY 2020 using the most recent cost report data. We indicated that we would update these ratios in this final rule with comment period if more recent cost report data are available.
We did not receive any public comments on our proposal to use statewide average default CCRs if we cannot calculate a CCR for a hospital and to use these CCRs to adjust charges on claims to costs for setting the final CY 2020 OPPS payment weights. Therefore, we finalizing our proposal without modification.
As we stated in the CY 2020 OPPS/ASC proposed rule (84 FR 39432), we are no longer publishing a table in the Federal Register containing the statewide average CCRs in the annual OPPS proposed rule and final rule. These CCRs with the upper limit will be available for download with each OPPS CY proposed rule and final rule on the CMS website. We refer readers to the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices.html; click on the link on the left of the page titled “Hospital Outpatient Regulations and Notices” and then select the relevant regulation to download the statewide CCRs and upper limit in the downloads section of the web page.
E. Adjustment for Rural Sole Community Hospitals (SCHs) and Essential Access Community Hospitals (EACHs) Under Section 1833(t)(13)(B) of the Act for CY 2020
In the CY 2006 OPPS final rule with comment period (70 FR 68556), we finalized a payment increase for rural sole community hospitals (SCHs) of 7.1 percent for all services and procedures paid under the OPPS, excluding drugs, biologicals, brachytherapy sources, and devices paid under the pass-through payment policy, in accordance with section 1833(t)(13)(B) of the Act, as added by section 411 of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) (Pub. L. 108-173). Section 1833(t)(13) of the Act provided the Secretary the authority to make an adjustment to OPPS payments for rural hospitals, effective January 1, 2006, if justified by a study of the difference in costs by APC between hospitals in rural areas and hospitals in urban areas. Our analysis showed a difference in costs for rural SCHs. Therefore, for the CY 2006 OPPS, we finalized a payment adjustment for rural SCHs of 7.1 percent for all services and procedures paid under the OPPS, excluding separately payable drugs and biologicals, brachytherapy sources, items paid at charges reduced to costs, and devices paid under the pass-through payment policy, in accordance with section 1833(t)(13)(B) of the Act.
In the CY 2007 OPPS/ASC final rule with comment period (71 FR 68010 and 68227), for purposes of receiving this rural adjustment, we revised our regulations at § 419.43(g) to clarify that essential access community hospitals (EACHs) are also eligible to receive the rural SCH adjustment, assuming these entities otherwise meet the rural adjustment criteria. Currently, two hospitals are classified as EACHs, and as of CY 1998, under section 4201(c) of Public Law 105-33, a hospital can no longer become newly classified as an EACH.
This adjustment for rural SCHs is budget neutral and applied before calculating outlier payments and copayments. We stated in the CY 2006 OPPS final rule with comment period (70 FR 68560) that we would not reestablish the adjustment amount on an annual basis, but we may review the adjustment in the future and, if appropriate, would revise the adjustment. We provided the same 7.1 percent adjustment to rural SCHs, including EACHs, again in CYs 2008 through 2019. Further, in the CY 2009 OPPS/ASC final rule with comment period (73 FR 68590), we updated the regulations at § 419.43(g)(4) to specify, in general terms, that items paid at charges adjusted to costs by application of a hospital-specific CCR are excluded from the 7.1 percent payment adjustment.
In the CY 2020 OPPS/ASC proposed rule (84 FR 58870 through 58871), for the CY 2020 OPPS, we proposed to continue the current policy of a 7.1 percent payment adjustment that is done in a budget neutral manner for rural SCHs, including EACHs, for all services and procedures paid under the OPPS, excluding separately payable drugs and biologicals, brachytherapy sources, items paid at charges reduced to costs, and devices paid under the pass-through payment policy.
Comment: Several commenters supported the proposal to continue the 7.1 percent payment adjustment.
Response: We appreciate the commenters' support.
Comment: One commenter requested that CMS make the 7.1 percent rural adjustment permanent. The commenter appreciated the policy that CMS adopted in CY 2019 where we stated that the 7.1 percent rural adjustment would continue to be in place until our data support establishing a different rural adjustment percentage. However, the commenter believed that this policy still does not provide enough certainty for rural SCHs and EACHs to know whether they should take into account the rural SCH adjustment when attempting to calculate expected revenues for their hospital budgets.
Response: We thank the commenter for their input. We believe that our currrent policy, which states that the 7.1 percent payment adjustment for rural SCHs and EACHs will remain in effect until our data show that a different percentage for the rural payment adjustment is necessary, provides sufficient budget predictability for rural SCHs and EACHs. Providers would receive notice in a proposed rule before any changes to the rural adjustment percentage would be implemented.
Comment: Some commenters requested that CMS expand the payment adjustment for rural SCHs and EACHs to additional types of hospitals. One commenter requested that the payment adjustment apply to include urban SCHs because, according to the commenter, urban SCHs care for patient populations similar to rural SCHs and EACHs, face similar financial challenges to rural SCHs and EACHs, and act as safety net providers for rural areas despite their designation as urban providers. Another commenter requested that the payment adjustment also apply to Medicare-dependent hospitals (MDHs) because, according to the commenter, these hospitals face similar financial challenges to rural SCHs and EACHs, and MDHs play a similar safety net role to rural SCHs and EACHs, especially for Medicare. One commenter requested that payment rates for OPPS services for all rural hospitals be increased to reduce financial vulnerability for rural hospitals related to the high share of Medicare and Medicaid beneficiaries they serve.
Response: We thank the commenters for their comments. However, the analysis we did to compare costs of urban providers to those of rural providers did not support an add-on adjustment for providers other than rural SCHs and EACHs. In addition, our follow-up analyses performed in recent years have not shown differences in costs for all services for any of the additional types of providers mentioned by the commenters. Accordingly, we do not believe we currently have a basis to expand the payment adjustment to any providers other than rural SCHs and EACHs.
After consideration of the public comments we received, we are finalizing our proposal, without modification, to continue the current policy of a 7.1 percent payment adjustment that is done in a budget neutral manner for rural SCHs, including EACHs, for all services and procedures paid under the OPPS, excluding separately payable drugs and biologicals, devices paid under the pass-through payment policy, and items paid at charges reduced to costs.
F. Payment Adjustment for Certain Cancer Hospitals for CY 2020
1. Background
Since the inception of the OPPS, which was authorized by the Balanced Budget Act of 1997 (BBA) (Pub. L. 105-33), Medicare has paid the 11 hospitals that meet the criteria for cancer hospitals identified in section 1886(d)(1)(B)(v) of the Act under the OPPS for covered outpatient hospital services. These cancer hospitals are exempted from payment under the IPPS. With the Medicare, Medicaid and SCHIP Balanced Budget Refinement Act of 1999 (Pub. L. 106-113), Congress established section 1833(t)(7) of the Act, “Transitional Adjustment to Limit Decline in Payment,” to determine OPPS payments to cancer and children's hospitals based on their pre-BBA payment amount (often referred to as “held harmless”).
As required under section 1833(t)(7)(D)(ii) of the Act, a cancer hospital receives the full amount of the difference between payments for covered outpatient services under the OPPS and a “pre-BBA amount.” That is, cancer hospitals are permanently held harmless to their “pre-BBA amount,” and they receive transitional outpatient payments (TOPs) or hold harmless payments to ensure that they do not receive a payment that is lower in amount under the OPPS than the payment amount they would have received before implementation of the OPPS, as set forth in section 1833(t)(7)(F) of the Act. The “pre-BBA amount” is the product of the hospital's reasonable costs for covered outpatient services occurring in the current year and the base payment-to-cost ratio (PCR) for the hospital defined in section 1833(t)(7)(F)(ii) of the Act. The “pre-BBA amount” and the determination of the base PCR are defined at 42 CFR 419.70(f). TOPs are calculated on Worksheet E, Part B, of the Hospital Cost Report or the Hospital Health Care Complex Cost Report (Form CMS-2552-96 or Form CMS-2552-10, respectively), as applicable each year. Section 1833(t)(7)(I) of the Act exempts TOPs from budget neutrality calculations.
Section 3138 of the Affordable Care Act amended section 1833(t) of the Act by adding a new paragraph (18), which instructs the Secretary to conduct a study to determine if, under the OPPS, outpatient costs incurred by cancer hospitals described in section 1886(d)(1)(B)(v) of the Act with respect to APC groups exceed outpatient costs incurred by other hospitals furnishing services under section 1833(t) of the Act, as determined appropriate by the Secretary. Section 1833(t)(18)(A) of the Act requires the Secretary to take into consideration the cost of drugs and biologicals incurred by cancer hospitals and other hospitals. Section 1833(t)(18)(B) of the Act provides that, if the Secretary determines that cancer hospitals' costs are higher than those of other hospitals, the Secretary shall provide an appropriate adjustment under section 1833(t)(2)(E) of the Act to reflect these higher costs. In 2011, after conducting the study required by section 1833(t)(18)(A) of the Act, we determined that outpatient costs incurred by the 11 specified cancer hospitals were greater than the costs incurred by other OPPS hospitals. For a complete discussion regarding the cancer hospital cost study, we refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74200 through 74201).
Based on these findings, we finalized a policy to provide a payment adjustment to the 11 specified cancer hospitals that reflects their higher outpatient costs, as discussed in the CY 2012 OPPS/ASC final rule with comment period (76 FR 74202 through 74206). Specifically, we adopted a policy to provide additional payments to the cancer hospitals so that each cancer hospital's final PCR for services provided in a given calendar year is equal to the weighted average PCR (which we refer to as the “target PCR”) for other hospitals paid under the OPPS. The target PCR is set in advance of the calendar year and is calculated using the most recently submitted or settled cost report data that are available at the time of final rulemaking for the calendar year. The amount of the payment adjustment is made on an aggregate basis at cost report settlement. We note that the changes made by section 1833(t)(18) of the Act do not affect the existing statutory provisions that provide for TOPs for cancer hospitals. The TOPs are assessed, as usual, after all payments, including the cancer hospital payment adjustment, have been made for a cost reporting period. For CYs 2012 and 2013, the target PCR for purposes of the cancer hospital payment adjustment was 0.91. For CY 2014, the target PCR was 0.90. For CY 2015, the target PCR was 0.90. For CY 2016, the target PCR was 0.92, as discussed in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70362 through 70363). For CY 2017, the target PCR was 0.91, as discussed in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79603 through 79604). For CY 2018, the target PCR was 0.88, as discussed in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59265 through 59266). For CY 2019, the target PCR was 0.88, as discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58871 through 58873).
2. Policy for CY 2020
Section 16002(b) of the 21st Century Cures Act (Pub. L. 114-255) amended section 1833(t)(18) of the Act by adding subparagraph (C), which requires that in applying § 419.43(i) (that is, the payment adjustment for certain cancer hospitals) for services furnished on or after January 1, 2018, the target PCR adjustment be reduced by 1.0 percentage point less than what would otherwise apply. Section 16002(b) also provides that, in addition to the percentage reduction, the Secretary may consider making an additional percentage point reduction to the target PCR that takes into account payment rates for applicable items and services described under section 1833(t)(21)(C) of the Act for hospitals that are not cancer hospitals described under section 1886(d)(1)(B)(v) of the Act. Further, in making any budget neutrality adjustment under section 1833(t) of the Act, the Secretary shall not take into account the reduced expenditures that result from application of section 1833(t)(18)(C) of the Act.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39433), for CY 2020, we proposed to provide additional payments to the 11 specified cancer hospitals so that each cancer hospital's final PCR is equal to the weighted average PCR (or “target PCR”) for the other OPPS hospitals, using the most recent submitted or settled cost report data that were available at the time of the development of the proposed rule, reduced by 1.0 percentage point, to comply with section 16002(b) of the 21st Century Cures Act.
We did not propose an additional reduction beyond the 1.0 percentage point reduction required by section 16002(b) for CY 2020. To calculate the proposed CY 2020 target PCR, we are using the same extract of cost report data from HCRIS, as discussed in section II.A. of the CY 2020 OPPS/ASC proposed rule and this final rule with comment period, used to estimate costs for the CY 2020 OPPS. Using these cost report data, we included data from Worksheet E, Part B, for each hospital, using data from each hospital's most recent cost report, whether as submitted or settled.
We then limited the dataset to the hospitals with CY 2018 claims data that we used to model the impact of the proposed CY 2020 APC relative payment weights (3,770 hospitals) because it is appropriate to use the same set of hospitals that are being used to calibrate the modeled CY 2020 OPPS. The cost report data for the hospitals in this dataset were from cost report periods with fiscal year ends ranging from 2016 to 2018. We then removed the cost report data of the 49 hospitals located in Puerto Rico from our dataset because we did not believe their cost structure reflected the costs of most hospitals paid under the OPPS, and, therefore, their inclusion may bias the calculation of hospital-weighted statistics. We also removed the cost report data of 23 hospitals because these hospitals had cost report data that were not complete (missing aggregate OPPS payments, missing aggregate cost data, or missing both), so that all cost reports in the study would have both the payment and cost data necessary to calculate a PCR for each hospital, leading to a proposed analytic file of 3,539 hospitals with cost report data.
Using this smaller dataset of cost report data, we estimated that, on average, the OPPS payments to other hospitals furnishing services under the OPPS were approximately 90 percent of reasonable cost (weighted average PCR of 0.90). Therefore, after applying the 1.0 percentage point reduction, as required by section 16002(b) of the 21st Century Cures Act, we proposed that the payment amount associated with the cancer hospital payment adjustment to be determined at cost report settlement would be the additional payment needed to result in a proposed target PCR equal to 0.89 for each cancer hospital.
We did not receive any public comments on our proposals. Therefore, we are finalizing our proposed cancer hospital payment adjustment methodology without modification. For this final rule with comment period, we are using the most recent cost report data through June 30, 2019 to update the adjustment. This updated yields a target PCR of 0.90. We limited the dataset to hospitals with CY 2018 claims data that we used to model the impact of the CY 2020 APC relative payment weights (3,763) because it is appropriate to use the same set of hospitals that we are using to calibrate the modeled CY 2020 OPPS. The cost report data for the hospitals in the dataset were from cost report periods with fiscal years ends ranging from 2010 to 2018. We then removed the cost report data of the 46 hospitals located in Puerto Rico from our dataset because we do not believe their cost structure reflects the cost of most hospitals paid under the OPPS and, therefore, their inclusion may bias the calculation of hospital-weighted statistics. We also removed the cost report data of 21 hospitals because these hospitals had cost report data that were not complete (missing aggregate OPPS payments, missing aggregate cost data, or missing both), so that all cost report in the study would have both the payment and cost data necessary to calculate a PCR for each hospital, leading to an analytic file of 3,523 hospitals with cost report data.
Using this smaller dataset of cost report data, we estimated a target PCR of 0.90. Therefore, after applying the 1.0 percentage point reduction as required by section 1602(b) of the 21st Century Cures Act, we are finalizing that the payment amount associated with the cancer hospital adjustment to be determined at cost report settlement will be the additional payment needed to result in a PCR equal to 0.89 for each cancer hospital.
Table 7 shows the estimated percentage increase in OPPS payments to each cancer hospital for CY 2020, due to the cancer hospital payment adjustment policy. The actual amount of the CY 2020 cancer hospital payment adjustment for each cancer hospital will be determined at cost report settlement and will depend on each hospital's CY 2020 payments and costs. We note that the requirements contained in section 1833(t)(18) of the Act do not affect the existing statutory provisions that provide for TOPs for cancer hospitals. The TOPs will be assessed, as usual, after all payments, including the cancer hospital payment adjustment, have been made for a cost reporting period.

G. Hospital Outpatient Outlier Payments
1. Background
The OPPS provides outlier payments to hospitals to help mitigate the financial risk associated with high-cost and complex procedures, where a very costly service could present a hospital with significant financial loss. As explained in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66832 through 66834), we set our projected target for aggregate outlier payments at 1.0 percent of the estimated aggregate total payments under the OPPS for the prospective year. Outlier payments are provided on a service-by-service basis when the cost of a service exceeds the APC payment amount multiplier threshold (the APC payment amount multiplied by a certain amount) as well as the APC payment amount plus a fixed-dollar amount threshold (the APC payment plus a certain amount of dollars). In CY 2019, the outlier threshold was met when the hospital's cost of furnishing a service exceeded 1.75 times (the multiplier threshold) the APC payment amount and exceeded the APC payment amount plus $4,825 (the fixed-dollar amount threshold) (83 FR 58874 through 58875). If the cost of a service exceeds both the multiplier threshold and the fixed-dollar threshold, the outlier payment is calculated as 50 percent of the amount by which the cost of furnishing the service exceeds 1.75 times the APC payment amount. Beginning with CY 2009 payments, outlier payments are subject to a reconciliation process similar to the IPPS outlier reconciliation process for cost reports, as discussed in the CY 2009 OPPS/ASC final rule with comment period (73 FR 68594 through 68599).
It has been our policy to report the actual amount of outlier payments as a percent of total spending in the claims being used to model the OPPS. Our estimate of total outlier payments as a percent of total CY 2018 OPPS payments, using CY 2018 claims available for the CY 2020 OPPS/ASC proposed rule (84 FR 39434 through 39435) was approximately 1.0 percent of the total aggregated OPPS payments. Therefore, for CY 2018, we estimated that we paid the outlier target of 1.0 percent of total aggregated OPPS payments. Using an updated claims dataset for this CY 2020 OPPS final rule with comment period, we estimate that we paid approximately 1.00 percent of the total aggregated OPPS payments in outliers for CY 2018.
For the CY 2020 OPPS/ASC proposed rule, using CY 2018 claims data and CY 2019 payment rates, we estimated that the aggregate outlier payments for CY 2019 would be approximately 1.03 percent of the total CY 2019 OPPS payments. We provided estimated CY 2020 outlier payments for hospitals and CMHCs with claims included in the claims data that we used to model impacts in the Hospital-Specific Impacts—Provider-Specific Data file on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
2. Outlier Calculation for CY 2020
In the CY 2020 OPPS/ASC proposed rule (84 FR 39434 through 39435), for CY 2020, we proposed to continue our policy of estimating outlier payments to be 1.0 percent of the estimated aggregate total payments under the OPPS. We proposed that a portion of that 1.0 percent, an amount equal to less than 0.01 percent of outlier payments (or 0.0001 percent of total OPPS payments), would be allocated to CMHCs for PHP outlier payments. This is the amount of estimated outlier payments that would result from the proposed CMHC outlier threshold as a proportion of total estimated OPPS outlier payments. As discussed in section VIII.C. of the CY 2020 OPPS/ASC proposed rule (84 FR 39435), we proposed to continue our longstanding policy that if a CMHC's cost for partial hospitalization services, paid under APC 5853 (Partial Hospitalization for CMHCs), exceeds 3.40 times the payment rate for proposed APC 5853, the outlier payment would be calculated as 50 percent of the amount by which the cost exceeds 3.40 times the proposed APC 5853 payment rate.
For further discussion of CMHC outlier payments, we refer readers to section VIII.C. of the CY 2020 OPPS/ASC proposed rule and this final rule with comment period.
To ensure that the estimated CY 2020 aggregate outlier payments would equal 1.0 percent of estimated aggregate total payments under the OPPS, we proposed that the hospital outlier threshold be set so that outlier payments would be triggered when a hospital's cost of furnishing a service exceeds 1.75 times the APC payment amount and exceeds the APC payment amount plus $4,950.
We calculated the proposed fixed-dollar threshold of $4,950 using the standard methodology most recently used for CY 2019 (83 FR 58874 through 58875). For purposes of estimating outlier payments for the proposed rule, we used the hospital-specific overall ancillary CCRs available in the April 2019 update to the Outpatient Provider-Specific File (OPSF). The OPSF contains provider-specific data, such as the most current CCRs, which are maintained by the MACs and used by the OPPS Pricer to pay claims. The claims that we use to model each OPPS update lag by 2 years.
In order to estimate the CY 2020 hospital outlier payments for the proposed rule, we inflated the charges on the CY 2018 claims using the same inflation factor of 1.11189 that we used to estimate the IPPS fixed-dollar outlier threshold for the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19596). We used an inflation factor of 1.05446 to estimate CY 2019 charges from the CY 2018 charges reported on CY 2018 claims. The methodology for determining this charge inflation factor is discussed in the FY 2019 IPPS/LTCH PPS final rule (83 FR 41717 through 41718). As we stated in the CY 2005 OPPS final rule with comment period (69 FR 65845), we believe that the use of these charge inflation factors is appropriate for the OPPS because, with the exception of the inpatient routine service cost centers, hospitals use the same ancillary and outpatient cost centers to capture costs and charges for inpatient and outpatient services.
As noted in the CY 2007 OPPS/ASC final rule with comment period (71 FR 68011), we are concerned that we could systematically overestimate the OPPS hospital outlier threshold if we did not apply a CCR inflation adjustment factor. Therefore, we proposed to apply the same CCR inflation adjustment factor that we proposed to apply for the FY 2020 IPPS outlier calculation to the CCRs used to simulate the proposed CY 2020 OPPS outlier payments to determine the fixed-dollar threshold. Specifically, for CY 2020, we proposed to apply an adjustment factor of 0.97517 to the CCRs that were in the April 2019 OPSF to trend them forward from CY 2019 to CY 2020. The methodology for calculating the proposed adjustment is discussed in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19597).
To model hospital outlier payments for the proposed rule, we applied the overall CCRs from the April 2019 OPSF after adjustment (using the proposed CCR inflation adjustment factor of 0.97517 to approximate CY 2020 CCRs) to charges on CY 2018 claims that were adjusted (using the proposed charge inflation factor of 1.11189 to approximate CY 2020 charges). We simulated aggregated CY 2020 hospital outlier payments using these costs for several different fixed-dollar thresholds, holding the 1.75 multiplier threshold constant and assuming that outlier payments would continue to be made at 50 percent of the amount by which the cost of furnishing the service would exceed 1.75 times the APC payment amount, until the total outlier payments equaled 1.0 percent of aggregated estimated total CY 2020 OPPS payments. We estimated that a proposed fixed-dollar threshold of $4,950, combined with the proposed multiplier threshold of 1.75 times the APC payment rate, would allocate 1.0 percent of aggregated total OPPS payments to outlier payments. For CMHCs, we proposed that, if a CMHC's cost for partial hospitalization services, paid under APC 5853, exceeds 3.40 times the payment rate for APC 5853, the outlier payment would be calculated as 50 percent of the amount by which the cost exceeds 3.40 times the APC 5853 payment rate.
Section 1833(t)(17)(A) of the Act, which applies to hospitals, as defined under section 1886(d)(1)(B) of the Act, requires that hospitals that fail to report data required for the quality measures selected by the Secretary, in the form and manner required by the Secretary under section 1833(t)(17)(B) of the Act, incur a 2.0 percentage point reduction to their OPD fee schedule increase factor; that is, the annual payment update factor. The application of a reduced OPD fee schedule increase factor results in reduced national unadjusted payment rates that will apply to certain outpatient items and services furnished by hospitals that are required to report outpatient quality data and that fail to meet the Hospital OQR Program requirements. For hospitals that fail to meet the Hospital OQR Program requirements, as we proposed, we are continuing the policy that we implemented in CY 2010 that the hospitals' costs will be compared to the reduced payments for purposes of outlier eligibility and payment calculation. For more information on the Hospital OQR Program, we referred readers to section XIV. of this final rule with comment period.
We received no public comments on our proposal. Therefore, we are finalizing our proposal, without modification, to continue our policy of estimating outlier payments to be 1.0 percent of the estimated aggregate total payments under the OPPS and to use our established methodology to set the OPPS outlier fixed-dollar loss threshold for CY 2020.
3. Final Outlier Calculation
Consistent with historical practice, we used updated data for this final rule with comment period for outlier calculations. For CY 2020, we are applying the overall CCRs from the October 2019 OPSF file after adjustment (using the CCR inflation adjustment factor of 0.97615 to approximate CY 2020 CCRs) to charges on CY 2018 claims that were adjusted using a charge inflation factor of 1.11100 to approximate CY 2020 charges. These are the same CCR adjustment and charge inflation factors that were used to set the IPPS fixed-dollar threshold for the FY 2020 IPPS/LTCH PPS final rule (84 FR 42629). We simulated aggregated CY 2020 hospital outlier payments using these costs for several different fixed-dollar thresholds, holding the 1.75 multiple-threshold constant and assuming that outlier payments will continue to be made at 50 percent of the amount by which the cost of furnishing the service would exceed 1.75 times the APC payment amount, until the total outlier payment equaled 1.0 percent of aggregated estimated total CY 2020 OPPS payments. We estimated that a fixed-dollar threshold of $5,075 combined with the multiple threshold of 1.75 times the APC payment rate, will allocate the 1.0 percent of aggregated total OPPS payments to outlier payments.
For CMHCs, if a CMHC's cost for partial hospitalization services, paid under APC 5853, exceeds 3.40 times the payment rate the outlier payment will be calculated as 50 percent of the amount by which the cost exceeds 3.40 times APC 5853.
H. Calculation of an Adjusted Medicare Payment From the National Unadjusted Medicare Payment
The basic methodology for determining prospective payment rates for HOPD services under the OPPS is set forth in existing regulations at 42 CFR part 419, subparts C and D. For this CY 2020 OPPS/ASC final rule with comment period, the payment rate for most services and procedures for which payment is made under the OPPS is the product of the conversion factor calculated in accordance with section II.B. of this final rule with comment period and the relative payment weight determined under section II.A. of this final rule with comment period. Therefore, the proposed national unadjusted payment rate for most APCs contained in Addendum A to this final rule with comment period (which is available via the internet on the CMS website) and for most HCPCS codes to which separate payment under the OPPS has been assigned in Addendum B to this final rule with comment period (which is available via the internet on the CMS website) was calculated by multiplying the proposed CY 2020 scaled weight for the APC by the CY 2020 conversion factor.
We note that section 1833(t)(17) of the Act, which applies to hospitals, as defined under section 1886(d)(1)(B) of the Act, requires that hospitals that fail to submit data required to be submitted on quality measures selected by the Secretary, in the form and manner and at a time specified by the Secretary, incur a reduction of 2.0 percentage points to their OPD fee schedule increase factor, that is, the annual payment update factor. The application of a reduced OPD fee schedule increase factor results in reduced national unadjusted payment rates that apply to certain outpatient items and services provided by hospitals that are required to report outpatient quality data and that fail to meet the Hospital OQR Program (formerly referred to as the Hospital Outpatient Quality Data Reporting Program (HOP QDRP)) requirements. For further discussion of the payment reduction for hospitals that fail to meet the requirements of the Hospital OQR Program, we refer readers to section XIV of this final rule with comment period.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39435), we demonstrated the steps used to determine the APC payments that will be made in a CY under the OPPS to a hospital that fulfills the Hospital OQR Program requirements and to a hospital that fails to meet the Hospital OQR Program requirements for a service that has any of the following status indicator assignments: “J1”, “J2”, “P”, “Q1”, “Q2”, “Q3”, “Q4”, “R”, “S”, “T”, “U”, or “V” (as defined in Addendum D1 to the proposed rule, which is available via the internet on the CMS website), in a circumstance in which the multiple procedure discount does not apply, the procedure is not bilateral, and conditionally packaged services (status indicator of “Q1” and “Q2”) qualify for separate payment. We noted that, although blood and blood products with status indicator “R” and brachytherapy sources with status indicator “U” are not subject to wage adjustment, they are subject to reduced payments when a hospital fails to meet the Hospital OQR Program requirements.
We did not receive any public comments on these steps under the methodology that we included in the CY 2020 CY OPPS/ASC proposed rule to determine the APC payments for CY 2020. Therefore, we are using the steps in the methodology specified below, as we proposed, to demonstrate the calculation of the final CY 2020 OPPS payments using the same parameters.
Individual providers interested in calculating the payment amount that they will receive for a specific service from the national unadjusted payment rates presented in Addenda A and B to this final rule with comment period (which are available via the internet on the CMS website) should follow the formulas presented in the following steps. For purposes of the payment calculations below, we refer to the national unadjusted payment rate for hospitals that meet the requirements of the Hospital OQR Program as the “full” national unadjusted payment rate. We refer to the national unadjusted payment rate for hospitals that fail to meet the requirements of the Hospital OQR Program as the “reduced” national unadjusted payment rate. The reduced national unadjusted payment rate is calculated by multiplying the reporting ratio of 0.980 times the “full” national unadjusted payment rate. The national unadjusted payment rate used in the calculations below is either the full national unadjusted payment rate or the reduced national unadjusted payment rate, depending on whether the hospital met its Hospital OQR Program requirements to receive the full CY 2020 OPPS fee schedule increase factor.
Step 1. Calculate 60 percent (the labor-related portion) of the national unadjusted payment rate. Since the initial implementation of the OPPS, we have used 60 percent to represent our estimate of that portion of costs attributable, on average, to labor. We refer readers to the April 7, 2000 OPPS final rule with comment period (65 FR 18496 through 18497) for a detailed discussion of how we derived this percentage. During our regression analysis for the payment adjustment for rural hospitals in the CY 2006 OPPS final rule with comment period (70 FR 68553), we confirmed that this labor-related share for hospital outpatient services is appropriate.
The formula below is a mathematical representation of Step 1 and identifies the labor-related portion of a specific payment rate for a specific service.
X is the labor-related portion of the national unadjusted payment rate.
X = .60 * (national unadjusted payment rate).
Step 2. Determine the wage index area in which the hospital is located and identify the wage index level that applies to the specific hospital. We note that, under the CY 2020 OPPS policy for continuing to use the OMB labor market area delineations based on the 2010 Decennial Census data for the wage indexes used under the IPPS, a hold harmless policy for the wage index may apply, as discussed in section II.C. of this final rule with comment period. The wage index values assigned to each area reflect the geographic statistical areas (which are based upon OMB standards) to which hospitals are assigned for FY 2020 under the IPPS, reclassifications through the Medicare Geographic Classification Review Board (MGCRB), section 1886(d)(8)(B) “Lugar” hospitals, reclassifications under section 1886(d)(8)(E) of the Act, as defined in § 412.103 of the regulations, and hospitals designated as urban under section 601(g) of Public Law 98-21. For further discussion of the changes to the FY 2020 IPPS wage indexes, as applied to the CY 2020 OPPS, we refer readers to section II.C. of this final rule with comment period. We are continuing to apply a wage index floor of 1.00 to frontier States, in accordance with section 10324 of the Affordable Care Act of 2010.
Step 3. Adjust the wage index of hospitals located in certain qualifying counties that have a relatively high percentage of hospital employees who reside in the county, but who work in a different county with a higher wage index, in accordance with section 505 of Public Law 108-173. Addendum L to this final rule with comment period (which is available via the internet on the CMS website) contains the qualifying counties and the associated wage index increase developed for the proposed FY 2020 IPPS, which are listed in Table 2 associated with the FY 2020 IPPS/LTCH PPS proposed rule and available via the internet on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. (Click on the link on the left side of the screen titled “FY 2020 IPPS Proposed Rule Home Page” and select “FY 2020 Proposed Rule Tables.”) This step is to be followed only if the hospital is not reclassified or redesignated under section 1886(d)(8) or section 1886(d)(10) of the Act.
Step 4. Multiply the applicable wage index determined under Steps 2 and 3 by the amount determined under Step 1 that represents the labor-related portion of the national unadjusted payment rate.
The formula below is a mathematical representation of Step 4 and adjusts the labor-related portion of the national unadjusted payment rate for the specific service by the wage index.
Xa is the labor-related portion of the national unadjusted payment rate (wage adjusted).
Xa = .60 * (national unadjusted payment rate) * applicable wage index.
Step 5. Calculate 40 percent (the nonlabor-related portion) of the national unadjusted payment rate and add that amount to the resulting product of Step 4. The result is the wage index adjusted payment rate for the relevant wage index area.
The formula below is a mathematical representation of Step 5 and calculates the remaining portion of the national payment rate, the amount not attributable to labor, and the adjusted payment for the specific service.
Y is the nonlabor-related portion of the national unadjusted payment rate.
Y = .40 * (national unadjusted payment rate).
Adjusted Medicare Payment = Y + Xa.
Step 6. If a provider is an SCH, as set forth in the regulations at § 412.92, or an EACH, which is considered to be an SCH under section 1886(d)(5)(D)(iii)(III) of the Act, and located in a rural area, as defined in § 412.64(b), or is treated as being located in a rural area under § 412.103, multiply the wage index adjusted payment rate by 1.071 to calculate the total payment.
The formula below is a mathematical representation of Step 6 and applies the rural adjustment for rural SCHs.
Adjusted Medicare Payment (SCH or EACH) = Adjusted Medicare Payment * 1.071.
We are providing examples below of the calculation of both the full and reduced national unadjusted payment rates that will apply to certain outpatient items and services performed by hospitals that meet and that fail to meet the Hospital OQR Program requirements, using the steps outlined above. For purposes of this example, we are using a provider that is located in Brooklyn, New York that is assigned to CBSA 35614. This provider bills one service that is assigned to APC 5071 (Level 1 Excision/Biopsy/Incision and Drainage). The CY 2020 full national unadjusted payment rate for APC 5071 is $609.94. The reduced national unadjusted payment rate for APC 5071 for a hospital that fails to meet the Hospital OQR Program requirements is $598.35. This reduced rate is calculated by multiplying the reporting ratio of 0.981 by the full unadjusted payment rate for APC 5071.
The FY 2020 wage index for a provider located in CBSA 35614 in New York, which includes the proposed adoption of IPPS 2020 wage index policies, is 1.2866. The labor-related portion of the full national unadjusted payment is approximately $470.84 (.60 * $609.94 * 1.2866). The labor-related portion of the reduced national unadjusted payment is approximately $461.90 (.60 * $598.35 * 1.2866). The nonlabor-related portion of the full national unadjusted payment is approximately $243.98 (.40 * $609.94). The nonlabor-related portion of the reduced national unadjusted payment is approximately $239.34 (.40 * $598.35). The sum of the labor-related and nonlabor-related portions of the full national adjusted payment is approximately $714.82 ($470.84 + $243.98). The sum of the portions of the reduced national adjusted payment is approximately $701.24 ($461.90 + $239.34).
I. Beneficiary Copayments
1. Background
Section 1833(t)(3)(B) of the Act requires the Secretary to set rules for determining the unadjusted copayment amounts to be paid by beneficiaries for covered OPD services. Section 1833(t)(8)(C)(ii) of the Act specifies that the Secretary must reduce the national unadjusted copayment amount for a covered OPD service (or group of such services) furnished in a year in a manner so that the effective copayment rate (determined on a national unadjusted basis) for that service in the year does not exceed a specified percentage. As specified in section 1833(t)(8)(C)(ii)(V) of the Act, the effective copayment rate for a covered OPD service paid under the OPPS in CY 2006, and in CYs thereafter, shall not exceed 40 percent of the APC payment rate.
Section 1833(t)(3)(B)(ii) of the Act provides that, for a covered OPD service (or group of such services) furnished in a year, the national unadjusted copayment amount cannot be less than 20 percent of the OPD fee schedule amount. However, section 1833(t)(8)(C)(i) of the Act limits the amount of beneficiary copayment that may be collected for a procedure (including items such as drugs and biologicals) performed in a year to the amount of the inpatient hospital deductible for that year.
Section 4104 of the Affordable Care Act eliminated the Medicare Part B coinsurance for preventive services furnished on and after January 1, 2011, that meet certain requirements, including flexible sigmoidoscopies and screening colonoscopies, and waived the Part B deductible for screening colonoscopies that become diagnostic during the procedure. Our discussion of the changes made by the Affordable Care Act with regard to copayments for preventive services furnished on and after January 1, 2011, may be found in section XII.B. of the CY 2011 OPPS/ASC final rule with comment period (75 FR 72013).
2. OPPS Copayment Policy
In the CY 2020 OPPS/ASC proposed rule (84 FR 39437), we proposed to determine copayment amounts for new and revised APCs using the same methodology that we implemented beginning in CY 2004. (We refer readers to the November 7, 2003 OPPS final rule with comment period (68 FR 63458).) In addition, we proposed to use the same standard rounding principles that we have historically used in instances where the application of our standard copayment methodology would result in a copayment amount that is less than 20 percent and cannot be rounded, under standard rounding principles, to 20 percent. (We refer readers to the CY 2008 OPPS/ASC final rule with comment period (72 FR 66687) in which we discuss our rationale for applying these rounding principles.) The proposed national unadjusted copayment amounts for services payable under the OPPS that would be effective January 1, 2020 are included in Addenda A and B to the proposed rule (which are available via the internet on the CMS website).
We did not receive any public comments on the proposed copayment amounts for new and revised APCs using the same methodology we implemented beginning in CY 2004 or the standard rounding principles we apply to our copayment amounts. Therefore, we are finalizing our proposed copayment policies, without modification.
As discussed in section XIV.E. of the CY 2020 OPPS/ASC proposed rule and this final rule with comment period, for CY 2020, the Medicare beneficiary's minimum unadjusted copayment and national unadjusted copayment for a service to which a reduced national unadjusted payment rate applies will equal the product of the reporting ratio and the national unadjusted copayment, or the product of the reporting ratio and the minimum unadjusted copayment, respectively, for the service.
We note that OPPS copayments may increase or decrease each year based on changes in the calculated APC payment rates, due to updated cost report and claims data, and any changes to the OPPS cost modeling process. However, as described in the CY 2004 OPPS final rule with comment period, the development of the copayment methodology generally moves beneficiary copayments closer to 20 percent of OPPS APC payments (68 FR 63458 through 63459).
In the CY 2004 OPPS final rule with comment period (68 FR 63459), we adopted a new methodology to calculate unadjusted copayment amounts in situations including reorganizing APCs, and we finalized the following rules to determine copayment amounts in CY 2004 and subsequent years.
- When an APC group consists solely of HCPCS codes that were not paid under the OPPS the prior year because they were packaged or excluded or are new codes, the unadjusted copayment amount would be 20 percent of the APC payment rate.
- If a new APC that did not exist during the prior year is created and consists of HCPCS codes previously assigned to other APCs, the copayment amount is calculated as the product of the APC payment rate and the lowest coinsurance percentage of the codes comprising the new APC.
- If no codes are added to or removed from an APC and, after recalibration of its relative payment weight, the new payment rate is equal to or greater than the prior year's rate, the copayment amount remains constant (unless the resulting coinsurance percentage is less than 20 percent).
- If no codes are added to or removed from an APC and, after recalibration of its relative payment weight, the new payment rate is less than the prior year's rate, the copayment amount is calculated as the product of the new payment rate and the prior year's coinsurance percentage.
- If HCPCS codes are added to or deleted from an APC and, after recalibrating its relative payment weight, holding its unadjusted copayment amount constant results in a decrease in the coinsurance percentage for the reconfigured APC, the copayment amount would not change (unless retaining the copayment amount would result in a coinsurance rate less than 20 percent).
- If HCPCS codes are added to an APC and, after recalibrating its relative payment weight, holding its unadjusted copayment amount constant results in an increase in the coinsurance percentage for the reconfigured APC, the copayment amount would be calculated as the product of the payment rate of the reconfigured APC and the lowest coinsurance percentage of the codes being added to the reconfigured APC.
We noted in the CY 2004 OPPS final rule with comment period that we would seek to lower the copayment percentage for a service in an APC from the prior year if the copayment percentage was greater than 20 percent. We noted that this principle was consistent with section 1833(t)(8)(C)(ii) of the Act, which accelerates the reduction in the national unadjusted coinsurance rate so that beneficiary liability will eventually equal 20 percent of the OPPS payment rate for all OPPS services to which a copayment applies, and with section 1833(t)(3)(B) of the Act, which achieves a 20-percent copayment percentage when fully phased in and gives the Secretary the authority to set rules for determining copayment amounts for new services. We further noted that the use of this methodology would, in general, reduce the beneficiary coinsurance rate and copayment amount for APCs for which the payment rate changes as the result of the reconfiguration of APCs and/or recalibration of relative payment weights (68 FR 63459).
3. Calculation of an Adjusted Copayment Amount for an APC Group
Individuals interested in calculating the national copayment liability for a Medicare beneficiary for a given service provided by a hospital that met or failed to meet its Hospital OQR Program requirements should follow the formulas presented in the following steps.
Step 1. Calculate the beneficiary payment percentage for the APC by dividing the APC's national unadjusted copayment by its payment rate. For example, using APC 5071, $121.99 is approximately 20 percent of the full national unadjusted payment rate of $609.94. For APCs with only a minimum unadjusted copayment in Addenda A and B to this final rule with comment period (which are available via the internet on the CMS website), the beneficiary payment percentage is 20 percent.
The formula below is a mathematical representation of Step 1 and calculates the national copayment as a percentage of national payment for a given service.
B is the beneficiary payment percentage.
B = National unadjusted copayment for APC/national unadjusted payment rate for APC.
Step 2. Calculate the appropriate wage-adjusted payment rate for the APC for the provider in question, as indicated in Steps 2 through 4 under section II.H. of this final rule with comment period. Calculate the rural adjustment for eligible providers, as indicated in Step 6 under section II.H. of this final rule with comment period.
Step 3. Multiply the percentage calculated in Step 1 by the payment rate calculated in Step 2. The result is the wage-adjusted copayment amount for the APC.
The formula below is a mathematical representation of Step 3 and applies the beneficiary payment percentage to the adjusted payment rate for a service calculated under section II.H. of this final rule with comment period, with and without the rural adjustment, to calculate the adjusted beneficiary copayment for a given service.
Wage-adjusted copayment amount for the APC = Adjusted Medicare Payment * B.
Wage-adjusted copayment amount for the APC (SCH or EACH) = (Adjusted Medicare Payment * 1.071) * B.
Step 4. For a hospital that failed to meet its Hospital OQR Program requirements, multiply the copayment calculated in Step 3 by the reporting ratio of 0.980.
The proposed unadjusted copayments for services payable under the OPPS that will be effective January 1, 2020, are shown in Addenda A and B to this final rule with comment period (which are available via the internet on the CMS website). We note that the national unadjusted payment rates and copayment rates shown in Addenda A and B to this final rule with comment period reflect the CY 2020 OPD fee schedule increase factor discussed in section II.B. of this final rule with comment period.
In addition, as noted earlier, section 1833(t)(8)(C)(i) of the Act limits the amount of beneficiary copayment that may be collected for a procedure performed in a year to the amount of the inpatient hospital deductible for that year.
III. OPPS Ambulatory Payment Classification (APC) Group Policies
A. OPPS Treatment of New and Revised HCPCS Codes
Payment for OPPS procedures, services, and items are generally based on medical billing codes, specifically, HCPCS codes, that are reported on HOPD claims. The HCPCS is divided into two principal subsystems, referred to as Level I and Level II of the HCPCS. Level I is comprised of CPT (Current Procedural Terminology), a numeric and alphanumeric coding system maintained by the American Medical Association (AMA), and consist of Category I, II, and III CPT codes. Level II, which is maintained by CMS, is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes. HCPCS codes are used to report surgical procedures, medical services, items, and supplies under the hospital OPPS. Specifically, CMS recognizes the following codes on OPPS claims:
- Category I CPT codes, which describe surgical procedures, diagnostic and therapeutic services, and vaccine codes;
- Category III CPT codes, which describe new and emerging technologies, services, and procedures; and
- Level II HCPCS codes (also known as alphanumeric codes), which are used primarily to identify drugs, devices, ambulance services, durable medical equipment, orthotics, prosthetics, supplies, temporary surgical procedures, and medical services not described by CPT codes.
CPT codes are established by the American Medical Association (AMA) while the Level II HCPCS codes are established by the CMS HCPCS Workgroup. These codes are updated and changed throughout the year. CPT and Level II HCPCS code changes that affect the OPPS are published through the annual rulemaking cycle and through the OPPS quarterly update Change Requests (CRs). Generally, these code changes are effective January 1, April 1, July 1, or October 1. CPT code changes are released by the AMA via their website while Level II HCPCS code changes are released to the public via the CMS HCPCS website. CMS recognizes the release of new CPT and Level II HCPCS codes and makes the codes effective (that is, the codes can be reported on Medicare claims) outside of the formal rulemaking process via OPPS quarterly update CRs. Based on our review, we assign the new codes to interim status indicators (SIs) and APCs. These interim assignments are finalized in the OPPS/ASC final rules. This quarterly process offers hospitals access to codes that more accurately describe items or services furnished and provides payment for these items or services in a timelier manner than if we waited for the annual rulemaking process. We solicit public comments on the new CPT and Level II HCPCS codes and finalize our proposals through our annual rulemaking process.
We note that, under the OPPS, the APC assignment determines the payment rate for an item, procedure, or service. Those items, procedures, or services not paid separately under the hospital OPPS are assigned to appropriate status indicators. Certain payment status indicators provide separate payment while other payment status indicators do not. In section XI. (CY 2020 OPPS Payment Status and Comment Indicators) of this final rule with comment period, we discuss the various status indicators used under the OPPS. We also provide a complete list of the status indicators and their definitions in Addendum D1 to this CY 2020 OPPS/ASC final rule with comment period.
1. HCPCS Codes That Were Effective April 1, 2019 for Which We Solicited Public Comments in the CY 2020 OPPS/ASC Proposed Rule
For the April 2019 update, there were no new CPT codes. However, eight new Level II HCPCS codes were established and made effective on April 1, 2019. These codes and their long descriptors were displayed in Table 7 of the proposed rule and are now listed in Table 8 of this final rule with comment period. Through the April 2019 OPPS quarterly update CR (Transmittal 4255, Change Request 11216, dated March 15, 2019), we recognized several new Level II HCPCS codes for separate payment under the OPPS. In the CY 2020 OPPS/ASC proposed rule (84 FR 39531-39532), we solicited public comments on the proposed APC and status indicator assignments for these Level II HCPCS codes, which were listed in Table 7 of the proposed rule.
We did not receive any public comments on the proposed OPPS APC and status indicator assignments for the new Level II HCPCS codes implemented in April 2019. Therefore, we are finalizing the proposed APC and status indicator assignments for these codes, as indicated in Table 8 below. We note that several of the HCPCS C-codes have been replaced with HCPCS J-codes, effective January 1, 2020. Their replacement codes are listed in Table 8. The final payment rates for these codes can be found in Addendum B to this final rule with comment period. In addition, the status indicator definitions can be found in Addendum D1 to this final rule with comment period. Both Addendum B and Addendum D1 are available via the internet on the CMS website.

2. HCPCS Codes That Were Effective July 1, 2019 for Which We Solicited Public Comments in the CY 2020 OPPS/ASC Proposed Rule
For the July 2019 update, 58 new codes were established and made effective July 1, 2019. The codes and long descriptors were listed in Table 8 of the proposed rule. Through the July 2019 OPPS quarterly update CR (Transmittal 4313, Change Request 11318, dated May 24, 2019), we recognized several new codes for separate payment and assigned them to appropriate interim OPPS status indicators and APCs. In the CY 2020 OPPS/ASC proposed rule, we solicited public comments on the proposed APC and status indicator assignments for the codes implemented on July 1, 2019, all of which were listed in Table 8 of the proposed rule.
We received some public comments related to CPT codes 0546T, 0548T, 0549T, 0554T, 0555T, 0556T, 0557T, and 0558T, which we address in section III.D. (OPPS APC-Specific Policies) of this final rule with comment period. With the exception of the eight codes, we did not receive any public comments on the proposed OPPS APC and status indicator assignments for the other new CPT and Level II HCPCS codes implemented in July 2019. Therefore, we are finalizing the proposed APC and status indicator assignments for the July 2019 codes, including the eight codes on which we received public comments, as indicated in Table 9 below. We note that several of the HCPCS C-codes have been replaced with HCPCS J-codes, effective January 1, 2020. Their replacement codes are listed in Table 9. The final payment rates for the codes can be found in Addendum B to this final rule with comment period. In addition, the status indicator meanings can be found in Addendum D1 to this final rule with comment period. Both Addendum B and Addendum D1 are available via the internet on the CMS website.





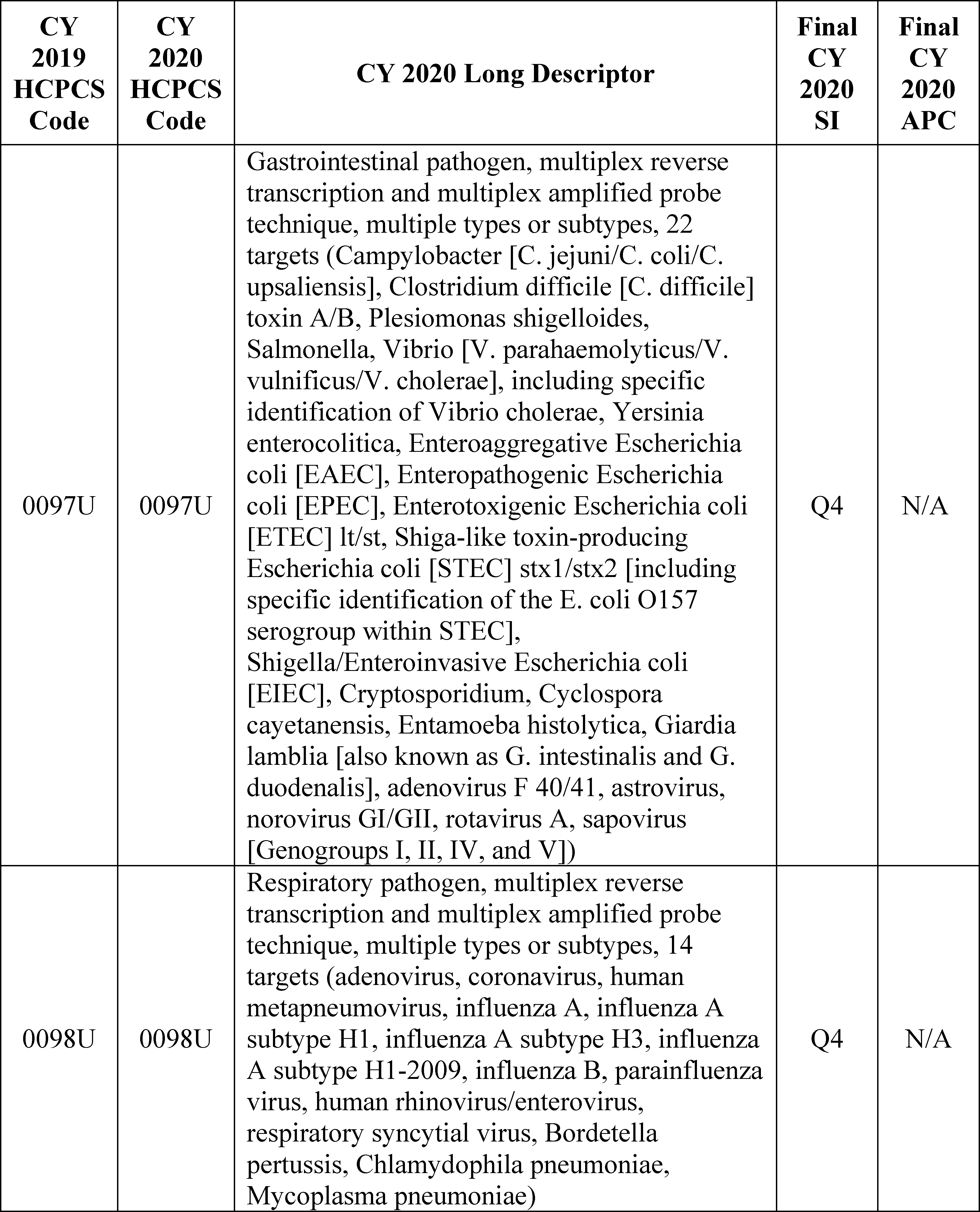


3. October 2019 HCPCS Codes for Which We Are Soliciting Public Comments in This CY 2020 OPPS/ASC Final Rule With Comment Period
As has been our practice in the past, we incorporate those new HCPCS codes that are effective October 1 in the final rule with comment period, thereby updating the OPPS for the following calendar year, as displayed in Table 9 of the proposed rule and reprinted as Table 10 of this final rule with comment period. These codes are released to the public through the October OPPS quarterly update CRs and via the CMS HCPCS website (for Level II HCPCS codes). For CY 2020, these codes are flagged with comment indicator “NI” in Addendum B to this OPPS/ASC final rule with comment period to indicate that we are assigning them an interim payment status which is subject to public comment. Specifically, the interim status indicator and APC assignments for codes flagged with comment indicator “NI” are open to public comment in this final rule with comment period, and we will respond to these public comments in the OPPS/ASC final rule with comment period for the next year's OPPS/ASC update.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39449), we proposed to continue this process for CY 2020. Specifically, for CY 2020, we proposed to include in Addendum B to the CY 2020 OPPS/ASC final rule with comment period the new HCPCS codes effective October 1, 2019, that would be incorporated in the October 2019 OPPS quarterly update CR. Also, as stated above, the October 1, 2019 codes are flagged with comment indicator “NI” in Addendum B to this CY 2020 OPPS/ASC final rule with comment period to indicate that we have assigned the codes an interim OPPS payment status for CY 2020. We are inviting public comments on the interim status indicator and APC assignments for these codes, if applicable, that will be finalized in the CY 2021 OPPS/ASC final rule with comment period.
We note that we received a comment related to HCPCS code Q4184 (Cellesta or Cellesta Duo, per square centimeter), which was assigned to comment indicator “NI” in Addendum B of the CY 2019 OPPS/ASC final rule. The comment and our response can be found in section V.B.7 (Skin Substitutes) of this CY 2020 OPPS/ASC final rule with comment period.
4. January 2020 HCPCS Codes
a. New Level II HCPCS Codes for Which We Are Soliciting Public Comments in This CY 2020 OPPS/ASC Final Rule With Comment Period
As shown in Table 10 below, and as stated in the CY 2020 OPPS/ASC proposed rule (84 FR 39449), consistent with past practice, we solicit comments on the new Level II HCPCS codes that will be effective January 1 in the OPPS/ASC final rule with comment period, thereby allowing us to finalize the status indicators and APC assignments for the codes in the next OPPS/ASC final rule with comment period. Unlike the CPT codes that are effective January 1 and are included in the OPPS/ASC proposed rules, most Level II HCPCS codes are not released until sometime around November to be effective January 1. Because these codes are not available until November, we are unable to include them in the OPPS/ASC proposed rules. Consequently, for CY 2020, we proposed to include in Addendum B to the CY 2020 OPPS/ASC final rule with comment period the new Level II HCPCS codes effective January 1, 2020, that would be incorporated in the January 2020 OPPS quarterly update CR. These codes will be released to the public through the January OPPS quarterly update CRs and via the CMS HCPCS website (for Level II HCPCS codes). For CY 2020, the Level II HCPCS codes effective January 1, 2020 codes are flagged with comment indicator “NI” in Addendum B to this CY 2020 OPPS/ASC final rule with comment period to indicate that we have assigned the codes an interim OPPS payment status for CY 2020. We are inviting public comments on the interim status indicator and APC assignments for these codes, if applicable, that will be finalized in the CY 2021 OPPS/ASC final rule with comment period.
b. CPT Codes for Which We Solicited Public Comments in the CY 2020 OPPS/ASC Proposed Rule
For CY 2020, we received the CY 2020 CPT code updates that would be effective January 1, 2020, from AMA in time for inclusion in the CY 2020 OPPS/ASC proposed rule. We note that in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66841 through 66844), we finalized a revised process of assigning APC and status indicators for new and revised Category I and III CPT codes that would be effective January 1. Specifically, for the new/revised CPT codes that we receive in a timely manner from the AMA's CPT Editorial Panel, we finalized our proposal to include the codes that would be effective January 1 in the OPPS/ASC proposed rules, along with proposed APC and status indicator assignments for them, and to finalize the APC and status indicator assignments in the OPPS/ASC final rules beginning with the CY 2016 OPPS update. For those new/revised CPT codes that were received too late for inclusion in the OPPS/ASC proposed rule, we finalized our proposal to establish and use HCPCS G-codes that mirror the predecessor CPT codes and retain the current APC and status indicator assignments for a year until we can propose APC and status indicator assignments in the following year's rulemaking cycle. We note that even if we find that we need to create HCPCS G-codes in place of certain CPT codes for the PFS proposed rule, we do not anticipate that these HCPCS G-codes will always be necessary for OPPS purposes. We will make every effort to include proposed APC and status indicator assignments for all new and revised CPT codes that the AMA makes publicly available in time for us to include them in the annual proposed rule, and to avoid the resort to HCPCS G-codes and the resulting delay in utilization of the most current CPT codes. Also, we finalized our proposal to make interim APC and status indicator assignments for CPT codes that are not available in time for the proposed rule and that describe wholly new services (such as new technologies or new surgical procedures), solicit public comments, and finalize the specific APC and status indicator assignments for those codes in the following year's final rule.
As stated above, for the CY 2020 OPPS update, we received the CY 2020 CPT codes from AMA in time for inclusion in the CY 2020 OPPS/ASC proposed rule. The new, revised, and deleted CY 2020 Category I and III CPT codes were included in Addendum B to the proposed rule (which is available via the internet on the CMS website). We noted in the proposed rule that the new and revised codes are assigned to new comment indicator “NP” to indicate that the code is new for the next calendar year or the code is an existing code with substantial revision to its code descriptor in the next calendar year as compared to current calendar year with a proposed APC assignment, and that comments will be accepted on the proposed APC and status indicator assignments.
Further, we reminded readers that the CPT code descriptors that appear in Addendum B are short descriptors and do not accurately describe the complete procedure, service, or item described by the CPT code. Therefore, we included the 5-digit placeholder codes and their long descriptors for the new and revised CY 2020 CPT codes in Addendum O to the proposed rule (which is available via the internet on the CMS website) so that the public could adequately comment on the proposed APCs and status indicator assignments. The 5-digit placeholder codes were included in Addendum O, specifically under the column labeled “CY 2020 OPPS/ASC Proposed Rule 5-Digit AMA Placeholder Code,” to the proposed rule. We noted that the final CPT code numbers will be included in this CY 2020 OPPS/ASC final rule with comment period. We also noted that not every code listed in Addendum O is subject to public comment. For the new and revised Category I and III CPT codes, we requested public comments on only those codes that are assigned to comment indicator “NP”.
In summary, in the CY 2020 OPPS/ASC proposed rule, we solicited public comments on the proposed CY 2020 status indicator and APC assignments for the new and revised Category I and III CPT codes that will be effective January 1, 2020. The CPT codes were listed in Addendum B to the proposed rule with short descriptors only. We listed them again in Addendum O to the proposed rule with long descriptors. We also proposed to finalize the status indicator and APC assignments for these codes (with their final CPT code numbers) in the CY 2020 OPPS/ASC final rule with comment period. The proposed status indicator and APC assignments for these codes were included in Addendum B to the proposed rule (which is available via the internet on the CMS website).
Commenters addressed several of the new CPT codes that were assigned to comment indicator “NP” in Addendum B to the CY 2020 OPPS/ASC proposed rule. We have responded to those public comments in sections III.D. (OPPS APC-Specific Policies), IV.B. (Device-Intensive Procedures) and XII. (Updates to the ASC Payment System) of this CY 2020OPPS/ASC final rule with comment period.
The final status indicators, APC assignments, and payment rates for the new CPT codes that are effective January 1, 2020 can be found in Addendum B to this final rule with comment period. In addition, the status indicator meanings can be found in Addendum D1 (OPPS Payment Status Indicators for CY 2020) to this final rule with comment period. Both Addendum B and D1 are available via the internet on the CMS website.
Finally, Table 10 below, which is a reprint of Table 9 from the CY 2020 OPPS/ASC proposed rule, shows the comment timeframe for new and revised HCPCS codes. The table provides information on our current process for updating codes through our OPPS quarterly update CRs, seeking public comments, and finalizing the treatment of these codes under the OPPS.

B. OPPS Changes—Variations Within APCs
1. Background
Section 1833(t)(2)(A) of the Act requires the Secretary to develop a classification system for covered hospital outpatient department services. Section 1833(t)(2)(B) of the Act provides that the Secretary may establish groups of covered OPD services within this classification system, so that services classified within each group are comparable clinically and with respect to the use of resources. In accordance with these provisions, we developed a grouping classification system, referred to as Ambulatory Payment Classifications (APCs), as set forth in regulations at 42 CFR 419.31. We use Level I (also known as CPT codes) and Level II HCPCS codes (also known as alphanumeric codes) to identify and group the services within each APC. The APCs are organized such that each group is homogeneous both clinically and in terms of resource use. Using this classification system, we have established distinct groups of similar services. We also have developed separate APC groups for certain medical devices, drugs, biologicals, therapeutic radiopharmaceuticals, and brachytherapy devices that are not packaged into the payment for the procedure.
We have packaged into the payment for each procedure or service within an APC group the costs associated with those items and services that are typically ancillary and supportive to a primary diagnostic or therapeutic modality and, in those cases, are an integral part of the primary service they support. Therefore, we do not make separate payment for these packaged items or services. In general, packaged items and services include, but are not limited to, the items and services listed in regulations at 42 CFR 419.2(b). A further discussion of packaged services is included in section II.A.3. of this final rule with comment period.
Under the OPPS, we generally pay for covered hospital outpatient services on a rate-per-service basis, where the service may be reported with one or more HCPCS codes. Payment varies according to the APC group to which the independent service or combination of services is assigned. In the CY 2020 OPPS/ASC proposed rule (84 FR 39451-39452), for CY 2020, we proposed that each APC relative payment weight represents the hospital cost of the services included in that APC, relative to the hospital cost of the services included in APC 5012 (Clinic Visits and Related Services). The APC relative payment weights are scaled to APC 5012 because it is the hospital clinic visit APC and clinic visits are among the most frequently furnished services in the hospital outpatient setting.
2. Application of the 2 Times Rule
Section 1833(t)(9)(A) of the Act requires the Secretary to review, not less often than annually, and revise the APC groups, the relative payment weights, and the wage and other adjustments described in paragraph (2) to take into account changes in medical practice, changes in technology, the addition of new services, new cost data, and other relevant information and factors. Section 1833(t)(9)(A) of the Act also requires the Secretary to consult with an expert outside advisory panel composed of an appropriate selection of representatives of providers to review (and advise the Secretary concerning) the clinical integrity of the APC groups and the relative payment weights. We note that the HOP Panel recommendations for specific services for the CY 2020 OPPS update are discussed in the relevant specific sections throughout this CY 2020 OPPS/ASC final rule with comment period.
In addition, section 1833(t)(2) of the Act provides that, subject to certain exceptions, the items and services within an APC group cannot be considered comparable with respect to the use of resources if the highest cost for an item or service in the group is more than 2 times greater than the lowest cost for an item or service within the same group (referred to as the “2 times rule”). The statute authorizes the Secretary to make exceptions to the 2 times rule in unusual cases, such as low-volume items and services (but the Secretary may not make such an exception in the case of a drug or biological that has been designated as an orphan drug under section 526 of the Federal Food, Drug, and Cosmetic Act). In determining the APCs with a 2 times rule violation, we consider only those HCPCS codes that are significant based on the number of claims. We note that, for purposes of identifying significant procedure codes for examination under the 2 times rule, we consider procedure codes that have more than 1,000 single major claims or procedure codes that both have more than 99 single major claims and contribute at least 2 percent of the single major claims used to establish the APC cost to be significant (75 FR 71832). This longstanding definition of when a procedure code is significant for purposes of the 2 times rule was selected because we believe that a subset of 1,000 or fewer claims is negligible within the set of approximately 100 million single procedure or single session claims we use for establishing costs. Similarly, a procedure code for which there are fewer than 99 single claims and that comprises less than 2 percent of the single major claims within an APC will have a negligible impact on the APC cost (75 FR 71832). In the CY 2020 OPPS/ASC proposed rule (84 FR 39451 through 39452), for CY 2020, we proposed to make exceptions to this limit on the variation of costs within each APC group in unusual cases, such as for certain low-volume items and services.
In the CY 2020 OPPS/ASC proposed rule, we identified the APCs with violations of the 2 times rule. Therefore, we proposed changes to the procedure codes assigned to these APCs in Addendum B to the proposed rule. We noted that Addendum B does not appear in the printed version of the Federal Register as part of the CY 2020 OPPS/ASC proposed rule. Rather, it is published and made available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html. To eliminate a violation of the 2 times rule and improve clinical and resource homogeneity, we proposed to reassign these procedure codes to new APCs that contain services that are similar with regard to both their clinical and resource characteristics. In many cases, the proposed procedure code reassignments and associated APC reconfigurations for CY 2020 included in the proposed rule were related to changes in costs of services that were observed in the CY 2018 claims data newly available for CY 2020 ratesetting. Addendum B to the CY 2020 OPPS/ASC proposed rule identified with a comment indicator “CH” those procedure codes for which we proposed a change to the APC assignment or status indicator, or both, that were initially assigned in the July 1, 2019 OPPS Addendum B Update (available via the internet on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Addendum-A-and-Addendum-B-Updates.html), which was the latest payment rate file for 2019 prior to issuance of the proposed rule.
3. APC Exceptions to the 2 Times Rule
Taking into account the APC changes that we proposed to make for CY 2020 in the CY 2020 OPPS/ASC proposed rule, we reviewed all of the APCs to determine which APCs would not meet the requirements of the 2 times rule. We used the following criteria to evaluate whether to propose exceptions to the 2 times rule for affected APCs:
- Resource homogeneity;
- Clinical homogeneity;
- Hospital outpatient setting utilization;
- Frequency of service (volume); and
- Opportunity for upcoding and code fragments.
Based on the CY 2018 claims data available for the CY 2020 proposed rule, we found 18 APCs with violations of the 2 times rule. We applied the criteria as described above to identify the APCs for which we proposed to make exceptions under the 2 times rule for CY 2020, and found that all of the 18 APCs we identified met the criteria for an exception to the 2 times rule based on the CY 2018 claims data available for the proposed rule. We did not include in that determination those APCs where a 2 times rule violation was not a relevant concept, such as APC 5401 (Dialysis), which only has two HCPCS codes assigned to it that have a similar geometric mean costs and do not create a 2 time rule violation. Therefore, we only identified those APCs, including those with criteria-based costs, such as device-dependent CPT/HCPCS codes, with violations of the 2 times rule.
We note that, for cases in which a recommendation by the HOP Panel appears to result in or allow a violation of the 2 times rule, we may accept the HOP Panel's recommendation because those recommendations are based on explicit consideration (that is, a review of the latest OPPS claims data and group discussion of the issue) of resource use, clinical homogeneity, site of service, and the quality of the claims data used to determine the APC payment rates.
Table 10 of the proposed rule listed the 18 APCs that we proposed to make an exception for under the 2 times rule for CY 2020 based on the criteria cited above and claims data submitted between January 1, 2018, and December 31, 2018, and processed on or before December 31, 2018. In the proposed rule, we stated that for the final rule with comment period, we intend to use claims data for dates of service between January 1, 2018, and December 31, 2018, that were processed on or before June 30, 2019, and updated CCRs, if available.
Based on the updated final rule CY 2018 claims data used for this CY 2020 final rule with comment period, we were able to remedy two APC violation out of the 18 APCs that appeared in Table 10 of the CY 2020 OPPS/ASC proposed rule. Specifically, APC 5672 (Level 2 Pathology) and APC 5733 (Level 3 Minor Procedures) no longer met the criteria for exception to the 2 times rule in this final rule with comment period. In addition, based on our analysis of the final rule claims data, we found a total of 17 APCs with violations of the 2 times rule. Of these 17 total APCs, 16 were identified in the proposed rule and one newly identified APC. Specifically, we found the following 16 APCs from the proposed rule continued to have violations of the 2 times rule for this final rule with comment period:
- APC 5112 (Level 2 Musculoskeletal Procedures);
- APC 5161 (Level 1 ENT Procedures)
- APC 5181 (Level 1 Vascular Procedures)
- APC 5311 (Level 1 Lower GI Procedures)
- APC 5521 (Level 1 Imaging without Contrast);
- APC 5522 (Level 2 Imaging without Contrast);
- APC 5523 (Level 3 Imaging without Contrast);
- APC 5524 (Level 4 Imaging without Contrast);
- APC 5571 (Level 1 Imaging with Contrast)
- APC 5612 (Level 2 Therapeutic Radiation Treatment Preparation);
- APC 5691 (Level 1 Drug Administration);
- APC 5721 (Level 1 Diagnostic Tests and Related Services);
- APC 5731 (Level 1 Minor Procedures);
- APC 5734 (Level 4 Minor Procedures);
- APC 5822 (Level 2 Health and Behavior Services); and
- APC 5823 (Level 3 Health and Behavior Services).
In addition, we found that APC 5593 (Level 3 Nuclear Medicine and Related Services) violated the 2 times rule using the final rule with comment period claims data.
Although we did not receive any comments on Table 10 of the proposed rule, we did receive comments on APC assignments for specific HCPCS codes. The comments, and our responses, can be found in section III.D. (OPPS APC-Specific Policies) of this final rule with comment period.
After considering the public comments we received on APC assignments and our analysis of the CY 2018 costs from hospital claims and cost report data available for this CY 2020 final rule with comment period, we are finalizing our proposals with some modifications. Specifically, we are finalizing our proposal to except 16 of the 18 proposed APCs from the 2 times rule for CY 2020 and also excepting one additional APC (APC 5593). As noted above, we were able to remedy two of the proposed rule 2 time violations in this final rule with comment period.
In summary, Table 11 below lists the 17 APCs that we are excepting from the 2 times rule for CY 2020 based on the criteria described earlier and a review of updated claims data for dates of service between January 1, 2018 and December 31, 2018, that were processed on or before June 30, 2019, and updated CCRs, if available. We note that, for cases in which a recommendation by the HOP Panel appears to result in or allow a violation of the 2 times rule, we generally accept the HOP Panel's recommendation because those recommendations are based on explicit consideration of resource use, clinical homogeneity, site of service, and the quality of the claims data used to determine the APC payment rates. The geometric mean costs for hospital outpatient services for these and all other APCs that were used in the development of this final rule with comment period can be found on the CMS website at: http://www.cms.gov.
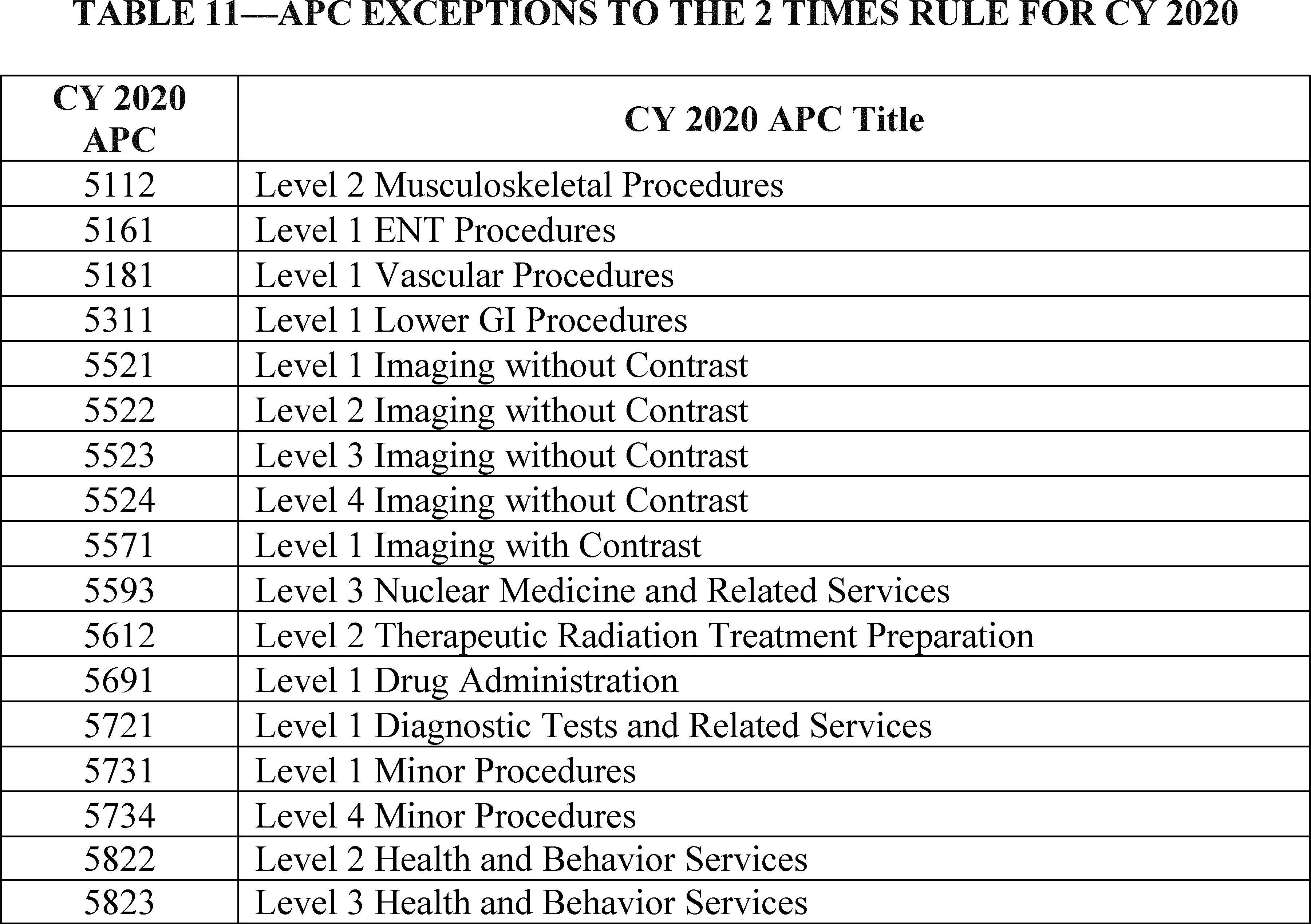
C. New Technology APCs
1. Background
In the CY 2002 OPPS final rule (66 FR 59903), we finalized changes to the time period in which a service can be eligible for payment under a New Technology APC. Beginning in CY 2002, we retain services within New Technology APC groups until we gather sufficient claims data to enable us to assign the service to an appropriate clinical APC. This policy allows us to move a service from a New Technology APC in less than 2 years if sufficient data are available. It also allows us to retain a service in a New Technology APC for more than 2 years if sufficient data upon which to base a decision for reassignment have not been collected.
In the CY 2004 OPPS final rule with comment period (68 FR 63416), we restructured the New Technology APCs to make the cost intervals more consistent across payment levels and refined the cost bands for these APCs to retain two parallel sets of New Technology APCs, one set with a status indicator of “S” (Significant Procedures, Not Discounted when Multiple. Paid under OPPS; separate APC payment) and the other set with a status indicator of “T” (Significant Procedure, Multiple Reduction Applies. Paid under OPPS; separate APC payment). These current New Technology APC configurations allow us to price new technology services more appropriately and consistently.
For CY 2019, there were 52 New Technology APC levels, ranging from the lowest cost band assigned to APC 1491 (New Technology-Level 1A ($0-$10)) through the highest cost band assigned to APC 1908 (New Technology-Level 52 ($145,001-$160,000)). We note that the cost bands for the New Technology APCs, specifically, APCs 1491 through 1599 and 1901 through 1908, vary with increments ranging from $10 to $14,999. These cost bands identify the APCs to which new technology procedures and services with estimated service costs that fall within those cost bands are assigned under the OPPS. Payment for each APC is made at the mid-point of the APC's assigned cost band. For example, payment for New Technology APC 1507 (New Technology-Level 7 ($501-$600)) is made at $550.50.
Under the OPPS, one of our goals is to make payments that are appropriate for the services that are necessary for the treatment of Medicare beneficiaries. The OPPS, like other Medicare payment systems, is budget neutral and increases are limited to the annual hospital inpatient market basket increase adjusted for multifactor productivity. We believe that our payment rates generally reflect the costs that are associated with providing care to Medicare beneficiaries. Furthermore, we believe that our payment rates are adequate to ensure access to services (80 FR 70374).
For many emerging technologies, there is a transitional period during which utilization may be low, often because providers are first learning about the technologies and their clinical utility. Quite often, parties request that Medicare make higher payment amounts under the New Technology APCs for new procedures in that transitional phase. These requests, and their accompanying estimates for expected total patient utilization, often reflect very low rates of patient use of expensive equipment, resulting in high per-use costs for which requesters believe Medicare should make full payment. Medicare does not, and we believe should not, assume responsibility for more than its share of the costs of procedures based on projected utilization for Medicare beneficiaries and does not set its payment rates based on initial projections of low utilization for services that require expensive capital equipment. For the OPPS, we rely on hospitals to make informed business decisions regarding the acquisition of high-cost capital equipment, taking into consideration their knowledge about their entire patient base (Medicare beneficiaries included) and an understanding of Medicare's and other payers' payment policies. (We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68314) for further discussion regarding this payment policy.)
We note that, in a budget neutral system, payments may not fully cover hospitals' costs in a particular circumstance, including those for the purchase and maintenance of capital equipment. We rely on hospitals to make their decisions regarding the acquisition of high-cost equipment with the understanding that the Medicare program must be careful to establish its initial payment rates, including those made through New Technology APCs, for new services that lack hospital claims data based on realistic utilization projections for all such services delivered in cost-efficient hospital outpatient settings. As the OPPS acquires claims data regarding hospital costs associated with new procedures, we regularly examine the claims data and any available new information regarding the clinical aspects of new procedures to confirm that our OPPS payments remain appropriate for procedures as they transition into mainstream medical practice (77 FR 68314). For CY 2020, we included the proposed payment rates for New Technology APCs 1491 to 1599 and 1901 through 1908 in Addendum A to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website). The final payment rates for these New Technology APCs are included in Addendum A to the CY 2020 OPPS/ASC final rule with comment period (which is available via the internet on the CMS website).
2. Establishing Payment Rates for Low-Volume New Technology Procedures
Procedures that are assigned to New Technology APCs are typically new procedures that do not have sufficient claims history to establish an accurate payment for the procedures. One of the objectives of establishing New Technology APCs is to generate sufficient claims data for a new procedure so that it can be assigned to an appropriate clinical APC. Some procedures that are assigned to New Technology APCs have very low annual volume, which we consider to be fewer than 100 claims. We consider procedures with fewer than 100 claims annually as low-volume procedures because there is a higher probability that the payment data for a procedure may not have a normal statistical distribution, which could affect the quality of our standard cost methodology that is used to assign services to an APC. In addition, services with fewer than 100 claims per year are not generally considered to be a significant contributor to the APC ratesetting calculations and, therefore, are not included in the assessment of the 2 times rule. As we explained in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58890), we were concerned that the methodology we use to estimate the cost of a procedure under the OPPS by calculating the geometric mean for all separately paid claims for a HCPCS procedure code from the most recent available year of claims data may not generate an accurate estimate of the actual cost of the procedure for these low-volume procedures.
In accordance with section 1833(t)(2)(B) of the Act, services classified within each APC must be comparable clinically and with respect to the use of resources. As described earlier, assigning a procedure to a new technology APC allows us to gather claims data to price the procedure and assign it to the APC with services that use similar resources and are clinically comparable. However, where utilization of services assigned to a New Technology APC is low, it can lead to wide variation in payment rates from year to year, resulting in even lower utilization and potential barriers to access to new technologies, which ultimately limits our ability to assign the service to the appropriate clinical APC. To mitigate these issues, we determined in the CY 2019 OPPS/ASC final rule with comment period that it was appropriate to utilize our equitable adjustment authority at section 1833(t)(2)(E) of the Act to adjust how we determined the costs for low-volume services assigned to New Technology APCs (83 FR 58892 through 58893). We have utilized our equitable adjustment authority at section 1833(t)(2)(E) of the Act, which states that the Secretary shall establish, in a budget neutral manner, other adjustments as determined to be necessary to ensure equitable payments, to estimate an appropriate payment amount for low-volume new technology procedures in the past (82 FR 59281). Although we have used this adjustment authority on a case-by-case basis in the past, we stated in the CY 2019 OPPS/ASC final rule with comment period that we believe it is appropriate to adopt an adjustment for low-volume services assigned to New Technology APCs in order to mitigate the wide payment fluctuations that have occurred for new technology services with fewer than 100 claims and to provide more predictable payment for these services.
For purposes of this adjustment, we stated that we believe that it is appropriate to use up to 4 years of claims data in calculating the applicable payment rate for the prospective year, rather than using solely the most recent available year of claims data, when a service assigned to a New Technology APC has a low annual volume of claims, which, for purposes of this adjustment, we define as fewer than 100 claims annually. We adopted a policy to consider procedures with fewer than 100 claims annually as low-volume procedures because there is a higher probability that the payment data for a procedure may not have a normal statistical distribution, which could affect the quality of our standard cost methodology that is used to assign services to an APC. We explained that we were concerned that the methodology we use to estimate the cost of a procedure under the OPPS by calculating the geometric mean for all separately paid claims for a HCPCS procedure code from the most recent available year of claims data may not generate an accurate estimate of the actual cost of the low-volume procedure. Using multiple years of claims data will potentially allow for more than 100 claims to be used to set the payment rate, which would, in turn, create a more statistically reliable payment rate.
In addition, to better approximate the cost of a low-volume service within a New Technology APC, we stated that we believe using the median or arithmetic mean rather than the geometric mean (which “trims” the costs of certain claims out) could be more appropriate in some circumstances, given the extremely low volume of claims. Low claim volumes increase the impact of “outlier” claims; that is, claims with either a very low or very high payment rate as compared to the average claim, which would have a substantial impact on any statistical methodology used to estimate the most appropriate payment rate for a service. We also explained that we believe having the flexibility to utilize an alternative statistical methodology to calculate the payment rate in the case of low-volume new technology services would help to create a more stable payment rate. Therefore, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58893), we established that, in each of our annual rulemakings, we will seek public comments on which statistical methodology should be used for each low-volume service assigned to a New Technology APC. In the preamble of each annual rulemaking, we stated that we would present the result of each statistical methodology and solicit public comment on which methodology should be used to establish the payment rate for a low-volume new technology service. In addition, we will use our assessment of the resources used to perform a service and guidance from the developer or manufacturer of the service, as well as other stakeholders, to determine the most appropriate payment rate. Once we identify the most appropriate payment rate for a service, we will assign the service to the New Technology APC with the cost band that includes its payment rate.
Accordingly for CY 2020, we proposed to continue the policy we adopted in CY 2019 under which we will utilize our equitable adjustment authority under section 1833(t)(2)(E) of the Act to calculate the geometric mean, arithmetic mean, and median using multiple years of claims data to select the appropriate payment rate for purposes of assigning services with fewer than 100 claims per year to a New Technology APC. Additional details on our policy is available in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58892 through 58893).
Comment: One commenter expressed support for the continuation of our policy regarding payment rates for low-volume new technology procedures.
Response: We appreciate the commenter's support.
After considering the public comments we received, we are finalizing this proposal without modification.
3. Procedures Assigned to New Technology APC Groups for CY 2020
As we explained in the CY 2002 OPPS final rule with comment period (66 FR 59902), we generally retain a procedure in the New Technology APC to which it is initially assigned until we have obtained sufficient claims data to justify reassignment of the procedure to a clinically appropriate APC.
In addition, in cases where we find that our initial New Technology APC assignment was based on inaccurate or inadequate information (although it was the best information available at the time), where we obtain new information that was not available at the time of our initial New Technology APC assignment, or where the New Technology APCs are restructured, we may, based on more recent resource utilization information (including claims data) or the availability of refined New Technology APC cost bands, reassign the procedure or service to a different New Technology APC that more appropriately reflects its cost (66 FR 59903).
Consistent with our current policy, for CY 2020, in the CY 2020 OPPS/ASC proposed rule (84 FR 39454), we proposed to retain services within New Technology APC groups until we obtain sufficient claims data to justify reassignment of the service to a clinically appropriate APC. The flexibility associated with this policy allows us to reassign a service from a New Technology APC in less than 2 years if sufficient claims data are available. It also allows us to retain a service in a New Technology APC for more than 2 years if sufficient claims data upon which to base a decision for reassignment have not been obtained (66 FR 59902).
a. Magnetic Resonance-Guided Focused Ultrasound Surgery (MRgFUS) (APCs 1575, 5114, and 5414)
Currently, there are four CPT/HCPCS codes that describe magnetic resonance image-guided, high-intensity focused ultrasound (MRgFUS) procedures, three of which we proposed to continue to assign to standard APCs, and one that we proposed to continue to assign to a New Technology APC for CY 2020. These codes include CPT codes 0071T, 0072T, and 0398T, and HCPCS code C9734. CPT codes 0071T and 0072T describe procedures for the treatment of uterine fibroids, CPT code 0398T describes procedures for the treatment of essential tremor, and HCPCS code C9734 describes procedures for pain palliation for metastatic bone cancer.
As shown in Table 11 of the CY 2020 OPPS/ASC proposed rule, and as listed in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to continue to assign the procedures described by CPT codes 0071T and 0072T to APC 5414 (Level 4 Gynecologic Procedures) for CY 2020. We also proposed to continue to assign the APC to status indicator “J1” (Hospital Part B services paid through a comprehensive APC). In addition, we proposed to continue to assign the services described by HCPCS code C9734 (Focused ultrasound ablation/therapeutic intervention, other than uterine leiomyomata, with magnetic resonance (mr) guidance) to APC 5115 (Level 5 Musculoskeletal Procedures) for CY 2020. We also proposed to continue to assign HCPCS code C9734 to status indicator “J1”. We refer readers to Addendum B to the proposed rule for the proposed payment rates for CPT codes 0071T and 0072T and HCPCS code C9734 under the OPPS. Addendum B is available via the internet on the CMS website.
For the procedure described by CPT code 0398T, we have identified 37 paid claims from CY 2016 through CY 2018 (1 claim in CY 2016, 11 claims in CY 2017, and 25 claims in CY 2018). We note that the procedure described by CPT code 0398T was first assigned to a New Technology APC in CY 2016. Accordingly, there are 3 years of claims data available for the OPPS ratesetting purposes. The payment amounts for the claims vary widely, with a cost of approximately $29,254 for the sole CY 2016 claim, a geometric mean cost of approximately $4,647 for the 11 claims from CY 2017, and a geometric mean cost of approximately $11,716 for the 25 claims from CY 2018. We are concerned about the large fluctuation in the cost of the procedure described by CPT code 0398T from year to year and the relatively small number of claims available to establish a payment rate for the service. In accordance with section 1833(t)(2)(B) of the Act, we must establish that services classified within each APC are comparable clinically and with respect to the use of resources.
Therefore, as discussed in section III.C.2. of the proposed rule, we proposed to apply the policy we adopted in CY 2019, under which we will utilize our equitable adjustment authority under section 1833(t)(2)(E) of the Act to calculate the geometric mean, arithmetic mean, and median costs using multiple years of claims data to select the appropriate payment rate for purposes of assigning CPT code 0398T to a New Technology APC. We believe using this approach to assign CPT code 0398T to a New Technology APC is more likely to yield a payment rate that will be representative of the cost of the procedure described by CPT code 0398T, despite the fluctuating geometric mean costs for the procedure available in the claims data used for the proposed rule. We continue to believe that the situation for the procedure described by CPT code 0398T is unique, given the limited number of claims for the procedure and the high variability for the cost of the claims, which makes it challenging to determine a reliable payment rate.
Our analysis found that the estimated geometric mean cost of the 37 claims over the 3 year period for which there are claims was approximately $8,829, the estimated arithmetic mean cost of the claims was approximately $10,021, and the median cost of the claims was approximately $11,985. While the results of using different methodologies range from approximately $8,800 to nearly $12,000, two of the estimates fall within the cost bands of New Technology APC 1575 (New Technology—Level 38 ($10,001-$15,000)), with a proposed payment rate of $12,500.50. Consistent with our low volume policy for procedures assigned to a new technology APC, we presented the result of each statistical methodology in the proposed rule, and we sought public comments on which methodology should be used to establish payment for the procedures described by CPT code 0398T. We noted that we believe that the median cost estimate was the most appropriate representative cost of the procedure described by CPT code 0398T because it was consistent with the payment rates established for the procedure from CY 2017 to CY 2019 and did not involve any trimming of claims. Calculating the payment rate using either the geometric mean cost or the arithmetic mean cost would involve trimming the one paid claim from CY 2016, because the paid amount for the claim of $29,254 is substantially larger than the amount for any other paid claim reported for the procedure described by CPT code 0398T. The median cost estimate for CPT code 0398T also falls within the same New Technology APC cost band that was used to set the payment rate for CY 2019, which is $12,500.50 for this procedure. Therefore, for purposes of determining the proposed CY 2020 payment rate, we proposed to estimate the cost for the procedure described by CPT code 0398T by calculating the median cost of the 37 paid claims for the procedures in CY 2016 through CY 2018, and assigned the procedure described by CPT code 0398T to the New Technology APC that includes the estimated cost. Accordingly, we proposed to maintain the procedure described by CPT code 0398T in APC 1575 (New Technology—Level 38 ($10,001-$15,000)), with a proposed payment rate of $12,500.50 for CY 2020. We refer readers to Addendum B to the proposed rule for the proposed payment rates for all codes reportable under the OPPS. Addendum B is available via the internet on the CMS website.


Comment: Multiple commenters, including the developer of MRgFUS, stated that the proposed payment rate for CPT code 0398T was too low because they believed the claims data for CPT code 0398T continue to underestimate the resources used to perform the procedure even when using the low-volume payment policy to establish the payment rate for the procedure. The developer also used the example of the service described by HCPCS code C9734 (Focused ultrasound ablation/therapeutic intervention, other than uterine leiomyomata, with magnetic resonance (mr) guidance), where the payment rate for the service had doubled from $5,222 in CY 2017 to $11,675 in the CY 2020 proposed rule, to argue that a similar increase could occur for CPT code 0398T. Commenters suggested several ideas for what they believed would be a more appropriate rate. Commenters believed the claims cost data reported for CPT code 0398T does not fully reflect the resource costs for the time the procedure takes, the cost of single-use supplies for the procedure, and hours of use of a provider's MRI machine. To reflect these costs, several commenters supported restoring the payment rate from CY 2018 of $17,500.50. Other commenters simply requested a higher rate than what was proposed such as a payment rate of either $22,000 or $25,000.
Response: We appreciate the commenters' concerns, but the claims data we currently have for CPT code 0398T do not support a higher payment rate even when using the low-volume payment policy. Also, while the payment rate for HCPCS code C9734 (Focused ultrasound ablation/therapeutic intervention, other than uterine leiomyomata, with magnetic resonance (mr) guidance) doubled from CY 2017 to CY 2020, the payment rate increase for HCPCS code C9734 is not predictive of the changes in cost that may occur with CPT code 0398T (Magnetic resonance image guided high intensity focused ultrasound (mrgfus), stereotactic ablation lesion, intracranial for movement disorder including stereotactic navigation and frame placement when performed). Rather, the payment rate for each service, including that described by HCPCS code C9734, is generally based on the costs associated with furnishing the service, which, in turn, drives the APC assignment. The geometric mean for C9734, which represents the cost of the individual procedure, increased from $8,655 in CY 2017 to $9,294 in CY 2020, and was reassigned to a higher level APC based clinical and resource similarity to other services.
Under the low-volume payment policy, we utilized our equitable adjustment authority under section 1833(t)(2)(E) of the Act to calculate the geometric mean, arithmetic mean, and median costs using multiple years of claims data to select the appropriate payment rate for purposes of assigning CPT code 0398T to a New Technology APC. We identified 43 claims reporting the procedure described by CPT code 0398T for the 3-year period of CY 2016 through CY 2018. We found the geometric mean cost for the procedure described by CPT code 0398T is approximately $8,485, the arithmetic mean cost is approximately $9,672, and the median cost is approximately $11,182. Based on our methodology, we will use the median cost of CPT code 0398T to set the payment rate for the procedure because the median cost is the highest rate of the three statistical methods and may reflect some of the higher resource costs, as described by commenters, for the procedure. The median cost for CPT code 0398T falls within the same New Technology APC 1575 (New Technology—Level 38 ($10,001-$15,000)) with a proposed payment rate of $12,500.50 that was proposed as the APC assignment for CPT code 0398T in the proposed rule.
Comment: Two commenters supported the assignment of CPT code 0398T to New Technology APC 1575 (New Technology—Level 38 ($10,001-$15,000)) with a proposed payment rate of $12,500.50. One of the commenters supported the proposed new technology APC assignment because it is reflective of the median cost of the service and would ensure that what the commenter believed would be a severe underpayment calculated from the geometric mean would not be used to establish the payment rate for CPT code 0398T, which the commenter believed could discourage providers from performing the service.
Response: We appreciate the support of the commenters.
Comment: One commenter, the developer, supported the assignment of HCPCS code C9734 to APC 5115 (Level 5 Musculoskeletal Procedures) for CY 2020.
Response: We appreciate the support of the commenter.
After consideration of the public comments we received, we are finalizing our proposal for the APC assignment of CPT code 0398T. Specifically, we are continuing to assign this code to New Technology APC 1575 (New Technology—Level 38 ($10,001-$15,000)), with a payment rate of $12,500.50, for CY 2020 through use of our low-volume payment policy for new technology procedures. In addition, we are finalizing our proposal, without modification, to assign HCPCS code C9734 to APC 5115. We also are finalizing our proposal to continue to assign CPT codes 0071T and 0072T to APC 5414, without modification. Table 11 above lists the final CY 2018 status indicator and APC assignments for MRgFUS procedures. We refer readers to Addendum B of this final rule with comment period for the final payment rates for all codes reportable under the OPPS. Addendum B is available via the internet on the CMS website.
b. Retinal Prosthesis Implant Procedure
CPT code 0100T (Placement of a subconjunctival retinal prosthesis receiver and pulse generator, and implantation of intra-ocular retinal electrode array, with vitrectomy) describes the implantation of a retinal prosthesis, specifically, a procedure involving the use of the Argus® II Retinal Prosthesis System. This first retinal prosthesis was approved by the Food and Drug Administration (FDA) in 2013 for adult patients diagnosed with severe to profound retinitis pigmentosa. Pass-through payment status was granted for the Argus® II device under HCPCS code C1841 (Retinal prosthesis, includes all internal and external components) beginning October 1, 2013, and this status expired on December 31, 2015. We note that after pass-through payment status expires for a medical device, the payment for the device is packaged into the payment for the associated surgical procedure. Consequently, for CY 2016, the device described by HCPCS code C1841 was assigned to OPPS status indicator “N” to indicate that payment for the device is packaged and included in the payment rate for the surgical procedure described by CPT code 0100T. For CY 2016, the procedure described by CPT code 0100T was assigned to New Technology APC 1599, with a payment rate of $95,000, which was the highest paying New Technology APC for that year. This payment included both the surgical procedure (CPT code 0100T) and the use of the Argus® II device (HCPCS code C1841). However, stakeholders (including the device manufacturer and hospitals) believed that the CY 2016 payment rate for the procedure involving the Argus® II System was insufficient to cover the hospital cost of performing the procedure, which includes the cost of the retinal prosthesis at the retail price of approximately $145,000.
For CY 2017, analysis of the CY 2015 OPPS claims data used for the CY 2017 OPPS/ASC final rule with comment period showed 9 single claims (out of 13 total claims) for the procedure described by CPT code 0100T, with a geometric mean cost of approximately $142,003 based on claims submitted between January 1, 2015, through December 31, 2015, and processed through June 30, 2016. Based on the CY 2015 OPPS claims data available for the final rule with comment period and our understanding of the Argus® II procedure, we reassigned the procedure described by CPT code 0100T from New Technology APC 1599 to New Technology APC 1906, with a final payment rate of $150,000.50 for CY 2017. We noted that this payment rate included the cost of both the surgical procedure (CPT code 0100T) and the retinal prosthesis device (HCPCS code C1841).
For CY 2018, the reported cost of the Argus® II procedure based on CY 2016 hospital outpatient claims data for 6 claims used for the CY 2018 OPPS/ASC final rule with comment period was approximately $94,455, which was more than $55,000 less than the payment rate for the procedure in CY 2017, but closer to the CY 2016 payment rate for the procedure. We noted that the costs of the Argus® II procedure are extraordinarily high compared to many other procedures paid under the OPPS. In addition, the number of claims submitted has been very low and has not exceeded 10 claims within a single year. We believed that it is important to mitigate significant payment differences, especially shifts of several tens of thousands of dollars, while also basing payment rates on available cost information and claims data. In CY 2016, the payment rate for the Argus® II procedure was $95,000.50. The payment rate increased to $150,000.50 in CY 2017. For CY 2018, if we had established the payment rate based on updated final rule claims data, the payment rate would have decreased to $95,000.50 for CY 2018, a decrease of $55,000 relative to CY 2017. We were concerned that these large fluctuations in payment could potentially create an access to care issue for the Argus® II procedure, and we wanted to establish a payment rate to mitigate the potential sharp decline in payment from CY 2017 to CY 2018.
In accordance with section 1833(t)(2)(B) of the Act, we must establish that services classified within each APC are comparable clinically and with respect to the use of resources. Therefore, for CY 2018, we used our equitable adjustment authority under section 1833(t)(2)(E) of the Act, which states that the Secretary shall establish, in a budget neutral manner, other adjustments as determined to be necessary to ensure equitable payments, to maintain the payment rate for this procedure, despite the lower geometric mean costs available in the claims data used for the final rule with comment period. For CY 2018, we reassigned the Argus® II procedure to APC 1904 (New Technology—Level 50 ($115,001-$130,000)), which established a payment rate for the Argus® II procedure of $122,500.50, which was the arithmetic mean of the payment rates for the procedure for CY 2016 and CY 2017.
For CY 2019, the reported cost of the Argus® II procedure based on the geometric mean cost of 12 claims from the CY 2017 hospital outpatient claims data was approximately $171,865, which was approximately $49,364 more than the payment rate for the procedure for CY 2018. In the CY 2019 OPPS/ASC final rule with comment period, we continued to note that the costs of the Argus® II procedure are extraordinarily high compared to many other procedures paid under the OPPS (83 FR 58897 through 58898). In addition, the number of claims submitted continued to be very low for the Argus® II procedure. We stated that we continued to believe that it is important to mitigate significant payment fluctuations for a procedure, especially shifts of several tens of thousands of dollars, while also basing payment rates on available cost information and claims data because we are concerned that large decreases in the payment rate could potentially create an access to care issue for the Argus® II procedure. In addition, we indicated that we wanted to establish a payment rate to mitigate the potential sharp increase in payment from CY 2018 to CY 2019, and potentially ensure a more stable payment rate in future years.
As discussed in section III.C.2. of the CY 2019 OPPS/ASC final rule with comment period (83 FR 58892 through 58893), we used our equitable adjustment authority under section 1833(t)(2)(E) of the Act, which states that the Secretary shall establish, in a budget neutral manner, other adjustments as determined to be necessary to ensure equitable payments, to establish a payment rate that is more representative of the likely cost of the service. We stated that we believed the likely cost of the Argus® II procedure is higher than the geometric mean cost calculated from the claims data used for the CY 2018 OPPS/ASC final rule with comment period but lower than the geometric mean cost calculated from the claims data used for the CY 2019 OPPS/ASC final rule with comment period.
For CY 2019, we analyzed claims data for the Argus® II procedure using 3 years of available data from CY 2015 through CY 2017. These data included claims from the last year that the Argus® II received transitional device pass-through payments (CY 2015) and the first 2 years since device pass-through payment status for the Argus® II expired. We found that the geometric mean cost for the procedure was approximately $145,808, the arithmetic mean cost was approximately $151,367, and the median cost was approximately $151,266. As we do each year, we reviewed claims data regarding hospital costs associated with new procedures. We regularly examine the claims data and any available new information regarding the clinical aspects of new procedures to confirm that OPPS payments remain appropriate for procedures like the Argus® II procedure as they transition into mainstream medical practice (77 FR 68314). We noted that the proposed payment rate included both the surgical procedure (CPT code 0100T) and the use of the Argus® II device (HCPCS code C1841). For CY 2019, the estimated costs using all three potential statistical methods for determining APC assignment under the New Technology low-volume payment policy fell within the cost band of New Technology APC 1908, which is between $145,001 and $160,000. Therefore, we reassigned the Argus® II procedure (CPT code 0100T) to APC 1908 (New Technology—Level 52 ($145,001-$160,000)), with a payment rate of $152,500.50 for CY 2019.
For CY 2020, the number of reported claims for the Argus® II procedure continues to be very low with a substantial fluctuation in cost from year to year. The high annual variability of the cost of the Argus® II procedure continues to make it difficult to establish a consistent and stable payment rate for the procedure. As previously mentioned, in accordance with section 1833(t)(2)(B) of the Act, we are required to establish that services classified within each APC are comparable clinically and with respect to the use of resources. Therefore, for CY 2020, we proposed to apply the policy we adopted in CY 2019, under which we utilize our equitable adjustment authority under section 1833(t)(2)(E) of the Act to calculate the geometric mean, arithmetic mean, and median costs using multiple years of claims data to select the appropriate payment rate for purposes of assigning the Argus® II procedure (CPT code 0100T) to a New Technology APC.
We identified 35 claims reporting the procedure described by CPT code 0100T for the 4-year period of CY 2015 through CY 2018. We found the geometric mean cost for the procedure described by CPT code 0100T to be approximately $146,059, the arithmetic mean cost to be approximately $152,123, and the median cost to be approximately $151,267. All of the resulting estimates from using the three statistical methodologies fall within the same New Technology APC cost band ($145,001-$160,000), where the Argus® II procedure is assigned for CY 2019. Consistent with our policy stated in section III.C.2. of the proposed rule, we presented the result of each statistical methodology in the proposed rule, and we sought public comments on which method should be used to assign procedures described by CPT code 0100T to a New Technology APC. All three potential statistical methodologies used to estimate the cost of the Argus® II procedure fell within the cost band for New Technology APC 1908, with the estimated cost being between $145,001 and $160,000. Accordingly, we proposed to maintain the assignment of the procedure described by CPT code 0100T in APC 1908 (New Technology—Level 52 ($145,001-$160,000)), with a proposed payment rate of $152,500.50 for CY 2020. We note that the proposed payment rate includes both the surgical procedure (CPT code 0100T) and the use of the Argus® II device (HCPCS code C1841). We refer readers to Addendum B to the proposed rule for the proposed payment rates for all codes reportable under the OPPS. Addendum B is available via the internet on the CMS website.
Comment: Two commenters, including the manufacturer, supported the assignment of 0100T to APC 1908 (New Technology—Level 52 ($145,001-$160,000)), with a proposed payment rate of $152,500.50 for CY 2020.
Response: We appreciate the support of the commenters. Consistent with our policy for low-volume services assigned to a New Technology APC, for this final rule, we calculated the geometric mean, arithmetic mean, and median costs using multiple years of claims data to select the appropriate payment rate for purposes of assigning the Argus® II procedure (CPT code 0100T) to a New Technology APC. We identified 41 claims reporting the procedure described by CPT code 0100T for the 4-year period of CY 2015 through CY 2018. We found the geometric mean cost for the procedure described by CPT code 0100T to be approximately $146,042, the arithmetic mean cost to be approximately $151,453, and the median cost to be approximately $151,426. All of the resulting estimates from using the three statistical methodologies fall within the same New Technology APC cost band ($145,001-$160,000), that was proposed as the APC assignment for CPT code 0100T in the proposed rule. Therefore, we are finalizing our proposal to maintain the assignment of the procedure described by CPT code 0100T in APC 1908 (New Technology—Level 52 ($145,001-$160,000)), with a payment rate of $152,500.50 for CY 2020. We refer readers to Addendum B to the proposed rule for the proposed payment rates for all codes reportable under the OPPS. Addendum B is available via the internet on the CMS website.
As we discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58898), the claims data from CY 2017 showed another payment issue with regard to the Argus® II procedure. We found that payment for the Argus® II procedure was sometimes bundled into the payment for another procedure. Therefore in CY 2019, we implemented a policy to exclude payment for all procedures assigned to New Technology APCs from being bundled into the payment for procedures assigned to a C-APC. For CY 2020, we proposed to continue this policy as described in section II.A.2.b.(3) of the proposed rule. Our proposal would continue to exclude payment for any procedure that is assigned to a New Technology APC from being packaged when included on a claim with a service assigned to status indicator “J1”. While we did not propose to exclude payment for a procedure assigned to a New Technology APC from being packaged when included on a claim with a service assigned to status indicator “J2”, we sought public comments on this issue.
Comment: Several commenters, including device manufacturers, device manufacturer associations and physicians were opposed to our proposal to package payment for procedures assigned to a New Technology APC into the payment for comprehensive observation services assigned status indicator “J2”. The commenters stated that there were instances where beneficiaries receiving observation services may require the types of procedures that are assigned to New Technology APCs. Several commenters specifically mentioned HeartFlow, and stated that it could be performed appropriately for a patient receiving observation services. The commenters also stated that providing separate payment for this new technology procedure will allow CMS to collect sufficient claims data to enable assignment of the procedure to an appropriate clinical APC.
Response: We appreciate the stakeholders' comments regarding this proposal and agree that, although rare, there are situations in which it is clinically appropriate to provide a new technology service when providing comprehensive observation services. As discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58847), the purpose of the new technology APC policy is to ensure that there are sufficient claims data for new services in order to assign these procedures to a clinical APC and therefore, we excluded procedures assigned to New Technology APCs from packaging under the C-APC policy. In the CY 2019 final rule, we specifically stated that the exclusion policy included circumstances when New Technology procedures were billed with comprehensive services assigned to status indicator “J1”, however we believe this rationale is also applicable to comprehensive observations services that are assigned status indicator “J2”.
Accordingly, for CY 2020 and subsequent years, we are modifying our policy for excluding procedures assigned to New Technology APCs from the C-APC policy. That is, we are finalizing our proposal to exclude payment for any procedure that is assigned to a New Technology APC from being packaged when included on a claim with a “J1” service assigned to a C-APC. For CY 2020 and subsequent years, we are also finalizing a policy to exclude payment for any procedures that are assigned to a New Technology APC from being packaged into the payment for comprehensive observation services assigned to status indicator “J2” when they are included on a claim with “J2” procedures. This policy is also described in section II.A.2.b.(3) of this final rule.
c. Bronchoscopy With Transbronchial Ablation of Lesion(s) by Microwave Energy
Effective January 1, 2019, CMS established HCPCS code C9751 (Bronchoscopy, rigid or flexible, transbronchial ablation of lesion(s) by microwave energy, including fluoroscopic guidance, when performed, with computed tomography acquisition(s) and 3-D rendering, computer-assisted, image-guided navigation, and endobronchial ultrasound (EBUS) guided transtracheal and/or transbronchial sampling (eg, aspiration[s]/biopsy[ies]) and all mediastinal and/or hilar lymph node stations or structures and therapeutic intervention(s)). This microwave ablation procedure utilizes a flexible catheter to access the lung tumor via a working channel and may be used as an alternative procedure to a percutaneous microwave approach. Based on our review of the New Technology APC application for this service and the service's clinical similarity to existing services paid under the OPPS, we estimated the likely cost of the procedure would be between $8,001 and $8,500. We have not received any claims data for this service. Therefore, we proposed to continue to assign the procedure described by HCPCS code C9751 to New Technology APC 1571 (New Technology—Level 34 ($8,001-$8,500)), with a proposed payment rate of $8,250.50 for CY 2020. Details regarding HCPCS code C9751 were shown in Table 12 of the CY 2020 OPPS/ASC proposed Rule, which is reprinted below in Table 13.

Comment: The developer of the procedure noted that there will be clinical trials for HCPCS code C9751 in CY 2020 and it is anticipated the procedure also will have a limited market release in CY 2020. Therefore, the developer is expecting claims to be reported billed with HCPCS code C9751 for CY 2020.
Response: We appreciate the update on the expected utilization for HCPCS code C9751 for CY 2020.
Comment: One commenter supported our proposal to assign HCPCS code C9751 to New Technology APC 1571 (New Technology—Level 34 ($8,001-$8,500)), with a proposed payment rate of $8,250.50 for CY 2020.
Response: We appreciate the support of the commenter.
After considering the public comments, we are finalizing our proposal to assign HCPCS code C9751 to New Technology APC 1571 (New Technology—Level 34 ($8,001-$8,500)), with a payment rate of $8,250.50 for CY 2020.
d. Pathogen Test for Platelets
As stated in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59281), HCPCS code P9100 is used to report any test used to identify bacterial or other pathogen contamination in blood platelets. Currently, there are two rapid bacterial detection tests cleared by FDA that are described by HCPCS code P9100. According to their instructions for use, rapid bacterial detection tests should be performed on platelets from 72 hours after collection. Currently, certain rapid and culture-based tests can be used to extend the dating for platelets from 5 days to 7 days. Blood banks and transfusion services may test and use 6-day old to 7-day old platelets if the test results are negative for bacterial contamination.
HCPCS code P9100 was assigned in CY 2019 to New Technology APC 1493 (New Technology—Level 1C ($21-$30)), with a payment rate of $25.50. For CY 2020, based on CY 2018 claims data, there are approximately 1,100 claims reported for this service with a geometric mean cost of approximately $32. This geometric mean cost would result in the assignment of the service described by HCPCS code P9100 to a New Technology APC, based on the associated cost band, with a higher payment rate than where the service is currently assigned. Therefore, for CY 2020, we proposed to reassign the service described by HCPCS code P9100 to New Technology APC 1494 (New Technology—Level 1D ($31-$40)), with a proposed payment rate of $35.50.
Comment: One commenter expressed support for the proposal.
Response: We appreciate the support of the commenter.
After considering the public comments, we are finalizing our proposal to assign HCPCS code P9100 to New Technology APC 1494 (New Technology—Level 1D ($31-$40)), with a payment rate of $35.50.
e. Fractional Flow Reserve Derived From Computed Tomography (FFRCT)
Fractional Flow Reserve Derived from Computed Tomography (FFRCT), also known by the trade name HeartFlow, is a noninvasive diagnostic service that allows physicians to measure coronary artery disease in a patient through the use of coronary CT scans. The HeartFlow procedure is intended for clinically stable symptomatic patients with coronary artery disease, and, in many cases, may avoid the need for an invasive coronary angiogram procedure. HeartFlow uses a proprietary data analysis process performed at a central facility to develop a three-dimensional image of a patient's coronary arteries, which allows physicians to identify the fractional flow reserve to assess whether or not patients should undergo further invasive testing (that is, a coronary angiogram).
For many procedures in the OPPS, payment for analytics that are performed after the main diagnostic/image procedure are packaged into the payment for the primary procedure. However, in CY 2018, we determined that HeartFlow should receive a separate payment because the procedure is performed by a separate entity (that is, a HeartFlow technician who conducts computer analysis offsite) rather than the provider performing the CT scan. We assigned CPT code 0503T, which describes the analytics performed, to New Technology APC 1516 (New Technology—Level 16 ($1,401-$1,500)), with a payment rate of $1,450.50 based on pricing information provided by the developer of the procedure that indicated the price of the procedure was approximately $1,500.
For CY 2020, based on our analysis of the CY 2018 claims data available for the proposed rule, we found that over 840 claims had been submitted for payment for HeartFlow during CY 2018. We stated that the estimated geometric mean cost of HeartFlow was $788.19, or roughly $660 lower that the payment rate for CY 2019 of $1,450.50. Therefore, for CY 2020, we proposed to reassign the service described by CPT code 0503T in order to adjust the payment rate to better reflect the cost for the service. We proposed to reassign the service described by CPT code 0503T to New Technology APC 1509 (New Technology—Level 9 ($701-$800)), with a proposed payment rate of $750.50 for CY 2020. We sought public comments on this proposal.
Comment: Multiple commenters requested that we retain the CY 2019 OPPS APC assignment of APC 1516 (New Technology—Level 16 ($1401-$1500)) for HeartFlow with a payment rate of $1,450.50. The commenters were concerned that reducing the payment rate to $750.50 would discourage hospitals from using the service because they stated that the list price of the HeartFlow service is substantially higher than the proposed payment rate. Commenters were concerned that reduced utilization of HeartFlow would cause some beneficiaries to have unnecessary invasive coronary angiograms that are more costly than the HeartFlow procedure.
Multiple commenters, including the developer of HeartFlow, provided additional reasons to maintain the current payment rate for the service of $1,450.50 despite claims data suggesting a lower payment rate for HeartFlow. The commenters believed that 78 single frequency claims used for the proposed rule solely represented a single year and that such a low number of claims would be an insufficient number of claims on which to base a payment rate reduction for the service. Two commenters suggested that CMS should collect another one or two years of claims data before making changes to the current payment rate. One of the commenters believed the reason the estimated cost of HeartFlow derived from claims data is substantially less than the current payment rate may be due to providers submitting claims without marked up gross charges for the services they provide.
Another commenter, the developer, encouraged CMS to use our equitable adjustment authority under section 1833(t)(2)(E) of the Act, which states that the Secretary shall establish, in a budget neutral manner, other adjustments as determined to be necessary to ensure equitable payments to maintain the current payment rate for HeartFlow. The developer suggested that CMS should use its own assessment of the resources required to perform the HeartFlow service to set the payment rate for the service. The developer cited instances in the last four years where CMS used its equitable adjustment authority to mitigate either large fluctuations or declines in annual payment rates. These cases include: (1) A CY 2018 decision to use multiple years of claims data to pay a higher rate for CPT code 0100T (Placement of a subconjunctival retinal prosthesis receiver and pulse generator, and implantation of intraocular retinal electrode array, with vitrectomy) of $122,500.50 rather than the payment rate generated by the most recent year of claims data of $95,000.50; (2) a CY 2016 decision regarding the payment rate of CPT code 0308T (Insertion of ocular telescope prosthesis including removal of crystalline lens or intraocular lens prosthesis) where the median cost of $18,365 was used to set the payment rate instead of the geometric mean cost of $13,865 because only 39 single frequency claims were reported for the service, and where we stated that “the median cost would be a more appropriate measure of the central tendency for purposes of calculating the cost and the payment rate for the procedure;” (3) a CY 2016 decision to adjust the geometric mean per diem cost for the partial hospital program to ensure a per diem payment for fewer services was less than a per diem payment for a larger number of services; and (4) a CY 2018 decision to establish a payment rate of $17,500.50 for CPT code 0398T (Magnetic resonance image guided high intensity focused ultrasound (mrgfus), stereotactic ablation lesion, intracranial for movement disorder including stereotactic navigation and frame placement when performed) instead of proposed payment rate of $9,750.50.
The developer believes that the proposed New Technology APC assignment for HeartFlow, which would result in a nearly 50 percent reduction in the payment rate between CY 2019 and CY 2020, is similar to these cases described in their comment. Therefore, the developer asked us to use our equitable adjustment authority to maintain the CY 2019 payment rate of $1,450.50 for the service rather than adopt the proposed payment rate.
Response: The proposed payment rate for CPT code 0503T was based on claims data from CY 2018, which is the first year the service was payable in the OPPS. For ratesetting for CY 2018 and CY 2019, there were no claims data available showing the cost of the service. Also, there were no services identified as comparable to CPT code 0503T, which meant we could not estimate the cost of CPT code 0503T by using the cost of a similar service. Accordingly, we previously based pricing for the service on pricing information provided by the developer of the procedure.
We recognize that there was a low volume of claims for HeartFlow based on the data available for the proposed rule and, thus, we should have applied the low-volume policy for new technology services in the proposed rule.
However, for the final rule, using the most recently available data, there are now 957 total claims billed with CPT code 0503T and 101 single frequency claims. We appreciate the concerns of the commenters who stated that there were not enough claims billed with HeartFlow to use claims data to revise the rate for HeartFlow. While 101 single claims is above the threshold we established for low-volume services assigned to a new technology APC, we agree with the commenters that a payment reduction of nearly 50 percent is significant for a new technology that still has relatively low volume.
Accordingly, given the low number of single frequency claims for CPT code 0503T, that number of claims for the Heartflow procedure was below the low-volume payment policy threshold for the proposed rule, and that it is only two claims above the threshold using data available for this final rule with comment period, we have decided to use our equitable adjustment authority under section 1833(t)(2)(E) of the Act to calculate the geometric mean, arithmetic mean, and median using the CY 2018 claims data to determine an appropriate payment rate for HeartFlow using our new technology APC low-volume payment policy. While the number of single frequency claims is just above our threshold to use the low-volume payment policy, we still have concerns about the normal cost distribution of the claims used to calculate the payment rate for Heartflow, and we decided the low-volume payment policy would be the best approach to address those concerns.
Our analysis found that the geometric mean cost for CPT code 0503T was $768.26, the arithmetic mean cost for CPT code 0503T was $960.12 and that the median cost for CPT code 0503T was $900.28. Of the three cost methods, the highest amount was for the arithmetic mean. The arithmetic mean falls within the cost band for New Technology APC 1511 (New Technology—Level 11 ($901-$1000)) with a payment rate of $950.50. The arithmetic mean helps to account for some of the higher costs of CPT code 0503T identified by the commenters that may not have been reflected by either the median or the geometric mean. We acknowledge the commenters' concern and recognize that it may be theoretically possible that the reported cost of CPT code 0503T is higher than what we calculated from the claims data due to some providers reporting costs lower than actual costs for the service. However, we rely on hospitals to bill all CPT codes accurately in accordance with their code descriptors and CPT and CMS instructions, as applicable, and to report charges on claims and charges and costs on their Medicare hospital cost reports appropriately. In addition, we do not specify the methodologies that hospitals must use to set charges for this or any other service.
After consideration of the public comments we received, we are utilizing our new technology low-volume payment policy to set the payment rate for the HeartFlow service CPT code 0503T based on the arithmetic mean for the procedure. Specifically, we are assigning CPT code 0503T to New Technology APC 1511 (New Technology—Level 11 ($901-$1000)) with a payment rate of $950.50.
f. Cardiac Positron Emission Tomography (PET)/Computed Tomography (CT) Studies
Effective January 1, 2020, we have assigned three CPT codes (78431, 78432, and 78433) that describe the services associated with cardiac PET/CT studies to New Technology APCs. Table 13 reports code descriptors, status indicators, and APC assignments for these CPT codes. These codes were listed in Addendum B to the CY 2020 OPPS/ASC proposed rule as 78X32, 78X33, and 78X44. More information about CPT codes 78431, 78432, and 78433 can be found in section III. D. b. of this final rule.
Comment: Several commenters reported that certain societies submitted a new technology application to CMS for CPT codes 78431, 78432, and 78433 that details the costs associated with providing these services. For CPT code 78431, these same commenters disagreed with the proposed APC placement and recommended its reassignment from APC 5594 (Level 4 Nuclear Medicine and Related Services) with a proposed payment rate of $1,466.16 to APC 1522 (New Technology—Level 23 ($2501-$3000)) with a proposed payment rate of $2,750.50. They reported that, based on the resource cost of the service described by CPT code 78431, APC 1522 provides adequate reimbursement for the service. Similarly, for CPT codes 78432 and 78433, the commenters indicated that APC 5594 would not adequately cover the resource costs associated with these procedures, and recommended their reassignment to APC 1523 (New Technology—Level 23 ($2501-$3000)) with a proposed payment rate of $ 2,750.50
Response: Based on the information provided in the new technology application, and the comments received, we are revising the APC assignments for these codes. Specifically, we are revising the APC assignment for CPT code 78431 from APC 5594 to APC 1522, and reassigning CPT codes 78432 and 78433 from APC 5594 to APC 1523.
In summary, after consideration of the public comments for the new cardiac PET/CT codes, and based on our evaluation of the new technology application which provided the estimated costs for the services and described the components and characteristics of the new codes, we are assigning CPT codes 78431, 78432, and 78433 to the final APCs listed in Table 14 below. Please refer to section III. D. b. of this final rule for more information on the finalized proposal to establish a payment rate for other new CPT codes associated with PET/CT studies. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period (which is available via the internet on the CMS website).


g. V-Wave Interatrial Shunt Procedure
A randomized, double-blinded control IDE study is currently in progress for the V-Wave interatrial shunt procedure. All participants who passed initial screening for the study receive a right heart catherization procedure described by CPT code 93451 (Right heart catheterization including measurement(s) of oxygen saturation and cardiac output, when performed). Participants assigned to the experimental group also receive the V-Wave interatrial shunt procedure while participants assigned to the control group only receive right heart catheterization. The developer of V-Wave is concerned that the current coding of these services by Medicare would reveal to the study participants whether they have received the interatrial shunt because an additional procedure code, CPT code 93799 (Unlisted cardiovascular service or procedure) would be included on the claims for participants receiving the interatrial shunt. Therefore, we created a temporary HCPCS code to describe the V-wave interatrial shunt procedure for both the experimental group and the control group in the study. Specifically, we established HCPCS code C9758 (Blinded procedure for NYHA class III/IV heart failure; transcatheter implantation of interatrial shunt or placebo control, including right heart catheterization, trans-esophageal echocardiography (TEE)/intracardiac echocardiography (ICE), and all imaging with or without guidance (for example, ultrasound, fluoroscopy), performed in an approved investigational device exemption (IDE) study) to describe the service, and we assigned the service to New Technology APC 1589 (New Technology—Level 38 ($10,001-$15,000)). Details about the temporary HCPCS code are shown in Table 15 below. The final CY 2020 payment rate for V-Wave interatrial shunt procedure can be found in Addendum B to this final rule with comment period (which is available via the internet on the CMS website).

D. OPPS APC-Specific Policies
1. Barostim NeoTM System (APC 5464)
In CY 2019, CPT codes 0266T and 0268T were assigned to APC 5463 (Level 3 Neurostimulator and Related Procedures) with a payment rate of $18,707.16. For CY 2020, as listed in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to reassign both codes to APC 5464 (Level 4 Neurostimulator and Related Procedures) with a proposed payment rate of $29,025.99. Table 16 below lists the long descriptors, proposed status indicator (SI), and APC assignments for these codes. We note that both codes are associated with the Barostim NeoTM System.
Comment: A medical device company agreed with the reassignment for CPT codes 0266T and 0268T to APC 5464. The commenter stated that APC 5464 is the more appropriate assignment for these codes based on clinical and resource homogeneity, and encouraged CMS to finalize the APC assignment.
Response: As we have stated every year since the implementation of the OPPS on August 1, 2000, we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on our analysis of the latest claims data.
Based on our analysis of the proposed rule claims data as well as clinical review of the services described, we proposed to revise the APC assignment for both CPT codes 0266T and 0268T to APC 5464. In our analysis of CPT code 0268T (which describes implantation/replacement of the pulse generator), we noticed that the APC assignment for CPT code 0266T (which describes the implantation or replacement of the complete system) was lower. We do not believe that the payment for the complete system (CPT code 0266T) should be less than the payment for the implantation/replacement of the pulse generator (CPT code 0268T) procedure. Consequently, we proposed to revise the APC assignment for CPT code 0266T to APC 5464. Although we had no claims data for CPT code 0266T, we believed it was necessary to revise the APC assignment to appropriately reflect the device cost associated with the procedure.
Similar to our findings for the proposed rule, based on updated claims data for this final rule with comment period, the geometric mean cost for CPT code 0268T supports its reassignment from APC 5463 to APC 5464. Specifically, our claims data show a geometric mean cost of approximately $25,558 for CPT code 0268T based on 6 single claims (out of 6 total claims), which is consistent with the geometric mean cost of approximately $28,491 for APC 5464, rather than the geometric mean cost of approximately $18,864 for APC 5463. Furthermore, as mentioned above, we are also assigning CPT code 0266T to APC 5464 even though we do not yet have claims data because we do not believe that the service for implantation of the entire system (CPT code 0266T) would be less resource intensive than the implantation of the pulse generator alone (CPT code 0268T).
In summary, after consideration of the public comment and analysis of the latest claims data, we are finalizing our proposal, without modification, to assign CPT codes 0266T and 0268T to APC 5464 for CY 2020. Table 16 below list the long descriptors for the codes and the final SI and APC assignments. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) assignments for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.

2. Biomechanical Computed Tomography (BCT) Analysis (APCs 5521, 5523, and 5731)
The CPT Editorial Panel established five new codes, specifically, CPT codes 0554T, 0555T, 0556T, 0557T, and 0558T, to describe the services associated with biomechanical computed tomography (BCT) analysis effective July 1, 2019. Through the July 2019 OPPS quarterly update CR (Transmittal 4313, Change Request 11318, dated May 24, 2019), we assigned these new codes to appropriate interim status indicators (SI) and APCs. Table 17 below lists the long descriptors and proposed SI and APCs of the codes.
Comment: A commenter agreed with the SI and APC assignments and stated that the APC assignments for these codes are the best available placements. The commenter also noted that CMS did not assign the comprehensive code (CPT code 0554T) and the physician interpretation code (CPT code 0557T) to an APC because the codes represent physician services.
Response: We thank the commenter for its feedback. We are finalizing the SIs and APC assignments for the codes. Table 17 below list the long descriptors and final SIs and APCs. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the complete list of the OPPS payment status indicators and their definitions for CY 2020. Both Addendum B and Addendum D1 are available via the internet on the CMS website.
As we do for all codes, we will reevaluate the APC assignments for CPT codes 0555T, 0556T, and 0558T once we have claims data. We remind hospitals that we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on the latest claims data.
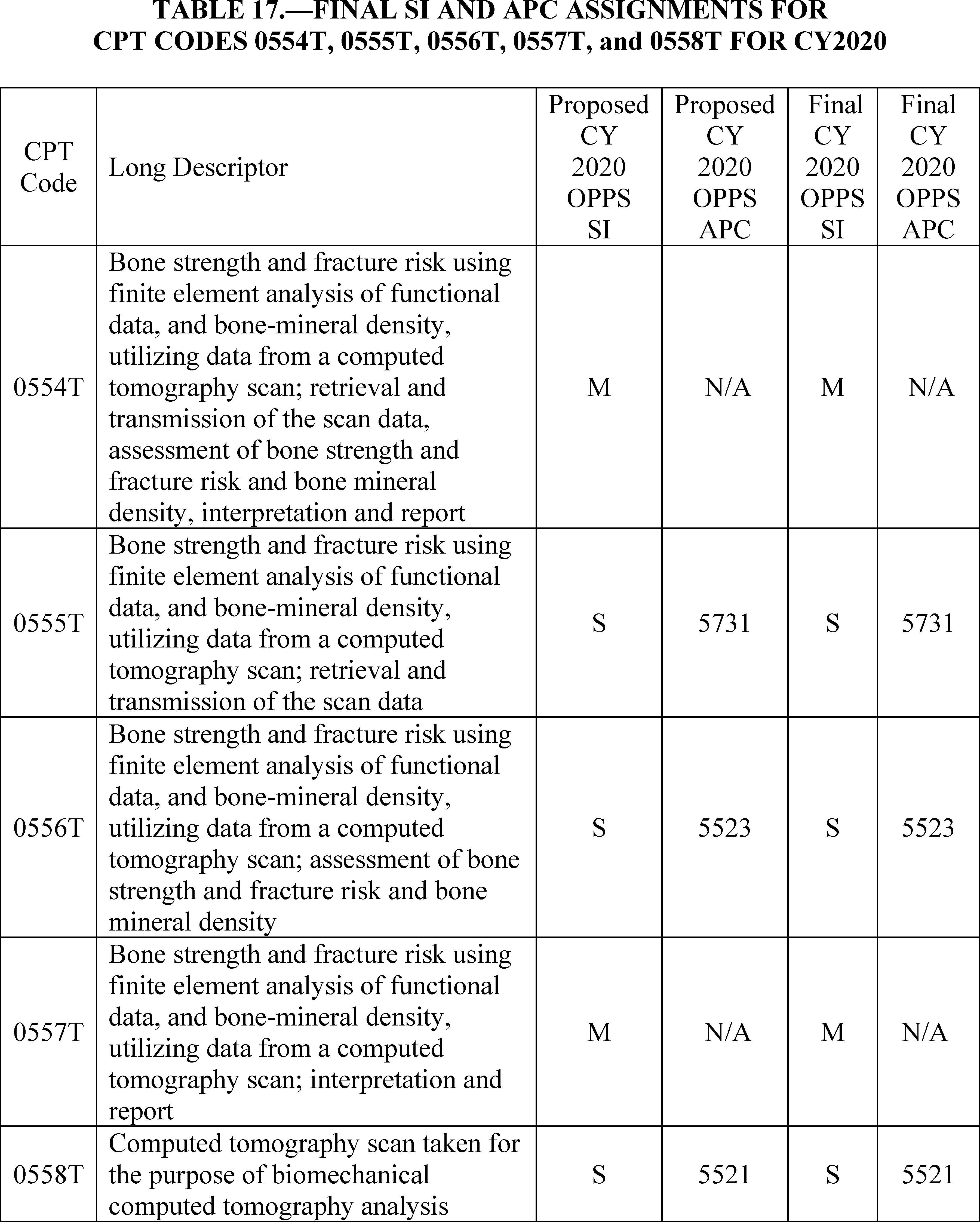
3. Cardiac Magnetic Resonance (CMR) Imaging (APC 5572)
For CY 2020, we proposed to maintain the APC assignment for CPT code 75561 (Cardiac magnetic resonance imaging for morphology and function without contrast material(s), followed by contrast material(s) and further sequences) to APC 5572 (Level 2 Imaging with Contrast) with a proposed payment rate of $373.45.
Comment: Some commenters expressed concern with the placement of CPT code 75561 in APC 5572, and stated that it is grouped with services that are not similar clinically or with respect to resource use. As an example, they observed that CPT code 75561 is unlike CT of the abdomen or pelvis or MRI of the neck and spine, and instead, is more similar to those services in APC 5573 (Level 3 Imaging with Contrast), with a proposed payment rate of $682.96.Another commenter expressed concern with the payment stability for CPT code 75561. The commenter noted that although the code is assigned to the same APC for CY 2020, the payment for the service is slated for another reduction. The commenter observed that the payment rate for the service has decreased in the last several years and noted the following yearly rates:
- CY 2017 OPPS payment rate: $426.52
- CY 2018 OPPS payment rate: $456.34
- CY 2019 OPPS payment rate: $385.88
- CY 2020 OPPS proposed payment rate: $373.45
This same commenter reported that the code was previously included in a nuclear medicine APC, which it maintained was appropriate based on its clinical and resource homogeneity to cardiovascular magnetic resonance and cardiac nuclear imaging services in the APC, and that, since its APC reassignment, the payment for the service has dropped. The commenter believed that the different cost reporting methods used by hospitals may contribute to the artificially low relative payment weights and payment amounts for CT and MR.
Response: For CY 2020, based on claims submitted between January 1, 2018 through December 30, 2018, that were processed on or before June 30, 2019, our analysis of the latest claims data for this final rule continues to support our proposal of assigning CPT code 75561 to APC 5572. Specifically, our claims data show a geometric mean cost of approximately $413 for CPT code 75561 based on 14,350 single claims (out of 18,118 total claims), which is comparable to the geometric mean cost of about $359 for APC 5572, rather than the geometric mean cost of approximately $660 for APC 5573. The geometric cost of approximately $413 for CPT code 75561 is also consistent with the costs for significant services in APC 5572, which range between about $269 (for CPT code 74174) to $515 (for CPT code 73525). Based on our analysis of the latest claims data, we believe that CPT code 75561 is appropriately assigned to APC 5572.
With regards to the issue of payment stability, we note that Section 1833(t)(9)(A) of the Act requires the Secretary to review, not less often than annually, and to revise the groups, relative payment weights, and the wage and other adjustments to take into account changes in medical practices, changes in technology, the addition of new services, new cost data, and other relevant information and factors. Therefore, every year we review and revise the APC assignments based on our evaluation of these factors using the latest OPPS claims data. While we recognize the concerns about payment stability, we note that changes made to payment rates are based on our calculations of geometric mean costs from the most recently available Medicare claims and cost report data analysis, which may or may not result in payment increases and/or reductions based on the most recent geometric mean costs available. We note that the geometric mean costs reflect the national average resources to furnish a service in the hospital outpatient setting. To the extent that costs decrease, so too, would the payment rate.
In addition, with regard to the issue of different hospital cost reporting methods, we are unable to determine whether hospitals are misreporting the procedure. It is generally not our policy to judge the accuracy of hospital charging and coding for purposes of ratesetting. We rely on hospitals to accurately report the use of HCPCS codes in accordance with their code descriptors and CPT and CMS instructions, and to appropriately report services on claims and charges and costs for the services on their Medicare hospital cost report. Also, we do not specify the methodologies that hospitals use to set charges for this or any other service. Furthermore, we state in Chapter 4 of the Medicare Claims Processing Manual that “it is extremely important that hospitals report all HCPCS codes consistent with their descriptors; CPT and/or CMS instructions and correct coding principles, and all charges for all services they furnish, whether payment for the services is made separately paid or is packaged” to enable CMS to establish future ratesetting for OPPS services.
Comment: One commenter who expressed concern with the APC assignment for CPT code 75561 also requested that we address in the final rule how we determine which services are clinically similar. The commenter noted that CMS has constructed many APCs with a mix of imaging services that are dissimilar and yet preserves the clinical homogeneity of some APCs, such as nuclear medicine services.
Response: Under the OPPS, each service is assigned to an APC based on the clinical and resource similarity to other services within the APC or family of APCS. The OPPS is a prospective payment system under which payment groupings (that is, APCs) are based on clinical and resource similarity rather than code-specific payment rates, which would result in a cost-based fee schedule. For example APCs 5111-5116, which are described as Levels 1 through 6 Musculoskeletal Procedures, all include services that involve musculoskeletal services/procedures and the various levels of that APC family differentiate such procedures based on resource homogeneity. That is, the descriptors for APCs 5111 through 5116 are general and broadly describe a variety of musculoskeletal procedures, and are differentiated by the various levels based on the geometric mean costs for each APC. Clinically, all the procedures in APCs 5111 through 5116 are similar in that they involve some form of musculoskeletal procedure. In addition, as stated in section III.B.2. (Application of the 2 Times Rule) of this final rule with comment, section 1833(t)(2) of the Act provides that, subject to certain exceptions, the items and services within an APC group cannot be considered comparable with respect to the use of resources if the highest cost for an item or service in the group is more than 2 times greater than the lowest cost for an item or service within the same group (referred to as the “2 times rule”). While it may seem appropriate to place one code in a specific grouping, based on our 2 times rule criteria, we must assign the code to the appropriate APC based on its geometric mean cost.
In summary, after consideration of the public comments, we are finalizing our proposal, without modification, to assign CPT code 75561 to APC 5572. The final CY 2020 payment rate for CPT code 75561 can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
4. CardioFluxTM Magnetocardiography (MCG) Myocardial Imaging (APC 5723)
For CY 2020, we proposed to maintain the APC assignment for CPT code 0541T to APC 5722 (Level 2 Diagnostic Tests and Related Services) with a proposed payment rate of $256.60. We also proposed to continue to assign CPT code 0541T, which is an add-on code, to status indicator “N” to indicate that the code is packaged and payment for it is included in the primary procedure or service. In this case, the payment for 0542T is included in CPT code 0541T. We note that CPT codes 0541T and 0542T are associated with the CardioFlux magnetocardiography imaging technology. Table 18 below lists the long descriptors for the codes as well as the proposed SI and APC assignments.
Comment: A commenter disagreed with the assignment to APC 5722 and reported that the service associated with CPT code 0541T is not clinically and resource comparable to the services in the APC. The commenter stated that the service is clinically comparable to the services that are assigned to APCs 5593 and 5724, specifically:
- APC 5593 (Level 3 Nuclear Medicine), with a proposed payment rate of $ 1,293.33, which includes—
+ CPT code 78451 (Myocardial perfusion imaging); and
+ CPT code 78452 (Myocardial perfusion imaging).
- APC 5724 (Level 4 Diagnostic Tests and Related Services), with a proposed payment rate of approximately $ 920.66, which includes—
+ CPT code 95965 (Magnetoencephalography (MEG)); and
+ CPT code 95966 (Magnetoencephalography (MEG)).
The commenter indicated that this new technology requires the use of very expensive capital equipment, and added that the CardioFlux System costs about $1.5 million with a useful life of seven years. The technology itself involves hospital site implementation and ongoing operation. The commenter stated that the proposed payment does not provide adequate payment for this novel technology. The commenter expressed concern that the proposed low payment rate will severely limit uptake of this new technology, and, consequently, urged CMS to reassign CPT code 0541T to either APC 5593 or APC 5724 to ensure patient access to this emerging technology and its potential for savings to the Medicare program.
Response: Under the OPPS, one of our goals is to make payments that are appropriate for the services that are necessary for the treatment of Medicare beneficiaries. The OPPS, like other Medicare payment systems, is a prospective payment system. The payment rates that are established reflect the geometric mean costs associated with items and services assigned to an APC and we believe that our payment rates generally reflect the costs that are associated with providing care to Medicare beneficiaries in cost efficient settings. Moreover, we strive to establish rates that are adequate to ensure access to medically necessary services for Medicare beneficiaries.
For many emerging technologies there is a transitional period during which utilization may be low, often because providers are first learning about the techniques and their clinical utility. Quite often, the requests for higher payment amounts are for new procedures in that transitional phase. These requests, and their accompanying estimates for expected Medicare beneficiary or total patient utilization, often reflect very low rates of patient use, resulting in high per use costs for which requesters believe Medicare should make full payment. Medicare does not, and we believe should not, assume responsibility for more than its share of the costs of procedures based on Medicare beneficiary projected utilization and does not set its payment rates based on initial projections of low utilization for services that require expensive capital equipment.
We note that in a budget neutral environment, payments may not fully cover hospitals' costs, including those for the purchase and maintenance of capital equipment. We rely on hospitals to make their decisions regarding the acquisition of high cost equipment with the understanding that the Medicare program must be careful to establish its initial payment rates for new services that lack hospital claims data based on realistic utilization projections for all such services delivered in cost-efficient hospital outpatient settings. As the OPPS acquires claims data regarding hospital costs associated with new procedures, we annually review the claims data and any available new information regarding the clinical aspects of new procedures to confirm that our OPPS payments remain appropriate for procedures as they transition into mainstream medical practice.
In addition, we note this new technology is currently under clinical trial (ClinicalTrials.gov Identifiers: NCT03968809 and NCT04044391) and does not appear to be a service that is typically performed in an HOPD facility. Further, based on our clinical evaluation, we do not agree that CardioFlux MCG is similar to the MEG procedures described by CPT codes 95965 and 95966 since MEG procedures involve the brain while the CardioFlux technology involves imaging of the heart. Also, we do not agree that CardioFlux MCG is similar to the myocardial perfusion scans described by CPT codes 78451 and 78452 because these scans involve the use of radioactive tracers, specialized staff, and more time as the test generally takes two to four hours to complete. Furthermore, based on our findings, the CardioFlux MCG scan is unlike other cardiac imaging tests because it does not require or expose the patient to radiation, and takes about 90 seconds to perform with physician review and return of interpretation of the results in an estimated 5 minutes per patient.
However, based on our review of the issue and feedback from our medical advisors, as well as the anticipated operating costs per case derived from the public comment and publicly available information about the service, we believe that CPT code 0541T should be assigned to APC 5723 (Level 3 Diagnostic Tests and Related Services) rather than to APC 5722 (Level 2 Diagnostic Tests and Related Services). Because we have neither claims data nor specific HOPD costs, including the cost to perform each exam (other than the cost of the capital equipment that was supplied to us), we believe that APC 5723 is the most appropriate assignment at this time.
Therefore, after consideration of the public comment, we are finalizing our proposal, with modification, to assign CPT code 0541T to APC 5723. Table 18 list the long descriptors and final SI and APC assignments for both codes. The final CY 2020 payment rate for CPT code 0541T can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.

5. Cataract Removal With Endoscopic Cyclophotocoagulation (ECP) (APC 5492)
For CY 2020, the CPT Editorial Panel established two new codes to describe cataract removal with endoscopic cyclophotocoagulation (ECP), specifically, CPT codes 66987 and 66988. As listed in Table 19 below with the long descriptors, and also in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign CPT code 66987 and 66988 to APC 5491 (Level 1 Intraocular Procedures) with a proposed payment rate of $2,053.39. The codes were listed as 66X01 and 66X02 (the 5-digit CMS placeholder codes), respectively, in Addendum B with the short descriptors and again in Addendum O with the long descriptors. We also assigned the codes to comment indicator “NP” in Addendum B to indicate that they are new for CY 2020 and that public comments would be accepted on their proposed status indicator assignments. We note these codes will be effective January 1, 2020.
Comment: A commenter disagreed with the APC assignment and, based on their analysis of the combined geometric mean costs for the existing cataract and ECP procedures (CPT codes 66982, 66984, and 66711), believed the new codes should be reassigned to APC 5492 (Level 2 Intraocular Procedures) with a proposed payment rate of $3,867.16. Four professional ophthalmology organizations suggested that CMS should establish the payment rate for CPT code 66987 based on the combined costs of CPT codes 66711 and 66982, and, similarly, determine the payment rate for CPT code 66988 based on the combined costs of CPT codes 66711 and 66984. They expressed concern that the proposed payment rates for the codes do not adequately capture the resources hospitals will expend for each combined procedure.
Response: APC assignment for a code is not typically based on combined costs of existing HCPCS codes, rather, it is based on similarity to other codes within an APC based clinical homogeneity and resource costs. As specified in 42 CFR 419.31(a)(1), CMS classifies outpatient services and procedures that are comparable clinically and in terms of resource use into APC groups. Also, as we stated in the CY 2012 OPPS/ASC final rule (76 FR 74224), the OPPS is a prospective payment system that provides payment for groups of services that share clinical and resource use characteristics. It should be noted that, with all new codes, our policy has been to assign the service or procedure to an APC based on feedback from a variety of sources, including but not limited to review of the clinical similarity of the service to existing procedures; advice from CMS medical advisors; information from interested specialty societies; and review of all other information available to us, including information provided to us by the public, whether through meetings with stakeholders or additional information that is mailed or otherwise communicated to us.
Based on our analysis of the public comment and input from our medical advisors, we believe that we should revise the APC assignment for these new cataract codes. We reviewed the components of the procedure associated with CPT codes 66987 and 66988, and after our analysis, we agree with commenters that the resources associated with the new codes are higher than the routine cataract and ECP procedures when performed by themselves. Therefore, we are reassigning the new codes from APC 5491 to APC 5492.
In summary, after consideration of the public comments, we are finalizing our proposal with modification, and revising the APC assignment for CPT codes 66987 and 66988 to APC 5492 for CY 2020. Table 19 lists the final SI and APC assignments for the two codes. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
We note that we will reevaluate the APC assignments for CPT codes 66987 and 66988 once we have claims data. We review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on the latest claims data that we have available.

6. Chimeric Antigen Receptor T-Cell (CAR T) Therapy (APCs 5694, 9035, and 9194)
Chimeric Antigen Receptor (CAR) T-cell therapy is a cell-based gene therapy in which T-cells are collected and genetically engineered to express a chimeric antigen receptor that will bind to a certain protein on a patient's cancerous cells. The CAR T-cells are then administered to the patient to attack certain cancerous cells and the individual is observed for potential serious side effects that would require medical intervention.
Two CAR T-cell therapies received FDA approval in 2017. KYMRIAH® (manufactured by Novartis Pharmaceuticals Corporation) was approved for use in the treatment of patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. In May 2018, KYMRIAH® received FDA approval for a second indication, treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL), high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma. YESCARTA® (manufactured by Kite Pharma, Inc.) was approved for use in the treatment of adult patients with relapsed or refractory large B-cell lymphoma and who have not responded to or who have relapsed after at least two other kinds of treatment.
The HCPCS code to describe the use of KYMRIAH® (HCPCS code Q2042) has been active since January 1, 2019 for OPPS, which replaced HCPCS code Q2040, active January 1, 2018 through December 31, 2018, as discussed in the CY2019 OPPS/ASC final rule with comment period. The HCPCS code to describe the use of YESCARTA® (HCPCS code Q2041) has been active since April, 1, 2018 for OPPS. The HCPCS Q-code for the currently approved CAR T-cell therapies include leukapheresis and dose preparation procedures because these services are included in the manufacturing of these biologicals. Both of these CAR T-cell therapies were approved for transitional pass-through payment status, effective April 1, 2018. The HCPCS codes that describe the use of these CAR T-cell therapies were assigned status indicator “G” in Addenda A and B to the CY2020 OPPS/ASC proposed rule.
As discussed in section V.A.4. (Drugs, Biologicals, and Radiopharmaceuticals with New or Continuing Pass-Through Payment Status in CY 2019) of this final rule with comment period, we are finalizing our proposal to continue pass-through payment status for HCPCS code Q2042 and HCPCS code Q2041 for CY 2020. In section V.A.4. of this final rule with comment period, we also are finalizing our proposal to determine the pass-through payment rate following the standard ASP methodology, updating pass-through payment rates on a quarterly basis if applicable information indicates that adjustments to the payment rates are necessary.
The AMA created four Category III CPT codes that are related to CAR T-cell therapy, effective January 1, 2019. As discussed in the CY 2019 OPPS/ASC final rule with comment period, we finalized our proposal to assign procedures described by CPT codes, 0537T, 0538T, and 0539T to status indicator “B” (Codes that are not recognized by OPPS when submitted on an outpatient hospital Part B bill type (12x and 13x)) to indicate that the services are not paid under the OPPS. The procedures described by CPT codes 0537T, 0538T, and 0539T describe the various steps required to collect and prepare the genetically modified T-cells, and Medicare does not generally pay separately for each step used to manufacture a drug or biological. Additionally, we finalized that the procedures described by CPT code 0540T would be assigned status indicator “S” (Procedure or Service, Not Discounted when Multiple) and APC 5694 (Level IV Drug Administration) for CY 2019. Additionally, the National Uniform Billing Committee (NUBC) established CAR T-cell related revenue codes and value code to be reportable on Hospital Outpatient Department (HOPD) claims effective for claims received on or after April 1, 2019.
As listed in Addendum B of the CY 2020 OPPS/ASC proposed rule, we proposed to assign procedures described by these CPT codes, 0537T, 0538T, and 0539T, to status indicator “B” (Codes that are not recognized by OPPS when submitted on an outpatient hospital Part B bill type (12x and 13x)) to indicate that the services are not paid under the OPPS. We proposed to assign CPT code 0540T to status indicator “S” (Procedure or Service, Not Discounted when Multiple) and APC 5694 (Level IV Drug Administration).
At the August 19, 2019 meeting, the HOP Panel recommended that CMS reassign the status indicator for the procedures described by the specific CPT codes 0537T, 0538T, and 0539T from “B” to “Q1” for CY2020.
Comment: Several commenters opposed our proposal to continue to assign status indicator “B” to CPT codes 0537T, 0538T, and 0539T for CY2020. Commenters proposed a variety of alternative status indicators including status indicators “N”, “S”, and “Q1.” Commenters believed that CPT codes 0537T, 0538T, and 0539T did not represent the steps required to manufacture the CAR T product as CMS has stated. Generally, those advocating for status indicator “N” (Items and Services Packaged into APC Rates) stated that this assignment would ease the billing burden and confusion experienced by providers under the current status indicator assignment of “B”. Generally, those advocating for status indicator “S” (Procedure or Service, Not Discounted When Multiple) believed that separate payment is warranted for these services as they are distinct procedures and are ordered and performed by clinicians. Finally, generally those advocating for status indicator “Q1”, indicating conditional separate payment, supported the HOP Panel's recommendation to assign this status indicator based on codes, such as CPT code 0565T (placeholder code 05X3T) (Autologous cellular implant derived from adipose tissue for the treatment of osteoarthritis of the knees; tissue harvesting and cellular implant creation). CPT code 0565T has a status indicator of “Q1” and commenters believe it is similar to the procedures described by CPT codes 0537T, 0538T, and 0539T, since CPT code 0565T involves the collection and harvest of cells, in the form of tissue, for the treatment of osteoarthritis of the knee. Additionally, commenters stated that the HCPCS drug Q-codes (Q2041 and Q2042) should be revised to eliminate the language referencing leukapheresis and dose preparation procedures.
Response: We thank the commenters for their feedback. CMS does not believe that separate or packaged payment under the OPPS is necessary for the procedures described by CPT codes 0537T, 0538T, and 0539T for CY2020. The existing CAR T-cell therapies on the market were approved as biologics and, therefore, provisions of the Medicare statute providing for payment for biological products apply. The procedures described by CPT codes 0537T, 0538T, and 0539T describe the various steps required to collect and prepare the genetically modified T-cells and Medicare does not generally pay separately for each step used to manufacture a drug or biological product. Additionally, we note that CAR T-cell therapy is a unique therapy approved as a biologic, with unique preparation procedures, and it cannot be directly compared to other therapies or existing CPT codes. We note that the current HCPCS coding for the currently approved CAR T-cell therapy drugs, HCPCS codes Q2041 and Q2042, include leukapheresis and dose preparation procedures as these services are including in the manufacturing of these biologicals. Therefore, payment for these services is incorporated into the drug Q-codes. We note that although there is no payment associated with 0537T, 0538T, and 0539T for reasons stated previously, these codes can still be reported to CMS for tracking purposes. Additionally, HOPDs can bill Medicare for reasonable and necessary services that are otherwise payable under the OPPS, and we believe that the comments in reference to payment for services in settings not payable under the OPPS are outside the scope of this proposed rule.
Accordingly, we are not revising the existing Q-codes for CAR T-cell therapies to remove leukapheresis and dose preparation procedures, and we are not accepting the recommendations to revise the status indicators for procedures described by CPT codes 0537T, 0538T, and 0539T. We will continue to evaluate and monitor our payment for CAR T-cell therapies.
Comment: We note that commenters were supportive of the decision to continue the assignment of status indicator “S” (Procedure or Service, Not Discounted When Multiple) to CPT code 0540T.
Response: We thank commenters for their support and are finalizing our proposal to maintain status indicator “S” for CPT code 0540T.
Comment: Some commenters recommended CMS evaluate modifications to CAR T-cell payments for future rule making years, including strategies such as creating a new statutory benefit category for cell and gene therapies and value-based payment. Specifically, commenters suggested value-based payments could include milestone-based payments over time, indication-based pricing or combination-based pricing.
Response: We thank commenters for their feedback. Currently, the existing CAR T-cell therapies on the market were approved as biologics and, therefore, provisions of the Medicare statute providing for payment for biologicals apply. In regards to the creation of a new statutory benefit category, that is out of the scope of existing CMS statutory authority.
In summary, after consideration of the public comments we received, we are finalizing our proposal to assign status indicator “B” to CPT codes 0537T, 0538T, and 0539T for CY2020. Additionally, we are continuing our policy from CY2019 to assign status indicator “S” to CPT code 0540T for CY2020. Tables 20 and 21 below show the final SI and APC assignments for HCPCS codes Q2041, Q2042, 0537T, 0538T, 0539T, and 0540T for CY 2020. We refer readers to Addendum B to this final rule with comment period for the payment rates for all codes reportable under the OPPS. Addendum B is available via the internet on the CMS website. In addition, we refer readers to Addendum D1 to this final rule with comment period for the complete list of the OPPS payment status indicators and their definitions for CY2020.


7. Colonoscopy and Sigmoidoscopy With Endoscopic Mucosal Resection (EMR) (APC 5313)
For CY 2020, we proposed to continue to assign CPT codes 45349 and 45390 to APC 5312 (Level 2 Lower GI Procedures), with a proposed payment rate of $1,024.08. The long descriptors and proposed SI and APC assignments for both codes can be found in Table 22 below.
Comment: A commenter believed that the two procedures are different from the other procedures currently assigned to APC 5312, and stated they are more similar to these procedures that are assigned to APC 5313:
- 46610 (Anoscopy; with removal of single tumor, polyp, or other lesion by hot biopsy forceps or bipolar cautery);
- 46612 (Anoscopy; with removal of multiple tumors, polyps, or other lesions by hot biopsy forceps, bipolar cautery or snare technique); and
- 46615 (Anoscopy; with ablation of tumor(s), polyp(s), or other lesion(s) not amenable to removal by hot biopsy forceps, bipolar cautery or snare technique) where lesions are being removed by methods other than just the snare wire technique.
Based on clinical and resource homogeneity, the commenter requested a reassignment from APC 5312 to APC 5313 (Level 3 Lower GI Procedures), which had a proposed payment rate of $2,512.28, for CPT code 45349 and 45390
Response: Upon review of data available for this final rule with comment period, we agree with the commenter that the most appropriate assignment for both codes is APC 5313. Based on the latest hospital outpatient claims data used for this final rule with comment period, our analysis supports the reassignment for the codes to APC 5313. Specifically, our analysis of the claims data show a geometric mean cost of approximately $1,941 for CPT code 45349 based on 386 single claims (out of 387 total claims), and a geometric mean cost of about $2,039 for CPT code 45390 based on 10,212 single claims (out of 10,246). In both instances, the geometric mean cost for the codes are most compatible with APC 5313, whose geometric mean cost is approximately $2,294, compared to APC 5312, whose geometric mean cost is about $983. We believe that maintaining both codes in APC 5312 would underpay for the procedures. Therefore, we are reassigning the codes from APC 5312 to APC 5313 for CY 2020.
In summary, after consideration of the public comment, we are finalizing our proposal with modification, and revising the APC assignment for 45349 and 45390 from APC 5312 to APC 5313 for CY 2020. Table 22 lists the final SI and APC assignments for the two codes. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
As we do every year, we will reevaluate the APC assignment for CPT codes 45349 and 45390 in the next rulemaking cycle. We remind hospitals that we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on the latest claims data available to us.

8. Coronary Computed Tomographic Angiography (CCTA) (APC 5571)
For CY 2020, we proposed to continue to assign CPT codes 75572, 75573, and 75574 to APC 5571 (Level 1 Imaging with Contrast) with a proposed payment rate of $179.91. The long descriptors and proposed status indicator (SI) and APC assignments for the codes can be found in Table 23 below.
Comment: Many commenters expressed concern with the decreased reimbursement for the codes and stated that the proposed payment rate underestimates the resources necessary to provide the service. They noted this is the third consecutive year of decreased reimbursement for cardiac CT. Some commenters added that the exams described by CPT codes 75572, 75573, and 75574 require more resources than the contrast-enhanced studies in APC 5571 because they require more time, are performed by highly trained technologists, involve higher risk patients, require administration of vasoactive medications, and require close supervision of patients during and after the procedure. A commenter urged CMS to reassign the codes to a higher paying APC that is more resource intensive and includes procedures that share similar clinical characteristics, such as APC 5572 (Level 2 Imaging with Contrast), which had a proposed payment rate of $373.45, or APC 5573 (Level 3 Imaging with Contrast), which had a proposed payment rate of $682.96. Other commenters specifically requested a reassignment to APC 5573 based on clinical and resource homogeneity to these services that are assigned to the APC: Stress cardiac magnetic resonance imaging (CPT code 75563), stress echocardiography (HCPCS codes C8928, C8930), and nuclear SPECT MPI (CPT codes 78451, 78452). One commenter recommended the reassignment of CPT code 75574 to APC 5191 (Level 1 Endovascular Procedures) with a proposed payment rate of $2,899.34 and believed the service is very similar to a cardiac catheterization procedure that is described by CPT code 93455 (Catheter placement in coronary artery(s) for coronary angiography, including intraprocedural injection(s) for coronary angiography, imaging supervision and interpretation; with catheter placement(s) in bypass graft(s) (internal mammary, free arterial, venous grafts) including intraprocedural injection(s) for bypass graft angiography). This same commenter suggested that the less-intensive CPT codes 75572 and 75573 be reassigned to APC 5572.
Response: CPT codes 75572, 75573, and 75574 were effective January 1, 2010, and prior to that they were described by Category III CPT codes from January 1, 2006 through December 31, 2009; therefore, we have many years of claims data associated with these services. For this final rule with comment period, based on claims submitted between January 1, 2018 through December 30, 2018, that were processed on or before June 30, 2019, our analysis of the latest claims data for this final rule supports maintaining CPT codes 75572, 75573, and 75574 in APC 5571. Specifically, our claims data show a geometric mean cost of approximately $159 for CPT code 75572 based on 12,299 single claims (out of 23,902 total claims), $185 for CPT code 75573 based on 323 single claims (out of 466 total claims), and $196 for CPT code 75574 based on 25,434 single claims (out of 40,219 total claims). Because the geometric mean costs for the CCTA codes range are between $159 and $196, we believe it would be inappropriate to reassign the codes to these suggested APCs because their geometric mean costs are significantly higher:
- APC 5572 (with geometric mean cost of about $359)
- APC 5573 (with a geometric mean cost of approximately $660)
- APC 5191 (with a geometric mean cost of about $2,788)
In our analysis to determine the cause of the decreased payment rates for the last several years, we also reviewed our claims data to determine whether changes in payment for certain computed tomography (CT) services impacted the OPPS payment rates. Specifically, section 218(a)(1) of the Protecting Access to Medicare Act of 2014 (PAMA) (Pub. L. 113-93) amended section 1834 of the Act by establishing a new subsection 1834(p). Effective for services furnished on or after January 1, 2016, section 1834(p) of the Act reduces payment for the technical component (TC) of applicable CT services paid under the MPFS and applicable CT services paid under the OPPS, with a 5-percent reduction required in 2016 and a 15-percent reduction required in 2017 and subsequent years. The applicable CT services are identified by HCPCS codes 70450 through 70498; 71250 through 71275; 72125 through 72133; 72191 through 72194; 73200 through 73206; 73700 through 73706; 74150 through 74178; 74261 through 74263; and 75571 through 75574 (and any succeeding codes) for services furnished using equipment that does not meet each of the attributes of the National Electrical Manufacturers Association (NEMA) Standard XR-29-2013, entitled “Standard Attributes on CT Equipment Related to Dose Optimization and Management.”
In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70470), we established a new “CT” modifier to be used on claims that include CT services furnished using equipment that does not meet each of the attributes of NEMA Standard XR-29-2013. Hospitals are required to report the “CT” modifier on claims for CT scans described by any of the HCPCS codes we identified (and any successor codes) that are furnished on non-NEMA Standard XR-29-2013-compliant CT scanners. The use of this modifier results in the applicable payment reduction for the CT service, as specified under section 1834(p) of the Act.
Based on our analysis, we observed declining use of the CT modifier in both billing volume and the number of providers using the modifier over the past several years. Further, we note that the payment reduction required by section 1834(p), as amended by section 218(a)(1) of PAMA, does not directly affect the geometric mean costs under the OPPS, because we do not use payment rates to establish CCRs, rather we use the charges submitted by hospitals on claims and costs estimated through applying the cost report CCRs for modeling purposes. The application of the payment reductions associated with the CT modifier only occurs after the prospective OPPS payments are already calculated.
Comment: Some commenters recommended the establishment of a new cost center specific to CCTA. They noted that hospitals currently do not submit any cost center data for cardiac CT services.
Response: We thank the commenters for their suggestion. CMS is currently reviewing non-standard cost centers used frequently in the Medicare cost report in order to establish additional standardized reporting. We will consider the establishment of a new cost center specific to cardiac CT services in our review.
In summary, after consideration of the public comments and after our analysis of the latest claims data, we are finalizing our proposal, without modification, to assign CPT codes 75572, 75573, and 75574 to APC 5571 for CY 2020. Table 23 lists the final SI and APC assignments for the three codes. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period (which is available via the internet on the CMS website).
As we do every year, we will reevaluate the APC assignment for CPT codes 75572, 75573, and 75574 for the next rulemaking cycle. We remind hospitals that we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on the latest claims data.

9. Deep Brain Stimulation (DBS) Programming (APC 5742)
In CY 2018, the DBS programming codes were described by CPT code 95978 (first 60 minutes), which was assigned to APC 5742, with a payment of $115.18, and CPT code 95979 (each additional 30 minutes), which was assigned to SI “N” to indicate that the code is packaged since it is an add-on code. For CY 2019, the CPT Editorial Panel deleted CPT code 95978 and replaced it with CPT code 95983 (first 15 minutes) effective January 1, 2019. Similarly, CPT code 95979 was deleted and replaced with CPT code 95984 (each additional 15 minutes) effective January 1, 2019. As a result of this coding change, we assigned the 15-minute CPT code 95983 to APC 5741 (Level 1 Electronic Analysis of Devices) with a payment rate of $37.16, and assigned CPT code 95984 to “N” to indicate that the code is packaged because it describes an add-on service, which is similar to the SI for its predecessor code (CPT code 95979). Table 24 below list the long descriptors and proposed SI and APC assignments for CPT codes 95983 and 95984.
At the August 21, 2019 HOP Panel Meeting, a presenter requested that the 15-minute CPT code 95983 be reassigned to APC 5742. The presenter added that the cost of providing the service from 2018 to 2019 has not changed but the reimbursement has reduced the hospital payment by about $100. The presenter requested an APC modification for CPT code 95983 from APC 5741 to APC 5742 so that hospitals receive adequate payment for providing the service. Based on the information presented at the meeting, the HOP Panel recommended a reassignment to APC 5742 for CPT code 95983. Specifically, the Panel recommended that “CMS move HCPCS code 95983, Electronic analysis of implanted neurostimulator pulse generator/transmitter (e.g., contact group[s], interleaving, amplitude, pulse width, frequency [hz], on/off cycling, burst, magnet mode, dose lockout, patient selectable parameters, responsive neurostimulation, detection algorithms, closed loop parameters, and passive parameters) by physician or other qualified health care professional; with brain neurostimulator pulse generator/transmitter programming, first 15 minutes face-to-face time with physician or other qualified health care professional, to APC code 5472, Level II Electronic Analysis of Devices, if the final data that are available in time for consideration of the Final Rule are consistent with preliminary data.”
For CY 2020, we proposed to continue to assign CPT code 95983 to APC 5741 (Level 1 Electronic Analysis of Devices) with a proposed payment rate of $36.81. In addition, we proposed to continue to assign CPT code 95984 to status indicator (SI) “N” to indicate that the code is an add-on that is packaged and payment for it is included in the primary service. In this case, the payment for the add-on code is included in CPT code 95983.
Comment: Several commenters requested the reassignment of CPT code 95983 to APC 5742. One commenter stated that the assignment of the primary CPT code 95983 to the lower level APC 5741 is not appropriate because the overall time and resources expended by a hospital when furnishing this service in the HOPD setting remains the same, even if the units are billed differently. This same commenter indicated that, based on the coding descriptor for the replacement codes with the primary service described as the first 15-minutes and the secondary service as each additional 15-minutes, hospitals will continue to receive a single line-item payment for the service, with the payment for the add-on CPT code packaged into it, regardless of the number of units billed. Another commenter stated that reassigning the code from APC 5741 to APC 5742 will have no effect on the geometric mean cost of either APC. Another commenter requested the reassignment based on the geometric mean cost of approximately $109 for the predecessor code (CPT code 95978) and the Panel's recommendation at the August 19, 2019 HOP Panel Meeting.
Response: As noted above, the predecessor CPT code 95978 described a 60-minute service, while the replacement code—CPT code 95983—describes a 15-minute service. Based on the new time specified in the descriptor for CPT code 95983, we believed that assigning the replacement code to APC 5741 was appropriate. However, at the August 21, 2019 HOP Panel meeting, the presenter indicated that the service of providing DBS programming during 2018 and 2019 are the same, but because of the coding change that packages any service after each additional 15 minutes, the maximum payment that a hospital would receive for the service is a single unit of the code. The presenter recommended a change in the APC assignment to APC 5742 so that hospitals receive adequate payment for the service based on the coding structure of the replacement codes.
As recommended by the HOP Panel, we reviewed the claims data associated with the predecessor code (CPT code 95978). Based on the latest hospital outpatient claims data used for this final rule with comment period, our analysis reveals a geometric mean cost of approximately $109 for the code, which is consistent with the geometric mean cost of about $111 for APC 5742 compared to APC 5741 whose geometric mean cost is about $35. Based on the information presented at the HOP Panel Meeting, the Panel's recommendation, as well as the final rule claims data, we agree with the commenters that APC 5741 may not adequately reflect the resources to provide the service described by CPT code 95983 and are, therefore, modifying the assignment for CPT code 95983 to APC 5742.
In summary, after consideration of the public comments and the presentation at the August 21 HOP Panel Meeting, we are finalizing our proposal, with modification, and revising the APC assignment for CPT code 95983 to APC 5742 for CY 2020. Table 24 list the final SI and APC assignments for CPT code 95983 and 95984. The final CY 2020 payment rate for CPT code 95983 can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
As we do every year, we will reevaluate the APC assignment for CPT code 95983 for the next rulemaking cycle. We remind hospitals that we review, on an annual basis, the APC assignments for all services and items paid under the OPPS.


10. Extracorporeal Shock Wave Lithotripsy (ESWL) (APC 5374)
For the CY 2019 OPPS/ASC final rule, we reviewed all of the procedures assigned to the Urology Procedures APCs, specifically, APCs 5371 through 5377, and made some modifications to more appropriately reflect the resource costs and clinical characteristics of the services within each APC grouping. Specifically, we revised the APC assignment of the procedures assigned to the family of Urology APCs to more appropriately reflect a prospective payment system that is based on payment groupings and not code-specific payment rates, while maintaining clinical and resource homogeneity. As we stated in the CY 2019 OPPS/ASC final rule (83 FR 58900), this modification was based on public comments we received in response to the CY 2019 OPPS/ASC proposed rule on the proposed APC assignments for certain urology procedures.
We received many comments on the APC reassignment for the extracorporeal shock wave lithotripsy (ESWL) procedure, which is described by CPT code 50590 (Lithotripsy, extracorporeal shock wave), in the CY 2019 OPPS/ASC final rule with comment period. The commenters indicated there was no discussion in the preamble on the reassignment of the code from APC 5375 (Level 5 Urology and Related Services) to APC 5374 (Level 4 Urology and Related Services), and they disagreed with the revision and believed that APC 5375 was the more appropriate assignment for the code. We remind the commenters that, as we have stated in every OPPS/ASC proposed and final rules, we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on our analysis of the latest claims data. Based on updated claims data for the final rule for CY 2019, we found that the geometric mean cost of approximately $3,265 for CPT code 50590 did not support its continued assignment to APC 5375, which had a geometric mean cost of about $4,055. We believed that we would have significantly overpaid for the procedure had we maintained the assignment to APC 5375. Consequently, we revised the APC assignment for CPT code 50590 to APC 5374, which had a geometric mean cost of approximately $2,952 for CY 2019.
We note that the SI and APC assignment for CPT code 50590 were subject to comment in the CY 2019 OPPS/ASC proposed rule but not in the CY 2019 OPPS/ASC final rule with comment period. Nevertheless, we received comments on this specific issue in response to the CY 2019 OPPS/ASC final rule with comment period. Because CPT code 50590 was not assigned to comment indicator “NI” in the final rule because it was not a new code for CY 2019, and therefore, the comments received related to this code were out-of-scope. Nonetheless, we discuss above to provide some clarity to this issue.
For CY 2020, as listed in Addendum B to the proposed rule, we proposed to maintain the APC assignment for CPT code 50590 to APC 5374 with a proposed payment rate of $3,059.21.
Comment: Some commenters requested that we restore the code to APC 5375 where it had been placed for several years prior to CY 2019. The commenters indicated that CPT code 50590 is similar to two ureteroscopy with lithotripsy (URSL) procedures that are assigned to APC 5375, specifically:
- CPT code 52353 (Cystourethroscopy, with ureteroscopy and/or pyeloscopy; with lithotripsy (ureteral catheterization is included)); and
- CPT code 52356 (Cystourethroscopy, with ureteroscopy and/or pyeloscopy; with lithotripsy including insertion of indwelling ureteral stent (e.g., gibbons or double-j type)).
In addition, some commenters suggested that placing the three procedures in two separate APCs may create an unintended consequence of unplanned admissions to the hospital. Specifically, the commenters indicated that if the proposed assignment for CPT code 50590 is finalized in APC 5374, while CPT codes 52353 and 52356 are finalized in APC 5375, hospitals might discontinue ESWL services (described by CPT code 50590) which would make it less accessible to Medicare beneficiaries and, ultimately, encourage hospitals to perform more URSL procedures, which, according to the commenter, have higher complication rates compared to ESWL. These commenters asserted that 90 percent of Medicare patients require an indwelling ureteral stent after a URSL procedure (described by CPT codes 52353 and 52356), and that the stents lead to infection, visits to the ER, and unplanned admissions. Hence, the commenters requested an APC reassignment to APC 5375 for CPT code 50590 to eliminate any unintended consequences.
Further, the commenters noted that because of the capital equipment expense associated with purchasing ($500,000) and maintaining ($65,000 per year) a lithotripter, hospitals rarely own their own lithotripter and generally contract under arrangement with suppliers to provide the service. Alternatively, the commenter asserted that all URSL equipment is owned by the hospitals furnishing the service and that the hospitals are therefore able to train clinicians on the equipment.
Response: As discussed above, we revised the APC assignment for CPT code 50590 based on our analysis of the latest claims data for the CY 2019 final rule. For this final rule with comment period, which is based on claims submitted between January 1, 2018 through December 30, 2018, that were processed on or before June 30, 2019, our findings do not support a reassignment to APC 5375. Instead, our analysis supports retaining CPT code 50590 in APC 5374. Specifically, our data reveal a geometric mean cost of approximately $3,247 for CPT code 50590 based on 40,009 single claims (out of 40,351 total claims). The geometric mean cost for APC 5374 is about $2,953 while APC 5375 shows a geometric mean cost of approximately $4,140. Based on the geometric mean cost, we believe that maintaining CPT code in APC 5374 is more appropriate than reassigning it to APC 5375, based on the geometric mean cost of CPT code 50590 relative to that of APCs 5374 and 5375.
In addition, we note that the resource costs associated with the URSL procedures (CPT codes 52353 and 52356) are higher than that of ESWL (CPT code 50590). Specifically, the geometric mean cost for CPT code 50590 for CY 2020 is $3,247 while the geometric mean cost for CPT codes 52353 and 52356 are $3,740 and $4,361, respectively. The geometric mean cost of $3,247 for CPT code 50590 falls within APC 5374, whose geometric mean costs for the significant procedures range between $2,495 (for CPT code 52351) and $3,472 (for CPT code 52318), while the geometric mean costs of $3,740 and $4,361 for CPT codes 52353 and 52356, respectively, fall within APC 5375, whose geometric mean costs for the significant procedures range between $3,575 (for CPT code 52630) and $5,655 (for CPT code 55875). Although all three procedures are used for the treatment of kidney stones, we disagree that CPT codes 50590, 52353, and 52356 are similar based on resource and clinical homogeneity. With regards to unintended consequences as a result of the assignment to APC 5374 for CPT code 50590, we rely on physicians to provide appropriate care based on the needs of their patients. While the payment rate for services assigned to APC 5375 is higher than that of APC 5374, it is based on the relative resources associated with furnishing the services assigned to that APC. While each of the lithotripsy procedures have some clinical similarity, as the commenters pointed out, they have clinical differences. While the commenters expected that these clinical differences may result in similar or higher resources for CPT code 50590 compared to CPT codes 52353 and 52356, that has not been borne out in the Medicare data we have available. As we do every year, we will review the claims data associated with CPT code 50590 to determine its appropriate APC placement for the next rulemaking update.
Comment: Some commenters suggested, based on their analysis of the OPPS Limited Data Sets (LDS) for the CY 2018 OPPS/ASC final rule, the CY 2019 OPPS/ASC final rule, and the CY 2020 OPPS/ASC proposed rule, that the methodology formula that was supplied with the LDS materials was flawed and, therefore, they were unable to validate CMS's calculation or the accuracy of the cost data upon which CMS relied to determine the payment rates. In addition, these same commenters suggested that because hospitals do not generally own lithotripters, they would not be surprised if the cost reports for CPT code 50590 were inaccurate.
Response: It is generally not our policy to judge the accuracy of hospital coding and charging for purposes of ratesetting. We rely on hospitals to accurately report the use of HCPCS codes in accordance with their code descriptors and CPT and CMS instructions, and to report services on claims and charges and costs for the services on their Medicare hospital cost report appropriately. We do not specify the methodologies that hospitals use to set charges for this or any other service. In addition, we state in Chapter 4 of the Medicare Claims Processing Manual that “it is extremely important that hospitals report all HCPCS codes consistent with their descriptors; CPT and/or CMS instructions and correct coding principles, and all charges for all services they furnish, whether payment for the services is made separately paid or is packaged” to enable CMS to establish future ratesetting for OPPS services.
Comment: To pay appropriately for CPT code 50590, some commenters suggested adding the cost of a ureteral stent in calculating the geometric mean cost since some procedures (less than 20 percent) require the device. They noted that the URSL procedure described by CPT code 52356 requires the insertion of a ureteral stent that costs $609.16.
Response: Geometric mean costs are determined based on the costs reported on the claim. If the CPT code descriptor describes the insertion of a device, we would expect the device cost to be packaged into the cost of the procedure since the charges associated with the device and its insertion should be reflected in claims submitted to Medicare. We note that the CPT code descriptor for the URSL procedures (CPT codes 52353 and 52356) describes the use of stents, consequently, the geometric mean cost for the procedures include the packaged cost of the devices. However, the CPT code descriptor for the ESWL procedure does not describe the use of a ureteral stent, so we disagree that device costs for a ureteral stent should be included in CPT code 50590. If a ureteral stent were involved in an ESWL procedure, HOPDs should report the CPT code that appropriately describes the procedure performed. Moreover, as we have stated previously, we rely on HOPDs to accurately report all HCPCS codes consistent with their descriptors; CPT and/or CMS instructions and correct coding principles, and all charges for all services they furnish, whether payment for the services is made separately paid or is packaged.
In summary, after consideration of the public comments and after our analysis of the updated claims data for this final rule with comment period, we are finalizing our proposal, without modification, to continue to assign CPT code 50590 to APC 5374 for CY 2020. The final CY 2020 payment rate for the code can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
As always, we will reevaluate the APC assignment for CPT code 50590 for the next rulemaking cycle. As stated above, we review, on an annual basis, the APC assignments for all services and items paid under the OPPS.
11. Extravascular Implantable Cardioverter Defibrillator (EV ICD)
As displayed in Table 25 and in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign CPT codes 0571T through 0580T to status indicator (SI) “E1” to indicate that the codes are not payable by Medicare when submitted on outpatient claims (any outpatient bill type) because the services associated with these codes are either not covered by any Medicare outpatient benefit category, are statutorily excluded from Medicare payment, or are not reasonable and necessary. The codes were listed as 06X0T through and 07X4T (the 5-digit CMS placeholder codes) in Addendum B with the short descriptors, and again in Addendum O with the long descriptors. We also assigned the codes to comment indicator “NP” in Addendum B to indicate that they are new for CY 2020 and that public comments would be accepted on their proposed status indicator assignments. We note that these codes will be effective January 1, 2020.
Comment: A commenter reported that the device associated with these codes is in a clinical trial and also received FDA approval with an IDE Category B designation. The commenter added that they are currently in the process of applying for Medicare national coverage for the clinical trial as a Category B IDE study. The commenter requested that we crosswalk the new codes to the SIs and APC assignments of comparable procedures involving ICD placement so that appropriate hospital outpatient payment may be made in the event the Category B IDE study is approved for Medicare coverage. The commenter listed the comparable codes with the SI and APCs assignments.
Response: Based on our review, the clinical trial has not met Medicare's standards for coverage, nor does it appear on the CMS Approved IDE List, which can be found at this CMS website: https://www.cms.gov/Medicare/Coverage/IDE/Approved-IDE-Studies.html. Because the clinical trial associated with these codes has not been approved for Medicare coverage, we believe we should continue to assign CPT codes 0571T through 0580T to status indicator “E1” for CY 2020. If Medicare approves the clinical trial as a Category B IDE study, we will reassess the SI and APC assignments for the codes.
Therefore, after consideration of the public comment received, we are finalizing our proposal without modification for CPT codes 0571T through 0580T. The final status indicator assignments for both codes are listed in Table 25 below. We refer readers to Addendum D1 of this final rule with comment period for the complete list of the OPPS payment status indicators and their definitions for CY 2020. Addendum D1 is available via the internet on the CMS website.


12. Genicular and Sacroiliac Joint Nerve Injections/Procedures (APCs 5442 and 5431)
For CY 2020, the CPT Editorial Panel established four new codes to describe genicular and sacroiliac joint nerve injections and procedures. As listed in Table 26 below with the long descriptors, and also in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign CPT codes 64451 and 64454 to APC 5442 (Level 2 Nerve Injections) with a proposed payment rate of $627.39. We note both CPT codes 64451 and 64454 describe therapeutic and/or diagnostic injection procedures. We also proposed to assign CPT code 64624 to APC 5443 (Level 3 Nerve Injections) with a proposed payment rate of $808.58. In addition, we proposed to assign CPT code 64625 to APC 5431 (Level 1 Nerve Procedures) with a proposed payment rate of $1,747.26. CPT codes 64451, 64454, 64624, and 64625 were listed as 6XX00, 64XX0, 64XX1, and 6XX01 (the 5-digit CMS placeholder codes), respectively, in Addendum B with the short descriptors, and again in Addendum O with the long descriptors. We also assigned these codes to comment indicator “NP” in Addendum B to indicate that the codes are new for CY 2020 and that public comments would be accepted on their proposed status indicator assignments. We note that these codes will be effective January 1, 2020.
Comment: Several commenters disagreed with the APC assignment for CPT code 64624 (shown in the proposed rule with placeholder code 64XX1) and suggested that it would be more appropriate, based on clinical homogeneity, to assign it to APC 5431, where similar radiofrequency ablation procedures are assigned, specifically, CPT codes 64633 (Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or ct); cervical or thoracic, single facet joint), 64635 (Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or ct); lumbar or sacral, single facet joint), and new CPT code 64625. Several commenters reported that, unlike CPT code 64640 (Destruction by neurolytic agent; other peripheral nerve or branch) which only involves one nerve, the procedure described by CPT code 64624 requires more expensive medical equipment and supplies and involves the destruction of three nerves. Most commenters agreed that the procedure is not a nerve injection. One commenter explained that the procedure describes the destruction of three nerve branches at three locations in the knee, and the destruction is typically done via radiofrequency ablation similar to those procedures described by CPT codes 64633 and 64635 that are assigned to APC 5431. Another commenter suggested that reassigning CPT code 64624 to APC 5431, similar to new CPT code 64625, would provide adequate reimbursement for the procedure and enable providers to offer patients with chronic knee pain an effective alternative to systemic opioids.
Response: After consideration of the public comments, and based on the characteristics of the procedure, as well as input from our medical advisors, we believe that it would be appropriate to revise the APC assignment for CPT code 64624 from APC 5443 to APC 5431. We agree with the commenters that this new procedure shares similar characteristics with CPT codes 64633 and 64635 that are assigned to APC 5431.
Comment: A commenter agreed with the proposed APC assignments for CPT codes 64451, 64454, and 64425.
Response: We thank the commenter for their feedback and are finalizing the APC assignments for these codes.
In summary, after consideration of the public comments, we are finalizing our proposal with modification. Specifically, we are finalizing the APC assignments for CPT codes 64451, 64454, and 64425 to the APCs listed in Table 26. In addition, we are revising the APC assignment for CPT code 64624 from APC 5443 to APC 5431. Table 26 lists the long descriptors for the codes, as well as the final APC and SI assignments for all four codes. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
As always, we will reevaluate the APC assignment for these codes once we have claims data. We review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on the latest claims data that we have available.

13. FemBloc® and FemChec®
For CY 2020, the CPT Editorial Panel established two new codes to describe FemBloc (0567T) and FemChec (0568T). As listed in Table 27 with the long descriptors, and in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign CPT code 0567T to APC 5414 (Level 4 Gynecologic Procedures) and status indicator (SI) “J1” (Hospital Part B services paid through a comprehensive APC) with a payment rate of $2,564.60. In addition, we proposed to assign new CPT code 0568T to APC 5732 (Level 2 Minor Procedures) and status indicator “Q1” (conditionally packaged) with a payment rate of $34.33. The codes were listed as 05X1T and 05X2T (the 5-digit CMS placeholder codes), respectively, in Addendum B with the short descriptors, and again in Addendum O with the long descriptors. We also assigned these codes to comment indicator “NP” in Addendum B to indicate that the codes are new for CY 2020 and that public comments would be accepted on their proposed status indicator assignments. We note these codes will be effective January 1, 2020.
Comment: A medical technology company disagreed with the proposed APC assignment for CPT code 0567T and suggested that we reassign the procedure code from APC 5414 to APC 5415 (Level 5 Gynecologic Procedures) with a proposed payment rate of $4,426.45. The commenter noted that the single-use, disposable device associated with the code contains two deployable and retractable balloon catheters and a biopolymer that retails for $1,800. The commenter believes the procedure more appropriately fits in APC 5415 based on its similarity to CPT code 58565 (Hysteroscopy, surgical; with bilateral fallopian tube cannulation to induce occlusion by placement of permanent implants). Specifically, the commenter explained that in both procedures, specifically CPT codes 58565 and 0567T, the entrances to the fallopian tubes are accessed and a device is placed that causes permanent occlusion of the tubes.
Response: Based on our findings associated with FemBloc, the procedure is currently in clinical trial with an estimated study completion date of September 2022 (ClinicalTrials.gov Identifier: NCT03067272). Because the FemBloc device has not received FDA approval, we believe that we should reassign CPT code 0567T to status indicator “E1” to indicate that the code is not payable by Medicare when submitted on outpatient claims (any outpatient bill type). If FDA approves the device, we will reassess the code and determine the appropriate SI and APC assignments.
Comment: The same commenter for FemBloc also requested an APC modification for the code associated with FemChec. Specifically, the commenter requested the reassignment for CPT code 0568T from APC 5732 (Level 2 Minor Procedures) to APC 5523 (Level 3 Imaging without Contrast) with a proposed payment rate of $231.28. The commenter reported that the code is more clinically related to one of the procedures assigned to APC 5523, specifically, CPT code 76831 (Saline infusion sonohysterography (sis), including color flow doppler, when performed). Both CPT codes 0568T and 76831 require ultrasound and saline to study the uterus.
Response: Our findings reveal that the clinical study associated with FemBloc also applies to FemChec. Based on the clinical study (ClinicalTrials.gov Identifier: NCT03067272), FemChec will be used with FemBloc. Because the FemBloc device has not received FDA approval, we believe that we should reassign CPT code 0568T to status indicator “E1” to indicate that the code is not payable by Medicare when submitted on outpatient claims (any outpatient bill type). If FDA approves FemBloc, we will reassess the code associated with FemChec and determine the appropriate OPPS SI and APC assignments for CPT code 0568T.
Therefore, after consideration of the public comments, we are revising the SI and APC assignments for CPT codes 0567T and 0568T. The final status indicator assignments for both codes are listed in Table 27 below. We refer readers to Addendum D1 of this final rule with comment period for the complete list of the OPPS payment status indicators and their definitions for CY 2020. Addendum D1 is available via the internet on the CMS website.

14. Hemodialysis Arteriovenous Fistula (AVF) Procedures (APC 5194)
For CY 2019, based on two new technology applications received by CMS for hemodialysis arteriovenous fistula creation, CMS established two new HCPCS codes to describe the procedures. Specifically, CMS established HCPCS code C9754 for the Ellipsys® System and C9755 for the WavelinQTM System effective January 1, 2019. Both HCPCS codes were assigned to APC 5193 (Level 3 Endovascular Procedures) with a payment rate of 9,669.04 for CY 2019.
At the August 21, 2019 HOP Panel Meeting, a presenter requested that we reassign the WavelinQ procedure to APC 5194. The presenter indicated that the APC payment associated with HCPCS code C9755 is inadequate to cover the cost of the procedure. According to the presenter, the conservative cost estimate for the procedure is over $12,500. The presenter also reported that their HOPD facility performed 35 procedures between October 2018 to July 31, 2019, and the average payment for each procedure ranged between $3,410 and $11,247. Based on the information presented at the meeting, the HOP Panel made no recommendation to CMS on the APC assignment for the WavelinQ procedure.
For CY 2020, as listed in Table 28 below with the long descriptors and proposed SI and APC assignments, we proposed to continue to assign HCPCS codes C9754 and C9755 to APC 5193 with a proposed payment rate of $10,013.25. We received several comments related to this proposal. Below are the comments and our responses.
Comment: Several physicians stated that the current payment rate does not cover the cost of the procedure and requested the reassignment of both HCPCS code C9754 and C9755 to APC 5194 (Level 4 Endovascular Procedures) with a proposed payment rate of $16,049.73. A physician association explained that the new technologies describe innovative new procedures that increase options for dialysis patients to have a successful arteriovenous fistula for dialysis access, and that the procedures are important in making fistula access possible for patients that either refuse open surgery or where skilled surgeons are not readily available. However, they expressed concern that the procedures may not be available to patients if the costs are higher than the payment, and requested that CMS carefully examine the most recent claims to determine if they should be reclassified to APC 5194.
Response: After consideration of the public comments received and based on input from our medical advisors, as well as our review of the latest claims data available to us, we believe that we should revise the APC assignment for HCPCS code C9754 and C9755 to APC 5194 for CY 2020.
Comment: A medical device company requested an APC reassignment based on data presented at the August 21, 2019 HOP Panel Meeting. They indicated that their analysis of the 1Q2019 Medicare Limited Data Set (LDS) Standard Analytic File (SAF) for HCPCS code C9755 showed a geometric mean cost of $12,960, and suggested reassigning the code to APC 5194. They also reminded CMS that the reassignment to APC 5194 is in line with various HHS initiatives, such as the HHS Initiative on “Advancing American Kidney Health” since the payment rate for the procedure would improve access to the service.
Response: As stated above, we believe that it is appropriate to revise the APC assignment for HCPCS code C9754 and C9755. Consequently, we are reassigning both codes from APC 5193 to APC 5194 for CY 2020.
Comment: A commenter representing 13 different health systems suggested that CMS adopt the recommendation they made at the August 21, 2019 HOP Panel Meeting. Specifically, they recommended the reassignment of HCPCS code C9755 from APC 5193 to APC 5194.
Response: Although there was a presentation at the August 21, 2019 meeting on HCPCS code C9755 with a request to reassign the code to APC 5194, the HOP Panel made no recommendation to CMS. We note that the August 21, 2019, HOP Panel recommendations are posted online and can be found on this CMS website: https://www.cms.gov/Regulations-and-Guidance/Guidance/FACA/AdvisoryPanelonAmbulatoryPaymentClassificationGroups.html. Although the HOP Panel made no recommendation to CMS, based on the proposed rule comments, and our review of the issue, we are revising the APC assignment for HCPCS code C9755 to APC 5194 for CY 2020.
Comment: A commenter stated that it was brought to their attention that other comments related to the WavelinQ procedure may urge CMS to revisit the APC assignment for HCPCS code C9755. The commenter indicated that if CMS were to revisit the issue and reassign the APC assignment for the WavelinQ procedure, it should also apply the same consideration to the Ellipsys procedure (C9754).
Response: We agree that the services described by HCPCS codes C9754 and C9755 are clinically similar and, therefore, we are revising the APC assignment for both HCPCS code C9754 and C9755 to APC 5194 for CY 2020. However, we note that claims data upon which we could determine the geometric mean costs associated with each procedure are not yet available for ratesetting but once such data become available, we will be able to determine whether the two services are similar in terms of resources. In addition, as has been our practice since the implementation of the OPPS in 2000, we review, on an annual basis, the APC assignments for the procedures and services paid under the OPPS. Consequently, we will review the cost data associated with HCPCS codes C9754 and C9755 for the next annual rulemaking.
In summary, after consideration of the public comments, we are finalizing our proposal with modification. Specifically, we are reassigning HCPCS codes C9754 and C9755 from APC 5193 to APC 5194 for CY 2020. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website. Table 28 lists the final SI and APC assignments for HCPCS codes C9754 and C9755.

15. Hemodialysis Duplex Studies (APCs 5522 and 5523)
For CY 2020, the CPT Editorial Panel established two new codes to describe hemodialysis duplex studies, specifically, CPT codes 93985 and 93986. The new codes replace HCPCS code G0365 (Vessel mapping of vessels for hemodialysis access (services for preoperative vessel mapping prior to creation of hemodialysis access using an autogenous hemodialysis conduit, including arterial inflow and venous outflow)). HCPCS code G0365 was assigned to status indicator “D” in the proposed rule to indicate that the code would be deleted on December 31, 2019.
As listed in Table 29 below with the long descriptors, and also in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign CPT code 93985 and 93986 to APC 5522 (Level 2 Imaging without Contrast) with a proposed payment rate of $111.04. The codes were listed as 93X00 and 93X01 (the 5-digit CMS placeholder codes), respectively, in Addendum B with the short descriptors, and again in Addendum O with the long descriptors. We also assigned these codes to comment indicator “NP” in Addendum B to indicate that the codes are new for CY 2020 and that public comments would be accepted on their proposed status indicator assignments. We note that these codes will be effective January 1, 2020.
Comment: Several commenters recommended a reassignment of CPT code 93985 from APC 5522 to APC 5523 (Level 3 Imaging without Contrast) with a proposed payment rate of $231.28. They indicated that the code represents a bilateral study, and as such, should be assigned to APC 5523 with similar bilateral/complete duplex studies.
Response: Based on the public comments that we received, our review of the procedure associated with CPT code 93985 and advice from our medical advisors, we agree that the code fits more appropriately in APC 5523 based on its clinical homogeneity and resource use to the other procedures in the APC. Therefore, we are reassigning the code to APC 5523. We received no comments on CPT code 93986. Consequently, we are finalizing its APC assignment to APC 5522.
In summary, after consideration of the public comments, we are finalizing our proposal with modification. Specifically, we are finalizing our proposal for CPT code 93986 to APC 5522, and reassigning CPT code 93985 to APC 5523. Table 29 below lists the long descriptors for the three codes and the final SI and APC assignments for CY 2020. The final CY 2020 OPPS payment rates can be found in Addendum B of this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator meanings for all codes reported under the OPPS for CY 2020. Both Addendum B and Addendum D1 are available via the internet on the CMS website.
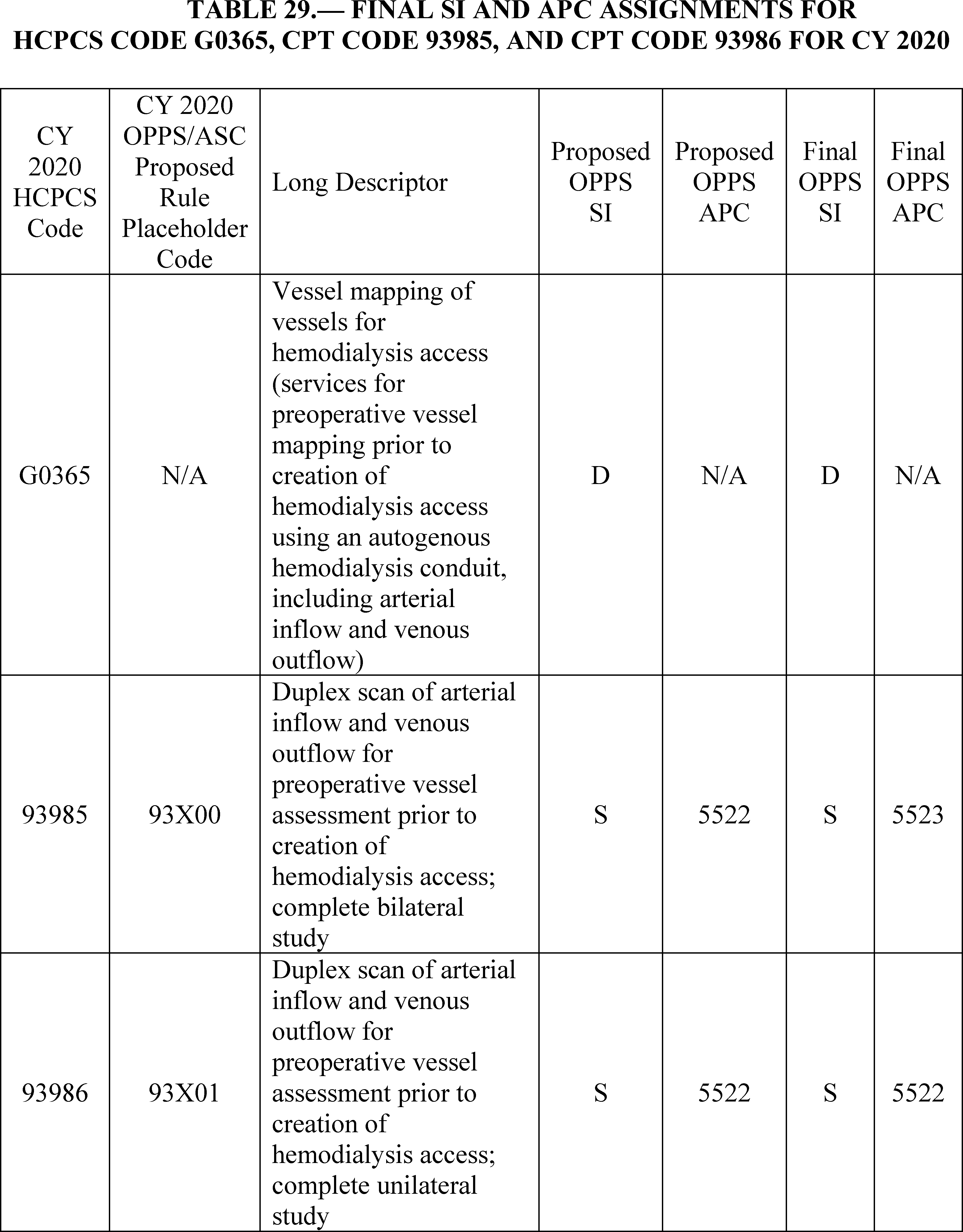
16. Intraocular Procedures (APCs 5491 Through 5494)
In prior years, CPT code 0308T (Insertion of ocular telescope prosthesis including removal of crystalline lens or intraocular lens prosthesis) was assigned to the APC 5495 (Level 5 Intraocular Procedures) based on its estimated costs. In addition, its relative payment weight has been based on its median cost under our payment policy for low-volume device-intensive procedures because the APC contained a low volume of claims. The low-volume device-intensive procedures payment policy is discussed in more detail in section III.C.2. of the proposed rule.
In the CY 2019 OPPS/ASC proposed rule, we proposed to reassign CPT code 0308T from APC 5495 to APC 5493 (Level 3 Intraocular Procedures), based on the data for two claims available for ratesetting for the proposed rule, and to delete APC 5495 (83 FR 37096 through 37097). However in the CY 2019 OPPS/ASC final rule with comment period, based on updated data on a single claim available for ratesetting for the final rule, we modified our proposal and reassigned procedure code CPT code 0308T to the APC 5494 (Level 4 Intraocular Procedures) (83 FR 58917 through 58918). We made this change based on the similarity of the estimated cost for the single claim of $12,939.75 to that of the APC ($11,427.14). However, this created a discrepancy in payments between the OPPS setting and the ASC setting in which the ASC payments would be higher than the OPPS payments for the same service because of the intersection of the estimated cost for the encounter determined under a comprehensive methodology within the OPPS and the estimated cost determined under the payment methodology for device-intensive services within the ASC payment system.
In reviewing the claims data available for the proposed rule for CY 2020 OPPS ratesetting, we found several claims reporting the procedure described by CPT code 0308T. Based on the claims data, the procedure would have a geometric mean cost of $28,122.51 and a median cost of $19,864.38. These cost statistics are significantly higher than the geometric mean cost of the other procedure assigned to APC 5494, that is, the procedure described by CPT code 67027 (Implant eye drug system), which has a geometric mean cost of $12,296.27. In addition, if we continued to assign the procedure described by CPT code 0308T to APC 5494 (the Level 4 Intraocular Procedures APC), the discrepancy between payments within the OPPS and the ASC payment system would also continue to exist. As a result, we proposed to reestablish APC 5495 (Level 5 Intraocular Procedures) because we believe that the procedure described by CPT code 0308T would be most appropriately placed in this APC based on its estimated cost. Assignment of the procedure to the Level 5 Intraocular Procedures APC is consistent with its historical placement and would also address the large discrepancy in payment for the procedure between the OPPS and the ASC payment system. We note that, based on data available for the proposed rule, the proposed payment rate for this procedure when performed in an ASC, as discussed in more detail in section XIII.D.1.c. of the proposed rule, would be no higher than the OPPS payment rate for this procedure when performed in the hospital outpatient setting. We will continue to monitor the volume of claims data available for the procedure for ratesetting purposes.
Therefore, for CY 2020, we proposed to reestablish APC 5495 (Level 5 Intraocular Procedures) and reassign the procedure described by CPT code 0308T from APC 5494 to APC 5495. Under this proposal, the proposed CY 2020 OPPS payment rate for the service would be established based on its median cost, as discussed in section V.A.5. of the proposed rule, because it is a device-intensive procedure assigned to an APC with fewer than 100 total annual claims within the APC.
Comment: Several commenters expressed support for our proposal to assign the HCPCS code 0308T to APC 5495 (Level 5 Intracoular Procedures).
Response: We thank commenters for their support.
After consideration of the public comments we received, we are finalizing our proposal, without modification, to assign HCPCS code CPT 0308T to APC 5495 for the CY 2020 OPPS.
17. Long-Term Electroencephalogram (EEG) Monitoring Services (APCs 5722, 5723, and 5724)
For CY 2020, the CPT Editorial Panel deleted four existing long-term EEG monitoring services, specifically, CPT codes 95950, 95951, 95953, and 95956, and replaced them with 23 new CPT codes that consisted of 10 professional component (PC) codes and 13 technical component (TC) codes. As listed in Table 30 below with the long descriptors, and also in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign the 13 technical component codes, specifically, CPT codes 95700 through 95716, to either APC 5722 (Level 2 Diagnostic Tests and Related Services) with a proposed payment rate of $256.60 or APC 5723 (Level 3 Diagnostic Tests and Related Services) with a proposed payment rate of $486.65. The codes were listed as 95X01 through and 95X13 (the 5-digit CMS placeholder codes) in Addendum B with the short descriptors, and again in Addendum O with the long descriptors. In addition, we proposed to assign the 10 professional component codes, specifically, CPT codes 95717 through 95726, to status indicator “M” to indicate that the services are not paid under the OPPS since they describe physician services. These codes were listed were listed as 95X14 through 95X23 (the 5-digit CMS placeholder codes) in Addendum B with the short descriptors, and again in Addendum O with the long descriptors. We assigned these 23 codes to comment indicator “NP” in Addendum B to indicate that the codes are new for CY 2020 and that public comments would be accepted on their proposed status indicator assignments. We note these codes will be effective January 1, 2020.
Comment: Many commenters expressed concern with the proposed APC assignments for CPT codes 95712, 95713, 95715, and 95716 and stated that the proposed payment rates for the codes do not provide adequate reimbursement. A commenter indicated that the proposed APC assignments for the EEG monitoring services for 2 to 12 hours does not appropriately reflect the resources and time required to monitor complex epilepsy patients. Several other commenters recommended the reassignment of CPT codes 95712 and 95713 to APC 5723 and stated they should be paid approximately half the rate of the 24-hour video EEG services. These same commenters stated that the reassignment of CPT codes 95715 and 95716 to APC 5724, which had a proposed payment rate of $920.66, would be appropriate since patients being tested may be classified as observation stays and will not be admitted to the hospital. The commenters added that these codes were previously described by predecessor CPT code 95951 (24 hour VEEG), which was assigned to APC 5724 (Level 4 Diagnostic Tests and Related Services).
Response: With respect to CPT codes 95712 (2-12 hours VEEG with intermittent monitoring) and 95713 (2-12 hours VEEG with continuous monitoring), we believe that the resources and time associated with intermittent monitoring (CPT code 95712) are less than that of continuous monitoring (CPT code 95713), and therefore, believe they should be assigned to different APCs. Based on input from our medical advisors that intermittent monitoring involves checking the patient every two hours rather than the full 12 hours, we believe it would be appropriate to modify the APC assignment for the continuous monitoring code (CPT code 95713) to APC 5723. Applying this same concept to the 12-24 VEEG technical component codes, we believe that the resources associated with the intermittent monitoring code (CPT code 95715) are not the same as the continuous monitoring code (CPT code 95716). Therefore, we are reassigning the APC assignment for CPT code 95716 to APC 5724. Although the commenters indicated that the predecessor code for 95715 and 95716 was CPT code 95951, we are uncertain whether the predecessor code describes continuous or intermittent monitoring since the code descriptor lacks this specificity.
Comment: Some commenters urged CMS not to finalize the policies proposed in the PFS or OPPS proposed rules. They indicated that the policies would dramatically reduce reimbursement for EEG and VEEG services and instead, suggested that we appropriately value these services so that people with epilepsy have access and can be diagnosed and treated in a timely manner.
Response: We believe these commenters did not fully understand our APC proposal. Because the existing EEG and VEEG CPT codes will be deleted on December 31, 2019, if we do not finalize our proposal for the 13 technical codes that will be effective January 1, 2020, there would be no codes to report the services associated with EEG and VEEG.
In summary, after consideration of the public comments, we are finalizing our proposal, with modification. Specifically, we are finalizing our proposal to assign CPT codes 95700 through 95712, 95714, and 95715 to the APCs listed in Table 30 below. In addition, we are modifying our proposal for CPT codes 95713 and 95716, and revising their APC assignments to APC 5723 and APC 5724, respectively. Further, we are finalizing our proposal to assign CPT codes 95717 through 95726 to status indicator “M”. These codes, along with the deleted codes, are listed in Table 30. The final CY 2020 payment rate for these codes can be found in Addendum B to this final rule with comment period (which is available via the internet on the CMS website).
As always, we will reevaluate the APC assignment for these codes once we have claims data. We review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on the latest claims data that we have available.


18. Musculoskeletal Procedures (APCs 5111 Through 5116)
Prior to the CY 2016 OPPS, payment for musculoskeletal procedures was primarily divided according to anatomy and the type of musculoskeletal procedure. As part of the CY 2016 reorganization to better structure the OPPS payments towards prospective payment packages, we consolidated those individual APCs so that they became a general Musculoskeletal APC series (80 FR 70397 through 70398).
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59300), we continued to apply a six-level structure for the Musculoskeletal APCs because doing so provided an appropriate distinction for resource costs at each level and provided clinical homogeneity. However, we indicated that we would continue to review the structure of these APCs to determine whether additional granularity would be necessary.
In the CY 2019 OPPS proposed rule (83 FR 37096), we recognized that commenters had previously expressed concerns regarding the granularity of the current APC levels and, therefore, requested comment on the establishment of additional levels. Specifically, we solicited comments on the creation of a new APC level between the current Level 5 and Level 6 within the Musculoskeletal APC series. While some commenters provided suggested APC reconfigurations and requests for change to APC assignments, many commenters requested that we maintain the current six-level structure and continue to monitor the claims data as they become available. Therefore, in the CY 2019 OPPS/ASC final rule with comment period, we maintained the six-level APC structure for the Musculoskeletal Procedures APCs (83 FR 58920 through 58921).
Based on the claims data available for the CY 2020 OPPS/ASC proposed rule, we continue to believe that the six-level APC structure for the Musculoskeletal Procedures APC series is appropriate. Therefore, we proposed to maintain the APC structure for the CY 2020 OPPS update.
We note that this is the first year for which claims data are available for the total knee arthroplasty procedure described by CPT code 27447, which was removed from the inpatient only list in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59382 through 59385). Based on approximately 60,000 hospital outpatient claims reporting the procedure that were available for ratesetting in the proposed rule, the geometric mean cost was approximately $12,472.05, which is similar to the geometric mean cost for APC 5115 (Level 5 Musculoskeletal Procedures) of $11,879.66, and within a range of the lowest geometric mean cost of the significant procedure costs of $9,969.37 and the highest geometric mean cost of the significant procedure costs of $12,894.18. Therefore, we believed that the assignment of the procedure described by CPT code 27447 in the Level 5 Musculoskeletal Procedures APC series remains appropriate and, therefore, we proposed to continue to assign CPT code 27447 to APC 5115 (Level 5 Musculoskeletal Procedures) for CY 2020.
We also proposed to remove the procedure described by CPT code 27130 (Total hip arthroplasty) from the CY 2020 OPPS inpatient only list. Based on the estimated costs derived from in the available claims data, as well as the 50th percentile IPPS payment for TKA/THA procedures without major complications or comorbidities (MS-DRG 470) of approximately $11,900 for FY 2020 when the procedure is performed on an inpatient basis, we believed that it was appropriate to assign the procedure described by CPT code 27130 to the Level 5 Musculoskeletal Procedures APC series, which had a geometric mean cost of $11,879.66. Therefore, for CY 2020, we also proposed to assign the procedure described by CPT code 27130 to APC 5115. We noted that we will monitor the claims data reflecting these procedures as they become available. For a more detailed discussion of the procedures that were proposed to be removed from the inpatient only (IPO) list for CY 2020 under the OPPS, we refer readers to section IX. of the proposed rule.
Table 31 displays the CY 2020 Musculoskeletal Procedures APC series' structure and APC geometric mean costs.

Comment: Several commenters requested that CMS reconsider the proposal to assign CPT code 22869 (Insertion of interlaminar/interspinous process stabilization/distraction device, without open decompression or fusion, including image guidance when performed, lumbar; single level) to APC 5115, and instead allow the code to remain in APC 5116, where it has been historically placed. They believed that the proposal to move the APC was based on inaccurate data, due to one hospital incorrectly reporting its costs and charges. They noted that the influence of that inaccurate data would be short term and that the claims would eventually support the higher placement, as the reporting issues were corrected. We also note that the HOP Panel made a recommendation that CMS examine the claims data for CPT code 22869 and determine an appropriate APC placement.
Response: While we recognize the concerns that the commenters have described, it is generally not our policy to judge the accuracy of hospital coding and charging for purposes of ratesetting. We rely on hospitals to accurately report the use of HCPCS codes in accordance with their code descriptors and CPT and CMS instructions, and to report services on claims and charges and costs for the services on their Medicare hospital cost report appropriately. However, we do not specify the methodologies that hospitals use to set charges for this or any other service. In addition, we state in Chapter 4 of the Medicare Claims Processing Manual that “it is extremely important that hospitals report all HCPCS codes consistent with their descriptors; CPT and/or CMS instructions and correct coding principles, and all charges for all services they furnish, whether payment for the services is made separately paid or is packaged” to enable CMS to establish future ratesetting for OPPS services.
After consideration of the public comments we received, we are finalizing the proposed six level Musculoskeletal Procedures APC structure. We also are finalizing the proposed assignment of the procedure described by CPT codes 22869 to APC 5115. As discussed in section IX. of this final rule, we are also finalizing the proposal to remove the procedure described by CPT code 27130 from the inpatient only list and to assign it to APC 5115 for the CY 2020 OPPS.
19. Nuclear Medicine Services
a. Cardiac Positron Emission Tomography (PET) Studies (APCs 5593 and 5594)
For CY 2020, we proposed to continue to assign CPT code 78459 (Myocardial imaging, positron emission tomography (pet), metabolic evaluation) to APC 5593 (Level 3 Nuclear Medicine and Related Services) with a proposed payment rate of $1,293.33. Similarly, we proposed to maintain the APC assignments for CPT codes 78491 (Myocardial imaging, positron emission tomography (pet), perfusion; single study at rest or stress) and 78492 (Myocardial imaging, positron emission tomography (pet), perfusion; multiple studies at rest and/or stress) to APC 5594 (Level 4 Nuclear Medicine and Related Services) with a proposed payment rate of $1,466.16.
Comment: Commenters agreed with the APC assignments for CPT codes 78459, 78491, and 78492 and stated they are placed appropriately in APCs 5593 and 5594. Some commenters added that the cost associated with CPT code 78492, which describes a wall motion and ejection fraction, supports its maintenance in APC 5594.
Response: We thank the commenters for their feedback and will finalize the APC assignments for CPT code 78459 to APC 5593, and for CPT codes 78491 and 78492 to APC 5594.
b. Cardiac Positron Emission Tomography (PET)/Computed Tomography (CT) Studies (APCs 1522, 1523, and 5594)
For CY 2020, the CPT Editorial established six new codes to describe the services associated with cardiac PET/CT studies, specifically, CPT codes 78429, 78430, 78431, 78432, 78433, and 78434. These codes were listed in Addendum B to the CY 2020 OPPS/ASC proposed rule as 78X29, 78X31, 78X32, 78X33, 78X34, and 78X35 (the 5-digit CMS placeholder codes), respectively, in Addendum B with the short descriptors, and again in Addendum O with the long descriptors. We also assigned these codes to comment indicator “NP” in Addendum B to indicate that the codes are new for CY 2020 and that public comments would be accepted on their proposed status indicator assignments. We note that these codes will be effective January 1, 2020. Table 32 below list the placeholder codes, long descriptors, and proposed SI and APC assignments.
Comment: Several commenters opposed the APC assignment for CPT code 78429 (placeholder code 78X29) and recommended its reassignment from APC 5593 to APC 5594. They stated that APC 5593 does not recognize the additional cost associated with the CT scan that is included in the service, and requested revising the code to APC 5594.
Response: Based on the commenters' feedback and our review of the components of this new service, we agree with the commenters that APC 5594 is the more appropriate assignment for CPT code 78429. Therefore, we will reassign CPT code 78429 from APC 5593 to APC 5594.
Comment: Several commenters agreed with the APC placement for CPT code 78430 (placeholder code 78X31) in APC 5594. They stated that APC 5594 allows adequate payment for the CT scanner that that is a component of this service.
Response: We thank the commenters for their feedback and are finalizing the APC assignment for CPT code 78430 to APC 5594.
Comment: Several commenters reported that certain societies submitted a new technology application to CMS for CPT codes 78431 (placeholder code 78X32), 78432 (placeholder code 78X33), and 78433 (placeholder code 78X34) that details the costs associated with providing the services. For CPT code 78431, these same commenters disagreed with the proposed APC placement and recommended its revision from APC 5594 (Level 4 Nuclear Medicine and Related Services) with a proposed payment rate of $1,466.16 to APC 1522 (New Technology—Level 23 ($2501-$3000)) with a proposed payment rate of $2,750.50. They reported that, based on the resource cost of the service described by CPT code 78431, APC 1522 provides adequate reimbursement for the service. Similarly, for CPT codes 78432 and 78433, the commenters indicated that APC 5594 would not adequately reimburse the resource costs associated with providing these services, and recommended their reassignment to APC 1523 (New Technology—Level 23 ($2501-$3000)) with a proposed payment rate of $ 2,750.50
Response: Based on our assessment of the information provided in the new technology application and the public comments received, we are revising the APC assignments for these codes. Specifically, we are revising the APC assignment for CPT code 78431 from APC 5594 to APC 1522, and reassigning CPT codes 78432 and 78433 from APC 5594 to APC 1523.
In summary, after consideration of the public comments for the new cardiac PET/CT codes, and based on our evaluation of the new technology application that provided the estimated costs for the services and described the components and characteristics of the new codes, we are finalizing our proposal, with modification, to assign CPT codes 78429, 78431, 78432, and 78433 to the final APCs listed in Table 32 below. In addition, we are finalizing our proposal, without modification, for CPT codes 78430 and 78434. In Table 32 below we list the long descriptors and final SI and APC assignments for the codes. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period (which is available via the internet on the CMS website).


c. Single-Photon Emission Computed Tomography (SPECT) Studies (APCs 5591, 5593, and 5594).
For CY 2020, we proposed to continue to assign CPT codes 78800 and 78801 to APC 5591 with a proposed payment rate of $372.69, CPT codes 78802 and 78804 to APC 5593 with a proposed payment rate of $1,293.33), and CPT code 78803 to APC 5592 with a proposed payment rate of $482.38.
We also proposed to assign new CPT codes 78830 and 78831 to APC 5593, and 78832 to APC 5594 with a proposed payment rate of $1,466.16. In addition, we proposed to assign new CPT code 78835 to status indicator “N” because it is an add-on code that is packaged and payment for it is included in the primary service. Table 33 below list the long descriptors and their proposed SI and APC assignments for these codes.
Comment: Some commenters agreed with the proposed APC assignments for CPT codes 78800, 78801, and 78802.
Response: We thank the commenters for their feedback and are finalizing the APC assignments for these codes.
Comment: Several commenters disagreed with the assignment for CPT codes 78803 and requested a modification from APC 5592 to APC 5593 because this one code will replace seven SPECT codes that will be deleted on December 31, 2019. Specifically, they reported that the seven CPT codes listed in Figure 34 will be deleted. Several commenters indicated that APC 5592 would not account for the deleted SPECT codes and recommended using a weighted average to determine an appropriate geometric mean cost for 78803. Based on their calculation, the geometric mean cost for the code should be $784.18, which is higher than the approximately $462 geometric mean cost for APC 5592, and is more consistent with the geometric mean cost for APC 5593.
Response: Based on our analysis of the latest claims data for this final rule with comment period, and as listed in the Figure 33 below, the range of geometric mean cost for CPT code 78803 and the seven deleted codes is between $433 and $1,417. We note that several of the deleted codes were assigned to APC 5593, and based on our review of these codes, we believe it would be appropriate to reassign CPT code 78803 from APC 5592 to APC 5593.

Comment: Some commenters disagreed with the assignment of CPT code 78804 to APC 5593, and stated that the APC assignment does not adequately capture the cost of multiple SPECTs provided. The commenters indicated that it would not make sense to continue to assign single and full sets of studies to the same APC and urged CMS to reassign the code to APC 5594.
Response: For CY 2020, based on claims submitted between January 1, 2018 and December 30, 2018 that were processed on or before June 30, 2019, our analysis of the latest claims data for this final rule supports maintaining CPT code 78804 in APC 5593. Specifically, our claims data show a geometric mean cost of approximately $1,298 for CPT code 78804 based on 1,656 single claims (out of 2,961 total claims), which is more appropriate in APC 5593 whose geometric mean cost is about $1,245 compared to the geometric mean cost of approximately $1,412 for APC 5594.
Comment: Some commenters agreed with the APC assignment for new CPT codes 78830 and 78832 to APC 5593 and APC 5594, respectively.
Response: We appreciate the commenters' feedback and are finalizing the APC assignment for CPT code 78830 to APC 5593 and for CPT code 78832 to APC 5594.
Comment: Several commenters opposed the APC assignment for CPT code 78831 to APC 5593. They indicated that the proposed APC assignment for CPT code 78831 does not adequately capture the resources required to perform the procedure and should be reassigned to APC 5594.
Response: We believe that new CPT code 78831 shares similar characteristics and resources to existing CPT code 78804. Consequently, we assigned the new code to APC 5593, which is the same APC assignment for CPT 78804. We note that once we have claims data for CPT code 78831, we will assess and determine whether a reassignment is necessary. As always, we review the APC assignments for all services under the OPPS based on the latest claims data.
In summary, after consideration of the public comments and after evaluation of our claims data for this final rule with comment period, we are finalizing our proposal, without modification, for CPT codes 78800, 78801, 78802, 78804, 78830, 78831, 78832, and 78835. However, we are finalizing our proposal, with modification, for CPT code 78803 and reassigning the code from APC 5592 to APC 5593 for CY 2020. Table 34 below list the long descriptors for these codes and their final SI and APC assignments. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period (which is available via the internet on the CMS website).



20. Radiofrequency Spectroscopy
As displayed in Table 8 and Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign CPT code 0546T (Radiofrequency spectroscopy, real time, intraoperative margin assessment, at the time of partial mastectomy, with report) to status indicator (SI) “N” to indicate that the code is packaged and payment for it is included in the primary surgical procedure. Specifically, payment for the codes assigned to status indicator “N” is made through the payment for the separately payable, independent services with which they are billed. No separate payment is made for services that we have assigned to status indicator “N.” We note that CPT code 0546T is associated with the MarginProbe procedure.
Comment: Several commenters requested separate payment for CPT code 0546T. One commenter stated that the code should be adequately valued and removed from packaging. Another commenter stated that packaging the code will limit the number of Medicare beneficiaries who will benefit from the procedure. Still another commenter suggested a modification in the status indicator from “N” to “J1” (comprehensive APC) but did not suggest any specific APC to which they believed the code should be assigned. Another commenter stated that assigning separate payment for CPT code 0546T is in line with CMS' objectives of reducing the number of repeat surgical excisions.
Response: As noted in the code descriptor, CPT code 0546T describes an intraoperative procedure that is performed at the time of partial mastectomy. As specified in 42 CFR 419.2(b)(14), intraoperative items and services are packaged under the OPPS. By definition, a service that is performed intraoperatively is provided during and, therefore on the same date of service, as another procedure that is separately payable under the OPPS. Because intraoperative services support the performance of an independent procedure and they are provided in the same operative session as the independent procedure, we have packaged the payment for the radiofrequency spectroscopy into the OPPS payment for the primary surgical procedure with which it is reported. In this case, the payment for CPT code 0546T is included in the breast mastectomy codes that are reported with the procedure.
We note that since 2008, intraoperative services have been packaged under the OPPS, however, packaging has always been a primary component of the OPPS since its implementation in 2000. As we state in section II.A.3. (Changes to Packaged Items and Services) of this final rule, because packaging encourages efficiency and is an essential component of a prospective payment system, packaging payment for items and services that are typically integral, ancillary, supportive, dependent, or adjunctive to a primary service has been a fundamental part of the OPPS since its implementation in August 2000.
Comment: A medical device company stated that although CPT code 0546T is a procedure provided during an operative session, it is a distinct procedure with a beginning, middle, and end. The commenter reported that the cost of the procedure is not included in the primary surgical procedure. The same commenter pointed out that based on the language below from the CY 2008 OPPS/ASC final rule (72 FR 66621), it believed CMS has the discretion not to package an intraoperative service:
“To the extent that a service for which New Technology APC status is being requested is ancillary and supportive of another service, for example, a new intraoperative service or a new guidance service, we might not consider it to be a complete service because its value is as part of an independent service. However, if the entire, complete service, including the guidance component of the service, for example, is `truly new,' as we explained that term at length . . . we would consider the new complete procedure for New Technology APC assignment.”
The commenter also indicated that, at its September 2018 meeting, the CPT Editorial Panel determined that radiofrequency spectroscopy is a stand-alone service and, therefore, issued a unique code, specifically, CPT code 0546T to be effective July 1, 2019. The commenter noted that until July 1, 2019 there was no code available to adequately describe the service, therefore, the procedure could not be represented in the claims data upon which CMS has established the CY 2020 OPPS payment determinations. Consequently, the commenter requested that CMS assign CPT code 0546T to New Technology APC 1518 (New Technology—Level 18 ($1601-$1700)) with a proposed payment rate of $1,650.50, and indicated that the payment would reflect the cost of the sterile, disposable, radiofrequency spectroscopy probe and supplies. The commenter asserted that assigning separate payment for the procedure would alleviate the barrier to access to care for the service.
Response: We note that the establishment of a new CPT code does not indicate that a code is always a stand-alone procedure or service. The current CPT code set lists hundreds of add-on codes that do not describe stand-alone services. For the list of add-on codes, refer to Appendix D (Summary of CPT Add-on Codes) of the latest CPT code book. We note that the CPT Editorial Panel does not establish new CPT codes because the service or procedure is considered stand-alone, rather they establish new codes for procedures and services that are not described by any existing code and have met their application criteria.
As stated above, CPT code 0546T is associated with the MarginProbe procedure. CPT code 0546T describes an intraoperative procedure that is performed at the time of partial mastectomy. As specified in 42 CFR 419.2(b)(14), intraoperative items and services are packaged under the OPPS.
We also disagree with the commenter's statement that CMS has the discretion not to package an intraoperative procedure. As noted above, 42 CFR 419.2(b)(14) states that intraoperative items and services are packaged under the OPPS. We do not agree that MarginProbe, for which CPT code 0546T was established, is a new, standalone procedure for which separate payment should be made. We note that the preamble language the commenter quoted only applies for services that are truly new and a complete service and, as mentioned in the quoted language, with respect to an ancillary service, which may include a new intraoperative service or a new guidance service, we might not consider it to be a complete service because its value is as part of an independent service. MarginProbe, received Premarket Approval (PMA) from the FDA on December 27, 2012, and has been on the market since February 2013, however, FDA approval alone does not compel a determination under Medicare that the technology represents a separate standalone service that would qualify for New Technology APC assignment.
Finally, because CPT code 0546T describes an intraoperative service that is performed during a mastectomy procedure, we are finalizing our proposal to assign the code to status indicator “N”. Therefore, after consideration of the public comments received, we are finalizing our proposal without modification for CPT code 0546T. The final status indicator assignment for the code is listed in Addendum B to this final with comment period. We refer readers to Addendum D1 of this final rule with comment period for the complete list of the OPPS payment status indicators and their definitions for CY 2020. Both Addendum B and Addendum D1 are available via the internet on the CMS website.
21. Reflectance Confocal Microscopy (RCM)
For CY 2020, we proposed to continue to assign CPT code 96932 to status indicator “Q1” (conditionally packaged) and APC 5731 (Level 1 Minor Procedures) with a proposed payment rate of $23.57. We note that the CPT Editorial Panel established six (6) CPT codes to describe the services associated with RCM. These codes are shown in Table 35 with the long descriptors and proposed status indicator assignments.
Comment: A commenter stated that the low payment rate for this service under the OPPS is based on misreporting of charges by a hospital. The commenter explained that based on their review and analysis of the OPPS claims, only two hospitals in the country are performing this imaging test, and that the proposed payment rate is based primarily on one hospital's charges. The same commenter stated that the cost of performing the imaging service is about $128, which is more than the proposed payment rate of $23.57. To correct the low payment for the test, the commenter suggested that CMS use its equitable adjustment authority to set an appropriate payment for 96932 and also recommended that we do one of the following:
- Reassign the code to APC 5522 (Level 1 Imaging without Contrast) with a proposed payment rate of $111.04;
- Reassign the code to New Technology APC 1503 (New Technology—Level 3 ($101-$200) with a proposed payment rate of $150.50; or
- Assign an unconditionally packaged (“N”) or non-payable status indicator to the code, similar to the other RCM codes.
The commenter also expressed concern that the low payment rate under the OPPS significantly impacts the payment for the service under the PFS. The commenter added that RCM is primarily performed in the physician office setting, however, because of the low payment rate established under the OPPS, the payment for the service is inadequate. To correct the low payment rate, the commenter suggested that CMS revise the status indicator of CPT code 96932 to identify the service as packaged or non-payable, and, therefore, not have a published OPPS payment rate for the code. The commenter believed that packaging the code or assigning it as non-payable will correct the payment rate and provide adequate payment for the service.
Response: Section 5102(b) of the Deficit Reduction Act of 2005 (DRA) amended the PFS statute to place a payment cap on the technical component (TC) of certain diagnostic imaging procedures and the TC portions of the global diagnostic imaging services at the amount paid under the OPPS. To implement this provision, the physician fee schedule (PFS) amount is compared to the OPPS payment amount and the lower amount is used for payment. CPT code 96932 is designated as a DRA imaging code whose payment under the PFS is capped at the OPPS rate even when performed in a physician office setting. Based on our review of the issue, we believe that we should revise the OPPS status indicator assignment for CPT code 96932 from “Q1” to “N”, similar to the status indicator assignment for several other RCM codes. Since CPT code was low volume under the OPPS, it may be inappropriate to establish an OPPS payment rate by which the PFS rate would be capped. Accordingly, this change will allow there not to be an OPPS cap for the service.
In summary, after consideration of the public comment, we are finalizing our proposal with modification and revising the status indicator assignment for CPT code 96930 to “N” for CY 2020. Table 35 below lists the long descriptors and final status indicator assignments for the six (6) codes that describe the services associated with RCM. We refer readers to Addendum D1 of this final rule with comment period for the complete list of the OPPS payment status indicators and their definitions for CY 2020. Addendum D1 is available via the internet on the CMS website.

22. remedē® System—Transvenous Phrenic Nerve Stimulation Therapy (APCs 5461-5464, 5724, and 5742)
For the CY 2020 update, we proposed to modify the APC assignment for certain CPT codes associated with the Transvenous Phrenic Nerve Stimulation Therapy or remedē® System. Of the 13 codes, we received a comment on the APC assignment for three codes, specifically, CPT codes 0426T, 0427T, and 0431T. As shown in Table 36 below with the long descriptors, and also in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to reassign CPT codes 0426T and 0431T from APC 5463 (Level 3 Neurostimulator and Related Procedures) to APC 5464 (Level 4 Neurostimulator and Related Procedures) with a proposed payment rate of $29,025.99. In addition, we proposed to continue to assign CPT code 0427T to APC 5463 ((Level 3 Neurostimulator and Related Procedures) with a proposed payment rate of $19,370.82.
Comment: A device company suggested that we maintain the current assignment and not revise the APC assignment to APC 5464 for CPT code 0426T. The commenter stated that the resources required for the procedure are more closely aligned with the procedures in APC 5463.
Response: Based on our evaluation of the procedure associated with CPT code 0426T, we agree that the procedure described by the code appropriately fits in APC 5463 based on its clinical similarity to other procedures in the APC. CPT code 0426T describes the insertion or replacement of the stimulation lead associated with a neurostimulator system for the treatment of central sleep apnea, and APC 5463 includes other procedures that involve the insertion or replacement of a stimulation lead for a neurostimulator system. Therefore, we will maintain the APC assignment for CPT code 0426T to APC 5463 for CY 2020.
Comment: The same device company that commented on CPT code 0426T also commented on the APC assignment for CPT code 0427T. According to the commenter, the procedure describes the initial insertion of the implantable pulse generator when the full system cannot be implanted for a patient, and added that the procedure does not occur frequently.
The commenter also noted that the hospital resources associated with CPT code 0427T are very similar to CPT code 0431T, which is assigned to APC 5464, and recommended the assignment of both procedures to APC 5464.
Response: Based on our review of the two procedures, we agree that the resources associated with inserting or replacing a pulse generator for a neurostimulator system that is described by CPT code 0427T are very similar to removing and replacing a pulse generator for a neurostimulator system that is described by CPT code 0431T. Consequently, we are modifying our proposal and reassigning CPT code 0427T to APC 5464.
Comment: The same device company that commented on CPT codes 0426T and 0427T also commented on CPT code 0431T. Specifically, the commenter concurred with the APC reassignment for the code to APC 5464.
Response: As indicated above, based on our review of the two procedures, we agree that the resources associated with inserting or replacing a pulse generator for a neurostimulator system that is described by CPT code 0427T are very similar to removing and replacing a pulse generator for a neurostimulator system that is described by CPT code 0431T. Therefore, we are finalizing our proposal for CPT code 0431T and assigning the code to APC 5464.
In summary, after consideration of the public comment, we are finalizing our proposal with modification. Specifically, we are finalizing our APC proposal for CPT code 0431T to APC 5464, however, we are maintaining the APC assignment for CPT code 0426T to APC 5463, and reassigning CPT code 0427T to APC 5464. We note that the final CY 2020 OPPS payment rates for all the codes associated with the Transvenous Phrenic Nerve Stimulation Therapy or remedē® System can be found in Addendum B of this final rule with comment period. Table 36 below lists the long descriptors for all 13 codes and the final APC and SI assignments for CY 2020. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator meanings for all codes reported under the OPPS for CY 2020. Both Addendum B and Addendum D1 are available via the internet on the CMS website.


23. Surgical Pathology Tissue Exam (APC 5673)
In CY 2019, CPT code 88307 (Level V—surgical pathology, gross and microscopic examination) was assigned to APC 5673 (Level 3 Pathology) with a payment rate of $274.22. For CY 2020, we proposed to reassign the code to APC 5672 (Level 2 Pathology) with a proposed payment rate of $148.62.
Comment: A commenter disagreed with the proposed reassignment and urged CMS to continue to assign CPT code 88307 to APC 5673. This same commenter reported that the service includes complex Level V surgical pathology specimens and the proposed change represents a 46 percent decrease in the payment amount. The commenter added that the proposed reassignment creates a resource cost rank order anomaly with other physician services and the technical costs will not be fully recovered from each unit of service. In addition, the commenter believed that the data do not identify actual costs for specific procedures, and stated that the cost associated with CPT code 88307 is greater than six times the cost of the services assigned to APC 5672 (Level 2 Pathology) based on physician fee schedule technical component cost differences. The commenter also believed that the data leading to the APC reassignment must be flawed and added that charge-based cost data were neither designed nor intended to be an accurate estimate of service/procedure level costs at the CPT code level. The commenter stated that the hospital charge-based cost data used for OPPS rate-setting allows CMS to estimate costs for purposes of grouping a number of services or procedures (multiple distinct codes) into appropriate clinically and economically homogeneous APCs.
Response: As stated in section III.B. (Final OPPS Changes—Variations Within APCs) of this final rule with comment period, payments for OPPS services and procedures are based on our analysis of the latest claims data. For the proposed rule, the OPPS proposed payment rates were based on claims data that were submitted between January 1, 2018 through December 31, 2018, that were processed on or before December 31, 2018. However, for the final rule, the OPPS final payment rates are based on claims that were submitted between January 1, 2018 through December 31, 2018, that were processed on or before June 30, 2019. Based on the latest hospital outpatient claims data used for this final rule with comment period, we agree with the commenter that the code should continue to be assigned to APC 5673 for CY 2020. Specifically, CPT code 88307 shows a geometric mean cost of approximately $219, which is more appropriate in APC 5673 whose geometric cost is approximately $277 compared to the geometric mean cost of about $140 for APC 5672. Consequently, we are revising our proposal and maintaining the APC assignment for CPT code 88307 to APC 5673 for CY 2020.
In summary, after consideration of the public comment, and after our analysis of the updated claims data for this final rule with comment period, we are finalizing our proposal with modification. Specifically, we are revising the APC assignment for CPT code 88307 to APC 5673 for CY 2020. The final CY 2020 payment rate for the code can be found in Addendum B to this final rule with comment period (which is available via the internet on the CMS website).
As we do every year, we will reevaluate the APC assignment for CPT code 88307 for the next rulemaking cycle. We note that we review, on an annual basis, the APC assignments for all services and items paid under the OPPS.
24. Urology Procedures
a. HIFU Procedure—High-Intensity Focused Ultrasound of the Prostate (APC 5375)
In 2017, CMS received a new technology application for the prostate HIFU procedure and established a new code, specifically, HCPCS code C9747 (Ablation of prostate, transrectal, high intensity focused ultrasound (hifu), including imaging guidance). Based on the estimated cost provided in the new technology application, we assigned the new code to APC 5376 (Level 6 Urology and Related Services) with a payment rate of $7,452.66 effective July 1, 2017. We announced the SI and APC assignment in the July 2017 OPPS quarterly update CR (Transmittal 3783, Change Request 10122, dated May 26, 2017).
For the CY 2018 update, we made no change to the APC assignment and continued to assign HCPCS code C9747 to APC 5376 with a payment rate of $7,596.26. We note that the payment rates for the CY 2018 OPPS update were based on claims submitted between January 1, 2016 through December 30, 2016, that were processed on or before June 30, 2017. Since HCPCS code C9747 was established on July 1, 2017, we had no claims data for the procedure for use in ratesetting for CY 2018.
However, for the CY 2019 update, based on the latest claims data for the final rule, we revised the APC assignment for HCPCS code C9747 from APC 5376 to APC 5375 with a payment rate of $4,020.54. We note that the payment rates for CY 2019 were based on claims submitted between January 1, 2017 through December 30, 2017, that were processed on or before June 30, 2018. Our claims data showed a geometric mean cost of approximately $5,000 for HCPCS code C9747 based on 64 single claims (out of 64 total claims), which was significantly lower than the geometric mean cost of about $7,717 for APC 5376. We believed that the geometric mean cost for HCPCS code C9747 was more comparable to the geometric mean cost of approximately $4,055 for APC 5375. Consequently, we reassigned the code from APC 5376 to APC 5375 (Level 5 Urology and Related Services) for CY 2019.
For CY 2020, we proposed to continue to assign HCPCS code C9747 to APC 5375 with a proposed payment rate $4,286.06.
Comment: Several commenters disagreed with the APC assignment for HCPCS code C9747 and recommended a reclassification to APC 5376 because they believed the service is clinically similar and comparable in terms of resources to cryoablation of the prostate, which is described by CPT code 55873 (Cryosurgical ablation of the prostate (includes ultrasonic guidance and monitoring), and placed in APC 5376 (Level 6 Urology and Related Services), with a proposed payment rate of $8,193.30. The commenters believed that the geometric mean cost, and ultimately, the APC determination for the prostate HIFU procedure was based on inaccurate hospital costs. They believed that the average cost of the procedure should be approximately $6,250, and requested a reassignment to APC 5376 to enable Medicare beneficiaries to continue to receive the treatment. They stated based on their projections that maintaining the APC assignment to APC 5375 for the procedure will decrease the number of Medicare beneficiaries receiving the treatment by 75 percent if the CY 2020 payment rate is finalized.
Response: As we have stated every year since the implementation of the OPPS on August 1, 2000, we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on our analysis of the latest claims data. For CY 2020, based on claims submitted between January 1, 2018 through December 30, 2018, that were processed on or before June 30, 2019, our analysis of the latest claims data for this final rule supports maintaining HCPCS code C9747 in APC 5375. Specifically, our claims data shows a geometric mean cost of approximately $5,850 for HCPCS code C9747 based on 264 single claims (out of 268 total claims), which is comparable to the geometric mean cost of about $4,140 for APC 5375, rather than the geometric mean cost of approximately $7,894 for APC 5376.
Also, we do not agree that the resource costs associated with the prostate HIFU procedure are similar to those of cryoablation of the prostate. Our claims data for the CY 2020 update shows a geometric mean cost of about $8,152 based on 1,417 single claims (out of 1,429 total claims) for cryoablation of the prostate. The geometric mean cost for CPT code 55873 is reasonably consistent with APC 5376, whose geometric mean cost is approximately $7,894.
With respect to the issue of inaccurate hospital cost reporting for HCPCS code C9747, based on our analysis of the CY 2020 hospital outpatient claims data used for this final rule with comment period, we are unable to determine whether hospitals are misreporting the procedure. It is generally not our policy to judge the accuracy of hospital coding and charging for purposes of ratesetting. We rely on hospitals to accurately report the use of HCPCS codes in accordance with their code descriptors and CPT and CMS instructions, and to report services on claims and charges and costs for the services on their Medicare hospital cost report appropriately. Also, we do not specify the methodologies that hospitals use to set charges for this or any other service. Furthermore, we state in Chapter 4 of the Medicare Claims Processing Manual that “it is extremely important that hospitals report all HCPCS codes consistent with their descriptors; CPT and/or CMS instructions and correct coding principles, and all charges for all services they furnish, whether payment for the services is made separately paid or is packaged” to enable CMS to establish future ratesetting for OPPS services.
Comment: A commenter reported that the prostate HIFU procedure (C9747) and cryoablation of the prostate (55873) are two clinically similar procedures for the ablation of prostate for cancer, and are the only two acknowledged treatments for radiorecurrent, non-metastatic prostate cancer. This same commenter requested that we either create a new APC group specific to prostate ablation procedures or modify the organization of HCPCS codes within the urology family of APCs. The commenter specifically noted that a reorganization for APCs 5374 through 5376 would be appropriate but added that there are other inconsistencies across procedures within the urology APCs. The commenter also mentioned that CPT codes 50555 (Renal endoscopy through established nephrostomy or pyelostomy, with or without irrigation, instillation, or ureteropyelography, exclusive of radiologic service; with biopsy) and 50557 (Renal endoscopy through established nephrostomy or pyelostomy, with or without irrigation, instillation, or ureteropyelography, exclusive of radiologic service; with fulguration and/or incision, with or without biopsy) are assigned to two different APCs, however, their APC assignments appear reversed. The commenter further suggested updating the procedures within APCs 5374, 5375, and 5376 so that the geometric mean costs for the procedure fall into the following ranges:

Response: We appreciate the commenter's suggestions and may consider a reorganization of the procedures in the urology APCs in future rulemaking. We note that each year, under the OPPS, we revise and make changes to the APC groupings based on the latest hospital outpatient claims data to appropriately place procedures and services in APCs based on clinical characteristics and resource similarity. For CY 2020, based on our analysis of the latest claims data for this final rule, we do not believe that establishing a new APC specific to prostate ablation procedures is necessary, nor do we believe that modifying the HCPCS codes within the urology family APCs is appropriate at this time.
With respect to CPT codes 50555 and 50557, based on our review of the claims data for this final rule with comment period, we revised the APC assignment for CPT code 50555 from APC 5375 to APC 5376, and maintained the APC assignment for CPT code 50557 in APC 5376. Specifically, our claims data show a geometric about $7,327 for CPT code 50555 and approximately $6,224 for CPT code 50557, which are more comparable with the geometric cost for APC 5376 of about $7,894 unlike that of APC 5375 whose geometric mean cost is approximately $4,140.
In summary, after consideration of the public comments, and after our analysis of the updated claims data for this final rule with comment period, we are finalizing our proposal, without modification, to continue to assign HCPCS code C9747 to APC 5375 for CY 2020. The final CY 2020 payment rate for the code can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
b. ProACT Procedure—Transperineal Periurethral Adjustable Balloon Continence Device Procedure (APCs 5371, 5374, 5375, and 5376)
In 2017, CMS received a new technology application for the transperineal periurethral adjustable balloon continence device procedure, which is associated with ProACT Therapy, and established a new code, specifically, HCPCS code C9746. Based on the estimated cost for the bilateral placement of the balloon continence devices, we assigned the code to APC 5377 (Level 7 Urology and Related Services) with a payment rate of $14,363.61 effective July 1, 2017. We announced the new code, and interim SI and APC assignments, and payment rate in the July 2017 quarterly update to the OPPS (Transmittal 3783, Change Request 10122, dated May 26, 2017).
For the CY 2018 update, we made no change to the APC assignment and continued to assign HCPCS code C9746 to APC 5377 with a payment rate of $15,697.82. We note that OPPS payment rates for the CY 2018 update were based on claims submitted between January 1, 2016 through December 30, 2016, that were processed on or before June 30, 2017. Since HCPCS code C9746 was established on July 1, 2017, we had no claims data for the procedure for use in ratesetting in CY 2018.
For the CY 2019 update, we again had no claims data for the code so we made no change to the APC assignment and continued to assign HCPCS code C9746 to APC 5377 with a payment rate of $16,319.55. We note that the payment rates for CY 2019 were based on claims submitted between January 1, 2017 through December 30, 2017, that were processed on or before June 30, 2018.
In July 2019, the CPT Editorial Panel established four new codes to describe the transperineal periurethral adjustable balloon continence device procedure, specifically, CPT codes 0548T, 0549T, 0550T, and 0551T. In the July 2019 quarterly update to the OPPS (Transmittal 4313, Change Request 11318, dated May 24, 2019), we listed the temporary APC assignments for the new codes in the July 2019 OPPS Update CR and announced the deletion of HCPCS code C9746 on June 30, 2019, since it was replaced with CPT code 0548T effective July 1, 2019. These codes are listed in Table 37 along with their long descriptors and proposed SI and APC assignments.
For CY 2020, we proposed to revise the APC assignment for new CPT code 0548T, which was previously described by HCPCS code C9746. In addition, we proposed to assign CPT codes 0549T, 0550T, and 0551T to APCs 5375, 5374, and 5371, respectively.
Comment: A medical device company suggested that CPT code 0548T remain in APC 5377, consistent with the APC assignment for the predecessor code (HCPCS code C9746). This commenter indicated that the calculated geometric mean cost does not accurately reflect the actual cost of the procedure. The commenter noted there were only two billings identified in the CMS data—one billing at the correct cost of $16,250 and one billing incorrectly recorded at $0. The commenter stated that the resulting calculation of the geometric mean cost of $8,125 does not accurately represent the actual cost of the bilateral procedure for CPT code 0548T. In addition, the same commenter requested a reassignment from APC 5375 to APC 5376 for CPT code 0549T.
Response: As we have stated every year since the implementation of the OPPS on August 1, 2000, we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on our analysis of the latest claims data. For CY 2020, based on claims submitted between January 1, 2018 through December 30, 2018, that were processed on or before June 30, 2019, our analysis of the latest claims data for this final rule supports revising the APC assignment for CPT code 0548T (which was previously described by predecessor HCPCS code C9746) from APC 5377 to APC 5376 (Level 6 Urology and Related Services). Specifically, our claims data shows a geometric mean cost of approximately $9,504 for HCPCS code C9746 based on 7 single claims (out of 7 total claims), which is most comparable to the geometric mean cost of about $7,894 for APC 5376, rather than the geometric mean cost of approximately $17,195 for APC 5377. We believe that assigning CPT code 0548T to APC 5377 would significantly overpay for the procedure.
In addition, based on the geometric mean cost for the placement of the bilateral balloon continence devices (CPT code 0548T), we do not agree that we should revise the APC assignment for CPT code 0549T, which represents the unilateral placement of the balloon continence device, from APC 5375 to APC 5376. We believe that the cost associated with CPT code 0549T should be less than that of CPT code 0548T since CPT code 0549T describes the use of only one device.
Moreover, we rely on hospitals to accurately report the use of HCPCS codes in accordance with their code descriptors and CPT and CMS instructions, and to appropriately report services on claims and charges and costs for the services on their Medicare hospital cost report. However, we do not specify the methodologies that hospitals use to set charges for this or any other service. We also state in Chapter 4 of the Medicare Claims Processing Manual that “it is extremely important that hospitals report all HCPCS codes consistent with their descriptors; CPT and/or CMS instructions and correct coding principles, and all charges for all services they furnish, whether payment for the services is made separately paid or is packaged” to enable CMS to establish future ratesetting for OPPS services.
In summary, after consideration of the public comment and after our analysis of the updated claims data for this final rule with comment period, we are finalizing our proposal, without modification, to assign CPT codes 0548T, 0549T, 0550T, and 0551T to the APCs listed in Table 37 below. The final CY 2020 payment rate for the codes can be found in Addendum B to this final rule with comment period. In addition, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.

c. Rezum Procedure—Transurethral High Energy Water Vapor Thermal Therapy of the Prostate (APC 5373)
In late 2017, CMS received a new technology application for the transurethral radiofrequency generated water vapor thermal therapy of the prostate, also known as the Rezum procedure, and established a new code, specifically, HCPCS code C9748 (Transurethral destruction of prostate tissue; by radiofrequency water vapor (steam) thermal therapy) effective January 1, 2018. Based on the estimated cost of the procedure, we assigned the new code to APC 5373 (Level 3 Urology and Related Services) with a payment rate of $1,695.68 effective January 1, 2018. The new code appeared in both the OPPS Addendum B of the CY 2018 OPPS/ASC final rule and the January 2018 OPPS Update CR (Transmittal 3941, Change Request 10417, dated December 22, 2017).
For the CY 2019 update, the CPT Editorial Panel established a new code to describe the Rezum procedure, specifically, CPT code 53854 (Transurethral destruction of prostate tissue; by radiofrequency generated water vapor thermotherapy) effective January 1, 2019. We deleted HCPCS code C9748 on December 31, 2018 because it was replaced with CPT code 53854 and assigned the new code to APC 5373, which was the same APC assignment for the predecessor code, with a payment rate of $1,739.75. We note that payment rates for the CY 2019 update were based on claims submitted between January 1, 2017 and December 30, 2017 that were processed on or before June 30, 2018.
For the CY 2020 update, we proposed to maintain the APC assignment for CPT code 53854 to APC 5373 with a proposed payment rate of $1,797.97.
Comment: Several commenters requested a reclassification for CPT code 53854 from APC 5373 to APC 5374 (Level 4 Urology and Related Services) with a proposed payment rate of $3,059.21. The commenters reported that the Rezum procedure is most clinically similar to the transurethral microwave therapy (TUMT), which is described by CPT code 53850 (Transurethral destruction of prostate tissue; by microwave thermotherapy), and transurethral needle (radiofrequency) ablation (TUNA), which is described by CPT code 53852 (Transurethral destruction of prostate tissue; by radiofrequency thermotherapy). Some commenters reported that the primary difference between each of these codes is the energy source used to destroy or shrink the prostate tissue, specifically, CPT code 53850 uses microwave energy, 53852 uses radiofrequency energy, and 53854 uses radiofrequency generated water vapor thermotherapy. Apart from the energy source, the commenters indicated that the procedures and resources used in these procedures are similar. Consequently, they recommended that all three procedures be placed in APC 5374.
Response: As we have stated every year since the implementation of the OPPS on August 1, 2000, we review, on an annual basis, the APC assignments for all services and items paid under the OPPS based on our analysis of the latest claims data. For CY 2020, based on claims submitted between January 1, 2018 through December 30, 2018, that were processed on or before June 30, 2019, our analysis of the latest claims data for this final rule supports maintaining the APC assignment for CPT code 53854 (which was previously described by predecessor HCPCS code C9748) to APC 5373. Our claims data show a geometric mean cost of approximately $1,899 for the predecessor HCPCS code C9748 based on 191 single claims (out of 192 total claims). The geometric mean cost for the Rezum procedure is more in line with the geometric mean cost of about $1,733 for APC 5373 rather than with APC 5374 whose geometric mean cost is approximately $2,953.
In addition, based on our analysis of the claims data, the resource costs associated with the TUMT and TUNA procedures are not similar to the Rezum procedure. While all three procedures treat the same indication and utilize the same type of technology, time, set up, and planning, their resource costs vary. Our claims data show a geometric mean cost of approximately $2,851 for the TUMT procedure (CPT code 53850) based on 41 single claims (out of 41 total claims), and about $3,027 for the TUNA procedure (CPT code 53852) based on 513 single claims (out of 514 total claims). In both cases, the resource costs for the TUMT and TUNA procedures are much higher than those for the Rezum procedure.
Therefore, after consideration of the public comments, and after our analysis of the updated claims data for this final rule with comment period, we are finalizing our proposal, without modification, and assigning CPT code 53854 to APC 5373. Table 38 below list the final APC assignments for CPT code 58350 (TUMT), 53852 (TUNA) and 53854 (Rezum). In addition, the final CY 2020 payment rates for these procedures can be found in Addendum B to this final rule with comment period. Further, we refer readers to Addendum D1 of this final rule with comment period for the status indicator (SI) meanings for all codes reported under the OPPS. Both Addendum B and D1 are available via the internet on the CMS website.
As always, we will reevaluate the APC assignment for CPT code 53854 in the next rulemaking cycle. As stated above, we review, on an annual basis, the APC assignments for all services and items paid under the OPPS.

d. VaporBlate Procedure—Transurethral Radiofrequency Generated Water Vapor Thermal Therapy of the Prostate
As displayed in Addendum B to the CY 2020 OPPS/ASC proposed rule, we proposed to assign the procedure described by CPT code 0582T (Transurethral ablation of malignant prostate tissue by high-energy water vapor thermotherapy, including intraoperative imaging and needle guidance) to status indicator “E1” to indicate that the code is not payable by Medicare when submitted on outpatient claims (any outpatient bill type) because the services associated with these codes are either not covered by any Medicare outpatient benefit category, are statutorily excluded by Medicare, or are not reasonable and necessary. The code was listed as 0X76T (the 5-digit CMS placeholder code) in Addendum B with the short descriptor, and again in Addendum O with the long descriptor. We also assigned the code to comment indicator “NP” in Addendum B to indicate that the code is new for CY 2020 and that public comments would be accepted on the proposed status indicator assignment. We note that the code will be effective January 1, 2020.
Comment: A medical device company reported that the technology associated with this new code received FDA approval as an IDE. Specifically, the VaporBlate technology was designated by the FDA as a Category B IDE on August 29, 2019. The commenter also stated that they are in the process of applying for Medicare coverage of the Category B IDE clinical trial. In the event the clinical trial is approved by Medicare, the commenter suggested assigning the code to one of the following APCs:
- APC 1590 (New Technology—Level 39 ($15,001-$20,000)) with a proposed payment rate of $ 17,500.50; or
- APC 5377 (Level 7 Urology and Related Services) with a proposed payment rate of $17,465.94.
The commenter explained that the VaporBlate procedure involves the transurethral ablation of malignant prostate tissue by high-energy water vapor thermotherapy, which is unlike that of the Rezum procedure that involves transurethral radiofrequency generated water vapor thermal therapy for benign prostatic hyperplasia (BPH). The commenter added that the resource costs associated with the VaporBlate procedure are significantly higher than those for the Rezum procedure. The Rezum generator (capital equipment) used in CPT code 53854 costs $32,500 and the Rezum supply kit (disposables) costs between $1,000 and $1,500, while the VaporBlate generator (capital equipment) used to perform the procedure described by the VaporBlate procedure costs $80,000 and the supply kits (disposables) cost $12,500 each. Based on the clinical and cost differences, the commenter stated that CPT code 0582T should not be assigned to the same APC as CPT code 53854 (Rezum procedure).
Response: Based on our understanding of the procedure, we found that the service associated with CPT code 0582T is currently in clinical trial (Study Title: “Ablation of Prostate Tissue in Patients With Intermediate Risk Localized Prostate Cancer”; ClinicalTrials.gov Identifier: NCT04087980). Further review of the clinical trial revealed that the clinical study has not yet met CMS' standards for coverage, nor does it appear on the CMS Approved IDE List, which can be found at this CMS website: https://www.cms.gov/Medicare/Coverage/IDE/Approved-IDE-Studies.html. Because the VaporBlate technology has not been approved for Medicare coverage as a Category B IDE, we believe that we should continue to assign CPT code 0582T to status indicator “E1”. If this technology later meets CMS' standards for coverage, we will reassess the APC assignment for the code in a future quarterly update and/or rulemaking cycle.
Therefore, after consideration of the public comment, we are finalizing our proposal, without modification, to assign CPT code 0582T to status indicator “E1”. We refer readers to Addendum D1 of this final rule with comment period for the complete list of the OPPS payment status indicators and their definitions for CY 2020. Addendum D1 is available via the internet on the CMS website.
IV. OPPS Payment for Devices
A. Pass-Through Payment for Devices
1. Beginning Eligibility Date for Device Pass-Through Status and Quarterly Expiration of Device Pass-Through Payments
a. Background
The intent of transitional device pass-through payment, as implemented at 42 CFR 419.66, is to facilitate access for beneficiaries to the advantages of new and truly innovative devices by allowing for adequate payment for these new devices while the necessary cost data is collected to incorporate the costs for these devices into the procedure APC rate (66 FR 55861). Under section 1833(t)(6)(B)(iii) of the Act, the period for which a device category eligible for transitional pass-through payments under the OPPS can be in effect is at least 2 years but not more than 3 years. Prior to CY 2017, our regulation at 42 CFR 419.66(g) provided that this pass-through payment eligibility period began on the date CMS established a particular transitional pass-through category of devices, and we based the pass-through status expiration date for a device category on the date on which pass-through payment was effective for the category. In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79654), in accordance with section 1833(t)(6)(B)(iii)(II) of the Act, we amended § 419.66(g) to provide that the pass-through eligibility period for a device category begins on the first date on which pass-through payment is made under the OPPS for any medical device described by such category.
In addition, prior to CY 2017, our policy was to propose and finalize the dates for expiration of pass-through status for device categories as part of the OPPS annual update. This means that device pass-through status would expire at the end of a calendar year when at least 2 years of pass-through payments had been made, regardless of the quarter in which the device was approved. In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79655), we changed our policy to allow for quarterly expiration of pass-through payment status for devices, beginning with pass-through devices approved in CY 2017 and subsequent calendar years, to afford a pass-through payment period that is as close to a full 3 years as possible for all pass-through payment devices.
We refer readers to the CY 2017 OPPS/ASC final rule with comment period (81 FR 79648 through 79661) for a full discussion of the current device pass-through payment policy.
We also have an established policy to package the costs of the devices that are no longer eligible for pass-through payments into the costs of the procedures with which the devices are reported in the claims data used to set the payment rates (67 FR 66763).
b. Expiration of Transitional Pass-Through Payments for Certain Devices
As stated earlier, section 1833(t)(6)(B)(iii) of the Act requires that, under the OPPS, a category of devices be eligible for transitional pass-through payments for at least 2 years, but not more than 3 years. There currently is one device category eligible for pass-through payment: C1823 Generator, neurostimulator (implantable), nonrechargeable, with transvenous sensing and stimulation leads), which was established effective January 1, 2019. The pass-through payment status of the device category for HCPCS code C1823 will end on December 31, 2021. HCPCS code C1823 will continue to receive pass-through status in CY 2020.
2. New Device Pass-Through Applications
a. Background
Section 1833(t)(6) of the Act provides for pass-through payments for devices, and section 1833(t)(6)(B) of the Act requires CMS to use categories in determining the eligibility of devices for pass-through payments. As part of implementing the statute through regulations, we have continued to believe that it is important for hospitals to receive pass-through payments for devices that offer substantial clinical improvement in the treatment of Medicare beneficiaries to facilitate access by beneficiaries to the advantages of the new technology. Conversely, we have noted that the need for additional payments for devices that offer little or no clinical improvement over previously existing devices is less apparent. In such cases, these devices can still be used by hospitals, and hospitals will be paid for them through appropriate APC payment. Moreover, a goal is to target pass-through payments for those devices where cost considerations might be most likely to interfere with patient access (66 FR 55852; 67 FR 66782; and 70 FR 68629). We note that, in section IV.A.4. of the CY 2020 OPPS/ASC proposed rule, we proposed an alternative pathway that would grant fast-track device pass-through payment under the OPPS for devices approved under the FDA Breakthrough Device Program for OPPS device pass-through payment applications received on or after January 1, 2020. We refer readers to section IV.A.4. of the CY 2020 OPPS/ASC proposed rule for a complete discussion on this proposal.
As specified in regulations at 42 CFR 419.66(b)(1) through (3), to be eligible for transitional pass-through payment under the OPPS, a device must meet the following criteria:
- If required by FDA, the device must have received FDA approval or clearance (except for a device that has received an FDA investigational device exemption (IDE) and has been classified as a Category B device by the FDA), or meet another appropriate FDA exemption; and the pass-through payment application must be submitted within 3 years from the date of the initial FDA approval or clearance, if required, unless there is a documented, verifiable delay in U.S. market availability after FDA approval or clearance is granted, in which case CMS will consider the pass-through payment application if it is submitted within 3 years from the date of market availability;
- The device is determined to be reasonable and necessary for the diagnosis or treatment of an illness or injury or to improve the functioning of a malformed body part, as required by section 1862(a)(1)(A) of the Act; and
- The device is an integral part of the service furnished, is used for one patient only, comes in contact with human tissue, and is surgically implanted or inserted (either permanently or temporarily), or applied in or on a wound or other skin lesion.
In addition, according to § 419.66(b)(4), a device is not eligible to be considered for device pass-through payment if it is any of the following: (1) Equipment, an instrument, apparatus, implement, or item of this type for which depreciation and financing expenses are recovered as depreciation assets as defined in Chapter 1 of the Medicare Provider Reimbursement Manual (CMS Pub. 15-1); or (2) a material or supply furnished incident to a service (for example, a suture, customized surgical kit, or clip, other than a radiological site marker).
Separately, we use the following criteria, as set forth under § 419.66(c), to determine whether a new category of pass-through payment devices should be established. The device to be included in the new category must—
- Not be appropriately described by an existing category or by any category previously in effect established for transitional pass-through payments, and was not being paid for as an outpatient service as of December 31, 1996;
- Have an average cost that is not “insignificant” relative to the payment amount for the procedure or service with which the device is associated as determined under § 419.66(d) by demonstrating: (1) The estimated average reasonable costs of devices in the category exceeds 25 percent of the applicable APC payment amount for the service related to the category of devices; (2) the estimated average reasonable cost of the devices in the category exceeds the cost of the device-related portion of the APC payment amount for the related service by at least 25 percent; and (3) the difference between the estimated average reasonable cost of the devices in the category and the portion of the APC payment amount for the device exceeds 10 percent of the APC payment amount for the related service (with the exception of brachytherapy and temperature-monitored cryoablation, which are exempt from the cost requirements as specified at § 419.66(c)(3) and (e)); and
- Demonstrate a substantial clinical improvement, that is, substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment.
Beginning in CY 2016, we changed our device pass-through evaluation and determination process. Device pass-through applications are still submitted to CMS through the quarterly subregulatory process, but the applications will be subject to notice-and-comment rulemaking in the next applicable OPPS annual rulemaking cycle. Under this process, all applications that are preliminarily approved upon quarterly review will automatically be included in the next applicable OPPS annual rulemaking cycle, while submitters of applications that are not approved upon quarterly review will have the option of being included in the next applicable OPPS annual rulemaking cycle or withdrawing their application from consideration. Under this notice-and-comment process, applicants may submit new evidence, such as clinical trial results published in a peer-reviewed journal or other materials for consideration during the public comment process for the proposed rule. This process allows those applications that we are able to determine meet all of the criteria for device pass-through payment under the quarterly review process to receive timely pass-through payment status, while still allowing for a transparent, public review process for all applications (80 FR 70417 through 70418).
More details on the requirements for device pass-through payment applications are included on the CMS website in the application form itself at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/passthrough_payment.html, in the “Downloads” section. In addition, CMS is amenable to meeting with applicants or potential applicants to discuss research trial design in advance of any device pass-through application or to discuss application criteria, including the substantial clinical improvement criterion.
b. Applications Received for Device Pass-Through Payment for CY 2020
We received seven complete applications by the March 1, 2019 quarterly deadline, which was the last quarterly deadline for applications to be received in time to be included in the CY 2020 OPPS/ASC proposed rule. We received one of the applications in the second quarter of 2018, three of the applications in the fourth quarter of 2018, and three of the applications in the first quarter of 2019. None of the applications were approved for device pass-through payment during the quarterly review process.
Applications received for the later deadlines for the remaining 2019 quarters (June 1, September 1, and December 1), if any, will be presented in the CY 2021 OPPS/ASC proposed rule. We note that the quarterly application process and requirements have not changed in light of the addition of rulemaking review. Detailed instructions on submission of a quarterly device pass-through payment application are included on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/catapp.pdf. A discussion of the applications received by the March 1, 2019 deadline is presented below.
(1) Surefire® SparkTM Infusion System
TriSalus Life Sciences submitted an application for a new device category for transitional pass-through payment status for the Surefire® SparkTM Infusion System. The Surefire® SparkTM Infusion System is described as a flexible, ultra-thin microcatheter with a self-expanding, nonocclusive one-way microvalve at the distal end. The applicant stated that it has designed the Pressure Enabled Drug DeliveryTM technology of the Surefire® SparkTM Infusion System to overcome intratumoral pressure in solid tumors and improve distribution and penetration of therapy during Transcatheter Arterial Chemoembolization (TACE) procedures. TACE is a minimally invasive, image-guided procedure used to infuse a high dose of chemotherapy into liver tumors. According to the applicant, the pliable, one-way valve at the distal tip of the Surefire® SparkTM Infusion System creates a temporary local increase in pressure during infusion, opening up collapsed vessels in tumors, which enables perfusion and therapy delivery in areas inaccessible to the systemic circulation, a positive hydrostatic pressure gradient, and restores convective flow to enable therapy to penetrate deeper into the tumor. During the TACE procedure, the physician first gains catheter access into the arterial system of the hepatic arteries through a small incision in the groin or the wrist. The applicant stated that the physician then uses real-time fluoroscopic guidance to navigate the Surefire® SparkTM Infusion System into the blood vessels feeding the tumors, infusing the chemotherapy and embolic materials through the Surefire® SparkTM Infusion System until the tumor bed is completely saturated.
With respect to the newness criterion at § 419.66(b)(1), FDA granted 510(k) premarket clearance as of April 3, 2018. The application for a new device category for transitional pass-through payment status for the Surefire® SparkTM Infusion System was received on November 29, 2018, which is within 3 years of the date of the initial FDA approval or clearance. We invited public comments on whether the Surefire® SparkTM Infusion System meets the newness criterion.
Comment: The manufacturer of Surefire® SparkTM Infusion System believed this device meets the eligibility criteria for device pass-through payment under the regulation at § 419.66, which includes the newness criterion.
Response: We appreciate the commenter's input. After consideration of the public comments we received and based on the fact that the Surefire® SparkTM Infusion System application was received within 3 years of FDA approval, we believe that the Surefire® SparkTM Infusion System meets the newness criterion.
With respect to the eligibility criterion at § 419.66(b)(3), according to the applicant, the use of the Surefire® SparkTM Infusion System is integral to the service of providing delivery of chemotherapy into liver tumors, is used for one patient only, comes in contact with human skin, and is applied in or on a wound or other skin lesion. The applicant also claimed the Surefire® SparkTM Infusion System meets the device eligibility requirements of § 419.66(b)(4) because it is not an instrument, apparatus, implement, or items for which depreciation and financing expenses are recovered, and it is not a supply or material furnished incident to a service. We invited public comments on whether the Surefire® SparkTM Infusion System meets the eligibility criteria at § 419.66(b).
Comment: The manufacturer of Surefire® SparkTM Infusion System believed that that the Surefire® SparkTM Infusion System met the eligibility criteria at § 419.66(b).
Response: We appreciate the commenter's input. Based on the information we have received and our review of the application, we have determined that Surefire® SparkTM Infusion System meets the eligibility criterion at § 419.66(b)(3) and (b)(4).
The criteria for establishing new device categories are specified at § 419.66(c). The first criterion, at § 419.66(c)(1), provides that CMS determines that a device to be included in the category is not appropriately described by any of the existing categories or by any category previously in effect, and was not being paid for as an outpatient service as of December 31, 1996. We identified several existing pass-through payment categories that may be applicable to the Surefire® SparkTM Infusion System. The Surefire® SparkTM Infusion System may be described by HCPCS code C1887 (Catheter, guiding (may include infusion/perfusion capability)). The applicant describes the Surefire® SparkTM Infusion System as a device used in vascular interventional procedures to deliver diagnostic and therapeutic agents in the peripheral vasculatures. The CMS List of Device Category Codes for Present or Previous Pass-Through Payment and Related Definitions describes HCPCS code C1887 as intended for the introduction of interventional/diagnostic devices into the coronary or peripheral vascular systems. In the CY 2020 OPPS/ASC proposed rule, we also stated that the Surefire® SparkTM Infusion System may also be described by HCPCS code C1751 (Catheter, infusion, inserted peripherally, centrally or midline (other than hemodialysis)). The applicant describes the Surefire® SparkTM Infusion System as being inserted through a small incision in the groin or the wrist. We invited public comments on this issue.
Comment: The manufacturer of the device does not believe there is an existing pass-through payment category that describes the Surefire® SparkTM Infusion System, commenting that the existing device categories that CMS identified do not adequately describe critical aspects of the device. The manufacturer noted that existing categories, such as C1887 Catheter, guiding (may include infusion/perfusion capability) and C1751 Catheter, infusion, inserted peripherally, centrally or midline (other than hemodialysis)—do not appropriately describe catheters with a pressure-enabled drug delivery (PEDD) valve, a key mechanism of action of the Surefire® SparkTM Infusion System. The manufacturer stated that the PEDD valve is closely associated with differential and improved outcomes as compared to catheters without PEDD valves and is not appropriately described by existing categories.
Response: We appreciate the commenter's input. After consideration of the public comments we received, we believe there is no existing pass-through payment category that appropriately describes the Surefire® SparkTM Infusion System, due to the pressure-enabled drug delivery (PEDD) valve which offers a unique mechanism for therapy delivery. Based on this information, we believe that the Surefire® SparkTM Infusion System meets the eligibility criterion.
The second criterion for establishing a device category, at § 419.66(c)(2), provides that CMS determines that a device to be included in the category has demonstrated that it will substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment. With respect to this criterion, the applicant submitted four studies to support the claim that their technology represents a substantial clinical improvement over existing technologies. The applicant asserts that the Surefire® SparkTM Infusion System represents a substantial clinical improvement over existing technologies because it offers a treatment option that no other catheters currently available can provide. The manufacturer notes that the self-expanding, nonocclusive, one-way valve can infuse therapy at pressure higher than the baseline mean arterial pressure, and this pressurized delivery opens up collapsed vessels in tumors and enables perfusion and therapy delivery into hypoxic areas of the liver tumors. The applicant also believes that the Surefire® SparkTM Infusion System represents a substantial clinical improvement because the technology has shown improved tumor response rates in hepatocellular carcinoma, as well as a decrease in the rate of disease recurrence and the need for subsequent treatment.
The first pilot study of nine patients being treated for hepatocellular carcinoma, who received infusions via both a conventional end-hole catheter and an antireflux microcatheter, demonstrated statistically significant reductions in downstream distribution of embolic particles with the antireflux catheter and increases in tumor deposition (p < 0.05).[13] The second singlecenter retrospective study was conducted with 22 patients treated for hepatocellular carcinoma with the Surefire® SparkTM Infusion System and TACE. As assessed by MRI, there appeared to be overall disease response in 91 percent of patients and 85 percent of lesions and complete response in 32 percent of patients and 54 percent of lesions.[14] In the first study for a case-control series, 19 patients undergoing treatment using SIS-TACE had a statistically significant improvement in disease response rate compared to 19 patients treated with end-hole microcatheters, 78.9 percent compared to 36.8 percent for initial overall response rate (p = 0.008).[15] In the second study, a multi-center registry of 72 patients demonstrated high response rate when compared to historical control at 6 months follow-up.[16]
Based on the information submitted by the applicant, one concern was that large-scale studies with long-term follow-up were limited. Also, the majority of studies presented had a sample size of less than 25 and the highest sample size presented was less than 100 patients. Additionally, patient follow-up occurred mostly within a 3 to 6 month timeframe with few studies occurring beyond this range. Another concern was that none of the studies presented improvements in mortality with the use of the Surefire® SparkTM Infusion System. Outcomes focused primarily on tumor response rates and lesion size, based upon imaging. We noted additional data on mortality endpoints would be helpful to fully assess substantial clinical improvement. We invited public comments on whether the Surefire® SparkTM Infusion System meets the substantial clinical improvement criterion.
Comment: The manufacturer responded to several statements regarding Surefire® SparkTM Infusion System and substantial clinical improvement in the CY 2020 OPPS/ASC proposed rule, and asserted that SparkTM Infusion System meets the substantial clinical improvement criterion. The manufacturer stated that the population size in the studies submitted to CMS are normal for a new and innovative technology, noting that the studies are methodologically rigorous and show statistically significant differentiation from comparators. The manufacturer also noted that overall survival is not an appropriate endpoint for hepatocellular carcinoma. They cited National Comprehensive Cancer Network (NCCN) guidelines, noting that tumor necrosis and pathologic response are primary predictors of success in these cases and locoregional therapy should be viewed as a way to transition patients to transplant or resection. The manufacturer also suggested that CMS should consider that clinical improvements vary based on the therapeutic agent being delivered by the SparkTM Infusion System and that these agents are approved on a variety of endpoints.
Response: We appreciate the response to the questions we had regarding SparkTM Infusion System. After reviewing the information provided in the public comment, we agree that while the opportunity for large-scale studies with long-term follow-up is limited for a new technology, the existing studies show statistically significant improvements. Additionally, with regard to our questions about impacts on mortality, we accept the applicant's statement that there are other key clinical endpoints, such as tumor necrosis and progression-free survival, that can be used to assess improvements from the SparkTM Infusion System.
Comment: Multiple commenters supported granting SparkTM Infusion System transitional pass-through payment status. Many of the commenters mentioned that SparkTM Infusion System provides substantial clinical benefit over conventional therapy and urged CMS to approve the transitional pass-through payment to reduce cost burden and increase patient access.
Response: We appreciate the additional information that the commenters provided on the performance and the benefits of SparkTM Infusion System.
After consideration of the public comments we received, we have determined that SparkTM Infusion System does meet the substantial clinical improvement criterion.
The third criterion for establishing a device category, at § 419.66(c)(3), requires us to determine that the cost of the device is not insignificant, as described in § 419.66(d). Section 419.66(d) includes three cost significance criteria that must each be met. The applicant provided the following information in support of the cost significance requirements. The applicant stated that the Surefire® SparkTM Infusion System would be reported with CPT code 37243, which is assigned to APC 5193 (Level 3 Endovascular Procedures). To meet the cost criterion for device pass-through payment status, a device must pass all three tests of the cost criterion for at least one APC. For our calculations, we used APC 5193, which has a CY 2019 payment rate of $9,669.04. Beginning in CY 2017, we calculated the device offset amount at the HCPCS/CPT code level instead of the APC level (81 FR 79657). CPT code 37243 had a device offset amount of $3,894.69 at the time the application was received. According to the applicant, the cost of the Surefire® SparkTM Infusion System is $7,750.
Section 419.66(d)(1), the first cost significance requirement, provides that the estimated average reasonable cost of devices in the category must exceed 25 percent of the applicable APC payment amount for the service related to the category of devices. The estimated average reasonable cost of $7,750 for the Surefire® SparkTM Infusion System is 80.2 percent of the applicable APC payment amount for the service related to the category of devices of $9,669.04 ($7,750/$9,669.04 × 100 = 80.2 percent). Therefore, we believe the Surefire® SparkTM Infusion System meets the first cost significance requirement.
The second cost significance requirement, at § 419.66(d)(2), provides that the estimated average reasonable cost of the devices in the category must exceed the cost of the device-related portion of the APC payment amount for the related service by at least 25 percent, which means that the device cost needs to be at least 125 percent of the offset amount (the device-related portion of the APC found on the offset list). The estimated average reasonable cost of $7,750 for the Surefire® SparkTM Infusion System exceeds the cost of the device-related portion of the APC payment amount for the related service of $3,894.69 by 199 percent ($7,750−$3,894.69) × 100 = 198.99 percent). Therefore, we believe that the Surefire® SparkTM Infusion System meets the second cost significance requirement.
The third cost significance requirement, at § 419.66(d)(3), provides that the difference between the estimated average reasonable cost of the devices in the category and the portion of the APC payment amount for the device must exceed 10 percent of the APC payment amount for the related service. The difference between the estimated average reasonable cost of $7,750 for the SparkTM Infusion System and the portion of the APC payment amount for the device of $3,894.69 exceeds the APC payment amount for the related service of $9,669.04 by 40 percent (($7,750−$3,894.69)/$9,669.04) × 100 = 39.87 percent). Therefore, we believe that the Surefire® SparkTM Infusion System meets the third cost significance requirement.
We invited public comments on whether the Surefire® SparkTM Infusion System meets the device pass-through payment criteria discussed in this section, including the cost criterion.
Comment: The manufacturer of the Surefire® SparkTM Infusion System believed that the device meets the cost criterion for device pass-through payment status.
Response: We appreciate the manufacturer's input. After consideration of the public comments we received, we believe that Surefire® SparkTM Infusion System meets the cost criterion for device pass-through payment status.
After consideration of the public comments we received, we are approving the Surefire® SparkTM Infusion System for device pass-through payment status beginning in CY 2020.
(2) TracPatch
According to the applicant, TracPatch is a wearable device that utilizes an accelerometer, temperature sensor and step counter to allow the surgeon and patient to monitor recovery and help ensure critical milestones are being met. The applicant states that TracPatch utilizes wearable monitoring technology and methods in an effort to enhance the rehabilitation experience for both patients and physicians. Accelerometers are utilized to recognize and record the results when patients perform standard physical therapy exercises, in addition to providing standard step count and high-acceleration events that may indicate a fall. A temperature sensor monitors the skin temperature near the joint.
TracPatch is described by the applicant as a 24/7 remote monitoring wearable device that captures a patient's key daily activities: such as range of motion progress, exercise compliance, and ambulation. TracPatch is used for pre- and post-operative patient monitoring, patient engagement, data analytics and post-op cost reduction.
According to the applicant, the wearable devices stick on the skin above and below the knee. The wearables are applied before total knee surgery to determine a patient's baseline activity levels, and then again after surgery to allow the patient and surgeon to monitor activity, pain, range of motion and physical therapy. The use of the Bluetooth connectivity allows the device to be paired with any smartphone and the TracPatch cloud allows for unlimited data collection and storage. The applicant states that TracPatch includes a web dashboard and computer application, which permit a health care provider to monitor a patient's recovery in real-time, allowing for immediate care adjustments and the ability for providers and patients to respond to issues that may occur during recovery from surgery.
With respect to the newness criterion at § 419.66(b)(1), the applicant stated that TracPatch does not need FDA clearance because it is a Class I device that would be assigned to a generic category of devices described in 21 CFR parts 862 through 892 that is exempt from FDA premarket notification. However, the applicant did not identify which category of exempted devices that TracPatch would be assigned. The applicant also stated that TracPatch will be introduced into the market in 2019, which would be within 3 years of the device pass-through payment application for TracPatch that was received in March 2019. We invited public comments on whether the TracPatch is exempt from FDA clearance and if the TracPatch meets the newness criterion.
Comment: One commenter, the manufacturer, stated that they had registered TracPatch as a Class I Exempt goniometer with FDA which was listed on the Global Unique Device Identification Database (GUDID) as of August 28, 2019.
Response: We thank the manufacturer for clarifying that TracPatch is now registered with FDA as a Class I Exempt goniometer as of August 28, 2019.
After consideration of the public comments, we have determined that TracPatch meets the newness criterion.
With respect to the eligibility criterion at § 419.66(b)(3), the applicant claimed that the TracPatch is an integral part of monitoring the range of motion for a knee prior to and after total knee arthroplasty, is used for one patient only, and is placed on the skin above and below the knee and secured by Velcro strips. The applicant stated that the device is not surgically implanted or inserted into the patient and is not applied in or on a wound or other skin lesion. We stated concerns in the proposed rule with TracPatch's eligibility with respect to the criterion at § 419.66(b)(3) because to be eligible for pass-through payment a device must be surgically implanted or inserted into the patient or applied in a wound or on other skin lesions. In addition, the applicant stated that the TracPatch meets the device eligibility requirements of § 419.66(b)(4) because it is not an instrument, apparatus, implement, or item for which depreciation and financing expenses are recovered. We determined that TracPatch was not a material or supply furnished incident to a service. We invited public comments on whether the TracPatch meets the eligibility criterion.
Comment: One commenter, the manufacturer, provided more information on whether TracPatch meets the eligibility criterion. The manufacturer states that the device is adhered to a patient's skin using a medical adhesive patch and not Velcro strips and that the device is placed near a wound (which we assume is the incision for the associated knee surgery) in a sterile setting. The placement of the device near the wound allows real time monitoring of changes to the wound and complications and abnormalities that may arise. Also the device placement is important to perform measurements related to the knee's range of motion.
Response: The commenter did not state or provide evidence either in its device pass-through application or in its comment on the CY 2020 OPPS/ASC proposed rule, that the TracPatch device is surgically implanted or inserted into a patient or is applied in a wound or on other skin lesions. In fact, the description of the Class I Exempt goniometer on the FDA product classification web page states that the goniometer is not an implantable device. To be considered for device pass-through payment, a device must meet this part of the eligibility criterion.
After consideration of all of the information we have received, we have determined that TracPatch is not surgically implanted or inserted into a patient or applied in a wound or on other skin lesions, and the product thus does not meet the eligibility criterion for device pass-through payment status. Because we have determined that TracPatch does not meet the basic eligibility criterion for transitional pass-through payment status, we have not evaluated this product to determine whether it meets the other criteria required for transitional pass-through payment for devices; that is the substantial clinical improvement criterion, and the cost criterion.
Comment: Multiple commenters, including physicians and patients, described the benefits of TracPatch and how it helped either them or their patients with their recoveries from knee surgery.
Response: We appreciate the comments we received about the benefits of TracPatch. However, we did not evaluate substantial clinical improvement for TracPatch because it did not meet the eligibility criterion.
After consideration of the public comments we received, we are not approving device pass-through payment status for TracPatch for CY 2020.
(3) Vagus Nerve Stimulation (VNS) Therapy® System for Treatment Resistant Depression (TRD)
LivaNova USA Inc. submitted an application for the Vagus Nerve Stimulation (VNS) Therapy® System for Treatment Resistant Depression (TRD). According to the applicant, the VNS Therapy® System consists of two implantable components: A programmable electronic pulse generator and a bipolar electrical lead that is connected to the programmable electronic pulse generator. The applicant stated that the surgical procedure to implant the VNS Therapy® System involves subcutaneous implanting of the pulse generator in the intraclavicular region as well as insertion of the bipolar electrical lead which entails wrapping two spiral electrodes around the cervical portion of the left vagus nerve within the carotid sheath.
According to the applicant, following implant and recovery, the physician programs the pulse generator to intermittently stimulate the vagus nerve at a level that balances efficacy and patient tolerability. The pulse generator delivers electrical stimulation via the bipolar electrical lead to the cervical portion of the left vagus nerve within the carotid sheath thereby relaying information to the brain stem modulating structures relevant to depression. Stimulation typically consists of a 30-second period of “on time,” during which the device stimulates at a fixed level of output current, followed by a 5-minute “off time” period of no stimulation.
The applicant states that a hand-held programmer is utilized to program the pulse generator stimulation parameters, including the current charge, pulse width, pulse frequency, and the on/off stimulus time, which is also known as the on/off duty cycle. Initial settings can be adjusted to enhance the tolerability of the device as well as its clinical effects on the patient. The generator runs continuously, but patients can temporarily turn off the device by holding a magnet over it. The generator can also be turned on and off by the programmer.
The applicant states that the VNS Therapy® System provides indirect modulation of brain activity through the stimulation of the vagus nerve. The vagus nerve, the tenth cranial nerve, has parasympathetic outflow that regulates the autonomic (that is, involuntary) functions of heart rate and gastric acid secretion, and also includes the primary functions of sensation from the pharynx, muscles of the vocal cords and swallowing. It is a nerve that carries both sensory and motor information to and from the brain. Importantly, the vagus nerve has influence over widespread brain areas and it is believed that electrical stimulation of the vagus nerve alters various networks of the brain in order to treat psychiatric disease.
With respect to the newness criterion at § 419.66(b)(1), the applicant received FDA clearance for the VNS Therapy® System for TRD through the premarket approval (PMA) process on July 15, 2005, and the VNS Therapy® for TRD device was introduced to the market in September 2005. However, on May 4, 2007, a national coverage determination (NCD 160.18) was released prohibiting Medicare from covering the use of the VNS Therapy® System for TRD. This NCD remained in effect until February 15, 2019, when CMS determined that the VNS Therapy® for TRD could receive payment if the service was performed in CMS-approved coverage with evidence development (CED) studies. Although the VNS Therapy® System for TRD was introduced to the market in September 2005, Medicare has only covered it for slightly more than 11/2 years. However, § 419.66(b)(1) states that a pass-through payment application for a device must be received within 3 years of when the device either received FDA approval or was introduced to the market. The applicant stated that the VNS Therapy® System for TRD was introduced to the market in September 2005, which means the device pass-through payment application would have needed to have been submitted to CMS by September 2008. However, the pass-through application for the device was not received by CMS until March 2019.
In addition, it appeared that the neurostimulator device for the VNS Therapy® System for TRD is the same device that has been used since 1997 to treat epilepsy.[17] The applicant stated the following three differences between the two devices: (1) How the device is programmed to treat epilepsy versus TRD; (2) how the external magnets of the device are used for epilepsy treatment as compared to TRD treatment; and (3) that the battery life of the device to treat epilepsy is different than the battery life of the device when treating TRD. However, it was not clear that these differences demonstrate that the actual device used to treat TRD is any different than the device used to treat epilepsy.
Based on the information presented, we invited public comments on whether the VNS Therapy® System for TRD meets the newness criterion.
Comment: One commenter, the manufacturer, made additional arguments for why the VNS Therapy® System for TRD meets the newness criterion. The manufacturer stated that there were 22 months between the FDA approval of the associated procedure to treat TRD in July 2005 and CMS' issuance of the national determination of non-coverage on May 4, 2007. The manufacturer asserts that during those 22 months the VNS Therapy® System for TRD was “realistically not available” because of concerns about covering the TRD treatment procedure during the period between FDA approval and the national determination of non-coverage. In another part of the manufacturer's comment, they state that the uncertainty of coverage for the TRD treatment procedure meant that the treatment was not available to patients during the July 2005 to May 2007 time period.
The manufacturer believes the most equitable reading of the rule that is consistent with the intent of the criterion when it was established in the CY 2016 OPPS final rule (80 FR 70418 through 70420) is that the 3-year period for newness from when the VNS Therapy® System for TRD was introduced into the market in July 2015 should have been held in suspension from May 4, 2007 when the original national determination of non-coverage by CMS until the subsequent national determination allowing coverage of the VNS Therapy® System for TRD with coverage with evidence development (CED) was released on February 15, 2019.
The manufacturer cites CMS statements from the CY 2016 OPPS final rule supporting this reading, including that device pass-through payment is for devices that are truly new and do not have sufficient claims data for CMS to analyze, and that market availability for a device could be considered to be after its FDA approval or clearance date where there is a national coverage determination of non-coverage of the device within the Medicare population. The manufacturer asserts that the reason that the newness criterion does not address the market availability situation faced by the VNS Therapy® System for TRD is that CMS simply did not envision that such a situation would occur. The manufacturer asserts that the VNS Therapy® System for TRD neurostimulator device has not been available in the market for 3 full years, and therefore still meets the newness criterion.
Response: We disagree with the commenter's conclusion. The manufacturer did not provide evidence to establish that the neurostimulator device for the VNS Therapy® System for TRD was not similar to the neurostimulator device that has been used since 1997 to treat epilepsy. With no evidence to the contrary, it appears the neurostimulator device for the VNS Therapy® System for TRD has been on the market continuously since 1997 and therefore fails the newness criterion.
However, even if we were to assume the neurostimulator device for the VNS Therapy® System for TRD was a new device upon FDA approval for the TRD treatment procedure in July 2005, the device would still not meet the newness criterion. The manufacturer's comment about suggesting an equitable reading of the newness criterion consistent with what it believed was our intent in the CY 2016 OPPS final rule (80 FR 70418 through 70420) implied that, for a device to meet the newness standard, it had to be available in the market for less than three years and that the availability period would be suspended if the device was unavailable in the market due to national non-coverage. This comment does not align with the language of § 419.66(b)(1), which states that the application for device pass-through payment must be received within 3 years from the date of market availability and makes no exception for periods of national non-coverage. As we stated in the proposed rule, based on information provided in the original device pass-through application, the device pass-through application had to be submitted by September 2008 to meet the newness requirement.
Comment: One commenter stated that it did not believe that the VNS Therapy® System for TRD meets the newness criterion for device pass-through payment. The commenter states that while there have been technical improvements with the VNS Therapy® System for TRD, the commenter believes these are typical upgrades of an existing technology and not evidence of a new device.
Response: We appreciate the feedback from the commenter, including their concern that the differences cited by the manufacturer between the neurostimulator VNS device to treat epilepsy and the neurostimulator VNS device to treat TRD are not substantial enough to establish the VNS Therapy® System for TRD neurostimulator device as a new device that meets the newness criterion. A device also will fail the newness criterion if, as noted above, it is on the market more than three years, based either on its FDA clearance or approval date or the date of U.S. market availability.
After consideration of all of the information we have received, we have determined that the VNS Therapy® System for TRD does not meet the newness criterion.
With respect to the eligibility criterion at § 419.66(b)(3), the applicant claimed that the VNS Therapy® System for TRD is an integral part of a procedure to provide adjunctive treatment of chronic or recurrent depression in adult patients that have failed four or more antidepressant treatments. The VNS Therapy® System for TRD is used for one patient only, comes in contact with human tissue, and is surgically implanted or inserted into the patient. In addition, the applicant stated that the VNS Therapy® System for TRD meets the device eligibility requirements of § 419.66(b)(4) because it is not an instrument, apparatus, implement, or item for which depreciation and financing expenses are recovered. We determined that the VNS Therapy® for TRD was not a material or supply furnished incident to a service. We invited public comments on whether the VNS Therapy® for TRD meets the eligibility criterion.
Comment: One commenter, the manufacturer, claimed that the VNS Therapy® for TRD device meets the basic eligibility criteria for pass-through status. The device is an integral part of the service provided which is the adjunctive treatment of TRD. The device is used by one patient, comes in contact with human tissue and is surgically implanted. The manufacturer also asserts that the device is not an instrument, apparatus, implement, or item for which depreciation and financing expenses are recovered. The manufacturer states that the device is not a material or supply furnished incident to a service.
Response: We appreciate the additional comments from the manufacturer. After consideration of all of the information we have received, we have determined that the VNS Therapy® System for TRD does meet the device eligibility criterion as described by § 419.66(b)(4).
The criteria for establishing new device categories are specified at § 419.66(c). The first criterion, at § 419.66(c)(1), provides that CMS determines that a device to be included in the category is not appropriately described by any existing categories or by any category previously in effect, and was not being paid for as an outpatient service as of December 31, 1996. With respect to the existence of a previous pass-through device category that describes the device used for the VNS Therapy® System for TRD, the applicant suggested a category descriptor of “Generator, neurostimulator (implantable), treatment resistant depression, non-rechargeable.” However, the device category represented by HCPCS code C1767 is described as “Generator, neurostimulator (implantable), non-rechargeable,” which appears to encompass the device category descriptor for the VNS Therapy® System for TRD suggested by the applicant. The applicant asserts that the device category descriptor for HCPCS code C1767 is overly broad and noted the establishment of HCPCS code C1823 (Generator, neurostimulator (implantable), nonrechargeable, with transvenous sensing and stimulation leads), effective January 1, 2019, as an example of where a new device category for a nonrechargeable neurostimulation system to treat central sleep apnea was carved out from the broad category described by HCPCS code C1767.
The applicant believes its proposed category for the device for the VNS Therapy® System for TRD should similarly qualify as a new category. However, HCPCS code C1823 was established due to specific device features which distinguish that device category from HCPCS code C1767. The applicant for the VNS Therapy® System for TRD requested a new device category based on a beneficiary's diagnosis, but OPPS does not differentiate payment by diagnosis.
Comment: The applicant asserts that the VNS Therapy® for TRD device is not described by any of the existing device categories in the OPPS and that the associated service was not paid as an outpatient service as of December 31, 1996.
Response: We do not agree with the applicant's assertion. We believe the VNS Therapy® for TRD device is described by existing HCPCS code C1767 (Generator, neurostimulator (implantable), non-rechargeable) and does not meet the criterion that is described by § 419.66(c)(1) because the device is described by an existing device category. As stated in the proposed rule, OPPS does not differentiate payment by diagnosis and therefore cannot establish new device categories based solely on a previously described device being used to treat a new indication. In the original pass-through application, the applicant cited the example of the establishment of a new category code, HCPCS code C1823 (Generator, neurostimulator (implantable), nonrechargeable, with transvenous sensing and stimulation leads), for the remede system even though that device is a non-rechargeable neurostimulator and initially appeared to be covered by HCPCS code C1767, like the VNS Therapy® for TRD device. However, as we stated in the proposed rule, HCPCS code C1823 was established due to specific device features that distinguish that device category from HCPCS code C1767. The applicant has not identified any device features of the VNS Therapy® for TRD device that distinguish it from the category described by HCPCS code C1767.
After consideration of all of the information we have received, we have determined that the VNS Therapy® System for TRD is described by either an existing category or by a category previously in effect and does not meets the requirements of § 419.66(c)(1) and the device category eligibility criterion.
Because we have determined that the VNS Therapy® System for TRD does not meet either the newness criterion or the device category eligibility criterion for transitional pass-through payment status, we have not evaluated this device to determine whether it meets the other criteria required for transitional pass-through payment for devices; namely, the substantial clinical improvement criterion and the cost criterion.
Comment: A commenter supported giving pass-through status for the VNS Therapy® System for TRD because the commenter believes the clinical benefits of the VNS Therapy® System for TRD have been demonstrated by the studies submitted for the recent national coverage determination that established coverage with evidence development for the procedure.
Response: We appreciate the comment in support of the clinical benefits of the VNS Therapy® System for TRD. However, we did not evaluate substantial clinical improvement for the VNS Therapy® System for TRD because this device does not meet the newness criterion or the device category eligibility criterion.
After consideration of the public comments we received, we are not approving VNS Therapy® System for TRD device pass-through payment status for CY 2020.
(4) Optimizer® System
Impulse Dynamics submitted an application for a new device category for transitional pass-through payment status for the Optimizer® System. According to the applicant, the Optimizer® System is an implantable device that delivers Cardiac Contractility Modulation (CCM) therapy for the treatment of patients with moderate to severe chronic heart failure. CCM therapy is intended to treat patients with persistent symptomatic heart failure despite receiving guideline directed medical therapy (GDMT). The applicant stated that the Optimizer System consists of the Optimizer Implantable Pulse Generator (IPG), Optimizer Mini Charger, and Omni II Programmer with Omni Smart Software. Lastly, the applicant stated that the Optimizer® System delivers CCM signals to the myocardium. CCM signals are nonexcitatory electrical signals applied during the cardiac absolute refractory period that, over time, enhance the strength of cardiac muscle contraction.
With respect to the newness criterion at § 419.66(b)(1), the applicant received a Category B-3 Investigational Device Exemption (IDE) from FDA on April 6, 2017. Subsequently, the applicant received its premarket approval (PMA) application from FDA on March 21, 2019. We received the application for a new device category for transitional pass-through payment status for the Optimizer® System on February 26, 2019, which is within 3 years of the date of the initial FDA approval or clearance. We invited public comments on whether the Optimizer® System meets the newness criterion.
Comment: The manufacturer believes that the Optimizer® System meets the newness criterion.
Response: We appreciate the commenter's input. After consideration of the public comment we received, we believe that the Optimizer® System meets the newness criterion.
With respect to the eligibility criterion at § 419.66(b)(3), according to the applicant, the Optimizer® System is integral to the CCM therapy service provided, is used for one patient only, comes in contact with human skin, and is applied in or on a wound or other skin lesion. The applicant also stated that the Optimizer® System meets the device eligibility requirements of § 419.66(b)(4) because it is not an instrument, apparatus, implement, or items for which depreciation and financing expenses are recovered, and it is not a supply or material furnished incident to a service.
We did not receive any public comments regarding whether Optimizer® System meets the eligibility criterion. Based on the information we have received, we have determined that Optimizer® System meets the eligibility criterion.
The criteria for establishing new device categories are specified at § 419.66(c). The first criterion, at § 419.66(c)(1), provides that CMS determines that a device to be included in the category is not appropriately described by any of the existing categories or by any category previously in effect, and was not being paid for as an outpatient service as of December 31, 1996. For the proposed rule, we had not identified an existing pass-through payment category that describes the Optimizer® System.
Comment: The manufacturer of the Optimizer® System indicated that there is not an existing pass-through payment category that describes the device.
Response: We appreciate the commenter's input. After consideration of the public comment we received, we believe that the Optimizer® System meets the device category eligibility criterion.
The second criterion for establishing a device category, at § 419.66(c)(2), provides that CMS determines that a device to be included in the category has demonstrated that it will substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment. The applicant stated that the use of CCM significantly improves clinical outcomes for a patient population compared to currently available treatments. With respect to this criterion, the applicant submitted studies that examined the impact of CCM on quality of life, exercise tolerance, hospitalizations, and mortality.
The applicant noted that the use of the Optimizer® System significantly improves clinical outcomes for patients with moderate-to-severe chronic heart failure, and specifically improves exercise tolerance, quality of life, and functional status of patients that are otherwise underserved. The applicant claims that the Optimizer® System fulfills an unmet need because there is currently no therapeutic medical device therapies available for the 70 percent of heart failure patients who have New York Heart Association (NYHA) Class III heart failure, normal QRS duration and reduced ejection fraction (EF). FDA approved the Optimizer® System for NYHA Class III heart failure patients who remain symptomatic despite guideline directed medical therapy, who are in normal sinus rhythm, are not indicated for Cardiac Resynchronization Therapy, and have a left ventricular ejection fraction ranging from 25 percent to 45 percent.[18]
The applicant presented several studies to support these claims. According to the applicant, the results of a randomized clinical study in which patients with NYHA functional Class III, ambulatory Class IV heart failure despite OMT, an EF from 25-45 percent, or a normal sinus rhythm with QRS duration <130ms (n = 160) were randomized to continued medical therapy (n = 86) or CCM with the Optimizer® System (n = 74) for 24 weeks showed a statistically significant improvement in the primary endpoint of peak oxygen consumption (pVO2 = 0.84, 95 percent Bayesian credible interval 0.123 to 1.52) compared with the patients who were randomized to continued medical therapy.[19] The secondary endpoint of quality of life, measured by Minnesota Living with Heart Failure Questionnaire (MLWHFQ) (p<0.001), 6-minute hall walk test (p = 0.02), and an NYHA function class assessment (p<0.001) were better in the treatment group versus control group. The secondary endpoint of heart failure-related hospitalizations was lowered from 10.8 percent to 2.9 percent (p = 0.048). The applicant also reported a registry study of 140 patients with a left ventricular ejection fraction from 25-45 percent receiving CCM therapy with a primary endpoint of comparing observed survival to Seattle Heart Failure Model (SHFM) predicted survival over 3 years of follow-up. All patients implanted with the Optimizer® System at participating centers were offered participation and 72 percent of patients agreed to enroll in the registry. There were improvements in quality of life markers (MLWHFQ) and a 75-percent reduction in heart failure hospitalizations (p<0.0001). Survival at 3 years was similar between the two study arms with CCM at 82.8 percent [73.4 percent-89.1 percent] and SHFM at 76.7 percent (p = 0.16). However, for patients with a left ventricular ejection fraction from 35-45 percent receiving CCM therapy, the 3-year mortality for CCM therapy was significantly better than predicted with 88 percent for CCM compared to 74.7 percent for SHFM (p = 0.0463).[20] The applicant presented a randomized, double blind, crossover study of CCM signals with 164 patients with EF ≤35 percent and NYHA Class II (24 percent) or III (76 percent) symptoms who received a CCM pulse generator. After the 6-month treatment period, results indicated statistically significantly improved peak VO2 and MLWHFQ (p = 0.03 for each parameter), concluding that CCM signals appear to be safe for patients and that exercise tolerance and quality of life were significantly better while patients were receiving active CCM treatment.[21]
A study was conducted with 68 consecutive heart failure patients with NYHA Class II or III symptoms, QRS duration ≤130 ms, and who had been implanted with a CCM device between May 2002 and July 2013 in Germany. Based upon pre-implant SHFM survival rates, 4.5 years mean follow-up, and an average patient age of 61 years old, the study found lower mortality rates for CCM therapy group with 0 percent at 1 year, 3.5 percent at 2 years, and 14.2 percent at 5 years, compared to 6.1 percent, 11.8 percent, and 27.7 percent predicted by SHFM, respectively (p = 0.007).[22] In a study on long-term outcomes, 41 consecutive heart failure patients with left ventricular ejection fraction (EF) < 40 percent receiving CCM therapy were compared to a control group of 41 similar heart failure patients and primarily evaluated for all-cause mortality, as well as heart failure hospitalization, cardiovascular death, and a death and heart failure hospitalization composite. After 6 years of follow-up, the results showed that all-cause mortality was lower for the CCM group as compared to the control group (39 percent versus 71 percent respectively, p = 0.001), especially among patients with EF ≥ 25-40 percent with 36 percent for the CCM group versus 80 percent for the control group (p <0.001). Although heart failure hospitalization was similar between the treatment and control cohorts, there was a significantly lower heart failure hospitalization rate for CCM patients with EF ≥ 25-40 percent (36 percent versus 64 percent respectively, p = 0.005).[23] The applicant also presented additional studies [24 25] that presented similar conclusions to the studies discussed above, noting that CCM therapy provided improvements in quality of life, exercise capacity, NYHA class, and mortality rates.
We noted several concerns with the studies presented by the applicant. One concern regarding the evidence for the Optimizer® System involves the mixed mortality outcomes presented. Three studies showed significantly lower mortality rates with the use of CCM compared to controls or predicted mortality. Each of these studies focused on slightly different mortality outcomes, including all-cause mortality, a composite of death and heart failure hospitalization, and cardiac mortality rates from 1 to 5 years. Two studies show mixed results. For the first, 3-year survival was not significant for the overall population, despite a significantly higher survival rate found in a subpopulation. For the second, mortality rates were significant compared to predictions at 1 year, but not 3 years. The final study did not report significance in its overall survival at 2 years. Although the studies and trials presented show improvements in mortality when evaluating CCM therapy with comparators, the studies have small sample sizes and limited timeframes for measuring survival. Additionally, three studies compared observed mortality rates to statistically projected mortality rates. In the two studies with observed mortality rates, the overall improvement in mortality was not significant, despite some significance found in subanalyses. These issues raise concerns about the strength of the conclusions related to the use of CCM therapy improving patient outcomes.
Another concern with the studies presented for the Optimizer® System is that the included study population may not be necessarily representative of the Medicare beneficiary population. Several studies had a predominantly white, male patient population, which could make generalization of study results to a more diverse Medicare population difficult. Additionally, the average age of patients for several studies was under 65 years old, which may also be a limitation in applying these study results to the Medicare population.
Overall, we were concerned that there was a lack of evidence from large trials for the CCM therapy provided by the Optimizer® System. The studies presented had sample sizes fewer than 500 patients. Other limitations include the potential placebo effects and selection bias that may have impacted study results. Only two studies presented were randomized and only one of those two was a double-blinded study. For the remaining studies, no blinding occurred to minimize potential biases, which indicates that patients and researchers knew they were receiving CCM therapy. This is a limitation because observed outcomes may be impacted by the placebo effect. Although most studies matched participants for similar demographics, there could be systematic differences and unmeasured bias between the two groups beyond the similarities addressed in the study that could affect outcomes. The lack of randomization may have implications for the strength of the studies' conclusions.
Based upon the evidence presented, we invited public comments on whether the Optimizer® System meets the substantial clinical improvement criterion.
Comment: The manufacturer responded to several statements regarding Optimizer® System and substantial clinical improvement in the CY 2020 OPPS/ASC proposed rule, and asserted that Optimizer® System meets the substantial clinical improvement criterion. The manufacturer noted that a mortality benefit cannot be claimed based on currently published data but that the Optimizer® System does not appear to have a negative impact on mortality. The manufacturer acknowledged that male patients and those that identify as white were prevalent in the Optimizer System studies but contended that for clinical trials in general, and for heart failure specifically, these groups are typically over-represented. They presented several examples of cardiac device and pharmaceutical clinical trials for the treatment of heart failure, where a similar mix of patients in terms of gender and race existed across unrelated trials and therapies. In response to the concern that the average age of patients for several studies was under 65 years old, limiting the application of the study results to the Medicare population, the manufacturer conducted additional analyses on patients aged 65 and older. The analysis showed that the two populations were not dissimilar, and the manufacturer believes the clinical trial results are applicable to the Medicare patient population.
The manufacturer presented data to demonstrate that the Optimizer® System delivers substantial clinical improvement in terms of improved functional status, quality of life, and exercise tolerance. In response to the concern regarding clinical trials enrolling sample sizes fewer than 500 patients, the manufacturer noted that there were 638 subjects enrolled and implanted with the Optimizer System in the U.S. randomized trials and that trials of this size are common in Class III medical device trials, which are tailored for gathering the required evidence to support FDA approval of novel technology. Regarding the concern about the lack of randomization and blinding in studies presented, the manufacturer noted that four out of the six studies were randomized, and two of the four were also blinded with both the control and the treatment group receiving the device.
Response: We appreciate the response to the questions we had regarding Optimizer® System. After reviewing the additional information provided during the public comment period, we agree that, for patients with NYHA Class III heart failure patients who remain symptomatic despite guideline directed medical therapy, who are in normal sinus rhythm, are not indicated for Cardiac Resynchronization Therapy, and have a left ventricular ejection fraction ranging from 25 percent to 45 percent, Optimizer® System is a substantial clinical improvement over existing treatment options for this population. The provided studies support improvements in functional status, quality of life, and exercise tolerance, all of which are relevant outcomes in this population. While the studies describe improved survival in a subset of patients and substantially reduced hospitalizations, the numbers are small, the observation period is short, and the data on readmissions are not specifically highlighted. However, we accept the manufacturer's note that while mortality benefit cannot be claimed based on currently published data, the Optimizer® System does not appear to have a negative impact on mortality.
Accordingly, we have determined that the Optimizer® System has demonstrated substantial clinical improvement relative to existing treatment options for patients diagnosed with moderate to severe chronic heart failure. As the Optimizer® System received a Breakthrough Device designation from FDA, it meets the substantial clinical improvement criterion under this alternative pathway as well.
The third criterion for establishing a device category, at § 419.66(c)(3), requires us to determine that the cost of the device is not insignificant, as described in § 419.66(d). Section 419.66(d) includes three cost significance criteria that must each be met. The applicant provided the following information in support of the cost significance requirements. The applicant stated that the Optimizer® System would be reported with CPT codes 0408T, 0409T, 0410T, 0411T, 0412T, 0413T, 0414T, 0415T, 0416T, 0417T, and 0418T. The associated APCs are APC 5231 (Level 1 ICD and Similar Procedures) and APC 5222 (Level 2 Pacemaker and Similar Procedures). To meet the cost criterion for device pass-through payment status, a device must pass all three tests of the cost criterion for at least one APC. For our calculations, we used APC 5222, which had a CY 2019 payment rate of $7,404.11 at the time the application was received. Beginning in CY 2017, we calculate the device offset amount at the HCPCS/CPT code level instead of the APC level (81 FR 79657). CPT code 0410T had a device offset amount of $2,295.27 at the time the application was received. According to the applicant, the cost of the Optimizer® System was $15,700.
Section 419.66(d)(1), the first cost significance requirement, provides that the estimated average reasonable cost of devices in the category must exceed 25 percent of the applicable APC payment amount for the service related to the category of devices. The estimated average reasonable cost of $15,700 for the Optimizer® System exceeds 212 percent of the applicable APC payment amount for the service related to the category of devices of $7,404.11 ($15,700/$7,404.11 × 100 = 212 percent). Therefore, we believe the Optimizer® System meets the first cost significance requirement.
The second cost significance requirement, at § 419.66(d)(2), provides that the estimated average reasonable cost of the devices in the category must exceed the cost of the device-related portion of the APC payment amount for the related service by at least 25 percent, which means that the device cost needs to be at least 125 percent of the offset amount (the device-related portion of the APC found on the offset list). The estimated average reasonable cost of $15,700 for the Optimizer® System exceeds the cost of the device-related portion of the APC payment amount for the related service of $2,295.27 by 684 percent ($15,700/$2,295.27) × 100 = 684 percent. Therefore, we believe that the Optimizer® System meets the second cost significance requirement.
The third cost significance requirement, at § 419.66(d)(3), provides that the difference between the estimated average reasonable cost of the devices in the category and the portion of the APC payment amount for the device must exceed 10 percent of the APC payment amount for the related service. The difference between the estimated average reasonable cost of $15,700 for the Optimizer® System and the portion of the APC payment amount for the device of $2,295.27 exceeds the APC payment amount for the related service of $7,404.11 by 181 percent (($15,700 − $2,295.27)/$7,404.11) × 100 = 181 percent). Therefore, we believe that the Optimizer® System meets the third cost significance requirement.
We invited public comments on whether the Optimizer® System meets the device pass-through payment criteria discussed in this section, including the cost criterion for device pass-through payment status.
Comment: The manufacturer of the Optimizer® System believed that the device meets the cost criterion for device pass-through payment status. The manufacturer noted a point of clarification regarding the average sales price (ASP) of the Optimizer® System used for these calculations. They stated that the $15,700 price in the application was based on discounted clinical trial pricing used during the FDA IDE clinical trials to cover the manufacturing and research costs only. After FDA approval on March 21, 2019, commercial pricing took effect, changing the Optimizer® System to $23,000. The manufacturer contended the Cost Criteria are still met with the current $23,000 ASP for the Optimizer Smart System.
Response: We appreciate the manufacturer's input. After consideration of the public comments we received, we believe that Optimizer® System meets the cost criterion for device pass-through payment status.
After consideration of the public comments we received, we believe that the Optimizer® System qualifies for device pass-through payment status and we are approving the application for device pass-through payment status for the Optimizer® System beginning in CY 2020.
(5) AquaBeam® System
PROCEPT BioRobotics Corporation submitted an application for a new device category for transitional pass-through payment status for the AquaBeam® System as a resubmission of their CY 2019 application. The AquaBeam® System is intended for the resection and removal of prostate tissue in males suffering from lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia (BPH). The applicant stated that this is a very common condition typically occurring in elderly men. The clinical symptoms of this condition can include diminished urinary stream and partial urethral obstruction.[26] According to the applicant, the AquaBeam® system resects the prostate to relieve symptoms of urethral compression. The resection is performed robotically using a high velocity, nonheated sterile saline water jet (in a procedure called Aquablation). The applicant stated that the AquaBeam® System utilizes real-time intra-operative ultrasound guidance to allow the surgeon to precisely plan the surgical resection area of the prostate and then the system delivers Aquablation therapy to accurately resect the obstructive prostate tissue without the use of heat. The materials submitted by the applicant state that the AquaBeam® System consists of a disposable, single-use handpiece as well as other components that are considered capital equipment.
With respect to the newness criterion at § 419.66(b)(1), FDA granted a De Novo request classifying the AquaBeam® System as a Class II device under section 513(f)(2) of the Federal Food, Drug, and Cosmetic Act on December 21, 2017. The application for a new device category for transitional pass-through payment status for the AquaBeam® System was received on March 1, 2018, which is within 3 years of the date of the initial FDA approval or clearance. We invited public comments on whether the AquaBeam® System meets the newness criterion. We did not receive any comments on the newness of the AquaBeam® System. We believe AquaBeam® System meets the transitional pass-through payment newness criterion.
With respect to the eligibility criterion at § 419.66(b)(3), according to the applicant, the AquaBeam® System is integral to the service provided, is used for one patient only, comes in contact with human skin, and is applied in or on a wound or other skin lesion. The applicant also claimed the AquaBeam® System meets the device eligibility requirements of § 419.66(b)(4) because it is not an instrument, apparatus, implement, or items for which depreciation and financing expenses are recovered, and it is not a supply or material furnished incident to a service. However, in the CY 2019 OPPS/ASC proposed and final rules, we cited the CY 2000 OPPS interim final rule with comment period (65 FR 67804 through 67805), where we explained how we interpreted § 419.43(e)(4)(iv). We stated that we consider a device to be surgically implanted or inserted if is surgically inserted or implanted via a natural or surgically created orifice, or inserted or implanted via a surgically created incision. We also stated that we do not consider an item used to cut or otherwise create a surgical opening to be a device that is surgically implanted or inserted. We consider items used to create incisions, such as scalpels, electrocautery units, biopsy apparatuses, or other commonly used operating room instruments to be supplies or capital equipment not eligible for transitional pass-through payments. We stated that we believe the function of these items is different and distinct from that of devices that are used for surgical implantation or insertion. Finally, we stated that, generally, we would expect that surgical implantation or insertion of a device occurs after the surgeon uses certain primary tools, supplies, or instruments to create the surgical path or site for implanting the device. In the CY 2006 OPPS final rule with comment period (70 FR 68329 and 68630), we adopted as final our interpretation that surgical insertion or implantation criteria include devices that are surgically inserted or implanted via a natural or surgically created orifice, as well as those devices that are inserted or implanted via a surgically created incision. We reiterated that we maintain all of the other criteria in § 419.66 of the regulations, namely, that we do not consider an item used to cut or otherwise create a surgical opening to be a device that is surgically implanted or inserted.
The applicant resubmitted their application with additional information that they believe supports their stance that the device should be considered eligible under the device pass-through payment eligibility criteria. The applicant stated that the AquaBeam® System's handpiece is temporarily surgically inserted into the urethra via the urinary meatus. The applicant indicated that the AquaBeam® System's handpiece does not create an incision or surgical opening or pathway, but instead ablates prostate tissue. The applicant further stated that the device only cuts the prostatic tissue after being inserted into the prostatic urethra and therefore it should be considered eligible. The applicant also stated that the prostatic urethra tissue is cut because it is at the center of the obstruction in the prostate. Additionally, the applicant explained that to relieve the symptoms of BPH, both the prostatic urethra and prostate tissue encircling the prostatic urethra must be ablated, or cut, to relieve the symptoms of BPH and provide some additional clearance for future swelling or growth of the prostate. The applicant stated that the prostatic urethra tissue is not cut or disturbed to access the prostate tissue underneath, but the removal of the prostatic urethra is a key aspect of treating the obstruction that causes BPH symptoms. Finally, the applicant believes that clinically the distinction between the prostatic urethra tissue and the prostate tissue are not meaningful in the context of a BPH surgical intervention. We invited public comments on whether the AquaBeam® System meets the eligibility criteria at § 419.66(b).
Comments: We received several comments in regards to the eligibility of the AquaBeam® System. While other stakeholders commented generally on the eligibility of the AquaBeam® System, the applicant provided additional detail in support of AquaBeam's eligibility. Stakeholders agreed that AquaBeam® System was eligible, and providing the following reasons: AquaBeam® System is not used to cut or otherwise create a surgical opening; the AquaBeam System handpiece is not a commonly used operation room instrument; the AquaBeam System handpiece is integral to the service provided; it is a single use item; it comes into contact with human tissue and finally, it is inserted into the prostatic urethra through a natural orifice.
The applicant restated that the AquaBeam® System does not cut or otherwise create a surgical opening. They reiterated that the AquaBeam® System is inserted into the body through a natural orifice at the meatus of the urethra without any cutting. The applicant again stated that the AquaBeam® System is not used to cut or otherwise create a surgical opening at the meatus, or the prostatic urethra. The applicant further detailed that the purpose of the ablation procedure is to remove the tissue that is obstructing urine flow through the urethra as well as to remove additional tissue that may obstruct the urethra causing LUTS. The applicant claimed that the removal of the obstruction is not the creation of a surgical opening for inserting the device and that the device is already positioned inside the body.
The applicant further argued that ablating both the prostatic urethra and the prostate tissue is central to the treatment of BPH symptoms. Additionally, they argued that clinically, the distinction between the prostatic urethra and the prostate tissue are not meaningful to treat BPH and the procedure does not create an opening at the urethra to access the prostate for tissue removal. The applicant further argued that the plain meaning of the language used to expand eligibility to include devices inserted through natural orifices [27] means that passing the AquaBeam® System through the natural orifice into the body is taking the place of creating a surgical opening.
Response: We appreciate the comments submitted by the stakeholders on the eligibility of the AquaBeam® System. After consideration of submitted comments and after gaining additional clarity on the clinical details of the procedure, we have determined that the AquaBeam® System meets the eligibility criteria at § 419.66(b). Specifically, we believe that the AquaBeam® System is inserted into the urethra, a natural orifice. We recognize that after being inserted into the urethra, the device then ablates both the prostatic urethra and the prostate tissue in order to relieve and treat the symptoms of BPH.
The criteria for establishing new device categories are specified at § 419.66(c). The first criterion, at § 419.66(c)(1), provides that CMS determines that a device to be included in the category is not appropriately described by any of the existing categories or by any category previously in effect, and was not being paid for as an outpatient service as of December 31, 1996. In the proposed rule, we had not identified an existing pass-through payment category that describes the AquaBeam® System. The applicant proposed a category descriptor for the AquaBeam® System of “Probe, image guided, robotic resection of prostate.” We invited public comments on whether the AquaBeam® System meets this criterion.
We did not receive public comments that identified an existing pass-through payment category that describes the AquaBeam® System. We believe that the AquaBeam® System meets this criterion.
The second criterion for establishing a device category, at § 419.66(c)(2), provides that CMS determines that a device to be included in the category has demonstrated that it will substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment. The applicant stated that the AquaBeam® System provides a substantial clinical improvement as the first autonomous tissue resection robot for the treatment of lower urinary tract symptoms due to BPH. The applicant further provided that the AquaBeam® System is also a substantial clinical improvement because the Aquablation procedure demonstrated superior efficacy and safety for larger prostates (prostates sized 50-80 mL) as compared to transurethral resection of the prostate (TURP). The applicant also believes that the Aquablation procedure would provide better outcomes for patients with large prostates (>80 mL) who may undergo open prostatectomy whereas the open prostatectomy procedure would require a hospital inpatient admission. With respect to this criterion, the applicant submitted several articles that examined the use of a current standard treatment for BPH—transurethral prostatectomy TURP, including complications associated with the procedure and the comparison of the effectiveness of TURP to other modalities used to treat BPH, including holmium laser enucleation of the prostate (HoLEP) [28] and photoselective vaporization (PVP).[29]
The most recent clinical study involving the AquaBeam® System was an accepted manuscript describing a double-blind trial that compared men treated with the AquaBeam® System versus men treated with traditional TURP.[30] This was a multicenter study in 4 countries with 17 sites, 6 of which contributed 5 patients or fewer. Patients were randomized to receive treatment with either the AquaBeam® System or TURP in a two-to-one ratio. With exclusions and dropouts, 117 patients were treated with the AquaBeam® System and 67 patients with TURP. The data on efficacy supported the equivalence of the two procedures based upon noninferiority analysis. The safety data were reported as showing superiority of the AquaBeam® System over TURP, although the data were difficult to track because adverse consequences were combined into categories. The applicant claimed that the International Prostate Symptom Scores (IPPS) were significantly improved in AquaBeam® System patients as compared to TURP patients in men whose prostate was greater the 50 mL in size. The applicant also claimed that the proportion of men with a worsening of sexual function (as shown with a decrease in Male Sexual Health Questionnaire for Ejaculatory Dysfunction (MSHQ) score of at least 2 points or a decrease in International Index of Erectile Function (IIEF-5) score of at least 6 points by 6 months) was lower for the Aquablation procedure at 32.9 percent compared to the TURP groups at 52.8 percent.
In the CY 2020 OPPS/ASC proposed rule, we stated that we believed that the comparison of the AquaBeam® System with TURP does not recognize that there are other treatment modalities available that are likely to have a similar safety profile as the AquaBeam® System. No studies comparing other treatment modalities were cited to show that the AquaBeam® System is a significant improvement over other available procedures.
Based on the evidence submitted with the application, we were concerned that there was a lack of sufficient evidence that the AquaBeam® System provides a substantial clinical improvement over other similar products, particularly in the outpatient setting where large prostates are less likely to be treated. We invited public comments on whether the AquaBeam® System meets the substantial clinical improvement criterion.
Comment: We received several comments regarding the substantial clinical improvement that the AquaBeam® System may provide. They were concerned that the comparison of the AquaBeam® System with TURP does not recognize that there are other treatment modalities available that are likely to have a similar safety profile as the AquaBeam® System and that there were no studies provided comparing other treatment modalities to show that the AquaBeam® System is a significant improvement over other available procedures.
The applicant commented that in the FY 2019 IPPS notice of final rulemaking, CMS concluded that the WATER study findings were statistically significant and showed Aquablation superior to TURP in safety, as well as that patients in the WATER study with prostates larger than 50 mL in volume treated with Aquablation had superior improvement in quantifiable symptom outcomes.
Additionally, the applicant provided that TURP is the gold standard and most common treatment for LUTS due to BPH and that through a direct comparison to TURP, the WATER study demonstrates that the AquaBeam® System is a substantial clinical improvement over the gold standard. The applicant also provides that the direct comparison to TURP in the WATER study allows a comparison of Aquablation to other treatment modalities, including transurethral incision of the prostate, photoselective vaporization prostatectomy, transurethral needle ablation of the prostate, transurethral microwave therapy, and prostatic urethral lift. The applicant included several additional pieces of clinical literature to demonstrate that the above-mentioned modalties are inferior in efficacy to TURP in numerous objective and subjective measurers, including peak urine flow, post-void reduction, and BPH symptom reduction.[31 32 33]
Additionally, the applicant provided published data on a list of all surgical treatment modalities. The applicant claims that based on this provided data it is evident that larger prostates are a clinical challenge for all other transurethral surgical approaches to BPH due to high rates of sexual dysfunction in TURP, SP, PVP, HoLEP, and ThuLEP; high rates of blood transfusions in TURP and SP; longer operative time due to the size of prostate in PVP, HoLEP, and ThuLEP; transurethral resection (TUR) syndrome due to length of procedure; high rates of re-intervention or secondary procedures in PVP; and, transient incontinence in HoLEP and ThuLEP. The applicant states that these complication have traditionally limited the treatment of larger prostates in the outpatient setting. The applicant further details that the reason for the increase in complications in large prostates is due to the length of the resection time required. In support of their claim of being appropriate for the outpatient study, the applicant restates findings from the WATER II study, which utilized Aquablation therapy to treat large prostates 80 to 150 mL in volume, with greater than 50 percent of the cases involving large prostates in the hospital outpatient setting. The average Aquablation operative time was 37 minutes, including 8 minutes of resection time and 29 minutes used for planning and robotic programming.
Response: We appreciate the submission of public comments. Specifically, we appreciate the additional scientific data provided that demonstrates the AquaBeam® System's superiority to other techniques, specifically for reducing operative time and complications in general, especially for larger prostates. We agree that the results of the WATER study are statistically significant with a 95 percent confidence interval of the difference between AquaBeam® and TURP and show AquaBeam® is superior to TURP in safety as evidenced by a lower proportion of persistent Clavien-Dindo (CD) Grade 1 adverse events (incontinence, ejaculatory dysfunction and erectile dysfunction) at 3 months. We also agree that when considering CD Grade 2 and above events (events requiring pharmacological treatment, blood transfusions, or endoscopic, surgical or radiological interventions) the WATER study demonstrated a superior safety rate to TURP. Additionally, patients enrolled in the WATER study with prostate sizes greater than 50 mL in volume and treated with AquaBeam® had superior BPH symptom reduction (IPSS) than those treated with TURP, as well as better peak urinary flow rates at 6 months (Qmax), improved ejaculatory function, and improved incontinence scores at 3 months.
Additionally, results from the WATER II study for patients with large prostates demonstrate better outcomes of the AquaBeam® System over open prostatectomy, regarding shorter operative time, shorter length of stay, and decreased rates of severe hemorrhage and transfusions. We also agree that the minimally invasive nature of Aquablation offers men with large prostates (>80 mL) an outpatient option. In conclusion, after review of the additional data and literature, we agree that the AquaBeam® System provides a substantial clinical improvement.
The third criterion for establishing a device category, at § 419.66(c)(3), requires us to determine that the cost of the device is not insignificant, as described in § 419.66(d). Section 419.66(d) includes three cost significance criteria that must each be met. The applicant provided the following information in support of the cost significance requirements. The applicant stated that the AquaBeam® System would be reported with CPT code 0421T. CPT code 0421T is assigned to APC 5375 (Level 5 Urology and Related Services). To meet the cost criterion for device pass-through payment status, a device must pass all three tests of the cost criterion for at least one APC. For our calculations, we used APC 5375, which has a CY 2018 payment rate of $3,706.03. Beginning in CY 2017, we calculate the device offset amount at the HCPCS/CPT code level instead of the APC level (81 FR 79657). CPT code 0421T had device offset amount of $0.00 at the time the application was received. According to the applicant, the cost of the handpiece for the AquaBeam® System is $2,500.
Section 419.66(d)(1), the first cost significance requirement, provides that the estimated average reasonable cost of devices in the category must exceed 25 percent of the applicable APC payment amount for the service related to the category of devices. The estimated average reasonable cost of $2,500 for the AquaBeam® System exceeds 25 percent of the applicable APC payment amount for the service related to the category of devices of $3,706.03 ($2,500/$3,706.03 × 100 = 67.5 percent). Therefore, we believe the AquaBeam® System meets the first cost significance requirement.
The second cost significance requirement, at § 419.66(d)(2), provides that the estimated average reasonable cost of the devices in the category must exceed the cost of the device-related portion of the APC payment amount for the related service by at least 25 percent, which means that the device cost needs to be at least 125 percent of the offset amount (the device-related portion of the APC found on the offset list). Given that there are no device-related costs in the APC payment amount and the AquaBeam® System has an estimated average reasonable cost of $2,500, we believe that the AquaBeam® System meets the second cost significance requirement.
The third cost significance requirement, at § 419.66(d)(3), provides that the difference between the estimated average reasonable cost of the devices in the category and the portion of the APC payment amount for the device must exceed 10 percent of the APC payment amount for the related service. The difference between the estimated average reasonable cost of $2,500 for the AquaBeam® System and the portion of the APC payment amount for the device of $0.00 exceeds the APC payment amount for the related service of $3,706.03 by 68 percent (($2,500 − $0.00)/$3,706.03 × 100 = 67.5 percent). Therefore, we believe that the AquaBeam® System meets the third cost significance requirement.
We invited public comments on whether the AquaBeam® System meets the device pass-through payment criteria discussed in this section, including the cost criterion.
Comment: The manufacturer believed that the AquaBeam® System meets the device pass-through payment criteria, including the cost criterion.
Response: We thank the manufacturer for their input. After consideration of the public comments we received, we believe the AquaBeam® System meets the cost criterion and we are approving it for device pass-through payment status beginning in CY 2020.
(6) EluviaTM Drug-Eluting Vascular Stent System
Boston Scientific Corporation submitted an application for new technology add-on payments for the EluviaTM Drug-Eluting Vascular Stent System for FY 2020. According to the applicant, the EluviaTM system is a sustained-release drug-eluting stent indicated for improving luminal diameter in the treatment of peripheral artery disease (PAD) with symptomatic de novo or restenotic lesions in the native superficial femoral artery (SFA) and/or the proximal popliteal artery (PPA) with reference vessel diameters (RVD) ranging from 4.0 to 6.0 mm and total lesion lengths up to 190 mm.
The applicant stated that PAD is a circulatory condition in which narrowed arteries reduce blood flow to the limbs, usually in the legs. Symptoms of PAD may include lower extremity pain due to varying degrees of ischemia, claudication which is characterized by pain induced by exercise and relieved with rest. According to the applicant, risk factors for PAD include individuals who are age 70 years old and older; individuals who are between the ages of 50 years old and 69 years old with a history of smoking or diabetes; individuals who are between the ages of 40 years old and 49 years old with diabetes and at least one other risk factor for atherosclerosis; leg symptoms suggestive of claudication with exertion, or ischemic pain at rest; abnormal lower extremity pulse examination; known atherosclerosis at other sites (for example, coronary, carotid, renal artery disease); smoking; hypertension, hyperlipidemia, and homocysteinemia.[34] PAD is primarily caused by atherosclerosis—the buildup of fatty plaque in the arteries. PAD can occur in any blood vessel, but it is more common in the legs than the arms. Approximately 8.5 million people in the U.S. have PAD, including 12 to 20 percent of individuals who are age 60 years old and older.[35]
Management of the disease is aimed at improving symptoms, improving functional capacity, and preventing amputations and death. Management of patients who have been diagnosed with lower extremity PAD may include medical therapies to reduce the risk for future cardiovascular events related to atherosclerosis, such as myocardial infarction, stroke, and peripheral arterial thrombosis. Such therapies may include antiplatelet therapy, smoking cessation, lipid-lowering therapy, and treatment of diabetes and hypertension. For patients with significant or disabling symptoms unresponsive to lifestyle adjustment and pharmacologic therapy, intervention (percutaneous, surgical) may be needed. Surgical intervention includes angioplasty, a procedure in which a balloon-tip catheter is inserted into the artery and inflated to dilate the narrowed artery lumen. The balloon is then deflated and removed with the catheter. For patients with limb-threatening ischemia (for example, pain while at rest and/or ulceration), revascularization is a priority to reestablish arterial blood flow. According to the applicant, treatment of the SFA is problematic due to multiple issues including high rate of restenosis and significant forces of compression.
The applicant describes the EluviaTM Drug-Eluting Vascular Stent System as a sustained-release drug-eluting self-expanding, nickel titanium alloy (nitinol) mesh stent used to reestablish blood flow to stenotic arteries. According to the applicant, the EluviaTM stent is coated with the drug paclitaxel, which helps prevent the artery from restenosis. The applicant stated that EluviaTM's polymer-based drug delivery system is uniquely designed to sustain the release of paclitaxel beyond 1 year to match the restenotic process in the SFA. According to the applicant, the EluviaTM Drug-Eluting Vascular Stent System is comprised of: (1) The implantable endoprosthesis; and (2) the stent delivery system (SDS). On both the proximal and distal ends of the stent, radiopaque markers made of tantalum increase visibility of the stent to aid in placement. The tri-axial designed delivery system consists of an outer shaft to stabilize the stent delivery system, a middle shaft to protect and constrain the stent, and an inner shaft to provide a guide wire lumen. The delivery system is compatible with 0.035 in (0.89 mm) guide wires. The EluviaTM stent is available in a variety of diameters and lengths. The delivery system is offered in 2 working lengths (75 cm and 130 cm).
With respect to the newness criterion at § 419.66(b)(1), EluviaTM received FDA premarket approval (PMA) on September 18, 2018. The application for a new device category for transitional pass-through payment status for EluviaTM was received on November 15, 2018, which is within 3 years of the date of the initial FDA approval or clearance. We invited public comments on whether the EluviaTM Drug-Eluting Vascular Stent System meets the newness criterion. We did not receive public comments in regards to Eluvia's newness, however, since the application was received within 3 years of the initial date of FDA approval or clearance, we believe that the EluviaTM Drug-Eluting Vascular Stent System meets the newness criterion.
With respect to the eligibility criterion at § 419.66(b)(3), according to the applicant, the EluviaTM Drug-Eluting Vascular Stent System is integral to the service provided, is used for one patient only, comes in contact with human skin, and is applied in or on a wound or other skin lesion. The applicant also claimed that the EluviaTM Drug-Eluting Vascular Stent System meets the device eligibility requirements of § 419.66(b)(4) because it is not an instrument, apparatus, implement, or items for which depreciation and financing expenses are recovered, and it is not a supply or material furnished incident to a service. We invited public comments on whether the EluviaTM Drug-Eluting Vascular Stent System meets the eligibility criterion at § 419.66(b).
We did not receive any public comments on this issue. We believe that EluviaTM Drug-Eluting Vascular Stent System meets the eligibility criterion.
The criteria for establishing new device categories are specified at § 419.66(c). The first criterion, at § 419.66(c)(1), provides that CMS determines that a device to be included in the category is not appropriately described by any of the existing categories or by any category previously in effect, and was not being paid for as an outpatient service as of December 31, 1996. We have not identified an existing pass-through payment category that describes the EluviaTM Drug-Eluting Vascular Stent System. The applicant proposed a category descriptor for the EluviaTM Drug-Eluting Vascular Stent System of “Stent, non-coronary, polymer matrix, minimum 12-month sustained drug release, with delivery system.” We invited public comments on this issue.
Comment: One commenter stated that the stent platform, the drug coating, and the polymer coating of the EluviaTM Drug-Eluting Vascular Stent System are not new. The commenter compared EluviaTM to the Zilver PTX drug-eluting stent, arguing that both are self-expanding nitinol stents coated with paclitaxel. The commenter also compared the underlying stent platform and delivery system of EluviaTM to Boston Scientific's Innova self-expanding stent.[36] Finally, the commenter believed that the polymers used in the EluviaTM coating are the same used in the Xience V and Promus Element coronary stents.[37]
Comment: Another commenter, the manufacturer, restated that they are vastly different than the Zilver PTX drug eluting stent, as well as any other device. The commenter provided that Eluvia's polymer matrix layer is different from the paclitaxel-coated Zilver PTX, and allows for targeted, localized, sustained, low-dose amorphous paclitaxel delivery with minimal systemic distribution or particulate loss. The commenter also states that there is a difference in the diffusion gradient: Paclitaxel is delivered to the lesion via a diffusion gradient with poly(vinylidene fluoride)-co-hexafluoropropylene, whereas they state that the Zilver PTX does not have a diffusion gradient. The commenter stated that EluviaTM releases paclitaxel directly to the target lesion, while Zilver PTX release is non-specific to the target lesion. The commenter also stated that Eluvia releases paclitaxel over approximately 12 to 15 months, while Zilver PTX's release is complete at two months. The commenter stated that these significant differences in the device designs impact drug dose, drug release mechanism, and drug release kinetics.
Response: We appreciate the stakeholders' comments and comparison of the polymer matrix EluviaTM versus the paclitaxel-coated Zilver PTX and several other devices. After consideration of the comments, we believe that EluviaTM device is a new design with a unique mechanism of action, and therefore is not described by any current device category. Therefore, the EluviaTM device meets the device category eligibility criterion.
The second criterion for establishing a device category, at § 419.66(c)(2), provides that CMS determines that a device to be included in the category has demonstrated that it will substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment. With respect to this criterion, the applicant submitted several articles that examined the use of a current standard treatment for peripheral artery disease (PAD) with symptomatic de novo or restenotic lesions in the native superficial femoral artery (SFA) and/or proximal popliteal artery (PPA), with claims of substantial clinical improvement in achieving superior primary patency; reducing the rate of subsequent therapeutic interventions; decreasing the number of future hospitalizations or physician visits; reducing hospital readmission rates; reducing the rate of device-related complications; and achieving similar functional outcomes and EQ-5D index values while associated with half the rate of target lesion revascularizations (TLRs) procedures.
The applicant submitted the results of the MAJESTIC study, a single-arm, first-in-human study of the EluviaTM Drug-Eluting Vascular Stent System. The MAJESTICT [38] study is a prospective, multi-center, single-arm, open-label study. According to the applicant, the MAJESTIC study demonstrated long-term treatment durability among patients whose femoropopliteal arteries were treated with the EluviaTM stent. The applicant asserted that the MAJESTIC study demonstrates the sustained impact of the EluviaTM stent on primary patency. The MAJESTIC study enrolled 57 patients who had been diagnosed with symptomatic lower limb ischemia and lesions in the SAF or PPA. Efficacy measures at 2 years included primary patency, defined as duplex ultrasound peak systolic velocity ratio of less than 2.5 and the absence of TLR or bypass. Safety monitoring through 3 years included adverse events and TLR. The 24-month clinic visit was completed by 53 patients; 52 had Doppler ultrasound evaluable by the core laboratory, and 48 patients had radiographs taken for stent fracture analysis. The 3-year follow-up was completed by 54 patients. At 2 years, 90.6 percent (48/53) of the patients had improved by 1 or more Rutherford categories as compared with the pre-procedure level without the need for TLR (when those with TLR were included, 96.2 percent sustained improvement); only 1 patient exhibited a worsening in level, 66.0 percent (35/53) of the patients exhibited no symptoms (Category 0) and 24.5 percent (13/53) had mild claudication (Category 1) at the 24-month visit. Mean ABI improved from 0.73 ± 0.22 at baseline to 1.02 ± 0.20 at 12 months and 0.93 ± 0.26 at 24 months. At 24 months, 79.2 percent (38/48) of the patients had an ABI increase of at least 0.1 compared with baseline or had reached an ABI of at least 0.9. The applicant also noted that at 12 months the Kaplan-Meier estimate of primary patency was 96.4 percent.
With regard to the EluviaTM stent achieving superior primary patency, the applicant submitted the results of the IMPERIAL [39] study in which the EluviaTM stent is compared, head-to-head, to the Zilver® PTX Drug-Eluting stent. The IMPERIAL study is a global, multi-center, randomized controlled trial consisting of 465 subjects. Eligible patients were aged 18 years old or older and had a diagnosis of symptomatic lower-limb ischaemia, defined as Rutherford Category 2, 3, or 4 and stenotic, restenotic (treated with a drug-coated balloon greater than 12 months before the study or standard percutaneous transluminal angioplasty only), or occlusive lesions in the native SFA or PPA, with at least 1 infrapopliteal vessel patent to the ankle or foot. Patients had to have stenosis of 70 percent or more (via angiographic assessment), vessel diameter between 4 mm and 6 mm, and total lesion length between 30 mm and 140 mm.
Patients who had previously stented target lesion/vessels treated with drug-coated balloon less than 12 months prior to randomization/enrollment and patients who had undergone prior surgery of the SFA/PPA in the target limb to treat atherosclerotic disease were excluded from the study. Two concurrent single-group (EluviaTM only) substudies were done: A nonblinded, nonrandomized pharmacokinetic sub-study and a nonblinded, nonrandomized study of patients who had been diagnosed with long lesions (greater than 140 mm in diameter).
The IMPERIAL study is a prospective, multi-center, single-blinded randomized, controlled (RCT) noninferiority trial. Patients were randomized (2:1) to implantation of either a paclitaxel-eluting polymer stent (EluviaTM) or a paclitaxel-coated stent (Zilver® PTX) after the treating physician had successfully crossed the target lesion with a guide wire. The primary endpoints of the study are Major Adverse Events defined as all causes of death through 1 month, Target Limb Major Amputation through 12 months and/or Target Lesion Revascularization (TLR) procedure through 12 months and primary vessel patency at 12 months post-procedure. Secondary endpoints included the Rutherford categorization, Walking Impairment Questionnaire, and EQ-5D assessments at 1 month, 6 months, and 12 months post-procedure. Patient demographic and characteristics were balanced between the EluviaTM stent and Zilver® PTX stent groups.
The applicant noted that lesion characteristics for the patients in the EluviaTM stent versus the Zilver® PTX stent arms were comparable. Clinical follow-up visits related to the study were scheduled for 1 month, 6 months, and 12 months after the procedure, with follow-up planned to continue through 5 years, including clinical visits at 24 months and 5 years and clinical or telephone follow-up at 3 and 4 years.
The applicant asserted that in the IMPERIAL study the EluviaTM stent demonstrated superior primary patency over the Zilver® PTX stent, 86.8 percent versus 77.5 percent, respectively (p = 0.0144). The noninferiority primary efficacy endpoint was also met. The applicant provided that the superior primary patency results at the SFA are notable because the SFA presents unique challenges with respect to maintaining long-term patency. There are distinct pathological differences between the SFA and coronary arteries. The SFA tends to have higher levels of calcification and chronic total occlusions when compared to coronary arteries. Following an intervention within the SFA, the SFA produces a healing response which often results in restenosis or re-narrowing of the arterial lumen. This cascade of events leading to restenosis starts with inflammation, followed by smooth muscle cell proliferation and matrix formation.[40] Because of the unique mechanical forces in the SFA, this restenotic process of the SFA can continue well beyond 300 days from the initial intervention. Results from the IMPERIAL study showed that primary patency at 12 months, by Kaplan-Meier estimate, was significantly greater for EluviaTM than for Zilver® PTX, 88.5 percent and 79.5 percent, respectively (p = 0.0119). According to the applicant, these results are consistent with the 96.4 percent primary patency rate at 12 months in the MAJESTIC study.
The IMPERIAL study included two concurrent single-group (EluviaTM only) substudies: A nonblinded, nonrandomized pharmacokinetic substudy and a nonblinded, nonrandomized study of patients with long lesions (greater than 140 mm in diameter). For the pharmacokinetic sub-study, patients had venous blood drawn before stent implantation and at intervals ranging from 10 minutes to 24 hours post implantation, and again at either 48 hours or 72 hours post implantation. The pharmacokinetics sub-study confirmed that plasma paclitaxel concentrations after EluviaTM stent implantation were well below thresholds associated with toxic effects in studies in patients who had been diagnosed with cancer (0·05 μM or ~43 ng/mL).
The IMPERIAL substudy long lesion subgroup consisted of 50 patients with average lesion length of 162.8 mm that were each treated with two EluviaTM stents. According to the applicant, 12-month outcomes for the long lesion subgroup are 87 percent primary patency and 6.5 percent TLR. According to the applicant, in a separate subgroup analysis of patients 65 years old and older (Medicare population), the primary patency rate in the EluviaTM stent group is 92.6 percent, compared to 75.0 percent for the Zilver® PTX stent group (p = 0.0386).
With regard to reducing the rate of subsequent therapeutic interventions, secondary outcomes in the IMPERIAL study included repeat re-intervention on the same lesion, referred to as target lesion revascularization (TLR), over the 12 months following the index procedure. The rate of subsequent interventions, or TLRs, in the EluviaTM stent group was 4.5 percent compared to 9.0 percent in the Zilver® PTX stent group. The applicant asserted that the TLR rate in the EluviaTM stent group represents a substantial reduction in reintervention on the target lesion compared to that of the Zilver® PTX stent group (at a p = 0.067 p-value). The Eluvia® stent group clinically driven TLR rates through 12 months following the index procedure were likewise lower for U.S. patients age 65 and older as well as for those with medically treated diabetes (confidential and unpublished as of the date of the device transitional pass-through payment application, data on file with Boston Scientific). In the subgroup of U.S. patients age 65 and older, the rates of TLR were 2.4 percent in the EluviaTM group compared to 3.1 percent in the Zilver® PTX group, and in the subgroup of medically treated diabetes patients, the rates of TLR were 3.7 percent compared to 13.6 percent in the Zilver® PTX group (p = 0.0269).
With regard to decreasing the number of future hospitalizations or physician visits, the applicant asserted that the substantial reduction in the lesion revascularization rate led to a reduced need to provide additional intensive care, distinguishing the EluviaTM stent group from the Zilver® PTX stent group. In the IMPERIAL study, the EluviaTM-treated patients required fewer days of re-hospitalization. Patients in the EluviaTM group averaged 13.9 days of rehospitalization for all adverse events compared to 17.7 days of rehospitalization for patients in the Zilver® PTX stent group. Patients in the EluviaTM group were rehospitalized for 2.8 days for TLR/Total Vessel Revascularization (TVR) compared to 7.1 days in the Zilver® PTX stent group. Lastly, patients in the EluviaTM stent group were rehospitalized for 2.7 days for procedure/device-related adverse events compared to 4.5 days from the Zilver® PTX stent group.
Regarding reduction in hospital readmission rates, the applicant asserted that patients treated in the EluviaTM stent group experienced reduced rates of hospital readmission following the index procedure compared to those in the Zilver® PTX stent group. Hospital readmission rates at 12 months were 3.9 percent for the EluviaTM stent group compared to 7.1 percent for the Zilver® PTX stent group. Similar results were noted at 1 and 6 months; 1.0 percent versus 2.6 percent and 2.4 percent versus 3.8 percent, respectively.
With regard to reducing the rate of device-related complications, the applicant asserted that while the rates of adverse events were similar in total between treatment arms in the IMPERIAL study, there were measurable differences in device-related complications. Device-related adverse-events were reported in 8 percent of the patients in the EluviaTM stent group compared to 14 percent of the patients in the Zilver® PTX stent group.
Lastly, the applicant asserted that while functional outcomes appear similar between the EluviaTM and Zilver® PTX stent groups at 12 months, these improvements for the Zilver® PTX stent group are associated with twice as many TLRs to achieve similar EQ-5D index values.[41] Secondary endpoints improved after stent implantation and were generally similar between the groups. At 12 months, of the patients with complete Rutherford assessment data, 241 (86 percent) of the 281 patients in the EluviaTM group and 120 (85 percent) of the 142 patients in the Zilver® PTX group had symptoms reported as Rutherford Category 0 or 1 (none to mild claudication). The mean ankle-brachial index was 1·0 (SD 0·2) in both groups at 12 months (baseline mean ankle-brachial index 0·7 [SD 0·2] for EluviaTM; 0·8 [0·2] for Zilver® PTX), with sustained hemodynamic improvement for approximately 80 percent of the patients in both groups. Walking function improved significantly from baseline to 12 months in both groups, as measured with the Walking Impairment Questionnaire and the 6-minute walk test. In both groups, the majority of patients had sustained improvement in the mobility dimension of the EQ-5D, and approximately half had sustained improvement in the pain or discomfort dimension. No significant between-group differences were observed in the Walking Impairment Questionnaire, 6-minute walk test, or EQ-5D. Secondary endpoint results for the EluviaTM stent and Zilver® PTX stent groups are shown in Table 39 as follows:

We noted that the IMPERIAL study, which showed significant differences in primary patency at 12 months, was designed for noninferiority and not superiority. Therefore, we wereconcerned that results showing primary patency at 12 months may not be valid given the study design. We also are concerned that the results of a recently published meta-analysis of randomized controlled trials of the risk of death associated with the use of paclitaxel-coated balloons and stents in the femoropopliteal artery of the leg, which found that there is increased risk of death following application of paclitaxel-coated balloons and stents in the femoropopliteal artery of the lower limbs and that further investigations are urgently warranted,[42] although the EluviaTM system was not included in the meta-analysis. We were also concerned that the findings from this study indicated that the data suggesting that drug-coated stents are substantially clinically improved are unconfirmed. We invited public comments on whether the EluviaTM Drug-Eluting Vascular Stent System meets the substantial clinical improvement criterion, including the implications of the meta-analysis results with respect to a finding of substantial clinical improvement for the EluviaTM system.
We further noted that the applicant for the EluviaTM Drug Eluting Vascular Stent System also applied for the IPPS new technology add-on payment (FY 2020 IPPS/LTCH PPS proposed rule; 86 FR 19314). In the FY 2020 IPPS/LTCH PPS proposed rule, we discussed several publicly available comments that also raised concerns relating to substantial clinical improvement. We list several of those concerns below. While the EluviaTM IMPERIAL study does cite a reduced rate of “Subsequent Therapeutic Interventions”, public comments for the IPPS proposed rule note that “Subsequent Therapeutic Interventions” was not further defined in the New Technology Town Hall presentation nor in the IMPERIAL study. The commenters stated that it would appear from the presentation materials, however, that this claim refers specifically to “target lesion revascularizations (TLR)”, which does not appear statistically significant.
With regard to the applicant's assertion that the use of the EluviaTM stent reduces hospital readmission rates, a commenter noted that during the New Technology Town Hall presentation, the presenter noted that the EluviaTM group had a hospital readmission rate at 12 months of 3.9 percent compared to the Zilver® PTX group's rate of 7.1 percent, and that no p-value was included on the slide used for the presentation to offer an assessment of the statistical significance of this difference. The commenter noted that the manufacturer of the EluviaTM stent did not discuss this particular hospital readmission rate data comparison in the main body of The Lancet paper; however, the data could be found in the online appendix and is shown as not statistically significant.
With regards to longer-term data on the Zilver® PTX stent and the EluviaTM stent, the commenter noted that in the commentary in The Lancet paper accompanying the IMPERIAL study, Drs. Salvatore Cassese and Robert Byrne write that a follow-up duration of 12 months is insufficient to assess late failure, which is not infrequently observed. According to Drs. Cassese and Byrne, the preclinical models of restenosis after stenting of peripheral arteries have shown that stents permanently overstretch the arterial wall, thus stimulating persistent neointimal growth, which might cause a catch-up phenomenon and late failure. The Lancet paper noted that, in this regard, data on outcomes beyond one year will be important to confirm the durability of the efficacy of the EluviaTM stent.[43] The commenter stated that, at this point in time, very limited longer-term data are available on the use of the EluviaTM stent and that the IMPERIAL study offers only 12-month data, although data out to three years have been published from the relatively small 57-patient single-arm MAJESTIC study. The commenter noted that the MAJESTIC study demonstrates a decrease in primary patency from 96.4 percent at one year to 83.5 percent at 2 years; and a doubling in TLR rates from 1 year to 2 years (3.6 percent to 7.2 percent) and again from 2 years to 3 years (7.2 percent to 14.7 percent). The commenter stated that this is not inconsistent with Drs. Cassese and Byrne's commentary regarding late failure, and that the relatively small, single-arm design of the study does not lend itself well to direct comparison to other SFA treatment options such as the Zilver® PTX stent.
The commenter also stated that EluviaTM's lack of long-term data contrasts with 5-year data that is available from the Zilver® PTX stent's pivotal 479-patient RCT comparing the use of the Zilver® PTX stent to angioplasty (with a sub-randomization comparing provisional use of Zilver® PTX stenting to bare metal Zilver stenting in patients experiencing an acute failure of percutaneous transluminal angioplasty (PTA)). The commenter believed that these 5-year data demonstrate that the superiority of the use of the Zilver® PTX stent demonstrated at 12 and 24 months is maintained through 5 years compared to PTA and provisional bare metal stenting, and actually increases rather than decreases over time. The commenter also believed that, given that these stent devices are permanent implants and they are used to treat a chronic disease, long-term data are important to fully understand an SFA stent's clinical benefits. The commenter stated that with 5-year data available to support the ongoing safety and effectiveness of the use of the Zilver® PTX stent, but no such corresponding data available for the use of the EluviaTM stent, it seems incongruous to suggest that the use of the EluviaTM stent results in a substantial clinical improvement compared to the Zilver® PTX stent.
The commenter further stated that, in addition to the limited long-term data available for the EluviaTM stent, there is also a lack of clinical data for the use of the EluviaTM stent to confirm the benefit of the device outside of a strictly controlled clinical study population. The commenter stated that, in contrast, the Zilver® PTX stent has demonstrated comparable outcomes across a broad patient population, including a 787 patient study conducted in Europe with 2-year follow-up and a 904-patient study of all-comers (no exclusion criteria) in Japan with 5-year follow-up completed. The commenter believed that, with no corresponding data for the use of the EluviaTM stent in a broad patient population, it seems unreasonable to suggest that the use of the EluviaTM stent results in a substantial clinical improvement compared to the Zilver® PTX stent.
Based on the evidence submitted with the application, we were concerned that there was a lack of sufficient evidence that the EluviaTM Vascular Drug-Eluting Stent System provides a substantial clinical improvement over other similar products. We invited public comments on whether EluviaTM Vascular Drug-Eluting Stent System meets the substantial clinical improvement criterion.
Comment: One commenter, the manufacturer, stated that the IMPERIAL trial's design as a non-inferiority study is consistent with accepted research methodology and is typical of many head-to-head trials of medical devices. The commenter stated that they defined a pre-specified, post-hoc superiority analysis before evaluation of the clinical trial results, the non-inferiority and subsequent superiority testing methodology and results are not subjected to bias. The commenter argued that the pre-specified success criteria for superiority used the same logic as the pre-specified success criteria for non-inferiority. The commenter stated: “Eluvia will be concluded to be superior to Zilver PTX for device effectiveness if the one-sided lower 95 percent confidence bound on the difference between treatment groups in 12-month primary patency is greater than zero.” The commenter believes that the more stringent one-sided lower 97.5 percent confidence bound (shown as two-sided 95 percent confidence interval on the difference between treatment groups) was observed to be greater than zero and the corresponding p-value was 0.0144. The commenter also provided that the aforementioned data were published in The Lancet following its rigorous peer-review process, suggesting that the claims are not misleading and are supported by valid scientific evidence. The commenters also claimed that clinical guidelines support performing a pre-specified post-hoc analysis given specific requirements, that they believe they met.
Comment: Two commenters mentioned the meta-analysis of paclitaxel-coated balloons and stents [44] that initiated an FDA panel and analysis. The meta-analysis and systematic review of several randomized controlled trials of the risk of death associated with the use of paclitaxel-coated balloons and stents in the femoropopliteal artery of the leg and found that there is an increased risk of death following the application of paclitaxel-coated devices.
Commenters stated that EluviaTM is different from the devices that were studied in the meta-analysis of paclitaxel-coated balloons and stents. Specifically, the commenters claim that EluviaTM delivers paclitaxel in lower doses than the devices in the meta-analysis and is the only peripheral device to deliver paclitaxel through a sustained-release mechanism of action where delivery of paclitaxel is controlled and focused on the target lesion. The commenters, including the applicant, believe that the suggestion in the meta-analysis of a late-term mortality risk associated with paclitaxel-coated devices is not directly applicable to the EluviaTM device.
Additionally, the applicant stated that given the differences between EluviaTM's paclitaxel delivery mechanisms and other peripheral paclitaxel-coated devices, it would be more appropriate to examine safety considerations and data for Eluvia relative to products with similar mechanisms of action and dose levels. The applicant provides the TAXUS coronary stent as such an appropriate comparator, stating that Eluvia and TAXUS are similar in design intent and mechanism of action. In support, the applicant provided additional data showing a 5-year all-cause mortality observed between paclitaxel-eluting and bare metal stents. The applicant also stated that coronary and peripheral atherosclerotic lesions have similar disease presentation and the same antiproliferative impact of paclitaxel on the lesions regardless of vessel bed. The applicant recommends that signals for any potential long-term systemic effects of targeted paclitaxel eluted from a stent polymer matrix would be apparent in patients treated with TAXUS. As opposed to the meta-analysis and the resulting FDA panel analysis, the applicant believes that data on TAXUS can be used to gauge potential system effects of paclitaxel eluted from Eluvia. The applicant argues that the TAXUS stent's safety and effects has been extensively studied with more than 14 years of commercial experience and clinical trial data out to 10 years [45 46 47 48] in patients with coronary implants and 5 years for those with infrapopliteal implants. The applicant then recognizes that mortality rates for patients treated for peripheral artery disease (PAD) are not directly comparable to rates for patients with coronary artery or infrapopliteal disease due to appreciable differences in baseline risk. The applicant states that an additive effect due to low dose paclitaxel elution over time, if it exists, would have been observed in patients receiving treatment in these vessel beds. In regards to the meta-analysis and the risk of late mortality, the applicant further argues that understanding possible effects of paclitaxel exposure is not possible without complete analysis of uniformly re-adjudicated patient level data, particularly with treatment arm crossover and previous interventions or subsequent reinterventions with paclitaxel-coated devices, which occurred in the analyzed studies.
The applicant also provided responses to several comments that CMS noted in the CY 2020 OPPS/ASC proposed rule that were originally mentioned during and following the NTAP Town Hall meeting (84 FR 39479). In the CY 2020 OPPS/ASC proposed rule, CMS noted a comment that showed concern over the EluviaTM IMPERIAL study's citation of a reduced rate of “Subsequent Therapeutic Interventions”. The applicant states that the use of the term “Subsequent Therapeutic Interventions” was used as a lay explanation for target lesion revascularization. The applicant then states that it has recently obtained and analyzed IMPERIAL trial 2-year TLR results, which they also released at the FDA panel meeting on June 19, 2019. The applicant states that 1-year trial results, published in The Lancet, demonstrated a 50 percent reduction in TLRs and 2-year data demonstrated a statistically significantly (p-value not provided) lower rate of repeat re-interventions at 2 years compared to Zilver PTX. The applicant states that the clinical impact of fewer TLR procedures is significant and therefore demonstrates substantial clinical improvement.
The applicant also addressed concerns regarding hospital readmissions. Specifically, the applicant stated that in the NTAP Town Hall Eluvia Meeting, they presented 12-month readmission rates for Eluvia (3.9 percent) and Zilver PTX (7.1 percent), with a self-reported p-value of 0.1369. The applicant argues that statistical significance of the 12-month readmission rates should not be expected to be statistically significant due to the small number of patients. They conclude their response by stating that the data suggests a lower patient and health system burden for rehospitalization of patients for EluviaTM versus patients for Zilver PTX.
Additionally, the applicant responded to concerns regarding long-term data and real-world evidence, stating that due to the nature of the transitional pass-through status requirements for medical devices, EluviaTM is new to the market and would no longer meet the newness criterion if the applicant were to wait until 5-year data are available. The applicant further stated that Medicare NTAP precedent suggests that one-year peer reviewed published results are sufficient to prove substantial clinical improvement, given that at the time of Zilver PTX's NTAP approval they only provided 12-month data published in peer-reviewed literature.[49] The applicant further argues that waiting for a substantial amount of real-world evidence for the use of the EluviaTM drug-eluting stent would disqualify the technology for the transitional pass-through consideration, as the technology would no longer be considered new by the time the data are available.
Response: We appreciate the comments. We are aware of FDA's actions in regards to the meta-analysis of paclitaxel devices and the late mortality signal in patients treated for PAD with paclitaxel-coated balloons and paclitaxel-eluting stents. We agree with the applicant that mortality rates for patients treated for peripheral artery disease are not directly comparable to rates for patients with coronary artery or infrapopliteal. We have continued to closely follow FDA's guidance and recommendations for the use of paclitaxel-coated balloons and paclitaxel-eluting stents for PAD, with details provided below.
On June 19-20, 2019, FDA convened a public meeting of the Circulatory System Devices Panel of the Medical Devices Advisory Committee to discuss, analyze, and make recommendations on the topic of a potential late mortality signal after treatment of PAD in the femoropopliteal artery with paclitaxel-coated balloons and paclitaxel-eluting stents. The Panel concluded that a late mortality signal associated with the use of paclitaxel-coated devices to treat femoropopliteal PAD was present. With that, the Panel and FDA cautiously interpreted the magnitude of the signal due to multiple limitations in the available data including: Wide confidence intervals due to a small sample size, pooling of studies of different paclitaxel-coated devices that were not intended to be combined, substantial amounts of missing study data, no clear evidence of a paclitaxel dose effect on mortality, and no identified pathophysiologic mechanism for the late deaths. The Panel and FDA further concluded that additional clinical study data are needed to fully evaluate the late mortality signal.
As of August 7, 2019,[50] FDA continues to actively work with the manufacturers and investigators on developing additional clinical evidence to better assess the long-term safety of paclitaxel-coated devices. They continue to assert that data could potentially suggest that paclitaxel-coated balloons and stents may improve blood flow to the legs and decrease the likelihood of repeat procedures to reopen blocked blood vessels compared to uncoated devices. However, they also continue to stress the importance of clinicians weighing potential benefits of the paclitaxel-coated devices with the potential risks, including late mortality.
After consideration of public comments and the latest available information from FDA advisory panel, we note that FDA's panel's has continued to review data that has identified a potentially concerning signal of increased long-term mortality in study subjects treated with paclitaxel-coated products compared to patients treated with uncoated devices. We also note that FDA determined that the analysis revealed no clear evidence of a paclitaxel dose effect on mortality. While FDA continues to further evaluate the increased long-term mortality signal and its impact on the overall benefit-risk profile of these devices, we remain concerned that we do not have enough information to determine that the EluviaTM device represents a substantial clinical improvement over existing devices. Therefore, we are not approving the EluviaTM device for CY 2020 device transitional payment. We will continue to monitor any new information and/or recommendations as they become available.
(7) AUGMENT® Bone Graft
Wright Medical submitted an application for a new device category for transitional pass-through payment status for the AUGMENT® Bone Graft. The applicant describes AUGMENT® Bone Graft as a device/drug indicated for use as an alternative to autograft in arthrodesis of the ankle and/or hindfoot where the need for supplemental graft material is required. The applicant stated that the product has two components: Recombinant human platelet-derived growth factor-BB (rhPDGF-BB) solution (0.3 mg/mL) and Beta-tricalcium phosphate (β-TCP) granules (1000-2000 μm). The two components are combined at the point of use and applied to the surgical site. The beta-TCP provides a porous osteoconductive scaffold for new bone growth and the rhPDGF-BB, which act as an osteoinductive chemo-attractant and mitogen for cells involved in wound healing and through promotion of angiogenesis.
According to the applicant, the AUGMENT® Bone Graft is indicated for use in arthrodesis of the ankle and/or hindfoot due to osteoarthritis, post-traumatic arthritis (PTA), rheumatoid arthritis, psoriatic arthritis, avascular necrosis, joint instability, joint deformity, congenital defect or joint arthropathy as an alternative to autograft in patients needing graft material. Osteoarthritis is the most common joint disease among middle aged and older individuals and has been shown to also have health related mental and physical disabilities, which can be compared to the severity as patients with end-stage hip arthritis.[51] Additionally, post-traumatic arthritis develops after an acute direct trauma to the joint and can cause 12 percent of all osteoarthritis cases.[52] Common causes leading to PTOA include intra-articular fractures and meniscal, ligamentous and chondral injuries.[53] The ankle is cited as the most affected joint, reportedly accounting for 54 to 78 percent of over 300,000 injuries occurring in the USA annually. The applicant stated that autologous bone graft has often been used in ankle arthrodesis. Autologous bone is retrieved from a donor site, which may require an incision separate from the arthrodesis.[54] The applicant stated that, in these procedures, harvested autologous bone graft is implanted to stimulate healing between the bones across a diseased joint. The applicant further stated that the procedures may require the use of synthetic bone substitutes to fill the bony voids or gaps or to serve as an alternative to the autograft where autograft is not feasible. The applicant stated that the AUGMENT® Bone Graft removes the need for autologous retrieval. The applicant noted that during the procedure, the surgeon prepares the joint for the graft application and locates any potential bony defect, then applying and packing the AUGMENT® Bone Graft into the joint defects intended for arthrodesis.
With respect to the newness criterion at § 419.66(b)(1), FDA granted the AUGMENT® Bone Graft premarket approval on September 1, 2015. The application for a new device category for transitional pass-through payment status for the AUGMENT® Bone Graft was received May 31, 2018, which is within 3 years of the date of the initial FDA approval or clearance. We invited public comments on whether the AUGMENT® Bone Graft meets the newness criterion.
Comment: We received one comment from the manufacturer restating the date of their application and their initial FDA approval or clearance.
Response: As the application was received within 3 years of the date of the initial FDA approval or clearance, we believe that AUGMENT® Bone Graft meets the newness criterion.
With respect to the eligibility criterion at § 419.66(b)(3), according to the applicant, the use of the AUGMENT® Bone Graft is integral to the service provided, is used for one patient only, comes in contact with human skin, and is applied in or on a wound or other skin lesion. The applicant also claimed that the AUGMENT® Bone Graft meets the device eligibility requirements of § 419.66(b)(4) because it is not an instrument, apparatus, implement, or items for which depreciation and financing expenses are recovered, and it is not a supply or material furnished incident to a service.
The criteria for establishing new device categories are specified at § 419.66(c). The first criterion, at § 419.66(c)(1), provides that CMS determines that a device to be included in the category is not appropriately described by any of the existing categories or by any category previously in effect, and was not being paid for as an outpatient service as of December 31, 1996. We have not identified an existing pass-through payment category that describes the AUGMENT® Bone Graft. The applicant proposed a category descriptor for the AUGMENT® of “rhPDGF-BB and β-TCP as an alternative to autograft in arthrodesis of the ankle and/or hindfoot.”
We did not receive any public comments on these issue. We continue to believe that there is no existing pass-through category that describes AUGMENT® Bone Graft and have determined that AUGMENT® Bone Graft meets this eligibility criterion.
The second criterion for establishing a device category, at § 419.66(c)(2), provides that CMS determines that a device to be included in the category has demonstrated that it will substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment. The applicant claims that the AUGMENT® Bone Graft provides a substantial clinical improvement over autograft procedures by reducing pain at the autograft donor site. With respect to this criterion, the applicant submitted data that examined the use of autograft arthrodesis of the ankle and/or hind foot and arthrodesis with the use of the AUGMENT® Bone Graft.
In a randomized, nonblinded, placebo controlled, noninferiority trial of the AUGMENT® Bone Graft versus autologous bone graft, the AUGMENT® arm showed equivalence bone bridging as demonstrated by CT, pain on weight bearing, The American Orthopaedic Foot & Ankle Society Ankle-Hindfoot (AOFAS—AHS) score, and the Foot Function Index to autologous bone graft. The study noted that patients experienced significantly decreased (in fact no) pain due to elimination of the donor site procedure. In the autograft group, at 6 months, 18/142 patients (13 percent) experienced pain >20 mm (of 100 mm) on the Visual Analog Scale (VAS) at the autograft donor site as compared to 0/272 in the AUGMENT® Bone Graft group. At 12 months, 13/142 autograft patients (9 percent) had pain defined as >20 mm VAS as compared to 0/272 AUGMENT® patients.[55] The VAS has patients mark a visual representation of pain on a ruler based scale from 1 to 100. The measured distance (in mm) on the 10‐cm line between the “no pain” anchor and the patient's mark represents the level of pain. We were concerned that we are unable to sufficiently determine substantial clinical improvement using the provided data, given that a comparison to alternatives to autologous bone graft, such as the reamer-irrigator-aspirator (RIA) technique were not evaluated. Specifically, the RIA technique has been suggested in a number of studies to be a viable alternative to bone autograft, because autogenous bone graft can be readily obtained without the need for additional incisions, therefore eliminating pain from an incisional site.[56] Another concern was the time period of the study because certain ankle arthrodesis complications such as ankle replacement and repeat arthrodesis can happen more than two years after the initial surgery.[57] A long-term study of at least 60 months is currently underway in order to assess long-term safety and efficacy, looking at the following 4 primary outcomes: bone bridging as demonstrated by CT, pain on weight bearing, The American Orthopaedic Foot & Ankle Society Ankle-Hindfoot (AOFAS—AHS) score, and the Foot Function Index. We believe that this long-term study is necessary for meaningful information about long-term efficacy of the Augment® Bone Graft. Further, there was a notable difference in the infection rate, musculoskeletal and tissue disorders, and pain in extremity for those in the AUGMENT® Bone Graft group. These findings were unfortunately not tested for significance and also were not necessarily focused on relevance to the procedure. Should these be significant and related to the device, these findings would suggest that the adverse outcomes due to the Augment® Bone Graft may outweigh its potential benefits.
We invited public comments on whether the AUGMENT® Bone Graft meets the substantial clinical improvement criterion.
Comment: We received several comments in regards to our inquiry of whether or not RIA is an appropriate comparator to AUGMENT® Bone Graft. Specifically, the applicant asserted that the standard of care has been autograft, as evidenced by peer-review literature, a review of claims, and randomized controlled trials. The commenters further asserted that the RIA technique is another way to harvest autograft, requires a separate incision, and is not appropriate given the volume of graft needed for ankle and hindfoot arthrodesis. The applicant further argued that given that the RIA technique still requires a separate incision, the concerns surrounding the second procedure, including pain and potential complications, would still apply. Finally, the applicant asserted that the RIA technique has additional risks and complications, including: A steep learning curve for surgeons with the potential for technical errors creating risk of potential complications;[58] select populations for whom the technique is not appropriate, including patients with osteoporosis and osteopenia, as well as elderly patients;[59] and, risk for fractures, penetration of the anterior cortex, violation of the knee joint, blood loss, and pressure emboli.[60 61 62]
The applicant also commented on concerns regarding long-term outcomes. In the CY 2020 OPPS/ASC proposed rule, we noted a potential lack of data on AUGMENT® beyond 2 years after the initial procedure. In response, the applicant submitted information on ongoing longer-term post-market surveillance data for AUGMENT®. Specifically, the applicant describes FDA post-market approval studies as a post-market requirement for the FDA PMA approval order to be submitted in Q4 2019.
In response to our concern about potential safety and adverse event rates, the applicant stated that available data demonstrates that the benefits of AUGMENT® outweigh the risks. Specifically, the applicant stated that although the reported percentage of infection rates outlined in the FDA's Summary of Safety and Effectiveness Data were higher for the AUGMENT® versus autograft, this is due to various infections unrelated to ankle and hindfoot arthrodesis. The applicant focused on infections related to the surgical support and commented that there was a dramatically lower infection rate, not significantly different between AUGMENT® versus autograft (p = 0.447). The applicant reported that surgical site infections occurred in 7 percent of AUGMENT® subjects and 9.2 percent in traditional autograft procedure subjects. The applicant also stated that it is common when studying a novel therapy against an active comparator that is known to be safe and effective to use a non-inferiority study. The applicant also stated that they conducted an additional analysis of the IDE trial data to determine the impact of graft type (AUGMENT® Bone Graft versus autograft) and subject age (over 65 vs those 65 and younger) on fusion outcomes.[63] The applicant believed that the data confirm results of prior studies that have found that autograft tissue quality is affected by age. The applicant suggested that while AUGMENT® was non-inferior to autograft overall, the elderly population data shows better odds of fusion success with AUGMENT® compared with autograft.
Response: We appreciate the additional information and analysis provided by the applicant and other stakeholders. After reviewing the additional information provided by the applicant and other stakeholders addressing our concerns raised in the CY 2020 OPPS/ASC proposed rule, we agree with the applicant that AUGMENT® provides a substantial clinical improvement by significantly reducing, or eliminating, chronic pain (measured at > 20mm on VAS) associated with the autograft donor site with the elimination of the donor site procedure, at 6 months and 12 months. We also note that in subjects 65+, AUGMENT® was more than twice as likely as autograft to result in fusion.[64] Finally, after analyzing the additional data provided through public comment, we believe that AUGMENT® will provide a substantial clinical improvement by reducing chronic pain and also reducing complications.
The third criterion for establishing a device category, at § 419.66(c)(3), requires us to determine that the cost of the device is not insignificant, as described in § 419.66(d). Section 419.66(d) includes three cost significance criteria that must each be met. The applicant provided the following information in support of the cost significance requirements. The applicant stated that the use of the AUGMENT® Bone Graft would be reported with CPT code 27870 (Arthrodesis, ankle, open), which is assigned to APC 5115 (Level 5 Musculoskeletal Procedures). To meet the cost criterion for device pass-through payment status, a device must pass all three tests of the cost criterion for at least one APC. For our calculations, we used APC 5115, which has a CY 2019 payment rate of $10,122.92. Beginning in CY 2017, we calculate the device offset amount at the HCPCS/CPT code level instead of the APC level (81 FR 79657). CPT code 27870 had a device offset amount of $4,553.29. According to the applicant, the cost of the AUGMENT® Bone Graft is $3,077 per device/drug combination. The applicant further provided a weighted average cost of the graft, accounting for how many procedures required one, two, or three AUGMENT® Bone Graft device/drug kits, equaling a weighted average cost of $6,020.22.
Section 419.66(d)(1), the first cost significance requirement, provides that the estimated average reasonable cost of devices in the category must exceed 25 percent of the applicable APC payment amount for the service related to the category of devices. The estimated average reasonable cost of the AUGMENT® Bone Graft is more than 25 percent of the applicable APC payment amount [65] for the service related to the category of devices of $10,122.92 (($6,020.22/$10,122.92) × 100 = 59 percent)). Therefore, we believe that the AUGMENT® Bone Graft meets the first cost significance requirement.
The second cost significance requirement, at § 419.66(d)(2), provides that the estimated average reasonable cost of the devices in the category must exceed the cost of the device-related portion of the APC payment amount for the related service by at least 25 percent, which means that the device cost needs to be at least 125 percent of the offset amount (the device-related portion of the APC found on the offset list). The estimated average reasonable cost of $6,020.22 for AUGMENT® Bone Graft exceeds the cost of the device-related portion of the APC payment amount for the related service of $4,553.29 by at least 25 percent (($6,020.22/$4,553.29) × 100 = 132 percent). Therefore, we believe AUGMENT® Bone Graft meets the second cost significance requirement.
The third cost significance requirement, at § 419.66(d)(3), provides that the difference between the estimated average reasonable cost of the devices in the category and the portion of the APC payment amount for the device must exceed 10 percent of the APC payment amount for the related service. The difference between the estimated average reasonable cost of $6,020.22 for the AUGMENT® Bone Graft and the portion of the APC payment amount for the device of $4,553.29 exceeds the APC payment amount for the related service of $10,122.92 by more than 10 percent (($6,020.22 − $4,553.29)/$10,122.92 × 100 = 15 percent). Therefore, we believe that AUGMENT® Bone Graft meets the third cost significance test. We invited public comments on whether the AUGMENT® Bone Graft meets the device pass-through payment criteria discussed in this section, including the cost criterion.
Comment: The applicant submitted a comment in support of our cost analysis of AUGMENT® Bone Graft.
Response: We thank the applicant for their comment in support, and continue to believe AUGMENT® Bone Graft meets the cost criteria.
After consideration of the public comments we received, we are approving the AUGMENT® Bone Graft for device pass-through payment status beginning in CY 2020.
3. Request for Information and Potential Revisions to the OPPS Device Pass-Through Substantial Clinical Improvement Criterion in the FY 2020 IPPS/LTCH PPS Proposed Rule
As mentioned earlier, section 1833(t)(6) of the Act provides for pass-through payments for devices, and section 1833(t)(6)(B) of the Act requires CMS to use categories in determining the eligibility of devices for pass-through payments. Separately, the criteria as set forth under § 419.66(c) are used to determine whether a new category of pass-through payment devices should be established. One of these criteria, at § 419.66(c)(2), states that CMS determines that a device to be included in the category has demonstrated that it will substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment. CMS considers the totality of the substantial clinical improvement claims and supporting data, as well as public comments, when evaluating this aspect of each application. CMS summarizes each applicant's claim of substantial clinical improvement as part of its discussion of the entire application in the relevant proposed rule, as well as any concerns regarding those claims. In the relevant final rule for the OPPS, CMS responds to public comments and discusses its decision to approve or deny the application for separate transitional pass-through payments.
Over the years, applicants and commenters have indicated that it would be helpful for CMS to provide greater guidance on what constitutes “substantial clinical improvement.” In the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19368 through 19371), we requested information on the substantial clinical improvement criterion for OPPS transitional pass-through payments for devices and stated that we were considering potential revisions to that criterion. In particular, we sought public comments in the FY 2020 IPPS/LTCH PPS proposed rule on the type of additional detail and guidance that the public and applicants for device pass-through transitional payment would find useful (84 FR 19367 to 19369). This request for public comments was intended to be broad in scope and provide a foundation for potential rulemaking in future years. We refer readers to the FY 2020 IPPS/LTCH proposed rule for the full text of this request for information.
In addition to the broad request for public comments for potential rulemaking in future years, in order to respond to stakeholder feedback requesting greater understanding of CMS' approach to evaluating substantial clinical improvement, we also solicited comments from the public in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19369 through 19371) on specific changes or clarifications to the IPPS and OPPS substantial clinical improvement criterion that CMS might consider making in the FY 2020 IPPS/LTCH PPS final rule to provide greater clarity and predictability. We refer readers to the FY 2020 IPPS/LTCH PPS proposed rule for complete details on those potential revisions. We noted that any responses to public comments we received on potential revisions to the OPPS substantial clinical improvement criterion in response to the FY 2020 IPPS/LTCH PPS proposed rule, as well as any revisions that might be adopted, would be included in this final rule with comment period and would inform future OPPS rulemaking.
Comment: We received one comment addressing this RFI, which recommended that CMS demonstrate greater flexibility in considering what constitutes substantial clinical improvement, including evidence developed through data registries and evidence from markets outside the U.S.
Response: We thank the commenter for their response. We note that we accept a wide range of data and other evidence to help determine whether a device meets the substantial clinical improvement criterion.
4. Proposed Alternative Pathway to the OPPS Device Pass-Through Substantial Clinical Improvement Criterion for Transformative New Devices
Since 2001 when we first established the substantial clinical improvement criterion, FDA programs for helping to expedite the development and review of transformative new devices that are intended to treat or diagnose serious diseases or conditions and address unmet medical needs (referred to, for purposes of this rule) as FDA's expedited programs) have continued to evolve in tandem with advances in medical innovations and technology. There is currently one FDA expedited program for devices, the Breakthrough Devices Program. The 21st Century Cures Act (Cures Act) (Pub. L. 144-255) established the Breakthrough Devices Program to expedite the development of, and provide for priority review of, medical devices and device-led combination products that provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions and which meet one of the following four criteria: (1) That represent breakthrough technologies; (2) for which no approved or cleared alternatives exist; (3) that offer significant advantages over existing approved or cleared alternatives, including the potential, compared to existing approved alternatives, to reduce or eliminate the need for hospitalization, improve patient quality of life, facilitate patients' ability to manage their own care (such as through self-directed personal assistance), or establish long-term clinical efficiencies; or (4) the availability of which is in the best interest of patients.
Some stakeholders over the years have requested that devices that receive marketing authorization and are part of an FDA expedited program be deemed as representing a substantial clinical improvement for purposes of OPPS device pass-through status. We understand this request would arguably create administrative efficiency because the commenters currently view the two sets of criteria as the same, overlapping, similar, or otherwise duplicative or unnecessary.
The Administration is committed to addressing barriers to health care innovation and ensuring Medicare beneficiaries have access to critical and life-saving new cures and technologies that improve beneficiary health outcomes. As detailed in the President's FY 2020 Budget (we refer readers to HHS FY 2020 Budget in Brief, Improve Medicare Beneficiary Access to Breakthrough Devices, pp. 84-85), HHS is pursuing several policies that will instill greater transparency and consistency around how Medicare covers and pays for innovative technology.
Therefore, given the existence of the current and past FDA programs for helping to expedite the development and review of certain devices intended to treat or diagnose serious or life-threatening or irreversibly debilitating diseases or conditions for which there is an unmet medical need), we considered whether it would also be appropriate to similarly facilitate access to these transformative new technologies for Medicare beneficiaries taking into consideration that, at the time of marketing authorization (that is, Premarket Approval (PMA); 510(k) clearance; or the granting of a De Novo classification request) for a product that is the subject of a FDA expedited program, the evidence base for demonstrating substantial clinical improvement in accordance with CMS' current standard may not be fully developed. We also considered whether FDA marketing authorization of a product that is part of an FDA expedited program is evidence that the product is sufficiently different from existing products for purposes of newness.
After consideration of these issues, and consistent with the Administration's commitment to addressing barriers to health care innovation and ensuring Medicare beneficiaries have access to critical and life-saving new cures and technologies that improve beneficiary health outcomes, we concluded that it would be appropriate to develop an alternative pathway for transformative medical devices. In situations where a new medical device is part of the Breakthrough Devices Program and has received FDA marketing authorization (that is, the device has received PMA; 510(k) clearance; or the granting of a De Novo classification request), we proposed an alternative outpatient pass-through pathway to facilitate access to this technology for Medicare beneficiaries beginning with applications received for pass-through payment on or after January 1, 2020.
We continue to believe that hospitals should receive pass-through payments for devices that offer clear clinical improvement and that cost considerations should not interfere with patient access. In light of the criteria designation as a Breakthrough Device, and because we recognize that such devices may not have a sufficient evidence base to demonstrate substantial clinical improvement at the time of FDA marketing authorization, we proposed to amend the OPPS device transitional pass-through payment regulations to create an alternative pathway to demonstrating substantial clinical improvement that would enable devices that receive FDA marketing authorization and are part of the FDA Breakthrough Devices Program to qualify for our quarterly approval process for device pass-through payment under the OPPS for pass-through payment applications received on or after January 1, 2020. With this proposal, OPPS device pass-through payment applicants for devices that have received FDA marketing authorization and are part of the FDA Breakthrough Devices Program would not be evaluated in terms of the current substantial clinical improvement criterion at § 419.66(c)(2) for the purposes of determining device pass-through payment status, but would continue to need to meet the other requirements for pass-through payment status in our regulation at § 419.66. Devices that have received FDA marketing authorization and are part of the Breakthrough Devices Program can be approved through the quarterly process and would be announced through that process (81 FR 79655). Finally, we would include proposals regarding these devices and whether pass-through payment status should continue to apply in the next applicable OPPS rulemaking cycle.
As such, we proposed to revise paragraph (c)(2) under § 419.66. Under proposed revised paragraph (c)(2), we proposed to establish an alternative pathway where applications for device pass-through payment status for new medical devices received on or after January 1, 2020 that are a part of FDA's Breakthrough Devices Program and have received FDA marketing authorization (that is, the device has received PMA, 510(k) clearance, or the granting of a De Novo classification request) will not be evaluated for substantial clinical improvement for the purposes of determining device pass-through payment status. Under this proposed alternative pathway, a medical device that has received FDA marketing authorization (that is, has been approved or cleared by, or had a De Novo classification request granted by, FDA) and that is part of FDA's Breakthrough Devices Program would still need to meet the eligibility criteria under § 419.66(b), the other criteria for establishing device categories under § 419.66(c), and the cost criterion under § 419.66(d). We noted that this proposal aligns with a proposal in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19371 through 19373) and final rule (84 FR 42292 through 42297) and will help achieve the goals of expedited access to innovative devices to further reduce administrative burden.
Comment: MedPAC opposed our proposal and stated that participation in the FDA Breakthrough Device Program does not necessarily reflect improvements in outcomes or justify increased payment for Medicare beneficiaries. MedPAC expressed concern that such a policy would provide inappropriate incentives for providers to use new technology without proven safety or efficacy by allowing increased payment for the new technology.
Most commenters supported the proposal for an alternative pathway and offered suggestions that they thought would enhance the proposal. Specifically, commenters requested that CMS expand the alternative pathway to include other FDA designations, namely the Expedited Access Pathway and the Regenerative Medicine Advanced Therapy (RMAT) Designation. A commenter requested that similar to the IPPS policy, we also waive the newness criterion under the alternative pathway. Commenters also requested that we expand the alternative pathway to New Technology APCs, drug pass-through payment, and non-opioid alternatives.
Finally, a number of commenters encouraged us to ensure coverage for devices that are approved under the alternative pathway.
Response: We appreciate the commenters' support for the alternative pathway proposal. After reviewing the public comments, we continue to believe that the benefits of providing earlier access to Breakthrough Devices can improve beneficiary health outcomes support establishing this alternative pathway. While we appreciate the commenter's concern regarding potential negative incentives, we continue to believe that it is appropriate to facilitate beneficiary access to transformative new medical devices by establishing an alternative pathway for devices that receive FDA marketing authorization through FDA's Breakthrough Devices Program, and not to require substantial clinical improvement as a requirement for pass-through status for these devices because the evidence base to demonstrate substantial clinical improvement may not be completely developed at the time of FDA marketing authorization for such devices, which would delay their eligibility for pass-through status.
In regards to expanding the alternative pathway to include pass-through drugs and New Technology APCs, we continue to believe that it is appropriate to distinguish between drugs and devices, while we continue to work on other initiatives for drug affordability; a priority for this Administration. Importantly, substantial clinical improvement is not a requirement to be assigned to a New Technology APC or for drug pass-through status, so it is not necessary to waive such a criterion under either of these policies. Finally, we appreciate the commenters' suggestion that we should apply the alternative pathway to other types of FDA designations and will continue to take those comments into consideration for future rulemaking, where appropriate.
Comment: Several commenters suggested that we revise the effective date of the policy, and specifically requested that the policy be effective on or after January 1, 2020 for applications submitted prior to the September 2019 quarterly application submission deadline.
Response: We thank the commenters for their input. We agree with commenters and do not believe applicants with devices that would qualify for the alternative pathway should be required to re-submit their pass-through applications after January 1, 2020 in order to be considered for the alternative pathway. Therefore, after considering the public comments we received, we are finalizing a policy that the alternative pathway will apply for devices that will receive pass-through payments effective on or after January 1, 2020 and we are revising paragraph (c)(2) under § 419.66 consistent with this final policy.
Where we received a device pass-through application by the September 2019 quarterly application deadline for a device that qualifies for the alternative pathway and the device meets the other criteria for device pass-through status, the device can be approved for pass-through status beginning on January 1, 2020. Similarly, devices for which we received a device pass-through application prior to the December 2019 quarterly deadline can receive pass-through status beginning April 1, 2020, assuming they qualify for the alternative pathway and meet the other criteria for device pass-through status.
In summary, we are finalizing our proposal with the change to the effective date suggested by commenters to establish an alternative pathway to the substantial clinical improvement criterion for devices that have FDA Breakthrough Devices Program designation and have received FDA marketing authorization (that is, the device has received PMA, 510(k) clearance, or the granting of a De Novo classification request) for devices approved for transitional pass-through status effective on or after January 1, 2020.
Devices Approved for Pass-Through Status Under the Breakthrough Device Alternative Pathway
We received two device pass-through applications by the September 2, 2019 quarterly application deadline that have received FDA marketing authorization and a Breakthrough Devices designation from FDA and that qualify for consideration under the alternative pathway to the OPPS device pass-through substantial clinical improvement criterion. These devices meet the other criteria for device pass-through including the eligibility criteria under § 419.66(b), the criteria for establishing device categories under § 419.66(c), and the cost criterion under § 419.66(d) and are approved for pass-through status beginning on January 1, 2020.
The devices include: (1) Optimizer® System which is discussed earlier in this section and approved under the standard pathway, and (2) ARTIFICIAL Iris® which is an iris prosthesis for the treatment of iris defects. The ARTIFICIAL Iris® application was received in June 2019 after the March 2019 quarterly deadline for applications to be received in time to be included in CY 2020 rulemaking. We are approving ARTIFICIAL Iris® for transitional pass-through payment under the alternative pathway for CY 2020. As previously stated, all applications that are preliminarily approved upon quarterly review will automatically be included in the next applicable OPPS annual rulemaking cycle, therefore a discussion of this application will be included in CY 2021 rulemaking.
B. Device-Intensive Procedures
1. Background
Under the OPPS, prior to CY 2017, device-intensive status for procedures was determined at the APC level for APCs with a device offset percentage greater than 40 percent (79 FR 66795). Beginning in CY 2017, CMS began determining device-intensive status at the HCPCS code level. In assigning device-intensive status to an APC prior to CY 2017, the device costs of all the procedures within the APC were calculated and the geometric mean device offset of all of the procedures had to exceed 40 percent. Almost all of the procedures assigned to device-intensive APCs utilized devices, and the device costs for the associated HCPCS codes exceeded the 40-percent threshold. The no cost/full credit and partial credit device policy (79 FR 66872 through 66873) applies to device-intensive APCs and is discussed in detail in section IV.B.4. of the CY 2020 OPPS/ASC proposed rule. A related device policy was the requirement that certain procedures assigned to device-intensive APCs require the reporting of a device code on the claim (80 FR 70422). For further background information on the device-intensive APC policy, we refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70421 through 70426).
a. HCPCS Code-Level Device-Intensive Determination
As stated earlier, prior to CY 2017, the device-intensive methodology assigned device-intensive status to all procedures requiring the implantation of a device that were assigned to an APC with a device offset greater than 40 percent and, beginning in CY 2015, that met the three criteria listed below. Historically, the device-intensive designation was at the APC level and applied to the applicable procedures within that APC. In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79658), we changed our methodology to assign device-intensive status at the individual HCPCS code level rather than at the APC level. Under this policy, a procedure could be assigned device-intensive status regardless of its APC assignment, and device-intensive APCs were no longer applied under the OPPS or the ASC payment system.
We believe that a HCPCS code-level device offset is, in most cases, a better representation of a procedure's device cost than an APC-wide average device offset based on the average device offset of all of the procedures assigned to an APC. Unlike a device offset calculated at the APC level, which is a weighted average offset for all devices used in all of the procedures assigned to an APC, a HCPCS code-level device offset is calculated using only claims for a single HCPCS code. We believe that this methodological change results in a more accurate representation of the cost attributable to implantation of a high-cost device, which ensures consistent device-intensive designation of procedures with a significant device cost. Further, we believe a HCPCS code-level device offset removes inappropriate device-intensive status for procedures without a significant device cost that are granted such status because of APC assignment.
Under our existing policy, procedures that meet the criteria listed below in section IV.B.1.b. of the CY 2020 OPPS/ASC proposed rule are identified as device-intensive procedures and are subject to all the policies applicable to procedures assigned device-intensive status under our established methodology, including our policies on device edits and no cost/full credit and partial credit devices discussed in sections IV.B.3. and IV.B.4. of the CY 2020 OPP/ASC proposed rule, respectively.
b. Use of the Three Criteria To Designate Device-Intensive Procedures
We clarified our established policy in the CY 2018 OPPS/ASC final rule with comment period (82 FR 52474), where we explained that device-intensive procedures require the implantation of a device and additionally are subject to the following criteria:
- All procedures must involve implantable devices that would be reported if device insertion procedures were performed;
- The required devices must be surgically inserted or implanted devices that remain in the patient's body after the conclusion of the procedure (at least temporarily); and
- The device offset amount must be significant, which is defined as exceeding 40 percent of the procedure's mean cost.
We changed our policy to apply these three criteria to determine whether procedures qualify as device-intensive in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66926), where we stated that we would apply the no cost/full credit and partial credit device policy—which includes the three criteria listed above—to all device-intensive procedures beginning in CY 2015. We reiterated this position in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70424), where we explained that we were finalizing our proposal to continue using the three criteria established in the CY 2007 OPPS/ASC final rule with comment period for determining the APCs to which the CY 2016 device intensive policy will apply. Under the policies we adopted in CYs 2015, 2016, and 2017, all procedures that require the implantation of a device and meet the above criteria are assigned device-intensive status, regardless of their APC placement.
2. Device-Intensive Procedure Policy for CY 2019 and Subsequent Years
As part of CMS' effort to better capture costs for procedures with significant device costs, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58944 through 58948), for CY 2019, we modified our criteria for device-intensive procedures. We had heard from stakeholders that the criteria excluded some procedures that stakeholders believed should qualify as device-intensive procedures. Specifically, we were persuaded by stakeholder arguments that procedures requiring expensive surgically inserted or implanted devices that are not capital equipment should qualify as device-intensive procedures, regardless of whether the device remains in the patient's body after the conclusion of the procedure. We agreed that a broader definition of device-intensive procedures was warranted, and made two modifications to the criteria for CY 2019 (83 FR 58948). First, we allowed procedures that involve surgically inserted or implanted single-use devices that meet the device offset percentage threshold to qualify as device-intensive procedures, regardless of whether the device remains in the patient's body after the conclusion of the procedure. We established this policy because we no longer believe that whether a device remains in the patient's body should affect its designation as a device-intensive procedure, as such devices could, nonetheless, comprise a large portion of the cost of the applicable procedure. Second, we modified our criteria to lower the device offset percentage threshold from 40 percent to 30 percent, to allow a greater number of procedures to qualify as device-intensive. We stated that we believe allowing these additional procedures to qualify for device-intensive status will help ensure these procedures receive more appropriate payment in the ASC setting, which will help encourage the provision of these services in the ASC setting. In addition, we stated that this change would help to ensure that more procedures containing relatively high-cost devices are subject to the device edits, which leads to more correctly coded claims and greater accuracy in our claims data. Specifically, for CY 2019 and subsequent years, we finalized that device-intensive procedures will be subject to the following criteria:
- All procedures must involve implantable devices assigned a CPT or HCPCS code;
- The required devices (including single-use devices) must be surgically inserted or implanted; and
- The device offset amount must be significant, which is defined as exceeding 30 percent of the procedure's mean cost (83 FR 58945).
In addition, to further align the device-intensive policy with the criteria used for device pass-through payment status, we finalized, for CY 2019 and subsequent years, that for purposes of satisfying the device-intensive criteria, a device-intensive procedure must involve a device that:
- Has received FDA marketing authorization, has received an FDA investigational device exemption (IDE), and has been classified as a Category B device by FDA in accordance with 42 CFR 405.203 through 405.207 and 405.211 through 405.215, or meets another appropriate FDA exemption from premarket review;
- Is an integral part of the service furnished;
- Is used for one patient only;
- Comes in contact with human tissue;
- Is surgically implanted or inserted (either permanently or temporarily); and
- Is not either of the following:
(a) Equipment, an instrument, apparatus, implement, or item of this type for which depreciation and financing expenses are recovered as depreciable assets as defined in Chapter 1 of the Medicare Provider Reimbursement Manual (CMS Pub. 15-1); or
(b) A material or supply furnished incident to a service (for example, a suture, customized surgical kit, scalpel, or clip, other than a radiological site marker) (83 FR 58945).
In addition, for new HCPCS codes describing procedures requiring the implantation of medical devices that do not yet have associated claims data, in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79658), we finalized a policy for CY 2017 to apply device-intensive status with a default device offset set at 41 percent for new HCPCS codes describing procedures requiring the implantation or insertion of a medical device that did not yet have associated claims data until claims data are available to establish the HCPCS code-level device offset for the procedures. This default device offset amount of 41 percent was not calculated from claims data; instead, it was applied as a default until claims data were available upon which to calculate an actual device offset for the new code. The purpose of applying the 41-percent default device offset to new codes that describe procedures that implant or insert medical devices was to ensure ASC access for new procedures until claims data become available.
As discussed in the CY 2019 OPPS/ASC proposed rule and final rule with comment period (83 FR 37108 through 37109 and 58945 through 58946, respectively), in accordance with our policy stated above to lower the device offset percentage threshold for procedures to qualify as device-intensive from greater than 40 percent to greater than 30 percent, for CY 2019 and subsequent years, we modified this policy to apply a 31-percent default device offset to new HCPCS codes describing procedures requiring the implantation of a medical device that do not yet have associated claims data until claims data are available to establish the HCPCS code-level device offset for the procedures. In conjunction with the policy to lower the default device offset from 41 percent to 31 percent, we continued our current policy of, in certain rare instances (for example, in the case of a very expensive implantable device), temporarily assigning a higher offset percentage if warranted by additional information such as pricing data from a device manufacturer (81 FR 79658). Once claims data are available for a new procedure requiring the implantation of a medical device, device-intensive status is applied to the code if the HCPCS code-level device offset is greater than 30 percent, according to our policy of determining device-intensive status by calculating the HCPCS code-level device offset.
In addition, in the CY 2019 OPPS/ASC final rule with comment period, we clarified that since the adoption of our policy in effect as of CY 2018, the associated claims data used for purposes of determining whether or not to apply the default device offset are the associated claims data for either the new HCPCS code or any predecessor code, as described by CPT coding guidance, for the new HCPCS code. Additionally, for CY 2019 and subsequent years, in limited instances where a new HCPCS code does not have a predecessor code as defined by CPT, but describes a procedure that was previously described by an existing code, we use clinical discretion to identify HCPCS codes that are clinically related or similar to the new HCPCS code but are not officially recognized as a predecessor code by CPT, and to use the claims data of the clinically related or similar code(s) for purposes of determining whether or not to apply the default device offset to the new HCPCS code (83 FR 58946). Clinically related and similar procedures for purposes of this policy are procedures that have little or no clinical differences and use the same devices as the new HCPCS code. In addition, clinically related and similar codes for purposes of this policy are codes that either currently or previously describe the procedure described by the new HCPCS code. Under this policy, claims data from clinically related and similar codes are included as associated claims data for a new code, and where an existing HCPCS code is found to be clinically related or similar to a new HCPCS code, we apply the device offset percentage derived from the existing clinically related or similar HCPCS code's claims data to the new HCPCS code for determining the device offset percentage. We stated that we believe that claims data for HCPCS codes describing procedures that have minor differences from the procedures described by new HCPCS codes will provide an accurate depiction of the cost relationship between the procedure and the device(s) that are used, and will be appropriate to use to set a new code's device offset percentage, in the same way that predecessor codes are used. If a new HCPCS code has multiple predecessor codes, the claims data for the predecessor code that has the highest individual HCPCS-level device offset percentage is used to determine whether the new HCPCS code qualifies for device-intensive status. Similarly, in the event that a new HCPCS code does not have a predecessor code but has multiple clinically related or similar codes, the claims data for the clinically related or similar code that has the highest individual HCPCS level device offset percentage is used to determine whether the new HCPCS code qualifies for device-intensive status.
As we indicated in the CY 2019 OPPS/ASC proposed rule and final rule with comment period, additional information for our consideration of an offset percentage higher than the default of 31 percent for new HCPCS codes describing procedures requiring the implantation (or, in some cases, the insertion) of a medical device that do not yet have associated claims data, such as pricing data or invoices from a device manufacturer, should be directed to the Division of Outpatient Care, Mail Stop C4-01-26, Centers for Medicare and Medicaid Services, 7500 Security Boulevard, Baltimore, MD 21244-1850, or electronically at outpatientpps@cms.hhs.gov. Additional information can be submitted prior to issuance of an OPPS/ASC proposed rule or as a public comment in response to an issued OPPS/ASC proposed rule. Device offset percentages will be set in each year's final rule.
For CY 2020, we did not propose any changes to our device-intensive policy.
Comment: Some commenters noted that CPT codes 22612 and 64912 had a device-offset percentage greater than 30 percent and should have been proposed to have device-intensive status for CY 2020.
Response: We agree with commenters that CPT codes 22612 and 64912 were inadvertently omitted from Addendum P and were not assigned device-intensive status in the CY 2020 OPPS/ASC proposed rule. For the CY 2020 OPPS/ASC final rule with comment period, the device offset for both procedures exceeds the 30 percent threshold and these procedures are assigned device-intensive status for CY 2020.
Comment: One commenter requested that we assign HCPCS code C9752 a higher device offset percentage. Additionally, one commenter requested that we assign HCPCS code C9754 a higher device offset percentage.
Response: We thank the commenters for their recommendations and their submission of device pricing information. After reviewing the pricing information provided by commenters, we believe a default device offset percentage of 31 percent appropriately reflects the device costs for these procedures for CY 2020.
Comment: One commenter requested we assign device-intensive status for CPT codes 36904, 36905, 50590, and HCPCS code 0275T for CY 2020.
Response: Using the most currently available data for this CY 2020 OPPS/ASC final rule with comment period, we have determined that the device offset percentages for CPT codes 36905, 50590, and HCPCS code 0275T are not above the 30-percent threshold and, therefore, these procedures are not eligible to be assigned device-intensive status. Additionally, based on the most currently available data for this CY 2020 OPPS/ASC final rule with comment period, we have determined that the device offset percentage for CPT code 36904 exceeds the 30-percent threshold and therefore, this procedure is assigned device-intensive status for CY 2020.
Comment: One commenter stated that the device offset for CPT code 53854 should be based on the predecessor code of HCPCS code 0275T and that CPT code 53854 should be assigned device-intensive status for CY 2020.
Response: We agree with the commenter that, in the absence of device cost statistics for a particular procedure, we may use the predecessor code (in this case HCPCS code 0275T) to make a device-intensive determination. However, we note that the device-intensive percentage for HCPCS code 0275T is below the 30 percent threshold and, therefore, we are not assigning CPT code 53854 device-intensive status for CY 2020.
The full listing of the proposed CY 2020 device-intensive procedures can be found in Addendum P to this CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website).
3. Device Edit Policy
In the CY 2015 OPPS/ASC final rule with comment period (79 FR 66795), we finalized a policy and implemented claims processing edits that require any of the device codes used in the previous device-to-procedure edits to be present on the claim whenever a procedure code assigned to any of the APCs listed in Table 5 of the CY 2015 OPPS/ASC final rule with comment period (the CY 2015 device-dependent APCs) is reported on the claim. In addition, in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70422), we modified our previously existing policy and applied the device coding requirements exclusively to procedures that require the implantation of a device that are assigned to a device-intensive APC. In the CY 2016 OPPS/ASC final rule with comment period, we also finalized our policy that the claims processing edits are such that any device code, when reported on a claim with a procedure assigned to a device-intensive APC (listed in Table 42 of the CY 2016 OPPS/ASC final rule with comment period (80 FR 70422)) will satisfy the edit.
In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79658 through 79659), we changed our policy for CY 2017 and subsequent years to apply the CY 2016 device coding requirements to the newly defined device-intensive procedures. For CY 2017 and subsequent years, we also specified that any device code, when reported on a claim with a device-intensive procedure, will satisfy the edit. In addition, we created HCPCS code C1889 to recognize devices furnished during a device-intensive procedure that are not described by a specific Level II HCPCS Category C-code. Reporting HCPCS code C1889 with a device-intensive procedure will satisfy the edit requiring a device code to be reported on a claim with a device-intensive procedure. In the CY 2019 OPPS/ASC final rule with comment period, we revised the description of HCPCS code C1889 to remove the specific applicability to device-intensive procedures (83 FR 58950). For CY 2019 and subsequent years, the description of HCPCS code C1889 is “Implantable/insertable device, not otherwise classified”.
We did not propose any changes to this policy for CY 2020.
Comment: Several commenters requested that CMS restore the device-to-procedure and procedure-to-device edits. Additionally, some commenters requested specific device edits for total hip arthroplasty procedures and total knee arthroplasty procedures as well as device-intensive “C” HCPCS codes.
Response: As we stated in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66794), we continue to believe that the elimination of device-to-procedure edits and procedure-to-device edits is appropriate due to the experience hospitals now have in coding and reporting these claims fully. More specifically, for the most costly devices, we believe the C-APCs will reliably reflect the cost of the device if charges for the device are included anywhere on the claim. We note that, under our current policy, hospitals are still expected to adhere to the guidelines of correct coding and append the correct device code to the claim when applicable. We also note that, as with all other items and services recognized under the OPPS, we expect hospitals to code and report their costs appropriately, regardless of whether there are claims processing edits in place. Further, we also note that our current device edit policy requires hospitals to report a device for certain device-intensive procedures, which include total knee arthroplasty, device-intensive “C” HCPCS codes, as well as total hip arthroplasty beginning in CY 2020.
4. Adjustment to OPPS Payment for No Cost/Full Credit and Partial Credit Devices
a. Background
To ensure equitable OPPS payment when a hospital receives a device without cost or with full credit, in CY 2007, we implemented a policy to reduce the payment for specified device-dependent APCs by the estimated portion of the APC payment attributable to device costs (that is, the device offset) when the hospital receives a specified device at no cost or with full credit (71 FR 68071 through 68077). Hospitals were instructed to report no cost/full credit device cases on the claim using the “FB” modifier on the line with the procedure code in which the no cost/full credit device is used. In cases in which the device is furnished without cost or with full credit, hospitals were instructed to report a token device charge of less than $1.01. In cases in which the device being inserted is an upgrade (either of the same type of device or to a different type of device) with a full credit for the device being replaced, hospitals were instructed to report as the device charge the difference between the hospital's usual charge for the device being implanted and the hospital's usual charge for the device for which it received full credit. In CY 2008, we expanded this payment adjustment policy to include cases in which hospitals receive partial credit of 50 percent or more of the cost of a specified device. Hospitals were instructed to append the “FC” modifier to the procedure code that reports the service provided to furnish the device when they receive a partial credit of 50 percent or more of the cost of the new device. We refer readers to the CY 2008 OPPS/ASC final rule with comment period for more background information on the “FB” and “FC” modifiers payment adjustment policies (72 FR 66743 through 66749).
In the CY 2014 OPPS/ASC final rule with comment period (78 FR 75005 through 75007), beginning in CY 2014, we modified our policy of reducing OPPS payment for specified APCs when a hospital furnishes a specified device without cost or with a full or partial credit. For CY 2013 and prior years, our policy had been to reduce OPPS payment by 100 percent of the device offset amount when a hospital furnishes a specified device without cost or with a full credit and by 50 percent of the device offset amount when the hospital receives partial credit in the amount of 50 percent or more of the cost for the specified device. For CY 2014, we reduced OPPS payment, for the applicable APCs, by the full or partial credit a hospital receives for a replaced device. Specifically, under this modified policy, hospitals are required to report on the claim the amount of the credit in the amount portion for value code “FD” (Credit Received from the Manufacturer for a Replaced Medical Device) when the hospital receives a credit for a replaced device that is 50 percent or greater than the cost of the device. For CY 2014, we also limited the OPPS payment deduction for the applicable APCs to the total amount of the device offset when the “FD” value code appears on a claim. For CY 2015, we continued our policy of reducing OPPS payment for specified APCs when a hospital furnishes a specified device without cost or with a full or partial credit and to use the three criteria established in the CY 2007 OPPS/ASC final rule with comment period (71 FR 68072 through 68077) for determining the APCs to which our CY 2015 policy will apply (79 FR 66872 through 66873). In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70424), we finalized our policy to no longer specify a list of devices to which the OPPS payment adjustment for no cost/full credit and partial credit devices would apply and instead apply this APC payment adjustment to all replaced devices furnished in conjunction with a procedure assigned to a device-intensive APC when the hospital receives a credit for a replaced specified device that is 50 percent or greater than the cost of the device.
b. Policy for No Cost/Full Credit and Partial Credit Devices
In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79659 through 79660), for CY 2017 and subsequent years, we finalized our policy to reduce OPPS payment for device-intensive procedures, by the full or partial credit a provider receives for a replaced device, when a hospital furnishes a specified device without cost or with a full or partial credit. Under our current policy, hospitals continue to be required to report on the claim the amount of the credit in the amount portion for value code “FD” when the hospital receives a credit for a replaced device that is 50 percent or greater than the cost of the device.
We did not propose any changes to our no cost/full credit and partial credit device policies in the CY 2020 OPPS/ASC proposed rule.
5. Payment Policy for Low-Volume Device-Intensive Procedures
In CY 2016, we used our equitable adjustment authority under section 1833(t)(2)(E) of the Act and used the median cost (instead of the geometric mean cost per our standard methodology) to calculate the payment rate for the implantable miniature telescope procedure described by CPT code 0308T (Insertion of ocular telescope prosthesis including removal of crystalline lens or intraocular lens prosthesis), which is the only code assigned to APC 5494 (Level 4 Intraocular Procedures) (80 FR 70388). We noted that, as stated in the CY 2017 OPPS/ASC proposed rule (81 FR 45656), we proposed to reassign the procedure described by CPT code 0308T to APC 5495 (Level 5 Intraocular Procedures) for CY 2017, but it would be the only procedure code assigned to APC 5495. The payment rates for a procedure described by CPT code 0308T (including the predecessor HCPCS code C9732) were $15,551 in CY 2014, $23,084 in CY 2015, and $17,551 in CY 2016. The procedure described by CPT code 0308T is a high-cost device-intensive surgical procedure that has a very low volume of claims (in part because most of the procedures described by CPT code 0308T are performed in ASCs). We believe that the median cost is a more appropriate measure of the central tendency for purposes of calculating the cost and the payment rate for this procedure because the median cost is impacted to a lesser degree than the geometric mean cost by more extreme observations. We stated that, in future rulemaking, we would consider proposing a general policy for the payment rate calculation for very low-volume device-intensive APCs (80 FR 70389).
For CY 2017, we proposed and finalized a payment policy for low-volume device-intensive procedures that is similar to the policy applied to the procedure described by CPT code 0308T in CY 2016. In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79660 through 79661), we established our current policy that the payment rate for any device-intensive procedure that is assigned to a clinical APC with fewer than 100 total claims for all procedures in the APC be calculated using the median cost instead of the geometric mean cost, for the reasons described above for the policy applied to the procedure described by CPT code 0308T in CY 2016. The CY 2018 final rule geometric mean cost for the procedure described by CPT code 0308T (based on 19 claims containing the device HCPCS C-code, in accordance with the device-intensive edit policy) was $21,302, and the median cost was $19,521. The final CY 2018 payment rate (calculated using the median cost) was $17,560.
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 58951), for CY 2019, we continued with our policy of establishing the payment rate for any device-intensive procedure that is assigned to a clinical APC with fewer than 100 total claims for all procedures in the APC based on calculations using the median cost instead of the geometric mean cost. For more information on the specific policy for assignment of low-volume device-intensive procedures for CY 2019, we refer readers to section III.D.13. of the CY 2019 OPPS/ASC final rule with comment period (83 FR 58917 through 58918).
For CY 2020, we proposed to continue our current policy of establishing the payment rate for any device-intensive procedure that is assigned to a clinical APC with fewer than 100 total claims for all procedures in the APC using the median cost instead of the geometric mean cost. For CY 2020, this policy would apply to CPT code 0308T, which we proposed to assign to APC 5495 (Level 5 Intraocular Procedures) in the CY 2020 OPPS/ASC proposed rule. The CY 2020 OPPS/ASC proposed rule geometric mean cost for the procedure described by CPT code 0308T (based on 7 claims containing the device HCPCS C-code, in accordance with the device-intensive edit policy) was $28,237, and the median cost was $19,270. The proposed CY 2020 payment rate (calculated using the median cost) was $19,740 and can be found in Addendum B to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website).
V. OPPS Payment Changes for Drugs, Biologicals, and Radiopharmaceuticals
A. OPPS Transitional Pass-Through Payment for Additional Costs of Drugs, Biologicals, and Radiopharmaceuticals
1. Background
Section 1833(t)(6) of the Act provides for temporary additional payments or “transitional pass-through payments” for certain drugs and biologicals. Throughout the proposed rule, the term “biological” is used because this is the term that appears in section 1861(t) of the Act. A “biological” as used in the proposed rule includes (but is not necessarily limited to) a “biological product” or a “biologic” as defined under section 351 of the Public Health Service Act. As enacted by the Medicare, Medicaid, and SCHIP Balanced Budget Refinement Act of 1999 (BBRA) (Pub. L. 106-113), this pass-through payment provision requires the Secretary to make additional payments to hospitals for: Current orphan drugs for rare disease and conditions, as designated under section 526 of the Federal Food, Drug, and Cosmetic Act; current drugs and biologicals and brachytherapy sources used in cancer therapy; and current radiopharmaceutical drugs and biologicals. “Current” refers to those types of drugs or biologicals mentioned above that are hospital outpatient services under Medicare Part B for which transitional pass-through payment was made on the first date the hospital OPPS was implemented.
Transitional pass-through payments also are provided for certain “new” drugs and biologicals that were not being paid for as an HOPD service as of December 31, 1996 and whose cost is “not insignificant” in relation to the OPPS payments for the procedures or services associated with the new drug or biological. For pass-through payment purposes, radiopharmaceuticals are included as “drugs.” As required by statute, transitional pass-through payments for a drug or biological described in section 1833(t)(6)(C)(i)(II) of the Act can be made for a period of at least 2 years, but not more than 3 years, after the payment was first made for the product as a hospital outpatient service under Medicare Part B. Proposed CY 2020 pass-through drugs and biologicals and their designated APCs are assigned status indicator “G” in Addenda A and B to the proposed rule (which are available via the internet on the CMS website).
Section 1833(t)(6)(D)(i) of the Act specifies that the pass-through payment amount, in the case of a drug or biological, is the amount by which the amount determined under section 1842(o) of the Act for the drug or biological exceeds the portion of the otherwise applicable Medicare OPD fee schedule that the Secretary determines is associated with the drug or biological. The methodology for determining the pass-through payment amount is set forth in regulations at 42 CFR 419.64. These regulations specify that the pass-through payment equals the amount determined under section 1842(o) of the Act minus the portion of the APC payment that CMS determines is associated with the drug or biological.
Section 1847A of the Act establishes the average sales price (ASP) methodology, which is used for payment for drugs and biologicals described in section 1842(o)(1)(C) of the Act furnished on or after January 1, 2005. The ASP methodology, as applied under the OPPS, uses several sources of data as a basis for payment, including the ASP, the wholesale acquisition cost (WAC), and the average wholesale price (AWP). In the proposed rule, the term “ASP methodology” and “ASP-based” are inclusive of all data sources and methodologies described therein. Additional information on the ASP methodology can be found on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/index.html.
The pass-through application and review process for drugs and biologicals is described on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/passthrough_payment.html.
2. Three-Year Transitional Pass-Through Payment Period for All Pass-Through Drugs, Biologicals, and Radiopharmaceuticals and Quarterly Expiration of Pass-Through Status
As required by statute, transitional pass-through payments for a drug or biological described in section 1833(t)(6)(C)(i)(II) of the Act can be made for a period of at least 2 years, but not more than 3 years, after the payment was first made for the product as a hospital outpatient service under Medicare Part B. Our current policy is to accept pass-through applications on a quarterly basis and to begin pass-through payments for newly approved pass-through drugs and biologicals on a quarterly basis through the next available OPPS quarterly update after the approval of a product's pass-through status. However, prior to CY 2017, we expired pass-through status for drugs and biologicals on an annual basis through notice-and-comment rulemaking (74 FR 60480). In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79662), we finalized a policy change, beginning with pass-through drugs and biologicals newly approved in CY 2017 and subsequent calendar years, to allow for a quarterly expiration of pass-through payment status for drugs, biologicals, and radiopharmaceuticals to afford a pass-through payment period that is as close to a full 3 years as possible for all pass-through drugs, biologicals, and radiopharmaceuticals.
This change eliminated the variability of the pass-through payment eligibility period, which previously varied based on when a particular application was initially received. We adopted this change for pass-through approvals beginning on or after CY 2017, to allow, on a prospective basis, for the maximum pass-through payment period for each pass-through drug without exceeding the statutory limit of 3 years. Notice of drugs whose pass-through payment status is ending during the calendar year will continue to be included in the quarterly OPPS Change Request transmittals.
3. Drugs and Biologicals With Expiring Pass-Through Payment Status in CY 2019
We proposed that the pass-through payment status of six drugs and biologicals would expire on December 31, 2019 as listed in Table 14. These drugs and biologicals will have received OPPS pass-through payment for 3 years during the period of January 1, 2017 until December 31, 2019.
In accordance with the policy finalized in CY 2017 and described earlier, pass-through payment status for drugs and biologicals newly approved in CY 2017 and subsequent years will expire on a quarterly basis, with a pass-through payment period as close to 3 years as possible. With the exception of those groups of drugs and biologicals that are always packaged when they do not have pass-through payment status (specifically, anesthesia drugs; drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure (including diagnostic radiopharmaceuticals, contrast agents, and stress agents); and drugs and biologicals that function as supplies when used in a surgical procedure), our standard methodology for providing payment for drugs and biologicals with expiring pass-through payment status in an upcoming calendar year is to determine the product's estimated per day cost and compare it with the OPPS drug packaging threshold for that calendar year (which is proposed to be $130 for CY 2020), as discussed further in section V.B.2. of the proposed rule. We proposed that if the estimated per day cost for the drug or biological is less than or equal to the applicable OPPS drug packaging threshold, we would package payment for the drug or biological into the payment for the associated procedure in the upcoming calendar year. If the estimated per day cost of the drug or biological is greater than the OPPS drug packaging threshold, we proposed to provide separate payment at the applicable relative ASP-based payment amount (which is proposed at ASP+6 percent for CY 2020, as discussed further in section V.B.3. of the proposed rule).
The proposed packaged or separately payable status of each of these drugs or biologicals is listed in Addendum B to the proposed rule (which is available via the internet on the CMS website).
Comment: One commenter suggested that CMS should establish a new policy to require equal payment for all drugs, biologicals, and radiopharmaceuticals included in the same CED trial to avoid affecting the trial by implicitly favoring one product over another through a higher payment rate. The commenter referenced a current CED trial for amyloid positron emission tomography (PET) that will be active into CY 2020. (Information on this CED trial can be found on the CMS website at https://www.cms.gov/Medicare/Coverage/Coverage-withEvidence-Development/AmyloidPET.html). In the CED trial, NeuraceqTM (florbetaben F18, HCPCS code Q9982) and VizamylTM (flutemetamol F18, HCPCS code Q9983) have not had pass-through status since December 31, 2018, while a third drug, AmyvidTM (florbetapir F18, HCPCS code A9586) continues to have pass-through status until September 30, 2020.
Response: We do not agree with the commenter's request that we establish a policy to require the equal payment of all drugs, biologicals, and radiopharmaceuticals in the same CED trial. The payment rate for each product is consistent with current OPPS statutory requirements. In the case of the particular products mentioned above, one product has drug pass-through status through September 30, 2020, as required by section 1833(t)(6)(G), while the pass-through period for the other products has already expired, meaning payment for these products is packaged into the payment for the primary procedure. Further, section 1833(t)(6) establishes the statutory authority for CMS to provide pass-through payment to cover the additional costs of innovative drugs including radiopharmaceuticals. All of these products receive payment that is consistent with statutory and regulatory requirements and payment will be packaged for all three products once the statutory pass-through period for Amyvid expires. We note that the payment rate for each product does not affect the protocol established under the CED trial because the protocol does not consider the cost of the radiopharmaceutical used for treatment. Therefore, we expect providers to make their own decision about which radiopharmaceutical to use to provide the treatment independent of the payment received for an individual drug.
After consideration of the public comments we received, we are finalizing our proposal, without modification, to expire the pass-through payment status of the 6 drugs and biologicals listed in Table 40 below on December 31, 2019.

4. Drugs, Biologicals, and Radiopharmaceuticals With New or Continuing Pass-Through Payment Status in CY 2020
We proposed to continue pass-through payment status in CY 2020 for 61 drugs and biologicals. These drugs and biologicals, which were approved for pass-through payment status between April 1, 2017 and April 1, 2019 are listed in Table 15. The APCs and HCPCS codes for these drugs and biologicals approved for pass-through payment status on or after January 1, 2020 are assigned status indicator “G” in Addenda A and B to the proposed rule (which are available via the internet on the CMS website). In addition, there are four drugs and biologicals that have already had 3 years of pass-through payment status but for which pass-through payment status is required to be extended for an additional 2 years, effective October 1, 2018 under section 1833(t)(6)(G) of the Act, as added by section 1301(a)(1)(C) of the Consolidated Appropriations Act of 2018 (Pub. L. 115-141). That means the last 9 months of pass-through status for these drugs will occur in CY 2020. Because of this requirement, these drugs and biologicals are also included in Table 15, which brings the total number of drugs and biologicals with proposed pass-through payment status in CY 2020 to 65.
Section 1833(t)(6)(D)(i) of the Act sets the amount of pass-through payment for pass-through drugs and biologicals (the pass-through payment amount) as the difference between the amount authorized under section 1842(o) of the Act and the portion of the otherwise applicable OPD fee schedule that the Secretary determines is associated with the drug or biological. For CY 2020, we proposed to continue to pay for pass-through drugs and biologicals at ASP+6 percent, equivalent to the payment rate these drugs and biologicals would receive in the physician's office setting in CY 2020. We proposed that a $0 pass-through payment amount would be paid for pass-through drugs and biologicals under the CY 2020 OPPS because the difference between the amount authorized under section 1842(o) of the Act, which is proposed at ASP+6 percent, and the portion of the otherwise applicable OPD fee schedule that the Secretary determines is appropriate, which is proposed at ASP+6 percent, is $0.
In the case of policy-packaged drugs (which include the following: Anesthesia drugs; drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure (including contrast agents, diagnostic radiopharmaceuticals, and stress agents); and drugs and biologicals that function as supplies when used in a surgical procedure), we proposed that their pass-through payment amount would be equal to ASP+6 percent for CY 2020 minus a payment offset for any predecessor drug products contributing to the pass-through payment as described in section V.A.6. of the proposed rule. We are making this proposal because, if not for the pass-through payment status of these policy-packaged products, payment for these products would be packaged into the associated procedure.
We proposed to continue to update pass-through payment rates on a quarterly basis on the CMS website during CY 2020 if later quarter ASP submissions (or more recent WAC or AWP information, as applicable) indicate that adjustments to the payment rates for these pass-through payment drugs or biologicals are necessary. For a full description of this policy, we refer readers to the CY 2006 OPPS/ASC final rule with comment period (70 FR 68632 through 68635).
For CY 2020, consistent with our CY 2019 policy for diagnostic and therapeutic radiopharmaceuticals, we proposed to provide payment for both diagnostic and therapeutic radiopharmaceuticals that are granted pass-through payment status based on the ASP methodology. As stated earlier, for purposes of pass-through payment, we consider radiopharmaceuticals to be drugs under the OPPS. Therefore, if a diagnostic or therapeutic radiopharmaceutical receives pass-through payment status during CY 2020, we proposed to follow the standard ASP methodology to determine the pass-through payment rate that drugs receive under section 1842(o) of the Act, which is proposed at ASP+6 percent. If ASP data are not available for a radiopharmaceutical, we proposed to provide pass-through payment at WAC+3 percent (consistent with our proposed policy in section V.B.2.b. of the proposed rule), the equivalent payment provided to pass-through payment drugs and biologicals without ASP information. Additional detail and comments on the WAC+3 percent payment policy can be found in section V.B.2.b. of the proposed rule. If WAC information also is not available, we proposed to provide payment for the pass-through radiopharmaceutical at 95 percent of its most recent AWP.
We did not receive any public comments regarding these proposals. Therefore, we are finalizing these proposals for CY 2020 without modification. We note that public comments pertaining to our proposal to continue to pay WAC+3 percent for drugs and biologicals without ASP information are addressed elsewhere in this final rule with comment period. The drugs and biologicals that continue to have pass-through payment status for CY 2020 or have been granted pass-through payment status as of January 2020 are shown in Table 41 below.






5. Drugs, Biologicals, and Radiopharmaceuticals With Pass-Through Status as a Result of Section 1301 of the Consolidated Appropriations Act of 2018 (Pub. L. 115-141)
As mentioned earlier, section 1301(a)(1) of the Consolidated Appropriations Act of 2018 (Pub. L. 115-141) amended section 1833(t)(6) of the Act and added a new section 1833(t)(6)(G), which provides that for drugs or biologicals whose period of pass-through payment status ended on December 31, 2017 and for which payment was packaged into a covered hospital outpatient service furnished beginning January 1, 2018, such pass-through payment status shall be extended for a 2-year period beginning on October 1, 2018 through September 30, 2020. There are four products whose period of drug and biological pass-through payment status ended on December 31, 2017 and for which payment would have been packaged beginning January 1, 2018. These products were listed in Table 39 of the CY 2019 OPPS/ASC final rule with comment period (83 FR 58962).
Starting in CY 2019, the HCPCS code Q4172 (PuraPly, and PuraPly Antimicrobial, any type, per square centimeter) was discontinued. In its place, two new HCPCS codes were established—Q4195 (Puraply, per square centimeter) and Q4196 (Puraply am, per square centimeter). Because these HCPCS codes are direct successors to HCPCS code Q4172, the provisions of section 1833(t)(6)(G) of the Act apply to HCPCS codes Q4195 and Q4196, and these codes were listed in Table 16 of the proposed rule (84 FR 39495). For CY 2020, we proposed to continue pass-through payment status for the drugs and biologicals listed in Table 16 of the proposed rule (we note that these drugs and biologicals are also listed in Table 15 of the proposed rule) through September 30, 2020 as required in section 1833(t)(6)(G) of the Act, as added by section 1301(a)(1)(C) of the Consolidated Appropriations Act of 2018. The APCs and HCPCS codes for these drugs and biologicals approved for pass-through payment status are assigned status indicator “G” in Addenda A and B to the proposed rule (which are available via the internet on the CMS website).
We proposed to continue to update pass-through payment rates for HCPCS codes Q4195 and Q4196 along with the other three drugs and biologicals covered by section 1833(t)(6)(G) of the Act on a quarterly basis on the CMS website during CY 2020 if later quarter ASP submissions (or more recent WAC or AWP information, as applicable) indicate that adjustments to the payment rates for these pass-through drugs or biologicals are necessary. The replacement of HCPCS code Q4172 by HCPCS codes Q4195 and Q4196 means there are five HCPCS codes for drugs and biologicals covered by section 1833(t)(6)(G) of the Act. For a full description of this policy, we refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 58960 through 58962).
The five HCPCS codes for drugs and biologicals that we proposed would have pass-through payment status for CY 2020 under section 1833(t)(6)(G) of the Act, as added by section 1301(a)(1)(C) of the Consolidated Appropriations Act of 2018, are shown in Table 16 of the CY 2020 OPPS/ASC proposed rule. Included as two of the five HCPCS codes for drugs and biologicals with pass-through payment status for CY 2020 are HCPCS codes Q4195 (Puraply, per square centimeter) and Q4196 (Puraply am, per square centimeter). PuraPly and PuraPly AM are skin substitute products that were approved for pass-through payment status on January 1, 2015 through the drug and biological pass-through payment process. Beginning on April 1, 2015, skin substitute products are evaluated for pass-through payment status through the device pass-through payment process. However, we stated in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66887) that skin substitutes that are approved for pass-through payment status as biologicals effective on or before January 1, 2015 would continue to be paid as pass-through biologicals for the duration of their pass-through payment period. Because PuraPly and PuraPly AM were approved for pass-through payment status through the drug and biological pass-through payment pathway, we finalized a policy to consider both PuraPly and PuraPly AM to be drugs or biologicals as described by section 1833(t)(6)(G) of the Act, as added by section 1301(a)(1)(C) of the Consolidated Appropriations Act of 2018, and to be eligible for extended pass-through payment under our proposal for CY 2020 (83 FR 58961 through 58962).
We did not receive any comments on this policy. Therefore, we are finalizing this proposal without modification. Starting on October 1, 2020, the drugs and biologicals listed in Table 42 will no longer receive pass-through status, and will be assigned to status indicator “N”, which means these drugs will once again be packaged in the OPPS.

6. Provisions for Reducing Transitional Pass-Through Payments for Policy-Packaged Drugs, Biologicals, and Radiopharmaceuticals To Offset Costs Packaged Into APC Groups
Under the regulations at 42 CFR 419.2(b), nonpass-through drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure are packaged in the OPPS. This category includes diagnostic radiopharmaceuticals, contrast agents, stress agents, and other diagnostic drugs. Also under 42 CFR 419.2(b), nonpass-through drugs and biologicals that function as supplies in a surgical procedure are packaged in the OPPS. This category includes skin substitutes and other surgical-supply drugs and biologicals. As described earlier, section 1833(t)(6)(D)(i) of the Act specifies that the transitional pass-through payment amount for pass-through drugs and biologicals is the difference between the amount paid under section 1842(o) of the Act and the otherwise applicable OPD fee schedule amount. Because a payment offset is necessary in order to provide an appropriate transitional pass-through payment, we deduct from the pass-through payment for policy-packaged drugs, biologicals, and radiopharmaceuticals an amount reflecting the portion of the APC payment associated with predecessor products in order to ensure no duplicate payment is made. This amount reflecting the portion of the APC payment associated with predecessor products is called the payment offset.
The payment offset policy applies to all policy packaged drugs, biologicals, and radiopharmaceuticals. For a full description of the payment offset policy as applied to diagnostic radiopharmaceuticals, contrast agents, stress agents, and skin substitutes, we refer readers to the discussion in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70430 through 70432). For CY 2020, as we did in CY 2019, we proposed to continue to apply the same policy packaged offset policy to payment for pass-through diagnostic radiopharmaceuticals, pass-through contrast agents, pass-through stress agents, and pass-through skin substitutes. The proposed APCs to which a payment offset may be applicable for pass-through diagnostic radiopharmaceuticals, pass-through contrast agents, pass-through stress agents, and pass-through skin substitutes are identified in Table 43 below.
We did not receive any comments on this proposal. Therefore, we are finalizing this proposal without modification.

We proposed to continue to post annually on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Annual-Policy-Files.html a file that contains the APC offset amounts that will be used for that year for purposes of both evaluating cost significance for candidate pass-through payment device categories and drugs and biologicals and establishing any appropriate APC offset amounts. Specifically, the file will continue to provide the amounts and percentages of APC payment associated with packaged implantable devices, policy-packaged drugs, and threshold packaged drugs and biologicals for every OPPS clinical APC.
B. OPPS Payment for Drugs, Biologicals, and Radiopharmaceuticals Without Pass-Through Payment Status
1. Criteria for Packaging Payment for Drugs, Biologicals, and Radiopharmaceuticals
a. Packaging Threshold
In accordance with section 1833(t)(16)(B) of the Act, the threshold for establishing separate APCs for payment of drugs and biologicals was set to $50 per administration during CYs 2005 and 2006. In CY 2007, we used the four quarter moving average Producer Price Index (PPI) levels for Pharmaceutical Preparations (Prescription) to trend the $50 threshold forward from the third quarter of CY 2005 (when the Pub. L. 108-173 mandated threshold became effective) to the third quarter of CY 2007. We then rounded the resulting dollar amount to the nearest $5 increment in order to determine the CY 2007 threshold amount of $55. Using the same methodology as that used in CY 2007 (which is discussed in more detail in the CY 2007 OPPS/ASC final rule with comment period (71 FR 68085 through 68086)), we set the packaging threshold for establishing separate APCs for drugs and biologicals at $125 for CY 2019 (83 FR 58963 through 58964).
Following the CY 2007 methodology, for this CY 2020 OPPS/ASC final rule, we used the most recently available four quarter moving average PPI levels to trend the $50 threshold forward from the third quarter of CY 2005 to the third quarter of CY 2020 and rounded the resulting dollar amount ($128.11) to the nearest $5 increment, which yielded a figure of $130. In performing this calculation, we used the most recent forecast of the quarterly index levels for the PPI for Pharmaceuticals for Human Use (Prescription) (Bureau of Labor Statistics series code WPUSI07003) from CMS' Office of the Actuary. For this CY 2019 OPPS/ASC final rule with comment period, based on these calculations using the CY 2007 OPPS methodology, we are finalizing a packaging threshold for CY 2020 of $130.
b. Packaging of Payment for HCPCS Codes That Describe Certain Drugs, Certain Biologicals, and Therapeutic Radiopharmaceuticals Under the Cost Threshold (“Threshold-Packaged Drugs”)
To determine the proposed CY 2020 packaging status for all nonpass-through drugs and biologicals that are not policy packaged, we calculated, on a HCPCS code-specific basis, the per day cost of all drugs, biologicals, and therapeutic radiopharmaceuticals (collectively called “threshold-packaged” drugs) that had a HCPCS code in CY 2018 and were paid (via packaged or separate payment) under the OPPS. We used data from CY 2018 claims processed before January 1, 2019 for this calculation. However, we did not perform this calculation for those drugs and biologicals with multiple HCPCS codes that include different dosages, as described in section V.B.1.d. of the proposed rule, or for the following policy-packaged items that we proposed to continue to package in CY 2020: Anesthesia drugs; drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure; and drugs and biologicals that function as supplies when used in a surgical procedure.
In order to calculate the per day costs for drugs, biologicals, and therapeutic radiopharmaceuticals to determine their proposed packaging status in CY 2020, we used the methodology that was described in detail in the CY 2006 OPPS proposed rule (70 FR 42723 through 42724) and finalized in the CY 2006 OPPS final rule with comment period (70 FR 68636 through 68638). For each drug and biological HCPCS code, we used an estimated payment rate of ASP+6 percent (which is the payment rate we proposed for separately payable drugs and biologicals for CY 2020, as discussed in more detail in section V.B.2.b. of the proposed rule) to calculate the CY 2020 proposed rule per day costs. We used the manufacturer-submitted ASP data from the fourth quarter of CY 2018 (data that were used for payment purposes in the physician's office setting, effective April 1, 2019) to determine the proposed rule per day cost.
As is our standard methodology, for CY 2020, we proposed to use payment rates based on the ASP data from the first quarter of CY 2019 for budget neutrality estimates, packaging determinations, impact analyses, and completion of Addenda A and B to the proposed rule (which are available via the internet on the CMS website) because these are the most recent data available for use at the time of development of the proposed rule. These data also were the basis for drug payments in the physician's office setting, effective April 1, 2019. For items that did not have an ASP-based payment rate, such as some therapeutic radiopharmaceuticals, we used their mean unit cost derived from the CY 2018 hospital claims data to determine their per day cost.
We proposed to package items with a per day cost less than or equal to $130, and identify items with a per day cost greater than $130 as separately payable unless they are policy-packaged. Consistent with our past practice, we cross-walked historical OPPS claims data from the CY 2018 HCPCS codes that were reported to the CY 2019 HCPCS codes that we display in Addendum B to the proposed rule (which is available via the internet on the CMS website) for proposed payment in CY 2020.
Comment: Two commenters suggested that CMS create an exception to the drug cost threshold packaging policy in situations where a shortage of a drug that is packaged under the drug cost threshold packaging policy requires providers to use a higher-cost substitute drug that presumably is still packaged because of the drug cost packaging threshold. The commenters suggested that the substitute drug be separately paid even though the per day cost of the substitute drug is still below the drug cost packaging threshold amount.
Response: We thank the commenter for its suggestion but disagree that such a policy is necessary at this time. We note that the purpose of the drug cost threshold is to require the packaging of relatively small per day drug costs into the associated outpatient hospital procedure. This suggestion runs contrary to our policy goal of bundling more services to encourage provider efficiency. However, we are cognizant of issues surrounding drug shortages and will consider this suggestion for the future.
Comment: One commenter requested that we no longer package HCPCS code J2274 (Injection, Morphine Sulfate, Preservative-Free For Epidural Or Intrathecal Use, 10 mg) because the drug is used in an implantable infusion pump for intrathecal management of pain and/or spasticity, and another drug, HCPCS code J0475 (injection, baclofen, 10 mg) which can be used with the same infusion pump, currently receives separate payment in the OPPS.
Response: We disagree with the commenter. Neither HCPCS code J2274 nor HCPCS code J0475 are classified as drugs that are policy packaged. We refer readers to section V.B.1.c. for a description of drugs that are policy packaged. Also, neither of these drugs is assigned to drug pass-through status. Therefore, we use our drug cost threshold methodology as described in this section of the rule to determine whether the drugs are packaged into an associated procedure or if the drugs are separately paid. The per day cost of HCPCS code J2274 is below the $130 drug packaging threshold, and therefore, the drug is packaged in the OPPS. The per day cost of HCPCS code J0475 is above the drug packaging threshold, and therefore, the drug is paid separately in the OPPS. The drug packaging threshold is based on the per day cost of the specific drug administered, and the threshold is not affected by the means by which the drug is administered to the beneficiary (in this case, through a pump). In the case brought up by the commenter, the per day cost of HCPCS code J2274 is below the $130 drug packaging threshold, and is therefore packaged into the payment for its associated procedure.
After consideration of the public comments we received, and consistent with our methodology for establishing the packaging threshold using the most recent PPI forecast data, we are adopting a CY 2019 packaging threshold of $130.
Our policy during previous cycles of the OPPS has been to use updated ASP and claims data to make final determinations of the packaging status of HCPCS codes for drugs, biologicals, and therapeutic radiopharmaceuticals for the OPPS/ASC final rule with comment period. We note that it is also our policy to make an annual packaging determination for a HCPCS code only when we develop the OPPS/ASC final rule with comment period for the update year. Only HCPCS codes that are identified as separately payable in the final rule with comment period are subject to quarterly updates. For our calculation of per day costs of HCPCS codes for drugs and biologicals in this CY 2020 OPPS/ASC proposed rule, we proposed to use ASP data from the fourth quarter of CY 2018, which is the basis for calculating payment rates for drugs and biologicals in the physician's office setting using the ASP methodology, effective April 1, 2019, along with updated hospital claims data from CY 2018. We note that we also proposed to use these data for budget neutrality estimates and impact analyses for this CY 2020 OPPS/ASC proposed rule.
Payment rates for HCPCS codes for separately payable drugs and biologicals included in Addenda A and B for the final rule with comment period will be based on ASP data from the third quarter of CY 2019. These data will be the basis for calculating payment rates for drugs and biologicals in the physician's office setting using the ASP methodology, effective October 1, 2019. These payment rates would then be updated in the January 2020 OPPS update, based on the most recent ASP data to be used for physicians' office and OPPS payment as of January 1, 2020. For items that do not currently have an ASP-based payment rate, we proposed to recalculate their mean unit cost from all of the CY 2018 claims data and update cost report information available for the CY 2020 final rule with comment period to determine their final per day cost.
Consequently, the packaging status of some HCPCS codes for drugs, biologicals, and therapeutic radiopharmaceuticals in the proposed rule may be different from the same drugs' HCPCS codes' packaging status determined based on the data used for the final rule with comment period. Under such circumstances, we proposed to continue to follow the established policies initially adopted for the CY 2005 OPPS (69 FR 65780) in order to more equitably pay for those drugs whose costs fluctuate relative to the proposed CY 2020 OPPS drug packaging threshold and the drug's payment status (packaged or separately payable) in CY 2019. These established policies have not changed for many years and are the same as described in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70434). Specifically, for CY 2020, consistent with our historical practice, we proposed to apply the following policies to these HCPCS codes for drugs, biologicals, and therapeutic radiopharmaceuticals whose relationship to the drug packaging threshold changes based on the updated drug packaging threshold and on the final updated data:
- HCPCS codes for drugs and biologicals that were paid separately in CY 2019 and that are proposed for separate payment in CY 2020, and that then have per day costs equal to or less than the CY 2020 final rule drug packaging threshold, based on the updated ASPs and hospital claims data used for the CY 2020 final rule, would continue to receive separate payment in CY 2020.
- HCPCS codes for drugs and biologicals that were packaged in CY 2019 and that are proposed for separate payment in CY 2020, and that then have per day costs equal to or less than the CY 2020 final rule drug packaging threshold, based on the updated ASPs and hospital claims data used for the CY 2020 final rule, would remain packaged in CY 2020.
- HCPCS codes for drugs and biologicals for which we proposed packaged payment in CY 2020 but that then have per-day costs greater than the CY 2020 final rule drug packaging threshold, based on the updated ASPs and hospital claims data used for the CY 2020 final rule, would receive separate payment in CY 2020.
We did not receive any public comments on our proposal to recalculate the mean unit cost for items that do not currently have an ASP-based payment rate from all of the CY 2018 claims data and updated cost report information available for this CY 2020 final rule with comment period to determine their final per day cost. We also did not receive any public comments on our proposal to continue to follow the established policies, initially adopted for the CY 2005 OPPS (69 FR 65780), when the packaging status of some HCPCS codes for drugs, biologicals, and therapeutic radiopharmaceuticals in the proposed rule may be different from the same drug HCPCS code's packaging status determined based on the data used for the final rule with comment period. Therefore, for CY 2020, we are finalizing these two proposals without modification.
c. Policy Packaged Drugs, Biologicals, and Radiopharmaceuticals
As mentioned earlier in this section, in the OPPS, we package several categories of drugs, biologicals, and radiopharmaceuticals, regardless of the cost of the products. Because the products are packaged according to the policies in 42 CFR 419.2(b), we refer to these packaged drugs, biologicals, and radiopharmaceuticals as “policy-packaged” drugs, biologicals, and radiopharmaceuticals. These policies are either longstanding or based on longstanding principles and inherent to the OPPS and are as follows:
- Anesthesia, certain drugs, biologicals, and other pharmaceuticals; medical and surgical supplies and equipment; surgical dressings; and devices used for external reduction of fractures and dislocations (§ 419.2(b)(4));
- Intraoperative items and services (§ 419.2(b)(14));
- Drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure (including, but not limited to, diagnostic radiopharmaceuticals, contrast agents, and pharmacologic stress agents) (§ 419.2(b)(15)); and
- Drugs and biologicals that function as supplies when used in a surgical procedure (including, but not limited to, skin substitutes and similar products that aid wound healing and implantable biologicals) (§ 419.2(b)(16)).
The policy at § 419.2(b)(16) is broader than that at § 419.2(b)(14). As we stated in the CY 2015 OPPS/ASC final rule with comment period: “We consider all items related to the surgical outcome and provided during the hospital stay in which the surgery is performed, including postsurgical pain management drugs, to be part of the surgery for purposes of our drug and biological surgical supply packaging policy” (79 FR 66875). The category described by § 419.2(b)(15) is large and includes diagnostic radiopharmaceuticals, contrast agents, stress agents, and some other products. The category described by § 419.2(b)(16) includes skin substitutes and some other products. We believe it is important to reiterate that cost consideration is not a factor when determining whether an item is a surgical supply (79 FR 66875).
We did not make any proposals to revise our policy-packaged drug policy.
Comment: CMS received several comments from stakeholders regarding the policy-packaged status of diagnostic radiopharmaceuticals. Several commenters recommended that CMS continue to apply the nuclear medicine procedure to radiolabeled product edits to ensure that all packaged costs are included on nuclear medicine claims in order to establish appropriate payment rates in the future. There was concern that many providers performing nuclear medicine procedures are not including the cost of diagnostic radiopharmaceuticals used for the procedures in their claims submissions. Commenters believe this lack of drug cost reporting could be causing the cost of nuclear medicine procedures to be underreported and therefore requests that the radiolabeled product edits be reinstated.
Response: We appreciated the commenter's feedback; however, we do not agree with the commenter that we should reinstate the nuclear medicine procedure to radiolabeled product edits, which required a diagnostic radiopharmaceutical to be present on the same claim as a nuclear medicine procedure for payment under the OPPS to be made. As previously discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58965), the edits were in place between CY 2008 and CY 2014 (78 FR 75033). We believe the period of time in which the edits were in place was sufficient for hospitals to gain experience reporting procedures involving radiolabeled products and to become accustomed to ensuring that they code and report charges so that their claims fully and appropriately reflect the costs of those radiolabeled products. As with all other items and services recognized under the OPPS, we expect hospitals to code and report their costs appropriately, regardless of whether there are claims processing edits in place.
Comment: Several commenters requested that diagnostic radiopharmaceuticals be paid separately in all cases, not just when the drugs have pass-through payment status. Some commenters suggested payment based upon ASP, WAC, AWP, or mean unit cost data derived from hospital claims. Some commenters mentioned that pass-through payment status helps the diffusion of new diagnostic radiopharmaceuticals into the market, but is not enough to make up for the inadequate payment after pass-through expires. Several commenters recommended treating diagnostic radiopharmaceuticals similarly to therapeutic radiopharmaceuticals. Commenters opposed incorporating the cost of the drug into the associated APC, and provided limited evidence showing procedures in which diagnostic radiopharmaceuticals are considered to be a surgical supply that the commenter believed are often paid at a lower rate than the payment rate for the diagnostic radiopharmaceutical itself when the drug was paid separately because it had pass-through payment status. Additionally, commenters proposed alternative payment methodologies such as subjecting diagnostic radiopharmaceuticals to the drug packaging threshold, creating separate APC payments for diagnostic radiopharmaceuticals that cost more than $500, or using ASP, WAC, or AWP to account for packaged radiopharmaceutical costs. Conversely, other commenters disagreed with the idea to pay separately for diagnostic radiopharmaceuticals that cost more than $500 because they claimed that this would incentivize radiopharmaceutical companies to raise their prices to exceed the threshold. Additionally, commenters stated that nearly 95 percent of radiopharmaceuticals are priced less than $500, so creating a diagnostic radiopharmaceutical packaging threshold of $500 would not be appropriate.
Response: We thank commenters for their responses. We continue to believe that diagnostic radiopharmaceuticals are an integral component of many nuclear medicine and imaging procedures and charges associated with them should be reported on hospital claims to the extent they are used. Therefore, the payment for the radiopharmaceuticals is reflected within the payment for the primary procedure. In response to the comment regarding the proposed cost of the packaged procedure in CY 2020 being substantially lower than the payment rate of the radiopharmaceutical when it was on pass-through payment status plus the payment rate of the procedure associated with the radiopharmaceutical, we note the rates are established in a manner that uses the average, more specifically the geometric mean, of reported costs to furnish the procedure based on data submitted to CMS from all hospitals paid under the OPPS to set the payment rate for the service. Accordingly, the costs that are calculated by Medicare reflect the average costs of items and services that are packaged into a primary procedure and will not necessarily equal the sum of the cost of the primary procedure and the average sales price of items and services because the billing patterns of hospitals may not reflect that a particular item or service is always billed with the primary procedure. Furthermore, the costs will be based on the reported costs submitted to Medicare by the hospitals and not the list price established by the manufacturer. Claims data that include the radiopharmaceutical packaged with the associated procedure reflect the combined cost of the procedure and the radiopharmaceutical used in the procedure. Additionally, we do not believe it is appropriate to create a new packaging threshold specifically for diagnostic radiopharmaceuticals as that does not align with our overall packaging policy and limited data has been submitted to support a specific threshold. With respect to the request that we create a new APC for each radiopharmaceutical product, we do not believe it is appropriate to create unique APCs for diagnostic radiopharmaceuticals. Diagnostic radiopharmaceuticals function as supplies during a diagnostic test or procedure and following our longstanding packaging policy, these items are packaged under the OPPS, which supports our goal of making OPPS payments consistent with those of a prospective payment system, which packages costs into a single aggregate payment for a service, encounter, or episode of care. Furthermore, diagnostic radiopharmaceuticals function as supplies that enable the provision of an independent service, and are not themselves the primary therapeutic modality, and therefore, we do not believe they warrant separate payment through creation of a unique APC at this time. We welcome ongoing dialogue with stakeholders regarding suggestions for payment changes for consideration for future rulemaking.
d. Packaging Determination for HCPCS Codes That Describe the Same Drug or Biological but Different Dosages
In the CY 2010 OPPS/ASC final rule with comment period (74 FR 60490 through 60491), we finalized a policy to make a single packaging determination for a drug, rather than an individual HCPCS code, when a drug has multiple HCPCS codes describing different dosages because we believe that adopting the standard HCPCS code-specific packaging determinations for these codes could lead to inappropriate payment incentives for hospitals to report certain HCPCS codes instead of others. We continue to believe that making packaging determinations on a drug-specific basis eliminates payment incentives for hospitals to report certain HCPCS codes for drugs and allows hospitals flexibility in choosing to report all HCPCS codes for different dosages of the same drug or only the lowest dosage HCPCS code. Therefore, we proposed to continue our policy to make packaging determinations on a drug-specific basis, rather than a HCPCS code-specific basis, for those HCPCS codes that describe the same drug or biological but different dosages in CY 2020.
For CY 2020, in order to propose a packaging determination that is consistent across all HCPCS codes that describe different dosages of the same drug or biological, we aggregated both our CY 2018 claims data and our pricing information at ASP+6 percent across all of the HCPCS codes that describe each distinct drug or biological in order to determine the mean units per day of the drug or biological in terms of the HCPCS code with the lowest dosage descriptor. The following drugs did not have pricing information available for the ASP methodology for this CY 2020 OPPS/ASC proposed rule, and as is our current policy for determining the packaging status of other drugs, we used the mean unit cost available from the CY 2018 claims data to make the proposed packaging determinations for these drugs: HCPCS code J1840 (Injection, kanamycin sulfate, up to 500 mg); HCPCS code J1850 (Injection, kanamycin sulfate, up to 75 mg); HCPCS code J3472 (Injection, hyaluronidase, ovine, preservative free, per 1000 usp units); HCPCS code J7100 (Infusion, dextran 40, 500 ml); and HCPCS code J7110 (Infusion, dextran 75, 500 ml).
For all other drugs and biologicals that have HCPCS codes describing different doses, we then multiplied the proposed weighted average ASP+6 percent per unit payment amount across all dosage levels of a specific drug or biological by the estimated units per day for all HCPCS codes that describe each drug or biological from our claims data to determine the estimated per day cost of each drug or biological at less than or equal to the proposed CY 2020 drug packaging threshold of $130 (so that all HCPCS codes for the same drug or biological would be packaged) or greater than the proposed CY 2020 drug packaging threshold of $130 (so that all HCPCS codes for the same drug or biological would be separately payable). The proposed packaging status of each drug and biological HCPCS code to which this methodology would apply in CY 2020 was displayed in Table 18 of the proposed rule (84 FR 39499).
We did not receive any public comments on this proposal. Therefore, for CY 2020, we are finalizing our CY 2020 proposal, without modification, to continue our policy to make packaging determinations on a drug-specific basis, rather than a HCPCS code-specific basis, for those HCPCS codes that describe the same drug or biological but different dosages. Table 44 below displays the final packaging status of each drug and biological HCPCS code to which the finalized methodology applies for CY 2020.

2. Payment for Drugs and Biologicals Without Pass-Through Status That Are Not Packaged
a. Payment for Specified Covered Outpatient Drugs (SCODs) and Other Separately Payable Drugs and Biologicals
Section 1833(t)(14) of the Act defines certain separately payable radiopharmaceuticals, drugs, and biologicals and mandates specific payments for these items. Under section 1833(t)(14)(B)(i) of the Act, a “specified covered outpatient drug” (known as a SCOD) is defined as a covered outpatient drug, as defined in section 1927(k)(2) of the Act, for which a separate APC has been established and that either is a radiopharmaceutical agent or is a drug or biological for which payment was made on a pass-through basis on or before December 31, 2002.
Under section 1833(t)(14)(B)(ii) of the Act, certain drugs and biologicals are designated as exceptions and are not included in the definition of SCODs. These exceptions are—
- A drug or biological for which payment is first made on or after January 1, 2003, under the transitional pass-through payment provision in section 1833(t)(6) of the Act.
- A drug or biological for which a temporary HCPCS code has not been assigned.
- During CYs 2004 and 2005, an orphan drug (as designated by the Secretary).
Section 1833(t)(14)(A)(iii) of the Act requires that payment for SCODs in CY 2006 and subsequent years be equal to the average acquisition cost for the drug for that year as determined by the Secretary, subject to any adjustment for overhead costs and taking into account the hospital acquisition cost survey data collected by the Government Accountability Office (GAO) in CYs 2004 and 2005, and later periodic surveys conducted by the Secretary as set forth in the statute. If hospital acquisition cost data are not available, the law requires that payment be equal to payment rates established under the methodology described in section 1842(o), section 1847A, or section 1847B of the Act, as calculated and adjusted by the Secretary as necessary for purposes of paragraph (14). We refer to this alternative methodology as the “statutory default.” Most physician Part B drugs are paid at ASP+6 percent in accordance with section 1842(o) and section 1847A of the Act.
Section 1833(t)(14)(E)(ii) of the Act provides for an adjustment in OPPS payment rates for SCODs to take into account overhead and related expenses, such as pharmacy services and handling costs. Section 1833(t)(14)(E)(i) of the Act required MedPAC to study pharmacy overhead and related expenses and to make recommendations to the Secretary regarding whether, and if so how, a payment adjustment should be made to compensate hospitals for overhead and related expenses. Section 1833(t)(14)(E)(ii) of the Act authorizes the Secretary to adjust the weights for ambulatory procedure classifications for SCODs to take into account the findings of the MedPAC study.[66]
It has been our policy since CY 2006 to apply the same treatment to all separately payable drugs and biologicals, which include SCODs, and drugs and biologicals that are not SCODs. Therefore, we apply the payment methodology in section 1833(t)(14)(A)(iii) of the Act to SCODs, as required by statute, but we also apply it to separately payable drugs and biologicals that are not SCODs, which is a policy determination rather than a statutory requirement. In this CY 2020 OPPS/ASC proposed rule, we proposed to apply section 1833(t)(14)(A)(iii)(II) of the Act to all separately payable drugs and biologicals, including SCODs. Although we do not distinguish SCODs in this discussion, we note that we are required to apply section 1833(t)(14)(A)(iii)(II) of the Act to SCODs, but we also are applying this provision to other separately payable drugs and biologicals, consistent with our history of using the same payment methodology for all separately payable drugs and biologicals.
For a detailed discussion of our OPPS drug payment policies from CY 2006 to CY 2012, we refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68383 through 68385). In the CY 2013 OPPS/ASC final rule with comment period (77 FR 68386 through 68389), we first adopted the statutory default policy to pay for separately payable drugs and biologicals at ASP+6 percent based on section 1833(t)(14)(A)(iii)(II) of the Act. We have continued this policy of paying for separately payable drugs and biologicals at the statutory default for CYs 2014 through 2019.
b. CY 2020 Payment Policy
For CY 2020, we proposed to continue our payment policy that has been in effect since CY 2013 to pay for separately payable drugs and biologicals at ASP+6 percent in accordance with section 1833(t)(14)(A)(iii)(II) of the Act (the statutory default). We proposed to continue to pay for separately payable nonpass-through drugs acquired with a 340B discount at a rate of ASP minus 22.5 percent, but we also solicited comments on alternative policies as well as the appropriate remedy for CYs 2018 and 2019 in the event that we do not prevail on appeal in the pending litigation, as discussed in greater detail later in this section. We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59353 through 59371) and the CY 2019 OPPS/ASC final rule with comment period (83 FR 58979 through 58981) for more information about how the payment rate for drugs acquired with a 340B discount was established.
In the case of a drug or biological during an initial sales period in which data on the prices for sales for the drug or biological are not sufficiently available from the manufacturer, section 1847A(c)(4) of the Act permits the Secretary to make payments that are based on WAC. Under section 1833(t)(14)(A)(iii)(II), the amount of payment for a separately payable drug equals the average price for the drug for the year established under, among other authorities, section 1847A of the Act. As explained in greater detail in the CY 2019 PFS final rule, under section 1847A(c)(4), although payments may be based on WAC, unlike section 1847A(b) of the Act (which specifies that payments using ASP or WAC must be made with a 6 percent add-on), section 1847A(c)(4) of the Act does not require that a particular add-on amount be applied to WAC-based pricing for this initial period when ASP data is not available. Consistent with section 1847A(c)(4) of the Act, in the CY 2019 PFS final rule (83 FR 59661 to 59666), we finalized a policy that, effective January 1, 2019, WAC-based payments for Part B drugs made under section 1847A(c)(4) of the Act will utilize a 3-percent add-on in place of the 6-percent add-on that was being used according to our policy in effect as of CY 2018. For the CY 2019 OPPS, we followed the same policy finalized in the CY 2019 PFS final rule (83 FR 59661 to 59666). For the CY 2020 OPPS, we proposed to continue to utilize a 3 percent add-on instead of a 6-percent add-on for WAC-based drugs pursuant to our authority under section 1833(t)(14)(A)(iii)(II) of the Act, which provides, in part, that the amount of payment for a SCOD is the average price of the drug in the year established under section 1847A of the Act. We also proposed to apply this provision to non-SCOD separately payable drugs. Because we proposed to establish the average price for a WAC-based drug under section 1847A of the Act as WAC+3 percent instead of WAC+6 percent, we believe it is appropriate to price separately payable WAC-based drugs at the same amount under the OPPS. We proposed that, if finalized, our proposal to pay for drugs or biologicals at WAC+3 percent, rather than WAC+6 percent, would apply whenever WAC-based pricing is used for a drug or biological. For drugs and biologicals that would otherwise be subject to a payment reduction because they were acquired under the 340B Program, the 340B Program rate (in this case, WAC minus 22.5 percent) would continue to apply. We refer readers to the CY 2019 PFS final rule (83 FR 59661 to 59666) for additional background on this proposal.
Comment: Several commenters opposed our proposal to utilize a 3 percent add-on instead of a 6 percent add-on for drugs that are paid based on WAC under section 1847A(c)(4) of the Act. Commenters were concerned that paying less for new drugs may discourage the use of new innovative drugs and inhibit access to patients. Commenters also noted that the sequestration cuts further decreased payment for drugs, which leaves a smaller margin for providers. Additionally, some commenters believe that this proposal would only negatively impact providers, and would not address increasing drug costs. Additionally, commenters suggested excluding certain drugs and biologicals from this policy, such as biosimilar biological products or radiopharmaceuticals. These commenters felt as though the policy was appropriate for drugs in general, but not for the previously mentioned products, which could potentially offer savings to the Medicare program if utilized in the case of biosimilars or which have a higher associated overhead in the case of radiopharmaceuticals. Commenters also discussed value-based payments as a more meaningful change than this proposal.
Response: We appreciate the commenter's feedback. We continue to believe our policy will improve Medicare payment rates by better aligning payments with drug acquisition costs, which is of the utmost importance to CMS as Part B drug spending has grown significantly. WAC plus a 3 percent add-on is more comparable to an ASP plus a 6 percent add-on, since the WAC pricing does not reflect many of the discounts associated with ASP, such as rebates. This proposal to continue to utilize a 3 percent add-on instead of a 6 percent add-on for drugs that are paid based on WAC under section 1847A(c)(4) of the Act is consistent with MedPAC's previous analysis and recommendations in its June 2017 Report to the Congress. This policy is not meant to provide preferential treatment to any specific drug or biological, but to address WAC based payment under 1847A of the Act. We remind commenters that this proposal still results in a net payment greater than the WAC. In addition, this policy decreases the beneficiary cost-sharing for these drugs. This could help Medicare beneficiaries afford to pay for new drugs by reducing their out-of-pocket expenses.
After consideration of the public comments we received, we are finalizing our proposal, without modification, to utilize a 3 percent add-on instead of a 6 percent add-on for drugs that are paid based on WAC under section 1847A(c)(4) of the Act pursuant to our authority under section 1833(t)(14)(A)(iii)(II) of the Act.
We proposed that payments for separately payable drugs and biologicals are included in the budget neutrality adjustments, under the requirements in section 1833(t)(9)(B) of the Act. We also proposed that the budget neutral weight scalar not be applied in determining payments for these separately paid drugs and biologicals.
We note that separately payable drug and biological payment rates listed in Addenda A and B to the proposed rule (available via the internet on the CMS website), which illustrate the proposed CY 2020 payment of ASP+6 percent for separately payable nonpass-through drugs and biologicals and ASP+6 percent for pass-through drugs and biologicals, reflect either ASP information that is the basis for calculating payment rates for drugs and biologicals in the physician's office setting effective April 1, 2019, or WAC, AWP, or mean unit cost from CY 2018 claims data and updated cost report information available for the proposed rule. In general, these published payment rates are not the same as the actual January 2020 payment rates. This is because payment rates for drugs and biologicals with ASP information for January 2020 will be determined through the standard quarterly process where ASP data submitted by manufacturers for the third quarter of CY 2019 (July 1, 2019 through September 30, 2019) will be used to set the payment rates that are released for the quarter beginning in January 2020 near the end of December 2019. In addition, payment rates for drugs and biologicals in Addenda A and B to the proposed rule for which there was no ASP information available for April 2019 are based on mean unit cost in the available CY 2018 claims data. If ASP information becomes available for payment for the quarter beginning in January 2020, we will price payment for these drugs and biologicals based on their newly available ASP information. Finally, there may be drugs and biologicals that have ASP information available for the proposed rule (reflecting April 2019 ASP data) that do not have ASP information available for the quarter beginning in January 2020. These drugs and biologicals would then be paid based on mean unit cost data derived from CY 2018 hospital claims. Therefore, the proposed payment rates listed in Addenda A and B to the proposed rule are not for January 2020 payment purposes and are only illustrative of the CY 2020 OPPS payment methodology using the most recently available information at the time of issuance of the proposed rule.
c. Biosimilar Biological Products
For CY 2016 and CY 2017, we finalized a policy to pay for biosimilar biological products based on the payment allowance of the product as determined under section 1847A of the Act and to subject nonpass-through biosimilar biological products to our annual threshold-packaged policy (for CY 2016, 80 FR 70445 through 70446; and for CY 2017, 81 FR 79674). In the CY 2018 OPPS/ASC proposed rule (82 FR 33630), for CY 2018, we proposed to continue this same payment policy for biosimilar biological products.
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59351), we noted that, with respect to comments we received regarding OPPS payment for biosimilar biological products, in the CY 2018 PFS final rule, CMS finalized a policy to implement separate HCPCS codes for biosimilar biological products. Therefore, consistent with our established OPPS drug, biological, and radiopharmaceutical payment policy, HCPCS coding for biosimilar biological products is based on the policy established under the CY 2018 PFS final rule.
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59351), after consideration of the public comments we received, we finalized our proposed payment policy for biosimilar biological products, with the following technical correction: All biosimilar biological products are eligible for pass-through payment and not just the first biosimilar biological product for a reference product. In the CY 2019 OPPS/ASC proposed rule (83 FR 37123), for CY 2019, we proposed to continue the policy in place from CY 2018 to make all biosimilar biological products eligible for pass-through payment and not just the first biosimilar biological product for a reference product.
In addition, in CY 2018, we adopted a policy that biosimilars without pass-through payment status that were acquired under the 340B Program would be paid the ASP of the biosimilar minus 22.5 percent of the reference product's ASP (82 FR 59367). We adopted this policy in the CY 2018 OPPS/ASC final rule with comment period because we believe that biosimilars without pass-through payment status acquired under the 340B Program should be treated in the same manner as other drugs and biologicals acquired through the 340B Program. As noted earlier, biosimilars with pass-through payment status are paid their own ASP+6 percent of the reference product's ASP. Separately payable biosimilars that do not have pass-through payment status and are not acquired under the 340B Program are also paid their own ASP+6 percent of the reference product's ASP. If a biosimilar does not have ASP pricing, but instead has WAC pricing, the WAC pricing add-on of either 3 percent or 6 percent is calculated from the biosimilar's WAC and is not calculated from the WAC price of the reference product.
As noted in the CY 2019 OPPS/ASC proposed rule (83 FR 37123), several stakeholders raised concerns to us that the current payment policy for biosimilars acquired under the 340B Program could unfairly lower the OPPS payment for biosimilars not on pass-through payment status because the payment reduction would be based on the reference product's ASP, which would generally be expected to be priced higher than the biosimilar, thus resulting in a more significant reduction in payment than if the 22.5 percent was calculated based on the biosimilar's ASP. We agreed with stakeholders that the current payment policy could unfairly lower the price of biosimilars without pass-through payment status that are acquired under the 340B Program. In addition, we believe that these changes would better reflect the resources and production costs that biosimilar manufacturers incur. We also believe this approach is more consistent with the payment methodology for 340B-acquired drugs and biologicals, for which the 22.5 percent reduction is calculated based on the drug or biological's ASP, rather than the ASP of another product. In addition, we believe that paying for biosimilars acquired under the 340B Program at ASP minus 22.5 percent of the biosimilar's ASP, rather than 22.5 percent of the reference product's ASP, will more closely approximate hospitals' acquisition costs for these products.
Accordingly, in the CY 2019 OPPS/ASC proposed rule (83 FR 37123), for CY 2019, we proposed changes to our Medicare Part B drug payment methodology for biosimilars acquired under the 340B Program. Specifically, for CY 2019 and subsequent years, in accordance with section 1833(t)(14)(A)(iii)(II) of the Act, we proposed to pay nonpass-through biosimilars acquired under the 340B Program at ASP minus 22.5 percent of the biosimilar's ASP instead of the biosimilar's ASP minus 22.5 percent of the reference product's ASP. This proposal was finalized without modification in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58977).
For CY 2020, we proposed to continue our policy to make all biosimilar biological products eligible for pass-through payment and not just the first biosimilar biological product for a reference product. We also proposed to continue our policy to pay nonpass-through biosimilars acquired under the 340B Program at the biosimilar's ASP minus 22.5 percent of the biosimilar's ASP instead of the biosimilar's ASP minus 22.5 percent of the reference product's ASP, in accordance with section 1833(t)(14)(A)(iii)(II) of the Act. In addition, as discussed further below, we solicited comments on the appropriate remedy in the event of an adverse decision on appeal in the litigation related to our policy for payment of 340B-acquired drugs and biologicals, including on whether paying for 340B-acquired biosimilars at ASP+3 percent of the reference product's ASP would be an appropriate policy in line with that discussion. Our policy for 340B-acquired drugs and biologicals is discussed in V.B.6. of this final rule with comment period.
Comment: Many commenters supported our biosimilar proposal to continue our policy from CY 2018 to make biosimilar biological products eligible for pass-through payment and not just the first biosimilar biological product for a reference product. Commenters believe this would continue to improve access to these treatments and lower costs, and they stressed the importance of consistency with biosimilar payment. Commenters stated that there is a large disparity between payment for biosimilars and their reference products and that this proposal helps to mitigate that concern. Commenters also advocated for additional proposals to increase the utilization of biosimilars, such as extended pass-through payment.
Response: We appreciate the commenters' support. We believe this proposal will continue to encourage competition, lower costs for the Medicare program and beneficiaries, and eliminate any financial incentive to utilize one product over another. We will continue to assess biosimilar utilization under the OPPS.
Comment: Several commenters supported our proposal to pay nonpass-through biosimilars acquired under the 340B Program at ASP minus 22.5 percent of the biosimilar's ASP in accordance with section 1833(t)(14)(A)(iii)(II) of the Act.
Response: We appreciate the commenters' support. Please see section V.B.6 for a discussion of payment for biosimilars aquired under 340B.
Comment: Some commenters did not support our proposal to continue our CY 2018 policy to make all biosimilar biological products eligible for pass-through payment and not just the first biosimilar biological product for a reference product. Commenters believe biosimilars are not new or innovative drugs or biologicals, because they believe the originator product is the only new and innovative product. Therefore, they stated biosimilars should not be considered for pass-through payment status. Additionally, commenters stated there should be a level playing field between biosimilars and their originator reference products in order to increase competition and reduce costs for beneficiaries. Commenters believe that this proposal could potentially lead to increased Medicare spending on biosimilars, and commenters articulated concerns that therapies will be interrupted by providers switching from innovator products to biosimilars.
Response: As discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58977), we continue to believe that eligibility for pass-through payment status reflects the unique, complex nature of biosimilars and is important as biosimilars become established in the market, just as it is for all other new drugs and biologicals. Additionally, we are not convinced that making all biosimilar biological products eligible for pass-through payment status will lead to inappropriate treatment changes from a reference product without pass-through payment to a biosimilar product with pass-through payment. Under current policy, both originator products and their associated biosimilars receive the same percentage add-on amount, regardless of the ASP of the product; therefore, we do not believe that therapies will be interrupted by providers switching from innovator products to biosimilars. We note that Section 351(i) of the Public Health Service Act defines biosimilarity to mean “that the biological product is highly similar to the reference product notwithstanding minor differences in clinically inactive components” and that “there are no clinically meaningful differences between the biological product and the reference product in terms of the safety, purity, and potency of the product.” Therefore, concerns that therapy would be interrupted by a switch from an innovator product to a biosimilar are unfounded as the biosimilar has been determined to have no clinically meaningful difference from the reference product. In regards to the increased payment of biosimilars under this policy, overall increased competition due to more biosimilars on the market as a result of this policy is expected to drive payments down for both Medicare and for beneficiaries over time, even if there may be increased spending on biosimilars in the short term.
For CY 2020, after consideration of the public comments we received, we are finalizing our proposed payment policy for biosimilar products, without modification, to continue the policy established in CY 2018 to make all biosimilar biological products eligible for pass-through payment and not just the first biosimilar biological product for a reference product. We also are finalizing our proposal to pay nonpass-through biosimilars acquired under the 340B Program at the biosimilar's ASP minus 22.5 percent of the reference product's ASP, in accordance with section 1833(t)(14)(A)(iii)(II) of the Act.
3. Payment Policy for Therapeutic Radiopharmaceuticals
In the CY 2020 OPPS/ASC proposed rule (84 FR 39502), for CY 2020, we proposed to continue the payment policy for therapeutic radiopharmaceuticals that began in CY 2010. We pay for separately payable therapeutic radiopharmaceuticals under the ASP methodology adopted for separately payable drugs and biologicals. If ASP information is unavailable for a therapeutic radiopharmaceutical, we base therapeutic radiopharmaceutical payment on mean unit cost data derived from hospital claims. We believe that the rationale outlined in the CY 2010 OPPS/ASC final rule with comment period (74 FR 60524 through 60525) for applying the principles of separately payable drug pricing to therapeutic radiopharmaceuticals continues to be appropriate for nonpass-through, separately payable therapeutic radiopharmaceuticals in CY 2020. Therefore, we proposed for CY 2020 to pay all nonpass-through, separately payable therapeutic radiopharmaceuticals at ASP+6 percent, based on the statutory default described in section 1833(t)(14)(A)(iii)(II) of the Act. For a full discussion of ASP-based payment for therapeutic radiopharmaceuticals, we refer readers to the CY 2010 OPPS/ASC final rule with comment period (74 FR 60520 through 60521). We also proposed to rely on CY 2018 mean unit cost data derived from hospital claims data for payment rates for therapeutic radiopharmaceuticals for which ASP data are unavailable and to update the payment rates for separately payable therapeutic radiopharmaceuticals according to our usual process for updating the payment rates for separately payable drugs and biologicals on a quarterly basis if updated ASP information is unavailable. For a complete history of the OPPS payment policy for therapeutic radiopharmaceuticals, we refer readers to the CY 2005 OPPS final rule with comment period (69 FR 65811), the CY 2006 OPPS final rule with comment period (70 FR 68655), and the CY 2010 OPPS/ASC final rule with comment period (74 FR 60524). The proposed CY 2020 payment rates for nonpass-through, separately payable therapeutic radiopharmaceuticals were included in Addenda A and B to the proposed rule (which are available via the internet on the CMS website).
Comment: Commenters supported the continuation of the policy to pay ASP+6 percent for radiopharmaceuticals, if available, and to base payment on the mean unit cost derived from hospital claims data when not available. Commenters also stressed the high overhead, handling, compounding and storage costs associated with delivering therapeutic radiopharmaceuticals and asked CMS to look into higher payment rates for radiopharmaceuticals or ways to compensate hospitals for the higher overhead and handling costs.
Response: We appreciate the commenters' support. As previously stated, we continue to believe a single payment is appropriate for therapeutic radiopharmaceuticals and that the payment rate of ASP+6 percent is appropriate because it provides payment for both the therapeutic radiopharmaceutical's acquisition cost and the associated costs such as storage and handling of the radiopharmaceuticals. Payment for the radiopharmaceutical and radiopharmaceutical processing services is made through the single ASP-based payment.
For CY 2020, after consideration of the public comments we received, we are finalizing our proposal, without modification, to continue to pay all nonpass-through, separately payable therapeutic radiopharmaceuticals at ASP+6 percent. We are also finalizing our proposal to continue to rely on CY 2018 mean unit cost data derived from hospital claims data for payment rates for therapeutic radiopharmaceuticals for which ASP data are unavailable. The CY 2020 final payment rates for nonpass-through separately payable therapeutic radiopharmaceuticals are included in Addenda A and B to this final rule with comment period (which are available via the internet on the CMS website).
4. Payment for Blood Clotting Factors
For CY 2019, we provided payment for blood clotting factors under the same methodology as other nonpass-through separately payable drugs and biologicals under the OPPS and continued paying an updated furnishing fee (83 FR 58979). That is, for CY 2019, we provided payment for blood clotting factors under the OPPS at ASP+6 percent, plus an additional payment for the furnishing fee. We note that when blood clotting factors are provided in physicians' offices under Medicare Part B and in other Medicare settings, a furnishing fee is also applied to the payment. The CY 2019 updated furnishing fee was $0.220 per unit.
For CY 2020, we proposed to pay for blood clotting factors at ASP+6 percent, consistent with our proposed payment policy for other nonpass-through, separately payable drugs and biologicals, and to continue our policy for payment of the furnishing fee using an updated amount. Our policy to pay for a furnishing fee for blood clotting factors under the OPPS is consistent with the methodology applied in the physician's office and in the inpatient hospital setting. These methodologies were first articulated in the CY 2006 OPPS final rule with comment period (70 FR 68661) and later discussed in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66765). The proposed furnishing fee update is based on the percentage increase in the Consumer Price Index (CPI) for medical care for the 12-month period ending with June of the previous year. Because the Bureau of Labor Statistics releases the applicable CPI data after the PFS and OPPS/ASC proposed rules are published, we were not able to include the actual updated furnishing fee in the proposed rules. Therefore, in accordance with our policy, as finalized in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66765), we proposed to announce the actual figure for the percent change in the applicable CPI and the updated furnishing fee calculated based on that figure through applicable program instructions and posting on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/index.html.
Comment: Commenters supported CMS' proposal to continue to pay for blood clotting factors at ASP+6 percent plus a blood clotting factor furnishing fee in the hospital outpatient department.
Response: We appreciate the commenters' support.
After consideration of the public comments we received, we are finalizing our proposal, without modification, to provide payment for blood clotting factors under the same methodology as other separately payable drugs and biologicals under the OPPS and to continue payment of an updated furnishing fee. We will announce the actual figure of the percent change in the applicable CPI and the updated furnishing fee calculation based on that figure through the applicable program instructions and posting on the CMS website.
5. Payment for Nonpass-Through Drugs, Biologicals, and Radiopharmaceuticals With HCPCS Codes But Without OPPS Hospital Claims Data
For CY 2020, we proposed to continue to use the same payment policy as in CY 2019 for nonpass-through drugs, biologicals, and radiopharmaceuticals with HCPCS codes but without OPPS hospital claims data, which describes how we determine the payment rate for drugs, biologicals, or radiopharmaceuticals without an ASP. For a detailed discussion of the payment policy and methodology, we refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70442 through 70443). The proposed CY 2020 payment status of each of the nonpass-through drugs, biologicals, and radiopharmaceuticals with HCPCS codes but without OPPS hospital claims data is listed in Addendum B to the proposed rule, which is available via the internet on the CMS website.
We did not receive any comments on our proposal. Therefore, we are finalizing our CY 2020 proposal without modification, including our proposal to assign drug or biological products status indicator “K” and pay for them separately for the remainder of CY 2020 if pricing information becomes available. The CY 2020 payment status of each of the nonpass-through drugs, biologicals, and radiopharmaceuticals with HCPCS codes but without OPPS hospital claims data is listed in Addendum B to this final rule with comment period, which is available via the internet on the CMS website.
6. CY 2020 OPPS Payment Methodology for 340B Purchased Drugs
In the CY 2018 OPPS/ASC proposed rule (82 FR 33558 through 33724), we proposed changes to the Medicare Part B drug payment methodology for 340B hospitals. We proposed these changes to better, and more accurately, reflect the resources and acquisition costs that these hospitals incur. We believe that such changes would allow Medicare beneficiaries (and the Medicare program) to pay a more appropriate amount when hospitals participating in the 340B Program furnish drugs to Medicare beneficiaries that are purchased under the 340B Program. Subsequently, in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59369 through 59370), we finalized our proposal and adjusted the payment rate for separately payable drugs and biologicals (other than drugs on pass-through payment status and vaccines) acquired under the 340B Program from average sales price (ASP) plus 6 percent to ASP minus 22.5 percent. We stated that our goal was to make Medicare payment for separately payable drugs more aligned with the resources expended by hospitals to acquire such drugs, while recognizing the intent of the 340B Program to allow covered entities, including eligible hospitals, to stretch scarce resources in ways that enable hospitals to continue providing access to care for Medicare beneficiaries and other patients. Critical access hospitals are not included in this 340B policy change because they are paid under section 1834(g) of the Act. We also excepted rural sole community hospitals, children's hospitals, and PPS-exempt cancer hospitals from the 340B payment adjustment in CY 2018. In addition, as stated in the CY 2018 OPPS/ASC final rule with comment period, this policy change does not apply to drugs on pass-through payment status, which are required to be paid based on the ASP methodology, or vaccines, which are excluded from the 340B Program.
In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79699 through 79706), we implemented section 603 of the Bipartisan Budget Act of 2015. As a general matter, applicable items and services furnished in certain off-campus outpatient departments of a provider on or after January 1, 2017 are not considered covered outpatient services for purposes of payment under the OPPS and are paid “under the applicable payment system,” which is generally the Physician Fee Schedule (PFS). However, consistent with our policy to pay separately payable, covered outpatient drugs and biologicals acquired under the 340B Program at ASP minus 22.5 percent, rather than ASP+6 percent, when billed by a hospital paid under the OPPS that is not excepted from the payment adjustment, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59015 through 59022), we finalized a policy to pay ASP minus 22.5 percent for 340B-acquired drugs and biologicals furnished in nonexcepted off-campus PBDs paid under the PFS. We adopted this payment policy effective for CY 2019 and for subsequent years.
As discussed in the CY 2019 OPPS/ASC proposed rule (83 FR 37125), another topic that was brought to our attention since we finalized the payment adjustment for 340B-acquired drugs in the CY 2018 OPPS/ASC final rule with comment period was whether drugs that do not have ASP pricing but instead receive WAC or AWP pricing are subject to the 340B payment adjustment. We did not receive public comments on this topic in response to the CY 2018 OPPS/ASC proposed rule. However, we later heard from stakeholders that there had been some confusion about this issue. We clarified in the CY 2019 proposed rule that the 340B payment adjustment applies to drugs that are priced using either WAC or AWP, and it has been our policy to subject 340B-acquired drugs that use these pricing methodologies to the 340B payment adjustment since the policy was first adopted. The 340B payment adjustment for WAC-priced drugs is WAC minus 22.5 percent and AWP-priced drugs have a payment rate of 69.46 percent of AWP when the 340B payment adjustment is applied. The 69.46 percent of AWP is calculated by first reducing the original 95 percent of AWP price by 6 percent to generate a value that is similar to ASP or WAC with no percentage markup. Then we apply the 22.5 percent reduction to ASP/WAC-similar AWP value to obtain the 69.46 percent of AWP, which is similar to either ASP minus 22.5 percent or WAC minus 22.5 percent. The number of separately payable drugs receiving WAC or AWP pricing that are affected by the 340B payment adjustment is small—consisting of less than 10 percent of all separately payable Medicare Part B drugs in April 2018.
Furthermore, data limitations previously inhibited our ability to identify which drugs were acquired under the 340B Program in the Medicare OPPS claims data. This lack of information within the claims data has limited researchers' and our ability to precisely analyze differences in acquisition cost of 340B and non-340B acquired drugs with Medicare claims data. Accordingly, in the CY 2018 OPPS/ASC proposed rule (82 FR 33633), we stated our intent to establish a modifier, to be effective January 1, 2018, for hospitals to report with separately payable drugs that were not acquired under the 340B Program. Because a significant portion of hospitals paid under the OPPS participate in the 340B Program, we stated our belief that it is appropriate to presume that a separately payable drug reported on an OPPS claim was purchased under the 340B Program, unless the hospital identifies that the drug was not purchased under the 340B Program. We stated in the CY 2018 proposed rule that we intended to provide further details about this modifier in the CY 2018 OPPS/ASC final rule with comment period and/or through subregulatory guidance, including guidance related to billing for dually eligible beneficiaries (that is, beneficiaries covered under Medicare and Medicaid) for whom covered entities do not receive a discount under the 340B Program. As discussed in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59369 through 59370), to effectuate the payment adjustment for 340B-acquired drugs, CMS implemented modifier “JG”, effective January 1, 2018. Hospitals paid under the OPPS, other than a type of hospital excluded from the OPPS (such as critical access hospitals or those hospitals paid under the Maryland waiver), or excepted from the 340B drug payment policy for CY 2018, are required to report modifier “JG” on the same claim line as the drug HCPCS code to identify a 340B-acquired drug. For CY 2018, rural sole community hospitals, children's hospitals and PPS-exempt cancer hospitals are excepted from the 340B payment adjustment. These hospitals are required to report informational modifier “TB” for 340B-acquired drugs, and continue to be paid ASP+6 percent.
We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59353 through 59370) for a full discussion and rationale for the CY 2018 policies and use of modifier “JG”.
In the CY 2019 OPPS/ASC proposed rule (83 FR 37125), for CY 2019, we proposed to continue the 340B Program policies that were implemented in CY 2018 with the exception of the way we calculate payment for 340B-acquired biosimilars (that is, we proposed to pay for nonpass-through 340B-acquired biosimilars at ASP minus 22.5 percent of the biosimilar's ASP, rather than of the reference product's ASP). More information on our revised policy for the payment of biosimilars acquired through the 340B Program is available in section V.B.2.c. of the CY 2019 OPPS/ASC final rule with comment period. For CY 2019, we proposed, in accordance with section 1833(t)(14)(A)(iii)(II) of the Act, to pay for separately payable Medicare Part B drugs (assigned status indicator “K”), other than vaccines and drugs on pass-through payment status, that meet the definition of “covered outpatient drug” as defined in section 1927(k) of the Act, that are acquired through the 340B Program at ASP minus 22.5 percent when billed by a hospital paid under the OPPS that is not excepted from the payment adjustment. Medicare Part B drugs or biologicals excluded from the 340B payment adjustment include vaccines (assigned status indicator “F”, “L” or “M”) and drugs with OPPS transitional pass-through payment status (assigned status indicator “G”). As discussed in section V.B.2.c. of the CY 2019 OPPS/ASC proposed rule, we proposed to pay nonpass-through biosimilars acquired under the 340B Program at the biosimilar's ASP minus 22.5 percent of the biosimilar's ASP. We also proposed for CY 2019 that Medicare would continue to pay for drugs or biologicals that were not purchased with a 340B discount at ASP+6 percent.
As stated earlier, to effectuate the payment adjustment for 340B-acquired drugs, CMS implemented modifier “JG”, effective January 1, 2018. For CY 2019, we proposed that hospitals paid under the OPPS, other than a type of hospital excluded from the OPPS, or excepted from the 340B drug payment policy for CY 2018, continue to be required to report modifier “JG” on the same claim line as the drug HCPCS code to identify a 340B-acquired drug. We also proposed for CY 2019 that rural sole community hospitals, children's hospitals, and PPS-exempt cancer hospitals would continue to be excepted from the 340B payment adjustment. We proposed for CY 2019 that these hospitals be required to report informational modifier “TB” for 340B-acquired drugs, and continue to be paid ASP+6 percent. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 58981), after consideration of the public comments we received, we finalized our proposals without modification.
Our CY 2018 and 2019 OPPS payment policies for 340B-acquired drugs are the subject of ongoing litigation. On December 27, 2018, in the case of American Hospital Association et al. v. Azar et al., the United States District Court for the District of Columbia (hereinafter referred to as “the district court”) concluded in the context of reimbursement requests for CY 2018 that the Secretary exceeded his statutory authority by adjusting the Medicare payment rates for drugs acquired under the 340B Program to ASP minus 22.5 percent for that year.[67] In that same decision, the district court recognized the “`havoc that piecemeal review of OPPS payment could bring about' in light of the budget neutrality requirement,” and ordered supplemental briefing on the appropriate remedy.[68] On May 6, 2019, after briefing on remedy, the district court issued an opinion that reiterated that the 2018 rate reduction exceeded the Secretary's authority, and declared that the rate reduction for 2019 (which had been finalized since the Court's initial order was entered) also exceeded his authority.[69] Rather than ordering HHS to pay plaintiffs their alleged underpayments, however, the district court recognized that crafting a remedy is “no easy task, given Medicare's complexity,” [70] and initially remanded the issue to HHS to devise an appropriate remedy while also retaining jurisdiction. The district court acknowledged that “if the Secretary were to retroactively raise the 2018 and 2019 340B rates, budget neutrality would require him to retroactively lower the 2018 and 2019 rates for other Medicare Part B products and services.” [71] Id. at 19. “And because HHS has already processed claims under the previous rates, the Secretary would potentially be required to recoup certain payments made to providers; an expensive and time-consuming prospect.” [72]
CMS respectfully disagreed with the district court's understanding of the scope of its adjustment authority. On July 10, 2019, the district court entered final judgment, and the agency has filed its appeal. Nonetheless, CMS is taking the steps necessary to craft an appropriate remedy in the event of an unfavorable decision on appeal. Notably, after the proposed rule was issued, CMS announced in the Federal Register (84 FR 51590) its intent to conduct a 340B hospital survey to collect drug acquisition cost data for CY 2018 and 2019. Such survey data may be used in setting the Medicare payment amount for drugs acquired by 340B hospitals for cost years going forward, and also may be used to devise a remedy for prior years if the district court's ruling is upheld on appeal. The district court itself acknowledged that CMS may base the Medicare payment amount on average acquisition cost when survey data are available. See 348 F. Supp. 3d at 82. No 340B hospital disputed in the rulemakings for CY 2018 and 2019 that the ASP minus 22.5 percent formula was a conservative adjustment that represented the minimum discount that hospitals receive for drugs acquired through the 340B program—a significant omission because 340B hospitals have their own data regarding their drug acquisition costs. We thus anticipate that survey data collected for CY 2018 and 2019 will confirm that the ASP minus 22.5 percent rate is a conservative measure that overcompensates 340B hospitals. A remedy that relies on such survey data could avoid the remedial complexities discussed below and in the proposed rule.
Recognizing Medicare's complexity in formulating an appropriate remedy, any changes to the OPPS must be budget neutral, and reversal of the policy change, which raised rates for non-drug items and services by an estimated $1.6 billion for 2018 alone, could have a significant economic impact on the approximate 3,900 facilities that are paid for outpatient items and services covered under the OPPS. Second, any remedy that increases payments to 340B hospitals is likely to significantly affect beneficiary cost-sharing. The items and services that could be affected by the remedy were provided to millions of Medicare beneficiaries, who, by statute, are required to pay cost-sharing for such items and services, which is usually 20 percent of the total Medicare payment rate.
CMS solicited initial public comments on how to formulate a solution that would account for all of the complexities the district court recognized in the event of an unfavorable decision on appeal. A summary of the public comments received on a potential remedy is included later in this section. In the event 340B hospital survey data are not used to devise a remedy, we intend to consider this public input to further inform the steps that are required under the Administrative Procedure Act to provide adequate notice and an opportunity for meaningful comment on our proposed policies, which would entail devising the specific remedy itself, presenting the specific budget neutrality implications of that remedy in the proposed rule, and potentially calculating all the different payment rates under the OPPS for 340B-acquired drugs, as well as all other items and services under the OPPS. (In essence, we would need to provide hospitals with sufficient notice of the impact of the remedy on their rates to enable them to comment meaningfully on the proposed rule.) Our own best practices for preparing notices of proposed rulemaking dictate that we begin policy development in the year before the proposed rule is issued, and that we begin the rule drafting process in the first quarter of each year.
In the event of an unfavorable decision on appeal, if 340B hospital survey data are not used to devise a remedy, as we stated in the CY 2020 OPPS/ASC proposed rule, we anticipate proposing the specific remedy for CYs 2018 and 2019 in the CY 2021 OPPS/ASC proposed rule in the event of an unfavorable decision on appeal. Those potential proposals for CY 2021 would be informed by the comments that CMS solicited in the CY 2020 proposed rule.
Thus, for CY 2020, we proposed to continue to pay ASP minus 22.5 percent for 340B-acquired drugs, including when furnished in nonexcepted off-campus PBDs paid under the PFS. We proposed to continue the 340B policies that were implemented in CY 2018 with the exception of the way we are calculating payment for 340B-acquired biosimilars, which is discussed in section V.B.2.c. of the CY 2019 OPPS/ASC final rule with comment period, as well as the policy we finalized in CY 2019 to pay ASP minus 22.5 percent for 340B-acquired drugs and biologicals furnished in nonexcepted off-campus PBDs paid under the PFS.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39504), we also solicited public comment on the appropriate OPPS payment rate for 340B-acquired drugs, including whether a rate of ASP+3 percent could be an appropriate remedial payment amount for these drugs, both for CY 2020 and for purposes of determining the remedy for CYs 2018 and 2019. This amount would result in payment rates that are well above the actual costs hospitals incur in purchasing 340B drugs, and we proposed it solely because of the court decision. However, to the extent the courts are limiting the size of the payment reduction the agency can permissibly apply, the agency believes it could be appropriate to apply a payment reduction that is at the upper end of that limit, to the extent it has been or could be clearly defined, given the substantial discounts that hospitals receive through the 340B program. For example, absent further guidance from the Court of Appeals on what it believes is an appropriate “adjustment” amount, CMS could look to the district court's December 27, 2018 opinion, which cites to payment reductions of 0.2 percent and 2.9 percent as “not significant enough” to fall outside of the Secretary's authority to “adjust” ASP.[73] This payment rate would apply to 340B-acquired drugs and biologicals billed by a hospital paid under the OPPS that are not excepted from the payment adjustment and to 340B-acquired drugs and biologicals furnished in nonexcepted off-campus PBDs paid under the PFS. We welcomed public comments on payment rates other than ASP+3 percent that commenters believe would be appropriate for purposes of addressing CY 2020 payment as an alternative to our proposal above, as well as for potential future rulemaking related to CY 2018 and 2019.
Comments on the Appropriate Payment Rate for 340B-Acquired Drugs in CY 2020
Comment: Several commenters supported the continuation of the 340B Program policy of ASP minus 22.5 percent for CY 2020. One commenter believed the 340B program's recent growth may be contributing to the consolidation of community oncology practices. This commenter and others asserted that the growth of the 340B program has resulted in a shift in the site of service for chemotherapy administration from the physician-office setting to the more costly hospital outpatient setting, since hospitals are able to acquire drugs, including oncologic drugs, at a significant discount under the 340B program. Another commenter believed that the 340B program is no longer serving its intended purpose to help America's most vulnerable patients access the drugs they need. They further asserted that instead, 340B profits are being used for hospitals to make larger profits.
Response: We appreciate the commenters' support. We note that comments related to the 340B program itself are outside the scope of this rule, however, we note that we adopted the 340B payment policy so that our payment policy would be more in line with the acquisition costs hospitals incur, and thereby lower drug expenditures for Medicare beneficiaries and the Medicare Trust Fund.
Comment: Many commenters, the majority of which represented hospitals or hospital associations, opposed CMS' proposal to continue to pay ASP minus 22.5 percent for 340B-acquired drugs in CY 2020. Many of these commenters believe the proposal undermines the intent and goals of the 340B program and will have negative impacts on patients and 340B hospitals. One commenter asserted that CMS should pay hospitals participating in the 340B program the statutory default payment of ASP+6 percent. Another commenter opposed the proposal on the belief that it undermines the Public Health Service Act (PHSA), which authorized the 340B program and exceeds CMS' statutory authority. Furthermore, a hospital organization commented that the application of the reduced payment for the 340B policy has resulted in negative consequences for patients and providers and does not save any money for Medicare because the policy is implemented in a budget-neutral manner.
Several commenters who opposed the continuation of the 340B program payment policy stated that the district court's ruling showed that the payment reduction is illegal and exceeded the Administration's authority. These commenters recommended CMS refrain from “doing more damage” to impacted hospitals by continuing the ASP minus 22.5 percent policy and return to the payment rate of ASP+6 percent for CY 2020.
Response: As noted in the CY 2018 OPPS/ASC final rule with comment period, we continue to believe that ASP minus 22.5 percent for drugs acquired through the 340B Program represents the average minimum discount that 340B enrolled hospitals receive and better represents acquisition costs.
We disagree with commenters that the 340B payment policy has had a negative impact on Medicare patients; we are not aware of any access issues related to the implementation of this policy. Further, we note that under the current policy, Medicare patients who receive 340B drugs for which the Medicare program paid ASP minus 22.5 percent have much lower cost sharing than if these beneficiaries received 340B drugs for which the Medicare program paid ASP+6 percent. As a result, we continue to believe that ASP minus 22.5 percent is a reasonable payment rate for these drugs.
In regards to the commenters' belief that CMS lacks the legal authority to continue paying a reduced amount for drugs and biologicals obtained through the 340B Program and that we should pay the statutory default amount of ASP+6 percent, we refer commenters to our detailed response regarding our statutory authority to require payment reductions for drugs and biologicals obtained through the 340B Program in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59359 through 59364), as well as our statements in the proposed rule regarding our appeal of the district court's decision.
After considering these public comments and the comments summarized below, and in light of the fact that we are awaiting a decision on our appeal in the litigation, for CY 2020, we are finalizing our proposal, without modification, to pay ASP minus 22.5 percent for 340B-acquired drugs including when furnished in nonexcepted off-campus PBDs paid under the PFS. Our finalized proposal continues the 340B policies that were implemented in CY 2018 with the exception of the way we are calculating payment for 340B-acquired biosimilars, which is discussed in section V.B.2.c. of the CY 2019 OPPS/ASC final rule with comment period, and would continue the policy we finalized in CY 2019 to pay ASP minus 22.5 percent for 340B-acquired drugs and biologicals furnished in nonexcepted off-campus PBDs paid under the PFS.
As noted in the proposed rule (84 FR 39504), we are appealing the district court's decision and are awaiting a decision from the Court of Appeals for the District of Columbia Circuit. Because we hope to prevail on appeal and have our 340B policy upheld, we believe it is appropriate to finalize our proposal of ASP minus 22.5 percent rather than an alternative payment amount of either ASP+3 percent or ASP+6 percent, and to maintain the other payment policies we adopted for 340B-acquired drugs in the CY 2018 and 2019 OPPS final rules with comment period. In the event of an adverse decision on appeal, we solicited public comments on the appropriate remedy for use in the CY 2021 rulemaking. Those comments are summarized below. We note that in the event 340B hospital survey data are not used to devise a remedy, we intend to consider the following comments to develop an appropriate remedy to propose in next year's rulemaking.
Comments on the CY 2020 Payment Policy for 340B-Aquired Drugs to Non-Excepted Off-Campus Provider Based Departments (PBDs)
Comment: Many commenters disagreed with CMS' assertion that 340B hospitals will move drug administration services for 340B-acquired drugs to non-excepted off-campus PBDs if CMS does not continue to pay for drugs furnished in these settings at the adjusted amount, and recommended CMS study hospital's drug administration behavior pre- and post-implementation of the CY 2018 final rule to confirm this presumption before finalizing the proposal to continue paying ASP minus 22.5 percent for 340B drugs furnished by non-excepted PBDs. Several commenters asserted that CMS should not continue with this policy for CY 2020 for non-excepted PBDs and stated that continuing to do so would be unlawful.
Response: We appreciate the commenters' input on the proposal to continue to pay at ASP minus 22.5 percent under the PFS for 340B drugs furnished in non-excepted off-campus PBDs. As we stated in the CY 2019 OPPS/ASC final rule with comment (83 FR 59017), because hospitals can, in some cases, acquire drugs and biologicals under the 340B Program for use in nonexcepted off-campus PBDs, we believe that not adjusting payment exclusively for these departments would present a significant incongruity between the payment amounts for these drugs depending on where they are furnished. This incongruity would distort the relative accuracy of the resource-based payment amounts under the site-specific PFS rates and could result in significant perverse incentives for hospitals to acquire drugs and biologicals under the 340B Program and avoid Medicare payment adjustments that account for the discount by providing these drugs to patients predominantly in nonexcepted off-campus PBDs. In light of the significant payment differences between excepted and nonexcepted off-campus PBDs, in combination with the potential eligibility for discounts, which result in reduced costs under the 340B Program for both kinds of departments, a different payment policy for 340B drugs in the two settings could undermine the use of the OPPS payment structure in nonexcepted off-campus PBDs. In order to avoid such perverse incentives and the potential resulting distortions in drug payment, pursuant to our authority at section 1833(t)(21)(c) of the Act we adopted a policy to identify the PFS as the “applicable payment system for 340B-acquired drugs and biologicals and, accordingly, to pay under the PFS instead of under section 1847A/1842(o) of the Act an amount equal to ASP minus 22.5 percent for drugs and biologicals acquired under the 340B Program that are furnished by nonexcepted off-campus PBDs. We continue to believe this payment policy is necessary to avoid the significant incongruity between the payment amounts that would exist for these drugs depending upon whether they are furnished by excepted off-campus PBDs or nonexcepted off-campus PBDs. We believe we have discretion under section 1833(t)(21)(c) of the Act to continue to adjust payments for nonexcepted off-campus PBDs.
Comments on Use of ASP Plus 3 Percent for CY 2020
Comment: Many commenters opposed a payment amount of ASP+3 percent as a potential remedial payment for 340B-acquired drugs furnished in CY 2018 and CY 2019 as well as for CY 2020 payments. These commenters believe CMS did not provide a rationale to support the proposed ASP+3 percent adjustment and stated that CMS does not have statutory authority to pay one group of hospitals at ASP+3 percent and all other hospitals at ASP+6 percent. Some commenters stated that section 1833(t)(14)(A)(iii)(II) requires CMS to pay hospitals for covered outpatient drugs at ASP+6 percent and that CMS does not have the legal authority to change that payment amount to ASP+3 percent. Furthermore, some commenters stated that although CMS has some authority to make adjustments, the agency's stated rationale of imposing a payment reduction at the upper end of the court's “limit [on] the size of the payment reduction the agency can permissibly apply . . . given the substantial discounts that hospitals receive under the 340B program” would be inconsistent with the law itself and therefore, reducing payment for 340B-acquired drugs to ASP+3 percent would be unlawful.
However, a few commenters supported the proposal to pay ASP+3 percent for 340B-acquired drugs in CY 2020, rather than to continue to pay ASP minus 22.5 percent. One commenter supported the approach of paying ASP+3 percent for 340B-acquired drugs if CMS receives an adverse decision on appeal.
Response: We appreciate commenters' support of CMS' suggestion to pay at ASP+3 percent if we are unsuccessful in the Appeals Court. As explained above, we are finalizing our proposal to continue to pay for 340B-acquired drugs at ASP minus 22.5 percent. In the event of an adverse decision on appeal, we will take these comments into consideration in crafting an appropriate remedy.
Comment: One commenter believed a rate closer to ASP+6 percent, such as ASP+3 percent, would mitigate remediation efforts should the Agency not ultimately prevail on appeal and have to return the difference in payments between ASP minus 22.5 percent and ASP+6 percent based on a negative court decision.
Response: We thank the commenter for its feedback. As explained above, we are finalizing our proposal to continue to pay for 340B-acquired drugs at ASP minus 22.5 percent. In the event of an adverse decision on appeal, we will take these comments into consideration in crafting an appropriate remedy.
Comments on Use of Hospital Acquisition Costs
Comment: Several commenters, including a large medical association, suggested that CMS gather hospitals' acquisition costs for drugs. One commenter stated that “since CMS has the authority to base reimbursement rates on the hospitals' acquisition cost (340B price) if the Agency considers hospital acquisition cost survey data, we urge CMS to collect such data.” Another commenter urged CMS to gather additional data to better understand 340B acquisition costs and the impact of payment reductions on 340B providers prior to making payment changes that the commenter believes jeopardizes access and 340B program participation.
Response: We appreciate the commenters' suggestion and note that we announced in the Federal Register (84 FR 51590) our intent to conduct a 340B hospital survey to collect drug acquisition cost data for CY 2018 and 2019. We have no evidence that the current 340B policy has limited patient access to 340B drugs or program participation. For the reasons explained above, we believe it is appropriate to continue our 340B payment policies for CY 2020.
Thus, for CY 2020, we are finalizing our proposal, without modification, to pay ASP minus 22.5 percent for 340B-acquired drugs including when furnished in nonexcepted off-campus PBDs paid under the PFS. Our finalized proposal continues the 340B Program policies that were implemented in CY 2018 with the exception of the way we are calculating payment for 340B-acquired biosimilars, which is discussed in section V.B.2.c. of the CY 2019 OPPS/ASC final rule with comment period, and continues the policy we finalized in CY 2019 to pay ASP minus 22.5 percent for 340B-acquired drugs and biologicals furnished in nonexcepted off-campus PBDs paid under the PFS.
Comments on a Potential Remedy for CYs 2018 and 2019
In addition to comments on the appropriate payment amount for calculating the remedy for CYs 2018 and 2019 and for use for CY 2020, we sought public comment on how to structure the remedy for CYs 2018 and 2019. This request for public comment included whether such a remedy should be retrospective in nature (for example, made on a claim-by-claim basis), whether such a remedy could be prospective in nature (for example, an upward adjustment to 340B claims in the future to account for any underpayments in the past), and whether there is some other mechanism that could produce a result equitable to hospitals that do not acquire drugs through the 340B program while respecting the budget neutrality mandate.
We stated in the CY 2020 OPPS/ASC proposed rule that one potential remedy for alleged underpayments in 2018 and 2019 would involve making additional payments to the parties who have demonstrated harm from the alleged underpayments (which could be defined as hospitals that submitted a claim for drug payment with the “JG” modifier in CYs 2018 and 2019) outside the normal claims process. Under this approach, we would calculate the amount that such hospitals should have been paid and would utilize our Medicare contractors to make one payment to each affected hospital. This approach—one additional payment made to each affected hospital by our contractors—is a different approach than reprocessing each and every claim submitted by plaintiff hospitals for 2018 and 2019. Then, depending on when a final decision is rendered, the Secretary would propose to budget-neutralize those additional expenditures for each of CYs 2018 and 2019. For example, if the Court of Appeals were to render a decision in February of 2020, we might propose those additional payments and an appropriate budget neutrality adjustment for each of CYs 2018, 2019, and, if necessary, 2020, in time for the CY 2021 rule. We noted that we would need to receive a final decision from the Court of Appeals sufficiently early in CY 2020 (likely no later than March 1, 2020) to make it potentially possible for us to propose and finalize an appropriate remedy and budget neutrality adjustments in the CY 2021 rulemaking. We solicited public comment on this approach as well as other suggested approaches from commenters.
In considering these potential future proposals, we noted that we would rely on our statutory authority under section 1833(t)(14) for determining the OPPS payment rates for drugs and biologicals as well as section 1833(t)(9)(A) of the Act to review certain components of the OPPS not less often than annually and to revise the groups, relative payment weights, and other adjustments. In addition, we noted that under section 1833(t)(14)(H) of the Act, any adjustments made by the Secretary to payment rates using the statutory formula outlined in section 1833(t)(14)(A)(iii)(II) of the Act are required to be taken into account under the budget neutrality requirements outlined in section 1833(t)(9)(B) of the Act. In the CY 2020 OPPS/ASC proposed rule (84 FR 39505), we solicited public comments on the best, most appropriate way to maintain budget neutrality, either under a retrospective claim-by-claim approach, with a prospective approach, or any other proposed remedy. We also solicited comments on whether, depending on the amount of those additional expenditures, we should consider spreading out the relevant budget neutrality adjustment across multiple years. We appreciated all the public comments that we received on the advantages and disadvantages of such an approach.
We also sought public comments on the best, most appropriate treatment of Medicare beneficiary cost-sharing responsibilities under any proposed remedy. We stated that the statutory budget neutrality requirement and beneficiary cost-sharing are extremely difficult to balance, and we sought stakeholder comments as we continue to review the viability of alternative remedies in the event of an adverse decision from the Court of Appeals.
We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59369 through 59370) and the CY 2019 OPPS/ASC final rule with comment period (83 FR 58976 through 58977 and 59015 through 59022) for more detail on the policies implemented in CY 2018 and CY 2019 for drugs acquired through the 340B Program.
We also note that since the CY 2020 OPPS/ASC proposed rule was published, we announced in the Federal Register (84 FR 51590) our intent to conduct a 340B hospital survey to collect drug acquisition cost data for CY 2018 and 2019. As noted above, we may use this survey data to devise a remedy for prior years if the district court's ruling is upheld on appeal. A remedy that relies on such survey data could avoid the remedial complexities discussed below and in the proposed rule. If, however, 340B hospital survey data are not used to devise a remedy, we intend to consider the comments summarized below to inform a remedy we would propose in the CY 2021 OPPS/ASC proposed rule in the event of an adverse decision upon appeal.
Comments on Potential Remedy Structure
Comment: On the issue of a remedy structure, many commenters supported a retrospective remedy on a claim-by-claim basis over a prospective adjustment of prior 340B claims. Several commenters believe it is CMS' responsibility to remedy the policy by requiring as little effort as possible on the part of affected hospitals, thus avoiding any additional injuries to the parties. Many commenters believe that CMS should repay the difference between ASP+6 percent and ASP minus 22.5 percent plus interest for all claims for 340B-acquired drugs for CYs 2018 and 2019. They asserted that CMS can calculate the amount owed to the affected 340B hospitals by using the JG modifier that identifies the claims for 340B drugs. One commenter suggested identifying the total amount paid to a hospital for drugs with the status indicator “K” and multiplying by 1.3677 (that is ASP+6 percent/ASP minus 22.5 percent = 1.06/0.775). Another commenter stated that the percentage of claims that each hospital was underpaid is the same in each case and that we can calculate the total payment for each hospital and multiply that number by a factor, in order to determine how much each hospital should have been paid. Some commenters supported a lump-sum payment. One commenter supported either a lump-sum payment or a prospective payment segmented out over multiple years. One commenter compared this case to those remedies that the courts and agency have adopted to handle past cases. This commenter believed the affected parties should receive a supplemental payment for those affected claims in an amount equal to the difference between ASP minus 22.5 percent and ASP+6 percent. Another commenter believed that the remedy should be decided by a federal judge.
Additionally, some commenters supported a prospective remedy, pointing out that a retrospective process would be too complex and administratively burdensome. Several commenters supported an aggregate payment for each affected 340B entity outside the normal claims process rather than a retrospective adjustment. One commenter suggested applying an increase factor of 26.89 percent that would pay the affected entities at an amount that would approximate ASP+6 percent. Another commenter supported an upward adjustment to future claims, which they believed would reduce administrative burden.
Another commenter believed that CMS should publish a proposed methodology for conducting the look-back and issuing the payment. Further, they believed that providers should have opportunity for public comment, and that CMS should revise and issue a final methodology in CY 2020 outside of the normal OPPS rulemaking cycle, with the applicable data set and calculation instructions posted on the CMS web page. Other commenters believed the remedy does not necessitate rulemaking.
One commenter offered three remedy suggestions. Two suggestions involved staggered methods of payment. Under the first suggested remedy, this commenter believed that CMS could pay for 340B drugs at the following amounts over three years, which the commenter believed would make affected providers whole: Beginning January 1, 2021, CMS would pay ASP+14.25 percent plus an additional 2 percent; beginning January 1, 2022 would pay ASP+14.25 percent plus an additional 1 percent; and finally, beginning January 1, 2023, CMS would pay ASP+6 percent going forward.
The same commenter suggested a second approach under which CMS would pay affected hospitals set amounts plus interest as follows:
The first payment would be for claims submitted between January 1, 2018 and June 30, 2018 and would be paid out by July 1, 2020. The second payment would be for claims submitted between July 1, 2018 and December 31, 2018 and would be paid out January 1, 2021. The third payment would be for claims submitted between January 1, 2019 and June 30, 2019 and would be paid out July 1, 2021. The final payment would be for claims submitted between July 1, 2019 and December, 31, 2019 and would be paid out January 1, 2022.
Alternatively, the same commenter suggested a third method of making remedy payments under which CMS could recalculate the payments for all claims paid for CYs 2018 and 2019 and pay affected 340B hospitals the difference (between ASP+6 and ASP minus 22.5 percent) in one lump-sum payment plus interest by January 1, 2021. The commenter suggested that CMS would provide affected 340B hospitals notice on or before July 1, 2021 of the calculated payment amount owed to the hospital. The commenter suggested that the repayment amounts should be placed in a 340B-specified account to be redistributed to eligible hospitals and distributed in equal payments over a two-year period beginning January 2021 for covered entities that demonstrate “responsible program integrity” as determined in collaboration with HRSA. The commenters suggested that funds not able to be distributed will be used to provide funding to CMS and HRSA to collaborate with industry stakeholders to identify and implement solutions for duplicate discount prevention.
Comments on Budget Neutrality
On the issue of budget neutrality, many commenters asserted that budget neutrality is not necessary given prior court precedents involving underpayments: Cape Cod Hospital v. Sebelius (DC Cir. 2011), H. Lee Moffitt Cancer Center & Research Institute, Inc. vs. Azar, (D.D.C. 2018), Shands Jacksonville Medical Center v. Burwell, (D.D.C. 2015). Other commenters asserted that neither (t)(9)(B) nor any other provision of the OPPS statue authorizes the agency to revisit budget neutrality if its estimates of money owed for a prior year turn out to be incorrect. They view the statute as directing CMS to make estimates for the purposes of setting prospective payment rates only, and not authorizing the agency to recalibrate those estimates after the fact if its predictions turn out to be incorrect. These commenters believe that the Congress drafted the OPPS statute to prohibit the agency from revisiting its budget-neutrality determinations after it first makes them on a prospective basis for a given year. They further asserted that CMS should exercise discretion in using its budget neutrality authority in seeking payments back from providers.
Some commenters supported a prospective payment rate reduction on OPPS non-drug items and services to maintain budget neutrality from any remedy. Other commenters supported a gradual rate reduction of the payment amounts for OPPS non-drug items and services ranging from a minimum of two to six years to lessen the impact of rate reduction to the affected entities. Several commenters supported a modest reduction in future OPPS payment by reducing the conversion factor.
Comments on Beneficiary Coinsurance
Additionally, many commenters asserted that there is no law that requires hospitals to adjust beneficiaries' coinsurance for 340B-acquired drugs. They stated that neither the False Claims nor the anti-kickback statutes would apply because beneficiaries did not receive any inducements to seek services. These commenters believe that beneficiaries already fully paid for the hospital care months or years ago and should not have to pay any additional payments. They requested that CMS clearly state in this final rule that there is no requirement for any beneficiary copay adjustments. One commenter offered estimates on what they believe are the percentage of patients who are impacted by any adjustment on the patient's copay citing 29 percent with Medigap, 22 percent enrolled in Medicaid (dually eligible), and 19 percent without a supplemental plan, with the remaining 30 percent enrolled in a Medicare Advantage plan. Thus, this commenter believed that only 19 percent of patients would be impacted directly by cost-sharing implications and CMS would need to calculate payment owed to Medicare for these beneficiaries.
Response: We thank the commenters for their comments on the appropriate remedy for CYs 2018 and 2019. As noted above, we may use the survey data for 2018 and 2019 that we plan to collect from 340B hospitals to devise a remedy for prior years if the district court's ruling is upheld on appeal. A remedy that relies on such survey data could avoid the remedial complexities discussed above and in the proposed rule. If, however, 340B hospital survey data are not used to devise a remedy in the event of an adverse decision from the Court of Appeals, we intend to consider all of these suggestions in determining the appropriate remedy to propose in the CY 2021 OPPS rulemaking. To the extent commenters made legal arguments relating to the False Claims Act or anti-kickback statutes, CMS offers no opinion.
7. High Cost/Low Cost Threshold for Packaged Skin Substitutes
In the CY 2014 OPPS/ASC final rule with comment period (78 FR 74938), we unconditionally packaged skin substitute products into their associated surgical procedures as part of a broader policy to package all drugs and biologicals that function as supplies when used in a surgical procedure. As part of the policy to finalize the packaging of skin substitutes, we also finalized a methodology that divides the skin substitutes into a high cost group and a low cost group, in order to ensure adequate resource homogeneity among APC assignments for the skin substitute application procedures (78 FR 74933).
Skin substitutes assigned to the high cost group are described by HCPCS codes 15271 through 15278. Skin substitutes assigned to the low cost group are described by HCPCS codes C5271 through C5278. Geometric mean costs for the various procedures are calculated using only claims for the skin substitutes that are assigned to each group. Specifically, claims billed with HCPCS code 15271, 15273, 15275, or 15277 are used to calculate the geometric mean costs for procedures assigned to the high cost group, and claims billed with HCPCS code C5271, C5273, C5275, or C5277 are used to calculate the geometric mean costs for procedures assigned to the low cost group (78 FR 74935).
Each of the HCPCS codes described above are assigned to one of the following three skin procedure APCs according to the geometric mean cost for the code: APC 5053 (Level 3 Skin Procedures): HCPCS codes C5271, C5275, and C5277); APC 5054 (Level 4 Skin Procedures): HCPCS codes C5273, 15271, 15275, and 15277); or APC 5055 (Level 5 Skin Procedures): HCPCS code 15273). In CY 2019, the payment rate for APC 5053 (Level 3 Skin Procedures) was $482.89, the payment rate for APC 5054 (Level 4 Skin Procedures) was $1,548.96, and the payment rate for APC 5055 (Level 5 Skin Procedures) was $2,766.13. This information also is available in Addenda A and B of the CY 2019 OPPS/ASC final rule with comment period (which is available via the internet on the CMS website).
We have continued the high cost/low cost categories policy since CY 2014, and we proposed to continue it for CY 2020. Under this current policy, skin substitutes in the high cost category are reported with the skin substitute application CPT codes, and skin substitutes in the low cost category are reported with the analogous skin substitute HCPCS C-codes. For a discussion of the CY 2014 and CY 2015 methodologies for assigning skin substitutes to either the high cost group or the low cost group, we refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 74932 through 74935) and the CY 2015 OPPS/ASC final rule with comment period (79 FR 66882 through 66885).
For a discussion of the high cost/low cost methodology that was adopted in CY 2016 and has been in effect since then, we refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70434 through 70435). For CY 2020, consistent with our policy since CY 2016, we proposed to continue to determine the high cost/low cost status for each skin substitute product based on either a product's geometric mean unit cost (MUC) exceeding the geometric MUC threshold or the product's per day cost (PDC) (the total units of a skin substitute multiplied by the mean unit cost and divided by the total number of days) exceeding the PDC threshold. For CY 2020, as we did for CY 2019, we proposed to assign each skin substitute that exceeds either the MUC threshold or the PDC threshold to the high cost group. In addition, as described in more detail later in this section, for CY 2020, as we did for CY 2019, we proposed to assign any skin substitute with a MUC or a PDC that does not exceed either the MUC threshold or the PDC threshold to the low cost group. For CY 2020, we proposed that any skin substitute product that was assigned to the high cost group in CY 2019 would be assigned to the high cost group for CY 2020, regardless of whether it exceeds or falls below the CY 2020 MUC or PDC threshold. This policy was established in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59346 through 59348).
For this CY 2020 OPPS/ASC final rule, consistent with the methodology as established in the CY 2014 through CY 2018 final rules with comment period, we analyzed CY 2018 claims data to calculate the MUC threshold (a weighted average of all skin substitutes' MUCs) and the PDC threshold (a weighted average of all skin substitutes' PDCs). The final CY 2020 MUC threshold is $48 per cm 2 (rounded to the nearest $1) (proposed at $49 per cm 2) and the final CY 2020 PDC threshold is $790 (rounded to the nearest $1) (proposed at $789).
For CY 2020, we proposed to continue to assign skin substitutes with pass-through payment status to the high cost category. We proposed to assign skin substitutes with pricing information but without claims data to calculate a geometric MUC or PDC to either the high cost or low cost category based on the product's ASP+6 percent payment rate as compared to the MUC threshold. If ASP is not available, we proposed to use WAC+3 percent to assign a product to either the high cost or low cost category. Finally, if neither ASP nor WAC is available, we would use 95 percent of AWP to assign a skin substitute to either the high cost or low cost category. We proposed to continue to use WAC+3 percent instead of WAC+6 percent to conform to our proposed policy described in section V.B.2.b. of the proposed rule to establish a payment rate of WAC+3 percent for separately payable drugs and biologicals that do not have ASP data available. New skin substitutes without pricing information would be assigned to the low cost category until pricing information is available to compare to the CY 2020 MUC threshold. For a discussion of our existing policy under which we assign skin substitutes without pricing information to the low cost category until pricing information is available, we refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70436).
Some skin substitute manufacturers have raised concerns about significant fluctuation in both the MUC threshold and the PDC threshold from year to year. The fluctuation in the thresholds may result in the reassignment of several skin substitutes from the high cost group to the low cost group which, under current payment rates, can be a difference of approximately $1,000 in the payment amount for the same procedure. In addition, these stakeholders were concerned that the inclusion of cost data from skin substitutes with pass-through payment status in the MUC and PDC calculations would artificially inflate the thresholds. Skin substitute stakeholders requested that CMS consider alternatives to the current methodology used to calculate the MUC and PDC thresholds and also requested that CMS consider whether it might be appropriate to establish a new cost group in between the low cost group and the high cost group to allow for assignment of moderately priced skin substitutes to a newly created middle group.
We share the goal of promoting payment stability for skin substitute products and their related procedures as price stability allows hospitals using such products to more easily anticipate future payments associated with these products. We have attempted to limit year-to-year shifts for skin substitute products between the high cost and low cost groups through multiple initiatives implemented since CY 2014, including: Establishing separate skin substitute application procedure codes for low-cost skin substitutes (78 FR 74935); using a skin substitute's MUC calculated from outpatient hospital claims data instead of an average of ASP+6 percent as the primary methodology to assign products to the high cost or low cost group (79 FR 66883); and establishing the PDC threshold as an alternate methodology to assign a skin substitute to the high cost group (80 FR 70434 through 70435).
To allow additional time to evaluate concerns and suggestions from stakeholders about the volatility of the MUC and PDC thresholds, in the CY 2018 OPPS/ASC proposed rule (82 FR 33627), we proposed that a skin substitute that was assigned to the high cost group for CY 2017 would be assigned to the high cost group for CY 2018, even if it does not exceed the CY 2018 MUC or PDC thresholds. We finalized this policy in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59347). We stated in the CY 2018 OPPS/ASC proposed rule that the goal of our proposal to retain the same skin substitute cost group assignments in CY 2018 as in CY 2017 was to maintain similar levels of payment for skin substitute products for CY 2018 while we study our skin substitute payment methodology to determine whether refinement to the existing policies are consistent with our policy goal of providing payment stability for skin substitutes.
We stated in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59347) that we would continue to study issues related to the payment of skin substitutes and take these comments into consideration for future rulemaking. We received many responses to our request for comments in the CY 2018 OPPS/ASC proposed rule about possible refinements to the existing payment methodology for skin substitutes that would be consistent with our policy goal of providing payment stability for these products. In addition, several stakeholders have made us aware of additional concerns and recommendations since the release of the CY 2018 OPPS/ASC final rule with comment period. As discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58967 through 58968), we identified four potential methodologies that have been raised to us that we encouraged the public to review and provide comments on. We stated in the CY 2019 OPPS/ASC final rule with comment period that we were especially interested in any specific feedback on policy concerns with any of the options presented as they relate to skin substitutes with differing per day or per episode costs and sizes and other factors that may differ among the dozens of skin substitutes currently on the market. We also specified in the CY 2019 OPPS/ASC final rule with comment period that we were interested in any new ideas that are not represented below along with an analysis of how different skin substitute products would fare under such ideas. Finally, we stated that we intend to explore the full array of public comments on these ideas for the CY 2020 rulemaking, and we indicated that we will consider the feedback received in response to our requests for comments in developing proposals for CY 2020.
a. Discussion of CY 2019 Comment Solicitation for Episode-Based Payment and Solicitation of Additional Comments for CY 2020
The methodology that commenters discussed most in response to our comment solicitation in CY 2019 and that stakeholders raised in subsequent meetings we have had with the wound care community has been a lump-sum “episode-based” payment for a wound care episode. Commenters that supported an episode-based payment believe that it would allow health care professionals to choose the best skin substitute to treat a patient's wound and would give providers flexibility with the treatments they administer. These commenters also believe an episode-based payment helps to reduce incentives for providers to use excessive applications of skin substitute products or use higher cost products to generate more payment for the services they furnish. In addition, they believe that episode-based payment could help with innovations with skin substitutes by encouraging the development of products that require fewer applications. These commenters noted that episode-based payment would make wound care payment more predictable for hospitals and provide incentives to manage the cost of care that they furnish. Finally, commenters for an episode-based payment believe that workable quality metrics can be developed to monitor the quality of care administered under the payment methodology and limit excessive applications of skin substitutes.
However, many commenters opposed establishing an episode-based payment. One of the main concerns of commenters who opposed episode-based payment was that wound care is too complex and variable to be covered through such a payment methodology. These commenters stated that every patient and every wound is different; therefore, it would be very challenging to establish a standard episode length for coverage. They noted that it would be too difficult to risk-stratify and specialty-adjust an episode-based payment, given the diversity of patients receiving wound care and their providers who administer treatment, as well as the variety of pathologies covered in treatment. Also, these commenters questioned how episodes would be defined for patients when they are having multiple wounds treated at one time or have another wound develop while the original wound was receiving treatment. These commenters expressed concerns that episode-based payment would be burdensome both operationally and administratively for providers. They believe that CMS will need to create a large number of new APCs and HCPCS codes to account for all of the patient situations that would be covered with an episode-based payment, which would increase burdens on providers. Finally, these commenters had concerns about the impacts of episode-based payment on the usage of higher cost skin substitute products. They believe that a single payment could discourage the use of higher-cost products because of the large variability in the cost of skin substitute products, which could limit innovations for skin substitute products.
The wide array of views on episode-based payment for skin substitute products and the unforeseen issues that may arise from the implementation of such a policy make us reluctant to present a proposal for this CY 2020 proposed rule without more review of the issues involved with episode-based payment. Therefore, we sought further comments from stakeholders and other interested parties regarding skin substitute payment policies that could be applied in future years to address concerns about excessive utilization and spending on skin substitute products, while avoiding administrative issues such as establishing additional HCPCS codes to describe different treatment situations. One possible policy construct that we sought comments on was whether to establish a payment period for skin substitute application services (CPT codes 15271 through 15278 and HCPCS codes C5271 through C5278) between 4 weeks and 12 weeks. Under this option, we could also assign CPT codes 15271, 15273, 15275, and 15277, and HCPCS codes C5271, C5273, C5275, and C5277 to comprehensive APCs with the option for a complexity adjustment that would allow for an increase in the standard APC payment for more resource-intensive cases. Our research has found that most wound care episodes require one to three skin substitute applications. Those cases would likely receive the standard APC payment for the comprehensive procedure. Then the complexity adjustment could be applied for the relatively small number of cases that require more intensive treatments.
Comment: Several commenters were in favor of establishing a comprehensive APC with either an option for a complexity adjustment or outlier payments to pay for higher cost skin substitute application procedures. The commenters supported the idea of having a traditional comprehensive APC payment for standard wound care cases with a complexity adjustment or outlier payment to handle complicated or costly cases. However, they also expressed concerns about how many payment levels would be available in the skin substitute procedures APC group since a complexity adjustment can only be used if there is an existing higher-paying APC to which the service receiving the complexity adjustment may be assigned. A couple of commenters wanted more opportunities for services to receive a complexity adjustment through using clusters of procedure codes that reflect the full range of wound care services a beneficiary receives instead of using code pairs to determine if a complexity adjustment should apply. A few commenters suggested that episodic payments be risk-adjusted to account for clinical conditions and co-morbidities of beneficiaries with outlier payments and that complexity adjustments be linked to beneficiaries with more co-morbidities.
Some commenters opposed the idea of a complexity adjustment for skin substitute application procedures. The commenters believe there was not enough detail in the comment solicitation to understand how a complexity adjustment would work with an episodic payment arrangement. Commenters also expressed concerns that payment rates for comprehensive APCs may not be representative of the wound care services that would be paid within those APCs. One commenter stated that payment policy is not the right way to resolve issues with the over-utilization and inappropriate use of skin substitutes because they are concerned that major changes in payment methodology, such as episodic payment, could lead to serious issues with the care beneficiaries receive.
Regarding the topic of episodic payment, commenters brought up some of the same issues they had mentioned in response to last year's comment solicitation. Supporters of episodic payments believe the policy idea would give providers more flexibility with the treatments they administer to their patients, and will help encourage innovation by encouraging the development of graft skin substitute products that require fewer applications.
Some commenters supported developing an episodic payment model first in the CMS Innovation Center before adopting episodic payment in the OPPS. One commenter wrote about the need for quality measures as a part of episodic payment to ensure providers render appropriate care during a treatment episode. However, another commenter wanted to ensure that quality measures would not prevent providers from using a medically necessary product. Commenters also discussed episode length with a couple of commenters supporting a 12-week payment episode as mentioned in the comment solicitation, and another commenter suggesting that an episode be based not only on the length of time but the number of allowed skin substitute applications during that time period. Commenters also favored establishing a separate payment episode for each wound receiving treatment.
Commenters who oppose episodic payment expressed similar concerns as they did in response to last year's comment solicitation. Many commenters believe that wound care is too complex and variable to be covered through episodic payment even with an option for a complexity adjustment. For example, one commenter noted that the care regimen for diabetic foot ulcers is very different than the care regimen for pressure wounds. A few commenters expressed concerns about the complexities associated with episodic payment, claiming that CMS will have to established several new HCPCS codes and clinical APCs to be able to have payment rates for all of the care scenarios covered by episodic payment. Commenters also believe it would take several years to implement an episode-based payment system and such system would be operationally and administratively burdensome for providers. Other commenters were concerned about financial incentives created by episodic payment that may discourage providers from rendering the best quality of care and encourage providers to use skin substitute products that may not be the most clinically appropriate for their patients. Finally, commenters had concerns about establishing the length of a payment episode, stating there was no clear evidence on what the appropriate episode length should be. These commenters believe it also would be difficult to establish separate payment episodes when a patient was being treated for multiple wounds at the same time.
Commenters also discussed which services should be included with an episodic payment. Commenters were divided over whether an episode should be limited to application of skin substitute products or encompass other related wound care treatments including hyperbaric oxygen and negative-pressure treatment. Some commenters were concerned that episodic payment may discourage the treatment of large or complicated wounds. There also was one commenter who wanted episodic payment to cover tissue repair products used in surgical procedures.
Response: We appreciate all of the feedback we received from commenters, and we will use the feedback as we consider potential refinements to how we pay for skin substitute products and procedures under the OPPS.
b. Potential Revisions to the OPPS Payment Policy for Skin Substitutes: Comment Solicitation for CY 2020
In addition to possible future rulemaking based on the responses to the comment solicitations in the preceding section, we noted that we were considering adopting for CY 2020 another payment methodology that generated significant public comments in response to the CY 2019 comment solicitation. That option would be to eliminate the high cost and low cost categories for skin substitutes and have only one payment category and set of procedure codes for the application of all graft skin substitute products. Under this option, the only available procedure codes to bill for skin substitute graft procedures would be CPT codes 15271 through 15278. HCPCS codes C5271 through C5278 would be eliminated. Providers would bill CPT codes 15271 through 15278 without having to consider either the MUC or PDC of the graft skin substitute product used in the procedure. There would be only one APC for the graft skin substitute application procedures described by CPT codes 15271 (Skin sub graft trnk/arm/leg), 15273 (Skin sub grft t/arm/lg child), 15275 (Skin sub graft face/nk/hf/g), and 15277 (Skn sub grft f/n/hf/g child). The payment rate would be the geometric mean of all graft skin substitutes procedures for a given CPT code that are covered through the OPPS. For example, under the current skin substitute payment policy, there are two procedure codes (CPT code 15271 and HCPCS code C5271) that are reported for the procedure described as “application of skin substitute graft to trunk, arms, legs, total wound surface area up to 100 sq cm; first 25 sq cm or less wound surface area”. The geometric mean cost for CPT code 15271 was $1,572.17 in the CY 2020 OPPS/ASC proposed rule and the geometric mean cost for HCPCS code C5271 was $728.28 in the proposed rule. We stated in the proposed rule that if this policy option was implemented, only CPT code 15271 would be available in the OPPS, and the geometric mean cost using data from the CY 2020 proposed rule for the procedure code would be $1,465.18.
Commenters that supported this option believe it would remove the incentives for manufacturers to develop and providers to use high cost skin substitute products and would lead to the use of lower-cost, quality products. Commenters noted that lower Medicare payments for graft skin substitute procedures would lead to lower copayments for beneficiaries. In addition, commenters believe a single payment category would reduce incentives to apply skin substitute products in excessive amounts. Commenters also believe a single payment category is clinically justified because they stated that many studies have shown that no one skin substitute product is superior to another. Finally, supporters of a single payment category believe it would simplify coding for providers and reduce administrative burden.
There were also commenters that raised concerns that a single payment category would not offer providers incentives to furnish high quality care and would reduce the use of higher-cost skin substitute products (which they seemed to imply are of higher quality than lower cost products). They argued that eliminating the high cost and low cost payment categories also does not maintain homogeneity among APC assignments for services using skin substitutes according to opponents of the single payment category. Commenters stated that instead of having categories grouped by the relative cost of products, there would be only one category to cover the payment of products with a mean unit cost ranging from less than $1 to over $750. Commenters believe a single payment category would favor inexpensive products, which could limit innovation, and could eliminate all but the most inexpensive products from the market. Finally, opponents of a single payment category believe a single payment category would discourage the treatment of wounds that are difficult and costly to treat.
The responses to the comment solicitation show the potential of a single payment category to reduce the cost of wound care services for graft skin substitute procedures for both beneficiaries and Medicare in general. In addition, a single payment category may help to lower administrative burden for providers. Conversely, we are cognizant of other commenters' concerns that a single payment category may hinder innovation of new graft skin substitute products and cause some products that are currently well-utilized to leave the market. Nonetheless, we are persuaded that a single payment category could potentially provide a more equitable payment for many products used with graft skin substitute procedures, while recognizing that procedures performed with expensive skin substitute products would likely receive substantially lower payment.
We believe a more equitable payment rate for graft skin substitute procedures could substantially reduce the amount Medicare pays for these procedures. We welcomed suggestions or other information regarding the possibility of utilizing a single payment category to pay for skin substitute products under the OPPS, and, depending on the information we received in response to this request, we noted we may consider modifying our skin substitute payment policy in the CY 2020 OPPS/ASC final rule with comment period.
We believe some of the concerns commenters who oppose a single payment category for skin substitute products raised might be mitigated if stakeholders have a period of time to adjust to the changes inherent in establishing a single payment category. Accordingly, we solicited public comments that provide additional information about how commenters believe we should transition from the current low cost/high cost payment methodology to a single payment category.
Such suggestions to facilitate the payment transition from a low cost/high cost payment methodology to a single payment category methodology could include, but are not limited to—
- Delaying implementation of a single category payment for 1 or 2 years after the payment methodology is adopted; and
- Gradually lowering the MUC and PDC thresholds over 2 or more years to add more graft skin substitute procedures into the current high cost group until all graft skin substitute procedures are assigned to the high cost group and it becomes a single payment category.
We sought commenters' feedback on these ideas, or other approaches, to mitigate challenges that could impact providers, manufacturers, and other stakeholders if we establish a single payment category, which we indicated we might include as part of a final skin substitute payment policy that we would adopt in the CY 2020 OPPS/ASC final rule with comment period.
Comment: A few commenters expressed support for a single payment category for the application of skin substitute products. These commenters supported the payment methodology because they believe it would remove incentives for manufacturers to develop and providers to use high-cost products. These commenters maintained that a single payment category would encourage product innovations that maintain the quality of care for beneficiaries while bringing down the cost of skin substitute products, which will help to reduce the co-payments beneficiaries pay for skin substitute application services. Commenters supported more payment homogeneity because they believe most skin substitute products perform in a similar manner and no product or group of products is clinically superior over other skin substitute products. One commenter noted that the device pass-through payment pathway continues to be available for manufacturers to receive additional payment if a superior skin substitute product is developed.
Several commenters in favor of a single payment category believe it would simplify coding for providers and reduce administrative burden. They also believe a single payment category provides adequate payment for providers based on the case mix of smaller, easier to treat wounds and larger, more complex wounds. Also, a single payment category would promote cost stability by eliminating the large payment fluctuation for skin substitutes who are close to the cost-group thresholds in the current high-cost/low-cost payment methodology for skin substitutes.
The vast majority of commenters were opposed to a single payment category for skin substitute products. Commenters stated that the large difference in resource costs between higher cost and lower cost skin substitute products would mean only the most inexpensive products would be used to provide care, which would hurt both product innovation and the quality of care beneficiaries receive. Commenters were concerned that a single payment category would encourage providers to choose financial benefit over clinical efficacy when determining which skin substitute products to use.
These commenters also stated that a single payment category would increase incentives for providers to use cheaper products that require more applications to generate more revenue. A couple of commenters believe that overall Medicare spending on skin substitutes would be higher with a single payment category than under the current payment methodology which has separate payment for higher cost and lower cost skin substitutes. The reason spending would go up according to the commenters is the overpayment for low cost skin substitutes by Medicare would exceed the savings Medicare would receive on reduced payments for higher cost skin substitutes.
Further, commenters stated that a single payment rate would lead to too much heterogeneity in the products receiving payment through the skin substitute application procedures. The same payment rate would apply to skin substitute products whether they cost less than $10 per cm2 or over $200 per cm2 and regardless of the type of wound they treat. Commenters would prefer to have multiple payment categories where the payment rate is more reflective of the cost of the product. Commenters believe that a single payment category would discourage providers from treating more complicated wounds.
Some commenters stated that CMS should not implement a single payment category methodology in CY 2020 because it only sought comments and did not propose it and that CMS should formally propose the methodology to allow commenters a meaningful opportunity to comment on the precise proposal before implementing it.
There also were comments about the idea of having a transition period of 1 to 2 years before the full implementation of a single category payment methodology. Those commenters in favor of a single payment category did not see a need for a transition period or wanted only a one-year transition period. Conversely, those commenters opposed to a single payment category either who did mention the idea of a transition period wanted it to last multiple years with one commenter suggesting a transition period of four years.
Response: We appreciate the comments we received for this comment solicitation, and we will use the feedback to help inform our development of our payment methodology for skin substitute application procedures in future rulemaking.
c. Proposals for Packaged Skin Substitutes for CY 2020
To allow stakeholders time to analyze and comment on the issues discussed above, we proposed for CY 2020 to continue our policy established in CY 2018 to assign skin substitutes to the low cost or high cost group. Specifically, we proposed to assign a skin substitute with a MUC or a PDC that does not exceed either the MUC threshold or the PDC threshold to the low cost group, unless the product was assigned to the high cost group in CY 2019, in which case we would assign the product to the high cost group for CY 2020, regardless of whether it exceeds the CY 2020 MUC or PDC threshold. We also proposed to assign to the high cost group any skin substitute product that exceeds the CY 2020 MUC or PDC thresholds and assign to the low cost group any skin substitute product that does not exceed the CY 2020 MUC or PDC thresholds and was not assigned to the high cost group in CY 2019. We proposed to continue to use payment methodologies including ASP+6 percent and 95 percent of AWP for skin substitute products that have pricing information but do not have claims data to determine if their costs exceed the CY 2020 MUC. In addition, we proposed to use WAC+3 percent for skin substitute products that do not have ASP pricing information or have claims data to determine if those products' costs exceed the CY 2020 MUC. We proposed to continue our established policy to assign new skin substitute products without pricing information to the low cost group.
Table 19 of the proposed rule displayed the proposed CY 2020 cost category assignment for each skin substitute product.
Comment: Most commenters supported our proposal to continue our policy to assign skin substitutes to the low cost or high cost group, mainly because they still want more information on both episode-based payment for skin substitutes and the possibility of creating a single payment category for skin substitutes. These commenters do not currently support either potential payment methodology and prefer to keep the current high-cost and low-cost payment methodology until an alternative methodology for skin substitutes is better developed.
Response: We appreciate the support of the commenters of our CY 2020 proposal for the payment of skin substitute application services.
Comment: One commenter was opposed to our proposal. This commenter requested that we no longer assign to the high-cost group skin substitute products that do not meet either the MUC or PDC thresholds in CY 2020 because the skin substitute product had previous been assigned to the high-cost group in CY 2019. The commenter believes skin substitute products should be assigned to the cost group that for which they qualify based on current MUC and PDC thresholds because the commenter believes that Medicare payment should reflect to some extent the relative cost of a skin substitute product compared to all other skin substitute products.
Response: We disagree with commenter. Requiring products to potentially switch annually between the high-cost and low-cost group leads to payment instability for skin substitute products (82 FR 59346-59347). The payment rate for a skin substitute application procedure may change by several hundred dollars depending on if a skin substitute product is assigned to the high-cost or low-cost group, which can make it challenging for manufacturers to estimate the payment their products will generate when used by providers. The policy to continue to assign skin substitute products to the high-cost group once they qualify for the group promotes payment stability and allows manufacturers and providers to know over a long period of time the payment rate of the procedures used with each skin substitute product.
Comment: For the CY 2019 OPPS/ASC final rule with comment period, a commenter, the manufacturer, requested that HCPCS code Q4184 (Cellesta, per square centimeter) be assigned to the high-cost skin substitute group because the ASP+6 percent price of HCPCS code Q4184 for Quarter 1 of 2019 was $110.02 per cm2 which was substantially higher than the MUC threshold for CY 2019 of $49 per cm2.
Response: HCPCS code Q4184 (Cellesta, per square centimeter) has been assigned to the high-cost group since April 1, 2019 and we proposed assigning the skin substitute product again to the high-cost group in CY 2020.
Comment: One commenter, the manufacturer, has requested that HCPCS codes Q4122 (Dermacell, per square centimeter) and Q4150 (Allowrap ds or dry, per square centimeter) continue to be assigned to the high-cost skin substitute group.
Response: HCPCS codes Q4122 (Dermacell, per square centimeter) and Q4150 (Allowrap ds or dry, per square centimeter) were both assigned to the high-cost group in CY 2019 and also were proposed to the high-cost group for CY 2020. Per our proposal, a skin substitute that has been proposed in the high-cost group in a proposed rule will remain in the high-cost group in the final rule. Also, any skin substitute assigned to the high-cost group in CY 2019 will continue to be assigned to the high-cost group in CY 2020 even if MUC and PDC for the skin substitute product is below the overall MUC and PDC thresholds for all skin substitute products. Accordingly, we are finalizing our proposal to assign HCPCS codes Q4122 and Q4150 to the high-cost group in CY 2020.
After consideration of the public comments we received, we are finalizing our proposal to assign a skin substitute with a MUC or a PDC that does not exceed either the MUC threshold or the PDC threshold to the low cost group, unless the product was assigned to the high cost group in CY 2019, in which case we would assign the product to the high cost group for CY 2020, regardless of whether it exceeds the CY 2020 MUC or PDC threshold. We also are finalizing our proposal to assign to the high cost group any skin substitute product that exceeds the CY 2020 MUC or PDC thresholds and assign to the low cost group any skin substitute product that does not exceed the CY 2020 MUC or PDC thresholds and was not assigned to the high cost group in CY 2019. We are finalizing our proposal to continue to use payment methodologies including ASP+6 percent and 95 percent of AWP for skin substitute products that have pricing information but do not have claims data to determine if their costs exceed the CY 2020 MUC. In addition, we are finalizing our proposal to continue to use WAC+3 percent instead of WAC+6 percent for skin substitute products that do not have ASP pricing information or claims data to determine if those products' costs exceed the CY 2020 MUC. We also are finalizing our proposal to retain our established policy to assign new skin substitute products with pricing information to the low cost group. Table 45 below displays the final CY 2020 cost category assignment for each skin substitute product.



VI. Estimate of OPPS Transitional Pass-Through Spending for Drugs, Biologicals, Radiopharmaceuticals, and Devices
A. Background
Section 1833(t)(6)(E) of the Act limits the total projected amount of transitional pass-through payments for drugs, biologicals, radiopharmaceuticals, and categories of devices for a given year to an “applicable percentage,” currently not to exceed 2.0 percent of total program payments estimated to be made for all covered services under the OPPS furnished for that year. If we estimate before the beginning of the calendar year that the total amount of pass-through payments in that year would exceed the applicable percentage, section 1833(t)(6)(E)(iii) of the Act requires a uniform prospective reduction in the amount of each of the transitional pass-through payments made in that year to ensure that the limit is not exceeded. We estimate the pass-through spending to determine whether payments exceed the applicable percentage and the appropriate prorata reduction to the conversion factor for the projected level of pass-through spending in the following year to ensure that total estimated pass-through spending for the prospective payment year is budget neutral, as required by section 1833(t)(6)(E) of the Act.
For devices, developing a proposed estimate of pass-through spending in CY 2020 entails estimating spending for two groups of items. The first group of items consists of device categories that are currently eligible for pass-through payment and that will continue to be eligible for pass-through payment in CY 2020. The CY 2008 OPPS/ASC final rule with comment period (72 FR 66778) describes the methodology we have used in previous years to develop the pass-through spending estimate for known device categories continuing into the applicable update year. The second group of items consists of items that we know are newly eligible, or project may be newly eligible, for device pass-through payment in the remaining quarters of CY 2019 or beginning in CY 2020. The sum of the proposed CY 2020 pass-through spending estimates for these two groups of device categories equaled the proposed total CY 2020 pass-through spending estimate for device categories with pass-through payment status. We based the device pass-through estimated payments for each device category on the amount of payment as established in section 1833(t)(6)(D)(ii) of the Act, and as outlined in previous rules, including the CY 2014 OPPS/ASC final rule with comment period (78 FR 75034 through 75036). We note that, beginning in CY 2010, the pass-through evaluation process and pass-through payment methodology for implantable biologicals newly approved for pass-through payment beginning on or after January 1, 2010, that are surgically inserted or implanted (through a surgical incision or a natural orifice) use the device pass-through process and payment methodology (74 FR 60476). As has been our past practice (76 FR 74335), in the proposed rule, we proposed to include an estimate of any implantable biologicals eligible for pass-through payment in our estimate of pass-through spending for devices. Similarly, we finalized a policy in CY 2015 that applications for pass-through payment for skin substitutes and similar products be evaluated using the medical device pass-through process and payment methodology (76 FR 66885 through 66888). Therefore, as we did beginning in CY 2015, for CY 2020, we also proposed to include an estimate of any skin substitutes and similar products in our estimate of pass-through spending for devices.
For drugs and biologicals eligible for pass-through payment, section 1833(t)(6)(D)(i) of the Act establishes the pass-through payment amount as the amount by which the amount authorized under section 1842(o) of the Act (or, if the drug or biological is covered under a competitive acquisition contract under section 1847B of the Act, an amount determined by the Secretary equal to the average price for the drug or biological for all competitive acquisition areas and year established under such section as calculated and adjusted by the Secretary) exceeds the portion of the otherwise applicable fee schedule amount that the Secretary determines is associated with the drug or biological. Our estimate of drug and biological pass-through payment for CY 2020 for this group of items is $224.1 million, as discussed below, because we proposed to pay for most nonpass-through separately payable drugs and biologicals under the CY 2020 OPPS at ASP+6 percent with the exception of 340B-acquired separately payable drugs that are paid at ASP minus 22.5 percent, and because we proposed to pay for CY 2020 pass-through payment drugs and biologicals at ASP+6 percent, as we discuss in section V.A. of the CY 2020 OPPS/ASC proposed rule. We refer readers to section V.B.6 of the CY 2020 OPPS/ASC proposed rule where we discuss the comments we solicited on an appropriate remedy in litigation involving our OPPS payment policy for 340B purchased drugs, which would inform CY 2021 rulemaking in the event of an adverse decision on appeal in that litigation.
Furthermore, payment for certain drugs, specifically diagnostic radiopharmaceuticals and contrast agents without pass-through payment status, is packaged into payment for the associated procedures, and these products will not be separately paid. In addition, we policy-package all nonpass-through drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure and drugs and biologicals that function as supplies when used in a surgical procedure, as discussed in section II.A.3. of the CY 2020 OPPS/ASC proposed rule and this final rule with comment period. In the CY 2020 OPPS/ASC proposed rule (84 FR 39511), we proposed that all of these policy-packaged drugs and biologicals with pass-through payment status would be paid at ASP+6 percent, like other pass-through drugs and biologicals, for CY 2020. Therefore, our estimate of pass-through payment for policy-packaged drugs and biologicals with pass-through payment status approved prior to CY 2020 was not $0, as discussed below. In section V.A.5. of the CY 2020 OPPS/ASC proposed rule, we discussed our policy to determine if the costs of certain policy-packaged drugs or biologicals are already packaged into the existing APC structure. If we determine that a policy-packaged drug or biological approved for pass-through payment resembles predecessor drugs or biologicals already included in the costs of the APCs that are associated with the drug receiving pass-through payment, we proposed to offset the amount of pass-through payment for the policy-packaged drug or biological. For these drugs or biologicals, the APC offset amount is the portion of the APC payment for the specific procedure performed with the pass-through drug or biological, which we refer to as the policy-packaged drug APC offset amount. If we determine that an offset is appropriate for a specific policy-packaged drug or biological receiving pass-through payment, we proposed to reduce our estimate of pass-through payments for these drugs or biologicals by this amount.
Similar to pass-through spending estimates for devices, the first group of drugs and biologicals requiring a pass-through payment estimate consists of those products that were recently made eligible for pass-through payment and that will continue to be eligible for pass-through payment in CY 2020. The second group contains drugs and biologicals that we know are newly eligible, or project will be newly eligible, in the remaining quarters of CY 2019 or beginning in CY 2020. The sum of the CY 2020 pass-through spending estimates for these two groups of drugs and biologicals equals the total CY 2020 pass-through spending estimate for drugs and biologicals with pass-through payment status.
B. Estimate of Pass-Through Spending
In the CY 2020 OPPS/ASC proposed rule (84 FR 39511 through 39512), we proposed to set the applicable pass-through payment percentage limit at 2.0 percent of the total projected OPPS payments for CY 2020, consistent with section 1833(t)(6)(E)(ii)(II) of the Act and our OPPS policy from CY 2004 through CY 2019 (82 FR 59371 through 59373).
For the first group, consisting of device categories that are currently eligible for pass-through payment and will continue to be eligible for pass-through payment in CY 2020, there is one active category for CY 2020. The active category is described by HCPCS code C1823 (Generator, neurostimulator (implantable), nonrechargeable, with transvenous sensing and stimulation leads). Based on the information from the device manufacturer, we estimated that 100 devices will receive payment in the OPPS in CY 2020 at an estimated cost of $5,655 per device. Therefore, we proposed an estimate for the first group of devices of $565,500. We did not receive any public comments on the proposal. Therefore, we are finalizing the proposed estimate for the first group of devices of $565,500 for CY 2020.
In estimating our proposed CY 2020 pass-through spending for device categories in the second group, we included: Device categories that we knew at the time of the development of the proposed rule will be newly eligible for pass-through payment in CY 2020; additional device categories that we estimated could be approved for pass-through status after the development of the proposed rule and before January 1, 2020; and contingent projections for new device categories established in the second through fourth quarters of CY 2020. For CY 2020, we proposed to use the general methodology described in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66778), while also taking into account recent OPPS experience in approving new pass-through device categories. For the proposed rule, the proposed estimate of CY 2020 pass-through spending for this second group of device categories was $10 million.
We did not receive any public comments on this proposal. As stated earlier in this final rule with comment period, we are approving five devices for pass-through payment status: Surefire® SparkTM Infusion System; Optimizer® System; AquaBeam® System; AUGMENT® Bone Graft and ARTIFICIAL Iris® . The manufacturers of these systems provided utilization and cost data that indicate the spending for the devices would be approximately $116.25 million for Surefire® SparkTM Infusion System, $46 million for Optimizer® System, $11.25 million for AquaBeam® System, $ 72.2 million for AUGMENT® Bone Graft, and $500,500 for ARTIFICIAL Iris®. Therefore, we are finalizing an estimate of $246.2 million for this second group of devices for CY 2020.
To estimate proposed CY 2020 pass-through spending for drugs and biologicals in the first group, specifically those drugs and biologicals recently made eligible for pass-through payment and continuing on pass-through payment status for at least one quarter in CY 2020, we proposed to use the most recent Medicare hospital outpatient claims data regarding their utilization, information provided in the respective pass-through applications, historical hospital claims data, pharmaceutical industry information, and clinical information regarding those drugs or biologicals to project the CY 2020 OPPS utilization of the products.
For the known drugs and biologicals (excluding policy-packaged diagnostic radiopharmaceuticals, contrast agents, drugs, biologicals, and radiopharmaceuticals that function as supplies when used in a diagnostic test or procedure, and drugs and biologicals that function as supplies when used in a surgical procedure) that will be continuing on pass-through payment status in CY 2020, we estimated the pass-through payment amount as the difference between ASP+6 percent and the payment rate for nonpass-through drugs and biologicals that will be separately paid. Separately payable drugs are paid at a rate of ASP+6 percent with the exception of 340B-acquired drugs that are paid at ASP minus 22.5 percent. Therefore, the payment rate difference between the pass-through payment amount and the nonpass-through payment amount is $224.1 million for this group of drugs. Because payment for policy-packaged drugs and biologicals is packaged if the product was not paid separately due to its pass-through payment status, we proposed to include in the CY 2020 pass-through estimate the difference between payment for the policy-packaged drug or biological at ASP+6 percent (or WAC+6 percent, or 95 percent of AWP, if ASP or WAC information is not available) and the policy-packaged drug APC offset amount, if we determine that the policy-packaged drug or biological approved for pass-through payment resembles a predecessor drug or biological already included in the costs of the APCs that are associated with the drug receiving pass-through payment, which we estimate for CY 2020 to be $17.0 million. For the proposed rule, using the proposed methodology described above, we calculated a CY 2020 proposed spending estimate for this first group of drugs and biologicals that includes drugs currently on pass-through payment status that would otherwise be separately payable or policy-packaged of approximately $241.1 million. We did not receive any public comments on our proposal. Using our methodology for this final rule with comment period, we calculated a CY 2020 spending estimate for this first group of drugs and biologicals of approximately $399.6 million.
To estimate proposed CY 2020 pass-through spending for drugs and biologicals in the second group (that is, drugs and biologicals that we knew at the time of development of the proposed rule were newly eligible for pass-through payment in CY 2020, additional drugs and biologicals that we estimated could be approved for pass-through status subsequent to the development of the proposed rule and before January 1, 2020 and projections for new drugs and biologicals that could be initially eligible for pass-through payment in the second through fourth quarters of CY 2020), we proposed to use utilization estimates from pass-through applicants, pharmaceutical industry data, clinical information, recent trends in the per unit ASPs of hospital outpatient drugs, and projected annual changes in service volume and intensity as our basis for making the CY 2020 pass-through payment estimate. We also proposed to consider the most recent OPPS experience in approving new pass-through drugs and biologicals. Using our proposed methodology for estimating CY 2020 pass-through payments for this second group of drugs, we calculated a proposed spending estimate for this second group of drugs and biologicals of approximately $17.1 million.
We did not receive any public comments on our proposal. Therefore, for CY 2020, we are continuing to use the general methodology described above. For this final rule with comment period, we calculated a CY 2020 spending estimate for this second group of drugs and biologicals of approximately $26 million.
In summary, in accordance with the methodology described earlier in this section, for this final rule with comment period, we estimate that total pass-through spending for the device categories and the drugs and biologicals that are continuing to receive pass-through payment in CY 2020 and those device categories, drugs, and biologicals that first become eligible for pass-through payment during CY 2020 is approximately $698.4 million (approximately $246.8 million for device categories and approximately $451.6 million for drugs and biologicals) which represents 0.88 percent of total projected OPPS payments for CY 2020 (approximately $79 billion). Therefore, we estimate that pass-through spending in CY 2020 will not amount to 2.0 percent of total projected OPPS CY 2020 program spending.
VII. OPPS Payment for Hospital Outpatient Visits and Critical Care Services
For CY 2020, we proposed to continue with our current clinic and emergency department (ED) hospital outpatient visits payment policies. For a description of the current clinic and ED hospital outpatient visits policies, we refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70448). We also proposed to continue our payment policy for critical care services for CY 2020. For a description of the current payment policy for critical care services, we refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70449), and for the history of the payment policy for critical care services, we refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75043). In the proposed rule, we sought public comments on any changes to these codes that we should consider for future rulemaking cycles. We continue to encourage commenters to provide the data and analysis necessary to justify any suggested changes.
Comment: We received two public comments, one from a health system and another from a health information management association, in response to our CY 2020 proposal. Commenters suggested that CMS should adopt the recommendation of the Medicare Payment Advisory Commission (MedPAC) for the development and implementation of a set of national guidelines for coding hospital emergency department (ED) visits under the OPPS. They argued that national guidelines would provide hospitals with a clear set of rules for coding ED visits.
Response: We thank the commenters for their responses. We will consider these comments for future rulemaking.
After consideration of the public comments received, we are finalizing our CY 2020 proposal to continue our current clinic and ED hospital outpatient visits and critical care services payment policies without modifications.
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59004 through 59015), we adopted a method to control unnecessary increases in the volume of covered outpatient department services under section 1833(t)(2)(F) of the Act by utilizing a Medicare Physician Fee Schedule (PFS)-equivalent payment rate for the hospital outpatient clinic visit (HCPCS code G0463) when it is furnished by excepted off-campus provider-based departments (PBDs). As discussed in section X.D of the proposed rule and the CY 2019 final rule (FR 58818 through 59179), CY 2020 will be the second year of the 2-year transition of this policy, and in CY 2020, these departments will be paid the site-specific PFS rate for the clinic visit service. For a full discussion of this policy, we refer readers to the CY 2020 final rule with comment period and section X.C of this final rule with comment period.
VIII. Payment for Partial Hospitalization Services
A. Background
A partial hospitalization program (PHP) is an intensive outpatient program of psychiatric services provided as an alternative to inpatient psychiatric care for individuals who have an acute mental illness, which includes, but is not limited to, conditions such as depression, schizophrenia, and substance use disorders. Section 1861(ff)(1) of the Act defines partial hospitalization services as the items and services described in paragraph (2) prescribed by a physician and provided under a program described in paragraph (3) under the supervision of a physician pursuant to an individualized, written plan of treatment established and periodically reviewed by a physician (in consultation with appropriate staff participating in such program), which sets forth the physician's diagnosis, the type, amount, frequency, and duration of the items and services provided under the plan, and the goals for treatment under the plan. Section 1861(ff)(2) of the Act describes the items and services included in partial hospitalization services. Section 1861(ff)(3)(A) of the Act specifies that a PHP is a program furnished by a hospital to its outpatients or by a community mental health center (CMHC), as a distinct and organized intensive ambulatory treatment service, offering less than 24-hour-daily care, in a location other than an individual's home or inpatient or residential setting. Section 1861(ff)(3)(B) of the Act defines a CMHC for purposes of this benefit.
Section 1833(t)(1)(B)(i) of the Act provides the Secretary with the authority to designate the outpatient department (OPD) services to be covered under the OPPS. The Medicare regulations that implement this provision specify, at 42 CFR 419.21, that payments under the OPPS will be made for partial hospitalization services furnished by CMHCs as well as Medicare Part B services furnished to hospital outpatients designated by the Secretary, which include partial hospitalization services (65 FR 18444 through 18445).
Section 1833(t)(2)(C) of the Act requires the Secretary, in part, to establish relative payment weights for covered OPD services (and any groups of such services described in section 1833(t)(2)(B) of the Act) based on median (or, at the election of the Secretary, mean) hospital costs using data on claims from 1996 and data from the most recent available cost reports. In pertinent part, section 1833(t)(2)(B) of the Act provides that the Secretary may establish groups of covered OPD services, within a classification system developed by the Secretary for covered OPD services, so that services classified within each group are comparable clinically and with respect to the use of resources. In accordance with these provisions, we have developed the PHP APCs. Since a day of care is the unit that defines the structure and scheduling of partial hospitalization services, we established a per diem payment methodology for the PHP APCs, effective for services furnished on or after July 1, 2000 (65 FR 18452 through 18455). Under this methodology, the median per diem costs were used to calculate the relative payment weights for the PHP APCs. Section 1833(t)(9)(A) of the Act requires the Secretary to review, not less often than annually, and revise the groups, the relative payment weights, and the wage and other adjustments described in section 1833(t)(2) of the Act to take into account changes in medical practice, changes in technology, the addition of new services, new cost data, and other relevant information and factors.
We began efforts to strengthen the PHP benefit through extensive data analysis, along with policy and payment changes finalized in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66670 through 66676). In that final rule with comment period, we made two refinements to the methodology for computing the PHP median: The first remapped 10 revenue codes that are common among hospital-based PHP claims to the most appropriate cost centers; and the second refined our methodology for computing the PHP median per diem cost by computing a separate per diem cost for each day rather than for each bill.
In CY 2009, we implemented several regulatory, policy, and payment changes, including a two-tier payment approach for partial hospitalization services under which we paid one amount for days with 3 services under PHP APC 0172 (Level 1 Partial Hospitalization) and a higher amount for days with 4 or more services under PHP APC 0173 (Level 2 Partial Hospitalization) (73 FR 68688 through 68693). We also finalized our policy to deny payment for any PHP claims submitted for days when fewer than 3 units of therapeutic services are provided (73 FR 68694). Additionally, for CY 2009, we revised the regulations at 42 CFR 410.43 to codify existing basic PHP patient eligibility criteria and to add a reference to current physician certification requirements under 42 CFR 424.24 to conform our regulations to our longstanding policy (73 FR 68694 through 68695). We also revised the partial hospitalization benefit to include several coding updates (73 FR 68695 through 68697).
For CY 2010, we retained the two-tier payment approach for partial hospitalization services and used only hospital-based PHP data in computing the PHP APC per diem costs, upon which PHP APC per diem payment rates are based. We used only hospital-based PHP data because we were concerned about further reducing both PHP APC per diem payment rates without knowing the impact of the policy and payment changes we made in CY 2009. Because of the 2-year lag between data collection and rulemaking, the changes we made in CY 2009 were reflected for the first time in the claims data that we used to determine payment rates for the CY 2011 rulemaking (74 FR 60556 through 60559).
In the CY 2011 OPPS/ASC final rule with comment period (75 FR 71994), we established four separate PHP APC per diem payment rates: Two for CMHCs (APC 0172 (for Level 1 services) and APC 0173 (for Level 2 services)) and two for hospital-based PHPs (APC 0175 (for Level 1 services) and APC 0176 (for Level 2 services)), based on each provider type's own unique data. For CY 2011, we also instituted a 2-year transition period for CMHCs to the CMHC APC per diem payment rates based solely on CMHC data. Under the transition methodology, CMHC APCs Level 1 and Level 2 per diem costs were calculated by taking 50 percent of the difference between the CY 2010 final hospital-based PHP median costs and the CY 2011 final CMHC median costs and then adding that number to the CY 2011 final CMHC median costs. A 2-year transition under this methodology moved us in the direction of our goal, which is to pay appropriately for partial hospitalization services based on each provider type's data, while at the same time allowing providers time to adjust their business operations and protect access to care for Medicare beneficiaries. We also stated that we would review and analyze the data during the CY 2012 rulemaking cycle and, based on these analyses, we might further refine the payment mechanism. We refer readers to section X.B. of the CY 2011 OPPS/ASC final rule with comment period (75 FR 71991 through 71994) for a full discussion.
In addition, in accordance with section 1301(b) of the Health Care and Education Reconciliation Act of 2010 (HCERA 2010), we amended the description of a PHP in our regulations to specify that a PHP must be a distinct and organized intensive ambulatory treatment program offering less than 24-hour daily care other than in an individual's home or in an inpatient or residential setting. In accordance with section 1301(a) of HCERA 2010, we revised the definition of a CMHC in the regulations to conform to the revised definition now set forth under section 1861(ff)(3)(B) of the Act (75 FR 71990).
For CY 2012, as discussed in the CY 2012 OPPS/ASC final rule with comment period (76 FR 74348 through 74352), we determined the relative payment weights for partial hospitalization services provided by CMHCs based on data derived solely from CMHCs and the relative payment weights for partial hospitalization services provided by hospital-based PHPs based exclusively on hospital data.
In the CY 2013 OPPS/ASC final rule with comment period, we finalized our proposal to base the relative payment weights that underpin the OPPS APCs, including the four PHP APCs (APCs 0172, 0173, 0175, and 0176), on geometric mean costs rather than on the median costs. We established these four PHP APC per diem payment rates based on geometric mean cost levels calculated using the most recent claims and cost data for each provider type. For a detailed discussion on this policy, we refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68406 through 68412).
In the CY 2014 OPPS/ASC proposed rule (78 FR 43621 through 43622), we solicited comments on possible future initiatives that may help to ensure the long-term stability of PHPs and further improve the accuracy of payment for PHP services, but proposed no changes. In the CY 2014 OPPS/ASC final rule with comment period (78 FR 75050 through 75053), we summarized the comments received on those possible future initiatives. We also continued to apply our established policies to calculate the four PHP APC per diem payment rates based on geometric mean per diem costs using the most recent claims data for each provider type. For a detailed discussion on this policy, we refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75047 through 75050).
In the CY 2015 OPPS/ASC final rule with comment period (79 FR 66902 through 66908), we continued to apply our established policies to calculate the four PHP APC per diem payment rates based on PHP APC geometric mean per diem costs, using the most recent claims and cost data for each provider type.
In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70455 through 70465), we described our extensive analysis of the claims and cost data and ratesetting methodology. We found aberrant data from some hospital-based PHP providers that were not captured using the existing OPPS ±3 standard deviation trims for extreme cost-to-charge ratios (CCRs) and excessive CMHC charges resulting in CMHC geometric mean costs per day that were approximately the same as or more than the daily payment for inpatient psychiatric facility services. Consequently, we implemented a trim to remove hospital-based PHP service days that use a CCR that was greater than five to calculate costs for at least one of their component services, and a trim on CMHCs with a geometric mean cost per day that is above or below 2 (±2) standard deviations from the mean. We stated in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70456) that, without using a trimming process, the data from these providers would inappropriately skew the geometric mean per diem cost for Level 2 CMHC services.
In addition, in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70459 through 70460), we corrected a cost inversion that occurred in the final rule data with respect to hospital-based PHP providers. We corrected the cost inversion with an equitable adjustment to the actual geometric mean per diem costs by increasing the Level 2 hospital-based PHP APC geometric mean per diem costs and decreasing the Level 1 hospital-based PHP APC geometric mean per diem costs by the same factor, to result in a percentage difference equal to the average percent difference between the hospital-based Level 1 PHP APC and the Level 2 PHP APC for partial hospitalization services from CY 2013 through CY 2015.
Finally, we renumbered the PHP APCs, which were previously APCs 0172 and 0173 for CMHCs' partial hospitalization Level 1 and Level 2 services, and APCs 0175 and 0176 for hospital-based partial hospitalization Level 1 and Level 2 services to APCs 5851 and 5852 for CMHCs' partial hospitalization Level 1 and Level 2 services, and APCs 5861 and 5862 for hospital-based partial hospitalization Level 1 and Level 2 services, respectively. For a detailed discussion of the PHP ratesetting process, we refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70462 through 70467).
In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79687 through 79691), we continued to apply our established policies to calculate the PHP APC per diem payment rates based on geometric mean per diem costs using the most recent claims and cost data for each provider type. However, we finalized a policy to combine the Level 1 and Level 2 PHP APCs for CMHCs and to combine the Level 1 and Level 2 APCs for hospital-based PHPs because we believed this would best reflect actual geometric mean per diem costs going forward, provide more predictable per diem costs, particularly given the small number of CMHCs, and generate more appropriate payments for these services, for example by avoiding the cost inversions for hospital-based PHPs addressed in the CY 2016 and CY 2017 OPPS/ASC final rules with comment period (80 FR 70459 and 81 FR 79682). We also implemented an eight-percent outlier cap for CMHCs to mitigate potential outlier billing vulnerabilities by limiting the impact of inflated CMHC charges on outlier payments. We stated that we will continue to monitor the trends in outlier payments and consider policy adjustments as necessary.
For a comprehensive description of PHP payment policy, including a detailed methodology for determining PHP per diem amounts, we refer readers to the CY 2016 and CY 2017 OPPS/ASC final rules with comment period (80 FR 70453 through 70455 and 81 FR 79678 through 79680).
In the CYs 2018 and 2019 OPPS/ASC final rules with comment period (82 FR 59373 through 59381, and 83 FR 58983 through 58998, respectively), we continued to apply our established policies to calculate the PHP APC per diem payment rates based on geometric mean per diem costs using the most recent claims and cost data for each provider type. We also continued to designate a portion of the estimated 1.0 percent hospital outpatient outlier threshold specifically for CMHCs, consistent with the percentage of projected payments to CMHCs under the OPPS, excluding outlier payments. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 58997 through 58998), we also included proposed updates to the PHP allowable HCPCS codes. Specifically, we proposed to delete six psychological and neuropsychological testing CPT codes, which affect PHPs, and to add nine new codes as replacements. We refer readers to section VIII.D. of the proposed rule for a discussion of those proposed updates and the applicability for CY 2020.
B. Final PHP APC Update for CY 2020
1. Final PHP APC Geometric Mean Per Diem Costs
In summary, for CY 2020, we are finalizing our proposal as proposed to use the CY 2020 CMHC geometric mean per diem cost calculated in accordance with our existing methodology, but with a cost floor equal to the CY 2019 final geometric mean per diem cost for CMHCs of $121.62 (83 FR 58991), as the basis for developing the CY 2020 CMHC APC per diem rate. We are also finalizing our proposal to use the CY 2020 hospital-based PHP geometric mean per diem cost of $233.52, calculated in accordance with our existing methodology for hospital-based PHPs, as the basis for developing the CY 2020 hospital-based APC per diem rate. We are finalizing our proposal to use the most recent updated claims and cost data to calculate CY 2020 geometric mean per diem costs in this final rule with comment period.
Also, we are finalizing our proposal to continue to use CMHC APC 5853 (Partial Hospitalization (3 or More Services Per Day)) and hospital-based PHP APC 5863 (Partial Hospitalization (3 or More Services Per Day)). These proposals, which we are finalizing as proposed in this final rule with comment period, are discussed in more detail.
2. Development of the Final PHP APC Geometric Mean Per Diem Costs
In preparation for CY 2020 and subsequent years, we followed the PHP ratesetting methodology described in section VIII.B.2. of the CY 2016 OPPS/ASC final rule with comment period (80 FR 70462 through 70466) to calculate the PHP APCs' geometric mean per diem costs and payment rates for APCs 5853 and 5863, incorporating the modifications made in the CY 2017 OPPS/ASC final rule with comment period. As discussed in section VIII.B.1. of the CY 2017 OPPS/ASC final rule with comment period (81 FR 79680 through 79687), the geometric mean per diem cost for hospital-based PHP APC 5863 is based upon actual hospital-based PHP claims and costs for PHP service days providing 3 or more services. Similarly, the geometric mean per diem cost for CMHC APC 5853 is based upon actual CMHC claims and costs for CMHC service days providing three or more services.
The CMHC or hospital-based PHP APC per diem costs are the provider-type specific costs derived from the most recent claims and cost data. The CMHC or hospital-based PHP APC per diem payment rates are the national unadjusted payment rates calculated from the CMHC or hospital-based PHP APC geometric mean per diem costs, after applying the OPPS budget neutrality adjustments described in section II.A.4. of this final rule with comment period.
As previously stated, in the CY 2020 OPPS/ASC proposed rule, we proposed to apply our established methodologies in calculating the CY 2020 geometric mean per diem costs and payment rates, including the application of a ±2 standard deviation trim on costs per day for CMHCs and a CCR greater than 5 hospital service day trim for hospital-based PHP providers. These two trims were finalized in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70455 through 70462) for CY 2016 and subsequent years.
a. CMHC Data Preparation: Data Trims, Exclusions, and CCR Adjustments
For this CY 2020 final rule with comment period, prior to calculating the final geometric mean per diem cost for CMHC APC 5853, we prepared the data by first applying trims and data exclusions, and assessing CCRs as described in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70463 through 70465), so that ratesetting is not skewed by providers with extreme data. Before any trims or exclusions were applied, there were 44 CMHCs in the PHP claims data file. Under the ±2 standard deviation trim policy, we excluded any data from a CMHC for ratesetting purposes when the CMHC's geometric mean cost per day was more than ±2 standard deviations from the geometric mean cost per day for all CMHCs. In applying this trim for CY 2020 ratesetting, no CMHCs had geometric mean costs per day below the trim's lower limit of $20.58 or had geometric mean costs per day above the trim's upper limit of $520.48. Therefore, we did not exclude any CMHCs because of the ±2 standard deviation trim.
In accordance with our PHP ratesetting methodology, we also remove service days with no wage index values, because we use the wage index data to remove the effects of geographic variation in costs prior to APC geometric mean per diem cost calculation (80 FR 70465). For this CY 2020 final rule with comment period ratesetting, no CMHC was missing wage index data for all of its service days and, therefore, no CMHC was excluded. However, one CMHC had no days with Medicare payment, and it was excluded from ratesetting.
In addition to our trims and data exclusions, before calculating the PHP APC geometric mean per diem costs, we also assess CCRs (80 FR 70463). Our longstanding PHP OPPS ratesetting methodology defaults any CMHC CCR greater than one to the statewide hospital CCR (80 FR 70457). For this CY 2020 OPPS/ASC final rule with comment period ratesetting, there were no CMHCs that showed CCRs greater than one. Therefore, it was not necessary to default any CMHC to its statewide hospital CCR for ratesetting.
In summary, these data preparation steps did not adjust the CCR for any CMHCs with a CCR greater than one during our ratesetting process. We also did not exclude any CMHCs for other missing data or for failing the ±2 standard deviation trim, but excluded one CMHC for having no Medicare payment data, resulting in the inclusion of 43 CMHCs. There were 319 CMHC claims removed during data preparation steps because they either had no PHP-allowable codes or had zero payment days, leaving 12,265 CMHC claims in our CY 2020 final rule ratesetting modeling.
After applying all of the previously listed trims, exclusions, and adjustments, we followed the methodology described in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70464 through 70465) and modified in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79687 through 79688, and 79691) to calculate a CMHC APC geometric mean per diem cost.[74] The calculated CY 2020 geometric mean per diem cost for all CMHCs for providing 3 or more services per day (CMHC APC 5853) is $103.50, a decrease from $121.62 calculated last year for CY 2019 ratesetting (83 FR 58986 through 58989). This final calculated per diem cost for CMHCs is almost the same as the $103.42 geometric mean per diem cost calculated for the CY 2020 OPPS/ASC proposed rule (84 FR 39515 to 39516).
Due to this fluctuation from the CY 2019 final CMHC geometric mean per diem cost, we investigated why the CY 2020 final calculated CMHC APC geometric mean per diem cost had decreased from the prior year, and found that two large providers reported lower costs per day than those reported for the CY 2019 final rule ratesetting; those two providers heavily influenced the calculated geometric mean per diem cost. Because these providers had a high number of paid PHP days, and because the CMHC data set is so small (n=43), these providers had a significant influence on the calculated CY 2020 CMHC APC geometric mean per diem cost. In the case of PHPs provided by CMHCs, we have a low number of PHP providers in our ratesetting dataset (43 CMHCs compared to 374 hospital-based PHPs) that provide a small volume of services and, therefore, account for a limited amount of payments, relative to the rest of OPPS payments (total CY 2018 CMHC payments are estimated to be approximately 0.02 percent of all OPPS payments).
As noted in the CY 2020 OPPS/ASC proposed rule (84 FR 39516), we are concerned that a final calculated CMHC APC geometric mean per diem cost of $103.50 would not support ongoing access to PHPs in CMHCs. This cost is nearly a 15 percent decrease from the final CY 2019 CMHC geometric mean per diem cost. We believe access to partial hospitalization services and PHPs is better supported when the geometric mean per diem cost does not fluctuate greatly. In addition, while the CMHC APC 5853 is described as providing 3 or more partial hospitalization services per day (81 FR 79680), 95 percent of CMHC paid days in CY 2018 were for providing 4 or more services per day. To be eligible for a PHP, a patient must need at least 20 hours of therapeutic services per week, as evidenced in the patient's plan of care (42 CFR 410.43(c)(1)). To meet those patient needs, most PHP provider paid days are for providing 4 or more services per day (we refer readers to Table 22.—Percentage of PHP Days by Service Unit Frequency of the proposed rule). Therefore, the CMHC APC 5853 is actually heavily weighted to the cost of providing 4 or more services. The per diem costs for CMHC APC 5853 have been calculated as $124.92, $143.22, and $121.62 for CY 2017 (81 FR 79691), CY 2018 (82 FR 59378), and CY 2019 (83 FR 58991), respectively. We do not believe it is likely that the actual cost of providing partial hospitalization services through a PHP by CMHCs has suddenly declined when costs generally increase over time. We are concerned by this fluctuation, which we believe is influenced by data from two large providers.
Therefore, rather than simply finalizing the calculated CY 2020 CMHC APC geometric mean per diem cost of $103.50 for CY 2020 ratesetting, we are instead finalizing our proposal as proposed, to use the CY 2020 CMHC APC geometric mean per diem cost, calculated in accordance with our existing methodology, but with a cost floor equal to the CY 2019 final geometric mean per diem cost for CMHCs of $121.62 (83 FR 58991), as the basis for developing the final CY 2020 CMHC APC per diem rate. We believe using the CY 2019 CMHC geometric mean per diem cost as the floor is appropriate because it is based on very recent CMHC PHP claims and cost data and would help to protect provider access by preventing wide fluctuation in the per diem costs for CMHC APC 5853. As we proposed, in this final rule with comment period, we used the most recent updated claims and cost data to calculate CY 2020 CMHC geometric mean per diem cost, which was $103.50. Because the final CY 2020 CMHC calculated geometric mean per diem cost of $103.50 is less than the proposed cost floor (which equals the final CY 2019 CMHC APC geometric mean per diem cost of $121.62), the final CY 2020 CMHC geometric mean per diem cost is $121.62. Implementing the cost floor for CY 2020 will protect CMHCs since the final CY 2020 calculated per diem cost of $103.50 still results in an amount that is less than $121.62. We believe finalizing the CMHC cost floor amount of $121.62 as the final CY 2020 CMHC APC geometric mean per diem cost allows us to use the most recent or very recent CMHC claims and cost reporting data while still protecting provider access. To be clear, this policy would only apply for the CY 2020 ratesetting.
As we noted in the CY 2020 OPPS/ASC proposed rule (84 FR 39516), we also considered proposing a 3-year rolling average calculated using the final PHP geometric mean per diem costs, by provider type, from CY 2018 (82 FR 59378), CY 2019 (83 FR 58991), and the calculated CY 2020 geometric mean per diem cost from that proposed rule of $103.42 for CMHCs, and the calculated CY 2020 geometric mean per diem costs for hospital-based PHPs discussed in section VIII.B.2.b. of the CY 2020 OPPS/ASC proposed rule. The 3-year rolling averages discussed in that proposed rule resulted in geometric mean per diem costs that would have been $122.75 for CMHCs, and $209.79 for hospital-based PHPs. While we believe this option would have avoided the fluctuation in the geometric mean per diem cost and, therefore, supported access to PHPs provided by CMHCs, it would have maintained the fluctuation in the geometric mean per diem costs used to derive the hospital-based PHP APC per diem payment rates. This is further discussed in the hospital-based PHP section VIII.B.2.b. of the CY 2020 OPPS/ASC proposed rule and section VIII.B.2.b. of this final rule. In addition, we believe that it is necessary to recalculate the CMHC geometric mean per diem cost for this final rule with comment period using updated claims and cost data, and simply proposing to use a 3-year rolling average for the CMHC geometric mean per diem cost for CY 2020 would not have allowed us to do so. Therefore, we believe that it is more appropriate to use the final CY 2019 geometric mean per diem costs, by provider type, as the cost floor for use with the final calculated CY 2020 PHP geometric mean per diem costs, by provider type, because those CY 2019 per diem costs are based on very recent CMHC and hospital-based PHP claims and cost data, are the easiest to understand, and would result in proposed geometric mean per diem costs which would support access for both CMHCs and hospital-based PHPs.
We estimate the aggregate difference in the (prescaled) CMHC geometric mean per diem costs for CY 2020 from finalizing the CMHC cost floor amount of $121.62 rather than the calculated CMHC geometric mean per diem cost of $103.50 to be $1.7 million. We refer readers to section XXVII. of this final rule with comment period for payment impacts, which are budget neutral.
We received 6 comments, with those focused on CMHC rate setting summarized as follows:
Comment: Nearly all commenters supported our proposal to calculate updated per diem costs with a cost floor, to avoid fluctuations in CMHC payments and help protect access.
Response: We thank the commenters for their support. For CY 2020, we are finalizing the CY 2020 CMHC geometric mean per diem cost as $121.62, which is the cost floor amount, rather than the calculated geometric mean per diem cost of $103.50.
Comment: Two commenters recommended that CMS pay CMHCs the same rate as hospital-based PHPs, since these two provider types provide the same services and have the same qualified clinical staff. One commenter objected to CMS' continuing use of the single-tier payment system for CMHCs, stating that it adversely affects the quality and intensity of PHP services.
Response: The OPPS pays for outpatient services, including partial hospitalization services, based on the costs of providing services using provider data from claims and cost reports, in accordance with statute. Section 1833(t)(2)(B) of the Act provides that the Secretary may establish groups of covered OPD services, within a classification system developed by the Secretary for covered OPD services, so that services classified within each group are comparable clinically and with respect to the use of resources. While CMHCs and hospital-based CMHCs provide the same clinical services, their resource use differs, because these two provider types have different cost structures. We see this difference in cost structures reflected when we calculate the geometric mean cost per day for CMHCs versus for hospital-based PHPs, where CMHC costs per day are consistently lower than hospital-based PHP costs per day. For example, the final CY 2020 calculated geometric mean costs for providing PHP services were $103.50 per day for CMHCs, but were $233.52 per day for hospital-based PHPs. In this final rule and in prior rulemaking, commenters and CMS have noted that hospitals tend to have higher costs than CMHCs, particularly higher overhead (83 FR 58986; 82 FR 59377; 81 FR 79686 to 69687). Therefore, we do not believe we can pay CMHCs the same APC rate as hospital-based PHPs, and should calculate a CMHC APC rate based on the CMHC costs which providers supply on their cost reports. We strongly encourage CMHCs to review cost reporting instructions to be sure they are reporting their costs correctly. These instructions are available in chapter 45 of the Provider Reimbursement Manual, Part 2, available on the CMS website at https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Paper-Based-Manuals.html.
We believe our policy to replace the existing Level 1 and Level 2 PHP APCs for both provider types with a single PHP APC, by provider type, is supported by the statute and regulations and will continue to pay for partial hospitalization services appropriately based upon actual provider costs (81 FR 79683). Regarding the commenter's concern about the small number of providers and the use of a single-tier payment system, we refer the commenter to the CY 2017 OPPS/ASC final rule with comment period (81 FR 79682 to 79685), where we discussed our rationale for implementing the single-tier payment system for CMHCs. A key reason behind implementing the single tier for CMHCs was to reduce cost fluctuations and bring more stability to CMHC APC rates, especially given the small number of providers (81 FR 79683). We also noted that the costs of providing a Level 1 CMHC day were nearly the same as the cost of providing a Level 2 CMHC day (81 FR 79684). In accordance with the regulations at 42 CFR 419.31, we could not justify continuing to separate these services into two APCs, but combined clinically similar services with similar resource use into a single APC (81 FR 79683 to 79684).
We do not believe the intensity of PHP services provided in hospitals and in CMHCs has been affected by using a single-tier payment system. Based on the utilization data found in Table 22 of this final rule, the percentage of paid PHP days which have only three services has been relatively stable over time. As we note in section VIII.B.3.b, with only 2 years of claims data reflecting the single-tiered payment system, we do not have enough data yet to identify any trends in utilization that could be associated with the change from two-tiered to single-tiered payment. We continue to monitor the percentage of 3-service days and are also monitoring the provision of 20 hours per week of PHP services, to ensure there are no unintended consequences of a single-tier payment system on PHP intensity. We are unable to determine the effects of the single-tier payment on CMHC quality, because there are no quality measures for CMHCs, nor is quality reporting required of CMHCs. However, we do not believe that a single-tier payment system would affect the quality of care provided in a CMHC.
Comment: One commenter noted that, in the past, CMS stated that CMHCs provide fewer services and have less costly staff than hospitals.
Response: We believe that the commenter may be referring to the CY 2011 OPPS/ASC final rule with comment period (75 FR 71991), which states that we believe that CMHCs have a lower cost structure than their hospital-based PHP counterparts because the data showed that CMHCs provide fewer PHP services in a day and use less costly staff than hospital-based PHPs. Those statements were based on CY 2009 claims and cost data, which differ from more recent claims and cost data. Each year, we calculate geometric mean per diem costs based on updated claims and cost reports. We do not have detailed labor cost data to make a direct comparison of CMHC versus hospital-based PHP staff costs, so we could not comment on whether CMHCs have lower labor costs than hospital-based PHPs. But we note that both provider types use similar types of clinical staff (see personnel qualifications in 42 CFR 485.904 for CMHCs, and in 42 CFR 482.12, 482.23, and 482.62 for hospitals). Regarding the level of services provided, we refer the commenter to the utilization data in section VIII.B.3.b. of this CY 2020 final rule with comment period for details on current level of services CMHCs provide, based on CY 2018 claims data. Table 22 shows that CMHCs provide more days with four or more services than hospital-based PHPs.
Comment: Several commenters expressed concern about the decline in the number of CMHCs and hospital-based PHPs, and the effects on beneficiary access to care. Two commenters wrote that the current payment methodology has resulted in reductions in provider access rather than protection of access. Commenters noted that these declines have occurred while the need for mental health services has increased; that the demand for mental health services is on track to outpace the supply of behavioral health care providers; and that as the number of PHPs declines, it may become even more difficult to calculate the appropriate per diems. A few commenters noted that decreased access to PHP services could result in increasing instances of patient recidivism and more inpatient psychiatric admissions. One commenter noted that beneficiaries would have their treatment alternatives limited if CMHCs closed, and therefore, be forced to use more costly hospital-based PHPs, with higher beneficiary co-payments.
A commenter expressed concerns about CMHC rate setting being based on only 41 providers, and wrote that the data are skewed, the calculations are incorrect, and the proposed low payment rates would result in the remaining CMHCs closing. This commenter noted that setting CMHCs' payment rates based on a small number of CMHCs does not reflect the actual cost of providing these services and expressed concern that by using the mean or median costs, more CMHCs would close. The same commenter also stated that CMHCs incur extra costs to meet the CMHC conditions of participation (CoPs), have experienced an increase in bad debt expense, and the effects of sequestration.
Response: We appreciate the work PHPs do to care for a particularly vulnerable population with serious mental illnesses and believe that having PHPs available to beneficiaries helps prevent patient recidivism and inpatient psychiatric admissions. We share the commenters' concerns about the decline in the number of PHPs, particularly at CMHCs, and the effect on access. Our goal is to protect access to both provider types, so beneficiaries have choices regarding where to receive treatment. We want to ensure that CMHCs remain a viable option as providers of mental health care in the beneficiary's own community. We agree that beneficiaries receiving care at a CMHC instead of a hospital-based PHP would have lower out-of-pocket costs.
We disagree that the CMHC data are skewed and that the calculations are incorrect. In the CY 2016 OPPS/ASC final rule (80 FR 70456 to 70459), we implemented a ±2 standard deviation trim on CMHC costs per day to remove aberrant data that could skew costs up or down inappropriately. We recognize that with a small number of providers, such as the 43 CMHCs used for this final rule rate setting, the calculations can be influenced by large providers. That occurred in this CY 2020 final rule rate setting, as discussed previously in this section, and we proposed and are finalizing a cost floor in CY 2020 to help protect CMHCs from this fluctuation and possible effects on access.
We are confident that the per diem costs we calculate follow the methodology we discussed in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70462 to 70466) and in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79691). Those costs are geometric mean per diem costs, rather than arithmetic mean or median per diem costs; in the CY 2013 OPPS final rule (77 FR 68409), we discussed the advantages of using geometric means rather than medians to calculate PHP costs, and noted that the geometric mean more accurately captures the full range of service costs (including outliers) than the median cost and promotes more stability in the payment system.
We believe that providing payment that is based upon actual provider-reported costs will not lead to provider closures. As we have noted in prior rulemaking (76 FR 74350; 79 FR 66906), the closure of PHPs may be due to any number of reasons, such as business management or marketing decisions, competition, oversaturation of certain geographic areas, and Federal and State fraud and abuse efforts, among others. It does not directly follow that closure could be due to reduced per diem payment rates alone, especially when the per diem payment rates reflect the costs of PHP providers, as stated in claims and cost data.
Furthermore, most (if not all) of the costs associated with adhering to CoPs should be captured in the cost report data used in ratesetting and, therefore, are accounted for when computing the geometric mean per diem costs. The reduction to bad debt reimbursement was a result of provisions of section 3201 of the Middle Class Tax Extension and Job Creation Act of 2012 (Pub. L. 112-96). The reduction to bad debt reimbursement impacted all providers eligible to receive bad debt reimbursement, as discussed in the CY 2013 End-Stage Renal Disease final rule (77 FR 67518). Medicare currently reimburses bad debt for eligible providers at 65 percent. Because this percentage was enacted by Congress, CMS does not have the authority to change the percentage. In contrast to the Medicare bad debt reimbursement policy, private sector insurers typically do not reimburse providers for any amounts of enrollees' unpaid deductibles or coinsurance. In light of budgetary constraints and the steady increase in bad debt claims over the years, a reduction in bad debt reimbursement is necessary to protect the Medicare Trust Fund and preserve beneficiary access to care without imposing an undue burden on hospitals.
Finally, the reduction in payments due to sequestration has been mandated by Congress, and we are unable to remove or modify it. This mandatory payment reduction was established by the Budget Control Act of 2011 (Pub. L. 112-25) and amended by the American Taxpayer Relief Act of 2012 (Pub. L. 112-240). Sequestration is discussed in a Medicare Fee-for-Service Provider eNews article available at: https://www.cms.gov/Outreach-and-Education/Outreach/FFSProvPartProg/Downloads/2013-03-08-standalone.pdf. Sequestration is outside the scope of the CY 2020 OPPS/ASC proposed rule and this final rule with comment period.
Comment: One commenter suggested that CMS use value-based purchasing for paying CMHCs instead of a cost-based system. This commenter recommended that CMS look at the value provided by the quality of provided services. This commenter believed that rewarding providers for higher-quality care, as measured by selected standards, instead of rewarding providers for increasing costs, is a better way to improve the quality of any service.
Response: We responded to a similar public comment in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70462) and refer readers to a summary of that comment and our response. Currently, there is no statutory language authorizing value-based purchasing for CMHCs or for outpatient hospital-based PHPs. To reiterate, sections 1833(t)(2) and 1833(t)(9) of the Act set forth the requirements for establishing and adjusting OPPS payment rates, which are based on costs, and which include PHP payment rates.
We note that section 1833(t)(17) of the Act authorizes the Hospital Outpatient Quality Reporting (OQR) Program, which applies a payment reduction to subsection (d) hospitals that fail to meet program requirements. In the CY 2015 OPPS/ASC proposed rule (79 FR 41040), we considered future inclusion of, and requested comments on, the following quality measures addressing PHP issues that would apply in the hospital outpatient setting: (1) 30-Day Readmission; (2) Group Therapy; and (3) No Individual Therapy. We refer readers to the CY 2015 OPPS/ASC final rule with comment period (79 FR 66957 through 66958) for a more detailed discussion of PHP measures considered for inclusion in the Hospital OQR Program in future years, and of the comments received as a result of the solicitation. However, the Hospital OQR Program does not apply to CMHCs, and there are no quality measures applied to CMHCs.
Comment: Several commenters recommended that more work be done to establish PHP rates accurately, that CMS reconsider its PHP policy positions to determine how to rebuild PHP services, or that CMS establish a task force to review and discuss the availability of PHPs for Medicare beneficiaries.
Response: We will continue to explore policy options for strengthening the PHP benefit and increasing access to the valuable services provided by CMHCs as well as by hospital-based PHPs. As part of that process, we regularly review our methodology to ensure that it is appropriately capturing the cost of care reported by providers. For example, for the CY 2016 ratesetting, we extensively reviewed the methodology used for PHP ratesetting. In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70462 through 70466), we also included a detailed description of the ratesetting process to help all PHP providers record costs correctly so that we can more fully capture PHP costs in ratesetting. In this CY 2020 ratesetting, we proposed and are finalizing a policy to calculate the CY 2020 per diem costs with a cost floor. We believe that policy helps to support access, particularly for CMHCs, whose calculated costs were still below the cost floor when we ran the calculations with updated data for this final rule with comment period.
We also recognize that as the number of providers decreases, the ratesetting calculations can be more strongly influenced by the costs of large providers. We are regularly evaluating our rate setting methodology to ensure that it is as accurate as possible, and captures provider cost data fully. However, our rate setting methodology must comply with requirements given in statute at 1833(t)(2) and 1833(t)(9), and depends heavily on provider-reported costs. As noted previously, we strongly encourage CMHCs to review cost reporting instructions to be sure they are reporting their costs correctly. These instructions are available in chapter 45 of the Provider Reimbursement Manual, Part 2, available on the CMS website at https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Paper-Based-Manuals.html. We also strongly encourage those CMHCs that do not file full cost reports to consider doing so, to help us in more fully capturing CMHC costs in rate setting.
We maintain positive working relationships with various industry leaders representing both CMHCs and hospital-based PHP providers with whom we have consistently met over the years to discuss industry concerns and ideas. These relationships have provided significant and valued input regarding PHP ratesetting. We also hold Hospital Outpatient Open Door Forum calls monthly, in which all individuals are welcome to participate and/or submit questions regarding specific issues, including questions related to PHPs. Furthermore, we initiate rulemaking annually, through which we receive public comments on proposals set forth in a proposed rule and respond to those comments in a final rule. All individuals are provided an opportunity to comment, and we give consideration to each comment that we receive. Given the relationships that we have established with various industry leaders and the various means for us to receive comments and recommendations, we believe that we receive adequate input regarding ratesetting and take that input into consideration when establishing the payment rates. We continue to welcome any input and information that the public is willing to provide.
After consideration of the comments, we are finalizing our proposal as proposed. Because the final CY 2020 calculated CMHC geometric mean per diem cost of $103.50 is less than the cost floor amount of $121.62, the final CY 2020 CMHC geometric mean per diem cost is $121.62.
b. Hospital-Based PHP Data Preparation: Data Trims and Exclusions
For this CY 2020 final rule with comment period, we prepared data consistent with our policies as described in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70463 through 70465) for hospital-based PHP providers, which is similar to that used for CMHCs. The CY 2018 PHP claims included data for 436 hospital-based PHP providers for our calculations in this CY 2020 OPPS/ASC final rule with comment period.
Consistent with our policies as stated in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70463 through 70465), we prepared the data by applying trims and data exclusions. We applied a trim on hospital service days for hospital-based PHP providers with a CCR greater than 5 at the cost center level. To be clear, the CCR greater than 5 trim is a service day-level trim in contrast to the CMHC ±2 standard deviation trim, which is a provider-level trim. Applying this CCR greater than 5 trim removed affected service days from one hospital-based PHP provider with a CCR of 6.398 from our final ratesetting. However, 100 percent of the service days for this one hospital-based PHP provider had at least one service associated with a CCR greater than 5, so the trim removed this provider entirely from our final ratesetting. In addition, 59 hospital-based PHPs were removed for having no PHP costs and, therefore, no days with PHP payment. Two hospital-based PHPs were removed because none of their days included PHP-allowable HCPCS codes. No hospital-based PHPs were removed for missing wage index data, nor were any hospital-based PHPs removed by the OPPS ±3 standard deviation trim on costs per day. (We refer readers to the OPPS Claims Accounting Document, available online at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/CMS-1695-FC-2019-OPPS-FR-Claims-Accounting.pdf.)
Overall, we removed 62 hospital-based PHP providers [(1 with all service days having a CCR greater than 5) + (59 with zero daily costs and no PHP payment) + (2 with no PHP-allowable HCPCS codes)], resulting in 374 (436 total − 62 excluded) hospital-based PHP providers in the data used for calculating ratesetting. In addition, no hospital-based PHP providers were defaulted to their overall hospital ancillary CCRs due to outlier cost center CCR values.
After completing these data preparation steps, we calculated the final CY 2020 geometric mean per diem cost for hospital-based PHP APC 5863 for hospital-based partial hospitalization services by following the methodology described in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70464 through 70465) and modified in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79687 and 79691).[75] The final calculated CY 2020 hospital-based PHP APC geometric mean per diem cost for hospital-based PHP providers that provide 3 or more services per service day (hospital-based PHP APC 5863) is $233.52, which is an increase of 4.8 percent from $222.76 calculated last year for CY 2019 ratesetting (83 FR 58989 through 58991). The increase in the final CY 2020 calculated hospital-based PHP APC geometric mean per diem cost from the prior year is influenced by two large providers with updated cost data, whose costs per day increased. We believe that a hospital-based PHP APC geometric mean per diem cost of $233.52 supports ongoing access to hospital-based PHPs. This cost is nearly a 5 percent increase from the final CY 2019 hospital-based PHP geometric mean per diem cost.
In the CY 2020 OPPS proposed rule (84 FR 39516 to 39518), the calculated CY 2020 hospital-based PHP APC geometric mean per diem cost for hospital-based PHP providers that provide 3 or more services per service day (hospital-based PHP APC 5863) was $198.53, which was a decrease from $222.76 calculated last year for CY 2019 ratesetting (83 FR 58989 through 58991). We stated that we believe access is better supported when the geometric mean per diem cost does not fluctuate greatly. In addition, while the hospital-based PHP APC 5863 is described as providing payment for the cost of 3 or more services per day (81 FR 79680), 89 percent of hospital-based PHP paid service days in CY 2018 were for providing 4 or more services per day. To be eligible for a PHP, a patient must need at least 20 hours of therapeutic services per week, as evidenced in the patient's plan of care (42 CFR 410.43(c)(1)). To meet those patient needs, most PHP paid service days provide 4 or more services (we refer readers to Table 22.—Percentage of PHP Days by Service Unit Frequency in the proposed rule). Therefore, the hospital-based PHP APC 5863 is actually heavily weighted to the cost of providing 4 or more services. The per diem costs for hospital-based PHP APC 5863 have been calculated as $213.14, $208.09, and $222.76 for CY 2017 (81 FR 79691), CY 2018 (82 FR 59378), and CY 2019 (83 FR 58991), respectively. We noted that we do not believe that it is likely that the cost of providing hospital-based PHP services has suddenly declined when costs generally increase over time. We were concerned by this fluctuation, which we believe was influenced by data from a single large provider that had low service costs per day.
Therefore, rather than proposing the calculated CY 2020 hospital-based PHP APC geometric mean per diem cost, we instead proposed to use the CY 2020 hospital-based PHP APC geometric mean per diem cost, calculated in accordance with our existing methodology, but with a cost floor equal to the CY 2019 final geometric mean per diem cost for hospital-based PHPs of $222.76 (83 FR 58991), as the basis for developing the CY 2020 hospital-based PHP APC per diem rate. As part of this proposal, we proposed that we would use the most recent updated claims and cost data to calculate CY 2020 geometric mean per diem costs for the final rule with comment period, just as we did for CMHCs. We believe using the CY 2019 hospital-based PHP per diem cost as the floor is appropriate because it is based on very recent hospital-based PHP claims and cost data and would help to protect provider access by preventing wide fluctuation in the per diem costs for hospital-based APC 5863.
In the CY 2020 OPPS/ASC proposed rule discussion of the proposed cost floor, we also considered proposing a 3-year rolling average calculated using the final PHP geometric mean per diem costs, by provider type, from CY 2018 (82 FR 59378) and CY 2019 (83 FR 58991), and the calculated CY 2020 geometric mean per diem cost of $198.53 discussed earlier in this section for hospital-based PHPs. As discussed previously in that proposed rule, the 3-year rolling average per diem cost floor for CMHCs would have been $122.75, but the resulting rolling average per diem cost floor for hospital-based PHPs would have been $209.79. While we believe that this option would have supported access to CMHCs, as discussed previously, it could have resulted in a geometric mean per diem cost for the hospital-based PHP APC which still would have been a decrease from the hospital-based PHP APC geometric mean per diem cost of $222.76 finalized in CY 2019 (83 FR 58991). In addition, we believed that it was necessary to recalculate the hospital-based PHP geometric mean per diem cost for the final rule using updated claims and cost data; had we simply proposed to use a 3-year rolling average per diem cost floor for the hospital-based PHP APC per diem costs for CY 2020, we could not have done so. We were concerned that the 3-year rolling average per diem cost would have continued to result in a fluctuation in the cost of a hospital providing 3 or more hospital-based PHP services per day.
We believe that it is important to support access to partial hospitalization services in both CMHCs and in hospital-based PHPs, and note that hospital-based PHPs provide 80 percent of all paid PHP service days. Therefore, we believe that it was more appropriate to have proposed to use the final CY 2019 geometric mean per diem costs, by provider type, as the cost floor for use with the calculated CY 2020 PHP geometric mean per diem costs, by provider type, because those CY 2019 per diem costs are based on very recent CMHC and hospital-based PHP claims and cost data, are the easiest to understand, and would result in final geometric mean per diem costs which would help to protect provider access by preventing wide fluctuation in the per diem costs for both CMHCs and hospital-based PHPs.
While the cost floor would have protected hospital-based PHPs if the final CY 2020 calculated hospital-based PHP APC geometric mean per diem cost were still less than $222.76, the final calculated hospital-based PHP geometric mean per diem cost of $233.52 is greater than the floor, and therefore, we are finalizing this calculated CY 2020 cost for hospital-based PHPs. We believe finalizing our proposal for CY 2020 ratesetting allows us to use the most recent or very recent hospital-based PHP claims and cost reporting data while still protecting provider access. To be clear, this policy of using a cost floor is only applied for the CY 2020 ratesetting.
In the CY 2020 OPPS/ASC proposed rule, we estimated that the aggregate difference in the (prescaled) hospital-based PHP geometric mean per diem costs for CY 2020 from proposing the hospital-based PHP cost floor amount of $222.76 rather than the calculated hospital-based PHP geometric mean per diem cost of $198.53 to be $9.3 million. However, because we are finalizing the CY 2020 calculated geometric mean per diem cost for hospital-based PHPs, there is no cost difference to Medicare from using a cost floor. We refer readers to section XXVII. of this final rule for payment impacts, which are budget neutral.
We received several comments on our proposal.
Comment: Several commenters expressed concern about the decline in the number of CMHCs and hospital-based PHPs, and the effects on beneficiary access to care. Two commenters wrote that the current payment methodology has resulted in reductions in provider access rather than protection of access. Commenters noted that these declines have occurred while the need for mental health services has increased; that the demand for mental health services is on track to outpace the supply of behavioral health care providers; that as the number of PHPs declines, it may become even more difficult to calculate the appropriate per diems; and that recent changes in OPPS rulemaking related to Section 603 of the Bipartisan Budget Act of 2015 require that the per diem for new hospital-based PHP programs must be set equal to the lower CMHC rate, which they said was not viable for hospital-based PHPs and would limit the ability to create new PHP programs. A few commenters noted that decreased access to PHP services could result in increasing instances of patient recidivism and more inpatient psychiatric admissions.
Response: We appreciate the work PHPs do to care for a particularly vulnerable population with serious mental illnesses and believe that having PHPs available to beneficiaries helps prevent patient recidivism and inpatient psychiatric admissions. We share the commenters' concerns about the decline in the number of PHPs and the effect on access. Our goal is to protect access to both provider types, so beneficiaries have choices regarding where to receive treatment. We also refer readers to section VIII.B.2.a. for a similar comment and response related to CMHCs.
Regarding the effects of Section 603 of the Bipartisan Budget Act of 2015 [76] on hospital-based PHP access, we note that this provision amended the statute at section 1833(t) of the Act to require that certain items and services furnished in certain off-campus provider-based departments (PBDs) shall not be considered covered outpatient department services for purposes of OPPS, and payment for those nonexcepted items and services shall be made “under the applicable payment system” beginning January 1, 2017 (81 FR 79720).
These amendments do not prevent hospitals from creating new PHP programs. Instead, they provide that certain items and services are no longer covered OPD services payable under the OPPS, and instead must be paid under another “applicable payment system.” CMS adopted the Medicare Physician Fee Schedule (MPFS) as the applicable payment system for these services (81 FR 79717). Although, nonexcepted off-campus provider-based departments are no longer paid under the OPPS and payments may be lower for these departments, the section 603 changes do not prohibit these departments from creating PHP programs. Excepted off-campus provider-based departments and the main campuses of hospitals continue to be paid under the OPPS, so it is unclear for these locations why entities could not create new PHPs.
Commenters were incorrect in stating that new hospital-based PHPs are paid at the CMHC per diem rate. Only non-excepted off-campus PHPs are paid through the MPFS at the CMHC rate; new hospital-based PHPs that are on-campus are paid at the hospital-based PHP per diem rate under the OPPS.
We believe that paying non-excepted off-campus PHPs through the MPFS at the CMHC APC rate is appropriate. We note that the clinical services, staffing, and documentation requirements are similar for CMHCs and hospital-based PHPs. As discussed in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79717), when a beneficiary receives services in an off-campus department of a hospital (such as in a hospital-based PHP), the Medicare payment is generally higher than when those same services are provided in a physician's office. Similarly, when partial hospitalization services are provided in a hospital-based PHP, Medicare pays more than when those same services are provided by a CMHC. CMHCs are freestanding providers that are not part of a hospital, and that have lower cost structures than hospital-based PHPs. This is similar to the differences between freestanding entities paid under the MPFS that furnish other services also provided by hospital-based entities. We believe that paying for non-excepted hospital-based partial hospitalization services at the lower CMHC per diem rate is in alignment with section 603 amendments to the OPPS statute, while also protecting access to the PHP benefit.
Furthermore, we note that our policy of paying non-excepted off-campus PHPs at the CMHC APC 5853 per diem rate provides some relief to those off-campus PHPs since non-PHP mental health services provided by non-excepted off-campus hospital provider departments are paid through the MPFS at 40 percent of the OPPS APC amount for the same service. Paying non-excepted off-campus hospital-based PHPs at the CY 2020 CMHC APC 5853 payment rate results in a payment that is 52 percent of the CY 2020 APC 5863 OPPS payment rate for hospital-based PHPs. The final FY 2020 payment rates for PHP APCs 5853 and 5863 are in Addendum A to this final rule with comment period, which is available in the FY 2020 OPPS/ASC final rule supporting documents found on our website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices.html.
Comment: One commenter suggested that CMS base PHP reimbursement on incentives determined by documented productivity results. This commenter suggested we consider Measurement-based Care and Patient Satisfaction.
Response: We believe “measurement-based care” that the commenter cited refers to administering a standardized instrument to measure some aspect of patient symptoms when he or she begins and ends receiving PHP services. This type of measure could inform clinical decision-making and quality improvement activities at minimum, but results could theoretically be used to adjust payment. We also believe that the commenter is asking if CMS could administer patient satisfaction surveys (like HCAHPS) and then reward high-performing PHPs.
Currently, there is no statutory language explicitly authorizing an incentive payment methodology based on productivity results or patient satisfaction for CMHCs or for outpatient hospital-based PHPs. We responded to a similar public comment in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70462) and refer readers to a summary of that comment and our response. To reiterate, sections 1833(t)(2) and 1833(t)(9) of the Act set forth the requirements for establishing and adjusting OPPS payment rates, which are based on costs, and which include PHP payment rates. We note that section 1833(t)(17) of the Act authorizes the Hospital Outpatient Quality Reporting (OQR) Program, which applies a payment reduction to subsection (d) hospitals that fail to meet program requirements; as finalized in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59109 to 59110), this payment reduction applies to HCPCS codes which include PHP services. In the CY 2015 OPPS/ASC proposed rule (79 FR 41040), we considered future inclusion of, and requested comments on, the following quality measures addressing PHP issues that would apply in the hospital outpatient setting: (1) 30-Day Readmission; (2) Group Therapy; and (3) No Individual Therapy. We also refer readers to the CY 2015 OPPS/ASC final rule with comment period (79 FR 66957 through 66958) for a discussion of the comments received and of PHP measures considered for inclusion in the Hospital OQR Program in future years.
Comment: Several commenters recommended that more work be done to establish PHP rates accurately, that CMS reconsider its PHP policy positions to determine how to rebuild PHP services, or that CMS establish a task force to review and discuss the availability of PHPs for Medicare beneficiaries.
Response: We will continue to explore policy options for strengthening the PHP benefit and increasing access to the valuable services provided by CMHCs as well as by hospital-based PHPs. As part of that process, we regularly review our methodology to ensure that it is appropriately capturing the cost of care reported by providers. For example, for the CY 2016 ratesetting, we extensively reviewed the methodology used for PHP ratesetting. In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70462 through 70466), we also included a detailed description of the ratesetting process to help all PHP providers record costs correctly so that we can more fully capture PHP costs in ratesetting. In this CY 2020 ratesetting, we proposed to calculate the CY 2020 per diem costs with a cost floor. We believe that proposal helped support access, particularly for CMHCs, whose calculated costs were still below the cost floor when we ran the calculations with updated data for this final rule with comment period.
We also recognize that as the number of providers decreases, the ratesetting calculations can be more strongly influenced by the costs of large providers. We are regularly evaluating our rate setting methodology to ensure that it is as accurate as possible, and captures provider cost data fully. However, our rate setting methodology must comply with requirements given in statute at 1833(t)(2) and 1833(t)(9), and depends heavily on provider-reported costs. We remind hospital-based PHPs that they are required to record PHP costs in cost center line 9399 (“Partial Hospitalization Program”), which was added to the cost report in response to commenters in prior OPPS rulemaking (81 FR 79691); this line is the primary source of the department-level CCR used for hospital-based PHP ratesetting in the Revenue Code to Cost Center crosswalk. Line 9399 should not mix other non-PHP mental health service costs with PHP costs. PHP costs incorrectly recorded in other cost centers may not be included for PHP rate setting, thereby affecting the hospital-based PHP per diem cost amount.
We maintain positive working relationships with various industry leaders representing both CMHCs and hospital-based PHP providers with whom we have consistently met over the years to discuss industry concerns and ideas. These relationships have provided significant and valued input regarding PHP ratesetting. We also hold Hospital Outpatient Open Door Forum calls monthly, in which all individuals are welcome to participate and/or submit questions regarding specific issues, including questions related to PHPs. Furthermore, we initiate rulemaking annually, through which we receive public comments on proposals set forth in a proposed rule and respond to those comments in a final rule. All individuals are provided an opportunity to comment, and we give consideration to each comment that we receive. Given the relationships that we have established with various industry leaders and the various means for us to receive comments and recommendations, we believe that we receive adequate input regarding ratesetting and take that input into consideration when establishing the payment rates. We continue to welcome any input and information that the public is willing to provide.
We refer readers to section VIII.B.2.a. for a similar comment and response related to CMHCs.
After consideration of the comments, we are finalizing our proposal as proposed. Because the final CY 2020 calculated hospital-based PHP geometric mean per diem cost of $233.52 is greater than the cost floor amount of $222.76, the final CY 2020 hospital-based PHP geometric mean per diem cost is $233.52.
In summary, for CY 2020, we are finalizing our proposal to use the calculated CY 2020 CMHC geometric mean per diem cost and the calculated CY 2020 hospital-based PHP geometric mean per diem cost, each calculated in accordance with our existing methodology, but with a cost floor equal to the CY 2019 final geometric mean per diem costs as the basis for developing the CY 2020 PHP APC per diem rates, as proposed. Because the final CY 2020 calculated geometric mean per diem cost for CMHCs is less than the cost floor amount of $121.62, we are finalizing a CY 2020 geometric mean per diem cost for CMHCs of $121.62. In addition, because the CY 2020 final calculated hospital-based PHP geometric mean per diem cost is greater than the hospital-based PHP cost floor amount of $222.76, we are finalizing the final calculated CY 2020 hospital-based PHP geometric mean per diem cost of $233.52. In this final rule with comment period, we used the most recent updated claims and cost data to calculate CY 2020 geometric mean per diem costs. The inclusion of a cost floor, which is based on very recent data, protected CMHCs as their final calculated per diem cost was still less than the cost floor amount, but was not needed for hospital-based PHPs.
These final CY 2020 PHP geometric mean per diem costs are shown in Table 45, and are used to derive the final CY 2020 PHP APC per diem rates for CMHCs and hospital-based PHPs. The final CY 2020 PHP APC per diem rates are included in Addendum A to this final rule with comment period (which is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices.html).[77]

3. PHP Service Utilization Updates
a. Provision of Individual Therapy
In the CY 2016 OPPS/ASC final rule with comment period (81 FR 79684 through 79685), we expressed concern over the low frequency of individual therapy provided to beneficiaries. The CY 2018 claims data used for this CY 2020 final rule with comment period revealed some changes in the provision of individual therapy compared to CY 2015, CY 2016, and CY 2017 claims data as shown in the Table 46.

As shown in Table 46A, the CY 2018 claims show that both CMHCs and hospital-based PHPs have slightly increased the provision of individual therapy on days with 4 or more services, compared to CY 2017 claims. However, on days with 3 services, CMHCs and hospital-based PHPs both decreased the provision of individual therapy compared to prior years.
b. Provision of 3-Service Days
In the CY 2018 OPPS/ASC proposed rule and final rule with comment period (82 FR 33640 and 82 FR 59378), we stated that we are aware that our single-tier payment policy may influence a change in service provision because providers are able to obtain payment that is heavily weighted to the cost of providing four or more services when they provide only 3 services. We indicated that we are interested in ensuring that providers furnish an appropriate number of services to beneficiaries enrolled in PHPs. Therefore, with the CY 2017 implementation of CMHC APC 5853 and hospital-based PHP APC 5863 for providing 3 or more PHP services per day, we are continuing to monitor utilization of days with only 3 PHP services.
For this CY 2020 OPPS/ASC final rule with comment period, we used the CY 2018 claims data. Table 46A shows the utilization findings based on the final claims data.

As shown in Table 46A, the CY 2018 claims data used for this final rule with comment period show that utilization of 3 service days is increasing compared to the 3 prior claim years. Compared to CY 2017, in CY 2018 hospital-based PHPs provided more days with 3 services only, more days with 4 services only, and fewer days with 5 or more services. Compared to CY 2017, in CY 2018 CMHCs provided more days with 3 services, fewer days with 4 services, and more days with 5 or more services.
The CY 2017 data are the first year of claims data to reflect the change to the single-tier PHP APCs. We hope the increase in the percentage of days with 3 services is simply an anomaly rather than the start of a trend, but more data will be needed to make that determination. As we noted in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79685), we will continue to monitor the provision of days with only 3 services, particularly now that the single-tier PHP APCs 5853 and 5863 are established for providing 3 or more services per day for CMHCs and hospital-based PHPs, respectively.
It is important to reiterate our expectation that days with only 3 services are meant to be an exception and not the typical PHP day. In the CY 2009 OPPS/ASC final rule with comment period (73 FR 68694), we clearly stated that we consider the acceptable minimum units of PHP services required in a PHP day to be 3 and explained that it was never our intention that 3 units of service represent the number of services to be provided in a typical PHP day. PHP is furnished in lieu of inpatient psychiatric hospitalization and is intended to be more intensive than a half-day program. We further indicated that a typical PHP day should generally consist of 5 to 6 units of service (73 FR 68689). We explained that days with only 3 units of services may be appropriate to bill in certain limited circumstances, such as when a patient might need to leave early for a medical appointment and, therefore, would be unable to complete a full day of PHP treatment. At that time, we noted that if a PHP were to only provide days with 3 services, it would be difficult for patients to meet the eligibility requirement in 42 CFR 410.43(c)(1) that patients must require a minimum of 20 hours per week of therapeutic services as evidenced in their plan of care (73 FR 68689).
We received 2 comments related to PHP utilization.
Comment: Two commenters noted that the data in Table 22 of the proposed rule demonstrate commitment by PHPs to comply with and exceed the 20-hour rule. These commenters noted that the vast majority of claim days for CMHCs and hospital-based PHPs have 4 or more services provided. The commenters noted that PHPs are voluntary, and that they cannot force patients to attend every day. They also noted that the typical patient profile includes behaviors that work against attendance and full daily participation. In addition, the commenters wrote that there are other challenges to providing 20 hours of services per week that are beyond providers' control, such as holidays, weather, and other medical appointments.
Response: We appreciate that most PHP days include 4 or more services being provided, but the updated data for this final rule showed an uptick in the percentage of 3-service days. We will continue to monitor the data over time.
The “20-hour rule” the commenters mentioned is from our regulations at 42 CFR 410.43(c) (discussed at 73 FR 68694 to 68695), which require that eligible PHP patients need at least 20 hours of therapeutic services per week, as evidenced in their plan of care. PHPs are intended to be intensive programs that are provided in lieu of inpatient hospitalization. We appreciate the efforts providers have made to increase beneficiary attendance, and also recognize the provider concerns about circumstances beyond their control which can affect the number of hours of services provided each week. We did not make any proposals related to the 20-hour requirement, and are continuing to monitor the claims data regarding the hours per week of services provided, sending providers informational messaging without affecting payment.
C. Outlier Policy for CMHCs
In this CY 2020 OPPS/ASC final rule with comment period, for CY 2020, we are finalizing to continue to calculate the CMHC outlier percentage, cutoff point and percentage payment amount, outlier reconciliation, outlier payment cap, and fixed-dollar threshold according to previously established policies. These topics are discussed in more detail. We refer readers to section II.G. of the CY 2020 OPPS/ASC proposed rule for our general policies for hospital outpatient outlier payments (84 CFR 39434 through 39435.
1. Background
As discussed in the CY 2004 OPPS final rule with comment period (68 FR 63469 through 63470), we noted a significant difference in the amount of outlier payments made to hospitals and CMHCs for PHP services. Given the difference in PHP charges between hospitals and CMHCs, we did not believe it was appropriate to make outlier payments to CMHCs using the outlier percentage target amount and threshold established for hospitals. Therefore, beginning in CY 2004, we created a separate outlier policy specific to the estimated costs and OPPS payments provided to CMHCs. We designated a portion of the estimated OPPS outlier threshold specifically for CMHCs, consistent with the percentage of projected payments to CMHCs under the OPPS each year, excluding outlier payments, and established a separate outlier threshold for CMHCs. This separate outlier threshold for CMHCs resulted in $1.8 million in outlier payments to CMHCs in CY 2004 and $0.5 million in outlier payments to CMHCs in CY 2005 (82 FR 59381). In contrast, in CY 2003, more than $30 million was paid to CMHCs in outlier payments (82 FR 59381).
2. CMHC Outlier Percentage
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59267 through 59268), we described the current outlier policy for hospital outpatient payments and CMHCs. We note that we also discussed our outlier policy for CMHCs in more detail in section VIII. C. of that same final rule (82 FR 59381). We set our projected target for all OPPS aggregate outlier payments at 1.0 percent of the estimated aggregate total payments under the OPPS (82 FR 59267). This same policy was also reiterated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58996). We estimate CMHC per diem payments and outlier payments by using the most recent available utilization and charges from CMHC claims, updated CCRs, and the updated payment rate for APC 5853. For increased transparency, we are providing a more detailed explanation of the existing calculation process for determining the CMHC outlier percentages. As previously stated, we proposed to continue to calculate the CMHC outlier percentage according to previously established policies, and we did not propose any changes to our current methodology for calculating the CMHC outlier percentage for CY 2020. To calculate the CMHC outlier percentage, we followed three steps:
- Step 1: We multiplied the OPPS outlier threshold, which is 1.0 percent, by the total estimated OPPS Medicare payments (before outliers) for the prospective year to calculate the estimated total OPPS outlier payments:
(0.01 × Estimated Total OPPS Payments) = Estimated Total OPPS Outlier Payments.
- Step 2: We estimated CMHC outlier payments by taking each provider's estimated costs (based on their allowable charges multiplied by the provider's CCR) minus each provider's estimated CMHC outlier multiplier threshold (we refer readers to section VIII.C.3. of this final rule with comment period). That threshold is determined by multiplying the provider's estimated paid days by 3.4 times the CMHC PHP APC payment rate. If the provider's costs exceeded the threshold, we multiplied that excess by 50 percent, as described in section VIII.C.3. of this final rule with comment period, to determine the estimated outlier payments for that provider. CMHC outlier payments are capped at 8 percent of the provider's estimated total per diem payments (including the beneficiary's copayment), as described in section VIII.C.5. of this final rule with comment period, so any provider's costs that exceed the CMHC outlier cap will have its payments adjusted downward. After accounting for the CMHC outlier cap, we summed all of the estimated outlier payments to determine the estimated total CMHC outlier payments.
(Each Provider's Estimated Costs—Each Provider's Estimated Multiplier Threshold) = A. If A is greater than 0, then (A × 0.50) = Estimated CMHC Outlier Payment (before cap) = B. If B is greater than (0.08 × Provider's Total Estimated Per Diem Payments), then cap-adjusted B = (0.08 × Provider's Total Estimated Per Diem Payments); otherwise, B = B. Sum (B or cap-adjusted B) for Each Provider = Total CMHC Outlier Payments.
- Step 3: We determined the percentage of all OPPS outlier payments that CMHCs represent by dividing the estimated CMHC outlier payments from Step 2 by the total OPPS outlier payments from Step 1:
(Estimated CMHC Outlier Payments/Total OPPS Outlier Payments).
In CY 2019, we designated approximately 0.01 percent of that estimated 1.0 percent hospital outpatient outlier threshold for CMHCs (83 FR 58996), based on this methodology. In the CY 2020 proposed rule (84 FR 39521), we proposed to continue to use the same methodology for CY 2020. Therefore, based on our CY 2020 payment estimates, CMHCs are projected to receive 0.02 percent of total hospital outpatient payments in CY 2020, excluding outlier payments. We proposed to designate approximately less than 0.01 percent of the estimated 1.0 percent hospital outpatient outlier threshold for CMHCs. This percentage is based upon the formula given in Step 3.
CMS did not receive any comments on the CMHC outlier percentage, so we are finalizing the proposal as proposed.
3. Cutoff Point and Percentage Payment Amount
As described in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59381), our policy has been to pay CMHCs for outliers if the estimated cost of the day exceeds a cutoff point. In CY 2006, we set the cutoff point for outlier payments at 3.4 times the highest CMHC PHP APC payment rate implemented for that calendar year (70 FR 68551). For CY 2018, the highest CMHC PHP APC payment rate is the payment rate for CMHC PHP APC 5853. In addition, in CY 2002, the final OPPS outlier payment percentage for costs above the multiplier threshold was set at 50 percent (66 FR 59889). In CY 2018, we continued to apply the same 50 percent outlier payment percentage that applies to hospitals to CMHCs and continued to use the existing cutoff point (82 FR 59381). Therefore, for CY 2018, we continued to pay for partial hospitalization services that exceeded 3.4 times the CMHC PHP APC payment rate at 50 percent of the amount of CMHC PHP APC geometric mean per diem costs over the cutoff point. For example, for CY 2018, if a CMHC's cost for partial hospitalization services paid under CMHC PHP APC 5853 exceeds 3.4 times the CY 2018 payment rate for CMHC PHP APC 5853, the outlier payment would be calculated as 50 percent of the amount by which the cost exceeds 3.4 times the CY 2018 payment rate for CMHC PHP APC 5853 [0.50 × (CMHC Cost−(3.4 × APC 5853 rate))]. This same policy was also reiterated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58996 through 58997).
In the CY 2020 OPPS/ASC proposed rule (84 FR 39521), in accordance with our existing policy, we proposed to continue to pay for partial hospitalization services that exceed 3.4 times the proposed CMHC PHP APC payment rate at 50 percent of the CMHC PHP APC geometric mean per diem costs over the cutoff point. That is, for CY 2020, if a CMHC's cost for partial hospitalization services paid under CMHC PHP APC 5853 exceeds 3.4 times the payment rate for CMHC APC 5853, the outlier payment will be calculated as [0.50 × (CMHC Cost−(3.4 × APC 5853 rate))].
CMS did not receive comments on the Cutoff Point and Percentage Payment Amount, so we are finalizing our proposal as proposed.
4. Outlier Reconciliation
In the CY 2009 OPPS/ASC final rule with comment period (73 FR 68594 through 68599), we established an outlier reconciliation policy to address charging aberrations related to OPPS outlier payments. We addressed vulnerabilities in the OPPS outlier payment system that lead to differences between billed charges and charges included in the overall CCR, which are used to estimate cost and would apply to all hospitals and CMHCs paid under the OPPS. CMS initiated steps to ensure that outlier payments appropriately account for the financial risk when providing an extraordinarily costly and complex service, but are only being made for services that legitimately qualify for the additional payment.
For a comprehensive description of outlier reconciliation, we refer readers to the CY 2019 OPPS/ASC final rules with comment period (83 FR 58874 through 58875 and 81 FR 79678 through 79680).
In the CY 2020 OPPS/ASC proposed rule, we proposed to continue these policies for partial hospitalization services provided through PHPs for CY 2020. The current outlier reconciliation policy requires that providers whose outlier payments meet a specified threshold (currently $500,000 for hospitals and any outlier payments for CMHCs) and whose overall ancillary CCRs change by plus or minus 10 percentage points or more, are subject to outlier reconciliation, pending approval of the CMS Central Office and Regional Office (73 FR 68596 through 68599). The policy also includes provisions related to CCRs and to calculating the time value of money for reconciled outlier payments due to or due from Medicare, as detailed in the CY 2009 OPPS/ASC final rule with comment period and in the Medicare Claims Processing Manual (73 FR 68595 through 68599 and Medicare Claims Processing Internet Only Manual, Chapter 4, Section 10.7.2 and its subsections, available online at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c04.pdf).
CMS did not receive comments on the Outlier Reconciliation Policy, so we are finalizing our proposal as proposed.
5. Outlier Payment Cap
In the CY 2017 OPPS/ASC final rule with comment period, we implemented a CMHC outlier payment cap to be applied at the provider level, such that in any given year, an individual CMHC will receive no more than a set percentage of its CMHC total per diem payments in outlier payments (81 FR 79692 through 79695). We finalized the CMHC outlier payment cap to be set at 8 percent of the CMHC's total per diem payments (81 FR 79694 through 79695). This outlier payment cap only affects CMHCs, it does not affect other provider types (that is, hospital-based PHPs), and is in addition to and separate from the current outlier policy and reconciliation policy in effect. For CY 2019, we continued this policy in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58997).
For CY 2020 and subsequent years, we proposed to continue to apply the 8 percent CMHC outlier payment cap to the CMHC's total per diem payments (84 FR 39522).
CMS did not receive comments on the CMHC outlier payment cap, so we are finalizing our proposal as proposed.
6. Fixed-Dollar Threshold
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59267 through 59268), for the hospital outpatient outlier payment policy, we set a fixed-dollar threshold in addition to an APC multiplier threshold. Fixed-dollar thresholds are typically used to drive outlier payments for very costly items or services, such as cardiac pacemaker insertions. CMHC PHP APC 5853 is the only APC for which CMHCs may receive payment under the OPPS, and is for providing a defined set of services that are relatively low cost when compared to other OPPS services. Because of the relatively low cost of CMHC services that are used to comprise the structure of CMHC PHP APC 5853, it is not necessary to also impose a fixed-dollar threshold on CMHCs. Therefore, in the CY 2018 OPPS/ASC final rule with comment period, we did not set a fixed-dollar threshold for CMHC outlier payments (82 FR 59381). This same policy was also reiterated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58996 through 58997.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39522), we proposed to continue this policy for CY 2020. CMS did not receive any comments on the fixed-dollar threshold, so we are finalizing our proposal as proposed.
D. Update to PHP Allowable HCPCS Codes
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 58997 through 58998), we discussed that, during the CY 2019 rulemaking, we received the Category I and III CPT codes from the AMA that were new, revised, and deleted, effective January 1, 2019. This included the deleting of the following psychological and neuropsychological testing CPT codes, which affect PHPs, as of January 1, 2019:
- CPT code 96101 (Psychological testing by psychologist/physician);
- CPT code 96102 (Psychological testing by technician);
- CPT code 96103 (Psychological testing administered by computer);
- CPT code 96118 (Neuropsychological testing by psychologist/physician)
- CPT code 96119 (Neuropsychological testing by technician); and
- CPT code 96120 (Neuropsychological test administered w/computer).
In addition, the AMA added the following psychological and neuropsychological testing CPT codes to replace the deleted codes, as of January 1, 2019:
- CPT code 96130 (Psychological testing evaluation by physician/qualified health care professional; first hour);
- CPT code 93131 (Psychological testing evaluation by physician/qualified health care professional; each additional hour);
- CPT code 96132 (Neuropsychological testing evaluation by physician/qualified health care professional; first hour);
- CPT code 96133 (Neuropsychological testing evaluation by physician/qualified health care professional; each additional hour);
- CPT code 96136 (Psychological/neuropsychological testing by physician/qualified health care professional; first 30 minutes);
- CPT code 96137 (Psychological/neuropsychological testing by physician/qualified health care professional; each additional 30 minutes);
- CPT code 96138 (Psychological/neuropsychological testing by technician; first 30 minutes);
- CPT code 96139 (Psychological/neuropsychological testing by technician; each additional 30 minutes); and
- CPT code 96146 (Psychological/neuropsychological testing; automated result only).
As we proposed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 58997 through 58998), we included these replacement codes in Addenda B and O. As is our usual practice for including new and revised Category I and III CPT codes under the OPPS, we included interim APC assignments and status indicators for these codes and provided an opportunity under the OPPS for the public to comment on these interim assignments. That is, we included comment indicator “NP” to indicate that the code is new for the next calendar year or the code is an existing code with substantial revision to its code descriptor in the next calendar year as compared to current calendar year with a proposed APC assignment, and that comments will be accepted on the proposed APC and status indicator assignments.
While these interim APC and status indicator assignments under the OPPS were included in Addendum B and Addendum O to the CY 2019 OPPS/ASC proposed rule and final rule with comment period, PHP providers may not have been aware of those changes because we did not also include these in the PHP discussion presented in the proposed rule; to be clear, PHP is a part of the OPPS. To ensure that PHP providers were aware of the new and replacement codes related to CMHC and hospital-based partial hospitalization programs and had the opportunity to comment on the changes, we utilized a practice similar to the one we use under the OPPS for new Level II HCPCS codes that become effective after the proposed rule is published. Therefore, in the CY 2019 OPPS/ASC final rule with comment period, we proposed to delete the same 6 CPT codes listed from the PHP-allowable code set for CMHC APC 5853 and hospital-based PHP APC 5863, and replace them with 9 new CPT codes as shown in Table 47 of the final rule with comment period, effective January 1, 2019. We also refer readers to section III.A.4. of the proposed rule for a detailed discussion of how we include new and revised Category I and III CPT codes for a related calendar year, assign interim APC and status indicator assignments, and allow for public comments on these interim assignments for finalization in the next calendar year final rule with comment period.
We solicited public comments on these proposals and since we did not receive any comments, we are finalizing our proposals as proposed.
IX. Procedures That Will Be Paid Only as Inpatient Procedures
A. Background
We refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74352 through 74353) for a full historical discussion of our longstanding policies on how we identify procedures that are typically provided only in an inpatient setting (referred to as the inpatient only (IPO) list) and, therefore, will not be paid by Medicare under the OPPS, and on the criteria that we use to review the IPO list each year to determine whether or not any procedures should be removed from the list. The complete list of codes that describe procedures that will be paid by Medicare in CY 2020 as inpatient only procedures is included as Addendum E to this CY 2020 OPPS/ASC final rule with comment period, which is available via the internet on the CMS website.
B. Changes to the Inpatient Only (IPO) List
1. Methodology for Identifying Appropriate Changes to IPO List
In the CY 2019 OPPS/ASC proposed rule (84 FR 39523 through 39525), for CY 2020, we proposed to use the same methodology (described in the November 15, 2004 final rule with comment period (69 FR 65834)) of reviewing the current list of procedures on the IPO list to identify any procedures that may be removed from the list. We have established five criteria that are part of this methodology. As noted in the CY 2012 OPPS/ASC final rule with comment period (76 FR 74353), we utilize these criteria when reviewing procedures to determine whether or not they should be removed from the IPO list and assigned to an APC group for payment under the OPPS when provided in the hospital outpatient setting. We note that a procedure is not required to meet all of the established criteria to be removed from the IPO list. The criteria include the following:
- Most outpatient departments are equipped to provide the services to the Medicare population.
- The simplest procedure described by the code may be performed in most outpatient departments.
- The procedure is related to codes that we have already removed from the IPO list.
- A determination is made that the procedure is being performed in numerous hospitals on an outpatient basis.
- A determination is made that the procedure can be appropriately and safely performed in an ASC and is on the list of approved ASC procedures or has been proposed by us for addition to the ASC list.
2. Procedures Proposed for Removal From the IPO List
Using the listed criteria, for the CY 2020 OPPS/ASC proposed rule, we identified one procedure described by CPT code 27130 (Arthroplasty, acetabular and proximal femoral prosthetic replacement (total hip arthroplasty) with or without autograft or allograft) that met the criteria for proposed removal from the IPO list. The procedure that we proposed to remove from the IPO list for CY 2020 and subsequent years, including the CPT/HCPCS code, long descriptor, and the proposed CY 2020 payment indicator was displayed in Table 23 of the proposed rule.
For a number of years, total hip arthroplasty (THA) has been a topic of discussion for removal from the IPO list with both stakeholder support and opposition. Most recently, in the CY 2018 OPPS/ASC proposed rule (82 FR 33644 and 33645), we sought public comment on the possible removal of partial hip arthroplasty (PHA), CPT code 27125 (Hemiarthroplasty, hip, partial (for example, femoral stem prosthesis, bipolar arthroplasty)), and total hip arthroplasty (THA) or total hip replacement, CPT code 27130 (Arthroplasty, acetabular and proximal femoral prosthetic replacement (total hip arthroplasty), with or without autograft or allograft from the IPO list. Both THA and PHA were placed on the original IPO list in the CY 2001 OPPS/ASC final rule with comment period (65 FR 18780).
Among those commenters expressing support in response to the CY 2018 OPPS/ASC proposed rule (which we summarized and responded to in the CY 2018 OPPS/ASC final rule with comment period (82 FR 52527 through 52528)) for removal of THA from the IPO list were several surgeons and other stakeholders who believed that, given thorough preoperative screening by medical teams with significant experience and expertise involving hip replacement procedures, the THA procedure could be provided on an outpatient basis for some Medicare beneficiaries. These commenters noted significant success involving same day discharge for patients who met the screening criteria and whose experienced medical teams were able to perform the procedure early enough in the day for the patients to achieve postoperative goals, allowing home discharge by the end of the day. The commenters believed that the benefits of providing the THA procedure on an outpatient basis include significant enhancements in patient well-being, improved efficiency, and cost savings to the Medicare program, including shorter hospital stays resulting in fewer medical complications, improved results, and enhanced patient satisfaction.
We stated in the CY 2018 OPPS/ASC proposed rule that, like most surgical procedures, both PHA and THA need to be tailored to the individual patient's needs. Patients with a relatively low anesthesia risk and without significant comorbidities who have family members at home who can assist them may likely be good candidates for an outpatient PHA or THA procedure. These patients may also be able to tolerate outpatient rehabilitation in either an outpatient facility or at home postsurgery. On the other hand, patients with multiple medical comorbidities, aside from their osteoarthritis, would more likely require inpatient hospitalization and possibly postacute care in a skilled nursing facility or other facility. Surgeons who discussed outpatient PHA and THA procedures in public comments in response to our CY 2017 OPPS/ASC proposed rule (81 FR 45679) comment solicitation (which we summarized and responded to in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79696)) on the TKA procedure emphasized the importance of careful patient selection and strict protocols to optimize outpatient hip replacement outcomes. These protocols typically manage all aspects of the patient's care, including the at-home preoperative and postoperative environment, anesthesia, pain management, and rehabilitation to maximize rapid recovery, ambulation, and performance of activities of daily living.
Numerous commenters representing a variety of stakeholders, including physicians and other care providers, individual stakeholders, specialty societies, hospital associations, hospital systems, ASCs, device manufacturers, and beneficiaries, responded to our solicitation of comments regarding the removal of PHA and THA from the IPO list (which we summarized and responded to in CY 2018 OPPS/ASC final rule with comment period (82 FR 52527 through 52528)). The comments were diverse and some were similar to the comments we received on our proposal to remove TKA from the IPO list. Some commenters, including hospital systems and associations, as well as specialty societies and physicians, stated that it would not be clinically appropriate to remove PHA and THA from the IPO list, indicating that the patient safety profile of outpatient THA and PHA in the non-Medicare population is not well-established. Commenters representing orthopedic surgeons also stated that patients requiring a hemiarthroplasty (PHA) for fragility fractures are, by nature, a higher risk, suffer more extensive comorbidities, and require closer monitoring and preoperative optimization; therefore, it would not be medically appropriate to remove the PHA procedure from the IPO list.
Other commenters, including ambulatory surgery centers (ASCs), physicians, and beneficiaries, supported the removal of PHA and THA from the IPO list. These commenters stated that the procedures were appropriate for certain Medicare beneficiaries and most outpatient departments are equipped to provide THA to some Medicare beneficiaries. They also referenced their own personal successful experiences with outpatient THA.
a. Removal of Total Hip Arthroplasty From the Inpatient Only List
After reviewing the clinical characteristics of the procedure described by CPT code 27130, considering the public comments described earlier from past rules, additional feedback from stakeholders, and with further consultation with our clinical advisors regarding this procedure, in the CY 2020 OPPS/ASC proposed rule (84 FR 39524), we stated our belief that this procedure meets criterion 2 (the simplest procedure described by the code may be performed in most outpatient departments) and criterion 3 (the procedure is related to codes that we have already removed from the IPO list). As such, we believe that appropriately selected patients could have this procedure performed on an outpatient basis. Therefore, we proposed to remove THA from the IPO list and to assign the THA procedure (CPT code 27130) to C-APC 5115 with status indicator “J1”. We sought public comments on our conclusion that the procedure described by CPT code 27130 meets criteria 2 and 3 and our proposal to assign the procedure to C-APC 5115 with status indicator “J1”. We did not propose to remove PHA from the IPO list because we continue to believe that it does not meet the criteria for removal.
Comment: In response to our proposal to remove CPT code 27130 from the IPO list, we received many of the same type of comments that we received in response to our CY 2018 proposed rule comment solicitation for removing THA. Many commenters, including health care providers and medical associations, supported the proposal. The commenters recognized that with careful, appropriate selection, THA could be performed in the outpatient setting with few to no complications. One commenter, an orthopaedic specialty society, agreed with the patient selection characteristics that were noted in the proposed rule—namely, that good candidates for outpatient THA have relatively low anesthesia risk, do not have significant comorbidities, have in-home support, and are able to tolerate post-surgical outpatient rehabilitation in either an outpatient facility or in the home.
One commenter suggested that a patient that requires a revision of a prior hip replacement, and/or has other complicating clinical conditions, including multiple co-morbidities such as obesity, diabetes, heart disease, is not a strong candidate for outpatient THA and should be scheduled for an inpatient stay. Furthermore, another commenter stated that the following social factors should be considered when analyzing the implications of outpatient THA: Living alone, pain, prior hospitalization, depression, functional status, high-risk medication, and health literacy. Additionally, both supporters and opponents requested that CMS provide detailed guidance on what those selection criteria should look like.
Some commenters did not support the proposal, citing both clinical and operational concerns based on their experience with the removal of TKA from the IPO in 2018. Those commenters believe that it would be hasty to remove THA without waiting for providers and MACs to have a better handle on performing TKA in the outpatient setting and developing better skill at performing appropriate patient selection. One commenter suggested delaying the removal of THA from the IPO list for a year, until CMS could provide greater evidence, specifically, a rigorous medical literature review, that THA could be performed safely in the outpatient or ASC setting, especially for beneficiaries with multiple co-morbidities.
Some commenters, including two major orthopaedic associations, raised concerns about whether the THA procedure meets the criteria required to be removed from the IPO list. One commenter, an orthopaedic surgery specialty society for hips and knees, shared that they do not believe THA meets criterion 2 (the simplest procedure described by the code may be performed in most outpatient departments)—they argued that there is no such thing as a simple THA and that all procedures described by CPT code 27130 have moderate risks for complications. The commenter further argues that criterion 3 (the procedure is related to codes that we have already removed from the IPO list) is also not met since they do not believe that THA and TKA are similar, except for the risks associated with each in moving the site of surgery. The commenter expressed additional concerns regarding criterion 4 (a determination is made that the procedure is being performed in numerous hospitals on an outpatient basis) and the lack of peer-reviewed literature that would provide supportive data. Finally, the commenter expressed concerns regarding criterion 5 (a determination is made that the procedure can be appropriately and safely performed in an ASC and is on the list of approved ASC procedures or has been proposed by us for addition to the ASC list), stating that there is a lack of peer-reviewed literature and the ability to guarantee excellent patient selection and education, tailored anesthetic techniques, well-done surgery, good medical care, and exceptional post-operative care coordination in the ASC setting. The commenter conceded that performance of THA in the outpatient setting is possible, but does not believe that data and guidance on appropriate patient selection and education, patient-specific anesthetic techniques, and post-operative care coordination are well demonstrated in peer-reviewed literature. This commenter did note that appropriate patient selection for outpatient THA candidates could mitigate some of its concerns.
Another orthopaedic surgery specialty society called the removal of THA from the IPO list “rash,” and expressed extensive concern that CMS would remove a procedure from the IPO list based on only two of the five criteria used to determine appropriate removals for the IPO list. The commenter further expressed concern that the rationale behind removing THA from the IPO list—specifically that CMS believes it meets criteria 2 and 3—fails to consider whether or not outpatient facilities are equipped and appropriate for outpatient THA, and whether or not THA is performed safely in outpatient settings a majority of the time.
Response: We thank commenters for providing public comments on the appropriateness of removing THA from the IPO list and providing it in outpatient settings. We appreciate the support for the proposal. We also recognize concerns for ensuring patient health and quality care. As we have stated numerous times, like most surgical procedures, the appropriate site of service for THA should be based on the physician's assessment of the patient and tailored to the individual patient's needs. As we stated in the proposed rule (84 FR 39524), patients with a relatively low anesthesia risk and without significant comorbidities who have family members at home who can assist them may likely be good candidates for an outpatient THA procedure. On one hand, it may be determined that these patients will also be able to tolerate outpatient rehabilitation either in an outpatient facility or at home postsurgery. On the other hand, patients that require a revision of a prior hip replacement, and/or have other complicating clinical conditions, including multiple co-morbidities such as obesity, diabetes, heart disease, may not be strong candidates for outpatient THA. We also recognize that elective THA, necessitated, for example, by osteoarthritis, for a generally healthy patient with at-home support is different than THA for a hip fracture that is performed on either an emergent or scheduled basis. While the former may be appropriate for outpatient THA if the physician believes that the patient may be safely discharged on the same or next day, the latter may be more appropriate for hospital inpatient admission.
As previously stated in the discussion of the CY 2018 OPPS/ASC final rule (82 FR 59383), we continue to believe that the decision regarding the most appropriate care setting for a given surgical procedure is a complex medical judgment made by the physician based on the beneficiary's individual clinical needs and preferences and on the general coverage rules requiring that any procedure be reasonable and necessary. We also reiterate our previous statement that the removal of any procedure from the IPO list does not require the procedure to be performed only on an outpatient basis. That is, when a procedure is removed from the IPO, it simply means that Medicare will pay for it in either the hospital inpatient or outpatient setting; it does not mean that the procedure must be performed on an outpatient basis. The 2-midnight rule, which is discussed in section X.B. of this final rule with comment period, provides general guidance on when payment under Medicare Part A (that is, hospital inpatient) may be appropriate. However, the 2-midnight rule also recognizes the importance of the attending physician's clinical judgment regarding the appropriate setting of care for a procedure to be performed.
While we continue to expect providers who perform outpatient THA on Medicare beneficiaries to use comprehensive patient selection criteria to identify appropriate candidates for the procedure, we believe that the surgeons, clinical staff, and medical specialty societies who perform outpatient THA and possess specialized clinical knowledge and experience are most suited to create such guidelines. Therefore, we do not expect to create or endorse specific guidelines or content for the establishment of providers' patient selection protocols.
With respect to certain criteria not being met, we remind commenters that not all criteria must be met for a service to be removed from the IPO. We continue to believe that THA meets criteria 2 and 3.
Comment: Several commenters stated concerns regarding the impact of removing THA from the IPO list in light of the 2-midnight rule and subsequent RAC review. Because of past concerns with the removal of TKA from the IPO list and fear of RAC review, commenters also suggested that if THA is removed from the IPO list, that CMS should provide a two-year exemption from site-of service denials and Recovery Audit Contractor (RAC) referrals. Commenters further stated that in addition to the exemption, CMS should also educate providers that CMS policy allows for case-by-case exceptions to the 2-midnight rule in consideration of patient history, co-morbidities, and risk of adverse events.
Response: We thank the commenters for their feedback. We will again refer readers to the more extensive discussion of an exemption from site-of service denials and RAC referrals in section X.B. of this final rule with comment period. The case-by-case exception under the 2-midnight rule continues to allow for Part A payment to be made, on a case-by-case basis, where the physician does not expect the patient to remain in the hospital for at least two midnights but nonetheless determines that inpatient admission is necessary based on the clinical characteristics of the patient and that determination is supported by the medical record.
Comment: Several commenters opposed the removal of THA due to potential detrimental impacts on hospitals participating in the Comprehensive Care for Joint Replacement (CJR) Program and the Bundled Payments for Care Initiative (BCPI). Some commenters supported the proposal, but requested that payment for THA in the context of alternative payment models be adjusted.
Response: We again refer readers to the CY 2017 OPPS/ACS final rule with comment period (81 FR 79698 through 79699) in which we originally proposed the removal of TKA procedural codes from the IPO list and sought comments on how to modify the CJR and BPCI programs to reflect the shift of some Medicare beneficiaries from an inpatient TKA procedure to an outpatient TKA procedure in the BPCI and CJR model pricing methodologies, including target price calculations and reconciliation processes, as we also believe it to be applicable to THA. As in the case of the policy change to move THAs from the IPO list, the CMS Innovation Center may consider making future changes to the CJR and BPCI Models to address the removal of THAs from the IPO list and the performance of THA procedures in the OPPS setting.
Additionally, CMS notes the concerns about appropriate patient selection raised by commenters and agrees that it is imperative that physicians and hospitals are mindful of factors that affect whether a patient would be a good candidate for outpatient THA or should instead be admitted as a hospital inpatient; however, for the reasons cited in the CY 2020 OPPS/ASC proposed rule, we continue to believe that it is appropriate to remove THA as described by CPT code 27130 from the IPO list. After consideration of the public comments we received, we are finalizing the removal of CPT code 27130, and assigning the procedure to C-APC 5115 (Level 5 Musculoskeletal Procedures) with status indicator “J1”. In addition, we are removing anesthesia code 01214, (anesthesia for open procedures involving hip joint; total hip arthroplasty) as a conforming change.
As stated above, the decision regarding the most appropriate care setting for a given surgical procedure is a complex medical judgment made by the physician based on the beneficiary's individual clinical needs and preferences and on the general coverage rules requiring that any procedure be reasonable and necessary. Further, the removal of any procedure from the IPO list, including THA, does not require the procedure to be performed only on an outpatient basis. That is, when a procedure is removed from the IPO, it simply means that Medicare will pay for it in either the hospital inpatient or outpatient setting; it does not mean that the procedure must be performed on an outpatient basis. The decision to admit as an inpatient admission or to perform the procedure on a hospital outpatient basis is subject to the complex medical judgment of the physician. While we have not established patient selection criteria for THA or any other procedure, we reiterate our finding that patients with a relatively low anesthesia risk and without significant comorbidities who have family members at home who can assist them may likely be (but are not necessarily) good candidates for an outpatient THA procedure. These patients may be determined to be able to tolerate outpatient rehabilitation either in an outpatient facility or at home postsurgery. While on the other hand, patients that require a revision of a prior hip replacement, and/or has other complicating clinical conditions, including multiple co-morbidities such as obesity, diabetes, heart disease, may not be strong candidates for outpatient THA. As stated previously, we also recognize that elective THA, necessitated, for example, by osteoarthritis, for a generally healthy patient with at-home support is different than THA for a hip fracture that is performed on either an emergent or scheduled basis. While the former may be appropriate for outpatient THA if the physician believes that the patient may be safely discharged on the same or next day, the latter may be more appropriate for hospital inpatient admission.
3. Solicitation of Public Comments on the Potential Removal of Procedures Described by CPT Codes 22633, 22634, 63265, 63266, 63267, and 63268 From the IPO List
Throughout the years, we have received several public comments on additional CPT codes that stakeholders believe fit our criteria and should be removed from the IPO list. In the CY 2020 OPPS/ASC proposed rule, we sought public comment on the removal of the following procedures from the IPO list in Table 47.

We reviewed the clinical characteristics of CPT codes 22633 and 22634 and stated that we believe they are related to codes that we have already removed from the IPO list. Specifically, stakeholders have suggested that CPT codes 22633 and 22634 are related to CPT code 22551 (Arthrodesis, anterior interbody, including disc space preparation, discectomy, osteophytectomy and decompression of spinal cord and/or nerve roots; cervical below c2), which is currently performed in the outpatient hospital setting. During the proposed rule, we sought public comments that would provide additional information on the safety of performing CPT codes 22633 and 22634 in the outpatient hospital setting.
In addition, we reviewed CPT codes 63265, 63266, 63267, and 63268. Over the years, stakeholders indicated that this series of CPT codes should be considered minimally invasive, arguing that CPT codes 63265, 63266, 63267, and 63268 meet criteria 1 and 2 for removal from the IPO list: Most outpatient departments are equipped to provide the services to the Medicare population and the simplest procedure described by the code may be performed in most outpatient departments. We sought public comment on whether CPT codes 63265 through 63268 meet criteria to be removed from the IPO list, including information from commenters to demonstrate that the codes meet these criteria.
Comment: We received a few comments in support of the removal of the services described by CPT codes 22633, 22634, 63265, 63266, 63267, and 63268. Commenters agreed that these procedures were both related to codes that were previously removed from the IPO list and are performed safely in numerous hospitals on an outpatient basis. Commenters largely provided anecdotal experience in support of removing these services from the IPO list. One commenter provided a March 2019 published retrospective cohort study of lumbar interbody fusion to treat spinal pathology using the American College of Surgeons National Surgical Quality Improvement Program database. The commenter believed that this study provided additional insight into the perioperative safety profile and operative efficiency and efficacy of performing transforaminal lumbar interbody fusions (TLIF) at an outpatient facility.
Commenters in support of the proposal argued that physicians perform the cases regardless of the IPO list—evaluating each patient carefully to determine the best fit clinically for that patient. Several ASCs commented that they often perform all listed procedures with few to no complications in that setting. This commenter supported not only removing all six procedures from the IPO list, but also adding them to the ASC-CPL list.
Commenters further stated that although their current patient volume does not constitute a large percentage of Medicare beneficiaries, they would expect to see similar results with Medicare patients that are active, have a relatively low anesthesia risk, do not have significant comorbidities and that also have a support system at home that can assist them post-procedure. The commenters specifically supported the removal of the six procedures based on the development of less invasive techniques, improved perioperative pain management, and expedited rehabilitation protocols.
Specifically for the services described by CPT codes 22633 and 22634, commenters agreed that related procedures and similar codes such as 22551 (Arthrodesis, anterior interbody, including disc space preparation, discectomy, osteophytectomy and decompression of spinal cord and/or nerve roots; cervical below c2); 22612 (Arthrodesis, posterior or posterolateral technique, single level; lumbar (with lateral transverse technique, when performed); and 22614 (Arthrodesis, posterior or posterolateral technique, single level; each additional vertebral segment) were previously removed from the IPO list. One commenter specifically pointed out that performance of CPT codes 22612, 22614, and 22551 are all allowed in the ASC setting, and that their safety was reconfirmed in the review of procedures added to the ASC covered procedures list in the CY 2019 OPPS/ASC final rule (83 FR 59057).
In reference to the laminectomy codes, commenters specifically supported their removal from the IPO list based on their perceived safe and effective performance in the outpatient setting, in accordance with criterion 2.
We also received a few general comments in opposition to the prospect of removing the codes. Specifically, those who opposed removing the procedures expressed concern that all six procedures in this comment solicitation are complex procedures and that very few Medicare beneficiaries are likely to be good candidates to receive the procedures in the outpatient setting because of their complexity. The commenters further stated that removing these procedures from the IPO list and providing them in the outpatient setting may impact patient safety and outcomes, which they believe should be the primary considerations when determining which procedures can be removed from the IPO list.
Response: After reviewing clinical evidence and the public comments, including input from multiple spinal specialty societies and ASCs we have determined that the services described by CPT codes 22633, 22634, 63265, 63266, 63267, and 63268 are appropriate candidates for removal from the IPO list. CMS notes the overall support and for the reasons cited in the proposed rule, we believe that it is appropriate to remove CPT codes 22633 and 22634 from IPO list because they meet criteria one and two: Most outpatient departments are equipped to provide the services to the Medicare population and the simplest procedure described by the code may be performed in most outpatient departments. We also believe that it is appropriate to remove CPT codes 63265, 63266, 63267, and 63268 from the inpatient only list, based on criterion one; most outpatient departments are equipped to provide the services to the Medicare population. Therefore, we are finalizing the removal of CPT codes 22633, 22634, 63265, 63266, 63267, and 63268, and assigning the procedures as follows. The APC and status indicator assignments are reflected in Table 48 below.
Additional Requests for Changes to the IPO List
Comment: CMS received two additional comments recommending the removal of several procedures not originally proposed for removal from the IPO list for CY 2020. These recommended procedures related to other procedures that were recently removed from the IPO. Specifically, the commenters referenced the following anesthesia codes for removal:

Response: We thank the commenters for their feedback. After consideration of the public comments, we agree that the recommended anesthesia CPT codes should be removed from the IPO list, as they meet criterion 3; the procedure is related to codes that we have already removed from the IPO list. Notably, these removed anesthesia codes will be assigned a status indicator of “N”.
Comment: Finally, we also received a comment from a provider organization that suggested that CMS eliminate the IPO list. Specifically, the commenter argued that the IPO list should to be eliminated to allow patient status to be determined by the physician based on the individual patient's clinical condition.
Response: We thank the commenters for their feedback and will consider this feedback for future rulemaking.
Table 49 contains the final changes that we are making to the IPO list for CY 2020.

X. Nonrecurring Policy Changes
A. Changes in the Level of Supervision of Outpatient Therapeutic Services in Hospitals and Critical Access Hospitals (CAHs)
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59390 through 59391) and in the CY 2009 OPPS/ASC proposed rule and final rule with comment period (73 FR 41518 through 41519 and 73 FR 68702 through 68704, respectively), we clarified that direct supervision is required for hospital outpatient therapeutic services covered and paid by Medicare that are furnished in hospitals as well as in provider-based departments (PBDs) of hospitals, as set forth in the CY 2000 OPPS final rule with comment period (65 FR 18525). In the CY 2010 OPPS/ASC final rule with comment period (74 FR 60575 through 60591), we finalized a technical correction to the title and text of the applicable regulation at 42 CFR 410.27 to clarify that this standard applies in critical access hospitals (CAHs) as well as hospitals. In response to concerns expressed by the hospital community, in particular CAHs and small rural hospitals, that they would have difficulty meeting this standard, on March 15, 2010, we instructed all MACs not to evaluate or enforce the supervision requirements for therapeutic services provided to outpatients in CAHs from January 1, 2010 through December 31, 2010, while the agency revisited the supervision policy during the CY 2011 OPPS/ASC rulemaking cycle.
Due to continued concerns expressed by CAHs and small rural hospitals, we extended this notice of nonenforcement (“enforcement instruction”) as an interim measure for CY 2011, and expanded it to apply to small rural hospitals having 100 or fewer beds (75 FR 72007). We continued to consider the issue further in our annual OPPS notice-and-comment rulemaking, and implemented an independent review process in 2012 to obtain advice from the HOP Panel on this matter (76 FR 74360 through 74371). Under this process used since CY 2012, the HOP Panel considers and advises CMS regarding stakeholder requests for changes in the required minimum level of supervision of individual hospital outpatient therapeutic services. In addition, we extended the enforcement instruction through CY 2012 and CY 2013. For the period of CY 2014 through CY 2017, Congress took legislative action (Pub. L. 113-198, Pub. L. 114-112, Pub. L. 114-255, and Pub. L. 115-123) to extend nonenforcement of the direct supervision requirement for hospital outpatient therapeutic services in CAHs and small rural hospitals having 100 or fewer beds through December 31, 2017. Then in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59391), we reinstated the enforcement instruction providing for the nonenforcement of the direct supervision requirement for hospital outpatient therapeutic services in CAHs and small rural hospitals having 100 or fewer beds through December 31, 2019. The current enforcement instruction is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Downloads/Supervision-Moratorium-on-Enforcement-for-CAHs-and-Certain-Small-Rural-Hospitals.pdf.
As discussed in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59390 through 59391), stakeholders have consistently requested that CMS continue the nonenforcement of the direct supervision requirement for hospital outpatient therapeutic services for CAHs and small rural hospitals having 100 or fewer beds. Stakeholders stated that some small rural hospitals and CAHs have insufficient staff available to furnish direct supervision. The primary reason stakeholders cited for this request is the difficulty that CAHs and small rural hospitals have in recruiting physicians and nonphysician practitioners to practice in rural areas. These stakeholders noted that it is particularly difficult to furnish direct supervision for critical specialty services, such as radiation oncology services, that cannot be directly supervised by a hospital emergency department physician or nonphysician practitioner because of the volume of emergency patients or lack of specialty expertise. In addition, we are not aware of any supervision-related complaints from beneficiaries or providers regarding quality of care for services furnished during the several years that the enforcement instruction has been in effect.
The upcoming expiration of the latest enforcement instruction providing for the nonenforcement of the direct supervision requirement for hospital outpatient therapeutic services for CAHs and small rural hospitals having 100 or fewer beds has prompted us to consider whether to change the level of supervision for hospital outpatient therapeutic services for all hospitals and CAHs. The enforcement instructions and legislative actions that have been in place since 2010 have created a two-tiered system of physician supervision requirements for hospital outpatient therapeutic services for providers in the Medicare program, with direct supervision required for most hospital outpatient therapeutic services in most hospital providers, but only general supervision required for most hospital outpatient therapeutic services in CAHs and small rural hospitals with fewer than 100 beds.
However, we have not learned of any data or information from CAHs and small rural hospitals indicating that the quality of outpatient therapeutic services has been affected by requiring only general supervision for these services. It is important to remember that the requirement for general supervision for outpatient therapeutic services does not preclude these hospitals from providing direct supervision for outpatient therapeutic services when the physicians administering the medical procedures decide that it is appropriate to do so. Many outpatient therapeutic services involve a level of complexity and risk such that direct supervision would be warranted even though only general supervision is required.
In addition, CAHs and hospitals in general continue to be subject to conditions of participation (CoPs) that complement the general supervision requirements for hospital outpatient therapeutic services to ensure that the medical services Medicare patients receive are properly supervised. CoPs for hospitals require Medicare patients to be under the care of a physician (42 CFR 482.12(c)(4))), and for the hospital to “have an organized medical staff that operates under bylaws approved by the governing body, and which is responsible for the quality of medical care provided to patients by the hospital” (42 CFR 482.22). The CoPs for CAHs (42 CFR 485.631(b)(1)(i)) require physicians to provide medical direction for the CAHs' health care activities, consultation for, and medical supervision of the health care staff. The physicians' responsibilities in hospitals and CAHs include supervision of all services performed at those facilities. In addition, physicians must also follow State laws regarding scope of practice.
Failure of an applicable physician to provide adequate supervision in accordance with the hospital and CAH CoPs does not cause payment to be denied for that individual service. However, consistent violations of the CoP supervision requirements can lead to a provider having to establish a corrective action plan to address supervision deficiencies, and if the provider still fails to meet the CoP requirements, the hospital or CAH can be terminated from Medicare participation.
Our experience indicates that Medicare providers will provide a similar quality of hospital outpatient therapeutic services, regardless of whether the minimum level of supervision required under the Medicare program is direct or general. We have come to believe that the direct supervision requirement for hospital outpatient therapeutic services places an additional burden on providers that reduces their flexibility to provide medical care. The issues with increased burden and reduced flexibility to provide medical care have a more significant impact on CAHs and small rural hospitals due to their recruiting and staffing challenges, as we have recognized over the years in providing for nonenforcement of the policy for these hospitals. Larger hospitals and hospitals in urban or suburban areas are less affected by the burden and reduced flexibility of the direct supervision requirement. However, given that the direct supervision requirement has not yet been enforced for CAHs and small rural hospitals, we believe it is time to end what is effectively a two-tiered system of supervision levels for hospital outpatient therapeutic services by proposing a policy that sets an appropriate and uniformly enforceable supervision standard for all hospital outpatient therapeutic services.
Therefore, we proposed to change the generally applicable minimum required level of supervision for hospital outpatient therapeutic services from direct supervision to general supervision for services furnished by all hospitals and CAHs. General supervision, as defined in our regulation at 42 CFR 410.32(b)(3)(i) means that the procedure is furnished under the physician's overall direction and control, but that the physician's presence is not required during the performance of the procedure. This proposal would ensure a standard minimum level of supervision for each hospital outpatient therapeutic service furnished incident to a physician's service in accordance with the statute. We proposed to amend the existing regulation at § 410.27(a)(1)(iv) to provide that the default minimum level of supervision for each hospital outpatient therapeutic service is “general.”
We will continue to have the HOP Panel provide advice on the appropriate supervision levels for hospital outpatient services as described in section I.E.2. of the proposed rule. We will also retain the ability to consider a change to the supervision level of an individual hospital outpatient therapeutic service to a level of supervision that is more intensive than general supervision through notice and comment rulemaking. We solicited public comments on this proposal.
The comments and our responses to the comments are set forth below.
Comment: A majority of commenters supported our proposal to change the generally applicable minimum required level of supervision for hospital outpatient therapeutic services from direct supervision to general supervision when these services are furnished by hospitals or CAHs. The commenters appreciated that we proposed to eliminate what is effectively a two-tiered system of supervision levels for hospital outpatient therapeutic services between CAHs and small rural hospitals and all other hospitals by proposing a policy that would set an appropriate and uniformly enforceable supervision standard for all hospital outpatient therapeutic services. The commenters also agreed with our observation that the quality of outpatient therapeutic services provided by CAHs and small rural hospitals has not been adversely affected by the nonenforcement instruction. The majority of commenters stated that our proposal would reduce burden for outpatient hospital providers, especially those providers in either rural or underserved areas. The commenters stated that our proposal would allow CAHs and small rural hospitals more flexibility to provide outpatient therapeutic care for the Medicare beneficiaries that they serve than what CAHs and small rural hospitals could provide when the temporary nonenforcement instruction for direct supervision was in effect, because a permanent, rather than temporary policy, would allow them to better make long-range staffing and budgetary plans.
Numerous commenters mentioned the many safeguards noted in our proposal, including our ongoing policy that gives providers discretion to require the appropriate amount of supervision to ensure a therapeutic outpatient procedure is performed without risking a beneficiary's safety or the quality of the care a beneficiary receives. Commenters also noted that outpatient hospital and CAH CoPs and state and federal laws and regulations are present in addition to the requirements for physician supervision to ensure the safety, health, and quality standards of the outpatient therapeutic services that beneficiaries receive.
Response: We appreciate the overall support for our proposal from a majority of the commenters. We agree with the commenters that this policy would support our goal of reducing burden on providers, especially CAHs and small rural hospitals. We also appreciate the commenters' point that this policy will allow these providers to be more flexible with their staffing and in turn provide better care to the communities they serve.
We also appreciate that the commenters noted that providers and physicians have flexibility to require a higher level of physician supervision for any service they render if they believe a higher level of supervision is required to ensure the quality and safety of the procedure and to protect a beneficiary from complications that might occur. We agree with the commenters that CoPs, state and federal laws and regulations, and supervision requirements will also ensure beneficiary health and safety when receiving outpatient therapeutic services.
The CoPs for hospitals require a doctor of medicine or osteopathy (MD/DO) to be responsible for the care of every Medicare patient with respect to any medical or psychiatric problem that is present on admission or develops during hospitalization and that is not specifically within the scope of practice of other types of practitioners (such as dentists, podiatrists, chiropractors, or clinical psychologists) as that scope of practice is defined by the medical staff and permitted by state law (42 CFR 482.12(c)(4)). The CoPs also require a hospital to “have an organized medical staff that operates under bylaws approved by the governing body, and which is responsible for the quality of medical care provided to patients by the hospital” (42 CFR 482.22). The CoPs for CAHs (42 CFR 485.631(b)(1)(i)) require an MD or DO to provide medical direction for the CAHs' health care activities, and consultation for, and medical supervision of, the health care staff. The responsibilities of an MD or DO in hospitals and CAHs include supervision of all services performed at those facilities. In addition, MDs and DOs must also follow state laws regarding scope of practice. State scope of practice laws are state-level regulations that apply to physicians and other health care practitioners that determine the tasks they can perform when caring for patients in healthcare settings in that state.
Comment: Two of the commenters, including MedPAC, strongly encouraged CMS to diligently monitor the impacts of our proposal on the quality and safety of outpatient therapeutic services that Medicare beneficiaries receive to ensure their quality of care is not compromised and that beneficiaries do not experience higher rates of medical errors. In addition, several commenters wrote in support of the Hospital Outpatient Payment Panel (HOP) Panel, which continues to evaluate and make recommendations on supervision levels for individual therapeutic outpatient services. These commenters also wrote in support of CMS' use of the regulatory process to set a higher minimum level of supervision for individual therapeutic services if needed.
Response: We agree with the commenters and will continue to have a system in place to change the default minimum level of physician supervision to a level of supervision higher than general supervision, which we believe will be important to the overall success of this policy. We are also committed to monitoring care furnished to Medicare beneficiaries to determine if there is any decline in the quality of therapeutic outpatient services provided to Medicare beneficiaries as a result of this policy, although we believe that the combination of the CoPs, state and federal laws and regulations, and supervision requirements will help beneficiaries to receive safe and high-quality care. We agree with commenters that the work of HOP Panel is helpful to identify individual outpatient therapeutic procedures that may require a higher minimum level of physician supervision, which can assist us in electing whether to establish higher minimum supervision levels on case-by-case basis through notice and comment rulemaking.
Comment: A few commenters were entirely opposed to our proposal to change the default level of supervision from direct to general and either requested that no changes be made to our current policy (which requires the default minimum level of physician supervision for outpatient therapeutic services to be direct supervision unless we establish a different minimum level of supervision) or requested that CMS evaluate outpatient therapeutic services individually to determine if the default minimum level of supervision should change from direct supervision to general supervision.
Several of these commenters appreciated the concerns from CAHs and small rural providers about the burden they face from the physician supervision requirements, but these commenters believed those concerns were outweighed by the need to have qualified physicians directly supervise services, especially in the fields of radiation therapy, hyperbaric oxygen treatment, and wound care. These commenters believed the default level of supervision for outpatient therapeutic services should be the same for all outpatient hospitals and CAHs.
Other commenters expressed concerns that allowing general supervision to be the minimum default level of supervision for certain types of services, including radiation therapy, hyperbaric oxygen treatment, and wound care, could put the health and safety of Medicare beneficiaries receiving these procedures at risk. These commenters described these particular services as requiring a high level of skill to perform and having complications that, while rare, can cause serious issues for a beneficiary's health. Therefore, these commenters believed that the minimum default level of supervision for radiation therapy, hyperbaric oxygen treatment, and wound care should be direct supervision.
Response: We agree with the commenters about the importance of ensuring the quality of outpatient therapeutic services and the health and safety of the beneficiaries who receive those services. We also appreciate the concerns several commenters raised about how this proposal will affect the quality and safety of outpatient therapeutic services including radiation therapy, hyperbaric oxygen treatments, and wound care services. We believe our supervision requirements continue to provide the safeguards Medicare beneficiaries need to ensure they receive quality care when they receive outpatient hospital therapeutic services and that health and safety of beneficiaries is protected.
Providers have the flexibility to establish what they believe is the appropriate level of physician supervision for these procedures, which may well be higher than the requirements for general supervision. In addition, providers must adhere to the hospital and CAH conditions of participation, federal and state regulations for radiation therapy, hyperbaric oxygen treatments, and wound care services, and state standards for scope of practice for medical personnel who provide these services. We believe that the combination of providers' desire to ensure the safety of their patients and the regulations governing these procedures discussed by the commenters should ensure that these procedures will be appropriately supervised without risking beneficiaries' safety or the quality of the care beneficiaries receive, whether the default level of physician supervision is direct supervision or general supervision.
We reiterate a key point that the commenters who are in support of our proposal mentioned, which is that establishing general supervision as the default level of physician supervision for outpatient therapeutic services does not prevent a hospital or CAH from requiring a higher level of supervision for a particular service if they believe such a supervision level is necessary. Providers and physicians have flexibility to require a higher level of physician supervision for any service they furnish if they believe a higher level of supervision is required to ensure the quality and safety of the procedure and to protect a beneficiary from complications that might occur. We believe this flexibility for individual providers to have a higher level of physician supervision for a given service, which has always been present in our supervision policies, should address the concerns of those commenters who believe general supervision is not sufficient for certain outpatient therapeutic services. In addition, CoP, other federal and state regulations, and state standards for scope of work for medical personnel are not affected by this policy, and remain in place to ensure that hospitals provide proper medical care to all of their patients including Medicare beneficiaries.
Comment: Two commenters wanted confirmation that our proposed policy was intended to be permanent and not just for CY 2020.
Response: This policy will take effect beginning in CY 2020 and will remain in place through subsequent years unless modified in future notice and comment rulemaking.
Comment: One commenter wanted more clarification on what constitutes general supervision. The commenter does not support Medicare requirements for physician supervision that do not help with patient safety.
Response: Our policies on supervision, along with hospital conditions of participation, state scope of practice laws, and other state and federal laws and regulations, all help ensure the quality and safety of outpatient hospital therapeutic services Medicare beneficiaries receive. General supervision is defined in our regulation at 42 CFR 410.32(b)(3)(i) to mean that the procedure is furnished under the physician's overall direction and control, but that the physician's presence is not required during the performance of the procedure.
With general supervision, our proposal would ensure a standard minimum level of supervision for each hospital outpatient therapeutic service furnished incident to a physician's service in accordance with the statute. General supervision ensures patient safety as it requires a physician to provide overall direction and control for outpatient hospital therapeutic procedures, which means the medical personnel performing the procedure are being monitored and receiving guidance from a qualified physician even if the physician is not physically present. Also, a provider may voluntarily choose to require a higher level of involvement in the medical procedure by the physician if the hospital believes it is necessary for the safety of the patient receiving the procedure.
Additionally, we solicited public comments on whether specific types of services, such as chemotherapy administration or radiation therapy, should be excepted from our proposal to change the generally applicable minimum required level of supervision for hospital outpatient therapeutic services from direct supervision to general supervision for services furnished by all hospitals and CAHs.
Comment: Multiple commenters supported our proposal to have general supervision be the minimum default level of supervision for outpatient hospital therapeutic chemotherapy and radiation therapy services. One commenter supported this policy because they were concerned that if direct supervision was required to be the default minimum level of physician supervision for chemotherapy and radiation therapy while all other outpatient hospital therapeutic services have a default minimum level of general supervision, it would be difficult to change the minimum default level of supervision for chemotherapy and radiation therapy to general supervision in the future. Another commenter wanted to know under what circumstances the minimum default supervision level for chemotherapy and radiation therapy would be direct physician supervision if the current policy has established general supervision as the minimum default level of supervision.
Response: We appreciate the feedback we received from commenters on this topic. Regarding the question from the one commenter about how the default minimum level of supervision for chemotherapy and radiation services could be direct supervision when the default minimum level of supervision is general supervision for other outpatient therapeutic services, we note that because we are finalizing our proposal to require general supervision for all outpatient therapeutic services, the required supervision level is the same for all of these services, including chemotherapy and radiation therapy services.
After reviewing all of the public comments, we are finalizing our proposal for CY 2020 and subsequent years to change the generally applicable minimum required level of supervision for hospital outpatient therapeutic services from direct supervision to general supervision for services furnished by all hospitals and CAHs without modification. We also note all of the policy safeguards that have been in place to ensure the safety, health, and quality standards of the outpatient therapeutic services that beneficiaries receive will continue to be in place under our new policy. These safeguards include allowing providers and physicians the discretion to require a higher level of supervision to ensure a therapeutic outpatient procedure is performed without risking a beneficiary's safety or their quality of the care, as well as the presence outpatient hospital and CAH CoPs, and other state and federal laws and regulations. We are also finalizing the accompanying changes we proposed to the regulatory text at § 410.27 with several technical changes.
B. Short Inpatient Hospital Stays
1. Background on the 2-Midnight Rule
In the FY 2014 IPPS/LTCH PPS final rule (78 FR 50913 through 50954), we clarified our policy regarding when an inpatient admission is considered reasonable and necessary for purposes of Medicare Part A payment. Under this policy, we established a benchmark providing that surgical procedures, diagnostic tests, and other treatments would be generally considered appropriate for inpatient hospital admission and payment under Medicare Part A when the physician expects the patient to require a stay that crosses at least 2 midnights and admits the patient to the hospital based upon that expectation. Conversely, when a beneficiary enters a hospital for a surgical procedure not designated as an inpatient-only (IPO) procedure as described in 42 CFR 419.22(n), a diagnostic test, or any other treatment, and the physician expects to keep the beneficiary in the hospital for only a limited period of time that does not cross 2 midnights, the services would be generally inappropriate for payment under Medicare Part A, regardless of the hour that the beneficiary came to the hospital or whether the beneficiary used a bed. With respect to services designated under the OPPS as IPO procedures, we explained that because of the intrinsic risks, recovery impacts, or complexities associated with such services, these procedures would continue to be appropriate for inpatient hospital admission and payment under Medicare Part A regardless of the expected length of stay. We also indicated that there might be further “rare and unusual” exceptions to the application of the benchmark, which would be detailed in subregulatory guidance.
2. Current Policy for Medical Review of Inpatient Hospital Admissions Under Medicare Part A
In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70538 through 70549), we revised the previous rare and unusual exceptions policy and finalized a proposal to allow for case-by-case exceptions to the 2-midnight benchmark, whereby Medicare Part A payment may be made for inpatient admissions where the admitting physician does not expect the patient to require hospital care spanning 2 midnights, if the documentation in the medical record supports the physician's determination that the patient nonetheless requires inpatient hospital care.
We note that, in the CY 2016 OPPS/ASC final rule with comment period, we reiterated our position that the 2-midnight benchmark provides clear guidance on when a hospital inpatient admission is appropriate for Medicare Part A payment, while respecting the role of physician judgment. We stated that the following criteria will be relevant to determining whether an inpatient admission with an expected length of stay of less than 2 midnights is nonetheless appropriate for Medicare Part A payment:
- Complex medical factors such as history and comorbidities;
- The severity of signs and symptoms;
- Current medical needs; and
- The risk of an adverse event.
In other words, for purposes of Medicare payment, an inpatient admission is payable under Part A if the documentation in the medical record supports either the admitting physician's reasonable expectation that the patient will require hospital care spanning at least 2 midnights, or the physician's determination based on factors such as those identified above that the patient nonetheless requires care on an inpatient basis. The exceptions for procedures on the IPO list and for “rare and unusual” circumstances designated by CMS as national exceptions were unchanged by the CY 2016 OPPS/ASC final rule with comment period.
As we stated in the CY 2016 OPPS/ASC final rule with comment period, the decision to formally admit a patient to the hospital is subject to medical review. For instance, for cases where the medical record does not support a reasonable expectation of the need for hospital care crossing at least 2 midnights, and for inpatient admissions not related to a surgical procedure specified by Medicare as an IPO procedure under 42 CFR 419.22(n) or for which there was not a national exception, payment of the claim under Medicare Part A is subject to the clinical judgment of the medical reviewer. The medical reviewer's clinical judgment involves the synthesis of all submitted medical record information (for example, progress notes, diagnostic findings, medications, nursing notes, and other supporting documentation) to make a medical review determination on whether the clinical requirements in the relevant policy have been met. In addition, Medicare review contractors must abide by CMS' policies in conducting payment determinations, but are permitted to take into account evidence-based guidelines or commercial utilization tools that may aid such a decision. While Medicare review contractors may continue to use commercial screening tools to help evaluate the inpatient admission decision for purposes of payment under Medicare Part A, such tools are not binding on the hospital, CMS, or its review contractors. This type of information also may be appropriately considered by the physician as part of the complex medical judgment that guides their decision to keep a beneficiary in the hospital and formulation of the expected length of stay.
3. Change for Medical Review of Certain Inpatient Hospital Admissions Under Medicare Part A for CY 2020 and Subsequent Years
As stated earlier in this section, the procedures on the IPO list of procedures under the OPPS are not subject to the 2-midnight benchmark for purposes of inpatient hospital payment. However, the 2-midnight benchmark is applicable once procedures have been removed from the IPO list. Procedures that are removed from the IPO list are also subject to initial medical reviews of claims for short-stay inpatient admissions conducted by Beneficiary and Family-Centered Care Quality Improvement Organizations (BFCC-QIOs).
BFCC-QIOs may also refer providers to the Recovery Audit Contractors (RACs) for further medical review due to exhibiting persistent noncompliance with Medicare payment policies, including, but not limited to:
- Having high denial rates;
- Consistently failing to adhere to the 2-midnight rule; or
- Failing to improve their performance after QIO educational intervention.
As part of our continued effort to facilitate compliance with our payment policy for inpatient admissions, we proposed to establish a 1-year exemption from certain medical review activities for procedures removed from the IPO list under the OPPS in CY 2020 and subsequent years. Specifically, we proposed that procedures that have been removed from the IPO list would not be eligible for referral to RACs for noncompliance with the 2-midnight rule within the first calendar year of their removal from the IPO list. These procedures would not be considered by the BFCC-QIOs in determining whether a provider exhibits persistent noncompliance with the 2-midnight rule for purposes of referral to the RAC nor would these procedures be reviewed by RACs for “patient status.” During this 1-year period, BFCC-QIOs would have the opportunity to review such claims in order to provide education for practitioners and providers regarding compliance with the 2-midnight rule, but claims identified as noncompliant would not be denied with respect to the site-of-service under Medicare Part A. Again, information gathered by the BFCC-QIO when reviewing procedures that are newly removed from the IPO list could be used for educational purposes and would not result in a claim denial during the proposed 1-year exemption period.
In the proposed rule, we stated that we believed that a 1-year exemption from BFCC-QIO referral to RACs and RAC “patient status” review of the setting for procedures removed from the IPO list under the OPPS and performed in the inpatient setting would be an adequate amount of time to allow providers to gain experience with application of the 2-midnight rule to these procedures and the documentation necessary for Part A payment for those patients for which the admitting physician determines that the procedures should be furnished in an inpatient setting. Furthermore, we stated our belief that this 1-year exemption from referrals to RACs, RAC patient status review, and claims denials would be sufficient to allow providers time to update their billing systems and gain experience with respect to newly removed procedures eligible to be paid under either the IPPS or the OPPS, while avoiding potential adverse site-of-service determinations. Nonetheless, we solicited public comments regarding the appropriate period of time for this proposed exemption. Specifically, we stated that commenters may indicate whether and why they believe the proposed 1-year period is appropriate, or whether they believe a longer or shorter exemption period would be more appropriate.
In summary, for CY 2020 and subsequent years, we proposed to establish a 1-year exemption from site-of-service claim denials, BFCC-QIO referrals to RACs, and RAC reviews for “patient status” (that is, site-of-service) for procedures that are removed from the IPO list under the OPPS beginning on January 1, 2020. We encourage BFCC-QIOs to review these cases for medical necessity in order to educate themselves and the provider community on appropriate documentation for Part A payment when the admitting physician determines that it is medically reasonable and necessary to conduct these procedures on an inpatient basis. We note that we will monitor changes in site-of-service to determine whether changes may be necessary to certain CMS Innovation Center models.
Comment: Numerous stakeholders including medical professional societies, health systems, hospital associations, and individuals supported the proposal of a 1-year exemption from site-of-service claim denials under Medicare Part A, eligibility for BFCC-QIO referrals to RACs for noncompliance with the 2-midnight rule, and RAC reviews for “patient status” (that is, site-of-service) for procedures that are removed from the IPO list under the OPPS beginning on January 1, 2020. However, many of these commenters supported an extension of the exemption policy past 1 year, with a majority of commenters recommending a period of 2 years, some commenters recommending three years or more, and others recommending that CMS permanently restrict RAC reviews of patient status for procedures removed from the IPO list in deference to physicians' clinical judgment. The commenters stated that a longer period of time is necessary for providers to adjust patterns of practice for procedures that have been removed from the IPO list and to prepare for system-wide implementation. Some commenters also requested that CMS maintain consistency with the policy finalized when total knee arthroplasty (TKA) was removed from the IPO list and limit RAC review for “patient status” for a period of 2 years.
Response: We appreciate the stakeholders' feedback regarding the appropriate period of time for this exemption. After considering the options recommended by commenters, we have decided to modify our proposal and exempt procedures that are removed from the IPO list from site-of-service claim denials under Medicare Part A, eligibility for BFCC-QIO referrals to RACs for noncompliance with the 2-midnight rule, and RAC reviews for “patient status” (that is, site-of-service) for a period of 2 years beginning in CY 2020. We agree with the majority of commenters who stated a two-year exemption period from certain medical review activities for procedures removed from the IPO list would be more beneficial to the provider community than a 1-year exemption, as such a time period will be sufficient to help hospitals and clinicians to become used to the availability of payment under both the hospital inpatient and outpatient setting for procedures newly removed from the IPO. Further, we were persuaded by the comments explaining that a 2-year exemption period of exemption will allow providers time to gather information on procedures newly removed from the IPO list to help inform education and guidance for the broader provider community, develop patient selection criteria to identify which patients are, and are not, appropriate candidates for outpatient procedures and to develop related policy protocols. We also believe that an extended exemption period will further facilitate compliance with our payment policy for inpatient admissions.
We believe that a 2-year exemption time period is adequate to let providers gain experience with the application of the 2-midnight rule to these procedures. We also believe that a 2-year exemption of the medical review activities discussed above for procedures removed from the IPO list will be sufficient time for providers and BFCC-QIOs to understand the documentation necessary to support Part A payment for those patients for which the admitting physician determines that the procedures should be furnished in an inpatient setting. At this time, we do not believe it is necessary to exempt procedures that have been removed from the IPO list from the medical review activities discussed above for a period of longer than 2 years. With regard to comments recommending that we permanently restrict RAC reviews of “patient status” in deference to physicians' clinical judgment, we believe that it is necessary to allow BFCC-QIOs to resume referring providers to the RACs for further medical review due to exhibiting persistent noncompliance with Medicare payment policies after the two-year exemption period.
Comment: Some commenters also requested clarifications regarding the proposed policy with regard to BFCC-QIO reviews. One commenter questioned if the proposed 1-year exemption from certain medical review activities applied to BFCC-QIO referrals to RACs for review of patient status only or if it also applied to BFCC-QIO review of medical necessity for surgery itself. Other commenters suggested that in the first year after a service is removed from the IPO list, the procedure should be exempt from both BFCC-QIO medical review and RAC review.
Response: For clarification, as stated in the CY 2020 OPPS/ASC proposed rule (84 FR 39527), this proposal does not exempt procedures that are removed from the IPO list from the initial medical reviews of claims for short-stay inpatient admissions conducted by BFCC-QIOs. The proposal was intended to exempt procedures that are removed from the IPO list from eligibility for BFCC-QIO referrals to RACs for noncompliance with the 2-midnight rule, and RAC reviews for “patient status” (that is, site-of-service) for procedures that are removed from the IPO list under the OPPS beginning on January 1, 2020. We also stated in the CY 2020 OPPS/ASC proposed rule that we encourage BFCC-QIOs to review these cases for medical necessity in order to educate themselves and the provider community on appropriate documentation for Part A payment when the admitting physician determines that it is medically reasonable and necessary to conduct these procedures on an inpatient basis (84 FR 39528).
Also, as stated in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70545), section 1154(a)(1) of the Act authorizes BFCC-QIOs to review whether services and items billed under Medicare are reasonable and medically necessary and whether services that are provided on an inpatient basis could be appropriately and effectively provided on an outpatient basis. Accordingly, BFCC-QIOs will continue to conduct initial medical reviews for both the medical necessity of the services, and the medical necessity of the site-of-service. BFCC-QIOs will continue to be permitted and expected to deny claims if the service itself is determined not to be reasonable and medically necessary. BFCC-QIOs will not make referrals to RACs for noncompliance with the 2-midnight rule for procedures that are removed from the IPO list within the first two years of their removal, RACs will not conduct reviews for “patient status” (that is, site-of-service) for procedures that are removed from the IPO list within the first two years of their removal, and claims with procedures that are removed from the IPO list that are identified as noncompliant with the 2-midnight rule will not be denied with respect to the site-of-service under Medicare Part A within the first 2 years of their removal beginning on January 1, 2020.
After considering comments received, we are finalizing our policy as proposed with one modification to the time period of the exemption. That is, for CY 2020 and subsequent years, we are finalizing a policy to exempt procedures that have been removed from the IPO list from eligibility for referral to RACs for noncompliance with the 2-midnight rule within the 2-calendar years following their removal from the IPO list. These procedures will not be considered by the BFCC-QIOs in determining whether a provider exhibits persistent noncompliance with the 2-midnight rule for purposes of referral to the RAC nor will these procedures be reviewed by RACs for “patient status.” During this 2-year period, BFCC-QIOs will have the opportunity to review such claims in order to provide education for practitioners and providers regarding compliance with the 2-midnight rule, but claims identified as noncompliant will not be denied with respect to the site-of-service under Medicare Part A.
C. Method To Control Unnecessary Increases in the Volume of Clinic Visit Services Furnished in Excepted Off-Campus Provider-Based Departments (PBDs)
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59004 through 59014), we adopted a method to control unnecessary increases in the volume of the clinic visit service furnished in excepted off-campus provider-based departments (PBDs) by removing the payment differential that drives the site-of-service decision and, as a result, unnecessarily increases service volume. We refer readers to the CY 2019 OPPS/ASC final rule with comment period for a detailed discussion of the background, legislative provisions, and the changes in payment policies we developed to address increases in the volume of covered outpatient department (OPD) services. Below we discuss the specific policy we finalized in the CY 2019 OPPS/ASC final rule with comment period and its application under the OPPS for CY 2020.
For the CY 2019 OPPS, using our authority under section 1833(t)(2)(F) of the Act to adopt a method to control unnecessary increases in the volume of covered outpatient department services, we applied an amount equal to the site-specific Medicare Physician Fee Schedule (PFS) payment rate for nonexcepted items and services furnished by a nonexcepted off-campus PBD (the PFS payment rate) for the clinic visit service, as described by HCPCS code G0463, when provided at an off-campus PBD excepted from section 1833(t)(21) of the Act (departments that bill the modifier “PO” on claim lines). However, we phased in the application of the reduction in payment for the clinic visit service described by HCPCS code G0463 in the excepted provider-based department setting over 2 years. For CY 2019, the payment reduction was transitioned by applying 50 percent of the total reduction in payment that was applied if these departments were paid the site-specific PFS rate for the clinic visit service. The PFS-equivalent rate was 40 percent of the OPPS payment for CY 2019 (that is, 60 percent less than the OPPS rate). We provided for a 2-year phase-in of this policy under which one-half of the total 60-percent payment reduction (a 30-percent reduction) was applied in CY 2019. These departments are paid approximately 70 percent of the OPPS rate (100 percent of the OPPS rate minus the 30-percent payment reduction that is applied in CY 2019) for the clinic visit service in CY 2019.
For CY 2020, the second year of the 2-year phase-in, we stated that we would apply the total reduction in payment that is applied if these departments (departments that bill the modifier “PO” on claims lines) are paid the site-specific PFS rate for the clinic visit service described by HCPCS code G0463. The PFS-equivalent rate for CY 2020 is 40 percent of the proposed OPPS payment (that is, 60 percent less than the proposed OPPS rate) for CY 2020. Under this policy, adopted in 2019, departments would be paid approximately 40 percent of the OPPS rate (100 percent of the OPPS rate minus the 60-percent payment reduction that is applied in CY 2020) for the clinic visit service in CY 2020.
In addition, as we stated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59013), for CY 2020, this policy will be implemented in a non-budget neutral manner. The estimated payment impact of this policy was displayed in Column 5 of Table 44-Estimated Impact of the Proposed CY 2020 Changes for the Hospital Outpatient Prospective Payment System in the CY 2020 OPPS/ASC proposed rule. In order to effectively establish a method for controlling the unnecessary growth in the volume of clinic visits furnished by excepted off-campus PBDs that does not simply increase other expenditures that are unnecessary within the OPPS and drive different service-distorting decisions, we believe that this method must be adopted in a non-budget neutral manner. The impact associated with this policy is further described in section XXVI. of this rule.
The comments and our responses to the comments are set forth below.
Comment: Numerous commenters, including organizations representing health insurance plans, physician associations, specialty medical associations and individual Medicare beneficiaries, supported moving forward with the phase-in of this proposal. Some of these commenters commended CMS for completing the two-year phase-in “since it increases the sustainability of the Medicare program and reduces costs for Medicare patients.” Commenters expressed that the alignment of payment between the outpatient and physician office setting “is an important and necessary reform that can help reduce provider consolidation and thereby provide beneficiaries with more care options at a lower cost.” Commenters continued to be supportive of the immediate impact this policy would have in lowering Medicare beneficiaries' out-of-pocket costs.
With respect to the policy being applied in a non-budget neutral manner, one commenter expressed support for the policy and stated that “the Agency correctly recognized that it cannot address the payment disparity between the outpatient hospital and physician office settings as long as it applies payment changes within the OPPS in a budget-neutral manner that effectively `traps' the potential savings from the change within the OPPS.”
Several commenters suggested that CMS “explore additional opportunities to expand site neutral payments for all clinically appropriate outpatient services” beyond the clinic visit service. They expressed that site neutral payment policies can create incentives for providers to make decisions that lower the cost of care for beneficiaries and the Medicare program.
Response: We appreciate the commenters' support. As we stated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59005), we continue to share the commenters' concern that the current payment incentives, rather than patient acuity or medical necessity, are affecting site-of-service decision-making. We continue to believe that these shifts in the sites of service are unnecessary if the beneficiary can safely receive the same services in a lower cost setting but instead receives care in a higher cost setting due to payment incentives. We remain concerned that this shift in care setting increases beneficiary cost-sharing liability because Medicare payment rates for the same or similar services are generally higher in hospital outpatient departments than in physician offices.
We appreciate the comments supporting the implementation of this policy in a non-budget neutral manner. As we stated in the CY 2019 OPPS ASC final rule with comment period (83 FR 59013), we believe implementing a volume control method in a budget neutral manner would not appropriately reduce the overall unnecessary volume of covered OPD services, and instead would simply shift services within the OPPS system because of payment rather than medical necessity. We also outlined in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59013) that while section 1833(t)(9)(B) of the Act requires that certain changes made under the OPPS be made in a budget neutral manner, this section does not apply to the volume control method under section 1833(t)(2)(F) of the Act. As we detailed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59005), “total spending under the OPPS is projected to further increase by more than $5 billion from approximately $70 billion in CY 2018 through CY 2019 to nearly $75 billion. This is approximately twice the total estimated spending in CY 2008, a decade ago.” And as for one of the drivers of this volume increase, the “Medicare Payment Advisory Commission (MedPAC) found that, from 2011 through 2016, combined program spending and beneficiary cost-sharing on services covered under the OPPS increased by 51 percent, from $39.8 billion to $60.0 billion, an average of 8.6 percent per year. In its 2018 report, MedPAC also noted that `A large source of growth in spending on services furnished in hospital outpatient departments (HOPDs) appears to be the result of the shift of services from (lower cost) physician offices to (higher cost) HOPDs'.” (83 FR 59006).
Section 1833(t)(9)(A) of the Act, titled “Periodic review,” provides, in part, that the Secretary must annually review and revise the groups, the relative payment weights, and the wage and other adjustments described in paragraph (2) to take into account changes in medical practice, changes in technology, the addition of new services, new cost data, and other relevant information and factors” (emphasis added). Section 1833(t)(9)(B) of the Act, titled “Budget neutrality adjustment” provides that if “the Secretary makes adjustments under subparagraph (A), then the adjustments for a year may not cause the estimated amount of expenditures under this part for the year to increase or decrease from the estimated amount of expenditures under this part that would have been made if the adjustments had not been made” (emphasis added).
However, section 1833(t)(2)(F) of the Act is not an “adjustment” under paragraph (2). Unlike the wage adjustment under section 1833(t)(2)(D) of the Act and the outlier, transitional pass-through, and equitable adjustments under section 1833(t)(2)(E) of the Act, section 1833(t)(2)(F) of the Act refers to a “method” for controlling unnecessary increases in the volume of covered OPD services, not an adjustment. Likewise, sections 1833(t)(2)(D) and (E) of the Act also explicitly require the adjustments authorized by those paragraphs to be budget neutral, while the volume control method authority at section 1833(t)(2)(F) of the Act does not. Therefore, the volume control method proposed under section 1833(t)(2)(F) of the Act is not one of the adjustments under section 1833(t)(2) of the Act that is referenced under section 1833(t)(9)(A) of the Act that must be included in the budget neutrality adjustment under section 1833(t)(9)(B) of the Act. Moreover, section 1833(t)(9)(C) of the Act specifies that, if the Secretary determines under methodologies described in paragraph (2)(F) that the volume of services paid for under this subsection increased beyond amounts established through those methodologies, the Secretary may appropriately adjust the update to the conversion factor otherwise applicable in a subsequent year. We continue to interpret this provision to mean that the Secretary will have implemented a volume control method under section 1833(t)(2)(F) of the Act in a nonbudget neutral manner in the year in which the method is implemented, and that the Secretary may then make further adjustments to the conversion factor in a subsequent year to account for volume increases that are beyond the amounts estimated by the Secretary under the volume control method.
As detailed later in this section, after consideration of public comments, we are continuing the second year of the two-year phase-in as adopted in CY 2019 rulemaking. We will continue to take information submitted by the commenters into consideration for future analysis.
Comment: MedPAC supported the proposal to adjust the OPPS payment rate for clinic visits that are provided in excepted off-campus PBDs so that it is the same as the payment rate for clinic visits provided in nonexcepted off-campus PBDs. They note that this policy would be consistent with past Commission recommendations for site-neutral payments between HOPDs and freestanding physician offices, although the recommendations it put forth in 2012 and 2014 would have applied to several services that met certain criteria and would have adjusted payment so that it equaled the total payment had the services been furnished in a freestanding office and did not distinguish between on- and off-campus services. MedPAC further noted that it shares CMS' concerns about the rate of growth in volume and spending under the OPPS. MedPAC also stated, perhaps inadvertently, that “CMS proposes to implement this policy in a budget-neutral manner.”
Response: We thank MedPAC for its comments and support of this policy. To clarify, this policy has been phased-in in a non-budget neutral manner.
Comment: Some commenters were concerned about the impact this payment change might have on rural providers and safety net health systems. Commenters suggested that CMS consider policy modifications to reduce the impact of the payment reduction. They said this could be accomplished by “providing the OPPS rate to outpatient departments located in federally designated Health Professional Shortage Areas or Medically Underserved Areas.” Some commenters also suggested that CMS monitor for any potential access to care issues in rural and underserved areas.
Response: We share the commenters' concerns about access to care, especially in rural areas where access issues may be more pronounced than in other areas of the country. While we understand the concerns regarding rural hospitals, we believe that implementing with a phase-in has helped to mitigate the immediate impact rural hospitals might otherwise face. We will continue to monitor trends for any access to care issues and may revisit this policy in future rulemaking.
Comment: One commenter, a large medical association, stated that while it generally supported site neutral payments, it did not “believe that it is possible to sustain a high-quality health care system if site neutrality is defined as shrinking all payments to the lowest amount paid in any setting.” The commenter went on to state that “any savings from site neutrality proposals derived from OPPS should be reinvested in improvements elsewhere in Part B, including payments to physicians as inflation is not a factor in annual physician payment updates and this contributes to the payment differential.” The commenter went on to underscore its position that “CMS should not implement site neutrality in a way that reduces payment to the lowest common denominator and should reinvest savings from lowering facility payments to other Part B services, including payments under the physician fee schedule.”
Response: We thank the commenter for its input. As we stated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59005), to the extent that similar services can be safely provided in more than one setting, we do not believe it is prudent for the Medicare program to pay more for these services in one setting than another. We believe the increase in the volume of clinic visits, in particular, is due to the payment incentive that exists to provide this service in the higher cost setting. Because these services could likely be safely provided in a lower cost setting, we believe that the growth in clinic visits paid under the OPPS is unnecessary. Further, we believe that setting the OPPS payment at the PFS-equivalent rate would be an effective method to control the volume of these unnecessary services because the payment differential that is driving the site-of-service decision will be removed.
We note that the overall amount of Medicare payments to physicians and other entities made under the PFS is determined by the PFS statute, and the rates for individual services are determined based on the resources involved in furnishing these services relative to other services paid under the PFS. To the extent the commenter believes that the PFS rate for a particular service is misvalued relative to other PFS services, we encourage the commenter to nominate the service for review as a potentially misvalued service under the PFS.
Comment: We received numerous comments urging CMS not to move forward with the phase-in of this policy. Many commenters believed that the final rule should reflect the recent decision from the United States District Court for the District of Columbia, American Hospital Association, et al. v. Azar, No. 1:18-cv-02841-RMC (D.D.C. Sept. 17, 2019), and that CMS, at a minimum, should maintain the 2019 payments and not complete the second year of the phase-in. Others believed the litigation mandated that CMS revert back to the higher payment rates. Commenters noted that the advisory Panel on Hospital Outpatient Payment unanimously recommended that CMS freeze the payment policy for clinic visits furnished by excepted off-campus PBDs at CY 2019 rates and evaluate whether beneficiary access has been compromised and whether the volume of outpatient services has decreased. Many commenters argued that there are several factors in the Medicare program (and outside of hospital control) that could influence more services moving to the hospital outpatient setting, including the hospital readmissions reduction program, hospital value-based purchasing, and the 2-midnight rule. Commenters reiterated their comments from the CY 2019 OPPS/ASC final rule with comment period (83 FR 59005) that, relative to patients seen in physician offices, patients seen in HOPDs:
- Have more severe chronic conditions;
- Have higher prior utilization of hospitals and EDs;
- Are more likely to live in low-income areas;
- Are 1.8 times more likely to be dually eligible for Medicare and Medicaid;
- Are 1.4 times more likely to be nonwhite;
- Are 1.6 times more likely to be under age 65 and disabled; and
- Are 1.1 times more likely to be over 85 years old.
Many commenters, including numerous state hospital associations, stated that making additional cuts to outpatient payment of the magnitude of the second year of phase-in of the clinic visit policy would be excessive and harmful. They expressed concern that the cuts could endanger the critical role that HOPDs play in their communities.
Response: We continue to believe that section 1833(t)(2)(F) of the Act grants the Secretary the authority to develop a method for controlling unnecessary increases in the volume of covered OPD services, including a method that controls unnecessary volume increases by removing a payment differential that is driving a site-of-service decision, and as a result, is unnecessarily increasing service volume.[78] We also continue to believe shifts in the sites of service described in CY 2019 OPPS/ASC final rule with comment period (83 FR 59013), are inherently unnecessary if the beneficiary can safely receive the same services in a lower cost setting but instead receives care in a higher cost setting due to the payment incentives created by the difference in payment amounts. While we did receive some data illustrating that certain HOPDs serve unique patient populations and provide services to medically complex beneficiaries, we continue to believe that this data has not demonstrated the need for higher payment for clinic visits furnished in excepted off-campus PBDs. As we asserted in the 2019 OPPS/ASC final rule with comment period (83 FR 59013), the fact that the commenters did not supply new or additional data supporting these assertions suggests that the payment differential is likely the main driver for unnecessary volume increases in outpatient department services, particularly clinic visits.
On September 17, 2019, the United States District Court for the District of Columbia (the district court) entered an order vacating the portion of the CY 2019 OPPS/ASC final rule with comment period that adopted the volume control method for clinic visit services furnished by nonexcepted off-campus PBDs and remanded the matter to the Secretary for further proceedings consistent with the district court's opinion.[79] On September 23, 2019, the Department of Health and Human Services (HHS) filed a motion requesting that the district court modify its order to remand the matter without vacatur or, alternatively, to stay the portion of the order vacating the rule for 60 days from the date of the order to allow the Solicitor General time to determine whether to authorize appeal. On October 21, 2019, the district court denied our motion to modify and request for stay, affirmed that the portion of the 2019 final rule that adopted the volume control method for clinic visits furnished by excepted off-campus PBDs is vacated, and entered final judgment. We acknowledge that the district court vacated the volume control policy for CY 2019 and we are working to ensure affected 2019 claims for clinic visits are paid consistent with the court's order. We do not believe it is appropriate at this time to make a change to the second year of the two-year phase-in of the clinic visit policy. The government has appeal rights, and is still evaluating the rulings and considering, at the time of this writing, whether to appeal from the final judgment.
With respect to the HOP panel, section 1833(t)(9)(A) of the Act provides that the Secretary shall consult with the Panel on policies affecting the clinical integrity of the ambulatory payment classifications and their associated weights under the OPPS. The Panel met on August 19, 2019, and recommended that CMS freeze the payment policy for off-campus clinic visits at the calendar year 2019 rates and evaluate whether beneficiary access has been compromised and whether the volume of outpatient services has decreased; the panel further recommended that CMS report its findings back to the Panel for review. We believe, for reasons outlined in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59013) and in this final rule that in order to appropriately control unnecessary increases in the volume of clinic visits services furnished in HOPDs, we must move forward with phasing-in this policy. Freezing the payment rate, even at the 2019 rate, still “traps” the unnecessary spending within the OPPS.
The HOP Panel's recommendations, along with public comments on provisions of the proposed rule, have been taken into consideration in the development of this final rule with comment period. While we are not accepting the HOP Panel's recommendation, we will continue to monitor and study the utilization of outpatient services as recommended by the Panel.
Comment: Many commenters referenced the ongoing litigation (described earlier in this section) in which the district court found that CMS exceeded its statutory authority by reducing payments for clinic visit services furnished in excepted off-campus PBDs as a method to control what we believe are unnecessary increases in the volume of those services. Several comments suggested that the continued implementation of this policy should be suspended until the ongoing litigation is adjudicated. They stated that “CMS should not take in further reductions in the clinic payments for off-campus PBDs in CY 2020 or future years until the matter is resolved.”
Commenters also submitted suggestions on how CMS might remedy payments following the district court's order vacating the portion of the CY 2019 OPPS/ASC final rule with comment period that adopted the volume control method for clinic visits. Some suggested that CMS must “make whole with interest” affected PBDs. Others recommended that CMS “make a lump sum payment to the facilities that were subject to the 2019 payment cut” and requested that “no additional copayment be required from patients” should CMS apply a retroactive remedy. One commenter suggested that “CMS provide as a remedy a lump sum payment to hospitals for the difference that would have been paid had the rule not been implemented.” Some commenters stated that “the remedy should be completed at a hospital specific level, on a claim by claim basis,” so as to ensure hospitals are adequately paid for clinic visits.
Several commenters wrote in urging CMS to restore the higher payment rates (which they believed would be consistent with the district court decision), promptly repay hospitals for the 2019 payment cuts, and abandon the second phase of the payment cut for 2020. Many noted that should the agency move forward with the second phase of the cut, it would cause additional harm to many hospitals, and they intended to continue pursuing legal remedies.
Another commenter suggested that while the court remanded to CMS the issue of remediation of cuts that occurred since January 1, 2019, they believe “at a minimum, the final rule should reflect the court decision and address the 30 percent cut implemented for calendar year 2019 and ensure the cuts are not finalized for 2020.”
Response: We thank the commenters for their suggestions.
As noted above, on September 23, 2019, HHS filed a motion requesting that the district court modify its order to remand the matter without vacatur or alternatively, to stay the portion of the order vacating the rule for 60 days from the date of the order to allow the Solicitor General time to determine whether to authorize appeal. This motion was denied on October 21, 2019. As we stated above, the government has appeal rights and is still evaluating the rulings and considering, at the time of this writing, whether to appeal from the final judgment. For CY 2020, CMS will be going forward with the phase-in. We respectfully disagree with the district court and continue to believe the Secretary has the authority to address unnecessary increases in the volume of outpatient services. CMS is still considering how we would remedy hospitals if we either do not appeal this ruling or do not succeed on appeal if one is so authorized.
Comment: One commenter suggested that even with the recent court decision CMS should “explore regulatory pathways to address site of service payment differentials in a budget neutral manner.” Commenters gave the example of “prospectively chang[ing] the manner in which hospitals allocate costs to outpatient cost centers in institutional cost reports, particularly for cost centers where similar services can be provided in physician offices which have no comparable overhead costs.” Another commenter expressed that “[p]atients should not be penalized and pay higher prices simply because a hospital owns the medical practice where they receive care.” The commenter encouraged CMS to “pursue a staunch defense of this proposal including, but not limited to, the appeal of recent court rulings that undermine these changes.” The commenter went on to say that CMS should “take the necessary steps to protect its authority to implement the second year of the two-year phase-in while the Agency takes an appeal to the D.C. Circuit.”
Response: We thank the commenters for their submissions and support of this policy. After consideration of public comments we received, we will be completing the phase-in of the application of the reduction in payment for HCPCS code G0463. Specifically, for CY 2020, we will apply the full amount of the reduction in payment that is applied if these departments (departments that bill the modifier “PO” on claims lines) are paid the site-specific PFS rate for the clinic visit service described by HCPCS code G0463. The PFS-equivalent rate for CY 2020 is 40 percent of the proposed OPPS payment (that is, 60 percent less than the proposed OPPS rate). Under this policy, departments will be paid approximately 40 percent of the OPPS rate (100 percent of the OPPS rate minus the 60-percent payment reduction that is applied in CY 2020) for the clinic visit service in CY 2020. Considering the effects of estimated changes in enrollment, utilization, and case-mix, this policy results in an estimated CY 2020 savings of approximately $800 million, with approximately $640 million of the savings accruing to Medicare, and approximately $160 million saved by Medicare beneficiaries in the form of reduced copayments, when compared to if the policy were not applied. We will continue to monitor the effect of this change in Medicare payment policy, including the volume of these types of OPD services. We also will continue to evaluate this policy in light of the litigation and judicial decision as they may arise.
XI. CY 2020 OPPS Payment Status and Comment Indicators
A. CY 2020 OPPS Payment Status Indicator Definitions
Payment status indicators (SIs) that we assign to HCPCS codes and APCs serve an important role in determining payment for services under the OPPS. They indicate whether a service represented by a HCPCS code is payable under the OPPS or another payment system, and also, whether particular OPPS policies apply to the code.
For CY 2020, we did not propose to make any changes to the definitions of status indicators that were listed in Addendum D1 to the CY 2019 OPPS/ASC final rule with comment period available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices-Items/CMS-1717-P.html?DLPage=1&DLEntries=10&10DLSort=2DLSortDir=descending.
We did not receive any public comments on the proposed 2020 definitions of the OPPS status indicators. We believe that the existing definitions of the OPPS status indicators will continue to be appropriate for CY 2020. Therefore, we are finalizing our proposed policy without modifications.
The complete list of the payment status indicators and their definitions that apply for CY 2020 is displayed in Addendum D1 to this final rule with comment period, which is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
The CY 2020 payment status indicator assignments for APCs and HCPCS codes are shown in Addendum A and Addendum B, respectively, to this final rule with comment period, which are available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
B. CY 2020 Comment Indicator Definitions
In the proposed rule, we proposed to use four comment indicators for the CY 2020 OPPS. These comment indicators, “CH”, “NC”, “NI”, and “NP”, are in effect for CY 2019 and we proposed to continue their use in CY 2020. The CY 2020 OPPS comment indicators are as follows:
- “CH”—Active HCPCS code in current and next calendar year, status indicator and/or APC assignment has changed; or active HCPCS code that will be discontinued at the end of the current calendar year.
- “NC”—New code for the next calendar year or existing code with substantial revision to its code descriptor in the next calendar year, as compared to current calendar year for which we requested comments in the proposed rule, final APC assignment; comments will not be accepted on the final APC assignment for the new code.
- “NI”—New code for the next calendar year or existing code with substantial revision to its code descriptor in the next calendar year, as compared to current calendar year, interim APC assignment; comments will be accepted on the interim APC assignment for the new code.
- “NP”—New code for the next calendar year or existing code with substantial revision to its code descriptor in the next calendar year, as compared to current calendar year, proposed APC assignment; comments will be accepted on the proposed APC assignment for the new code.
The definitions of the OPPS comment indicators for CY 2020 are listed in Addendum D2 to this final rule with comment period, which is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html.
We did not receive any public comments on the proposed use of comment indicators for CY 2020. We believe that the CY 2019 definitions of the OPPS comment indicators continue to be appropriate for CY 2020. Therefore, we are continuing to use those definitions without modification for CY 2020.
XII. MedPAC Recommendations
The Medicare Payment Advisory Commission (MedPAC) was established under section 1805 of the Act in large part to advise the U.S. Congress on issues affecting the Medicare program. As required under the statute, MedPAC submits reports to the Congress no later than March and June of each year that present its Medicare payment policy recommendations. The March report typically provides discussion of Medicare payment policy across different payment systems and the June report typically discusses selected Medicare issues. We are including this section to make stakeholders aware of certain MedPAC recommendations for the OPPS and ASC payment systems as discussed in its March 2019 report.
A. OPPS Payment Rates Update
The March 2019 MedPAC “Report to the Congress: Medicare Payment Policy,” recommended that Congress update Medicare OPPS payment rates by 2 percent, with the difference between this and the update amount specified in current law to be used to increase payments in a new suggested Medicare quality program, the “Hospital Value Incentive Program (HVIP).” We refer readers to the March 2019 report for a complete discussion on these recommendations, which is available for download at www.medpac.gov. We appreciate MedPAC's recommendations, but as MedPAC acknowledged in its March 2019 report, Congress would need to change current law to enable us to implement its recommendations. MedPAC did not comment on the proposed OPPS payment rate update. Comments received from MedPAC for other OPPS policies are discussed in the applicable sections of this rule.
B. ASC Conversion Factor Update
In the March 2019 MedPAC “Report to the Congress: Medicare Payment Policy”, MedPAC found that, based on its analysis of indicators of payment adequacy, the number of Medicare-certified ASCs had increased, beneficiaries' use of ASCs had increased, and ASC access to capital has been adequate.[80] As a result, for CY 2020, MedPAC stated that payments to ASCs are adequate and recommended that no payment update should be given for 2020 (that is, the update factor would be 0 percent).
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59079), we adopted a policy, which we codified at 42 CFR 416.171(a)(2), to apply the hospital market basket update to ASC payment system rates for an interim period of 5 years. We refer readers to the CY 2019 OPPS/ASC final rule with comment period for complete details regarding our policy to use the hospital market basket update for the ASC payment system. Therefore, consistent with our policy for the ASC payment system, in the CY 2020 OPPS/ASC proposed rule, we proposed to apply a 2.7 percent MFP-adjusted hospital market basket update factor to the CY 2019 ASC conversion factor for ASCs meeting the quality reporting requirements to determine the CY 2020 ASC payment amounts.
Comment: MedPAC reiterated their previous comments in their March 2019 report; specifically, that they do not support using the hospital market basket index as an interim method for updating the ASC conversion factor because evidence indicates the hospital market basket index does not accurately reflect the cost of providing services in the ASC setting.
Response: We believe providing ASCs with the same rate update mechanism as hospitals could encourage the migration of appropriate services from the hospital setting to the ASC setting and increase the presence of ASCs in health care markets or geographic areas where previously there were none or few, thus promoting better beneficiary access to care. As published in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42343), based on IGI's 2019 second quarter forecast with historical data through the first quarter of 2019, the hospital market basket update is 3.0 percent, and the MFP adjustment is 0.4 percentage point. Therefore, for this CY 2020 OPPS/ASC final rule with comment period we are finalizing the application of a 2.6 percent MFP-adjusted hospital market basket update factor to the CY 2019 ASC conversion factor for ASCs meeting the quality reporting requirements to determine the CY 2020 ASC payment amounts, as discussed at section XXVI of this final rule with comment period.
C. ASC Cost Data
In the March 2019 MedPAC “Report to the Congress on Medicare Payment Policy”, MedPAC recommended that Congress require ASCs to report cost data to enable the Commission to examine the growth of ASCs' costs over time and analyze Medicare payments relative to the costs of efficient providers, and that CMS could use ASC cost data to examine whether an existing Medicare price index is an appropriate proxy for ASC costs or an ASC specific market basket should be developed. Further, MedPAC suggested that CMS could limit the scope of the cost reporting system to minimize administrative burden on ASCs and the program.[81]
Comment: MedPAC reiterated their previous comments in their March 2019 report and requested that CMS use available authority to act quickly in gathering ASC cost data to inform ASC input costs and determine whether an existing Medicare price index is an appropriate proxy for ASC costs or whether an ASC-specific market basket index should be developed. Additionally, MedPAC asserts there is sufficient evidence that ASCs are capable of submitting cost data to CMS.
Response: We did not propose any cost reporting requirements for ASCs in the CY 2020 OPPS/ASC proposed rule and are not finalizing any cost reporting requirements for ASCs in this final rule.
The full March 2019 MedPAC Report to Congress can be downloaded from MedPAC's website at: http://www.medpac.gov.
XIII. Updates to the Ambulatory Surgical Center (ASC) Payment System
A. Background
1. Legislative History, Statutory Authority, and Prior Rulemaking for the ASC Payment System
For a detailed discussion of the legislative history and statutory authority related to payments to ASCs under Medicare, we refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74377 through 74378) and the June 12, 1998 proposed rule (63 FR 32291 through 32292). For a discussion of prior rulemaking on the ASC payment system, we refer readers to the CYs 2012, 2013, 2014, 2015, 2016, 2017, 2018 and 2019 OPPS/ASC final rules with comment period (76 FR 74378 through 74379; 77 FR 68434 through 68467; 78 FR 75064 through 75090; 79 FR 66915 through 66940; 80 FR 70474 through 70502; 81 FR 79732 through 79753; 82 FR 59401 through 59424; and 83 FR 59028 through 59080, respectively).
2. Policies Governing Changes to the Lists of Codes and Payment Rates for ASC Covered Surgical Procedures and Covered Ancillary Services
Under 42 CFR 416.2 and 42 CFR 416.166 of the Medicare regulations, subject to certain exclusions, covered surgical procedures in an ASC are surgical procedures that are separately paid under the OPPS, that would not be expected to pose a significant risk to beneficiary safety when performed in an ASC, and for which standard medical practice dictates that the beneficiary would not typically be expected to require active medical monitoring and care at midnight following the procedure (“overnight stay”). We adopted this standard for defining which surgical procedures are covered under the ASC payment system as an indicator of the complexity of the procedure and its appropriateness for Medicare payment in ASCs. We use this standard only for purposes of evaluating procedures to determine whether or not they are appropriate to be furnished to Medicare beneficiaries in ASCs. Historically, we have defined surgical procedures as those described by Category I CPT codes in the surgical range from 10000 through 69999 as well as those Category III CPT codes and Level II HCPCS codes that directly crosswalk or are clinically similar to procedures in the CPT surgical range that we have determined do not pose a significant safety risk, that we would not expect to require an overnight stay when performed in ASCs, and that are separately paid under the OPPS (72 FR 42478).
In the August 2, 2007 final rule (72 FR 42495), we also established our policy to make separate ASC payments for the following ancillary items and services when they are provided integral to ASC covered surgical procedures: (1) Brachytherapy sources; (2) certain implantable items that have pass-through payment status under the OPPS; (3) certain items and services that we designate as contractor-priced, including, but not limited to, procurement of corneal tissue; (4) certain drugs and biologicals for which separate payment is allowed under the OPPS; and (5) certain radiology services for which separate payment is allowed under the OPPS. In the CY 2015 OPPS/ASC final rule with comment period (79 FR 66932 through 66934), we expanded the scope of ASC covered ancillary services to include certain diagnostic tests within the medicine range of Current Procedural Terminology (CPT) codes for which separate payment is allowed under the OPPS when they are provided integral to an ASC covered surgical procedure. Covered ancillary services are specified in § 416.164(b) and, as stated previously, are eligible for separate ASC payment. Payment for ancillary items and services that are not paid separately under the ASC payment system is packaged into the ASC payment for the covered surgical procedure.
We update the lists of, and payment rates for, covered surgical procedures and covered ancillary services in ASCs in conjunction with the annual proposed and final rulemaking process to update the OPPS and the ASC payment system (§ 416.173; 72 FR 42535). We base ASC payment and policies for most covered surgical procedures, drugs, biologicals, and certain other covered ancillary services on the OPPS payment policies, and we use quarterly change requests (CRs) to update services covered under the OPPS. We also provide quarterly update CRs for ASC covered surgical procedures and covered ancillary services throughout the year (January, April, July, and October). We release new and revised Level II HCPCS codes and recognize the release of new and revised CPT codes by the American Medical Association (AMA) and make these codes effective (that is, the codes are recognized on Medicare claims) via these ASC quarterly update CRs. We recognize the release of new and revised Category III CPT codes in the July and January CRs. These updates implement newly created and revised Level II HCPCS and Category III CPT codes for ASC payments and update the payment rates for separately paid drugs and biologicals based on the most recently submitted ASP data. New and revised Category I CPT codes, except vaccine codes, are released only once a year, and are implemented only through the January quarterly CR update. New and revised Category I CPT vaccine codes are released twice a year and are implemented through the January and July quarterly CR updates. We refer readers to Table 41 in the CY 2012 OPPS/ASC proposed rule for an example of how this process, is used to update HCPCS and CPT codes, which we finalized in the CY 2012 OPPS/ASC final rule with comment period (76 FR 42291; 76 FR 74380 through 74384).
In our annual updates to the ASC list of, and payment rates for, covered surgical procedures and covered ancillary services, we undertake a review of excluded surgical procedures (including all procedures newly proposed for removal from the OPPS inpatient list), new codes, and codes with revised descriptors, to identify any that we believe meet the criteria for designation as ASC covered surgical procedures or covered ancillary services. Updating the lists of ASC covered surgical procedures and covered ancillary services, as well as their payment rates, in association with the annual OPPS rulemaking cycle is particularly important because the OPPS relative payment weights and, in some cases, payment rates, are used as the basis for the payment of many covered surgical procedures and covered ancillary services under the revised ASC payment system. This joint update process ensures that the ASC updates occur in a regular, predictable, and timely manner.
3. Definition of ASC Covered Surgical Procedures
Since the implementation of the ASC prospective payment system, we have historically defined a “surgical” procedure under the payment system as any procedure described within the range of Category I CPT codes that the CPT Editorial Panel of the AMA defines as “surgery” (CPT codes 10000 through 69999) (72 FR 42478). We also have included as “surgical,” procedures that are described by Level II HCPCS codes or by Category III CPT codes that directly crosswalk or are clinically similar to procedures in the CPT surgical range that we have determined do not pose a significant safety risk, would not expect to require an overnight stay when performed in an ASC, and that are separately paid under the OPPS (72 FR 42478).
As we noted in the August 7, 2007 final rule that implemented the revised ASC payment system, using this definition of surgery would exclude from ASC payment certain invasive, “surgery-like” procedures, such as cardiac catheterization or certain radiation treatment services that are assigned codes outside the CPT surgical range (72 FR 42477). We stated in that final rule that we believed continuing to rely on the CPT definition of surgery is administratively straightforward, is logically related to the categorization of services by physician experts who both establish the codes and perform the procedures, and is consistent with a policy to allow ASC payment for all outpatient surgical procedures (72 FR 42477).
However, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59029 through 59030), after consideration of public comments received in response to the CY 2019 OPPS/ASC proposed rule and earlier OPPS/ASC rulemaking cycles, we revised our definition of a surgical procedure under the ASC payment system. We now define a surgical procedure under the ASC payment system as any procedure described within the range of Category I CPT codes that the CPT Editorial Panel of the AMA defines as “surgery” (CPT codes 10000 through 69999) (72 FR 42476), as well as procedures that are described by Level II HCPCS codes or by Category I CPT codes or by Category III CPT codes that directly crosswalk or are clinically similar to procedures in the CPT surgical range that we have determined are not expected to pose a significant risk to beneficiary safety when performed in an ASC, for which standard medical practice dictates that the beneficiary would not typically be expected to require an overnight stay following the procedure, and are separately paid under the OPPS.
The comments and our responses to the comments are set forth below.
Comment: Commenters supported our revised definition and recommended that we modify our definition of an ASC covered surgical procedure for CY 2020 and subsequent years.
Response: We thank the commenters for their support. In review of the public comments we received, we realized that our modified definition of an ASC covered surgical procedure was initially finalized in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59029 through 59030) but that we only referenced CY 2019 and did not reference subsequent years. While we did not specifically propose to continue our modified definition of surgery for CY 2020 in the CY 2020 OPPS/ASC proposed rule, we did not propose to remove any procedures from the ASC list of covered surgical procedures that we had added as a result of our modified definition of a surgical procedure, and, therefore, we intended to continue our modified definition. For this final rule with comment period, after consideration of the public comments we are adopting a policy to continue to apply the modified definition of a surgical procedure for CY 2020, which was finalized for CY 2019 in our CY 2019 OPPS/ASC final rule with comment period (83 FR 59029 through 59030). We intend to address subsequent calendar years in future rulemaking.
B. ASC Treatment of New and Revised Codes
1. Background on Current Process for Recognizing New and Revised HCPCS Codes
Payment for ASC items and services are generally based on medical billing codes, specifically, HCPCS codes, that are reported on ASC claims. The HCPCS is divided into two principal subsystems, referred to as Level I and Level II of the HCPCS. Level I is comprised of CPT codes, a numeric and alphanumeric coding system maintained by the AMA, and includes Category I, II, and III CPT codes. Level II of the HCPCS, which is maintained by CMS, is a standardized coding system that is used primarily to identify products, supplies, and services not included in the CPT codes. Together, Level I and II HCPCS codes are used to report procedures, services, items, and supplies under the ASC payment system. Specifically, we recognize the following codes on ASC claims:
- Category I CPT codes, which describe surgical procedures, diagnostic and therapeutic services, and vaccine codes;
- Category III CPT codes, which describe new and emerging technologies, services, and procedures; and
- Level II HCPCS codes (also known as alphanumeric codes), which are used primarily to identify drugs, devices, supplies, temporary procedures, and services not described by CPT codes.
We finalized a policy in the August 2, 2007 final rule (72 FR 42535) to evaluate each year all new HCPCS codes that describe surgical procedures, and to make preliminary determinations during the annual OPPS/ASC rulemaking process regarding whether or not they meet the criteria for payment in the ASC setting as covered surgical procedures and, if so, whether or not they are office-based procedures. In addition, we identify new and revised codes as ASC covered ancillary services based upon the final payment policies of the revised ASC payment system. In prior rulemakings, we refer to this process as recognizing new codes. However, this process has always involved the recognition of new and revised codes. We consider revised codes to be new when they have substantial revision to their code descriptors that necessitate a change in the current ASC payment indicator. To clarify, we refer to these codes as new and revised in this CY 2020 OPPS/ASC final rule with comment period.
We have separated our discussion below based on when the codes are released and whether we solicited public comments in the proposed rule (and respond to those comments in this CY 2020 OPPS/ASC final rule with comment period) or whether we are soliciting public comments in this CY 2020 OPPS/ASC final rule with comment period (and will respond to those comments in the CY 2021 OPPS/ASC final rule with comment period).
We note that we sought public comments in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59034 through 59035) on the new and revised Level II HCPCS codes effective October 1, 2018 or January 1, 2019. These new and revised codes were flagged with comment indicator “NI” in Addenda AA and BB to the CY 2019 OPPS/ASC final rule with comment period to indicate that we were assigning them an interim payment status and payment rate, if applicable, which were subject to public comment following publication of the CY 2019 OPPS/ASC final rule with comment period. In the CY 2019 OPPS/ASC proposed rule, we stated that we will finalize the treatment of these codes under the ASC payment system in this CY 2020 OPPS/ASC final rule with comment period.
2. April 2019 HCPCS Codes for Which We Solicited Public Comments in the Proposed Rule
For the April 2019 update, there were no new CPT codes, however, there were several new Level II HCPCS codes. In the April 2019 ASC quarterly update (Transmittal 4263, CR 11232, dated March 22, 2019), we added eight new Level II HCPCS codes to the list of covered ancillary services. Table 25 of the CY 2020 OPPS/ASC proposed rule displayed the new Level II HCPCS codes that were implemented on April 1, 2019, along with their proposed payment indicators for CY 2020.
We invited public comments on the proposed payment indicators and payment rates for the new HCPCS codes that were recognized as ASC ancillary services in April 2019 through the quarterly update CRs, as listed in Table 25 of the CY 2020 OPPS/ASC proposed rule. We proposed to finalize their payment indicators in the CY 2020 OPPS/ASC final rule with comment period.
We did not receive any public comments on the proposed ASC payment indicator assignments for the new Level II HCPCS codes implemented in April 2019. Therefore, we are finalizing the proposed ASC payment indicator assignments for these codes, as indicated in Table 50 below. We note that several of the temporary drug HCPCS C-codes have been replaced with permanent drug HCPCS J-codes, effective January 1, 2020. Their replacement codes are also listed in Table 50. The final payment rates for these codes can be found in Addendum BB to this final rule with comment period (which is available via the internet on the CMS website). In addition, the status indicator meanings can be found in Addendum DD1 to this final rule with comment period (which is available via the internet on the CMS website).

3. July 2019 HCPCS Codes for Which We Solicited Public Comments in the Proposed Rule
In the July 2019 ASC quarterly update (Transmittal 4076, Change Request 10788, dated June 14, 2019), we added several separately payable Category III CPT and Level II HCPCS codes to the list of covered surgical procedures and ancillary services. Table 26 of the CY 2020 OPPS/ASC proposed rule displayed the new HCPCS codes that were effective July 1, 2019.
In addition, through the July 2019 quarterly update CR, we also implemented an ASC payment for one new Category III CPT code as an ASC covered ancillary service, effective July 1, 2019. This code was listed in Table 27 of the CY 2020 OPPS/ASC proposed rule, along with the proposed comment indicator and payment indicator.
We invited public comments on these proposed payment indicators for the new Category III CPT code and Level II HCPCS codes newly recognized as ASC covered surgical procedures or covered ancillary services in July 2019 through the quarterly update CRs, as listed in Tables 25, 26, and 27 of the proposed rule.
We did not receive any other public comments on the proposed ASC payment indicator assignments for the new Category III CPT codes or Level II HCPCS codes implemented in July 2019. Therefore, we are finalizing the proposed ASC payment indicator assignments for these codes, as indicated in Table 51 and 52 below. We note that several of the HCPCS C-codes have been replaced with HCPCS J-codes, effective January 1, 2020. Their replacement codes are listed in Table 51. The final payment rates for these codes can be found in Addendum AA and BB to this final rule with comment period (which is available via the internet on the CMS website). In addition, the status indicator meanings can be found in Addendum DD1 to this final rule with comment period (which is available via the internet on the CMS website).


4. October 2019 HCPCS Codes for Which We Are Soliciting Public Comments in This CY 2020 OPPS/ASC Final Rule With Comment Period
In the past, we released new and revised HCPCS codes that are effective October 1 through the October OPPS quarterly update CRs and incorporated these new codes in the final rule with comment period.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39534), for CY 2020, consistent with our established policy, we proposed that the Level II HCPCS codes that will be effective October 1, 2019 would be flagged with comment indicator “NI” in Addendum BB to the CY 2020 OPPS/ASC final rule with comment period to indicate that we have assigned the codes an interim ASC payment indicator for CY 2020. We did not receive any public comments on our proposal. As we stated that we would do in the CY 2020 OPPS/ASC proposed rule, we are inviting public comments in this CY 2020 OPPS/ASC final rule with comment period on the interim ASC payment indicator for these codes that we intend to finalize in the CY 2021 OPPS/ASC final rule with comment period.
5. January 2020 HCPCS Codes
a. New Level II HCPCS Codes for Which We Are Soliciting Public Comments in the CY 2020 OPPS/ASC Final Rule With Comment Period
Consistent with past practice, we are soliciting comment on the new Level II HCPCS codes that are effective January 1, 2020 in the CY 2020 OPPS/ASC final rule with comment period, thereby updating the ASC payment system for the calendar year. These codes are released to the public via the CMS HCPCS website, and also through the January OPPS quarterly update CRs. We note that unlike the CPT codes that are effective January 1 and are included in the OPPS/ASC proposed rules, and except for the G-codes listed in Addendum O to the CY 2020 OPPS/ASC proposed rule, most Level II HCPCS codes are not released until November to be effective January 1. Because these codes are not available until November, we are unable to include them in the OPPS/ASC proposed rules. Therefore, these Level II HCPCS codes will be released to the public through the CY 2020 OPPS/ASC final rule with comment period, January 2020 ASC Update CR, and the CMS HCPCS website.
In addition, for CY 2020, we proposed to continue our established policy of assigning comment indicator “NI” in Addendum AA and Addendum BB to the CY 2020 OPPS/ASC final rule with comment period to the new Level II HCPCS codes that will be effective January 1, 2020 to indicate that we are assigning them an interim payment indicator, which is subject to public comment. We are inviting public comments in the CY 2020 OPPS/ASC final rule with comment period on the payment indicator assignments, which would then be finalized in the CY 2021 OPPS/ASC final rule with comment period.
b. CPT Codes for Which We Solicited Public Comments in the Proposed Rule
In the CY 2015 OPPS/ASC final rule with comment period (79 FR 66841 through 66844), we finalized a revised process of assigning APC and status indicators for new and revised Category I and III CPT codes that would be effective January 1. Specifically, for the new/revised CPT codes that we receive in a timely manner from the AMA's CPT Editorial Panel, we finalized our proposal to include the codes that would be effective January 1 in the OPPS/ASC proposed rules, along with proposed APC and status indicator assignments for them, and to finalize the APC and status indicator assignments in the OPPS/ASC final rules beginning with the CY 2016 OPPS update. For those new/revised CPT codes that were received too late for inclusion in the OPPS/ASC proposed rule, we finalized our proposal to establish and use HCPCS G-codes that mirror the predecessor CPT codes and retain the current APC and status indicator assignments for a year until we can propose APC and status indicator assignments in the following year's rulemaking cycle. We note that even if we find that we need to create HCPCS G-codes in place of certain CPT codes for the PFS proposed rule, we do not anticipate that these HCPCS G-codes will always be necessary for OPPS purposes. We will make every effort to include proposed APC and status indicator assignments for all new and revised CPT codes that the AMA makes publicly available in time for us to include them in the proposed rule, and to avoid the resort to HCPCS G-codes and the resulting delay in utilization of the most current CPT codes. Also, we finalized our proposal to make interim APC and status indicator assignments for CPT codes that are not available in time for the proposed rule and that describe wholly new services (such as new technologies or new surgical procedures), solicit public comments, and finalize the specific APC and status indicator assignments for those codes in the following year's final rule.
For the CY 2020 OPPS update, we received the CPT codes that will be effective January 1, 2020 from AMA in time to be included in the proposed rule. The new, revised, and deleted CPT codes were listed in Addendum AA and Addendum BB to the CY 2020 OPPS/ASC proposed rule. We note that the new and revised CPT codes were assigned to comment indicator “NP” in Addendum AA and Addendum BB of the CY 2020 OPPS/ASC proposed rule to indicate that the code is new for the next calendar year or the code is an existing code with substantial revision to its code descriptor in the next calendar year as compared to current calendar year with a proposed ASC payment assignment, and that comments would be accepted on the proposed ASC payment indicator.
Further, we note that the CPT code descriptors that appeared in Addendum AA and BB were short descriptors and did not accurately describe the complete procedure, service, or item described by the CPT code. Therefore, we included the 5-digit placeholder codes and the long descriptors for the new and revised CY 2020 CPT codes in Addendum O to the proposed rule so that the public could adequately comment on the proposed ASC payment indicator assignments. The 5-digit placeholder codes were listed in Addendum O, specifically under the column labeled “CY 2020 OPPS/ASC Proposed Rule 5-Digit AMA Placeholder Code”. The final CPT code numbers are included in this CY 2020 OPPS/ASC final rule with comment period, and can be found in Addendum AA, Addendum BB, and Addendum O.
For new and revised CPT codes effective January 1, 2020 that were received in time to be included in the CY 2020 OPPS/ASC proposed rule, we proposed the appropriate payment indicator assignments, and solicited public comments on the payment assignments. We stated we would accept comments and finalize the payment indicators in this CY 2020 OPPS/ASC final rule with comment period. We note that we received comments on the ASC payment indicator for certain new CPT codes that will be effective January 1, 2020. These comments, and our responses, can be found in section XIII.C.1.a.(2). of this final rule with comment period.
Also, we note that we inadvertently omitted new CPT and new HCPCS codes effective January 1, 2020 from Table 32 (Proposed Additions to the List of ASC Covered Surgical Procedures for CY 2020) of the CY 2020 OPPS/ASC proposed rule (84 FR 39544), however, we included these 12 procedures in Addendum AA to the proposed rule. The procedures described by the 12 new CPT and HCPCS codes are displayed in Table 53 of this CY 2020 OPPS/ASC final rule with comment period.
Finally, shown in Table 28 of the CY 2020 OPPS/ASC proposed rule (84 FR 39565) and reprinted in Table 53 below, we summarize our process for updating codes through our ASC quarterly update CRs, seeking public comments, and finalizing the treatment of these new codes under the ASC.

C. Update to the List of ASC Covered Surgical Procedures and Covered Ancillary Services—
1. Covered Surgical Procedures
a. Covered Surgical Procedures Designated as Office-Based
(1) Background
In the August 2, 2007 ASC final rule, we finalized our policy to designate as “office-based” those procedures that are added to the ASC Covered Procedures List (CPL) in CY 2008 or later years that we determine are performed predominantly (more than 50 percent of the time) in physicians' offices based on consideration of the most recent available volume and utilization data for each individual procedure code and/or, if appropriate, the clinical characteristics, utilization, and volume of related codes. In that rule, we also finalized our policy to exempt all procedures on the CY 2007 ASC list from application of the office-based classification (72 FR 42512). The procedures that were added to the ASC CPL beginning in CY 2008 that we determined were office-based were identified in Addendum AA to that rule by payment indicator “P2” (Office-based surgical procedure added to ASC list in CY 2008 or later with MPFS nonfacility PE RVUs; payment based on OPPS relative payment weight); “P3” (Office-based surgical procedures added to ASC list in CY 2008 or later with MPFS nonfacility PE RVUs; payment based on MPFS nonfacility PE RVUs); or “R2” (Office-based surgical procedure added to ASC list in CY 2008 or later without MPFS nonfacility PE RVUs; payment based on OPPS relative payment weight), depending on whether we estimated the procedure would be paid according to the standard ASC payment methodology based on its OPPS relative payment weight or at the MPFS nonfacility PE RVU-based amount.
Consistent with our final policy to annually review and update the ASC CPL to include all covered surgical procedures eligible for payment in ASCs, each year we identify covered surgical procedures as either temporarily office-based (these are new procedure codes with little or no utilization data that we have determined are clinically similar to other procedures that are permanently office-based), permanently office-based, or non office-based, after taking into account updated volume and utilization data.
(2) Changes for CY 2020 to Covered Surgical Procedures Designated as Office-Based
In developing the CY 2020 OPPS/ASC proposed rule, we followed our policy to annually review and update the covered surgical procedures for which ASC payment is made and to identify new procedures that may be appropriate for ASC payment, including their potential designation as office-based. We reviewed CY 2018 volume and utilization data and the clinical characteristics for all covered surgical procedures that are assigned payment indicator “G2” (Nonoffice-based surgical procedure added in CY 2008 or later; payment based on OPPS relative payment weight) in CY 2018, as well as for those procedures assigned one of the temporary office-based payment indicators, specifically “P2”, “P3”, or “R2” in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59039 through 59040).
Our review of the CY 2018 volume and utilization data resulted in our identification of 9 covered surgical procedures that we believed met the criteria for designation as permanently office-based. We understood the data to indicate that these procedures are performed more than 50 percent of the time in physicians' offices, and we believed that the services are of a level of complexity consistent with other procedures performed routinely in physicians' offices. The CPT codes that we proposed to permanently designate as office-based for CY 2020 were listed in Table 29 of the CY 2020 OPPS/ASC proposed rule, which is reprinted below as Table 54.


As we stated in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59036), the office-based utilization for CPT codes 36902 and 36905 (dialysis vascular access procedures) was greater than 50 percent. However, we did not designate CPT codes 36902 and 36905 as office-based procedures for CY 2019. These codes became effective January 1, 2017 and CY 2017 was the first year we had claims volume and utilization data for CPT codes 36902 and 36905. We shared commenters' concerns that the available data were not adequate to make a determination that these procedures should be office-based, and believed it was premature to assign office-based payment status to those procedures for CY 2019. For CY 2019, CPT codes 36902 and 36905 were assigned payment indicators of “G2”—Non office-based surgical procedure added in CY 2008 or later; payment based on OPPS relative weight.
In reviewing the CY 2018 volume and utilization data for CPT code 36902 we determined that the procedure was performed more than 50 percent of the time in physicians' offices based on 2018 volume and utilization data.
However, the office-based utilization for CPT code 36902 has fallen from 62 percent based on 2017 data to 52 percent based on 2018 data. In addition, there was a sizeable increase in claims for this service in ASCs—from approximately 14,000 in 2017 to 38,000 in 2018. As previously stated in the CY 2019 OPPS/ASC final rule (83 FR 59036), when we believe that the available data for our review process are inadequate to make a determination that a procedure should be office-based, we either make no change to the procedure's payment status or make the change on a temporary basis, and reevaluate our decision when more data become available for our next evaluation. In light of these changes in utilization and due to the high utilization of this procedure in all settings (over 125,000 claims in 2018), we believe it may be premature to assign office-based payment status to CPT code 36902 at this time.
Therefore, for CY 2020, we did not propose to designate CPT code 36902 as an office-based procedure, but proposed to continue to assign CPT code 36902 a payment indicator of “G2”—nonoffice-based surgical procedure paid based on OPPS relative weights.
The CY 2018 volume and utilization data for CPT code 36905 show the procedure was not performed more than 50 percent of the time in physicians' offices. Therefore, in the CY 2020 OPPS/ASC proposed rule, we did not propose to assign an office-based designation for CPT code 36905. Therefore the procedure will retain its payment indicator of “G2”—non office-based surgical procedure based on OPPS relative weights.
The comments and our responses to the comment are set forth below.
Comment: Commenters supported our decision to refrain from proposing to designate CPT code 36902 as an office-based procedure and to continue to assign both CPT codes 36902 and 36905 a payment indicator of “G2”—nonoffice-based surgical procedure paid based on OPPS relative weights.
Response: We thank commenters for their support of our proposal. After reviewing the public comments we received, we are finalizing our proposal to assign CPT code 36902 a payment indicator of “G2”—nonoffice-based surgical procedure paid based on OPPS relative weights.
Comment: Some commenters suggested that CPT codes 31634, 31647, 50727, 59414, and 61880 should not be designated as office-based procedures and that the level of complexity is not consistent with other procedures performed routinely in physicians' offices
Response: We agree with the commenters. We inadvertently proposed to assign office-based designations to CPT codes 31634, 31647, 50727, 59414, and 61880. The volume and utilization data for these procedures do not suggest the procedures are performed more than 50 percent of the time in physicians' offices, and we do not believe that the services are of a level of complexity consistent with other procedures performed routinely in physicians' offices. Therefore, CPT codes 31634, 50727, 59414, 61880 are assigned payment indicators “G2”—non office-based surgical procedure based on OPPS relative weights—for CY 2020. Additionally, as CPT code 31647 exceeds our device offset percentage threshold of 30 percent for device-intensive designation, we are assigning this procedure a payment indicator of “J8”—device-intensive procedure; paid at adjusted rate—for CY 2020. These procedures and their assigned payment indicators can be found in Addendum AA to the CY 2020 OPPS/ASC final rule with comment period (which is available via the internet on the CMS website).
After consideration of the public comments we received, we are finalizing our proposal with modification, to designate the four ASC covered surgical procedures in Table 55 as permanently office-based for CY 2020 and subsequent years.

We also reviewed CY 2018 volume and utilization data and other information for 12 procedures designated as temporarily office-based in Tables 57 and 58 in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59039 through 59040). Of these 12 procedures, there were very few claims in our data and no claims data for 11 procedures described by CPT codes 10005, 10007, 10009, 10011, 11102, 11104, 11106, 65785, 67229, 0402T and 0512T. Consequently, we proposed to maintain the temporary office-based designations for these 11 CPT codes for CY 2020. The procedures for which the proposed office-based designations for CY 2020 are temporary are also indicated by asterisks in Addendum AA to the proposed and final rule (which are available via the internet on the CMS website).
The volume and utilization data for the one remaining procedure that has a temporary office-based designation for CY 2019, described by CPT code 38222 (Diagnostic bone marrow; biopsy(ies) and aspiration(s)), are sufficient to indicate that this covered surgical procedures was not performed predominantly in physicians' offices and, therefore, we proposed to assign a nonoffice-based payment indicator—“G2”—to this code for CY 2020.
We did not receive any public comments on our proposal. Therefore, we are finalizing our proposal, without modification, to designate the procedures shown in Table 56 below as temporarily office-based. The procedures for which the office-based designation for CY 2020 is temporary are indicated by an asterisk in Addendum AA to this final rule with comment period (which is available via the internet on the CMS website).


For CY 2020, we proposed to designate 7 new CY 2020 CPT codes for ASC covered surgical procedures as temporarily office-based, as displayed in Table P31X. After reviewing the clinical characteristics, utilization, and volume of related procedure codes, we determined that the procedures in Table 30 of the CY 2020 OPPS/ASC proposed rule described by the new CPT codes would be predominantly performed in physicians' offices. We stated that we believed the procedure described by CPT codes 93X00 (Duplex scan of arterial inflow and venous outflow for preoperative vessel assessment prior to creation of hemodialysis access; complete bilateral study) and 93X01 (Duplex scan of arterial inflow and venous outflow for preoperative vessel assessment prior to creation of hemodialysis access; complete unilateral study) was clinically similar to HCPCS code G0365 (Vessel mapping of vessels for hemodialysis access (services for preoperative vessel mapping prior to creation of hemodialysis access using an autogenous hemodialysis conduit, including arterial inflow and venous outflow)), which is currently on the list of covered surgical procedures and assigned a proposed payment indicator “R2”—Office-based surgical procedure added to ASC list in CY 2008 or later without MPFS nonfacility PE RVUs; payment based on OPPS relative payment weight—for CY 2020. As such, we proposed to add CPT codes 93X00 and 93X01 in Table 30 of the CY 2020 OPPS/ASC proposed rule to the list of temporarily office-based covered surgical procedures.
Because we have no utilization data for the procedures specifically described by these new CPT codes, we proposed to make the office-based designation temporary rather than permanent, and we will reevaluate the procedures when data become available. The procedures for which the proposed office-based designation for CY 2020 is temporary are indicated by asterisks in Addendum AA to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website).
We did not receive any public comments on our proposal. Therefore, we are finalizing our proposal, without modification, to designate the procedures shown in Table 57 below as temporarily office-based. The procedures for which the office-based designation for CY 2020 is temporary are indicated by an asterisk in Addendum AA to this final rule with comment period (which is available via the internet on the CMS website).


b. ASC Covered Surgical Procedures To Be Designated as Device-Intensive
(1) Background
We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59040 through 59041), for a summary of our existing policies regarding ASC covered surgical procedures that are designated as device-intensive.
(2) Changes to List of ASC Covered Surgical Procedures Designated as Device-Intensive for CY 2020
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 590401 through 59043), for CY 2019, we modified our criteria for device-intensive procedures to better capture costs for procedures with significant device costs. We adopted a policy to allow procedures that involve surgically inserted or implanted, high-cost, single-use devices to qualify as device-intensive procedures. In addition, we modified our criteria to lower the device offset percentage threshold from 40 percent to 30 percent. Specifically, for CY 2019 and subsequent years, we adopted a policy that device-intensive procedures would be subject to the following criteria:
- All procedures must involve implantable devices assigned a CPT or HCPCS code;
- The required devices (including single-use devices) must be surgically inserted or implanted; and
- The device offset amount must be significant, which is defined as exceeding 30 percent of the procedure's mean cost. Corresponding to this change in the cost criterion we adopted a policy that the default device offset for new codes that describe procedures that involve the implantation of medical devices will be 31 percent beginning in CY 2019. For new codes describing procedures that are payable when furnished in an ASC involving the implantation of a medical device, we adopted a policy that the default device offset would be applied in the same manner as the policy we adopted in section IV.B.2. of the CY 2019 OPPS/ASC final rule with comment period (83 FR 58944 through 58948). We amended § 416.171(b)(2) of the regulations to reflect these new device criteria.
In addition, as also adopted in section IV.B.2. of CY 2019 OPPS/ASC final rule with comment period, to further align the device-intensive policy with the criteria used for device pass-through status, we specified, for CY 2019 and subsequent years, that for purposes of satisfying the device-intensive criteria, a device-intensive procedure must involve a device that:
- Has received Food and Drug Administration (FDA) marketing authorization, has received an FDA investigational device exemption (IDE) and has been classified as a Category B device by the FDA in accordance with 42 CFR 405.203 through 405.207 and 405.211 through 405.215, or meets another appropriate FDA exemption from premarket review;
- Is an integral part of the service furnished;
- Is used for one patient only;
- Comes in contact with human tissue;
- Is surgically implanted or inserted (either permanently or temporarily); and
- Is not any of the following:
++ Equipment, an instrument, apparatus, implement, or item of this type for which depreciation and financing expenses are recovered as depreciable assets as defined in Chapter 1 of the Medicare Provider Reimbursement Manual (CMS Pub. 15-1); or
++ A material or supply furnished incident to a service (for example, a suture, customized surgical kit, scalpel, or clip, other than a radiological site marker).
Based on our modified device-intensive criteria, for CY 2020, we proposed to update the ASC CPL to indicate procedures that are eligible for payment according to our device-intensive procedure payment methodology, based on the proposed individual HCPCS code device-offset percentages using the CY 2018 OPPS claims and cost report data available for the CY 2020 OPP/ASC proposed rule.
The ASC covered surgical procedures that we proposed to designate as device-intensive, and therefore subject to the device-intensive procedure payment methodology for CY 2020, are assigned payment indicator “J8” and are included in ASC Addendum AA to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website). The CPT code, the CPT code short descriptor, and the proposed CY 2020 ASC payment indicator, and an indication of whether the full credit/partial credit (FB/FC) device adjustment policy would apply because the procedure is designated as device-intensive are also included in Addendum AA to the proposed rule (which is available via the internet on the CMS website). In addition, we note that in our CY 2019 OPPS/ASC proposed rule (83 FR 37158 through 37159), we proposed to apply our device-intensive procedure payment methodology to device-intensive procedures under the ASC payment system only when the device-intensive procedure is furnished with a surgically-inserted or implanted device (including single-used medical devices). We inadvertently omitted language finalizing this policy for CY 2019. For CY 2020 and subsequent calendar years, we proposed to only apply our device-intensive procedure payment methodology to device-intensive procedures under the ASC payment system when the device-intensive procedure is furnished with a surgically inserted or implanted device (including single use medical devices). The payment rate under the ASC payment system for device-intensive procedures furnished with an implantable or inserted medical device would be calculated by applying the device offset percentage based on the standard OPPS APC ratesetting methodology to the OPPS national unadjusted payment to determine the device cost included in the OPPS payment rate for a device intensive ASC covered surgical procedure, which we then set as equal to the device portion of the national unadjusted ASC payment rate for the procedure. We calculate the service portion of the ASC payment for device intensive procedures by applying the uniform ASC conversion factor to the service (non-device) portion of the OPPS relative payment weight for the device-intensive procedure. Finally, we sum the ASC device portion and ASC service portion to establish the full payment for the device-intensive procedure under the revised ASC payment system. (82 FR 59409)
The comments and our responses to the comments are set forth below.
Comment: Commenters continued to support the policy we implemented last year to lower the device offset percentage threshold to 30 percent for purposes of designating device-intensive procedures.
Response: We thank commenters for their support.
Comment: Some commenters requested that device implants, which we interpret to mean surgically inserted or implanted, single-use devices, be included in ASC payment at invoice price based on manufacturer reported pricing or at device pass-through payment as described in section IV.A of this final rule with comment period so that the payment rate for these device-intensive procedures would more appropriately reflect the cost of care and encourage migration from the more expensive hospital setting to the ASC setting.
Response: We thank the commenters for their recommendation. As discussed in this section, the ASC payment rate for surgical procedures includes payment for device costs, which are packaged into the procedure payment. For device-intensive procedures and procedures using pass-through devices, the device portion is held equal to the device portion under the OPPS using the standard ratesetting methodology. We believe this methodology provides consistency with device-intensive policies under the OPPS and provides an appropriate payment for the device costs for device-intensive procedures in the ASC setting.
Comment: Some commenters stated that we calculate the device portions of a service in two ways. The first, using the device offset from APC payment rates developed under the comprehensive ratesetting methodology, and, the second using the device offset from the APC payment rates developed under the standard (non-comprehensive) ratesetting methodology. Commenters requested that we designate device-intensive procedures using only our standard (non-comprehensive) ratesetting methodology for determining whether the cost of a device exceeds our device-intensive threshold of 30 percent as they believed that method is more consistent with the overall ASC payment system.
Response: As we stated in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66924), under 42 CFR 416.167 and 416.171, most ASC payment rates are based on the OPPS relative payment weights, and our ASC policy with respect to device-intensive procedures is designed to be consistent with the OPPS. “Device-intensive” identifies those procedures with significant device costs and applies to services that are performed both in the hospital outpatient department and the ASC setting. We believe that the device-intensive methodology for ASCs should align with the device-intensive policies for OPPS, and, therefore, procedures should not be device-intensive in the ASC setting if they are not device-intensive in the hospital outpatient setting. The device offset percentage for device-intensive procedures under the OPPS are based on the comprehensive ratesetting methodology. However, to be assigned device-intensive status in the ASC setting, the procedure must be identified as device-intensive in the hospital outpatient setting and have a device offset percentage exceeds the 30 percent threshold as calculated using our standard ratesetting methodology as stated in 42 CFR 416.171(b)(2). Additionally, for purposes of the ASC payment system, the device amount is calculated by applying the device offset percentage calculated under our standard ratesetting methodology to the APC payment weights calculated under our standard ratesetting methodology.
Comment: One commenter requested that we re-evaluate the device-intensive designation for CPT code 22869 (Insertion of interlaminar/interspinous process stabilization/distraction device, without open decompression or fusion, including image guidance when performed, lumbar; single level). The commenter stated the ASC payment rate was too low to reflect the cost of the device in ASCs in California, and, therefore, the device offset should be increased.
Response: After reviewing the most recently available claims data for the CY 2020 OPPS/ASC final rule with comment period, CPT code 22869 has a device offset percentage of 74.0 percent and a device offset amount of $8,383.12. The offset percentage increased by 2.9 percentage points from 71.1 percent in the CY 2020 OPPS/ASC proposed rule and the device offset amount increased by 3.0 percent from $8,141.12. We note that device cost information for CPT code 22869 has only been available from CY 2017 claims (for CY 2019 ratesetting) and CY 2018 claims (for CY 2020 ratesetting) and therefore we are unable to draw any historical comparisons to determine if the CY 2020 device offset is inconsistent with historical device offsets for this procedure. For this CY 2020 OPPS/ASC final rule with comment period, the device cost of $8,383.12 for CPT code 22869 is based on 372 claims and we believe represents our best estimate of the cost of devices for performing the surgical procedure in CY 2020. Further, we note that 50 percent of the final ASC payment rate (both the device portion and non-device portion) is adjusted by the ASC wage index to reflect variation in labor costs. We believe the ASC payment rate for CPT code 22869 provides an appropriate payment for both device and non-device costs for facilities in all areas of the country.
Comment: One commenter requested that CPT code 50590 (Lithotripsy, extracorporeal shock wave) be assigned device-intensive status.
Response: We thank the commenter for its request. Based on the most recently available claims data for this CY 2020 OPPS/ASC final rule with comment period, the device offset percentage for CPT code 50590 continues to be below the 30 percent threshold and, therefore, is ineligible to be assigned device-intensive status.
c. Adjustment to ASC Payments for No Cost/Full Credit and Partial Credit Devices
Our ASC payment policy for costly devices implanted in ASCs at no cost/full credit or partial credit, as set forth in § 416.179 of our regulations, is consistent with the OPPS policy that was in effect until CY 2014. Specifically, the OPPS policy that was in effect through CY 2013 provided a reduction in OPPS payment by 100 percent of the device offset amount when a hospital furnishes a specified device without cost or with a full credit and by 50 percent of the device offset amount when the hospital receives partial credit in the amount of 50 percent or more of the cost for the specified device (77 FR 68356 through 68358). The established ASC policy reduces payment to ASCs when a specified device is furnished without cost or with full credit or partial credit for the cost of the device for those ASC covered surgical procedures that are assigned to APCs under the OPPS to which this policy applies. We refer readers to the CY 2009 OPPS/ASC final rule with comment period (73 FR 68742 through 68744) for a full discussion of the ASC payment adjustment policy for no cost/full credit and partial credit devices.
In the CY 2019 OPPS/ASC proposed rule (83 FR 37159), we noted that, as discussed in section IV.B. of the CY 2014 OPPS/ASC final rule with comment period (78 FR 75005 through 75006), we finalized our proposal to modify our former policy of reducing OPPS payment for specified APCs when a hospital furnishes a specified device without cost or with a full or partial credit. Formerly, under the OPPS, our policy was to reduce OPPS payment by 100 percent of the device offset amount when a hospital furnished a specified device without cost or with a full credit and by 50 percent of the device offset amount when the hospital received partial credit in the amount of 50 percent or more (but less than 100 percent) of the cost for the specified device. For CY 2014, we finalized our proposal to reduce OPPS payment for applicable APCs by the full or partial credit a provider receives for a replaced device, capped at the device offset amount.
Although we finalized our proposal to modify the policy of reducing payments when a hospital furnishes a specified device without cost or with full or partial credit under the OPPS, in the CY 2014 OPPS/ASC final rule with comment period (78 FR 75076 through 75080), we finalized our proposal to maintain our ASC policy for reducing payments to ASCs for specified device-intensive procedures when the ASC furnishes a device without cost or with full or partial credit. Unlike the OPPS, there is currently no mechanism within the ASC claims processing system for ASCs to submit to CMS the actual credit received when furnishing a specified device at full or partial credit. Therefore, under the ASC payment system, we finalized our proposal for CY 2014 to continue to reduce ASC payments by 100 percent or 50 percent of the device offset amount when an ASC furnishes a device without cost or with full or partial credit, respectively.
All ASC covered device-intensive procedures are subject to the no cost/full credit and partial credit device adjustment policy. Specifically, when a device-intensive procedure is performed to implant a device that is furnished at no cost or with full credit from the manufacturer, the ASC would append the HCPCS “FB” modifier on the line in the claim with the procedure to implant the device. The contractor would reduce payment to the ASC by the device offset amount that we estimate represents the cost of the device when the necessary device is furnished without cost or with full credit to the ASC. We continue to believe that the reduction of ASC payment in these circumstances is necessary to pay appropriately for the covered surgical procedure furnished by the ASC.
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59043 through 59044), for partial credit, we adopted a policy to reduce the payment for a device-intensive procedure for which the ASC receives partial credit by one-half of the device offset amount that would be applied if a device was provided at no cost or with full credit, if the credit to the ASC is 50 percent or more (but less than 100 percent) of the cost of the new device. The ASC will append the HCPCS “FC” modifier to the HCPCS code for the device-intensive surgical procedure when the facility receives a partial credit of 50 percent or more (but less than 100 percent) of the cost of a device. To report that the ASC received a partial credit of 50 percent or more (but less than 100 percent) of the cost of a new device, ASCs have the option of either: (1) Submitting the claim for the device replacement procedure to their Medicare contractor after the procedure's performance, but prior to manufacturer acknowledgment of credit for the device, and subsequently contacting the contractor regarding a claim adjustment, once the credit determination is made; or (2) holding the claim for the device implantation procedure until a determination is made by the manufacturer on the partial credit and submitting the claim with the “FC” modifier appended to the implantation procedure HCPCS code if the partial credit is 50 percent or more (but less than 100 percent) of the cost of the replacement device. Beneficiary coinsurance would be based on the reduced payment amount. As finalized in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66926), to ensure our policy covers any situation involving a device-intensive procedure where an ASC may receive a device at no cost or receive full credit or partial credit for the device, we apply our “FB”/“FC” modifier policy to all device-intensive procedures.
In the CY 2020 OPPS/ASC proposed rule, we did not propose any changes to these policies and we are finalizing continuing our existing policies for CY 2020.
d. Additions to the List of ASC Covered Surgical Procedures
(1) Additions to the List of ASC Covered Surgical Procedures for CY 2020
As finalized in section XII.A.3. of the CY 2019 OPPS/ASC final rule with comment period (83 FR 59029 through 59030), we revised our definition of “surgery” for CY 2019 to include certain “surgery-like” procedures that are assigned codes outside the CPT surgical range. For CY 2020 and subsequent years we proposed to adopt the modified definition we finalized for CY 2019, to include procedures that are described by Category I CPT codes that are not in the surgical range but directly crosswalk or are clinically similar to procedures in the Category I CPT code surgical range that we have determined do not pose a significant safety risk, would not be expected to require an overnight stay when performed in an ASC, and are separately paid under the OPPS. We also proposed to continue to include in our definition of surgical procedures those procedures described by Category I CPT codes in the surgical range from 10000 through 69999 as well as those Category III CPT codes and Level II HCPCS codes that directly crosswalk or are clinically similar to procedures in the CPT surgical range that we have determined do not pose a significant safety risk, that we would not expect to require an overnight stay when performed in ASCs, and that are separately paid under the OPPS.
We conducted a review of HCPCS codes that currently are paid under the OPPS, but not included on the ASC CPL, and that meet our proposed definition of surgery to determine if changes in technology or medical practice affected the clinical appropriateness of these procedures for the ASC setting. Based on this review, we proposed to update the list of ASC covered surgical procedures by adding total knee arthroplasty, a knee mosaicplasty procedure and three coronary intervention procedures (as well as the three associated add-on codes for the coronary intervention procedures) to the list for CY 2020, as was shown in Table 32 of the CY 2020 OPPS/ASC proposed rule. After reviewing the clinical characteristics of these procedures and consulting with stakeholders and our clinical advisors, we determined that these eight procedures would not be expected to pose a significant risk to beneficiary safety when performed in an ASC and would not be expected to require active medical monitoring and care of the beneficiary at midnight following the procedure. The regulations at § 416.166(c) list general exclusions from the list of ASC covered surgical procedures based primarily on factors relating to safety, including procedures that generally result in extensive blood loss, require major or prolonged invasion of body cavities, or directly involve major blood vessels. We assessed each of the proposed added procedures against the regulatory safety criteria and determined that these procedures meet each of the criteria. Although the proposed coronary intervention procedures may involve blood vessels that could be considered major, as stated in the August 2, 2007 ASC final rule (72 FR 42481), we believe the involvement of major blood vessels is best considered in the context of the clinical characteristics of individual procedures, and we do not believe that it is logically or clinically consistent to exclude certain cardiac procedures from the list of ASC covered surgical procedures on the basis of the involvement of major blood vessels, yet continue to provide ASC payment for similar procedures involving major blood vessels that have a history of safe performance in ASCs, such as CPT code 36473 (Mechanicochemical destruction of insufficient vein of arm or leg, accessed through the skin using imaging guidance) and CPT code 37223 (Insertion of stents into groin artery, endovascular, accessed through the skin or open procedure). Based on our review of the clinical characteristics of the procedures and their similarity to other procedures that are currently included on the ASC CPL, we believe these procedures can be safely performed in an ASC. Therefore, we proposed to include these three coronary intervention procedures on the list of ASC covered surgical procedures for CY 2020. We also proposed to add their respective add-on procedures which are packaged under the ASC payment system.
In the CY 2018 OPPS/ASC proposed rule, we solicited public comments on whether the total knee arthroplasty (TKA) procedure, CPT code 27447 (Arthroplasty, knee, condyle and plateau; medial and lateral compartments with or without patella resurfacing (total knee arthroplasty)), should be added to the ASC CPL. In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59411 through 59412) we noted that some commenters stated that many ASCs are equipped to perform these procedures and orthopedic surgeons in ASCs are increasingly performing these procedures safely and effectively on non-Medicare patients and appropriate Medicare patients. However, other commenters noted that the majority of ASCs were not well-equipped to safely perform TKA procedures on patients and that the majority of Medicare patients are not suitable candidates to receive joint arthroplasty procedures in an ASC setting. For CY 2018, we did not finalize adding TKA to the ASC covered surgical procedures list, but noted that we would take the suggestions and recommendations into consideration for future rulemaking.
In this CY 2020 OPPS/ASC final rule, we continue to promote site-neutrality, where possible, between the hospital outpatient department and ASC settings. Further, we agree with commenters that there is a small subset of Medicare beneficiaries who may be suitable candidates to receive TKA procedures in an ASC setting based on their clinical characteristics. For example, based on Medicare Advantage encounter data, we estimate over 800 TKA procedures were performed in an ASC on Medicare Advantage enrollees in 2016. We believe that beneficiaries not enrolled in an MA plan should also have the option of choosing to receive the TKA procedure in an ASC setting based on their physicians' determinations.
As we stated in the August 2, 2007 final rule (72 FR 42483 through 42484), we exclude procedures that would otherwise pose a significant safety risk to the typical Medicare beneficiary. However, we believe physicians should continue to play an important role in exercising their clinical judgment when making site-of-service determinations, including for TKA. In light of the information commenters submitted in support of adding TKA to the ASC CPL in response to our CY 2018 public comment solicitation, we proposed to add TKA to the ASC CPL in CY 2020.
We note that TKA procedures were still predominantly performed in the inpatient hospital setting in CY 2018 (82 percent of the time) based on professional claims data, and we are cognizant of the fact that the majority of beneficiaries may not be suitable candidates to receive TKA in an ASC setting. We believe that appropriate limits are necessary to ensure that Medicare Part B payment will only be made for TKA procedures performed in the ASC setting when that setting is clinically appropriate. Therefore, we solicited public comment on the appropriate approach to provide safeguards for Medicare beneficiaries who should not receive the TKA procedure in an ASC setting. Specifically, we solicited public comment on methods to ensure beneficiaries receive surgical procedures in the ASC setting only as clinically appropriate. For instance, we stated that CMS could issue a new modifier that indicates the physician believes that the beneficiary would not be expected to require active medical monitoring and care at midnight following a particular procedure furnished in the ASC setting. CMS could require that such a modifier be included on the claims line for a surgical procedure performed in an ASC. Alternatively, given the importance of post-operative care in making determinations about whether the ASC is an appropriate setting for a procedure, CMS could require that an ASC has a defined plan of care for each beneficiary following a surgical procedure. We also stated that we could establish certain requirements for ASCs that choose to perform certain surgical procedures on Medicare patients, such as requiring an ASC to have a certain amount of experience in performing a procedure before being eligible for payment for performing the procedure under Medicare. We solicited comment on these options, and other options, for ensuring that beneficiaries receive surgical procedures, including TKA, that do not pose a significant safety risk when performed in an ASC.
In light of the information we received from commenters in support of adding TKA to the ASC CPL in response to our comment solicitation in the CY 2018 OPPS/ASC proposed rule, we stated our belief that TKA would meet our regulatory requirements established under §§ 416.2 and 416.166(b) for covered surgical procedures in the ASC setting. Therefore, we proposed to add TKA to the ASC CPL as shown in Table 32 in the CY 2020 OPPS/ASC proposed rule. At that time we stated our intent to consider appropriate safeguards and limitations for surgical procedures furnished in the ASC setting based on public comments we receive.
As we stated in the CY 2019 OPPS/ASC proposed rule (83 FR 59054 through 59055), section 1833(i)(1) of the Act requires us, in part, to specify, in consultation with appropriate medical organizations, surgical procedures that are appropriately performed on an inpatient basis in a hospital, but can be safely performed in an ASC, and to review and update the ASC covered surgical procedures list at least every 2 years.
We also solicited comment on how CMS should think about the role of the ASC CPL compared to state regulations and market forces in providing payment for certain surgical procedures in an ASC and whether any modifications should be made to the ASC CPL. Comments on this topic could help formulate the basis for future policy development regarding how we determine what procedures are payable for Medicare fee-for-service beneficiaries in the ASC setting and maintain the balance between safety and access. Finally, we solicited comment on how our proposed additions to the list of ASC covered surgical procedures might affect rural hospitals to the extent rural hospitals rely on providing such procedures.
The comments and our responses to the comments are set forth below.
Comment: Many commenters supported our proposal to add three coronary intervention procedures as well as the additional three procedures that represented their associated add-on procedures to the ASC CPL. They stated that our proposed additions meet our criteria to be included on the ASC CPL and that claims analyses, clinical trials, expert consensus and clinical guidelines, among other materials supported the inclusion of such coronary intervention procedures on the ASC CPL. Further, many ASC commenters contended that ASCs are well-equipped to safely perform these procedures on Medicare beneficiaries. However, some commenters stated that without defined criteria for risk stratification, beneficiaries would be exposed to significant risk if these procedures were added to the ASC CPL. Additionally, some commenters believed the percutaneous coronary intervention procedures should be performed in a hospital setting where there is an available on-site cardiac surgical backup and intensive care unit in the event of an emergency.
Response: We thank the commenters for their support. We assessed each of the procedures we proposed to add to the ASC CPL against the regulatory safety criteria and determined that these procedures meet each of the criteria. Although the proposed coronary intervention procedures may involve blood vessels that could be considered major, as stated in the August 2, 2007 ASC final rule (72 FR 42481), we believe the involvement of major blood vessels is best considered in the context of the clinical characteristics of individual procedures. We do not believe that it is appropriate to exclude certain cardiac procedures from the list of ASC covered surgical procedures because they involve major blood vessels, yet continue to provide ASC payment for similar procedures involving major blood vessels that have a history of safe performance in ASCs, such as CPT code 36473 (Mechanicochemical destruction of insufficient vein of arm or leg, accessed through the skin using imaging guidance) and CPT code 37223 (Insertion of stents into groin artery, endovascular, accessed through the skin or open procedure). Based on our review of the clinical characteristics of the procedures and their similarity to other procedures that are currently included on the ASC CPL, we believe these three coronary intervention procedures (CPT codes 92920, 92928, and HCPCS code C9600) and three associated add-on procedures (CPT code 92921, 92929, and HCPCS code C9601) can be safely performed in the ASC setting, for certain Medicare patients and note that the physician should determine whether a particular case would be a good candidate to be furnished in the ASC setting rather than the hospital setting based on the clinical assessment of the patient. We agree with commenters who stated that expert consensus, clinical guidelines, and clinical studies establish that percutaneous coronary interventions can be safely performed in an ASC setting. While we acknowledge that a majority of Medicare beneficiaries may not be suitable candidates to receive these procedures in an ASC setting due to factors such as age and comorbidities, we believe it is important to make these procedures payable in the ASC setting, in order to ensure access to these coronary intervention procedures for those beneficiaries who are appropriate candidates to receive them in an ASC setting.
Therefore, in this final rule with comment period, we are finalizing our proposal without modification to add three coronary intervention procedures as well as three associated add-on procedures. These procedures are:
- CPT code 92920 (Percutaneous transluminal coronary angioplasty; single major coronary artery or branch),
- CPT code 92921 (Percutaneous transluminal coronary angioplasty; each additional branch of a major coronary artery (list separately in addition to code for primary procedure)),
- CPT code 92928 (Percutaneous transcatheter placement of intracoronary stent(s), with coronary angioplasty when performed; single major coronary artery or branch),
- CPT code 92929 (Percutaneous transcatheter placement of intracoronary stent(s), with coronary angioplasty when performed; each additional branch of a major coronary artery (list separately in addition to code for primary procedure)),
- CPT code C9600 (Percutaneous transcatheter placement of drug eluting intracoronary stent(s), with coronary angioplasty when performed; single major coronary artery or branch), and
- CPT code C9601 (Percutaneous transcatheter placement of drug-eluting intracoronary stent(s), with coronary angioplasty when performed; each additional branch of a major coronary artery (list separately in addition to code for primary procedure)) to the ASC CPL.
Comment: Many commenters supported our proposal to add TKA to the ASC CPL for CY 2020 and subsequent years.
Response: We thank commenters for their support of our proposal.
Comment: One commenter requested that we delay adding TKA to the ASC CPL until more data can be collected on the impact of case-mix and patient populations for participants in the CMS Innovation Center's Bundled Payments for Care Improvement Initiative.
Response: We believe there are a small number of less medically complex TKA patients that could appropriately receive TKA in an ASC setting. Because we believe this group will be small, we do not believe our proposal would have a substantial impact on the patient-mix for the Bundled Payments for Care Improvement Advanced (BPCI Advanced) or the Initiative and Comprehensive Care Joint Replacement (CJR) models. Therefore, we do not believe any delay in the implementation of our proposed addition to the ASC CPL is warranted.
Comment: Some commenters opposed our proposal to add TKA to the ASC CPL. These commenters stated that the Medicare population would not be suitable candidates to receive TKA in an ASC setting and that complications arising from TKA could be devastating and life-threatening if not performed in a hospital setting. Specifically, patients could be at risk for the development of deep vein thrombosis with the potential to propagate lethal pulmonary embolus, anesthesia-related risks, as well as other risks. Some commenters also noted that CMS eliminated the requirement that ASCs have a written transfer agreement with a nearby hospital and the requirement that their physicians have admitting privileges at a hospital. Further, some commenters noted that in the absence of the physician self-referral law, which does not apply to procedures performed in an ASC, there will be no other safeguard against a physician's profitable, but clinically inappropriate, referral to an ASC in which the physician has an ownership interest.
Response: We agree with commenters that the majority of Medicare beneficiaries would not be suitable candidates to receive TKA procedures in an ASC setting. Factors such as age, comorbidity, and body mass index are among the many factors that must be taken into account to determine if performing a TKA procedure in an ASC would be appropriate for a particular Medicare beneficiary. However, we believe there are a small number of less medically complex beneficiaries that could appropriately receive the TKA procedure in an ASC setting and we believe physicians should continue to play an important role in exercising their clinical judgment when making site-of-service determinations, including for TKA. While we acknowledge that the physician self-referral law does not apply to TKA performed in an ASC, physicians should be aware of other Federal and state laws that may potentially limit this activity, such as the Anti-Kickback Statute.
Comment: Commenters also noted that beneficiary coinsurance for TKA procedures could be higher in the ASC setting and therefore did not support our proposal, or recommended that we notify beneficiaries that the coinsurance for a TKA procedure could be lower in a hospital outpatient setting.
Response: We are aware that beneficiaries may incur greater cost-sharing for TKA procedures in an ASC setting under our proposal. However, this would not be an occurrence that is unique to TKA. Section 1833(t)(8)(C)(i) of the Act limits the amount of beneficiary copayment that may be collected for a procedure paid under the OPPS (including items such as drugs and biologicals) performed in a year to the amount of the inpatient hospital deductible for that year. We note that this section of the Act does not apply to the ASC payment system. Rather, ASC cost-sharing is described by 1833(a)(4) of the Act and there may be instances where beneficiary cost-sharing in an ASC may be higher than beneficiary cost-sharing in a hospital outpatient department for the same procedure. We note that the ASC payment rate for a TKA procedure is $8,609.17 for CY 2020 while the CY 2020 OPPS payment rate is $11,899.39. This means that ASC coinsurance would be $1,721.83 while hospital OPPS coinsurance would have been $2,379.88, but for the statutory cap limiting it to the inpatient deductible amount ($1,364 in CY 2019). However, the payment rates are publicly available and despite the higher cost-sharing, some beneficiaries, especially those with supplemental insurance, may still choose to have their procedure performed in the ASC setting.
In addition, as we stated in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59389), section 4011 of the 21st Century Cures Act (Pub. L. 114-255) requires the Secretary to make available to the public via a searchable website, with respect to an appropriate number of items and services, the estimated payment amount for the item or service under the OPPS and ASC payment system and the estimated beneficiary liability applicable to the item or service. We implemented this provision by providing our Outpatient Procedure Price Lookup tool available via the internet at https://www.medicare.gov/procedure-price-lookup. This web page allows beneficiaries to compare their potential cost-sharing liability for procedures performed in the hospital outpatient setting versus the ASC setting. We believe this tool allows beneficiaries to be informed of potential cost-sharing amounts and therefore mitigates the commenters' concern about providing payment for procedures in an ASC setting even if the beneficiary cost-sharing in an ASC would be greater than in the hospital outpatient department setting.
Comment: Some commenters suggested that CMS work closely with specialty societies regarding best practices and any appropriate limitations or conditions for Medicare Part B payment for TKA in the ASC setting. Other commenters stated that our suggestions, such as requiring a modifier or a plan of care, were unnecessary and would increase administrative burden by complicating the processes for scheduling, performing and billing for ASCs, without improving beneficiary safety because physicians are best-equipped to determine the clinical appropriateness of the site of service for their patients. Some commenters did not support our suggested approaches and believed that such requirements would be superfluous and provide no beneficial oversight to ensure patient safety. Two orthopedic specialty societies supported the concept of having defined plans of care for each beneficiary following a surgical procedure. One orthopedic specialty society requested that we re-establish the requirement that ASCs have formal arrangements with a nearby hospital in case a patient is unable to go home following a procedure. Other commenters suggested that a defined plan of care requirement is already an existing Condition for Coverage for ASCs.
Response: We agree with commenters that ASCs are currently required to follow the discharge protocols following a surgical procedure, as set out at 42 CFR 416.52(c). For example, our regulations require that each patient be provided written discharge instructions and overnight supplies; prescription and physician contact information; and post-operative instructions; and that patients be discharged in the company of a responsible adult, except those patients exempted by the attending physician.
We remind ASCs that beneficiaries should receive discharge care instructions that meet our requirements following a TKA procedure as well as other surgical procedures. ASCs should also review our State Operations Manual for further guidance on this condition for coverage, as well as others.
With respect to reinstating the requirement that ASCs have a formal transfer agreement with a nearby hospital, we note that such issue is related to Conditions for Coverage and is outside the scope of this final rule with comment.
After considering the public comments we received, and in response to commenters' support for this proposal, we are finalizing our proposal without modification to add TKA, CPT code 27447 (Arthroplasty, knee, condyle and plateau; medial and lateral compartments with or without patella resurfacing (total knee arthroplasty)), to the ASC CPL for CY 2020 and subsequent years.
Based on the public comments we received, we are not finalizing any of the additional requirements on which we sought comment, such as adding a modifier or requiring an ASC to have a certain amount of experience in performing a procedure before being eligible for payment for performing the procedure under Medicare.
Comment: Commenters who responded to the CY 2020 OPPS/ASC proposed rule also requested that CMS add several additional procedures to the ASC CPL, which we had not proposed to add to the ASC CPL in the CY 2020 OPPS/ASC proposed rule. These additional procedures are listed in Table 58.



Response: We appreciate the commenters' recommendations. We reviewed all of the services that commenters requested that we add to the ASC CPL. Of these procedures, we did not consider procedures that are unconditionally packaged under the OPPS (identified by status indicator “N” in addendum B of this final rule with comment period) as such procedures would not meet our requirement for ASC covered surgical procedures at § 416.166(b) that the procedure be separately paid under the OPPS.
Of the procedures listed in Table 58, CPT codes 57267, 62290, 62291, 92938, 92973, 92978, 92979, 93463, 93563, 93564, 93565, 93566, 93567, 93568, 93571, 93572, and C9605 are unconditionally packaged under the ASC payment system. For the procedures identified by CPT codes 92960, 93312, 93313, 93315, and 93530, we do not believe these procedures meet our criteria as established under § 416.166(b) and would pose a significant safety risk to beneficiaries if performed in an ASC setting. For the procedures identified by CPT codes 27412, 57282, 57283, 57425, 62365, 62367, and 62368, we will continue to review whether these procedures meet the criteria to be added to the ASC CPL and take commenters input into consideration in future rulemaking.
(2) Comment Solicitation on Coronary Intervention Procedures
For CY 2020, as discussed above, we proposed to add three coronary intervention procedures (along with the codes describing their respective add-on procedures) that involve major blood vessels that we believe can be safely performed in an ASC setting and would not pose a significant safety risk to beneficiaries if performed in an ASC setting. In the CY 2020 OPPS/ASC proposed rule, in addition to the three coronary intervention procedures (and their three add-on codes) we proposed to add to the ASC CPL, we also reviewed several other coronary intervention procedures. While we did not believe the procedures included in Table P33 of the CY 2020 OPPS/ASC proposed rule met our criteria for inclusion on the ASC CPL at that time, and we did not propose to add such procedures to the ASC CPL for CY 2020, we solicited public comments on whether stakeholders believe these procedures can be safely performed in an ASC setting. Additionally, we requested that commenters provide any materials supporting their position, in particular information and data that specifically address the requirements in our regulations at §§ 416.2 and 416.166 (84 FR 39544). For example, we requested that commenters provide information that supports their position as to whether each of these procedures would be expected to pose a significant risk to beneficiary safety when performed in an ASC, whether standard medical practice dictates that the beneficiary would typically be expected to require active medical monitoring and care at midnight following the procedure (“overnight stay”), and whether the procedure would fall under our general exclusions for covered surgical procedures at § 416.166(c) (for example, would it generally result in extensive blood loss). We stated that we would consider public comments we receive in future rulemaking cycles.


Comment: Some commenters supported adding all of the procedures listed in Table 33 of the CY 2020 OPPS/ASC proposed rule. Other commenters recommended adding CPT codes 92937, 92938, 92973, C9604, and C9605. These commenters stated these percutaneous transluminal revascularization procedures through coronary artery bypass graft meet our established criteria for addition to the ASC CPL and that claims data, clinical trials, and clinical guidelines support their addition.
Other commenters did not support adding any of the procedures list in Table 59 as listed above. The commenters stated that these procedures often carry the risk of serious possible complications, such as in-facility death, damage to or perforations of coronary arteries, and intramural hematoma, among others. Therefore, commenters indicated, such procedures should only be performed in hospital settings that include rapid access to on-site cardiac surgery as well as intensive care units.
Response: We appreciate the commenters' feedback and recommendations. Additionally, we note that we had the incorrect long descriptor for CPT 92973 displayed in our CY 2020 OPPS/ASC proposed rule. In the proposed rule, we had the long descriptor as “Percutaneous transcatheter placement of drug eluting intracoronary stent(s), with coronary angioplasty when performed; single major coronary artery or branch.” The correct long descriptor for CPT 92973 should be “Percutaneous transluminal coronary thrombectomy mechanical (list separately in addition to code for primary procedure)” and is displayed in Table 59 of this final rule with comment period.
Based on the public comments we received, we believe the procedures listed in Table 59 would expose beneficiaries to significant safety risk if performed in an ASC setting at this time and would not meet our criteria established under § 416.166(b). Specifically, we believe that transluminal revascularization of a bypass graft carries an inherent higher risk of complication and may require the assistance of on-site cardiac surgical backup. Additionally, we believe atherectomy procedures carry a greater risk of complication than coronary intervention procedures without an atherectomy procedure. Therefore, at this time, we believe that adding any of the procedures identified in Table 59 of this final rule with comment period to the ASC CPL would expose beneficiaries to significant risk. We believe that such procedures should be performed in a hospital setting with an immediate response available in case of emergencies.
We received no comments on our proposal to add CPT code 29867 (Arthroscopy, knee, surgical; osteochondral allograft (for example, mosaicplasty)) to the ASC CPL for CY 2020 and subsequent years.
After consideration of the public comments we received, we are finalizing our proposal without modification to add CPT codes: 27447, 29867, 92920, 92921, 92928, 92929, and HCPCS codes C9600 and C9601 to the ASC CPL. We have determined these procedures would not be expected to pose a significant risk to beneficiary safety when performed in an ASC, that standard medical practice would not dictate that the beneficiary would typically be expected to require active medical monitoring and care at midnight following the procedure, and are separately paid under the OPPS. The 8 procedures we are adding to the ASC CPL, including the long descriptors and the final CY 2020 payment indicators, are displayed in Table 60.
Additionally, we note that we inadvertently omitted new CPT and new HCPCS codes effective January 1, 2020 from Table 32, Proposed Additions to the List of ASC Covered Surgical Procedures for CY 2020, of our CY 2020 OPPS/ASC proposed rule (84 FR 39544); however, we included these 12 procedures in Addendum AA to our proposed rule. The procedures described by the 12 new CPT and HCPCS codes meet our criteria established under §§ 416.2 and 416.166 for addition to the ASC CPL and are displayed in Table 60. These 12 procedures include—
- CPT code 15769 (Grafting of autologous soft tissue, other, harvested by direct excision (for example, fat, dermis, fascia));
- CPT code 15771 (Grafting of autologous fat harvested by liposuction technique to trunk, breasts, scalp, arms, and/or legs; 50 cc or less injectate);
- CPT code 15773 (Grafting of autologous fat harvested by liposuction technique to face, eyelids, mouth, neck, ears, orbits, genitalia, hands, and/or feet; 25 cc or less injectate);
- CPT code 33016 (Pericardiocentesis, including imaging guidance, when performed);
- CPT code 46948 (Hemorrhoidectomy, internal, by transanal hemorrhoidal dearterialization, 2 or more hemorrhoid columns/groups, including ultrasound guidance, with mucopexy, when performed);
- CPT code 62328 (Spinal puncture, lumbar, diagnostic; with fluoroscopic or CT guidance);
- CPT code 62329 (Spinal puncture, therapeutic, for drainage of cerebrospinal fluid (by needle or catheter); with fluoroscopic or CT guidance);
- CPT Code 64451 (Injection(s), anesthetic agent(s) and/or steroid; nerves innervating the sacroiliac joint, with image guidance (that is, fluoroscopy or computed tomography));
- CPT Code 64625 (Radiofrequency ablation, nerves innervating the sacroiliac joint, with image guidance (that is, fluoroscopy or computed tomography));
- CPT Code 66987 (Extracapsular cataract removal with insertion of intraocular lens prosthesis (1-stage procedure), manual or mechanical technique (for example, irrigation and aspiration or phacoemulsification), complex, requiring devices or techniques not generally used in routine cataract surgery (for example, iris expansion device, suture support for intraocular lens, or primary posterior capsulorrhexis) or performed on patients in the amblyogenic developmental stage; with endoscopic cyclophotocoagulation);
- CPT Code 66988 (Extracapsular cataract removal with insertion of intraocular lens prosthesis (1 stage procedure), manual or mechanical technique (for example, irrigation and aspiration or phacoemulsification); with endoscopic cyclophotocoagulation); and
- CPT code 0587T (Percutaneous implantation or replacement of integrated single device neurostimulation system including electrode array and receiver or pulse generator, including analysis, programming, and imaging guidance when performed, posterior tibial nerve).
We did not receive comments on the addition of these codes to the ASC CPL and are finalizing without modification. The table below shows all additions to the ASC CPL for CY 2020, these additions are also reflected in Addendum AA.



2. Covered Ancillary Services
Consistent with the established ASC payment system policy (72 FR 42497), we proposed to update the ASC list of covered ancillary services to reflect the payment status for the services under the CY 2020 OPPS. We stated in the proposed rule that maintaining consistency with the OPPS may result in proposed changes to ASC payment indicators for some covered ancillary services because of changes that are being proposed under the OPPS for CY 2020. For example, if a covered ancillary service was separately paid under the ASC payment system in CY 2019, but is proposed for packaged status under the CY 2020 OPPS, to maintain consistency with the OPPS, we would also propose to package the ancillary service under the ASC payment system for CY 2020. We proposed to continue this reconciliation of packaged status for subsequent calendar years. Comment indicator “CH”, which is discussed in section XIII.F. of the CY 2020 OPPS/ASC proposed rule, is used in Addendum BB to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website) to indicate covered ancillary services for which we proposed a change in the ASC payment indicator to reflect a proposed change in the OPPS treatment of the service for CY 2020.
Comment: One commenter requested that we add CPT code 91040 (Esophageal balloon distension study, diagnostic, with provocation when performed) to our list of covered ancillary services. Commenter stated that esophageal balloon distension studies are often performed in conjunction with esophagogastroduodenoscopy procedures.
Response: Services listed in our list of covered ancillary services must be integral to the performance of a covered surgical procedure. Based on the description of the procedure, we do not believe this service is integral to the performance of the surgical procedures identified by the commenter, specifically CPT codes 43235 (Esophagogastroduodenoscopy, flexible, transoral; diagnostic, including collection of specimen(s) by brushing or washing, when performed (separate procedure)), 43236 (Esophagogastroduodenoscopy, flexible, transoral; with directed submucosal injection(s), any substance), or 43239 (Esophagogastroduodenoscopy, flexible, transoral; with biopsy, single or multiple), or other surgical procedures. Therefore, we are not adding CPT code 91040 to the list of ASC covered ancillary services for CY 2020.
All ASC covered ancillary services and their proposed payment indicators for CY 2020 are included in Addendum BB to the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website).
D. Update and Payment for ASC Covered Surgical Procedures and Covered Ancillary Services
1. ASC Payment for Covered Surgical Procedures
a. Background
Our ASC payment policies for covered surgical procedures under the revised ASC payment system are fully described in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66828 through 66831). Under our established policy, we use the ASC standard ratesetting methodology of multiplying the ASC relative payment weight for the procedure by the ASC conversion factor for that same year to calculate the national unadjusted payment rates for procedures with payment indicators “G2” and “A2”. Payment indicator “A2” was developed to identify procedures that were included on the list of ASC covered surgical procedures in CY 2007 and, therefore, were subject to transitional payment prior to CY 2011. Although the 4-year transitional period has ended and payment indicator “A2” is no longer required to identify surgical procedures subject to transitional payment, we retained payment indicator “A2” because it is used to identify procedures that are exempted from the application of the office-based designation.
The rate calculation established for device-intensive procedures (payment indicator “J8”) is structured so only the service portion of the rate is subject to the ASC standard ratesetting methodology. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59028 through 59080), we updated the CY 2018 ASC payment rates for ASC covered surgical procedures with payment indicators of “A2”, “G2”, and “J8” using CY 2017 data, consistent with the CY 2019 OPPS update. We also updated payment rates for device-intensive procedures to incorporate the CY 2019 OPPS device offset percentages calculated under the standard APC ratesetting methodology, as discussed earlier in this section.
Payment rates for office-based procedures (payment indicators “P2”, “P3”, and “R2”) are the lower of the PFS nonfacility PE RVU-based amount or the amount calculated using the ASC standard rate setting methodology for the procedure. In the CY 2018 OPPS/ASC final rule with comment period, we updated the payment amounts for office-based procedures (payment indicators “P2”, “P3”, and “R2”) using the most recent available MPFS and OPPS data. We compared the estimated CY 2018 rate for each of the office-based procedures, calculated according to the ASC standard rate setting methodology, to the PFS nonfacility PE RVU-based amount to determine which was lower and, therefore, would be the CY 2018 payment rate for the procedure under our final policy for the revised ASC payment system (§ 416.171(d)).
In the CY 2014 OPPS/ASC final rule with comment period (78 FR 75081), we finalized our proposal to calculate the CY 2014 payment rates for ASC covered surgical procedures according to our established methodologies, with the exception of device removal procedures. For CY 2014, we finalized a policy to conditionally package payment for device removal procedures under the OPPS. Under the OPPS, a conditionally packaged procedure (status indicators “Q1” and “Q2”) describes a HCPCS code where the payment is packaged when it is provided with a significant procedure but is separately paid when the service appears on the claim without a significant procedure. Because ASC services always include a covered surgical procedure, HCPCS codes that are conditionally packaged under the OPPS are always packaged (payment indicator “N1”) under the ASC payment system. Under the OPPS, device removal procedures are conditionally packaged and, therefore, would be packaged under the ASC payment system. There would be no Medicare payment made when a device removal procedure is performed in an ASC without another surgical procedure included on the claim; therefore, no Medicare payment would be made if a device was removed but not replaced. To ensure that the ASC payment system provides separate payment for surgical procedures that only involve device removal—conditionally packaged in the OPPS (status indicator “Q2”)—we continued to provide separate payment since CY 2014 and assigned the current ASC payment indicators associated with these procedures.
b. Update to ASC Covered Surgical Procedure Payment Rates for CY 2020
We proposed to update ASC payment rates for CY 2020 and subsequent years using the established rate calculation methodologies under § 416.171 and using our definition of device-intensive procedures, as discussed in section XII.C.1.b. of the CY 2020 OPPS/ASC proposed rule. Because the proposed OPPS relative payment weights are generally based on geometric mean costs, the ASC system would generally use geometric means to determine proposed relative payment weights under the ASC standard methodology. We proposed to continue to use the amount calculated under the ASC standard ratesetting methodology for procedures assigned payment indicators “A2” and “G2”.
We proposed to calculate payment rates for office-based procedures (payment indicators “P2”, “P3”, and “R2”) and device-intensive procedures (payment indicator “J8”) according to our established policies and, for device-intensive procedures, using our modified definition of device-intensive procedures, as discussed in section XII.C.1.b. of the CY 2020 OPPS/ASC proposed rule. Therefore, we proposed to update the payment amount for the service portion of the device-intensive procedures using the ASC standard rate setting methodology and the payment amount for the device portion based on the proposed CY 2020 OPPS device offset percentages that have been calculated using the standard OPPS APC ratesetting methodology. Payment for office-based procedures would be at the lesser of the proposed CY 2020 MPFS nonfacility PE RVU-based amount or the proposed CY 2020 ASC payment amount calculated according to the ASC standard ratesetting methodology.
As we did for CYs 2014 through 2019, for CY 2020, we proposed to continue our policy for device removal procedures, such that device removal procedures that are conditionally packaged in the OPPS (status indicators “Q1” and “Q2”) would be assigned the current ASC payment indicators associated with these procedures and would continue to be paid separately under the ASC payment system.
Our responses to the comments are set forth below.
Comment: We received several comments from professional societies expressing concern about assigning CPT codes 36465, 36466, and 31298 to a P2 payment indicator and CPT code 36482 to a P3 payment indicator. Commenters also expressed concerns with the appropriateness of the ASC payment policy to assign procedures to the lowest published payment rate across multiple payment systems, based upon CMS's determination that the level of complexity for a procedure is consistent with procedures performed in a physician's office. Commenters agreed with the proposal not designate CPT code 36902 as an office-based procedure and continue to assign CPT code 36902 a payment indicator of “G2”—nonoffice-based surgical procedure paid based on OPPS relative weights.
Response: We appreciate the commenters' input. Based on our analysis of the latest hospital outpatient and ASC claims data used for this final rule with comment period, we are updating ASC payment rates for CY 2020 using the established rate calculation methodologies under § 416.171 of the regulations and using our finalized modified definition of device-intensive procedures, as discussed in section XIII.C.1.b of this final rule with comment period. We do not generally make additional payment adjustments to specific procedures. As such, we are finalizing the proposed APC assignment and payment indicators for CPT codes 36465, 36466, 31298, 36482, and 36902 as discussed in XIII.C.1.A of this final rule with comment period.
Comment: Several commenters disagreed with the proposed CY 2020 ASC payment rates for the surgical procedures described by the following CPT/HCPCS codes, requesting that CMS increase payment in the ASC setting:
- HCPCS code C9754 (Creation of arteriovenous fistula, percutaneous; direct, any site, including all imaging and radiologic supervision and interpretation, when performed and secondary procedures to redirect blood flow)
- HCPCS code C9755 (Creation of arteriovenous fistula, percutaneous using magnetic-guided arterial and venous catheters and radiofrequency energy, including flow-directing procedures (for example, vascular coil embolization with radiologic supervision and interpretation, when performed) and fistulogram(s), angiography, venography, and/or ultrasound, with radiologic supervision and interpretation, when performed)
- CPT code 37243 (Vascular embolization or occlusion, inclusive of all radiological supervision and interpretation, intraprocedural roadmapping, and imaging guidance necessary to complete the intervention; for tumors, organ ischemia, or infarction)
- CPT code 53854 (Transurethral destruction of prostate tissue by radiofrequency generated water vapor thermotherapy)
- CPT code 22869 (Insertion of interlaminar/interspinous process stabilization/distraction device, without open decompression or fusion, including image guidance when performed, lumbar; single level)
- CPT code 22870 (Insertion of interlaminar/interspinous process stabilization/distraction device, without open decompression or fusion, including image guidance when performed, lumbar; second level (List separately in addition to code for primary procedure)
Response: We update the data on which we establish payment rates each year through rulemaking and note that ASC rates are derived from OPPS payment rates which are required to be reviewed and updated at least annually under section 1833(t)(9) of the Act. ASC payment is dependent upon the APC assignment for each procedure. Based on our analysis of the latest hospital OPPS and ASC claims data used for this final rule with comment period, we are updating ASC payment rates for CY 2020 using the established rate calculation methodologies under § 416.171 of the regulations and our definition of device-intensive procedures, as discussed in section XII.C.1.b. of this CY 2020 OPPS/ASC final rule with comment period. We do not generally make additional payment adjustments to specific procedures. Therefore, we are finalizing the payment indicators for HCPCS codes C9754 and C9755 and CPT codes 37243, 53854, 22869, and 22870 for CY 2020.
Comment: One commenter recommended that CMS eliminate the prohibition against billing for services using an unlisted CPT surgical procedure code.
Response: Under § 416.166(c)(7), covered surgical procedures do not include procedures that can only be reported using a CPT unlisted surgical procedure code. Therefore, such procedures are not currently payable under the ASC payment system. As discussed in the August 2, 2008 final rule (72 FR 42484 through 42486), it is not possible to know what specific procedure would be represented by an unlisted code. We are required to evaluate each surgical procedure for potential safety risk and the expected need for overnight monitoring and to exclude such procedures from ASC payment. It is not possible to evaluate procedures reported by unlisted CPT codes according to these criteria. Therefore, we are not accepting this recommendation.
After consideration of the public comments we received, we are finalizing our proposed policies without modification, to calculate the CY 2020 payment rates for ASC covered surgical procedures according to our established methodologies using the modified definition of device-intensive procedures. For covered office-based surgical procedures, the payment rate is the lesser of the final CY 2020 MPFS nonfacility PE RVU-based amount or the final CY 2020 ASC payment amount calculated according to the ASC standard ratesetting methodology, the final payment indicators and rates set forth in this final rule with comment period are based on a comparison using the PFS PE RVUs and the conversion factor effective January 1, 2020. For a discussion of the PFS rates, we refer readers to the CY 2020 PFS final rule with comment period.
c. Limit on ASC Payment Rates for Low Volume Device-Intensive Procedures
As stated in section XIII.D.1.b. of the CY 2020 OPPS/ASC proposed rule, the ASC payment system generally uses OPPS geometric mean costs under the standard methodology to determine proposed relative payment weights under the standard ASC ratesetting methodology. However, for low-volume device-intensive procedures, the proposed relative payment weights are based on median costs, rather than geometric mean costs, as discussed in section IV.B.5. of the CY 2020 OPPS/ASC proposed rule.
While we believe this policy generally helps to provide more appropriate payment for low-volume device-intensive procedures, these procedures can still have data anomalies as a result of the limited data available for these procedures in our ratesetting process. For the Level 5 Intraocular APC, which includes only HCPCS code 0308T (insj ocular telescope prosth), based on the CY 2018 claims data available for the proposed rule, the geometric mean cost and median cost under the standard ASC ratesetting methodology is $67,946.51 and $111,019.30, respectively. As described in section IV.B.5. of the CY 2020 OPPS/ASC proposed rule, a device-intensive procedure that is assigned to a clinical APC with fewer than 100 total claims for all procedures is considered “low-volume” and the cost of the procedure is based on calculations using the APC's median cost instead of the APC's geometric mean cost. Since this APC meets the criteria for low-volume device-intensive procedure designation, the ASC relative weight would be based on the median cost rather than the geometric mean cost. We note that this median cost for this APC is significantly higher than either the OPPS geometric mean cost or median cost based on the OPPS comprehensive ratesetting methodology, which are $28,122.51 and $19,269.55, respectively. This very large difference in cost calculations between these two settings is largely attributable to the APC's low claims volume and to the comprehensive methodology used under the OPPS which is not utilized in ratesetting under the ASC payment system. The cost calculation for this APC under the ASC payment system is primarily based on charges from one hospital with a significantly higher device cost center cost-to-charge ratio and significantly higher charges when compared to other hospitals providing the procedure.
If the ASC payment system were to base the CY 2020 payment rate for HCPCS code 0308T on the median cost of $111,019.30, the ASC payment rate would be several times greater than the OPPS payment rate for HCPCS code 0308T. We note that the median cost under the OPPS ratesetting methodology based on CY 2018 claims data is closer to the historical average for the median cost of HCPCS code 0308T (approximately $19,000). In addition, given that the outpatient hospital setting is generally considered to have higher costs than the ASC setting and that the payment rates for both settings are based on hospital outpatient cost data, we do not believe there should be a scenario where the payment rate for a low-volume device-intensive procedure under the ASC payment system is significantly greater than payment under the OPPS.
Therefore, for CY 2020 and subsequent years, we proposed to limit the ASC payment rate for low-volume device-intensive procedures to a payment rate equal to the OPPS payment rate for that procedure. Under this proposal, where the ASC payment rate based on the standard ASC ratesetting methodology for low volume device-intensive procedures would exceed the rate paid under the OPPS for the same procedure, we proposed to establish an ASC payment rate for such procedures equal to the OPPS payment rate for the same procedure. In the CY 2020 OPPS/ASC proposed rule, we noted that this policy would only affect HCPCS code 0308T, which has very low claims volume (7 claims used for ratesetting in the OPPS). We proposed to amend § 416.171(b) of the regulations to reflect the proposed new limit on ASC payment rates for low-volume device-intensive procedures. CMS' existing regulation at § 416.171(b)(2) requires the payment of the device portion of a device-intensive procedure at an amount derived from the payment rate for the equivalent item under the OPPS using our standard ratesetting methodology. We proposed to add paragraph (b)(4) to § 416.171 to require that, notwithstanding paragraph (b)(2), low volume device-intensive procedures where the otherwise applicable payment rate calculated based on the standard methodology for device-intensive procedures would exceed the payment rate for the equivalent procedure set under the OPPS, the payment rate for the procedure under the ASC payment system would be equal to the payment rate for the same procedure under the OPPS.
Covered surgical procedures and their proposed payment rates for CY 2020 are listed in Addendum AA of the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website).
Comment: One commenter requested that CMS consider adopting a consistent payment methodology for low volume procedures, regardless of whether a procedure is assigned to a clinical or New Technology APC. The commenter noted that 0308T is one of only two procedures to which CMS has applied either of the low volume payment methodologies. The commenter suggested CMS could determine the payment rate for low volume, device-intensive procedures in clinical APCs by using 4 years of claims data and gathering input through the public comment period on whether arithmetic mean, geometric mean, or median should be the basis for the payment amount.
Response: We appreciate the stakeholder's comments regarding changes in estimated costs based on the claims data available for ratesetting. In our CY 2017 OPPS/ASC final rule with comment period (81 FR 79660 through 79661), we finalized our policy that the payment rate for any device-intensive procedure that is assigned to a clinical APC with fewer than 100 total claims for all procedures in the APC be calculated using the median cost instead of the geometric mean cost. We believe using the median cost instead of the geometric mean cost has generally provided an appropriate payment for low-volume device-intensive procedures in cases where there are no data anomalies. However, we note that we are adding paragraph (b)(4) to § 416.171 to require that, notwithstanding paragraph (b)(2), low volume device-intensive procedures where the otherwise applicable ASC payment rate calculated based on the standard methodology for device-intensive procedures would exceed the payment rate for the equivalent procedure set under the OPPS, the payment rate for the procedure under the ASC payment system would be equal to the payment rate for the same procedure under the OPPS to address such data anomalies in the future.
Additionally, as we noted in our CY 2020 OPPS/ASC proposed rule (84 FR 39453-39454), one of the objectives of establishing New Technology APCs is to generate sufficient claims data for a new procedure so that it can be assigned to an appropriate clinical APC. In cases where procedures are assigned to New Technology APCs have very low annual volume, we may use up to 4 years of claims data in calculating the applicable payment rate for the prospective year. We believe our payment policy for low-volume new technology procedures provides an appropriate payment for new technology procedures so that they may be assigned to an appropriate clinical APC in the future. Further, we believe this payment policy should only be applicable to procedures assigned to New Technology APCs and not to all clinical APCs since we believe it would be less common for a clinical APC to have fewer than 100 total claims than a new technology APC.
After consideration of the public comment we received, we are finalizing our proposed policy without modification, to limit the ASC payment rate for a low-volume device-intensive procedure to a payment rate equal to the OPPS payment rate for that procedure, including our proposed regulation text at § 416.171(b)(4).
2. Payment for Covered Ancillary Services
a. Background
Our payment policies under the ASC payment system for covered ancillary services generally vary according to the particular type of service and its payment policy under the OPPS. Our overall policy provides separate ASC payment for certain ancillary items and services integrally related to the provision of ASC covered surgical procedures that are paid separately under the OPPS and provides packaged ASC payment for other ancillary items and services that are packaged or conditionally packaged (status indicators “N”, “Q1”, and “Q2”) under the OPPS. In the CY 2013 OPPS/ASC rulemaking (77 FR 45169 and 77 FR 68457 through 68458), we further clarified our policy regarding the payment indicator assignment of procedures that are conditionally packaged in the OPPS (status indicators “Q1” and “Q2”). Under the OPPS, a conditionally packaged procedure describes a HCPCS code where the payment is packaged when it is provided with a significant procedure but is separately paid when the service appears on the claim without a significant procedure. Because ASC services always include a surgical procedure, HCPCS codes that are conditionally packaged under the OPPS are generally packaged (payment indictor “N1”) under the ASC payment system (except for device removal procedures, as discussed in section IV. of the CY 2020 OPPS/ASC proposed rule). Thus, our policy generally aligns ASC payment bundles with those under the OPPS (72 FR 42495). In all cases, in order for those ancillary services also to be paid, ancillary items and services must be provided integral to the performance of ASC covered surgical procedures for which the ASC bills Medicare.
Our ASC payment policies generally provide separate payment for drugs and biologicals that are separately paid under the OPPS at the OPPS rates and package payment for drugs and biologicals for which payment is packaged under the OPPS. However, as discussed in section XIII.D.3. of the CY 2020 OPPS/ASC proposed rule, for CY 2019, we finalized a policy to unpackage and pay separately at ASP + 6 percent for the cost of non-opioid pain management drugs that function as surgical supplies when furnished in the ASC setting, even though payment for these drugs continues to be packaged under the OPPS. We generally pay for separately payable radiology services at the lower of the PFS nonfacility PE RVU-based (or technical component) amount or the rate calculated according to the ASC standard ratesetting methodology (72 FR 42497). However, as finalized in the CY 2011 OPPS/ASC final rule with comment period (75 FR 72050), payment indicators for all nuclear medicine procedures (defined as CPT codes in the range of 78000 through 78999) that are designated as radiology services that are paid separately when provided integral to a surgical procedure on the ASC list are set to “Z2” so that payment is made based on the ASC standard ratesetting methodology rather than the MPFS nonfacility PE RVU amount (“Z3”), regardless of which is lower (42 CFR 416.171(d)(1)).
Similarly, we also finalized our policy to set the payment indicator to “Z2” for radiology services that use contrast agents so that payment for these procedures will be based on the OPPS relative payment weight using the ASC standard ratesetting methodology and, therefore, will include the cost for the contrast agent (§ 416.171(d)(2)).
ASC payment policy for brachytherapy sources mirrors the payment policy under the OPPS. ASCs are paid for brachytherapy sources provided integral to ASC covered surgical procedures at prospective rates adopted under the OPPS or, if OPPS rates are unavailable, at contractor-priced rates (72 FR 42499). Since December 31, 2009, ASCs have been paid for brachytherapy sources provided integral to ASC covered surgical procedures at prospective rates adopted under the OPPS.
Our ASC policies also provide separate payment for: (1) Certain items and services that CMS designates as contractor-priced, including, but not limited to, the procurement of corneal tissue; and (2) certain implantable items that have pass-through payment status under the OPPS. These categories do not have prospectively established ASC payment rates according to ASC payment system policies (72 FR 42502 and 42508 through 42509; § 416.164(b)). Under the ASC payment system, we have designated corneal tissue acquisition and hepatitis B vaccines as contractor-priced. Corneal tissue acquisition is contractor-priced based on the invoiced costs for acquiring the corneal tissue for transplantation. Hepatitis B vaccines are contractor-priced based on invoiced costs for the vaccine.
Devices that are eligible for pass-through payment under the OPPS are separately paid under the ASC payment system and are contractor-priced. Under the revised ASC payment system (72 FR 42502), payment for the surgical procedure associated with the pass-through device is made according to our standard methodology for the ASC payment system, based on only the service (non-device) portion of the procedure's OPPS relative payment weight if the APC weight for the procedure includes other packaged device costs. We also refer to this methodology as applying a “device offset” to the ASC payment for the associated surgical procedure. This ensures that duplicate payment is not provided for any portion of an implanted device with OPPS pass-through payment status.
In the CY 2015 OPPS/ASC final rule with comment period (79 FR 66933 through 66934), we finalized that, beginning in CY 2015, certain diagnostic tests within the medicine range of CPT codes for which separate payment is allowed under the OPPS are covered ancillary services when they are integral to an ASC covered surgical procedure. We finalized that diagnostic tests within the medicine range of CPT codes include all Category I CPT codes in the medicine range established by CPT, from 90000 to 99999, and Category III CPT codes and Level II HCPCS codes that describe diagnostic tests that crosswalk or are clinically similar to procedures in the medicine range established by CPT. In the CY 2015 OPPS/ASC final rule with comment period, we also finalized our policy to pay for these tests at the lower of the PFS nonfacility PE RVU-based (or technical component) amount or the rate calculated according to the ASC standard ratesetting methodology (79 FR 66933 through 66934). We finalized that the diagnostic tests for which the payment is based on the ASC standard ratesetting methodology be assigned to payment indicator “Z2” and revised the definition of payment indicator “Z2” to include a reference to diagnostic services and those for which the payment is based on the PFS nonfacility PE RVU-based amount be assigned payment indicator “Z3,” and revised the definition of payment indicator “Z3” to include a reference to diagnostic services.
b. Payment for Covered Ancillary Services for CY 2020
We proposed to update the ASC payment rates and to make changes to ASC payment indicators, as necessary, to maintain consistency between the OPPS and ASC payment system regarding the packaged or separately payable status of services and the proposed CY 2020 OPPS and ASC payment rates and subsequent year payment rates. We also proposed to continue to set the CY 2020 ASC payment rates and subsequent year payment rates for brachytherapy sources and separately payable drugs and biologicals equal to the OPPS payment rates for CY 2020 and subsequent year payment rates.
We note that stakeholders requested that we propose to add CPT code 91040 (Esophageal balloon distension study, diagnostic, with provocation when performed) to the ASC Covered Procedures List (CPL) and ASC list of covered ancillary services as it is integral to the performance of covered surgical procedures such as CPT code 43235 (Esophagogastroduodenoscopy, flexible, transoral; diagnostic, including collection of specimen(s) by brushing or washing, when performed (separate procedure)) and 43239 (Esophagogastroduodenoscopy, flexible, transoral; with biopsy, single or multiple). Based on available data and other information related to CPT code 91040, we do not believe this diagnostic test is integral to the covered surgical procedures of CPT codes 43235 or 43239. Therefore, we did not propose to add CPT code 91040 as a covered ancillary service.
Covered ancillary services and their proposed payment indicators for CY 2020 are listed in Addendum BB of the CY 2020 OPPS/ASC proposed rule (which is available via the internet on the CMS website). For those covered ancillary services where the payment rate is the lower of the proposed rates under the ASC standard rate setting methodology and the PFS final rates, the proposed payment indicators and rates set forth in the proposed rule are based on a comparison using the proposed PFS rates effective January 1, 2020. For a discussion of the PFS rates, we refer readers to the CY 2020 PFS proposed rule, which is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices.html.
3. CY 2020 ASC Packaging Policy for Non-Opioid Pain Management Treatments
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59066 through 59072), we finalized the policy to unpackage and pay separately at ASP+6 percent for the cost of non-opioid pain management drugs that function as surgical supplies when they are furnished in the ASC setting for CY 2019. We also finalized conforming changes to § 416.164(a)(4) to exclude non-opioid pain management drugs that function as a supply when used in a surgical procedure from our policy to package payment for drugs and biologicals for which separate payment is not allowed under the OPPS into the ASC payment for the covered surgical procedure. We added a new § 416.164(b)(6) to include non-opioid pain management drugs that function as a supply when used in a surgical procedure as covered ancillary services that are integral to a covered surgical procedure. Finally, we finalized a change to § 416.171(b)(1) to exclude non-opioid pain management drugs that function as a supply when used in a surgical procedure from our policy to pay for ASC covered ancillary services an amount derived from the payment rate for the equivalent item or service set under the OPPS.
In the CY 2019 OPPS/ASC final rule with comment period, we noted that we will continue to analyze the issue of access to non-opioid alternatives in the OPPS and ASC settings as we implement section 6082 of the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT for Patients and Communities Act or SUPPORT Act) (Pub. L. 115-271), enacted on October 24, 2018. We also discussed our policy to unpackage and pay separately at ASP+6 percent for the cost of non-opioid pain management drugs that function as surgical supplies when furnished in the ASC setting in section II.A.3.b. of the CY 2019 OPPS/ASC final rule with comment period (83 FR 58854 through 58860). As required under section 6082(b) of the SUPPORT Act, we will continue to review and revise ASC payments for non-opioid alternatives for pain management, as appropriate. For more information on our implementation of section 6082 of the SUPPORT for Patients and Communities Act and related proposals, we refer readers to section II.A.3.b. of the CY 2020 OPPS/ASC proposed rule.
The comments and our responses are set forth below.
Comment: Multiple commenters, including individual stakeholders, hospital and physician groups, national medical associations, device manufacturers, and groups representing the pharmaceutical industry, supported the proposal to continue unpackage and pay separately for the cost of non-opioid pain management drugs that function as surgical supplies, such as Exparel, in the ASC setting for CY 2020. These commenters believed that packaged payment for non-opioid alternatives presents a barrier to care and that separate payment for non-opioid pain management drugs would be an appropriate response to the opioid drug abuse epidemic.
Other commenters, including MedPAC, did not support this proposal and stated that the policy was counter to the OPPS packaging policies created to increase the size of payment bundles in the OPPS, which increases incentives for efficient delivery of care. MedPAC noted that they prefer a policy that maintains the packaging of drugs that function as supplies in surgical procedures.
Response: We appreciate these comments. After reviewing the information provided by the commenters, we continue to believe the separate payment is appropriate for non-opioid pain management drugs that function as surgical supplies when furnished in the ASC setting for CY 2020. We note that preliminary data suggest that utilization of Exparel has increased significantly in the ASC setting in 2019. We intend to continue to monitor Exparel utilization in the ASC setting and monitor whether there is an associated decrease under Part B or D in opioids once more data are available.
Comment: Several commenters supported the assignment of status indicator “K” (Nonpass-Through Drugs and Nonimplantable Biologicals, Including Therapeutic Radiopharmaceuticals) and continuing to pay separately for the drug Prialt (HCPCS J2278, injection, ziconitide), a non-narcotic pain reliever administered via intrathecal injection. The commenters discussed data indicating that Prialt potentially could lower opioid use, including opioids such as morphine. In addition to continued separate payment, several commenters recommended CMS reduce or eliminate the coinsurance for the drug in order to increase beneficiary access. The commenters noted due to the drug's significant cost, the 20 percent coinsurance would put the drug out of reach for beneficiaries. Additionally, the commenters discussed that there is not enough financial incentive for providers to use Prialt in their patients compared to lower cost opioids. Commenters claimed that Prialt is only paid at invoice costs, which they believe discourages provider use.
Response: We thank commenters for their feedback and for their support of the continued assignment of status indicator “K” to HCPCS J2278. The corresponding ASC payment indicator for HCPCS J2278 would be “K2”. Prialt is paid at its average sales price (ASP) plus 6 percent according to the ASP methodology under the OPPS, and therefore, is also paid at ASP plus 6 percent in the ASC setting. We note that under 1833(a)(1)(G) of the Act, the payment is subject to applicable deductible and coinsurance, and we are unaware of statutory authority to alter beneficiary coinsurance for payments made in the ASC setting. We note that because the dollar value of beneficiary coinsurance is directly proportionate to the payment rate (which is ASP+6 percent for HCPCS code J2278), a lower sales price for the drug (which would lead to a lower Medicare payment rate under the current policy) would be necessary for beneficiaries to have a lower coinsurance amount.
Comment: Many commenters requested that the drug Omidria (HCPCS code C9447, injection, phenylephrine ketorolac), be excluded from the packaging policy once its pass-through status expires on September 30, 2020. Omidria is indicated for maintaining pupil size by preventing intraoperative miosis and reducing postoperative ocular pain in cataract or intraocular surgeries. The commenters stated that the available data and multiple peer-reviewed articles on Omidria support the packaging exclusion. Commenters asserted the use of Omidria decreases patients' need for fentanyl during surgeries and another commenter believes that Omidria reduces opioid use after cataract surgeries. In addition, commenters asserted that the OPPS and ASC payment system do not address the cost of packaged products used by small patient populations. Therefore, the OPPS and ASC payment structures for packaged supplies creates an access barrier and patients are forced to use inferior products that have increased complication risk and require the continued use of opioids to manage pain. One commenter referenced the results of a study that Omidria reduces the need for opioids during cataract surgery by nearly 80 percent while decreasing pain scores by more than 50 percent.
Response: We thank commenters for their feedback on Omidria. Omidria received pass-through status for a 3-year period from 2015 to 2017. After expiration of its pass-through status, it was packaged under both the OPPS and ASC payment system. Subsequently, Omidria's pass-through status under the OPPS was reinstated in October 2018 through September 30, 2020 as required by section 1833(t)(6)(G) of the Act, as added by section 1301(a)(1)(C) of the Consolidated Appropriations Act of 2018 (Pub. L. 115-141), which means that Omidria continues to be paid separately under the ASC payment system through September 30, 2020. While our analysis supports the commenter's assertion that there was a decrease in the utilization of Omidria in 2018 following its pass-through expiration, we note that there could be many reasons that utilization declines after the pass-through period, including the availability of other alternatives on the market (many of which had been used for several years before Omidria came on the market and are sold for a lower price), the lack of separate payment being available, or physician preference.
Further, our clinical advisors' review of the clinical evidence submitted concluded that the study the commenter submitted was not sufficiently compelling or authoritative to overcome contrary evidence. Moreover, the results of a CMS analysis of cataract procedures performed on Medicare beneficiaries in the OPPS between January 2015 and July 2019 comparing procedures performed with Omidria to procedures performed without Omidria did not demonstrate a significant decrease in fentanyl utilization during the cataract surgeries in the OPPS when Omidria was used. Our findings also did not suggest any decrease in opioid utilization post-surgery for procedures involving Omidria. As a result, we do not have compelling evidence to exclude Omidria from packaging after its current pass-through expires on September 30, 2020. While we were not able to perform similar analysis using ASC data, we expect that the results may be similar. We will continue to analyze the evidence and monitor utilization of this drug.
Comment: One commenter requested that MKO Melt, a non FDA-approved, compounded drug comprised of midazolam/ketamine/ondansetron for exclusion from the packaging policy per section 1833(t)(22)(A)(i) of the Act. The commenter contended that MKO Melt is a drug functioning as surgical supply in the ASC setting. The commenter provided a reference to a study titled, “Anesthesia for opioid addicts: Challenges for perioperative physician” by Goyal et al., on the need for pain management in the opioid-dependent patient. The commenter also referenced a review article, “Perioperative Management of Acute Pain in the Opioid-dependent Patient,” by Mitra et al., on the special needs of opioid-dependent patients in surgeries and the potential opioid relapse in those patients who are recovering from opioid use disorder. Additionally, the commenter referenced a clinical trial registered in clinicaltrials.gov (NCT03653520) that supports sublingual MKO Melt for use during cataract surgeries to replace opioids. The study looked at 611 patients that were divided into three arms: (1) MKO melt arm, (2) diazepam/tramadol/ondansetron arm, (3) diazepam only arm. The study concluded that the MKO melt arm had the lowest incidence for supplemental injectable anesthesia to control pain.
Response: We thank the commenter for the comment. Based on information submitted, we are not able to validate that MKO Melt reduces the use of opioids. We note that ketamine, one component of MKO melt, exhibits some addictive properties. Moreover, we did not identify any evidence that MKO Melt is effective for patients with a prior opioid addiction nor did we receive any data demonstrating that the current ASC packaging policy incentivized providers to use opioids over MKO Melt. In accordance with section 1833(i)(8) of the Act, the fact that there is no HPCPS code for the drug, and lack of FDA approval, we were not able to identify any compelling evidence that MKO Melt should be excluded from packaged payment.
Comment: Several commenters, including individual physicians, medical associations, and device manufacturers commented supporting separate payment for continuous peripheral nerve blocks as they significantly reduce opioid use. One commenter suggested that CMS provide separate payment for HCPCS code A4306 (Disposable drug delivery system, flow rate of less than 50 ml per hour) in the hospital outpatient department setting and the ASC setting because packaging represents a cost barrier for providers. The commenter contended that continuous nerve block procedures have been shown in high quality clinical studies to reduce the use of opioids, attaching studies for review. They believe that separate payment for A4306 will remove the financial disincentive for HOPDs and ASCs, encouraging continuous nerve blocks as a non-opioid alternative for post-surgical pain management.
Response: We appreciate the commenter's suggestion. We examined the data for A4306 and noted an overall trend of increasing utilization from CY 2014 through CY 2017. Additionally, the geometric mean cost for A4306 was approximately $30 each year during that four-year period. We acknowledge that use of these items may help in the reduction of opioid use. However, we note that packaged payment of such an item does not prevent the use of these items. We do not believe that the current utilization trends for HCPCS code A4306 in the ASC setting suggest that the packaged payment is preventing use and remind readers that payment for packaged items is included in the payment for the primary service. We share the commenter's concern about the need to reduce opioid use and will take the commenter's suggestion regarding the need for separate payment for HCPCS code A4306 in the ASC setting into consideration for future rulemaking.
Comment: Multiple commenters identified other non-opioid pain management alternatives that they believe decrease the dose, duration, and/or number of opioid prescriptions beneficiaries receive during and following an outpatient visit or procedure (especially for beneficiaries at high-risk for opioid addiction) and may warrant separate payment for CY 2020. Commenters representing various stakeholders requested separate payments for various non-opioid pain management treatments, such as continuous nerve blocks (neuromodulation, radiofrequency ablation, implants for lumbar stenosis, protocols (ERAS®) IV acetaminophen, IV ibuprofen, Polar ice devices for postoperative pain relief, THC oil, acupuncture, and dry needling procedures.
For neuromodulation, several commenters noted that spinal cord stimulators (SCS) may lead to a reduction in the use of opioids for chronic pain patients. One manufacturer of SCS devices commented that SCS provides the opportunity to potentially stabilize or decrease opioid usage and that neuromodulation retains its efficacy over multiple years. Regarding barriers to access, the commenter noted that Medicare beneficiaries often do not have access to SCS until after they have exhausted other treatments, which often includes opioids. The commenter presented evidence from observational studies that use of SCS earlier in a patient's treatment could help reduce opioid use while controlling pain, and suggested that CMS look for ways to incorporate SCS earlier in the treatment continuum, suggesting CMS develop additional education and outreach efforts and incentives for appropriate referrals of patients with chronic pain to comprehensive pain management practices for consultation and evaluation prior to the administration of opioids. The commenter suggested that CMS could provide alerts to providers regarding the benefits of pain management consultation with a qualified pain management professional prior to the administration of opioids for chronic conditions.
Another commenter asserted that the standard endpoints, such as a greater than 50 percent reduction in pain, that are used to determine if a neuromodulation-based non-opioid pain alternative therapy is effective are well-established and validated in all types of clinical trials and that CMS should establish a general, national coverage determination for neuromodulation-based non-opioid pain therapy based on these endpoints, rather than taking the time to create and process specific national coverage determinations or local coverage determinations. The commenter suggested that this would be a much faster and streamlined process for enhancing Medicare beneficiary access to neuromodulation-based pain management therapies.
One manufacturer of a high-frequency SCS device stated that additional payment was warranted for non-opioid pain management treatments because they provide an alternative treatment option to opioids for patients with chronic leg or back pain. The commenter provided supporting studies which claimed that patients treated with their high-frequency SCS device reported a statistically significant average decrease in opioid use compared to the control group. This commenter also submitted data that showed a decline in the mean daily dosage of opioid medication taken and that fewer patients were relying on opioids at all to manage their pain when they used the manufacturer's device.
Other commenters wrote regarding their personal experiences in regards to radiofrequency ablation for sacral iliac joints and knees. One commenter referenced several studies, one of which found a decrease in analgesic medications associated with radiofrequency ablation; however, it did not provide evidence regarding a decrease in opioid usage.
One national hospital association commenter recommended that while “certainly not a solution to the opioid epidemic, unpackaging appropriate non-opioid therapies, like Exparel, is a low-cost tactic that could change long-standing practice patterns without major negative consequences.” This same commenter suggested that Medicare consider separate payment for IV acetaminophen, IV ibuprofen, and Polar ice devices for postoperative pain relief after knee procedures. The commenter also noted that therapeutic massage, topically applied THC oil, acupuncture, and dry needling procedures are very effective therapies for relief of both postoperative pain and long-term and chronic pain. Several other commenters expressed support for IV acetaminophen.
Response: We appreciate the detailed responses from commenters on this topic. At this time, we have not found compelling evidence for other non-opioid pain management alternatives described above to warrant separate payment under the OPPS or ASC payment systems for CY 2020, however we plan to take these comments and suggestions into consideration for future rulemaking. We agree that providing incentives to avoid or reduce opioid prescriptions may be one of several strategies for addressing the opioid epidemic. To the extent that the items and services mentioned by the commenters are effective alternatives to opioid drugs, we encourage providers to use them when medically appropriate. We note that some of the items and services mentioned by commenters are not covered by Medicare, and we do not intend to establish payment for noncovered items and services. We look forward to working with stakeholders as we further consider suggested refinements to the OPPS and the ASC payment system that will encourage use of medically necessary items and services that have demonstrated efficacy in decreasing opioid prescriptions or opioid abuse or misuse during or after an outpatient visit or procedure.
After reviewing the non-opioid pain management alternatives suggested by the commenters as well as the studies and other data provided to support the request for separate payment, we have not determined that separate payment is warranted at this time for most of the non-opioid pain management alternatives discussed above. However, we continue to believe the separate payment is appropriate for non-opioid pain management drugs that function as surgical supplies, like Exparel, when furnished in the ASC setting and are finalizing this policy for CY 2020.
Comment: Several commenters addressed payment barriers that may inhibit access to non-opioid pain management treatments previously discussed throughout this section. Several commenters disagreed with CMS's assessment that current payment policies do not represent barriers to access for certain non-opioid pain management alternatives. One commenter encouraged CMS to provide timely insurance coverage for evidence-informed interventional procedures early in the course of treatment when clinically appropriate, noting that they hope CMS will reconsider its position and provide mechanisms for separate payment and patient access to evidence-based, FDA approved and cleared medical device enabled interventions that would provide alternatives to opioid pain management interventions. Several other commenters encouraged CMS to more broadly evaluate all of its packaging policies to help ensure patient access to appropriate therapies and to assess how packaging affects the utilization of a medicine and use the results of that evaluation to guide future policy development.
Response: We appreciate the various, insightful comments we received from stakeholders regarding barriers that may inhibit access to non-opioid alternatives for pain treatment and management in order to more effectively address the opioid epidemic. We will take these comments into consideration for future consideration. Many of these comments have been previously addressed throughout this section.
After consideration of the public comments that we received, we are finalizing the policy to continue to unpackage and pay separately at ASP + 6 percent for the cost of non-opioid pain management drugs that function as surgical supplies when they are furnished in the ASC setting for CY 2020 as proposed. We will continue to analyze the issue of access to non-opioid alternatives in the OPPS and ASC settings as we implement section 6082 of the SUPPORT Act and section 1833(i)(8). This policy is also discussed in section II.A.3.b. of this final rule with comment period.
E. New Technology Intraocular Lenses (NTIOLs)
New Technology Intraocular Lenses (NTIOLs) are intraocular lenses that replace a patient's natural lens that has been removed in cataract surgery and that also meet the requirements listed in 42 CFR 416.195.
1. NTIOL Application Cycle
Our process for reviewing applications to establish new classes of NTIOLs is as follows:
- Applicants submit their NTIOL requests for review to CMS by the annual deadline. For a request to be considered complete, we require submission of the information that is found in the guidance document entitled “Application Process and Information Requirements for Requests for a New Class of New Technology Intraocular Lenses (NTIOLs) or Inclusion of an IOL in an Existing NTIOL Class” posted on the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/NTIOLs.html.
- We announce annually, in the proposed rule updating the ASC and OPPS payment rates for the following calendar year, a list of all requests to establish new NTIOL classes accepted for review during the calendar year in which the proposal is published. In accordance with section 141(b)(3) of Public Law 103-432 and our regulations at § 416.185(b), the deadline for receipt of public comments is 30 days following publication of the list of requests in the proposed rule.
- In the final rule updating the ASC and OPPS payment rates for the following calendar year, we—
++ Provide a list of determinations made as a result of our review of all new NTIOL class requests and public comments;
++ When a new NTIOL class is created, identify the predominant characteristic of NTIOLs in that class that sets them apart from other IOLs (including those previously approved as members of other expired or active NTIOL classes) and that is associated with an improved clinical outcome.
++ Set the date of implementation of a payment adjustment in the case of approval of an IOL as a member of a new NTIOL class prospectively as of 30 days after publication of the ASC payment update final rule, consistent with the statutory requirement.
++ Announce the deadline for submitting requests for review of an application for a new NTIOL class for the following calendar year.
2. Requests To Establish New NTIOL Classes for CY 2020
We did not receive any requests for review to establish a new NTIOL class for CY 2020 by March 1, 2019, the due date published in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59072).
3. Payment Adjustment
The current payment adjustment for a 5-year period from the implementation date of a new NTIOL class is $50 per lens. Since implementation of the process for adjustment of payment amounts for NTIOLs in 1999, we have not revised the payment adjustment amount, and we did not proposing to revise the payment adjustment amount for CY 2020.
The comments and our responses to the comments are set forth below.
Comment: Two commenters requested that we re-evaluate our payment adjustment for new NTIOL class. Commenters noted that our $50 payment adjustment has not been adjusted since CY 1999 and that the stagnant payment adjustment has been a barrier to intraocular lens innovation. One commenter requested that the $50 be inflated to 2020 dollars and updated by inflation in subsequent years. Another commenter requested that we updated the $50 payment adjustment to $100, which is the approximate dollar amount of our $50 payment adjustment had we increased the adjustment based on the increase in CPI-U for medical care.
Response: We thank the commenters for their recommendation. We did not propose revising the payment adjustment amount for CY 2020. However, we will take commenters recommendations into consideration in future rulemaking.
After consideration of the public comments we received, we are finalizing our proposal to maintain the payment adjustment of a new NTIOL class at $50 per lens for CY 2020 without modification.
F. ASC Payment and Comment Indicators
1. Background
In addition to the payment indicators that we introduced in the August 2, 2007 final rule, we created final comment indicators for the ASC payment system in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66855). We created Addendum DD1 to define ASC payment indicators that we use in Addenda AA and BB to provide payment information regarding covered surgical procedures and covered ancillary services, respectively, under the revised ASC payment system. The ASC payment indicators in Addendum DD1 are intended to capture policy-relevant characteristics of HCPCS codes that may receive packaged or separate payment in ASCs, such as whether they were on the ASC CPL prior to CY 2008; payment designation, such as device-intensive or office-based, and the corresponding ASC payment methodology; and their classification as separately payable ancillary services, including radiology services, brachytherapy sources, OPPS pass-through devices, corneal tissue acquisition services, drugs or biologicals, or NTIOLs.
We also created Addendum DD2 that lists the ASC comment indicators. The ASC comment indicators included in Addenda AA and BB to the proposed rules and final rules with comment period serve to identify, for the revised ASC payment system, the status of a specific HCPCS code and its payment indicator with respect to the timeframe when comments will be accepted. The comment indicator “NI” is used in the OPPS/ASC final rule to indicate new codes for the next calendar year for which the interim payment indicator assigned is subject to comment. The comment indicator “NI” also is assigned to existing codes with substantial revisions to their descriptors such that we consider them to be describing new services, and the interim payment indicator assigned is subject to comment, as discussed in the CY 2010 OPPS/ASC final rule with comment period (74 FR 60622).
The comment indicator “NP” is used in the OPPS/ASC proposed rule to indicate new codes for the next calendar year for which the proposed payment indicator assigned is subject to comment. The comment indicator “NP” also is assigned to existing codes with substantial revisions to their descriptors, such that we consider them to be describing new services, and the proposed payment indicator assigned is subject to comment, as discussed in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70497).
The “CH” comment indicator is used in Addenda AA and BB to the proposed rule (which are available via the internet on the CMS website) to indicate that the payment indicator assignment has changed for an active HCPCS code in the current year and the next calendar year, for example if an active HCPCS code is newly recognized as payable in ASCs; or an active HCPCS code is discontinued at the end of the current calendar year. The “CH” comment indicators that are published in the final rule with comment period are provided to alert readers that a change has been made from one calendar year to the next, but do not indicate that the change is subject to comment.
2. ASC Payment and Comment Indicators for CY 2020
In the CY 2020 OPPS/ASC proposed rule, we proposed new and revised Category I and III CPT codes as well as new and revised Level II HCPCS codes. Therefore, proposed Category I and III CPT codes that are new and revised for CY 2020 and any new and existing Level II HCPCS codes with substantial revisions to the code descriptors for CY 2020 compared to the CY 2019 descriptors are included in ASC Addenda AA and BB to this proposed rule were labeled with proposed comment indicator “NP” to indicate that these CPT and Level II HCPCS codes were open for comment as part of the proposed rule. Proposed comment indicator “NP” meant a new code for the next calendar year or an existing code with substantial revision to its code descriptor in the next calendar year, as compared to current calendar year; and denoted that comments would be accepted on the proposed ASC payment indicator for the new code.
In the CY 2020 OPPS/ASC proposed rule, we stated that we would respond to public comments on ASC payment and comment indicators and finalize their ASC assignment in the CY 2020 OPPS/ASC final rule with comment period. We referred readers to Addenda DD1 and DD2 of the CY 2020 OPPS/ASC proposed rule (which are available via the internet on the CMS website) for the complete list of ASC payment and comment indicators proposed for the CY 2020 update. We did not receive any public comments on the ASC payment and comment indicators. Therefore, we are finalizing their use as proposed without modification. Addenda DD1 and DD2 to this final rule with comment period (which are available via the internet on the CMS website) contain the complete list of ASC payment and comment indicators for CY 2020.
G. Calculation of the ASC Payment Rates and the ASC Conversion Factor
1. Background
In the August 2, 2007 final rule (72 FR 42493), we established our policy to base ASC relative payment weights and payment rates under the revised ASC payment system on APC groups and the OPPS relative payment weights. Consistent with that policy and the requirement at section 1833(i)(2)(D)(ii) of the Act that the revised payment system be implemented so that it would be budget neutral, the initial ASC conversion factor (CY 2008) was calculated so that estimated total Medicare payments under the revised ASC payment system in the first year would be budget neutral to estimated total Medicare payments under the prior (CY 2007) ASC payment system (the ASC conversion factor is multiplied by the relative payment weights calculated for many ASC services in order to establish payment rates). That is, application of the ASC conversion factor was designed to result in aggregate Medicare expenditures under the revised ASC payment system in CY 2008 being equal to aggregate Medicare expenditures that would have occurred in CY 2008 in the absence of the revised system, taking into consideration the cap on ASC payments in CY 2007, as required under section 1833(i)(2)(E) of the Act (72 FR 42522). We adopted a policy to make the system budget neutral in subsequent calendar years (72 FR 42532 through 42533; § 416.171(e)).
We note that we consider the term “expenditures” in the context of the budget neutrality requirement under section 1833(i)(2)(D)(ii) of the Act to mean expenditures from the Medicare Part B Trust Fund. We do not consider expenditures to include beneficiary coinsurance and copayments. This distinction was important for the CY 2008 ASC budget neutrality model that considered payments across the OPPS, ASC, and MPFS payment systems. However, because coinsurance is almost always 20 percent for ASC services, this interpretation of expenditures has minimal impact for subsequent budget neutrality adjustments calculated within the revised ASC payment system.
In the CY 2008 OPPS/ASC final rule with comment period (72 FR 66857 through 66858), we set out a step-by-step illustration of the final budget neutrality adjustment calculation based on the methodology finalized in the August 2, 2007 final rule (72 FR 42521 through 42531) and as applied to updated data available for the CY 2008 OPPS/ASC final rule with comment period. The application of that methodology to the data available for the CY 2008 OPPS/ASC final rule with comment period resulted in a budget neutrality adjustment of 0.65.
For CY 2008, we adopted the OPPS relative payment weights as the ASC relative payment weights for most services and, consistent with the final policy, we calculated the CY 2008 ASC payment rates by multiplying the ASC relative payment weights by the final CY 2008 ASC conversion factor of $41.401. For covered office-based surgical procedures, covered ancillary radiology services (excluding covered ancillary radiology services involving certain nuclear medicine procedures or involving the use of contrast agents, as discussed in section XII.D.2. of the CY 2020 OPPS/ASC proposed rule), and certain diagnostic tests within the medicine range that are covered ancillary services, the established policy is to set the payment rate at the lower of the MPFS unadjusted nonfacility PE RVU-based amount or the amount calculated using the ASC standard ratesetting methodology. Further, as discussed in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66841 through 66843), we also adopted alternative ratesetting methodologies for specific types of services (for example, device-intensive procedures).
As discussed in the August 2, 2007 final rule (72 FR 42517 through 42518) and as codified at § 416.172(c) of the regulations, the revised ASC payment system accounts for geographic wage variation when calculating individual ASC payments by applying the pre-floor and pre-reclassified IPPS hospital wage indexes to the labor-related share, which is 50 percent of the ASC payment amount based on a GAO report of ASC costs using 2004 survey data. Beginning in CY 2008, CMS accounted for geographic wage variation in labor costs when calculating individual ASC payments by applying the pre-floor and pre-reclassified hospital wage index values that CMS calculates for payment under the IPPS, using updated Core Based Statistical Areas (CBSAs) issued by OMB in June 2003.
The reclassification provision in section 1886(d)(10) of the Act is specific to hospitals. We believe that using the most recently available pre-floor and pre-reclassified IPPS hospital wage indexes results in the most appropriate adjustment to the labor portion of ASC costs. We continue to believe that the unadjusted hospital wage indexes, which are updated yearly and are used by many other Medicare payment systems, appropriately account for geographic variation in labor costs for ASCs. Therefore, the wage index for an ASC is the pre-floor and pre-reclassified hospital wage index under the IPPS of the CBSA that maps to the CBSA where the ASC is located.
Generally, OMB issues major revisions to statistical areas every 10 years, based on the results of the decennial census. On February 28, 2013, OMB issued OMB Bulletin No. 13-01, which provides the delineations of all Metropolitan Statistical Areas, Metropolitan Divisions, Micropolitan Statistical Areas, Combined Statistical Areas, and New England City and Town Areas in the United States and Puerto Rico based on the standards published on June 28, 2010 in the Federal Register (75 FR 37246 through 37252) and 2010 Census Bureau data. (A copy of this bulletin may be obtained at: https://www.whitehouse.gov/sites/whitehouse.gov/files/omb/bulletins/2013/b13-01.pdf.) In the FY 2015 IPPS/LTCH PPS final rule (79 FR 49951 through 49963), we implemented the use of the CBSA delineations issued by OMB in OMB Bulletin 13-01 for the IPPS hospital wage index beginning in FY 2015.
OMB occasionally issues minor updates and revisions to statistical areas in the years between the decennial censuses. On July 15, 2015, OMB issued OMB Bulletin No. 15-01, which provides updates to and supersedes OMB Bulletin No. 13-01 that was issued on February 28, 2013. OMB Bulletin No. 15-01 made changes that are relevant to the IPPS and ASC wage index. We refer readers to the CY 2017 OPPS/ASC final rule with comment period (81 FR 79750) for a discussion of these changes and our implementation of these revisions. (A copy of this bulletin may be obtained at https://www.whitehouse.gov/sites/whitehouse.gov/files/omb/bulletins/2015/15-01.pdf.)
On August 15, 2017, OMB issued OMB Bulletin No. 17-01, which provided updates to and superseded OMB Bulletin No. 15-01 that was issued on July 15, 2015. We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 58864 through 58865) for a discussion of these changes and our implementation of these revisions. (A copy of this bulletin may be obtained at https://www.whitehouse.gov/sites/whitehouse.gov/files/omb/bulletins/2017/b-17-01.pdf.)
For CY 2020, the proposed CY 2020 ASC wage indexes fully reflect the OMB labor market area delineations (including the revisions to the OMB labor market delineations discussed above, as set forth in OMB Bulletin Nos. 15-01 and 17-01).
We note that, in certain instances, there might be urban or rural areas for which there is no IPPS hospital that has wage index data that could be used to set the wage index for that area. For these areas, our policy has been to use the average of the wage indexes for CBSAs (or metropolitan divisions as applicable) that are contiguous to the area that has no wage index (where “contiguous” is defined as sharing a border). For example, for CY 2014, we applied a proxy wage index based on this methodology to ASCs located in CBSA 25980 (Hinesville-Fort Stewart, GA) and CBSA 08 (Rural Delaware).
When all of the areas contiguous to the urban CBSA of interest are rural and there is no IPPS hospital that has wage index data that could be used to set the wage index for that area, we determine the ASC wage index by calculating the average of all wage indexes for urban areas in the state (75 FR 72058 through 72059). (In other situations, where there are no IPPS hospitals located in a relevant labor market area, we continue our current policy of calculating an urban or rural area's wage index by calculating the average of the wage indexes for CBSAs (or metropolitan divisions where applicable) that are contiguous to the area with no wage index.)
2. Calculation of the ASC Payment Rates
a. Updating the ASC Relative Payment Weights for CY 2020 and Future Years
We update the ASC relative payment weights each year using the national OPPS relative payment weights (and PFS nonfacility PE RVU-based amounts, as applicable) for that same calendar year and uniformly scale the ASC relative payment weights for each update year to make them budget neutral (72 FR 42533). Consistent with our established policy, we proposed to scale the CY 2020 relative payment weights for ASCs according to the following method. Holding ASC utilization, the ASC conversion factor, and the mix of services constant from CY 2018, we proposed to compare the total payment using the CY 2019 ASC relative payment weights with the total payment using the CY 2020 ASC relative payment weights to take into account the changes in the OPPS relative payment weights between CY 2019 and CY 2020. We proposed to use the ratio of CY 2019 to CY 2020 total payments (the weight scalar) to scale the ASC relative payment weights for CY 2020. The proposed CY 2020 ASC weight scalar is 0.8452 and scaling would apply to the ASC relative payment weights of the covered surgical procedures, covered ancillary radiology services, and certain diagnostic tests within the medicine range of CPT codes, which are covered ancillary services for which the ASC payment rates are based on OPPS relative payment weights.
Scaling would not apply in the case of ASC payment for separately payable covered ancillary services that have a predetermined national payment amount (that is, their national ASC payment amounts are not based on OPPS relative payment weights), such as drugs and biologicals that are separately paid or services that are contractor-priced or paid at reasonable cost in ASCs. Any service with a predetermined national payment amount would be included in the ASC budget neutrality comparison, but scaling of the ASC relative payment weights would not apply to those services. The ASC payment weights for those services without predetermined national payment amounts (that is, those services with national payment amounts that would be based on OPPS relative payment weights) would be scaled to eliminate any difference in the total payment between the current year and the update year.
For any given year's ratesetting, we typically use the most recent full calendar year of claims data to model budget neutrality adjustments. At the time of the proposed rule, we had available 98 percent of CY 2018 ASC claims data.
The comments and our responses to the comments are set forth below.
Comment: A majority of commenters believe that CMS needs to reduce the disparity in payments between ASCs and HOPDs. Commenters stated that ASC payment rates are less than 50 percent of the HOPD payment rates for some high volume procedures. Many of these same commenters support the discontinuation of the ASC weight scalar, which they believe is the cause of the payment gap between ASCs and HOPDs. Commenters suggested that the ASC weight scalar as currently applied may make it economically infeasible for ASC facilities to continue to perform Medicare cases, which would hurt beneficiaries and limit their access to high-quality outpatient surgical care. They suggested that eliminating the secondary rescaling that is currently applied to ASC payments would allow ASCs to continue to provide quality surgical care for Medicare patients.
Several commenters requested that CMS apply the same OPPS relative weights to ASC services and discontinue rescaling the ASC relative weights. They provided that while they understand the additional scaling factor that CMS applies to the ASC APC weight maintains budget neutrality within the ASC payment system, this scaling contributes to the large payment differentials for similar services between the ASC and HOPD systems.
Response: We note that applying the weight scalar in calculation of ASC payment rates, for this final rule with comment period it is 0.8550, ensures that the ASC payment system remains budget neutral. We understand the commenters do not believe that calculation of the weight scalar in the ASC is necessary and their belief that its application leads to large payment differentials for similar services between the OPPS and ASC payment systems. However, as noted in previous rulemaking (83 FR 59076), we do not believe that the ASC cost structure is identical to the hospital cost structure. Further, we do not collect cost data from ASCs, and therefore we are unsure of the actual differences in costs between the two sites of service. We have not witnessed beneficiary access issues when it comes to receiving care in an ASC and note that there are more ASCs than there are hospitals; we do not agree that the current ASC payment methodology has created an access to care issue for ASCs. Additionally, the ASC payment system was not designed to mirror that of the OPPS; a large part of the value of ASCs is that they provide a lower cost option for surgical procedures than some other settings.
To create an analytic file to support calculation of the weight scalar and budget neutrality adjustment for the wage index (discussed below), we summarized available CY 2017 ASC claims by ASC and by HCPCS code. We used the National Provider Identifier for the purpose of identifying unique ASCs within the CY 2018 claims data. We used the supplier zip code reported on the claim to associate state, county, and CBSA with each ASC. This file, available to the public as a supporting data file for the proposed rule, is posted on the CMS website at http://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/LimitedDataSets/ASCPaymentSystem.html.
b. Updating the ASC Conversion Factor
Under the OPPS, we typically apply a budget neutrality adjustment for provider level changes, most notably a change in the wage index values for the upcoming year, to the conversion factor. Consistent with our final ASC payment policy, for the CY 2017 ASC payment system and subsequent years, in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79751 through 79753), we finalized our policy to calculate and apply a budget neutrality adjustment to the ASC conversion factor for supplier level changes in wage index values for the upcoming year, just as the OPPS wage index budget neutrality adjustment is calculated and applied to the OPPS conversion factor. For CY 2020, we calculated the proposed adjustment for the ASC payment system by using the most recent CY 2018 claims data available and estimating the difference in total payment that would be created by introducing the proposed CY 2020 ASC wage indexes. Specifically, holding CY 2018 ASC utilization, service-mix, and the proposed CY 2020 national payment rates after application of the weight scalar constant, we calculated the total adjusted payment using the CY 2019 ASC wage indexes and the total adjusted payment using the proposed CY 2020 ASC wage indexes. We used the 50-percent labor-related share for both total adjusted payment calculations. We then compared the total adjusted payment calculated with the CY 2019 ASC wage indexes to the total adjusted payment calculated with the proposed CY 2020 ASC wage indexes and applied the resulting ratio of 1.0008 (the proposed CY 2020 ASC wage index budget neutrality adjustment) to the CY 2019 ASC conversion factor to calculate the proposed CY 2020 ASC conversion factor.
Section 1833(i)(2)(C)(i) of the Act requires that, if the Secretary has not updated amounts established under the revised ASC payment system in a calendar year, the payment amounts shall be increased by the percentage increase in the Consumer Price Index for all urban consumers (CPI-U), U.S. city average, as estimated by the Secretary for the 12-month period ending with the midpoint of the year involved. The statute does not mandate the adoption of any particular update mechanism, but it requires the payment amounts to be increased by the CPI-U in the absence of any update. Because the Secretary updates the ASC payment amounts annually, we adopted a policy, which we codified at § 416.171(a)(2)(ii)), to update the ASC conversion factor using the CPI-U for CY 2010 and subsequent calendar years.
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59075 through 59080), we finalized our proposal to apply the hospital market basket update to ASC payment system rates for an interim period of 5 years (CY 2019 through CY 2023), during which we will assess whether there is a migration of the performance of procedures from the hospital setting to the ASC setting as a result of the use of a hospital market basket update, as well as whether there are any unintended consequences, such as less than expected migration of the performance of procedures from the hospital setting to the ASC setting. In addition, we finalized our proposal to revise our regulations under § 416.171(a)(2), which address the annual update to the ASC conversion factor. During this 5-year period, we intend to assess the feasibility of collaborating with stakeholders to collect ASC cost data in a minimally burdensome manner and could propose a plan to collect such information. We refer readers to that final rule for a detailed discussion of the rationale for these policies.
As stated in the CY 2020 OPPS/ASC proposed rule (84 FR 39552), the hospital market basket update for CY 2020 was to be 3.2 percent, as published in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19402), based on IHS Global Inc.'s (IGI's) 2018 fourth quarter forecast with historical data through the third quarter of 2018. For this CY 2020 OPPS/ASC final rule with comment period, as published in the FY 2019 IPPS/LTCH PPS final rule (84 FR 42343), based on IGI's 2019 second quarter forecast with historical data through the first quarter of 2019, the hospital market basket update for CY 2020 is 3.0 percent.
We finalized the methodology for calculating the MFP adjustment in the CY 2011 PFS final rule with comment period (75 FR 73394 through 73396) and revised it in the CY 2012 PFS final rule with comment period (76 FR 73300 through 73301) and the CY 2016 OPPS/ASC final rule with comment period (80 FR 70500 through 70501). As stated in the CY 2020 OPPS/ASC proposed rule (84 FR 39553), the proposed MFP adjustment for CY 2020 was projected to be 0.5 percentage point, as published in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 19402) based on IGI's 2018 fourth quarter forecast. For this CY 2020 OPPS/ASC final rule with comment period, as published in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42343) based on IGI's 2019 second quarter forecast, the final MFP adjustment for CY 2020 is 0.4 percentage point.
For CY 2020, we proposed to utilize the hospital market basket update of 3.2 percent minus the MFP adjustment of 0.5 percentage point, resulting in an MFP-adjusted hospital market basket update factor of 2.7 percent for ASCs meeting the quality reporting requirements. Therefore, we proposed to apply a 2.7 percent MFP-adjusted hospital market basket update factor to the CY 2019 ASC conversion factor for ASCs meeting the quality reporting requirements to determine the CY 2020 ASC payment amounts. The ASCQR Program affected payment rates beginning in CY 2014 and, under this program, there is a 2.0 percentage point reduction to the update factor for ASCs that fail to meet the ASCQR Program requirements. We referred readers to section XIV.E. of the CY 2019 OPPS/ASC final rule with comment period (83 FR 59138 through 59139) and section XIV.E. of the CY 2020 OPPS/ASC proposed rule for a detailed discussion of our policies regarding payment reduction for ASCs that fail to meet ASCQR Program requirements. We proposed to utilize the hospital market basket update of 3.2 percent reduced by 2.0 percentage points for ASCs that do not meet the quality reporting requirements and then subtract the 0.5 percentage point MFP adjustment. Therefore, we proposed to apply a 0.7 percent MFP-adjusted hospital market basket update factor to the CY 2019 ASC conversion factor for ASCs not meeting the quality reporting requirements. We also proposed that if more recent data are subsequently available (for example, a more recent estimate of the hospital market basket update and MFP), we would use such data, if appropriate, to determine the CY 2020 ASC update for the CY 2020 OPPS/ASC final rule with comment period.
For CY 2020, we proposed to adjust the CY 2019 ASC conversion factor ($46.532) by the proposed wage index budget neutrality factor of 1.0008 in addition to the MFP-adjusted hospital market basket update factor of 2.7 percent discussed above, which results in a proposed CY 2020 ASC conversion factor of $47.827 for ASCs meeting the quality reporting requirements. For ASCs not meeting the quality reporting requirements, we proposed to adjust the CY 2019 ASC conversion factor ($46.532) by the proposed wage index budget neutrality factor of 1.0008 in addition to the quality reporting/MFP-adjusted hospital market basket update factor of 0.7 percent discussed above, which results in a proposed CY 2020 ASC conversion factor of $46.895.
The comments and our responses are set forth below.
Comment: The majority of commenters supported continued use of the hospital market basket for updating ASC payments on an annual basis. Some commenters suggested that aligning the update factors between the OPPS and ASC settings will encourage the migration of care to the ASC setting by making ASC payment more competitive with hospital payment, while other commenters supported the decision as it would promote site-neutrality between the two settings of care through more competitive payment. However, other commenters, despite their support for the use of the hospital market basket to update ASC payment rates, believed that the migration of services to ASCs would be limited due to the ASC budget neutrality adjustments. Commenters stated that CMS' current approach to maintaining budget neutrality in the ASC payment system caused increasing differentials in payment for services provided in the ASC and HOPD settings, and there was no evidence of corresponding changes in capital and operating costs between the ASC and HOPD settings to support this growing payment differential. Commenters noted that widening the gap in payments could make it economically difficult for ASCs to perform certain procedures, discouraging ASCs from furnishing those procedures and thereby discouraging the migration of services from the HOPD to the ASC setting. MedPAC did not support using the hospital market basket index as an interim method for updating the ASC conversion factor, noting that evidence has indicated the hospital market basket index does not accurately reflect the costs of ASCs. MedPAC noted the differences in cost structure between the HOPD and ASC settings could be attributed to a number of factors, including different patient populations, expenses, employee compensation, and regulations.
Response: We appreciate the commenters' support. We believe providing ASCs with the same rate update as hospitals encourages the migration of services from the hospital setting to the ASC setting and could increase the presence of ASCs in health care markets or geographic areas where previously there were none or few. The migration of services from the higher cost hospital outpatient setting to the ASC setting is likely to result in savings to beneficiaries and the Medicare program. This policy also gives both physicians and beneficiaries greater choice in selecting the best care setting.
In addition, we acknowledge MedPAC's comment regarding the collection of ASC cost data and differences in cost structure between the HOPD and ASC settings. We appreciate these comments and will take these comments into consideration in future policy development.
Comment: Multiple commenters expressed their opposition to collecting ASC cost data, due to the anticipated administrative burden associated with collecting this data. Commenters suggested that collecting ASC cost data would prevent ASCs from providing efficient low-cost care. MedPAC suggested that CMS begin collecting ASC cost data immediately, forgoing the final four years of its planned five-year period to assess the feasibility of collaborating with stakeholders to collect ASC cost data in a minimally burdensome manner and potentially to propose a plan to collect such information. MedPAC suggested that CMS use its existing authority and resources to act quickly in gathering ASC cost data. MedPAC noted that beneficial information could be gathered to inform ASC payment updates and asserted that there is sufficient evidence that ASC can capably submit cost data.
Response: We thank the commenters for their input. As discussed in the CY 2019 OPPS/ASC final rule with comment period, we intend to assess the feasibility of collaborating with stakeholders to collect ASC cost data in a minimally burdensome manner and potentially propose a plan to collect such information over a 5-year period (83 FR 59077). We will continue to assess the feasibility of collaborating with stakeholders to collect ASC cost data in a minimally burdensome manner for future policy development.
After consideration of the public comments we received, consistent with our proposal that if more recent data are subsequently available (for example, a more recent estimate of the hospital market basket update and MFP), we would use such data, if appropriate, to determine the CY 2020 ASC update for the CY 2020 OPPS/ASC final rule with comment period, we are incorporating more recent data to determine the final CY 2020 ASC update. Therefore, for this CY 2020 OPPS/ASC final rule with comment period, the hospital market basket update for CY 2020 is 3.0 percent, as published in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42343), based on IGI's 2019 second quarter forecast with historical data through the first quarter of 2019. The MFP adjustment for this CY 2020 OPPS/ASC final rule with comment period is 0.4 percentage point, as published in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42343) based on IGI's 2019 second quarter forecast.
For CY 2020, we are finalizing the hospital market basket update of 3.0 percent minus the MFP adjustment of 0.4 percentage point, resulting in an MFP-adjusted hospital market basket update factor of 2.6 percent for ASCs meeting the quality reporting requirements. Therefore, we apply a 2.6 percent MFP-adjusted hospital market basket update factor to the CY 2019 ASC conversion factor for ASCs meeting the quality reporting requirements to determine the CY 2020 ASC payment rates.
3. Display of Final CY 2020 ASC Payment Rates
Addenda AA and BB to this final rule (which are available on the CMS website) display the final updated ASC payment rates for CY 2020 for covered surgical procedures and covered ancillary services, respectively. For those covered surgical procedures and covered ancillary services where the payment rate is the lower of the proposed rates under the ASC standard ratesetting methodology and the MPFS final rates, the final payment indicators and rates set forth in this final rule are based on a comparison using the finalized PFS rates that would be effective January 1, 2020. For a discussion of the PFS rates, we refer readers to the CY 2020 PFS final rule that is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices.html.
The final payment rates included in addenda AA and BB to this final rule reflect the full ASC payment update and not the reduced payment update used to calculate payment rates for ASCs not meeting the quality reporting requirements under the ASCQR Program. These addenda contain several types of information related to the proposed CY 2020 payment rates. Specifically, in Addendum AA, a “Y” in the column titled “To be Subject to Multiple Procedure Discounting” indicates that the surgical procedure would be subject to the multiple procedure payment reduction policy. As discussed in the CY 2008 OPPS/ASC final rule with comment period (72 FR 66829 through 66830), most covered surgical procedures are subject to a 50-percent reduction in the ASC payment for the lower-paying procedure when more than one procedure is performed in a single operative session.
Display of the comment indicator “CH” in the column titled “Comment Indicator” indicates a change in payment policy for the item or service, including identifying discontinued HCPCS codes, designating items or services newly payable under the ASC payment system, and identifying items or services with changes in the ASC payment indicator for CY 2020. Display of the comment indicator “NI” in the column titled “Comment Indicator” indicates that the code is new (or substantially revised) and that comments will be accepted on the interim payment indicator for the new code. Display of the comment indicator “NP” in the column titled “Comment Indicator” indicates that the code is new (or substantially revised) and that comments will be accepted on the ASC payment indicator for the new code.
The values displayed in the column titled “Final CY 2020 Payment Weight” are the proposed relative payment weights for each of the listed services for CY 2020. The proposed relative payment weights for all covered surgical procedures and covered ancillary services where the ASC payment rates are based on OPPS relative payment weights were scaled for budget neutrality. Therefore, scaling was not applied to the device portion of the device-intensive procedures, services that are paid at the MPFS nonfacility PE RVU-based amount, separately payable covered ancillary services that have a predetermined national payment amount, such as drugs and biologicals and brachytherapy sources that are separately paid under the OPPS, or services that are contractor-priced or paid at reasonable cost in ASCs. This includes separate payment for non-opioid pain management drugs.
To derive the final CY 2020 payment rate displayed in the “Final CY 2020 Payment Rate” column, each ASC payment weight in the “Final CY 2020 Payment Weight” column was multiplied by the final CY 2020 conversion factor of $47.747. The conversion factor includes a budget neutrality adjustment for changes in the wage index values and the annual update factor as reduced by the productivity adjustment. The final CY 2020 ASC conversion factor uses the CY 2020 MFP-adjusted hospital market basket update factor of 2.6 percent (which is equal to the projected hospital market basket update of 3.0 percent minus a projected MFP adjustment of 0.4 percentage point).
In Addendum BB, there are no relative payment weights displayed in the “Final CY 2020 Payment Weight” column for items and services with predetermined national payment amounts, such as separately payable drugs and biologicals. The “Final CY 2020 Payment” column displays the proposed CY 2020 national unadjusted ASC payment rates for all items and services. The proposed CY 2020 ASC payment rates listed in Addendum BB for separately payable drugs and biologicals are based on ASP data used for payment in physicians' offices in 2019.
Addendum EE provides the HCPCS codes and short descriptors for surgical procedures that are proposed to be excluded from payment in ASCs for CY 2020.
XIV. Requirements for the Hospital Outpatient Quality Reporting (OQR) Program
A. Background
1. Overview
CMS seeks to promote higher quality and more efficient healthcare for Medicare beneficiaries. Consistent with these goals, CMS has implemented quality reporting programs for multiple care settings including the quality reporting program for hospital outpatient care, known as the Hospital Outpatient Quality Reporting (OQR) Program, formerly known as the Hospital Outpatient Quality Data Reporting Program (HOP QDRP). The Hospital OQR Program is generally aligned with the quality reporting program for hospital inpatient services known as the Hospital Inpatient Quality Reporting (IQR) Program, formerly known as the Reporting Hospital Quality Data for Annual Payment Update (RHQDAPU) Program.
We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 58820 through 58822) where we discuss our Meaningful Measures Initiative and our approach in evaluating quality program measures.
2. Statutory History of the Hospital OQR Program
We refer readers to the CY 2011 OPPS/ASC final rule with comment period (75 FR 72064 through 72065) for a detailed discussion of the statutory history of the Hospital OQR Program.
3. Regulatory History of the Hospital OQR Program
We refer readers to the CY 2008 through 2019 OPPS/ASC final rules with comment period (72 FR 66860 through 66875; 73 FR 68758 through 68779; 74 FR 60629 through 60656; 75 FR 72064 through 72110; 76 FR 74451 through 74492; 77 FR 68467 through 68492; 78 FR 75090 through 75120; 79 FR 66940 through 66966; 80 FR 70502 through 70526; 81 FR 79753 through 79797; 82 FR 59424 through 59445; and 83 FR 59080 through 59110) for the regulatory history of the Hospital OQR Program. We have codified certain requirements under the Hospital OQR Program at 42 CFR 419.46.
B. Hospital OQR Program Quality Measures
1. Considerations in the Selection of Hospital OQR Program Quality Measures
We refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74458 through 74460) for a detailed discussion of the priorities we consider for the Hospital OQR Program quality measure selection. We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39554).
2. Retention of Hospital OQR Program Measures Adopted in Previous Payment Determinations
We previously adopted a policy to retain measures from a previous year's Hospital OQR Program measure set for subsequent years' measure sets in the CY 2013 OPPS/ASC final rule with comment period (77 FR 68471) whereby quality measures adopted in a previous year's rulemaking are retained in the Hospital OQR Program for use in subsequent years unless otherwise specified. For more information regarding this policy, we refer readers to that final rule with comment period. We codified this policy at 42 CFR 419.46(h)(1) in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59082). We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39554).
3. Removal of Quality Measures From the Hospital OQR Program Measure Set
In the CY 2010 OPPS/ASC final rule with comment period (74 FR 60635), we finalized a process to use the regular rulemaking process to remove a measure for circumstances for which we do not believe that continued use of a measure raises specific patient safety concerns.[82] We codified this policy at 42 CFR 419.46(h)(3) in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59082). We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39554).
a. Considerations in Removing Quality Measures From the Hospital OQR Program
(1) Immediate Removal
In the CY 2010 OPPS/ASC final rule with comment period (74 FR 60634 through 60635), we finalized a process for immediate retirement, which we later termed “removal,” of Hospital OQR Program measures, based on evidence that the continued use of the measure as specified raises patient safety concerns.[83] We codified this policy at 42 CFR 419.46(h)(2) in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59082). We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39554).
(2) Consideration Factors for Removing Measures
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59083 through 59085), we clarified, finalized, and codified at 42 CFR 419.46(h)(2) and (3) an updated set of factors [84] and policies for determining whether to remove measures from the Hospital OQR Program. We refer readers to that final rule with comment period for a detailed discussion of our policies regarding measure removal. The factors are:
- Factor 1. Measure performance among hospitals is so high and unvarying that meaningful distinctions and improvements in performance can no longer be made (“topped out” measures).
- Factor 2. Performance or improvement on a measure does not result in better patient outcomes.
- Factor 3. A measure does not align with current clinical guidelines or practice.
- Factor 4. The availability of a more broadly applicable (across settings, populations, or conditions) measure for the topic.
- Factor 5. The availability of a measure that is more proximal in time to desired patient outcomes for the particular topic.
- Factor 6. The availability of a measure that is more strongly associated with desired patient outcomes for the particular topic.
- Factor 7. Collection or public reporting of a measure leads to negative unintended consequences other than patient harm.
- Factor 8. The costs associated with a measure outweigh the benefit of its continued use in the program.
b. Removal of Quality Measure From the Hospital OQR Program Measure Set: OP-33: External Beam Radiotherapy (NQF# 1822)
In the CY 2020 OPPS/ASC proposed rule (84 FR 39554 through 39556), we proposed to remove one measure from the Hospital OQR Program for the CY 2022 payment determination as discussed below. Specifically, beginning with the CY 2022 payment determination, we proposed to remove OP-33: External Beam Radiotherapy for Bone Metastases under removal Factor 8, the costs associated with a measure outweigh the benefit of its continued use in the program.
We refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70507 through 70510), where we adopted OP-33: External Beam Radiotherapy (NQF# 1822), beginning with the CY 2018 payment determination and for subsequent years. This measure assesses the “percentage of patients (all-payer) with painful bone metastases and no history of previous radiation who receive External Beam Radiotherapy (EBRT) with an acceptable dosing schedule.” [85] We adopted this measure to address the performance gap in EBRT treatment variation, ensure appropriate use of EBRT, and prevent the overuse of radiation therapy (80 FR 70508).
We believe that removing OP-33 from the Hospital OQR Program is appropriate at this time because the costs associated with this measure outweigh the benefit of its continued use in the program (removal Factor 8). The Hospital OQR Program implemented the OP-33 measure using “radiation delivery” Current Procedural Terminology (CPT) codes, which are appropriate for hospital-level measurement. We have identified issues with reporting this measure, finding that more questions are received about how to report the OP-33 measure than about any other measure in the program. In addition, the measure steward has received feedback on data collection of the measure in the outpatient setting, and has indicated new and significant concerns regarding the “radiation delivery” CPT coding used to report the OP-33 measure in the Hospital OQR Program including complicated measure exclusions, sampling concerns, and administrative burden.
“Radiation delivery” CPT codes require complicated measure exclusions, and the use of “radiation delivery” CPT codes causes the administration of EBRT to different anatomic sites to be considered separate cases for this measure. The numerator for this measure includes all patients, regardless of age, with painful bone metastases, and no previous radiation to the same anatomic site who receive EBRT with any of the following recommended fractionation schemes: 30Gy/10fxns, 24Gy/6fxns, 20Gy/5fxns, and 8Gy/1fxn. The denominator for this measure includes all patients with painful bone metastases and no previous radiation to the same anatomic site who receive EBRT.[86] As noted above, each anatomic site is considered a different case, and as a result it is necessary to determine when EBRT has been administered to different anatomic sites. This determination is not possible without completing a detailed manual review of the patient's record, creating burden and difficulty in determining which sites and instances of EBRT administration are considered cases and should be included in the denominator for the measure. These challenges in determining which cases are included in the denominator for the measure result in difficulty in determining if sample size requirements for the measure are being met.
Further, current information systems do not automatically calculate the total dose provided, so manual review of patient records by practice staff is also required in order to determine the total dose and fractionation scheme, which in turn is used to determine which cases fall into the numerator for this measure. This manual review of patient records is a labor-intensive process that contributes to burden and difficulty in reporting this measure. As a result, we believe that the complexity of reporting this measure places substantial administrative burden on facilities. This also reflects observations made by the measure steward that implementing the measure in the outpatient setting has proven overly burdensome, given that facilities have noted confusion regarding when the administration of EBRT to different numbers and locations of bone metastases are considered separate cases. These issues identifying cases have led to questions about sampling and difficulty determining if sample size requirements are met. Additional burdens associated with this measure have come to our attention, including complicated measure exclusions, sampling concerns, and administrative burden. These challenges cause difficulty in tracking and reporting data for this measure and additional administrative burden, as evidenced by numerous questions about how to report this measure received by CMS and its contractors.
This EBRT measure was also adopted into another CMS quality reporting program, the PPS-Exempt Cancer Hospital Quality Reporting (PCHQR) Program (79 FR 50278 through 50279). That program initially used “radiation planning” CPT codes billable at the physician level, but beginning in March 2016, the PCHQR program updated the measure to enable the use of “radiation delivery” CPT codes.[87] In the FY 2020 IPPS/LTCH PPS final rule (84 FR 42513), we finalized the removal of the measure from the PCHQR Program because the burden associated with the measure outweighs the value of its inclusion in the PCHQR Program. Specifically, the PCHQR Program removed the measure because it is overly burdensome and because the measure steward is no longer maintaining the measure. As such, the PCHQR Program stated it can no longer ensure that the measure is in line with clinical guidelines and standards (84 FR 42513). We note that while the version of the measure using “radiation planning” CPT codes is less burdensome, Hospital Outpatient Departments (HOPDs) do not have access to physician billing data, and so it is not operationally feasible to use “radiation planning” CPT codes (as opposed to the current “radiation delivery” CPT codes) for the EBRT measure in the Hospital OQR Program.
This measure was originally adopted to address the performance gap in EBRT treatment variation, ensure appropriate use of EBRT, and prevent the overuse of radiation therapy. While we still believe that these goals are important, the benefits of this measure have diminished. Stakeholder feedback has shown that this measure is burdensome and difficult to report. Since the measure steward is no longer maintaining this measure,[88] we no longer believe that we can ensure that the measure is in line with clinical guidelines and standards. Thus, considering these circumstances, we believe the costs associated with this measure outweigh the benefit of its continued use in the program (removal Factor 8).
Therefore, in the CY 2020 OPPS/ASC proposed rule (84 FR 39554 through 39556), we proposed to remove the measure beginning with October 2020 encounters used in the CY 2022 payment determination and for subsequent years. We wish to clarify here in this final rule that the measure would be removed beginning with CY 2020 encounters (January 2020) used in the CY 2022 payment determination and for subsequent years rather than beginning in October 2020 as incorrectly noted in the proposed rule. We refer readers to our response to comments below. We considered removing this measure beginning with the CY 2021 payment determination, but we decided to propose to delay removal until the CY 2022 payment determination to be sensitive to facilities' planning and operational procedures given that data collection for this measure began during CY 2019 for the CY 2021 payment determination. We believe that this proposed removal date balances reporting burden while recognizing that HOPDs must use resources to modify information systems and reporting processes to discontinue reporting the measure.
In summary, we proposed to remove OP-33: External Beam Radiotherapy for Bone Metastases (NQF #1822) from the Hospital OQR Program beginning with the CY 2022 payment determination and for subsequent years under removal Factor 8.
We provided a summary of the comments received and our responses to those comments.
Comment: Many commenters supported the proposal to remove EBRT for Bone Metastases (OP-33) from the Hospital OQR Program beginning in CY 2022. Several commenters stated that they support the removal of OP-33 from the Hospital OQR Program for the reasons CMS outlined in the proposed rule. Specifically, several commenters stated that they support the removal of OP-33 from the Hospital OQR Program because the measure is burdensome and because it is no longer being maintained by the measure steward so it may no longer be aligned with clinical guidelines. A few commenters stated that they support the removal of OP-33 to align with the removal of the measure from PCHQR and because the measure is no longer endorsed by the National Quality Forum (NQF).
Response: We thank the commenters for their support to remove EBRT for Bone Metastases (OP-33) from the Hospital OQR Program due to burden and alignment issues. While NQF endorsement is not a requirement for measure inclusion in the Hospital OQR Program, it can be considered when assessing a measure (section 1833(t)(17)(C)(i) of the Act).
Comment: Several commenters requested that CMS clarify the last reporting date for EBRT for Bone Metastases (OP-33) if it is removed and recommended that removal should begin with January 1, 2020 encounters rather than October 2020 encounters. A few commenters requested that the removal of OP-33 begin with the Calendar Year 2021 payment determination rather than the Calendar Year 2022 payment determination due to the significant burden of the reporting requirements. One commenter recommended CMS to remove OP-33 as soon as possible.
Response: Regarding the timeframe for measure removal, in the CY 2020 OPPS/ASC proposed rule (84 FR 39554 through 39556), we proposed to remove OP-33: External Beam Radiotherapy for Bone Metastases (NQF #1822) from the Hospital OQR Program beginning with the CY 2022 payment determination and for subsequent years under removal Factor 8. We chose this timeframe to be sensitive to facilities' planning and operational procedures given that data collection for this measure began during CY 2019 for the CY 2021 payment determination. We realize that in our proposal on pages 84 FR 39554 through 39556, we inadvertently stated that we wished to remove the measure beginning with October 2020 encounters used in the CY 2022 payment determination and for subsequent years. We refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70521 through 70522) where we finalized that beginning with the CY 2017 payment determination, hospitals must report data submitted via a Web-based tool between January 1 and May 15 of the year prior to the payment determination with respect to the encounter period of January 1 to December 31 of 2 years prior to the payment determination year. For the CY 2022 payment determination, the data submission window for this measure would then be January 1, 2021 to May 15, 2021 for the January 1, 2020 through December 31, 2020 encounter period. Thus, as OP-33 is a Web-based measure, its removal from the Hospital OQR Program beginning with the CY 2022 payment determination would also begin with January 1, 2020 encounters rather than October 2020 encounters. So, we are finalizing a modification of what was proposed to correct that we are removing the measure beginning with January 2020 encounters used for the CY 2022 payment determination and for subsequent years. For the OP-33 measure, the final data submission of data collected for CY 2019 encounters will be required by May 15, 2020 for use toward CY 2021 payment determinations; hospitals would not be required to collect data for OP-33 as of January 1, 2020 encounters.
Comment: A few commenters expressed concern about the proposal to remove EBRT for Bone Metastases (OP-33) from the Hospital OQR Program. One commenter stated that the OP-33 measure gives valuable information for monitoring hospital performance improvement. One commenter stated that the OP-33 measure is valuable because it gauges overuse of health services in a setting where overuse exposes people unnecessarily to radiation, putting patients at risk of harm. This commenter stated that though one of the reasons provided for the removal of OP-33 is that it is difficult and burdensome for healthcare providers to report; the commenter recommends that CMS adopt a measurement framework that prioritizes consumer needs over industry preference. The commenter also stated that because the measure steward is no longer maintaining the measure, CMS should either continue to maintain the measure or identify an entity to act as the measure steward to allow the measure to remain in the Hospital OQR Program.
Response: We thank the commenters for these suggestions regarding EBRT for Bone Metastases (OP-33). We agree that ensuring appropriate use of EBRT and preventing the overuse of radiation therapy which were goals of the OP-33 measure are important for safeguarding patients and consumers. We proposed to remove OP-33 under removal Factor 8, the costs associated with a measure outweigh the benefit of its continued use in the program as stakeholder feedback has shown that this measure is burdensome and difficult to report. Regarding measure maintenance, as stated, the measure steward is no longer maintaining this measure and there are issues with the measure as specified. We do not seek to become the steward for this measure as we do not believe that we can maintain this measure in the Hospital OQR Program in a way that ensures that the measure is in line with clinical guidelines and standards and has specifications that are not overly burdensome for which to collect data. Our Meaningful Measures Initiative provides a measurement framework that prioritizes patient and consumer needs while limiting provider burden. Consistent with this framework, we note that the Hospital OQR Program continues to have quality measures that assess appropriate use of radiation (OP-8: MRI Lumbar Spine for Low Back Pain, OP-10: Abdomen CT—Use of Contrast Material, OP-13: Cardiac Imaging for Preoperative Risk Assessment for Non-Cardiac, Low-Risk Surgery, and OP-23: Head CT or MRI Scan Results for Acute Ischemic Stroke or Hemorrhagic Stroke who Received Head CT or MRI Scan Interpretation Within 45 minutes of ED Arrival).
After consideration of the public comments, we are finalizing a modification of what was proposed for the removal of OP-33 from the Hospital OQR Program. Instead of removing the measure beginning with October 2020 encounters as inadvertently stated, we are finalizing removal beginning with January 2020 encounters used in the CY 2022 payment determination and for subsequent years.
4. Summary of Hospital OQR Program Measure Sets for the CY 2022 Payment Determination
We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59099 through 59102) for a summary of the previously finalized Hospital OQR Program measure sets for the CY 2020 and CY 2021 payment determinations and subsequent years.
We did not propose to add any measures; however, we did propose and are finalizing the removal of one measure for the CY 2022 payment determination and subsequent years for the Hospital OQR Program. Table 61 summarizes the finalized Hospital OQR Program measure set for the CY 2022 payment determination and subsequent years (including previously adopted measures and excluding one measure finalized for removal in this final rule).


5. Hospital OQR Program Measures and Topics for Future Consideration
In the CY 2020 OPPS/ASC proposed rule (84 FR 39557), we requested comment on the potential future adoption of four patient safety measures as well as future outcome measures generally.
a. Request for Comment on the Potential Future Adoption of Four Patient Safety Measures
In the CY 2020 OPPS/ASC proposed rule (84 FR 39557) we sought comment on the potential future adoption of four patient safety measures for the Hospital OQR Program that were previously adopted for the ASCQR Program: ASC-1: Patient Burn; ASC-2: Patient Fall; ASC-3: Wrong Site, Wrong Side, Wrong Procedure, Wrong Implant; and ASC-4: All-Cause Hospital Transfer/Admission.[89] We refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74497 through 74499), where we adopted these measures (referred to as NQF #0263, NQF #0266, NQF #0267, and NQF #0265 at the time) in the ASCQR Program. We note that data collection for these measures was suspended in the ASCQR Program due to concerns with their data submission method using quality data codes (QDCs) in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59117 through 59123; 59134 through 59135); however, we refer readers to section XV.B.5. of the CY 2020 OPPS/ASC proposed rule (84 FR 39567), in which the ASCQR Program requested public comment on updating the submission method for these measures in the future. We requested public comment on potentially adding these measures with the updated submission method using a CMS online data submission tool, to the Hospital OQR Program in future rulemaking. These measures are currently specified for the ASC setting. If specified for the hospital outpatient setting, we would seek collaboration with the measure steward.
We believe these measures could be valuable to the Hospital OQR Program because they would allow us to monitor these types of events and prevent their occurrence to ensure that they remain rare, and because they provide critical data to beneficiaries and further transparency for care provided in the outpatient setting that could be useful in choosing a HOPD. In addition, these measures address an important Meaningful Measure Initiative quality priority, Making Care Safer by Reducing Harm Caused in the Delivery of Care.[90] There has been broad stakeholder support for these measures in the ASC setting; stakeholders believe these measures provide important data for facilities and patients because they are serious and the occurrence of these events should be zero (83 FR 59118). A few commenters noted in the CY 2019 OPPS/ASC final rule with comment period that it would be beneficial to also include these ASCQR Program measures in the Hospital OQR Program in order to provide patients with more meaningful data to compare sites of service (83 FR 59119). The future addition of these measures would further align the Hospital OQR and ASCQR Programs, which would benefit patients because these are two outpatient settings that patients may be interested in comparing, especially if they are able to choose in which of these two settings they receive care.
Although NQF endorsement for these ASC measures was removed (in February 2016 for the All-Cause Hospital Transfer/Admission measure; [91] in May 2016 for the Patient Burn [92] and the Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant [93] measures; and in June 2018 for the Patient Fall measure [94] ), as one commenter pointed out in the CY 2019 OPPS/ASC final rule with comment period, the NQF endorsement of the ASC measures was removed as endorsement was allowed to lapse by the measure steward, not because they failed the endorsement maintenance process (83 FR 59119). If specified for the HOPD setting, we plan to coordinate with the measure steward to seek NQF endorsement for those measures. These measures are discussed in more detail below.
(1) Patient Burn
The ASCQR Patient Burn measure assesses the percentage of admissions experiencing a burn prior to discharge. The numerator for this measure is defined as ASC admissions experiencing a burn prior to discharge and the denominator is defined as all ASC admissions.[95] We believe this measure, if specified for the hospital outpatient setting, would allow HOPDs, Medicare beneficiaries, and other stakeholders to develop a better understanding of the incidence of these events. In the CY 2012 OPPS/ASC final rule with comment period (76 FR 74497 through 74498), we adopted this measure for the ASCQR Program because ASCs serve surgical patients who may face the risk of burns during ambulatory surgical procedures and we believe monitoring patient burns is valuable to patients and other stakeholders. HOPDs also serve surgical patients who may face the risk of burns during outpatient procedures, so we believe this measure would be valuable for the HOPD setting. Further, we have reviewed studies demonstrating the high impact of monitoring patient burns because patient burns are serious reportable events in healthcare [96] and because patient burns are preventable.[97 98]
(2) Patient Fall
The ASCQR Program Patient Fall measure assesses the percentage of admissions experiencing a fall. The numerator for this measure is defined as ASC admissions experiencing a fall within the confines of the ASC and excludes ASC admissions experiencing a fall outside the ASC. The denominator is defined as all ASC admissions and excludes ASC admissions experiencing a fall outside the ASC.[99] We believe this measure, if specified for the hospital outpatient setting, would enable HOPDs to take steps to reduce the risk of falls. In the CY 2012 OPPS/ASC final rule with comment period (76 FR 74498), we adopted this measure for the ASCQR Program because falls, particularly in the elderly, can cause injury and loss of functional status; because the use of anxiolytics, sedatives, and anesthetic agents may put patients undergoing outpatient surgery at increased risk for falls; and because falls in healthcare settings can be prevented through the assessment of risk, care planning, and patient monitoring. These same risks for patient falls are a concern in the HOPD setting. Further, we have reviewed studies demonstrating the high impact of monitoring patient burns because patient falls are serious reportable events in healthcare [100] and because patient falls are preventable.[101]
(3) Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant
The ASCQR Program Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant measure assesses the percentage of admissions experiencing a wrong site, wrong side, wrong patient, wrong procedure, or wrong implant. The numerator for this measure is defined as ASC admissions experiencing a wrong site, a wrong side, a wrong patient, a wrong procedure, or a wrong implant, and the denominator is defined as all ASC admissions.[102] We believe this measure, if specified for the hospital outpatient setting, would provide important HOPD information about surgeries and procedures performed on the wrong site/side, and wrong patient. In the CY 2012 OPPS/ASC final rule with comment period (76 FR 74498 through 74499), we adopted this measure for the ASCQR Program because surgeries and procedures performed on the wrong site/side, and wrong patient can result in significant impact on patients, including complications, serious disability or death. We also stated that while the prevalence of such serious errors may be rare, such events are considered serious reportable events. These same significant impacts on patients apply for the HOPD setting. Further, we have reviewed studies demonstrating the high impact of monitoring wrong site, wrong side, wrong patient, wrong procedure, wrong implant procedures and surgeries because these types of errors are serious reportable events in healthcare [103] and because these errors are preventable.[104]
(4) All-Cause Hospital Transfer/Admission
The All-Cause Hospital Transfer/Admission measure assesses the rate of admissions requiring a hospital transfer or hospital admission upon discharge. The numerator for this measure is defined as ASC admissions requiring a hospital transfer or hospital admission upon discharge from the ASC and the denominator is defined as all ASC admissions.[105] We believe this measure, if specified for the hospital outpatient setting, would be valuable for HOPDs. In the CY 2012 OPPS/ASC final rule with comment period (76 FR 74499), we adopted this measure for ASCs because the transfer or admission of a surgical patient from an outpatient setting to an acute care setting can be an indication of a complication, serious medical error, or other unplanned negative patient outcome. We also stated that while acute intervention may be necessary in these circumstances, a high rate of such incidents may indicate suboptimal practices or patient selection criteria. These same potential negative patient outcomes apply to the HOPD setting. Further, we have reviewed studies demonstrating the high impact of monitoring patient transfers and admissions because facilities can take steps to prevent and reduce these types of events.[106 107]
We have provided a summary of the comments received and our responses to those comments.
Comment: Many commenters were supportive of the potential future specification of ASC-1, ASC-2, ASC-3, and ASC-4 for the hospital outpatient setting and the potential future addition of these measures to the Hospital OQR Program. Several commenters stated that these four measures should be adopted in the Hospital OQR Program in order to align with the ASCQR Program and to provide meaningful data for patients to compare performance in ASCs and HOPDs. A few commenters stated that these four patient safety measures should be adopted in the Hospital OQR Program because they focus on areas of critical importance. A few commenters supported the plan for CMS to work with the measure developer to improve the data submission methods and to ensure the measures are appropriately specified for the hospital outpatient setting. A few commenters recommended expedited development and implementation of these measures in the hospital outpatient setting.
Response: We thank the commenters for their support for the potential future specification of ASC-1, ASC-2, ASC-3, and ASC-4 for the hospital outpatient setting and the potential future addition of these measures to the Hospital OQR Program.
Comment: Many commenters provided recommendations regarding potentially specifying ASC-1, ASC-2, ASC-3, and ASC-4 for the hospital outpatient setting and potentially adding these measures to the Hospital OQR Program in the future. Several commenters stated that decisions made by the NQF about these measures should be considered and prioritized by CMS. Several commenters suggested that these measures should be specified for the HOPD setting, field tested, reliability tested, and reviewed by the Measure Applications Partnership (MAP) before inclusion in the Hospital OQR Program. Several commenters suggested that, with respect to ASC-4, CMS should consider overlap with OP-36 Hospital Visits after Hospital Outpatient Surgery and should assess the need for clinical risk adjustment in the HOPD setting. A few commenters provided recommendations about potential data submission methods for these measures in the Hospital OQR Program, with some specifically supporting the use of an online data submission tool such as QualityNet. However, several commenters did not support using the QualityNet online tool (or a similar online tool) for submission, and one commenter suggested that if a manual abstraction process is required, hospitals should be provided ample time to test and implement the measures. One commenter recommended that CMS work with HOPDs and ASCs to identify current forums where these safety issues are documented, discussed, and remedied. One commenter recommended that these measures should apply to all adult patients, not just Medicare fee-for-service patients.
Response: We thank the commenters for their recommendations regarding potentially specifying ASC-1, ASC-2, ASC-3, and ASC-4 for the hospital outpatient setting, interface with existing ASCQR Program measures, data submission methods, risk adjustment issues, and potentially adding these measures to the Hospital OQR Program in the future. We note that as currently specified, these measures apply to all patients and they are not limited to fee-for-service Medicare patients.[108]
Comment: Many commenters expressed concern to the potential future specification of ASC-1, ASC-2, ASC-3, and ASC-4 for the hospital outpatient setting and the potential future addition of these measures to the Hospital OQR Program. Several expressed concern that the measures are not endorsed by the National Quality Forum. A few commenters stated that they believe because these measures were designed specifically for ASCs, they would not be appropriate for use in the hospital outpatient setting. Several commenters expressed concern about adding these measures to the Hospital OQR Program because the events of interest are already rare, and a few pointed out that hospitals are already required to implement policies and processes to mitigate the risk of these events and several states have mandatory reporting of these types of events. A few commenters stated concerns about the burden that would be created if these measures are added to the Hospital OQR Program. One commenter stated that because these events are rare in the outpatient setting, the data is at risk of becoming identifiable if disclosed and publicly reported. One commenter stated that adding these measures to the Hospital OQR Program would not contribute to the CMS Meaningful Measurement goal.
Response: We thank the commenters for their recommendations and raising these important concerns regarding the use of the ASC-1 through ASC-4 measures for the Hospital OQR Program. We will take these suggestions into consideration as we consider adding these measures to the Hospital OQR Program in the future.
b. Future Outcome Measures
In the CY 2020 OPPS/ASC proposed rule (84 FR 39558), we also requested public comment on future measure topics for the Hospital OQR Program. Specifically, we requested public comment on any outcome measures that would be useful to add as well as feedback on any process measures that should be eliminated from the Hospital OQR Program to further our goal of developing a comprehensive set of quality measures for informed decision-making and quality improvement in HOPDs. We are moving towards greater use of outcome measures and away from use of clinical process measures across our Medicare quality reporting programs to better assess the results of care. The current measure set for the Hospital OQR Program includes measures that assess process of care, imaging efficiency patterns, care transitions, (Emergency Department) ED throughput efficiency, Health Information Technology (health IT) use, care coordination, and patient safety. Measures are of various types, including those of process, structure, outcome, and efficiency. Through future rulemaking, we intend to propose new measures that support our goal of achieving better health care and improved health for Medicare beneficiaries who receive health care in the HOPD setting, while aligning quality measures across the Medicare program to the extent possible.
Comment: A few commenters recommended that CMS add more measures to the Hospital OQR Program that would align with the ASCQR Program. One commenter suggested that CMS incorporate patient experience, safety and reliability, clinical quality, and provider engagement measures in the Hospital OQR Program. One commenter recommended that CMS include the Adult Immunization Status measure in the Hospital OQR Program.
Response: We thank the commenters for these recommendations for additional measures for the Hospital OQR Program. We agree that alignment with the ASCQR Program is an important consideration; to that end, as discussed in section XIV.B.a of this final rule with comment period, we requested comment on the use of the ASCQR Program's ASC-1 through ASC-4 measures for the Hospital OQR Program.
We thank the commenters for their responses and will take these suggestions into consideration as we develop future Hospital OQR Program measures and topics.
6. Maintenance of Technical Specifications for Quality Measures
CMS maintains technical specifications for previously adopted Hospital OQR Program measures. These specifications are updated as we modify the Hospital OQR Program measure set. The manuals that contain specifications for the previously adopted measures can be found on the QualityNet website at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1196289981244. We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59104 through 59105), where we changed the frequency of the Hospital OQR Program Specifications Manual release beginning with CY 2019 and for subsequent years, such that we will release a manual once every 12 months and release addenda as necessary. We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39558).
7. Public Display of Quality Measures
We refer readers to the CY 2014 and CY 2017 OPPS/ASC final rules with comment period (78 FR 75092 and 81 FR 79791 respectively) for our previously finalized policies regarding public display of quality measures. In the CY 2020 OPPS/ASC proposed rule (84 FR 39558), we did not propose any changes to our previously finalized public display policies.
C. Administrative Requirements
1. QualityNet Account and Security Administrator
The previously finalized QualityNet security administrator requirements, including setting up a QualityNet account and the associated timelines, are described in the CY 2014 OPPS/ASC final rule with comment period (78 FR 75108 through 75109). We codified these procedural requirements at 42 CFR 419.46(a) in that final rule with comment period. We did not propose any changes to our requirements for the QualityNet account and security administrator in the CY 2020 OPPS/ASC proposed rule (84 FR 39559).
2. Requirements Regarding Participation Status
We refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75108 through 75109), the CY 2016 OPPS/ASC final rule with comment period (80 FR 70519) and the CY 2019 OPPS/ASC final rule with comment period (83 FR 59103 through 59104) for requirements for participation and withdrawal from the Hospital OQR Program. We codified these procedural requirements regarding participation status at 42 CFR 419.46(a) and (b). We did not propose any changes to our participation status policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39559).
D. Form, Manner, and Timing of Data Submitted for the Hospital OQR Program
1. Hospital OQR Program Annual Payment Determinations
In the CY 2014 OPPS/ASC final rule with comment period (78 FR 75110 through 75111) and the CY 2016 OPPS/ASC final rule with comment period (80 FR 70519 through 70520), we specified our data submission deadlines. We codified these submission requirements at 42 CFR 419.46(c).
We refer readers to the CY 2016 OPPS/ASC final rule with comment period (80 FR 70519 through 70520), where we finalized our proposal to shift the quarters upon which the Hospital OQR Program payment determinations are based beginning with the CY 2018 payment determination. The deadlines for the CY 2022 payment determination and subsequent years are illustrated in Table 62.

In the CY 2018 OPPS/ASC final rule with comment period, we finalized a policy to align the initial data submission timeline for all hospitals that did not participate in the previous year's Hospital OQR Program and made conforming revisions at 42 CFR 419.46(c)(3). We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39559).
2. Requirements for Chart-Abstracted Measures Where Patient-Level Data Are Submitted Directly to CMS for the CY 2022 Payment Determination and Subsequent Years
We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68481 through 68484) for a discussion of the form, manner, and timing for data submission requirements of chart-abstracted measures for the CY 2014 payment determination and subsequent years. We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39559).
The following previously finalized Hospital OQR Program chart-abstracted measures will require patient-level data to be submitted for the CY 2022 payment determination and subsequent years:
- OP-2: Fibrinolytic Therapy Received Within 30 Minutes of ED Arrival (NQF #0288);
- OP-3: Median Time to Transfer to Another Facility for Acute Coronary Intervention (NQF #0290);
- OP-18: Median Time from ED Arrival to ED Departure for Discharged ED Patients (NQF #0496); and
- OP-23: Head CT Scan Results for Acute Ischemic Stroke or Hemorrhagic Stroke Patients who Received Head CT Scan Interpretation Within 45 Minutes of ED Arrival (NQF #0661).
3. Claims-Based Measure Data Requirements for the CY 2022 Payment Determination and Subsequent Years
Currently, the following previously finalized Hospital OQR Program claims-based measures are required for the CY 2022 payment determination and subsequent years:
- OP-8: MRI Lumbar Spine for Low Back Pain (NQF #0514);
- OP-10: Abdomen CT—Use of Contrast Material;
- OP-13: Cardiac Imaging for Preoperative Risk Assessment for Non-Cardiac, Low Risk Surgery (NQF #0669);
- OP-32: Facility 7-Day Risk-Standardized Hospital Visit Rate after Outpatient Colonoscopy (NQF #2539);
- OP-35: Admissions and Emergency Department Visits for Patients Receiving Outpatient Chemotherapy; and
- OP-36: Hospital Visits after Hospital Outpatient Surgery (NQF #2687).
We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59106 through 59107), where we established a 3-year reporting period for OP-32: Facility 7-Day Risk-Standardized Hospital Visit Rate after Outpatient Colonoscopy beginning with the CY 2020 payment determination and for subsequent years. In that final rule with comment period (83 FR 59136 through 59138), we established a similar policy under the ASCQR Program. We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39559).
4. Data Submission Requirements for the OP-37a-e: Outpatient and Ambulatory Surgery Consumer Assessment of Healthcare Providers and Systems (OAS CAHPS) Survey-Based Measures for the CY 2022 Payment Determination and Subsequent Years
We refer readers to the CY 2017 OPPS/ASC final rule with comment period (81 FR 79792 through 79794) for a discussion of the previously finalized requirements related to survey administration and vendors for the OAS CAHPS Survey-based measures. In addition, we refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59432 through 59433), where we finalized a policy to delay implementation of the OP-37a-e OAS CAHPS Survey-based measures beginning with the CY 2020 payment determination (2018 reporting period) until further action in future rulemaking. In the CY 2020 OPPS/ASC proposed rule (84 FR 39560), we did not propose any changes to the previously finalized requirements related to survey administration and vendors for the OAS CAHPS Survey-based measures.
5. Data Submission Requirements for Measures for Data Submitted Via a Web-Based Tool for the CY 2022 Payment Determination and Subsequent Years
We refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75112 through 75115) and the CY 2016 OPPS/ASC final rule with comment period (80 FR 70521) and the CMS QualityNet website (https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1205442125082) for a discussion of the requirements for measure data submitted via the CMS QualityNet website for the CY 2017 payment determination and subsequent years. In addition, we refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75097 through 75100) for a discussion of the requirements for measure data submitted via the CDC NHSN website. In the CY 2020 OPPS/ASC proposed rule (84 FR 39560), we did not propose any changes to our policies regarding the submission of measure data submitted via a web-based tool. However, as discussed in section XIV.B.3.b. of this final rule, we are finalizing our proposal with modification to remove OP-33: EBRT for Bone Metastases beginning with the CY 2022 payment determination and for subsequent years; so the following previously finalized quality measures will require data to be submitted via a web-based tool for the CY 2022 payment determination and subsequent years with the exception of OP-31: Cataracts: Improvement in Patient's Visual Function within 90 Days Following Cataract Surgery (NQF #1536): for which data submission remains voluntary:
- OP-22: Left Without Being Seen (NQF #0499) (via CMS' QualityNet website);
- OP-29: Endoscopy/Polyp Surveillance: Appropriate Follow-up Interval for Normal Colonoscopy in Average Risk Patients (NQF #0658) (via CMS' QualityNet website); and
- OP-31: Cataracts: Improvement in Patient's Visual Function within 90 Days Following Cataract Surgery (NQF #1536) (via CMS' QualityNet website).
6. Population and Sampling Data Requirements for the CY 2021 Payment Determination and Subsequent Years
We refer readers to the CY 2011 OPPS/ASC final rule with comment period (75 FR 72100 through 72103) and the CY 2012 OPPS/ASC final rule with comment period (76 FR 74482 through 74483) for discussions of our population and sampling requirements. We did not propose any changes to our population and sampling requirements for chart-abstracted measures in the CY 2020 OPPS/ASC proposed rule (84 FR 39560).
7. Hospital OQR Program Validation Requirements
We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68484 through 68487), the CY 2015 OPPS/ASC final rule with comment period (79 FR 66964 through 66965), the CY 2016 OPPS/ASC final rule with comment period (80 FR 70524), and the CY 2018 OPPS/ASC final rule with comment period (82 FR 59441 through 59443), and 42 CFR 419.46(e) for our policies regarding validation. We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39560).
8. Extraordinary Circumstances Exception (ECE) Process for the CY 2021 Payment Determination and Subsequent Years
We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68489), the CY 2014 OPPS/ASC final rule with comment period (78 FR 75119 through 75120), the CY 2015 OPPS/ASC final rule with comment period (79 FR 66966), the CY 2016 OPPS/ASC final rule with comment period (80 FR 70524), the CY 2017 OPPS/ASC final rule with comment period (81 FR 79795), the CY 2018 OPPS/ASC final rule with comment period (82 FR 59444), and 42 CFR 419.46(d) for a complete discussion of our extraordinary circumstances exception (ECE) process under the Hospital OQR Program. We did not propose any changes to our ECE policy in the CY 2020 OPPS/ASC proposed rule (84 FR 39560).
9. Hospital OQR Program Reconsideration and Appeals Procedures for the CY 2021 Payment Determination and Subsequent Years
We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68487 through 68489), the CY 2014 OPPS/ASC final rule with comment period (78 FR 75118 through 75119), the CY 2016 OPPS/ASC final rule with comment period (80 FR 70524), the CY 2017 OPPS/ASC final rule with comment period (81 FR 79795), and 42 CFR 419.46(f) for our reconsideration and appeals procedures. We did not propose any changes to our reconsideration and appeals procedures in the CY 2020 OPPS/ASC proposed rule (84 FR 39560).
E. Payment Reduction for Hospitals That Fail To Meet the Hospital OQR Program Requirements for the CY 2020 Payment Determination
1. Background
Section 1833(t)(17) of the Act, which applies to subsection (d) hospitals (as defined under section 1886(d)(1)(B) of the Act), states that hospitals that fail to report data required to be submitted on measures selected by the Secretary, in the form and manner, and at a time, specified by the Secretary will incur a 2.0 percentage point reduction to their Outpatient Department (OPD) fee schedule increase factor; that is, the annual payment update factor. Section 1833(t)(17)(A)(ii) of the Act specifies that any reduction applies only to the payment year involved and will not be taken into account in computing the applicable OPD fee schedule increase factor for a subsequent year.
The application of a reduced OPD fee schedule increase factor results in reduced national unadjusted payment rates that apply to certain outpatient items and services provided by hospitals that are required to report outpatient quality data in order to receive the full payment update factor and that fail to meet the Hospital OQR Program requirements. Hospitals that meet the reporting requirements receive the full OPPS payment update without the reduction. For a more detailed discussion of how this payment reduction was initially implemented, we refer readers to the CY 2009 OPPS/ASC final rule with comment period (73 FR 68769 through 68772).
The national unadjusted payment rates for many services paid under the OPPS equal the product of the OPPS conversion factor and the scaled relative payment weight for the APC to which the service is assigned. The OPPS conversion factor, which is updated annually by the OPD fee schedule increase factor, is used to calculate the OPPS payment rate for services with the following status indicators (listed in Addendum B to the proposed rule, which is available via the internet on the CMS website): “J1”, “J2”, “P”, “Q1”, “Q2”, “Q3”, “R”, “S”, “T”, “V”, or “U”. In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79796), we clarified that the reporting ratio does not apply to codes with status indicator “Q4” because services and procedures coded with status indicator “Q4” are either packaged or paid through the Clinical Laboratory Fee Schedule and are never paid separately through the OPPS. Payment for all services assigned to these status indicators will be subject to the reduction of the national unadjusted payment rates for hospitals that fail to meet Hospital OQR Program requirements, with the exception of services assigned to New Technology APCs with assigned status indicator “S” or “`T”. We refer readers to the CY 2009 OPPS/ASC final rule with comment period (73 FR 68770 through 68771) for a discussion of this policy.
The OPD fee schedule increase factor is an input into the OPPS conversion factor, which is used to calculate OPPS payment rates. To reduce the OPD fee schedule increase factor for hospitals that fail to meet reporting requirements, we calculate two conversion factors—a full market basket conversion factor (that is, the full conversion factor), and a reduced market basket conversion factor (that is, the reduced conversion factor). We then calculate a reduction ratio by dividing the reduced conversion factor by the full conversion factor. We refer to this reduction ratio as the “reporting ratio” to indicate that it applies to payment for hospitals that fail to meet their reporting requirements. Applying this reporting ratio to the OPPS payment amounts results in reduced national unadjusted payment rates that are mathematically equivalent to the reduced national unadjusted payment rates that would result if we multiplied the scaled OPPS relative payment weights by the reduced conversion factor. For example, to determine the reduced national unadjusted payment rates that applied to hospitals that failed to meet their quality reporting requirements for the CY 2010 OPPS, we multiplied the final full national unadjusted payment rate found in Addendum B of the CY 2010 OPPS/ASC final rule with comment period by the CY 2010 OPPS final reporting ratio of 0.980 (74 FR 60642).
In the CY 2009 OPPS/ASC final rule with comment period (73 FR 68771 through 68772), we established a policy that the Medicare beneficiary's minimum unadjusted copayment and national unadjusted copayment for a service to which a reduced national unadjusted payment rate applies would each equal the product of the reporting ratio and the national unadjusted copayment or the minimum unadjusted copayment, as applicable, for the service. Under this policy, we apply the reporting ratio to both the minimum unadjusted copayment and national unadjusted copayment for services provided by hospitals that receive the payment reduction for failure to meet the Hospital OQR Program reporting requirements. This application of the reporting ratio to the national unadjusted and minimum unadjusted copayments is calculated according to § 419.41 of our regulations, prior to any adjustment for a hospital's failure to meet the quality reporting standards according to § 419.43(h). Beneficiaries and secondary payers thereby share in the reduction of payments to these hospitals.
In the CY 2009 OPPS/ASC final rule with comment period (73 FR 68772), we established the policy that all other applicable adjustments to the OPPS national unadjusted payment rates apply when the OPD fee schedule increase factor is reduced for hospitals that fail to meet the requirements of the Hospital OQR Program. For example, the following standard adjustments apply to the reduced national unadjusted payment rates: The wage index adjustment; the multiple procedure adjustment; the interrupted procedure adjustment; the rural sole community hospital adjustment; and the adjustment for devices furnished with full or partial credit or without cost. Similarly, OPPS outlier payments made for high cost and complex procedures will continue to be made when outlier criteria are met. For hospitals that fail to meet the quality data reporting requirements, the hospitals' costs are compared to the reduced payments for purposes of outlier eligibility and payment calculation. We established this policy in the OPPS beginning in the CY 2010 OPPS/ASC final rule with comment period (74 FR 60642). For a complete discussion of the OPPS outlier calculation and eligibility criteria, we refer readers to section II.G. of the proposed rule.
2. Reporting Ratio Application and Associated Adjustment Policy for CY 2020
We proposed to continue our established policy of applying the reduction of the OPD fee schedule increase factor through the use of a reporting ratio for those hospitals that fail to meet the Hospital OQR Program requirements for the full CY 2020 annual payment update factor. For the CY 2020 OPPS/ASC proposed rule (84 FR 39560), the proposed reporting ratio was 0.980, which when multiplied by the proposed full conversion factor of $81.398 equaled a proposed conversion factor for hospitals that fail to meet the requirements of the Hospital OQR Program (that is, the reduced conversion factor) of $79.770. We proposed to continue to apply the reporting ratio to all services calculated using the OPPS conversion factor. For the CY 2020 OPPS/ASC proposed rule (84 FR 39560), we proposed to apply the reporting ratio, when applicable, to all HCPCS codes to which we have proposed status indicator assignments of “J1”, “J2”, “P”, “Q1”, “Q2”, “Q3”, “R”, “S”, “T”, “V”, and “U” (other than new technology APCs to which we have proposed status indicator assignment of “S” and “T”). We proposed to continue to exclude services paid under New Technology APCs. We proposed to continue to apply the reporting ratio to the national unadjusted payment rates and the minimum unadjusted and national unadjusted copayment rates of all applicable services for those hospitals that fail to meet the Hospital OQR Program reporting requirements. We also proposed to continue to apply all other applicable standard adjustments to the OPPS national unadjusted payment rates for hospitals that fail to meet the requirements of the Hospital OQR Program. Similarly, we proposed to continue to calculate OPPS outlier eligibility and outlier payment based on the reduced payment rates for those hospitals that fail to meet the reporting requirements.
For the CY 2020 OPPS/ASC final rule, the final reporting ratio is 0.981, which when multiplied by the final full conversion factor of 80.784 equals a final conversion factor for hospitals that fail to meet the requirements of the Hospital OQR Program (that is, the reduced conversion factor) of 79.250. We also are finalizing the remainder of our proposals regarding the payment reduction for hospitals that fail to meet the Hospital OQR Program requirements for CY 2019 payment.
XV. Requirements for the Ambulatory Surgical Center Quality Reporting (ASCQR) Program
A. Background
1. Overview
We refer readers to section XIV.A.1. of this final rule with comment period for a general overview of our quality reporting programs and to the CY 2019 OPPS/ASC final rule with comment period (83 FR 58820 through 58822) where we discuss our Meaningful Measures Initiative and our approach in evaluating quality program measures.
2. Statutory History of the ASCQR Program
We refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74492 through 74494) for a detailed discussion of the statutory history of the ASCQR Program.
3. Regulatory History of the ASCQR Program
We seek to promote higher quality and more efficient health care for beneficiaries. This effort is supported by the adoption of widely accepted quality of care measures. We have collaborated with relevant stakeholders to define such measures in most healthcare settings and currently measure some aspect of care for almost all settings of care available to Medicare beneficiaries. These measures assess structural aspects of care, clinical processes, patient experiences with care, and clinical outcomes. We have implemented quality measure reporting programs for multiple healthcare settings. To measure the quality of ASC services and to make such information publicly available, we implemented the ASCQR Program. We refer readers to the CYs 2014 through 2019 OPPS/ASC final rules with comment period (78 FR 75122; 79 FR 66966 through 66987; 80 FR 70526 through 70538; 81 FR 79797 through 79826; 82 FR 59445 through 59476; and 83 FR 59110 through 59139, respectively) for an overview of the regulatory history of the ASCQR Program. We have codified certain requirements under the ASCQR Program at 42 CFR, part 16, subpart H (42 CFR 416.300 through 416.330).
B. ASCQR Program Quality Measures
1. Considerations in the Selection of ASCQR Program Quality Measures
We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68493 through 68494) for a detailed discussion of the priorities we consider for ASCQR Program quality measure selection. We did not propose any changes to these policies in the CY 2020 OPPS/ASC proposed rule (84 FR 39562).
2. Policies for Retention and Removal of Quality Measures From the ASCQR Program
a. Retention of Previously Adopted ASCQR Program Measures
We previously finalized a policy that quality measures adopted for an ASCQR Program measure set for a previous payment determination year be retained in the ASCQR Program for measure sets for subsequent payment determination years, except when they are removed, suspended, or replaced as indicated (76 FR 74494 and 74504; 77 FR 68494 through 68495; 78 FR 75122; and 79 FR 66967 through 66969). We did not propose any changes to this policy in the CY 2020 OPPS/ASC proposed rule (83 FR 39562).
b. Removal Factors for ASCQR Program Measures
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59111 through 59115), we clarified, finalized and codified at 42 CFR 416.320 an updated set of factors [109] and the process for removing measures from the ASCQR Program. The factors are:
- Factor 1. Measure performance among ASCs is so high and unvarying that meaningful distinctions and improvements in performance can no longer be made (“topped-out” measures).
- Factor 2. Performance or improvement on a measure does not result in better patient outcomes.
- Factor 3. A measure does not align with current clinical guidelines or practice.
- Factor 4. The availability of a more broadly applicable (across settings, populations, or conditions) measure for the topic.
- Factor 5. The availability of a measure that is more proximal in time to desired patient outcomes for the particular topic.
- Factor 6. The availability of a measure that is more strongly associated with desired patient outcomes for the particular topic.
- Factor 7. Collection or public reporting of a measure leads to negative unintended consequences other than patient harm.
- Factor 8. The costs associated with a measure outweigh the benefit of its continued use in the program.
We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59111 through 59115) for a detailed discussion of our process regarding measure removal.
3. Proposal to Adopt ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357) for the ASCQR Program Measure Set
In the CY 2020 OPPS/ASC proposed rule (84 FR 39562 through 39567), we proposed one new quality measure for the ASCQR Program for the CY 2024 payment determination and subsequent years; ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357).
a. Background
Ambulatory surgery in the outpatient setting is common in the United States. Nearly 70 percent of all surgeries in the United States are performed in an outpatient setting with an expanding number and variety of procedures being performed at stand-alone ASCs.[110 111] General surgery procedures are commonly performed at ASCs. Based on an analysis of Medicare fee-for-service (FFS) claims for patients aged 65 years and older, from January 1, 2015 through December 31, 2015, 3,251 ASCs performed 149,468 general surgery procedures. These procedures include abdominal, alimentary tract, breast, skin/soft tissue, wound, and varicose vein stripping procedures. Of the 3,251 ASCs that performed general surgery procedures, 1,157 (35.5 percent) performed at least 25 such procedures during this time period. Because of the large number of general surgery procedures that occur in the ambulatory setting, we believe that adopting ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers in the ASCQR Program will provide beneficiaries with transparent quality data that can be utilized in choosing healthcare facilities.
While ambulatory surgery is considered low risk for complications, there are well-described and potentially preventable adverse events that can occur after ambulatory surgery leading to unplanned care at a hospital, such as emergency department (ED) visits, observation stays, or hospital admissions. These events include uncontrolled pain, urinary retention, infection, bleeding, and venous thromboembolism.[112 113]
Hospital visits following same-day surgery are an important and broadly accepted patient-centered outcome reported in the literature.[114 115 116 117 118 119 120 121] National estimates of hospital visit rates following outpatient surgery vary from 0.5 to 9.0 percent, based on the type of surgery, outcome measured (admissions alone or admissions and ED visits), and length of time between the surgery and the hospital visit.[122 123 124 125 126 127 128 129 130] The frequency of such events also varies among ASCs, suggesting variation in quality of pre-surgical assessment, surgical care, post-surgical care, and the care and support provided to patients post-discharge.[131 132 133 134 135 136 137 138]
We calculated the national unadjusted rate of hospital visits (ED visits, observation stays, or hospital admissions) following any general surgery procedure at an ASC. In a Medicare FFS dataset of claims for services during CY 2015 (January 1, 2015-December 31, 2015), the distribution of unadjusted outcome rates was skewed, suggesting variation in quality of care. Among 1,153 ASCs with at least 25 qualifying general surgery cases in the Medicare FFS CY 2015 dataset, the unadjusted rate of unplanned hospital visits ranged from 0.0 percent to 13.2 percent. These results suggest opportunity for ASCs to improve the quality of care for patients seeking general surgery procedures.
ASCs may be unaware of patients' subsequent unplanned hospital visits given that patients tend to present to the ED or to hospitals unaffiliated with the ASC. In addition, information on the rate of patients' subsequent unplanned hospital visits would provide transparent data to beneficiaries that could be utilized when choosing ambulatory surgery sites of care. Quality measurement of the number of unplanned hospital visits following general surgery procedures performed at ASCs, coupled with transparency through public reporting would make these outcomes more visible to both ASCs and beneficiaries. Therefore, we expect that this would encourage ASCs to incorporate quality improvement activities to reduce the number of unplanned hospital visits and track quality improvement over time.
Therefore, in the CY 2020 OPPS/ASC proposed rule (84 FR 39562 through 39567), we proposed to adopt ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357) (hereafter referred to as the proposed ASC-19 measure) into the ASCQR Program for the CY 2024 payment determination and subsequent years.
The proposed ASC-19 measure was developed in conjunction with two other measures adopted for the ASCQR Program beginning with the CY 2022 payment determination as finalized in the CY 2018 OPPS/ASC final rule with comment period: ASC-17: Hospital Visits After Orthopedic Ambulatory Surgical Center Procedures (82 FR 59455) and ASC-18: Hospital Visits After Urology Ambulatory Surgical Center Procedures (82 FR 59463). All three measures assess the same patient outcome for care provided in the ASC setting and use the same risk-adjustment methodology. These three measures differ in surgical procedures considered (orthopedic, urological, or general surgery), specific risk variables included, and reporting of the outcome, unplanned hospital visits. The proposed ASC-19 measure reports the outcome as a risk-standardized ratio because the diverse mix of procedures included in the proposed ASC-19 measure can have varying levels of risk of unplanned hospital visits; while the ASC-17 and ASC-18 measures report a risk-standardized rate that reflects clinically specific cohorts with fairly comparable mixes of procedures. We refer readers to section XV.B.3.d. of this final rule with comment period for a full discussion on the measure outcome calculation.
b. Overview of Measure
The proposed ASC-19 measure is a risk-adjusted outcome measure of acute, unplanned hospital visits within 7 days of a general surgery procedure performed at an ASC among Medicare FFS patients aged 65 years and older. We define an unplanned hospital visit as including an ED visit, observation stay, or unplanned inpatient admission. The measure aligns with the Admissions and Readmissions to Hospitals and Preventable Healthcare Harm Meaningful Measure areas of our Meaningful Measures Initiative.[139] This measure was developed with input from a national Technical Expert Panel (TEP) consisting of patients, surgeons, methodologists, researchers, and providers. We also held a three-week public comment period soliciting stakeholder input on the measure methodology, and publicly posted a summary of the comments received as well as our responses (available in the Downloads section at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/PC-Updates-on-Previous-Comment-Periods.html).
During the measure development public comment period, we received public comment recommending the removal of two specific procedures (CPT 29893 endoscopic plantar and CPT 69222 clean out mastoid cavity) deemed outside the scope of general surgery and to review the cohort procedure list with general surgeons to ensure appropriateness. In response to this feedback, we reviewed the cohort of procedures incorporating feedback from general surgeons and removed 15 individual skin/soft tissue and wound procedure codes from the measure that are outside the scope of general surgery practice. These procedures include those specifically suggested for removal (that is, endoscopic plantar and clean out mastoid cavity) as well as chemical peels, dermabrasions, and nerve procedures.
Section 1890A of the Act requires the Secretary to establish a pre-rulemaking process with respect to the selection of certain categories of quality and efficiency measures. Under section 1890A(a)(2) of the Act, the Secretary must make available to the public by December 1 of each year a list of quality and efficiency measures that the Secretary is considering. The ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers measure was included on a publicly available document entitled “List of Measures under Consideration for December 1, 2017.” [140] The Measures Applications Partnership (MAP) reviewed this measure (MUC17-233) and provided conditional support for rulemaking, pending NQF review and endorsement, with the recognition that this measure assesses an important outcome for patients receiving care at ASCs.[141] The MAP had some concerns about the attribution model of the measure, noting that hospital visits after ASC procedures are relatively rare events and could disproportionately affect low-income or rural ASCs and that the measure may need risk adjustment for social risk factors. At the time of the MAP's review, this measure was still undergoing field testing.
Since the MAP's conditional support,[142] we completed testing for the proposed ASC-19 measure by estimating risk-standardized scores using two full years of Medicare FFS claims data (CYs 2014 and 2015) containing 286,999 procedures. The results showed score variation across ASCs, from a minimum risk-standardized ratio of 0.42 to a maximum of 2.13; the median was 0.97 and the 25th and 75th percentiles were 0.90 and 1.10, respectively. After adjusting for case and procedure mixes of ASCs, these results suggest there are underlying differences in the quality of care and opportunities for quality improvement. The reliability testing found an intraclass correlation coefficient (ICC) score of 0.530, indicating moderate measure score reliability.[143] We considered the face validity of the measure score among TEP members. Among the 14 TEP members, 12 agreed that the measure scores are valid and useful measures of ASC quality of care for general surgery procedures and will provide ASCs with information that can be used to improve their quality of care. Detailed testing results are available in the technical report for this measure, located at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
On June 6, 2018, the NQF's Consensus Standards Approval Committee endorsed ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357).[144] The proposed ASC-19 measure is consistent with the information submitted to the NQF and the MAP, supporting its scientific acceptability for use in quality reporting programs. We note that we have made minor annual coding updates to the measure to incorporate changes to the CPT and ICD-10 coding systems and to incorporate clinical input to remove select procedures outside the scope of general surgery as noted above, endoscopic plantar, clean out mastoid cavity, chemical peels, dermabrasions, and nerve procedures. For the current list of codes that define the proposed ASC-19 measure and a description of updates since development, we refer readers to the zip file labeled “Version 1.0 Hospital Visits General Surgery ASC Procedures Measure Technical Report” located at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
We believe this proposed measure reflects consensus among stakeholders because it was developed with stakeholder input from a TEP convened by a CMS contractor as well as from the measure development public comment period.[145] During the measure development processes and the MAP meeting, the majority of public commenters supported the measure's focus on assessing patient outcomes after general surgery procedures performed in ASC setting of care. Most commenters supported MAP's conditional support of the measure, noting it should be further developed and NQF-endorsed before implementation in the ASCQR Program. Importantly, the proposed ASC-19 measure addresses the MAP-identified priority measure area of addressing preventable healthcare harm, such as surgical complications, for the ASCQR Program.[146] Therefore, we believe it is appropriate to incorporate this proposed measure into the ASCQR Program measure set because collecting and publicly reporting these data would increase transparency, inform patients and ASCs, and foster quality improvement efforts.
c. Data Sources
The proposed ASC-19 measure is claims-based using Part A and Part B Medicare administrative claims and Medicare enrollment data to calculate the measure.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39562 through 39567), we proposed that the data collection period for the proposed ASC-19 measure would be the 2 calendar years ending 2 years prior to the applicable payment determination year. For example, for the CY 2024 payment determination, the data collection period would be CYs 2021 to 2022. Because the measure data are collected via claims, ASCs will not need to submit any additional data directly to CMS. We refer readers to section XV.D.4. of this final rule with comment period for a more detailed discussion of the requirements for data submitted via claims.
d. Measure Calculation
The measure outcome is all-cause, unplanned hospital visits within 7 days of any general surgery procedure performed at an ASC. For the purposes of this measure, “hospital visits” include emergency department visits, observation stays, and unplanned inpatient admissions. The outcome of hospital visits is limited to 7 days since existing literature suggests that the vast majority of adverse events after outpatient surgery occur within the first 7 days following the surgery.[147 148] When there are two or more qualifying surgical procedures within a 7-day period, the measure considers all procedures as index procedures; however, the timeframe for outcome assessment is defined as the interval between procedures (including the day of the next procedure) and then 7 days after the last procedure.
The facility-level score is a risk-standardized hospital visit ratio (RSHVR), an approach that accounts for the clustering of patients within ASCs and variation in sample size across ASCs. The proposed ASC-19 measure reports the outcome as a risk-standardized ratio because the diverse mix of procedures included in the proposed measure can have varying levels of risk of unplanned hospital visits. The RSHVR is calculated as the ratio of the predicted to the expected number of unplanned hospital visits among ASC patients. For each ASC, the numerator of the ratio is the number of hospital visits predicted for the ASC's patients accounting for its observed rate, the number of the general surgery procedures performed at the ASC, the case-mix, and the surgical complexity mix. The denominator of the ratio is the number of hospital visits expected nationally given the ASC's case-mix and surgical complexity mix. To calculate an ASC's predicted-to-expected (P/E) ratio, the measure uses a two-level hierarchical logistic regression model. The log-odds of the outcome for an index procedure is modeled as a function of the patient demographic, comorbidity, procedure characteristics, and a random ASC-specific intercept. A ratio of less than one indicates the ASC facility's patients were estimated as having fewer post-surgical visits than expected compared to ASCs with similar surgical complexity and patients; and a ratio of greater than one indicates the ASC facility's patients were estimated as having more visits than expected. This approach is analogous to an observed-to-expected ratio, but the method accounts for within-facility correlation of the observed outcome and sample size differences, accommodates the assumption that underlying differences in quality across ASCs lead to systematic differences in outcomes, and is tailored to and appropriate for a publicly reported outcome measure as articulated in published scientific guidelines.[149 150 151] For more information on measure calculations, we refer readers to: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
e. Cohort
The patient cohort for the proposed ASC-19 measure includes all Medicare beneficiaries ages 65 and older undergoing outpatient general surgery procedures at an ASC who have 12 prior months of Medicare FFS (Medicare Parts A and B) enrollment. The target group of procedures includes those that: (1) Are routinely performed at ASCs; (2) involve some increased risk of post-surgery hospital visits; and (3) are within the scope of general surgery training. These include the following types of procedures: Abdominal (for example, hernia repair), alimentary tract (for example, hemorrhoid procedures), breast (for example, mastectomies), skin/soft tissue (for example, skin grafting), wound (for example, incision and drainage of skin and subcutaneous tissue), and varicose vein stripping. The proposed ASC-19 measure does not include gastrointestinal endoscopy, endocrine, or vascular procedures, other than varicose vein procedures, because for these procedures, reasons for hospital visits are typically related to patients' underlying comorbidities.
The scope of general surgery overlaps with that of other specialties (for example, vascular surgery and plastic surgery). For this measure, we targeted surgeries that general surgeons are trained to perform with the understanding that other subspecialists may also be performing many of these surgeries at ASCs. Since the type of surgeon performing a particular procedure may vary across ASCs in ways that affect quality, the measure is neutral to surgeons' specialty training.
Procedures included in the measure cohort are on CMS' list of covered ASC procedures.[152] We developed this list to identify surgeries that have a low-to-moderate risk profile. Surgeries on the ASC list of covered procedures do not involve or require major or prolonged invasion of body cavities, extensive blood loss, major blood vessels, or care that is either urgent or life threatening. We annually review and update this list, which includes a transparent public comment submission and review process for addition and/or removal of procedures codes.[153] The current list is accessible in the Downloads section at: https://www.cms.gov/medicare/medicare-fee-for-service-payment/ascpayment/11_addenda_updates.html.
In addition, the measure includes only “major” and “minor” procedures, as indicated by the Medicare Physician Fee Schedule global surgery indicator (GSI) values of 090 and 010, respectively, to focus the measure only on the subset of surgeries on CMS' list of covered ASC procedures that impose a meaningful risk of post-procedure hospital visits. This list of GSI values is publicly available for CY 2015 at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1612-FC.html (download PFS Addenda, Addendum B). Moreover, to identify the subset of ASC procedures within the scope of general surgery, we used the Clinical Classifications Software (CCS) developed by the Agency for Healthcare Research and Quality (AHRQ).[154] We identified and included CCS categories within the scope of general surgery, and only included individual procedures within the CCS categories at the procedure (CPT code) level if they were within the scope of general surgery practice. For more cohort details, we refer readers to the measure technical report located at: https://www.cms.gov/medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology .html.
To ensure that all patients included under this measure have full data available for outcome assessment, the measure excludes patients who survived at least 7 days following general surgery procedures at an ASC, but were not continuously enrolled in Medicare FFS (Medicare Parts A and B) during the 7 days after surgery. There are no additional patient inclusion or exclusion criteria for the proposed ASC-19 measure. Additional methodology and measure development details are available at: https://www.cms.gov/medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
f. Risk Adjustment
The statistical risk-adjustment model includes clinically relevant risk-adjustment variables that are strongly associated with risk of hospital visits within 7 days following ASC general surgery procedures. Accordingly, only comorbidities that convey information about the patient at that time or in the 12 months prior, and not complications that arise during the course of the index procedure, are included in the risk adjustment. The measure risk adjusts for age, 18 comorbidities, procedure type (abdomen vs. alimentary tract vs. breast vs. skin/soft tissue vs. wound vs. varicose vein), a variable for work Relative Value Units (RVUs) to adjust for surgical complexity, and an interaction term of procedure type and surgical complexity.[155]
To select the final set of variables for the risk-adjustment model, candidate risk variables were entered into logistic regression analyses [156] predicting the outcome of hospital visits within 7 days. To develop a parsimonious risk model, non-significant variables were iteratively removed from the model using a stepwise selection approach described by Hosmer and Lemeshow.[157] All variables significant at p < 0.05 were retained in the final model. We also tested interaction terms and retained those that were both significant at p < 0.05 and demonstrated a clinically plausible relationship to the outcome. Finally, after reviewing TEP and public comments, as well as the statistically selected variables for face validity, we settled upon the model variables. We retained one additional variable (opioid use) for the final risk model because experts advised it was an important risk predictor and expressed a strong preference for including it in the model even though it was not statistically selected. Additional details on risk model development and testing are available in the technical report at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
g. Public Reporting
We proposed that if the proposed ASC-19 measure is adopted, we would publicly report results only for facilities with sufficient case numbers to meet moderate reliability standards.[158] We would determine the case size cutoff for meeting moderate reliability standards by calculating reliability at different case sizes using the ratio of true variance to observed variance during the measure dry run (discussed below).[159] We would provide confidential performance data directly to all facilities including those which do not meet the criteria for sufficient case numbers for reliability considerations so that all facilities can benefit from seeing their measure results and individual patient-level outcomes. We believe that the measure will provide beneficiaries with information about the quality of care for general surgery procedures in the ASC setting. In addition, we believe that these performance data may help ASCs track their patient outcomes and provide information on their cases that facilities can use to improve quality of care.
h. Provision of Facility-Specific Information Prior to Public Reporting
If this proposed measure is finalized, we intend to conduct a dry run before the official data collection period or any public reporting. A dry run is a period of confidential reporting and feedback during which ASCs may review their dry run measure results, and in addition, further familiarize themselves with the measure methodology and ask questions. For the dry run, we intend to use the most current 2-year set of complete claims (usually 12 months prior to the start date) available at the time of dry run. For example, if the dry run began in June 2020, the most current 2-year set of data available would likely be July 2017 to June 2019. Because we use paid, final action Medicare claims, ASCs would not need to submit any additional data for the dry run. The dry run would generate confidential feedback reports for ASCs, including patient-level data indicating whether the patient had a hospital visit and, if so, the type of visit (emergency department visit, observation stay, or unplanned inpatient admission), the admitting facility, and the principal discharge diagnosis. Further, the dry run would enable ASCs to see their dry run measure results prior to the measure being implemented. General information about the dry run as well as confidential facility-specific reports would be made available for ASCs to review on their accounts at: http://www.qualitynet.org. We plan to continue to generate these reports for ASCs after we implement the proposed measure if it is finalized so ASCs can use the information to identify performance gaps and develop quality improvement strategies.
These confidential dry run results are not publicly reported and do not affect payment. We expect the dry run to take approximately 1 month to conduct, during which facilities would be provided the confidential report and the opportunity to review their performance and provide feedback to us. After the dry run, measure results would have a payment impact and would be publicly reported as discussed above beginning with the CY 2024 payment determination and for subsequent years.
We have provided a summary of the public comments and responses to those comments.
Comment: Several commenters supported the proposal to adopt ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers for the ASCQR Program beginning with the CY 2024 payment determination and for subsequent years. Some commenters noted that this measure will provide valuable information and does not add reporting burden.
Response: We thank the commenters for supporting the adoption of this measure for the ASCQR Program. We agree that measuring quality of care associated with procedures performed at ASCs within the scope of general surgery training will provide useful information for facilities as well as beneficiaries and other stakeholders while limiting facility burden.
Comment: One commenter recommended that we adopt the measure sooner than the CY 2024 payment determination. One commenter requested that dry run reports be provided as early as 2020 to allow sufficient time for ASCs to review their performance and ask questions. One commenter recommended that the dry run process include 2 months of data.
Response: We appreciate the commenters' input on the timing and data collection for the dry run and desires for earlier supply of their data, but we disagree that the measure should be adopted sooner. We note that the timeline proposed for implementation of this measure was to allow adequate time to conduct a dry run with at least 2 years of data and to collect data with sufficient reliability prior to the measure being used toward payment determinations and believe that the CY 2024 payment determination best fits these needs.
Comment: A few commenters expressed concern that because the measure assesses mainly skin and soft tissue procedures, it assesses only a small subset of the procedures performed in ASCs. One commenter recommended that several exclusions be removed to enable the measure to reflect more procedures.
Response: We thank commenters for their thoughtful evaluation of the cohort specifications of ASC-19. The intent of ASC-19 is to assess the quality of care for surgical procedures that (1) are routinely performed at ASCs, (2) involve risk of post-surgery hospital visits, and (3) are within the scope of general surgery training. The measure cohort includes a set of procedures informed by a group of clinical consultants and a national TEP consisting of patients, clinicians, methodologists, researchers, and providers.[160] To identify eligible ASC general surgery procedures, we first identified a list of procedures from Medicare's 2014 and 2015 ASC lists of covered procedures. This list of surgical procedures is publicly available at: https://www.cms.gov/medicare/medicare-fee-for-service-payment/ascpayment/11_addenda_updates.html. Using an existing, defined list of surgeries, rather than defining surgeries de novo, is useful for long-term measure maintenance.
Ambulatory procedures include a heterogeneous mix of non-surgical procedures, minor surgeries, and more substantive surgeries. The measure is not intended to include very low-risk (minor) surgeries or non-surgical procedures, which typically have a high volume and a very low adverse outcome rate. To focus the measure only on the subset of surgeries on Medicare's list of covered ASC procedures that impose a meaningful risk of post-procedure hospital visits; the measure includes only “major” and “minor” procedures, as indicated by the Medicare Physician Fee Schedule GSI values of 090 and 010, respectively.[52] The GSI code reflects the number of post-operative days that are included in a given procedure's global surgical payment and identifies surgical procedures of greater complexity and follow-up care.[161] This list of GSI values is publicly available for CY 2014 at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1600-FC.html and for CY 2015 at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1612-FC.html (download PFS Addenda, Addendum B).
To identify the final subset of ASC general surgery procedures to be included in the measure, we reviewed with general surgeons and TEP members the CCS categories of procedures developed by the AHRQ. We identified and included CCS categories within the scope of general surgery, and only included individual procedures within the CCS categories at the procedure (CPT® code) level if they were within the scope of general surgery practice. We did not include in the measure calculations, gastrointestinal endoscopy, endocrine, or vascular procedures, other than varicose vein procedures, because reasons for hospital visits are typically related to patients' underlying comorbidities.
The sole patient characteristic measure exclusion criterion is “Medicare coverage: beneficiaries who survived at least 7 days, but without continuous enrollment in Medicare FFS Parts A and B in the 7 days after surgery;” these beneficiaries are excluded to ensure all patients have full data available for outcome assessment.
We will continue to evaluate whether there are additional procedures that are clinically appropriate for inclusion or exclusion in the cohort definition as part of measure reevaluation.
Comment: One commenter expressed concern that for certain procedure categories (such as “Other therapeutic procedures, hemic and lymphatic system” and “Lumpectomy, quadrantectomy of breast and Mastectomy” procedures), the top 10 primary diagnoses include diagnoses that reflect patients' underlying condition rather than the quality of care received. This commenter expressed concern that facilities will be held accountable for these outcomes and recommended that the measure specifications be updated to ensure that these diagnoses are not to be used as quality signals or included in the measure results.
Response: We appreciate the commenter's review of the top diagnoses associated with a hospital visit within 7 days of general surgery procedures. Although the top reasons for hospitals visits are likely due to complications of care, as the commenter points out, some hospital visits post procedure may be due to a patient's underlying condition. As discussed in section XV.B.3.f. of this final rule with comment period, the measure is adjusted to account for variation in patients' underlying risk of using the hospital within 7 days of a procedure. Therefore, the measure score is designed to reflect differences in quality rather than differences in pre-procedure patient risk and we believe the measure specifications account for such primary diagnoses that reflect patients' underlying conditions.
Further, the measure is designed to include only unplanned inpatient admissions occurring after general surgery procedures performed at ASCs. For the purposes of this measure, a planned admission is defined as a non-acute admission for a scheduled procedure (for example, total hip replacement or cholecystectomy). Post-discharge admissions for an acute illness or for complications of care are never considered planned. In contrast, “planned” admissions are those scheduled in advance for anticipated medical treatment or procedures that must be provided in the inpatient setting. To identify admissions as planned or unplanned, we applied an algorithm previously developed for CMS's hospital readmission measures, the CMS Planned Readmission Algorithm Version 4.0.[162] In brief, the algorithm uses the procedure codes and principal discharge diagnosis codes on each hospital claim to identify admissions that are typically planned.54 A few specific, limited types of care are always considered planned (for example, major organ transplant, rehabilitation, or maintenance chemotherapy).
For more information on the measure calculation in regard to planned versus unplanned admissions, we refer readers to: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Comment: One commenter expressed concern that the reliability of the measure, which has an ICC of 0.530, is not adequate, due to the number of low-volume ASCs. The commenter stated that the reliability of a measure intended for public reporting should be at least “substantial” (ICC between 0.61 and 0.80). This commenter recommended that the minimum number of qualifying procedures be increased to improve reliability.
Response: We thank the commenter for their comment regarding reliability of the measure. We tested the reliability of the measure score by calculating the ICC. The ICC evaluates the agreement between the risk-standardized hospital visit ratios (RSHVRs) calculated in two randomly selected patient samples. Since we measured the underlying quality of general surgery procedures performed at the ASC using patient outcomes, we anticipated that two independent, random samples of patients from an ASC would generate scores that are similar. We calculated measure score reliability for a 2-year reporting period and found that the agreement between the two RSHVR values for each ASC was calculated for 2 years to be ICC [2,1] = 0.526, indicating moderate measure score reliability. Thus, we do not believe that it is necessary increase the minimum number of qualifying procedures for reliability purposes as we view the measure as having a sufficient level of reliability for adoption by the ASCQR Program.
In addition, the results of reliability testing for this measure are consistent with current ASCQR Program claims-based measures of hospital visits post-specified procedures in the ASC setting as well as with similar outcome measures endorsed by NQF; this measure was endorsed by NQF in June 2018. The measure evaluation criteria of NQF committees are considered to be rigorous and these committees typically require moderate or high reliability to achieve endorsement.
Comment: One commenter expressed concern that the risk adjusted outcome rates show little variability between ASCs and that as a result there is little opportunity for ASCs to use the data for quality improvement or for patients to discern differences in quality. The commenter expressed concern that the measure would be considered topped-out. Some commenters expressed concern that many ASCs will not meet the minimum volume threshold for the measure, because it covers such a specific range of procedures. A few commenters expressed concern that measure results will not be shared with ASCs until months after patient visits, which will limit the usefulness of the information.
Response: We understand the commenters' concerns about the ability of ASC-19 to discern differences in quality of care; however, we believe the distribution of the estimates of the measure rates for individual facilities convey meaningful variation for discerning differences between facilities and for use in quality improvement efforts. As presented in the measure technical report using Medicare FFS CYs 2014 and 2015 data, we found that the facility RSHVR ranged from 0.42 to 2.13, with a median RSHVR of 0.97 (the 25th and 75th percentiles were 0.90 and 1.10, respectively) (measure technical report available in the Downloads section at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html).
As the commenter pointed out, the descriptive approach categorized few facilities as outliers; in our measure development calculations, we identified 15 ASCs that had better than the national average and 16 ASCs that performed worse than the national average. We believe this indicates few facilities are outliers, evidencing very high or very low measure rates. The approach to categorizing facility outliers is very conservative using 95 percent confidence interval estimates (indicating a 95 percent certainty that the range of values determined by the measure calculation contains the true mean of the population of facilities) to identify outliers so as to limit erroneously designating facilities as having extreme measure rates.
Regarding the specific range of procedures for this measure, as discussed previously in this section, we focused the measure only on the subset of surgeries on Medicare's list of covered ASC procedures that impose a meaningful risk of post-procedure hospital visits.
Regarding the concern that many small-volume ASCs will not meet the minimum criteria threshold for reporting; we have sought to include as many procedures on Medicare's list of covered ASC procedures that impose a meaningful risk of post-procedure hospital visits in the measure as possible that fit within the scope of general surgery practice. In a national Medicare FFS claims dataset for CY 2014 and 2015 that included 286,999 procedures,52 1,642 ASCs were found to be performing at least 25 procedures during the data collection time period; these 1,642 ASCs had facility measure scores ranging from 0.42 to 2.13, with a median RSHVR of 0.97 (the 25th and 75th percentiles were 0.90 and 1.10, respectively). Thus, we believe that the measure as specified utilizing 2 years of claims data provides sufficient numbers of ASCs meeting the minimum volume threshold.
These findings also show that based upon the variation in the measure, while measure rates could be considered high, they are not sufficiently unvarying to not distinguish between facilities and, thus, would not be considered “topped out”. During measure development testing using a very conservative approach of a 95 percent confidence level, ASC-19 measure calculations identified 31 outliers and sufficient variation in the RSHVRs to distinguish facilities.
Irrespective of claim volumes, all facilities will receive reports with any detected cases with patient-level information to inform quality improvement activities. To support continuous improvement across the full distribution of performance scores, we typically provide measure scores and patient-level reports to facilities that indicate whether their patients had a hospital visit within 7 days, and the diagnoses and locations of visits, and intend to provide these reports to ASCs once ASC-19 is implemented. Facilities can use these data to reduce hospital visits for important procedure-related outcomes that may be preventable, including urinary retention, pain, nausea, vomiting, syncope, and other surgery-related complications.
We will continue to monitor the data used for measure score calculation prior to and during any implementation of the measure. We will continue our multiyear assessment to weigh the tradeoffs between having an adequate number of cases for the greatest number of facilities and ensure that data are timely and actionable.
Regarding the availability of data for ASC-19, our goal is to provide ASCs with the timeliest claims data available. The expedience of the Medicare claims submission and processing timelines provide constraints to the timeliness of measure production. We continue to investigate the timeliness of claims data in efforts to increase timeliness of measure production without compromising accuracy.
Comment: One commenter recommended that additional analyses be performed on high and low performing ASCs to determine if risk adjustment washes out differences and to determine what diagnoses were associated with ASCs that showed poor performance.
Response: We thank the commenter for their attention to risk adjustment for the measure. We agree that risk adjustment obscuring differences can be a concern. However, we believe the current approach to risk adjustment for the ASC-19 measure is appropriate. As part of our standard process for measure reevaluation, we will continue to monitor measure calculations as additional years of data become available.
Comment: Some commenters believed that the title of the measure, which refers to General Surgery Procedures, will mislead beneficiaries by suggesting that the score reflects the practice of general surgery. One commenter recommended clarifying the name of the measure to specify “abdominal, alimentary tract, breast, skin/soft tissue, wound, and varicose vein stripping procedures”. A few commenters expressed concern that the measure name, Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers, inaccurately suggests that it is assessing hospital visits that are 7 days in duration. Commenters recommended that the name be clarified.
Response: We appreciate the commenters' thoughtful recommendations for the measure title. We agree that it is important for the measure title to accurately reflect the focus of the measure. The scope of the measure was defined by the scope of practice of general surgeons, which includes abdominal, alimentary tract, breast, skin/soft tissue, wound, and varicose vein stripping procedures. In response to stakeholder input received during the public comment period in 2017 (available in the Downloads section at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/PC-Updates-on-Previous-Comment-Periods.html), we revised the measure's title from “Hospital Visits after General Surgery Ambulatory Surgical Center Procedures” to, “Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers” to clarify the scope of the procedures included in the measure's cohort.
We have chosen not to further revise the measure title as “7-Day” represents the duration of hospital visits that define the outcome, and the title format is consistent with other CMS outcome measure titles (for example, “Hospital 30-day all-cause risk-standardized readmission rate following acute myocardial infarction hospitalization”).
Comment: One commenter expressed concern that the measure may harm patients by discouraging necessary care, for example in a situation where an unforeseen clinical issue is discovered during a procedure and sound clinical judgement calls for a provider to recommend hospitalization or observation.
Response: We appreciate the commenter's considerations of potential unintended consequences of implementing ASC-19. We believe that adverse impact on clinical decisions will be minimal due to risk adjustment. Risk adjustment ensures that ASCs are given credit for providing care for more complex patients who are at greater risk of hospital visits. A team of clinical consultants and the national TEP provided input on the measure risk-adjustment model at multiple points during development,[52] and the measure passed the NQF surgery committee's scientific acceptability criteria.[163]
After consideration of the public comments, we are finalizing our proposal to adopt ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357) for the CY 2024 payment determination and subsequent years as proposed.
4. Summary of ASCQR Program Quality Measure Set Finalized for the CY 2024 Payment Determination and for Subsequent Years
As discussed above, we are finalizing our proposal to add one measure beginning with the CY 2024 payment determination and for subsequent years to the ASCQR Program. We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59129 through 59132) for previously finalized ASCQR Program measure sets.
Table 63 summarizes the finalized ASCQR Program measure set for the CY 2024 payment determination and subsequent years (including previously adopted measures).

5. ASCQR Program Measures and Topics for Future Consideration
In the CY 2020 OPPS/ASC proposed rule (84 FR 39567 through 39568), we considered one topic for future implementation: Updates to the submission method for ASC-1: Patient Burn, ASC-2: Patient Fall, ASC-3: Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant, and ASC-4: All-Cause Hospital Transfer/Admission measures.
ASC-1, ASC-2, ASC-3, and ASC-4 were adopted into the ASCQR Program in the CY 2012 OPPS/ASC final rule with comment period beginning with the CY 2014 payment determination (76 FR 74496 through 74500). These measures were developed by the ASC Quality Collaboration (ASC QC). The ASC QC is a cooperative effort of organizations and companies formed in 2006 with a common interest in ensuring that ASC quality data is measured and reported in a meaningful way.[164] Stakeholders in the ASC QC include ASC corporations, ASC associations, professional societies and accrediting bodies that focus on ASC quality and safety.[165] The ASC QC initiated a process of standardizing ASC quality measure development through evaluation of existing nationally endorsed quality measures to determine which could be directly applied to the outpatient surgery facility setting.[166]
The ASC QC developed and pilot-tested ASC-1, ASC-2, ASC-3, and ASC-4 at the facility-level for feasibility and usability (76 FR 74496). These measures are calculated via quality data codes (QDCs), as described in section XV.D.1. of this final rule with comment period. ASCs were formerly required to submit the appropriate QDCs on individual Medicare FFS claims billed by the facility (78 FR 75135). In the FY 2013 IPPS/LTCH PPS final rule (77 FR 53640 through 53641), we finalized our policy that the minimum threshold for successful reporting be that at least 50 percent of claims meeting measure specifications contain QDCs. At that time, we believed that 50 percent was a reasonable minimum threshold for the initial implementation years of the ASCQR Program, because ASCs were not yet familiar with how to report quality data under the ASCQR Program and because many ASCs are relatively small and may have needed more time to set up reporting systems (77 FR 53641). We stated in that final rule that we intended to propose to increase this percentage for subsequent years' payment determinations as ASCs become more familiar with reporting requirements for the ASCQR Program. We have assessed this reporting threshold annually and have found that over 78 percent of reporting ASCs report data for at least 90 percent of eligible claims.
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59117 through 59123), we expressed concern that the data submission method for these measures may impact the completeness and accuracy of the data due to the inability of ASCs to correct errors in submitted QDCs that are used to calculate these measures. An ASC that identifies an erroneous or missing QDC is unable to correct or add a QDC if the claim has already been submitted to Medicare and been processed. We also stated that we believe that revising the data submission method for the measures, such as via QualityNet, would address this issue and allow ASCs to correct any data submissions errors, resulting in more complete and accurate data. In that final rule with comment period, we explained that we agree it is important to continue to monitor the types of events included in these measures considering the potential negative impacts to patients' morbidity and mortality, in order to continue to prevent their occurrence and ensure that they remain rare. We acknowledged that these measures provide critical data to beneficiaries and further transparency for care provided in the ASC setting that would be useful in choosing an ASC for care, and that these measures are valuable to the ASC community.
As such, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59117 through 59123; 59134 through 59135), we retained these measures in the ASCQR Program, but suspended their data submission until further action in rulemaking with the goal of updating their data submission method.
In the CY 2020 OPPS/ASC proposed rule (84 FR 39567 through 39568), we requested comment about potential future updates to the data submission method for ASC-1: Patient Burn, ASC-2: Patient Fall, ASC-3: Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant, and ASC-4: All-Cause Hospital Transfer/Admission. Specifically, we have considered updating the data submission method to a CMS online data submission tool. We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59473) (and the previous rulemakings cited therein) and 42 CFR 416.310(c)(1) for our requirements regarding data submitted via a CMS online data submission tool. We are currently using the QualityNet website (https://www.qualitynet.org) as our CMS online data submission tool.
To submit measures via an online data submission tool to the QualityNet website, ASCs and any agents submitting data on an ASC's behalf would have to maintain a QualityNet account (§ 416.310(c)(1)). A QualityNet security administrator would be necessary to set up such an account for the purpose of submitting this information (§ 416.310(c)(1)). We believe that using a CMS online data collection tool would address our concern about the ability of ASCs to correct data submission errors because ASCs would simply report their data via the online tool. If data for these measures were submitted via QualityNet, ASCs would still submit claims for reimbursement to CMS, but would not be required to include QDCs. As specified at § 416.310(c)(ii), the data collection time period for quality measures for which data are submitted via a CMS online data submission tool is for services furnished during the calendar year 2 years prior to the payment determination year. ASCs would then submit their data for ASC-1, ASC-2, ASC-3, and ASC-4 via QualityNet during the data submission period, January 1 through May 15 in the year prior to the payment determination year. ASCs would be able to submit and modify their data throughout the data submission period and could correct any errors during this period. We are seeking comments on whether updating the data submission method for ASC-1, ASC-2, ASC-3, and ASC-4 to a CMS online data submission tool would be appropriate for these measures in the future.
We are committed to work with stakeholders to ensure the ASCQR Program measure set does not place an inappropriate amount of burden on facilities while addressing and providing information about these types of patient safety, adverse, rare events to patients and other consumers. We recognize that updating the data submission method to a CMS online data submission tool would add some burden to the ASCQR Program due to the additional time for submitting any of these four measures via QualityNet for each payment determination year. Thus, we are also seeking comment about the burden associated with potentially updating the data submission method for ASC-1, ASC-2, ASC-3, and ASC-4 to a CMS online data submission tool (for example, the QualityNet website) in future years.
The comments and our responses to the comments regarding the ASCQR Program Measures and Topics for Future Consideration are set forth below.
Comment: Several commenters supported the inclusion of these measures in the ASCQR Program. Commenters also specifically supported the potential future updates to the data collection method for ASC-1: Patient Fall, ASC-2: Patient Burn, ASC-3: Wrong Site, Wrong Side, Wrong Procedure, Wrong Implant, and ASC-4: All-Cause Hospital Transfers/Admissions and noted that the measure steward has noted that the measures are suitable for submission through the QualityNet site. Commenters noted that the change would reduce cost and burden and limit the delay that results from QDC reporting.
Several commenters supported the inclusion of these four patient safety measures in both the ASCQR and HOQR Programs; these commenters cited supporting reasons, stating that these measures are outcome measures important to beneficiaries and the Medicare program and that their inclusion in both of these quality reporting programs would facilitate meaningful comparisons between ASCs and HOPDs.
Response: We thank the commenters for their support of the inclusion of the ASC-1, ASC-2, ASC-3, and ASC-4 measures in the ASCQR Program and for their support for submission of data for these measures through the QualityNet site.
Comment: Some commenters did not support the inclusion of the ASC-1 to ASC-4 measures in the ASCQR Program. These commenters cited: That the measures lacked NQF endorsement, stating concerns about the usefulness of measuring rare events or being “topped out”; that there could be data submission systems issues; and concerns about burden. A few commenters recommended that we continue the suspension of these measures rather than revise the data collection method. One commenter noted that CMS should not change the data collection method for these measures if it would increase burden or require manual data abstraction. One commenter suggested we work with HOPDs and ASCs to identify current forums or internal hospital portals where these safety issues are documented, discussed and remedied.
Response: We thank the commenters for their views, expressing their concerns and suggesting alternatives regarding the inclusion of the ASC-1 to ASC-4 measures in the ASCQR Program. We will take them into consideration as we determine future updates to ASC-1, ASC-2, ASC-3, and ASC-4 in the ASCQR Program.
6. Maintenance of Technical Specifications for Quality Measures
We refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74513 through 74514), where we finalized our proposal to follow the same process for updating the ASCQR Program measures that we adopted for the Hospital OQR Program measures, including the subregulatory process for updating adopted measures. In the CY 2013 OPPS/ASC final rule with comment period (77 FR 68496 through 68497), the CY 2014 OPPS/ASC final rule with comment period (78 FR 75131), and the CY 2015 OPPS/ASC final rule with comment period (79 FR 66981), we provided additional clarification regarding the ASCQR Program policy in the context of the previously finalized Hospital OQR Program policy, including the processes for addressing nonsubstantive and substantive changes to adopted measures. In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70531), we provided clarification regarding our decision to not display the technical specifications for the ASCQR Program on a CMS website, but stated that we will continue to display the technical specifications for the ASCQR Program on the QualityNet website. In addition, our policies regarding the maintenance of technical specifications for the ASCQR Program are codified at 42 CFR 416.325. In the CY 2020 OPPS/ASC proposed rule (84 FR 39568 through 39569), we did not propose any changes to our policies regarding the maintenance of technical specifications for the ASCQR Program.
7. Public Reporting of ASCQR Program Data
In the CY 2012 OPPS/ASC final rule with comment period (76 FR 74514 through 74515), we finalized a policy to make data that an ASC submitted for the ASCQR Program publicly available on a CMS website after providing an ASC an opportunity to review the data to be made public. In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70531 through 70533), we finalized our policy to publicly display data by the National Provider Identifier (NPI) when the data are submitted by the NPI and to publicly display data by the CCN when the data are submitted by the CCN. In addition, we codified our policies regarding the public reporting of ASCQR Program data at 42 CFR 416.315 (80 FR 70533). In the CY 2017 OPPS/ASC final rule with comment period (81 FR 79819 through 79820), we formalized our current public display practices regarding timing of public display and the preview period by finalizing our proposals to: Publicly display data on the Hospital Compare website, or other CMS website as soon as practicable after measure data have been submitted to CMS; to generally provide ASCs with approximately 30 days to review their data before publicly reporting the data; and to announce the timeframes for each preview period starting with the CY 2018 payment determination on a CMS website and/or on our applicable listservs. In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59455 through 59470), we discussed specific public reporting policies associated with two measures beginning with the CY 2022 payment determination: ASC-17: Hospital Visits after Orthopedic Ambulatory Surgical Center Procedures, and ASC-18: Hospital Visits after Urology Ambulatory Surgical Center Procedures. In the CY 2020 OPPS/ASC Proposed Rule (84 FR 39569), we did not propose any changes to our public reporting policies.
C. Administrative Requirements
1. Requirements Regarding QualityNet Account and Security Administrator
We refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75132 through 75133) for a detailed discussion of the QualityNet security administrator requirements, including setting up a QualityNet account, and the associated timelines, for the CY 2014 payment determination and subsequent years. In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70533), we codified the administrative requirements regarding maintenance of a QualityNet account and security administrator for the ASCQR Program at § 416.310(c)(1)(i). In the CY 2020 OPPS/ASC proposed rule (84 FR 39569), we did not propose any changes to these policies.
2. Requirements Regarding Participation Status
We refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75133 through 75135) for a complete discussion of the participation status requirements for the CY 2014 payment determination and subsequent years. In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70533 through 70534), we codified these requirements regarding participation status for the ASCQR Program at 42 CFR 416.305. In the CY 2020 OPPS/ASC proposed rule (84 FR 39569), we did not propose any changes to these policies.
D. Form, Manner, and Timing of Data Submitted for the ASCQR Program
1. Requirements Regarding Data Processing and Collection Periods for Claims-Based Measures Using Quality Data Codes (QDCs)
We refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75135) for a complete summary of the data processing and collection periods for the claims-based measures using QDCs for the CY 2014 payment determination and subsequent years. In the CY 2016 OPPS/ASC final rule with comment period (80 FR 70534), we codified the requirements regarding data processing and collection periods for claims-based measures using QDCs for the ASCQR Program at 42 CFR 416.310(a)(1) and (2).
In the CY 2020 OPPS/ASC proposed rule (84 FR 39569) we did not propose any changes to these requirements. We note that data submission for the following claims-based measures using QDCs was suspended in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59117 through 59123; 59134 through 59135) until further action in rulemaking:
- ASC-1: Patient Burn;
- ASC-2: Patient Fall;
- ASC-3: Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant; and
- ASC-4: Hospital Transfer/Admission.
We also note that we are requesting comment on updating the submission method for the above measures in section XV.B.5. of this final rule with comment period.
These data processing and collection period requirements will remain in the ASCQR Program for application to any future claims-based measures using QDCs adopted by the ASCQR Program.
2. Minimum Threshold, Minimum Case Volume, and Data Completeness for Claims-Based Measures Using QDCs
We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59472) (and the previous rulemakings cited therein), as well as 42 CFR 416.310(a)(3) and 42 CFR 416.305(c) for our policies about minimum threshold, minimum case volume, and data completeness for claims-based measures using QDCs. In the CY 2020 OPPS/ASC proposed rule (84 FR 39569), we did not propose any changes to these policies.
3. Requirements for Data Submitted via an Online Data Submission Tool
We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59472) (and the previous rulemakings cited therein) and 42 CFR 416.310(c) for our previously finalized policies for data submitted via an online data submission tool. For more information on data submission using QualityNet, we refer readers to: https://www.qualitynet.org.
a. Requirements for Data Submitted via a Non-CMS Online Data Submission Tool
We refer readers to the CY 2014 OPPS/ASC final rule with comment period (78 FR 75139 through 75140) and the CY 2015 OPPS/ASC final rule with comment period (79 FR 66985 through 66986) for our requirements regarding data submitted via a non-CMS online data submission tool (that is, the CDC NHSN website). We codified our existing policies regarding the data collection time periods for measures involving online data submission and the deadline for data submission via a non-CMS online data submission tool at 42 CFR 416.310(c)(2).
As we noted in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59135), no measures submitted via a non-CMS online data submission tool remain in the ASCQR Program beginning with the CY 2020 payment determination. In the CY 2020 OPPS/ASC proposed rule (84 FR 39569 through 39570), we did not propose any changes to our non-CMS online data submission tool reporting requirements; these requirements would apply to any future non-CMS online data submission tool measures adopted in the ASCQR Program.
b. Requirements for Data Submitted via a CMS Online Data Submission Tool
We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59473) (and the previous rulemakings cited therein) and § 416.310(c)(1) for our requirements regarding data submitted via a CMS online data submission tool. We are currently using the QualityNet website to host our CMS online data submission tool: https://www.qualitynet.org. We note that in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59473), we finalized expanded submission via the CMS online tool to also allow for batch data submission and made corresponding changes to the § 416.310(c)(1)(i).
In the CY 2020 OPPS/ASC proposed rule (84 FR 39570), we did not propose any changes to this policy. The following previously finalized measures require data to be submitted via a CMS online data submission tool for the CY 2021 payment determination and subsequent years:
- ASC-9: Endoscopy/Polyp Surveillance: Appropriate Follow-Up Interval for Normal Colonoscopy in Average Risk Patients
- ASC-11: Cataracts: Improvement in Patients' Visual Function within 90 Days Following Cataract Surgery
- ASC-13: Normothermia Outcome
- ASC-14: Unplanned Anterior Vitrectomy
4. Requirements for Non-QDC Based, Claims-Based Measure Data
We did not propose any changes to our requirements for non-QDC based, claims-based measures in the CY 2020 OPPS/ASC proposed rule (84 FR 39570). We refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59136 through 59138, where we established a 3-year reporting period for the previously adopted measure, ASC-12: Facility 7-Day Risk-Standardized Hospital Visit Rate after Outpatient Colonoscopy. In that final rule with comment period (83 FR 59106 through 59107), we established a similar policy under the Hospital OQR Program.
We also note that we are finalizing our proposal to adopt ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357) in section XV.B.3. of this final rule with comment period to which these requirements for non-QDC based, claims-based measures apply.
5. Requirements for Data Submission for ASC-15a-e: Outpatient and Ambulatory Surgery Consumer Assessment of Healthcare Providers and Systems (OAS CAHPS) Survey-Based Measures
We refer readers to the CY 2017 OPPS/ASC final rule with comment period (81 FR 79822 through 79824) for our previously finalized policies regarding survey administration and vendor requirements for the CY 2020 payment determination and subsequent years. In addition, we codified these policies at 42 CFR 416.310(e). However, in the CY 2018 OPPS/ASC final rule with comment period (82 FR 59450 through 59451), we delayed implementation of the ASC-15a-e: OAS CAHPS Survey-based measures beginning with the CY 2020 payment determination (CY 2018 data submission) until further action in future rulemaking, and we refer readers to that discussion for more details. In the CY 2020 OPPS/ASC proposed rule (84 FR 39570), we did not propose any changes to this policy.
6. Extraordinary Circumstances Exception (ECE) Process for the CY 2020 Payment Determination and Subsequent Years
We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59474 through 59475) (and the previous rulemakings cited therein) and 42 CFR 416.310(d) for the ASCQR Program's policies for extraordinary circumstance exceptions (ECE) requests.
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59474 through 59475), we: (1) Changed the name of this policy from “extraordinary circumstances extensions or exemption” to “extraordinary circumstances exceptions” for the ASCQR Program, beginning January 1, 2018; and (2) revised 42 CFR 416.310(d) of our regulations to reflect this change. We also clarified that we will strive to complete our review of each request within 90 days of receipt. In the CY 2020 OPPS/ASC proposed rule (84 FR 39570), we did not propose any changes to these policies.
7. ASCQR Program Reconsideration Procedures
We refer readers to the CY 2016 OPPS/ASC final rule with comment period (82 FR 59475) (and the previous rulemakings cited therein) and 42 CFR 416.330 for the ASCQR Program's reconsideration policy. In the CY 2020 OPPS/ASC proposed rule (84 FR 39570), we did not propose any changes to this policy.
E. Payment Reduction for ASCs That Fail To Meet the ASCQR Program Requirements
1. Statutory Background
We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68499) for a detailed discussion of the statutory background regarding payment reductions for ASCs that fail to meet the ASCQR Program requirements.
2. Policy Regarding Reduction to the ASC Payment Rates for ASCs That Fail To Meet the ASCQR Program Requirements for a Payment Determination Year
The national unadjusted payment rates for many services paid under the ASC payment system are equal to the product of the ASC conversion factor and the scaled relative payment weight for the APC to which the service is assigned. For CY 2020, the ASC conversion factor is equal to the conversion factor calculated for the previous year updated by the multifactor productivity (MFP)-adjusted hospital market basket update factor. The MFP adjustment is set forth in section 1833(i)(2)(D)(v) of the Act. The MFP-adjusted hospital market basket update is the annual update for the ASC payment system for a 5-year period (CY 2019 through CY 2023). Under the ASCQR Program in accordance with section 1833(i)(7)(A) of the Act and as discussed in the CY 2013 OPPS/ASC final rule with comment period (77 FR 68499), any annual increase shall be reduced by 2.0 percentage points for ASCs that fail to meet the reporting requirements of the ASCQR Program. This reduction applied beginning with the CY 2014 payment rates (77 FR 68500). For a complete discussion of the calculation of the ASC conversion factor and our finalized proposal to update the ASC payment rates using the inpatient hospital market basket update for CYs 2019 through 2023, we refer readers to the CY 2019 OPPS/ASC final rule with comment period (83 FR 59073 through 59080).
In the CY 2013 OPPS/ASC final rule with comment period (77 FR 68499 through 68500), in order to implement the requirement to reduce the annual update for ASCs that fail to meet the ASCQR Program requirements, we finalized our proposal that we would calculate two conversion factors: A full update conversion factor and an ASCQR Program reduced update conversion factor. We finalized our proposal to calculate the reduced national unadjusted payment rates using the ASCQR Program reduced update conversion factor that would apply to ASCs that fail to meet their quality reporting requirements for that calendar year payment determination. We finalized our proposal that application of the 2.0 percentage point reduction to the annual update may result in the update to the ASC payment system being less than zero prior to the application of the MFP adjustment.
The ASC conversion factor is used to calculate the ASC payment rate for services with the following payment indicators (listed in Addenda AA and BB to the proposed rule, which are available via the internet on the CMS website): “A2”, “G2”, “P2”, “R2” and “Z2”, as well as the service portion of device-intensive procedures identified by “J8” (77 FR 68500). We finalized our proposal that payment for all services assigned the payment indicators listed above would be subject to the reduction of the national unadjusted payment rates for applicable ASCs using the ASCQR Program reduced update conversion factor (77 FR 68500).
The conversion factor is not used to calculate the ASC payment rates for separately payable services that are assigned status indicators other than payment indicators “A2”, “G2”, “J8”, “P2”, “R2” and “Z2.” These services include separately payable drugs and biologicals, pass-through devices that are contractor-priced, brachytherapy sources that are paid based on the OPPS payment rates, and certain office-based procedures, radiology services and diagnostic tests where payment is based on the PFS nonfacility PE RVU-based amount, and a few other specific services that receive cost-based payment (77 FR 68500). As a result, we also finalized our proposal that the ASC payment rates for these services would not be reduced for failure to meet the ASCQR Program requirements because the payment rates for these services are not calculated using the ASC conversion factor and, therefore, not affected by reductions to the annual update (77 FR 68500).
Office-based surgical procedures (generally those performed more than 50 percent of the time in physicians' offices) and separately paid radiology services (excluding covered ancillary radiology services involving certain nuclear medicine procedures or involving the use of contrast agents) are paid at the lesser of the PFS nonfacility PE RVU-based amounts or the amount calculated under the standard ASC ratesetting methodology. Similarly, in the CY 2015 OPPS/ASC final rule with comment period (79 FR 66933 through 66934), we finalized our proposal that payment for certain diagnostic test codes within the medical range of CPT codes for which separate payment is allowed under the OPPS will be at the lower of the PFS nonfacility PE RVU-based (or technical component) amount or the rate calculated according to the standard ASC ratesetting methodology when provided integral to covered ASC surgical procedures. In the CY 2013 OPPS/ASC final rule with comment period (77 FR 68500), we finalized our proposal that the standard ASC ratesetting methodology for this type of comparison would use the ASC conversion factor that has been calculated using the full ASC update adjusted for productivity. This is necessary so that the resulting ASC payment indicator, based on the comparison, assigned to these procedures or services is consistent for each HCPCS code, regardless of whether payment is based on the full update conversion factor or the reduced update conversion factor.
For ASCs that receive the reduced ASC payment for failure to meet the ASCQR Program requirements, we believe that it is both equitable and appropriate that a reduction in the payment for a service should result in proportionately reduced coinsurance liability for beneficiaries (77 FR 68500). Therefore, in the CY 2013 OPPS/ASC final rule with comment period (77 FR 68500), we finalized our proposal that the Medicare beneficiary's national unadjusted coinsurance for a service to which a reduced national unadjusted payment rate applies will be based on the reduced national unadjusted payment rate.
In that final rule with comment period, we finalized our proposal that all other applicable adjustments to the ASC national unadjusted payment rates would apply in those cases when the annual update is reduced for ASCs that fail to meet the requirements of the ASCQR Program (77 FR 68500). For example, the following standard adjustments would apply to the reduced national unadjusted payment rates: the wage index adjustment; the multiple procedure adjustment; the interrupted procedure adjustment; and the adjustment for devices furnished with full or partial credit or without cost (77 FR 68500). We believe that these adjustments continue to be equally applicable to payment for ASCs that do not meet the ASCQR Program requirements (77 FR 68500).
In the CY 2015, CY 2016, CY 2017, CY 2018, and CY 2019 OPPS/ASC final rules with comment period (79 FR 66981 through 66982; 80 FR 70537 through 70538; 81 FR 79825 through 79826; 82 FR 59475 through 59476; and 83 FR 59138 through 59139, respectively), we did not make any other changes to these policies. We did not propose any changes to these policies for CY 2020 in the CY 2020 OPPS/ASC proposed rule (84 FR 39570 through 39571), did not receive any public comments on these policies, and are finalizing the continuation of these policies for CY 2020.
XVI. Requirements for Hospitals To Make Public a List of Their Standard Charges and Request for Information (RFI): Quality Measurement Relating to Price Transparency for Improving Beneficiary Access to Provider and Supplier Charge Information
In the CY 2020 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Proposed Rule (84 FR 39398), we proposed requirements for hospitals to make public a list of their standard charges pursuant to 2718(e) of the Public Health Service (PHS) Act. We received over 1,400 comments on our proposed requirements for hospitals to make public their standard charges. We intend to summarize and respond to public comments on the proposed policies in a forthcoming final rule.
In addition, to inform our future efforts to develop policies related to transparency in health care charges, we published a Request for Information that sought stakeholder input on a number of related quality of health care issues. We received over 63 comments. We appreciate the feedback we received and will take it into account as we further consider our future policies.
XVII. Organ Procurement Organizations (OPOs) Conditions for Coverage (CfCs): Proposed Revision of the Definition of “Expected Donation Rate”
A. Revision of the Definition of “Expected Donation Rate”
To be an OPO, an entity must meet the applicable requirements of both the Act and the Public Health Service Act (the PHS Act). Section 1138(b) of the Act provides the statutory qualifications and requirements that an OPO must meet in order for organ procurement costs to be paid under the Medicare program or the Medicaid program. Section 1138(b)(1)(A) of the Act specifies that an OPO must operate under a grant made under section 371(a) of the PHS Act or must be certified or recertified by the Secretary as meeting the standards to be a qualified OPO within a certain time period. Congress has provided that payment may be made for organ procurement cost “only if” the OPO meets the performance-related standards prescribed by the Secretary. To receive payment under the Medicare program or the Medicaid program for organ procurement costs, the entity must have an agreement with, or be designated by, the Secretary (section 1138(b)(1)(F) of the Act and 42 CFR 486.304).
Pursuant to section 371(b)(1)(D)(ii)(II) of the PHS Act, the Secretary is required to establish outcome and process performance measures for OPOs to meet based on empirical evidence, obtained through reasonable efforts, of organ donor potential and other related factors in each service area of the qualified OPO. An OPO also must be a member of and abide by the rules and requirements of the OPTN that have been approved by the Secretary (section 1138(b)(1)(D) of the Act). We established Conditions for Coverage (CfCs) for OPOs to be able to receive payments from the Medicare and Medicaid programs at 42 CFR part 486, subpart G, to implement the statutory requirements. These regulations set forth the certification and recertification processes, outcome requirements, and process performance measures for OPOs and were effective on July 31, 2006 (71 FR 30982).
We proposed to harmonize the CMS definition of “expected donation rate” with the Scientific Registry for Transplant Recipient's (SRTR) definition of the term. The SRTR operates under contract from the Health Resources and Services Administration (HRSA) and is responsible for providing statistical and other analytic support to the Organ Procurement and Transplantation Network (OPTN) for purposes including the formulation and evaluation of organ allocation and other OPTN policies.[167] As we noted in the proposed rule (84 FR 39596), in 2009 the SRTR determined that a more precise method to calculate an OPO's expected donation rate would be to base it on the national experience for OPOs serving similar eligible donor populations and donation service areas (DSAs) and then adjust for patient characteristics, that is age, sex, race, and cause of death among eligible deaths. We agree with the SRTR's assessment for this specific measure and we proposed to revise such definition to state that the expected donation rate per 100 eligible deaths would be the rate expected for an OPO based on the national experience for OPOs serving similar eligible donor populations and DSAs. We proposed that this rate would be adjusted for the distributions of age, sex, race, and cause of death among eligible deaths.
We noted that if we finalize this proposal, this change would take effect on the effective date of the final rule with comment period, which would occur during the 2022 recertification cycle. Because the final regulation change would be prospective from the final rules' effective date in order to give OPOs adequate time to comply with the change to the definition for “expected donation rate,” we also proposed to change the time period for the observed donation rate for the second outcome measure for the 2022 recertification cycle only. As a result, we proposed to revise § 486.318(a)(2), (b)(2), and (c)(1) to reduce the time period for this outcome measure. We proposed to calculate the expected donation rate using 12 of the 24 months of data following the effective date of the final rule with comment period (using data from January 1, 2020 through December 31, 2021). After the 2022 recertification cycle, and if there were no other changes to the OPO outcome measures, we would return to assess OPO performance based on 36 months of data.
Comment: We received public comments from a wide range of individuals, OPOs, national associations and coalitions, and the Organ Procurement and Transplantation Network/United Network for Organ Sharing (OPTN/UNOS). The vast majority of comments were supportive of the proposed change to the definition of “expected donation rate”.
Response: We appreciate the commenters' support for our proposal and we thank them for their feedback. Our proposal to align our definition of “expected donation rate” with the SRTR's definition will enable us to continue to enforce our second outcome measure, eliminate provider confusion, and provide consistency between the CMS requirements and the SRTR's data. We therefore are finalizing our proposal to revise the definition of “expected donation rate” to align with the SRTR's definition, without modification. Specifically, the revised definition will state that the expected donation rate per 100 eligible deaths is the rate expected for an OPO based on the national experience for OPOs serving similar eligible donor populations and DSAs. This rate would be adjusted for the distributions of age, sex, race, and cause of death among eligible deaths.
Comment: Many commenters disagreed with the proposed change to the timeframe, which would reduce the time period for this outcome measure for the 2022 recertification cycle only. The commenters stated that reducing the time period may have unintended consequences and distort, in a positive or negative way, an OPO's performance. Some also stated that this proposal would affect OPOs with smaller volumes, and those that may be sensitive to random variability over short periods of time. In summary, the commenters stated that this change would not provide adequate time period for a statistically meaningful set of data and may incorrectly identify OPOs as failing the metric due to normal random fluctuation in activity, rather than underlying performance concerns. The commenters requested that the new definition of “expected donation rate” therefore apply to the next recertification cycle, after the completion of the current cycle.
Response: We understand commenters' concerns regarding the proposed change to the time period for this second outcome measure and we are sensitive as to how such a change might negatively impact OPOs. We note that it was not our intention to unfairly penalize OPOs or undermine our goals of accurately measuring OPO performance. Rather, given the fact that the finalization of the CY 2020 OPPS/ASC proposed rule would occur during the 2022 recertification cycle, we attempted to mitigate any timing issues with regards to the use of data for purposes of determining the second outcome measure by applying the same standard to all OPOs for the identical time period once the rule was effective. We believed that a 12-month period of the 24 months of data following the effective date of the final rule with comment period would be sufficient to determine an OPO's performance on this measure. However, we agree that using 12 out of the 24 months of data may have unintended consequences on OPOs and the recertification process, and therefore we are not finalizing this proposal.
In order to ensure fairness for OPOs and in order to finalize our change to the definition of “expected donation rate” after the effective date of the final rule, we are finalizing a policy that would not require all OPOs to meet the standards of the second outcome measure for the 2022 recertification cycle only. We are requiring OPOs to meet one of the two other outcome measures in order to be recertified (the OPO's donation rate measure and aggregate donor yield measure) for the 2022 recertification cycle only. By deferring the use of the new standard, we would ensure that no OPOs would be prejudiced by the limited time period and OPOs that may not be able to meet the second measure due to limitations of the data or other variables as described by the commenters would not be decertified based only on the changed regulation. If no subsequent changes are made to the outcome measure requirements via rulemaking, the new definition of “expected donation rate” will apply after the 2022 recertification cycle. OPOs must continue to comply with the other CfCs and continue their quality improvement efforts through their Quality Assurance and Performance Improvement (QAPI) program, as required by our rules at § 486.348.
B. Request for Information Regarding Potential Changes to the Organ Procurement Organization and Transplant Center Regulations
In the proposed rule (84 FR 39597), we stated that we were considering a comprehensive proposal to update the CfCs for OPOs and possibly the CoPs for transplant centers, and that we were therefore seeking public input regarding what revisions may be appropriate for the current CfCs for OPOs, set forth at 42 CFR 486.301 through 486.360, and the current CoPs for transplant centers, set forth at 42 CFR 482.68 through 482.104.
We also solicited comments on whether the following two potential OPO outcome measures would be valid measures and would be consistent with statutory requirements. We noted that we were especially interested in public comments about the validity and reliability of these possible measures.
The first potential measure would be the actual deceased donors as a percentage of inpatient deaths among patients 75 years of age or younger with a cause of death consistent with organ donation. The data on inpatient deaths, including additional related demographic data, would be derived from the Center for Disease Control (CDC) Detailed Mortality File and the National Center for Health Statistic's National Vital Statistics Report.
The second potential measure is the actual organs transplanted as a percentage of inpatient deaths among patients 75 years of age or younger with a cause of death consistent with organ donation.
Comment: We received a wide range of comments on the RFI. Most commenters supported changing the OPO and transplant center CfCs and CoPs, and offered specific suggestions on potential changes to these requirements. Some of those suggestions included, but were not limited to: Recommendations that CMS work with the Health Resources and Services Administration (HRSA) and the OPTN to develop combined OPO and transplant center metrics; support for the development of best practices regarding donation after cardiac death (DCD) and regulations to require support for DCD; support for a cause, age, and, location consistent (CALC) deaths metric, recommendations to develop metrics that include donor hospitals and transplant centers; recommendations that referral and notifications of imminent death and potential donors be improved; support for addressing issues that OPOs in non-contiguous states and territories face; requests to improve reimbursement for transplant centers and OPOs; and suggestions to better align definitions and terminology.
Additional suggestions included: A recommendation that CMS not use the observed versus expected measure to evaluate OPOs and that the yield measure should ultimately be replaced or supplemented with a combined OPO and transplant center metric that measures how they interact to maximize organ transplants; a recommendation that CMS take into consideration an OPO's work and commitment to research and development, deceased donor research, and participation in such projects/practices as the HOPE Project, Donor Hypothermia Study and Stanford Donor Heart Study; a recommendation that an in-patient assessment of ICU deaths be conducted; a recommendation that CMS eliminate or revise the transplant center outcomes and that the SRTR star ratings or denominator for metrics or adjustments be eliminated; that CMS should prioritize national databases for regulatory purposes; and a recommendation that CMS, HRSA, OPTN, SRTR and the Centers for Disease Control (CDC) form a taskforce to examine publically available data sources that would evaluate sources and identify the practicality of identifying ventilated patient who die in hospitals/emergency departments.
Response: We thank the commenters for their responses to our RFI. We will continue to review the public comments on the RFI for future rulemaking and potential revisions to the CfCs for OPOs and the CoPs for transplant centers.
C. Miscellaneous Comments
Although not specifically discussed in the CY 2020 OPPS/ASC proposed rule, we wanted to address the multiple commenters who urged us to finalize our proposal on the transplant center CoPs. We note that, in response to public comments that we received on the CY 2020 OPPS/ASC proposed rule, we finalized our proposals to remove the Medicare re-approval requirements for transplant centers. We refer readers to the Medicare and Medicaid Programs; Regulatory Provisions To Promote Program Efficiency, Transparency, and Burden Reduction; Fire Safety Requirements for Certain Dialysis Facilities; Hospital and Critical Access Hospital (CAH) Changes To Promote Innovation, Flexibility, and Improvement in Patient Care final rule (84 FR 51732) for more information.
XVIII. Clinical Laboratory Fee Schedule: Revisions to the Laboratory Date of Service Policy
A. Background on the Medicare Part B Laboratory Date of Service Policy
The date of service (DOS) is a required data field on all Medicare claims for laboratory services. However, a laboratory service may take place over a period of time—the date the laboratory test is ordered, the date the specimen is collected from the patient, the date the laboratory accesses the specimen, the date the laboratory performs the test, and the date results are produced may occur on different dates. In the final rule on coverage and administrative policies for clinical diagnostic laboratory services published in the Federal Register on November 23, 2001 (66 FR 58791 through 58792), we adopted a policy under which the DOS for clinical diagnostic laboratory services generally is the date the specimen is collected. In that final rule, we also established a policy that the DOS for laboratory tests that use an archived specimen is the date the specimen was obtained from storage (66 FR 58792).
In 2002, we issued Program Memorandum AB-02-134, which permitted contractors discretion in making determinations regarding the length of time a specimen must be stored to be considered “archived.” In response to comments requesting that we issue a national standard to clarify when a stored specimen can be considered “archived,” in the Procedures for Maintaining Code Lists in the Negotiated National Coverage Determinations for Clinical Diagnostic Laboratory Services final notice, published in the Federal Register on February 25, 2005 (70 FR 9357), we defined an “archived” specimen as a specimen that is stored for more than 30 calendar days before testing. Specimens stored for 30 days or less continued to have a DOS of the date the specimen was collected.
B. Medicare DOS Policy and the “14-Day Rule”
In the final rule with comment period entitled, in relevant part, “Revisions to Payment Policies, Five-Year Review of Work Relative Value Units, Changes to the Practice Expense Methodology Under the Physician Fee Schedule, and Other Changes to Payment Under Part B” published in the Federal Register on December 1, 2006 (December 1, 2006 MPFS final rule) (71 FR 69705 through 69706), we added a new § 414.510 in title 42 of the CFR regarding the clinical laboratory DOS requirements and revised our DOS policy for stored specimens. We explained in that MPFS final rule that the DOS of a test may affect payment for the test, especially in situations in which a specimen that is collected while the patient is being treated in a hospital setting (for example, during a surgical procedure) is later used for testing after the patient has been discharged from the hospital. We noted that payment for the test is usually bundled with payment for the hospital service, even when the results of the test did not guide treatment during the hospital stay. To address concerns raised for tests related to cancer recurrence and therapeutic interventions, we finalized modifications to the DOS policy in § 414.510(b)(2)(i) for a test performed on a specimen stored less than or equal to 30 calendar days from the date it was collected (a non-archived specimen), so that the DOS is the date the test was performed (instead of the date of collection) if the following conditions are met:
- The test is ordered by the patient's physician at least 14 days following the date of the patient's discharge from the hospital;
- The specimen was collected while the patient was undergoing a hospital surgical procedure;
- It would be medically inappropriate to have collected the sample other than during the hospital procedure for which the patient was admitted;
- The results of the test do not guide treatment provided during the hospital stay; and
- The test was reasonable and medically necessary for the treatment of an illness.
As we stated in the December 1, 2006 MPFS final rule, we established these five criteria, which we refer to as the “14-day rule,” to distinguish laboratory tests performed as part of posthospital care from the care a beneficiary receives in the hospital. When the 14-day rule applies, laboratory tests are not bundled into the hospital stay, but are instead paid separately under Medicare Part B (as explained in more detail below).
We also revised the DOS requirements for a chemotherapy sensitivity test performed on live tissue. As discussed in the December 1, 2006 MPFS final rule (71 FR 69706), we agreed with commenters that these tests, which are primarily used to determine posthospital chemotherapy care for patients who also require hospital treatment for tumor removal or resection, appear to be unrelated to the hospital treatment in cases where it would be medically inappropriate to collect a test specimen other than at the time of surgery, especially when the specific drugs to be tested are ordered at least 14 days following hospital discharge. As a result, we revised the DOS policy for chemotherapy sensitivity tests, based on our understanding that the results of these tests, even if they were available immediately, would not typically affect the treatment regimen at the hospital. Specifically, we modified the DOS for chemotherapy sensitivity tests performed on live tissue in § 414.510(b)(3) so that the DOS is the date the test was performed if the following conditions are met:
- The decision regarding the specific chemotherapeutic agents to test is made at least 14 days after discharge;
- The specimen was collected while the patient was undergoing a hospital surgical procedure;
- It would be medically inappropriate to have collected the sample other than during the hospital procedure for which the patient was admitted;
- The results of the test do not guide treatment provided during the hospital stay; and
- The test was reasonable and medically necessary for the treatment of an illness.
We explained in the December 1, 2006 MPFS final rule that, for chemotherapy sensitivity tests that meet this DOS policy, Medicare would allow separate payment under Medicare Part B; that is, separate from the payment for hospital services.
C. Billing and Payment for Laboratory Services Under the OPPS
As we explained in the CY 2020 OPPS/ASC proposed rule (84 FR 39599), the DOS requirements at 42 CFR 414.510 are used to determine whether a hospital bills Medicare for a clinical diagnostic laboratory test (CDLT) or whether the laboratory performing the test bills Medicare directly. Separate regulations at 42 CFR 410.42(a) and 411.15(m) generally provide that Medicare will not pay for a service furnished to a hospital patient during an encounter by an entity other than the hospital unless the hospital has an arrangement (as defined in 42 CFR 409.3) with that entity to furnish that particular service to its patients, with certain exceptions and exclusions. These regulations, which we refer to as the “under arrangements” provisions in this discussion, require that if the DOS falls during an inpatient or outpatient stay, payment for the laboratory test is usually bundled with the hospital service.
Under our current rules, if a test meets all DOS requirements in § 414.510(b)(2)(i), (b)(3), or (b)(5) (an additional exception finalized in the CY 2018 OPPS/ASC final rule with comment period that we describe later in this section), the DOS is the date the test was performed. In this situation, the laboratory would bill Medicare directly for the test and would be paid under the Clinical Laboratory Fee Schedule (CLFS) directly by Medicare. However, if the test does not meet the DOS requirements in § 414.510(b)(2)(i), (b)(3), or (b)(5), the DOS would be the date the specimen was collected from the patient. In that case, the hospital would bill Medicare for the test and then would pay the laboratory that performed the test, if the laboratory provided the test under arrangement.
In recent rulemakings, we have reviewed appropriate payment under the OPPS for certain diagnostic tests that are not commonly performed by hospitals. In CY 2014, we finalized a policy to package certain CDLTs under the OPPS (78 FR 74939 through 74942 and 42 CFR 419.2(b)(17) and 419.22(l)). In CYs 2016 and 2017, we made some modifications to this policy (80 FR 70348 through 70350; 81 FR 79592 through 79594). Under our current policy, certain CDLTs that are listed on the CLFS are packaged as integral, ancillary, supportive, dependent, or adjunctive to the primary service or services provided in the hospital outpatient setting during the same outpatient encounter and billed on the same claim. Specifically, we conditionally package most CDLTs and only pay separately for a laboratory test when it is: (1) The only service provided to a beneficiary on a claim; (2) considered a preventive service; (3) a molecular pathology test; or (4) an advanced diagnostic laboratory test (ADLT) that meets the criteria of section 1834A(d)(5)(A) of the Act (78 FR 74939 through 74942; 80 FR 70348 through 70350; and 81 FR 79592 through 79594). In the CY 2016 OPPS/ASC final rule with comment period, we excluded all molecular pathology laboratory tests from packaging because we believed these relatively new tests may have a different pattern of clinical use, which may make them generally less tied to a primary service in the hospital outpatient setting than the more common and routine laboratory tests that are packaged.
For similar reasons, in the CY 2017 OPPS/ASC final rule with comment period (81 FR 79592 through 79594), we extended the exclusion to also apply to all ADLTs that meet the criteria of section 1834A(d)(5)(A) of the Act, which we describe below. We stated that we will assign status indicator “A” (Separate payment under the CLFS) to ADLTs once a laboratory test is designated an ADLT under the CLFS. Laboratory tests that are separately payable and are listed on the CLFS are paid at the CLFS payment rates outside the OPPS.
D. ADLTs Under the New Private Payor Rate-Based CLFS
Section 1834A of the Act, as established by section 216(a) of Public Law 113-93, the Protecting Access to Medicare Act of 2014 (PAMA), required significant changes to how Medicare pays for CDLTs under the CLFS. Section 216(a) of PAMA also established a new subcategory of CDLTs known as ADLTs, with separate reporting and payment requirements under section 1834A of the Act. In the CLFS final rule published in the Federal Register on June 23, 2016, entitled “Medicare Program; Medicare Clinical Diagnostic Laboratory Tests Payment System Final Rule” (81 FR 41036), we implemented the requirements of section 1834A of the Act.
As defined in § 414.502, an ADLT is a CDLT covered under Medicare Part B that is offered and furnished only by a single laboratory, and cannot be sold for use by a laboratory other than the single laboratory that designed the test or a successor owner. Also, an ADLT must meet either Criterion (A), which implements section 1834A(d)(5)(A) of the Act, or Criterion (B), which implements section 1834A(d)(5)(B) of the Act, as follows:
- Criterion (A): The test is an analysis of multiple biomarkers of deoxyribonucleic acid (DNA), ribonucleic acid (RNA), or proteins; when combined with an empirically derived algorithm, yields a result that predicts the probability a specific individual patient will develop a certain condition(s) or respond to a particular therapy(ies); provides new clinical diagnostic information that cannot be obtained from any other test or combination of tests; and may include other assays.
Or:
- Criterion (B): The test is cleared or approved by the Food and Drug Administration.
Generally, under the revised CLFS, ADLTs are paid using the same methodology based on the weighted median of private payor rates as other CDLTs. However, updates to ADLT payment rates occur annually instead of every 3 years. The payment methodology for ADLTs is detailed in the June 23, 2016 CLFS final rule (81 FR 41076 through 41083). For additional information regarding ADLTs, we refer readers to the CMS website: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ClinicalLabFeeSched/PAMA-regulations.html.
E. Additional Laboratory DOS Policy Exception for the Hospital Outpatient Setting
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59393 through 59400), we established an additional exception at § 414.510(b)(5) for the hospital outpatient setting so that the DOS for molecular pathology tests and certain ADLTs that are excluded from the OPPS packaging policy is the date the test was performed (instead of the date of specimen collection) if certain conditions are met. Under the exception that we finalized at § 414.510(b)(5), in the case of a molecular pathology test or a test designated by CMS as an ADLT under paragraph (1) of the definition of an ADLT in § 414.502, the DOS of the test must be the date the test was performed only if:
- The test was performed following a hospital outpatient's discharge from the hospital outpatient department;
- The specimen was collected from a hospital outpatient during an encounter (as both are defined in 42 CFR 410.2);
- It was medically appropriate to have collected the sample from the hospital outpatient during the hospital outpatient encounter;
- The results of the test do not guide treatment provided during the hospital outpatient encounter; and
- The test was reasonable and medically necessary for the treatment of an illness.
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59397), we explained that we believed the laboratory DOS policy in effect prior to CY 2018 created administrative complexities for hospitals and laboratories with regard to molecular pathology tests and laboratory tests expected to be designated by CMS as ADLTs that meet the criteria of section 1834A(d)(5)(A) of the Act. We noted that under the laboratory DOS policy in effect prior to CY 2018, if the tests were ordered less than 14 days following a hospital outpatient's discharge from the hospital outpatient department, laboratories generally could not bill Medicare directly for the molecular pathology test or ADLT. In those circumstances, the hospital had to bill Medicare for the test, and the laboratory had to seek payment from the hospital. We noted that commenters informed us that because ADLTs are performed by only a single laboratory and molecular pathology tests are often performed by only a few laboratories, and because hospitals may not have the technical ability to perform these complex tests, the hospital may be reluctant to bill Medicare for a test it would not typically (or never) perform. The commenters also stated that as a result, the hospital might delay ordering the test until at least 14 days after the patient is discharged from the hospital outpatient department, or even cancel the order to avoid the DOS policy, which may restrict a patient's timely access to these tests. In addition, we noted that we had heard from commenters that the laboratory DOS policy in effect prior to CY 2018 may have disproportionately limited access for Medicare beneficiaries under Medicare Parts A and B, because Medicare Advantage plans under Medicare Part C and other private payors allow laboratories to bill directly for tests they perform.
We also recognized that greater consistency between the laboratory DOS rules and the current OPPS packaging policy would be beneficial and would address some of the administrative and billing issues created by the DOS policy in effect prior to CY 2018. We noted that we exclude all molecular pathology tests and ADLTs under section 1834A(d)(5)(A) of the Act from the OPPS packaging policy because we believe these tests may have a different pattern of clinical use, which may make them generally less tied to a primary service in the hospital outpatient setting than the more common and routine laboratory tests that are packaged, and we had already established exceptions to the DOS policy that permit the DOS to be the date of performance for certain tests that we believe are not related to the hospital treatment and are used to determine posthospital care. We stated that we believed a similar exception is justified for the molecular pathology tests and ADLTs excluded from the OPPS packaging policy, which we understood are used to guide and manage the patient's care after the patient is discharged from the hospital outpatient department. We noted that we believed that, like the other tests currently subject to DOS exceptions, these tests can legitimately be distinguished from the care the patient receives in the hospital, and thus we would not be unbundling services that are appropriately associated with hospital treatment. Moreover, we reiterated that these tests are already paid separately outside of the OPPS at CLFS payment rates. Therefore, we agreed with the commenters that the laboratory performing the test should be permitted to bill Medicare directly for these tests, instead of relying on the hospital to bill Medicare on behalf of the laboratory under arrangements.
A list of the specific laboratory tests currently subject to the laboratory DOS exception at § 414.510(b)(5) is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ClinicalLabFeeSched/Clinical-Lab-DOS-Policy.html.
Following publication of the CY 2018 OPPS/ASC final rule with comment period, we issued Change Request (CR) 10419, Transmittal 4000, the claims processing instruction implementing the laboratory DOS exception at § 414.510(b)(5), with an effective date of January 1, 2018 and an implementation date of July 2, 2018. After issuing CR 10419, we heard from stakeholders that many hospitals and laboratories were having administrative difficulties implementing the DOS exception set forth at § 414.510(b)(5). On July 3, 2018, we announced that, for a 6-month period, we would exercise enforcement discretion with respect to the laboratory DOS exception at § 414.510(b)(5). We explained that stakeholder feedback suggested many providers and suppliers would not be able to implement the laboratory DOS exception by the July 2, 2018 implementation date established by CR 10419, and that such entities required additional time to develop the systems changes necessary to enable the performing laboratory to bill for tests subject to the exception. We noted that this enforcement discretion applies to all providers and suppliers with regard to ADLTs and molecular pathology tests subject to the laboratory DOS exception policy, and that during the enforcement discretion period, hospitals may continue to bill for these tests that would otherwise be subject to the laboratory DOS exception.
We then extended the enforcement discretion period for two additional, consecutive 6-month periods, after learning through communications with representatives of providers and suppliers affected by the policy that there are still many entities who will not be able to implement the laboratory DOS exception and will need additional time to come into compliance. The enforcement discretion period is currently in effect until January 2, 2020. The latest enforcement discretion announcement as well as CR 10419, Transmittal 4000 is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ClinicalLabFeeSched/Clinical-Lab-DOS-Policy.html.
As we explained in the CY 2020 OPPS/ASC proposed rule (84 FR 39600), during this time of enforcement discretion, we have continued to gage the industry's readiness to implement the laboratory DOS exception at § 414.510(b)(5). Stakeholders, including representatives of hospitals, have informed us that hospitals, in particular, are having difficulty with developing the systems changes necessary to provide the performing laboratory with the patient's hospital outpatient status, beneficiary demographic information, and insurance information, such as whether the beneficiary is enrolled in original fee-for-service Medicare or a specific Medicare Advantage plan. According to stakeholders, the performing laboratory requires this information so that it can bill Medicare directly for the test instead of seeking payment from the hospital.
In addition, stakeholders, including representatives of laboratories, have noted that some entities performing molecular pathology testing subject to the laboratory DOS exception, such as blood banks and blood centers, may not be enrolled in the Medicare program and may not have established a mechanism to bill Medicare directly. According to these stakeholders, blood banks and blood centers that are not currently enrolled in the Medicare program would need to establish a billing mechanism so that they can bill Medicare directly when the requirements of § 414.510(b)(5) are met. Stakeholders have asserted that establishing a billing mechanism is labor intensive and that blood banks and blood centers currently lack the financial resources and expertise to take on this task.
We also noted in the CY 2020 OPPS/ASC proposed rule that protein-based Multianalyte Assays with Algorithmic Analysis (MAAAs) that are not considered molecular pathology tests and are not designated as ADLTs under paragraph (1) of the definition of ADLT in § 414.502, are also conditionally packaged under the OPPS at this time. Several stakeholders have suggested that they believe that the pattern of clinical use of some of these protein-based MAAAs make them relatively unconnected to the primary hospital outpatient service, though they do not currently qualify for the DOS exception at § 414.510(b)(5) solely because they are MAAAs. We stated that a protein-based MAAA that is designated by CMS as an ADLT under paragraph (1) of the definition of an ADLT in § 414.502 would be eligible for the DOS exception at § 414.510(b)(5), and we intend to consider policies regarding MAAAs for future rulemaking.
F. Potential Revisions to Laboratory DOS Policy and Request for Public Comments
In the CY 2020 OPPS/ASC proposed rule (84 FR 39601), we stated that in response to the implementation concerns raised by stakeholders, we were considering making additional changes to the laboratory DOS policy.
We reiterated that, under the exception that we finalized at § 414.510(b)(5), for a molecular pathology test or a test designated by CMS as an ADLT under paragraph (1) of the definition of an ADLT in § 414.502, the DOS of the test must be the date the test was performed only if: (i) The test was performed following a hospital outpatient's discharge from the hospital outpatient department; (ii) the specimen was collected from a hospital outpatient during an encounter (as both are defined in 42 CFR 410.2); (iii) it was medically appropriate to have collected the sample from the hospital outpatient during the hospital outpatient encounter; (iv) the results of the test do not guide treatment provided during the hospital outpatient encounter; and (v) the test was reasonable and medically necessary for the treatment of an illness. When all conditions under the laboratory DOS exception at § 414.510(b)(5) are met, the DOS is the date of test performance, instead of the date of specimen collection, which effectively unbundles the test from the hospital outpatient encounter. As such, the test is not considered a hospital outpatient service for which the hospital must bill Medicare and for which the performing laboratory must seek payment from the hospital, but rather a laboratory test under the CLFS for which the performing laboratory must bill Medicare directly. In the CY 2020 OPPS/ASC proposed rule we considered three options for potential changes to the laboratory DOS exception at § 414.510(b)(5), and we requested comment on these changes. Specifically, we sought comment on:
- Changing the test results requirement at 42 CFR 414.510(b)(5)(iv);
- Limiting the laboratory DOS exception at 42 CFR 414.510(b)(5) to ADLTs; and/or
- Excluding blood banks and blood centers from the laboratory DOS exception at 42 CFR 414.510(b)(5).
These potential revisions are discussed below.
1. Changing the Test Results Requirement at 42 CFR 414.510(b)(5)(iv)
We explained in the CY 2020 OPPS/ASC proposed rule that, since finalizing the laboratory DOS exception at § 414.510(b)(5), we have continued to review and analyze the factors we use to determine whether a molecular pathology test or Criterion (A) ADLT is unrelated to the hospital treatment and used to determine posthospital care, and therefore should have a DOS that is the date of performance rather than the date of specimen collection. One such factor, in § 414.510(b)(5)(iv), is that the results of the test must not guide treatment provided during the hospital outpatient encounter—meaning, the encounter in which the specimen was collected. We stated in the proposed rule that we were no longer convinced that the determination as to whether a molecular pathology test or ADLT is separable from a hospital service should be based on whether the test results guide treatment during the specific hospital outpatient encounter in which the specimen was collected. We suggested that a molecular pathology test or an ADLT that is performed on a specimen collected during a hospital outpatient encounter, in which the results of the test are intended to guide treatment during a future hospital outpatient encounter, is a hospital service, and therefore should be billed by the hospital that collected the specimen under arrangements, just like if the test does not meet one of the other prongs of § 414.510(b)(5). In contrast, if the results of the test are not intended to guide treatment during a hospital outpatient encounter, and if all other requirements in § 414.510(b)(5) are met, the test is separable from a hospital service and therefore, should be considered a laboratory service and the performing laboratory should bill for the test.
We noted that a test's relationship to a hospital outpatient encounter depends on many factors, including the patient's current diagnosis (or lack of a current diagnosis), the procedure(s) being considered for the patient, the patient's current and previous medical history, and other factors and that the ordering physician would be aware of these beneficiary characteristics. As such, we indicated that it should be the role of the ordering physician to determine whether the results of a molecular pathology test or ADLT are or are not intended to guide treatment during a hospital outpatient encounter.
Therefore, we considered a revision to our current laboratory DOS policy at § 414.510(b)(5)(iv) to specify that the ordering physician would determine whether the results of the ADLT or molecular pathology test are intended to guide treatment provided during a hospital outpatient encounter, if the other four requirements under § 414.510(b)(5) are met. We noted that, under this approach, the test would be considered a hospital service unless the ordering physician determines that the test does not guide treatment during a hospital outpatient encounter. If the ordering physician determines that the test results are not intended to guide treatment during the hospital outpatient encounter from which the specimen was collected or during a future hospital outpatient encounter, for purposes of the laboratory DOS exception at § 414.510(b)(5), the DOS service of the test would be the date of test performance. In this situation, we stated, the test would not be considered a hospital service and the performing laboratory would be required to bill for the test.
We noted that, conversely, if the other four requirements under § 414.510(b)(5) are met but the ordering physician determines that the results of the laboratory test are intended to guide treatment during a hospital outpatient encounter, the DOS would be the date of specimen collection. As a result, the hospital that collected the specimen would bill for the laboratory test under arrangements and the laboratory would seek payment from the hospital for the test. We stated that this potential revision to the laboratory DOS exception at § 414.510(b)(5) would be consistent with our belief that a molecular pathology test or a Criterion (A) ADLT is a hospital service when the results of the test are intended to guide treatment during a hospital outpatient encounter.
We requested comments from hospitals, laboratories, physicians and non-physician practitioners, and other interested stakeholders regarding this potential revision to the laboratory DOS exception at § 414.510(b)(5). In particular we sought comments regarding our view that when the results of molecular pathology testing and Criterion (A) ADLTs are intended to guide treatment during a future hospital outpatient encounter, the test is a hospital service. We also requested public comments regarding the administrative aspects of requiring the ordering physician to determine when the test results are not intended to guide the treatment during a hospital outpatient encounter, as well as the process for the ordering physician to document this decision and provide notification to the hospital that collected the specimen for billing purposes. We noted that we would consider finalizing this potential revision to the laboratory DOS policy as a result of our review of the comments received on this topic.
We also noted that we were only soliciting comments on potential changes to the laboratory DOS exception at § 414.510(b)(5), and not the 14-day rule DOS exception at § 414.510(b)(2) or the chemotherapy sensitivity test DOS exception at § 414.510(b)(3). We stated that these exceptions would continue to include the requirement that the results of the test do not guide treatment provided during the hospital stay, meaning the hospital stay in which the specimen was collected. Although we recognized that the considerations about how a hospital service is determined under § 414.510(b)(5) discussed previously may also be applicable to the 14-day rule DOS exception and chemotherapy sensitivity test DOS exception, we explained that we were only considering revisions to the laboratory DOS exception at § 414.510(b)(5) at that time. Because of the administrative issues raised by stakeholders regarding the implementation of the laboratory DOS exception at § 414.510(b)(5), we stated that we believed a cautious and incremental approach to making changes to laboratory DOS policy is warranted. As such, any potential changes to the 14-day rule DOS exception at § 414.510(b)(2) and the chemotherapy sensitivity test DOS exception at § 414.510(b)(3) would be addressed in future rulemaking.
A summary of the public comments received on this potential revision and our responses are provided below.
Comment: Many commenters stated that the current laboratory DOS exception at § 414.510(b)(5) has improved beneficiary access to precision testing like molecular pathology testing and ADLTs and urged us not to make any changes that would jeopardize beneficiary access to such testing. They asserted that this exception to laboratory DOS policy has limited delays in ordering precision diagnostic tests for patients seeking care during a hospital outpatient encounter and has afforded physicians more consistent and timely access to precision diagnostic information to guide clinical decision-making. A few commenters also submitted a summary analysis of Medicare Part B claims data comparing the utilization of molecular pathology testing in CY 2018, which reflects the first year of the laboratory DOS exception, to CY 2017, which was the last year before that exception became effective. The analysis found that the total number of molecular pathology test claims following a hospital outpatient encounter increased from 43,012 claims in 2017 to 66,637 claims in 2018, which represents an increase of about 55 percent. The commenters noted that despite the CMS announcement of enforcement discretion with respect to the laboratory DOS exception at § 414.510(b)(5), even in its first year this exception for the hospital outpatient setting has improved beneficiary access to timely diagnostic information and more effective targeted therapy and/or clinical management. As such, they urged us not to make any changes to the current laboratory DOS exception at § 414.510(b)(5), except for the change that would exclude blood banks and centers.
Response: We appreciate these comments and the claims analysis supporting the commenters' statements about increased beneficiary access to molecular pathology testing since the laboratory DOS exception at § 414.510(b)(5) became effective. As discussed later in this section, because of the concerns and objections raised by commenters, we are not finalizing the potential change to the test results requirement at § 414.510(b)(5)(iv) or the potential revision that would limit § 414.510(b)(5) to ADLTs approved under Criterion (A).
Comment: The overwhelming majority of commenters urged us not to finalize the potential change to the test results requirement at § 414.510(b)(5)(iv) because doing so would be inconsistent with current clinical practice and administratively burdensome, and may lead to beneficiary access issues. A few stakeholders also contended that this potential change to the laboratory DOS exception would be inconsistent with longstanding policy related to services performed outside the hospital outpatient setting. We discuss these comments in more detail below.
Many stakeholders stated that requiring the ordering physician to determine whether the test results are intended to guide treatment during a future hospital encounter is unworkable because it would be inconsistent with current clinical practice. They noted that the very reason why the physician is ordering the test is to determine the next clinical intervention steps for the patient. However, the ordering physician cannot be expected to reasonably predict how he or she will use the test results because the physician lacks the information to make that prediction at the time of ordering. They also noted that the physician ordering the testing may not be the only physician who treats the patient based on the test results. For example, patients with complex or chronic conditions, like cancer, often have multidisciplinary care teams that coordinate various aspects of the patients' treatment plan. In addition, the patient, and the patient's family are frequently involved in the treatment decision, which is informed by the results of the test. Therefore, commenters expressed that it is impossible for the ordering physician to predict the treatment preferences and/or site of treatment of the entire care team, as well as the preferences of the patient and the patient's family.
Many stakeholders also pointed out the administrative complexities associated with requiring the ordering physician to predict the future use of the test results, which would also require documentation in the beneficiary's medical record and coordination with the hospital and performing laboratory to ensure that the correct entity bills for the test. They contended that this potential policy change would result in a significant amount of ongoing administrative burden. For example, the hospital would need to develop a mechanism to ensure that the ordering physician actually makes a determination as to whether the test results guide treatment during a hospital outpatient encounter for each molecular pathology test and ADLT that meets the requirements of laboratory DOS exception at § 414.510(b)(5). The hospital would then need to extract that determination from the beneficiary's medical record and reflect it in the hospital's billing system, and make certain not to bill for a test that is not intended to guide treatment during the current hospital outpatient encounter or a future hospital outpatient encounter. In turn, the hospital would need to add this data element to the other data elements that it already must convey to the performing laboratory (for example, beneficiary demographic and insurance information) so that the performing laboratory can bill Medicare directly for the test.
Additionally, many commenters asserted that changing the test results requirement may lead to delayed beneficiary access to molecular pathology testing and ADLTs. For instance, several commenters noted that the performing laboratory would be permitted to bill and be paid directly by Medicare only when the ordering physician determines that the test results do not guide treatment during any hospital outpatient encounter. They noted that if the ordering physician cannot make a prediction about the future use of the test results, which as discussed above, they believed is likely to be the case, the default date of service would be the date of specimen collection and the hospital would be required to bill for the test. Therefore, they suggested test orders would most likely be delayed until at least 14 days following the patient's discharge from the hospital outpatient department to allow the performing laboratory to bill Medicare directly for the test. As a result, they contended that changing the test results requirement would once again lead to the same beneficiary access issues that prompted us to establish the laboratory DOS exception under § 414.510(b)(5) in the first place.
Finally, a few commenters stated that the potential change to the test results requirement would be inconsistent with longstanding policy related to services performed outside the hospital outpatient setting. For example, they noted that in the final rule with comment period entitled, “Office of Inspector General; Medicare Program; Prospective Payment System for Hospital Outpatient Services, Final Rule” published in the Federal Register on April 7, 2000 (65 FR 18440 through 18441), the agency stated that “[a] free-standing entity, that is, one that is not provider-based, may bill for services furnished to beneficiaries who do not meet the definition of a hospital outpatient at the time the service is furnished”. . . and that “[o]ur bundling requirements apply to services furnished to a `hospital outpatient,' as defined in § 410.2, during an `encounter,' also defined in § 410.2.” As such, they suggested the potential revision to the test results requirement would not be consistent with this longstanding policy position because it could require the hospital to bill for testing furnished days, and sometimes weeks, after the patient's hospital outpatient encounter. Therefore, they urged us not to finalize the change to the test results requirement discussed in the CY 2020 OPP/ASC proposed rule.
Response: We appreciate the stakeholder feedback regarding the various problems that could arise if we were to finalize the potential revision to the test results requirement under the laboratory DOS exception at § 414.510(b)(5)(iv) that we discussed in the CY 2020 OPP/ASC proposed rule. Based on the comments received on this potential revision, we agree that requiring the ordering physician to predict whether the results of the test will guide treatment during a future hospital outpatient encounter may be overly burdensome and inconsistent with clinical practice. As noted by the commenters, the results of the test are unknown at the time the test is ordered and, therefore, the ordering physician cannot be expected to reasonably predict how he or she will use those test results. In addition, we understand that the ordering physician typically will consult with other physicians and practitioners of the patient's care team, as well as the patient, to determine the future treatment of a patient and/or the site of service for that treatment. As such, we understand from commenters that it would be difficult for the ordering physician alone to determine whether the test results will or will not guide treatment during a future hospital outpatient encounter. We also agree that changing the test results requirement at § 414.510(b)(5)(iv) as discussed in the CY 2020 OPPS/ASC proposed rule may be administratively burdensome for the ordering physician, hospital, and performing laboratory and may lead to beneficiary access concerns. As the commenters pointed out, if the ordering physician does not make a determination as to whether the test results guide treatment during the current hospital outpatient encounter or a future hospital outpatient encounter, the default laboratory DOS would be the date of specimen collection and the hospital would be required to bill Medicare directly for the test. We agree with commenters that these circumstances could once again lead to delayed test ordering which may result in similar beneficiary access issues that existed prior to the implementation of the laboratory DOS exception at § 414.510(b(5). We also acknowledge the concerns about the potential change to the test results requirement being inconsistent with longstanding CMS policy. For these reasons, after considering the many concerns and objections raised by commenters, we are not finalizing the change to the test results requirement at § 414.510(b)(5)(iv).
2. Limiting the Laboratory DOS Exception at 42 CFR 414.510(b)(5) to ADLTs
As discussed previously in this section, we established the laboratory DOS exception at § 414.510(b)(5), in part, because of stakeholder concerns that the laboratory DOS policy in effect prior to CY 2018 created beneficiary access issues with regard to molecular pathology tests and laboratory tests expected to be designated by CMS as ADLTs that meet the criteria of section 1834A(d)(5)(A) of the Act. In the CY 2018 OPPS/ASC proposed rule (82 FR 33653), we considered revising the DOS rule to create an exception only for ADLTs that meet the criteria in section 1834A(d)(5)(A) of the Act because ADLTs are offered and furnished only by a single laboratory (as defined in 42 CFR 414.502). We noted that a hospital, or another laboratory that is not the single laboratory (as defined in 42 CFR 414.502), cannot furnish the ADLT, and there may be additional beneficiary concerns for these ADLTs that may not apply to the molecular pathology tests. For example, a hospital may not have an arrangement with the single laboratory that furnishes a particular ADLT, which could lead the hospital to delay the order for the ADLT until 14 days after the patient's discharge to avoid financial risk and thus potentially delay medically necessary care for the beneficiary. We solicited comments as to whether molecular pathology tests present the same concerns of delayed access to medically necessary care as ADLTs, noting that molecular pathology tests are not required to be furnished by a single laboratory and that there may be “kits” for certain molecular pathology tests that a hospital can purchase, allowing the hospital to perform the test. In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59399) we agreed with commenters that limiting the new laboratory DOS exception to include only ADLTs (and not molecular pathology tests) would be inconsistent with the OPPS packaging policy and that relatively few laboratories may perform certain molecular pathology testing. We also acknowledged that hospitals may not currently have the technical expertise or certification requirements necessary to perform molecular pathology testing and therefore must rely on independent laboratories to perform the test. Therefore, we concluded that similar beneficiary access concerns that apply to ADLTs may also apply to molecular pathology tests, and we decided not to limit the exception at 42 CFR 414.510(b)(5) to ADLTs only.
However, in the CY 2020 OPPS/ASC proposed rule, we stated that after further review of this issue, we no longer believed the same beneficiary access concerns that apply to ADLTs also apply to molecular pathology tests. In particular, unlike ADLTs, molecular pathology tests are not required by statute to be furnished by a single laboratory, so hospital laboratories and independent laboratories are not prevented from performing molecular pathology testing. In addition, we stated that we understood a number of kits have recently been developed and approved by FDA that would allow a hospital to more easily perform some of these molecular pathology tests. As such, we were no longer convinced that molecular pathology tests present the same concerns of delayed access to medically necessary care as ADLTs, which must be performed by a single laboratory. We noted that we believed a hospital's laboratory can develop the expertise to perform a molecular pathology test or establish an arrangement with an independent laboratory to perform the test. Therefore, we believed that any incentives that may exist to delay ordering until at least 14 days following a patient's discharge from the hospital outpatient department do not apply to molecular pathology tests.
We also recognized in the CY 2020 OPPS/ASC proposed rule that limiting the laboratory DOS exception to ADLTs is not consistent with OPPS packaging policy. As discussed previously in this section of the final rule, we exclude all molecular pathology laboratory tests from OPPS packaging because we believe these tests may have a different pattern of clinical use, which may make them generally less tied to a primary service in the hospital outpatient setting than the more common and routine laboratory tests that are packaged (80 FR 70348 through 70350). However, we stated in the proposed rule that consistency with the OPPS packaging policy only formed part of the basis for the laboratory DOS exception at § 414.510(b)(5). We noted that beneficiary access concerns were the primary reason for establishing this laboratory DOS exception and we no longer believed the access concerns are sufficiently compelling for the molecular pathology tests. In light of the billing and enrollment concerns raised by the blood banks and blood centers and administrative issues raised by other stakeholders, we expressed that the policy reasons for removing these tests from the laboratory DOS exception at § 414.510(b)(5) outweigh the difference it creates with the OPPS packaging policy.
Therefore, as discussed in the proposed rule, we considered a potential revision that would limit the laboratory DOS provisions of § 414.510(b)(5) to tests designated by CMS as an ADLT under paragraph (1) of the definition of an ADLT in § 414.502. Molecular pathology tests would be removed from the provisions of § 414.510(b)(5). However, we noted that molecular pathology tests would still be subject to the laboratory DOS provisions of § 414.510(b)(2) and (3).
We requested comments on potentially limiting the laboratory DOS exception policy at § 414.510(b)(5) to laboratory tests that have been granted Criterion (A) ADLT status by CMS. We also noted that we would consider finalizing this approach as a result of the public comments received.
A summary of the public comments received on this potential revision and our response is provided below.
Comment: Many stakeholders objected to this potential change to the laboratory DOS exception because molecular pathology tests continue to have similar beneficiary access issues as ADLTs. For example, they asserted that many molecular pathology tests that do not meet the clinical requirements of an ADLT under Criterion (A), are performed by a single laboratory (or very few laboratories) for specific clinical indications and that very few “kits” have been approved by the FDA. They noted that the vast majority of molecular pathology tests are performed by the laboratories that developed and validated them and therefore, hospitals rarely perform molecular pathology tests. A few commenters explained that about 50 test kits are available for purchase, but that many of them are redundant and test for the same analyte, leaving no more than 15-20 unique kits available for molecular testing that might be used by a hospital laboratory. In addition, these commenters stated that many hospitals would not have the capability to perform such specialized testing and the cost of bringing this specialized testing capability in-house may be prohibitive for many hospitals, particularly if the volume of testing is expected to be low, as would be the case for smaller and rural hospitals.
Several stakeholders pointed out that molecular pathology tests approved for ADLT status under Criterion (B), which requires FDA clearance or approval, are also statutorily required to be performed by a single laboratory and therefore have similar beneficiary access issues as Criterion (A) ADLTs. They contended that there is no reason why a sole-source molecular pathology test that is FDA cleared or approved should be excluded from the laboratory DOS exception, while sole-source testing approved as an ADLT under Criterion (A) are included. They noted that if the laboratory DOS exception at § 414.510(b)(5) was limited to tests granted ADLT status under Criterion (A), the performing laboratory would not be permitted to bill Medicare directly for any other molecular pathology testing performed on specimens collected during a hospital outpatient encounter, including those sole source tests approved as an ADLT under Criterion (B), unless the test meets the 14-day rule requirements under § 414.510(b)(2)(i). Therefore, these commenters maintained that limiting the laboratory DOS policy exception at § 414.510(b)(5) to ADLTs approved by CMS under Criterion (A) would once again lead to delayed test orders and timely beneficiary access concerns.
Response: We appreciate stakeholder feedback on the beneficiary access concerns related to molecular pathology testing that are not Criterion (A) ADLTs. As noted previously in this section of this final rule with comment period, we considered limiting the laboratory DOS exception at § 414.510(b)(5) to Criterion (A) ADLTs based on our belief that the beneficiary access concerns were no longer the same for molecular pathology testing, largely because they are not statutorily required to be performed by a single laboratory and we believed more kits are now available for hospitals to perform these tests. In addition, we noted this change could help address the billing and enrollment concerns raised by the blood banks and centers and administrative issues raised by other stakeholders. However, after reviewing the comments received on this topic, we no longer believe that limiting the laboratory DOS exception at § 414.510(b)(5) to ADLTs would be appropriate at this time. Commenters have informed us that many molecular pathology tests are performed by very few laboratories (or even by a single laboratory) and therefore, have similar beneficiary access concerns as ADLTs. In addition, based on the comments received, we understand that very few unique molecular pathology test kits are available for hospitals to use for molecular testing. We also acknowledge the comments that molecular pathology tests approved as ADLTs under Criterion (B) are also required by law to be performed by a single laboratory, and therefore, have similar beneficiary access issues as tests granted ADLT status under Criterion (A). As discussed later in this section of this final rule with comment period, we are finalizing the exclusion of molecular pathology testing performed by blood banks or centers from the laboratory DOS exception at § 414.510(b)(5). As such, we are no longer considering limiting the exception to ADLTs as a mechanism for addressing the billing and enrollment concerns raised by the blood bank and center industry. In summary, because of the concerns raised by commenters, we are not finalizing this potential revision to limit the laboratory DOS policy exception at § 414.510(b)(5) to laboratory tests that have been granted Criterion (A) ADLT status by CMS.
Comment: Several stakeholders contended that limiting the laboratory DOS exception at § 414.510(b)(5) to Criterion (A) ADLTs would result in additional administrative burden for hospitals, laboratories and CMS. For example, they noted that because many molecular pathology tests are sole-source tests, we would receive a large number of requests for ADLT status under Criterion (A) so that the performing laboratory may bill for the test directly when performed on a specimen collected during a hospital outpatient encounter. As a result, they asserted that hospitals and laboratories may be required to reverse their billing policies multiple times over the course of a few years, or even a few months. For example, if the laboratory DOS exception at § 414.510(b)(5) were limited to ADLTs, the performing laboratory would no longer be permitted to bill for molecular pathology tests that are not currently Criterion (A) ADLTs, and therefore, the hospital and laboratory would be required to reverse its current billing practices so that the hospital bills Medicare directly for the test, instead of the performing laboratory. Stakeholders explained that for those molecular pathology tests that eventually receive approval as a Criterion (A) ADLT, the performing laboratory and hospital would again be required to reverse their billing policies and perhaps reverse those billing policies another time if the molecular pathology test ever loses its Criterion (A) ADLT status. They contended that this potential fluctuation in billing requirements would be administratively burdensome for hospitals and laboratories and urged us not to finalize this change to the laboratory DOS policy.
Response: We agree that if we were to finalize this change, potential fluctuation in billing may occur as a result of molecular pathology testing being granted Criterion (A) ADLT status in the future, and this could result in additional burden on hospitals and performing laboratories. As noted previously, because of the concerns raised by commenters, we are not finalizing the potential revision to limit the laboratory DOS policy exception at § 414.510(b)(5) to laboratory tests that have been granted Criterion (A) ADLT status by CMS.
Comment: A few commenters supported the revision that would limit the laboratory DOS exception at § 414.510(b)(5) to Criterion (A) ADLTs as discussed in the proposed rule. They contended that removing molecular pathology tests from the exception would greatly reduce the administrative burden associated with ensuring that the appropriate entity bill Medicare directly and would therefore allow work to be devoted to actual beneficiary care.
Response: As discussed previously in this section, as a result of our review of public comments on this topic, we believe that limiting the laboratory DOS exception to ADLTs could lead to a delay in test ordering and therefore, result in similar beneficiary access issues that prompted us to establish the laboratory DOS exception at § 414.510(b)(5). For this and other reasons discussed previously, we are not finalizing this change.
3. Excluding Blood Banks and Blood Centers From the Laboratory DOS Exception at 42 CFR 414.510(b)(5)
As we discussed in the CY 2020 OPPS/ASC proposed rule (84 FR 39603), following publication of the CY 2018 OPPS/ASC final rule with comment period, stakeholders informed us that blood banks and blood centers perform some of the molecular pathology test codes that are subject to the laboratory DOS exception at § 414.510(b)(5). We noted that, based on information from stakeholders, it was our understanding that blood banks and centers are entities whose primary function is the collection, storage and dissemination of blood products and are typically accredited by the AABB (formally known as the American Association of Blood Banks). We explained that representatives of blood banks and centers contend that while these entities may perform the same molecular pathology tests that are performed and billed by other laboratories that are not blood banks and centers, the blood banks and centers perform these tests for different reasons. Specifically, they assert that the blood banks and centers perform molecular pathology testing primarily to identify the most compatible blood product for a patient, whereas other laboratories typically provide molecular pathology testing for diagnostic purposes. We stated that, according to these stakeholders, the patient has already been diagnosed with a specific disease or condition before the blood sample is provided to the blood bank or center, which are then tasked with providing compatible blood products and assessing risks of incompatibility for hospitals. In other words, blood banks and centers perform molecular pathology testing for patients to enable hospitals to prevent adverse conditions associated with blood transfusions, rather than perform molecular pathology testing for diagnostic purposes. We provided examples of molecular pathology testing performed by blood banks and centers, including red blood cell phenotyping, as described by HCPCS code 81403, red blood cell antigen testing as described by HCPCS code 0001U, and platelet antigen testing as described by HCPCS code 81105.
As discussed previously, when a test meets all of the conditions in the current laboratory DOS exception at § 414.510(b)(5), the DOS of the test must be the date the test was performed, and the laboratory that performed the test must bill Medicare directly for the test. This would include circumstances when a laboratory that is a blood bank or blood center performs the test. However, given the different purpose of molecular pathology testing performed by the blood banks and centers, that is, blood compatibility testing, in the CY 2020 OPPS/ASC proposed rule, we questioned whether the molecular pathology testing performed by blood banks and centers is appropriately separable from the hospital stay, given that it typically informs the same patient's treatment during a future hospital stay. We stated that we were concerned that our current policy may unbundle molecular testing performed by a blood bank or center for a hospital patient. We stated in the CY 2020 OPPS/ASC proposed rule that based on our concern and the comments we had received from stakeholders, we were considering a regulatory change that would exclude blood banks and centers from the laboratory DOS exception at § 414.510(b)(5). Under this potential revision, the DOS for molecular pathology testing performed by blood banks and centers on specimens collected from a hospital outpatient during a hospital outpatient encounter would be the date of specimen collection unless another exception to the DOS policy applies. As a result, the hospital would bill for the molecular pathology test under arrangements and the blood bank or center performing the test would seek payment from the hospital. In addition, we noted that for purposes of excluding blood banks and centers from the provisions of § 414.510(b)(5), we would define a blood bank and center as an entity whose primary function is the collection, storage and dissemination of blood products. We stated that we believed this potential definition of a blood bank and center describes the primary responsibility of all blood banks and centers, which distinguishes these entities from other laboratory types. We further noted that in developing a definition of blood banks and centers we were distinguishing blood banks and blood centers from non-blood bank and blood center laboratories that perform the same molecular pathology test codes but for different reasons, that is, for diagnostic purposes rather than for blood compatibility testing. We requested comments from hospitals, blood banks and centers, and other interested stakeholders regarding a potential revision to laboratory DOS policy that would exclude blood banks and centers from the laboratory DOS exception at § 414.510(b)(5). We also requested specific comments as to how a blood bank and blood center may be defined in the context of this provision, and particularly how to distinguish blood banks and centers from other clinical laboratories. We noted that we would consider finalizing a revision to the laboratory DOS policy that excludes blood banks and centers from the provisions of § 414.510(b)(5) as a result of comments received on this topic.
A summary of the public comments received on this potential revision and our responses are provided below.
Comment: Many stakeholders strongly supported the potential revision to exclude blood banks and centers from the laboratory DOS exception at § 414.510(b)(5) because this change would ensure beneficiary access to timely specialized molecular testing performed by blood banks and centers. They concurred with our reasoning that blood banks and centers typically perform molecular pathology testing to identify the most compatible blood product for the patient, which enables hospitals to prevent adverse conditions associated with blood transfusions and is inherently tied to a hospital service. They also noted that excluding blood banks and centers makes sense from a policy perspective because blood banks and centers are typically not Medicare enrolled entities, and therefore cannot bill Medicare directly. Therefore, the commenters stated that requiring blood banks and centers to comply with the laboratory DOS exception at § 414.510(b)(5) would create considerable burden and has the potential to cause delays in testing for blood compatibility and jeopardize Medicare beneficiaries' access to care. As such, stakeholders overwhelmingly supported the exclusion of blood banks and centers from the laboratory DOS exception at § 414.510(b)(5) so that the hospital is required to bill for molecular pathology testing performed by blood banks and centers.
In addition, a few commenters asserted that the potential definition of a blood bank and center, as discussed in the proposed rule, that is, “an entity whose primary function is the collection, storage and dissemination of blood products” omits “processing” and “testing” which are two critical, unique functions performed by blood banks and centers. Therefore, they recommended revisions to the potential definition of blood bank and blood center so that it clearly defines the role of blood banks and blood centers and better distinguishes these entities from other types of laboratories. Specifically, these commenters suggested that we define a blood bank and center as “an entity whose primary function is the performance or responsibility for the performance of, the collection, processing, testing, storage and/or distribution of blood or blood components intended for transfusion and transplantation.” They noted that the suggested revisions are consistent with the definition used by the AABB, which accredits the activities conducted by blood centers and blood banks.
Response: For the reasons discussed in the CY 2020 OPPS/ASC proposed rule, and based on the support received from stakeholders, we are finalizing the revision to exclude blood banks and centers from the laboratory DOS exception at § 414.510(b)(5). In addition, we agree with commenters that their suggested revised definition of blood banks and centers clearly defines the primary role of blood banks and centers and better distinguishes blood banks and centers from other types of laboratories. To effectuate this policy change, we are revising § 414.510(b)(5) to exclude molecular pathology tests when performed by a laboratory that is a blood bank or center. We are defining the term “blood bank or center” instead of “blood bank and center” to reflect that a molecular pathology test is excluded when performed by either a blood bank or blood center. We are also defining “blood bank or center” at § 414.502 as an entity whose primary function is the performance or responsibility for the performance of, the collection, processing, testing, storage and/or distribution of blood or blood components intended for transfusion and transplantation.
Comment: A few commenters urged us to clarify that all molecular testing performed by blood banks and blood centers, including molecular testing for red blood cells, white blood cells and platelets, is excluded from the laboratory DOS exception at § 414.510(b)(5). They noted that most blood banks and centers do not currently bill Medicare directly as laboratories and lack the infrastructure, resources and expertise to engage in direct billing. They also reiterated that requiring blood banks and centers to comply with the laboratory DOS exception would create considerable administrative burden on the blood bank and blood center industry. One stakeholder stated that requiring hospitals to “tease out” different purposes for molecular pathology tests performed by blood banks or centers would add even more complexity to the laboratory DOS policy exception. However, a few commenters that supported excluding blood banks and centers from the laboratory DOS exception at § 414.510(b)(5) believe that only molecular pathology testing performed for blood compatibility purposes should be excluded from the laboratory DOS exception; otherwise, blood banks or centers should be required to bill Medicare directly.
Response: We clarify that this policy change categorically excludes molecular pathology testing performed by laboratories that are blood banks or blood centers from the laboratory DOS exception at § 414.510(b)(5). Under our final policy, molecular pathology testing performed by blood banks or centers on a specimen collected during a hospital outpatient encounter is never subject to the laboratory DOS exception at § 414.510(b)(5). We believe that the burden on hospitals will be mitigated with the policy we are finalizing.
Comment: One commenter contended that excluding molecular pathology testing from the laboratory DOS exception at § 414.510(b)(5) would be consistent with existing CMS policy. The commenter noted that the Medicare Claims Processing Manual, chapter 16, section 100.2, already states that “codes for procedures, services, blood products[,] auto- transfusions . . . codes such as whole blood, various red blood cell products, platelets, plasma, and cryoprecipitate,” along with “[o]ther codes for tests primarily associated with the provision of blood products” are “not clinical laboratory tests and are therefore never subject to [clinical laboratory] fee schedule limitations.” The commenter noted that this is because “[s]uch tests identify various characteristics of blood products, but are not diagnostic in nature.” The commenter suggested that this Manual guidance already excludes molecular pathology tests performed by blood banks and centers from the laboratory DOS policy exception at § 414.510(b)(5), because paragraph (b)(5), like the rest of § 414.510, applies to the date of service for “a clinical laboratory test.” However, the commenter stated that it would be appropriate to clarify that molecular pathology testing performed by blood banks and centers must be billed by the hospital.
Response: The Medicare Claims Processing Manual, chapter 16, section 100.2, describes laboratory test codes that are never subject to the CLFS because they are not clinical laboratory tests. They include test codes for procedures, services, blood products and auto-transfusions, and other test codes primarily associated with the provision of blood products. However, as discussed previously in this section, blood banks and centers also perform some of the same molecular pathology test codes that are performed and billed by other laboratories that are not blood banks or centers, and these molecular pathology test codes are subject to the laboratory DOS exception at § 414.510(b)(5). These molecular pathology test codes are not addressed in the manual guidance discussed by the commenter. Since blood banks and centers perform some of the same molecular pathology test codes as other laboratories that are not blood banks or centers, we believe that a regulatory revision is necessary to exclude these entities from the laboratory DOS exception at § 414.510(b)(5).
4. Additional Comments
Comment: One commenter submitted two alternative policy proposals. The first alternative policy proposal involves allowing hospitals the flexibility to negotiate with independent laboratories to determine which entity is responsible for billing Medicare for tests that are subject to the laboratory DOS exception at § 414.510(b)(5). Under this approach, the laboratory DOS exception at § 414.510(b)(5) would only apply if the hospital and the performing laboratory have not agreed that the hospital will bill for the test. For instance, the hospital and laboratory would affirm their agreement that the hospital will always bill for a molecular pathology test or ADLT performed on a specimen collected during a hospital outpatient encounter. If the hospital and a specific performing laboratory do not agree to this condition, the DOS would be the date of test performance and the performing laboratory would bill Medicare directly for the test. However, only one bill for the molecular pathology test or ADLT would be permitted. That is, under no circumstances would both the hospital and performing laboratory be permitted to bill for the same test for the same beneficiary with the same date of service. The same commenter suggested another alternative policy approach that would involve amending the referring laboratory billing for referred laboratory testing provision. The commenter stated that when a test does not guide treatment during a hospital outpatient encounter, the hospital laboratory is acting as a referring laboratory in accordance with section 1833(h)(5)(A) of the Act. Under this statutory provision, a referring laboratory may bill for a referred laboratory test subject to certain conditions. The commenter asserted that it would be reasonable for CMS to amend its current policy, which only permits independent clinical laboratories to bill claims for referred laboratory services, to also include the hospital laboratory when the requirements of the laboratory DOS policy exception at § 414.510(b)(5) are met.
The commenter asserted that these alternative policies would serve as a permanent solution that would address the many operational difficulties experienced by some hospitals and performing laboratories with respect to the DOS policy. The commenter urged us to finalize these suggested policy approaches effective January 1, 2020. Or in the alternative, the commenter requested that we extend the current enforcement discretion through CY 2020. The commenter contended that the additional time of enforcement discretion would allow us to address this issue in the CY 2021 OPPS/ASC proposed rule so that we could solicit stakeholder input on another solution.
Response: We are not adopting these suggestions for CY 2020. However, we will consider the commenter's suggestions as we continue to review, evaluate and refine the laboratory DOS exception at § 414.510(b)(5).
Comment: Two commenters recommended us to articulate a final implementation date for the laboratory DOS policy exception at § 414.510(b)(5). They explained that some hospitals have incurred significant cost to implement this change, however, due to CMS's announcements of enforcement discretion, some performing laboratories have refused to implement the change, which has forced hospitals to have different billing practices depending on the performing laboratory. They requested that CMS implement the revised laboratory DOS policy exception at § 414.510(b)(5), which was effective January 1, 2018, so that hospitals and performing laboratories can proceed with implementing this change.
Response: We appreciate the commenter's feedback on this topic. However, we wish to clarify that we have implemented the laboratory DOS exception at § 414.510(b)(5). The laboratory DOS exception at § 414.510(b)(5) is currently in effect; however, we have announced that we will exercise enforcement discretion, which has allowed hospitals to continue to bill for tests that would otherwise be subject to the exception. As discussed previously in this final rule with comment period, we heard from stakeholders that many hospitals and laboratories were experiencing administrative difficulties implementing the laboratory DOS exception at § 414.510(b)(5). Therefore, we issued consecutive enforcement discretions to allow more time for hospitals and laboratories to make the necessary systems changes to enable the performing laboratory to bill Medicare directly.
Comment: One commenter requested that we apply the same laboratory DOS exception for ADLTs and molecular pathology laboratory tests in the hospital outpatient setting to tests ordered for hospital inpatients. The commenter stressed the importance of having consistent policies across all care settings and asserted that allowing the same laboratory DOS exception to apply in the inpatient setting would improve CMS' ability to track the provision of molecular pathology tests and ADLTs using HCPCS codes, which would be useful for analyzing how specific tests contribute to episode cost, outcomes, and survival rates.
Response: As discussed in the CY 2018 OPPS/ASC final rule (82 FR 59398) we believe that a similar laboratory DOS exception for ADLTs approved under Criterion (A) and molecular pathology tests performed on specimens collected from hospital inpatients would have broader policy implications for the IPPS that need to be carefully considered. We also note that we did not discuss revising the laboratory DOS policy for the inpatient setting or to improve CMS' ability to evaluate patient outcomes in the CY 2020 OPPS/ASC proposed rule. However, we intend to continue studying the laboratory DOS exception and, if warranted, consider changes to the laboratory DOS policy for laboratory tests performed on specimens collected during an inpatient hospital stay in future rulemaking.
Comment: Several stakeholders requested that we add the technical component of physician pathology services, such as in situ hybridization (ISH), and flow cytometry, to the list of test codes subject to the laboratory DOS exception at § 414.510(b)(5) because, like molecular pathology tests and ADLTs, timely access to these services are essential to determine the best course of clinical care. They also requested that molecular tests furnished as technical components of physician pathology services be excluded from OPPS packaging policy and paid at the Medicare physician fee schedule rate.
Response: We will consider the suggestions raised by commenters as we continue to review, evaluate and refine OPPS packaging policy and the laboratory DOS policy exception at § 414.510(b)(5).
Comment: A few commenters requested that CMS clarify that the date of performance is the date of a laboratory's final report. They suggested this clarification would avoid any ambiguity regarding the date of performance of the test.
Response: We appreciate the commenters' suggestion. However, as discussed in the CY 2018 OPPS/ASC final rule (82 FR 59398 through 59399) we continue to have concerns with this approach because we believe there is no clear and consistent definition of “final report” that applies to all laboratories and all types of specimens collected; that is, liquid-based, cellular, or tissue samples. Therefore, we are not making this clarification.
XIX. Prior Authorization Process and Requirements for Certain Hospital Outpatient Department (OPD) Services
A. Background
As part of our responsibility to protect the Medicare Trust Funds, we routinely analyze data associated with all facets of the Medicare program. This responsibility includes monitoring the total amount or types of claims submitted by providers and suppliers; analyzing the claims data to assess the growth in the number of claims submitted over time (for example, monthly and annually, among other intervals); and conducting comparisons of the data with other relevant data, such as the total number of Medicare beneficiaries served by providers to help ensure the continued appropriateness of payment for services furnished in the hospital outpatient department (OPD).
In line with this responsibility, we noted in the CY 2020 OPPS/ASC proposed rule that we recently completed an analysis of the volume of covered OPD services provided and determined that CMS has experienced significant increases in the utilization volume of some covered OPD services. In conducting the analysis, we targeted services that represent procedures that are likely to be cosmetic surgical procedures and/or are directly related to cosmetic surgical procedures that are not covered by Medicare, but may be combined with or masquerading as therapeutic services.[168] We also recognized the need to establish baseline measures for comparison purposes, including, but not limited to, the yearly rate-of-increase in the number of OPD claims submitted and the average annual rate-of-increase in Medicare allowed amounts. Our analysis included the review of over 1.1 billion claims related to OPD services during the 11-year period from 2007 through 2017 [169] and detailed that the overall rate of OPD claims submitted for payment to the Medicare program increased each year by an average rate of 3.2 percent. This equated to an increase from approximately 90 million OPD claims submitted for payment in 2007 to approximately 118 million claims submitted for payment in 2017. Our analysis also showed an average annual rate-of-increase in the Medicare allowed amount (the amount that Medicare would pay for services regardless of external variables, such as beneficiary plan differences, deductibles, and appeals) of 8.2 percent. We found that the total Medicare allowed amount for the OPD services claims processed in 2007 was approximately $31 billion and increased to $65 billion in 2017, while during this same 11-year period, the average annual increase in the number of Medicare beneficiaries per year was only 1.1 percent. The 8.2 percent increase exceeded the average annual increase of 5.8 percent per year in overall health care spending during that same time period (2007-2017), according to the analysis of the U.S. Bureau of Labor and Statistics Consumer Price Index for medical care.[170]
Upon reviewing specific OPD categories of services in comparison to these figures, we found higher than expected volume increases for several services. Many of these services fell within the following five general categories of services: (1) Blepharoplasty; (2) botulinum toxin injections; (3) panniculectomy; (4) rhinoplasty; and (5) vein ablation.
As discussed in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59004 through 59015), and addressed again in section X.D. of the CY 2020 OPPS/ASC proposed rule, we have developed many payment policies with the goal in mind of managing the growth in Medicare spending for OPD services, and most recently, to control unnecessary increases in the volume of OPD services using our authority under section 1833(t)(2)(F) of the Act. Section 1833(t)(2)(F) of the Act authorizes CMS to develop a method for controlling unnecessary increases in the volume of covered OPD services. We believe the increases in volume associated with certain covered OPD services described earlier in this section are unnecessary because the data show that the volume of utilization of these services far exceeds what would be expected in light of the average rate-of-increase in the number of Medicare beneficiaries; these procedures are often considered cosmetic and, in those instances, would not be covered by Medicare; and we are unaware of other factors that might contribute to clinically valid increases in volume. Therefore, these above-average increases in volume suggest an increase in unnecessary utilization. As discussed in detail below, we proposed to use the authority under section 1833(t)(2)(F) of the Act to require prior authorization for certain covered OPD services as a condition of Medicare payment.
B. Prior Authorization Process for Certain OPD Services
We believe a prior authorization process for certain OPD services would ensure that Medicare beneficiaries continue to receive medically necessary care while protecting the Medicare Trust Funds from improper payments, and at the same time keeping the medical necessity documentation requirements unchanged for providers. We believe prior authorization for these services will be an effective method for controlling increases in the volume of these services because we expect that it will reduce the instances in which Medicare pays for these services when they are merely cosmetic and not medically necessary. As a method for controlling unnecessary increases in the volume of certain covered OPD services, we proposed to use our authority under section 1833(t)(2)(F) of the Act to establish a process through which providers would submit a prior authorization request for a provisional affirmation of coverage before a covered OPD service is furnished to the beneficiary and before the claim is submitted for processing. We proposed to establish a new subpart I under 42 CFR part 419 to codify the conditions and requirements for the proposed prior authorization for certain covered OPD services to help control unnecessary increases in the volume of covered OPD services. This subpart would establish the conditions of payment for OPD services that require prior authorization; establish the submission requirements for prior authorization requests, including methods for expedited review of prior authorization requests; and provide for suspension of the prior authorization process generally, or for particular services. In order to allow time for providers to better understand this proposed prior authorization process, for CMS to ensure sufficient time is allowed for outreach and education to affected stakeholders, and for contractor operational updates to be in place, we proposed that this requirement would begin for dates of service on or after July 1, 2020. We note that we proposed to pattern some of the provisions for prior authorization for covered OPD services after the prior authorization program that we have already established for certain durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) under 42 CFR 414.234.
As we noted, CMS routinely analyzes data as part of its oversight of the Medicare program, and our analysis was used as a basis for the CY 2020 OPPS/ASC proposed rule. Moreover, the Medicare program is continuing to incorporate advancements in health information technology (health IT) into its program operations. This includes improvements in interoperability, the secure electronic transmission of clinical data, and the potential incorporation of artificial intelligence into the claims review process. As these advancements in health IT continue, we are committed to ensuring that these efficiencies and enhancements will be considered, whenever possible, to reduce the burden placed on providers.
As stated earlier, we proposed to establish a new subpart I under part 419 (containing §§ 419.80 through 419.89 (§§ 419.84 through 419.89 would be reserved)) to codify the following proposed policies for prior authorization for certain covered OPD services.
1. Basis, Scope, and Definitions for Proposed New Subpart I Under Part 419
We proposed to specify the basis and scope of the proposed subpart under proposed new § 419.80, using section 1833(t)(2)(F) of the Act as our authority to establish the prior authorization process and requirements.
We proposed to define key terms associated with the proposed prior authorization process for certain covered OPD services under proposed new § 419.81. We proposed to define “prior authorization” to mean a process through which a request for provisional affirmation of coverage is submitted to CMS or its contractors for review before the service is provided to the beneficiary and before the claim is submitted. We proposed to define “provisional affirmation” to mean a preliminary finding that a future claim for the service will meet Medicare's coverage, coding, and payment rules. As previously mentioned, we patterned these proposed definitions after the prior authorization process for certain DMEPOS under 42 CFR 414.234. Lastly, we proposed to define the “list of hospital outpatient department services requiring prior authorization” as the list of outpatient department services CMS publishes in accordance with proposed new § 419.83(a) that require prior authorization as a condition of payment.
2. Prior Authorization as a Method for Controlling Unnecessary Increases in the Volume of Covered Outpatient Services (Proposed New § 419.82)
In proposed new § 419.82(a), we proposed that, as a condition of Medicare payment, a provider must submit a prior authorization request for services on the list of hospital outpatient department services requiring prior authorization to CMS that meets the requirements of the proposed new § 419.82(c); namely, that the prior authorization request includes all documentation necessary to show that the service meets applicable Medicare coverage, coding, and payment rules, and that the request be submitted before the service is provided to the beneficiary and before the claim is submitted. We proposed that claims submitted for services that require prior authorization that have not received a provisional affirmation of coverage from CMS or its contractors would be denied, unless the provider is exempt under § 419.83(c) (proposed new in § 419.82(b)(1)). This would include the denial of any claims associated with the denial of a service listed in proposed § 419.83(a)(1), including services such as anesthesiology services, physician services, and/or facility services. Moreover, we proposed that even when a provisional affirmation has been received, a claim for services may be denied based on either technical requirements that can only be evaluated after the claim has been submitted for formal processing or information not available at the time the prior authorization request is received (proposed new § 419.82(b)(2)(i) and (ii)).
We proposed that a provider must submit a prior authorization request for any service on the list of outpatient department services requiring prior authorization that would be published by CMS (proposed new § 419.82(c)). As noted earlier, we proposed that, in submitting a prior authorization request, the provider must include all relevant documentation necessary to show that the service meets applicable Medicare coverage, coding, and payment rules and that the request be submitted before the service is provided to the beneficiary and before the claim is submitted (proposed new § 419.82(c)(1)(i) and (ii)). We also proposed that providers have an opportunity to submit prior authorization requests for expedited review when a delay could seriously jeopardize the beneficiary's life, health, or ability to regain maximum function (proposed new § 419.82(c)(2). Documentation that the beneficiary's life, health, or ability to regain maximum function is in serious jeopardy must be submitted with this request.
We proposed that CMS or its contractor will review a prior authorization request for compliance with applicable Medicare coverage, coding, and payment rules (proposed new § 419.82(d)). If the request meets the applicable Medicare coverage, coding, and payment rules, CMS or its contractor would issue a provisional affirmation to the requesting provider (proposed new § 419.82(d)(1)(i)). If the request does not meet the applicable Medicare coverage, coding, and payment rules, CMS or its contractor would issue a non-affirmation decision to the requesting provider (proposed new § 419.82(d)(1)(ii)). In proposed new § 419.82(d)(iii), we proposed that CMS or its contractor would issue a decision (affirmative or non-affirmative) within 10 business days.
We proposed that, if the provider receives a non-affirmation decision, we would allow the provider to resubmit a prior authorization request with any applicable additional relevant documentation. This would include the resubmission of requests for expedited reviews (proposed new § 419.82(e)(1) and (2)).
We proposed that CMS or its contractor would initiate an expedited review of a prior authorization request when requested by a provider and where CMS or its contractor determines that a delay could seriously jeopardize the beneficiary's life, health or ability to regain maximum function (proposed new § 419.82(d)(2)). Upon making this determination, we proposed that CMS or its contractor would issue a provisional affirmation or non-affirmation in accordance with proposed new § 419.82(d)(1) using an expedited timeframe of two business days.
As part of the requirements for the DMEPOS prior authorization process,[171] under 42 CFR 405.926(t), we specified that a prior authorization request that is non-affirmed is not an initial determination on a claim for payment for services provided and, therefore, would not be appealable. We proposed to apply this same provision to the OPD services prior authorization process. Therefore, we proposed to revise § 405.926(t) so that OPD prior authorization requests that are determined non-affirmed also would not be considered an initial determination and, therefore, would not be appealable. However, the provider will still have the opportunity to resubmit a prior authorization request under proposed new § 419.82(e) provided the claim has not yet been submitted and denied.
If a claim is submitted for the services listed in proposed new § 419.83(a)(1) without a provisional affirmation, it will be denied. The claim denial is an initial determination and a redetermination request may be submitted in accordance with 42 CFR 405.940. Consistent with current medical review and claims processing guidance, we also proposed in proposed new § 419.82(b)(3) that any claims associated with or related to a service listed in proposed new § 419.83(a)(1) for which a claim denial is issued will be denied as well since these services would be unnecessary if the service listed in proposed new § 419.83(a)((1) had not been provided. These associated services include, but are not limited to, services such as anesthesiology services, physician services, and/or facility services. The associated claims would be denied whether a non-affirmation was received for a service listed in proposed new § 419.83(a)(1) or the provider did not request a prior authorization request. A contractor is not required to request medical documentation from the provider who billed the associated claims before making such a denial. We requested public comments on whether the requirement in proposed new § 419.82(b)(3) should remain in 42 CFR part 419 or be co-located with the regulatory provisions governing initial determinations located in 42 CFR part 405.
3. Proposed List of Outpatient Department Services That Would Require Prior Authorization (Proposed New § 419.83)
We proposed that the list of covered OPD services that would require prior authorization are those identified by the CPT codes in Table 38. For ease of review, we are only including the five categories of services within which these CPT codes fall in proposed new § 419.83(a)(1). The five categories of services would be: Blepharoplasty; botulinum toxin injections; panniculectomy; rhinoplasty; and vein ablation. In proposed new § 419.83(a)(2), we proposed that technical updates, such as corrections or conforming changes to the names of the services or CPT codes, may be made on the CMS web page.
Also, we proposed that CMS may elect to exempt a provider from the prior authorization process in proposed new § 419.82 upon a provider's demonstration of compliance with Medicare coverage, coding, and payment rules and that this exemption would remain in effect until CMS elects to withdraw the exemption (proposed new § 419.83(c)). We would exempt providers that achieve a prior authorization provisional affirmation threshold of at least 90 percent during a semiannual assessment. We anticipate that an exemption will take approximately 90 calendar days to effectuate. We believe that, by achieving this percentage of provisional affirmations, the provider would be demonstrating an understanding of the requirements for submitting accurate claims. We do not believe it is necessary for a provider to achieve 100 percent compliance to qualify for an exemption because innocent and sporadic errors could occur that are not deliberate or systematic attempts to submit claims that are not payable. In addition, we propose that we might withdraw an exemption if evidence becomes available based on a review of claims that the provider has begun to submit claims that are not payable based on Medicare's billing, coding, or payment requirements. If the rate of nonpayable claims submitted becomes higher than 10 percent during a semiannual assessment, we will consider withdrawing the exemption. We anticipate that withdrawing the exemption may also take approximately 90 calendar days to effectuate.
Moreover, we proposed that CMS may suspend the outpatient department services prior authorization process requirements generally or for a particular service(s) at any time by issuing notification on CMS' web page (proposed new § 419.83(d)). While we believe this is unlikely to occur, we nonetheless believe it is necessary for us to retain flexibility in the event of certain circumstances, such as where the cost of the prior authorization program exceeds the savings it generates.
C. List of Outpatient Department Services Requiring Prior Authorization
As mentioned earlier, we have identified a list of specific services (Table 38) that, based on review and analysis of claims data for the 11-year period from 2007 through 2017, show higher than expected, and therefore, we believe, unnecessary increases in the volume of service utilization. These services fall within the following five categories: Blepharoplasty; botulinum toxin injections; panniculectomy; rhinoplasty; and vein ablation. In making the decision to propose to include the specific services in the proposed list of hospital outpatient department services requiring prior authorization as shown in Table 38, we first considered that these services are most often considered cosmetic and, therefore, are only covered by Medicare in very rare circumstances. We then viewed the current volume of utilization of these services and determined that the utilization far exceeds what would be expected in light of the average rate-of-increase in the number of Medicare beneficiaries. In the CY 2020 OPPS/ASC proposed rule, we noted that we are unaware of other factors that might contribute to increases in volume of services that indicate that the services are increasingly medically necessary, such as clinical advancements or expanded coverage criteria that would have led to the increases. Below we describe what we believe are the unnecessary increases in volume of each of the categories of services for which we proposed to require prior authorization:
- Botulinum Toxin Injections: In reviewing CMS data available through the Integrated Data Repository (IDR), we determined that destruction of nerves to muscles of the face via botulinum toxin injections had an overall average annual increase in the number of unique claims of approximately 19.3 percent from 2007 through 2017, with an average annual increase in financial expense to the Medicare program as a result of allowed amounts in service costs and payments of approximately 27.8 percent and an average annual increase in the number of unique patients of approximately 17.9 percent. Based on analysis and comparisons of claims data, these increases in service utilization volume, financial expense, and the number of Medicare patients far exceed the typical baseline rates or trends we identified.
- Panniculectomy: Our analysis of IDR data showed that panniculectomy had an average annual increase in the number of unique claims of approximately 9.2 percent from 2007 through 2017, with an average annual increase in financial expense to the Medicare program as a result of allowed amounts in service costs and payments of approximately 13.9 percent and an average annual increase in the number of unique patients of approximately 9.2 percent. Based on analysis and comparisons of claims data, these increases in service utilization volume, financial expense to the Medicare program, and the number of Medicare patients also far exceed the typical baseline rates or trends we identified (that is, the 9.2 percent average annual increase in the rate of Medicare beneficiaries receiving a panniculectomy is significantly higher than the 1.1 percent average annual increase in the Medicare beneficiaries who received outpatient services over that 11-year period). Additionally, some panniculectomy services were reported on claims by providers in combination with procedures performed on the patient's chest region, in addition to abdominal procedures.
- Vein Ablation: In reviewing the available data from the IDR, vein ablation had an average annual increase in the number of unique claims of approximately 11.1 percent from 2007 through 2017, with an average annual increase in financial expense to the Medicare program as a result of allowed amounts in service costs and payments of approximately 11.5 percent and an average annual increase in the number of unique patients of approximately 9.5 percent. Based on analysis and comparisons of claims data, these increases in service utilization volume, financial expense to the Medicare program, and the number of Medicare patients also far exceed the typical baseline rates or trends we identified (that is, the 9.5 percent average annual increase in the rate of Medicare beneficiaries receiving vein ablation is significantly higher than the 1.1 percent average annual increase in the Medicare beneficiaries who received outpatient services over that 11-year period).
- Rhinoplasty: In reviewing available IDR data, rhinoplasty had an average annual increase in the number of unique patients of approximately 1.9 percent. This represents a 64.1 percent increase in comparison to the 1.1 percent rate of increase for unique patients for all OPPS services for that same time period. Even though this category of services includes some procedures that had annual increases in service utilization volume far exceeding what we would expect based on the typical rate, this was not true for all services within the category. One example that did exceed the expected rate was the number of unique claims for the procedure of widening of the nasal passage. This rate increased significantly more than the expected rate and was as much as 34.8 percent from 2016 through 2017.
- Blepharoplasty: In reviewing the IDR data, blepharoplasty, like rhinoplasty, had overall statistics that were similar to the rate increases expected for outpatient services. However, some procedures had annual increases in service utilization volume that far exceeded these expected rates. As an example, the number of unique claims for the procedure of repairing of the upper eyelid muscle to correct drooping or paralysis increased as high as 48.9 percent from 2011 through 2012, which far exceeds the rate we would expect for such a service.
Table 38 lists the specific procedures within the five categories of services that we proposed for the proposed list of hospital outpatient department services requiring prior authorization.


4. Summary of the Public Comments and Responses to Comments on the Proposed Rule
The proposed rule, titled “Medicare Program; Proposed Changes to Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs; Price Transparency of Hospital Standard Charges; Proposed Revisions of Organ Procurement Organizations Conditions of Coverage; Proposed Prior Authorization Process and Requirements for Certain Covered Outpatient Department Services; Potential Changes to the Laboratory Date of Service Policy; Proposed Changes to Grandfathered Children's Hospitals-Within-Hospitals” (84 FR 39398 through 39644), hereinafter referred to as the “CY 2020 OPPS/ASC proposed rule,” was published in the Federal Register on August 6, 2019, with a comment period that ended on September 27, 2019. In that rule, for prior authorization, we received 96 public comments on our proposals, including comments from healthcare providers, professional and trade organizations, drug manufacturers, beneficiary advocacy organizations, and health care systems. The following is a summary of the comments we received and our responses.
Comment: We received several comments in support of prior authorization, with some adding they were “intrigued” by the promise prior authorization has in Fee-For-Service Medicare. Others commented that CMS is underestimating the amount of time and education providers will require in learning the new process. Some commenters suggested that CMS delay implementation of prior authorization beyond July 1, 2020, while others suggested that CMS proceed cautiously and roll out prior authorization on a limited basis and then scale nationally, similar to how the DMEPOS prior authorization process was implemented.
Response: We thank the commenters for their comments. We appreciate the positive responses to our proposed prior authorization process. In assessing the operational implementation schedule for prior authorization, we believe that the July 1, 2020 implementation date is reasonable and will allow enough time to educate and prepare stakeholders to be able to submit the necessary documentation for prior authorization for these services. No new documentation requirements are created as a result of this process. Instead, currently needed documents are submitted earlier in the process.
Comment: Some commenters questioned whether section 1833(t)(2)(F) of the Act grants CMS the authority to establish a prior authorization process and noted that when Congress intended to give CMS authority to implement a prior authorization process, it has done so explicitly. Still others suggested the development of the new process is “arbitrary and capricious” because the commenters believed that CMS has not demonstrated that increases in the volume of services for which we proposed to require prior authorization are unnecessary. Several commenters quoted a recent decision from the United States District Court for the District of Columbia,[172] in which the court invalidated the policy we adopted in the CY 2019 OPPS/ASC final rule with comment period to reduce payment for clinic visits furnished in excepted off-campus provider-based departments to a Physician Fee Schedule-equivalent amount as a method to control unnecessary increases in the volume of clinic visits furnished in these settings. In its decision the court stated with respect to this policy, which we also adopted under section 1833(t)(2)(F) of the Act, that “Congress did not intend CMS to use an untethered `method' to directly alter expenditures independent of other processes.” These commenters quoted the court as going on to state that, “. . . Congress directed any `methods' developed under paragraph (t)(2)(F) be implemented through other provisions of the statute.” The commenters contended that we cannot point to any other provision of the OPPS statute that would authorize a prior authorization requirement, which the commenters believed we must do following the court's decision. Still others compared CMS' attempts to establish a prior authorization process to the “functional equivalence” initiative that CMS previously undertook, which Congress later prohibited.
Response: We disagree with the commenters' contentions. We believe section 1833(t)(2)(F) of the Act gives us discretion to determine the appropriate methods to control unnecessary increases in the volume of covered OPD services. We believe that where, as here, we have determined that there have been unnecessary increases in services that are often cosmetic, section 1833(t)(2)(F) of the Act gives us authority to utilize prior authorization as a method to control those unnecessary increases. We carefully considered all available options in choosing to propose the prior authorization process, which has already been shown to be an effective tool in Fee-for-Service Medicare, and which we believe will be effective at controlling unnecessary increases for those procedures that are often cosmetic and for which we have identified unnecessary volume increases. We also believe that the description of our extensive data analysis in the CY 2020 OPPS/ASC proposed rule, comparing trends for the procedures discussed against 1.1 billion OPD claims over 11 years, demonstrated that there have been unnecessary increases for all services for which we proposed to require prior authorization and that there have not been other, legitimate reasons for the sustained increases.
We also disagree with the commenters who believe the District Court's decision in the clinic visit litigation decision forecloses our ability to adopt a method to control unnecessary increases in the volume of covered outpatient department services under section 1833(t)(2)(F) of the Act without tying that method to another provision of the OPPS statute. Rather, we believe that, unlike the clinic visit policy at issue in that decision, the prior authorization policy does not have an immediate impact on the amount of payment or the budget neutrality calculations for the OPPS, and therefore, we believe it is distinguishable from the clinic visit policy that the court invalidated and does not need to be adopted under separate authority in addition to section 1833(t)(2)(F) of the Act.
Comment: Several commenters questioned why ambulatory surgical centers (ASCs) and other provider types are exempt from this prior authorization process. The commenters believed the prior authorization process should not be implemented until CMS can also establish a prior authorization process for ASCs because they believe physicians will simply provide the affected services in ASCs instead of hospitals, thereby avoiding the OPPS prior authorization process altogether. Still others believed that physicians should be required to obtain prior authorization instead of hospitals, and that CMS should adopt regulations under the Physician Fee Schedule to require physicians to adhere to the documentation and related requirements for prior authorization.
Response: This prior authorization process is being adopted under section 1833(t)(2)(F) of the Act, which is specific to the OPPS, which provides payment only to hospital outpatient departments. As such, we cannot extend the process to ASCs or other healthcare provider types, including physicians outside of the outpatient department setting, because these entities are paid under other payment systems. We thank the commenters for noting the potential to shift these services to ASCs and will monitor these data and may consider additional program integrity oversight if such shifts are realized.
Comment: Several commenters suggested that prior authorization is not an effective method for controlling fraud and that other tools, such as CMS' development of National Coverage Decisions (NCDs) and Local Coverage Determinations (LCDs), prepayment and post-payment reviews, provider outreach and education, and law enforcement actions are more effective methods to control unnecessary increases in volume. In fact, some commenters suggested that we place providers on 100 percent pre-payment review in lieu of establishing the new prior authorization process. Others commented that prior authorization is nothing more than a “blunt instrument;” is contrary to some LCDs which clearly convey certain services are not covered; and that CMS needs to ensure coverage criteria are more easily identifiable and searchable so that hospitals can more readily comply with the requirements. One commenter questioned how to give input on establishing medical necessity and how medical necessity criteria will be set and another commenter specifically lauded CMS' not-yet-completed development of the documentation requirements look-up service (DRLS).
Response: We note that we have a variety of tools that can be used in making reasonable and necessary determinations for several procedures on the list of outpatient department services requiring prior authorization. For procedures that do not have specific LCDs or NCDs, contractors may make individual claim determinations to assess whether or not the services are reasonable and necessary, per section 1862(a)(1)(A) of the Act. This prior authorization process does not make any changes to current documentation requirements. While we recognize the utility of NCDs and LCDs and the importance of conducting prepayment and post-payment reviews, we also believe that a broad program integrity strategy must use a variety of tools to best account for potential fraud, waste and abuse, including unnecessary increases in volume. Prior authorization has already proven to be an effective method for controlling improper payments and decreasing the volume of potentially improperly billed services for certain DMEPOS items. Thus, we believe that the use of prior authorization in the OPD context will be an effective tool in controlling unnecessary increases in the volume of covered OPD services by ensuring that the correct payments are made for medically necessary OPD services, while also being consistent with our overall strategy of protecting the Medicare Trust Fund from improper payments, reducing the number of Medicare appeals, and improving provider compliance with Medicare program requirements. We will continue to work toward enhancing our overall program integrity strategy in meaningful ways. We also appreciate the positive input regarding the DRLS, and we agree that, once available, it will facilitate overall transparency in coverage requirements, which should benefit all parties.
Comment: Several commenters stated that prior authorization processes add burden, can result in unnecessary delays in care, and interfere with the physician-patient care decision or otherwise negatively affect patient care. Some commenters specifically mentioned problems associated with prior authorization processes within Medicare Advantage Plans while others conveyed that prior authorization is contrary to CMS' Patients Over Paperwork initiative.
Response: The process we are establishing specifically relates to Medicare FFS, not Medicare Advantage, and we have had demonstrated success in implementing prior authorization processes in the Medicare FFS for DMEPOS. As with our other prior authorization processes, we believe that the OPD prior authorization process for certain discrete, often cosmetic procedures can be implemented without the referenced delays in patient care. This is because we are establishing timeframes for contractors to render decisions on prior authorization requests as well as an expedited review process when the regular review timeframe could seriously jeopardize the beneficiary's health that we believe will enable hospitals to receive timely provisional affirmations. Additionally, we note that our prior authorization policy does not create any new documentation or administrative requirements. Instead, it will just require the same documents that are currently required to be submitted earlier in the process. Resources should not need to be diverted from patient care. We note that prior authorization has the added benefit of giving hospitals some assurance of payment for services for which they received a provisional affirmation. In addition, beneficiaries will have information regarding coverage prior to receiving the service, and will benefit by knowing in advance of receiving a service if they will incur financial liability for non-covered services. We believe that some assurance of payment and some protection from future audits will ultimately reduce burdens associated with denied claims and appeals.
Comment: We received comments with general questions regarding the proposed process such as who will be responsible for obtaining the prior authorization, that is, the physician or the hospital, and whether all related claims will be denied if prior authorization is not obtained. Some commenters expressed concern that physicians could be denied payment for services rendered if a hospital fails to submit a prior authorization request or fails to notify the physician of a denial.
Response: As noted above, this prior authorization process is being adopted under section 1833(t)(2)(F) of the Act, which is specific to OPD services, which provides payment only to hospital outpatient departments. In light of the different arrangements that could exist in different hospitals, we determined that enabling either the physician or the hospital to submit the prior authorization request on behalf of the hospital outpatient department was the best approach, though the hospital ultimately remains responsible for ensuring this condition of payment is met. Physicians and the hospitals are in the best position to account for the various relationships and obligations that exist and should account for the prior authorization process. Part of that process should be communication of prior authorization decisions between entities, as a unique tracking number (UTN) corresponding to the prior authorization decision must be included on the OPD claim for these services. Consistent with all Medicare Fee-for-Service prior authorization and pre-claim review processes, when a prior authorization request is submitted, the request will be assigned a UTN. The UTN must be included on any claim submitted for the services listed, which will be used to verify compliance with the prior authorization process.
Additionally, we stated that any claims associated with or related to a service that requires prior authorization for which a claim denial is issued would also be denied. These associated services include, but are not limited to, services such as anesthesiology services, physician services, and/or facility services. Consistent with current medical review and claims processing guidance (for example, Program Integrity Manual (internet Only Manuals, No. 100-08 chapter 3, section 3.2.3 et seq. and chapter 7, section 7.2.2.2), and in accordance with new § 419.82(b)(3), these related claims would be denied if the service listed in § 419.83(a)(1) had also been denied. Claims for physicians' services outside of the OPD setting will not be affected if the hospital fails to submit a prior authorization request for the OPD service.
Comment: Some commenters expressed concern that even when a provisional affirmation is obtained, the claim could ultimately be denied and that the requirement should be changed so that no claim could be denied for which a provisional affirmation was obtained. Still others asked for clarification regarding whether all claims would be denied in situations where a provisional affirmation was received but the corresponding claim was later denied. Others expressed concern that no appeal rights exist for those instances where a non-affirmation is received and that CMS should determine the cost of care to beneficiaries who are negatively impacted by the receipt of a non-affirmation or who have care denied.
Response: Having a provisional affirmation shows that a claim likely meets Medicare's coverage and payment rules and is likely to be paid. Absent evidence of fraud or gaming, a provider can anticipate payment as long as other payment requirements are met. We anticipate that most, if not all, claims for which a provisional affirmation is obtained would not be denied on the basis of medical necessity. However, it is possible the claim could be denied because it did not meet a coding or billing requirement (examples include, but are not limited to, when there are duplicate claims submitted, when some element of the claim form is incorrectly completed, or if a modifier is placed on a claim that prevents it from processing appropriately). In addition, The Improper Payments Elimination and Recovery Improvement Act of 2012 (IPERIA) (Pub. L. 112-248), requires all federal agencies to evaluate their programs for improper payments. The CMS Comprehensive Error Rate Testing (CERT) program reviews a stratified, random sample of claims annually to identify and measure improper payments. It is possible for a claim subject to prior authorization to fall within the sample. In this situation, the subject claim would not be protected from the CERT audit. In addition, the Office of Inspector General's (OIG) authority to audit claims is not impacted by the protection from future audits provided by the provisional affirmation prior authorization decision.
While we appreciate that there is concern over the lack of appeal rights for non-affirmations, we note that providers are not limited in the number of times they can resubmit requests that were previously non-affirmed, and that appeal rights still exist once a claim is actually denied. Lastly, with regard to the impact on care for those beneficiaries for which hospitals receive non-affirmations, we note that we specifically chose services that are often cosmetic and believe that it is appropriate to deny such services in the case of a non-affirmation, because a non-affirmation would indicate that Medicare's coverage, coding, and/or payment rules for the service are not being met. Consistent with current Medicare Fee-for-Service prior authorization and pre-claim review processes, the provider will receive a detailed explanation as to why the request was non-affirmed and will be afforded an unlimited number of request resubmissions. Our experience in our other prior authorization and pre-claim review processes has been that approximately 95 percent of submissions are affirmed within two requests, and that the impact of non-affirmation decisions has been minimal for necessary, covered services.
Comment: Some commenters recommended that CMS decrease the ten business day time frame for issuing provisional affirmations and non-affirmations, because the commenters believed there could be occasions where the decision ultimately takes 15 days in light of weekends and holidays being excluded from the ten business day calculation. Still others commented that providers should be exempt from having to complete the prior authorization process in emergency situations or that retroactive provisional affirmations should be issued in these circumstances; the expedited review process should be completed within 24 hours if urgent circumstances exist; and the need to submit a request for an expedited review be eliminated and instead the judgment of the physician should suffice in triggering the expedited processing time frame.
Response: We appreciate the comments in response to our proposed process. While we recognize the desire to obtain provisional affirmations as quickly as possible, given that these services are typically cosmetic and would be provided in the outpatient hospital department setting, we believe the identified time frames adequately balance program integrity, provider burden, and beneficiary concerns. In those circumstances where approval is needed more expeditiously, an expedited request can be requested and if granted, will result in a provisional affirmation or non-affirmation being issued within two business days of the expedited request, which we believe is sufficient where expedition is necessary. With respect to the OPD services selected for this program, we believe that requests for expedited review will be minimal, and note that this prior authorization process does not remove or alter the clinical judgment process in any way. We are only requesting currently required documentation earlier in the process. As the OPD is ultimately responsible for this condition of payment to be met through the prior authorization process, we respectfully disagree with the commenter's suggestion to allow the OPD to be waived from their requirement to submit the prior authorization request solely on a physician's recommendation. All requests for expedited reviews will be considered based upon the documentation submitted by the OPD, including any justification provided by physicians on behalf of the OPD, and the timeframes designed into the process are intended to ensure that beneficiaries receive necessary care for these services when appropriate.
Comment: One commenter suggested that certain provisions, including the exemption rate and the notice of exemption and/or withdrawal of an exemption, should be explicitly accounted for within the regulations located in Part 419. Still other commenters suggested that CMS determine the rate of compliance with the coverage requirements prior to the implementation of this prior authorization process so that certain providers could begin the new process with an exemption in place for attaining or exceeding the requisite 90 percent compliance rate. Alternatively, one commenter suggested that CMS use existing data to identify egregious providers to reduce burden on historically compliant providers. Finally, one commenter suggested exempting providers from prior authorization if the providers participate in standardized data collection and are willing to share their data.
Response: We thank the commenters for these suggestions. We believe we have accounted for the exemption rate in the preamble and intend to maintain the 90 percent rate. With regard to the notice of exemption and/or withdrawal of an exemption, we agree that the regulations should account for this process in more detail. We had initially stated in the CY 2020 OPPS/ASC proposed rule (84 FR 39606) that we anticipate that an exemption will take approximately 90 calendar days to effectuate. In the interest of helping ensure providers incur the least burden possible, we will formalize the ability to notify providers before our anticipated 90-day period (that is, at least 60 days). As such, we have revised § 419.83(c) to redesignate the last sentence of proposed paragraph (c)—“An exemption will remain in effect until CMS elects to withdraw the exemption” —as new subparagraph (1). We are adding a new provision at new paragraph (c)(2), which will account for the notice of an exemption or withdrawal of an exemption being delivered at least 60 calendar days prior to the implementation date. Because we are unable to determine a compliance or non-compliance rate prior to the initiation of the process because most claims have not undergone full medical review and were likely paid or denied based upon the completeness of the elements on the face of the claim, we cannot exempt certain providers or only require prior authorization for certain providers in advance of implementing the new process. Lastly, we do not believe it is sufficient to exempt providers who provide data. Through the prior authorization process, we are best able to identify problems before they occur and control for unnecessary increases in the volume of these procedures, while ensuring that beneficiaries receive medically necessary services.
Comment: Some commenters suggested that MACs do not have the clinical review capabilities to sufficiently handle prior authorization requests and suggested that CMS require specific credentials of the MAC medical reviewers to ensure the accuracy of MAC decisions. Still other commenters related several principles of prior authorization with which they believed we should comply as we implement the new prior authorization process. These principles include selective application of prior authorization to only “outliers,” review/adjustment of prior authorization lists to remove services/drugs that represent low-value prior authorization; transparency of prior authorization requirements and their clinical basis to patients and physicians; protections of patient continuity of care; and automation to improve prior authorization and process efficiency.
Response: In all Medicare Fee-for-Service medical review programs we require that MACs utilize clinicians, specifically, registered nurses, when reviewing medical documentation. We also require the oversight of a Medical Director and additional clinician engagement if necessary. We are confident that MACs have the requisite expertise to effectively administer the prior authorization process, and we maintain a robust oversight process to ensure the accuracy and consistency of their review decisions. Further, we believe the prior authorization process we are adopting aligns with the principles outlined by the commenters. Of note, we have included a process to exempt providers who consistently demonstrate compliance with Medicare rules through this prior authorization process. We also are focusing initially on procedures that are not urgent and likely cosmetic and of high value, and we have included an expedited process if circumstances warrant. Along with our contractors, we will continue to analyze the value of the services that we target for prior authorization to be sure that services are selected that are appropriate for this process. As the process matures and CMS implements new technologies, such as the DRLS or other industry standards, we will effectuate improvements to the prior authorization process and coverage requirements.
Comment: Some commenters asked for clarification regarding how CMS would carry out certain provisions of the CY 2020 OPPS/ASC proposed rule, such as establishing standardized prior authorization protocols, including timely resolution of clinical reviews and clearly articulated decision criteria and rationale in an effort to minimize case delays and encourage effective communication changes between providers and health plans. Other commenters requested that CMS adopt a required response period for initial and repeat prior authorization requests, noted CMS' lack of experience in using prior authorization in Medicare Fee-For-Service, and referenced a lack of administrative structure and guidelines as well as the need for a well-functioning portal through which prior authorization requests could be submitted.
Response: In developing this prior authorization process, we indicated that we were building upon our already established prior authorization program established for certain DMEPOS under 42 CFR 414.234, and included more detailed requirements, such as decision timeframes for both regular and expedited reviews, as well as the percentages needed to demonstrate continued compliance with Medicare coverage, coding and payment rules in order to be exempt from the prior authorization process. We have considerable experience in light of the DMEPOS prior authorization program and are leveraging this experience accordingly. As we indicated in our prior responses, we are making additional changes, including adding specific regulatory provisions, to ensure the program's administrative requirements are clear. Once finalized, CMS and our contractors will provide additional educational and outreach materials to all stakeholders.
Comments: Some commenters requested changes that are out of the scope of this rule related to Medicare Advantage plans.
Response: This prior authorization policy is specific to Medicare FFS, so we are not able to respond to comments that raise concerns regarding Medicare Advantage prior authorization programs.
Comments: One commenter pointed out that we had used U.S. Bureau of Labor and Statistics (BLS) data when attempting to compare overall health care costs against the OPD payments trending data when other spending data may be more appropriate.
Response: We thank this commenter and have evaluated U.S. Bureau of Economic Analysis (BEA) data, which we agree may be more appropriate. We had compared the 8.2 percent average annual increase for OPD services over the 11-year period of 2007 through 2017 to the 5.8 percent average annual spending calculated from the BLS data; however, after consulting with both bureaus, the BEA data better aligns with our analytic process (that is, comparing overall expenditures for OPPS services via CMS data against overall expenditures for health care services via BEA data to as opposed to comparing overall expenditures for OPPS services via CMS data against the cost of health care services for the typical consumer via BLS data). The BEA data reflected a 2.3 percent average annual increase per year in overall health care spending using data publicly available on the BEA web page, located at: https://apps.bea.gov/iTable/iTable.cfm?reqid=51&step=2&isuri=1https.
Comment: We received comments that the growth in utilization of a procedure/product class exceeding the baseline growth rates in the Medicare population is not a sufficient basis for inferring that utilization is inappropriate or that utilization growth is unwarranted and that CMS should analyze readily available clinical information that would explain changes in utilization before the agency adopts broad-based interventions such as imposing prior authorization on outpatient hospitals. The same commenter suggested that the increases seen in CPT codes 64612 and 64615 are likely due to other factors such as FDA's approval of BOTOX® in 2010, increased support for BOTOX® as a migraine treatment, and the addition of chronic migraine to the list of covered indications for BOTOX® in Medicare contractor LCDs. This commenter also recommended that if CMS chooses to move forward with implementing this prior authorization process that CMS expand the prior authorization requirements to apply to all four FDA-approved botulinum toxin therapeutic products to include DYSPORT® (J0586) and XEOMIN® (J0588) in addition to BOTOX® and MYOBLOC® so as not to create distortion in the marketplace and incentivize providers to administer those botulinum toxin therapeutic products that are not subject to prior authorization. One commenter also expressed concern that the prior authorization process could impact women and veterans more significantly than other categories because these groups tend to experience migraines at higher rates than other categories and this could ultimately lead to an increase in opioid abuse within these groups. We received several comments asking whether a provisional affirmation for botulinum toxin injections would be per injection or for a specific course of treatment over a period of time, such as twelve months. We also received comments to add codes to the list for alternative treatment options for varicose veins, such as phlebectomy and sclerotherapy.
Response: We thank the commenters for their input. In determining the specific services to which this prior authorization process would apply, we considered all available data and believe that comparing the utilization rate to the baseline growth rate is an appropriate method for identifying potentially unnecessary increases in volume. By identifying trends over the 11-year period for OPD services, we are able to contrast and compare specific services as targets for increases in volume versus our expectations. Moreover, in making our decision we did consider the impact of changes in the use of these items and available clinical information. Of note, we determined that the increased utilization of botulinum toxin injections was not solely attributable to the Food and Drug Administration's approval for the treatment of migraines. We conducted additional analysis of the additional botulinum toxin products suggested by the commenter and determined that these too had similar increases in volume. As noted in the preamble, our statistical analysis of the botulinum toxin injection codes originally proposed showed an overall average annual increase in the number of unique claims of approximately 19.3 percent from 2007 through 2017, an annual average increase in costs and payments of approximately 27.8 percent, and an average annual increase in the number of unique patients of approximately 17.9 percent. When adding these two additional codes to our statistical analyses, utilizing the same methodology, we have identified that the overall average annual increase in the number of unique claims is now approximately 19.4 percent from 2007 through 2017, the annual average increase in payments is now approximately 26.1 percent, and the average annual increase in the number of unique patients is approximately 18.0 percent. Moreover, although we did observe some increases of the original botulinum toxin codes after the 2010 FDA clearance for chronic migraines, we noted an average annual increase in claims volume of 16.6 percent for J0585, 23.6 percent for J0586, 12.2 percent for J0587, and 17.9 percent for J0588. These statistics are for the period 2010 through 2017 for all four codes except J0588, which only had data beginning 2012 (with data for interim years within the four codes reflecting increases as high as 65.9 percent). These sustained and persistent increases above expected volumes are not explained by the new FDA approval in 2010. So as not to create distortion in the marketplace and incentivize providers to administer those botulinum toxin therapeutic products that are not subject to prior authorization, as the commenter suggests, we are including the two additional botulinum toxin codes on the final list, since they also show similar unnecessary increases in volume.
We acknowledge that circumstances exist where a prior authorization could apply for a specific course of treatment for the botulinum toxin injection procedures, such as a number of treatments over a specific period of time, and will allow for such prior authorization requests.
We performed similar data analysis on vein treatments and saw several of the procedures had similar unnecessary increases in volume; however, these procedures account for a different approach in treatment for varicose veins than the vein ablation procedures we discussed in the proposed rule. Since these are procedures and not products, we do not have the same concern about marketplace distortion and are not adding them to the list at this time. We will continue to monitor these and other OPD procedures for unnecessary increases in volume and will propose additional procedures through rulemaking.
In sum, we are finalizing our proposed prior authorization policy as proposed, including our proposed regulation text, with the following modifications: We are adding additional language at § 419.83(c) regarding the notice of exemption or withdraw of an exemption. We are including in this process the two additional botulinum toxin injections codes, J0586 and J0588. See Table 64 below for the final list of outpatient department services requiring prior authorization.


4. Summary of the Public Comments and Responses to Comments on the Proposed Rule
The proposed rule, titled “Medicare Program; Proposed Changes to Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs; Price Transparency of Hospital Standard Charges; Proposed Revisions of Organ Procurement Organizations Conditions of Coverage; Proposed Prior Authorization Process and Requirements for Certain Covered Outpatient Department Services; Potential Changes to the Laboratory Date of Service Policy; Proposed Changes to Grandfathered Children's Hospitals-Within-Hospitals” (84 FR 39398 through 39644), hereinafter referred to as the “CY 2020 OPPS/ASC proposed rule,” was published in the Federal Register on August 6, 2019, with a comment period that ended on September 27, 2019. In that rule, for prior authorization, we received 96 public comments on our proposals, including comments from healthcare providers, professional and trade organizations, drug manufacturers, beneficiary advocacy organizations, and health care systems. The following is a summary of the comments we received and our responses.
Comment: We received several comments in support of prior authorization, with some adding they were “intrigued” by the promise prior authorization has in Fee-For-Service Medicare. Others commented that CMS is underestimating the amount of time and education providers will require in learning the new process. Some commenters suggested that CMS delay implementation of prior authorization beyond July 1, 2020, while others suggested that CMS proceed cautiously and roll out prior authorization on a limited basis and then scale nationally, similar to how the DMEPOS prior authorization process was implemented.
Response: We thank the commenters for their comments. We appreciate the positive responses to our proposed prior authorization process. In assessing the operational implementation schedule for prior authorization, we believe that the July 1, 2020 implementation date will reasonably allow enough time to educate and prepare stakeholders to be able to submit the necessary documentation for prior authorization for these services. No new documentation requirements are created as a result of this process. Instead, currently needed documents are submitted earlier in the process.
Comment: Some commenters questioned whether section 1833(t)(2)(F) of the Act grants CMS the authority to establish a prior authorization process and noted that when Congress intended to give CMS authority to implement a prior authorization process, it has done so explicitly. Still others suggested the development of the new process is “arbitrary and capricious” because the commenters believed that CMS has not demonstrated that increases in the volume of services for which we proposed to require prior authorization are unnecessary. Several commenters quoted a recent decision from the United States District Court for the District of Columbia,[173] in which the court invalidated the policy we adopted in the CY 2019 OPPS/ASC final rule with comment period to reduce payment for clinic visits furnished in excepted off-campus provider-based departments to a Physician Fee Schedule-equivalent amount as a method to control unnecessary increases in the volume of clinic visits furnished in these settings. In its decision the court stated with respect to this policy, which we also adopted under section 1833(t)(2)(F) of the Act, that “Congress did not intend CMS to use an untethered `method' to directly alter expenditures independent of other processes.” These commenters quoted the court as going on to state that, “. . . Congress directed any `methods' developed under paragraph (t)(2)(F) be implemented through other provisions of the statute.” The commenters contended that we cannot point to any other provision of the OPPS statute that would authorize a prior authorization requirement, which the commenters believed we must do following the court's decision. Still others compared CMS' attempts to establish a prior authorization process to the “functional equivalence” initiative that CMS previously undertook, which Congress later prohibited.
Response: We disagree with the commenters' contentions. We believe section 1833(t)(2)(F) of the Act gives us significant discretion to determine the appropriate methods to control unnecessary increases in the volume of covered OPD services. We believe that where, as here, we have determined that there have been unnecessary increases in services that are often cosmetic, section 1833(t)(2)(F) of the Act gives us authority to utilize prior authorization as a method to control those unnecessary increases. We carefully considered all available options in choosing to propose the prior authorization process, which has already been shown to be an effective tool in Fee-for-Service Medicare, and which we believe will be effective at controlling unnecessary increases for those procedures that are often cosmetic and for which we have identified unnecessary volume increases. We also believe that the description of our extensive data analysis in the CY 2020 OPPS/ASC proposed rule, comparing trends for the procedures discussed against 1.1 billion OPD claims over 11 years, demonstrated that there have been unnecessary increases for all services for which we proposed to require prior authorization and that there have not been other, legitimate reasons for the sustained increases.
We also disagree with the commenters who believe the District Court's decision in the clinic visit litigation decision forecloses our ability to adopt a method to control unnecessary increases in the volume of covered outpatient department services under section 1833(t)(2)(F) of the Act without tying that method to another provision of the OPPS statute. Rather, we believe that, unlike the clinic visit policy at issue in that decision, the prior authorization policy does not have an immediate impact on the amount of payment or the budget neutrality calculations for the OPPS, and therefore, we believe it is distinguishable from the clinic visit policy that the court invalidated and does not need to be adopted under separate authority in addition to section 1833(t)(2)(F) of the Act.
Comment: Several commenters questioned why ambulatory surgical centers (ASCs) and other provider types are exempt from this prior authorization process. The commenters believed the prior authorization process should not be implemented until CMS can also establish a prior authorization process for ASCs because they believe physicians will simply provide the affected services in ASCs instead of hospitals, thereby avoiding the OPPS prior authorization process altogether. Still others believed that physicians should be required to obtain prior authorization instead of hospitals, and that CMS should adopt regulations under the Physician Fee Schedule to require physicians to adhere to the documentation and related requirements for prior authorization.
Response: This prior authorization process is being adopted under section 1833(t)(2)(F) of the Act, which is specific to the OPPS, which provides payment only to hospital outpatient departments. As such, we cannot extend the process to ASCs or other healthcare provider types, including physicians outside of the outpatient department setting, because these entities are paid under other payment systems. We thank the commenters for noting the potential to shift these services to ASCs and will monitor these data and may consider additional program integrity oversight if such shifts are realized.
Comment: Several commenters suggested that prior authorization is not an effective method for controlling fraud and that other tools, such as CMS' development of National Coverage Decisions (NCDs) and Local Coverage Determinations (LCDs), prepayment and post-payment reviews, provider outreach and education, and law enforcement actions are more effective methods to control unnecessary increases in volume. In fact, some commenters suggested that we place providers on 100 percent pre-payment review in lieu of establishing the new prior authorization process. Others commented that prior authorization is nothing more than a “blunt instrument;” is contrary to some LCDs which clearly convey certain services are not covered; and that CMS needs to ensure coverage criteria are more easily identifiable and searchable so that hospitals can more readily comply with the requirements. One commenter questioned how to give input on establishing medical necessity and how medical necessity criteria will be set and another commenter specifically lauded CMS' not-yet-completed development of the documentation requirements look-up service (DRLS).
Response: We note that we have a variety of tools that can be used in making reasonable and necessary determinations. for several procedures on the list of outpatient department services requiring prior authorization. For other procedures that do not have specific LCDs or NCDs, contractors may make individual claim determinations to assess whether or not the services are reasonable and necessary, per section 1862(a)(1)(A) of the Act. This prior authorization process does not make any changes to current documentation requirements. While we recognize the utility of NCDs and LCDs and the importance of conducting of prepayment and post-payment reviews, we also believe that a broad program integrity strategy must use a variety of tools to best account for potential fraud, waste and abuse, including unnecessary increases in volume. Prior authorization has already proven to be an effective method for controlling improper payments and decreasing the volume of potentially improperly billed services for certain DMEPOS items. Thus, we believe that the use of prior authorization in the OPD context twill be an effective tool in controlling unnecessary increases in the volume of covered OPD services by ensuring that the correct payments are made for medically necessary OPD services, while also being consistent with our overall strategy of protecting the Medicare Trust Fund from improper payments, reducing the number of Medicare appeals, and improving provider compliance with Medicare program requirements. We will continue to work toward enhancing our overall program integrity strategy in meaningful ways. We also appreciate the positive input regarding the DRLS, and we agree that, once available, it will facilitate overall transparency in coverage requirements, which should benefit all parties.
Comment: Several commenters stated that prior authorization processes add burden, can result in unnecessary delays in care, and interfere with the physician-patient care decision or otherwise negatively affect patient care. Some commenters specifically mentioned problems associated with prior authorization processes within Medicare Advantage Plans while others conveyed that prior authorization is contrary to CMS' Patients Over Paperwork initiative.
Response: The process we are establishing specifically relates to Medicare FFS, not Medicare Advantage, and we have had demonstrated success in implementing prior authorization processes in the Medicare FFS for DMEPOS. As with our other prior authorization processes, we believe that the OPD prior authorization process for certain discrete, often cosmetic procedures can be implemented without the referenced delays in patient care. This is because we are establishing timeframes for contractors to render decisions on prior authorization requests as well as an expedited review process when the regular review timeframe could seriously jeopardize the beneficiary's health that we believe will enable hospitals to receive timely provisional affirmations. Additionally, we note that our prior authorization policy does not create any new documentation or administrative requirements. Instead, it will just require the same documents that are currently required to be submitted earlier in the process. Resources should not need to be diverted from patient care. We note that prior authorization has the added benefit of giving hospitals some assurance of payment for services for which they received a provisional affirmation. In addition, beneficiaries will have information regarding coverage prior to receiving the service, and will benefit by knowing in advance of receiving a service if they will incur financial liability for non-covered services. We believe that some assurance of payment and some protection from future audits will ultimately reduce burdens associated with denied claims and appeals.
Comment: We received comments with general questions regarding the proposed process such as who will be responsible for obtaining the prior authorization, that is, the physician or the hospital, and whether all related claims will be denied if prior authorization is not obtained. Some commenters expressed concern that physicians could be denied payment for services rendered if a hospital fails to submit a prior authorization request or fails to notify the physician of a denial.
Response: As noted above, this prior authorization process is being adopted under section 1833(t)(2)(F) of the Act, which is specific to OPD services, which provides payment only to hospital outpatient departments. In light of the different arrangements that could exist with physicians in different hospitals, we determined that enabling either the physician or the hospital to submit the prior authorization on behalf of the hospital outpatient department was the best approach. Physicians and the hospitals are in the best position to account for the various relationships and obligations that exist and should account for the prior authorization process. Part of that process should be communication of prior authorization decisions between entities, as a unique tracking number (UTN) corresponding to the prior authorization decision must be included on the OPD claim for these services. Consistent with all Medicare Fee-for-Service prior authorization and pre-claim review processes, when a prior authorization request is submitted, the request will be assigned a UTN. The UTN must be included on any claim submitted for the services listed, which will be used to verify compliance with the prior authorization process.
Additionally, we stated that any claims associated with or related to a service that requires prior authorization for which a claim denial is issued would also be denied. These associated services include, but are not limited to, services such as anesthesiology services, physician services, and/or facility services. Consistent with current medical review and claims processing guidance (for example, Program Integrity Manual (internet Only Manuals, Pub. L. 100-08 chapter 3, section 3.2.3 et sec and chapter 7, section 7.2.2.2), and in accordance with new § 419.82(b)(3), these related claims would be denied as well if the service listed in § 419.83(a)(1) had also been denied. If the prior authorization is not submitted by the hospital and the physician submits a claim for the service, it cannot be processed as an OPD service as this program requires prior authorization of the OPD service as a condition of payment.
Comment: Some commenters expressed concern that even when a provisional affirmation is obtained, the claim could ultimately be denied and that the requirement should be changed so that no claim could be denied for which a provisional affirmation was obtained. Still others asked for clarification regarding whether all claims would be denied in situations where a provisional affirmation was received but the corresponding claim was later denied. Others expressed concern that no appeal rights exist for those instances where a non-affirmation is received and that CMS should determine the cost of care to beneficiaries who are negatively impacted by the receipt of a non-affirmation or who have care denied.
Response: Having a provisional affirmation shows that a claim likely meets Medicare's coverage and payment rules and is likely to be paid. Absent evidence of fraud or gaming, a provider can anticipate payment as long as other payment requirements are met. We anticipate that most, if not all, claims for which a provision affirmation is obtained would not be denied on the basis of medical necessity. However, it is possible the claim could be denied because it did not meet a coding or billing requirement (examples include, but are not limited to, when there are duplicate claims submitted, when some element of the claim form is incorrectly completed, or if a modifier is placed on a claim that prevents it from processing appropriately). In addition, The Improper Payments Elimination and Recovery Improvement Act of 2012 (IPERIA) (Pub. L. 112-248), requires all federal agencies to evaluate their programs for improper payments. The CMS Comprehensive Error Rate Testing (CERT) program reviews a stratified, random sample of claims annually to identify and measure improper payments. It is possible for a claim subject to prior authorization to fall within the sample. In this situation, the subject claim would not be protected from the CERT audit. In addition, the Office of Inspector General's (OIG) authority to audit claims is not impacted by the protection from future audits provided by the provisional affirmation prior authorization decision.
While we appreciate that there is concern over the lack of appeal rights for non-affirmations, we note that providers are not limited in the number of times they can resubmit requests that were previously non-affirmed, and that appeal rights still exist once a claim is actually denied. Lastly, with regard to the impact on care for those beneficiaries for which hospitals receive non-affirmations, we note that we specifically chose services that are often cosmetic and believe that it is appropriate to deny such services in the case of a non-affirmation, because a non-affirmation would indicate that Medicare's coverage, coding, and/or payment rules for the service are not being met. Consistent with current Medicare Fee-for-Service prior authorization and pre-claim review processes, the provider will receive a detailed explanation as to why the request was non-affirmed and will be afforded an unlimited number of request resubmissions. Our experience in our other prior authorization and pre-claim review processes has been that approximately 95 percent of submissions are affirmed within two requests, and that the impact of non-affirmation decisions has been minimal for necessary, covered services.
Comment: Some commenters recommended that CMS decrease the ten business day time frame for issuing provisional affirmations and non-affirmations, because the commenters believed there could be occasions where the decision ultimately takes 15 days in light of weekends and holidays being excluded from the ten business day calculation. Still others commented that providers should be exempt from having to complete the prior authorization process in emergency situations or that retroactive provisional affirmations should be issued in these circumstances; the expedited review process should be completed within 24 hours if urgent circumstances exist; and the need to submit a request for an expedited review be eliminated and instead the judgment of the physician should suffice in triggering the expedited processing time frame.
Response: We appreciate the comments in response to our proposed process. While we recognize the desire to obtain provisional affirmations as quickly as possible, given that these are services are typically cosmetic and would be provided in the outpatient hospital department setting, we believe the identified time frames adequately balance program integrity, provider burden, and beneficiary concerns. In those circumstances where approval is needed more expeditiously, an expedited request can be requested and if granted, will result in a in a provisional affirmation or non-affirmation being issued within two business days of the expedited request, which we believe is sufficient where expedition is necessary. With respect to clinical judgement, the prior authorization process does not remove or alter the clinical judgement process in any way. We are only requesting currently required documentation earlier in the process. Physicians remain fully capable and responsible to support the reasonableness and necessity of the proposed services.
Comment: One commenter suggested that certain provisions, including the exemption rate and the notice of exemption and/or withdrawal of an exemption, should be explicitly accounted for within the regulations located in Part 419. Still other commenters suggested that CMS determine the rate of compliance with the coverage requirements prior to the implementation of this prior authorization process so that certain providers could begin the new process with an exemption in place for attaining or exceeding the requisite 90 percent compliance rate. Alternatively, one commenter suggested that CMS use existing data to identify egregious providers to reduce burden on historically compliant providers. Finally, one commenter suggested exempting providers from prior authorization if the providers participate in standardized data collection and are willing to share their data.
Response: We thank the commenters for these suggestions. We believe we have accounted for the exemption rate in the preamble and intend to maintain the 90 percent rate. With regard to the notice of exemption and/or withdrawal of an exemption, we agree that the regulations should account for this process in more detail. We had initially stated in the CY 2020 OPPS/ASC proposed rule (84 FR 39606) that we anticipate that an exemption will take approximately 90 calendar days to effectuate. In the interest of helping ensure providers incur the least burden possible, we have offered to formalize the ability to notify providers before our anticipated 90-day period (that is, at least 60 days) if and when possible. As such, we have revised § 419.83(c) to redesignate the last sentence of proposed paragraph (c)—“An exemption will remain in effect until CMS elects to withdraw the exemption”—as new subparagraph (1). We are adding a new provision at new paragraph (c)(2), which will account for the notice of an exemption or withdrawal of an exemption being delivered at least 60 calendar days prior to the implementation date. Because we are unable to determine a compliance or non-compliance rate prior to the initiation of the process because most claims have not undergone full medical review and were likely paid or denied based upon the completeness of the elements on the face of the claim, we cannot exempt certain providers or only require prior authorization for certain providers in advance of implementing the new process. Lastly, we do not believe it is sufficient to exempt providers who provide data. Through the prior authorization process, we are best able to identify problems before they occur and control for unnecessary increases in the volume of these procedures, while ensuring that beneficiaries receive medically necessary services.
Comment: Some commenters suggested that MACs do not have the clinical review capabilities to sufficiently handle prior authorization requests and suggested that CMS require specific credentials of the MAC medical reviewers, to ensure the accuracy of MAC decisions. Still other commenters related several principles of prior authorization with which they believed we should comply as we implement the new prior authorization process. These principles include selective application of prior authorization to only “outliers,” review/adjustment of prior authorization lists to remove services/drugs that represent low-value prior authorization; transparency of prior authorization requirements and their clinical basis to patients and physicians; protections of patient continuity of care; and automation to improve prior authorization and process efficiency.
Response: In all Medicare Fee-for-Service medical review programs we require that MACs utilize clinicians, specifically, registered nurses, when reviewing medical documentation. We also require the oversight of a Medical Director and additional clinician engagement if necessary. We are confident that MACs have the requisite expertise to effectively administer the prior authorization process, and we maintain a robust oversight process to ensure the accuracy and consistency of their review decisions. Further, we believe the prior authorization process we are adopting aligns with the principles outlined by the commenters. Of note, we have included a process to exempt providers who consistently demonstrate compliance with Medicare rules through this prior authorization process. We also are focusing initially on procedures that are not urgent and likely cosmetic and of high value, and we have included an expedited process if circumstances warrant. Along with our contractors, we will continue to analyze the value of the services that we target for prior authorization to be sure that services are selected that are appropriate for this process. As the process matures and CMS implements new technologies, such as the DRLS or other industry standards, we will effectuate improvements to the prior authorization process and coverage requirements.
Comment: Some commenters asked for clarification regarding how CMS would carry out certain provisions of the CY 2020 OPPS/ASC proposed rule, such as establishing standardized prior authorization protocols, including timely resolution of clinical reviews and clearly articulated decision criteria and rationale in an effort to minimize case delays and encourage effective communication changes between providers and health plans. Other commenters requested that CMS adopt a required response period for initial and repeat prior authorization requests, noted CMS' lack of experience in using prior authorization in Medicare Fee-For-Service, and referenced a lack of administrative structure and guidelines as well as the need for a well-functioning portal through which prior authorization requests could be submitted.
Response: In developing this prior authorization process, we indicated that we were building upon our already established prior authorization program established for certain DMEPOS under 42 CFR 414.234, and included more detailed requirements, such as decision timeframes for both regular and expedited reviews, as well as the percentages needed to demonstrate continued compliance with Medicare coverage, coding and payment rules in order to be exempt from the prior authorization process. We have considerable experience in light of the DMEPOS prior authorization program and are leveraging this experience accordingly. As we indicated in our prior responses, we are making additional changes, including adding specific regulatory provisions, to ensure the program's administrative requirements are clear. Once finalized, CMS and our contractors will provide additional educational and outreach materials to all stakeholders.
Comments: Some commenters requested changes that are out of the scope of this rule related to Medicare Advantage plans.
Response: This prior authorization policy is specific to Medicare FFS, so we are not able to respond to comments that raise concerns regarding Medicare Advantage prior authorization programs.
Comments: One commenter pointed out that we had used U.S. Bureau of Labor and Statistics data when attempting to compare overall health care costs against the OPD payments trending data when other spending data may be more appropriate.
Response: We thank this commenter and have evaluated U.S. Bureau of Economic Analysis (BEA) data, which we agree may be more appropriate. We had compared the 8.2 percent average annual increase for OPD services over the 11-year period of 2007 through 2017 to the 5.8 percent average annual spending calculated from the Bureau of Labor and Statistics data; however, after consulting with both bureaus, the BEA data better aligns with our analytic process, which reflected a 2.3 percent average annual increase per year in overall health care spending using data publicly available on the BEA web page, located at: https://apps.bea.gov/iTable/iTable.cfm?reqid=51&step=2&isuri=1https.
Comment: We received comments that the growth in utilization of a procedure/product class exceeding the baseline growth rates in the Medicare population is not a sufficient basis for inferring that utilization is inappropriate or that utilization growth is unwarranted and that CMS should analyze readily available clinical information that would explain changes in utilization before the agency adopts broad-based interventions such as imposing prior authorization on outpatient hospitals. The same commenter suggested that the increases seen in CPT codes 64612 and 64615 are likely due to other factors such as FDA's approval of BOTOX in 2010, increased support for BOTOX as a migraine treatment, and the addition of chronic migraine to the list of covered indications for BOTOX in Medicare contractor LCDs. This commenter also recommended that if CMS chooses to move forward with implementing this prior authorization process that CMS expand the prior authorization requirements to apply to all four FDA-approved botulinum toxin therapeutic products to include DYSPORT® (J0586) and XEOMIN® (J0588) in addition to BOTOX and MYOBLOC so as not to create distortion in the marketplace and incentivize providers to administer those botulinum toxin therapeutic products that are not subject to prior authorization. One commenter also expressed concern that the prior authorization process could impact women and veterans more significantly than other categories because these groups tend to experience migraines at higher rates than other categories and this could ultimately lead to an increase in opioid abuse within these groups. We received several comments asking whether a provisional affirmation for botulinum toxin injections would be per injection or for a specific course of treatment over a period of time, such as twelve months. We also received comments to add codes to the list for alternative treatment options for varicose veins, such as phlebectomy and sclerotherapy.
Response: We thank the commenters for their input. In determining the specific services to which this prior authorization process would apply, we considered all available data and believe that comparing the utilization rate to the baseline growth rate is an appropriate method for identifying potentially unnecessary increases in volume. By identifying trends over the 11-year period for OPD services, we are able to contrast and compare specific services as targets for increases in volume versus our expectations. Moreover, in making our decision we did consider the impact of changes in the use of these items and available clinical information. Of note, we determined that the increased utilization of botulinum toxin injections was not solely attributable to the Food and Drug Administration's approval for the treatment of migraines. We conducted additional analysis of the additional botulinum toxin injections and determined that these too had similar increases in volume and are including the two additional botulinum toxin codes on the final list. We acknowledge that circumstances exist where a prior authorization could apply for a specific course of treatment for the botulinum toxin injection procedures, such as a number of treatments over a specific period of time, and will allow for such prior authorization requests.
We performed similar data analysis on vein treatments and saw several of the procedures had similar unnecessary increases in volume; however, these procedures account for a different approach in treatment for varicose veins than vein ablation procedures. Since these are procedures and not products, we do not have the same concern about marketplace distortion and are not adding them to the list at this time. We will continue to monitor these and other OPD procedures for unnecessary increases in volume and will propose additional procedures through rulemaking.
In sum, we are finalizing our proposed prior authorization policy as proposed, including our proposed regulation text, with the following modifications: We are adding additional language at § 419.83(c) regarding the notice of exemption or withdraw of an exemption. We are including in this process the two additional botulinum toxin injections codes, J0586 and J0588. See Table 65 below for the final list of outpatient department services requiring prior authorization. Further, we had offered examples from our statistical analysis of the botulinum toxin injection in the preamble that explained that we had seen an overall average annual increase in the number of unique claims of approximately 19.3 percent from 2007 through 2017, an annual average increase in costs and payments of approximately 27.8 percent, and an average annual increase in the number of unique patients of approximately 17.9 percent. When adding these two additional codes to our statistical analyses, utilizing the same methodology, we have identified that the overall average annual increase in the number of unique claims is now approximately 19.4 percent from 2007 through 2017, the annual average increase in payments is now approximately 26.1 percent, and the average annual increase in the number of unique patients of approximately 18.0 percent. Moreover, although we did observe some increases of the original botulinum toxin codes after the 2010 FDA clearance for chronic migraines, we noted an average annual increase in claims volume of 16.6 percent for J0585, 23.6 percent for J0586, 12.2 percent for J0587, and 17.9 percent for J0588. These statistics are for the period 2010 through 2017 for all four codes except J0588, which only had data beginning 2012 (with data for interim years within the four codes reflecting increases as high as 65.9 percent). These sustained and persistent increases above expected volumes are not explained by the new FDA approval in 2010, which is why these codes, coupled with the specific procedures, have been included in this program.


XX. Comments Received in Response to Comment Solicitation on Cost Reporting, Maintenance of Hospital Chargemasters, and Related Medicare Payment Issues
In the CY 2020 OPPS/ASC proposed rule (84 FR 39609), we included a Request for Information (RFI) related to the relationship of hospital chargemasters to the Medicare cost report and its use in setting Medicare payment for hospital services. We received approximately 46 timely pieces of correspondence on this RFI. We appreciate the input provided by commenters.
XXI. Changes to Requirements for Grandfathered Children's Hospitals-Within-Hospitals (HwHs)
Existing regulations at § 412.22(e) define a hospital-within-a-hospital (HwH) as a hospital that occupies space in the same building as another hospital, or in one or more entire buildings located on the same campus as buildings used by another hospital. Existing § 412.22(f) provides for the grandfathering of HwHs that were in existence on or before September 30, 1995, so long as the HwH continues to operate under the same terms and conditions, including the number of beds. Sections 412.22(h) and 412.25(e), relating to satellites of hospitals and hospital units, respectively, excluded from the IPPS, define a satellite facility as a part of a hospital or unit that provides inpatient services in a building also used by another hospital, or in one or more entire buildings located on the same campus as buildings used by another hospital. Sections 412.22(h)(3) and 412.25(e)(3) provide for the grandfathering of excluded hospitals and units that were structured as satellite facilities on September 30, 1999, to the extent that they operate under the same terms and conditions in effect on that date. While these rules initially only applied to LTCHs, in 1997, CMS expanded the scope of these rules to all hospitals excluded from the IPPS (including children's hospitals) because the underlying policy concern of hospitals creating new entities that were separate in name only (essentially operating as units of the hospital) in order to increase Medicare revenue was not unique to LTCHs. For example, we have expressed our concerns that an HwH's “configuration could result in patient admission, treatment, and discharge patterns that are guided more by attempts to maximize Medicare payments than by patient welfare” and that “the unregulated linking of an IPPS hospital and a hospital excluded from the IPPS could lead to two Medicare payments for what was essentially one episode of patient care” (69 FR 48916 and 49191). HwHs which are grandfathered are not required to comply with the separateness and control requirements applicable to other HwHs.
In the FY 2018 IPPS/LTCH PPS final rule (82 FR 38292 through 38294), we finalized a change to our HwH regulations at § 412.22(e) to only require, as of October 1, 2017, that IPPS-excluded HwHs that are co-located with IPPS hospitals comply with the separateness and control requirements in those regulations. We adopted this change because we believe that the policy concerns that underlay the previous HwH regulations are sufficiently moderated in situations where IPPS-excluded hospitals are co-located with each other, in large part due to changes that have been made to the way most types of IPPS-excluded hospitals are paid under Medicare. (We note that non-grandfathered HwHs, whether children's hospitals or not, which are co-located with IPPS hospitals must comply with separateness and control requirements. For more information we refer readers to the FY 2018 IPPS/LTCH PPS final rule (82 FR 38292 through 38294)). As part of our ongoing efforts to reduce regulatory burdens, we have continued to examine areas in which the rules for co-located entities are no longer necessary. As a result of this examination, we believe that there is no Medicare payment policy rationale for prohibiting grandfathered children's HwHs from increasing their number of beds. Given the low number of Medicare claims submitted by these children's hospitals, which results in a minimal level of Medicare payment to them relative to the payments they receive from other payers, we believe that such a regulatory change would allow these hospitals to address changing community needs for services without any increased incentive for inappropriate patient shifting to maximize Medicare payments. Additionally, we do not believe that allowing grandfathered children's HwHs to increase their bed size would impart an economic advantage to these hospitals relative to other hospitals. However, in the CY 2020 OPPS/ASC proposed rule, we proposed to revise § 412.22(f)(1) and (2) to allow a grandfathered children's HwH to increase its number of beds without resulting in the loss of grandfathered status. Additionally, we solicited comments on whether the proposal could create unintended or inadvertent consequences.
Comment: We received several comments on our proposal, all of which supported it. Some commenters also agreed with our assessment that allowing grandfathered children's HwHs to increase their beds would not impart an economic advantage to these hospitals.
Response: We thank commenters for their support.
In light of the comments received, we are finalizing our proposal without modification.
XXII. Notice of Closure of Two Teaching Hospitals and Opportunity To Apply for Available Slots
a. Background
Section 5506 of the Affordable Care Act (Pub. L. 111-148) added subsection (vi) to section 1886(h)(4)(H) of the Act and modified language at section 1886(d)(5)(B)(v) of the Act, to instruct the Secretary to establish a process to redistribute residency slots after a hospital that trained residents in an approved medical residency program closes. Specifically, the Secretary is instructed to increase the full-time equivalent (FTE) resident caps for teaching hospitals based upon the FTE resident caps in teaching hospitals that closed “on or after a date that is 2 years before the date of enactment” (that is, March 23, 2008). In the CY 2011 OPPS final rule with comment period (75 FR 72212), we established regulations at 42 CFR 413.79(o) and an application process for qualifying hospitals to apply to CMS to receive direct graduate medical education (DGME) and indirect medical education (IME) FTE resident cap slots from the hospital that closed. We made certain modifications to those regulations in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53434), and we made changes to the section 5506 application process in the FY 2015 IPPS/LTCH PPS final rule (79 FR 50122 through 50134). The procedures we established apply both to teaching hospitals that closed on or after March 23, 2008, and on or before August 3, 2010, and to teaching hospitals that close after August 3, 2010.
b. Notice of Closure of Hahnemann University Hospital, Located in Philadelphia, PA, and the Application Process—Round 16
CMS has learned of the closure of Hahnemann University Hospital, located in Philadelphia, PA (CCN 390290). Accordingly, this notice serves to notify the public of the closure of this teaching hospital and initiate another round of the section 5506 application and selection process. This round will be the 16th round (“Round 16”) of the application and selection process. Table 66 below contains the identifying information and IME and DGME FTE resident caps for the closed teaching hospital, which are part of the Round 16 application process under section 5506 of the Affordable Care Act.

c. Notice of Closure of Ohio Valley Medical Center, Located in Wheeling, WV, and the Application Process—Round 17
CMS has learned of the closure of Ohio Valley Medical Center, located in Wheeling, WV (CCN 510039). Accordingly, this notice serves to notify the public of the closure of this teaching hospital and initiate another round of the section 5506 application and selection process. This round will be the 17th round (“Round 17”) of the application and selection process. Table 67 below contains the identifying information and IME and DGME FTE resident caps for the closed teaching hospital, which are part of the Round 17 application process under section 5506 of the Affordable Care Act.

d. Application Process for Available Resident Slots
The application period for hospitals to apply for slots under section 5506 of the Affordable Care Act is 90 days following notice to the public of a hospital closure (77 FR 53436). Therefore, hospitals that wish to apply for and receive slots from the above hospitals' FTE resident caps, must submit applications (Section 5506 Application Form posted on Direct Graduate Medical Education (DGME) website as noted at the end of this section) directly to the CMS Central Office no later than January 30, 2020. The mailing address for the CMS Central Office is included on the application form. Applications must be received by the CMS Central Office by the January 30, 2020 deadline date. It is not sufficient for applications to be postmarked by this date.
After an applying hospital sends a hard copy of a section 5506 slot application to the CMS Central Office mailing address, the hospital is encouraged to notify the CMS Central Office of the mailed application by sending an email to: ACA5506application@cms.hhs.gov. In the email, the hospital should state: “On behalf of [insert hospital name and Medicare CCN#], I, [insert your name], am sending this email to notify CMS that I have mailed to CMS a hard copy of a section 5506 application under Round [16 or 17] due to the closure of [Hahnemann University Hospital or Ohio Valley Medical Center]. If you have any questions, please contact me at [insert phone number] or [insert your email address].” An applying hospital should not attach an electronic copy of the application to the email. The email will only serve to notify the CMS Central Office to expect a hard copy application that is being mailed to the CMS Central Office.
We have not established a deadline by when CMS will issue the final determinations to hospitals that receive slots under section 5506 of the Affordable Care Act. However, we review all applications received by the deadline and notify applicants of our determinations as soon as possible.
We refer readers to the CMS Direct Graduate Medical Education (DGME) website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/DGME.html to download a copy of the section 5506 application form (Section 5506 Application Form) that hospitals must use to apply for slots under section 5506 of the Affordable Care Act. Hospitals should also access this same website for a list of additional section 5506 guidelines for the policy and procedures for applying for slots, and the redistribution of the slots under sections 1886(h)(4)(H)(vi) and 1886(d)(5)(B)(v) of the Act
XXIII. Files Available to the Public via the Internet
The Addenda to the OPPS/ASC proposed rules and the final rules with comment period are published and available via the internet on the CMS website. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59154), for CY 2019, we changed the format of the OPPS Addenda A, B, and C, by adding a column entitled “Copayment Capped at the Inpatient Deductible of $1,364.00” where we flag, through use of an asterisk, those items and services with a copayment that is equal to or greater than the inpatient hospital deductible amount for any given year (the copayment amount for a procedure performed in a year cannot exceed the amount of the inpatient hospital deductible established under section 1813(b) of the Act for that year). For CY 2020, we are retaining these columns, updated to reflect the amount of the 2020 inpatient deductible.
To view the Addenda to this final rule with comment period pertaining to CY 2020 payments under the OPPS, we refer readers to the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices.html; select “1717-FC” from the list of regulations. All OPPS Addenda to this final rule with comment period are contained in the zipped folder entitled “2020 NFRM OPPS Addenda” at the bottom of the page. To view the Addenda to this final rule with comment period pertaining to CY 2020 payments under the ASC payment system, we refer readers to the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/ASC-Regulations-and-Notices.html; select “1717-FC” from the list of regulations. All ASC Addenda to this final rule with comment period are contained in a zipped folder entitled “Addendum AA, BB, DD1, DD2, and EE.”
XXV. Collection of Information Requirements
A. Statutory Requirement for Solicitation of Comments
Under the Paperwork Reduction Act of 1995, we are required to provide 60-day notice in the Federal Register and solicit public comment before a collection of information requirement is submitted to the Office of Management and Budget (OMB) for review and approval. In order to fairly evaluate whether an information collection should be approved by OMB, section 3506(c)(2)(A) of the Paperwork Reduction Act of 1995 requires that we solicit comment on the following issues:
- The need for the information collection and its usefulness in carrying out the proper functions of our agency.
- The accuracy of our estimate of the information collection burden.
- The quality, utility, and clarity of the information to be collected.
- Recommendations to minimize the information collection burden on the affected public, including automated collection techniques.
In the final rule with comment period, we are soliciting public comment on each of these issues for the following sections of this document that contain information collection requirements (ICRs).
B. ICRs for the Hospital OQR Program
1. Background
The Hospital OQR Program is generally aligned with the CMS quality reporting program for hospital inpatient services known as the Hospital IQR Program. We refer readers to the CY 2011 through CY 2019 OPPS/ASC final rules with comment periods (75 FR 72111 through 72114; 76 FR 74549 through 74554; 77 FR 68527 through 68532; 78 FR 75170 through 75172; 79 FR 67012 through 67015; 80 FR 70580 through 70582; 81 FR 79862 through 79863; 82 FR 59476 through 59479; and 83 FR 59155 through 59156, respectively) for detailed discussions of Hospital OQR Program information collection requirements we have previously finalized. The information collection requirements associated with the Hospital OQR Program are currently approved under OMB control number 0938-1109 which expires on March 31, 2021. Below we discuss only the changes in burden that will result from the finalized policies in this final rule with comment period.
In section XIV.B.3.b. of this final rule with comment period, we are finalizing our proposal with modification to remove one measure from the Hospital OQR Program for the CY 2022 payment determination; OP-33: External Beam Radiotherapy for Bone Metastases. The reduction in burden associated with this measure removal is discussed below.
In the CY 2018 OPPS/ASC final rule with comment period (82 FR 59477), we finalized a proposal to utilize the median hourly wage rate, in accordance with the Bureau of Labor Statistics (BLS), to calculate our burden estimates for the Hospital OQR Program. The BLS describes Medical Records and Health Information Technicians as those responsible for organizing and managing health information data; therefore, we believe it is reasonable to assume that these individuals will be tasked with abstracting clinical data for submission for the Hospital OQR Program. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59156), we utilized a median hourly wage of $18.29 per hour. Since then, more recent wage data have become available and we are updating the wage rate used in these calculations. The latest data (May 2018) from the BLS reflects a median hourly wage of $19.40 [174] per hour for a Medical Records and Health Information Technician professional. We have finalized a policy to calculate the cost of overhead, including fringe benefits, at 100 percent of the mean hourly wage (82 FR 59477). This is necessarily a rough adjustment, both because fringe benefits and overhead costs vary significantly from employer-to-employer and because methods of estimating these costs vary widely from study-to-study. Nonetheless, we believe that doubling the hourly wage rate ($19.40 × 2 = $38.80) to estimate total cost is a reasonably accurate estimation method and allows for a conservative estimate of hourly costs. This approach is consistent with our previously finalized burden calculation methodology (82 FR 59477). Accordingly, we calculate cost burden to facilities using a wage plus benefits estimate of $38.80 per hour throughout the discussion below for the Hospital OQR Program.
2. Finalized Removal of OP-33 for the CY 2022 Payment Determination and Subsequent Years
In section XIV.B.3.b. of this final rule with comment period, we are finalizing our proposal with modification to remove one measure submitted via a web-based tool beginning with the CY 2022 payment determination and for subsequent years: OP-33: External Beam Radiotherapy for Bone Metastases. In the CY 2020 OPPS/ASC proposed rule, we inadvertently stated that we were proposing to remove this measure beginning with October 2020 encounters for CY 2022 payment determination and subsequent years (84 FR 39554 through 39556). As discussed in section XXVI.B.2. of this final rule with comment period, we intended to remove this measure beginning with the CY 2022 payment determination and subsequent years, but starting with January 2020 encounters, not October.
Because we are finalizing removal of this measure beginning with the same CY 2022 payment determination, as was proposed, the estimated effects remain the same as discussed in the proposed rule. As we stated in the CY 2016 OPPS/ASC final rule with comment period (80 FR 70582), we estimate that hospitals spend approximately 10 minutes, or 0.167 hours, per measure to report web-based measures. Accordingly, we believe that the removal of OP-33 for the CY 2022 payment determination will reduce burden by 0.167 hours per hospital, resulting in a burden reduction of 551 hours (0.167 hours × 3,300 hospitals) and $21,379 (551 hours × $38.80) across 3,300 hospitals.
C. ICRs for the ASCQR Program
1. Background
We refer readers to the CY 2012 OPPS/ASC final rule with comment period (76 FR 74554), the FY 2013 IPPS/LTCH PPS final rule (77 FR 53672), and the CY 2013, CY 2014, CY 2015, CY 2016, CY 2017, CY 2018, and CY 2019 OPPS/ASC final rules with comment period (77 FR 68532 through 68533; 78 FR 75172 through 75174; 79 FR 67015 through 67016; 80 FR 70582 through 70584; 81 FR 79863 through 79865; 82 FR 59479 through 59481; and 83 FR 59156 through 59157, respectively) for detailed discussions of the ASCQR Program information collection requirements we have previously finalized. The information collection requirements associated with the ASCQR Program are currently approved under OMB control number 0938-1270 which expires on January 31, 2022. As discussed below, there are only nominal changes in burden that will result from the finalized policies in this final rule with comment period.
2. Adoption of ASC-19: Facility-Level 7-Day Hospital Visits After General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357)
In section XV.B.3. of this this final rule with comment period, we are finalizing our proposal, beginning with the CY 2024 payment determination and for subsequent years, to adopt one measure collected via Medicare claims: ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357). Data used to calculate scores for this measure are collected via Medicare Part A and Part B administrative claims and Medicare enrollment data; therefore, ASCs will not be required to report any additional data. Because this measure does not require ASCs to submit any additional data, we believe there will be only a nominal change in other costs experienced by ASCs associated with this measure adoption due to having to review and track confidential feedback and reports related to the finalized ASC-19 measure.
D. ICRs for Revision of the Definition of “Expected Donation Rate” for Organ Procurement Organizations
We are finalizing our proposal to revise the definition of “expected donation rate” in the OPO CfCs. This change would allow OPOs to receive payment for organ donor costs under the Medicare and Medicaid programs using a definition that is consistent with the definition used by the Scientific Registry of Transplant Recipients (SRTR). Because we will be using data from the OPTN and the SRTR in assessing whether OPOs have satisfied the outcome measures of 42 CFR 486.318(b), we are adopting the definition currently used by the OPTN and SRTR in their statistical evaluation of OPO performance. This revision would not change the data that are already collected by the OPTN and SRTR, and therefore it will not affect the information collection burden on OPOs.
E. ICR for Prior Authorization Process and Requirements for Certain Hospital Outpatient Department (OPD) Services
In section XX. of the proposed rule, we proposed to establish a prior authorization process for certain hospital outpatient services as a condition for Medicare payment. We proposed to use our authority under section 1833(t)(2)(F) of the Act, which authorizes CMS to develop a method for controlling unnecessary increases in the volume of covered OPD services, to establish the prior authorization process. We believe a prior authorization process for OPD services will ensure beneficiaries receive medically necessary care while minimizing the risk of improper payments without changing the documentation requirements for providers and, therefore, will protect the Medicare Trust fund.
We proposed that providers would be required to obtain prior authorization from CMS for five groups of services and their related services before the services are provided to Medicare beneficiaries and before the provider could submit claims for payment under Medicare for these services. The five groups of services proposed are: Blepharoplasty, Botulinum Toxin Injections, Panniculectomy, Rhinoplasty, and Vein Ablation. The ICRs associated with prior authorization requests for these covered outpatient department services would be the required documentation submitted by providers. We proposed that a prior authorization request must include all relevant documentation necessary to show that the service meets applicable Medicare coverage, coding, and payment rules and that the request be submitted before the service is provided to the beneficiary and before the claim is submitted for processing. The burden associated with this finalized process is the time and effort necessary for the submitter to locate and obtain the relevant supporting documentation to show that the service meets applicable coverage, coding, and payment rules, and to forward the information to CMS or its contractor (MAC) for review and determination of a provisional affirmation. We expect that this information will generally be maintained by providers within the normal course of business and that this information will be readily available. We estimate that the average time for office clerical activities associated with this task will be 30 minutes, which is equivalent to that for normal prepayment or post payment medical review. We anticipate that most prior authorization requests would be sent by means other than mail. However, we estimate a cost of $5 per request for mailing medical records. Due to a July start date, the first year of the prior authorization will only include 6 months. Based on calendar year (CY) 2018 data, we estimate that for those first 6 months at a minimum there will be 15,191 initial requests mailed during that timeframe. In addition, we estimate there will be 4,987 resubmissions of a request mailed following a non-affirmed decision. Therefore, the total mailing cost is estimated to be $100,890 (20,178 mailed requests × $5). Based on CY 2018 data, we estimate that annually at a minimum there will be 30,381 initial requests mailed during a year. In addition, we estimate there will be 9,971 resubmissions of a request mailed following a non-affirmed decision. Therefore, the total mailing cost is estimated to be $201,762 (40,352 mailed requests × $5). We also estimate that an additional 3 hours would be required for attending educational meetings and reviewing training documents. While there may be an associated burden on beneficiaries while they wait for the prior authorization decision, we are unable to quantify that burden.
The average labor costs (including 100 percent fringe benefits) used to estimate the costs were calculated using data available from the BLS. Based on the BLS information, we estimate an average hourly rate of $16.63 with a loaded rate of $33.26. The prior authorization program does not create any new documentation or administrative requirements. Instead, it just requires the currently required documents to be submitted earlier in the claim process. Therefore, the estimate uses the clerical rate as we do not believe that clinical staff would need to spend more time on completing the documentation than would be needed in the absence of the demonstration. The hourly rate reflects the time needed for the additional clerical work of submitting the prior authorization request itself. Therefore, we estimate that the total burden for the first year (6 months), allotted across all providers, would be 50,826 hours (.5 hours × 67,260, submissions plus 3 hours × 5,732 providers for education). The burden cost for the first year (6 months) is $1,791,363 (50,826 hours × $33.26 plus $100,890 for mailing costs). In addition, we estimate that the total annual burden hours, allotted across all providers, would be 84,450 hours (.5 hours × 134,508 submissions plus 3 hours × 5,732 providers for education). The annual burden cost would be $3,010,569 (84,450 hours × $33.26 plus $201,762 for mailing costs). For the total burden and associated costs, we estimate the annualized burden to be 73,242 hours and $2,604,167 million. The annualized burden is based on an average of 3 years, that is, 1 year at the 6-month burden and 2 years at the 12-month burden. The information collection request is under development and will be submitted to OMB for approval.
F. Revision to Laboratory Date of Service (DOS) Policy
In section XIX. of this final rule with comment period, we discuss our comment solicitation regarding potential revisions to the laboratory date of service (DOS) provisions at § 414.510(b)(5) for a molecular pathology test or a test designated by CMS as an ADLT under paragraph (1) of the definition of an “advanced diagnostic laboratory test” in § 414.502. As a result of our evaluation of public comments, we are finalizing a revision to exclude blood banks or centers from the laboratory DOS policy exception at § 414.510(b)(5). This revision to our laboratory DOS policy does not impose any information collection requirements. Consequently, review by the Office of Management and Budget under the authority of the PRA is not required.
XXV. Response to Comments
Because of the large number of public comments we normally receive on Federal Register documents, we are not able to acknowledge or respond to them individually. We will consider all comments we receive by the date and time specified in the DATES section of this final rule with comment period, and, when we proceed with a subsequent document(s), we will respond to those comments in the preamble to that document.
XXVI. Economic Analyses
A. Statement of Need
This final rule with comment period is necessary to make updates to the Medicare hospital OPPS rates. It is necessary to make changes to the payment policies and rates for outpatient services furnished by hospitals and CMHCs in CY 2020. We are required under section 1833(t)(3)(C)(ii) of the Act to update annually the OPPS conversion factor used to determine the payment rates for APCs. We also are required under section 1833(t)(9)(A) of the Act to review, not less often than annually, and revise the groups, the relative payment weights, and the wage and other adjustments described in section 1833(t)(2) of the Act. We must review the clinical integrity of payment groups and relative payment weights at least annually. We are revising the APC relative payment weights using claims data for services furnished on and after January 1, 2018, through and including December 31, 2018, and processed through June 30, 2019, and updated cost report information.
We note that we are completing the phase-in of our method, as described below, to control unnecessary increases in the volume of covered outpatient department services by paying for clinic visits furnished at off-campus PBDs at an amount equal to the site-specific PFS payment rate for nonexcepted items and services furnished by a nonexcepted off-campus PBD (the PFS payment rate). The site-specific PFS payment rate for clinic visits furnished in excepted off-campus PBDs is the OPPS rate reduced to the amount paid for clinic visits furnished by nonexcepted off-campus PBDs under the PFS, which is 40 percent of the OPPS rate. In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59013 through 59014), we implemented this policy with a 2-year phase-in. In CY 2019, the payment reduction was transitioned by applying 50 percent of the total reduction in payment that would apply if these off-campus PBDs were paid the site-specific PFS payment rate for the clinic visit service. In other words, these excepted off-campus PBDs were paid 70 percent of the OPPS rate for the clinic visit service in CY 2019. In CY 2020, we are completing the transition of paying the PFS-equivalent amount for clinic visits furnished in excepted off-campus PBDs. In other words, these excepted off-campus PBDs will be paid the full reduced payment, or 40 percent of the OPPS rate for the clinic visit service in CY 2020. We acknowledge that the United States District Court for the District of Columbia vacated the volume control policy for CY 2019 and we are working to ensure affected 2019 claims for clinic visits are paid consistent with the court's order. We do not believe it is appropriate at this time to make a change to the second year of the two-year phase-in of the clinic visit policy. The government has appeal rights, and is still evaluating the rulings and considering, at the time of this writing, whether to appeal from the final judgment.
This final rule with comment period also is necessary to make updates to the ASC payment rates for CY 2020, enabling CMS to make changes to payment policies and payment rates for covered surgical procedures and covered ancillary services that are performed in an ASC in CY 2020. Because ASC payment rates are based on the OPPS relative payment weights for most of the procedures performed in ASCs, the ASC payment rates are updated annually to reflect annual changes to the OPPS relative payment weights. In addition, we are required under section 1833(i)(1) of the Act to review and update the list of surgical procedures that can be performed in an ASC, not less frequently than every 2 years.
In the CY 2019 OPPS/ASC final rule with comment period (83 FR 59075 through 59079), we finalized a policy to update the ASC payment system rates using the hospital market basket update instead of the CPI-U for CY 2019 through 2023. We believe that this policy will help stabilize the differential between OPPS payments and ASC payments, given that the CPI-U has been generally lower than the hospital market basket, and encourage the migration of services to lower cost settings as clinically appropriate.
B. Overall Impact for Provisions of This Final Rule With Comment Period
We have examined the impacts of this final rule with comment period, as required by Executive Order 12866 on Regulatory Planning and Review (September 30, 1993), Executive Order 13563 on Improving Regulation and Regulatory Review (January 18, 2011), the Regulatory Flexibility Act (RFA) (September 19, 1980, Pub. L. 96-354), section 1102(b) of the Social Security Act, section 202 of the Unfunded Mandates Reform Act of 1995 (UMRA) (March 22, 1995, Pub. L. 104-4), Executive Order 13132 on Federalism (August 4, 1999), the Congressional Review Act (5 U.S.C. 804(2)), and Executive Order 13771 on Reducing Regulation and Controlling Regulatory Costs (January 30, 2017). This section of this final rule with comment period contains the impact and other economic analyses for the provisions we are finalizing for CY 2020.
Executive Orders 12866 and 13563 direct agencies to assess all costs and benefits of available regulatory alternatives and, if regulation is necessary, to select regulatory approaches that maximize net benefits (including potential economic, environmental, public health and safety effects, distributive impacts, and equity). Executive Order 13563 emphasizes the importance of quantifying both costs and benefits, of reducing costs, of harmonizing rules, and of promoting flexibility. This final rule with comment period has been designated as an economically significant rule under section 3(f)(1) of Executive Order 12866 and a major rule under the Congressional Review Act. Accordingly, this final rule with comment period has been reviewed by the Office of Management and Budget. We have prepared a regulatory impact analysis that, to the best of our ability, presents the costs and benefits of the provisions of this final rule with comment period. In the CY 2020 OPPS/ASC proposed rule (84 FR 39398), we solicited public comments on the regulatory impact analysis in the proposed rule, and we address any public comments we received in this final rule with comment period, as appropriate.
We estimate that the total increase in Federal Government expenditures under the OPPS for CY 2020, compared to CY 2019, due only to the changes to the OPPS in this final rule with comment period, will be approximately $1.21 billion. Taking into account our estimated changes in enrollment, utilization, and case-mix for CY 2020, we estimate that the OPPS expenditures, including beneficiary cost-sharing, for CY 2020 will be approximately $79.0 billion, which is approximately $6.3 billion higher than estimated OPPS expenditures in CY 2019. We note that these spending estimates include the CY 2020 completion of the phase-in, finalized in CY 2019, to control for unnecessary increases in the volume of covered outpatient department services by paying for clinic visits furnished at excepted off-campus PBDs in CY 2020 at a rate that will be 40 percent of the OPPS rate for a clinic visit service. Because the provisions of the OPPS are part of a final rule that is economically significant, as measured by the threshold of an additional $100 million in expenditures in 1 year, we have prepared this regulatory impact analysis that, to the best of our ability, presents its costs and benefits. Table 68 of this final rule with comment period displays the distributional impact of the CY 2020 changes in OPPS payment to various groups of hospitals and for CMHCs.
As noted in section V.B.5 of this final rule with comment period, we are finalizing our proposal for CY 2020 to pay for separately payable drugs and biological products that do not have pass-through payment status and are not acquired under the 340B program at WAC+3 percent instead of WAC+6 percent, if ASP data are unavailable for payment purposes. If WAC data are not available for a drug or biological product, we will continue our policy to pay separately payable drugs and biological products at 95 percent of the AWP. We note that under our CY 2020 policy, drugs and biologicals that are acquired under the 340B Program would continue to be paid at ASP minus 22.5 percent, WAC minus 22.5 percent, or 69.46 percent of AWP, as applicable.
We note that in the impact tables as displayed in this impact analysis, we have modeled current and prospective payments as if separately payable drugs acquired under the 340B program from hospitals not excepted from the policy are paid in CY 2020 under the OPPS at ASP-22.5 percent.
We estimate that the update to the conversion factor and other adjustments (not including the effects of outlier payments, the pass-through payment estimates, the application of the frontier State wage adjustment for CY 2020, and the completion of the phase-in to control for unnecessary increases in the volume of covered outpatient department services described in section X.D. of this final rule with comment period) will increase total OPPS payments by 1.3 percent in CY 2020. The changes to the APC relative payment weights, the changes to the wage indexes, the continuation of a payment adjustment for rural SCHs, including EACHs, and the payment adjustment for cancer hospitals will not increase OPPS payments because these changes to the OPPS are budget neutral. However, these updates will change the distribution of payments within the budget neutral system. We estimate that the total change in payments between CY 2019 and CY 2020, considering all budget neutral payment adjustments, changes in estimated total outlier payments, pass-through payments, the application of the frontier State wage adjustment, and the completion of the phase-in to control unnecessary increases in the volume of outpatient services as described in section X.D. of this final rule with comment period, in addition to the application of the OPD fee schedule increase factor after all adjustments required by sections 1833(t)(3)(F), 1833(t)(3)(G), and 1833(t)(17) of the Act, will increase total estimated OPPS payments by 1.3 percent.
We estimate the total increase (from changes to the ASC provisions in this final rule with comment period as well as from enrollment, utilization, and case-mix changes) in Medicare expenditures (not including beneficiary cost-sharing) under the ASC payment system for CY 2020 compared to CY 2019, to be approximately $180 million. Because the provisions for the ASC payment system are part of a final rule that is economically significant, as measured by the $100 million threshold, we have prepared a regulatory impact analysis of the changes to the ASC payment system that, to the best of our ability, presents the costs and benefits of this portion of this final rule with comment period. Tables 42 and 43 of this final rule with comment period display the redistributive impact of the CY 2020 changes regarding ASC payments, grouped by specialty area and then grouped by procedures with the greatest ASC expenditures, respectively.
C. Detailed Economic Analyses
1. Estimated Effects of OPPS Changes in This Final Rule With Comment Period
a. Limitations of Our Analysis
The distributional impacts presented here are the projected effects of the CY 2020 policy changes on various hospital groups. We post on the CMS website our hospital-specific estimated payments for CY 2020 with the other supporting documentation for this final rule with comment period. To view the hospital-specific estimates, we refer readers to the CMS website at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/index.html. At the website, select “regulations and notices” from the left side of the page and then select “CMS-1717-FC” from the list of regulations and notices. The hospital-specific file layout and the hospital-specific file are listed with the other supporting documentation for this final rule with comment period. We show hospital-specific data only for hospitals whose claims were used for modeling the impacts shown in Table 41. We do not show hospital-specific impacts for hospitals whose claims we were unable to use. We refer readers to section II.A. of this final rule with comment period for a discussion of the hospitals whose claims we do not use for ratesetting and impact purposes.
We estimate the effects of the individual policy changes by estimating payments per service, while holding all other payment policies constant. We use the best data available, but do not attempt to predict behavioral responses to our policy changes in order to isolate the effects associated with specific policies or updates, but any policy that changes payment could have a behavioral response. In addition, we have not made adjustments for future changes in variables, such as service volume, service-mix, or number of encounters.
b. Estimated Effects of the CY 2020 Completion of Phase-in to Control for Unnecessary Increases in the Volume of Outpatient Services
In section X.D. of this final rule with comment period, we discuss the CY 2020 completion of the phase-in of our CY 2019 finalized method to control for unnecessary increases in the volume of outpatient department services by paying for clinic visits furnished at an off-campus PBD at an amount equal to the site-specific PFS payment rate for nonexcepted items and services furnished by a nonexcepted off-campus PBD (the PFS payment rate). Specifically, in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59013 through 59014), we finalized our proposal to pay for HCPCS code G0463 (Hospital outpatient clinic visit for assessment and management of a patient) when billed with modifier “PO” at an amount equal to the site-specific PFS payment rate for nonexcepted items and services furnished by a nonexcepted off-campus PBD (the PFS payment rate), with a 2-year transition period. For a discussion of the PFS payment amount for outpatient clinic visits furnished at nonexcepted off-campus PBDs, we refer readers to the CY 2018 PFS final rule with comment period discussion (82 FR 53023 through 53024), as well as the CY 2019 PFS final rule and the CY 2020 PFS proposed rule.
To develop an estimated impact of this policy, we began with CY 2018 outpatient claims data used in ratesetting for the CY 2020 OPPS. We then flagged all claim lines for HCPCS code G0463 that contained modifier “PO” because the presence of this modifier indicates that such claims were billed for services furnished by an off-campus department of a hospital paid under the OPPS. Next, we excluded those that were billed as a component of C-APC 8011 (Comprehensive Observation Services) or packaged into another C-APC because, in those instances, OPPS payment is made for a broader package of services. We then simulated payment for the remaining claim lines as if they were paid at the PFS-equivalent rate. An estimate of the policy that includes the effects of estimated changes in enrollment, utilization, and case-mix based on the FY 2020 Midsession Review approximates the estimated decrease in total payment under the OPPS at $800 million, with Medicare OPPS payments decreasing by $640 million and beneficiary copayments decreasing by $160 million. We note that the additional impact specifically as a result of completing the phase-in in CY 2020, is $400 million, with Medicare payments decreasing by $320 million and beneficiary copayments decreasing by $80 million. This estimate is utilized for the accounting statement displayed in Table 42 of this final rule with comment period because the impact of this CY 2020 policy, which is not budget neutral, is combined with the impact of the OPD update, which is also not budget neutral, to estimate changes in Medicare spending under the OPPS as a result of the changes in this final rule with comment period.
We note that our estimates may differ from the actual effect of the proposed policy due to offsetting factors, such as changes in provider behavior. We note that, by removing this payment differential that may influence site-of-service decision-making, we anticipate an associated decrease in the volume of clinic visits provided in the excepted off-campus PBD setting. In the proposed rule, we reminded readers that this estimate could change in the final rule with comment period based on factors such as the availability of updated data. Finally, we acknowledge that the United States District Court for the District of Columbia vacated the volume control policy for CY 2019 and we are working to ensure affected 2019 claims for clinic visits are paid consistent with the court's order. Our estimates may differ from the actual effect of this policy depending on the outcome of this litigation.
c. Estimated Effects of OPPS Changes on Hospitals
Table 41 shows the estimated impact of this final rule with comment period on hospitals. Historically, the first line of the impact table, which estimates the change in payments to all facilities, has always included cancer and children's hospitals, which are held harmless to their pre-BBA amount. We also include CMHCs in the first line that includes all providers. We include a second line for all hospitals, excluding permanently held harmless hospitals and CMHCs.
We present separate impacts for CMHCs in Table 41, and we discuss them separately below, because CMHCs are paid only for partial hospitalization services under the OPPS and are a different provider type from hospitals. In CY 2020, we are finalizing our proposal to pay CMHCs for partial hospitalization services under APC 5853 (Partial Hospitalization for CMHCs), and finalizing our proposal to pay hospitals for partial hospitalization services under APC 5863 (Partial Hospitalization for Hospital-Based PHPs).
The estimated increase in the total payments made under the OPPS is determined largely by the increase to the conversion factor under the statutory methodology. The distributional impacts presented do not include assumptions about changes in volume and service-mix. The conversion factor is updated annually by the OPD fee schedule increase factor, as discussed in detail in section II.B. of this final rule with comment period.
Section 1833(t)(3)(C)(iv) of the Act provides that the OPD fee schedule increase factor is equal to the market basket percentage increase applicable under section 1886(b)(3)(B)(iii) of the Act, which we refer to as the IPPS market basket percentage increase. The IPPS market basket percentage increase for FY 2020 is 3.0 percent. Section 1833(t)(3)(F)(i) of the Act reduces that 3.0 percent by the multifactor productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act, which is 0.4 percentage point for FY 2020 (which is also the MFP adjustment for FY 2020 in the FY 2020 IPPS/LTCH PPS final rule (84 FR 19411)), resulting in the OPD fee schedule increase factor of 2.6 percent. We are using the OPD fee schedule increase factor of 2.6 percent in the calculation of the CY 2020 OPPS conversion factor. Section 10324 of the Affordable Care Act, as amended by HCERA, further authorized additional expenditures outside budget neutrality for hospitals in certain frontier States that have a wage index less than 1.0000. The amounts attributable to this frontier State wage index adjustment are incorporated in the CY 2020 estimates in Table 41 of this final rule with comment period.
To illustrate the impact of the CY 2020 changes, our analysis begins with a baseline simulation model that uses the CY 2019 relative payment weights, the FY 2019 final IPPS wage indexes that include reclassifications, and the final CY 2019 conversion factor. Table 41 shows the estimated redistribution of the increase or decrease in payments for CY 2020 over CY 2019 payments to hospitals and CMHCs as a result of the following factors: the impact of the APC reconfiguration and recalibration changes between CY 2019 and CY 2020 (Column 2); the wage indexes and the provider adjustments (Column 3); the combined impact of all of the changes described in the preceding columns plus the 2.6 percent OPD fee schedule increase factor update to the conversion factor (Column 4); the finalized off-campus PBD clinic visits payment policy (Column 5), and the estimated impact taking into account all payments for CY 2020 relative to all payments for CY 2019, including the impact of changes in estimated outlier payments, and changes to the pass-through payment estimate (Column 6).
We did not model an explicit budget neutrality adjustment for the rural adjustment for SCHs because we are maintaining the current adjustment percentage for CY 2020. Because the updates to the conversion factor (including the update of the OPD fee schedule increase factor), the estimated cost of the rural adjustment, and the estimated cost of projected pass-through payment for CY 2020 are applied uniformly across services, observed redistributions of payments in the impact table for hospitals largely depend on the mix of services furnished by a hospital (for example, how the APCs for the hospital's most frequently furnished services will change), and the impact of the wage index changes on the hospital. However, total payments made under this system and the extent to which this final rule with comment period will redistribute money during implementation also will depend on changes in volume, practice patterns, and the mix of services billed between CY 2019 and CY 2020 by various groups of hospitals, which CMS cannot forecast.
Overall, we estimate that the rates for CY 2020 will increase Medicare OPPS payments by an estimated 1.3 percent. Removing payments to cancer and children's hospitals because their payments are held harmless to the pre-OPPS ratio between payment and cost and removing payments to CMHCs results in an estimated 1.3 percent increase in Medicare payments to all other hospitals. These estimated payments will not significantly impact other providers.
Column 1: Total Number of Hospitals
The first line in Column 1 in Table 41 shows the total number of facilities (3,732), including designated cancer and children's hospitals and CMHCs, for which we were able to use CY 2018 hospital outpatient and CMHC claims data to model CY 2019 and CY 2020 payments, by classes of hospitals, for CMHCs and for dedicated cancer hospitals. We excluded all hospitals and CMHCs for which we could not plausibly estimate CY 2019 or CY 2020 payment and entities that are not paid under the OPPS. The latter entities include CAHs, all-inclusive hospitals, and hospitals located in Guam, the U.S. Virgin Islands, Northern Mariana Islands, American Samoa, and the State of Maryland. This process is discussed in greater detail in section II.A. of this final rule with comment period. At this time, we are unable to calculate a DSH variable for hospitals that are not also paid under the IPPS because DSH payments are only made to hospitals paid under the IPPS. Hospitals for which we do not have a DSH variable are grouped separately and generally include freestanding psychiatric hospitals, rehabilitation hospitals, and long-term care hospitals. We show the total number of OPPS hospitals (3,625), excluding the hold-harmless cancer and children's hospitals and CMHCs, on the second line of the table. We excluded cancer and children's hospitals because section 1833(t)(7)(D) of the Act permanently holds harmless cancer hospitals and children's hospitals to their “pre-BBA amount” as specified under the terms of the statute, and therefore, we removed them from our impact analyses. We show the isolated impact on the 41 CMHCs at the bottom of the impact table (Table 41) and discuss that impact separately below.
Column 2: APC Recalibration—All Changes
Column 2 shows the estimated effect of APC recalibration. Column 2 also reflects any changes in multiple procedure discount patterns or conditional packaging that occur as a result of the changes in the relative magnitude of payment weights. As a result of APC recalibration, we estimate that urban hospitals will experience a 0.1 percent increase, with the impact ranging from a decrease of 0.1 percent to an increase of 0.4 depending on the number of beds. Rural hospitals will experience a decrease of up to 0.9 percent depending on the number of beds. Major teaching hospitals will experience no change.
Column 3: Wage Indexes and the Effect of the Provider Adjustments
Column 3 demonstrates the combined budget neutral impact of the APC recalibration; the updates for the wage indexes with the FY 2020 IPPS post-reclassification wage indexes; the rural adjustment; the frontier adjustment, and the cancer hospital payment adjustment. We modeled the independent effect of the budget neutrality adjustments and the OPD fee schedule increase factor by using the relative payment weights and wage indexes for each year, and using a CY 2019 conversion factor that included the OPD fee schedule increase and a budget neutrality adjustment for differences in wage indexes.
Column 3 reflects the independent effects of the proposed updated wage indexes, including the application of budget neutrality for the rural floor policy on a nationwide basis, as well as the CY 2020 proposed changes in wage index policy discussed in section II.C. of the CY 2020 OPPS/ASC proposed rule. We did not model a budget neutrality adjustment for the rural adjustment for SCHs because we are continuing the rural payment adjustment of 7.1 percent to rural SCHs for CY 2020, as described in section II.E. of this final rule with comment period. We also modeled a budget neutrality adjustment for the cancer hospital payment adjustment because we are using a payment-to-cost ratio target for the cancer hospital payment adjustment in CY 2020 of .90, which is higher than the ratio that was reported for the CY 2019 OPPS/ASC final rule with comment period (83 FR 58873). We note that, in accordance with section 16002 of the 21st Century Cures Act, we are applying a budget neutrality factor calculated as if the cancer hospital adjustment target payment-to-cost ratio was 0.90, not the 0.89 target payment-to-cost ratio we are applying in section II.F. of this final rule with comment period.
We modeled the independent effect of updating the wage indexes by varying only the wage indexes, holding APC relative payment weights, service-mix, and the rural adjustment constant and using the CY 2020 scaled weights and a CY 2019 conversion factor that included a budget neutrality adjustment for the effect of the changes to the wage indexes between CY 2019 and CY 2020.
Column 4: All Budget Neutrality Changes Combined With the Market Basket Update
Column 4 demonstrates the combined impact of all of the changes previously described and the update to the conversion factor of 2.6 percent. Overall, these changes will increase payments to urban hospitals by 2.7 percent and to rural hospitals by 2.8 percent. The increase for classes of rural hospitals will vary with sole community hospitals receiving a 2.8 percent increase and other rural hospitals receiving an increase of 2.7 percent.
Column 5: Off-Campus PBD Visits Payment Policy
Column 5 displays the estimated effect of our finalized CY 2020 volume control method, finalized in CY 2019, to pay for clinic visit HCPCS code G0463 (Hospital outpatient clinic visit for assessment and management of a patient) when billed with modifier “PO” by an excepted off-campus PBD at a rate that will be 40 percent of the OPPS rate for a clinic visit service for CY 2020. We note that the numbers provided in this column isolate the estimated effect of this policy adjustment relative to the numerator of Column 4. Therefore, the numbers reported in Column 5 show how much of the difference between the estimates in Column 4 and the estimates in Column 6 are a result of the finalized off-campus PBD visits policy for CY 2020, as finalized in the CY 2019 OPPS/ASC final rule with comment period (83 FR 59013 through 59014).
Column 6: All Changes for CY 2020
Column 6 depicts the full impact of the CY 2020 policies on each hospital group by including the effect of all changes for CY 2020 and comparing them to all estimated payments in CY 2019. Column 6 shows the combined budget neutral effects of Columns 2 through 3; the OPD fee schedule increase; the effect of the CY 2020 off-campus PBD visits policy finalized in CY 2019, the impact of estimated OPPS outlier payments, as discussed in section II.G. of this final rule with comment period; the change in the Hospital OQR Program payment reduction for the small number of hospitals in our impact model that failed to meet the reporting requirements (discussed in section XIV. of this final rule with comment period); and the difference in total OPPS payments dedicated to transitional pass-through payments.
Of those hospitals that failed to meet the Hospital OQR Program reporting requirements for the full CY 2019 update (and assumed, for modeling purposes, to be the same number for CY 2020), we included 24 hospitals in our model because they had both CY 2018 claims data and recent cost report data. We estimate that the cumulative effect of all changes for CY 2020 will increase payments to all facilities by 1.3 percent for CY 2020. We modeled the independent effect of all changes in Column 6 using the final relative payment weights for CY 2019 and the relative payment weights for CY 2020. We used the final conversion factor for CY 2019 of $79.490 and the final CY 2020 conversion factor of $80.784 discussed in section II.B. of this final rule with comment period.
Column 6 contains simulated outlier payments for each year. We used the 1-year charge inflation factor used in the FY 2020 IPPS/LTCH PPS final rule (84 FR 42629) of 5.4 percent (1.05404) to increase individual costs on the CY 2018 claims, and we used the most recent overall CCR in the July 2019 Outpatient Provider-Specific File (OPSF) to estimate outlier payments for CY 2019. Using the CY 2018 claims and a 5.4 percent charge inflation factor, we currently estimate that outlier payments for CY 2019, using a multiple threshold of 1.75 and a fixed-dollar threshold of $4,825, will be approximately 1.0 percent of total payments. The estimated current outlier payments of 1.0 percent are incorporated in the comparison in Column 6. We used the same set of claims and a charge inflation factor of 11.1 percent (1.11100) and the CCRs in the July 2019 OPSF, with an adjustment of 0.97615, to reflect relative changes in cost and charge inflation between CY 2018 and CY 2020, to model the final CY 2020 outliers at 1.0 percent of estimated total payments using a multiple threshold of 1.75 and a fixed-dollar threshold of $5,075. The charge inflation and CCR inflation factors are discussed in detail in the FY 2020 IPPS/LTCH PPS proposed rule (84 FR 42629).
Overall, we estimate that facilities will experience an increase of 1.3 percent under this final rule with comment period in CY 2020 relative to total spending in CY 2019. This projected increase (shown in Column 6) of Table 68 reflects the 2.6 percent OPD fee schedule increase factor, minus 0.6 percent for the off-campus PBD visits policy, minus 0.74 percent for the change in the pass-through payment estimate between CY 2019 and CY 2020, plus no difference in estimated outlier payments between CY 2019 (1.00 percent) and CY 2020 (1.00 percent). We estimate that the combined effect of all final changes for CY 2020 will increase payments to urban hospitals by 1.3 percent. Overall, we estimate that rural hospitals will experience a 1.1 percent increase as a result of the combined effects of all the changes for CY 2020.
Among hospitals, by teaching status, we estimate that the impacts resulting from the combined effects of all changes will include an increase of 0.9 percent for major teaching hospitals and an increase of 1.5 percent for nonteaching hospitals. Minor teaching hospitals will experience an estimated increase of 1.3 percent.
In our analysis, we also have categorized hospitals by type of ownership. Based on this analysis, we estimate that voluntary hospitals will experience an increase of 1.1 percent, proprietary hospitals will experience an increase of 2.1 percent, and governmental hospitals will experience an increase of 1.3 percent.




d. Estimated Effects of OPPS Changes on CMHCs
The last line of Table 68 demonstrates the isolated impact on CMHCs, which furnish only partial hospitalization services under the OPPS. In CY 2019, CMHCs are paid under APC 5853 (Partial Hospitalization (3 or more services) for CMHCs). We modeled the impact of this APC policy assuming CMHCs will continue to provide the same number of days of PHP care as seen in the CY 2018 claims used for ratesetting in the proposed rule. We excluded days with 1 or 2 services because our policy only pays a per diem rate for partial hospitalization when 3 or more qualifying services are provided to the beneficiary. We estimate that CMHCs will experience an overall 3.7 percent increase in payments from CY 2019 (shown in Column 6). We note that this includes the trimming methodology as well as the final CY 2020 floor on geometric mean costs used for developing the PHP payment rates described in section VIII.B. of this final rule. The CY 2020 proposal to establish a floor based on geometric mean costs, rather than based on a predetermined payment rate, makes the OPPS budget neutrality adjustments for both the weight scaler and the conversion factor applicable.
Column 3 shows that the estimated impact of adopting the final FY 2020 wage index values will result in an increase of 0.5 percent to CMHCs. Column 4 shows that combining this proposed OPD fee schedule increase factor, along with final changes in APC policy for CY 2020 and the final FY 2020 wage index updates, will result in an estimated increase of 4.5 percent. Column 5 shows that the off-campus PBD clinic visits payment policy has no estimated effect on CMHCs. Column 6 shows that adding the final changes in outlier and pass-through payments will result in a total 3.7 percent increase in payment for CMHCs. This reflects all final changes for CMHCs for CY 2020.
e. Estimated Effect of OPPS Changes on Beneficiaries
For services for which the beneficiary pays a copayment of 20 percent of the payment rate, the beneficiary's payment will increase for services for which the OPPS payments will rise and will decrease for services for which the OPPS payments will fall. For further discussion on the calculation of the national unadjusted copayments and minimum unadjusted copayments, we refer readers to section II.I. of the CY 2020 OPPS/ASC proposed rule. In all cases, section 1833(t)(8)(C)(i) of the Act limits beneficiary liability for copayment for a procedure performed in a year to the hospital inpatient deductible for the applicable year.
We estimate that the aggregate beneficiary coinsurance percentage will be 18.1 percent for all services paid under the OPPS in CY 2020. The estimated aggregate beneficiary coinsurance reflects general system adjustments, including the final CY 2020 comprehensive APC payment policy discussed in section II.A.2.b. of this final rule.
f. Estimated Effects of OPPS Changes on Other Providers
The relative payment weights and payment amounts established under the OPPS affect the payments made to ASCs, as discussed in section XIII of the final rule. No types of providers or suppliers other than hospitals, CMHCs, and ASCs will be affected by the final changes in the final rule.
g. Estimated Effects of OPPS Changes on the Medicare and Medicaid Programs
The effect on the Medicare program is expected to be an increase of $1.21 billion in program payments for OPPS services furnished in CY 2020. The effect on the Medicaid program is expected to be limited to copayments that Medicaid may make on behalf of Medicaid recipients who are also Medicare beneficiaries. We estimate that the final changes in the final rule will increase these Medicaid beneficiary payments by approximately $45 million in CY 2020. Currently, there are approximately 10 million dual-eligible beneficiaries, which represents approximately one third of Medicare Part B fee-for-service beneficiaries. The impact on Medicaid was determined by taking one-third of the beneficiary cost-sharing impact. The national average split of Medicaid payments is 57 percent Federal payments and 43 percent State payments. Therefore, for the estimated $80 million Medicaid increase, approximately $45 million will be from the Federal Government and $35 million will be from State governmenwe dis. Alternative OPPS Policies Considered
Alternatives to the OPPS changes we proposed and the reasons for our selected alternatives are discussed throughout the final rule.
- Alternatives Considered for the Methodology for Assigning Skin Substitutes to High or Low Cost Groups
We refer readers to section V.B.7. of the CY 2020 OPPS/ASC proposed rule for a discussion of our policy to assign any skin substitute product that was assigned to the high cost group in CY 2019 to the high cost group in CY 2020, regardless of whether the product's mean unit cost (MUC) or the product's per day cost (PDC) exceeds or falls below the overall CY 2020 MUC or PDC threshold. We will continue to assign products that exceed either the overall CY 2020 MUC or PDC threshold to the high cost group. We also considered, but are not proposing, reinstating our methodology from CY 2017 and assigning skin substitutes to the high cost group based on whether an individual product's MUC or PDC exceeded the overall CY 2020 MUC or PDC threshold based on calculations done for either the proposed rule or the final rule with comment period.
- Alternatives Considered for the Methodology for Payment for Non-Opioid Pain Management Treatments
We refer readers to sections II.A.3.b. and XIII.D.3. of the CY 2020 OPPS/ASC proposed rule (84 FR 39425 for a discussion of our packaging policy for certain drugs when administered in the ASC setting and policy of providing separate payment for non-opioid pain management drugs that function as a supply when used in a surgical procedure when the procedure is performed in an ASC. In those sections of the CY 2020 OPPS/ASC proposed rule, we discuss our proposal to continue paying separately at ASP+6 percent for the cost of non-opioid pain management drugs that function as surgical supplies in the performance of surgical procedures when they are furnished in the ASC setting and continue to package payment for non-opioid pain management drugs that function as surgical supplies in the performance of surgical procedures in the hospital outpatient department setting for CY 2020. In the CY 2020 OPPS/ASC final rule with comment period, we discuss the comments we received on whether we should pay separately for various non-opioid treatments for pain under the OPPS and the ASC payment system and also finalize the policy for non-opioid pain management drugs that function as surgical supplies.
- Alternatives Considered for the Proposed Changes in the Level of Supervision of Outpatient Therapeutic Services in Hospitals and Critical Access Hospitals (CAHs)
We refer readers to section X.A. of the proposed rule for a discussion of our proposal to change the minimum required default level of supervision from direct supervision to general supervision for all hospital outpatient therapeutic services provided by all hospitals and CAHs. We also considered, but did not propose, reevaluation of the level of physician supervision for cardiac rehabilitation services to determine whether we should propose to change the supervision level from direct supervision to general supervision. Under this alternative, direct supervision would have remained the minimum required default level for most hospital outpatient therapeutic services with the exception of those services that have been evaluated by the HOP Panel and received a change in supervision level based on those recommendations.
2. Estimated Effects of CY 2020 ASC Payment System Changes
Most ASC payment rates are calculated by multiplying the ASC conversion factor by the ASC relative payment weight. As discussed fully in section XIII of this final rule with comment period, we are setting the CY 2020 ASC relative payment weights by scaling the proposed CY 2020 OPPS relative payment weights by the proposed ASC scalar of 0.8550. The estimated effects of the proposed updated relative payment weights on payment rates are varied and are reflected in the estimated payments displayed in Tables 39 and 40 below.
Beginning in CY 2011, section 3401 of the Affordable Care Act requires that the annual update to the ASC payment system (which we proposed will be the hospital market basket for CY 2020) after application of any quality reporting reduction be reduced by a productivity adjustment. The Affordable Care Act defines the productivity adjustment to be equal to the 10-year moving average of changes in annual economy-wide private nonfarm business multifactor productivity (MFP) (as projected by the Secretary for the 10-year period, ending with the applicable fiscal year, year, cost reporting period, or other annual period). For ASCs that fail to meet their quality reporting requirements, the CY 2020 payment determinations will be based on the application of a 2.0 percentage point reduction to the annual update factor, which we proposed will be the hospital market basket for CY 2020. We calculated the CY 2020 ASC conversion factor by adjusting the CY 2019 ASC conversion factor by 1.0001 to account for changes in the pre-floor and pre-reclassified hospital wage indexes between CY 2019 and CY 2020 and by applying the CY 2020 MFP-adjusted hospital market basket update factor of 2.6 percent (which is equal to the projected hospital market basket update of 3.0 percent minus an MFP adjustment of 0.4 percentage point). The proposed CY 2020 ASC conversion factor is $47.747 for ASCs that successfully meet the quality reporting requirements.
a. Limitations of Our Analysis
Presented here are the projected effects of the proposed changes for CY 2020 on Medicare payment to ASCs. A key limitation of our analysis is our inability to predict changes in ASC service-mix between CY 2018 and CY 2020 with precision. We believe the net effect on Medicare expenditures resulting from the proposed CY 2020 changes will be small in the aggregate for all ASCs. However, such changes may have differential effects across surgical specialty groups, as ASCs continue to adjust to the payment rates based on the policies of the revised ASC payment system. We are unable to accurately project such changes at a disaggregated level. Clearly, individual ASCs will experience changes in payment that differ from the aggregated estimated impacts presented below.
b. Estimated Effects of ASC Payment System Policies on ASCs
Some ASCs are multispecialty facilities that perform a wide range of surgical procedures from excision of lesions to hernia repair to cataract extraction; others focus on a single specialty and perform only a limited range of surgical procedures, such as eye, digestive system, or orthopedic procedures. The combined effect on an individual ASC of the proposed update to the CY 2020 payments will depend on a number of factors, including, but not limited to, the mix of services the ASC provides, the volume of specific services provided by the ASC, the percentage of its patients who are Medicare beneficiaries, and the extent to which an ASC provides different services in the coming year. The following discussion presents tables that display estimates of the impact of the proposed CY 2020 updates to the ASC payment system on Medicare payments to ASCs, assuming the same mix of services, as reflected in our CY 2018 claims data. Table 70 depicts the estimated aggregate percent change in payment by surgical specialty or ancillary items and services group by comparing estimated CY 2019 payments to estimated proposed CY 2020 payments, and Table 69 shows a comparison of estimated CY 2019 payments to estimated proposed CY 2020 payments for procedures that we estimate will receive the most Medicare payment in CY 2019.
In Table 70, we have aggregated the surgical HCPCS codes by specialty group, grouped all HCPCS codes for covered ancillary items and services into a single group, and then estimated the effect on aggregated payment for surgical specialty and ancillary items and services groups. The groups are sorted for display in descending order by estimated Medicare program payment to ASCs. The following is an explanation of the information presented in Table 70.
- Column 1—Surgical Specialty or Ancillary Items and Services Group indicates the surgical specialty into which ASC procedures are grouped and the ancillary items and services group which includes all HCPCS codes for covered ancillary items and services. To group surgical procedures by surgical specialty, we used the CPT code range definitions and Level II HCPCS codes and Category III CPT codes, as appropriate, to account for all surgical procedures to which the Medicare program payments are attributed.
- Column 2—Estimated CY 2019 ASC Payments were calculated using CY 2018 ASC utilization data (the most recent full year of ASC utilization) and CY 2019 ASC payment rates. The surgical specialty and ancillary items and services groups are displayed in descending order based on estimated CY 2019 ASC payments.
- Column 3—Estimated CY 2020 Percent Change is the aggregate percentage increase or decrease in Medicare program payment to ASCs for each surgical specialty or ancillary items and services group that is attributable to proposed updates to ASC payment rates for CY 2020 compared to CY 2019.
As shown in Table 69, for the six specialty groups that account for the most ASC utilization and spending, we estimate that the proposed update to ASC payment rates for CY 2020 will result in a 4-percent increase in aggregate payment amounts for eye and ocular adnexa procedures, a 3-percent increase in aggregate payment amounts for nervous system procedures, 1-percent increase in aggregate payment amounts for digestive system procedures, a 2-percent increase in aggregate payment amounts for musculoskeletal system procedures, a 2-percent increase in aggregate payment amounts for genitourinary system procedures, and a 5-percent increase in aggregate payment amounts for cardiovascular system procedures. We note that these changes can be a result of different factors, including updated data, payment weight changes, and proposed changes in policy. In general, spending in each of these categories of services is increasing due to the 2.6 percent proposed payment rate update. After the payment rate update is accounted for, aggregate payment increases or decreases for a category of services can be higher or lower than a 2.6-percent increase, depending on if payment weights in the OPPS APCs that correspond to the applicable services increased or decreased or if the most recent data show an increase or a decrease in the volume of services performed in an ASC for a category. For example, we estimate a 4-percent increase in proposed aggregate eye and ocular adnexa procedure payments due to an increase in hospital reported costs for the primary payment grouping for this category under the OPPS. This increases the payment weights for eye and ocular adnexa procedure payments and, overall, is further increased by the proposed 2.6 percent ASC rate update for these procedures. For estimated changes for selected procedures, we refer readers to Table 70 provided later in this section.
Also displayed in Table 69 is a separate estimate of Medicare ASC payments for the group of separately payable covered ancillary items and services. The payment estimates for the covered surgical procedures include the costs of packaged ancillary items and services. We estimate that aggregate payments for these items and services will decrease by 12 percent for CY 2020. This is largely attributed to the drug packaging policies adopted under the OPPS and ASC payment system.

Table 70 shows the estimated impact of the updates to the revised ASC payment system on aggregate ASC payments for selected surgical procedures during CY 2020. The table displays 30 of the procedures receiving the greatest estimated CY 2019 aggregate Medicare payments to ASCs. The HCPCS codes are sorted in descending order by estimated CY 2019 program payment.
- Column 1—CPT/HCPCS code.
- Column 2—Short Descriptor of the HCPCS code.
- Column 3—Estimated CY 2019 ASC Payments were calculated using CY 2018 ASC utilization (the most recent full year of ASC utilization) and the CY 2019 ASC payment rates. The estimated CY 2019 payments are expressed in millions of dollars.
- Column 4—Estimated CY 2020 Percent Change reflects the percent differences between the estimated ASC payment for CY 2019 and the estimated payment for CY 2020 based on the proposed update.


c. Estimated Effects of ASC Payment System Policies on Beneficiaries
We estimate that the proposed CY 2020 update to the ASC payment system will be generally positive (that is, result in lower cost-sharing) for beneficiaries with respect to the new procedures we proposed to add to the ASC list of covered surgical procedures and for those we proposed to designate as office-based for CY 2020. For example, using 2018 utilization data and proposed CY 2020 OPPS and ASC payment rates, we estimate that if 5 percent of coronary intervention procedures migrate from the hospital outpatient setting to the ASC setting as a result of this proposed policy, Medicare payments will be reduced by approximately $20 million in CY 2020 and total beneficiary copayments will decline by approximately $5 million in CY 2020. First, other than certain preventive services where coinsurance and the Part B deductible is waived to comply with sections 1833(a)(1) and (b) of the Act, the ASC coinsurance rate for all procedures is 20 percent. This contrasts with procedures performed in HOPDs under the OPPS, where the beneficiary is responsible for copayments that range from 20 percent to 40 percent of the procedure payment (other than for certain preventive services), although the majority of HOPD procedures have a 20-percent copayment. Second, in almost all cases, the ASC payment rates under the ASC payment system are lower than payment rates for the same procedures under the OPPS. Therefore, the beneficiary coinsurance amount under the ASC payment system will almost always be less than the OPPS copayment amount for the same services. (The only exceptions will be if the ASC coinsurance amount exceeds the hospital inpatient deductible. The statute requires that copayment amounts under the OPPS not exceed the hospital inpatient deductible.) Beneficiary coinsurance for services migrating from physicians' offices to ASCs may decrease or increase under the ASC payment system, depending on the particular service and the relative payment amounts under the MPFS compared to the ASC. While the ASC payment system bases most of its payment rates on hospital cost data used to set OPPS relative payment weights, services that are performed a majority of the time in a physician office are generally paid the lesser of the ASC amount according to the standard ASC ratesetting methodology or at the nonfacility practice expense based amount payable under the PFS. For those additional procedures that we proposed to designate as office-based in CY 2020, the beneficiary coinsurance amount under the ASC payment system generally will be no greater than the beneficiary coinsurance under the PFS because the coinsurance under both payment systems generally is 20 percent (except for certain preventive services where the coinsurance is waived under both payment systems).
3. Accounting Statements and Tables
As required by OMB Circular A-4 (available on the Office of Management and Budget website at: https://www.whitehouse.gov/sites/whitehouse.gov/files/omb/assets/OMB/circulars/a004/a-4.html), we have prepared accounting statements to illustrate the impacts of the OPPS and ASC changes in this final rule with comment period. The first accounting statement, Table 71, illustrates the classification of expenditures for the CY 2020 estimated hospital OPPS incurred benefit impacts associated with the proposed CY 2020 OPD fee schedule increase. This $1.21 billion in additional Medicare spending estimate includes the $1.53 billion in additional Medicare spending associated with updating the CY 2019 OPPS payment rates by the hospital market basket update for CY 2020, offset by the $320 million in Medicare savings associated with the CY 2020 completion of phase-in finalized in CY 2019 to pay for clinic visits furnished at off-campus PBDs at a PFS-equivalent rate. In addition, we estimate that these OPPS changes in the final rule will increase copayments that Medicaid may make on behalf of Medicaid recipients who are also Medicare beneficiaries by approximately $45 million in CY 2020. The second accounting statement, Table 72, illustrates the classification of expenditures associated with the 2.6 percent CY 2020 update to the ASC payment system, based on the provisions of the final rule with comment period and the baseline spending estimates for ASCs. Both tables classify most estimated impacts as transfers. The estimated costs of ICR Burden and Regulatory Familiarization are included in Table 73.



4. Effects of Changes in Requirements for the Hospital OQR Program
a. Background
We refer readers to the CY 2018 OPPS/ASC final rule with comment period (82 FR 59492 through 59494), for the previously estimated effects of changes to the Hospital OQR Program for the CY 2018, CY 2019, and CY 2020 payment determinations. Of the approximately 3,300 hospitals that met eligibility requirements for the CY 2019 payment determination, we determined that 14 hospitals did not meet the requirements to receive the full OPD fee schedule increase factor. In the CY 2020 OPPS/ASC Proposed Rule (84 FR 39556), we did not propose to add any quality measures to the Hospital OQR Program measure set for the CY 2021 or CY 2022 payment determinations. However, we are finalizing our proposal to remove one measure from the program measure set, as discussed in section XIV.B.3.b. of this final rule with comment period. We do not believe that this finalized policy will increase the number of hospitals that do not receive a full annual payment update for the CY 2021 or CY 2022 payment determinations.
b. Estimated Effects of Finalized Removal of OP-33 for the CY 2022 Payment Determination and Subsequent Years
In section XIV.B.3.b. of this final rule with comment period, we are finalizing our proposal with modification to remove one measure submitted via a web-based tool beginning with the CY 2022 payment determination and for subsequent years: OP-33: External Beam Radiotherapy for Bone Metastases. In the CY 2020 OPPS/ASC proposed rule, we inadvertently stated that we were proposing to remove this measure beginning with October 2020 encounters for CY 2022 payment determination and subsequent years (84 FR 39554 through 39556). As discussed in section XXVI.B.2. of this final rule with comment period, we intended to remove this measure beginning with the CY 2022 payment determination and subsequent years, but starting with January 2020 encounters, not October. Because we are finalizing removal of this measure beginning with the same CY 2022 payment determination, as was proposed, the estimated impacts and burden reduction remain the same as discussed in the proposed rule. As discussed in section XXVI.B.2. of this final rule with comment period, we anticipate a burden reduction of 551 hours and $21,379 associated with the removal of OP-33 for the CY 2022 payment determination. In addition to burden associated with information collection, we also anticipate that hospitals will experience a general burden and cost reduction associated with this removal stemming from no longer having to implement, review, track, and maintain program requirements associated with this measure.
5. Effects of Requirements for the ASCQR Program
a. Background
In section XV.B of this final rule with comment period, we discuss our finalized policies affecting the ASCQR Program. For the CY 2019 payment determination, of the 6,393 ASCs that met eligibility requirements for the ASCQR Program, 203 ASCs did not meet the requirements to receive the full annual payment update. In section XV.B.3. of this final rule with comment period, we are finalizing our proposal to adopt ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers to the ASCQR Program measure set for the CY 2024 payment determination and subsequent years. We do not believe that adoption of the finalized ASC-19 measure will cause any ASCs to fail to meet the ASCQR Program requirements. Therefore, we do not believe this measure adoption will increase the number of ASCs that do not receive a full annual payment update for the CY 2024 payment determination. Below we discuss only the effects that will result from the provisions finalized in this final rule with comment period.
b. Estimated Effects of Adoption of ASC-19: Facility-Level 7-Day Hospital Visits After General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357)
In section XV.B.3. of this final rule with comment period, we are finalizing our proposal, beginning with the CY 2024 payment determination and for subsequent years, to adopt one measure: ASC-19: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers (NQF #3357). As discussed in section XXVI.C.2. of this final rule with comment period, data used to calculate scores for this finalized measure are collected via Medicare Part A and Part B administrative claims and Medicare enrollment data. Therefore, ASCs will not be required to report any additional data. Because this change does not affect ASCQR Program participation requirements or data reporting requirements, we do not expect this finalized measure to change the information collection burden; it will only nominally affect other costs experienced by ASCs due to having to review and track confidential feedback and reports related to the finalized ASC-19 measure.
XXVI. Economic Analyses
D. Effects of Prior Authorization Process and Requirements for Certain Hospital Outpatient Department (OPD) Services
1. Overall Impact
As discussed in section XX. CY 2020 OPPS/ASC proposed rule (84 FR 39556), we proposed developing a new prior authorization process and requirements for certain hospital outpatient department (OPD) services. This proposal will use our authority in section 1833(t)(2)(f) of the Act to require provisional affirmation of coverage as a condition of Medicare payment unless the provider is exempt. This new requirement for prior authorization of certain covered OPD services aims to reduce the unnecessary increases in volume of certain covered hospital outpatient department services.
We believe there are a number of factors that may contribute to the potential growth assumed in the estimate presented below. For example, as the provider community acclimates to using prior authorization as part of their billing practice, there may be greater systemic or other processing efficiencies to allow more extensive implementation.
The overall economic impact on the health care sector is dependent on the number of claims affected. Table 74, Overall Economic Impact to the Health Sector, lists an estimate for the overall economic impact to the health sector for the services combined. The values populating this table were obtained from the cost reflected in Table 48, Annual Private Sector Costs, and Table 76, Estimated Annual Medicare Costs. Together, Tables 75 and 76 combine to convey the overall economic impact to the health sector, which is illustrated in Table 74. It should be noted that due to a July start date, year one will include only 6 months of prior authorization requests.
Based on the estimate, the overall economic impact is approximately $5.7 million in the first year based on 6 months. The 5-year impact is approximately $46.5 million, and the 10-year impact is approximately $98.7 million. The 5 and 10 year impacts account for year one including only 6 months. Additional administrative paperwork costs to private sector providers and an increase in Medicare spending to conduct reviews combine to create the financial impact. However, this impact is offset by some savings. We believe there are likely to be other benefits and cost savings that result from the OPD service prior authorization requirement. However, many of those benefits are difficult to quantify. For instance, we expect to see savings in the form of reduced unnecessary utilization, fraud, waste, and abuse, including a reduction in improper Medicare fee-for-service payments (we note that not all improper payments are fraudulent).

The rationale behind requiring prior authorization is to control unnecessary increases in the volume of certain covered OPD services that are often cosmetic. We believe that the purpose of the statute is to avoid unnecessary utilization of OPD services. Therefore, we do not view decreased revenues from OPD services subject to unnecessary utilization by providers to be a condition that we must mitigate. We believe that the effect will be minimal on providers who are compliant with Medicare coverage and payment rules and requirements. This policy will offer an additional protection to a provider's cash flow as the provider will know in advance if the Medicare requirements are met.
2. Anticipated Specific Cost Effects
a. Private Sector Costs
We do not believe that this finalized policy will significantly affect the number of legitimate claims submitted for these services. However, we do expect a decrease in the overall amount paid for OPD services resulting from a reduction in unnecessary utilization of the services requiring prior authorization.
As described previously in the CY 2020 OPPS/ASC proposed rule (84 FR 39556), we have identified a list of specific services that, based on review and analysis of claims data, show higher than expected, and therefore we believe unnecessary, increases in the volume of service utilization. In making the decision to include the specific services in the list of hospital outpatient department services requiring prior authorization, we first considered that these services are primarily cosmetic and, therefore, are only covered by Medicare in very rare circumstances. We then viewed the current volume of utilization of these services and determined that the utilization far exceeded what will be expected.
We have developed a list of potential OPD services categories for inclusion in the OPD services prior authorization process—blepharoplasty; botulinum toxin injections; panniculectomy; rhinoplasty; and vein ablation. The list includes services from each of five categories that have demonstrated unnecessary increases in volume and that are likely to be cosmetic surgical procedures and/or are directly related to cosmetic surgical procedures that are not covered by Medicare, but may be combined with or masquerading as therapeutic services.
We estimate that the private sector's per-case time burden attributed to submitting documentation and associated clerical activities in support of a prior authorization request is equivalent to that of submitting documentation and clerical activities associated for prepayment review, which is 0.5 hours. We apply this time burden estimate to initial submissions and resubmissions.

b. Medicare Costs
Medicare will incur additional costs associated with processing prior authorization requests. We use the range of potentially affected cases (submissions and resubmissions) and multiply it by $50, the estimated cost to review each request. The cost also includes other elements such as appeals, education and outreach, and system changes.

c. Estimated Beneficiary Costs
We expect a reduction in the utilization of Medicare OPD services when such utilization does not comply with one or more of Medicare's coverage, coding, and payment rules. While there may be an associated burden on beneficiaries while they wait for the prior authorization decision, we are unable to quantify that burden. Although the system is designed to permit utilization that is medically necessary, OPD services that are not medically necessary may still provide convenience or usefulness for beneficiaries; any rule-induced loss of such convenience or usefulness constitutes a cost of the rule that we lack data to quantify. Additionally, beneficiaries may have out-of-pocket costs for those services that are determined not to comply with Medicare requirements and thus, are not eligible for Medicare payment. We lack the data to quantify these costs as well.
3. Estimated Benefits
There will be quantifiable benefits because we expect a reduction in the unnecessary utilization of those Medicare OPD services subject to prior authorization. It is difficult to project the decrease in unnecessary utilization. However, for the first 6 months we estimate the savings to be $6,059,950 and the net savings as $2,112,362. Annually, the estimated savings are $12,119,899 and the net savings are $4,679,966. We will closely monitor utilization and billing practices. The expected benefits will include a changed billing practice that also enhances the coordination of care for the beneficiary. For example, requiring prior authorization for certain OPD services ensures that the primary care practitioner recommending the service and the facility collaborate more closely to provide the most appropriate OPD services to meet the needs of the beneficiary. The practitioner recommending the service evaluates the beneficiary to determine his or her condition and what services are needed and medically necessary. This requires the facility to collaborate closely with the practitioner early on in the process to ensure the services are truly necessary and meet all requirements and the documentation is complete and correct. Improper payments made because the practitioner did not evaluate the patient or the patient does not meet the Medicare requirements, will likely be reduced by the requirement that a provider submit clinical documentation created by as part of its prior authorization request.
E. Effects of Requirements Relating to Changes in the Definition of Expected Donation Rate for Organ Procurement Organizations
We are finalizing our proposal to revise the definition of “expected donation rate” in the CfCs for OPOs. This change will allow OPOs to receive payment for organ donor costs under the Medicare and Medicaid programs using a definition that is consistent with the definition used by the Scientific Registry of Transplant Recipients (SRTR).
Due to comments received on the CY 2020 OPPS/ASC proposed rule (and discussed in section XVIII.A of this final rule with comment period), we are finalizing a policy that would not require all OPOs to meet the standards of the second outcome measure for the 2022 recertification cycle only. As a result, OPOs will only have to meet one of the remaining outcome measures, which may provide temporary relief for a small number of OPOs that, absent this waiver, might have faced de-certification and the appeal process due to only meeting one outcome measure.
For subsequent recertification cycles, all 58 OPOs will once again be required to meet two out of three outcome measures detailed in the CfCs for OPOs regulations at 42 CFR 486.318(a) and (b). The second outcome measure relies on the aforementioned “expected donation rate” definition, and therefore all OPOs will be affected by the finalized change. This revision will eliminate the potential for confusion in the OPO community due to different definitions of the same term; however, it will not affect data collection or reporting by OPTNs and SRTRs, nor their statistical evaluation of OPO performance, and therefore it will not result in any quantifiable impact.
F. Revisions to the Laboratory Date of Service Policy
In section XIX of this final rule with comment period, we discuss our comment solicitation on potential revisions to the laboratory date of service (DOS) exception at 42 CFR 414.510(b)(5) for molecular pathology tests and tests designated by CMS as an ADLT under paragraph (1) of the definition of advanced diagnostic laboratory test in § 414.502. As a result of our evaluation of public comments, we are finalizing a revision to exclude blood banks or centers from the laboratory DOS exception at § 414.510(b)(5). Because the molecular pathology tests performed by blood banks or centers are excluded from our packaging policy under the OPPS, and are paid at the applicable rate for the laboratory test under the CLFS, regardless of whether the hospital or the performing laboratory bills Medicare for the test, this revision will not result in net costs or savings to the Medicare program. Accordingly, the discussion in section XIX of this final rule with comment period is not reflected in Table 41 in the regulatory impact analysis under section XXVI.C.1. of this final rule with comment period.
G. Effect of Changes to Requirements for Grandfathered Children's Hospitals-Within-Hospitals (HwHs)
In section XXII. of this final rule, we are finalizing our proposal to revise § 412.22(f)(1) and (2) to allow grandfathered children's HwHs to increased beds while maintaining their grandfathered status. This policy change will allow providers to address changing community needs for services without any increased incentive for inappropriate patient shifting to maximize Medicare payments given the low Medicare utilization in children's hospitals. Based on the best available information, there are currently very few grandfathered children's HwHs (3 or less). For these reasons, we estimate any impact on Medicare expenditures as a result of this policy change will be negligible. On average there are approximately 50 Medicare discharges per year from children's hospitals at an average cost of approximately $33,000 per discharge. There are two possible sources for an increase, if any, in Medicare discharges at grandfathered children's hospitals as a result of our policy change—(1) either the discharges will have been treated at another children's hospital; or (2) the cases will have been treated at an IPPS hospital. In either case given the few number of Medicare discharges at children's hospitals, the impact of this policy change on Medicare spending is negligible
H. Regulatory Review Costs
If regulations impose administrative costs on private entities, such as the time needed to read and interpret a rule, we should estimate the cost associated with regulatory review. Due to the uncertainty involved with accurately quantifying the number of entities that will review a rule, we assumed that the number of commenters on the CY 2020 OPPS/ASC proposed rule (3,853) will be the number of reviewers of this final rule with comment period. We acknowledge that this assumption may understate or overstate the costs of reviewing this final rule with comment period. It is possible that not all commenters will review this final rule with comment period in detail, and it is also possible that some reviewers will choose not to comment on this final rule with comment period. Nonetheless, we believed that the number of commenters on the CY 2019 OPPS/ASC proposed rule would be a fair estimate of the number of reviewers of this final rule with comment period. In the CY 2020 OPPS/ASC proposed rule (84 FR 39637), we welcomed any comments on the approach in estimating the number of entities that will review the proposed rule. We also recognize that different types of entities are, in many cases, affected by mutually exclusive sections of the proposed rule and the final rule with comment period, and, therefore, for the purposes of our estimate, we assumed that each reviewer reads approximately 50 percent of the rule.
Using the wage information from the 2018 BLS for medical and health service managers (Code 11-9111), we estimated that the cost of reviewing this rule is $109.36 per hour, including overhead and fringe benefits (https://www.bls.gov/oes/current/oes_nat.htm). Assuming an average reading speed, we estimate that it will take approximately 8 hours for the staff to review half of this final rule with comment period. For each facility that reviewed this final rule with comment period, the estimated cost is $874.88 (8 hours × $109.36). Therefore, we estimated that the total cost of reviewing this final rule with comment period is $3,370,913 ($874.88 × 3,853 reviewers).
I. Regulatory Flexibility Act (RFA) Analysis
The RFA requires agencies to analyze options for regulatory relief of small entities, if a rule has a significant impact on a substantial number of small entities. For purposes of the RFA, many hospitals are considered small businesses either by the Small Business Administration's size standards with total revenues of $41.0 million or less in any single year or by the hospital's not-for-profit status. Most ASCs and most CMHCs are considered small businesses with total revenues of $16.5 million or less in any single year. For details, we refer readers to the Small Business Administration's “Table of Size Standards” at http://www.sba.gov/content/table-small-business-size-standards. As its measure of significant economic impact on a substantial number of small entities, HHS uses a change in revenue of more than 3 to 5 percent. We do not believe that this threshold will be reached by the requirements in this final rule with comment period. As a result, the Secretary has determined that this final rule with comment period will not have a significant impact on a substantial number of small entities.
In addition, section 1102(b) of the Act requires us to prepare a regulatory impact analysis if a rule may have a significant impact on the operations of a substantial number of small rural hospitals. This analysis must conform to the provisions of section 604 of the RFA. For purposes of section 1102(b) of the Act, we define a small rural hospital as a hospital that is located outside of a metropolitan statistical area and has 100 or fewer beds. We estimate that this final rule with comment period will increase payments to small rural hospitals by less than 2 percent; therefore, it should not have a significant impact on approximately 609 small rural hospitals. We note that the estimated payment impact for any category of small entity will depend on both the services that they provide as well as the payment policies and/or payment systems that may apply to them. Therefore, the most applicable estimated impact may be based on the specialty, provider type, or payment system.
The analysis above, together with the remainder of this preamble, provides a regulatory flexibility analysis and a regulatory impact analysis.
J. Unfunded Mandates Reform Act Analysis
Section 202 of the Unfunded Mandates Reform Act of 1995 (UMRA) also requires that agencies assess anticipated costs and benefits before issuing any rule whose mandates require spending in any 1 year of $100 million in 1995 dollars, updated annually for inflation. That threshold level is currently approximately $154 million. This final rule with comment period does not mandate any requirements for State, local, or tribal governments, or for the private sector.
K. Reducing Regulation and Controlling Regulatory Costs
Executive Order 13771, titled Reducing Regulation and Controlling Regulatory Costs, was issued on January 30, 2017. It has been determined that this final rule with comment period, will be a regulatory action for the purposes of Executive Order 13771. We estimate that this final rule with comment period will generate $2.5 million in annualized cost at a 7-percent discount rate, discounted relative to 2016, over a perpetual time horizon.
L. Conclusion
The changes we are making in this final rule with comment period will affect all classes of hospitals paid under the OPPS and will affect both CMHCs and ASCs. We estimate that most classes of hospitals paid under the OPPS will experience a modest increase or a minimal decrease in payment for services furnished under the OPPS in CY 2020. Table 68 demonstrates the estimated distributional impact of the OPPS budget neutrality requirements that will result in a 1.3 percent increase in payments for all services paid under the OPPS in CY 2020, after considering all of the changes to APC reconfiguration and recalibration, as well as the OPD fee schedule increase factor, wage index changes, including the frontier State wage index adjustment, estimated payment for outliers, the finalized off-campus provider-based department clinic visits payment policy, and changes to the pass-through payment estimate. However, some classes of providers that are paid under the OPPS will experience more significant gains or losses in OPPS payments in CY 2020.
The updates to the ASC payment system for CY 2020 will affect each of the approximately 5,600 ASCs currently approved for participation in the Medicare program. The effect on an individual ASC will depend on its mix of patients, the proportion of the ASC's patients who are Medicare beneficiaries, the degree to which the payments for the procedures offered by the ASC are changed under the ASC payment system, and the extent to which the ASC provides a different set of procedures in the coming year. Table 69 demonstrates the estimated distributional impact among ASC surgical specialties of the MFP-adjusted hospital market basket update factor of 2.6 percent for CY 2020.
XXVII. Federalism Analysis
Executive Order 13132 establishes certain requirements that an agency must meet when it promulgates a proposed rule (and subsequent final rule) that imposes substantial direct costs on State and local governments, preempts State law, or otherwise has federalism implications. We have examined the OPPS and ASC provisions included in this final rule with comment period in accordance with Executive Order 13132, Federalism, and have determined that they will not have a substantial direct effect on State, local or tribal governments, preempt State law, or otherwise have a federalism implication. As reflected in Table 68 of this final rule with comment period, we estimate that OPPS payments to governmental hospitals (including State and local governmental hospitals) will increase by 1.3 percent under this final rule with comment period. While we do not know the number of ASCs or CMHCs with government ownership, we anticipate that it is small. The analyses we have provided in this section of this final rule with comment period, in conjunction with the remainder of this document, demonstrate that this final rule with comment period is consistent with the regulatory philosophy and principles identified in Executive Order 12866, the RFA, and section 1102(b) of the Act.
This final rule with comment period will affect payments to a substantial number of small rural hospitals and a small number of rural ASCs, as well as other classes of hospitals, CMHCs, and ASCs, and some effects may be significant.
List of Subjects
42 CFR Part 405
- Administrative practice and procedure
- Health facilities
- Health professions
- Kidney diseases
- Medical devices
- Medicare
- Reporting and recordkeeping requirements
- Rural areas
- X-rays
42 CFR Part 410
- Diseases
- Health facilities
- Health professions
- Laboratories
- Medicare
- Reporting and recordkeeping requirements
- Rural areas
- X-rays
42 CFR Part 412
- Administrative practice and procedure
- Health facilities
- Medicare
- Puerto Rico
- Reporting and recordkeeping requirements
42 CFR Part 414
- Administrative practice and procedure
- Biologics
- Drugs
- Health
42 CFR Part 416
- Health facilities
- Health professions
- Medicare
- Reporting and recordkeeping requirements
42 CFR Part 419
- Hospitals
- Medicare
- Reporting and recordkeeping requirements
42 CFR Part 486
- Definitions
- Medicare
- Organ procurement
For reasons stated in the preamble of this document, the Centers for Medicare & Medicaid Services amends 42 CFR chapter IV as set forth below:
PART 405—FEDERAL HEALTH INSURANCE FOR THE AGED AND DISABLED
1. The authority citation for part 405 continues to read as follows:
2. Section 405.926 is amended by revising paragraph (t) to read as follows:
(t) A contractor's prior authorization determination with regard to—
(1) Durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS)); and
(2) Hospital outpatient department (OPD) services.
PART 410—SUPPLEMENTARY MEDICAL INSURANCE (SMI) BENEFITS
3. The authority citation for part 410 continues to read as follows:
4. Section 410.27 is amended by revising paragraph (a)(1)(iv) to read as follows:
(a) * * *
(1) * * *
(iv) Under the general supervision (or other level of supervision as specified by CMS for the particular service) of a physician or a nonphysician practitioner as specified in paragraph (g) of this section, subject to the following requirements:
(A) For services furnished in the hospital or CAH, or in an outpatient department of the hospital or CAH, both on and off-campus, as defined in § 413.65 of this chapter, general supervision means the definition specified at § 410.32(b)(3)(i).
(B) Certain therapeutic services and supplies may be assigned either direct supervision or personal supervision. For purposes of this section, direct supervision means that the physician or nonphysician practitioner must be immediately available to furnish assistance and direction throughout the performance of the procedure. It does not mean that the physician or nonphysician practitioner must be present in the room when the procedure is performed. Personal supervision means the definition specified at § 410.32(b)(3)(iii);
PART 412—PROSPECTIVE PAYMENT SYSTEMS FOR INPATIENT HOSPITAL SERVICES
5. The authority citation for part 412 continues to read as follows:
6. Section 412.22 is amended by revising paragraphs (f)(1) and (2) to read as follows:
(f) * * *
(1) Continues to operate under the same terms and conditions, including the number of beds, unless the hospital is a children's hospital as defined at § 412.23(d), and square footage considered to be part of the hospital for purposes of Medicare participation and payment in effect on September 30, 1995; or
(2) In the case of a hospital that changes the terms and conditions under which it operates after September 30, 1995, but before October 1, 2003, continues to operate under the same terms and conditions, including the number of beds, unless the hospital is a children's hospital as defined at § 412.23(d), and square footage considered to be part of the hospital for purposes of Medicare participation and payment in effect on September 30, 2003.
PART 414—PAYMENT FOR PART B MEDICAL AND OTHER HEALTH SERVICES
7. The authority citation for part 414 continues to read as follows:
8. Section 414.502 is amended by adding a definition for “Blood bank or center” in alphabetical order to read as follows:
Blood bank or center means an entity whose primary function is the performance or responsibility for the performance of, the collection, processing, testing, storage and/or distribution of blood or blood components intended for transfusion and transplantation.
9. Section 414.510 is amended by revising paragraph (b)(5) introductory text to read as follows:
(b) * * *
(5) In the case of a molecular pathology test performed by a laboratory other than a blood bank or center, or a test designated by CMS as an ADLT under paragraph (1) of the definition of an advanced diagnostic laboratory test in § 414.502, the date of service of the test must be the date the test was performed only if—
PART 416—AMBULATORY SURGICAL SERVICES
10. The authority citation for part 416 continues to read as follows:
11. Section 416.171 is amended by adding paragraph (b)(4) to read as follows:
(b) * * *
(4) Notwithstanding paragraph (b)(2) of this section, low volume device-intensive procedures where the otherwise applicable payment rate calculated based on the standard methodology for device intensive procedures described in this paragraph (b) would exceed the payment rate for the equivalent service set under the payment system established under part 419 of this chapter, for which the payment rate will be set at an amount equal to the amount under that payment system.
PART 419—PROSPECTIVE PAYMENT SYSTEM FOR HOSPITAL OUTPATIENT DEPARTMENT SERVICES
12. The authority citation for part 419 continues to read as follows:
13. Section 419.66 is amended by revising paragraph (c)(2) to read as follows:
(c) * * *
(2) CMS determines either of the following:
(i) The device to be included in the category has demonstrated that it will substantially improve the diagnosis or treatment of an illness or injury or improve the functioning of a malformed body part compared to the benefits of a device or devices in a previously established category or other available treatment; or
(ii) For devices for which pass-through payment status will begin on or after January 1, 2020, as an alternative pathway to paragraph (c)(2)(i) of this section, the device has received FDA marketing authorization and is part of the FDA's Breakthrough Devices Program.
14. Subpart I, consisting of §§ 419.80 through 419.89, is added to read as follows:
- 419.80
- Basis and scope of this subpart.
- 419.81
- Definitions.
- 419.82
- Prior authorization for certain covered hospital outpatient department services.
- 419.83
- List of hospital outpatient department services requiring prior authorization.
- 419.84-419.89
- [Reserved]
Subpart I—Prior Authorization for Outpatient Department Services
(a) Basis. The provisions in this subpart are issued under the authority of section 1833(t)(2)(F) of the Act, which authorizes the Secretary to develop a method for controlling unnecessary increases in the volume of covered hospital outpatient department services.
(b) Scope. This subpart specifies the process and requirements for prior authorization for certain hospital outpatient department services as a condition of Medicare payment.
As used in this subpart, unless otherwise specified, the following definitions apply:
List of hospital outpatient department services requiring prior authorization means the list of hospital outpatient department services described in § 419.83(a) that CMS adopts in accordance with § 419.83(b) that require prior authorization as a condition of Medicare payment.
Prior authorization means the process through which a request for provisional affirmation of coverage is submitted to CMS or its contractors for review before the service is provided to the beneficiary and before the claim is submitted for processing.
Provisional affirmation means a preliminary finding that a future claim meets the Medicare coverage, coding, and payment rules in chapter IV of this title or in Title XVIII of the Social Security Act.
(a) Prior authorization as condition of payment. As a condition of Medicare payment for the services in the categories of services on the list of hospital outpatient department services requiring prior authorization as specified in § 419.83(a), a provider must submit to CMS or its contractors a prior authorization request in accordance with the requirements of paragraph (c) of this section.
(b) Denial of claim. (1) CMS or its contractors will deny a claim for a service that requires prior authorization if the provider has not received a provisional affirmation of coverage on the claim from CMS or its contractor unless the provider is exempt under § 419.83(c).
(2) CMS or its contractor may deny a claim that has received a provisional affirmation based on either of the following:
(i) Technical requirements that can only be evaluated after the claim has been submitted for formal processing; or
(ii) Information not available at the time of a prior authorization request.
(3) CMS or its contractor may deny claims for services related to services on the list of hospital outpatient department services for which the provider has received a denial.
(c) Submission of prior authorization request. A provider must submit to CMS or its contractor a prior authorization request for any service on the list of outpatient department services requiring prior authorization.
(1) Prior authorization request requirements. A prior authorization request must—
(i) Include all documentation necessary to show that the service meets applicable Medicare coverage, coding, and payment rules in chapter IV of this title or in Title XVIII of the Social Security Act.
(ii) Be submitted before the service is provided to the beneficiary and before the claim is submitted.
(2) Request for expedited review. A provider may submit a request for expedited review of a prior authorization request. The request for expedited review must comply with the requirements in paragraphs (c)(1)(i) and (ii) of this section and include documentation showing that the processing of the prior authorization request must be expedited due to the beneficiary's life, health, or ability to regain maximum function being in serious jeopardy.
(d) Reviews—(1) Review of prior authorization request. Upon receipt of a prior authorization request, CMS or its contractor will review the request for compliance with applicable Medicare coverage, coding, and payment rules in chapter IV of this title or in Title XVIII of the Social Security Act.
(i) CMS or its contractor will issue a provisional affirmation to the provider if it is determined that applicable Medicare coverage, coding, and payment rules in chapter IV of this title or in Title XVIII of the Social Security Act are met.
(ii) CMS or its contractor will issue a non-affirmation to the provider if it is determined that applicable Medicare coverage, coding, and payment rules in chapter IV of this title or in Title XVIII of the Social Security Act are not met.
(iii) The provisional affirmation or non-affirmation will be issued within 10 business days of receipt of the prior authorization request.
(2) Review of expedited review request. Upon receipt of a request for expedited review, CMS or its contractor will complete an expedited review of the prior authorization request if it is determined that a delay could seriously jeopardize the beneficiary's life, health, or ability to regain maximum function, and issue a provisional affirmation or non-affirmation decision in accordance with paragraph (d)(1) of this section within 2 business days of the expedited review request.
(e) Resubmission. (1) A provider may resubmit a prior authorization request, upon receipt of a non-affirmation, consistent with the requirements in paragraph (c)(1) of this section.
(2) A provider may resubmit a request for expedited review consistent with the requirements in paragraph (c)(1) of this section.
(a) Service categories for the list of hospital outpatient department services requiring prior authorization. (1) The following service categories comprise the list of hospital outpatient department services requiring prior authorization:
(i) Blepharoplasty.
(ii) Botulinum toxin injections.
(iii) Panniculectomy.
(iv) Rhinoplasty.
(v) Vein ablation.
(2) Technical updates to the list of services, such as changes to the name of the service or CPT code, will be published on the CMS website.
(b) Adoption of the list of services. CMS will adopt the list of hospital outpatient department service categories requiring prior authorization and any updates or geographic restrictions through formal notice-and-comment rulemaking.
(c) Exemptions. CMS may elect to exempt a provider from the prior authorization process in § 419.82 upon a provider's demonstration of compliance with Medicare coverage, coding, and payment rules in chapter IV of this title or in Title XVIII of the Social Security Act through such prior authorization process.
(1) An exemption will remain in effect until CMS elects to withdraw the exemption.
(2) Notice of an exemption or withdraw of an exemption will be provided at least 60 days prior to the effective date.
(d) Suspension of prior authorization process or services. CMS may suspend the outpatient department services prior authorization process requirements generally or for a particular service(s) at any time by issuing notification on the CMS website.
PART 486—CONDITIONS FOR COVERAGE OF SPECIALIZED SERVICES FURNISHED BY SUPPLIERS
15. The authority citation for part 486 is revised to read as follows:
16. Section 486.302 is amended by revising the definition of “Expected donation rate” to read as follows:
Expected donation rate means the expected donation rate per 100 eligible deaths that is the rate expected for an OPO based on the national experience for OPOs serving similar eligible donor populations and donation service areas. This rate is adjusted for the distributions of age, sex, race, and cause of death among eligible deaths.
17. Section 486.316 is amended by adding paragraph (a)(3) and revising paragraph (b) to read as follows:
(a) * * *
(3) For the 2022 recertification cycle only, an OPO is recertified for an additional 4 years and its service area is not opened for competition when the OPO meets one out of the two outcome measure requirements described in § 486.318(a)(1) and (3) for OPOs not operating exclusively in the noncontiguous States, Commonwealths, Territories, or possessions; or § 486.318(b)(1) and (3) for OPOs operating exclusively in noncontiguous States, Commonwealths, Territories, and possessions. An OPO is not required to meet the second outcome measure described in § 486.318(a)(2) or (b)(2) for the 2022 recertification cycle.
(b) De-certification and competition. (1) If an OPO does not meet two out of the three outcome measures as described in paragraph (a)(1) of this section or the requirements described in paragraph (a)(2) of this section, the OPO is de-certified. If the OPO does not appeal or the OPO appeals and the reconsideration official and CMS hearing officer uphold the de-certification, the OPO's service area is opened for competition from other OPOs. The de-certified OPO is not permitted to compete for its open area or any other open area. An OPO competing for an open service area must submit information and data that describe the barriers in its service area, how they affected organ donation, what steps the OPO took to overcome them, and the results.
(2) For the 2022 recertification cycle only, if an OPO does not meet one of the outcome measures as described in paragraphs § 486.318(a)(1), (a)(3), (b)(1), or (b)(3), or the requirements described in paragraph (a)(2) of this section, the OPO is de-certified. If the OPO does not appeal or the OPO appeals and the reconsideration official and CMS hearing officer uphold the de-certification, the OPO's service area is opened for competition from other OPOs. The de-certified OPO is not permitted to compete for its open area or any other open area. An OPO competing for an open service area must submit information and data that describe the barriers in its service area, how they affected organ donation, what steps the OPO took to overcome them, and the results.
Dated: October 24, 2019.
Seema Verma,
Administrator, Centers for Medicare and Medicaid Services.
Dated: October 28, 2019
Alex M. Azar II,
Secretary, Department of Health and Human Services.
Footnotes
1. 2011 product label available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/022496s000lbl.pdf.
2. 2011 FDA approval letter available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2011/022496Orig1s000Approv.pdf.
Back to Citation3. President's Commission on Combating Drug Addiction and the Opioid Crisis, Report (2017). Available at: https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Final_Report_Draft_11-1-2017.pdf.
Back to Citation4. Ibid, at page 57, Recommendation 19.
Back to Citation5. Ibid.
Back to Citation6. Available at: https://www.hhs.gov/about/leadership/secretary/speeches/2017-speeches/secretary-price-announces-hhs-strategy-for-fighting-opioid-crisis/index.html.
Back to Citation7. Available at: https://www.hhs.gov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisis.html.
Back to Citation8. Available at: https://www.phe.gov/emergency/news/healthactions/phe/Pages/default.aspx.
Back to Citation9. Food and Drug Administration, Meeting of the Anesthetic and Analgesic Drug Products Advisory Committee Briefing Document (2018). Available at: https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/AnestheticAndAnalgesicDrugProductsAdvisoryCommittee/UCM596314.pdf.
Back to Citation10. Ibid, page 9.
Back to Citation11. 2018 updated product label available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/022496s009lbledt.pdf.
Back to Citation12. Available at: http://www.medpac.gov/-documents-/reports.
Back to Citation13. Pasciak AS, McElmurray JH, Bourgeois AC, Heidel RE, Bradley YC. Impact of an antireflux catheter on target volume particulate distribution in liver-directed embolotherapy: a pilot study. J Vasc Interv Radiol. 2015 May;26(5):660-9.
Back to Citation14. Kim AY, Frantz S, Krishnan P, DeMulder D, Caridi T, Lynskey GE, et al. (2017) Short-term imaging response after drug-eluting embolic trans- arterial chemoembolization delivered with the Surefire Infusion System® for the treatment of hepatocellular carcinoma. PloS one 12.9 (2017): e0183861.
Back to Citation15. N Apseloff, J Keung, T Caridi, D Buckley, G Lynskey, A Kim. Case-control evaluation of endhole microcatheter versus Surefire Infusion System for use during transarterial chemoembolization for hepatocellular carcinoma. Conference abstract presented at 2017 Society of Intervention Radiology Annual Congress, March 8, 2017.
Back to Citation16. Kapoor B, Contreras F, Katz M, Arepally A, Fischman A, Rose S, Kim A, Ferraro J. Surefire Infusion System (SIS) hepatocellular carcinoma registry study interim results: A multicenter study of the safety, feasibility, and outcomes of the SIS expandable-tip microcatheter in DEB-TACE.
Conference abstract presented at 2018 Society of Intervention Radiology Annual Congress, March 19, 2017.
Back to Citation17. Current Behavioral Neuroscience Reports. 2014 Jun; 1(2): 64-73.
Back to Citation18. https://www.accessdata.fda.gov/cdrh_docs/pdf18/P180036B.pdf.
Back to Citation19. Abraham, W. T., Kuck, K. H., Goldsmith, R. L., Lindenfeld, J., Reddy, V. Y., Carson, P. E., . & Wiegn, P. (2018). A randomized controlled trial to evaluate the safety and efficacy of cardiac contractility modulation. JACC: Heart Failure, 6(10), 874-883.
Back to Citation20. Anker, S. D., Borggrefe, M., Neuser, H., Ohlow, M. A., Röger, S., Goette, A., . & Rousso, B. Cardiac contractility modulation improves long-term survival and hospitalizations in heart failure with reduced ejection fraction. Eur J Heart Fail .2019 Jan 16. doi: 10.1002/ejhf.1374. [Epub ahead of print]
Back to Citation21. Borggrefe MM, Lawo T, Butter C, Schmidinger H, Lunati M, Pieske B, Misier AR, Curnis A, Bocker D, Remppis A, Kautzner J, Stuhlinger M, Leclerq C, Taborsky M, Frigerio M, Parides M, Burkhoff D and Hindricks G. Randomized, double blind study of non-excitatory, cardiac contractility modulation electrical impulses for symptomatic heart failure. Eur Heart J. 2008;29:1019-28.
Back to Citation22. Kloppe A, Lawo T, Mijic D, et al. Long-term survival with Cardiac Contractility Modulation in patients with NYHA II or III symptoms and normal QRS duration. Int J Cardiol. 2016 Apr 15;209:291-5.
Back to Citation23. Liu M, Fang F, Luo XX, Shlomo BH, Burkhoff D, Chan JY, Chan CP, Cheung L, Rousso B, Gutterman D, Yu CM. Improvement of long-term survival by cardiac contractility modulation in heart failure patients: A case-control study. Int J Cardiol. 2016 Mar 1;206:122-6.
Back to Citation24. Müller D, Remppis A, Schauerte P, et al. Clinical effects of long-term cardiac contractility modulation (CCM) in subjects with heart failure caused by left ventricular systolic dysfunction. Clin Res. Cardiol. 2017 Nov 1;106(11):893-904.
25. Kuschyk J, Roeger S, Schneider R, et al. Efficacy and survival in patients with cardiac contractility modulation: Long-term single center experience in 81 patients. Int J Cardiol. 2015;183C:76-81.
Back to Citation26. Chungtai B. Forde JC. Thomas DDM et al. Benign Prostatic Hyperplasia. Nature Reviews Disease Primers 2 (2016) article 16031.
Back to Citation27. 70 FR 68630.
Back to Citation28. Montorsi, F. et al.: Holmium Laser Enucleation Versus Transurethral Resection of The Prostate: Results from A 2-Center, Prospective, Randomized Trial In Patients With Obstructive Benign Prostatic Hyperplasia. J. Urol. 172, 1926-1929 (2004).
Back to Citation29. Bachmann A, et al.: 180-W XPS GreenLight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European Multicentre Randomised Trial—the GOLIATH study. Eur Urol, 2014;65(5):931-42.
Back to Citation30. Gilling P. Barber M. Anderson P et al.: WATER—A Double-Blind Randomized Controlled Trial of Aquablation vs Transurethal Resection of the Prostate in Benign Prostatic Hyperplasia. J Urol. Accepted December 29, 2017 doi 10.1016/j.juro.2017.12.065.
Back to Citation31. Christidis, D. et al. Minimally Invasive Therapies for Benign Prostatic Hypertrophy: The Rise in Minimally Invasive Surgical Therapies, Prostate International. 5, 41-46 (2017).
32. Bachmann A, Tubaro A, Barber N et al: 180-W XPS GreenLight laser vaporisation versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of a European multicenter randomised trial—the GOLIATH study. Eur Urol 2014; 65: 931.
33. Sonksen J et al. Prospective, Randomized, Multinational Study of Prostatic Urethral Lift Versus Transurethral Resection of the Prostate: 12-month Results from the BPH6 Study. Eur Urol 2015; 68:643-52.
Back to Citation34. Neschis, David G. & MD, Golden, M., “Clinical features and diagnosis of lower extremity peripheral artery disease.” Available at: https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-lower-extremity-peripheral-artery-disease.
Back to Citation35. Centers for Disease Control and Prevention, “Peripheral Arterial Disease (PAD) Fact Sheet,” 2018, Available at: https://www.cdc.gov/DHDSP/data_statistics/fact_sheets/fs_PAD.htm.
Back to Citation36. Gray W, et al. A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): a randomised, non-inferiority trial. Lancet; Published Online September 22, 2018; http://dx.doi.org/10.1016/S0140-6736(18)32262-1.
Back to Citation37. Gray W, et al. A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): a randomised, non-inferiority trial. Lancet; Published Online September 22, 2018; http://dx.doi.org/10.1016/S0140-6736(18)32262-1.
Back to Citation38. Müller-Hülsbeck, S., et al., “Long-Term Results from the MAJESTIC Trial of the Eluvia Paclitaxel-Eluting Stent for Femoropopliteal Treatment: 3-Year Follow-up,” Cardiovasc Intervent Radiol, December 2017, vol. 40(12), pp. 1832-1838.
Back to Citation39. Gray, W.A., et al., “A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): a randomised, non-inferiority trial,” Lancet, September 24, 2018.
Back to Citation40. Forrester, J.S., Fishbein, M., Helfant, R., Fagin, J., “A paradigm for restenosis based on cell biology: clues for the development of new preventive therapies,” J Am Coll Cardiol, March 1, 1991, vol. 17(3), pp. 758-69.
Back to Citation41. Gray, W.A., Keirse, K., Soga, Y., et al., “A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): A randomized, non-inferiority trial,” Lancet, 2018. Available at: http://dx.doi.org/10.1016/S0140-6736(18)32262-1.
Back to Citation42. Katsanos, K., et al., “Risk of Death Following Application of Paclitaxel-Coated Balloons and Stents in the Femoropopliteal Artery of the Leg: A Systematic Review and Meta-Analysis of Randomized Controlled Trials,” JAHA, vol. 7(24).
Back to Citation43. Cassese, S., & Byrne, R.E., “Endovascular stenting in femoropopliteal arteries,” The Lancet, 2018, vol. 392(10157), pp. 1491-1493.
Back to Citation44. Katsanos, K., Spiliopoulos, S., Kitrou, P., Krokidis, M., & Karnabatidis, D. (2018). Risk of Death Following Application of Paclitaxel‐Coated Balloons and Stents in the Femoropopliteal Artery of the Leg: A Systematic Review and Meta‐Analysis of Randomized Controlled Trials. Journal of the American Heart Association, 7(24). https://doi.org/10.1161/jaha.118.011245.
Back to Citation45. Yamaji K, Raber L, Zanchin T, et al. Ten-year clinical outcomes of first-generation drug-eluting stents: The Sirolimus-Eluting vs. Paclitaxel-Eluting Stents for Coronary Revascularization (SIRTAX) VERY LATE trial. Eur Heart J. 2016;37(45):3386-3395.
46. Ormiston JA, Charles O, Mann T, et al. Final 5-year results of the TAXUS ATLAS, TAXUS ATLAS Small Vessel, and TAXUS ATLAS Long Lesion clinical trials of the TAXUS Liberte paclitaxel-eluting stent in de-novo coronary artery lesions. Coron Artery Dis. 2013;24(1):61-68.
47. Kereiakes DJ, Cannon LA, Dauber I, et al. Long-term follow-up of the platinum chromium TAXUS Element (ION) stent: The PERSEUS Workhorse and Small Vessel trial five-year results. Catheter Cardiovasc Interv. 2015;86(6):994-1001.
48. Stone GW, Ellis SG, Colombo A, et al. Long-term safety and efficacy of paclitaxel-eluting stents final 5-year analysis from the TAXUS Clinical Trial Program. JACC Cardiovasc Interv. 2011;4(5):530-542.
Back to Citation49. 84 FR 39479.
Back to Citation50. https://www.fda.gov/medical-devices/letters-health-care-providers/august-7-2019-update-treatment-peripheral-arterial-disease-paclitaxel-coated-balloons-and-paclitaxel.
Back to Citation51. Greaser M, Ellington JK. 2014. “Ankle arthritis.” Journal of Arthritis, 3:129. doi:10.4172/2167-7921.1000129.
Back to Citation52. Punzi, Leonardo et al. 2016. “Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation.” Rheumatic & Musculoskeletal Diseases. RMD open, 2 (2), e000279. doi:10.1136/rmdopen-2016-000279.
Back to Citation53. Ibid.
Back to Citation54. Lareau, Craig R. et al. 2015.”Does autogenous bone graft work? A logistic regression analysis of data from 159 papers in the foot and ankle literature.” Foot and Ankle Surgery. 21 (3):150-59.
Back to Citation55. DiGiovanni CW, Lin SS, Baumbauer JF, et al. 2013. “Recombinant Human Platelet-Derived Growth Factor-BB and Beta-Tricalcium Phosphate (rhPDGF-BB/b-TCP): An Alternative to Autogenous Bone Graft.” J Bone Joint Surg Am., 95: 1184-92.
Back to Citation56. Herscovici, D., Scaduto, J.M. 2012. “Use of the reamer-irrigator-aspirator technique to obtain autograft for ankle and hindfoot arthrodesis.” The Journal of Bone & Joint Surgery. 94-B:75-9.
Back to Citation57. Stavrakis, AL., SooHoo, NF. 2016. “Trends in complication rates following ankle arthrodesis and total ankle replacement.” The Journal of Bone & Joint Surgery. JBJS 1453-1458.
Back to Citation58. Haubruck P, Ober J, Heller R, Miska M, Schmidmaier G, Tanner MC (2018) Complications and risk management in the use of the reaming-irrigator-aspirator (RIA) system: RIA is a safe and reliable method in harvesting autologous bone graft. PLoS ONE 13(4): e0196051.
Back to Citation59. Ibid.
Back to Citation60. Dimitriou R, Mataliotakis GI, Angoules AG, et al. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury. 2011 Sep;42 Suppl 2:S3-15.
61. See Complications and risk management in the use of the reaming-irrigator-aspirator (RIA) system: RIA is a safe and reliable method in harvesting autologous bone graft, supra.
62. See Use of the reamer-irrigator-aspirator technique to obtain autograft for ankle and hindfoot arthrodesis, supra.
Back to Citation63. Haddad SL, Berlet GC, Baumhauer JF, et al. Impact of patient age and graft type on fusion following ankle and hindfoot arthrodesis. Combined Australia & New Zealand Orthopaedic Foot & Ankle Societies Conference, Surfers Paradise, Queensland, Australia, 2019
Back to Citation64. Ibid.
Back to Citation65. Due to the timing of the application, the AUGMENT® Bone Graft cost values were calculated using the 2018 proposed rule data.
Back to Citation66. Medicare Payment Advisory Committee. June 2005 Report to the Congress. Chapter 6: Payment for pharmacy handling costs in hospital outpatient departments. Available at: http://www.medpac.gov/docs/default-source/reports/June05_ch6.pdf?sfvrsn=0.
Back to Citation67. American Hosp. Ass'n, et al. v. Azar, et al., No. 1:18-cv-2084 (D.D.C. Dec. 27, 2018).
Back to Citation68. Id. at 35 (quoting Amgen, Inc. v. Smith, 357 F.3d 103, 112 (D.C. Cir. 2004) (citations omitted)).
Back to Citation69. See May 6, 2019 Memorandum Opinion, Granting in Part Plaintiffs' Motion for a Permanent Injunction; Remanding the 2018 and 2019 OPPS Rules to HHS at 10-12.
Back to Citation70. Id. at 13.
Back to Citation71. Id. at 19.
Back to Citation72. Id. (citing Declaration of Elizabeth Richter).
Back to Citation73. 348 F. Supp. 3d 62, 81 (D.D.C. 2018) (citing to payment reductions of 0.2 percent and 2.9 percent that other decisions have recognized as being within the agency's adjustment authority for Medicare rates under the inpatient prospective payment system).
Back to Citation74. Each revenue code on the CMHC claim must have a HCPCS code and charge associated with it. We multiply each claim service line's charges by the CMHC's overall CCR from the OPSF (or statewide CCR, where the overall CCR was greater than 1) to estimate CMHC costs. Only the claims service lines containing PHP allowable HCPCS codes and PHP allowable revenue codes from the CMHC claims remaining after trimming are retained for CMHC cost determination. The costs, payments, and service units for all service lines occurring on the same service date, by the same provider, and for the same beneficiary are summed. CMHC service days must have 3 or more services provided to be assigned to CMHC APC 5853. The final geometric mean per diem cost for CMHC APC 5853 is calculated by taking the n th root of the product of n numbers, for days where 3 or more services were provided. CMHC service days with costs ±3 standard deviations from the geometric mean costs within APC 5853 are deleted and removed from modeling. The remaining PHP service days are used to calculate the final geometric mean per diem cost for each PHP APC by taking the n th root of the product of n numbers for days where 3 or more services were provided.
Back to Citation75. Each revenue code on the hospital-based PHP claim must have a HCPCS code and charge associated with it. We multiply each claim service line's charges by the hospital's department-level CCR; in CY 2020 and subsequent years, that CCR is determined by using the PHP-only revenue-code-to-cost-center crosswalk. Only the claims service lines containing PHP-allowable HCPCS codes and PHP-allowable revenue codes from the hospital-based PHP claims remaining after trimming are retained for hospital-based PHP cost determination. The costs, payments, and service units for all service lines occurring on the same service date, by the same provider, and for the same beneficiary are summed. Hospital-based PHP service days must have 3 or more services provided to be assigned to hospital-based PHP APC 5863. The final geometric mean per diem cost for hospital-based PHP APC 5863 is calculated by taking the n th root of the product of n numbers, for days where 3 or more services were provided. Hospital-based PHP service days with costs ±3 standard deviations from the geometric mean costs within APC 5863 are deleted and removed from modeling. The remaining hospital-based PHP service days are used to calculate the final geometric mean per diem cost for hospital-based PHP APC 5863.
Back to Citation76. Public Law 114-74.
Back to Citation77. As discussed in section II.A. of this CY 2020 OPPS/ASC final rule, final OPPS APC geometric mean per diem costs (including final PHP APC geometric mean per diem costs) are divided by the final geometric mean per diem costs for APC 5012 (Clinic Visits and Related Services) to calculate each PHP APC's unscaled relative payment weight. An unscaled relative payment weight is one that is not yet adjusted for budget neutrality. Budget neutrality is required under section 1833(t)(9)(B) of the Act, and ensures that the estimated aggregate weight under the OPPS for a calendar year is neither greater than nor less than the estimated aggregate weight that would have been made without the changes. To adjust for budget neutrality (that is, to scale the weights), we compare the estimated aggregated weight using the scaled relative payment weights from the previous calendar year at issue. We refer readers to the ratesetting procedures described in Part 2 of the OPPS Claims Accounting narrative and in section II. of this final rule for more information on scaling the weights, and for details on the final steps of the process that leads to final PHP APC per diem payment rates. The OPPS Claims Accounting narrative is available on the CMS website at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Hospital-Outpatient-Regulations-and-Notices.html.
Back to Citation78. Available at: https://www.ssa.gov/OP_Home/ssact/title18/1833.htm.
Back to Citation79. American Hospital Ass'n, et al. v. Azar, No. 1:18-cv-02841-RMC (D.D.C. Sept. 17, 2019).
Back to Citation80. Medicare Payment Advisory Committee. March 2019 Report to the Congress. Chapter 5: Ambulatory surgical center services. Available at: http://www.medpac.gov/docs/default-source/reports/mar19_medpac_ch5_sec.pdf?sfvrsn=0.
Back to Citation81. Medicare Payment Advisory Committee. March 2019 Report to the Congress. Chapter 5: Ambulatory surgical center services. Available at: http://www.medpac.gov/docs/default-source/reports/mar19_medpac_ch5_sec.pdf?sfvrsn=0.
Back to Citation82. We initially referred to this process as “retirement” of a measure in the 2010 OPPS/ASC proposed rule, but later changed it to “removal” during final rulemaking.
Back to Citation83. We refer readers to the CY 2013 OPPS/ASC final rule with comment period (77 FR 68472 through 68473) for a discussion of our reasons for changing the term “retirement” to “removal” in the Hospital OQR Program.
Back to Citation84. We note that we previously referred to these factors as “criteria” (for example, 77 FR 68472 through 68473); we now use the term “factors” in order to align the Hospital OQR Program terminology with the terminology we use in other CMS quality reporting and pay-for-performance (value-based purchasing) programs.
Back to Citation85. 80 FR 70508.
Back to Citation86. National Quality Forum. NQF #1822 External Beam Radiotherapy for Bone Metastases. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=70374.
Back to Citation87. QualityNet. 2018 EBRT Measure Information Form. Available at: https://www.qualitynet.org/dcs/ContentServer?cid=1228774479863&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
Back to Citation88. See language about measure steward no longer maintaining this measure in the FY 2020 IPPS/LTCH PPS proposed rule at 84 FR 19502 through 19503.
Back to Citation89. ASCQR Specifications Manual, discussing these measures, available at: http://qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1228772475754.
Back to Citation90. Centers for Medicare & Medicaid Services. Meaningful Measures Hub. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/MMF/General-info-Sub-Page.html.
Back to Citation91. National Quality Forum. 0265 All-Cause Hospital Transfer/Admission. Available at: http://www.qualityforum.org/QPS/0265.
Back to Citation92. National Quality Forum. 0263 Patient Burn. Available at: http://www.qualityforum.org/QPS/0263.
Back to Citation93. National Quality Forum. 0267 Wrong Site, Wrong Side, Wrong Patient, Wrong Procedure, Wrong Implant. Available at: http://www.qualityforum.org/QPS/0267.
Back to Citation94. National Quality Forum. 0266 Patient Fall. Available at: http://www.qualityforum.org/QPS/0266.
Back to Citation95. ASC Quality Collaboration. Quality measures developed and tested by the ASC Quality Collaboration. Available at: http://ascquality.org/documents/2019-Summary-ASC-QC-Measures.pdf.
Back to Citation96. National Quality Forum. Serious Reportable Events in Healthcare 2006 Update. Washington, DC: NQF, 2007. Available at: https://www.qualityforum.org/Publications/2007/03/Serious_Reportable_Events_in_Healthcare%E2%80%932006_Update.aspx.
Back to Citation97. ECRI Institute. New clinical guide to surgical fire prevention. Health Devices 2009 Oct;38(10):314-32.
98. 170. National Fire Protection Association (NFPA). NFPA 99: Standard for health care facilities. Quincy (MA): NFPA; 2005.
Back to Citation99. ASC Quality Collaboration. Quality measures developed and tested by the ASC Quality Collaboration. Available at: http://ascquality.org/documents/2019-Summary-ASC-QC-Measures.pdf.
Back to Citation100. National Quality Forum. Serious Reportable Events in Healthcare—2006 Update: A Consensus Report. March 2007. Available at: https://www.qualityforum.org/Publications/2007/03/Serious_Reportable_Events_in_Healthcare%E2%80%932006_Update.aspx.
Back to Citation101. Boushon B, Nielsen G, Quigley P, Rutherford P, Taylor J, Shannon D. Transforming Care at the Bedside How-to Guide: Reducing Patient Injuries from Falls. Cambridge, MA: Institute for Healthcare Improvement; 2008.
Back to Citation102. ASC Quality Collaboration. Quality measures developed and tested by the ASC Quality Collaboration. Available at: http://ascquality.org/documents/2019-Summary-ASC-QC-Measures.pdf.
Back to Citation103. National Quality Forum. Serious Reportable Events in Healthcare—2006 Update: A Consensus Report. March 2007. Available at: https://www.qualityforum.org/Publications/2007/03/Serious_Reportable_Events_in_Healthcare%E2%80%932006_Update.aspx.
Back to Citation104. American College of Obstetricians and Gynecologists. ACOG committee opinion #464: patient safety in the surgical environment. Obstet Gynecol. 2010;116(3):786-790.
Back to Citation105. ASC Quality Collaboration. Quality measures developed and tested by the ASC Quality Collaboration. Available at: http://ascquality.org/documents/2019-Summary-ASC-QC-Measures.pdf.
Back to Citation106. Coley KC, Williams BA, DaPos SV, Chen C, Smith RB. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. J Clin Anesth. 2002 Aug; 14(5):349-53.
107. Junger A, Klasen J, Benson M, Sciuk G, Hartmann B, Sticher J, Hempelmann G. Factors determining length of stay of surgical day-case patients. Eur J Anaesthesiol. 2001 May;18(5):314-21.
Back to Citation108. ASCQR Specifications Manuals are available at https://www.qualitynet.org/asc/specifications-manuals.
Back to Citation109. We note that we previously referred to these factors as “criteria” (for example, 79 FR 66967 through 66969); we now use the term “factors” in order to align the ASCQR Program terminology with the terminology we use in other CMS quality reporting and pay-for-performance (value-based purchasing) programs.
Back to Citation110. Cullen KA, Hall MJ, Golosinskiy A, Statistics NCfH. Ambulatory surgery in the United States, 2006. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2009.
111. Medicare Payment Advisory Committee. Report for the Congress: Medicare Payment Policy, March 2019. http://medpac.gov/docs/default-source/reports/mar19_medpac_entirereport_sec.pdf?sfvrsn=0. Accessed May 24, 2019.
Back to Citation112. Coley KC, Williams BA, DaPos SV, Chen C, Smith RB. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. Journal of clinical anesthesia. 2002;14(5):349-353.
113. Bain J, Kelly H, Snadden D, Staines H. Day surgery in Scotland: Patient satisfaction and outcomes. Quality in Health Care. 1999;8(2):86-91.
Back to Citation114. Majholm BB. Is day surgery safe? A Danish multicentre study of morbidity after 57,709 day surgery procedures. Acta anaesthesiologica Scandinavica. 2012;56(3):323-331.
115. Whippey A, Kostandoff G, Paul J, Ma J, Thabane L, Ma HK. Predictors of unanticipated admission following ambulatory surgery: A retrospective case-control study. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2013;60(7):675-683.
116. Fleisher LA, Pasternak LR, Herbert R, Anderson GF. Inpatient hospital admission and death after outpatient surgery in elderly patients: Importance of patient and system characteristics and location of care. Arch Surg. 2004;139(1):67-72.
117. Coley KC, Williams BA, DaPos SV, Chen C, Smith RB. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. Journal of clinical anesthesia. 2002;14(5):349-353.
118. Hollingsworth JMJM. Surgical quality among Medicare beneficiaries undergoing outpatient urological surgery. The Journal of urology. 2012;188(4):1274-1278.
119. Bain J, Kelly H, Snadden D, Staines H. Day surgery in Scotland: Patient satisfaction and outcomes. Quality in Health Care. 1999;8(2):86-91.
120. Fortier J, Chung F, Su J. Unanticipated admission after ambulatory surgery—a prospective study. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 1998;45(7):612-619.
121. Aldwinckle R, Montgomery J. Unplanned admission rates and postdischarge complications in patients over the age of 70 following day case surgery. Anaesthesia. 2004;59(1):57-59.
Back to Citation122. Coley KC, Williams BA, DaPos SV, Chen C, Smith RB. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. Journal of clinical anesthesia. 2002;14(5):349-353.
123. Hollingsworth JMJM. Surgical quality among Medicare beneficiaries undergoing outpatient urological surgery. The Journal of urology. 2012;188(4):1274-1278.
124. Baugh RR. Safety of outpatient surgery for obstructive sleep apnea. Otolaryngology—head and neck surgery. 2013;148(5):867-872.
125. Bhattacharyya N. Ambulatory sinus and nasal surgery in the United States: Demographics and perioperative outcomes. The Laryngoscope. 2010;120(3):635-638.
126. Bhattacharyya NN. Unplanned revisits and readmissions after ambulatory sinonasal surgery. The Laryngoscope. 2014;124(9):1983-1987.
127. Bhattacharyya NN. Revisits and postoperative hemorrhage after adult tonsillectomy. The Laryngoscope. 2014;124(7):1554-1556.
128. Hansen DG, Abbott LE, Johnson RM, Fox JP. Variation in hospital-based acute care within 30 days of outpatient plastic surgery. Plastic and reconstructive surgery (1963). 2014;134(3):370e-378e.
129. Mahboubi HH. Ambulatory laryngopharyngeal surgery: Evaluation of the national survey of ambulatory surgery. JAMA otolaryngology— head & neck surgery. 2013;139(1):28-31.
130. Orosco RKRK. Ambulatory thyroidectomy: A multistate study of revisits and complications. Otolaryngology—head and neck surgery. 2015;152(6):1017-1023.
Back to Citation131. Baugh RR. Safety of outpatient surgery for obstructive sleep apnea. Otolaryngology—head and neck surgery. 2013;148(5):867-872.
132. Bhattacharyya N. Ambulatory sinus and nasal surgery in the United States: Demographics and perioperative outcomes. The Laryngoscope. 2010;120(3):635-638.
133. Bhattacharyya NN. Unplanned revisits and readmissions after ambulatory sinonasal surgery. The Laryngoscope. 2014;124(9):1983-1987.
134. Bhattacharyya NN. Revisits and postoperative hemorrhage after adult tonsillectomy. The Laryngoscope. 2014;124(7):1554-1556.
135. Hansen DG, Abbott LE, Johnson RM, Fox JP. Variation in hospital-based acute care within 30 days of outpatient plastic surgery. Plastic and reconstructive surgery (1963). 2014;134(3):370e-378e.
136. Mahboubi HH. Ambulatory laryngopharyngeal surgery: Evaluation of the national survey of ambulatory surgery. JAMA otolaryngology— head & neck surgery. 2013;139(1):28-31.
137. Menachemi. Quality of care differs by patient characteristics: Outcome disparities after ambulatory surgical procedures. American journal of medical quality. 2007;22(6):395-401.
138. Orosco RKRK. Ambulatory thyroidectomy: A multistate study of revisits and complications. Otolaryngology—head and neck surgery. 2015;152(6):1017-1023.
Back to Citation139. 83 FR 58820 through 58822.
Back to Citation140. National Quality Forum. List of Measures under Consideration for December 1, 2017. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=86526.
Back to Citation141. National Quality Forum. MAP 2018 Considerations for Implementing Measures: Hospitals—Final Report. Available at: http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=87096.
Back to Citation142. Ibid.
Back to Citation143. Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33(1):159-174.
Back to Citation144. National Quality Forum. Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers. Available at: http://www.qualityforum.org/QPS/3357.
Back to Citation145. National Quality Forum. “MAP 2018 Considerations for Implementing Measures in Federal Programs: Hospitals.” Report. 2017. Available at: http://www.qualityforum.org/map/ under “Hospitals—Final Report.”
Back to Citation146. The Centers for Medicare and Medicaid Services Center for Clinical Standards and Quality. “2018 Measures under Consideration List: Program-Specific Measure Needs and Priorities”. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/Downloads/2018-CMS-Measurement-Priorities-and-Needs.pdf. Accessed February 28, 2019.
Back to Citation147. Fleisher LA, Pasternak LR, Herbert R, Anderson GF. Inpatient hospital admission and death after outpatient surgery in elderly patients: importance of patient and system characteristics and location of care. Arch Surg. 2004;139(1):67-72.
148. Mattila K, Toivonen J, Janhunen L, Rosenberg PH, Hynynen M. Postdischarge symptoms after ambulatory surgery: First-week incidence, intensity, and risk factors. Anesthesia and analgesia. 2005;101(6):1643-1650.
Back to Citation149. Krumholz HM, Brindis RG, Brush JE, et al. Standards for Statistical Models Used for Public Reporting of Health Outcomes An American Heart Association Scientific Statement From the Quality of Care and Outcomes Research Interdisciplinary Writing Group: Cosponsored by the Council on Epidemiology and Prevention and the Stroke Council Endorsed by the American College of Cardiology Foundation. Circulation. 2006;113(3):456-462.
150. Normand S-LT, Shahian DM. Statistical and clinical aspects of hospital outcomes profiling. Statistical Science. 2007;22(2):206-226.
151. National Quality Forum. Measure Evaluation Criteria and Guidance for Evaluating Measures for Endorsement. 2015. Available at: http://www.qualityforum.org/Measuring_Performance/Submitting_Standards/2015_Measure_Evaluation_Criteria.aspx. Accessed July 26, 2016.
Back to Citation152. Centers for Medicare and Medicaid Services. “Ambulatory Surgical Center (ASC) Payment: Addenda Updates.” Available at: https://www.cms.gov/medicare/medicare-fee-for-service-payment/ascpayment/11_addenda_updates.html.
Back to Citation153. Ibid.
Back to Citation154. Healthcare Cost and Utilization Project. Clinical Classifications Software for Services and Procedures. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp.
Back to Citation155. S. Coberly. The Basics; Relative Value Units (RVUs). National Health Policy Forum. January 12, 2015. Available at: http://www.nhpf.org/library/the-basics/Basics_RVUs_01-12-15.pdf.
Back to Citation156. Hosmer DW, Lemeshow S. Introduction to the logistic regression model. Applied Logistic Regression, Second Edition. 2000:1-30.
Back to Citation157. Hosmer DW, Lemeshow S. Introduction to the logistic regression model. Applied Logistic Regression, Second Edition. 2000:1-30.
Back to Citation158. Ibid.
Back to Citation159. Snijders TA, Bosker RJ. Multilevel Analysis: An introduction to basic and advanced multilevel modeling. SAGE Publications. 2000. London.
Back to Citation160. Centers for Medicare & Medicaid Services. (2017). 2017 Measure Technical Report: Facility-Level 7-Day Hospital Visits after General Surgery Procedures Performed at Ambulatory Surgical Centers. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
Back to Citation161. Medicare Learning Network. (2018) Global Surgery Booklet: United States, 2017. Retrieved from Centers for Medicare & Medicaid Services website: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/GloballSurgery-ICN907166.pdf.
Back to Citation162. Horwitz, L.I., Grady, J.N., Cohen, D.B., Lin, Z., Volpe, M., Ngo, C.K., . . . Bernheim, S.M. (2015). Development and Validation of an Algorithm to Identify Planned Readmissions From Claims Data. Journal of hospital medicine, 10 (10), 670-677. doi:10.1002/jhm.2416.
Back to Citation163. National Quality Forum. (2017). Surgery, Fall 2017 Cycle: CDP Report, 2017. Retrieved from https://www.qualityforum.org/Publications/2018/08/Surgery_Final_Report_-_Fall_2017_Cycle.aspx.
Back to Citation164. ASC Quality Collaboration. ASC Quality Measures Implementation Guide Version 6.1 March 2019. Available at: http://ascquality.org/documents/ASC-QC-Implementation-Guide-6.1-March-2019.pdf.
Back to Citation165. Ibid.
Back to Citation166. Ibid.
Back to Citation167. https://www.srtr.org/about-srtr/mission-vision-and-values/.
Back to Citation168. Medicare Benefit Policy Manual. Internet Only. Publication 100-02, Chapter 16, § 120.
Back to Citation169. The data reviewed are maintained in the CMS Integrated Data Repository (IDR). The IDR is a high-volume data warehouse integrating Medicare Parts A, B, C, and D, and DME claims, beneficiary and provider data sources, along with ancillary data such as contract information and risk scores. Additional information is available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/IDR/index.html.
Back to Citation170. The 5.8 percent average increase per year in overall health care spending was arrived at using data publicly available on the Bureau of Labor and Statistics web page, located at: https://www.bls.gov/cpi/factsheets/medical-care.htm.
Back to Citation171. 80 FR 81674 (December 30, 2015).
Back to Citation172. AHA et al. v. Azar, No. 18-CV-2841, at *25 (D.D.C. Sept. 17, 2019).
Back to Citation173. AHA et al. v. Azar, No. 18-CV-2841, at *25 (D.D.C. Sept. 17, 2019). [Do we want to mention the motion to modify?]
Back to Citation174. Occupational Employment and Wages, May 2018. Available at: https://www.bls.gov/ooh/healthcare/medical-records-and-health-information-technicians.htm. Accessed May 7, 2019.
Back to CitationBILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
[FR Doc. 2019-24138 Filed 11-1-19; 4:15 pm]
BILLING CODE 4120-01-P
